Académique Documents
Professionnel Documents
Culture Documents
CMSA Standards 2016
Transféré par
fanny_febrianiCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
CMSA Standards 2016
Transféré par
fanny_febrianiDroits d'auteur :
Formats disponibles
Standards of Practice for
Case Management REVISED 2016
Foreword ............................................................................................................. 2
Preface ............................................................................................................. 3
I. INTRODUCTION........................................................................................... 5
II. EVOLUTION OF THE STANDARDS OF PRACTICE FOR CASE
MANANGMENT........................................................................................... 8
A. Standards of Practice for Case Management (1995)............................... 8
B. Standards of Practice for Case Management (2002).............................. 8
C. Standards of Practice for Case Management (2010)............................... 9
D. Standards of Practice for Case Management (2016)............................... 9
III. DEFINITION OF CASE MANAGEMENT.......................................................... 11
IV. PHILOSOPHY AND GUIDING PRINCIPLES..................................................... 12
A. Statement of Philosophy ....................................................................... 12
B. Guiding Principles ................................................................................. 12
V. CASE MANAGEMENT PRACTICE SETTINGS................................................. 14
VI. PROFESSIONAL CASE MANAGEMENT ROLES AND
RESPONSIBIILTIES........................................................................................ 15
VII. COMPONENTS OF THE CASE MANAGEMENT PROCESS............................... 18
1. Client Identification, Selection and Engagement in Professional
Case Management................................................................................ 18
2. Assessment and Opportunity Identification........................................... 18
3. Development of the Case Management Plan of Care............................. 18
4. Implementation and Coordination of the Case Management
Plan of Care........................................................................................... 19
5. Monitoring and Evaluation of the Case Management Plan of Care........ 19
6. Closure of the Professional Case Management Services......................... 19
VIII. STANDARDS OF PROFESSIONAL CASE MANAGEMENT PRACTICE............... 20
A. Client Selection Process for Professional Case Management Services.... 20
B. Client Assessment................................................................................. 20
C. Care Needs and Opportunities Identification......................................... 22
D. Planning................................................................................................ 23
E. Monitoring............................................................................................ 23
F. Outcomes.............................................................................................. 24
G. Closure of Professional Case Management Services............................... 24
H. Facilitation, Coordination, and Collaboration......................................... 25
I. Qualifications for Professional Case Managers...................................... 26
J. Legal..................................................................................................... 27
1. Confidentiality and Client Privacy...................................................... 27
2. Consent for Professional Case Management Services........................ 27
K. Ethics.................................................................................................... 28
L. Advocacy............................................................................................... 28
M. Cultural Competence............................................................................. 29
N. Resource Management and Stewardship............................................... 29
O. Professional Responsibilities and Scholarship......................................... 30
IX. ACKNOWLEDGEMENTS............................................................................... 31
2016 X. GLOSSARY................................................................................................... 32
2016
References............................................................................................................. 37
CMSA Standards of Practice for Case Management 1
Foreword
It is my honor to present the 2016 revision of the Case Management Society of Americas (CMSA)
Standards of Practice for Case Management. CMSA, an interprofessional organization, remains dedicated
to the support and development of case management professionals. An outstanding hallmark of our
profession is the willingness of its members to help one another learn and, thereby, improve the services
that our profession performs. Unity is truly our strength. This fourth revision of our Standards of Practice
came together with that same united commitment to excellence as seen within our profession.
We recognized the need to revise the Standards of Practice in order to be reflective of the
expanding role of the professional case manager. The awareness that case managers are crucial
members of the health care team has been realized providing the need to reexamine and redefine
our role in the current complex health care tomography. The body of knowledge required to practice
case management is rapidly growing as the specialty continues to evolve. Modern patient care must
be based upon the holistic intertwining of information from a variety of disciplines. As our activities
become more sophisticated, so must our resources which in turn must remain relevant.
Professional case management is neither linear nor a one-way exercise. Facilitation, coordination
and collaboration occur throughout the clients health care encounter. Collaboration among physi-
cians, nurses, case managers, social workers, pharmacists, allied health professionals, and support
staff is critical in achieving the goals of the team, the organization and changing the way we deliver
healthcare today. Unity is our strength and this edition of the Standards of Practice, is the product of
many hours of literature review, discussion, deliberation and collaboration among those who served
on the taskforce (see page 31). It is this total body of work we are so proud to roll out.
Before I close I would be remiss if a special thank you was not given to the key to our success,
Cheri Lattimer, our Executive Director. Cheri worked tirelessly as our facilitator from beginning to end
and through her support and guidance we were able to bring this project to fruition. We could not
have completed it to this caliber without her leadership and for this we are grateful.
Lastly I want to dedicate these standards, to all of the professional case managers who make
a difference every day in the lives of their clients. My dear late father knew firsthand what a case
manager could accomplish and he would frequently ask What do people do without a Kathleen? My
hope is that in the not so distant future, such question will not need to be asked any longer because
all people with complex conditions will have case managers who make their health care experience
exponentially greater.
Kathleen Fraser, MSN, MHA, RN-BC, CCM, CRRN
President 2014-2016
2 CMSA Standards of Practice for Case Management
Preface
The Case Management Society of America (CMSA) first introduced the Standards of Practice for Case
Management in 1995 and revised them in 2002 and 2010 thereafter. CMSA and its Board of Directors
are pleased to offer the Standards of Practice for Case Management, 2016 revision, which provides
practice guidelines for the case management industry and its diverse stakeholders. These Standards
of Practice identify and address important foundational knowledge, skills, and competencies for the
professional case manager within a spectrum of case management practice settings, specialties, and
health and human service disciplines.
Similar to past revisions, the 2016 Standards reflect recent changes in the industry, which reso-
nate with current practice. Some of these changes include the following:
Minimizing fragmentation in the health care system, application of evidence-based guidelines in
practice to promote collaborative care coordination, navigating transitions of care, and incorpo-
rating adherence guidelines and other standardized practice tools.
Expanding and maximizing the contribution of the interprofessional collaborative health care
team to planning care and services for individuals, improving the experience of those who
are the recipients of professional case management services, and ensuring safe, quality and
cost-effective outcomes.
We believe these are all important factors that professional case managers need to address in
their practice. The 2016 Standards of Practice contain information about case management including
an updated definition, practice settings, roles and responsibilities, case management process, philoso-
phy and guiding principles, as well as the standards and how they are demonstrated.
This document is intended for voluntary use. It is not intended to replace professional judgment
or relevant legal, ethical or optimal practice requirements. In all cases, case managers should consult
their own compliance and legal advisors. CMSA provides these Standards of Practice as a resource
to professional case managers and in no event shall CMSA be held liable for damages of any kind in
connection with the material, methods, information, techniques, opinions, or procedures expressed,
presented, or illustrated in these Standards of Practice even if CMSA has been information of the
possibility of such liability.
Our hope is that the Standards of Practice serve as a unifying force for professional case
management practice by providing a common understanding and application of the role, process,
and expectations. As such, the Standards serve to drive accountability for best practice for individual
professional case managers as well as for the organizations within which they work.
A dedicated team of expert and professional case managers spent countless hours in synthe-
sizing relevant information from recent changes and developments in the industry. The 2016 revision
of the Standards reflect what this team thought to be important for the professional practice of case
management. The team included:
1. A core task force made up of representatives of the case management field from various prac-
tice settings and professional disciplines.
2. A larger reference group that included the CMSA leadership and Board of Directors, legal advi-
CMSA Standards of Practice for Case Management 3
sors, and the case management industry.
3. Other case management experts in the industry who acted in a peer review capacity.
It has been our pleasure to work on this project with the talented and committed individuals who
are raising the bar of excellence in the field of case management.
Mary Beth Newman, MSN, RN-BC, CCP, CCM, CHCQM, 2016 Taskforce Co-Chair
Kathleen Fraser, MSN, MHA, RN-BC, CCM, CRRN, 2016 Taskforce Co-Chair
4 CMSA Standards of Practice for Case Management
I. Introduction
The consistent delivery of quality health availability of affordable services. Through case
and human services and the high financial costs management, health care providers and organi-
generally associated with these services are zations are able to meet or exceed the quality,
important concerns that touch everyone, from safety, and cost related expectations of these key
our leaders in Washington, D.C., to health care regulations and programs.
providers, and ultimately the American public at Professional case management today fosters
large. Payers today continue to seek innovative the careful shepherding of health care dollars
methods to reduce costs while advancing quality, while maintaining a primary and consistent focus
safety, optimal care experience, and transparen- on quality of care, safe transitions, timely access
cy in outcomes of care. Providers explore inno- to and availability of services, and most impor-
vative ways to define, impact, and report on the tantly client self-determination and provision of
value of professional case management services client-centered and culturally-relevant care. These
and their benefits to all stakeholders while max- without a doubt enhance the health of individuals
imizing reimbursement. Too frequently however, and communities. They also demand a profes-
the health care consumer is still left to wander a sional case manager who (a) is academically pre-
complex health care system without the neces- pared in a health or human services discipline; (b)
sary support, tools, resources, or knowledge to possesses an unrestricted license or certification
self-manage complex care needs in an effective, as required by the jurisdiction of employment; (c)
timely, and safe manner. All of these dynamics is able to function independently and according
will continue to shape the context and effects of to the scope of practice of the background health
case management. discipline; (d) demonstrates current knowledge,
A number of recently enacted regulations, skills, and competence to effectively provide
such as the Patient Protection and Affordable holistic and client-centered care; and (e) acts in a
Care Act (PPACA) and the Health Information supervisory capacity of other personnel who are
Technology for Economic and Clinical Health involved in the clients care but unable to function
(HITECH) Act, has resulted in the emergence independently due to limitations of license and/or
and legitimization of case management as a education.
necessary care delivery model and intervention. Founded in 1990, the CMSA is the leading
The PPACA has reduced the rate of the uninsured non-profit and interprofessional association
and demanded health care providers and organi- dedicated to the support, development, and
zations to transform their care provision practices advancement of case management. The strategic
financially, technologically, and clinically to vision of CMSA approved in 2009 and slightly
drive better health outcomes, lower costs, and modified in 2016 is as follows:
improvements in the access to and distribution of Case managers are recognized ex-
resources while the HITEC Act has promoted the perts and vital participants in the care
adoption and meaningful use of health informa- coordination team who empower peo-
tion technology. Simultaneously, initiatives such ple to understand and access quality,
as the Value-based Purchasing programs and the safe, and efficient health care services.
National Quality Strategy that is guided by the To complement this vision, case manage-
Institute of Healthcare Improvements Triple Aim ment professionals, educators and leaders have
have contributed to better care, improvements in come together to reach consensus regarding
the health of people and communities, and the the guiding principles and fundamental spirit
CMSA Standards of Practice for Case Management 5
of the practice of case management. As initially of case management services.
presented in 1992, and with each subsequent The term support system, as indicated by the
revision, the Standards of Practice for Case Man- client, may include a biological relative, spouse,
agement have served the professional practice of partner, friend, neighbor, colleague, health care
case management. These Standards, described proxy, or any individual supporting the client.
within this document, are not intended to be a The term caregiver is important to recog-
structured recipe for the delivery of case man- nize. As part of the clients support system,
agement services and interventions. Rather, they a caregiver is the individual designated by
are recommendations for practice and present the client to be involved in the clients care
a range of core functions, roles, responsibilities, throughout and following the engagement of
and relationships that are integral to the effective case management services. The caregiver, also
interprofessional practice of case management. referred to as family caregiver, is not a member
The review process of the Standards of of the interprofessional health care team; rather
Practice for Case Management encourages vigor- a member of the clients support system. Note
ous discussion of each section and necessitates that when using the term client, it may also
certain updates where appropriate to assure be inclusive of the clients support system,
the Standards remain relevant and reflective of family or family caregiver.
current knowledge and practice. The following are The term case management is used through-
important considerations to bear in mind when out the Standards rather than a variety of terms
reading and applying the Standards: (e.g., care management, care coordination,
transitional care). The Glossary includes a defi-
The term client is consistently used through- nition for each of these terms. For consistency
out the Standards and refers to the individual purposes, the term case management is used
recipient of case management services. The one throughout the Standards as an inclusive term.
exception is Figure 1, The Continuum of Health The term case management plan of care
Care and Professional Case Management, on is used to indicate the individualized and
page 7, in which both client and patient are client-centered plan for the provision of care,
used. Depending on the practice setting, this services, and resources necessary to meet
individual may be referred to as the patient, the clients identified care goals, needs, and
beneficiary, injured worker, claimant, enrollee, preferences.
member, college student, resident or health
care consumer. Client is not an age-dependent When applying the Standards into individual
term. It is recognized that the term client has a practice and care settings, adjustments in
context-specific meaning. Client may also imply terminology may be necessary. As previously
the business relationship with a company that noted, the Standards primarily use client; how-
contracts, or pays, for the delivery of case man- ever, the setting of care rubric may use another
agement services. Careful interpretation and term (e.g., member, resident, beneficiary,
application of the Standards in these diverse enrollee, claimant, patient, and individual).
contexts is advised to avoid unintentionally or In this situation, substitution of terminology
inappropriately advocating for the individual or is not only acceptable, but advised as well to
organization which has contracted the services maintain consistency with the practice setting
versus the individual who is the actual recipient requirements.
