Académique Documents
Professionnel Documents
Culture Documents
Ok 2
Transféré par
laudyaFebTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Ok 2
Transféré par
laudyaFebDroits d'auteur :
Formats disponibles
1040-5488/14/9112-e301/0 VOL. 91, NO. 12, PP.
e301Ye304
OPTOMETRY AND VISION SCIENCE
Copyright * 2014 American Academy of Optometry
CLINICAL CASE
Severe Primary Ocular Surface Involvement
in Behcet Disease
Jun Zeng* and Baihua Chen
ABSTRACT
Purpose. Behcet disease (BD) is a chronic, relapsing inflammatory disorder of unknown etiology characterized by ob-
structive vasculitis. Ocular surface involvement is a less frequent anterior segment finding. We report a patient with BD
whose ocular presentation was severe surface involvement.
Case Report. A 26-year-old Chinese woman, who was diagnosed as having BD by a dermatologist because of oral and
genital ulceration and erythema nodosum in the upper extremities 1 month ago, presented with dry eye syndrome, corneal
ulceration, and conjunctival lesions. Both clinical and confocal microscope examination revealed bilateral severe in-
flammatory ocular surface disease. However, she did not have the common clinical ocular manifestations such as
iridocyclitis, vitritis, retinal perivasculitis, or retinitis for BD. In addition to oral methylprednisolone and thalidomide, topical
1% prednisolone acetate ophthalmic suspension, tacrolimus ophthalmic suspension, and artificial tears were used. We
observed for the first time histopathological changes of the eyelid in BD by confocal microscopy.
Conclusions. Ocular surface lesions should be noted as an uncommon but possible manifestation of BD. Such severe
ocular surface lesions without uveitis require a thorough medical history, dermatological examination, and serological
testing to arrive at a diagnosis of BD. Accordingly, routine examination of the ocular surface is recommended in patients
with BD, and BD should be included in a list of differential diagnoses for patients with ocular surface lesions.
(Optom Vis Sci 2014;91:e301Ye304)
Key Words: Behcet disease, ocular surface, dry eye
B
ehcet disease (BD) is a chronic, recurrent, multisystemic edema, cystoid macular degeneration, venous or arterial occlusion,
inflammatory disorder of unknown etiology, characterized disc edema, and retinal detachment.3 Despite the wide range of
by the presence of oral ulceration plus any two of the fol- ocular involvement in BD, isolated ocular surface involvement in
lowing: genital ulceration, typical defined ocular lesions, typical BD has been described in only a few reports6Y13 and it is difficult
defined skin lesions, or a positive pathergy test.1 Behcet disease is a to diagnose for an eye care practitioner. We herein report a case of
systemic vasculitis of small and large vessels affecting both veins BD with severe ocular surface involvement, occurring in a young
and arteries. The underlying pathology shows a nonspecific in- Chinese woman. We also observed the histopathological changes
flammatory process of blood vessels.2 It occurs more frequently of the eyelid in BD by Heidelberg confocal microscopy. Our
from eastern Asia to the Mediterranean basin, mainly between 18- objective is to emphasize this rare condition and to discuss possible
and 40-year-old men.3 HLA-B51 is the most strongly associated mechanisms of ocular surface involvement.
known genetic factor to BD.4 Ocular manifestations are consid-
ered among the major criteria for the diagnosis of BD, occurring
in 50 to 70% of the patients with BD.5 Ocular impairment is CASE REPORT
frequent and severe with a variety of ocular lesions reported in-
A 26-year-old Chinese woman presented in October 11, 2012,
cluding anterior uveitis, cataract, glaucoma, posterior segment
complaining of severe foreign body sensation, dryness, irritation,
involvement with vasculitis, vitritis, retinitis, panuveitis, retinal
and photophobia in both eyes for 1 month. Because of a history of
severe oral and genital ulceration and erythema nodosum in the
upper extremities during the past 1 month, she had been diag-
*PhD
MD, PhD nosed as having BD based on the clinical findings by a derma-
Department of Ophthalmology, The Second Xiangya Hospital, Central South tologist and had taken oral methylprednisolone 40 mg daily
University, Changsha, Hunan Province, China (both authors). and thalidomide 25 mg daily as directed by the dermatologist.
