Académique Documents
Professionnel Documents
Culture Documents
Chronic Kidney Disease PDF
Transféré par
Georich NarcisoTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Chronic Kidney Disease PDF
Transféré par
Georich NarcisoDroits d'auteur :
Formats disponibles
jslum.
com | Medicine
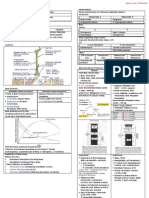
Chronic Ki dney Disease
Definition Processes Pr omoting Progressive Kidney Failure
Kidney damage 3 months Partial Loss of
Structural, Functional abnormalities of kidney Function
With/ without GFR
Manifest by Fibrosis Compensatory Renin AII Afferent
Pathological abnormalities apoptosis Growth Activation vasodilation
Markers of Kidney Damage
(including abnormal composition of Blood, Urine, imaging studies) Release of Wall Tension Systemic Glomerular
GFR < 60mL/min/1.73 m2 for 3 months, with/ without Kidney Damage Cytokines, Hypertension hypertension
Process of continuing significant Irreversible in Nephron number Growth Factors
Corresponds to CKD stages 3-5
End-Stage Renal Disease (ESRD) Capillary Injury Proteinuria
CKD + Uremic Syndrome = Stage 5 CKD
Angiotensin II in Promoting Progressive CKD
Markers of Kidney Damage Release of
Pathological Abnormalities Abnormal Blood, Urine Cytokines
Growth Factors
Kidney stones Hypokalaemia (RTA)
Polycystic kidneys Urine Haematruia, Proteinuria
Protein Filtration Angiotensin II Hyperplasia
Hydronephrosis
Hypertrophy
Stages of Chronic Kidney Disease Systemic, Glomerular
1 2 3 4 5 Hypertension
GFR (mL/min/1.73m2) > 90 60-89 30-59 15-29 < 15
CRF CRF ESRF Declining Renal Function & Development of Uraemic Symptoms
Estimation of GFR
Inulin, 125I-Iothalamate, 99mTc-DTPA, Iohe xol, 51Cr-EDTA
24-hour clearance, Serum Ceratinine
Adult Children
MDRD Study Schwartz Formula
Cockcroft-Gault Formula Counahan-Barratt Equations
Causes of Chroni c Renal Failure
Diabetes Mellitus
DM Nephropathy
(Microvascular complication)
(eg. Glomerular damage, Arteriolosclerosis, Pyelonephritis)
Hypertension Development of Uraemic symptoms
Hyaline, Arteriolosclerosis as Serum Creatinine with Renal Function
(eg. Ischaemia, Fibrosis, Glomerular Damage) Approximately 50% of Glomerular Filtration is lost,
Polycystic Disease before Serum Creatinine exceeds the upper-limit of Nor mal
Glomerulonephritis
Toxic Nephropathy Detection of Chronic Ki dney Disease
Obstructive Nephropathy Urine Examination
SLE Microalbuminuria, Proteinuria, Red Blood Cell, White Blood Cell, Casts
Blood Examination
1 Renal Disease in Paediatric eGFR calculation using Cockcroft-Gault, MDRD formula
Kidney Biopsy
Unknown (47.2%)
Kidney Imaging
Glomerulonephritis (21.9%)
Ultrasound
Focal Segmental Glomerulosclerosis (FSGS) (7.5%)
Reflux Nep hropathy (4.3%)
Clinical Features
SLE (6.1%)
Anaemia
Obstructive Uropathy (4.9%)
Pallor, Lethargy, Breathlessness on exercise
Renal Dysplasia (2.4%)
Platelet Abnormality
Hereditary Nephritis (2.2%) Epistaxis, Bruising
Cystic Kidney Disease (1.6%) Skin
Drug Induced Nephropathy (1.0%) Pigmentation, Pruritus
Metabolic (0.1%) GI Tract
Anorexia, Nausea, Vomiting, Diarrhoea
Pathophysiol ogy Endocrine / Gonads
Intraglomerular Hypertension, Glomerular Hypertrophy Amenorrhoea, Erectile impotence, Infertility