6 CMSA Standards of Practice for Case Management
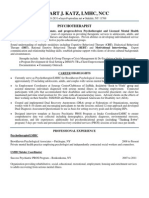
FIGURE 1: The Continuum of Health Care and
Professional Case Management
While the Standards of Practice are offered Additionally, the Standards serve to depict
to standardize the process of case management, the scope of case management practice to
they are intended to be realistic and attainable colleagues, employers of case managers, health
by members of the interprofessional health care consumers, legislators, policy makers, and
care team who use appropriate and reasonable other stakeholders who partner with the case
clinical judgment regarding the delivery of management professional.
professional case management services.
CMSA Standards of Practice for Case Management 7
II. Evolution of the Standards of
Practice for Case Management
A. Standards of Practice for Case the Standards (CMSA, 1995).
Management (1995) B. Standards of Practice for Case
In 1995, the President of the CMSA wrote Management (2002)
a foreword in the 1995 CMSA Standards of The 2001 Board of Directors of CMSA identified
Practice. In it he stated that the development the need for a careful and thorough review and,
of national Standards represents a major step if appropriate, revision of the 1995 published
forward for case managers. The future of our Standards. The revised Standards of Practice for
practice lies in the quality of our performance, Case Management were then published in 2002.
as well as our outcomes (CMSA, 1995, pg.3). The previously articulated definition of case man-
These first Standards included this definition of agement was amended at the time to highlight
case management (CMSA, 1995, pg.8): the importance of the case managers role in
Case management is a collaborative client advocacy (CMSA, 2002, pg. 5):
process which assesses, plans, implements, Case management is a collaborative
coordinates, monitors and evaluates options and process of assessment, planning, facilitation and
services to meet an individuals health needs advocacy for options and services to meet an
through communication and available resources individuals health needs through communica-
to promote quality cost-effective outcomes. tion and available resources to promote quality
The 1995 Standards of Practice were recog- cost-effective outcomes.
nized as an anticipated tool that case manage- The section on Performance Indicators was
ment professionals would use within every case also expanded to further define the case manag-
management practice arena. They were seen as er. The purpose of case management was revised
a guide to move case management practice to to address quality, safety and cost-effective care,
excellence. The Standards explored the planning, as well as to focus upon facilitating the clients
monitoring, evaluating and outcomes phases appropriate access to care and services.
of the case management process, followed by Primary case management functions in
Performance Standards for the practicing case 2002 included both current and new skills
manager. and concepts: positive relationship-building;
The Performance Standards addressed how effective written and verbal communication;
the case manager worked within each of the es- negotiation skills; knowledge of contractual and
tablished Standards and with other disciplines to risk arrangements, the importance of obtaining
follow all related legal and ethical requirements. consent, confidentiality, and client privacy;
Even at that first juncture, the Standards attention to cultural competency; ability to
committee recognized the importance of the effect change and perform ongoing evaluation;
case managers basing their individual practice use of critical thinking and analysis; ability to
on valid research findings. The committee plan and organize effectively; promoting client
encouraged case managers to participate in the autonomy and self-determination; and demon-
research process, programs, and development strating knowledge of funding sources, health
of specific tools for the effective practice of case care services, human behavior dynamics, health
management. This was evidenced by key sections care delivery and financing systems, and clinical
that highlighted measurement criteria in the standards and outcomes.
collaborative, ethical, and legal components of
8 CMSA Standards of Practice for Case Management
The Standards in 2002 indicated that his/her willingness to change, and his/
case management work applied to individual her support to maintain health behavior
clients or to groups of clients, such as in disease change.
management or population health models. The Expanding the interdisciplinary team to in-
facilitation section of the Standards included clude clients and/or their identified support
more detail about the importance of communica- system, health care providers, and commu-
tion and collaboration on behalf of the client and nity-based and facility-based professionals
the payer. The practice settings for case man- (i.e., pharmacists, nurse practitioners,
agement were increased to capture the evolution holistic care providers, etc.).
of, and the increase in, the number of venues in Expanding the case management role to
which case managers practiced. collaborate within ones practice setting to
support regulatory adherence.
C. Standards of Practice for Case
Moving clients to optimal levels of health
Management (2010)
and well-being.
The 2010 Standards of Practice for Case Man- Improving client safety and satisfaction.
agement addressed topics that influenced the Improving medication reconciliation for a
practice of case management in the dynamic client through collaborative efforts with
health care environment while the definition of medical staff.
case management generally remained as that Improving adherence to the plan of care for
articulated in 2002. Included in the 2010 revision the client, including medication adherence.
however were (CMSA, 2010):
Those changes advanced case manage-
Addressing the total individual, inclusive ment credibility and complemented the trends
of medical, psychosocial, behavioral, and and changes in the health care delivery system
spiritual needs. occurring at the time.
Collaborating efforts that focused upon
moving the individual to self-care whenever D. Standards of Practice for Case
possible. Management (2016)
Increasing involvement of the individual During the 2010s revision of the Standards
and caregiver in the decision-making of Practice for Case Management, the team
process. involved thought that future case management
Minimizing fragmentation of care within Standards of Practice would likely reflect the
the health care delivery system. climate of health care and build upon the evi-
Using evidence-based guidelines, as avail- dence-based guidelines that were to be proven
able, in the daily practice of case manage- successful in the coming years. That prediction
ment. was not far from becoming reality.
Focusing on transitions of care, which The impetus for the 2016s revision of the
included a clients transfer to the next care Standards of Practice for Case Management
setting or provider while assuring effective, is the need to emphasize the professional
safe, timely, and complete transition. nature of the practice and the role of the case
Improving outcomes by using adherence manager. The maturity of the practice of case
guidelines, standardized tools, and proven management, the importance of protecting the
processes to measure a clients understand- professional role of case managers, and the
ing and acceptance of the proposed plans, enactment of new laws and regulations including
CMSA Standards of Practice for Case Management 9
the Patient Protection and Affordable Care Act, Reflect legislative and regulatory changes
all legitimize professional case management affecting professional case management
as an integral and necessary component of the practice such as the need to include the
health care delivery system in the United States. clients family or family caregiver in the
It is important to note that the 2016 Stan- provision of case management services and
dards of Practice for Case Management remain to the clients satisfaction.
primarily similar to and aligned with those Replace the use of stigmatizing terms such
released in 2010 except for some modifications as problems and issues with others that
which are meant to communicate the value of are empowering to the client such as care
professional case management practice and needs and opportunities.
demonstrate adherence to relevant and recently Communicate the closure of professional
enacted laws and regulations. The revised case management services and the case
Standards: manager-client relationship instead of
termination of services and/or the case
Update the definition of case management management process. This subtle change is
to reflect recent changes in the practice. better reflective of the reality that despite
Clarify who the professional case manager case closure, a client may continue to receive
is and the qualifications expected of this health care services however not in a case
professional. management context.
Emphasize the practice of professional case Emphasize the provision of client-centered
management in the ever-expanding care and culturally and linguistically-appropriate
settings across the entire continuum of case management services.
health and human services, and in constant Highlight the value of professional case
collaboration with the client, clients family management practice and the role of the
or family caregiver, and members of the professional case manager.
interprofessional health care team. Recognize the need for professional case
Communicate practical expectations of pro- managers to engage in scholarly activi-
fessional case managers in the application ties, including research, evidence-based
of each Standard. These are found in the practice, performance improvement and
how demonstrated section that follows innovation, and life-long learning.
each Standard.
10 CMSA Standards of Practice for Case Management
III. Definition of Case Management
The basic concept of case management involves 2009 and modified to further align with the
the timely coordination of quality services to practice of case management at the time. The
address a clients specific needs in a cost-effec- definition was as follows (CMSA, 2009):
tive and safe manner in order to promote optimal Case management is a collabora-
outcomes. This can occur in a single health care tive process of assessment, planning,
setting or during the clients transitions of care facilitation, care coordination, eval-
throughout the care continuum. The professional uation, and advocacy for options and
case manager serves as an important facilitator services to meet an individuals and
among the client, family or family caregiver, the familys comprehensive health needs
interprofessional health care team, the payer, through communication and available
and the community. resources to promote quality cost-ef-
As demonstrated in the section on the fective outcomes.
Evolution of the Standards of Case Management, While one may believe that the 2009 defi-
the definition of case management has evolved nition of case management remains appropriate
over a period of time; it reflects the vibrant and today, with the recent focus on client safety, the
dynamic progression of the standards of practice. CMSA Board of Directors has decided to explicit-
Following more than a year of study and ly reference safety in the 2016 definition:
discussion with members of the national Case Case Management is a collabora-
Management Task Force, the CMSAs Board of tive process of assessment, planning,
Directors approved a definition of case manage- facilitation, care coordination, eval-
ment in 1993. uation and advocacy for options and
Since that time, the CMSA Board of services to meet an individuals and
directors has repeatedly reviewed and analyzed familys comprehensive health needs
the definition of case management to ensure its through communication and available
continued application in the dynamic health envi- resources to promote patient safety,
ronment. The definition was modified in 2002 to quality of care, and cost effective out-
reflect the process of case management outlined comes.
within the Standards. It was again revisited in
CMSA Standards of Practice for Case Management 11
IV. Philosophy and Guiding Principles
A. Statement of Philosophy including the diverse group of stakeholders.
Through these efforts, case management focuses
A philosophy is a statement of belief and values
simultaneously on achieving optimal health and
that sets forth principles to guide a program, its
attaining wellness to the highest level possible
meaning, its context, and the role of the individ-
for each client.
ual(s) that exist in it. The CMSAs philosophy of
It is the philosophy of case management
case management articulates that:
that when the provision of health care is
effective and efficient, all parties benefit. Case
The underlying premise of case man-
management, provided as part of a collabo-
agement is based in the fact that, when
rative and interprofessional health care team,
an individual reaches the optimum level
serves to identify options and resources which
of wellness and functional capability,
are acceptable to the client and clients family
everyone benefits: the individual client
or family caregiver. This then, in turn, increases
being served, the clients family or family
the potential for effective clients engagement
caregiver, the health care delivery system,
in self-management, adherence to the case
the reimbursement source or payer, and
management plan of care, and the achievement
other involved parties such as the employer
of successful outcomes.
and consumer advocates.
Case management interventions focus on
Professional case management serves as
improving care coordination and reducing the
a means for achieving client wellness and
fragmentation of the services the recipients of
autonomy through advocacy, ongoing
care often experience especially when multiple
communication, health education,
health care providers and different care settings
identification of service resources, and
are involved. Taken collectively, case manage-
service facilitation.
ment interventions are intended to enhance
Professional case management services
client safety, well-being, and quality of life.
are best offered in a climate that allows
These interventions carefully consider health care
clients engagement and direct communi-
costs through the professional case managers
cation among the case manager, the client,
recommendations of cost-effective and efficient
the clients family or family caregiver, and
alternatives for care. Thus, effective case
appropriate service personnel, in order to
management directly and positively impacts the
optimize health outcomes for all concerned
health care delivery system especially in realizing
(CMSA, 2009).
the goals of the Triple Aim which include
improving the health outcomes of individuals and
The philosophy of case management
populations, enhancing the experience of health
underscores the recommendation that at-risk in-
care, and reducing the cost of care.
dividuals, especially those with complex medical,
behavioral, and/or psychosocial needs, be evalu-
ated for case management intervention. The key B. Guiding Principles
philosophical components of case management Guiding principles are relevant and meaningful
address care that is holistic and client-centered, concepts that clarify or guide practice. Guiding
with mutual goals, allowing stewardship of re- principles for case management practice provide
sources for the client and the health care system that professional case managers:
12 CMSA Standards of Practice for Case Management
Use a client-centric, collaborative part- Pursue professional knowledge and prac-
nership approach that is responsive to the tice excellence and maintain competence in
individual clients culture, preferences, case management and health and human
needs, and values. service delivery.
Facilitate clients self-determination and Support systematic approaches to quality
self-management through the tenets of ad- management and health outcomes im-
vocacy, shared and informed decision-mak- provement, implementation of practice in-
ing, counseling, and health education, novations, and dissemination of knowledge
whenever possible. and practice to the health care community.