Optometry and Vision Science, Vol. 91, No. 12, December 2014
Copyright American Academy of Optometry. Unauthorized reproduction of this article is prohibited.
e302 Ocular Surface Involvement in Behcet DiseaseVZeng et al.
She denied any other recent illness or vaccinations and did not oral and genital ulceration improved. The dosage of drugs was
wear contact lenses before. The patient did not have diabetes or reduced under the supervision of the eye care practitioner and the
hypertension. On ophthalmic examination, best-corrected vi- dermatologist. About 2 months later, all of the above symptoms
sual acuity (BCVA) was 20/60 in the right eye and 20/40 in the relapsed and the dry eye symptoms worsened with a BCVA of
left eye. Intraocular pressure measured by a Goldmann to- 20/100 in the right eye and 20/40 in the left eye. The Schirmer I
nometer was 16 mm Hg in each eye. Examination revealed test without anesthetic was 1 mm OD and 2 mm OS. In addition
conjunctival vasodilation, mucosa keratosis of the palpebral to oral methylprednisolone 50 mg daily and thalidomide 25 mg
margin, conjunctival scarring, symblepharon, trichiasis, and daily, topical tacrolimus and prednisolone ophthalmic suspension
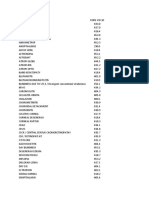
canalicular atresia in both eyes (Fig. 1A to E). Some granulation- and artificial tears were again used for 2 months with relief of most
like tissue proliferation was also noted in the upper palpebral of the symptoms. The dry eye symptoms persisted and the ocular
margins of both eyes (Fig. 1A, B). There was scattered punctate surface lesions were recalcitrant to therapy.
fluorescein staining in both corneas and a 1-mm round ulcer lesion
near the center of cornea with mild infiltration by fluorescein
staining in the right eye (Fig. 1D, E). The pupils were equal and
round, with a brisk reaction to light and no relative afferent
DISCUSSION
pupillary defect. No inflammation was found in the aqueous, Behcet disease, a vasculitic disorder affecting many organs, is
vitreous, or fundus. Fluorescein angiography showed no retinal characterized by three primary components: iridocyclitis (histor-
vascular inflammation. We had taken some samples with moist ically with hypopyon), aphthous lesions in the mouth, and ul-
swabs from the lower fornix of both eyes to incubate and did not ceration of the genitalia. Erythema nodosum, arthropathy, and
find pathogenic microorganisms. The Schirmer I test without thrombophlebitis often accompany these manifestations. In BD,
anesthetic was 2.5 mm OD and 3 mm OS. Heidelberg confocal there is no relevant biological test for diagnosis. It depends on
microscopy showed palpebral conjunctiva infiltration with a the clinical presentation of BD; however, sarcoidosis, multiple
large number of mature Langerhans cells of characteristic den- sclerosis, Crohn disease, Takayasu arteritis, polychondritis, or
dritic form and meibomian gland infiltration with a large antiphospholipid syndrome needs to be considered in the dif-
number of inflammation cells in both eyes. The granulation-like ferential.3 International criteria of classification have been defined
tissue on the conjunctiva appeared as amorphous structures under with a sensitivity of 85% and a specificity of 96%.1 Although there
Heidelberg confocal microscopy (Fig. 1F to H). The results of are many factors that can cause dry eye, in this case, the primary
autoimmune screening including rheumatoid factor (G10.1 IU/ml; considerations were Steven-Johnson syndrome and cicatricial
reference range, 0 to 15 IU/ml), antinuclear antibody, antineu- pemphigoid. Steven-Johnson syndrome is usually induced by drugs
trophil cytoplasmic antibodies, extractable nuclear antigen, and and it will not relapse if it healed. Cicatricial pemphigoid can be
antimitochondrial antibody were negative. After administration distinguished from BD by laboratory test results. The results of
of topical prednisolone and artificial tear eye drops four times autoimmune screen in our case were useful for differential diag-
daily for 3 months, symptoms subsided and there was no fluo- noses. The etiology and pathogenesis of BD are not well under-
rescein staining in both corneas. The corneal ulceration was healed stood, although immunologic mechanisms have been suspected
with a corneal macula resulting in a BCVA of 20/50 in the right eye to be pathologically important because of the vasculitic nature of
and 20/30 in the left eye. Concurrently, the erythema nodosum and BD and its cellular characteristics. A variety of ocular manifestations
FIGURE 1.
