Académique Documents
Professionnel Documents
Culture Documents
Guia para El TDAH
Transféré par
EstebanGiraTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Guia para El TDAH
Transféré par
EstebanGiraDroits d'auteur :
Formats disponibles
PRIMER
Attention-deficit/hyperactivity disorder
Stephen V.Faraone1,2, Philip Asherson3, Tobias Banaschewski4, Joseph Biederman5,
JanK.Buitelaar6, Josep Antoni Ramos-Quiroga79, Luis Augusto Rohde10,11,
EdmundJ.S.Sonuga-Barke12,13, Rosemary Tannock14,15 and Barbara Franke16
Abstract | Attention-deficit/hyperactivity disorder (ADHD) is a persistent neurodevelopmental disorder
that affects 5% of children and adolescents and 2.5% of adults worldwide. Throughout an individuals
lifetime, ADHD can increase the risk of other psychiatric disorders, educational and occupational failure,
accidents, criminality, social disability and addictions. No single risk factor is necessary or sufficient to cause
ADHD. In most cases ADHD arises from several genetic and environmental risk factors that each have a
small individual effect and act together to increase susceptibility. The multifactorial causation of ADHD is
consistent with the heterogeneity of the disorder, which is shown by its extensive psychiatric co-morbidity,
its multiple domains of neurocognitive impairment and the wide range of structural and functional brain
anomalies associated with it. The diagnosis of ADHD is reliable and valid when evaluated with standard
criteria for psychiatric disorders. Rating scales and clinical interviews facilitate diagnosis and aid screening.
The expression of symptoms varies as a function of patient developmental stage and social and academic
contexts. Although there are no curative treatments for ADHD, evidenced-based treatments can markedly
reduce its symptoms and associated impairments. For example, medications are efficacious and normally
well tolerated, and various non-pharmacological approaches are also valuable. Ongoing clinical and
neurobiological research holds the promise of advancing diagnostic and therapeutic approaches to ADHD.
For an illustrated summary of this Primer, visit: http://go.nature.com/J6jiwl
Attention-deficit/hyperactivity disorder (ADHD; also associated with ADHD. These studies have created relia-
known as hyperkinetic disorder) is a common dis- ble and valid measurement tools for screening, diagnosis
order characterized by inattention or hyperactivity and monitoring of treatment. Likewise, rigorous clinical
impulsivity, or both. The evidence base for the diagnosis trials have documented the safety and efficacy of ADHD
and treatment of ADHD has been growing exponentially treatment, and it is now clear which ADHD treatments
since the syndrome was first described by a German work, which do not and which require further study. In
physician in 1775 (REF.1) (FIG.1). In 1937, the efficacy this Primer, we discuss the evidence base that has created
of amphetamine use to reduce symptom severity was a firm foundation for future work to further clarify the
serendipitously discovered. In the 1940s, the brainwas aetiology and pathophysiology of ADHD and to advance
implicated as the source of ADHD-like symptoms, which diagnostic and therapeutic approaches to this disorder.
were described as minimal brain damage in the wake of
Correspondence to S.V.F.
e-mail: sfaraone@
an encephalitis epidemic. In 1980, the third edition of Epidemiology
childpsychresearch.org the Diagnostic and Statistical Manual of Mental Disorders Age-dependent prevalence of ADHD
Departments of Psychiatry (DSM) created the first reliable operational diagnostic ADHD is a common disorder among young people
and of Neuroscience and criteria for the disorder. These criteria initiated many worldwide. In 2007, a meta-analysis of more than 100
Physiology, State University
programmes of research that ultimately led the scien- studies estimated the worldwide prevalence of ADHD in
of New York (SUNY) Upstate
Medical University, Syracuse,
tific community to view ADHD as a seriously impair- children and adolescents to be 5.3% (95% CI: 5.015.56)2.
New York 13210, USA; ing, often persistent neurobiological disorder of high Three methodological factors explained this variabil-
K.G.Jebsen Centre for prevalence that is caused by a complex interplay between ity among studies: the choice of diagnostic criteria, the
Neuropsychiatric Disorders, genetic and environmental risk factors. These risk fac- source of information used and the inclusion of a require-
Department of Biomedicine,
University of Bergen,
tors affect the structural and functional capacity of brain ment for functional impairment as well as symptoms for
5020Bergen, Norway. networks and lead to ADHD symptoms, neurocognitive diagnosis. After adjusting for these factors, a subsequent
deficits and a wide range of functionalimpairments. meta-analysis concluded that the prevalence of ADHD
Article number: 15020
doi:10.1038/nrdp.2015.20
We now have many large and well-designed epi does not significantly differ between countries in Europe,
Published online demiological, clinical and longitudinal studies that have Asia, Africa and the Americas, as well as in Australia3.
6 August 2015 clarified the features, co-morbidities and impairments Although other meta-analyses have found either lower or
NATURE REVIEWS | DISEASE PRIMERS VOLUME 1 | 2015 | 1
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
Author addresses
symptoms; and third, enabling ADHD to be diagnosed
in the presence of an autism spectrum disorder. The
1
Departments of Psychiatry and of Neuroscience and Physiology, State University third change is consistent with the reconceptualization
ofNewYork (SUNY) Upstate Medical University, Syracuse, New York 13210, USA. of ADHD in DSM5 as a neurodevelopmental disorder
2
K.G.Jebsen Centre for Psychiatric Disorders, Department of Biomedicine, rather than a disruptive behavioural disorder. Overall,
UniversityofBergen, 5020 Bergen, Norway.
these new criteria have yielded an increase in ADHD
3
Social Genetic and Developmental Psychiatry, Institute of Psychiatry Psychology
andNeuroscience, Kings College London, London, UK.
prevalence, which is insubstantial for children but is likely
4
Department of Child and Adolescent Psychiatry and Psychotherapy, Central Institute of to have had a more considerable effect on diagnosis rates
Mental Health, Medical Faculty Mannheim, Heidelberg University, Mannheim, Germany. in adults13,14.
5
Department of Psychiatry, Harvard Medical School, Massachusetts General Hospital,
Pediatric Psychopharmacology Unit, Massachusetts General Hospital, Boston, Sociodemographic factors
Massachusetts, USA. Alongside age, other factors such as sex, ethnicity and
6
Radboud University Medical Center, Donders Institute for Brain, Cognition and socioeconomic status are also important when consider
Behaviour, Department of Cognitive Neuroscience and Karakter Child and Adolescent ing the prevalence of ADHD. In children andadolescents,
Psychiatry University Centre, Nijmegen, The Netherlands. ADHD predominantly affects males and exhibits a male-
7
ADHD Program, Department of Psychiatry, Hospital Universitari Vall dHebron,
to-female sex ratio of 4:1 in clinical studies and 2.4:1 in
Barcelona, Spain.
8
Biomedical Network Research Centre on Mental Health (CIBERSAM), Barcelona, Spain.
population studies2. In adulthood, this sex discrepancy
9
Department of Psychiatry and Legal Medicine, Universitat Autnoma de Barcelona, almost disappears14, possibly owing to referral biases
Barcelona, Spain. among treatment-seeking patients or to sexspecific
10
ADHD Outpatient Program, Hospital de Clinicas de Porto Alegre, Department of effects of ADHD over the course of thedisorder.
Psychiatry, Federal University of Rio Grande do Sul, Porto Alegre, Brazil. Larsson and colleagues 15 found that low family
11
National Institute of Developmental Psychiatry for Children and Adolescents, income predicted an increased likelihood of ADHD in
SaoPaulo, Brazil. a Swedish population-based cohort study of 811,803
12
Department of Psychology, University of Southampton, Southampton, UK. individuals. However, this finding does not necessar-
13
Department of Experimental Clinical and Health Psychology, Ghent University, Ghent, ily support the conclusion that socioeconomic status
Belgium.
increases the risk of ADHD because the disorder
14
Neuroscience and Mental Health Research Program, Research Institute of The Hospital
for Sick Children, Toronto, Canada.
runs in families and leads to educational and occupa-
15
Department of Applied Psychology and Human Development, Ontario Institute for tional underattainment. Underemployment could in
Studies in Education, University of Toronto, Toronto, Ontario, Canada. turn lead to the over-representation of socioeconomic
16
Radboud University Medical Center, Donders Institute for Brain, Cognition and disadvantage among families affected by ADHD16.
Behaviour, Departments of Human Genetics and Psychiatry, Nijmegen, The Netherlands. Finally, although the true prevalence of ADHD does
not vary with ethnicity, some studies have inconsistently
associated ethnicity with ADHD owing to referral pat-
higher prevalence rates, these presented important limita- terns and barriers to care that disproportionately affect
tions, such as the exclusive use of DSM criteria to diagnose particular ethnic groups1719.
ADHD and the use of simulated prevalence rates4,5. In
addition, there is no evidence, worldwide, of an increase Mechanisms/pathophysiology
in the real prevalence of ADHD over the past three Genes and environment
decades3. Despite the fact that both overdiagnosis and Genetic epidemiology. ADHD runs in families, with
underdiagnosis are common concerns in medicine, the parents and siblings of patients with ADHD show-
common public perception that ADHD is overdiagnosed ing between a fivefold and tenfold increased risk of
in the United States might not be warranted6. developing the disorder compared with the general
ADHD also affects adults. Although the majority population20,21. Twin studies show that ADHD has a
of children with ADHD will not continue to meet the heritability of 7080% in both children and adults2225,
full set of criteria for ADHD as adults, the persistence of with little or no evidence that the effects of environ
either functional impairment 7 or subthreshold (three or mental risk factors shared by siblings substantially influ-
fewer) impairing symptoms into adulthood is high8. For ence aetiology 26. Environmental risk factors play their
instance, on the basis of a meta-analysis of six studies, greatest part in the non-shared familial environment
Simon and colleagues9 found the pooled prevalence of and/or act through interactions with genes and DNA
ADHD to be 2.5% (95% CI: 2.13.1) in adults. In addi- variants that regulate gene expression such as those
tion, studies in older adults have found prevalence rates in promoters, untranslated regions of genes or loci that
in the same range10,11, and prospective longitudinal stud- encodemicroRNAs.
ies support the notion that approximately two-thirds of Although ADHD is a categorical diagnosis, results
youths with ADHD retain impairing symptoms of the from twin studies suggest that it is the extreme and
disorder in adulthood7 (FIG.2). impairing tail of one or more heritable quantitative traits27.
Recent alterations to diagnostic criteria have had an The disorder is influenced by both stable genetic factors
impact on ADHD prevalence measures in both young and those that emerge at different developmental stages
and adult populations. In 2013, DSM5 (REF.12) included from childhood through to adulthood28. Thus, genes con-
three important changes: first, increasing the age of onset tribute to the onset, persistence and remission of ADHD,
from 7years to 12years; second, decreasing the symptom presumably through stable neurobiological deficits as
threshold for patients 17years of age from six to five well as maturational or compensatory processes that
2 | 2015 | VOLUME 1 www.nature.com/nrdp
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
Weikard describes ADHD syndrome in a German textbook DSM-II describes hyperkinetic reaction Omega-3 is a weak but eective
treatment
Douglas neurocognitive model of ADHD
Homan cartoons of Still describes DSM-5 extends age of onset
Fidgeting Philip and defect of moral to 12 years and adjusts criteria
control in ADHD-like symptoms Twin studies for adults
Johnny Head-in-the-Air
The Lancet described as minimal document high
brain damage heritability CBT for adult ADHD
Bourneville, Boulanger, Paul-Boncour US FDA approves DSM-III Rare genomic insertions and
and Philippe describe ADHD symptoms methylphenidate operationalizes deletions discovered
as mental instability in French medical for depression diagnostic
and educational literature and narcolepsy criteria Molecular polygenic
background conrmed
1775 1798 1845 1887 1901 1910 1930s 1940s 1950s 1960s 1970s 1980s 1985 1990s 1995 2000s 2010s
Sagvolden describes an ADHD rat model
Bradley shows that benzedrine
reduces hyperactivity Similar correlates of ADHD found in boys and girls CDC describes
Crichton describes ADHD as a
ADHD syndrome in KramerPollnow syndrome Neuroimaging documents structural and serious public
a Scottish textbook discovered Parent training functional brain anomalies health problem
treatments
DSM-IV renes criteria Long-acting
Methylphenidate stimulants
Prediagnostic era ADHD in adults recognized as a valid disorder developed
indicated for
Minimal brain dysfunction era behavioural
Attention-decit disorder era disorders Co-morbidity with anxiety, mood or autism spectrum Non-stimulants
ADHD era in children disorders and executive dysfunction conrmed approved
Nature Reviews | Disease Primers
Figure 1 | The history of attention-deficit/hyperactivity disorder. Attention-deficit/hyperactivity disorder (ADHD)
syndromes have been described in the medical literature since the eighteenth century, but the growth of systematic
research required the development of operational diagnostic criteria in the late twentieth century. This schematic
outlines selected important developments in the history of ADHD research. CBT, cognitivebehavioural therapy;
CDC,Centers for Disease Control and Prevention; DSM, Diagnostic and Statistical Manual of Mental Disorders.
influence development. The inattention and hyperactiv- and twin studies that found significant coaggregation
ity or impulsivity that characterize ADHD are separate of ADHD with depression37, conduct problems39 and
domains of psychopathology, with a genetic correlation schizophrenia40. Furthermore, combined GWAS of
of around 0.6, reflecting substantial geneticoverlap but ADHD, autism spectrum disorders, depression, bipolar
also genetic influences that are domain specific29. Shared disorder and schizophrenia identified four genome-wide
genetic factors also account for the cooccurrence of significant loci shared by these disorders37.
