Académique Documents
Professionnel Documents
Culture Documents
Articles: Background
Transféré par
Seleccion PersonalTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Articles: Background
Transféré par
Seleccion PersonalDroits d'auteur :
Formats disponibles
Articles
Safety and ecacy of adjunctive second-generation
antidepressant therapy with a mood stabiliser or an atypical
antipsychotic in acute bipolar depression: a systematic review
and meta-analysis of randomised placebo-controlled trials
Alexander McGirr, Paul A Vhringer, S Nassir Ghaemi, Raymond W Lam, Lakshmi N Yatham
Summary
Background Although mania and hypomania dene bipolar disorder, depressive episodes are more common and Lancet Psychiatry 2016
impairing, with few proven treatments. Adjunctive therapy with second-generation antidepressants is widely used to Published Online
treat acute bipolar depression, but their ecacy and safety remain controversial. October 26, 2016
http://dx.doi.org/10.1016/
S2215-0366(16)30264-4
Methods In this systematic review and meta-analysis, we searched MEDLINE, Embase, the Cochrane Central Register
See Online/Comment
of Controlled Trials, and ClinicalTrials.gov from inception to Jan 31, 2016, for randomised, double-blind, http://dx.doi.org/10.1016/
placebo-controlled trials of second-generation antidepressants adjunctive to a mood stabiliser or an antipsychotic in S2215-0366(16)30347-9
patients with acute bipolar depression. We extracted data from published reports. The primary outcome was change Department of Psychiatry
in clinician-rated depressive symptom score; secondary outcomes were clinical response, clinical remission, (A McGirr MD, R W Lam MD,
treatment-emergent mania or hypomania, and tolerability (using dropout rates as a proxy). We used pooled L N Yatham MBBS) and Mood
Disorders Centre of Excellence
random-eects models, subgroup comparisons, and meta-regression for analyses. We made subgroup comparisons (R W Lam, L N Yatham),
on the basis of mood stabiliser or antipsychotic treatment and did meta-regression examining trial duration. This University of British Columbia,
study is registered with PROSPERO, number CRD#42015016024. Vancouver, BC, Canada; Unidad
Tratornos del Animo, Hospital
Clinico Universidad de Chile,
Findings We identied six trials representing 1383 patients with bipolar depression. Second-generation antidepressants Santiago, Chile
were associated with a small but signicant improvement in clinician-rated depressive symptom score (standardised (P A Vhringer MD); Millennium
mean dierences 0165 [95% CI 00510278], p=0004). However, clinical response and remission rates did not Institute for Depression and
dier signicantly between patients receiving adjunctive antidepressants and those receiving placebo (1158 Personality Resarch, Ministry
of Economy, Santiago, Chile
[08401597], p=0371 for clinical response; 1220 [08741703], p=0243 for remission). Acute treatment was not (P A Vhringer); and Mood
associated with an increased risk of treatment-emergent mania or hypomania (0926 [05761491], p=0753), but Disorders Program, Tufts
52 week extension periods were associated with an increase in risk (1774 [10183091], p=0043). University Medical School,
Boston, MA, USA
(P A Vhringer, S N Ghaemi MD)
Interpretation Adjunctive second-generation antidepressants are associated with reduced symptoms of acute bipolar
Correspondence to:
depression, but the magnitude of benet is small because they do not increase clinical response or remission rates. Dr Alexander McGirr,
However, these medications should be used only in the short term because prolonged use is associated with an Department of Psychiatry,
increased risk of treatment-emergent mania or hypomania. University of British Columbia,
2255 Wesbrook Mall, Vancouver,
BC V6T 2A1, Canada
Funding None. alexander.mcgirr@alumni.
ubc.ca
Introduction side-eects. Thus, treatment for bipolar depression or
Bipolar disorder is a common condition and cause of remains a substantial unmet need. Prof Lakshmi N Yatham,
global disability.1 Although it is dened by episodes of In view of the dearth of proven treatments, clinicians Department of Psychiatry,
mania or hypomania, it is also characterised by chronic widely use antidepressants to treat acute bipolar University of British Columbia,
2255 Wesbrook Mall, Vancouver,
and recurring depressive episodes that account for a depression.6,7 However, the eectiveness of these med- BC V6T 2A1, Canada
substantial proportion of disability.2,3 With an early age of ications for the relief of depressive symptoms remains yatham@mail.ubc.ca
onset,4 patients are reported to spend as much as half of controversial because of the small evidence base. Previous
their lives with mood symptoms.2 meta-analyses that included data from studies of
There are several level 1 pharmacological strategies for rst-generation and second-generation antidepressants
the management of acute mania, but few level 1 reported on the ecacy of antidepressants; of these,
treatments exist for acute bipolar depression.5 two suggest that antidepressants are more ecacious
Quetiapine, uoxetine plus olanzapine, and lurasidone than placebo8,9 whereas the third did not.10 Overall,
alone or in conjunction with lithium or valproate are the antidepressants were no more likely to switch patients
only treatments approved by the US Food and Drug into mania or hypomania (ie, aective switch) compared
Administration (FDA) for bipolar depression. Many with placebo;8,10 however, additional analyses suggested
patients with bipolar depression either do not respond to that tricyclic antidepressants and SNRIs were more likely
these medications or have diculty tolerating the to induce mania than were SSRIs or bupropion.8,10,11
www.thelancet.com/psychiatry Published online October 26, 2016 http://dx.doi.org/10.1016/S2215-0366(16)30264-4 1
Articles
Research in context
Evidence before this study treated with a second-generation antidepressant in addition
The use of antidepressants in the treatment of bipolar depression to a mood stabiliser or an antipsychotic. Random-eect
is a controversial area in psychiatry. We searched MEDLINE from analyses showed a small benet of antidepressant treatment
inception to Jan 31, 2016, for meta-analyses using the search in reducing depressive symptoms, and no evidence of acute
term (bipolar disorder OR bipolar depression) AND risk of treatment-emergent aective switch. However,
antidepressive agents AND meta-analysis. We found four treatment with second-generation antidepressants over
previous meta-analyses of antidepressants in bipolar depression 52 week extension periods was associated with an increased
that included agents and interventions that are discouraged risk of aective switch despite adequate mood stabilisation.
notably, antidepressant monotherapy, tricyclic antidepressants,
Implications of all the available evidence
and monoamine oxidase inhibitors. Therefore, the clinical
Concomitant to adequate mood stabilisation, time-limited
relevance of existing evidence is unclear, and additional
use of second-generation antidepressants is associated with a
examination restricted to trials of second-generation
small clinical benet and no acute risk of treatment-emergent
antidepressants adjunctive to adequate mood stabilisation, a
mania or hypomania in the short term. However, prolonged
strategy now widely used by clinicians, is necessary.
treatment should be avoided.
Added value of this study
Our systematic review identied six randomised
placebo-controlled trials representing a total of 1383 patients
Furthermore, little evidence suggests that non-SNRI included patients aged 1875 years with a major
second-generation antidepressants increase the risk of depressive episode and a primary diagnosis of bipolar I
manic switch.8,10,12,13 disorder or bipolar II disorder according to DSM-III-R,
The International Society for Bipolar Disorders (ISBD) DSM-IV, DSM-5, or ICD-9 criteria. Furthermore,
expert consensus statement discourages the use of patients had to have treatment with a mood stabiliser
antidepressant monotherapy for the treatment of acute (lithium, valproate, or carbamazepine) or an atypical
bipolar depression.14 However, previous meta-analyses antipsychotic agent, to which a second-generation
have not distinguished between antidepressant mono- antidepressant was added as adjunctive treatment.
therapy and antidepressants as adjuncts to adequate We dened second-generation antidepressants as SSRIs,
mood stabilisation, and therefore this important SNRIs, norepinephrine dopamine reuptake inhibitors,
clinical question remains unaddressed. Additionally, and melatonergic antidepressants. Studies were excluded
previous meta-analyses included studies of tricyclic if they used tricyclic or tetracyclic antidepressants,
antidepressants and inhibitors of monoamine oxidase, inhibitors of monoamine oxidase A or B, antipsychotics,
classes that carry an increased risk of aective switch NMDA receptor antagonists, stimulants, hormones, or
and cycle acceleration.15 Therefore, we aimed to natural supplements. Additionally, studies were excluded
determine whether second-generation antidepressant if they did not report raw data and such data could not
adjunctive therapy is ecacious and safe in the otherwise be obtained.