A, B, Granulation-like tissue proliferation and scar on the right and left conjunctiva. C, Symblepharon and canalicular atresia on lateral nasal conjunctiva
(OS). D, E, Corneal ulceration and scattered punctate uorescein staining in the right eye. F, Inammatory cell inltration and meibomian gland on
Heidelberg confocal microscopy. G, A large amount of Langerhans cells presented in the palpebral conjunctiva under Heidelberg confocal microscopy.
H, Granulation-like tissue proliferation on the palpebral conjunctiva appeared as an acellular structure under Heidelberg confocal microscopy.
Optometry and Vision Science, Vol. 91, No. 12, December 2014
Copyright American Academy of Optometry. Unauthorized reproduction of this article is prohibited.
Ocular Surface Involvement in Behcet DiseaseVZeng et al. e303
have been found including anterior uveitis, cataract, glaucoma, confocal microscopy. The incidence of corneal ulceration ap-
posterior segment involvement with vasculitis, vitritis, retini- pears rather high,10 but the reason remains unknown.
tis, panuveitis, retinal edema, cystoid macular degeneration, In our report, ocular surface damage developed in accordance
venous or arterial occlusion, disc edema, and retinal detach- with the exacerbation of systemic symptoms of BD such as oral
ment.3 However, the presentation of ocular surface disease without and genital ulcerations and erythema nodosum. Our findings
intraocular inflammation is rare. This case presented an unusual indicated that ocular surface damage may develop as a clinical
severe ocular surface involvement in BD whose manifestations manifestation of BD. In addition to conjunctival lesions, corneal
were severe dry eye syndrome, symblepharon, granulation-like ulceration with infiltration was noted associated with ocular
tissue proliferation in the conjunctiva, and corneal ulceration, surface damage. From our findings, ocular surface damage may
all without coincident intraocular inflammation. Involvement of present as an isolated finding in BD without other retinal or in-
the conjunctiva is not without explanation as it is a mucous traocular inflammation. The present diagnostic criteria for BD
membrane like oral and genital mucosa. Therefore, changes in requires the presence of at least three of four signs such as oral and
conjunctiva would be expected to parallel the findings in the genital ulcerations or skin and ocular lesions, with an emphasis on
other mucosa. Matsuo et al.6 and Tugal-Tutkun et al.14 found oral ulcerations. The ocular lesions specified in the criteria do not
intraepithelial neutrophil infiltration, lymphocytes, and plasma include ocular surface damage; however, to better diagnose BD,
cell infiltration around the vessels beneath the conjunctival ep- the dissociation of ocular surface damage without intraocular
ithelium by biopsy in BD. Matsuo et al.6 identified small lym- inflammation in this patient suggests that ocular surface damage
phocytes as both T cells and B cells by immune-histochemical may be recognized as one additional sign of ocular lesions in BD.
staining, supporting the role of involvement of T cells in BD. In The primary goals of treatment in BD are symptom control,
this case, we observed a large number of mature Langerhans cells early suppression of inflammation, and prevention of end-organ
of characteristic dendritic form and other inflammatory cells damage. Currently, the most commonly used agents are corticoste-
infiltrated in the palpebral conjunctiva by Heidelberg confocal roids, cytotoxic drugs, colchicine, cyclosporine-A, and tacrolimus.