Use a comprehensive, holistic, and com- Maintain compliance with federal, state,
passionate approach to care delivery which and local rules and regulations, and orga-
integrates a clients medical, behavioral, nizational, accreditation, and certification
social, psychological, functional, and other standards.
needs. Demonstrate knowledge, skills, and compe-
Practice cultural and linguistic sensitivity, tency in the application of case manage-
and maintain current knowledge of diverse ment standards of practice and relevant
populations within their practice demo- codes of ethics and professional conduct.
graphics.
Implement evidence-based care guidelines Case management guiding principles,
in the care of clients, as available and appli- interventions, and strategies target the
cable to the practice setting and/or client achievement of optimal wellness, function, and
population served. autonomy for the client and clients family or
Promote optimal client safety at the individ- family caregiver through advocacy, assessment,
ual, organizational, and community level. planning, communication, health education,
Promote the integration of behavioral resource management, care coordination,
change science and principles throughout collaboration, and service facilitation.
the case management process. The professional case manager applies
Facilitate awareness of and connections these principles into practice based on the
with community supports and resources. individualized needs and values of the client to
Foster safe and manageable navigation assure, in collaboration with the interprofessional
through the health care system to enhance health care team, the provision of safe, appropri-
the clients timely access to services and the ate, effective, client-centered, timely, efficient,
achievement of successful outcomes. and equitable care and services.
CMSA Standards of Practice for Case Management 13
V. Case Management Practice Settings
Professional case management practice extends care practices, and federally qualified
to all health care settings across the continuum health centers.
of health and human services. This may include Corporations.
the payer, provider, government, employer, Schools.
community, and clients home environment. The Public health insurance and benefit
practice varies in degrees of complexity, intensi- programs such as Medicare, Medicaid, and
ty, urgency and comprehensiveness based on the state-funded programs.
following four factors (Powell and Tahan, 2008; Private health insurance programs such
Tahan and Treiger, 2017): as workers compensation, occupational
health, catastrophic and disability manage-
1. The context of the care setting such as ment, liability, casualty, automotive, acci-
wellness and prevention, acute, subacute dent and health, long-term care insurance,
and rehabilitative, skilled care, or end-of- group health insurance, and managed care
life. organizations.
2. The health conditions and needs of the Independent and private case management
client population(s) served, and the needs companies.
of the clients family or family caregivers. Government-sponsored programs such as
3. The reimbursement method applied, such correctional facilities, military health and
as managed care, workers compensation, Veterans Administration, and public health.
Medicare, or Medicaid. Provider agencies and community-based
4. The health care professional discipline of facilities such as mental/behavioral health
the designated case manager such as but facilities, home health services, ambulatory,
not limited to a registered nurse, social and day care facilities.
worker, physician, rehabilitation counselor, Geriatric services, including residential,
and disability manager. senior centers, assisted living facilities, and
continuing care retirement communities.
The following is a representative list of case Long-term care services, including home,
management practice settings; however, it is not skilled, custodial, and community based
an exhaustive reflection of where professional programs.
case managers exist today. Case managers End-of-Life, hospice, palliative, and respite
practice in: care programs.
Physician and medical group practices,
Hospitals and integrated care delivery Patient Centered Medical Home (PCMH),
systems, including acute care, sub-acute Accountable Care Organizations (ACOs),
care, long-term acute care (LTAC) facilities, and Physician Hospital Organizations
skilled nursing facilities (SNFs), and rehabili- (PHOs).
tation facilities. Life care planning programs.
Ambulatory care clinics and communi- Population health, wellness and prevention
ty-based organizations, including student programs, and disease and chronic care
or university counseling and health care management companies.
centers, medical and health homes, primary
14 CMSA Standards of Practice for Case Management
VI. Professional Case Management Roles
and Responsibilities
It is necessary to differentiate between the terms case managers may vary based on their health
role, function, and activity before de- discipline background and the environment or
scribing the responsibilities of professional case care setting they practice in.
managers. Defining these terms provides a clear Successful care outcomes cannot be
and contextual understanding of the roles and achieved without the specialized skills,
responsibilities of case managers in the various knowledge, and competencies professional
practice settings. case managers apply throughout the case
A role is a general and abstract term that management process. These include, but are
refers to a set of behaviors and expected conse- not limited to, motivational interviewing and
quences that are associated with ones position positive relationship-building; effective written
in a social structure. A function is a grouping or and verbal communication; negotiation and
a set of specific tasks or activities within the role. brokerage of services; cost-conscious allocation
An activity is a discrete action, behavior or task of resources; knowledge of contractual health
a person performs to address the expectations of insurance or risk arrangements; client activation,
the role assumed (Tahan and Campagna, 2010). empowerment, and engagement; the ability to
A role consists of several functions and effect change, perform ongoing evaluation and
each function is described through a list of critical analysis; and the skill to plan, organize,
specific and related activities. These descriptions and manage competing priorities effectively.
constitute what is commonly known as a job To facilitate effective and competent
description (Tahan and Campagna, 2010). The performance, the professional case manager
roles professional case managers assume may should demonstrate knowledge of health insur-
vary based on the same four factors described ance and funding sources, health care services,
earlier in the section entitled, Case Management human behavior dynamics, health care delivery
Practice Settings. and financing systems, community resources,
The professional case manager performs ethical and evidence-based practice, applicable
the primary functions of assessment, planning, laws and regulations, clinical standards and
facilitation, coordination, monitoring, evaluation, outcomes, and health information technology
and advocacy. Integral to these functions is and digital media relevant to case management
collaboration and ongoing communication with practice. The skills and knowledge base of a
the client, clients family or family caregiver, and professional case manager may be applied to
other health care professionals involved in the individual clients such as in the hospital setting,
clients care. Nationally recognized professional or to groups of clients such as in disease, chronic
associations and specialty certifying bodies have care, or population health management models.
identified key responsibilities of case managers Often case managers execute their responsibil-
through expert opinions, practice analyses, and ities across settings, providers, over time, and
roles and functions research. beyond the boundaries of a single episode of
It is not the intent of the Standards of care. They also employ the use of health and
Practice for Case Management to parallel these information technology and tools.
key responsibilities. The Standards broadly define The role functions of professional case
major functions involved in the case manage- managers may include, but are not limited to, the
ment process to achieve desired outcomes. The following:
specific roles and responsibilities of professional
CMSA Standards of Practice for Case Management 15
Considering predictive modeling, screening, support services, consults, and resources
and other data, where appropriate, in de- across involved health providers and care
ciding whether a client would benefit from settings.
case management services. Communicating on an ongoing basis with
Conducting an assessment of the clients the client, clients family or family caregiver,
health, physical, functional, behavioral, other involved health care professionals
psychological, and social needs, includ- and support service providers, and assuring
ing health literacy status and deficits, that all are well-informed and current on
self-management abilities and engagement the case management plan of care and
in taking care of own health, availability services.
of psychosocial support systems including Educating the client, the family or family
family caregivers, and socioeconomic caregiver, and members of the interprofes-
background. The assessment leads to the sional health care team about treatment
development and implementation of a cli- options, community resources, health in-
ent-specific case management plan of care surance benefits, psychosocial and financial
in collaboration with the client and family concerns, and case management services,
or family caregiver, and other essential in order to make timely and informed
health care professionals. care-related decisions.
Identifying target care goals in collabora- Counseling and empowering the client
tion with the client, clients family or family to problem-solve by exploring options
caregiver, and other members of the health of care, when available, and alternative
care team. Securing clients agreement on plans, when necessary, to achieve desired
the target goals and desired outcomes. outcomes.
Planning the care interventions and needed Completing indicated notifications for and
resources with the client, family or family pre-authorizations of services, medical
caregiver, the primary care provider, other necessity reviews, and concurrent or retro-
health care professionals, the payer, and spective communications, based on payers
the community-based agents, to maximize requirements and utilization management
the clients health care responses, quality, procedures.
safety, cost-effective outcomes, and opti- Ensuring the appropriate allocation, use,
mal care experience. and coordination of health care services
Facilitating communication and coordi- and resources while striving to improve
nation among members of the interpro- safety and quality of care, and maintain
fessional health care team, and involving cost effectiveness on a case-by-case basis.
the client in the decision-making process Identifying barriers to care and clients
in order to minimize fragmentation in the engagement in own health; addressing
services provided and prevent the risk for these barriers to prevent suboptimal care
unsafe care and suboptimal outcomes. outcomes.
Collaborating with other health care profes- Assisting the client in the safe transitioning
sionals and support service providers across of care to the next most appropriate level,
care settings, levels of care, and profession- setting, and/or provider.
al disciplines, with special attention to safe Striving to promote client self-advocacy,
transitions of care. independence, and self-determination,
Coordinating care interventions, referrals to and the provision of client-centered and
specialty providers and community-based culturally-appropriate care.
16 CMSA Standards of Practice for Case Management
Advocating for both the client and the applying outcomes measures reflective of
payer to facilitate positive outcomes for organizational policies and expectations,
the client, the interprofessional health care accreditation standards, and regulatory
team, and the payer. However, when a requirements.
conflict arises, the needs of the client must Engaging in performance improvement
be the number one priority. activities with the goal of improving clients
Evaluating the value and effectiveness of access to timely care and services, and
case management plans of care, resource enhancing the achievement of target goals
allocation, and service provision while and desired outcomes.
CMSA Standards of Practice for Case Management 17
VII. Components of the Case
Management Process
The case management process is carried out of effective communication skills such as
within the ethical and legal realms of a case active listening, meaningful conversa-
managers scope of practice, using critical tion, motivational interviewing, and use
thinking and evidence-based knowledge. The of open-ended questions.
overarching themes in the case management Care needs and opportunities are identi-
process include the activities described below. fied through analysis of the assessment
Note that the case management process findings and determination of identified
is cyclical and recurrent, rather than linear and needs, barriers, and/or gaps in care.
unidirectional. For example, key functions of the Assessment is an ongoing process
professional case manager, such as communi- occurring intermittently, as needed, to
cation, facilitation, coordination, collaboration, determine efficacy of the case manage-
and advocacy, occur throughout all the steps of ment plan of care and clients progress
the case management process and in constant toward achieving target goals.
contact with the client, clients family or family Assessment should cover medical,
caregiver, and other members of the interpro- behavioral health, substance use and
fessional health care team. Primary steps in the abuse and social determinants of health.
case management process include: 3. Development of the Case
1. Client Identification, Selection Management Plan of Care:
and Engagement in Professional The case management plan of care is a
Case Management: structured, dynamic tool used to docu-
Focus on screening clients identified or ment the opportunities, interventions,
referred by other professionals for case and expected goals, the professional
management to determine appropriate- case manager applies during the clients
ness for and benefits from services. engagement in case management
Engagement of the client and family or services. It includes:
family caregiver in the process. Identified care needs, barriers and op-
Obtaining consent for case management portunities for collaboration with the
services as part of the case initiation process. client, family and/or family caregiver,
and members of the interprofessional
2. Assessment and Opportunity
care team in order to provide more
Identification:
effective integrated care;
Assessment begins after screening, Prioritized goals and/or outcomes to
identification and engagement in case be achieved; and
management. It involves data gathering, Interventions or actions needed to
analysis, and synthesis of information for reach the goals.
the purpose of developing a client-cen- Client and/or clients family or family
tric case management plan of care. caregiver input and participation in the
Assessment helps establish the development of the case management
client-case manager's relationship and plan of care is essential to promote
the client's readiness to engage in own client-centered care and maximize
health and well-being. It requires the use potential for achieving the target goals.
18 CMSA Standards of Practice for Case Management
4. Implementation and Monitoring activities include assessing
Coordination of the Case clients progress with planned interventions
Management Plan of Care: Evaluating if care goals and interventions
remain appropriate, relevant, and realistic.
The case management plan of care is put
Determining if any revisions or modifica-
into action by facilitating the coordination
tions are needed to the care needs, goals,
of care, services, resources, and health edu-
or interventions specified in the clients
cation specified in the planned interven-
case management plan of care.
tions.
Effective care coordination requires ongo- 6. Closure of the Professional
ing communication and collaboration with Case Management Services:
the client and/or clients family or family Bringing mutually-agreed upon closure to
caregiver, as well as the provider and the the client-case manager relationship and
entire interprofessional health care team. engagement in case management.
5. Monitoring and Evaluation Case closure focuses on discontinuing the
of the Case Management professional case management services
Plan of Care: when the client has attained the highest
level of functioning and recovery, the best
Ongoing follow-up with the client, family
possible outcomes, or when the needs and
and/or family caregiver and evaluation of
desires of the client have changed.
the clients status, goals, and outcomes.