treatment of acute bipolar depression, a crucial
consideration in clinical practice. Data analysis
For each published study, summary estimates were
Methods extracted independently by AM and LNY, with subsequent
Search strategy and selection criteria verication (by PAV), review, and consensus. The
In this systematic review and meta-analysis, we searched following variables were extracted in a structured manner:
MEDLINE, Embase, and the Cochrane Central Register of patient characteristics (mean age, sex, and primary
Controlled Trials from their inception until Jan 31, 2016, diagnosis), mood stabiliser or atypical antipsychotic used,
using the search term (bipolar disorder OR bipolar second-generation antidepressant (dose and titration
depression) AND antidepressive agents AND (clinical trial schedule) used, the placebo condition, treatment-emergent
See Online for appendix OR randomized controlled trial; see appendix for search hypomania or mania episodes, and dropouts. For un-
syntaxes, parameters, and results). We reviewed references published studies identied from ClinicalTrials.gov, we
and citations of articles retained in this study for additional contacted study authors to obtain summary estimates. We
unidentied studies. We also searched ClinicalTrials.gov assessed study quality using the Cochrane Collaborations
using the search term bipolar depression. Tool for Assessing Risk of Bias.16
Studies reported in English were included if they The primary outcome was change in clinician-rated
were double-blind, placebo-controlled trials with random depressive symptom score at study end, calculated as
allocation and allocation concealment, and if they standardised mean dierences (SMDs).17 Secondary
2 www.thelancet.com/psychiatry Published online October 26, 2016 http://dx.doi.org/10.1016/S2215-0366(16)30264-4
Articles
outcomes were clinical response, clinical remission, meta-analysis. Assessment of risk of bias of the included
episodes of treatment-emergent mania or hypomania, studies is shown in the appendix.
and tolerability. For analyses of secondary outcomes, we Our meta-analysis included 1383 patients with bipolar
used odds ratios (ORs, with 95% CIs), as well as risk disorder (1127 with bipolar I disorder, 166 with bipolar II
dierences (RDs) to calculate number needed to treat or disorder, 78 with DSM-III-R bipolar disorder, and
number needed to harm to provide clinical signicance. 12 for whom the exact diagnosis was unspecied; table).
Clinical response was dened by the study authors (except Three trials12,26,28 included only patients with bipolar
for one study for which we dened clinical response) as at disorder I, whereas three trials13,27,29 included both types
least a 50% reduction in primary ecacy measure of the condition. The mean age of patients was
(Montgomerysberg Depression Rating Scale [MADRS],18 4193 years (SD 1221), and the overall patient population
Hamilton depression rating scale [HDRS],19 or clinical consisted of 559 men and 822 women (sex of two patients
monitoring form for mood disorders20) or Clinical Global was unspecied).
Impressionsglobal improvement [CGI-I] of 2 or less. Five trials12,13,2729 involved patients using lithium,
Clinical remission was dened as MADRS18 of 12 or less, valproate, or carbamazepine for the duration of the trial,
HDRS of 7 or less, or two or fewer manic or depressive although the STEP-BD trial13 allowed patients to be on
symptoms for 17 weeks on the clinical monitoring form. any FDA-approved antimanic agent in the nal 2 years
We used dropout rates as a proxy for tolerability, although of recruitment (table). One study27 involved a three-group
they might also reect the absence of ecacy. design and used risperidone in addition to lithium,
Since true treatment eects are likely to vary valproate, or carbamazepine for mood stabilisation;
between studies because of dierent methodological of the three study groups, we included the groups
characteristicsincluding patient selection, primary receiving risperidone plus placebo and risperidone
diagnosis, mood stabiliser or antipsychotic used, anti- plus paroxetine. One trial used olanzapine.26 SSRIs
depressant used, and trial durationwe used pooled were the most studied class of modern antidepressants
random-eects models.21 Only intention-to-treat data were (paroxetine,12,13,27 uoxetine,26 citalopram29), in addition
analysed.22 We also did subgroup analyses to test the eect to 5-HT2B and 5-HT2C antagonist and melatonergic
of mood stabilisers versus antipsychotics. Although some agonist (agomelatine)28 and norepinephrinedopamine
trials allowed both mood stabilisers and antipsychotics, reuptake inhibitor (bupropion).13 In one trial,13 patients
we dichotomised trials on the basis of the predominant were randomly assigned to receive either paroxetine
intervention to which second-generation antidepressants or bupropion. We did not identify any placebo-controlled
were adjuncts. We also did meta-regression to test the trials of SNRI adjunctive therapy. The duration of
eect of study duration on SMDs and RDs. the trials were 6 weeks,29 8 weeks,26,28 12 weeks,27 and
We used Q statistics and I to assess heterogeneity 26 weeks.13
between trials (ie, clinical and methodological diversity),
with the threshold for heterogeneity dened as p value
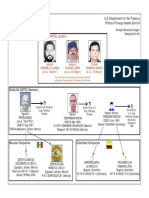
587 potentially eligible studies identied
for the Q statistic less than 01 or I greater than 35%.23 233 MEDLINE
We used funnel plots and Eggers regression intercept24 207 Embase
130 CENTRAL
to test for publication bias.23,25 Comprehensive 2 ClinicalTrials.gov
Meta-Analyses version 2.0 (Biostat, Englewood, NJ, USA) 15 reference review
was used for statistical analyses.
This study is registered with PROSPERO, number
CRD#42015016024. 156 duplicates removed
Role of the funding source
431 screened
There was no funding source for this study.
Results 410 excluded
We initially identied 587 potentially eligible studies
(gure 1). Removal of duplicates and screening of titles
and abstracts left 21 records, of which 14 were excluded 21 reviewed in depth and assessed for eligibility
after full-text review; all trials that were excluded because
of the nature of the antidepressant also did not meet at
15 excluded
least one other inclusion criterion (appendix). One trial
identied from ClinicalTrials.gov (NCT00464191) was
also excluded because the trial was terminated owing to 6 studies included in qualitative and quantitative synthesis
insucient recruitment. We included the remaining
ve published studies12,13,2628 and an additional trial Figure 1: Study selection
from ClinicalTrials.gov (the CAPE-BD trial29) in the CENTRAL=Cochrane Central Register of Controlled Trials.
www.thelancet.com/psychiatry Published online October 26, 2016 http://dx.doi.org/10.1016/S2215-0366(16)30264-4 3
Articles
Diagnosis Mood stabiliser or Antidepressant Number of Number of Mean age Primary Duration of treatment
antipsychotic patients patients (range or SD), outcome
receiving receiving years instrument
antidepressant placebo
Nemero DSM-III-R bipolar Lithium Paroxetine 35 (19 men, 43 (23 men, 425 (2466) in HDRS-21 10 weeks
et al (2001)12 disorder 2050 mg 16 women) 20 women) antidepressant
group,
404 (2166) in
placebo group
Tohen et al Bipolar I disorder Olanzapine (520 mg) Fluoxetine 86 (28 men, 370 (139 men, 4184 (1259) MADRS 8 weeks
(2003)26 2550 mg 58 women) 231 women)
Shelton et al Bipolar I disorder Risperidone (14 mg) in Paroxetine 10 (5 men, 10 (5 men, 356 (107) HDRS-17 12 weeks
(2004)27 (n=12) and bipolar II addition to lithium, 2040 mg 5 women) 5 women)
disorder (n=8) valproate, or carbamazepine
STEP-BD Bipolar I disorder Lithium, valproate, Bupropion 179 (75 men, 187 (82 men, 400 (117) Clinical 26 weeks, of which the rst
(2007)13 (n=240) and carbamazepine, or other 150375 mg or 102 women, 105 women) monitoring 6 weeks were double blind
bipolar II disorder FDA-approved antimanic paroxetine 2 unspecied) form without additions of
(n=114); 12 patients medications 1040 mg subsequent antidepressants
unspecied allowed by the protocol
Yatham et al Bipolar I disorder Lithium or valproate Agomelatine 172 (67 men, 172 (67 men, 4515 (1264) MADRS 8 weeks
(2016)28 2550 mg 105 women) 105 women)
CAPE-BD29 Bipolar I disorder Lithium, valproate, Citalopram 60 (22 men, 59 (27 men, 4149 (1193) MADRS 6 weeks
(n=75) and bipolar II carbamazepine, 1050 mg 38 women) 32 women)
disorder (n=44) antipsychotic, or lamotrigine,
or a combination of these
medications
HDRS=Hamilton depression rating scale. MADRS=Montgomerysberg depression rating scale. FDA=US Food and Drug Administration.