microscopy consistent with the report of Matsuo et al.6 Mature A trial showed that depot corticosteroids were useful only for er-
Langerhans cells of characteristic dendritic form found in pal- ythema nodosum lesions among women but not in men, whereas
pebral conjunctiva by Heidelberg confocal microscopy may be there was no effect on genital ulcers, oral ulcerations, folliculitis, or
associated with inflammation.15 We observed palpebral con- arthritis.21 Colchicine (1 to 2 mg/d) was effective only for genital
junctiva infiltrated with a large number of mature Langerhans ulcers, erythema nodosum, and arthritis among women, but only
cells of characteristic dendritic form, as well as meibomian gland for arthritis among men.22 Thalidomide was effective for sig-
and corneal ulceration infiltrated with a great many inflamma- nificantly reducing the mean number of oral and genital ulcers
tory cells in both eyes. The findings indicated the presence of and follicular lesions.23 Because of well-known adverse effects of
inflammation in the process of ocular surface lesions in BD. The polyneuropathy, teratogenesis, and sedation, thalidomide should
results of confocal microscopy suggest that it is an optional tool be used for a short period and adverse effects should be closely
to observe the histopathological changes of the eyelid in BD. In monitored. Azathioprine significantly decreased the attacks of
addition to inflammation, the ocular surface damage in BD may hypopyon uveitis and the development of new eye disease among
be related to the abnormity of conjunctival vessels.16,17 A video- patients without eye involvement and preserved visual acuity.24
capillaroscopic study to assess the conjunctival microvascular Topical steroids provide high ocular surface drug concentrations
condition in BD has revealed significant changes in arterio/ and promote lymphocyte apoptosis and suppress cell-mediated
venous diameter with an involvement of both the number and inflammation.25 Ocular surface damage showed a positive re-
the whole vessel structure.17 Flammer et al.18 reported that va- sponse to topical corticosteroids.11,12 Cyclosporine-A decreases
sospasm plays a role in BD etiology, which causes ischemic the severity and frequency of ocular attacks and improves visual
consequences. The vasospasm of conjunctival vessels may be the acuity. It also has a beneficial effect on mucocutaneous lesions.26
main reason for necrosis of conjunctival goblet and epithelial Topical cyclosporine 0.05% or 1% compounded preparation may
cells, and it may also be related to meibomian gland atrophy in be used for treatment of dry eye syndrome associated with various
the region, which leads to irreversible loss of function and xe- causes. The mechanism of action of this therapeutic agent is
rophthalmia. Gunduz et al.19 found Schirmer I and BUT to be through inhibition of T-cell activation and down-regulation of in-
significantly lower in BD patients than in the control group; flammatory cytokines in the conjunctiva and lacrimal gland.27,28
however, there was no significant difference in conjunctival The reduction in anterior-segment inflammation is thought to allow
surface epithelial morphology in the two groups, consistent with enhanced tear production.29 Topical cyclosporine also increases
reported results. The ocular surface is known to play a major role goblet cell density and decreases epithelial cell apoptosis.30 Although
in the stabilization of the tear film. This stabilization is ensured the mechanism of tacrolimus is similar to that of cyclosporine-A
primarily by the mucin secreted by goblet cells. A decrease in (calcineurin inhibitor), the potency in vitro has been shown to be
goblet cells and changes in conjunctival surface epithelial cells significantly greater, exhibiting similar effects at 100 times lower
disturb the stability of the ocular tear film.20 In our case, the concentrations.31 In this case, in addition to tacrolimus, oral
continuous dry eye syndrome may be associated with the damage methylprednisolone, topical prednisolone, and artificial tear eye
of conjunctiva. Corneal ulceration was also reported as an ocular drops managed ocular damage at the early stage. Over the long term,
lesion in BD, the incidence of which was as high as 16%.10 In our however, the ocular surface could not be significantly improved.
patient, there was a corneal ulceration in the right eye with mild In conclusion, ocular surface disease may be an uncommon but
infiltration, predominantly with inflammatory cells revealed by possible manifestation of BD. Therefore, routine examination of
Optometry and Vision Science, Vol. 91, No. 12, December 2014
Copyright American Academy of Optometry. Unauthorized reproduction of this article is prohibited.
e304 Ocular Surface Involvement in Behcet DiseaseVZeng et al.
the ocular surface is recommended in patients with BD, and BD Microvascular assessment in Behcet disease: videocapillaroscopic
should be included in a list of differential diagnoses for patients study. Int J Tissue React 2003;25:105Y15.
with ocular surface damage. In this context, eye care professionals 18. Flammer J, Pache M, Resink T. Vasospasm, its role in the patho-
should look for systemic signs of BD in patients presenting with genesis of diseases with particular reference to the eye. Prog Retin
ocular surface damage. The confocal microscope may be an optional Eye Res 2001;20:319Y49.
tool to observe the histopathological changes of the eyelid in BD. 19. Gunduz A, Cumurcu T, Demirel EE, Akpolat N, Karincaoglu Y.
