Académique Documents
Professionnel Documents
Culture Documents
Opinions of Dental Students On Newly Implemented Tobacco Cessation Protocol
Transféré par
DentalLearningTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Opinions of Dental Students On Newly Implemented Tobacco Cessation Protocol
Transféré par
DentalLearningDroits d'auteur :
Formats disponibles
Opinions of Dental Students
on Newly Implemented Tobacco Cessation Protocol
Abstract
O
bjectives: Tobacco cessation and tobacco-use cessation counseling are important in the prevention of both oral and
systemic diseases. The University at Buffalo School of Dental Medicine recently added the Tobacco Cessation Coun-
seling Protocol (TCCP) to the predoctoral curriculum, in which students are trained to provide this service to patients.
The purpose of this study was 3-fold: to evaluate the opinions of students regarding the new TCCP, to identify barriers for suc-
cessful implementation of the program, and to explore ways to improve effectiveness of the TCCP from the perspective of den-
tal medicine.
M
ethods: A total of 120 third- and fourth-year tients’ nicotine dependence and 50% reported that they
dental students were asked to complete a sur- had sufficient skills to provide tobacco cessation counsel-
vey regarding the TCCP, which included ques- ing. Fifty-five percent of students believed they had re-
tions on identification of barriers to counseling, ceived adequate training in tobacco cessation counseling;
student/patient relationships, and students’ confidence 81% of students were somewhat confident about being
about providing tobacco cessation counseling. able to prevent their patients from starting to use tobacco.
Results: The survey was completed by 108 students Eighty-three percent of students identified the TCCP serv-
(90%). Nearly all (99%) believed that dentists should as- ice fees and 78% identified lack of faculty involvement as
sist their patients in tobacco cessation. Of the respondents, perceived barriers associated with the TCCP.
63% were confident about assessing and treating their pa- Conclusions: Students believe helping smokers to quit
using tobacco is a dentist’s professional responsibility. How-
Othman Shibly, DDS, MS ever, lack of faculty involvement was perceived to be a major
Diplomate, American Board of Periodontology barrier for students’ implementation of tobacco counseling.
Director, Preventive Dentistry
Coordinator, International Advanced Dental
Education Introduction
Associate Director, Center for Dental Studies The US Surgeon General has reported smoking to be a
University at Buffalo School of Dental Medicine
Buffalo, NY major factor in the development of oral and maxillofacial
cancers.1 Studies report that tobacco is a causal factor in
Adeela Khan, BA the development of stomatitis nicotina, gingival bleeding,
MPH Candidate, The George Washington University gingival recession, acute necrotizing ulcerative gingivitis,
School of Public Health and Health Sciences
Washington, DC increased dental calculus, halitosis, and dental staining.2
Research Assistant Recent studies show that even smokeless tobacco causes
Department of Periodontics and Endodontics
University at Buffalo School of Dental Medicine
systemic effects, such as nicotine dependence, transient hy-
Buffalo, NY pertension, and cardiovascular disease.3 Tobacco products
Vol. 4, No. 8 (Suppl 1) Dental Learning / August 2010 1
clearly have a negative effect on oral health4-6; however, curricula have included only the first two A’s—ask and
in clinical practice many healthcare providers do not ad- advise—our newly designed TCCP consists of all 5 A’s.
dress tobacco dependence as an oral disease. (Figure 1) Students are trained to include all five A’s while
In 2008 the Surgeon General declared that tobacco de- counseling patients and prescribing adjunctive medication
pendence is a chronic disease for which healthcare providers as needed. In summary, the modified 5 A’s are:
must provide ongoing counseling as an effective form of to- • Ask patients about their smoking habits, type of to-
bacco cessation.7 Tobacco counseling methods have been in- bacco used, and frequency of use.
tegrated into US dental school curricula since 1989.8,9 An • Advise patients about the effects of tobacco on their
objective of Healthy People 2010, a national program de- oral health. The patient’s present oral condition, diag-
signed to identify the most significant preventable threats to nosis, prognosis, and clinical outcome must be ex-
health and establish national goals to reduce these threats, plained to the patient with regards to tobacco use.
is to increase the percentage of dentists who counsel on to- Therefore, this step is done as part of the treatment
bacco cessation.10 Despite such efforts, recent reports suggest plan, not part of the dental history.
that many dentists do not perform tobacco cessation coun- • Assess patients to determine their interest in quitting
seling. A 2006 Texas study found that 90% of dentists were on a scale of 1 to 10 (with 10 being “most interested”).
unfamiliar with the “5 A’s” protocol for tobacco cessation • Assist patients who want to quit by offering nicotine
counseling (Ask, Advise, Assess, Assist, and Arrange),11 and patches and suggestions on how to avoid the temptation
a 2007 survey of South Carolina dental students reported to smoke (eg, throwing away tobacco products, and stor-
that only 39% thought they were adequately trained to pro- ing ashtrays). Other medications for the treatment of to-
vide tobacco cessation education.10 Additional studies indi- bacco dependence are: nicotine gum (nonprescription),
cate that many dentists are still less active in promoting nicotine inhaler (prescription), nicotine nasal spray (pre-
tobacco cessation than are other healthcare providers.12-14 scription), nicotine lozenge (nonprescription), and bupro-
It has been demonstrated that incorporating a Tobacco pion hydrochloride (brand name, Zyban) (prescription).
Cessation Counseling Protocol (TCCP) during the aca- A relatively new medication is varenicline (brand name,
demic program increases the use of tobacco cessation tech- Chantix). Varenicline blocks the ability of nicotine to ac-
niques by dental students.15 Although an increasing tivate α4β2 receptors which prevents stimulation of the
number of tobacco cessation counseling programs have central nervous mesolimbic dopamine system.17
been implemented throughout US dental schools, there is • Arrange for follow-up visits to the dental clinic to see
little written on the methods for successful implementa- how the patients are doing and encourage continued
tion of such programs.16 The purpose of this article is to abstinence.
explain the model used by the University at Buffalo School In the past few years the UBSDM has included several
of Dental Medicine (UBSDM) for implementation of its new protocols in the dental curriculum and dental clinic.