Table: Characteristics of included randomised trials
For sensitivity analyses, we excluded the STEP-BD trial13 000 (degree of freedom [df ]=5; p=065). In sensitivity
because it used the clinical monitoring form for mood analyses, eect sizes remained small when excluding
disorders to dene remission, whereas other studies used the STEP-BD trial13 (0171 [00350306], p=0014) or
MADRS or HDRS. Furthermore, open-label treatment the olanzapineuoxetine trial26 (0134 [00050263],
allowed psychiatrists to add antidepressants at their p=0041). Heterogeneity between trials using a mood
discretion after 6 weeks of placebo-controlled treatment. stabiliser and those using an antipsychotic was not
We also excluded the olanzapineuoxetine trial26 because signicant (Q=060, df=1; p=043). Findings of the
this was the only study with ndings supporting the funnel plot (appendix) and Eggers intercept (075,
ecacy of adjunctive antidepressant therapy. t(4)=084; p=044) suggested a low possibility of
Depressive symptom scores were available for publication bias.
ve trials,12,2629 and we obtained data for the remaining Data for response rates were available for all six trials.
trial13 from the controlled access datasets distributed For the STEP-BD trial,13 we used published outcomes
from the National Database for Clinical Trials for secondary analyses because the clinical monitoring
(NCT00012558) supported by the US National Institute form was used. By study end, 259 (48%) of 542 patients
of Mental Health, which allowed us to extract receiving antidepressants and 360 (43%) of 841 patients
clinician-rated depressive symptoms from the rst receiving placebo achieved response criteria. Pooled OR
6 weeks (the double-blind period) of the trial without the was 1158 (95% CI 08401597, p=0371; gure 3A)
confounding eect of subsequent antidepressants and RD was 0035 (0043 to 0113, p=0377). Exclusion
allowed by the protocol. However, symptoms were of the STEP-BD trial13 enhanced the clinical response of
measured with dierent instruments, including antidepressants to a small degree (199 [55%] of 363 vs
MADRS,26,28,29 HDRS,12,27 and clinical monitoring form.13 286 [44%] of 654; OR 1332 [10101756], p=0042),
We conservatively assumed a correlation coecient of corresponding to a number needed to treat of
07 in SMD calculation because we could not retrieve 15 (95% CI 8250 000; RD 0068 [00000137],
the correlations between scores before and after p=0046). There was heterogeneity between these trials,
treatment for all trials.30 Compared with placebo, with a Q statistic of 835 and I of 4012 (df=5; p=013).
adjunctive antidepressants were associated with a small We found heterogeneity between trials using mood
but signicant improvement in clinician-rated stabilisers and those using antipsychotics (Q=613,
depressive symptoms (SMD 0165 [95% CI 00510278], df=1, p=0013). Antidepressants were associated with
p=0004; gure 2). Between-sample heterogeneity was increased clinical response in antipsychotic trials (OR
not signicant, with a Q statistic of 330 and I of 1881 [11882979], p=0007; RD 0151 [00400263];
4 www.thelancet.com/psychiatry Published online October 26, 2016 http://dx.doi.org/10.1016/S2215-0366(16)30264-4
Articles
Antidepressant (N) Placebo (N) SMD (95% CI) SE p value Weight (%)
Nemero et al (2001)12 35 43 0294 (0154 to 0743) 0229 0199 636
Tohen et al (2003)26 86 370 0265 (0030 to 0500) 0120 0027 2313
Shelton et al (2004)27 10 10 0143 (0734 to 1021) 0448 0749 166
STEP-BD (2007)13 179 187 0150 (0055 to 0356) 0105 0151 3039
Yatham et al (2016)28 172 172 0024 (0188 to 0235) 0108 0825 2866
CAPE-BD29 60 59 0303 (0059 to 0664) 0184 0101 980
Overall 0165 (0051 to 0278) 0058 0004 10000
2 1 0 1 2
Favours placebo Favours antidepressant
Figure 2: Clinician-rated depressive symptoms
STEP-BD13 data are presented at 6 weeks. SMD=standardised mean dierence.
A
Antidepressant (n/N) Placebo (n/N) OR (95% CI) p value Weight (%)
Nemero et al (2001)12 17/35 18/43 1312 (05343220) 0554 1003
Tohen et al (2003)26 46/86 137/370 1956 (12183140) 0005 2306
Shelton et al (2004)27 3/10 3/10 1000 (01486772) 1000 266
STEP-BD (2007)13 58/179 71/187 0783 (05091204) 0266 2525
Yatham et al (2016)28 106/172 104/172 1050 (06811620) 0825 2509
CAPE-BD29 29/60 27/59 1109 (05402278) 0779 1391
Overall 1158 (08401597) 0371 10000
B
Antidepressant (n/N) Placebo (n/N) OR (95% CI) p value Weight (%)
Nemero et al (2001)12 15/35 15/43 1400 (05593504) 0472 1045
Tohen et al (2003)26 40/86 115/370 1928 (11963108) 0007 2458
Shelton et al (2004)27 3/10 1/10 3857 (032645570) 0284 176
STEP-BD (2007)13 32/179 40/187 0800 (04771343) 0399 2257
Yatham et al (2016)28 91/172 91/172 1000 (06551527) 1000 2754
CAPE-BD29 19/60 16/59 1245 (05652746) 0586 1310
Overall 1220 (08741703) 0243 10000
01 02 05 1 2 5 10
Favours placebo Favours antidepressant
Figure 3: (A) Clinical response and (B) clinical remission
OR=odds ratio.
number needed to treat 7 [425]) but not in mood receiving an antidepressant and 278 (33%) of 841 patients
stabiliser trials (OR 0963 [07361259], p=0783; receiving placebo achieved clinical remission. Pooled
RD 0029 [0026 to 0084]). In patients receiving an OR was 1220 (0874 to 1703, p=0243; gure 3B) and
antipsychotic, 49 (51%) of 96 patients receiving RD was 0044 (0029 to 0118, p=0235). Sensitivity
adjunctive antidepressants achieved clinical response, analyses revealed a marginal dierence in favour of
compared with 140 (37%) of 380 patients receiving antidepressants when the STEP-BD trial13 was excluded
placebo. By contrast, clinical response was achieved in (168 [46%] of 363 vs 238 [36%] of 654; OR 1365
similar proportions of patients given an antidepressant [09851891], p=0061; RD 0073 [00030144],
plus a mood stabiliser (47% [210 of 446]) and those p=0042), with a number needed to treat of 14 (7334).
given placebo plus a mood stabiliser (48% [220 of 461]). Overall, there was evidence of heterogeneity between
Additionally, we used meta-regression to test the the studies (Q=842, I=4067, df=5, p=013).
relation between response RD and study duration, and Heterogeneity between trials using a mood stabiliser
found decreasing ecacy with increasing trial duration and those using an antipsychotic was signicant
(slope 001 [95% CI 000 to 002]; Q=386, df=1, (Q=601, df=1, p=0014), an eect that persisted when
p=0049). Examination of the funnel plots revealed one the STEP-BD trial13 was excluded (Q=396, df=1,
outlier26 (appendix), but Eggers intercept (030, p=0046). This nding suggested that the ecacy
t(4)=030, p=077) did not suggest publication bias. of antidepressants was greater in antipsychotic
Data for remission rates were available for all six trials (OR 1977 [12373159], p=0004; RD 0159
studies. By the study end, 200 (37%) of 542 patients [00500268], number needed to treat 7 [420]), but not
www.thelancet.com/psychiatry Published online October 26, 2016 http://dx.doi.org/10.1016/S2215-0366(16)30264-4 5
Articles
A
Antidepressant (n/N) Placebo (n/N) OR (95% CI) p value Weight (%)
Nemero et al (2001)12 0/35 2/43 0234 (00115033) 0353 240
Tohen et al (2003)26 5/86 19/370 1140 (04143145) 0800 2202
Shelton et al (2004)27 0/10 0/10
STEP-BD (2007)13 18/179 20/187 0934 (04761829) 0841 5008
Yatham et al (2016)28 7/172 4/172 1782 (05126201) 0364 1457
CAPE-BD29 3/39 7/35 0333 (00791407) 0135 1093
Overall 0926 (05761491) 0753 10000
B
Antidepressant (n/N) Placebo (n/N) OR (95% CI) p value Weight (%)
Yatham et al (2016)28 20/172 13/172 1609 (07733349) 0203 5745
CAPE-BD29 19/60 11/59 2022 (08634738) 0105 4255
Overall 1774 (10183091) 0043 10000
01 02 05 1 2 5 10
Placebo switch Antidepressant switch
Figure 4: Treatment-emergent aective switches
(A) Acute treatment. (B) 52 week extensions. OR=odds ratio.
