Académique Documents
Professionnel Documents
Culture Documents
Kelompok 5 Seizure and Prograsive Weakness
Transféré par
prabuCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Kelompok 5 Seizure and Prograsive Weakness
Transféré par
prabuDroits d'auteur :
Formats disponibles
The n e w e ng l a n d j o u r na l of m e dic i n e
case records of the massachusetts general hospital
Founded by Richard C. Cabot
Eric S. Rosenberg, M.D., Editor Nancy Lee Harris, M.D., Editor
Jo-Anne O. Shepard, M.D., Associate Editor Alice M. Cort, M.D., Associate Editor
Sally H. Ebeling, Assistant Editor Emily K. McDonald, Assistant Editor
Case 34-2014: A 7-Year-Old Boy with Focal
Seizures and Progressive Weakness
Ronald L. Thibert, D.O., M.S.P.H., Ann-Christine Duhaime, M.D.,
Paul A. Caruso, M.D., and Anat Stemmer-Rachamimov, M.D.
Pr e sen tat ion of C a se
Dr. Michael Ho (Neurology): A 7-year-old boy was evaluated in an outpatient clinic at From the Departments of Neurology
this hospital because of focal seizures and progressive right-sided weakness. (R.L.T.), Neurosurgery (A.-C.D.), Radiol
ogy (P.A.C.), and Pathology (A.S.-R.),
The patient had been well until 18 months earlier, when intermittent shaking Massachusetts General Hospital, and the
of his right hand developed, which quickly progressed to involve the entire right Departments of Neurology (R.L.T.), Neuro
arm. Evaluation at another hospital included electroencephalography (EEG) that surgery (A.-C.D.), Radiology (P.A.C.), and
Pathology (A.S.-R.), Harvard Medical
revealed frequent left-sided discharges, magnetic resonance imaging (MRI) of the School both in Boston.
head that revealed no clear atrophy but a lesion in the left motor strip, and a lum-
N Engl J Med 2014;371:1737-46.
bar puncture with normal results on cerebrospinal fluid analysis. A diagnosis of DOI: 10.1056/NEJMcpc1305993
focal motor seizures was made; levetiracetam and glucocorticoids were adminis- Copyright 2014 Massachusetts Medical Society.
tered. Approximately 2 months after the onset of symptoms, twitching of the arm
and hand became nearly constant and was accompanied by facial twitching; a
clinical diagnosis of epilepsia partialis continua was made. Intravenous immune
globulin was administered, and the twitching in his face and arm almost com-
pletely resolved. Approximately 3 months later, however, the symptoms recurred.
During the year before this evaluation, the right arm and the right side of the
face began to twitch nearly continuously, with more intense focal clonic activity
occurring 2 to 20 times per day; there was associated progressive weakness of the
muscles of the right arm (more severe distally than proximally) and the right side
of the face, increasing spasticity in the fingers and wrist, and subtle weakness of
the right leg. There was no history of loss of consciousness, apnea, cyanosis, or
seizure activity involving the left side. MRI studies of the head that were performed
between 9 months and 3 months before this evaluation reportedly revealed a T2-
weighted hyperintense lesion in the left motor strip involving the adjacent white
matter and, in more recent studies, the parietal region, with no clear evidence of
atrophy. A brain biopsy was recommended. The family sought a second opinion at
this hospital.
The patient was born at 36 weeks of gestation after the onset of preterm labor
and had normal or advanced developmental milestones (including reading at 3 years
of age). He had reactive airway disease and had undergone tonsillectomy, adenoid-
ectomy, and urologic surgery. Medications included levetiracetam (800 mg twice
n engl j med 371;18nejm.orgoctober 30, 2014 1737
The New England Journal of Medicine
Downloaded from nejm.org on November 25, 2015. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
daily), clonazepam (0.5 mg in the morning and somatosensory-evoked magnetic fields in the
1 mg in the evening), oxcarbazepine (360 mg in left hemisphere, findings suggestive of cortical
the morning and 420 mg in the evening), val- dysfunction. During the MEG recording, there
proic acid (375 mg twice daily), lipoic acid, vita- was continuous right facial twitching and some
min B6, and coenzyme Q10. Immunizations were evidence that the right hemisphere was domi-
current. He had no known drug allergies. He nant for language.
consumed a ketogenic diet (a high-fat, low-carbo- Three months later, the patient was admitted
hydrate diet), which helped to control his sei- to this hospital. A 24-hour EEG showed that the
zures, and he participated in occupational and focus of his continuous right facial twitching was
physical therapy. He lived with his parents and in the left frontal area, with a broad electrical
older sibling, was in second grade, and did well field involving the entire left hemisphere. EEG
academically. His mother and sibling had atten- also recorded six generalized tonicclonic sei-
tion deficithyperactivity disorder, a paternal aunt zures characterized by spike-and-wave discharges
had bipolar disorder, and other paternal relatives (1 to 2 Hz); the site of maximal amplitude was
had depression. the midline central region, and the duration was
On examination, the patient was awake, alert, approximately 15 to 40 seconds.
and pleasant. His speech was clear and fluent, The next day, a diagnostic procedure was per-
with mild dysarthria. He seemed to be intelligent, formed.