The ocular surface in the Behcets disease patient. Can J Ophthalmol
2012;47:429Y34.
20. Tseng SC, Hirst LW, Maumenee AE, Kenyon KR, Sun TT,
ACKNOWLEDGMENTS Green WR. Possible mechanisms for the loss of goblet cells in
The authors declare no conflict of interest. mucin-deficient disorders. Ophthalmology 1984;91:545Y52.
Received January 8, 2014; accepted September 1, 2014. 21. Mat C, Yurdakul S, Uysal S, Gogus F, Ozyazgan Y, Uysal O, Fresko I,
Yazici H. A double-blind trial of depot corticosteroids in Behcets
syndrome. Rheumatology (Oxford) 2006;45:348Y52.
22. Yurdakul S, Mat C, Tuzun Y, Ozyazgan Y, Hamuryudan V, Uysal O,
REFERENCES Senocak M, Yazici H. A double-blind trial of colchicine in Behcets
1. International Study Group for Behcets Disease. Criteria for diag- syndrome. Arthritis Rheum 2001;44:2686Y92.
nosis of Behcets disease. Lancet 1990;335:1078Y80. 23. Hamuryudan V, Mat C, Saip S, Ozyazgan Y, Siva A, Yurdakul S,
2. Yurdakul S, Yazici H. Behcets syndrome. Best Pract Res Clin Zwingenberger K, Yazici H. Thalidomide in the treatment of the
Rheumatol 2008;22:793Y809. mucocutaneous lesions of the Behcet syndrome. A randomized,
3. Saadoun D, Wechsler B. Behcets disease. Orphanet J Rare Dis double-blind, placebo-controlled trial. Ann Intern Med 1998;
2012;7:20. 128:443Y50.
4. Ohno S, Ohguchi M, Hirose S, Matsuda H, Wakisaka A, Aizawa M. 24. Yazici H, Pazarli H, Barnes CG, Tuzun Y, Ozyazgan Y, Silman A,
Close association of HLA-Bw51 with Behcets disease. Arch Serdaroglu S, Oguz V, Yurdakul S, Lovatt GE et al. A controlled
Ophthalmol 1982;100:1455Y8. trial of azathioprine in Behcets syndrome. N Engl J Med 1990;
322:281Y5.
5. Kitaichi N, Miyazaki A, Iwata D, Ohno S, Stanford MR, Chams H.
Ocular features of Behcets disease: an international collaborative 25. Pflugfelder SC. Antiinflammatory therapy for dry eye. Am J
study. Br J Ophthalmol 2007;91:1579Y82. Ophthalmol 2004;137:337Y42.
6. Matsuo T, Itami M, Nakagawa H, Nagayama M. The incidence and 26. Masuda K, Nakajima A, Urayama A, Nakae K, Kogure M, Inaba G.
pathology of conjunctival ulceration in Behcets syndrome. Br J Double-masked trial of cyclosporin versus colchicine and long-term
Ophthalmol 2002;86:140Y3. open study of cyclosporin in Behcets disease. Lancet 1989;1:1093Y6.
7. Olivieri I, Genovesi-Ebert F, Signorini G, Pasero G. Conjunctival 27. Pflugfelder SC, Wilhelmus KR, Osato MS, Matoba AY, Font RL.
ulceration in Behcets syndrome. Ann Rheum Dis 1992;51:574Y5. The autoimmune nature of aqueous tear deficiency. Ophthalmology
1986;93:1513Y7.
8. Ouertani A, Lasram L, Mili I. [Behcets disease disclosed by ocular
conjunctival aphthous ulcer. Apropos of a case]. J Fr Ophthalmol 28. Stern ME, Gao J, Siemasko KF, Beuerman RW, Pflugfelder SC.
1992;15:131Y2. The role of the lacrimal functional unit in the pathophysiology of
dry eye. Exp Eye Res 2004;78:409Y16.