ADHD with emotional dysregulation an independ- In addition to the common-variant studies, rare
ent source of impairment in ADHD30,31. Family and twin (prevalence of <1%) genomic insertions and deletions
studies have also demonstrated that genetic influences known as copy number variants (CNVs) have a role
are shared between ADHD and a wide range of other in ADHD41,42. One study found that 15.6% of patients
neurodevelopmental and psychopathological traits and with ADHD carry large CNVs of >500,000 base pairs
disorders, including conduct disorder and problems32, in length compared with 7.5% of individuals without
cognitive performance33, autism spectrum disorders34 the disorder. The rate of large CNV carriage was even
and mood disorders35,36. higher (42.4%) in those with both ADHD and an IQ
below 705 (which, along with poor adaptive function-
Molecular genetics. On the basis of data from genome- ing, defines intellectual disability)42. These findings have
wide association studies (GWAS), approximately 40% of been replicated43, and together these studies implicate
the heritability of ADHD can be attributed to numer- genes at 16p13.11 along with the 15q1115q13 region in
ous common genetic variants37. In polygenic risk score ADHD. The 15q1115q13 region contains the gene that
analysis, the genetic signals attributed to common vari- encodes the nicotinic 7 acetylcholine receptor subunit,
ants derived from a discovery sample are used to predict which participates in neuronal and nicotinic signalling
phenotypic effects in a second sample. The polygenic risk pathways. Finally, ADHD-associated CNVs also span
for clinically diagnosed ADHD predicts ADHD symp- several glutamate receptor genes, which are essential
toms in the population more broadly 38, confirming the for neuronal glutamatergic transmission44, and the gene
conclusion from twin studies that the genes determining encoding neuropeptide Y, which is involved in signal-
the diagnosis of ADHD also regulate the expression of ling in the brain and autonomic nervous system45. CNVs
subclinical levels of ADHD symptoms. Inaddition, these associated with ADHD also occur in schizophrenia
analyses have confirmed earlier evidence from family andautism42.
NATURE REVIEWS | DISEASE PRIMERS VOLUME 1 | 2015 | 3
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
100 evoke hostile styles of parenting, and genes linked to
ADHD might explain the association of parental vari-
ables, such as maternal smoking during pregnancy,
75 with offspring who have ADHD51,52. One notable study
71% investigated maternal hostility while controlling for
Persistence (%)
65% genetic effects by studying children adopted at birth
50 and children conceived through in vitro fertiliza-
tionand their genetically unrelated rearing mothers53.
The study found a role for genetically influenced early
25 Functional impairment child behaviour on the hostility of biologically unrelated
Impairing symptoms 15% mothers, which in turn was a predictor of subsequent
Full diagnostic criteria ADHD symptoms developed by the children. Another
0 study followed Romanian adoptees who had experi-
0 5 10 15 20 25 30 enced severe early maternal deprivation in orphanages
Mean age at follow-up (years) before adoption. It showed a dose-dependent relation-
Figure 2 | The age-dependent decline and persistence of attention-deficit/ ship between length of deprivation and risk of develop-
Nature Reviews | Disease Primers
hyperactivity disorder throughout the lifetime. Followup studies have assessed ing ADHD-like symptoms54. Other environmental risk
children with attention-deficit/hyperactivity disorder (ADHD) at multiple time points factors that have been associated with ADHD include
after their initial diagnosis. Although they document an age-dependent decline in ADHD prenatal and perinatal factors, such as maternal smok-
symptoms, ADHD is also a highly persistent disorder when defined by the persistence of ing and alcohol use, low birth weight, premature birth
functional impairment7 or the persistence of subthreshold (three or fewer) impairing
and exposure to environmental toxins, such as organo-
symptoms8. By contrast, many patients remit full diagnostic criteria7.
phosphate pesticides, polychlorinated biphenyls, zinc
and lead55,56. Animal models have also contributed
Although GWAS that investigated common genetic much to the study of environmental risk factors5759.
variants (FIG.3) have not identified specific ADHD genes Similar to genetic risk factors, the effects of any one
at genome-wide levels of significance46, intriguing results environmental risk factor are small and could reflect
have emerged from meta-analyses of studies of candi- either small effects in many cases or larger effects in a
date genes involved in the monoamine neurotransmit- few cases. Furthermore, rather than being specific to
ter systems47. These systems had been implicated in the ADHD, these environmental risk factors are associated
pathophysiology of ADHD by the mechanisms of action with several psychiatric disorders29.
of drugs used in clinical management. Methylphenidate In addition to the main effects of the environment,
and amphetamine target the sodium-dependent dopa- the high heritability of ADHD suggests that gene
mine transporter (encoded by SLC6A3), atomoxetine environment (GE) interactions might be the main
targets the sodium-dependent noradrenaline trans- mechanism by which environmental risk factors increase
porter, and both extended-release guanfacine and the risk of ADHD. For example, a variant of 5HTTLPR
extended-release clonidine target the 2A-adrenergic a polymorphic region located in the promoter of SLC6A4
receptor. Within the monoamine systems, the strongest is involved in the hyperactivity and impulsivity dimen-
evidence of ADHD association is for variants in the genes sions of ADHD in interaction with stress60. Although
encoding the D4 and D1B dopamine receptors47. The some early studies identified other GE effects, none
association of the SLC6A3 gene variant is equivocal47, has been reliably reproduced. Future success in this area
possibly owing to age-related effects48. Other genes that requires the use of large data sets, such as those emerg-
show possible associations with ADHD include SLC6A4 ing from the use of national databases in Denmark and
(which encodes the sodium-dependent serotonin trans- Sweden, which can combine large-scale genetic studies
porter), HTR1B (which encodes 5hydroxytryptamine with recorded data on exposure to environmentalrisks.
receptor 1B (also known as serotonin receptor 1B)) and Another approach to identify environmental risk fac-
SNAP25 (which encodes synaptosomal-associated pro- tors in ADHD is to focus on the detection of epigenetic
tein 25)47. Owing to methodological issues, a cautious changes, such as DNA methylation, which are revers-
approach must be taken to the interpretation of candi ible changes in genomic function that are independent
date gene studies. Nevertheless, the role of the dopa- of DNA sequence. Epigenetics provides a mechanism
mine, noradrenaline, serotonin and neurite outgrowth by which environmental risk factors alter gene func-
systems is supported by genome-wide association study- tion. However, as epigenetic changes are highly tissue
based gene-set analyses reporting that, as a group, genes specific, they are difficult to study in ADHD because of
regulating these systems were associated with ADHD limited access to brain tissue. Studies must, therefore,
and hyperactivity or impulsivity 46,49,50. rely on peripheral tissues such as blood, the epigenetic
profile of which partly overlaps with that of brain tis-
Environmental risk factors. Identifying environmental sue. Environmental toxins and stress can all induce epi
causes of ADHD is difficult because environmen- genetic changes, thus the identification of genes that
talassociations might arise from other sources, such show epigenetic changes linked to ADHD, or in response
as from child or parental behaviours that shape the to environmental risk factors, might in the future pro-
environment, or they might reflect unmeasured third vide new insights into the mechanisms involved in the
variables. For example, children with ADHD might pathogenesis ofADHD61.
4 | 2015 | VOLUME 1 www.nature.com/nrdp
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
Brain mechanisms anticipation of reward than in controls75. ADHD is also
Cognition. ADHD is characterized by decits in multi- associated with hyperactivation in somatomotor and vis-
ple, relatively independent, cognitive domains. Executive ual systems74, which possibly compensates for impaired
functioning deficits are seen in visuospatial and verbal functioning of the prefrontal and anterior cingulate cor-
working memory, inhibitory control, vigilance and tices76. A single dose of methylphenidate (a stimulant)
planning 62,63. Studies of reward dysregulation show that markedly enhances activation in the inferior frontal cor-
patients with ADHD make suboptimal decisions64, pre- tex and insula bilaterally which are key areas of cogni-
fer immediate rather than delayed rewards65 and over- tive control during inhibition and time discrimination
estimate the magnitude of proximal relative to distal but does not affect working memory networks77. By con-
rewards66. Other domains impaired in ADHD include trast, long-term treatment with stimulants is associated
temporal information processing and timing 67; speech with normal activation in the right caudate nucleus dur-
and language68; memory span, processing speed and ing the performance of attention tasks78. Resting-state
response time variability 69; arousal and activation70; MRI studies have shown that ADHD is associated with
and motor control71. Although most patients with less-pronounced or absent anti-correlations between the
ADHD show deficits in one or two cognitive domains, default-mode network (DMN) and the cognitive control
some have no deficits and very few show decits in all network, lower connectivity within the DMN itself and
domains72. In addition, across the lifespan of patients lower connectivity within the cognitive and motivational
with ADHD, deficits in cognitive control, reward sensi loops of the frontostriatal circuits79.
tivity and timing have been shown to be independent Along with functional changes, a range of struc-
of one another 73, and it is currently unclear whether tural brain alterations are also associated with ADHD.
cognitive deficits cause ADHD symptoms and drivethe For example, ADHD is associated with a 35% smaller
development of the clinical phenotype 72 or reflect total brain size than unaffected controls80,81 that can be
thepleiotropic outcomes of risk factors. attributed to a reduction of grey matter 82. Consistent
with genetic data that support a model of ADHD as the
Structural and functional brain imaging. Several brain extreme of a population trait, total brain volume cor-
regions and neural pathways have been implicated relates negatively with ADHD symptoms in the general
inADHD (FIG.4). Functional MRI studies in patients with population83. In patients with ADHD, meta-analyses
ADHD that used inhibitory control, working memory have documented smaller volumes across several brain
and attentional tasks have shown underactivation of fron- regions, most consistently in the right globus pallidus,
tostriatal, frontoparietal and ventral attention networks74. right putamen, caudate nucleus and cerebellum84,85.
The frontoparietal network mediates goal-directed Inaddition, a meta-analysis of diffusion tensor imaging
executive processes, whereas the ventral attention net- studies showed widespread alterations in white matter
work facilitates reorientation of attention towards salient integrity, especially in the right anterior corona radiata,
and behaviourally relevant external stimuli. In reward- right forceps minor, bilateral internal capsule and left
processing paradigms, most studies report lower activa- cerebellum86. Both structural and functional imaging
tion of the ventral striatum of patients with ADHD in findings are very variable across studies, suggesting that
the neural underpinnings of ADHD are heterogeneous,
which is consistent with studies of cognition.