with good social skills. The pupils and extra-
ocular movements were normal. There was weak- Differ en t i a l Di agnosis
ness on the right side of the face, the palate was
elevated symmetrically, and the tongue protruded Dr. Paul A. Caruso: The neuroimaging studies re-
along the midline. There was nearly continuous veal the following two principal pathological fea-
twitching of the right lower facial muscles. tures: progressive atrophy in the left cerebral
Muscle bulk, tone, and strength were normal in hemisphere, and a focal lesion that raises the
the left arm and leg. In the right arm, strength possibility of focal cortical dysplasia or inflam-
was 4/5 proximally, with little movement of the mation. The progressive atrophy in the left cere-
fingers or wrist and distal-muscle spasticity. bral hemisphere is seen on the series of axial
Strength in the right leg was 4+/5, with slightly T2-weighted images obtained when the patient
increased reflexes. The gait was mildly hemipa- was between 6 years of age and 8 years of age
retic. A brain biopsy was recommended, and the (Fig. 1). During this period, the left inferior, mid-
family resumed care at the other hospital. dle, and superior frontal sulci and left parieto-
During the next 6 months, twitching was occipital sulci enlarge progressively and the un-
constant in the right side of the face and nearly derlying cortex thins segmentally, findings that
continuous in the right arm. The focal seizures reflect progressive cortical atrophy and loss of
in the right side of the face and right arm and white-matter volume.
leg (which frequently caused the patient to fall) The focal lesion with high signal intensity
occurred up to 20 times daily when he was tired that is seen on T2-weighted images (Fig. 2A)
or sick or had not adhered to his diet. Weakness involves the left precentral and postcentral gyral
of the right leg and arm increased, and his gait cortex (including the motor strip) and subcorti-
became more hemiparetic, despite continued cal white matter, and trails radially through the
medical therapy with levetiracetam, clonazepam, deep white matter toward the left lateral ventri-
oxcarbazepine, and valproic acid and general cle; these features are suggestive of focal cortical
adherence to the ketogenic diet. dysplasia. Magnetic resonance spectroscopy that
Six months after the initial evaluation at this was performed over the lesion (Fig. 2B) reveals
hospital, the patient returned to this hospital for a decrease in the ratio of N-acetylaspartate to
care. Magnetoencephalography (MEG) revealed creatine but no increase in the ratio of choline
seizure activity in the left frontal lobe, with dis- to creatine, features that may also be associated
charges predominantly in the posterior left fron- with focal cortical dysplasia.
tal cortex, along the frontal operculum of the MEG was performed to evaluate the distribu-
motor cortex (precentral gyrus) and the area as- tion of epileptogenic foci in the left cerebral
sociated with control of the hand, and abnormal hemisphere. MEG is a neuroimaging technique
1738 n engl j med 371;18nejm.orgoctober 30, 2014
The New England Journal of Medicine
Downloaded from nejm.org on November 25, 2015. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
case records of the massachuset ts gener al hospital
A B C
D E F
Figure 1. MRI Scans of the Head at 6, 7, and 8 Years of Age.
A series of axial T2 -weighted images were taken from MRI studies of the head that were performed when the patient
was 6 years of age (Panels A and B), 7 years of age (Panels C and D), and 8 years of age (Panels E and F). Progressive
enlargement of the cerebral sulci and contraction of the gyri in the left cerebral hemisphere are shown at the level of
the cerebral peduncles (Panels A, C, and E) and at the level of the lateral ventricles (Panels B, D, and F); these pro-
gressive findings are consistent with atrophy in the left cerebral hemisphere.
that uses biomagnetism to produce an image of of refractory epilepsy is very broad, so this dis-
the brain. As a result of the behavior described cussion will focus on the differential diagnosis
by Maxwells equations, electric currents induce of this patients specific seizure type, which is
orthogonally directed magnetic fields. MEG uses rare in children. His clinical seizure activity is
the magnetic fields induced by cerebral neuronal most consistent with epilepsia partialis continua,
electric currents to determine the location of which is defined as almost continuous regular
electric (neuronal) activity in the brain. The elec- or irregular muscular clonic twitching affecting
tric activity is represented as equivalent dipoles a limited part of the body.1 Consciousness is
(see blue dots and dashes in Fig. 1 in the typically preserved, and the twitching most
Supplementary Appendix, available with the full commonly involves the face, arms, or both.
text of this article at NEJM.org). In this case, According to the definition of epilepsia partialis
MEG shows that the magnetic dipoles overlap continua, the twitching must last at least 1 hour
but cluster mostly lateral and inferior to the (but may last hours or years) and the twitches
focal lesion in the atrophied left cerebral hemi- must occur at least once every 10 seconds, typi-
sphere. cally in isolation or in clusters of 1 to 2 Hz.
Dr. Ronald L. Thibert: The differential diagnosis The differential diagnosis for epilepsia parti-
n engl j med 371;18 nejm.org october 30, 2014 1739
The New England Journal of Medicine
Downloaded from nejm.org on November 25, 2015. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
A Table 1. Differential Diagnosis of Epilepsia Partialis
Continua.*
Nonprogressive causes
Vascular causes (stroke, cerebral venous sinus throm-
bosis)
Metabolic causes (hyperosmolar hyperglycemic non-
ketotic syndrome, hyponatremia)
Neoplasm (central nervous system neoplasm or
hematologic neoplasm)
Infectious or immunologic causes (human immuno-
deficiency virus, encephalitis)
Cortical dysplasia
Mitochondrial causes or inborn error of metabolism
Perinatal central nervous system injury
B Cryptogenic causes
Progressive cause
Rasmussens encephalitis
* Data are from Sinha and Satishchandra,2 Phabphal et al.,3
and Kravljanac et al.4
On the basis of this patients clinical presen-
tation and neuroimaging studies, the two most
likely causes of the epilepsia partialis continua
Figure 2. Imaging Studies of the Head at 7 Years of Age. are Rasmussens encephalitis and cortical dys-
A coronal fluid-attenuated inversion recovery (FLAIR) plasia. Rasmussens encephalitis, which was
image from MRI performed at 7 years of age (Panel A) first described in 1958 by Dr. Theodore Ras-
shows a lesion with high signal intensity (arrows) in mussen, is a progressive neurologic disease of
the precentral and postcentral gyri that involves the unknown cause (Table 2). Patients typically
cortex and subcortical white matter and trails infero-
present in childhood with focal-onset seizures,
medially toward the left lateral ventricle, features that
are suggestive of focal cortical dysplasia. Multivoxel which then progress over a period of months to
magnetic resonance spectroscopy performed over the refractory epilepsy with progressive hemiparesis.