CMSA Standards of Practice for Case Management 19
VIII. Standards of Professional
Case Management Practice
A. STANDARD: CLIENT SELECTION Polypharmacy and medication adher-
PROCESS FOR PROFESSIONAL CASE ence needs
MANAGEMENT SERVICES Poor nutritional status
Poor pain control
The professional case manager should screen
Presence of actionable gaps in care
clients referred for case management services to
and services
identify those who are appropriate for and most
Previous home health and durable
likely to benefit from case management services
medical equipment usage
available within a particular practice setting.
Results of established predictive
modeling analysis and/or health risk
How Demonstrated:
screening tools indicative of need for
Documentation of consistent use of the case management
client selection process within the organiza- Risk taking behaviors
tions policies and procedures.
Recognition that a professional case man-
Use of screening criteria as appropriate to
ager may receive pre-screened client refer-
select a client for inclusion in case manage-
rals from various sources, including (but not
ment. Examples of screening criteria may
limited to) direct referrals from health care
include, but are not limited to:
professionals and system-generated flags,
Barriers to accessing care and services alerts, or triggers. In these situations, the
Advanced age case manager should document the referral
Catastrophic or life-altering conditions source and why the client is appropriate for
Chronic, complex, or terminal conditions case management services.
Concerns regarding self-management
B. STANDARD:
ability and adherence to health regimens
CLIENT ASSESSMENT
Developmental disabilities
End-of-life or palliative care The professional case manager should complete
History of abuse or neglect a thorough individualized client centered assess-
History of mental illness, substance ment that takes into account the unique cultural
use, suicide risk, or crisis intervention and linguistic needs of that client including
Financial hardships clients family or family caregiver as appropriate.
Housing and transportation needs It is recognized that an assessment:
Lack of adequate social support
including family caregiver support is a process, that focuses on evolving client
Low educational levels needs identified by the case manager over
Low health literacy, reading literacy, the duration of the professional relationship
or numeracy literacy levels and across the transitions of care;
Impaired functional status and/or involves each client and/or the clients fami-
cognitive deficits ly or family caregiver as appropriate, and;
Multiple admissions, readmissions, is inclusive of the medical, cognitive,
and emergency department (ED) visits behavioral, social, and functional domains,
Multiple providers delivering care and/ as pertinent to the practice setting (Kathol,
or no primary care provider Perez, & Cohen, 2010) the client uses to
20 CMSA Standards of Practice for Case Management
access care. Learning and technology capabilities
How Demonstrated: Social
Documented client assessments using stan- Psychosocial status:
dardized tools, both electronic and written, Family or family caregiver dynamics
when appropriate. The assessment may Caregiver resources: availability and
include, but is not limited to the following degree of involvement
components: Environmental and residential
Financial Circumstances
Medical
Client beliefs, values, needs, and prefer-
Presenting health status and conditions ences including cultural and spiritual
Medical history including use of pre- Access to care
scribed or over the counter medica- Health insurance status and avail-
tions and herbal therapies ability of health care benefits
Relevant treatment history
Health care providers involved in
Prognosis
clients care
Nutritional status
Barriers to getting care and resources
Cognitive and Behavioral Safety concerns and needs
History of neglect, abuse, violence,
Mental health
or trauma
History of substance use
Safety of the living situation
Depression risk screening
Advanced directives planning and
History of treatment including
availability of documentation
prescribed or over the counter
Pertinent legal situations (e.g. custody,
medications and herbal therapies
marital discord, and immigration
Cognitive functioning
status)
Language and communication
preferences, needs, or limitations Functional
Client strengths and abilities Client priorities and self-identified care
Self-care and self-management goals
capability Functional status
Readiness to change Transitional or discharge planning needs
Client professional and educational
and services, if applicable
focus Health care services currently receiv-
Vocational and/or educational ing or recently received in the home
interests setting
Recreational and leisure pursuits Skilled nursing, home health aide,
Self-Management and Engagement
durable medical equipment (DME),
Status or other relevant services
Health literacy Transportation capability and con-
Health activation level straints
Knowledge of health condition Follow-up care (e.g., primary care,
Knowledge of and adherence to specialty care, and appointments)
plan of care Safety and appropriateness of home
Medication management and adherence or residential environment
CMSA Standards of Practice for Case Management 21
Reassessment of the clients condition, services and resources
response to the case management plan Use of multiple providers and/or agen-
of care and interventions, and progress cies
toward achieving care goals and target Lack of integrated care
outcomes. Use of inappropriate services or level of
Documentation of resource utilization care
and cost management, provider options, Lack of a primary provider or any
and available health and behavioral care provider
benefits. Non-adherence to the case manage-
Evidence of relevant information and data ment plan of care (e.g. medication
required for the clients thorough assess- adherence) which may be associated
ment and obtained from multiple sources with the following:
including, but not limited to: Low reading level
Client interviews; Low health literacy and/or numeracy
Initial and ongoing assessments Low health activation levels
and care summaries available in the Language and communication
clients health record and across the barriers
transitions of care; Lack of education or understanding of:
Family caregivers (as appropriate), Disease process
physicians, providers, and other Current condition(s)
involved members of the interprofes- The medication list
sional health care team; Substance use and abuse
Past medical records available as Social determinants of health
appropriate; and Lack of ongoing evaluation of the
Claims and administrative data. client's limitations in the following
aspects of health condition:
C. STANDARD: Medical
CARE NEEDS AND OPPORTUNITIES Cognitive and Behavioral
IDENTIFICATION Social
Functional
The professional case manager should identify the
Lack of support from the clients family
clients care needs or opportunities that would
or family caregiver especially when
benefit from case management interventions.
under stress
How Demonstrated: Financial barriers to adherence of the
Documented agreement among the client case management plan of care
and/or clients family or family caregiver, Determination of patterns of care or
and other providers and organizations behavior that may be associated with
regarding the care needs and opportunities increased severity of condition
identified. Compromised client safety
Documented identification of opportunities Inappropriate discharge or delay from
for intervention, such as: other levels of care
Lack of established, evidenced-based High cost injuries or illnesses
plan of care with specific goals Complications related to medical,
Over-utilization or under-utilization of psychosocial or functional condition or
22 CMSA Standards of Practice for Case Management
needs indicators expected to be achieved within
Frequent transitions between care specified time frames. These measures
settings or providers could include clinical as well as non-clinical
Poor or no coordination of care be- domains of outcomes management. For ex-
tween settings or providers ample, access to care, cost-effectiveness of
care, safety and quality of care, and clients
D. STANDARD: PLANNING experience of care.
Evidence of supplying the client, clients
The professional case manager, in collaboration
family, or family caregiver with information
with the client, clients family or family caregiver,
and resources necessary to make informed
and other members of the interprofessional health
decisions.
care team, where appropriate, should identify rele-
Promoted awareness of client care goals,
vant care goals and interventions to manage the
outcomes, resources, and services included
clients identified care needs and opportunities.
in the case management plan of care.
The case manager should also document these in
Adherence to payer expectations with re-
an individualized case management plan of care.
spect to how often to contact and reevalu-
How Demonstrated: ate the client, redefine long and short term
Documented relevant, comprehensive goals, or update the case management
information and data using analysis of plan of care.
assessment findings, client and/or clients
family or family caregiver interviews, input E. STANDARD: MONITORING
from the clients interprofessional health The professional case manager should employ
care team, and other methods as needed ongoing assessment with appropriate documen-
to develop an individualized case manage- tation to measure the clients response to the case
ment plan of care. management plan of care.
Documented client and/or clients family or
How Demonstrated:
family caregiver participation in the devel-
opment of the written case management Documented ongoing collaboration with
plan of care. the client, family or family caregiver, pro-
Documented client agreement with the viders, and other pertinent stakeholders, so
case management plan of care, including that the clients response to interventions
agreement with target goals, expected is reviewed and incorporated into the case
outcomes, and any changes or additions to management plan of care.
the plan. Awareness of circumstances necessitating
Recognized clients needs, preferences, and revisions to the case management plan of
desired role in decision-making concerning care, such as changes in the clients condition,
the development of the case management lack of response to the case management
plan of care. interventions, change in the clients prefer-
Validated that the case management plan ences, transitions across care settings and/or
of care is consistent with evidence-based providers, and barriers to care and services.
practice, when such guidelines are available Evidence that the plan of care continues to
and applicable, and that it continues to be reviewed and is appropriate, under-
meet the clients changing needs and stood, accepted by client and/or clients
health condition. family or family caregiver, and documented.
Established measurable goals and outcome Ongoing collaboration with the client,
CMSA Standards of Practice for Case Management 23
family or family caregiver, providers, and Applied evidence-based guidelines relevant
other pertinent stakeholders regarding any to the care of specific client populations.
revisions to the plan of care. Evaluated client and/or clients family or
family caregiver experience with case
F. STANDARD: OUTCOMES management services.
Used national performance measures for
The professional case manager, through a thor-
transitional care and care coordination such
ough individualized client-centered assessment,
as those endorsed by the regulatory, ac-
should maximize the clients health, wellness,
creditation, and certification agencies, and
safety, physical functioning, adaptation, health
health-related professional associations to
knowledge, coping with chronic illness, engage-
ultimately enhance quality, efficiency and
ment, and self-management abilities.
optimal client experience.
How Demonstrated:
G. STANDARD: CLOSURE OF
Created a case management plan of care PROFESSIONAL CASE MANAGEMENT
based on the thorough individualized SERVICES
client-centered assessment.
The professional case manager should appropri-
Achieved through quality and cost-effi-
ately complete closure of professional case man-
cient case management services, clients
agement services based upon established case
satisfaction with the experience of care,
closure guidelines. The extent of applying these
shared and informed decision-making, and
guidelines may differ in various case management
engagement in own health and health care.
practice and/or care settings.
Evaluated the extent to which the goals
and target outcomes documented in the How Demonstrated:
case management plan of care have been Achieved care goals and target outcomes,
achieved. including those self-identified by the client
Demonstrated efficacy, efficiency, qual- and/or clients family or family caregiver.
ity, safety, and cost-effectiveness of the Identified reasons for and appropriateness
professional case managers interventions of closure of case management services,
in achieving the goals documented in the such as:
case management plan of care and agreed Reaching maximum benefit from case
upon with the client and/or clients family management services;
caregiver. Change of health care setting which
Measured and reported impact of the case warrants the transition of the clients
management plan of care. care to another health care provider(s)
Applied evidence-based adherence guide- and/or setting;
lines, standardized tools and proven care The employer or purchaser of case
processes. These can be used to measure management services requests the
the clients preference for, and understand- closure of case management;
ing of: Services no longer meet program or
The proposed case management plan
benefit eligibility requirements;
of care and needed resources; Client refuses further case manage-
Motivation to change and demonstrate
ment services;
healthy lifestyle behavior; and Determination by the professional case
Importance of availability of engaged
manager that he/she is no longer able
client, family or family caregiver.
24 CMSA Standards of Practice for Case Management
to provide appropriate case manage- The professional case manager should facilitate
ment services because of situations coordination, communication, and collaboration
such as a clients ongoing disen- with the client, clients family or family caregiver,
gagement in self-management and involved members of the interprofessional health
unresolved non-adherence to the case care team, and other stakeholders, in order to
management plan of care; achieve target goals and maximize positive client
Death of the client; care outcomes.
There is a conflict of interest; and
How Demonstrated:
When a dual relationship raises ethical
concerns. Recognition of the professional case man-
Evidence of agreement for closure of case agers role and practice setting in relation
management services by the client, family to those of other providers and organiza-
or family caregiver, payer, professional case tions involved in the provision of care and
manager, and/or other appropriate parties. case management services to the client.
Evidence that when a barrier to closure of Developing and sustaining proactive
professional case management services client-centered relationships through open
arises, the case manager has discussed the communication with the client, clients fam-
situation with the appropriate stakeholders ily or family caregiver, and other relevant
and has reached agreement on a plan to stakeholders, to maximize outcomes and
resolve the barrier. enhance clients safety and optimal care
Documented reasonable notice for closure experience.
of professional case management services Evidence of facilitation, coordination, and
and actual closure that is based upon the collaboration to support the transitions of
facts and circumstances of each individual care, including:
Transfers of clients to the most ap-
clients case and care outcomes supporting
case closure. Evidence should show verbal propriate health care provider or care
and/or written notice of case closure to the setting are coordinated in a timely and
client and other directly involved health complete manner.
Documentation reflective of the col-
care professionals and support service
providers. laborative and transparent communi-
Evidence of client education about service cation between the professional case
and/or funding resources provided by the manager and other health care team
professional case manager to address members, especially during each transi-
any further needs of the client upon case tion to another level of care within or
closure. outside of the clients current setting.