in mood stabiliser trials (OR 0993 [07451324], p=0079) suggested publication bias. When considering
p=0964; RD 0030 [0021 to 0081]). 43 (45%) of the two studies with 52 week treatment extensions,28,29
96 receiving an antipsychotic plus an antidepressant adjunctive antidepressant therapy was associated with an
achieved remission criteria, compared with 116 (31%) of increased risk of treatment-emergent aective switch
380 patients treated with an antipsychotic and placebo. (39 [17%] of 232 vs 24 [10%] of 231; OR 1774 [10183091],
By contrast, in patients given a mood stabiliser, p=0043; RD 0053 [0004 to 0111], p=0070; number
remission rates were similar in those receiving an needed to harm 19; gure 4B).
antidepressant (35% [157 of 446]) and in those receiving Overall, 164 (30%) of 542 patients given antidepressants
placebo (35% [162 of 461]). Although Eggers and 323 (38%) of 841 those given placebo were lost to
intercept (175, t(4)=143, p=022) did not suggest follow-up (OR 0897 [06371262], p=0532; appendix).
publication bias, visual inspection of funnel plots There was evidence of heterogeneity between studies,
indicated a skewed distribution (appendix). with a Q statistic of 789 and I of 3668 (df=5, p=016).
The rates of acute treatment-emergent mania or In subgroup analysis, dropout rates were higher in
hypomania were available for all six studies; however, in antipsychotic trials (49% [231 of 476]) than in mood
one trial,29 such data were available for only half the stabiliser trials (28% [256 of 907]; Q=617, df=1,
participants because these data were not collected at one p=0013), mostly driven by dropouts in patients given
of the participating sites. Two studies28,29 had data for placebo plus antipsychotic (196 [52%] of 380). Funnel
52 week extensions of treatment. At the end of the acute plots revealed one outlier26 (appendix), but Eggers
phase of treatment, 33 (6%) of 521 patients given intercept (023, t(4)=016, p=087) did not suggest
antidepressants and 52 (6%) of 817 patients given placebo publication bias.
had episodes of treatment-emergent mania or hypomania,
and antidepressant therapy was not associated with an Discussion
increased risk of aective switch (OR 0926 [0576 to 1491], Although previous meta-analyses have examined the
p=0753; RD 0000 [0025 to 0026], p=0971; gure 4A). safety and ecacy of antidepressants in bipolar
Sensitivity analyses did not reveal eects of either the depression, the clinical relevance of their ndings is
STEP-BD trial13 (p=091) or the olanzapineuoxetine limited by the inclusion of studies of antidepressant
trial26 (p=073) on the risk of aective switch. Meta- monotherapy as well as tricyclic antidepressants and
regression did not show a signicant relation between risk inhibitors of monoamine oxidase. We restricted our
and study duration (Q=251, df=1, p=011). Heterogeneity analyses to randomised, placebo-controlled trials that
between studies was not signicant (Q=377, I=000, tested the ecacy of second-generation antidepressants
df=5, p=058), and subgroup analyses showed no versus placebo adjunctive to a mood stabiliser or an
statistical dierence between studies using a mood atypical antipsychotic. Therefore, our analyses provide
stabiliser or an antipsychotic (Q=009, df=1, p=075), data to inform not only ecacy but also the risk of
although interpretability of both is limited by the small treatment-emergent aective switches when following
number of studies. The asymmetrical funnel plot ISBD recommendations.14 Our ndings show that
(appendix) and Eggers intercept (148, t(4)=233, second-generation antidepressants, when used in
6 www.thelancet.com/psychiatry Published online October 26, 2016 http://dx.doi.org/10.1016/S2215-0366(16)30264-4
Articles
combination with a mood stabiliser or an atypical acceleration.37 Accordingly, although we did not identify
antipsychotic, have a signicant but small eect size a risk with time-limited use of adjuntive second-
and are not associated with notable acute mania or generation antidepressants, the risk of treatment-
hypomania switch risks. The small eect size did not emergent mania or hypomania increased with prolonged
translate into increased clinical response or remission; use (in 52 week placebo-controlled extensions) despite
however, we noted statistical separation for the adequate mood stabilisation (number needed to
subgroup of trials using an antidepressant as an adjunct harm 19).28,29 Thus, prolonged treatment might be
to an antipsychotic. detrimental, as reected in international guidelines5 and
With the exception of the STEP-BD trial,13 clinical recommendations from the British Association for
trials of acute bipolar depression are typically 68 weeks Psychopharmacology.38 However, this conclusion is
in duration. Therefore, to compute the mean change provisional and based on only two trials, and additional
in depressive symptoms for inclusion in our meta- investigation is needed.
analysis as a primary outcome, we extracted data from A limitation of our meta-analysis was the multiple
the 6 week double-blind period from the 26 week sources of diversity between the trials included
STEP-BD trial.13 Another important consideration when (dierent antidepressants, mood stabilisers, and
examining data from these trials is the high rates of antipsychotics, outcome metrics, and durations of
clinical remission and response in the placebo groups. study). Indeed, statistical heterogeneity was noted in
Indeed, in one 8 week randomised controlled trial,28 analyses of clinical response and remission, which
remission rate in the placebo group was as high seemed attributable to the use of mood stabilisers
as 53%.28 Remission rates of patients given placebo in versus antipsychotics. Unfortunately, the small number
trials of schizophrenia and depression have been of studies limited our exploration of clinical or
increasing.31,32 Although placebo responses are relatively methodological causes of heterogeneity beyond trials
stable in acute mania trials and do not seem to interfere using mood stabilisers and those using antipsychotics.
with detection of the ecacy of antimanic treatments, The study with the greatest antidepressant eect size26
placebo responses have been steadily increasing driving heterogeneity involved a washout period
in bipolar depression trials (similar to the situation followed by initiation of the study intervention, whereas
seen in trials of major depression),28,33,34 which the remainder trials all required stable psychotropics
substantially interfere with the detection of ecacy before trial commencement. One study29 had
signals. Therefore, strategies to address increasing incomplete data with respect to treatment-emergent
placebo response rates are urgently needed in trials aective switches in the acute phase. Our ndings
in psychiatry. should be interpreted in light of both type I and type II
The risk of short-term treatment-emergent aective errors, and the possible eects of multiple testing in
switches with antidepressant treatment in bipolar secondary outcomes. Dierential remission rates
depression is one of the most contentious issues in the between antipsychotic and mood stabiliser trials should
mood disorder literature. As has been highlighted,14 the be interpreted in light of the high dropout rate (>50%)
uctuant nature of mood in bipolar disorder makes in antipsychotic plus placebo trials.
the assignment of causality dicult. Yet, the use of The literature itself is subject to limitations, including
antidepressant monotherapy is clearly associated with an a small number of randomised controlled trials,
increased risk of mania6 and is discouraged by expert elevated placebo eects, and methodological exclusion
recommendations.14 Moreover, several agentsnotably, of patients with rapid cycling courses or comorbid
tricyclics, tetracyclics, and SNRIshave been associated substance use disorders. Furthermore, trials have not
with an increased risk of short-term treatment-emergent yet systematically addressed other important questions
aective switch.8,10,11,35 Although concern and caution with a double-blind design, such as the risk of
have spread to all antidepressants, other classes of depressive relapse with antidepressant discontinuation
antidepressants such as SSRIs and other antidepressants, in patients who respond to second-generation
such as bupropion, have not separated from placebo in antidepressants as an adjunct to mood stabilisers or
meta-analyses.10,36 antipsychotics. Such data might modify the risk-benet
Although additional trials are needed because the assessment of prophylactic treatment.
assumption of a class eect might ultimately prove Our meta-analysis of randomised placebo-controlled
erroneous, we did not nd an increased risk of trials of second-generation antidepressants in con-
short-term treatment-emergent aective switches with junction with a mood stabiliser or an antipsychotic in
adjunctive second-generation antidepressant therapy acute bipolar depression suggests that they have a small
during acute treatment of bipolar depression in this antidepressant eect, and short-term use of these
population with predominantly bipolar I disorder. medications is not associated with an increased risk of
However, denitions of treatment-emergent mania treatment-emergent aective switches. This supports
diered among the trials, and more sensitive measures rst-line recommendations by the joint guidelines of
could reveal changes and be best suited to identify cycle ISBD and the Canadian Network for Mood and Anxiety
www.thelancet.com/psychiatry Published online October 26, 2016 http://dx.doi.org/10.1016/S2215-0366(16)30264-4 7
Articles
Treatments (CANMAT).5 Antidepressants are well 8 Gijsman HJ, Geddes JR, Rendell JM, Nolen WA, Goodwin GM.
tolerated acutely, although subthreshold manic symptoms Antidepressants for bipolar depression: a systematic review of
randomized, controlled trials. Am J Psychiatry 2004; 161: 153747.
have not been adequately characterised. However, 9 Vazquez GH, Tondo L, Undurraga J, Baldessarini RJ.
antidepressants are accompanied by an increased risk for Overview of antidepressant treatment of bipolar depression.
manic or hypomanic episodes with prolonged use Int J Neuropsychopharmacol 2013; 16: 167385.