lesion at an echo time of 288 msec (Panel B) reveals a Epilepsia partialis continua develops in approxi-
decrease in the ratio of N-acetylaspartate to creatine mately 50 to 90% of persons with Rasmussens
(arrows) but no increase in the ratio of choline to creatine.
encephalitis, and fixed hemiparesis typically oc-
curs within 2 to 3 years after the onset of sei-
zures. Seizures are typically refractory to medi-
alis continua is divided into nonprogressive and cation, as was the case with this patient, but
progressive causes (Table 1); this patients clini- glucocorticoids and intravenous immune globu-
cal presentation is most consistent with a pro- lin can be effective in controlling seizures.
gressive process. Much of the literature on epi- Various other immunosuppressive medications
lepsia partialis continua focuses on adults, but a have been tried, but the most effective therapy
recent study involving 51 children with epilepsia remains hemispherectomy.
partialis continua4 showed that Rasmussens This patient had normal development before
encephalitis was the most common cause, with the onset of symptoms and no other symptoms
other common causes including immune or in- of metabolic disease or infection; therefore, the
flammatory processes (e.g., acute and subacute most likely cause of epilepsia partialis continua
encephalitis and subacute sclerosing panenceph- in this patient is Rasmussens encephalitis or
alitis), metabolic disorders (e.g., mitochondrial cortical dysplasia. Malformations of cortical
disease and neuronal ceroid lipofuscinosis), cor- development are present at birth and often cause
tical malformations, and vascular causes. refractory epilepsy, but they do not typically lead
1740 n engl j med 371;18 nejm.org october 30, 2014
The New England Journal of Medicine
Downloaded from nejm.org on November 25, 2015. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
case records of the massachuset ts gener al hospital
to progressive hemiparesis. In some cases, how-
Table 2. Diagnostic Criteria for Rasmussens Encephalitis.*
ever, dysplasia can mimic Rasmussens encepha-
litis and can cause motor symptoms when the Part A (all three)
motor strip is involved. Focal seizures (with or without epilepsia partialis
In patients with epilepsia partialis continua, continua) and unilateral cortical deficits
interictal activity on EEG typically consists of On EEG: unilateral hemispheric slowing (with or
focal or generalized background slowing and without epileptiform activity) and unilateral
seizure onset
focal or multifocal epileptiform discharges, in
On MRI: unilateral hemispheric progressive cortical
some cases periodic lateralized epileptiform dis- atrophy and one of the following findings
charges. Ictal activity on EEG is variable and
Hyperintense signal abnormality or atrophy of
may consist of focal slowing, rhythmic spike- ipsilateral caudate head
and-wave activity, or an electrodecrement (an epi-
Gray- or white-matter hyperintensity on T2-weighted
sode of voltage attenuation occurring at the same FLAIR images
time as an epileptic spasm).6 Part B (two of three)
On EEG, Rasmussens encephalitis is typi-
Epilepsia partialis continua or progressive cortical
cally manifested by slowing and attenuation in deficits
the affected hemisphere, with multifocal dis-
On MRI: unilateral hemispheric progressive cortical
charges confined to the same hemisphere. A re- atrophy
cent study comparing the EEG findings associ- One of the following groups of histopathological
ated with Rasmussens encephalitis with the features:
EEG findings associated with cortical dysplasia7 T-celldominated encephalitis with activated
showed no marked differences between the two, microglial cells (typically but not necessarily
but it showed that slowing in one hemisphere is forming nodules) and reactive astrogliosis
typical among persons with Rasmussens en- Numerous parenchymal macrophages (B cells,
plasma cells, or viral inclusion bodies rule out a
cephalitis and that there is a higher prevalence diagnosis of Rasmussens encephalitis)
of contralateral discharges among persons with
Rasmussens encephalitis than among persons * These diagnostic criteria were described in the 2005
with cortical dysplasia. Furthermore, the contra- European Consensus Statement by Bien et al.5 Diagnosis
requires that the criteria in either Part A or Part B be met.
lateral discharges were predictive of cognitive EEG denotes electroencephalogram, and FLAIR fluid-
decline, and it was suggested that contralateral attenuated inversion recovery.
discharges could be an indication for resective
surgery. This patient has focal slowing that is
clearly located in the left hemisphere and most
DR . RONA L D L . THIBER T S
prominent in the left frontocentral region, with DI AGNOSIS
some spread to the vertex and the right fronto-
central region (Fig. 2 in the Supplementary Rasmussens encephalitis, possibly with cortical
Appendix). These findings are suggestive of dysplasia.
Rasmussens encephalitis but could still be con-
sistent with cortical dysplasia in the left fronto- Pathol o gic a l Discussion
central region.