TCCP and to help improve the new protocol by discussing Some of these protocols are tobacco counseling, nutrition
students’ feedback. Upon completion of this study, the counseling, determination of motivation for plaque con-
data collected will be used to improve the effectiveness of trol and oral hygiene, salivary flow rate, and caries risk
the TCCP and make it available to other dental schools test, all of which include a comprehensive risk assessment
and dentists in individual practice. for dental and periodontal diseases, including oral can-
cers. In addition, students also receive training to perform
Methods nonjudgmental and personalized tobacco-use assessments
University at Buffalo Tobacco Counseling Program and to counsel by prescibing medications that help pa-
Using a modified form of the traditional 5 A’s ap- tients reduce nicotine dependency.
proach, the UBSDM emphasizes the role of the dental The UBSDM is taking a progressive approach to help
team in including promotion of oral health and preven- patients quit using tobacco. Until 2 years ago there was
tion of oral diseases. Although traditionally most dental limited content in the predoctoral program on the TCCP
2 Dental Learning / August 2010 Vol. 4, No. 8 (Suppl 1)
for patients who use tobacco. However, the effect of to- fourth-year students. Percentages and frequencies were also
bacco on oral health based on current clinical research was generated to determine distributions for several responses.
extensively covered in the dental curriculum. This resulted
in a gap between clinical practice and clinical research Results
within dental education. To close this gap, the University Role of the Dental Professional
at Buffalo developed a comprehensive TCCP, one of the Dental students were asked to evaluate several state-
few programs in the nation that uses each of the “5 A’s” ments about their professional role in tobacco counseling.
and includes cessation advice incorporated into a person- In response to a question about the extent to which they
alized dental treatment plan.16 In this program, third- and believe it is the dentist’s role to “assist your patients to
fourth-year dental students do not refer tobacco users to a quit using tobacco,” approximately 99%, or 104 students
telephone-based tobacco-use cessation program or tobacco felt that it was important. Similarly, we found that 81.0%
cessation clinic; rather, the students are taught to imple- of third- and fourth-year students agreed or strongly
ment nonjudgmental tobacco counseling to encourage agreed that good dental care should include tobacco ces-
their patients to quit using tobacco, as well as to offer sation counseling. Our data also indicated that less than
treatment options to assist their patients who desire to 8% of the students surveyed felt that dental students
quit. should not be trained in the TCCP methods. Table 1
shows the breakdown in responses, by class year, to ques-
Survey tions pertaining to the role of dental professionals.
For this study, 120 third- and fourth-year students at
UBSDM were given a self-administered survey in 2008. Students’ Perceptions: Patient-Related Barriers
The survey used purposive sampling methods, as all third- Students were asked to evaluate potential patient-re-
and fourth-year students were eligible to take the survey. lated barriers that reduce the students’ ability to provide
Of the 120 students, 108 returned their surveys (response the TCCP. This was done to rank the specific barriers and
rate, 90%). understand student concerns. Figure 1 shows the percent-
Recruitment attempts included handing students the sur- ages of students who agreed with the potential barriers we
vey at the beginning of class or during their clinic. Students listed as choices in our survey. Broken down by class,
were asked to complete the entire survey. Two attempts were 57.8% of the third-year students believed that patients are
made to increase response rate. Students individually not motivated to quit. Similar numbers of fourth-year stu-
handed the completed survey to the instructor. Each stu- dents (57.1%) agreed with this sentiment.
dents’class year was obtained; no personal identifying ma- As shown in Figure 1, the third- and fourth-year stu-
terial for the student was necessary for our purposes. dents identified lack of patient motivation and the idea that
The questions used in this survey were adapted from 2 patients do not expect counseling from dental students to
previous surveys: a survey of pediatric dentists and an ear- be the strongest barriers with respect to implementation of
lier Australian study of dental students.18, 9 Students were a TCCP. Other perceptions with regard to patient-related
evaluated on their readiness and confidence in following barriers included: students feeling too intrusive when ask-
the tobacco cessation protocol while also taking a critical ing patients about tobacco use, patients not listening to den-
look at the training provided by the school. tal students’ counselling, fear of upsetting the dentist/patient
Data entry and analysis were performed using, respec- relationship, and belief that patients do not consider the
tively, Microsoft Office Excel 2007 and the Statistical Pack- TCCP to be part of the dental professional’s role.
age for Social Sciences, version 6.1 (SPSS Inc). The survey
consisted of 25 questions, with 22 of the questions using a Student Opinions: The TCCP
5-point Likert scale (“strongly agree” to “strongly dis- Table 2 represents student self-assessment of skills
agree”). Descriptive statistics were generated and used to gained from the TCCP training they have received at
evaluate the differences between the responses for third- and UBSDM. The data were not broken down by class be-
Vol. 4, No. 8 (Suppl 1) Dental Learning / August 2010 3
1
Table 2 Dental students attitudes regarding the role of the dental professional.
Survey Response Forth Year % Third Year % Total % Combined
Question Students Students (3rd and 4th Year
(N=42) (N=63) Students, N=105)
To what extent do you
think it is part of your role Not Important 1 2.4% 0 0.0% 1.0%
as a dentist to assist your Important 26 61.9% 48 76.2% 70.5%
patients to quit using tobacco? Very Important 15 35.7% 15 23.8% 28.6%
Students should be trained Agree/Strongly Agree 26 61.9% 44 71.0% 66.7%
in smoking cessation counseling. Disagree/
Strongly Disagree 6 14.3% 2 3.2% 7.6%
Neutral 10 23.8% 16 25.8% 24.8%
Good Dental Care should Agree/Strongly Agree 33 78.6% 52 82.5% 81.0%
include tobacco smoking Disagree/
cessation counseling Strongly Disagree 4 9.5% 3 4.8% 6.7%
Neutral 5 11.9% 8 12.7% 12.4%
cause this portion of the data sought to understand how tor in hindering the implementation of the TCCP, 83% of
students on the whole feel about their TCCP education. students agreed and indicated that elimination of the fee
The data indicate that students are confident about their for tobacco cessation counseling would increase patient
received training, with more than 60% responding that acceptance of the TCCP. In an unpublished study by
they are able to treat patients at several levels, including UBSDM faculty members in 2007, it was found that al-
prevention and intervention. When asked how confident though many students were performing the TCCP, they
students were in assisting patients to quit smoking, 67.6% were not adding the service to the patient’s bill.
of students were ‘confident,’ with an additional 10.5% of In addition to identification of barriers to implementa-
students feeling ‘very confident’ responded that they were tion of the TCCP, students were also asked to rank the use-
‘confident’. Similarly 80% of students felt ‘confident’ or fulness (1 through 5, with 5 being the most useful) of 5
‘very confident’ (60.0% and 20.0% respectively) about tobacco cessation resources to which the school uses or has
the delivery of tobacco prevention counseling. When we access. Students identified the New York State Quit-line
combined the categories of ‘confident’ and ‘very confi- (self-help pamphlets and brochures and coordinated care)
dent,’ a lesser percentage (66.7%) were confident about as the most useful resource. Free nicotine replacement ther-
their ability to assess and treat nicotine dependence. apy was ranked as the second most useful option.