22q11.2 deletion syndrome 16p13.11 Monoamine Just as the prevalence of ADHD is associated with
15q1115q11 13 region containing systems
Jacobsen syndrome genes age (FIG.2), so too are many changes in the brains of
(deletions of the end of 11q) nicotinic 7 acetylcholine
receptor subunit gene Neurite patients with ADHD7. Some brain volumetric alterations
Turner syndrome (X0) outgrowth
Klinefelter syndrome (XXY) Rare point mutations expected
genes observed in childhood normalize with age82,85, whereas
from sequencing studies
other measures remain fixed. For example, a longitudi-
nal MRI study found lower basal ganglion volumes and
High
Rare reduced dorsal surface area in adolescents with ADHD
chromosomal compared with controls, and this difference did not
anomalies
change as patients aged87. Furthermore, for ventral striatal
surfaces, control individuals showed surface area expan-
Rare and low
Eect size
sion with age, whereas patients with ADHD experienced
frequency copy
number variants a progressive contraction of the surface area. The as-yet-
unknown process underlying this contraction might
explain abnormal processing of reward in ADHD87.
Common variants
explain ~40% ADHD is also associated with delayed maturation of the
of heritability cerebral cortex. In one study, the age of attaining peak
cortical thickness was 10.5years for patients with ADHD
Low
Very rare Rare Low Common
and 7.5years for unaffected individuals; this delay was
Allele frequency most prominent in the prefrontal regions that are impor-
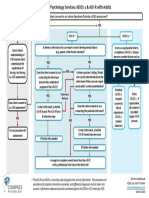
Figure 3 | Genetics of attention-deficit/hyperactivity disorder. Common variants tant for executive functioning, attention and motor plan-
Nature Reviews | Diseasedisorder
explain approximately 40% of the heritability of attention-deficit/hyperactivity Primers ning 88. The development of cortical surface area was
but, compared with rarer causes, individual common variants have much smaller effects also shown to be delayed in patients with ADHD, but
on the expression of the disorder. ADHD was not associated with altered developmental
NATURE REVIEWS | DISEASE PRIMERS VOLUME 1 | 2015 | 5
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
a Dorsolateral Parietal b Ventral anterior Dorsal anterior c d
Nigrostriatal
prefrontal cortex cortex cingulate cortex cingulate cortex Mesocortical Locus Cortex Thalamus
Caudate coeruleus
nucleus
Dorsal
Mesolimbic anterior
Nucleus
Ventromedial accumbens Substantia nigra cingulate Basal
prefrontal tegmentum cortex ganglia
Putamen
cortex Noradrenergic Executive control Pons
Amygdala Cerebellum Dopaminergic Corticocerebellar
e f g
Orbitofrontal Frontal Medial view Lateral view Lateral
cortex cortex parietal
cortex
Medial Medial
Ventromedial prefrontal prefrontal
prefrontal Ventral cortex Posterior cortex
cortex striatum cingulate Medial
cortex temporal lobe
Figure 4 | Brain mechanisms in attention-deficit/hyperactivity disorder. a | The cortical regions
Nature (lateral
Reviews view) ofPrimers
| Disease the
brain have a role in attention-deficit/hyperactivity disorder (ADHD). The dorsolateral prefrontal cortex is linked to working
memory, the ventromedial prefrontal cortex to complex decision making and strategic planning, and the parietal cortex
toorientation of attention. b | ADHD involves the subcortical structures (medial view) of the brain. The ventral anterior
cingulate cortex and the dorsal anterior cingulate cortex subserve affective and cognitive components of executive
control. Together with the basal ganglia (comprising the nucleus accumbens, caudate nucleus and putamen), they form
the frontostriatal circuit. Neuroimaging studies show structural and functional abnormalities in all of these structures in
patients with ADHD, extending into the amygdala and cerebellum. c | Neurotransmitter circuits in the brain are involved in
ADHD. The dopamine system plays an important part in planning and initiation of motor responses, activation, switching,
reaction to novelty and processing of reward. The noradrenergic system influences arousal modulation, signal-to-noise
ratios in cortical areas, state-dependent cognitive processes and cognitive preparation of urgent stimuli. d| Executive
control networks are affected in patients with ADHD. The executive control and corticocerebellar networks coordinate
executive functioning, that is, planning, goal-directed behaviour, inhibition, working memory and the flexible adaptation
to context. These networks are underactivated and have lower internal functional connectivity in individuals with ADHD
compared with individuals without the disorder. e | ADHD involves the reward network. The ventromedial prefrontal
cortex, orbitofrontal cortex and ventral striatum are at the centre of the brain network that responds to anticipation and
receipt of reward. Other structures involved are the thalamus, the amygdala and the cell bodies of dopaminergic neurons
in the substantia nigra, which, as indicated by the arrows, interact in a complex manner. Behavioural and neural responses
to reward are abnormal in ADHD. f | The alerting network is impaired in ADHD. The frontal and parietal cortical areas and
the thalamus intensively interact in the alerting network (indicated by the arrows), which supports attentional functioning
and is weaker in individuals with ADHD than in controls. g | ADHD involves the default-mode network (DMN). The DMN
consists of the medial prefrontal cortex and the posterior cingulate cortex (medial view) as well as the lateral parietal
cortex and the medial temporal lobe (lateral view). DMN fluctuations are 180degrees out of phase with fluctuations in
networks that become activated during externally oriented tasks, presumably reflecting competition between opposing
processes for processing resources. Negative correlations between the DMN and the frontoparietal control network are
weaker in patients with ADHD than in people who do not have the disorder.
trajectories of cortical gyrification89. Remission of ADHD widespread deviations in cortical thickness persist in
has been associated with normalization of abnormalities many adults with ADHD. Findings include both cortical
as measured by activation during functional imaging thinning (in the superior frontal cortex, precentral cor-
tasks90, cortical thinning 91 and structural and functional tex, inferior and superior parietal cortex, temporal pole
brain connectivity 9295. and medial temporal cortex)89,96 and cortical thickening
Although these data could be taken to suggest that the (in the pre-supplementary motor area, somatosensory
age-dependent decline in the prevalence of ADHDmight cortex and occipital cortex)97. More work is needed to
be due to the late development of ADHD-associated brain determine how developmental changes in patterns of
structures and functions, most patients with ADHD do cortical thickness predict developmental changes in
not show complete developmental catchup. Indeed, ADHD symptom expression.
6 | 2015 | VOLUME 1 www.nature.com/nrdp
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
Summary Children and adolescents
Neurocognitive, neuroimaging and genetic theories The diagnosis of ADHD relies on clinical symptoms
of ADHD have shifted from single-cause or single- reported by patients or informants (including rela-
pathway models to models that delineate causes that tives and teachers), which is standard for all psychiatric
lead to ADHD through several molecular, neural and disorders12. National clinical guidelines and practice
neurocognitive pathways33,98102. These approaches have parameters for ADHD, developed over the past dec-
received clear support from aetiological studies indi- ade, show good consensus and the potential to enhance
cating that most cases of ADHD arise from a pool of evidence-based clinical practice105. Diagnosis is based
genetic and environmental risk factors. Most of these on information from a detailed clinical interview, which
risk factors have only a small effect on causal pathways. remains the gold standard. Diagnosticians ask about
Cumulative vulnerability increases ADHD trait scores, each ADHD symptom, the age of onset and resultant
and our current model suggests thatADHDemerges functional impairments. Aclinical interview aims to
when these exceed a certain threshold. In most cases, no establish whether symptoms are more extreme, persis-
single factor is necessary or sufficient to cause ADHD. tent and impairing than expected for the developmen-
However, in some patients, rare genetic variants41,42 or tal level of the patient. Validated rating scales (TABLE1)
environmental risk factors for example, psychosocial help with such decisions, as they enable informants to
deprivation54 might have a majorinfluence. quantitatively rate the behaviour of the patient at home,
The multifactorial causation of ADHD leads to a at school and in the community.
heterogeneous profile of psychopathology, neuro Several factors present challenges to clinicians aiming
cognitive deficits and abnormalities in the struc- to determine whether a diagnosis of ADHD is appro-
ture and functionof the brain. Many cases probably priate. For instance, cultural and ethnic differences can
involve dysregulation ofthe structure and function hinder diagnosis owing to variability in attitudes towards
of the frontals ubcorticalc erebellar pathways ADHD, willingness to report symptoms or the accept-
that control attention, response to reward, salience ance of the diagnosis. For example, a literature review
thresholds, inhibitory control and motor behaviour. suggested that African-American youths had more
A meta-a nalysis of peripheral biomarkers in the ADHD symptoms than Caucasian youths but were
blood and urine of drug-naive or drug-free patients diagnosed with ADHD only two-thirds as often, possi-
with ADHD and unaffected individuals found several bly owing to parent beliefs about ADHD and the lack of
measures specifically, noradrenaline, 3methoxy4 treatment access and use106. In addition, patient age can
hydroxyphenylethylene glycol (MHPG), monoamine be an issue. Developmental changes can internalize or
oxidase (MAO) and cortisol to be significantly modify some symptoms. For example, the hyperactivity
associated with ADHD56. Several of these metabolites of childhood might be experienced as inner restless-
were also related to response to ADHD medication ness in adolescence, and distractibility could manifest
and symptom severity of ADHD. These results sup- as distracting thoughts. Accordingly, self-reports from
port the idea that catecholaminergic neurotransmitter adolescents are useful, but patients can sometimes
systems (discussed in further detail in the following lack insight into their own difficulties. Furthermore,
section) and the hypothalamicpituitaryadrenal although younger children can provide useful informa-
axis are dysregulated in ADHD. Finally, genetic and tion, especially about internalizing symptoms107, parents
clinical studies also implicate other systems, including remain the main source of information for this group of
the serotonergic, nicotinic, glutamatergic and neurite patients. Parents can report on symptoms during school
outgrowthsystems. recesses and vacations when teacher reports are not
available. Although parent reports show good concur-
Diagnosis, screening and prevention rent and predictive validity 108,109, information from other
The diagnostic process for ADHD assesses the inatten informants such as teachers, when available, is valuable
tive and hyperactiveimpulsive symptom criteria for for documenting ADHD in other settings, for predicting
ADHD, evidence that symptoms cause functional prognosis and for increasing the confidence of diagno-
impairments and age of onset before 12years. Although ses110112. Finally, diagnosticians can also inquire about
ADHD is associated with other features such as execu- other medical conditions associated with symptoms
tive dysfunction62 and emotional dysregulation31,103, of ADHD, such as seizure disorders, sleep disorders,
these are commonly observed in other disorders and hyperthyroidism, physical or sexual abuse and sensory
are not core diagnostic criteria for ADHD12. To assist impairments113, as these can confound diagnosis.
diagnosis, several open access assessment tools have Although screening for ADHD is theoretically feasi
been created for use in both children (TABLE1) and adults ble given the availability of parent and self-reported
(TABLE2), and excellent, well-normed (standardized) scales (TABLE1), the few studies that have investigated the
commercial scales are available104. Importantly, patient use of early screening for ADHD have yielded inconsist-
age is relevant when assessing standard diagnostic cri- ent findings. For example, a 6-year longitudinal study
teria, such as those of the DSM or the International suggested that aparent-rated questionnaire might help
Statistical Classification of Diseases and Related Health with early detection, prediction and treatment plan-
Problems (ICD), owing to changes in the expression ning 114. However, owing to a lack of accurate predic-
of ADHD symptoms and impairments throughout an tors of onset, attempts at early prevention of ADHD
individuals lifetime (FIGS2,5). currently rely on population-level efforts to mitigate
NATURE REVIEWS | DISEASE PRIMERS VOLUME 1 | 2015 | 7
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
the effects of environmental risk factors for the dis screening programmes in primary care, parent training
order. Primary prevention strategies optimize maternal programmes, and specific games and play-based pro-
health during pregnancy by reducing extreme stress and grammes to enhance selfregulation when symptoms
psychosocial adversity, eliminating smoking, alcohol are identified115,116.