9. Merle H, Donnio A, Richer R, Dubreuil F, Arfi S. Isolated con-
junctival ulcerations as the first sign of Behcets disease. Eur J 29. Sall K, Stevenson OD, Mundorf TK, Reis BL. Two multicenter,
Ophthalmol 2006;16:751Y2. randomized studies of the efficacy and safety of cyclosporine oph-
thalmic emulsion in moderate to severe dry eye disease. CsA Phase 3
10. Al-Towerki AE, Al-Motowa S. Corneal perforation in a patient
Study Group. Ophthalmology 2000;107:631Y9.
with Behcets disease. Saudi J Ophthalmol 2006;20:194Y5.
30. Kunert KS, Tisdale AS, Gipson IK. Goblet cell numbers and epi-
11. Zamir E, Bodaghi B, Tugal-Tutkun I, See RF, Charlotte F, Wang RC,
thelial proliferation in the conjunctiva of patients with dry eye
Wechsler B, LeHoang P, Anteby I, Rao NA. Conjunctival ulcers in
syndrome treated with cyclosporine. Arch Ophthalmol 2002;
Behcets disease. Ophthalmology 2003;110:1137Y41.
120:330Y7.
12. Shenoy R. Conjunctival ulcerVmucocutaneous or ocular manifes-
31. Kino T, Hatanaka H, Hashimoto M, Nishiyama M, Goto T,
tation of Behcets disease? A case report. Eur J Ophthalmol 2002;
Okuhara M, Kohsaka M, Aoki H, Imanaka H. FK-506, a novel
12:435Y6.
immunosuppressant isolated from a Streptomyces. I. Fermentation,
13. Rohatgi J, Singal A. Ocular manifestations of Behcets disease in
isolation, and physico-chemical and biological characteristics.
Indian patients. Indian J Ophthalmol 2003;51:309Y13.
J Antibiot (Tokyo) 1987;40:1249Y55.
14. Tugal-Tutkun I, Urgancioglu M, Foster CS. Immunopathologic
study of the conjunctiva in patients with Behcet disease. Ophthal-
mology 1995;102:1660Y8. Baihua Chen
15. Efron N, Al-Dossari M, Pritchard N. In vivo confocal microscopy Department of Ophthalmology
of the palpebral conjunctiva and tarsal plate. Optom Vis Sci 2009; The Second Xiangya Hospital
86:1303Y8. Central South University
16. Sahin OG. Conjunctival microvascular abnormalities in two cases 139 Renming Middle Rd
with Behcets disease. Ocul Immunol Inflamm 2009;17:345Y7. Changsha Hunan Province 410011
17. Pasqui AL, Pastorelli M, Puccetti L, Beerman U, Biagi F, Camarri A, China
Palazzuoli A, Servi M, Bischeri D, Saletti M, Bruni F, Auteri A. e-mail: chenbh2006@163.com
Optometry and Vision Science, Vol. 91, No. 12, December 2014
Copyright American Academy of Optometry. Unauthorized reproduction of this article is prohibited.
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Pao Vic 2013Document8 pagesPao Vic 2013laudyaFebPas encore d'évaluation
- 10.1111/jcpe.12555: Deposited On: 22 April 2016Document26 pages10.1111/jcpe.12555: Deposited On: 22 April 2016laudyaFebPas encore d'évaluation
- The Uveitis - Periodontal Disease Connection in Pregnancy: Controversy Between Myth and RealityDocument5 pagesThe Uveitis - Periodontal Disease Connection in Pregnancy: Controversy Between Myth and RealitylaudyaFebPas encore d'évaluation
- Inggris IndonesiaDocument26 pagesInggris IndonesialaudyaFebPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- State Medical and Pharmaceutical University "Nicolae Testemiţanu"Document49 pagesState Medical and Pharmaceutical University "Nicolae Testemiţanu"Ansares SultanPas encore d'évaluation
- Uveitis & Retinal DetachmentDocument8 pagesUveitis & Retinal Detachmentjumi26Pas encore d'évaluation
- Ocular Hypotony - A Comprehensive ReviewDocument20 pagesOcular Hypotony - A Comprehensive ReviewJavier Infantes MolinaPas encore d'évaluation