Compensatory response to Nephron loss in attempt to maintain total GFR Polyneuropathy
1 Renal Vasodilatation, occurs in Diabetes Mellitus, leading to Hyperfiltration CNS
Compensatory Adaptation Confusi on, Coma, Fits (severe uraemia)
(to in permeability of glomerular capillary wall to small solutes, water) CVS
Intraglomerular Pressure (to minimize GFR) Uraemic Pericarditis, Hypertension, Peripheral Vascular Disease, Heart Failure
Mediated by flow to Macula Densa Renal
Activation of Tubuloglomerular Feedback Nocturia, Polyuria, Salt & Water Retention, Edema
Renal Osteodystrophy
Other 2 Causes Osteomalacia, Muscle Weakness, Bone Pain, Hyperparathyroidism,
Proteinuria Osteosclerosis
Podocyte Injury/ loss
Tubulointerstitial disease (Fibrosis) Laboratory Results
Calcium Phosp hate deposition Creatinine > 100 umol/L
Metabolic acidosis Glomerular Filtration Rate (GFR/ Creatinine Clearance) < 60ml/min/1.73m2
Hyperlipidaemia
jslum.com | Medicine
Complications Renal Replacement Therapy
Fluid, Electrolyte Dialysis
Fluid Retention, Hyperkalemia, Hyperphosphatemia Haemodialysis Peritoneal Dialysis
Endocrine Metaboli c Continuous Ambulatory Peritoneal Dialysis (CAPD)
Metabolic Acidosis, Renal Osteodystrophy Continuous Cyclic Peritoneal Dialysis (CCPD)
Neuromuscular Criteria
Fatigue, Drowsiness, Asterixis, Muscle Cramps, Myopathy Presence of Uremic Symptoms
Hematologic, Immunologic Hyperkalaemia
Anaemia, Bleeding, Susceptible to Infection Persistent Extracellular Volume Expansion
Cardiovascular, Pulmonary Creatinine Clearance/ Estimated GFR < 10mL/min/1.73m2
Uraemic Pericarditis, Renovascular Hypertension Acidosis
Dermatologic Bleeding Diathesis
Hyperpigmentation (due to Urobilin) Choosi ng Type of Dialysis (Psychosocial Factors)
Pruritus Preference, Motivation
Gastrointestinal Body Image (young adults)
Anorexia, Nausea & Vomiting, Gastroenteritis, PUD, Peritonitis Occupation
Anaemia, Malnutrition, Bone Growth Economi c considerations
Home, Workplace Environment
Management Family Support
Complication Management Distance from nearest HD center
Anaemia Erythropoietin
IV Ferritin
Renal Bone Disease Phosphate Binder
Vitamin D
Hypertension Strict BP Control < 130/80
ACEI / ARB < 125/75
Diabetes Strict Glycaemic Control (HbA1c < 7%)
Fluid Overload Salt, Water Restriction
Dose Loop Diuretics
Estimating Time to Kidney Failure
Renal Transplantation
Treatment of choice (for advanced chronic renal failure) Best quality of Life
Transplant centres in Malaysia
KL Hospital
HUKM
UMMC
Selayang Hospital
Recipient Selection
Thorough Risk-Versus-Bene fit Evaluation
Donors
Deceased
Volunteer Living Donors
Benefits
Better quality of Life, Survival
Contraindications
Elderly age group (> 65 y/o)
HIV Infection, Diabetes with MOF, Psychosis, Malignancy, Severe CVD,
Chronic Active Hepatitis, Cirrhosis
Active Substance Abuse
Complications
Rejection
Infections
HPT
Post-Transplant DM
Immuno-sup pressive agents side effects (eg. Cancer)
Vous aimerez peut-être aussi
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Pathology of Thyroid DiseasesDocument5 pagesPathology of Thyroid DiseasesGerardLum100% (2)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Posterior Pituitary SyndromeDocument1 pagePosterior Pituitary SyndromeGerardLumPas encore d'évaluation