It is possible that this patient has both Ras Dr. Anat Stemmer-Rachamimov: Pathological exami-
mussens encephalitis and cortical dysplasia. In nation of a biopsy specimen of the left frontal
one case series involving seven patients8 and in lobe reveals a single small focus of intracortical
individual case reports,9,10 there is histologic chronic inflammation composed predominantly
evidence of coexisting cortical dysplasia and of CD3+ T cells scattered in the parenchyma and
Rasmussens encephalitis, but it is still unclear clustered around small blood vessels (Fig. 3A
whether these cases represent two distinct pro- and 3B). In addition, immunohistochemical
cesses. Case reports and series have also docu- staining for CD68 and CD163 reveals focal,
mented Rasmussens encephalitis with coexist- marked microglial activation (Fig. 3C). These
ing anaplastic astrocytoma, ganglioglioma, and findings are associated with reactive gliosis, fo-
findings suggestive of the tuberous sclerosis cal neuronophagia, and loss of individual neu-
complex.11,12 rons from an otherwise well-laminated cerebral
n engl j med 371;18nejm.orgoctober 30, 2014 1741
The New England Journal of Medicine
Downloaded from nejm.org on November 25, 2015. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
A B
C D
E F
Figure 3. Biopsy and Resection Specimens of the Left Frontal Lobe.
Hematoxylin and eosin staining of the biopsy specimen shows increased cellularity in the cortex due to lymphocytic
infiltrates (Panel A). Immunohistochemical staining of the biopsy specimen for CD3 reveals that most of the lym-
phocytes are CD3+ T cells (Panel B). Immunohistochemical staining of the biopsy specimen for CD68 reveals prom-
inent microglial activation (Panel C), and immunohistochemical staining of the resection specimen for CD68 reveals
microglial nodules (Panel D). Immunohistochemical staining of the resection specimen for glial fibrillary acidic pro-
tein (GFAP) highlights many intracortical reactive astrocytes (Panel E). Immunohistochemical staining for neuronal
nuclei in an area of the resection specimen that was considered suspicious for cortical dysplasia on imaging studies
shows normal cortical lamination (Panel F).
cortex. There is no evidence of cortical dysplasia Discussion of M a nagemen t
or other malformations. These findings are not
specific for Rasmussens encephalitis, but in the Dr. Ann-Christine Duhaime: Making the decision to
appropriate clinical context, they would be con- perform surgery for the treatment of intractable
sistent with the diagnosis. epilepsy requires weighing the potential risks
1742 n engl j med 371;18 nejm.org october 30, 2014
The New England Journal of Medicine
Downloaded from nejm.org on November 25, 2015. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
case records of the massachuset ts gener al hospital
against the potential benefits. We need to pay undergo resection of the rolandic cortex because
specific attention to how definitively we can lo- of congenital problems have some weakness but
calize the seizure-onset zone and how reliably we preservation of most other functions. After a
can predict the deficits that will result from re- patient has undergone anatomical hemispherec-
section of that zone. In this patient, the differen- tomy or hemispheric disconnection, the long-
tial diagnosis of the seizures includes Rasmus- term outcome typically includes spastic hemiple-
sens encephalitis, focal cortical dysplasia, and a gia with return of ambulation (patients can walk
combination of both conditions. but have a spastic-type limp), development of a
In patients with intractable epilepsia partialis helper arm without fine motor manipulative
continua that arises from an area of focal corti- abilities (patients can use the arm to help lift
cal dysplasia, control of seizures generally re- objects but cannot perform fine motor functions
quires resection of as much of that area as pos- with the hand), permanent hemianopsia, and
sible.13,14 Risks in this situation depend on the various degrees of language and cognitive func-
function of that area of the brain and of the area tion (depending on preoperative status and age
immediately surrounding the dysplastic tissue. If at surgery).
dysplasia is located in the rolandic area (the In this case, in order to decide whether to
motor area of the cerebral cortex that is just perform focal resection of the region containing
anterior to the central sulcus and accounts for the abnormality that was seen on fluid-attenuated
part of the precentral gyrus), as in this case, inversion recovery (FLAIR) MRI imaging or to
contralateral weakness or paralysis is the ex- perform hemispheric disconnection, we had to
pected outcome of complete resection of the af- determine whether the patient was more likely
fected tissue. to have focal cortical dysplasia or Rasmussens
In contrast, treatment of Rasmussens en- encephalitis, on the basis of the course of the
cephalitis requires removal or disconnection of disease, EEG findings, and radiologic evaluation.
the entire affected hemisphere. Focal resection We favored a diagnosis of Rasmussens encepha-
has not been shown to be effective in the treat- litis, but we could not rule out focal cortical
ment of this disorder, but hemispheric proce- dysplasia. In a case like this one, in which the
dures are associated with a high rate of success seizure-onset zone cannot be determined by
in stopping seizures and also halting progres- noninvasive means, surgical implantation of in-
sion of the disease. Over time, a number of tracranial electrodes for direct monitoring of the
techniques have been developed to accomplish brain parenchyma over a period of days or weeks
this goal, ranging from complete anatomical is the typical strategy. However, in this case, we
hemispherectomy to newer, less extensive proce- decided to use an approach that involved multi-
dures that disconnect the affected hemisphere ple methods in an attempt to determine, during
from the opposite hemisphere and from the re- a single operation, which disorder was the most
mainder of the nervous system.15 With hemi- likely cause of the patients intractable epilepsy
spheric disconnection, the affected hemisphere and thus to determine which surgical procedure
continues to have seizure activity but the dis- to undertake.
charges cannot propagate and do not produce The team worked out the following strategy.