10 Sidor MM, Macqueen GM. Antidepressants for the acute treatment
and therefore only time-limited use is supported by of bipolar depression: a systematic review and meta-analysis.
our analysis. J Clin Psychiatry 2011; 72: 15667.
Contributors 11 Post RM, Altshuler LL, Leverich GS, et al. Mood switch in bipolar
depression: comparison of adjunctive venlafaxine, bupropion and
AM and LNY conceived the study. AM did the literature review and
sertraline. Br J Psychiatry 2006; 189: 12431.
statistical analyses, and drafted the report. AM, PAV, and LNY extracted
12 Nemero CB, Evans DL, Gyulai L, et al. Double-blind,
the data. All authors interpreted the data, and edited and approved the
placebo-controlled comparison of imipramine and paroxetine in
nal report. the treatment of bipolar depression. Am J Psychiatry 2001;
Declaration of interests 158: 90612.
AM is a Canadian Institutes of Health Research Vanier Scholar. PAV has 13 Sachs GS, Nierenberg AA, Calabrese JR, et al. Eectiveness of
received salary support through the Fund for Innovation and adjunctive antidepressant treatment for bipolar depression.
Competitiveness (FIC) of the Chilean Ministry of Economy, N Engl J Med 2007; 356: 171122.
Development and Tourism, through the Millennium Scientic Initiative 14 Pacchiarotti I, Bond DJ, Baldessarini RJ, et al. The International
(grant number IS130005). SNG has received research support from Society for Bipolar Disorders (ISBD) task force report on
Takeda and has consulted for Sunovion Pharmaceuticals. RWL has antidepressant use in bipolar disorders. Am J Psychiatry 2013;
170: 124962.
received funds for research (through the University of British Columbia)
from Brain Canada, Bristol-Myers Squibb, the Canadian Institutes of 15 Himmelhoch JM, Thase ME, Mallinger AG, Houck P.
Tranylcypromine versus imipramine in anergic bipolar depression.
Health Research, the Canadian Depression Research and Intervention
Am J Psychiatry 1991; 148: 91016.
Network, the Canadian Network for Mood and Anxiety Treatments,
16 Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane
Janssen, Lundbeck, the Movember Foundation, Pzer, St Jude Medical,
Collaborations tool for assessing risk of bias in randomised trials.
the University Health Network Foundation, and the Vancouver Coastal BMJ 2011; 343: d5928.
Health Research Institute; honoraria for advising or consulting from
17 Deeks JJ. Issues in the selection of a summary statistic for
Allergan, the Asia-Pacic Economic Cooperation, Bristol-Myers Squibb, meta-analysis of clinical trials with binary outcomes. Stat Med 2002;
the Canadian Depression Research and Intervention Network, the 21: 1575600.
Canadian Network for Mood and Anxiety Treatments, Janssen, 18 Montgomery SA, Asberg M. A new depression scale designed to be
Lundbeck, Medscape, Pzer, and Takeda; and honoraria for speaking sensitive to change. Br J Psychiatry 1979; 134: 38289.
from AstraZeneca, the Canadian Network for Mood and Anxiety 19 Hamilton M. A rating scale for depression.
Treatments, the Canadian Psychiatric Association, Lundbeck, the J Neurol Neurosurg Psychiatry 1960; 23: 5662.
Lundbeck Institute, and Otsuka. LNY has received research grants from 20 Sachs GS, Guille C, McMurrich SL. A clinical monitoring form for
AstraZeneca, Bristol-Myers Squibb, the Canadian Institutes of Health mood disorders. Bipolar Disord 2002; 4: 32327.
Research, the Canadian Network for Mood and Anxiety Treatments, 21 Riley RD, Higgins JP, Deeks JJ. Interpretation of random eects
Dainippon Sumitomo, Eli Lilly & Co, GlaxoSmithKline, Janssen, the meta-analyses. BMJ 2011; 342: d549.
Michael Smith Foundation for Health Research, Novartis, Pzer, Servier, 22 Fergusson D, Aaron SD, Guyatt G, Hebert P. Post-randomisation
and the Stanley Foundation. He has been on the advisory boards for exclusions: the intention to treat principle and excluding patients
AstraZeneca, Bristol-Myers Squibb, Dainippon Sumitomo, Eli Lilly & from analysis. BMJ 2002; 325: 65254.
Co, GlaxoSmithKline, Janssen, Lundbeck, Novartis, Pzer, Servier, and 23 Borenstein M, Hedges L, Higgins J, Rothstein H. Introduction to
Sunovion. He has been a speaker for AstraZeneca, Bristol-Myers Squibb, meta-analysis. West Sussex: Wiley & Sons, 2009.
the Canadian Network for Mood and Anxiety Treatments, Eli Lilly & Co, 24 Egger M, Davey Smith G, Schneider M, Minder C. Bias in
GlaxoSmithKline, Janssen, Pzer, Ranbaxy, and Sunovion. meta-analysis detected by a simple, graphical test. BMJ 1997;
315: 62934.
References
1 WHO. The global burden of disease: 2004 update. Geneva: 25 Cooper H, Hedges L, Valentine J. The handbook of research
World Health Organization, 2008. synthesis and meta-analysis. New York: Russell Sage Foundation
Publications, 2009.
2 Judd LL, Schettler PJ, Solomon DA, et al. Psychosocial disability
and work role function compared across the long-term course of 26 Tohen M, Vieta E, Calabrese J, et al. Ecacy of olanzapine and
bipolar I, bipolar II and unipolar major depressive disorders. olanzapine-uoxetine combination in the treatment of bipolar I
J Aect Disord 2008; 108: 4958. depression. Arch Gen Psychiatry 2003; 60: 107988.
3 Kupka RW, Altshuler LL, Nolen WA, et al. Three times more days 27 Shelton RC, Stahl SM. Risperidone and paroxetine given singly and
depressed than manic or hypomanic in both bipolar I and bipolar II in combination for bipolar depression. J Clin Psychiatry 2004;
disorder. Bipolar Disord 2007; 9: 53135. 65: 171519.
4 Perlis RH, Miyahara S, Marangell LB, et al. Long-term implications of 28 Yatham LN, Vieta E, Goodwin GM, et al. Agomelatine or placebo as
early onset in bipolar disorder: data from the rst 1000 participants in adjunctive therapy to a mood stabilizer in bipolar I depression:
the systematic treatment enhancement program for bipolar randomised double-blind placebo controlled trial.
disorder (STEP-BD). Biol Psychiatry 2004; 55: 87581. Br J Psychiatry 2016; 208: 7886.
5 Yatham LN, Kennedy SH, Parikh SV, et al. Canadian Network for 29 Ghaemi SN. Antidepressants in bipolar depression: an update.
Mood and Anxiety Treatments (CANMAT) and International Society 168th Annual Meeting of the American Psychiatric Association;
for Bipolar Disorders (ISBD) collaborative update of CANMAT Toronto, ON, Canada; May 1620, 2015.
guidelines for the management of patients with bipolar disorder: 30 Rosenthal R. Meta-analytic procedures for social research.
update 2013. Bipolar Disord 2013; 15: 144. Newbury Park, CA: Sage Publications, 1993.
6 Viktorin A, Lichtenstein P, Thase ME, et al. The risk of switch to 31 Bridge JA, Birmaher B, Iyengar S, Barbe RP, Brent DA.
mania in patients with bipolar disorder during treatment with an Placebo response in randomized controlled trials of antidepressants
antidepressant alone and in combination with a mood stabilizer. for pediatric major depressive disorder. Am J Psychiatry 2009;
Am J Psychiatry 2014; 171: 106773. 166: 4249.
7 Mauer S, Alahmari R, Vohringer PA, et al. International prescribing 32 Agid O, Siu CO, Potkin SG, et al. Meta-regression analysis of
patterns for mood illness: the International Mood Network (IMN). placebo response in antipsychotic trials, 19702010.