- Soft Tissue InfectionsDocument3 pagesSoft Tissue InfectionsGerardLum100% (1)
- Pathogenesis Chronic Complications DiabetesDocument5 pagesPathogenesis Chronic Complications DiabetesGerardLum100% (1)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Pathophysiology of Calcium, Phosphate HomeostasisDocument5 pagesPathophysiology of Calcium, Phosphate HomeostasisGerardLum100% (1)
- Pituitary DysfunctionDocument2 pagesPituitary DysfunctionGerardLum0% (1)
- Pathology of DiabetesDocument4 pagesPathology of DiabetesGerardLum100% (4)
- Soft Tissue TumoursDocument8 pagesSoft Tissue TumoursGerardLum100% (2)
- Prostate GlandsDocument3 pagesProstate GlandsDragan PetrovicPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Pathology GlomerulonephritisDocument4 pagesPathology GlomerulonephritisGerardLum100% (2)
- Sexually Transmitted DiseasesDocument6 pagesSexually Transmitted DiseasesGerardLum100% (3)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Pathology of TestesDocument4 pagesPathology of TestesGerardLum100% (1)
- Obstructive UropathyDocument3 pagesObstructive UropathyGerardLum100% (1)
- Urinary Tract Infections in ChildrenDocument1 pageUrinary Tract Infections in ChildrenGerardLumPas encore d'évaluation
- Pathophysiology of Nerve InjuryDocument2 pagesPathophysiology of Nerve InjuryGerardLum100% (1)
- ThalassaemiaDocument4 pagesThalassaemiaGerardLum100% (4)
- Diet Plan of Different DiseasesDocument43 pagesDiet Plan of Different DiseasesSanaPas encore d'évaluation
- Urinary Tract InfectionDocument4 pagesUrinary Tract InfectionGerardLum100% (2)
- Nejmra 2100152Document10 pagesNejmra 2100152Ricardo CastañedaPas encore d'évaluation
- Renal Excretion of DrugsDocument3 pagesRenal Excretion of DrugsGerardLum100% (3)
- Pituitary Gland PathologyDocument4 pagesPituitary Gland PathologyGerardLumPas encore d'évaluation
- Paediatrics OrthopaedicsDocument5 pagesPaediatrics OrthopaedicsGerardLumPas encore d'évaluation
- Chronic Kidney DiseaseDocument15 pagesChronic Kidney Diseaseapi-270623039Pas encore d'évaluation
- Pathogenesis Bleeding DisordersDocument4 pagesPathogenesis Bleeding DisordersGerardLumPas encore d'évaluation
- Fresenius 5008 Hemodialysis System - User ManualDocument328 pagesFresenius 5008 Hemodialysis System - User ManualCarl Azzopardi100% (6)
- ThrombophiliaDocument3 pagesThrombophiliaGerardLum100% (1)
- Acute Renal FailureDocument13 pagesAcute Renal FailureGlorianne Palor100% (2)
- Indian School of Business: January 31, 2019Document23 pagesIndian School of Business: January 31, 2019Sarvesh KashyapPas encore d'évaluation
- Contoh Jurnal Meta AnalisisDocument17 pagesContoh Jurnal Meta AnalisisMia Audina Miyanoshita100% (1)
- Vesico Ureteral RefluxDocument1 pageVesico Ureteral RefluxGerardLumPas encore d'évaluation
- Renal Function in Disease StateDocument2 pagesRenal Function in Disease Statedamai140390Pas encore d'évaluation
- Thyroid PhysiologyDocument2 pagesThyroid PhysiologyGerardLum100% (2)
- Skeletal Muscle RelaxantsDocument1 pageSkeletal Muscle RelaxantsGerardLum100% (2)
- Principles of Blood TransfusionDocument2 pagesPrinciples of Blood TransfusionGerardLum100% (3)