and drug use and reducing risk factors for preterm birth
and low birth weight. Secondary prevention approaches Adults
that detect symptoms of ADHD at an early stage Over the past 40years, clinical, family, treatment,
for example at infancy or preschoolage include longitudinal and population studies have generated
Table 1 | A selection of open access resources for assessing attention-deficit/hyperactivity disorder in childhood
Approach Comments Websites
Interviews
Schedule for Affective A semi-structured diagnostic interview http://www.psychiatry.pitt.edu/node/8233
Disorders and Evaluates past and current psychopathology in children and
Schizophrenia in adolescents, according to DSMIV and DSM-III criteria
School Age Children Translations in many languages
(KSADS) A DSM5 version is imminent
Diagnostic Interview A structured diagnostic that uses DSMIV to assess psychopathology http://www.cdc.gov/nchs/data/nhanes/
Schedule for Children in children and adolescents limited_access/interviewer_manual.pdf
(DISC) Translations in many languages
Child and Adolescent A semi-structured interview that evaluates current psychopathology https://devepi.duhs.duke.edu/capa.html
Psychiatric Assessment in children and adolescents
https://devepi.duhs.duke.edu/pubs/
(CAPA) Based on DSMIV criteria
papachapter.pdf
Versions for youths and preschool-aged children
Spanish and Portuguese translations
Development and For clinicians and trained non-clinicians http://www.dawba.com/b0.html
Well-Being Assessment Uses a prespecified set of questions and probes for impairment
(DAWBA) Generally used together with the SDQ
Translations in many languages
Parent Interview for A semi-structured interview focused on diagnostic criteria for ADHD, http://www.sickkids.ca/MS-Office-Files/
Child Symptoms (PICS) ODD and CD in children and adolescents Psychiatry/17145-Administration_Guidelines_
Addresses symptoms of other psychiatric disorders PICS6.pdf
Has been updated for DSM5 criteria
http://www.sickkids.ca/pdfs/Research/
Includes the TTI, which assesses symptoms of ADHD, ODD and CD in
Tannock/6013-TTI-IVManual.pdf
school, with screening questions for other psychopathology
Dutch translation
Child ADHD A structured telephone interview for teachers Available from the authors254
TTI(CHATTI) Focuses on DSMIV criteria for ADHD in school
Only available in English
Scales
Vanderbilt ADHD Versions for a parent or caregiver and teacher http://www.nichq.org/childrens-health/adhd/
Diagnostic Rating Part of the American Academy of Pediatrics ADHD Toolkit resources/vanderbilt-assessment-scales
Scales (VARS) Spanish translation
Swanson, Nolan and A rating scale for symptoms of ADHD and ODD Short scale (26item) available from: http://www.
Pelham (SNAP)-IV Can be completed by a teacher, parent or caregiver caddra.ca/pdfs/caddraGuidelines2011SNAP.pdf
Rating Scale Sensitive to changes related to treatment
Scoring guidelines available from: http://
Portuguese, Spanish and French translations
www.caddra.ca/pdfs/caddraGuidelines2011
SNAPInstructions.pdf
Full scale (90item) available from:
http://www.adhd.net/snap-iv-form.pdf
Scoring guidelines available from:
http://www.adhd.net/snap-iv-instructions.pdf
Strengths and Versions for a teacher, parent or caregiver http://www.adhd.net/SWAN_SCALE.pdf
Weaknesses of ADHD Based on DSMIV criteria
Symptoms and Normal Unusual in that the items are positively worded and it covers both
Behavior Scale (SWAN) strengths as well as weaknesses in ADHD and ODD symptoms
Spanish and French translations
SDQ Brief measure of emotional, ADHD, conduct and relationship problems http://sdqinfo.org
Versions for a parent, caregiver or teacher and a self-report
Translations in many languages
ADHD, attention-deficit/hypersensitivity disorder; CD, conduct disorder; DSM, Diagnostic and Statistical Manual of Mental Disorders; ODD, oppositional defiant
disorder; SDQ, Strengths and Difficulties Questionnaire; TTI, Teacher Telephone Interview.
8 | 2015 | VOLUME 1 www.nature.com/nrdp
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
Table 2 | A selection of open access resources for assessing attention-deficit/hyperactivity disorder in adulthood
Approach Comments Websites
Interviews
Diagnostic Interview for Adult A structured diagnostic interview for ADHD in adults according to http://www.divacenter.eu/
ADHD, second edition (DIVA 2.0) DSMIV DIVA.aspx
A new version based on DSM5 criteria is in press
Adult (ACDS) v1.2 A semi-structured interview of current symptoms of ADHD in adults Available from the author (Lenard
Provides age-specific prompts for rating both childhood and adulthood Adler) at: http://www.med.nyu.edu/
symptoms biosketch/adlerl01
Scales
Adult ADHD Self-Report Scale Developed by WHO to measure ADHD symptoms in individuals http://www.hcp.med.harvard.edu/
(ASRS) >18years of age ncs/asrs.php
An 18item version covers all DSMIV symptoms of ADHD
A 6item version is a screening tool validated for adolescents and adults
The 6item version (ASRS-Telephone Interview Probes for Symptoms;
ASRS-TIPS) uses semi-structured interview probes for examples of
ADHD symptoms
Both versions have been translated into many languages
Adult ADHD Investigator Incorporates suggested prompts for each ADHD item Available from Lenard Adlerat:
Symptom Rating Scale (AISRS) Descriptors for each ADHD item are explicitly defined http://www.med.nyu.edu/
Takes context into account biosketch/adlerl01
Wender Utah Rating Scale (WURS) Developed to retrospectively diagnose childhood ADHD in adults Available from the authors255
ADHD, attention-deficit/hypersensitivity disorder; DSM, Diagnostic and Statistical Manual of Mental Disorders.
very strong evidence that ADHD frequently persists satisfactory grades, a university student with ADHD
into adulthood, although its presentation changes with might need to work twice as hard as peers with the same
age23,117119 (FIG.5). Nevertheless, ADHD in adults is still aptitude to focus attention or to organize school work.
undertreated120, leading to international efforts to edu- If that restricts the students social life or causes other
cate clinicians (TABLE3) and to drive changes to DSM. problems, it might be viewed as impairing. Nonetheless,
DSM5 provides guidance about the differential expres- ADHD can be reliably diagnosed in these patients124.
sion of ADHD symptoms throughout the patients Finally, in adults with ADHD, hyperactiveimpulsive
lifetime. For instance, in contrast to young children, symptoms usually become internalized, such as feeling
adults with many impairing ADHD symptoms do not restless, and deficient emotional self-regulation125 and
typically climb on tables, have boundless energy or executive dysfunction126 become increasingly promi-
run around in a place where one should remain still. nent. Although deficient emotional regulation and
Hyperactivity in adulthood is often experienced as a executive dysfunction are not diagnostic for ADHD,
feeling of inner restlessness an internal motor that they are highly characteristic of the disorder in adults
never stops which makes it difficult for the indivi and could indicate the need for specific treatments,
dual to relax 121. By adopting symptom descriptors of such as cognitiveb ehavioural therapy, to improve
this sort, DSM5 is easier to apply to adults compared organizational or emotional self-regulationskills.
with its predecessors.
Despite these differences in symptom presentation, Heterogeneity of ADHD
the diagnostic process for adults parallels the process for Patients with ADHD show marked variation in profiles
youths in regards to documenting symptoms, impair- of symptoms, impairments, complicating factors, neuro
ment and onset of the disorder on the basis of a clinical psychological weaknesses and underlying causes127.
interview with the patient and, when available, reports Accordingly, effective partitioning of this heterogeneity
from informants. This process is aided by the avail- to refine diagnostic approaches and to provide tailored
ability of structured diagnostic interviews, such as the and targeted treatments remains an important research
Conners Adult ADHD Diagnostic Interview 122, along goal. To address this aim, DSM5 recognizes three
with rating scales for patients and informants, including presentations: predominantly inattentive, predomi-
the Adult Self-Report Scale (TABLE2)123. nantly hyperactiveimpulsive and combined. These
In adulthood, additional domains of impairment presentations are no longer deemed subtypes, as in
emerge and can include difficulties related to occupa- prior versions, because they can change over time128.
tion, marriage and parenting. Patients with high intelli Moreover, even within presentations, patients greatly
gence also present with a unique set of challenges. In differ in symptom profiles. For instance, the predomi-
these individuals, impairment can be assessed relative nantly inattentive presentation applies to individuals
to their aptitude. Some of these patients go to great with a wide range of inattention and can include sub-
lengths to accommodate their symptoms, which itself threshold hyperactiveimpulsive symptoms. Although
indicates impairment to the degree that it causes distress common in population samples, inattentive ADHD
or displaces other activities. For example, to achieve is less common in the clinic, which suggests that
NATURE REVIEWS | DISEASE PRIMERS VOLUME 1 | 2015 | 9
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
Behavioural disinhibition, emotional ability Full expression of ADHD, Inattention persists and
and emergence of diagnosis in preschool years psychiatric co-morbidity, hyperactiveimpulsive symptoms wane
school failure, peer
Prodrome: hyperactivity; and speech, language rejection and Smoking Substance abuse, low self-esteem and
and motor coordination problems neurocognitive dysfunction initiation social disability
In utero Childhood Adolescence Adulthood
Genetic predisposition Psychosocial inuences, chaotic family environments, peer inuences and mismatch with school and/or work environments
Fetal exposures Dierent genetic risk factors aect the course of ADHD at dierent stages of the lifespan
and epigenetic
changes Frontalsubcorticalcerebellar dysfunction via structural and functional brain abnormalities and downregulation of
catecholamine systems that regulate attention, reward, executive control and motor functions
Clinical progression
Aetiology Persistence of cortical thickness, default-mode
Pathophysiology network and white matter tract abnormalities
Naturecases.
Figure 5 | Developmental course of attention-deficit/hyperactivity disorder in persistent Reviews | Disease
Although noPrimers
single
sequence of events describes the pathway from in utero to adulthood, this figure describes key developmental events,
with boxes spanning their approximate onset along with hypotheses about the timing of the biological underpinnings
ofaetiological events and pathophysiological expression. ADHD, attention-deficit/hyperactivity disorder.
population screening for marked inattention should be The heterogeneity of ADHD has implications for
considered, especially in female children and adults, in both research and practice. In research, the diluting
which this pattern might be particularly impairing 129. effect of heterogeneity reduces effect sizes in ADHD
Persistent inattention even at subthreshold levels is casecontrol comparisons and renders biomarkers
a key predictor of poor academic outcomes130. that are identified on the assumption that ADHD is
Psychiatric co-morbidity is another clinically impor- pathophysiologically homogeneous obsolete. Clinically,
tant dimension of ADHD heterogeneity. At one extreme, heterogeneity means that tests either neuropsycho
a small proportion of clinic-referred individuals are free logical or tests of other underlying processes that
of co-morbidity; at the other end, some patients have a focus on only one domain will be of very limited diag-
complex pattern of multiple problems, including com- nostic value. However, such assessments could help to
munication disorders, intellectual disabilities131, sleep identify specific targets for therapeutic and educational
disorders132, specific learning disabilities131, mood dis- interventions that are aimed at remediating particular
orders131, disruptive behaviour 131, anxiety disorders131, areas of impairment and weakness. For instance, indivi
tic disorders131, autism spectrum disorders131,133 and sub- duals with working memory deficits might respond
stance use disorders131,134,135. Consideration of a patients favourably to working memory training 138.
co-morbidity profile is important, as it will influence
treatment planning. Management
Pathophysiological heterogeneity might be impor- By educating patients and families, clinicians can cre-
tant clinically although new research is required to ate a framework that increases treatment adherence,
determine whether subtyping on the basis of genetic, proactively plans for continuity of treatment through-
environmental, neurobiological or neuropsycho- out the lifetime of the patient and effectively integrates
logical factors will improve diagnostic and treatment pharmacological and non-pharmacological approaches.
approaches. In this regard, the largest body of evidence Education includes information about the causes of
relates to cognition. Objective tests indicate that sev- ADHD, its associated morbidity, the potential for a
eral distinct deficit profiles exist. For example, only a compromised course, the rationale for treatments and
minority of patients show a deficit in executive func- plans for key life transitions139. This education sets
tion136, which was once thought to be the core deficit in the stage for managing ADHD within a chronic care
ADHD. Other patients, who are clear of such deficits, paradigm that uses shared decision making to bol-
have problems in non-executive cognitive processes, ster treatment adherence and prepare patients for
which include those involved in basic memory and developmentalchallenges140.
temporal processing, motivational processing (delay There are geographic variations in the sequencing
tolerance or reinforcement processing) and cognitive of pharmacological and non-pharmacological treat-
energetic regulation72,73,137. Four cognitive ADHD sub- ments. For example, in the United States pharmaco
types were revealed in a study based on a community logical treatment is typically the first approach,
of children with or without ADHD70; however, whether whereas in Europe medication is usually reserved for
these subtypes predict treatment response or course severe cases or for milder cases that do not respond to
remains unclear. non-pharmacologicaltreatments141.