symptoms. The less extensive procedures are During the operation, we would use intraopera-
associated with less blood loss and fewer long- tive MRI-guided stereotactic localization to ex-
term complications but with a slightly lower pose the area of the brain that included the ab-
likelihood of seizure control.16-18 normality that was seen on FLAIR imaging, as
Hemispherectomy and hemispheric disconnec- well as the adjacent regions needed for hemi-
tion can each result in varying degrees of con- spheric disconnection. We would perform intra-
tralateral weakness, language and other cogni- operative electrocorticography before any resec-
tive dysfunction, and hemianopsia, depending tion to determine whether a focal epileptogenic
on the degree to which such functions already zone could be identified. We would then resect
have been or can be subserved by the contralat- the presumptive dysplastic region and send a
eral hemisphere. The ultimate outcome of either sample of the tissue for frozen-section analysis,
procedure depends on a number of factors, in- to see whether there were features consistent
cluding neurologic condition before surgery and with dysplasia or inflammation. After the focal
degree of brain plasticity. Most children who resection, we would perform repeat electrocorti-
n engl j med 371;18nejm.orgoctober 30, 2014 1743
The New England Journal of Medicine
Downloaded from nejm.org on November 25, 2015. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
cography; if seizure activity was absent and the cytomegalovirus, and EpsteinBarr virus) are neg-
pathological findings were suggestive of dyspla- ative. An immunohistochemical stain for neuro-
sia, surgery would be terminated. However, if nal nuclei shows that the area that was identified
continued epileptiform discharges were identi- as having features of cortical dysplasia on im-
fied outside the zone of focal resection and if aging studies has normal cortical architecture
the pathological findings were suggestive of an (Fig. 3F).
inflammatory process, we would then proceed The two key histopathological findings as-
with hemispheric disconnection. sociated with cortical dysplasia are disorganiza-
We began by performing a large, vessel-sparing tion of the cortical architecture, with loss of
resection of the rolandic region, which we iden- normal cortical lamination and neuronal cluster-
tified with the use of image guidance as the ing, and the presence of neurons with cytologic
area containing the abnormality that was seen abnormalities, such as irregular shape, large
on FLAIR imaging. A review of frozen sections by size, and clumping of Nissl substance.19-21 Other
the pathology service revealed no findings sug- histopathological features that may be present
gestive of cortical dysplasia. Electrocorticography are balloon cells and heterotopic neurons in the
revealed continued discharges in the frontal and white matter and in the cortical molecular layer.22
occipital cortex. For these reasons, we proceeded None of these features are present in this case.
as planned with hemispheric disconnection. The The histologic features of Rasmussens en-
procedure involved resection of the anterior tem- cephalitis consist of chronic encephalitis with
poral lobe, intraventricular disconnection of the predominance of T lymphocytes, prominent mi-
perisylvian cortex, intraventricular section of the croglial activation with microglial nodules, neu-
corpus callosum, and section through the medial ronophagia, and gliosis; the disease is also as-
frontal and posterior periventricular white-matter sociated with negative immunohistochemical
tracts. When the patient awoke after the surgical stains for known viruses. These findings are not
procedure, he had slower psychomotor function specific for Rasmussens encephalitis, but in a
but was immediately able to follow commands patient with unilateral hemispheric atrophy and
and name objects, and he had preserved ability intractable seizures, they are consistent with the
to move his right arm and minimal movement diagnosis. Several studies suggest a progressive
in his right leg. The epilepsia partialis continua course, with early symptoms and signs including
was absent. During the following days, tone re- intense inflammation and numerous microglial
turned in the right leg, and by 2 weeks after the nodules and later symptoms and signs including
procedure, he was walking with assistance and necrosis, marked gliosis, and neuronal loss with
using his right arm. mild inflammation.23 A coexisting condition
was present in about 10% of patients involved in
Pathol o gic a l Discussion a large case series.11,24
Dr. Thibert: On awakening after the surgical
Dr. Stemmer-Rachamimov: The histologic features procedure, the patient had expressive speech,
of the resection specimen are similar to those of and when he was discharged to rehabilitation
the biopsy specimen but more diffuse and more services 8 days later, he was walking with as-
pronounced. There is a chronic inflammatory sistance. He was discharged from the hospital
infiltrate in the leptomeninges. The underlying approximately 3 to 4 weeks postoperatively and
cortex is hypercellular, with scattered intrapa- seen for follow-up 8 weeks postoperatively, at
renchymal lymphocytes, cuffs of perivascular which time he also returned to school. His
lymphocytes, and numerous activated microglia speech and mood are back to baseline and his
(highlighted by immunohistochemical staining strength continues to improve. Six months after
for CD68), some of which were tightly clustered the operation, he was seizure-free, and clonaze-
and formed microglial nodules (Fig. 3D). Stain- pam and dietary therapy had been successfully
ing for glial fibrillary acidic protein (GFAP) re- tapered off.
veals moderate reactive gliosis (Fig. 3E). Multi- The Patients Mother: Two months after the op-
ple immunohistochemical stains for viruses eration, my son wanted to go on a half-mile hike
(herpes simplex virus, varicellazoster virus, to a fire tower in New Hampshire. I said, Can
1744 n engl j med 371;18nejm.orgoctober 30, 2014
The New England Journal of Medicine
Downloaded from nejm.org on November 25, 2015. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
case records of the massachuset ts gener al hospital
you do it? and he said, Yes. We put a bicycle A major mystery that Dr. Rasmussen empha-
helmet on him, in case he fell on the uneven sized was that the inflammatory process begins
terrain because of the orthosis for his ankle and unilaterally but also has the propensity to cross
foot. He now talks about his Wahoo! moment the midline. The likelihood of eventual bilateral
he made it to the top of the fire tower. He involvement is unclear, but the fear of progres-
wanted to know where Boston was, and you sion has been one important driver of early
could look right down and see the city. He took surgery to try to avoid that evolution.
a picture. When we were coming down, I had to Finally, Dr. Rasmussen recognized that al-
support him because his legs were shaking so though the histopathology of the disease is in-
badly, but he said, Im not quitting yet. So, hes flammatory, the cause is unknown, and it still
doing great. remains unclear whether the primary process is
Dr. Duhaime: The patient followed the typical viral, autoimmune, or genetically determined.