J Aect Disord 2014; 167: 13639. Am J Psychiatry 2013; 170: 133544.
8 www.thelancet.com/psychiatry Published online October 26, 2016 http://dx.doi.org/10.1016/S2215-0366(16)30264-4
Articles
33 Lombardo I, Sachs G, Kolluri S, Kremer C, Yang R. Two 6-week, 36 Peet M. Induction of mania with selective serotonin re-uptake
randomized, double-blind, placebo-controlled studies of ziprasidone inhibitors and tricyclic antidepressants. Br J Psychiatry 1994;
in outpatients with bipolar I depression: did baseline characteristics 164: 54950.
impact trial outcome? J Clin Psychopharmacol 2012; 32: 47078. 37 Berk M, Ng F, Dodd S, Goldberg JF, Malhi GS. Do we need to ick
34 Durgam S, Earley W, Lipschitz A, et al. An 8-week randomized, the switch? The need for a broader conceptualization of iatrogenic
double-blind, placebo-controlled evaluation of the safety and ecacy course aggravation in clinical trials of bipolar disorder.
of cariprazine in patients with bipolar I depression. Psychiatry Clin Neurosci 2010; 64: 36771.
Am J Psychiatry 2016; 173: 27181. 38 Goodwin GM, Haddad PM, Ferrier IN, et al. Evidence-based
35 Sachs GS, Lafer B, Stoll AL, et al. A double-blind trial of bupropion guidelines for treating bipolar disorder: revised third edition
versus desipramine for bipolar depression. J Clin Psychiatry 1994; recommendations from the British Association for
55: 39193. Psychopharmacology. J Psychopharmacol 2016; 30: 495553.
www.thelancet.com/psychiatry Published online October 26, 2016 http://dx.doi.org/10.1016/S2215-0366(16)30264-4 9
Vous aimerez peut-être aussi
- A Double-Blind, Placebo-Controlled Study of Quetiapine and Paroxetine As Monotherapy in Adults With Bipolar Depression (EMBOLDEN II)Document12 pagesA Double-Blind, Placebo-Controlled Study of Quetiapine and Paroxetine As Monotherapy in Adults With Bipolar Depression (EMBOLDEN II)HugoMattosPas encore d'évaluation
- The Catecholamines in Psychiatric and Neurologic DisordersD'EverandThe Catecholamines in Psychiatric and Neurologic DisordersPas encore d'évaluation
- Nejmoa 2300184Document11 pagesNejmoa 2300184Hector RivasPas encore d'évaluation
- Brady 2015Document15 pagesBrady 2015alfredoibcPas encore d'évaluation
- Embolden IDocument13 pagesEmbolden IAlejandra Campo MartinezPas encore d'évaluation
- Background: Lancet Psychiatry 2017Document11 pagesBackground: Lancet Psychiatry 2017Manya DhuparPas encore d'évaluation
- Pi Is 2215036616303789Document11 pagesPi Is 2215036616303789U of T MedicinePas encore d'évaluation
- Duração Terapia Adjuvante Com Antipsicótico Na Bipolaridade - YathamDocument7 pagesDuração Terapia Adjuvante Com Antipsicótico Na Bipolaridade - YathamLorrane NevesPas encore d'évaluation
- Clozapine For Treatment-Resistant Bipolar Disorder: A Systematic ReviewDocument14 pagesClozapine For Treatment-Resistant Bipolar Disorder: A Systematic ReviewAsepDarussalamPas encore d'évaluation
- Depresi Pada DMDocument1 pageDepresi Pada DMnigoPas encore d'évaluation
- Review ArticleDocument9 pagesReview ArticleMuhammad YanazPas encore d'évaluation
- PIIS2215036623002584Document12 pagesPIIS2215036623002584Dr. Nivas SaminathanPas encore d'évaluation
- Minociclina - Piloto 2018Document9 pagesMinociclina - Piloto 2018Merari Lugo OcañaPas encore d'évaluation
- Clozapine For Treatment-Resistant Bipolar Disorder: A Systematic ReviewDocument13 pagesClozapine For Treatment-Resistant Bipolar Disorder: A Systematic ReviewAsepDarussalamPas encore d'évaluation
- Treatment of Bipolar DisorderDocument20 pagesTreatment of Bipolar DisorderShana Wl100% (1)
- New England Journal Medicine: The ofDocument12 pagesNew England Journal Medicine: The ofwardahPas encore d'évaluation
- Bipolar 3 PDFDocument9 pagesBipolar 3 PDFPrecious Ann ParelPas encore d'évaluation
- A Randomized, Double-Blind, Placebo-Controlled Trial of Quetiapine in The Treatment of Bipolar I or II DepressionDocument10 pagesA Randomized, Double-Blind, Placebo-Controlled Trial of Quetiapine in The Treatment of Bipolar I or II DepressionSyifa FadyaPas encore d'évaluation
- Jamapsychiatry Buckman 2022 Oi 220004 1646792725.75755Document11 pagesJamapsychiatry Buckman 2022 Oi 220004 1646792725.75755SabrinaPas encore d'évaluation
- Trastorno Límite ChenDocument10 pagesTrastorno Límite ChenGabyMaría DelValle Cordero Gómez ⃝⃤Pas encore d'évaluation
- Single-Dose Synthetic Psilocybin With Psychotherapy For Treatment-Resistant Bipolar Type II Major Depressive EpisodesDocument8 pagesSingle-Dose Synthetic Psilocybin With Psychotherapy For Treatment-Resistant Bipolar Type II Major Depressive EpisodesPepa PIGPas encore d'évaluation
- Artigo InglesDocument11 pagesArtigo InglesEllen AndradePas encore d'évaluation
- Comentario Vieta MaDocument2 pagesComentario Vieta MaHelier FusterPas encore d'évaluation
- Treatment of Mania, Mixed State, and Rapid CyclingDocument9 pagesTreatment of Mania, Mixed State, and Rapid CyclingFernando PerezPas encore d'évaluation
- Canmat 2005 PDFDocument65 pagesCanmat 2005 PDFFábio C NetoPas encore d'évaluation
- Bel Maker 2007Document3 pagesBel Maker 2007VictorVicencioPas encore d'évaluation
- Bipolar Disord - 2023 P99-109. 2Document11 pagesBipolar Disord - 2023 P99-109. 2tnvkcwwwsjPas encore d'évaluation
- Feeling GreatDocument243 pagesFeeling GreatSunny LamPas encore d'évaluation
- Adjunctive Psychotherapy For Bipolar DisorderDocument10 pagesAdjunctive Psychotherapy For Bipolar DisorderAgustin NunezPas encore d'évaluation
- Nej MCP 2305428Document10 pagesNej MCP 2305428Josue LeivaPas encore d'évaluation
- Bdi 25 9Document16 pagesBdi 25 9NormanPas encore d'évaluation
- Jamapsychiatry Henssler 2022 Oi 210086 1644862555.37977Document13 pagesJamapsychiatry Henssler 2022 Oi 210086 1644862555.37977Juan JosePas encore d'évaluation
- Lee effectivenessofNonpharmacologicalInterventionsforTreatingPostStrokeDepressiveSymptomsSystematicReviewMetaanalysisofRCTs Topstrokerehab2020Document33 pagesLee effectivenessofNonpharmacologicalInterventionsforTreatingPostStrokeDepressiveSymptomsSystematicReviewMetaanalysisofRCTs Topstrokerehab2020dianaPas encore d'évaluation
- E Cacy of Modern Antipsychotics in Placebo-Controlled Trials in Bipolar Depression: A Meta-AnalysisDocument10 pagesE Cacy of Modern Antipsychotics in Placebo-Controlled Trials in Bipolar Depression: A Meta-AnalysisRisda AprilianiPas encore d'évaluation
- Journal of A Ffective Disorders: Research PaperDocument8 pagesJournal of A Ffective Disorders: Research PaperTrinanda ChoirunissaPas encore d'évaluation
- Combining Antidepressants Vs Antidepressant MonotherapyDocument13 pagesCombining Antidepressants Vs Antidepressant Monotherapyindah karyaPas encore d'évaluation
- 2022 Article 1757Document17 pages2022 Article 1757funny guyPas encore d'évaluation
- Psychedelics As MedicinesDocument12 pagesPsychedelics As MedicineswawawawemnPas encore d'évaluation
- 2016 - Ross, Et Al - Rapid and Sustained Symptom Reduction Following Psilocybin Treatment For Anxiety and Depressing in Patient With Life-Threatening CancerDocument16 pages2016 - Ross, Et Al - Rapid and Sustained Symptom Reduction Following Psilocybin Treatment For Anxiety and Depressing in Patient With Life-Threatening CancerEduardo BorgesPas encore d'évaluation