10 | 2015 | VOLUME 1 www.nature.com/nrdp
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
Pharmacological treatments school or work day, such as socializing, driving, doing
Before choosing a treatment, clinical experience advises homework and functioning in the familyenvironment.
several common-sense precautions. Appropriate atten- The pharmacological decision-making approach
tion needs to be given to the psychosocial environ- starts with whether the patient will benefit from a stimu
ment. In children, particular attention needs to be lant or non-stimulant treatment. Meta-analyses have
paid as to whether the family is intact or separated, demonstrated that stimulant and non-stimulant medi-
whether both parents are supportive of the childs cations for ADHD effectively reduce ADHD symptoms
treatment and whether there are any concerns about inchildren and adults142,143. By contrast, in preschool-
abuse or maltreatment. In addition, legal concerns, aged children, evidenced-based non-pharmacological
psychop athology and substance use in the parents, treatments are recommended as the first approach, when
psychosocial stressors (such as financial and medical available, but medication is indicated when symptoms
distress), access to firearms and the intellectual abilities are severe144. On average, stimulants (amphetamine
of the parents are assessed because treatments might and methylphenidate) are more efficacious than non-
not be effective in chaotic or potentially dangerous stimulants (atomoxetine, guanfacine and clonidine)145.
environments. Access to medications can also be an Accordingly, stimulants continue to be the first-line
issue, owing to a lack of health insurance or restric- psychopharmacological treatment for patients of all ages
tive policies by some governments or managed care with ADHD120.
formularies. Pharmacotherapy for ADHD will not Pharmacological treatments are typically long term,
address these issues, but appropriate social services except for those patients who do not have a persistent
or non-pharmacological interventions can mitigate course of ADHD. These treatments are generally associ-
their effects. It is important to educate parents and ated with improved outcomes in children and adults, as
patients about ADHD and its treatments to help them have been demonstrated by systematic reviews that con-
to understand the value of treatment options. sidered a range of different criteria to measure long-term
The choice of medication is guided by assessing the outcomes. For instance, a systematic review examined
severity of the symptoms, the presence of co-morbidities five randomized controlled trials (RCTs) and tenopen-
(FIG.6) and what periods of the day symptom relief is label extension studies of adults with ADHD that had
needed for example, during school hours only, dur- been conducted for at least 2years146. The authors con-
ing an extended school day, during a work day or during cluded that stimulant therapy for ADHD has long-term
the evening. With few exceptions, medications to treat beneficial effects and is well tolerated. In addition, a sys-
ADHD help patients 7days a week throughout the year tematic review of adult and child studies that had been
because the condition affects aspects of life outside the carried out over at least 2years concluded that treating
Table 3 | Selected resources for clinicians, parents and patients
Organization Content Websites
US NIMH Information for patients and families http://www.nimh.nih.gov
American Professional Society for Meetings for health professionals and researchers http://www.apsard.org
ADHD and Related Disorders
ADHD World Federation Meetings for health professionals and researchers http://www.adhd-federation.org
Children and Adults with ADHD Information for patients and families http://www.chadd.org
ADHD in Adults Continuing education for health professionals http://www.adhdinadults.com
Canadian ADHD Resource Alliance Continuing education and meetings for health professionals and http://www.caddra.ca
researchers; National Clinical Guidelines for ADHD; and policy
work with the government
Australian NHMRC Information for health professionals, patients and families http://www.nhmrc.gov.au/
guidelines-publications/mh26
ADHD Europe Information for patients and families http://www.adhdeurope.eu
European Network on Adult ADHD Meetings for health professionals and researchers http://www.eunetworkadultadhd.com/
International Collaboration on Meetings for health professionals and researchers http://www.adhdandsubstanceabuse.org
ADHD and Substance Abuse
UK Adult ADHD Network Meetings for health professionals and researchers http://www.ukaan.org
ADHD India Information for patients and families http://www.adhdindia.com
China ADHD Alliance Information for patients and families http://www.adhd-china.org/en-index.htm
Zentrales adhs-netz (German Information for patients and families http://www.zentrales-adhs-netz.de
Central ADHD Network)
American Academy of Pediatrics Information for health professionals http://www2.aap.org/pubserv/
ADHD Toolkit adhd2/1sted.html
ADHD, attention-deficit/hyperactivity disorder; NHMRC, National Health and Medical Research Council; NIMH, National Institute of Mental Health.
NATURE REVIEWS | DISEASE PRIMERS VOLUME 1 | 2015 | 11
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
Preschoolers, children and adolescents Adults
effects is prudent the goal being to provide the optimal
Parents Self-report duration of coverage throughout the day according to the
Teachers Signicant other (when available) needs of the patient151. For all stimulant formulations, the
duration of effect varies from patient to patient152. Thus,
the titration of stimulants addresses the onset and dura-
DSM-5 or ICD-10 diagnosis of ADHD tion of effect as well as overall efficacy and adverse events.
For example, long-acting stimulants take 12hours to
Preschoolers
begin working; thus, patients are told when to take the
When available, use evidenced-based non-pharmacological treatment rst medication to secure benefit at the beginning of the school
For severe symptoms, medication is indicated or work day. For some patients, the effects of long-acting
stimulants can wear off by mid-to-late afternoon, and they
might, therefore, need additional pharmacological cover-
With co-morbidity Without co-morbidity age to help to control symptoms later in the day. In such
cases, the prescription of a short-acting formulation of the
same drug can be used to extend itscoverage.
Mania and psychosis are Common adverse effects of stimulants are initial
Learning disorders, Cardiovascular
contraindications for stimulants
executive function disease and seizures
insomnia, decreased appetite, dysphoria and irritability.
Depression, tics and anxiety decits and low IQ are potential Sleep disturbances are very common in patients with
can worsen with stimulants
Substance use disorders might
are not responsive to contraindications ADHD, independent of stimulant use132, but those related
ADHD medications for stimulants
lead to abuse or diversion to stimulant use require parents to be instructed on how to
improve sleep hygiene or pharmacological management.
Figure 6 | Assessment guides management. The management | Disease Primers
of attention-deficit/
Nature Reviews
For example, a long-acting stimulant can be replaced with
hyperactivity disorder (ADHD) considers psychiatric, psychological and medical
an intermediate-acting formulation, or sleep onset can be
co-morbidity. DSM-5, Diagnostic and Statistical Manual of Mental Disorders, fifth edition;
ICD10, International Statistical Classification of Diseases and Related Health Problems,
improved with sleep aids such as melatonin153. As appe-
tenth edition; IQ, intelligence quotient. tite suppression usually occurs in the middle of the day,
its effects can usuallybe mitigated by taking the medica-
tion after breakfast. Inaddition, a substantial breakfast
ADHD improved long-term outcomes but generally and dinner as well as snacking during the day will manage
not to normal levels147. Another study found that long- energy levels and safeguard nutrition. If these measures
term medication use was associated with improved are not sufficient, nutritional supplementation can be
achievement test scores148. Furthermore, a systematic useful154. Insevere cases of weight loss or growth delays,
review of placebo-controlled discontinuation studies reducing the dose or discontinuing it over the weekend
and prospective long-term observational studies con- may be appropriate. Management of dysphoria and irri-
cluded that medication reduced ADHD symptoms and tability depends on whether these symptoms occur during
impairments, but that there was limited and inconsistent the peak or trough of the bioavailability of the medication,
evidence for long-term medication effects on improved as indicated by its pharmacokinetic curve155,156. If these
social functioning, academic achievement, employment symptoms occur during the peaks of drug bioavailabil-
status and psychiatric co-morbidity 149. Finally, although ity, switching to another stimulant is an option. If they
pharmacological approaches are generally efficacious, an occur during the troughs, they might be attributable to
important source of treatment failure is non-adherence withdrawal or rebound effects, which can be mitigated
to medication. For example, this was demonstrated in by adding a small dose of a short-acting stimulant 1hour
the 2-year followup of the Multimodal Treatment of before the symptoms occur. For patients that are sensi-
ADHD (MTA) study of children with ADHD, which tive to peaks and troughs of bioavailability, single-peak
reported that continuing medication use partly mediated formulations can be considered.
improved long-termoutcomes150. Although serious adverse effects are rare, they do
occur. The onset of tics, acute anxiety states, depression,
Stimulants. When choosing a stimulant, the first deci- psychosis and mania requires both the prompt discon-
sion is whether to use a methylphenidate product or tinuation of treatment and the search for alternative
an amphetamine product, both of which modulate the approaches consistent with emergent symptoms and diag-
action of dopamine. Methylphenidate and amphetamine noses157. Stimulants can be associated with small delays
block the dopamine transporter and amphetamine also in growth in height, but these tend to attenuate with time
promotes the release and reverse transport of dopamine. and seem not to affect ultimate height and weight in adult-
Although the efficacy of both classes of stimulants is hood158. Nevertheless, abnormal growth parameters can
similar, some patients preferentially respond to and toler- indicate the need to change treatments. Evidence for the
ate one or the other 143. There are no reliable predictors association of other serious adverse events with stimulant
of individual patient responses. Both families of stimu- use for ADHD is less robust. For example, some studies
lants have short-acting (24hours), intermediate-acting have raised concerns that stimulants cause sudden car-
(68hours) and long-acting (1012hours) formulations diac death, and one Danish study (n=714,258) found that
that enable clinicians to tailor duration of coverage for stimulant use was associated with an increased riskof
each patient. Starting the patient on a low dose andtitrat- any adverse cardiovascular event (adjusted hazard ratio
ing at weekly intervals depending on response and adverse of 1.83). These data from the Danish study are difficult
12 | 2015 | VOLUME 1 www.nature.com/nrdp
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
to interpret because the category of any included hyper- disorder is appropriately managed, ADHD can then be
tension, rheumatic fever and cardiovascular disease not treated effectively 170. As a result, combined treatments
otherwise specified; this final category accounted for are frequently used for the management of ADHD in
40% of cases159. Moreover, a study from the United States individuals withco-morbidity.