Use of the case management plan
Completed transition of care handover to
health care providers at the next level of of care, target goals, and clients
care, where appropriate, with permission needs and preferences to guide the
from client, and inclusive of communication facilitation and coordination of services
of relevant client information and continuity and collaboration among members
of the case management plan of care to of the interprofessional health care
optimize client care outcomes. team, client and clients family or family
caregiver.
H. STANDARD: Adherence to client privacy and confi-
FACILITATION, COORDINATION, dentiality mandates during all aspects of
AND COLLABORATION
CMSA Standards of Practice for Case Management 25
facilitation, coordination, communication, from an institution that is fully accredited
and collaboration within and outside the by a nationally recognized educational
clients care setting. accreditation organization, and;
Use of special techniques and strate- The individual must have completed a su-
gies such as motivational interviewing, pervised field experience in case manage-
mediation, and negotiation, to facilitate ment, health or behavioral health as part of
transparent communication and building of the degree requirements.
effective relationships. How Demonstrated:
Coordination and implementation of the
use of problem-solving skills and tech- Possession of the education, experience,
niques to reconcile potentially differing and expertise required for the professional
points of view. case managers area(s) of practice.
Evidence of collaboration that optimizes Compliance with national, state, and/or
client outcomes; this may include working local laws and regulations that apply to the
with community, local and state resources, jurisdiction(s) and discipline(s) in which the
primary care providers, members of the in- professional case manager practices.
terprofessional health care team, the payer, Maintenance of competence through
and other relevant stakeholders. participation in relevant and ongoing con-
Evidence of collaborative efforts to maxi- tinuing education, certification, academic
mize adherence to regulatory and accred- study, and internship programs.
itation standards within the professional Practicing within the professional case
case managers practice and employment managers area(s) of expertise, making
setting. timely and appropriate referrals to, and
seeking consultation with, others when
I. STANDARD: needed.
QUALIFICATIONS FOR
PROFESSIONAL CASE MANAGERS Supervision
The professional case manager should maintain The professional case manager acts in a super-
competence in her/his area(s) of practice by visory and/or leadership role of other personnel
having one of the following: who are unable to function independently due to
limitations of license and/or education.
Current, active and unrestricted licensure or Due to the variation in academic de-
certification in a health or human services grees and other educational requirements, it
discipline that allows the professional to is recommended that individuals interested in
conduct an assessment independently as pursuing a professional case management career
permitted within the scope of practice of seek guidance as to the appropriate educational
the discipline; or preparation and academic degree necessary to
In the case of an individual who practices practice case management. These interested
in a state that does not require licensure individuals may seek the Case Management So-
or certification, the individual must have a ciety of America, American Nurses Association,
baccalaureate or graduate degree in social or Commission for Case Manager Certification,
work or another health or human services or other relevant professional organizations for
field that promotes the physical, psycho- further advice and guidance.
social, and/or vocational well-being of the
persons being served. The degree must be NOTE: Social workers who are prepared at the
26 CMSA Standards of Practice for Case Management
Masters in Social Work (MSW) degree level and lands, any issues of concern should direct them
educated under a program that would preclude to the licensing authority and/or federal law.
them from sitting for licensure (where required)
or practice at the clinical level should consult with How Demonstrated:
their state licensing board to determine if additional Demonstration of up-to-date knowledge
education and/or practicum hours are required. of, and adherence to, applicable laws and
J. STANDARD: LEGAL regulations concerning confidentiality, pri-
vacy, and protection of the clients medical
The professional case manager shall adhere to information.
all applicable federal, state, and local laws and Evidence of a good faith effort to obtain
regulations, which have full force and effect the clients written acknowledgement that
of law, governing all aspects of case manage- she/he has received notice of privacy rights
ment practice including, but not limited to, and practices.
client privacy and confidentiality rights. It is the
responsibility of the professional case manager 2. Standard:
to work within the scope of his/her license and/ Consent for Professional Case
or underlying profession. Management Services
The professional case manager should obtain
NOTE: In the event that the professional case appropriate and informed consent before the
managers employer policies or those of other implementation of case management services.
entities are in conflict with applicable legal
How Demonstrated:
requirements, the case manager should under-
stand that the law prevails. In these situations, Evidence that the client and/or clients fam-
case managers should seek clarification of ily or family caregiver have been thoroughly
questions or concerns from an appropriate and informed with regard to:
reliable expert resource, such as a legal counsel, Proposed case management process
compliance officer, or an appropriate govern- and services relating to the clients
ment agency. health condition(s) and needs;
Possible benefits and costs of such
1. Standard: services;
Confidentiality and Client Privacy Alternatives to proposed services;
Potential risks and consequences of
The professional case manager should adhere
to federal, state, and local laws, as well as proposed services and alternatives; and
Clients right to decline the proposed
policies and procedures, governing client privacy
and confidentiality, and should act in a manner case management services and aware-
consistent with the clients best interest in all ness of potential risks and consequenc-
aspects of communication and recordkeeping es of such decision.
whether through traditional paper records and/or Evidence that the information was commu-
electronic health records (EHR). nicated in a client-sensitive manner, which
is intended to permit the client to make
NOTE: Federal law preempts (supersedes) voluntary and informed choices.
state and local law and provides a minimum Documented informed consent where client
mandatory national standard; states may enlarge consent is a prerequisite to the provision of
client rights, but not reduce them. For those who case management services.
work exclusively on federal enclaves or on tribal
CMSA Standards of Practice for Case Management 27
K. STANDARD: ETHICS and policy-making levels. The case manager is
uniquely positioned as an expert in care coordi-
The professional case manager should behave
nation and advocacy for health policy change to
and practice ethically, and adhere to the tenets
improve access to quality, safe, and cost-effec-
of the code of ethics that underlie her/his profes-
tive services.
sional credentials (e.g., nursing, social work, and
rehabilitation counseling). How Demonstrated:
How Demonstrated: Documentation demonstrating:
Promotion of the clients self- de-
Awareness of the five basic ethical princi-
termination, informed and shared
ples and how they are applied. These are:
Beneficence (to do good),
decision-making, autonomy, growth,
Nonmaleficence (to do no harm),
and self-advocacy.
Education of other health care and
Autonomy (to respect individuals
service providers in recognizing and
rights to make their own decisions),
Justice (to treat others fairly), and
respecting the needs, strengths, and
Fidelity (to follow-through and to keep
goals of the client.
Facilitation of client access to necessary
promises).
and appropriate services while edu-
Recognition that:
A primary obligation is to the clients
cating the client and family or family
caregiver about resource availability
cared for, with
A secondary obligation is engagement
within practice settings.
Recognition, prevention, and elim-
in and maintenance of respectful rela-
ination of disparities in accessing
tionships with coworkers, employers,
high-quality care and experiencing
and other professionals.
Laws, rules, policies, insurance bene-
optimal client health care outcomes,
as related to race, ethnicity, national
fits, and regulations are sometimes in
origin, and migration background; sex
conflict with ethical principles. In such
and marital status; age, religion, and
situations, the professional case man-
political belief; physical, mental, or
ager is bound to address the conflicts
cognitive disability; gender identity or
to the best of her/his abilities and/or
gender expression; or other cultural
seek appropriate consultation.
All clients are unique individuals and
factors.
Advocacy for expansion or establish-
the professional case manager en-
ment of services and for client-centered
gages them without regard to gender
changes in organizational and govern-
identity, race or ethnicity, and practice,
mental policy.
religious, other cultural preferences, or
Ensuring a culture of safety by engagement
socioeconomic status.
in quality improvement initiatives in the
Maintained policies that are universally
workplace.
respectful of the integrity and worth of
Encouraging the establishment of client,
each person.
family and/or family caregiver advisory
L. STANDARD: ADVOCACY councils to improve client-centered care
The professional case manager should advocate standards within the organization.
for the client, clients family or family caregiver, Joining relevant professional organizations
at the service delivery, benefits administration, in call to action campaigns, whenever
28 CMSA Standards of Practice for Case Management
possible, to improve the quality of care and N. STANDARD: RESOURCE
reduce health disparities. MANAGEMENT AND STEWARDSHIP
Recognition that client advocacy can The professional case manager should inte-
sometimes conflict with a need to balance grate factors related to quality, safety, access,
cost constraints and limited resources.
and cost-effectiveness in assessing, planning,
Documentation indicates that the profes- implementing, monitoring, and evaluating health
sional case manager has weighed decisions resources for client care.
with the intent to uphold client advocacy,
whenever possible. How Demonstrated:
M. STANDARD: Documented evaluation of safety, effec-
CULTURAL COMPETENCY tiveness, cost, and target outcomes when
designing a case management plan of care
The professional case manager should maintain to promote the ongoing care needs of the
awareness of and be responsive to cultural and client.
linguistic diversity of the demographics of her/ Evidence of follow-through on the ob-
his work setting and to the specific client and/or jectives of the case management plan of
caregiver needs. care which are based on the ongoing care
How Demonstrated: needs of the client and the competency,
knowledge, and skills of the professional
Evidence of communicating in an effective,
case manager.
respectful, and sensitive manner, and in
Application of evidence-based guidelines
accordance with the clients cultural and
and practices, when appropriate, in recom-
linguistic context.
mending resource allocation and utilization
Assessments, goal-setting, and develop-
options.
ment of a case management plan of care
Evidence of linking the client and fam-
to accommodate each clients cultural and
ily or family caregiver with cultural and
linguistic needs and preference of services.
linguistically appropriate resources to meet
Identified appropriate resources to enhance
the needs and goals identified in the case
the clients access to care and improve
management plan of care.
health care outcomes. These may include
Documented communication with the client
the use of interpreters and health educa-
and family or family caregiver about the
tional materials which apply language and
length of time for availability of a necessary
format demonstrative of understanding of
resource, potential and actual financial
the clients cultural and linguistic commu-
responsibility associated with a resource,
nication patterns, including but not limited
and the range of outcomes associated with
to speech volume, context, tone, kinetics,
resource utilization.
space, and other similar verbal/non-verbal
Documented communication with the
communication patterns.
client and other interprofessional health
Pursuit of professional education to
care team members, especially during care
maintain and advance ones level of cultural
transitions or when there is a significant
competence and effectiveness while work-
change in the clients situation.
ing with diverse client populations.
Evidence of promoting the most effective
and efficient use of health care services and
financial resources.
CMSA Standards of Practice for Case Management 29
Documentation which reflects that the Accountability and responsibility for
intensity of case management services own professional development and
rendered corresponds with the needs of the advancement.
client. Participation in ongoing training and/
or educational opportunities (e.g.,
O. STANDARD:
conferences, webinars, academic programs)
PROFESSIONAL RESPONSIBILITIES
to maintain and expand ones skills,
AND SCHOLARSHIP
knowledge and competencies.
The professional case manager should engage Participation in research activities which
in scholarly activities and maintain familiarity support quantification and definition of
with current knowledge, competencies, case valid and reliable outcomes, especially
management-related research, and evidence- those that demonstrate the value of case
supported care innovations. The professional management services and their impact on
case manager should also identify best practices the individual client and population health.
in case management and health care service Identification and evaluation of best
delivery, and apply such in transforming practice, practices and innovative case management
as appropriate. interventions.
How Demonstrated: Leveraging opportunities in the
employment setting to conduct innovative
Incorporation of current and relevant
performance improvement projects and
research findings into ones practice,
formally report on their results.
including policies, procedures, care
Dissemination, through publication and/
protocols or guidelines, and workflow
or presentation at conferences, of practice
processes, and as applicable to the care
innovations, research findings, evidence-
setting.
based practices, and quality or performance
Efficient retrieval and appraisal of research
improvement efforts.
evidence that is pertinent to ones practice
Membership in professional case
and client population served.
management-related associations and
Proficiency in the application of research-
involvement in local, regional, or national
related and evidence-based practice tools
committees and taskforces.
and terminologies.
Mentoring and coaching of less experienced
Ability to distinguish peer-reviewed
case managers, other interprofessional
materials (e.g., research results,
health care team members, and providers.
publications) and apply preference to
such work in practice, as available and
appropriate.