- Reprodutibilidade Da Eficácia Do Escitalopram em Pacientes Com Depressão Maior Anteriormente Remitidos Com EscitalopramDocument2 pagesReprodutibilidade Da Eficácia Do Escitalopram em Pacientes Com Depressão Maior Anteriormente Remitidos Com EscitalopramIratanFernandesPas encore d'évaluation
- Canmat Bipolar Treatment Olanzpaina RisperidonaDocument7 pagesCanmat Bipolar Treatment Olanzpaina RisperidonaGerardo TellezPas encore d'évaluation
- Ketamine Versus Midazolam in Bipolar Depression With Suicidal Thoughts: A Pilot Midazolam-Controlled Randomized Clinical TrialDocument8 pagesKetamine Versus Midazolam in Bipolar Depression With Suicidal Thoughts: A Pilot Midazolam-Controlled Randomized Clinical TrialDiane MxPas encore d'évaluation
- A Systematic Review of Nutraceuticals For The Treatment of Bipolar DisorderDocument12 pagesA Systematic Review of Nutraceuticals For The Treatment of Bipolar DisorderFikria Nawaf AuliaPas encore d'évaluation
- Gangguan BipolarDocument8 pagesGangguan BipolarjulianasanjayaPas encore d'évaluation
- Treatment Outcomes of Acute Bipolar Depressive Episode With PsychosisDocument9 pagesTreatment Outcomes of Acute Bipolar Depressive Episode With PsychosisMega LidwinaPas encore d'évaluation
- Declebck Smits 1999 Zolpidem A Valuable Alternative To Benzodiazepine Hypnotics For Chronic InsomniaDocument1 pageDeclebck Smits 1999 Zolpidem A Valuable Alternative To Benzodiazepine Hypnotics For Chronic InsomniaFábio Yutani KosekiPas encore d'évaluation
- Q&A ACV ManejoDocument7 pagesQ&A ACV ManejoAngélica Paola Almeida RodríguezPas encore d'évaluation
- Zhou 2020Document8 pagesZhou 2020Rosalía PattyPas encore d'évaluation
- Effectiveness of Videoconference-Delivered Cognitive Behavioral Therapy For Adults With Psychiatric Disorders: Systematic and Meta-Analytic ReviewDocument16 pagesEffectiveness of Videoconference-Delivered Cognitive Behavioral Therapy For Adults With Psychiatric Disorders: Systematic and Meta-Analytic ReviewlaiaPas encore d'évaluation
- Correspondence: The 341 737 Ways of Qualifying For The Melancholic SpecifierDocument2 pagesCorrespondence: The 341 737 Ways of Qualifying For The Melancholic SpecifierBetu SasuPas encore d'évaluation
- Bipolar Disorders - 2022 - Neuromodulacion en TAB MutzDocument16 pagesBipolar Disorders - 2022 - Neuromodulacion en TAB MutzLa Placa Pasquin Cemuc 2005Pas encore d'évaluation
- Appi Ajp 2014 13111517Document11 pagesAppi Ajp 2014 13111517witwiiwPas encore d'évaluation
- Antidepressants in Bipolar Depression: An Enduring ControversyDocument7 pagesAntidepressants in Bipolar Depression: An Enduring ControversyAgusPas encore d'évaluation
- Jiwa 3 PDFDocument7 pagesJiwa 3 PDFsondiPas encore d'évaluation
- Paper 2Document5 pagesPaper 2fernanda cornejoPas encore d'évaluation
- Tec 2022Document6 pagesTec 2022Diana RamosPas encore d'évaluation
- Brainsci 13 00909Document21 pagesBrainsci 13 00909Genis OnnaPas encore d'évaluation
- Tec 2022Document6 pagesTec 2022Diana RamosPas encore d'évaluation
- Jamapsychiatry Buckman 2022 Oi 220004 1651602243.58743Document11 pagesJamapsychiatry Buckman 2022 Oi 220004 1651602243.58743vedavathiPas encore d'évaluation
- Revista de Psicología Del Deporte 1132-239X: Issn: DPSSEC@ps - Uib.es, DPSSEC@uib - EsDocument8 pagesRevista de Psicología Del Deporte 1132-239X: Issn: DPSSEC@ps - Uib.es, DPSSEC@uib - EsSeleccion PersonalPas encore d'évaluation
- (Susan S. Levine) Loving Psychoanalysis TechniqueDocument165 pages(Susan S. Levine) Loving Psychoanalysis TechniqueLorenaUlloa100% (1)
- Brundin Et Al-2019-Acta Psychiatrica ScandinavicaDocument3 pagesBrundin Et Al-2019-Acta Psychiatrica ScandinavicaSeleccion PersonalPas encore d'évaluation
- Becoming A PsychotherapistDocument7 pagesBecoming A PsychotherapistSeleccion PersonalPas encore d'évaluation
- Dialnet ValidacionDelInventarioDeConductasParentales 2879538Document19 pagesDialnet ValidacionDelInventarioDeConductasParentales 2879538Seleccion Personal100% (2)
- Kantrowitz MatchDocument28 pagesKantrowitz MatchSeleccion PersonalPas encore d'évaluation
- Dialnet ValidacionDelInventarioDeConductasParentales 2879538Document18 pagesDialnet ValidacionDelInventarioDeConductasParentales 2879538Erick Escalante MPas encore d'évaluation
- Dialnet ValidacionDelInventarioDeConductasParentales 2879538Document18 pagesDialnet ValidacionDelInventarioDeConductasParentales 2879538Erick Escalante MPas encore d'évaluation
- Childhood Onset SchizophreniaDocument9 pagesChildhood Onset SchizophreniaSeleccion PersonalPas encore d'évaluation
- Childhood Adversity and PsichosisDocument12 pagesChildhood Adversity and PsichosisSeleccion PersonalPas encore d'évaluation
- Guia EsquizoDocument8 pagesGuia EsquizoSeleccion PersonalPas encore d'évaluation
- The History of Benzodiazepines: in PracticeDocument10 pagesThe History of Benzodiazepines: in PracticeKairo AlbernazPas encore d'évaluation
- Fact Sheet Final Ruth Venegas 2017 5Document1 pageFact Sheet Final Ruth Venegas 2017 5api-356468876Pas encore d'évaluation
- Course Title: Cdi 8 Vice and Drug Education and Control COURSE DESCRIPTION: This Course Will Talk About The Different Kinds of Human VicesDocument3 pagesCourse Title: Cdi 8 Vice and Drug Education and Control COURSE DESCRIPTION: This Course Will Talk About The Different Kinds of Human VicesHilron Diokno0% (1)
- Forensic Chemistry & Toxicology Dangerous DrugsDocument17 pagesForensic Chemistry & Toxicology Dangerous DrugsKeano AnanayoPas encore d'évaluation
- Lowinson and Ruiz's Substance Abuse A Comprehensiv... - (SECTION 8 MODELS OF PREVENTION)Document23 pagesLowinson and Ruiz's Substance Abuse A Comprehensiv... - (SECTION 8 MODELS OF PREVENTION)Bareeha AhmedPas encore d'évaluation
- The Addiction Casebook - Chap 04Document11 pagesThe Addiction Casebook - Chap 04Glaucia MarollaPas encore d'évaluation
- Drug Abuse PreventionDocument1 pageDrug Abuse PreventionAllain ChristopherPas encore d'évaluation
- Buy 4mmc Mephedrone Miaow Miaow Meow Meow Mkat Mcat BubblesDocument3 pagesBuy 4mmc Mephedrone Miaow Miaow Meow Meow Mkat Mcat Bubbleschemicals_uk201033% (3)
- 5 Reel World Brands Inc 2919 30STGE230119 Strawberry GelatoDocument1 page5 Reel World Brands Inc 2919 30STGE230119 Strawberry GelatoTiffany BarnesPas encore d'évaluation
- 2.0 Drug Statistics and TrendsDocument108 pages2.0 Drug Statistics and TrendsAnkita Kaliraman100% (1)
- Sinaloa Cartel Press ChartDocument1 pageSinaloa Cartel Press ChartcairePas encore d'évaluation
- NJ Mpje PDFDocument168 pagesNJ Mpje PDFPatrick Mata100% (3)
- Narcotics and Antimigraine Agents (AE, Drug-Drug Interactions)Document5 pagesNarcotics and Antimigraine Agents (AE, Drug-Drug Interactions)ShiraishiPas encore d'évaluation
- Chemical DiversionDocument20 pagesChemical Diversionjwiz007Pas encore d'évaluation
- A Fatal Intoxication Following The Ingestion of AyahuascaDocument4 pagesA Fatal Intoxication Following The Ingestion of AyahuascaPaula Polvora VictoriaPas encore d'évaluation