- Casos Clínicos Sobre UveíteDocument16 pagesCasos Clínicos Sobre UveíteMirella Lopes da RochaPas encore d'évaluation
- PracticeExam 2 AnsDocument51 pagesPracticeExam 2 AnsBehrouz YariPas encore d'évaluation
- Ocular Manifestations of Connective Tissue Disorders: A Descriptive Cross Sectional StudyDocument4 pagesOcular Manifestations of Connective Tissue Disorders: A Descriptive Cross Sectional StudyIJAR JOURNALPas encore d'évaluation
- Second Class UveitisDocument42 pagesSecond Class Uveitisabhishek tPas encore d'évaluation
- Glaucoma, Hyphema: Synonyms and Related Keywords: Hyphema, Microhyphema, Hemorrhage in The AnteriorDocument22 pagesGlaucoma, Hyphema: Synonyms and Related Keywords: Hyphema, Microhyphema, Hemorrhage in The AnteriorWulandari EmyPas encore d'évaluation
- Managing The Red Eye: Speaker NotesDocument46 pagesManaging The Red Eye: Speaker NotesAlina DănescuPas encore d'évaluation
- Corneea EnglishDocument57 pagesCorneea EnglishGermanyPas encore d'évaluation
- UVEITIS ESSENTIALSeditDocument38 pagesUVEITIS ESSENTIALSeditSatria WidyatamaPas encore d'évaluation
- Core Ophthalmic Knowledge: Academy MOC Essentials® Practicing Ophthalmologists Curriculum 2017-2019Document294 pagesCore Ophthalmic Knowledge: Academy MOC Essentials® Practicing Ophthalmologists Curriculum 2017-2019Dayana Rosales DuránPas encore d'évaluation
- Dams Ophthal TestDocument76 pagesDams Ophthal TestShrikant Shukla100% (1)
- Pod Uveitis DWNLD PDFDocument252 pagesPod Uveitis DWNLD PDFVanesia Hera SaiduyPas encore d'évaluation
- Intermediate UveitisDocument33 pagesIntermediate UveitismitaamayPas encore d'évaluation
- Rheumatology NotesDocument31 pagesRheumatology Noteskatherine nunnPas encore d'évaluation
- TM2 - K37 - Eye Disorders Due To Tropical DiseasesDocument86 pagesTM2 - K37 - Eye Disorders Due To Tropical DiseasesedelinPas encore d'évaluation
- Healing Prayer WordDocument6 pagesHealing Prayer WordabbajiePas encore d'évaluation
- TOS眼科62手冊 57-64 PDFDocument8 pagesTOS眼科62手冊 57-64 PDFAriel LiPas encore d'évaluation
- Eye Care Centre - Best Eye Hospital in India - Shroff Eye CentreDocument19 pagesEye Care Centre - Best Eye Hospital in India - Shroff Eye CentreShroff Eye Centre - Eye hospitalPas encore d'évaluation
- Navle NotesDocument32 pagesNavle NotesRyan Fortier94% (18)
- Ophthalmology MCQsDocument18 pagesOphthalmology MCQsRamachandharan Nethaji67% (9)
- Kode Icd MataDocument5 pagesKode Icd Mataindah ramadhaniPas encore d'évaluation
- FIQ - Focal and Diffuse Choroidal and Retinal InflammationDocument34 pagesFIQ - Focal and Diffuse Choroidal and Retinal InflammationHikban FiqhiPas encore d'évaluation
- BCQs POOLDocument39 pagesBCQs POOLabusaudinternationalPas encore d'évaluation
- Anatomy of Uvea: Dr. Binu AsharafDocument48 pagesAnatomy of Uvea: Dr. Binu AsharafBinu AshrafPas encore d'évaluation
- Anterior Uveitis: Ophthalmology Management TreeDocument2 pagesAnterior Uveitis: Ophthalmology Management TreeSandro PandurevicPas encore d'évaluation
- Chorioretinitis: By. Bimo Nugroho SaktiDocument14 pagesChorioretinitis: By. Bimo Nugroho SaktiSalman AlkomaPas encore d'évaluation
- Auto Immune Disease ProtocolDocument5 pagesAuto Immune Disease ProtocolHitesh ParmarPas encore d'évaluation
- Eye & EarDocument127 pagesEye & EarMaria Sheila BelzaPas encore d'évaluation