course of recovery after hemispheric disconnec- Dr. Duhaime: I agree that this is one of the
tion, with gradual improvement in language most mysterious diseases I have treated. I am
function, spastic hemiparesis with resumption struck by the similarities between the unilateral
of ambulation, and return to baseline arm brain atrophy in patients with Rasmussens en-
strength. Most important, his personality and cephalitis and in some infants with subdural
sense of humor were preserved, and the disease hematoma. Both conditions are characterized by
can be expected to stop progressing, with con- continuous or frequent seizure discharges and
tinued improvement over time as the intact by near-total destruction of one hemisphere with
hemisphere consolidates functional control. At potentially near-complete preservation of the
his last follow-up, 2 years after the operation, he contralateral hemisphere. After hemispheric dis-
was not taking any medications and was seizure- connection is performed to treat either condi-
free. He has right-sided homonymous hemi- tion, the affected hemisphere is still seizing, but
anopsia and moderate spastic hemiplegia but is the confinement of the seizures somehow con-
able to walk, run, climb, and bike and is taking trols symptoms and keeps the disease from pro-
cello lessons. gressing. This feature probably has implications
Dr. Nancy Lee Harris (Pathology): Are there any for the pathogenesis of both disorders that we
questions or comments? do not yet fully understand.
Dr. Kevin Staley (Neurology): Did you consider Dr. Harris: Why does a ketogenic diet help to
continuing therapy with intravenous immune control seizures?
globulin? It looks as if the patient had a pretty Dr. Thibert: We do not know exactly why the
good response to the therapy initially. diet works, although it has been around for 100
Dr. Thibert: No, the intravenous immune glob- years. The diet mimics starvation; basically, the
ulin had lost its effectiveness over time. At the body receives foods that are high in fat and low
initial visit, the patient himself actually asked us in carbohydrates, and the brain uses the fatty
to do the surgery. acids as its fuel source. It is a very helpful treat-
Dr. Andrew J. Cole (Neurology): I was honored to ment, and in this case, it was the only thing that
be able to work with Dr. Rasmussen when I was was helping to control the patients seizures
a resident, and I saw a number of his patients. I before he underwent surgery.
think one of the differences between this case
and classic cases of Rasmussens encephalitis is A nat omic a l Di agnosis
the remarkably short duration of illness. In this
case, the time between the initial onset of symp- Chronic meningoencephalitis consistent with
toms and surgery was approximately 2 years, Rasmussens encephalitis.
whereas in most of the cases that Dr. Rasmussen
This case was presented at Neurology Grand Rounds.
encountered, the disease had already undergone No potential conflict of interest relevant to this article was re-
many years of evolution. I suspect that is the ported.
reason why the progressive atrophy was less Disclosure forms provided by the authors are available with
the full text of this article at NEJM.org.
striking in this patient than in the patients de- We thank Dr. Thomas Byrne for assistance with organizing
scribed in historical reports. the conference.
n engl j med 371;18nejm.orgoctober 30, 2014 1745
The New England Journal of Medicine
Downloaded from nejm.org on November 25, 2015. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
case records of the massachuset ts gener al hospital
References
1. Thomas JE, Reagan TJ, Klass DW. 9. Prayson RA. Dual pathology in Ras spherectomy. Neurosurgery 2001;49:891-
Epilepsia partialis continua: a review of mussens encephalitis: a report of coexis- 900.
32 cases. Arch Neurol 1977;34:266-75. tent focal cortical dysplasia and review of 18. Harvey AS, Cross JH, Shinnar S,
2. Sinha S, Satishchandra P. Epilepsia the literature. Case Rep Pathol 2012;2012: Mathern GW. Defining the spectrum of
partialis continua over last 14 years: expe- 569170. international practice in pediatric epilep-
rience from a tertiary care center from 10. Palmer CA, Geyer JD, Keating JM, et al. sy surgery patients. Epilepsia 2008;49:146-
south India. Epilepsy Res 2007;74:55-9. Rasmussens encephalitis with concomi- 55.
3. Phabphal K, Limapichat K, Sathira tant cortical dysplasia: the role of GluR3. 19. Taylor DC, Falconer MA, Bruton CJ,
panya P, Setthawatcharawanich S, Geater A. Epilepsia 1999;40:242-7. Corsellis JA. Focal dysplasia of the cere-
Clinical characteristics, etiology and long- 11. Hart YM, Andermann F, Robitaille Y, bral cortex in epilepsy. J Neurol Neurosurg
term outcome of epilepsia partialis conti- Laxer KD, Rasmussen T, Davis R. Double Psychiatry 1971;34:369-87.
nua in adult patients in Thailand. Epilepsy pathology in Rasmussens syndrome: 20. Mischel PS, Nguyen LP, Vinters HV.
Res 2012;100:179-87. a window on the etiology? Neurology Cerebral cortical dysplasia associated
4. Kravljanac R, Djuric M, Jovic N, Djord 1998;50:731-5. with pediatric epilepsy: review of neuro-
jevic M, Zamurovic D, Pekmezovic T. 12. Firlik KS, Adelson PD, Hamilton RL. pathologic features and proposal for a
Etiology, clinical features and outcome of Coexistence of a ganglioglioma and Ras grading system. J Neuropathol Exp Neurol
epilepsia partialis continua in cohort of mussens encephalitis. Pediatr Neurosurg 1995;54:137-53.
51 children. Epilepsy Res 2013;104:112-7. 1999;30:278-82. 21. Vinters HV. Histopathology of brain
5. Bien CG, Granata T, Antozzi C, et al. 13. Rowland NC, Englot DJ, Cage TA, tissue from patients with infantile spasms.
Pathogenesis, diagnosis and treatment of Sughrue ME, Barbaro NM, Chang EF. A Int Rev Neurobiol 2002;49:63-76.