(n=1,200,438) reported that ADHD drugs (methylpheni- For patients with active substance use disorders,
date, amphetamine and atomoxetine) did not increase the stimulants are contraindicated or are used cautiously,
risk of serious cardiovascular events in children and young owing to concerns about the potential for abuse, mis-
adults160. The same was true for a subanalysis limited to use or diversion by the patient or caregiver. Such con-
methylphenidate, which was the only drug with sufficient cerns contrast with substantial literature that indicates
data. Inaddition, a meta-analysis of observational stud- stimulant use in childhood has a protective effect on
ies concluded that ADHD drugs (mostly methylphenidate subsequent smoking 171 and neutral or protective effects
and amphetamine) did not increase the risk of sudden on subsequent drug and alcohol use disorders172175.
death in children161. Thus, for patients with pre-existing However, substantial data indicate that a minority of
cardiac conditions, stimulants should be used cautiously patients with ADHD divert their stimulant medication
and only after consultation with a cardiologist162,163, and in for misuse byothers176.
all patients treated with stimulants, blood pressure should Atomoxetine has been tested successfully in the
be monitored during treatment. Stimulants can be used management of ADHD in the context of co-morbidity
cautiously or not at all in the presence of tic, bipolar, with tics, anxiety and depression177,178, and one review
anxiety, and substance use disorders and seizures. suggested that 2adrenergic agonists yield the best
combined improvement for ADHD that is co-morbid
Non-stimulants. Two classes of non-stimulants have with tic disorders179. Bupropion is approved for use in
been approved by regulatory agencies for the treatment depression in adults, and its efficacy in ADHD has been
of ADHD. These include the selective noradrenaline confirmedin a meta-analysis180. Some reports have docu
reuptake inhibitor atomoxetine164 and long-acting formu- mented the efficacy of stimulants181, extended-release
lations of two 2adrenergic agonist drugs clonidine165 guanfacine182 and atomoxetine183 for the treatment of
and guanfacine166. These drugs are effective in the manage- comorbid oppositional defiant disorder symptoms.
ment of ADHD, but the sedative effects of 2adrenergic When treated with ADHD medications, patients with
agonists limit their use in somepatients165,167. intellectual disabilities184 or traumatic brain injury 185
Similar to stimulants, these medications require slow show a reduction in ADHD symptoms. General cog-
titration to avoid adverse effects by starting with a low nitive ability is not responsive to ADHD pharmaco
dose and adjusting it based on outcomes. Atomoxetine therapy; however, some data suggest that atomoxetine
can be administered once or twice daily. Long-acting can modestly improve dyslexia186 and that stimulants187
guanfacine was tested in children and found to be more and atomoxetine 188 yield modest improvements in
effective at higher doses, but these doses were associated behavioural measures of executive functioning as well
with more adverse effects. 2adrenergic agonists can as performance on executive memory, reaction time and
also be administered once or twice daily. Their efficacy inhibitory control tasks72. Although some academic per-
has been documented for young children but not for formance problems associated with symptoms of ADHD
adolescents andadults. (for example, homework completion) can improve with
Combined therapy with stimulants and atomoxetine or treatment, medication cannot replace missing skills,
a long-acting 2adrenergic agonist might be effective for improve academic achievement scores or ameliorate
patients who have been unresponsive to monotherapy 168, specific learningdisabilities189.
but the implications of these combined therapies for Taken together, it is clear that finding an effective for-
cardiovascular safety have not been adequately studied. mulation, daily dose and dosing schedule for an ADHD
Patients who do not respond to stimulants, atomoxetine medication is crucial for successful treatment. The use
or 2adrenergic agonists might respond to other medica- of tools such as management decision trees that sum-
tions that have been used off-label in the management of marize recommendations about pharmacotherapy and
ADHD, such as tricyclic antidepressants, bupropion (an the integration of non-pharmacological treatments can
antidepressant) or modafinil (a wakefulness-promoting be useful in guiding ADHD management (FIG.7). The
agent that is commonly used to treat narcolepsy). efficacy of these treatments will be augmented by moni-
Although some data support the efficacy of these off- toring both symptomatic and functional outcomes and
label medications for the treatment of ADHD169, regula- promotingadherence151.
tory agencies in the United States and the European Union
have not approved their use in thiscontext. Non-pharmacological treatments
Non-pharmacological approaches for the treatment of
Psychiatric co-morbidity. The co-morbidities of ADHD ADHD might be required for several reasons. First, some
affect the clinical picture of this disorder and its manage- patients do not respond positively to medication and
ment. The rule of thumb is to address the most serious might experience, for example, poor symptom control,
disorder first. For example, it would be almost impos- unmanageable adverse events or both. Second, medica-
sible to manage ADHD in the presence of a serious, tion alone might not produce optimal results across all
active mood or substance use disorder; these conditions domains of ADHD-related impairment. Third, patients
need to be addressed first. However, when the other might not have access to medication because of either
NATURE REVIEWS | DISEASE PRIMERS VOLUME 1 | 2015 | 13
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
parent or clinician concern or restrictive government supplementation with free fatty acids, but the clinical
policies that limit access. Even in jurisdictions where effects were small193. Insufficient evidence supports
medications are licensed and available, there are varia- other supplement types, for example, vitamins or
tions in expert recommendations. Last, patients might herbs, or homeopathic approaches. Finally, exclusion
be considered too young or to have an insufficiently diets those generally targeting artificial additives
severe presentation to warrant medication190. and those addressing idiosyncratic intolerances also
A range of dietary, behavioural and neurocognitive demonstrated positive effects, but these were, on aver-
therapies are used as either precursors to, instead of, age, very small (when blinded measures were used) or
or as a complement to medication to target co-morbid predominantly in a subgroup of patients with known
conditions and broader patterns of psychosocial impair- foodintolerances193,194.
ment. The strength and quality of supporting evidence
vary widely from treatment to treatment; in general, Behavioural interventions. Behavioural interven-
even when efficacy is shown, effect sizes are substantially tions are the best-established, most positively recom-
smaller than for optimized medication191,192. In addi- mended and most widely used form of psychological
tion, adverse events are typically not reported in non- treatment 195. The well-tested principles of positive and
pharmacological trials whether the lack of reporting is negative reinforcement and social learning provide the
because adverse events do not occur or are not measured foundation for a range of techniques that are often modi-
remains unclear. Data on the cost effectiveness of treat- fied to increase their value for patients with ADHD, to
ment are also scant. No simple algorithm can choose reduce inappropriate and promote appropriate behav-
among these treatments, and treatment use should be iour and to improve parentchild relationships195,196.
determined by the individual needs and circumstances Inearly and middle childhood, this practice typically
of patients and their families. takes the form of parent training. In addition, behaviour-
ally based, school-focused interventions combined with
Dietary interventions. Dietary interventions are of two approaches aimed at adapting classroom structure to aid
general types: supplements and exclusions. Ameta- concentration and deportment also have value197. Group
analysis concluded that dietary treatments can play a and individually administered interventions are also
potentially positive but limited therapeutic part in man- available198, and game-like elements designed to increase
aging ADHD193. The clearest evidence has supported the childs core regulatory abilities are being intro-
duced. Parent training is positively received by families,
especially when child compliance is the primary prob-
Co-morbid condition more severe than ADHD? lem140. However, on the basis of a recent meta-analysis of
RCTs restricted to blinded outcomes, behavioural inter-
Yes No
ventions are probably best used to complement not
replace ADHD medication199. Although behavioural
Treat co-morbid condition interventions have minimal effects on symptoms of
ADHD, they have a considerable influence on the qual-
When co-morbid condition is stable, treat ADHD ity of parenting and cooccurring conduct problems in
children with ADHD199.
More-focused approaches improve specific areas
Contraindications from stimulants or personal preference against stimulants?
of daily functioning, such as social200 or organizational
Yes No skills201. Although perhaps most beneficial for chil-
dren who have cooccurring difficulties, behavioural
approaches might also be valuable for children with-
Non-stimulants Stimulants
2-adrenergic Amphetamine out these difficulties. Indeed, improving the quality of
medications Methylphenidate parenting has longer-term protective effects and thereby
Atomoxetine reduces the chance that ADHD will escalate to more-
complex and severe forms. School-based approaches
Short acting Intermediate acting Long acting that focus on broad-based skills training and academic
(24 hours) (68 hours) (1012 hours)
achievement are also of value in the long term197,202.
In addition to approaches for children with ADHD,
Full response Full response cognitivebehavioural therapy and life-management
Monitor progress Monitor progress
skills coaching are recommended for adolescent 203 and
Partial response Partial response
Target residual disability with Target residual disability with adult 204 patients. These skills include selfinstructional
non-pharmacological treatments non-pharmacological treatments self-control training, problem solving, use of compensa-
Poor or no response Poor or no response tory strategies, diaries or time schedules and social com-
Try an alternative non-stimulant Try an alternative stimulant or a non-stimulant
munication coaching205. Individual RCTs provide support
Figure 7 | Management decision tree. The choice ofNature Reviews
medication | Disease Primers
for treating for these approaches based on patient-reported ratings,
attention-deficit/hyperactivity disorder (ADHD) considers contraindications, personal but corroboration through meta-analyses is required.
preferences, psychiatric co-morbidity and the duration of coverage required. Individual trials also suggest that psychotherapy 206, fam-
Nonpharmacological treatments target residual disability and are used initially for ily therapy 207 and lifestyle interventions115 might improve
preschool-aged children or when medication is declined by the patient or parent. specific areas of functioning in somepatients.
14 | 2015 | VOLUME 1 www.nature.com/nrdp
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
Health problems and psychiatric Social disability Premature mortality
co-morbidities Risky behaviours
Psychological dysfunction Overweight, obesity and hypertension
Academic and occupational failure
Delinquency and criminality, smoking and addictions
Specic learning disabilities and executive dysfunction
Disruptive behaviour, mood, anxiety, elimination, tic and autism spectrum disorders
Developmental coordination disorder, and speech and Marital discord, separation and divorce, parenting problems,
language disorders and legal problems, arrests and incarcerations
Poor social skills, impaired family relationships, poor peer relationships and rejection by peers
Suicidal ideation, suicide attempts and suicide
Lower quality of life and low self-esteem
Emotional dysregulation and lack of motivation
Underachievement, grade repetition, special education needs, Reduced occupational performance, unemployment
school expulsion and dropping out and lower socioeconomic status
Unplanned pregnancies
Accidents and injuries, trac accidents and violation, and licence suspensions
Childhood Adolescence Adulthood
Figure 8 | Quality of life and attention-deficit/hyperactivity disorder. Throughout the lifetime
Nature of the patient,
Reviews | Disease Primers
theimpairments of attention-deficit/hyperactivity disorder manifest in psychiatric co-morbidities, health problems,
psychological dysfunction, academic and occupational failure, social disability and risky behaviours.
Neurocognitive interventions. Neurofeedback interven- of these effects to non-targeted deficits, ADHD symp-
tions use adaptive reward-based techniques to normalize toms or other areas of impairment 138. Alternative non-
specific elements of a patients aberrant electrophysio computerized meditation-based approaches such as
logical profile that are thought to mediate problems with mindfulness training seek to improve the regulation
attention208. Such interventions target either specific of attentional processes212. However, owing to insuf-
electroencephalogram frequency bands or slow or late ficient evidence from well-designed trials, mindful-
components of event-related potentials. Some RCTs have ness training cannot be recommended as a treatment
provided evidence for the value of neurofeedback for forADHD.
reducing ADHD symptoms, with the most pronounced
effect of neurofeedback found for treating inattention209. Quality of life
However, recent meta-analyses have concluded that ADHD impairs psychosocial functioning in a range of
more evidence is required before neurofeedback can be contexts that include social, academic and occupational
endorsed for treating ADHD symptoms, owing to the settings, and the disorder directly affects perceptions
lack of robust effects for blinded measures191,210. of well-being (FIG.8). For instance, children and ado-
Other neurocognitive approaches target functions lescents with ADHD are at high risk of school failure,
such as working memory and inhibition. Using com- parental and family conflict, social rejection by peers,
puters, such approaches train these functions over mul- low self-esteem and delinquent behaviour. In addi-
tiple sessions that continuously challenge the patients tion, compared with the general population, the risk
competence by increasing difficulty as performance of smoking and substance use disorders is increased
improves211. Recent meta-analyses have demonstrated in patients with ADHD, especially among patients
only small effects on ADHD symptoms when different who also have conduct or antisocial personality dis
training approaches were grouped together and effects order 213,214. Adverse outcomes in adolescence and
were measured using blinded outcomes138,210. Evidence adulthood for people with ADHD include academic
was weakest for working memory training and strong- and vocational underachievement, reduced occupa
est for interventions targeting multiple neurocognitive tional functioning, obesity 215, emotional dysregu
deficits. Effects on targeted deficits, such as working lation103, unemployment and suicide attempts121,216.
memory in training trials, were positive and highly Traffic accidents and violations are more frequent in
significant, although no evidence supported the transfer drivers with ADHD121,217,218 than in those without the
NATURE REVIEWS | DISEASE PRIMERS VOLUME 1 | 2015 | 15
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
disorder, and family relationships involving indivi The strongest effects on HRQOL measures were
duals with ADHD might be characterized by discord found in the psychosocial, achievement and family life
and negative interactions compared with families unaf- domains. Children with ADHD also rated their HRQOL
fected by ADHD217,219221. Finally, patients with ADHD to be lower than that of their peers without ADHD225.
or a history of childhood ADHD, particularly from Similarly, adults with ADHD have a low HRQOL both
non-medical causes, have higher mortality rates than in adulthood227,228 and in their retrospective reports
those without ADHD, as consistently documented in fromchildhood229.
longitudinal studies222,223 and a recent registry study 224. Although increases in ADHD symptom severity and
These functional impairments reduce the psycho functional impairment predict poorer HRQOL, the
logical and social well-being and health-related qual- correlations are moderate, which indicates that ADHD
ity of life (HRQOL) of patients with ADHD 225. For symptoms, functional impairment and HRQOL are
example, in the pan-European ADHD Observational related but distinct constructs. Accordingly, HRQOL
Research in Europe (ADORE) study, parents reported is an important component of a comprehensive assess-
low HRQOL for their children across a broad range ment. For instance, in the ADORE study, several family
of psychos ocial, achievement and self-evaluation factors, such as having a parent with a health or men-
domains, which accords with findings from clini- tal health problem, the child living in a single-parent
cal studies 225,226. Both inattentive and hyperactive household and maternal smoking during pregnancy,
impulsive symptoms diminished HRQOL ratings. also predicted poorer HRQOL226.