30 CMSA Standards of Practice for Case Management
XI. Acknowledgements
We, the CMSA and its Board of Directors, extend Sandra Lowery, BSN, RN, CCM, CNLCP
our gratitude to all of the professionals who Kathleen Moreo, BSN, BHSA, RN-BC, CCM,
graciously gave their time and expertise to revise CDMS
and comment on the Standards of Practice for Deborah Smith, MN, RN-BC
Case Management (2016). Charlotte Sortedahl, MPH, MS, DNP, RN, CCM
We would especially like to thank those CMSA Board of Directors:
who participated in the various workgroups: Kathleen Fraser, MSN, MHA, RN-BC, CCM,
Taskforce Chairs: CRRN, President 2014-2016
Mary Beth Newman, MSN, RN-BC, A-CCC, Mary McLaughlin-Davis, MSN, PhD, RN,
CMAC, CCP, MEP ACNS-BC, CCM, President-Elect 2015-2016
Kathleen Fraser, MSN, MHA, RN-BC, CCM, Rebecca Perez, BSN, RN, CCM,
CRRN Secretary 2015-2017
Catherine Campbell, MSN, MBA, RN, CCM, CHC,
Executive Director, CMSA:
FACHE, Treasurer 2014-2017
Cheri Lattimer, BSN, RN
Debra Bellitter, MBA, RN, CCM,
Staff Liaisons: Danielle Marshall, Director 2013-2016
Valerie Emmons, and Michele Lee Veronica Chepak, BSN, MPA, RN,
Contributor and Medical Writer: Director 2014-2016
Hussein M. Tahan, PhD, RN Margaret Chu, BSN, MPA, RNC, CCM, CPHQ,
Director 2014-2017
Legal Review: Barbara Dunn ONeal, Partner,
Janet Coulter, MSN, MS, RN, CCM,
Barnes & Thornburg, LLP
Director 2014-2017
Revision Taskforce Members: Deborah Gutteridge, MS, CBIST,
Margaret Chu, BSN, MPA, RN, RNC, CCM, CPHQ Director 2015-2018
Ellen Fink-Samnick, MSW, ACSW, LCSW, CCM, Jose Santoro, MBA, Director 2013-2016
CRP Stefany Almaden, MSN, PHD, RN, CCM, CPUM,
Deborah Gutteridge, MS, CBIST CMCN, Chapter Presidents Council Rep,
Mary McLaughlin-Davis, PhD, MSN, RN, 2015-2016
ACNS-BC, CCM
Lynn S. Muller, JD, BA-HCM, RN, CCM
Patricia Noonan, MBA, RN, CCM
Teresa M. Treiger, MA, RN-BC, CHCQM-CM/
TOC, CCM
Sandra Zawalski, BSN, RN, CRRN, CCM, MSCC,
ABDA
Peer Review Members:
Catherine Campbell, MSN, MBA, RN, CCM, CHC,
FACHE
Michael Demoratz, PhD, LCSW, CCM
Margaret (Peggy) Leonard, MS, RN-BC, FNP
Anne Llewellyn, BHSA, MS, RN-BC, CCM, CRRN
CMSA Standards of Practice for Case Management 31
X. Glossary
Activity: A discrete action, behavior, or task a of care produced by each provider to address
person performs to meet the expectations of the specific health concerns. It serves as a blueprint
role assumed. For example, an acute care case shared by all [health care team] participants
manager completes concurrent reviews with a to guide individuals care. As such, it provides
payer-based case manager (Tahan & Campagna, the structure required to coordinate care across
2010). multiple sites, providers and episode of care
(Standards & Interoperability Longitudinal Coor-
Advocacy: The act of recommending, pleading
dination of Care Workgroup, 2012, pg.2).
the cause of another; to speak or write in favor of.
Case Management: A collaborative process
Assessment: A systematic process of data col-
of assessment, planning, facilitation, care coor-
lection and analysis involving multiple elements
dination, evaluation and advocacy for options
and sources.
and services to meet an individuals and familys
Care Coordination: (1) The deliberate orga- comprehensive health needs through commu-
nization of patient care activities between two or nication and available resources to promote
more participants (including the patient) involved patient safety, quality of care, and cost effective
in a patients care to facilitate the appropriate outcomes (CMSA, 2016).
delivery of health care services. Organizing
Case Management Plan of Care: A
care involves the marshalling of personnel and
comprehensive plan that includes a statement of
other resources needed to carry out all required
the clients care needs, opportunities, and goals
patient care activities, and is often managed by
determined upon a thorough assessment of the
the exchange of information among participants
client; strategies to address these needs; and
responsible for different aspects of care (AHRQ,
measurable outcomes to demonstrate resolution
2007). (2) A function that helps ensure that
of the care needs and achievement of goals,
the patients needs and preferences for health
the time frame, the resources available, and the
services and information sharing across people,
desires and motivation of the client. The plan of
functions, and sites are met over time (NQF,
care should address the multiple conditions the
2010, p.1).
client suffers and the necessary involvement of
Care Management: (1) Often refers to the providers and support service personnel within
management of long-term health care, legal, and across care settings.
and financial services by professionals serving
Case Management Process: The man-
social welfare, aging and nonprofit care delivery
ner in which case management functions are
systems. Services are delivered under a psycho-
performed, including: client identification,
logical model (Powell & Tahan, 2008, pg.162).
selection and engagement in case management;
(2) A healthcare delivery process that helps
assessment and opportunity identification; devel-
achieve better health outcomes by anticipating
opment of the case management plan of care
and linking clients with the services they need
including specification of care goals and target
more quickly. It also helps to avoid unnecessary
outcomes; implementation and coordination of
services by preventing health problems from
the case management plan of care; monitoring
escalating.
and evaluation of the case management plan of
Care Plan: A document that represents the care; closure of case management services.
synthesis and reconciliation of the multiple plans
32 CMSA Standards of Practice for Case Management
Certification: A process by which a govern- of the clients support. (2) Client can also imply
ment or non-government agency grants recog- the business relationship with a company which
nition to those who have met predetermined contracts or pays for case management services.
qualifications as set forth by a credentialing The first definition is the one used throughout
body. the Standards of Practice 2016.
Chronic Care Management: An approach Client Support System: The clients support
to care which encompasses the oversight system is defined by each client and may include
of health and human service provision and biological relatives, a spouse, a partner, friends,
education activities conducted by health care neighbors, colleagues, a health care proxy, or
professionals to assist individuals with one or any individual who supports the client.
more chronic illnesses, such as diabetes, asthma, Consumer: A person who is the direct or
high blood pressure, heart failure, end stage indirect recipient of the services of the organi-
renal disease, and HIV or AIDS, to understand zation. Depending on the context, consumers
their health condition and live productive lives. may be identified by different names, such as
This approach involves motivating patients to client, member, enrollee, beneficiary,
become actively engaged in own health, adhere patient, injured worker, claimant, college
to necessary therapies and interventions, and student, or resident. A consumer relationship
achieve acceptable health outcomes including may exist even in cases where there is not a
reasonable quality of life and well-being. direct relationship between the consumer and
Chronic Care Management Services: the organization. For example, if an individual
Reimbursable care coordination services provid- is a member of a health plan that relies on the
ed to Medicare beneficiaries with two or more services of a utilization management organiza-
chronic conditions which place the beneficiary tion, then the individual is a consumer of the
at significant risk for death, acute exacerbation utilization management organization.
or functional decline; and require the implemen- Cultural Competence: The process by which
tation of comprehensive plans of care that are individuals and systems understand and respond
monitored over time. The services are accessible respectfully and effectively to people of all
on a 24-hour-a-day, 7-day-a week basis and cultures, languages, classes, races, ethnic back-
consist of at least 20 minutes of clinical staff grounds, religions, and other diversity factors in
time directed by a physician or another qualified a manner that recognizes, affirms, and values the
health care professional during a calendar worth of individuals, families, and communities
month. The services include systematic assess- and protects and preserves the dignity of each
ments of the beneficiarys medical, functional, (NASW, 2007).
and psychosocial needs; preventive services; a
review of medication reconciliation, adherence, Culture: The integrated pattern of human be-
and self-management; and creation of client-cen- havior that includes thoughts, communications,
tered care transitions (USDHHS - CMS, 2015a). actions, customs, beliefs, values, practices, cour-
tesies, relationships, languages, manners, rituals
Client: (1) Individual who is the recipient of and institutions of a racial, ethnic, religious,
case management services. This individual can social, or political group. Culture may include,
be a patient, beneficiary, injured worker, claim- but is not limited to, race, ethnicity, national
ant, enrollee, member, college student, resident, origin, and migration background; sex, sexual
or health care consumer of any age group. In ad- orientation, and marital status; age, religion,
dition, the term client may also infer the inclusion and political belief; physical, mental, or cognitive
CMSA Standards of Practice for Case Management 33
disability; gender, gender identity, or gender Health & National Alliance for Caregiving, 2010,
expression (Cross, T., Bazron, B., Dennis, K., & pg. 1).
Isaacs, M., as cited in USDHHS, OMH, 2001). Function: A grouping or a set of specific tasks
Disease Management: A system of coordi- within a role. The set of tasks that constitutes
nated health care interventions and communi- one function tends to focus on a common theme
cations for populations with conditions in which and share the same goal; for example, evalua-
patient self-care efforts are significant. This tion of outcomes or coordination of treat-
system supports the physician or practitioner/ ments (Tahan & Campagna, 2010).
client relationship and plan of care; emphasizes Handover: sometimes referred to as handoff.
prevention of exacerbations and complications The transfer of authority, responsibility and ac-
using evidence-based practice guidelines and countability for something to another individual.
patient empowerment strategies; and evaluates In the context of professional case management,
clinical, humanistic, and economic outcomes handover refers to the transfer of authority,
on an on-going basis with the goal of improv- responsibility and accountability for the care of a
ing overall health. Because of the presence of client to another health care professional within
co-morbidities or multiple conditions in most or outside a health care setting as indicated
high-risk patients, this approach may become based on the clients needs and care goals.
operationally difficult to execute, with patients
being cared for by more than one program. over Health: In addition to the four definitions
time, the industry has moved more toward a of health listed below (based on the World
whole person model in which all the diseases Health Organizations Key Policy Documents con-
a patient has are managed by a single disease cerning Humanitarian Health Action-Definitions,
management program (Population Health retrieved from http://www.who.int/hac/about/
Alliance, 2016). definitions/en/ on May 23, 2016, case man-
agements definition of health takes on a more
Evidence-Based Criteria: Guidelines for comprehensive meaning that includes biopsy-
clinical practice that incorporate current and chosocial, as well as educational and vocational,
validated research findings. aspects of the client.
Family: Family members and/or those indi- 1. health is a state of complete physical, men-
viduals designated by the client as the clients tal and social well-being and not merely
support system. Family members are not limited the absence of disease or infirmity (World
to blood relatives; they rather constitute any Health Organization, 1946).
person the client wishes to designate as family or 2. The extent to which an individual or a
support system. group is able to realize aspirations and
Family Caregiver: A person who cares for satisfy needs, and to change or cope with
relatives or loved ones. The care recipient may the environment. health is a resource for
be a member of the caregivers family of origin, everyday life, not the objective of living; it
or his or her family of choice, such as a friend, is a positive concept, emphasizing social
neighbor, support group member or life partner. and personal resources as well as physical
In either instant, the term family caregiver capabilities (World Health Organization,
refers to a non-professional who provides unpaid 1984).
care for others in the home and usually such 3. A state characterized by anatomic, physi-
person is identified as the designated caregiver ologic and psychological integrity; ability
by the recipient of care her/himself (Emblem to perform personally valued family, work
34 CMSA Standards of Practice for Case Management
and community roles; ability to deal with care plans, while considering the clients person-
physical, biologic, psychological and social al needs, preferences, and treatment options.
stress; a feeling of well-being; and freedom Licensure: licensure is a process by which a
from the risk of disease and untimely death government agency grants permission to an indi-
(Stokes, Noren, & Shindell, 1982).
vidual to engage in a given occupation, provided
4. A state of equilibrium between humans and that person possesses the minimum degree of
the physical, biologic and social envi- competency required to reasonably protect public
ronment, compatible with full functional health, safety, and welfare.
activity (Last, 1997).
Managed Care: Services or strategies
Health Literacy: The degree to which designed to improve access to care, quality
individuals have the capacity to obtain, process of care, and the cost-effective use of health
and understand basic health information needed resources. Managed care services include, but
to make appropriate health decisions (USDHHS- are not limited to, case management, utilization
HRSA, 2016). management, peer review, disease management,
Health Numeracy: The ability to access, use, and population health.
interpret, and communicate mathematical and Medical Home: A medical home model
quantitative health information and ideas, to provides accessible, continuous, coordinated
engage in and manage mathematical demands and comprehensive patient-centered care, and
and computations in a range of situations (CDC, is managed centrally by a primary care physician
2015). with the active involvement of non-physician
Health Outcomes: Changes in current or practice personnel. Providers deemed a medical
future health status of individuals, groups, or home may receive supplemental payments
communities that can be attributed to anteced- to support operations expected of a medical
ent actions or measures (EURO European Centre home. Physician practices may be encouraged or
for Health Policy, 1999). The change may be required to improve practice infrastructure and
the result of a planned intervention or series of meet certain qualifications in order to achieve
interventions, regardless of whether such an eligibility.
intervention was intended to change an individu- Outcomes: Measurable results of case man-
als health status. agement interventions, such as client knowl-
Health Services: Medical and/or health and edge, adherence, self-care, satisfaction, and
human services. attainment of a meaningful lifestyle.