- Overview of AnaemiaDocument2 pagesOverview of AnaemiaGerardLumPas encore d'évaluation
- Nocturnal EnuresisDocument1 pageNocturnal EnuresisGerardLumPas encore d'évaluation
- Nsaids DrugsDocument2 pagesNsaids DrugsIrene Zae MwandotoPas encore d'évaluation
- Health-Related Quality of Life in Patients On Hemodialysis and Peritoneal DialysisDocument8 pagesHealth-Related Quality of Life in Patients On Hemodialysis and Peritoneal DialysislamyaaPas encore d'évaluation
- Mba Final Project PresentationDocument34 pagesMba Final Project PresentationabijithPas encore d'évaluation
- Kajian Ilmiah CKD KDIGO 2012Document27 pagesKajian Ilmiah CKD KDIGO 2012giggs_libraPas encore d'évaluation
- Nutrition equations and calorie requirementsDocument1 pageNutrition equations and calorie requirementsDorel PlantusPas encore d'évaluation
- HCEN4966 2 AK96 Advance LowDocument2 pagesHCEN4966 2 AK96 Advance LowBuket Ozay Çakir100% (1)
- Haemodialysis Access UKDocument19 pagesHaemodialysis Access UKmadimadi11Pas encore d'évaluation
- Cell Membrane Experiment ObservationsDocument25 pagesCell Membrane Experiment ObservationsAngela MagnoPas encore d'évaluation
- BR - Multifiltrate FreseniusDocument16 pagesBR - Multifiltrate FreseniusLeonardo Jose HernandezPas encore d'évaluation
- Biomedical Technology Lecture Notes 2015Document11 pagesBiomedical Technology Lecture Notes 2015Phi NguyenPas encore d'évaluation
- Anemia in CKDDocument9 pagesAnemia in CKDM. Ryan RamadhanPas encore d'évaluation
- BiBag OperacaoDocument20 pagesBiBag OperacaoJoséPas encore d'évaluation
- Diacap-Pro B Braun Broshure PDFDocument2 pagesDiacap-Pro B Braun Broshure PDFLeonardo Jose HernandezPas encore d'évaluation
- Contrast Induced NephropathyDocument25 pagesContrast Induced NephropathyXin Yee TanPas encore d'évaluation
- 2008 K Hemodialysis System: Technician'S ManualDocument49 pages2008 K Hemodialysis System: Technician'S ManualokboPas encore d'évaluation
- Implications of The CANUSA Study PDFDocument6 pagesImplications of The CANUSA Study PDFCarlos Navarro YslaPas encore d'évaluation
- Chronic Kidney Disease: Diagnosis and TherapyDocument21 pagesChronic Kidney Disease: Diagnosis and TherapyLindsPas encore d'évaluation
- Science MODEL TEST PAPER FOR SUMMATIVE ASSESSMENT - 2Document10 pagesScience MODEL TEST PAPER FOR SUMMATIVE ASSESSMENT - 2Apex InstitutePas encore d'évaluation
- Diagnovision Products CorporationDocument25 pagesDiagnovision Products CorporationkprakxPas encore d'évaluation
- PRIO Lemus Acute Pain and Risk For Def. Fluid VolumeDocument3 pagesPRIO Lemus Acute Pain and Risk For Def. Fluid VolumeChe ValenzuelaPas encore d'évaluation
- Biology ProjectDocument7 pagesBiology ProjectRayyan Malik0% (1)
- THE EFFECTIVENESS OF INTRADIALYSIS STATIC BIKE EXERCISE TOWARD FUNCTIONAL CAPACITY IN HEMODIALYSIS PATIENTS OkeeDocument5 pagesTHE EFFECTIVENESS OF INTRADIALYSIS STATIC BIKE EXERCISE TOWARD FUNCTIONAL CAPACITY IN HEMODIALYSIS PATIENTS OkeeriadesnitaPas encore d'évaluation
- NxStage Neph Driver Survey - 18MAR2019 - ProgrammingDocument26 pagesNxStage Neph Driver Survey - 18MAR2019 - ProgrammingKapil BajajPas encore d'évaluation
- General Policy StatementDocument6 pagesGeneral Policy StatementCynthia RinosPas encore d'évaluation