The survey also asked students questions pertaining to
their perceptions of UBSDM faculty and staff. Students Discussion
were asked how helpful the faculty, staff, and dental assis- Instructing healthcare students in the classroom and
tants are in terms of the TCCP implementation. A supple- clinics is a vital step in ensuring that, with proper coun-
mental question was asked regarding the familiarity with seling, tobacco-using patients will stop using tobacco
the TCCP within the faculty. Students in general had over- products. It is the goal of a dental professional to help in-
all neutral responses to these questions (data not shown). dividuals achieve and maintain maximum oral health
throughout their lives. Given that almost one-third of peo-
Elimination of Barriers ple see a dentist, the dental clinic offers an environment
Initially, patients were charged a $13 clinic fee for the conducive for tobacco counseling.19
TCCP counseling services that was added to the regular Furthermore, implementation of a TCCP within den-
cost of the checkup. When asked if the clinic fee was a fac- tal education is gaining importance as universities and
4 Dental Learning / August 2010 Vol. 4, No. 8 (Suppl 1)
Table 2 Student Skills Assessment.
Survey Question Responses (%)
By virtue of the training you have received at UBSDM, how
confident are you in your ability to … Not Confident Confident Very Confident
… assist your patients to quit smoking? 21.9 67.6 10.5
… prevent patients from starting to use tobacco products? 19.0 60.0 20.0
... assess and treat nicotine dependence? 33.3 61.9 4.8
health centers increasingly become tobacco-free environ- appropriate. Following this procedure allows the TCCP
ments. Beginning with the 2009 academic year, the Uni- to be more individualized for every tobacco user and gives
versity at Buffalo became a smoke-free campus as part of patients the convenience of having an assessment, coun-
the UBreathe Free Initiative. In collaboration with several seling, and individualized treatment (including nicotine re-
state and regional associations, the program will help to- placement therapy if indicated) in 1 appointment.
bacco users by offering cessation tools and support. Also, UBSDM helped students implement the TCCP
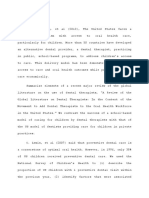
At UBSDM the new TCCP includes providing dental stu- by developing a quick guide brochure on the 5 A’s along
dents with 8 hours of in-class lectures starting in their second with a patient sticker that is included in the patient’s chart
year, which includes information on the effect of tobacco (Figure 2). The patient sticker summarizes the patient’s re-
products on systemic health, oral health, and the epidemiol- sponse to the counseling and is used as a checklist by den-
ogy of tobacco-associated diseases. Tobacco components and tal students to ensure all aspects of counseling are covered.
the role of nicotine in addiction are also covered. The inte- In addition to using the 5 A’s, students are taught to iden-
gration of the TCCP within multiple disciplines produces a tify tobacco dependence as an oral health problem and a
more comprehensive protocol, fortifying the message to stu- chronic disease; thus the TCCP becomes part of the treat-
dents and making it relevant for application.20 ment plan. Through the TCCP, students are able to offer pa-
At UBSDM, the first “A” in the traditional 5 A’s (“Ask tients a free 2-week supply of nicotine patches and a quit
at every appropriate opportunity”) differs in that the pa- guide to help them achieve their goals. If nicotine patches
tient is always asked if he or she is a tobacco user. Students were contraindicated, students were trained about alternative
are required to ask patients if they use tobacco products nicotine replacement therapies or appropriate medications.
when taking patient medical histories. The patient’s smok- UBSDM teaches the importance of practitioners pro-
ing status is updated each time his or her medical history viding intervention and prevention counseling. For exam-
is updated. Unlike many other programs, UBSDM students ple, tobacco intervention counseling becomes mandatory
do not provide tobacco counseling on determining the pa- any time a patient is identified as a tobacco user. Similarly,
tient’s tobacco-use status (taken from their medical his- when the patient is not a tobacco user, students are in-
tory), but rather after the dental history is taken, diagnosis structed to encourage prevention and provide positive
has been established, and the treatment plan formulated. morale for the patient to stay tobacco free. This is critical,
This has demonstrated to be a beneficial change, as 1 study especially among younger patients, to prevent them from
described that people are less likely to seek any type of den- becoming smokers. Each treatment is marked by a special
tal care when their self-rated dental health status is lower, insurance code—U1322 for Tobacco Counseling Cessa-
and that when “episodic, problem-driven dental care tion when the patient is a smoker or U1323 for Tobacco
users” are more likely to rate themselves at a lower health Prevention when the patient is not a smoker. This ensures
status, they are also more likely to use tobacco.21 that every patient is asked about his or her tobacco use
The UBSDM process ensures that the TCCP will be the and that none of the tobacco users will miss receiving to-
first item in the treatment plan. Doing so allows advice to bacco counseling. The students are also given school cred-
be systematic and more effective by relating any dental, its for using the TCCP, to emphasize that it is an integral
oral, and periodontal findings to tobacco use whenever part of dental treatment. A survey of third- and fourth-
Vol. 4, No. 8 (Suppl 1) Dental Learning / August 2010 5
Figure 1 — Perceived barriers for third- and 4th year dental students about the Tobacco Cessation Counseling Program (TCCP). (N=106)
Percent agreement reflects the number of students that ‘agreed’ or ‘strongly agreed’ with the given barrier.