Table4 | Outlook for attention-deficit/hyperactivity disorder research and practice
Area Approach Comments
Technological GWAS, exome sequencing and GWAS will discover genome-wide significant common DNA risk variants and quantify the
advances whole-genome sequencing polygenic risk for ADHD
Sequencing will discover rare, functional DNA variants
Expect insights into causal biological pathways relevant to treatment and biomarkers
iPSCs iPSCs derived from peripheral tissue of patients with ADHD who carry known mutations will be
used to create brain cells
Studying these cells will clarify mechanisms and provide insights for treatment
Epigenomics, transcriptomics Epigenomics will show how genes and the environment combine to modify gene expression
and proteomics Mapping these pathways will describe the molecular mechanisms underlying the
pathophysiology of ADHD
Small animal models (such as Drug discovery requires faster and cheaper model systems to screen molecules for activity
zebrafish and fruitfly) and iPSCs against targets identified by omic studies
Clinical Therapeutic games and Computer training methods could target specific deficits and adapt to the needs of patients
research computer technologies Incorporating game features should improve acceptability and adherence
Treatment adherence protocols Mobile technologies such as text messaging should improve adherence to ADHD treatments
Development of screening Screening methods might decrease the lag between onset of symptoms and treatment,
andprevention models andthus improve outcomes
Neurobiological subtypes Neuropsychological, neuroimaging and genetic studies might parse the heterogeneity
ofADHD ofADHD to aid the development of better diagnostic and treatment strategies
New ADHD drugs Biological research will yield new drug targets for drug development
Longitudinal Studies beginning at conception Environmental effects on the fetus need to be studied prospectively to better quantify risk
research andclarify developmental trajectories associated with ADHD genotypes
Longitudinal neuroimaging Clarify the reasons for the persistence and remission of ADHD
Future work will solidify these findings and use multimodal imaging to show how aberrant
neurodevelopment is associated with symptom trajectories
International PGC Provides a platform for large-scale data sharing of large samples
collaboration Enables highly powered studies for the discovery of potential biomarkers and treatment targets
ENIGMA Enables large-scale studies of how genetic risk variants affect brain structure and function
Will provide insight into brain-based biomarkers and the neural pathways underlying
ADHDsymptoms
Altered The RDoC project of the US Encourages researchers to study dimensional constructs that underlie the expression
funding NIMH ofmultiple disorders
priorities Might lead to a change in how psychiatric disorders are viewed and classified
The EU Horizon 2020 European funding is increasingly organized around traits and characteristics shared among
programme diseases and disorders
This will direct research to focus on larger, potentially more quantitative disease definitions
ADHD, attention-deficient/hyperactivity disorder; ENIGMA, Enhancing Neuro Imaging Genetics through Meta-Analysis; EU, European Union; GWAS, genome-wide
association studies; iPSCs, induced pluripotent stem cells; NIMH, National Institute of Mental Health; PGC, Psychiatric Genomics Consortium; RDoC, Research
Domain Criteria.
16 | 2015 | VOLUME 1 www.nature.com/nrdp
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
Treatments for ADHD reduce functional impair- Research in humans will be needed to validate the
ments and improve HRQOL. This evidence is, so far, relevance of cell-based and animal model studies.
almost entirely limited to pharmacological treatments. Neuroimaging genetic studies could fill this gap but
Epidemiological and clinical studies have found benefi- will require large international collaborations, such as
cial effects of medication on functioning and HRQOL for the Enhancing Neuro Imaging Genetics through Meta-
stimulants and for atomoxetine230. These effects which Analysis (ENIGMA) consortium243. More importantly,
were reported for both youths and adults mirror, to tissue resource centres should prioritize the preservation
some extent, medication effects on symptoms of ADHD, of brain tissue from patients with ADHD; post-mortem
although with smaller effect sizes. Medication effects studies of the brains of patients with ADHD are essential
on HRQOL have been found across multiple domains, for progress in understanding the molecular mechanisms
including key domains relating to achievement in of the disorder. In addition, neurobiological studies will
school231. Moreover, findings from national registry need to implement systematic and statistically sophisti
studies indicate that the use of medication, particularly cated biological subtyping approaches to clarify the
stimulants, reduces the risk of accidents and trauma- clinical and biological heterogeneity ofADHD.
related emergency department admissions and might Future work will first improve the behavioural diag-
have protective effects on substance abuse, suicidal and nosis of ADHD and, in the long run, set the stage for
delinquent behaviour 175,214,232,233. Given that few data are diagnoses that are assisted by biomarker technologies.
available on longer-term treatment effects234,235, the extent Current diagnostic criteria will probably be refined to
to which changes in HRQOL are mediated by symptom improve the developmental sensitivity of diagnostic cri-
changes, changes in functional impairment or other fac- teria from childhood through to adulthood. Research
tors remain unclear 146. For example, one study found that into the best symptom threshold for ADHD in adults
medication-related improvement of HRQOL persisted will continue. For example, studies have shown that
following medication withdrawal, even when symptom among adults who had at least six out of nine symptoms
severity increased236, indicating that any potential cause in childhood, having only four out of six symptomsin
effect relationships between medication use, symptom adulthood predicts substantial impairment later in life244.
and functional impairment reduction and HRQOL Future studies should consider balancing symptom
require further investigation. thresholds and functional impairment to define valid
diagnostic algorithms for more-refined age groups (for
Outlook example, preschool, childhood, adolescence and adult-
In 2011, the Grand Challenges in Global Mental Health hood). There is also a need to learn more about the
Initiative (GCMHI) defined a set of 25 urgent research validity of the ADHD diagnosis when onset occurs after
priorities237. Four GCMHI themes are of high relevance 12years of age. Such research will increase diagnostic
to ADHD: clarifying the causes of the disorder, improv- accuracy and provide screening methods for clinicians.
ing diagnosis and treatment, developing preventive Finally, the evolution of diagnostic approaches will be
strategies and defining the global burden of disease. influenced by a renewed focus on dimensional clinical
These research themes are intertwined. Clarification and cognitive constructs, such as those described in the
of the causes of ADHD and identification of the mech Research Domain Criteria (RDoC) project of the US
anisms underpinning pathophysiology will be the most National Institute of Mental Health245. These approaches
direct path towards improving therapeutic strategies and discard diagnostic categories when looking into the
identifying biomarkers to create objective diagnoses that cognitive and clinical features of ADHD and other
can select participants for primary prevention protocols relateddisorders.
(TABLE4). The discovery of biomarkers that objectify the diag-
Ongoing and planned research in the next 5years nosis of ADHD will reduce stigma and might foster
should yield robust information about which genes and precision medicine approaches that are tailored to indi-
regulatory regions increase the risk of ADHD. This infor- vidual patients. No proposed biomarker currently meets
mation will come from more powerful GWAS and the the criteria for validity 246, but the future application of
use of exome sequencing or whole-genome sequencing machine learning 247 might reveal multivariate patterns
technologies238. To translate genetic findings into mech in biomarker data that have better predictive accuracy.
anisms and to map the biological pathways from genetic Given the heterogeneity and multifactorial aetiology of
variation to disease risk50 calls for various approaches ADHD, a successful biomarker will probably incorporate
that encompass bioinformatics, cell-based and animal multiple domains of measurement.
model research, neuroimaging and behavioural genetic Several new drugs for ADHD have passed safety tests
analyses. Although many animal models of ADHD and are being tested in humans. Some of these agents
have been developed239, very few lend themselves to the have mechanisms of action previously unexploited in
much-needed medium-throughput or high-throughput ADHD; others are new formulations of existing medi-
analyses of the effects of genetic risk variants. Promising cations that will provide new options for the timing
first steps include models of ADHD that are based on and duration of efficacy throughout the day. Whereas
zebrafish240 and fruitflies241. Cellular models of ADHD current medications have dopaminergic or noradren-
will benefit from advances in induced pluripotent stem ergic targets, future work might capitalize on studies
cell technology 242. The ultimate goal of this work will be that implicate the nicotinic acetylcholine58, glutamate44,
to discover new targets for treatment. aminobutyric acid (GABA)248, serotonin249, neurite
NATURE REVIEWS | DISEASE PRIMERS VOLUME 1 | 2015 | 17
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
outgrowth50 or endosomal250 systems. For example, a people with ADHD that the goal of treatment studies
mouse model has demonstrated that fetal exposure to is evolving from reducing ADHD symptoms to elimi-
nicotine yields hyperactivity, reduces cingulate cortex nating all ADHD symptoms and achieving functional
volume, reduces dopamine turnover and responsive- remission and improvedQOL151.
ness to methylphenidate and might thereby lead to An important research principle explicitly named by
the identification of new pharmacotherapies58. New the GCMHI is the implementation of a life-course per-
drugs for ADHD could help clinicians to target specific spective. With some notable exceptions, research into
symptomdomains. child and adult forms of ADHD has been carried out in
Further improvements to non-pharmacological isolation; certain age groups, especially preschool-aged
approaches involving diet, mindfulness training, neuro children, adolescents and the elderly, have a relatively
feedback, cognitive training and specific computer small research base. Longitudinal studies are, therefore,
gaming might yield innovative approaches. Even if they needed to define the developmental course of ADHD and
do not treat the core symptoms of ADHD, they might to understand why some children with ADHD achieve
complement medication and behavioural approaches functional normality in adulthood but others continue to
by treating associated symptoms. Novel approaches to experience a chronic, severely impairing form of the dis-
improve adherence to treatment are also being devel- order. New research is indeed beginning to define neu-
oped. These strategies might have immediate clinical ral predictors and correlatesof remission94,95,253. Defining
impact given the low level of adherence to ADHD treat- predictors and correlates ofremission might eventually
ments251. Interventions are also needed to prevent the lead to a better allocationof treatment resources to chil-
misuse and diversion of ADHD medications, especially dren and adolescents who are at highest risk for persistent
on university campuses176. and complicatedADHD.
Increased patient involvement in research will yield Research innovations along with international and
treatment studies of real-world or patient-centred out- interdisciplinary collaborations promise a bright future
comes, such as academic performance, driving, social for ADHD research. By applying an integrated, bench-
functioning and QOL. Given that such issues are dif- to-bedside approach, we can make great strides in under-
ficult to address in RCTs, the cautious application of standing the aetiology of ADHD, refining its diagnosis,
pragmatic clinical trials252 should lead to a better under- optimizing treatment outcomes and improving the QOL
standing of how to manage ADHD. It is good news for of patients of allages with ADHD.
1. Barkley,R.A. & Peters,H. The earliest reference to 10. Michielsen,M. etal. Prevalence of attention-deficit factors in DSM-III attention deficit disorder. J.Am.
ADHD in the medical literature? Melchior Adam hyperactivity disorder in older adults in The Acad. Child Adolesc. Psychiatry 29, 526533 (1990).