Interprofessional Health Care Team: (1) Patient Activation: also known as client
Health care professionals with complementary activation. A behavioral concept that focuses on
roles, knowledge, and skills who are commit- patient involvement and contributes to engage-
ted to a common purpose, performance goals, ment. It is patients knowledge, skills, ability,
and approach for which they hold themselves willingness, and confidence to manage own
mutually accountable. (2) Relevant medical and health and health care (Hibbard & Gilburt, 2014;
allied health professionals coming together in a Health Policy Brief, 2013).
relational and client-centered approach to care Patient Engagement: also known as client
provision where they collaboratively develop a engagement. A broader concept that combines
client-centered case management plan of care patient activation with interventions designed to
and discuss care options and make joint deci- increase activation and promote positive patient
sions about the clients treatment and supportive
CMSA Standards of Practice for Case Management 35
behavior, such as obtaining preventive care or activities. Usually, organizations and employers
exercising regularly (Health Policy Brief, 2013, use a persons title as a proxy for her/his role; for
pg.1). Patient engagement is known to increase example, acute care case manager (Tahan &
patients' participation in informed and shared Campagna, 2010).
decision making regarding their care options and
Speech Context: A communication pattern
to improve health outcomes. referring to the use/non-use of emotion by an
Payer: An individual or entity that funds related individual in verbal communication.
services, income, and/or products for an individ- Speech Kinetics: A communication pattern
ual with health needs. referring to the use of stance, gestures, eye
Plan of Care: see Care Plan. Some experts behavior and other posturing by an individual in
may refer to a plan of care to mean an individual nonverbal communication.
clinicians plan to caring for a client with one Speech Space: A communication pattern
or multiple conditions while a care plan is the referring to the physical distance or comfort
integration of the plans designed by multiple proximity selected by an individual when com-
providers to caring for a client with multiple con- municating with another individual.
ditions (Standards & Interoperability Longitudinal
Coordination of Care Workgroup, 2012). Speech Volume: A communication pattern
referring to the level of loudness or softness used
Predictive Modeling: Modeling is the by an individual in verbal communication.
process of mapping relationships among data
elements that have a common thread. Through Standard: An authoritative statement agreed to
predictive modeling, data are mined with and promulgated by the practice based on which
software to examine and recognize patterns the quality of practice and service can be judged.
and trends, which can then potentially fore- Stewardship: Responsible and fiscally
cast clinical and cost outcomes. This allows an thoughtful management of resources.
organization to make better decisions regarding
Transitional Care: Transitional care includes
current/future staff and equipment expenditures,
all the services required to facilitate the coordi-
provider and client education needs, allocation
nation and continuity of health care as the client
of finances, as well as to better risk stratify
moves between one health care service provider
population groups.
and another.
Provider: The individual, service organization,
Transitions of Care: Transitions of care
or vendor who provides health care services to
is the movement of patients from one health
the client.
care practitioner or setting to another as their
Risk Stratification: The process of categoriz- condition and care needs change. Also known as
ing individuals and populations according to their care transitions.
likelihood of experiencing adverse outcomes,
Value-Based Purchasing: A program provid-
e.g., high risk for hospitalization.
ed by the Centers for Medicare & Medicaid Services
Role: A general and abstract term that refers to as part of the Patient Protection and Affordable
a set of behaviors and expected consequences Care Act of 2010. This program rewards acute care
that are associated with ones position in a social hospitals with incentive payments based on the
structure. A role consists of several functions quality of care they provide to Medicare beneficia-
which constitute what is commonly known as ries; how closely best clinical practices are followed;
a job description. Each function in a role is and how well the patient experience of care is
described through a list of specific and related enhanced (USDHHS - CMS, 2015b).
36 CMSA Standards of Practice for Case Management
References to Patient Activation. Retrieved from http://
www.kingsfund.org.uk/sites/files/kf/field/
Agency for Healthcare Research and Quality
field_publication_file/supporting-people-man-
(AHRQ). (2007). Closing the Quality Gap: A Crit-
age-health-patient-activation-may14.pdf on May
ical Analysis of Quality Improvement Strategies.
Publication no. 04(07)-0051-7, volume 7 - Care 23, 2016. London, United Kingdom: The Kings
Fund.
Coordination, June 2007.
Kathol, R.G., Perez, R., & Cohen, J.S. (2010). The
Case Management Society of America (CMSA).
Integrated Case Management Manual: Assisting
(1995). Standards of Practice for Case Manage-
Complex Patients Regain Physical and Mental
ment. Little Rock, Arkansas: CMSA.
Health. New York, NY: Case Management Soci-
Case Management Society of America (CMSA). ety of America and Springer Publishing Company.
(revised, 2002). Standards of Practice for Case
Last, J.M. (1997). Public Health and Human Ecol-
Management. Little Rock, Arkansas: CMSA.
ogy, (Ed. 2). Stamford, CT: Appleton and Lange.
Case Management Society of America (CMSA).
National Association of Social Workers (NASW).
(2009). Mission and vision. Retrieved from http://
(2007). Indicators for the achievement of the
www.cmsa.org/home/CMSA/ourMissionvision/
NASW standards for cultural competence in
tabid/226/default.aspx on July 7, 2009.
social work practice. Washington, DC: NASW
Case Management Society of America (CMSA). Press.
(revised, 2010). Standards of Practice for Case
National Quality Forum (NQF). (2010). Pre-
Management. Little Rock, Arkansas: CMSA.
ferred Practices and Performance Measures for
Case Management Society of America (CMSA). Measuring and Reporting Care Coordination: A
(revised, 2016). Standards of Practice for Case Consensus Report. Washington, DC: NQF.
Management. Little Rock, Arkansas: CMSA.
Population Health Alliance. (2016). PHM
Center for Disease Control (CDC). (September 25, Glossary: D, Disease Management. Retrieved
2015). Understanding Literacy and Numeracy. from http://www.populationhealthalliance.org/
Retrieved from http://www.cdc.gov/healthlitera- research/phm-glossary/d.html, on May 23, 2016,
cy/Learn/UnderstandingLiteracy.html on May 23, Washington, DC: Population Health Alliance.
2016. Atlanta, GA: CDC.
Powell, S.K. & Tahan, H. (2008). Case Manage-
Emblem Health & National Alliance for Caregiv- ment Society of America (CMSA) Core Curriculum
ing. (March 2010). Care for the Family Caregiver: for Case Management, (Ed. 2). Philadelphia:
A Place to Start. Retrieved from http://www. Lippincott Williams & Wilkins.
caregiving.org/data/Emblem_CfC10_Final2.pdf
Standards & Interoperability Longitudinal
on May 23, 2016.
Coordination of Care Workgroup. (December
EURO European Centre for Health Policy (ECHP). 2012). Care Plan Terms and Proposed Defini-
(1999). Dictionary Definitions. Retrieved from tions. Retrieved from http://wiki.siframework.
http://apps.who.int/disasters/repo/13849_files/n/ org/LCC+Longitudinal+Care+Plan+%28L-
definitions_EURO_ECHP.pdf on May 23, 2016. CP%29+SWG#Care%20Plan%20Glossary%20
Brussels: ECHP. Archive on May 23, 2016.
Health Policy Brief. (2013). Patient Engagement. Stokes, J., Noren, J., & Shindell, S. (1982). Defini-
Health Affairs, February 14, 2013: 1-6. tion of Terms and Concepts Applicable to Clinical
Hibbard J. & Gilburt, G. (May, 2014). Supporting Preventive Medicine. Journal of Community
People to Manage Their Health: An Introduction Health, 8:33-41.
CMSA Standards of Practice for Case Management 37
Tahan, H. & Campagna, V. (2010). Case Man- http://www.who.int/about/mission/en/ on May
agement Roles and Functions across Various 23, 2016, Geneva, Switzerland: WHO.
Settings and Professional Disciplines. Profession- World Health Organization (WHO). (1984).
al Case Management, 15(5): 245-277. Health Promotion: A Discussion Document on the
Tahan, H. M. & Treiger, T.M. (2017). Case Man- Concepts and Principles. Copenhagen: WHO.
agement Society of America (CMSA) Core Curric-
ulum for Case Management, (Ed 3). Philadelphia,
PA: Wolters Kluwer.
United States Department of Health and Human
Services (USDHHS), Centers for Medicare &
Medicaid Services (CMS). (2015a). Chronic Care
Management Services, May 2015. Retrieved from
https://www.cms.gov/Outreach-and-Education/
Medicare-Learning-Network-MLN/MLNProducts/
Downloads/ChronicCareManagement.pdf on
May 23, 2016, ICN 909188, Baltimore, MD:
CMS.
United States Department of Health and Human
Services (USDHHS), Centers for Medicare &
Medicaid Services (CMS). (2015b). Hospital
Value-Based Purchasing. Medicare Learning
Network, September, 2015. Retrieved from
https://www.cms.gov/Outreach-and-Education/
Medicare-Learning-Network-MLN/MLNProducts/
downloads/Hospital_VBPurchasing_Fact_Sheet_
ICN907664.pdf on May 23, 2016, ICN 907664,
Baltimore, MD: CMS.
United States Department of Health and Human
Services (USDHHS), Health Resources and
Services Administration (HRSA). (2016). Health
Literacy. Retrieved from http://www.hrsa.gov/
publichealth/healthliteracy/ on May 23, 2016,
Rockville, MD: HRSA. Case Management Society of America
United States Department of Health and Human 6301 Ranch Dr., Little Rock, Arkansas 72223
Services (USDHHS), Office of Minority Health T 501.225.2229 | F 501.221.9068
(OMH). (2001). National Standards for Culturally E cmsa@cmsa.org | W www.cmsa.org
and Linguistically Appropriate Services in Health The Standards of Practice for Case Management
Care, Final report. Retrieved from http://www. 2016 Copyright 2016. Case Management Society
omhrc.gov/assets/pdf/checked/finalreport.pdf on of America, U.S.A. All rights reserved under both
June 29, 2009, Rockville, MD: OMH. international and Pan American law. No repro-
duction of any part of this material may be made
World Health Organization (WHO). (1946). without the prior written consent of the copyright
Constitution of WHO: Principles. Retrieved from holder.