year students sought to evaluate the current TCCP by dents should be trained in the TCCP and were more con-
means of gathering student opinion on the effectiveness fident in the program’s implementation. This is different
of the program and their confidence with their own skill from the 2006 Texas study in which 90% were not fa-
set. In addition, our survey was able to identify barriers miliar with a TCCP.10
facing implementation so that current protocol could be Talking with and counseling dental patients may be dif-
improved and adjustments made wherever needed. ficult and challenging, especially with the presence of patient-
Experience demonstrates that including tobacco coun- related barriers. Students identified several barriers to
seling and training in the dental curriculum was very ef- tobacco cessation counseling, including professional fees,
fective. We found that 99% of students surveyed agreed lack of time, and apparent lack of faculty involvement. These
that tobacco cessation counseling is part of the dentist’s results are consistent with findings of other studies.7, 25, 26
professional role and 81.3% of students that were sur- With the high demands of clinical practice and didac-
veyed felt that good dental care should include the TCCP. tic requirements of every dental program, it is under-
Fried, et al22 reported that 90.6% of dental students be- standable that students felt that lack of time was a barrier
lieved that the TCCP was part of a dental professional’s to providing tobacco counseling. Better time management
role. Other studies also concluded that the role of the den- during patient appointments may alleviate the stress that
tal professional should include a TCCP.23, 24 The data also causes dental students to take no action regarding tobacco
indicated that more third-year students agreed that stu- cessation counseling. A large number of studies have been
6 Dental Learning / August 2010 Vol. 4, No. 8 (Suppl 1)
TOBACCO CESSATION PROTOCOL portant, but will also impress on students that it is as es-
DATE: ________________________
sential as any dental procedure needed for a patient.
Where dentists and dental students are concerned as pro-
ASK THE PATIENT: SMOKING HISTORY
fessionals, they must understand the important role they
# cigs/day _____ # cigs/wk _____ # yrs smoking _____
play as proponents of oral health, prevention, and treat-
# cigars/wk _____ # bowls pipe tobacco/wk _____
ment of oral disease and thus implementation of a TCCP.
# pouches/cans smokeless tobacco/wk _____
Overall, questions pertaining to students’ perceptions
ADVISE THE PATIENT: TOBACCO-RELATED of faculty and staff had overwhelmingly neutral responses.
ORAL PROBLEMS NOTED (check all present) Neutrality was not synonymous with silence in this study.
Stain ____ Periodontitis _____ Halitosis _____ Several focus groups were held between students and fac-
Oral Lesion _____ Other _____ ulty, in which concerns about the faculty and staff’s fa-
ASSESS THE PATIENT: miliarity, helpfulness, implementation, and barriers of
Patient interest in quitting from 1 to 10 ______ TCCP were discussed. Several studies identify lack of ed-
ASSIST THE PATIENT: ucation among dentists and hygienists as significant bar-
Literature given: Yes ____ No____ riers to student program implementation.28, 29 To increase
Quit Date: Now ____ Later ____ confidence among dental students, it would be beneficial
Expected quitting date: ___________
to have continuing education programs geared toward
faculty, so that they may better help students with imple-
Patch Dispensed: Yes ____ No ____
mentation of a TCCP.
ARRANGE FOR THE PATIENT:
With respect to the clinic fee associated with tobacco
Willing to be called: Yes ____ No ____
cessation, because of the presentation of these findings at
Time __________ Number ________________
several student/faculty focus groups, the clinic fee has now
Referred to Quitline: Yes ___ No___ been eliminated and the TCCP is provided at no cost to
the patient. This was a necessary step in furthering the re-
Figure 2 — TCCP sticker that is inserted in patient chart as part solve to help patients, as charging patients for the TCCP
of comprehensive Tobacco Cessation.
was met with largely negative reviews by dental students,
who believed their patients often became hostile to the
devoted to the idea that dentists can greatly increase to- idea that they had to pay for such services, which are typ-
bacco cessation rates by simply counseling patients.18, 27 ically not paid for by dental insurance.
In the US Centers for Disease Control and Prevention’s Dental students may find tobacco cessation counsel-
Treating Tobacco Use and Dependence: 2008 Update, ex- ing harder to implement on unwilling patients. This is ev-
perts recommend that 3- to 10-minute counseling sessions idenced by the higher percentages of third-year students
can have dramatic effects on cessation rates.27 The report versus fourth-year students who believed that they should
states that the more time a dentist can spend with a pa- be trained in the TCCP. It is likely the result of several fac-
tient, the better, but that even low-intensity counseling, tors, including the idea that the third-year students are
defined as a 3-minute session, can significantly increase more optimistic because they have had less experience in
abstinence rates compared with no discussion of tobacco the actual clinic setting. However, to improve student will-
as an oral health issue. The TCCP program at UBSDM ingness for training, it may be beneficial to include addi-
has implemented 10-minute counseling of patients within tional TCCP training throughout the students’ dental
the allotted appointment time. education. A limitation of our study was that we per-
Also, because students at UBSDM receive credit points formed no pretest survey of student opinions before they
for the TCCP, it would be to their benefit to continue im- underwent TCCP training. However, based on past re-
plementing the program with patients. Getting points will search,11, 14 it is reasonable to expect that students who
not only give students the message that the TCCP is im- have not had training in the TCCP would feel less willing
Vol. 4, No. 8 (Suppl 1) Dental Learning / August 2010 7
and less prepared to provide tobacco cessation counseling 5. Krall EA, Abreu Sosa C, et al. Cigarette smoking increases
to patients. Furthermore, the survey elicited helpful ideas the risk of root canal treatment. J Dent Res. 2006;85:313-317.
on improving the protocol that did not require a pretest 6. Chuang SK, Wei LJ, Douglass CW, et al. Risk factors for
(ie, identifying barriers, elimination of the clinic fee, added dental implant failure: a strategy for the analysis of clustered
continuing education courses on the TCCP for faculty). failure-time observations. J Dent Res. 2002;81:572-577.
7. Fiore MC, Jaén CR, Baker TB, et al. Treating Tobacco Use
Conclusion and Dependence: 2008 Update. Clinical Practice Guide-
After adding a TCCP to the dental curriculum, most den- line 18. Rockville, MD: US Dept of Health and Human Serv-
tal students believe that tobacco cessation counseling is a ices, Agency for Healthcare Research and Quality. May
dentist’s professional responsibility and that both dental stu- 2008. http://www.ahrq.gov/path/tobacco.htm. Accessed
dents and dental school faculty require additional training. July 7, 2010.