Rasmussen encephalitis: a European con- meta-analysis of predictors of seizure 22. Dehay C, Kennedy H. Cell-cycle con-
sensus statement. Brain 2005;128:454-71. freedom in the surgical management of trol and cortical development. Nat Rev
6. Pandian JD, Thomas SV, Santoshku focal cortical dysplasia. J Neurosurg 2012; Neurosci 2007;8:438-50. [Erratum, Nat Rev
mar B, et al. Epilepsia partialis continua 116:1035-41. Neurosci 2007;8:568.]
a clinical and electroencephalography 14. Schachter SC, Saper CB. Vagus nerve 23. Robitaille Y. Neuropathologic aspects
study. Seizure 2002;11:437-41. stimulation. Epilepsia 1998;39:677-86. of chronic encephalitis. In: Andermann F,
7. Longaretti F, Dunkley C, Varadkar S, 15. Schramm J, Behrens E, Entzian W. ed. Chronic encephalitis and epilepsy:
Vargha-Khadem F, Boyd SG, Cross JH. Hemispherical deafferentation: an alter- Rasumussens syndrome. Boston: Butter
Evolution of the EEG in children with native to functional hemispherectomy. worth-Heinemann, 1991:79-103.
Rasmussens syndrome. Epilepsia 2012; Neurosurgery 1995;36:509-15. 24. Bien CG, Urbach H, Deckert M, et al.
53:1539-45. 16. Villemure JG, Mascott CR. Peri- Diagnosis and staging of Rasmussens
8. Takei H, Wilfong A, Malphrus A, et al. insular hemispherotomy: surgical prin- encephalitis by serial MRI and histopa-
Dual pathology in Rasmussens encepha- ciples and anatomy. Neurosurgery 1995; thology. Neurology 2002;58:250-7.
litis: a study of seven cases and review of 37:975-81. Copyright 2014 Massachusetts Medical Society.
the literature. Neuropathology 2010;30: 17. Schramm J, Kral T, Clusmann H.
381-91. Transsylvian keyhole functional hemi-
Lantern Slides Updated: Complete PowerPoint Slide Sets from the Clinicopathological Conferences
Any reader of the Journal who uses the Case Records of the Massachusetts General Hospital as a teaching exercise or reference
material is now eligible to receive a complete set of PowerPoint slides, including digital images, with identifying legends,
shown at the live Clinicopathological Conference (CPC) that is the basis of the Case Record. This slide set contains all of the
images from the CPC, not only those published in the Journal. Radiographic, neurologic, and cardiac studies, gross specimens,
and photomicrographs, as well as unpublished text slides, tables, and diagrams, are included. Every year 40 sets are produced,
averaging 50-60 slides per set. Each set is supplied on a compact disc and is mailed to coincide with the publication of the
Case Record.
The cost of an annual subscription is $600, or individual sets may be purchased for $50 each. Application forms for the current
subscription year, which began in January, may be obtained from the Lantern Slides Service, Department of Pathology,
Massachusetts General Hospital, Boston, MA 02114 (telephone 617-726-2974) or e-mail Pathphotoslides@partners.org.
1746 n engl j med 371;18nejm.orgoctober 30, 2014
The New England Journal of Medicine
Downloaded from nejm.org on November 25, 2015. For personal use only. No other uses without permission.
Copyright 2014 Massachusetts Medical Society. All rights reserved.
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Nursing Students Peritonitis Care PlanDocument2 pagesNursing Students Peritonitis Care PlanJide Manuel100% (1)
- C Post Concussion ChecklistDocument1 pageC Post Concussion Checklistalston96Pas encore d'évaluation
- Pathology Outlines - Papillary Carcinoma - GeneralDocument6 pagesPathology Outlines - Papillary Carcinoma - Generalpatka1rPas encore d'évaluation
- HAP & VAP IDSA Pocketcard Guidelines (2016)Document12 pagesHAP & VAP IDSA Pocketcard Guidelines (2016)David GerickPas encore d'évaluation
- Pathology PDFDocument28 pagesPathology PDFRoman PanditPas encore d'évaluation
- Cutaneous Larva Migrans LinDocument24 pagesCutaneous Larva Migrans LinprabuPas encore d'évaluation
- Judul Skenario 5Document1 pageJudul Skenario 5prabuPas encore d'évaluation
- Our Important Asset Is Our Great PeopleDocument8 pagesOur Important Asset Is Our Great PeopleprabuPas encore d'évaluation
- Sfar ScoreDocument8 pagesSfar ScoreprabuPas encore d'évaluation
- WolfeandSharp 2002 Anti VaccinationistspastandpresentwsupplDocument10 pagesWolfeandSharp 2002 Anti VaccinationistspastandpresentwsupplprabuPas encore d'évaluation
- Khadijah Gina PuspitaDocument44 pagesKhadijah Gina PuspitaprabuPas encore d'évaluation
- Microstructure Female Reproductive System - 2018Document46 pagesMicrostructure Female Reproductive System - 2018prabuPas encore d'évaluation
- 521 2345 1 PB Converted 1Document14 pages521 2345 1 PB Converted 1prabuPas encore d'évaluation
- Qualitative Analysis of Mothers' Decision-Making About Vaccines For InfantsDocument12 pagesQualitative Analysis of Mothers' Decision-Making About Vaccines For InfantsprabuPas encore d'évaluation