38 CMSA Standards of Practice for Case Management
Vous aimerez peut-être aussi
- The Diary of Anne Frank PacketDocument24 pagesThe Diary of Anne Frank Packetcnakazaki1957Pas encore d'évaluation
- Collegiate Recovery Programs: Results From The First National SurveyDocument76 pagesCollegiate Recovery Programs: Results From The First National SurveyThe Stacie Mathewson FoundationPas encore d'évaluation
- Template Outpatient Psych Note Counseling and Coord StartDocument1 pageTemplate Outpatient Psych Note Counseling and Coord Starttrowell33Pas encore d'évaluation
- National Core Standards 2011 1Document52 pagesNational Core Standards 2011 1yos_peace86Pas encore d'évaluation
- Canna DispensariesDocument35 pagesCanna DispensariesWaf Etano100% (1)
- Book3 79 111000 0000100120 DAH MPL RPT 000005 - ADocument101 pagesBook3 79 111000 0000100120 DAH MPL RPT 000005 - ANassif Abi AbdallahPas encore d'évaluation
- Palliative Care VS Hospice CareDocument3 pagesPalliative Care VS Hospice CareLPas encore d'évaluation
- Culturally Competent Presentation Portfolio AssignmentDocument21 pagesCulturally Competent Presentation Portfolio Assignmentapi-628734736Pas encore d'évaluation
- Sample EssayDocument9 pagesSample EssayBrian SrotaPas encore d'évaluation
- Schizophrenia Spectrum and Other Psychotic DisordersDocument41 pagesSchizophrenia Spectrum and Other Psychotic DisordersNoelle Grace Ulep BaromanPas encore d'évaluation
- Guide To: Medi-Cal Mental Health ServicesDocument53 pagesGuide To: Medi-Cal Mental Health ServicesJRSPas encore d'évaluation
- RAD: Reactive Attachment Disorder ResourcesDocument8 pagesRAD: Reactive Attachment Disorder ResourcesveronicaPas encore d'évaluation
- Case Management InterviewsDocument29 pagesCase Management Interviewsapi-257433350Pas encore d'évaluation
- Addiction in the Lives of Registered Nurses and Their Wake-Up Jolt to RecoveryD'EverandAddiction in the Lives of Registered Nurses and Their Wake-Up Jolt to RecoveryPas encore d'évaluation
- MI Change PlanDocument3 pagesMI Change Planeclatant100% (1)
- Richet Vacine Policy LetterDocument3 pagesRichet Vacine Policy LetterThirumalaiappan MuthukumaraswamyPas encore d'évaluation
- 14 Essentials To Assessment and Care PlanMT2013!08!018-BRODATY - 0Document9 pages14 Essentials To Assessment and Care PlanMT2013!08!018-BRODATY - 0Danielcc Lee100% (1)
- Home Treatment and Palliative Care for SeniorsDocument41 pagesHome Treatment and Palliative Care for Seniorspeca65Pas encore d'évaluation
- General Principles of The InterviewDocument76 pagesGeneral Principles of The InterviewEdi DrimaPas encore d'évaluation
- Telehealth Projects: A Practical GuideDocument66 pagesTelehealth Projects: A Practical GuideAmadasun Bigyouth OsayiPas encore d'évaluation
- Comprehensive Counseling and Guidance Model For Alabama Public SchoolsDocument105 pagesComprehensive Counseling and Guidance Model For Alabama Public SchoolsMontgomery AdvertiserPas encore d'évaluation
- Advanced Case Management A Complete Guide - 2020 EditionD'EverandAdvanced Case Management A Complete Guide - 2020 EditionPas encore d'évaluation
- Intake Assessment FormDocument3 pagesIntake Assessment Formapi-608114435Pas encore d'évaluation
- Event Planner Resume SampleDocument2 pagesEvent Planner Resume Sampleresume7.com100% (10)
- Case Analysis: Bipolar 1 Diagnosis & Treatment PlanDocument2 pagesCase Analysis: Bipolar 1 Diagnosis & Treatment PlanJoshua Ringor100% (1)
- B H Outpatient Treatment Form CDocument3 pagesB H Outpatient Treatment Form Cjirehcounseling100% (1)
- Rehab FraudDocument24 pagesRehab FraudofficialcchrPas encore d'évaluation
- Brief Evaluation of Executive Dysfunction PDFDocument2 pagesBrief Evaluation of Executive Dysfunction PDFAlejandra SwanPas encore d'évaluation
- Module 4: Mood Disorders: Disorders and Individuals With Bipolar Disorders. The Key Difference BetweenDocument7 pagesModule 4: Mood Disorders: Disorders and Individuals With Bipolar Disorders. The Key Difference BetweenLiz Evermore0% (1)
- Challenging the Stigma of Mental Illness: Lessons for Therapists and AdvocatesD'EverandChallenging the Stigma of Mental Illness: Lessons for Therapists and AdvocatesÉvaluation : 4 sur 5 étoiles4/5 (1)
- Schizoaffective DisorderDocument9 pagesSchizoaffective DisorderIka KawaiiPas encore d'évaluation
- Check List For PT ETOH Alcohol UseDocument12 pagesCheck List For PT ETOH Alcohol Usesen APas encore d'évaluation
- FC Psych (SA) Regulations (11!3!2010)Document37 pagesFC Psych (SA) Regulations (11!3!2010)Megan CloetePas encore d'évaluation
- Mental health assessment formDocument6 pagesMental health assessment formalotfya100% (1)
- DSM-5 and Culture - The Need To Move Towards A Shared Model of Care Within A More Equal Patient-Physician PartnershipDocument3 pagesDSM-5 and Culture - The Need To Move Towards A Shared Model of Care Within A More Equal Patient-Physician PartnershipSergioMSaraivaPas encore d'évaluation
- Lesson 1-Documentation and ReportingDocument8 pagesLesson 1-Documentation and ReportingCHRISTIAN ROY MAXINO100% (1)
- Medical Claims Processing Company Marketing PlanDocument19 pagesMedical Claims Processing Company Marketing PlanPalo Alto Software100% (2)
- Addiction Treatment Center in HoustonDocument8 pagesAddiction Treatment Center in Houstonemma rebel100% (1)
- Levac Rehab-Detox PackageDocument160 pagesLevac Rehab-Detox PackageHugo RodriguesPas encore d'évaluation
- Gambling Addiction: Mahdiya Bhiwandiwala 11GDocument15 pagesGambling Addiction: Mahdiya Bhiwandiwala 11GMahdiya100% (1)
- Challenge The Status QuoDocument49 pagesChallenge The Status QuoChris StewartPas encore d'évaluation
- Australian mental health recovery measures reviewDocument79 pagesAustralian mental health recovery measures reviewHarry Dean100% (1)
- Example of A Psychosocial AssessmentDocument8 pagesExample of A Psychosocial Assessmentkaty_mll8950100% (2)
- Psychiatric Mental Health Comprehensive Case StudyDocument13 pagesPsychiatric Mental Health Comprehensive Case Studyapi-604569933Pas encore d'évaluation
- Assessment of Abnormal BehaviorDocument6 pagesAssessment of Abnormal Behaviorperfidia1Pas encore d'évaluation
- Integrative Support and Interprofessional Collaboration in Palliative Care ServicesDocument56 pagesIntegrative Support and Interprofessional Collaboration in Palliative Care Servicesrose fania100% (1)
- NewJersey06 12 Core FunctionsDocument11 pagesNewJersey06 12 Core FunctionsChinchusha T JanardhananPas encore d'évaluation
- PTSDDocument9 pagesPTSDAnisa Putri100% (1)
- Intake Assessment Treatment Psychotherapist in Long Island NY Resume Stuart KatzDocument2 pagesIntake Assessment Treatment Psychotherapist in Long Island NY Resume Stuart KatzStuartKatzPas encore d'évaluation
- Thesis Project PMDocument101 pagesThesis Project PMObi A Agusiobo100% (1)
- Marine Health, Safety, Quality and Environmental Management: Guide ForDocument56 pagesMarine Health, Safety, Quality and Environmental Management: Guide ForgabelendaPas encore d'évaluation
- Career Development: An Overview Fadel ShaitoDocument23 pagesCareer Development: An Overview Fadel ShaitoNely SofwaPas encore d'évaluation
- EnglishDocument100 pagesEnglishtsegaab yosephPas encore d'évaluation
- Environmental Management Systems (Jean S. Waters)Document19 pagesEnvironmental Management Systems (Jean S. Waters)Karlo ZeverichPas encore d'évaluation
- Overview of Healthcare ComplianceDocument132 pagesOverview of Healthcare ComplianceKaushik VelingkarPas encore d'évaluation
- Recruitment and Selection Policy and ProcedureDocument18 pagesRecruitment and Selection Policy and ProcedureBobo SwePas encore d'évaluation
- Understanding Management of Professional OrganizationsDocument93 pagesUnderstanding Management of Professional OrganizationssudhaPas encore d'évaluation
- Libro Communicating The Value of Supply Cain Managamente To Your CEODocument24 pagesLibro Communicating The Value of Supply Cain Managamente To Your CEOthekatPas encore d'évaluation
- Grupo 12Document154 pagesGrupo 12Obi A AgusioboPas encore d'évaluation
- CSG Report CompleteDocument34 pagesCSG Report CompleteIzaan Ahmed KhanPas encore d'évaluation
- Managed Fund Association's Sound Practices For Hedge Fund Managers 2007Document276 pagesManaged Fund Association's Sound Practices For Hedge Fund Managers 2007NaisscentPas encore d'évaluation
- NASP 2020 Professional Standards WebDocument81 pagesNASP 2020 Professional Standards WebGenie NguyenPas encore d'évaluation
- Drury and Shishini 2005Document65 pagesDrury and Shishini 2005David Mc CurryPas encore d'évaluation
- NEWSFull ReportAugust2014Document130 pagesNEWSFull ReportAugust2014fanny_febrianiPas encore d'évaluation
- Case Management PDFDocument30 pagesCase Management PDFfanny_febrianiPas encore d'évaluation
- KGH Code Blue Team RolesDocument5 pagesKGH Code Blue Team Rolesfanny_febrianiPas encore d'évaluation
- CMSA Standards 2016Document40 pagesCMSA Standards 2016fanny_febrianiPas encore d'évaluation
- Patients With Anaplastic Thyroid CancerDocument45 pagesPatients With Anaplastic Thyroid Cancerfanny_febrianiPas encore d'évaluation
- Guidelines For Adult Patients With Thyroid NodulesDocument191 pagesGuidelines For Adult Patients With Thyroid Nodulesfanny_febrianiPas encore d'évaluation
- Management of Medullary Thyroid CarcinomaDocument57 pagesManagement of Medullary Thyroid Carcinomafanny_febrianiPas encore d'évaluation
- Hyperviscosity SyndromeDocument2 pagesHyperviscosity Syndromefanny_febrianiPas encore d'évaluation
- Aggregation of YG3 ProteinsDocument12 pagesAggregation of YG3 Proteinsfanny_febrianiPas encore d'évaluation
- Para Protein Emi ADocument8 pagesPara Protein Emi Afanny_febrianiPas encore d'évaluation
- EINC ChecklistDocument3 pagesEINC ChecklistMARK JEFTE BRIONESPas encore d'évaluation
- Reasons Why Coca Cola Has A Large Market Share in Kenya and The WorldDocument9 pagesReasons Why Coca Cola Has A Large Market Share in Kenya and The WorldAludahPas encore d'évaluation
- Connection Between Academic and Professional IntegrityDocument3 pagesConnection Between Academic and Professional IntegrityJoshua NyabindaPas encore d'évaluation
- 740 (Q50, V40, Awa 4Document10 pages740 (Q50, V40, Awa 4rawat2583Pas encore d'évaluation
- OTGNNDocument13 pagesOTGNNAnh Vuong TuanPas encore d'évaluation
- Product Manual 82434 (Revision C) : Generator Loading ControlDocument26 pagesProduct Manual 82434 (Revision C) : Generator Loading ControlAUGUSTA WIBI ARDIKTAPas encore d'évaluation
- Gujarat Technological University: Emester ViDocument4 pagesGujarat Technological University: Emester ViPradeep SutharPas encore d'évaluation
- 20comm Um003 - en PDocument270 pages20comm Um003 - en PRogério BotelhoPas encore d'évaluation
- Gantt Chart Engr110 - Gantt Chart Template 3Document1 pageGantt Chart Engr110 - Gantt Chart Template 3api-375485735Pas encore d'évaluation
- Ir Pc-1: Pre-Check (PC) Design Criteria For Freestanding Signs and Scoreboards: 2019 CBCDocument15 pagesIr Pc-1: Pre-Check (PC) Design Criteria For Freestanding Signs and Scoreboards: 2019 CBCAbrar AhmadPas encore d'évaluation
- Comparing Financial Performance of Conventional and Islamic BanksDocument9 pagesComparing Financial Performance of Conventional and Islamic BanksIkbal HardiyantoPas encore d'évaluation
- The Seven Kings of Revelation 17Document9 pagesThe Seven Kings of Revelation 17rojelio100% (1)
- Measures of CentralityDocument13 pagesMeasures of CentralityPRAGASM PROGPas encore d'évaluation
- Chams 1Document78 pagesChams 1Das RavindraPas encore d'évaluation
- Quality Management - QuestionDocument4 pagesQuality Management - QuestionLawzy Elsadig SeddigPas encore d'évaluation
- Ownership and Governance of State Owned Enterprises A Compendium of National Practices 2021Document104 pagesOwnership and Governance of State Owned Enterprises A Compendium of National Practices 2021Ary Surya PurnamaPas encore d'évaluation
- Symasym BBDocument37 pagesSymasym BBChandraRizkyPas encore d'évaluation
- 02 - Order Quantities When Demand Is Approximately LevelDocument2 pages02 - Order Quantities When Demand Is Approximately Levelrahma.samyPas encore d'évaluation
- S 212 Pre Course WorkDocument5 pagesS 212 Pre Course Workafiwierot100% (2)
- Magnets Catalog 2001Document20 pagesMagnets Catalog 2001geckx100% (2)
- Cloud Security Training and Awareness Programs For OrganizationsDocument2 pagesCloud Security Training and Awareness Programs For OrganizationsdeePas encore d'évaluation
- Potato Peroxidase LabDocument2 pagesPotato Peroxidase LabKarla GutierrezPas encore d'évaluation
- Effect of Dust On The Performance of Wind Turbines PDFDocument12 pagesEffect of Dust On The Performance of Wind Turbines PDFJallal ArramachPas encore d'évaluation
- Rock Laboratory PricelistDocument1 pageRock Laboratory PricelistHerbakti Dimas PerdanaPas encore d'évaluation
- SomDocument191 pagesSomVivek GosaviPas encore d'évaluation
- Institutional Competency Assessment Instrument (ICAI)Document12 pagesInstitutional Competency Assessment Instrument (ICAI)Bea EtacPas encore d'évaluation
- ProSteel Connect EditionDocument2 pagesProSteel Connect EditionInfrasys StructuralPas encore d'évaluation