In summary, based on the findings of this study, den- 8. Fried JL, Rubinstein-DeVore L. Tobacco use cessation cur-
tal schools and dentists must do the following to improve ricula in the US dental schools and dental hygiene pro-
implementation of a TCCP, which should, in turn, help gram. J Dent Educ. 1990;54:730-735.
more patients to quit using tobacco: 9. Rickard-Bell G, Groenlund C, Ward J. Australian dental stu-
• Motivate and educate the faculty and staff about a dents’ views about smoking cessation counseling and their
TCCP and offer more continuing education programs. skills as counselors. J Public Health Dent. 2003:63:200-206.
• Include TCCP training throughout the dental curricu- 10. Hu S, Pallonen U, McAlister AL, et al. Knowing How to
lum in all years of dental education, not limiting it only Help Tobacco Users: dentists’ familiarity and compliance
to the first 2 years. with clinical practice guideline. J Am Dent Assoc. 2006;
• Make the TCCP services free for patients. 137:170-179.
• Provide tobacco cessation counseling after taking both 11. Cannick GF, Horowitz AM, Reed SG, et al. Day TA. Opin-
the medical and dental history, to make the TCCP ions of South Carolina dental students toward tobacco use
more individualized by relating patients’ dental find- interventions. J Pub Health Dent. 2006;66:44-48.
ings to their tobacco use.30,31 12. Weaver RG, Whittaker L, Valachovic RW, et al. Tobacco
• Make a TCCP part of dental practices when treating control and prevention efforts in dental education. J Dent
smokers. A recent publication by one of the authors Educ. 2002;66:426-429.
showed significant efficacy of a TCCP on the quitting 13. Albert D, Ward A, Ahluwalia K, et al. Addressing tobacco in
rates of smokers.32 managed care: a survey of dentists’ knowledge, attitudes,
and behaviors. Am J Public Health. 2002;92:997-1001.
References 14. Victoroff KZ, Dankulich-Huryn T, Haque S. Attitudes of in-
1. US Dept of Health and Human Services. The Health Con- coming dental students toward tobacco cessation promo-
sequences of Smoking: A Report of the Surgeon General. tion in the dental setting. J Dent Educ. 2004;68:563-568.
Atlanta, GA: Centers for Disease Control and Prevention, 15. Barker GJ, Williams KB, Taylor TS, et al. Practice behaviors
National Center for Chronic Disease Prevention and Health of alumni trained as students in tobacco use cessation in-
Promotion, Office on Smoking and Health; 2004. terventions. J Dent Hyg. 2001;75:165-169.
2. Campbell HS, Sletten M, Petty T. Patient perceptions of 16. Christen AC. Tobacco cessation, the dental profession, and
tobacco cessation services in dental offices. J Am Dent the role of dental education. J Dent Ed. 2001;65:368-374.
Soc. 1999;130:219-226. 17. Am J of Health-System Pharmacy. 2007;64(13):1381-1384.
3. Walsh PM, Epstein JB. The oral effects of smokeless to- 18. Warren CW, Jones NR, Chauvin J, et al. Tobacco use and
bacco. J Can Dent Assoc. 2000;66:22-25. cessation counselling: cross-country. Data from the Global
4. Tonetti MS. Cigarette smoking and periodontal diseases: Health Professions Student Survey (GHPSS), 2005-7. To-
etiology and management of disease. Ann Periodontol. bacco Control. 2008;17:238-47. Epub 2008 May 12.
1998;3:88-101. 19. Drilea SK, Reid BC, Li CH, et al. Dental visits among smok-
8 Dental Learning / August 2010 Vol. 4, No. 8 (Suppl 1)
ing and nonsmoking US adults in 2000. Am J Health 26. Watt RG, McGlone P, Dykes J, et al. Barriers limiting den-
Behav. 2005;29:462-471. tists’ active involvement in smoking cessation. Oral Health
20. Harris JL, Patton LL, Wilder RS, et al. North Carolina den- Prev Dent. 2004;2:95-102.
tal hygiene students’ opinions about tobacco cessation 27. US Dept of Health and Human Services. Reducing to-
education and practices in their programs. J Dent Educ. bacco use: a report of the Surgeon General. Atlanta, GA:
2009;73:539-549. US Centers for Disease Control and Prevention, 2000.
21. Dye BA, Morin NM, Robison V. The relationship between 28. Warnakulasuriya S. Effectiveness of tobacco counseling in
cigarette smoking and perceived dental treatment needs the dental office. J Dent Educ. 2002;66:1079-1087.
in the United States, 1988-1994. J Am Dent Assoc. 2006; 29. Walsh MM, Ellison JA. Treatment of tobacco use and de-
137:224-234. pendence: the role of the dental professional. J Dent Educ.
22. Fried JL, Reid CD, DeVore LE. A comparison of health pro- 2005;69:521-537.
fessions student attitudes regarding tobacco curricula and 30. Shibly O, Cummings KM, Zambon JJ. Resolution of oral
interventionist roles. J Dent Educ. 2004;68:370-377. lesions after tobacco cessation. Periodontology. 2008;79:
23. Yip JK, Hay JL, Ostroff JS, et al. Dental students’ attitudes 1797-1801.
toward smoking cessation guidelines. J Dent Educ. 2000; 31. Gansky SA, Ellison JA, Kavanagh C, et al Oral screening
64:641-650. and brief spit tobacco cessation counseling: a review and
24. Shenkin JD, Horowitz AM, Drury TF, et al. Attitudes of pedi- findings. J Dent Educ. 2002;66:1088-1098.
atric dentists towards tobacco intervention for children and 32. Shibly O. Effect of tobacco counseling by dental students
adolescents: a pilot survey. Pediatr Dent. 2003;25:53-60. on quitting rate. J Dent Educ. 2010;74:140-148.
25. Stacey F, Heasman PA, Heasman L, et al. Smoking cessa-
tion as a dental intervention—views of the profession. Br
Dent J. 2006;201:109-113.