- Paradigm Shift EssayDocument15 pagesParadigm Shift Essayapi-608886638Pas encore d'évaluation
- Legalizing Marijuana: Utilitarian ViewpointDocument3 pagesLegalizing Marijuana: Utilitarian ViewpointGiselle LisondraPas encore d'évaluation
- Mislim To Je ToDocument2 pagesMislim To Je ToIslami IsmailPas encore d'évaluation
- Opioids AutacoidsDocument22 pagesOpioids AutacoidsSiddharth Anand80% (5)
- Suboxone - Notes For PharmacistsDocument1 pageSuboxone - Notes For Pharmacistsgarima_montuPas encore d'évaluation
- Granny Storm Crowns ListDocument750 pagesGranny Storm Crowns ListMichael Grant WhitePas encore d'évaluation
- Alcohol & DrugsDocument17 pagesAlcohol & DrugsLECHUPas encore d'évaluation
- AnxiolyticsDocument10 pagesAnxiolyticsSharon PanaderoPas encore d'évaluation
- Nama-Nama Obat PrekurDocument2 pagesNama-Nama Obat PrekurWatini Daiman Fii QolbyPas encore d'évaluation
- Final - Narcotic Drugs and Psychotropic Substance Usage in HospitalDocument23 pagesFinal - Narcotic Drugs and Psychotropic Substance Usage in HospitalJAGDISH SAINIPas encore d'évaluation
- CH11. Substance-Related Disorders PDFDocument44 pagesCH11. Substance-Related Disorders PDFAngie morenoPas encore d'évaluation
- Clinical Handbook of Psychotropic Drugs, 25e (May 8, 2023) - (0889376328) - (Hogrefe Publishing) (Etc.) (Z-Library)Document555 pagesClinical Handbook of Psychotropic Drugs, 25e (May 8, 2023) - (0889376328) - (Hogrefe Publishing) (Etc.) (Z-Library)Dragutin PetrićPas encore d'évaluation
- R A-6425Document76 pagesR A-6425Lovely Ann Ayapana100% (1)
- Ketamine For Opiate WithdrawalDocument3 pagesKetamine For Opiate WithdrawalroboPas encore d'évaluation
- MCQ-Multimedia Test 6th Periodical With Key, Mon July 22, 2019 (KEY)Document37 pagesMCQ-Multimedia Test 6th Periodical With Key, Mon July 22, 2019 (KEY)Amara AsifPas encore d'évaluation
- The Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeD'EverandThe Upward Spiral: Using Neuroscience to Reverse the Course of Depression, One Small Change at a TimeÉvaluation : 4.5 sur 5 étoiles4.5/5 (140)
- Summary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDD'EverandSummary of The Body Keeps the Score: Brain, Mind, and Body in the Healing of Trauma by Bessel van der Kolk MDÉvaluation : 4.5 sur 5 étoiles4.5/5 (167)
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisD'EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisÉvaluation : 4 sur 5 étoiles4/5 (9)
- Rewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryD'EverandRewire Your Anxious Brain: How to Use the Neuroscience of Fear to End Anxiety, Panic, and WorryÉvaluation : 4.5 sur 5 étoiles4.5/5 (157)
- Somatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionD'EverandSomatic Therapy Workbook: A Step-by-Step Guide to Experiencing Greater Mind-Body ConnectionPas encore d'évaluation
- My Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesD'EverandMy Grandmother's Hands: Racialized Trauma and the Pathway to Mending Our Hearts and BodiesÉvaluation : 5 sur 5 étoiles5/5 (70)
- An Autobiography of Trauma: A Healing JourneyD'EverandAn Autobiography of Trauma: A Healing JourneyÉvaluation : 5 sur 5 étoiles5/5 (2)
- Don't Panic: Taking Control of Anxiety AttacksD'EverandDon't Panic: Taking Control of Anxiety AttacksÉvaluation : 4 sur 5 étoiles4/5 (12)
- The Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeD'EverandThe Complex PTSD Workbook: A Mind-Body Approach to Regaining Emotional Control & Becoming WholeÉvaluation : 4.5 sur 5 étoiles4.5/5 (49)
- Heal the Body, Heal the Mind: A Somatic Approach to Moving Beyond TraumaD'EverandHeal the Body, Heal the Mind: A Somatic Approach to Moving Beyond TraumaÉvaluation : 4.5 sur 5 étoiles4.5/5 (56)
- How to Be Miserable: 40 Strategies You Already UseD'EverandHow to Be Miserable: 40 Strategies You Already UseÉvaluation : 4.5 sur 5 étoiles4.5/5 (57)
- Rapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreD'EverandRapid Weight Loss Hypnosis: How to Lose Weight with Self-Hypnosis, Positive Affirmations, Guided Meditations, and Hypnotherapy to Stop Emotional Eating, Food Addiction, Binge Eating and MoreÉvaluation : 5 sur 5 étoiles5/5 (17)
- Summary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisD'EverandSummary: No Bad Parts: Healing Trauma and Restoring Wholeness with the Internal Family Systems Model by Richard C. Schwartz PhD & Alanis Morissette: Key Takeaways, Summary & AnalysisÉvaluation : 5 sur 5 étoiles5/5 (5)
- Critical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsD'EverandCritical Thinking: How to Effectively Reason, Understand Irrationality, and Make Better DecisionsÉvaluation : 4.5 sur 5 étoiles4.5/5 (39)
- The Worry Trick: How Your Brain Tricks You into Expecting the Worst and What You Can Do About ItD'EverandThe Worry Trick: How Your Brain Tricks You into Expecting the Worst and What You Can Do About ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (107)
- Brain Inflamed: Uncovering the Hidden Causes of Anxiety, Depression, and Other Mood Disorders in Adolescents and TeensD'EverandBrain Inflamed: Uncovering the Hidden Causes of Anxiety, Depression, and Other Mood Disorders in Adolescents and TeensÉvaluation : 5 sur 5 étoiles5/5 (2)
- Redefining Anxiety: What It Is, What It Isn't, and How to Get Your Life BackD'EverandRedefining Anxiety: What It Is, What It Isn't, and How to Get Your Life BackÉvaluation : 4.5 sur 5 étoiles4.5/5 (152)
- BORDERLINE PERSONALITY DISORDER: Help Yourself and Help Others. Articulate Guide to BPD. Tools and Techniques to Control Emotions, Anger, and Mood Swings. Save All Your Relationships and Yourself. NEW VERSIOND'EverandBORDERLINE PERSONALITY DISORDER: Help Yourself and Help Others. Articulate Guide to BPD. Tools and Techniques to Control Emotions, Anger, and Mood Swings. Save All Your Relationships and Yourself. NEW VERSIONÉvaluation : 4.5 sur 5 étoiles4.5/5 (24)
- The Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouD'EverandThe Autoimmune Cure: Healing the Trauma and Other Triggers That Have Turned Your Body Against YouPas encore d'évaluation
- Winning the War in Your Mind: Change Your Thinking, Change Your LifeD'EverandWinning the War in Your Mind: Change Your Thinking, Change Your LifeÉvaluation : 5 sur 5 étoiles5/5 (559)
- A Profession Without Reason: The Crisis of Contemporary Psychiatry—Untangled and Solved by Spinoza, Freethinking, and Radical EnlightenmentD'EverandA Profession Without Reason: The Crisis of Contemporary Psychiatry—Untangled and Solved by Spinoza, Freethinking, and Radical EnlightenmentPas encore d'évaluation
- I Don't Want to Talk About It: Overcoming the Secret Legacy of Male DepressionD'EverandI Don't Want to Talk About It: Overcoming the Secret Legacy of Male DepressionÉvaluation : 4.5 sur 5 étoiles4.5/5 (106)
- Binaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationD'EverandBinaural Beats: Activation of pineal gland – Stress reduction – Meditation – Brainwave entrainment – Deep relaxationÉvaluation : 5 sur 5 étoiles5/5 (9)
- Anxious for Nothing: Finding Calm in a Chaotic WorldD'EverandAnxious for Nothing: Finding Calm in a Chaotic WorldÉvaluation : 4.5 sur 5 étoiles4.5/5 (1245)