- Team BuildingDocument26 pagesTeam BuildingprabuPas encore d'évaluation
- SfarDocument7 pagesSfarprabuPas encore d'évaluation
- 4281 - Gestational Iron Deficiency Is Associated With Pica BehaviorsDocument16 pages4281 - Gestational Iron Deficiency Is Associated With Pica BehaviorsprabuPas encore d'évaluation
- Schistosoma Japonicum: Perforation of Small Bowel Caused By: A Case ReportDocument4 pagesSchistosoma Japonicum: Perforation of Small Bowel Caused By: A Case ReportAyuPas encore d'évaluation
- Digestive System GuideDocument25 pagesDigestive System GuideprabuPas encore d'évaluation
- Viremia in Acute Herpes ZosterDocument16 pagesViremia in Acute Herpes ZosterprabuPas encore d'évaluation
- Digestive System BpwsDocument17 pagesDigestive System BpwsprabuPas encore d'évaluation
- FixDocument13 pagesFixprabuPas encore d'évaluation
- Modul Anatomy Blok 2-2Document46 pagesModul Anatomy Blok 2-2AyuPas encore d'évaluation
- ReviewDocument7 pagesReviewprabuPas encore d'évaluation
- Treatment of Nasal PolipDocument4 pagesTreatment of Nasal PolipprabuPas encore d'évaluation
- Diagnosis BandingDocument7 pagesDiagnosis BandingprabuPas encore d'évaluation
- Presentation 1Document3 pagesPresentation 1prabuPas encore d'évaluation
- Kel.1 Kanker Kepala Leher PDFDocument10 pagesKel.1 Kanker Kepala Leher PDFprabuPas encore d'évaluation
- Patophysiology of Nasal PolypDocument2 pagesPatophysiology of Nasal PolypprabuPas encore d'évaluation
- Diagnosis BandingDocument7 pagesDiagnosis BandingprabuPas encore d'évaluation
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofprabuPas encore d'évaluation
- Jurnal BlokDocument3 pagesJurnal BlokprabuPas encore d'évaluation
- Review JurnalDocument4 pagesReview JurnalprabuPas encore d'évaluation
- Hyperthyroid in Pregnancy Kel 3 PDFDocument7 pagesHyperthyroid in Pregnancy Kel 3 PDFprabuPas encore d'évaluation
- MECONIUM Aspiration SyndromeDocument37 pagesMECONIUM Aspiration SyndromekamalaPas encore d'évaluation
- Acupressure Points For Relieving ArthritisDocument18 pagesAcupressure Points For Relieving ArthritisAgustin Benitez Holguin100% (4)
- Ayurvedic Diabetes CureDocument13 pagesAyurvedic Diabetes CureYassine KrinePas encore d'évaluation
- Laporan Kasus - Dendy Dwi Ramadhani - PPDS Anestesi BrawijayaDocument1 pageLaporan Kasus - Dendy Dwi Ramadhani - PPDS Anestesi BrawijayaDendyPas encore d'évaluation
- Aeromonas InfectionDocument27 pagesAeromonas Infection周治剛Pas encore d'évaluation
- Harris Hip ScorHarrise - Orthopaedic ScoresDocument2 pagesHarris Hip ScorHarrise - Orthopaedic Scoresw00tzxPas encore d'évaluation
- Sti Villains Project InstructionsDocument2 pagesSti Villains Project Instructionsapi-544556482Pas encore d'évaluation
- 2-Physiotherapy For FracturesDocument17 pages2-Physiotherapy For FracturesJuanitoCabatañaLimIIIPas encore d'évaluation
- Classification of Endometriosis: Birmingham, AlabamaDocument2 pagesClassification of Endometriosis: Birmingham, AlabamaAsela SubhasinghePas encore d'évaluation
- Knee PainDocument2 pagesKnee PainKKPas encore d'évaluation
- The Floppy Infant:: Evaluation of HypotoniaDocument13 pagesThe Floppy Infant:: Evaluation of HypotoniaminipredatorPas encore d'évaluation
- Tah BsoDocument27 pagesTah BsoCephradine DolientePas encore d'évaluation
- Obg MCQSDocument11 pagesObg MCQSShriyansh ChaharPas encore d'évaluation
- Practneurol 2020 002550Document9 pagesPractneurol 2020 002550Phuphinyo LimchantraPas encore d'évaluation
- Endometriosis & Adenomyosis Dr. Selly Septina, SpogDocument25 pagesEndometriosis & Adenomyosis Dr. Selly Septina, SpogRezkiRamadhanPas encore d'évaluation
- Physiotherapy Guidelines For Manual HyperinflationDocument5 pagesPhysiotherapy Guidelines For Manual HyperinflationAhmed Abd Elrauf100% (2)
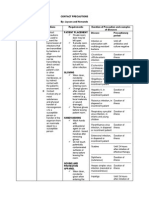
- Contact PrecautionsDocument2 pagesContact PrecautionsCristina L. JaysonPas encore d'évaluation
- Guideline Karsinoma HepatoselulerDocument11 pagesGuideline Karsinoma HepatoselulerMohammad Ihsan RifasantoPas encore d'évaluation
- Thyroid CancerDocument38 pagesThyroid CancerNinikPas encore d'évaluation
- Activity IntoleranceDocument4 pagesActivity IntoleranceDianne MacaraigPas encore d'évaluation
- NCP HeadDocument11 pagesNCP Headann-lisel-manahan-7670100% (2)
- HemorrhoidectomyDocument5 pagesHemorrhoidectomydrnareshkumar3281100% (1)
- AphasiaDocument71 pagesAphasiaVarun B RenukappaPas encore d'évaluation
- Classification System For Oral Submucous FibrosisDocument6 pagesClassification System For Oral Submucous FibrosisMohamed FaizalPas encore d'évaluation
- Pernicious Anemia in Young: A Case Report With Review of LiteratureDocument5 pagesPernicious Anemia in Young: A Case Report With Review of LiteratureeditorijmrhsPas encore d'évaluation