Vol. 4, No. 8 (Suppl 1) Dental Learning / August 2010 9
Vous aimerez peut-être aussi
- Tobacco Cessation kj1Document47 pagesTobacco Cessation kj1api-244989408Pas encore d'évaluation
- Treating Nicotine Dependence with Nitrous Oxide/Oxygen (PAN): A Manual for Health ProfessionalsD'EverandTreating Nicotine Dependence with Nitrous Oxide/Oxygen (PAN): A Manual for Health ProfessionalsPas encore d'évaluation
- Ensayo 3Document9 pagesEnsayo 3AlejandraGonzalezRodriguezPas encore d'évaluation
- 520 2014 Article 2282Document6 pages520 2014 Article 2282Diana IancuPas encore d'évaluation
- Oral Health PromotionDocument29 pagesOral Health PromotionRob21aPas encore d'évaluation
- 1 s2.0 S0020653921000356 MainDocument6 pages1 s2.0 S0020653921000356 MainSasi DaranPas encore d'évaluation
- Evidence-Based Dentistry for the Dental HygienistD'EverandEvidence-Based Dentistry for the Dental HygienistPas encore d'évaluation
- Alcohol, Betel-Nut and Cigarette Consumption Are Negatively Associated With Health Promoting Behaviors in Taiwan: A Cross-Sectional StudyDocument8 pagesAlcohol, Betel-Nut and Cigarette Consumption Are Negatively Associated With Health Promoting Behaviors in Taiwan: A Cross-Sectional StudyJuita Auglina PasaribuPas encore d'évaluation
- 10.1007/s00520 013 1942 0 PDFDocument13 pages10.1007/s00520 013 1942 0 PDFhendra ardiantoPas encore d'évaluation
- Bansal 2012Document6 pagesBansal 2012carmen mendo hernandezPas encore d'évaluation
- Intro To Biological DentistryDocument7 pagesIntro To Biological DentistryFelipe LazzarottoPas encore d'évaluation
- Factores de Riesgo de CariesDocument10 pagesFactores de Riesgo de CariesKarla González GPas encore d'évaluation
- Research Paper FinalDocument7 pagesResearch Paper Finalapi-643588876Pas encore d'évaluation
- CDH 2498 AmemoriDocument4 pagesCDH 2498 AmemoriEliza DNPas encore d'évaluation
- Communicating in Dental Practice: Stress-Free Dentistry and Improved Patient CareD'EverandCommunicating in Dental Practice: Stress-Free Dentistry and Improved Patient CareÉvaluation : 5 sur 5 étoiles5/5 (1)
- Delivering Better Oral HealthDocument3 pagesDelivering Better Oral Healthsam paulPas encore d'évaluation
- 6 - Original Article PDFDocument7 pages6 - Original Article PDFIna BogdanPas encore d'évaluation
- Periodontal Referral Patterns of General Dentists: Lessons For Dental EducationDocument12 pagesPeriodontal Referral Patterns of General Dentists: Lessons For Dental EducationVio VisanPas encore d'évaluation
- Bell 2012Document13 pagesBell 2012badria bawazirPas encore d'évaluation
- Carranza 2020Document40 pagesCarranza 2020Soo SoniPas encore d'évaluation
- Oral Health Academics' Conceptualisation of Health Promotion and Perceived Barriers and Opportunities in Dental Practice: A Qualitative StudyDocument13 pagesOral Health Academics' Conceptualisation of Health Promotion and Perceived Barriers and Opportunities in Dental Practice: A Qualitative StudySarbu AndraPas encore d'évaluation
- Contemporary Dental Pharmacology: Evidence-Based ConsiderationsD'EverandContemporary Dental Pharmacology: Evidence-Based ConsiderationsPas encore d'évaluation
- Prevention Perspective in Orthodontics and Dento-Facial OrthopedicsDocument6 pagesPrevention Perspective in Orthodontics and Dento-Facial OrthopedicsRalucaPas encore d'évaluation
- Foreign LiteratureDocument13 pagesForeign LiteratureJm. n BelPas encore d'évaluation
- Oral HygieneDocument2 pagesOral HygieneprojecybioPas encore d'évaluation
- Oral Health EducationDocument6 pagesOral Health EducationIonela AlexandraPas encore d'évaluation
- Research Project PaperDocument6 pagesResearch Project Paperapi-369452069Pas encore d'évaluation
- Hill Adult Dental Health SurveyDocument8 pagesHill Adult Dental Health Surveydesy purnama sariPas encore d'évaluation
- Oral Cancer Prevention and Early Detection: Using The PRECEDE-PROCEED Framework To Guide The Training of Health Professional StudentsDocument5 pagesOral Cancer Prevention and Early Detection: Using The PRECEDE-PROCEED Framework To Guide The Training of Health Professional StudentswaterprincessPas encore d'évaluation
- Smoking Cessation AdviceDocument4 pagesSmoking Cessation AdviceJillPas encore d'évaluation
- Entry Reentry, Allied, and Alternative Careers An IWLC Working Group ReportDocument2 pagesEntry Reentry, Allied, and Alternative Careers An IWLC Working Group ReportMega Arti UtamiPas encore d'évaluation
- Understanding Periodontal Diseases: Assessment and Diagnostic Procedures in PracticeD'EverandUnderstanding Periodontal Diseases: Assessment and Diagnostic Procedures in PracticePas encore d'évaluation
- Editorial June 2016Document3 pagesEditorial June 2016Risha faricha NabilaPas encore d'évaluation
- Implementation OralDocument19 pagesImplementation OralZira RizkaPas encore d'évaluation
- Ref 7Document19 pagesRef 7indah anggarainiPas encore d'évaluation
- 1 s2.0 S001185322200595X MainDocument15 pages1 s2.0 S001185322200595X MainRashmita NayakPas encore d'évaluation
- Research Article: Outcome of Chair-Side Dental Fear Treatment: Long-Term Follow-Up in Public Health SettingDocument7 pagesResearch Article: Outcome of Chair-Side Dental Fear Treatment: Long-Term Follow-Up in Public Health SettingAdriani PanjaitanPas encore d'évaluation
- Research Article: Outcome of Chair-Side Dental Fear Treatment: Long-Term Follow-Up in Public Health SettingDocument7 pagesResearch Article: Outcome of Chair-Side Dental Fear Treatment: Long-Term Follow-Up in Public Health SettingAdriani PanjaitanPas encore d'évaluation
- Advancing Infection Control in Dental Care SettingDocument12 pagesAdvancing Infection Control in Dental Care SettingEndang SetiowatiPas encore d'évaluation
- Taf PDFDocument14 pagesTaf PDFrania azzahraPas encore d'évaluation
- Australian Dental Students' Views About Smoking Cessation Counseling and Their Skills As CounselorsDocument8 pagesAustralian Dental Students' Views About Smoking Cessation Counseling and Their Skills As CounselorsGurpinder TungPas encore d'évaluation
- Jurnal AntibiotikDocument5 pagesJurnal AntibiotikSela PutrianaPas encore d'évaluation
- Exploring The World of Science: Dental Caries: A ReviewDocument5 pagesExploring The World of Science: Dental Caries: A ReviewjulfikaPas encore d'évaluation
- Dental Care During COVID-19 Outbreak: A Web-Based SurveyDocument7 pagesDental Care During COVID-19 Outbreak: A Web-Based SurveyDermatoLovers OficialPas encore d'évaluation
- Examining The Oral Health of Filipinos: Policy Analysis: Original ArticleDocument7 pagesExamining The Oral Health of Filipinos: Policy Analysis: Original ArticleTimothy LimaPas encore d'évaluation
- BMC Oral HealthDocument8 pagesBMC Oral Healthina09Pas encore d'évaluation
- 7111 Dental Hygiene Diagnosis Position PaperDocument6 pages7111 Dental Hygiene Diagnosis Position PaperDiana Lozano OlveraPas encore d'évaluation
- 31priti EtalDocument4 pages31priti EtaleditorijmrhsPas encore d'évaluation
- Cigarette Smoking and Root Filled Teeth Extraction: Systematic Review and Meta-AnalysisDocument13 pagesCigarette Smoking and Root Filled Teeth Extraction: Systematic Review and Meta-AnalysisYen-ching ChaoPas encore d'évaluation
- Randomized Clinical Trial of Oral Health Promotion Interventions Among Patients Following StrokeDocument9 pagesRandomized Clinical Trial of Oral Health Promotion Interventions Among Patients Following StrokeAuliasari SiskaPas encore d'évaluation
- Jurnal 5, EAPD - ECC - Management - 2016,, Best Clinical Practice Guidance For Management of Early CariesDocument10 pagesJurnal 5, EAPD - ECC - Management - 2016,, Best Clinical Practice Guidance For Management of Early CariesZulccPaluPas encore d'évaluation
- Review of Related Literature and Studies: Pediatr Dent 10 (4), 328B329, 2009members of The College ofDocument4 pagesReview of Related Literature and Studies: Pediatr Dent 10 (4), 328B329, 2009members of The College ofZoella ZoePas encore d'évaluation
- Oral Health ElderlyDocument2 pagesOral Health ElderlyatikramadhaniPas encore d'évaluation
- Jashinsky 2017Document7 pagesJashinsky 2017Jacob RobinsonPas encore d'évaluation
- ESMO Guidelines MucositisDocument5 pagesESMO Guidelines MucositisJulio S. UrrutiaPas encore d'évaluation
- ResearchDocument6 pagesResearchjinny1_0Pas encore d'évaluation
- 04 Momoi 2012 Clinical Guidelines For Treating Caries in Adults JouDen40 - 95Document31 pages04 Momoi 2012 Clinical Guidelines For Treating Caries in Adults JouDen40 - 95Cherif100% (1)
- Dental Status of Children Receiving School Oral Health Services in TshwaneDocument7 pagesDental Status of Children Receiving School Oral Health Services in TshwaneTy WrPas encore d'évaluation
- Working Practices and Job Satisfaction of Victorian Dental HygienistsDocument6 pagesWorking Practices and Job Satisfaction of Victorian Dental Hygieniststea metaPas encore d'évaluation
- Acteon SorpoCARE Technique ArticleDocument3 pagesActeon SorpoCARE Technique ArticleDentalLearningPas encore d'évaluation
- Isolite - Isolation and Digital - Ricci PDFDocument4 pagesIsolite - Isolation and Digital - Ricci PDFDentalLearningPas encore d'évaluation
- DPS Case Study (Scherer)Document4 pagesDPS Case Study (Scherer)DentalLearning100% (1)
- DPS Case Study (Scherer2)Document4 pagesDPS Case Study (Scherer2)DentalLearningPas encore d'évaluation
- Acteon SorpoCARE Technique ArticleDocument3 pagesActeon SorpoCARE Technique ArticleDentalLearningPas encore d'évaluation
- DPS Case Study (Scherer2)Document4 pagesDPS Case Study (Scherer2)DentalLearningPas encore d'évaluation
- Acteon SorpoCARE Technique ArticleDocument3 pagesActeon SorpoCARE Technique ArticleDentalLearningPas encore d'évaluation
- Isolation in Clinical Practice White Papers - REVDocument3 pagesIsolation in Clinical Practice White Papers - REVDentalLearningPas encore d'évaluation
- Isolation in Clinical Practice White Papers - REVDocument3 pagesIsolation in Clinical Practice White Papers - REVDentalLearningPas encore d'évaluation
- Acteon SorpoCARE Technique ArticleDocument3 pagesActeon SorpoCARE Technique ArticleDentalLearningPas encore d'évaluation
- Acteon SorpoCARE Technique ArticleDocument3 pagesActeon SorpoCARE Technique ArticleDentalLearningPas encore d'évaluation
- Infection PreventionDocument3 pagesInfection PreventionDentalLearningPas encore d'évaluation
- Isolation in Clinical Practice White Papers - REVDocument3 pagesIsolation in Clinical Practice White Papers - REVDentalLearningPas encore d'évaluation
- Acteon SorpoCARE Technique ArticleDocument3 pagesActeon SorpoCARE Technique ArticleDentalLearningPas encore d'évaluation
- A Simplified Approach To The Immediate Provisionalization of An Implant in The Esthetic Zone 0Document4 pagesA Simplified Approach To The Immediate Provisionalization of An Implant in The Esthetic Zone 0DentalLearning100% (1)
- Isolation in Clinical Practice White Papers - REVDocument3 pagesIsolation in Clinical Practice White Papers - REVDentalLearningPas encore d'évaluation
- Acteon SorpoCARE Technique ArticleDocument3 pagesActeon SorpoCARE Technique ArticleDentalLearningPas encore d'évaluation
- Clinical Application of The Closed Sandwich Technique in A Class II RestorationDocument3 pagesClinical Application of The Closed Sandwich Technique in A Class II RestorationDentalLearning100% (1)
- Complete Denture Impression 101Document3 pagesComplete Denture Impression 101DentalLearningPas encore d'évaluation
- Loupes: Magnification and IlluminationDocument2 pagesLoupes: Magnification and IlluminationDentalLearningPas encore d'évaluation
- An Efficient Approach To in Office Tooth WhiteningDocument3 pagesAn Efficient Approach To in Office Tooth WhiteningDentalLearningPas encore d'évaluation
- AccelDent White Papers 2Document2 pagesAccelDent White Papers 2DentalLearning100% (1)
- Alginate SubstituteDocument3 pagesAlginate SubstituteDentalLearningPas encore d'évaluation
- Isolation in Clinical Practice White Papers - REVDocument3 pagesIsolation in Clinical Practice White Papers - REVDentalLearningPas encore d'évaluation
- Guidelines For Immediate Implant Placement in Periodontally Compromised PatientsDocument8 pagesGuidelines For Immediate Implant Placement in Periodontally Compromised PatientsDentalLearningPas encore d'évaluation
- Infection PreventionDocument3 pagesInfection PreventionDentalLearningPas encore d'évaluation
- Infection PreventionDocument3 pagesInfection PreventionDentalLearningPas encore d'évaluation
- New Designs Technologies Promise To Modify Implant OptionsDocument1 pageNew Designs Technologies Promise To Modify Implant OptionsDentalLearningPas encore d'évaluation
- Infection PreventionDocument3 pagesInfection PreventionDentalLearningPas encore d'évaluation
- Infection PreventionDocument3 pagesInfection PreventionDentalLearningPas encore d'évaluation
- Sips 1328Document64 pagesSips 1328Jean Claude De AldánPas encore d'évaluation
- SRS For Travel AgencyDocument5 pagesSRS For Travel AgencyHardik SawalsaPas encore d'évaluation
- 1en 02 PDFDocument96 pages1en 02 PDFAndrey100% (2)
- Operation and Maintenance Manual Compressor Models: P105WJD, P130DWJD, P160DWJD, P175DWJDDocument70 pagesOperation and Maintenance Manual Compressor Models: P105WJD, P130DWJD, P160DWJD, P175DWJDManuel ParreñoPas encore d'évaluation
- Uniden PowerMax 5.8Ghz-DSS5865 - 5855 User Manual PDFDocument64 pagesUniden PowerMax 5.8Ghz-DSS5865 - 5855 User Manual PDFtradosevic4091Pas encore d'évaluation
- Student Research Project Science ReportDocument8 pagesStudent Research Project Science Reportapi-617553177Pas encore d'évaluation
- Introduction To Microelectronic Fabrication PDFDocument332 pagesIntroduction To Microelectronic Fabrication PDFChristy Moore92% (13)
- Industrial Motor Control Part IDocument38 pagesIndustrial Motor Control Part Ikibrom atsbha100% (2)
- Taylorism vs. FordismDocument2 pagesTaylorism vs. FordismLiv Maloney67% (3)
- Book Chapter 11 SubmissionDocument18 pagesBook Chapter 11 Submissioncristine_2006_g5590Pas encore d'évaluation
- Nbme NotesDocument3 pagesNbme NotesShariq AkramPas encore d'évaluation
- The Limits of The Sectarian Narrative in YemenDocument19 pagesThe Limits of The Sectarian Narrative in Yemenهادي قبيسيPas encore d'évaluation
- GNSS COrs SystemDocument20 pagesGNSS COrs SystemKostPutriMalangPas encore d'évaluation
- CryptogrophyDocument37 pagesCryptogrophyFarah EssidPas encore d'évaluation
- RS2 Stress Analysis Verification Manual - Part 1Document166 pagesRS2 Stress Analysis Verification Manual - Part 1Jordana Furman100% (1)
- Circuit Construction: Assignment 3Document45 pagesCircuit Construction: Assignment 3ali morisyPas encore d'évaluation
- Big Brother Naija and Its Impact On Nigeria University Students 2 PDFDocument30 pagesBig Brother Naija and Its Impact On Nigeria University Students 2 PDFIlufoye Tunde100% (1)
- Coal Mining Technology and SafetyDocument313 pagesCoal Mining Technology and Safetymuratandac3357Pas encore d'évaluation
- Lesson 1 Concepts About Educational TechnologyDocument17 pagesLesson 1 Concepts About Educational TechnologyMarvin ContigaPas encore d'évaluation
- FS 1 Episode 2Document6 pagesFS 1 Episode 2Jayson Garcillan UmipigPas encore d'évaluation
- Lecture 7 - Friction - NptelDocument18 pagesLecture 7 - Friction - Nptels_murugan02Pas encore d'évaluation
- NCERT Solutions For Class 10 Maths Chapter 5 Arithmetic Progression (Ex 5.1) Exercise 5.1Document8 pagesNCERT Solutions For Class 10 Maths Chapter 5 Arithmetic Progression (Ex 5.1) Exercise 5.1Akash DasPas encore d'évaluation
- Project Analysis - M5 - MotorwayDocument6 pagesProject Analysis - M5 - MotorwayMuhammad Haroon ArshadPas encore d'évaluation
- 12 Logarithm Approximate FloatingDocument6 pages12 Logarithm Approximate FloatingPhilippe Englert VelhaPas encore d'évaluation
- S4 Computer Sciences Exercises PDFDocument2 pagesS4 Computer Sciences Exercises PDFHenriette Desanges UwayoPas encore d'évaluation
- Nails Care: Word Search: Name: - DateDocument1 pageNails Care: Word Search: Name: - DateDeverly Hernandez Balba-AmplayoPas encore d'évaluation
- PedagogicalDocument94 pagesPedagogicalEdson MorenoPas encore d'évaluation
- Level I 2018 2019 Program Changes PDFDocument2 pagesLevel I 2018 2019 Program Changes PDFMuhammad BurairPas encore d'évaluation
- PretestDocument8 pagesPretestAlmonte Aira LynPas encore d'évaluation
- Pot-Roasted Beef BrisketDocument4 pagesPot-Roasted Beef Brisketmarcelo nubilePas encore d'évaluation