Weikards description in 1775 of attention deficit Netherlands. Br. J.Psychiatry 201, 298305 (2012). 22. Larsson,H., Chang,Z., DOnofrio,B.M. &
(Mangel der Aufmerksamkeit, Attentio Volubilis). 11. Guldberg-Kjar,T. & Johansson,B. Old people Lichtenstein,P. The heritability of clinically diagnosed
J.Atten. Disord. 16, 623630 (2012). reporting childhood AD/HD symptoms: retrospectively attention deficit hyperactivity disorder across the
2. Polanczyk,G., de Lima,M.S., Horta,B.L., self-rated AD/HD symptoms in a population-based lifespan. Psychol. Med. 44, 22232229 (2014).
Biederman,J. & Rohde,L.A. The worldwide prevalence Swedish sample aged 6580. Nord. J.Psychiatry 63, 23. Franke,B. etal. The genetics of attention deficit/
of ADHD: a systematic review and metaregression 375382 (2009). hyperactivity disorder in adults, a review.
analysis. Am. J.Psychiatry 164, 942948 (2007). 12. American Psychiatric Association. Diagnostic and Mol.Psychiatry 17, 960987 (2012).
This meta-analysis provides both a comprehensive Statistical Manual of Mental Disorders 5th edn 24. Faraone,S.V. etal. Molecular genetics of attention-
estimate of the prevalence of ADHD in youths (American Psychiatric Publishing, 2013). deficit/hyperactivity disorder. Biol. Psychiatry 57,
andthe reasons for its variability worldwide. 13. Polanczyk,G. etal. Implications of extending the 13131323 (2005).
3. Polanczyk,G.V., Willcutt,E.G., Salum,G.A., Kieling,C. ADHD ageofonset criterion to age 12: results from 25. Asherson,P. & Gurling,H. Quantitative and molecular
& Rohde,L.A. ADHD prevalence estimates across aprospectively studied birth cohort. J.Am. Acad. genetics of ADHD. Curr. Top. Behav. Neurosci. 9,
three decades: an updated systematic review and Child Adolesc. Psychiatry 49, 210216 (2010). 239272 (2012).
metaregression analysis. Int. J.Epidemiol. 43, 14. Matte,B. etal. ADHD in DSM5: a field trial in a large, 26. Burt,S.A. Rethinking environmental contributions
434442 (2014). representative sample of 18- to 19year-old adults. tochild and adolescent psychopathology:
4. Thomas,R., Sanders,S., Doust,J., Beller,E. Psychol. Med. 45, 361373 (2015). ametaanalysis of shared environmental influences.
&Glasziou,P. Prevalence of attention-deficit/ 15. Larsson,H., Sariaslan,A., Langstrom,N., Psychol.Bull. 135, 608637 (2009).
hyperactivity disorder: a systematic review and DOnofrio,B. & Lichtenstein,P. Family income in 27. Larsson,H., Anckarsater,H., Rastam,M., Chang,Z.
metaanalysis. Pediatrics 135, e994e1001 (2015). earlychildhood and subsequent attention deficit/ &Lichtenstein,P. Childhood attention-deficit
5. Erskine,H.E. etal. Epidemiological modelling of hyperactivity disorder: a quasi-experimental study. hyperactivity disorder as an extreme of a continuous
attention-deficit/hyperactivity disorder and conduct J.Child Psychol. Psychiatry 55, 428435 (2014). trait: a quantitative genetic study of 8,500 twin pairs.
disorder for the Global Burden of Disease Study 2010. 16. Biederman,J. etal. Educational and occupational J.Child Psychol. Psychiatry 53, 7380 (2012).
J.Child Psychol. Psychiatry 54, 12631274 (2013). underattainment in adults with attention-deficit/ 28. Chang,Z., Lichtenstein,P., Asherson,P.J.
6. Sciutto,M.J. & Eisenberg,M. Evaluating the evidence hyperactivity disorder: a controlled study. J.Clin. &Larsson,H. Developmental twin study of attention
for and against the overdiagnosis of ADHD. J.Atten. Psychiatry 69, 12171222 (2008). problems: high heritabilities throughout development.
Disord. 11, 106113 (2007). 17. Lingineni,R.K. etal. Factors associated with attention JAMA Psychiatry 70, 311318 (2013).
7. Faraone,S. V., Biederman,J. & Mick,E. The age deficit/hyperactivity disorder among US children: 29. Larsson,H. etal. Genetic and environmental
dependent decline of attention-deficit/hyperactivity results from a national survey. BMC Pediatr. 12, 50 influences on adult attention deficit hyperactivity
disorder:a meta-analysis of followup studies. (2012). disorder symptoms: a large Swedish population-
Psychol.Med. 36, 159165 (2006). 18. Visser,S.N. etal. Trends in the parent-report of health based study of twins. Psychol. Med. 43, 197207
This meta-analysis provides a clear estimate ofthe care provider-diagnosed and medicated attention- (2013).
persistence of ADHD from childhood to adulthood deficit/hyperactivity disorder: United States, 30. Merwood,A. etal. Genetic associations between the
and highlights that, although the majority of ADHD 20032011. J.Am. Acad. Child Adolesc. Psychiatry symptoms of attention-deficit/hyperactivity disorder
cases detected in childhood donot fulfil the entire 53, 3446.e2 (2014). and emotional lability in child and adolescent twins.
diagnostic criteria in adulthood, persistence of 19. Zwirs,B.W. etal. Prevalence of psychiatric disorders J.Am. Acad. Child Adolesc. Psychiatry 53, 209220.
impairing systems iscommon. among children of different ethnic origin. J.Abnorm. e4 (2014).
8. Biederman,J., Mick,E. & Faraone,S.V. Age-dependent Child Psychol. 35, 556566 (2007). 31. Surman,C.B. etal. Deficient emotional self-regulation
decline of symptoms of attention deficit hyperactivity 20. Biederman,J. etal. Further evidence for family- and adult attention deficit hyperactivity disorder:
disorder: impact of remission definition and symptom genetic risk factors in attention deficit hyperactivity afamily risk analysis. Am. J.Psychiatry 168,
type. Am. J.Psychiatry 157, 816818 (2000). disorder. Patterns of comorbidity in probands and 617623 (2011).
9. Simon,V., Czobor,P., Balint,S., Meszaros,A. &Bitter,I. relatives in psychiatrically and pediatrically referred 32. Christiansen,H. etal. Cotransmission of conduct
Prevalence and correlates of adult attention-deficit samples. Arch. Gen. Psychiatry 49, 728738 (1992). problems with attention-deficit/hyperactivity disorder:
hyperactivity disorder: meta-analysis. Br. J.Psychiatry 21. Biederman,J., Faraone,S.V., Keenan,K., Knee,D. familial evidence for a distinct disorder. J.Neural
194, 204211 (2009). &Tsuang,M.T. Family-genetic and psychosocial risk Transm. 115, 163175 (2008).
18 | 2015 | VOLUME 1 www.nature.com/nrdp
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
33. Kuntsi,J. etal. The separation of ADHD inattention and 54. Stevens,S.E. etal. Inattention/overactivity following 75. Plichta,M.M. & Scheres,A. Ventralstriatal
hyperactivityimpulsivity symptoms: pathways from early severe institutional deprivation: presentation responsiveness during reward anticipation in ADHD
genetic effects to cognitive impairments and symptoms. andassociations in early adolescence. J.Abnorm. and its relation to trait impulsivity in the healthy
J.Abnorm. Child Psychol. 42, 127136 (2014). Child Psychol. 36, 385398 (2008). population: a meta-analytic review of the fMRI
34. Rommelse,N.N., Franke,B., Geurts,H.M., 55. Banerjee,T.D., Middleton,F. & Faraone,S.V. literature. Neurosci.Biobehav. Rev. 38, 125134
Hartman,C.A. & Buitelaar,J.K. Shared heritability Environmental risk factors for attention-deficit (2014).
ofattention-deficit/hyperactivity disorder and autism hyperactivity disorder. Acta Pediatr. 96, 12691274 76. Fassbender,C. & Schweitzer,J.B. Is there evidence
spectrum disorder. Eur. Child Adolesc. Psychiatry 19, (2007). for neural compensation in attention deficit
281295 (2010). 56. Scassellati,C., Bonvicini,C., Faraone,S.V. hyperactivity disorder? A review of the functional
35. Cole,J., Ball,H.A., Martin,N.C., Scourfield,J. &Gennarelli,M. Biomarkers and attention-deficit/ neuroimaging literature. Clin. Psychol. Rev. 26,
&McGuffin,P. Genetic overlap between measures hyperactivity disorder: a systematic review and 445465 (2006).
ofhyperactivity/inattention and mood in children metaanalyses. J.Am. Acad. Child Adolesc. Psychiatry 77. Rubia,K. etal. Effects of stimulants on brain
andadolescents. J.Am. Acad. Child Adolesc. 51, 10031019.e20 (2012). functioninattention-deficit/hyperactivity disorder:
Psychiatry 48, 10941101 (2009). 57. Dasbanerjee,T. etal. A comparison of molecular a systematic review and meta-analysis.
36. Doyle,A.E. & Faraone,S. V. Familial links between alterations in environmental and genetic rat models Biol.Psychiatry 76, 616628 (2014).
ADHD, conduct disorder and bipolar disorder. ofADHD: a pilot study. Am. J.Med. Genet. B 78. Hart,H., Radua,J., Nakao,T., Mataix-Cols,D.
Curr.Psychiatry Rep. 4, 146152 (2002). Neuropsychiatr. Genet. 147B, 15541563 (2008). & Rubia,K. Meta-analysis of functional magnetic
37. Cross-Disorder Group of the Psychiatric Genomics 58. Zhu,J. etal. Prenatal nicotine exposure mouse model resonance imaging studies of inhibition and
Consortium. Identification of risk loci with shared showing hyperactivity, reduced cingulate cortex attentioninattention-deficit/hyperactivity disorder:
effects on five major psychiatric disorders: a genome- volume, reduced dopamine turnover, and exploring task-specific, stimulant medication,
wide analysis. Lancet 381, 13711379 (2013). responsiveness to oral methylphenidate treatment. andageeffects. JAMA Psychiatry 70, 185198
38. Martin,J., Hamshere,M.L., Stergiakouli,E., J.Neurosci. 32, 94109418 (2012). (2013).
ODonovan,M.C. & Thapar,A. Genetic risk for 59. Sagvolden, T., Russell, V. A., Aase, H., Johansen, E. B. 79. Posner,J., Park,C. & Wang,Z. Connecting the dots:
attention-deficit/hyperactivity disorder contributes to &Farshbaf, M. Rodent models of attention-deficit/ a review of resting connectivity MRI studies in
neurodevelopmental traits in the general population. hyperactivity disorder. Biol. Psychiatry 57, attention-deficit/hyperactivity disorder.
Biol. Psychiatry 76, 664671 (2014). 12391247 (2005). Neuropsychol.Rev. 24, 315 (2014).
39. Hamshere,M.L. etal. High loading of polygenic risk 60. van der Meer,D. etal. The serotonin transporter 80. Castellanos,F.X. etal. Developmental trajectories
for ADHD in children with comorbid aggression. gene polymorphism 5HTTLPR moderates the effects ofbrain volume abnormalities in children and
Am.J.Psychiatry 170, 909916 (2013). of stress on attention-deficit/hyperactivity disorder. adolescents with attention-deficit/hyperactivity
40. Hamshere,M.L. etal. Shared polygenic contribution J.Child Psychol. Psychiatry 55, 13631371 (2014). disorder. JAMA 288, 17401748 (2002).
between childhood attention-deficit hyperactivity 61. Mill,J. & Petronis,A. Pre- and peri-natal 81. Durston,S. etal. Magnetic resonance imaging of boys
disorder and adult schizophrenia. Br. J.Psychiatry environmental risks for attention-deficit hyperactivity with attention-deficit/hyperactivity disorder and their
203, 107111 (2013). disorder (ADHD): the potential role of epigenetic unaffected siblings. J.Am. Acad. Child Adolesc.
41. Elia,J. etal. Rare structural variants found in processes in mediating susceptibility. J.Child Psychol. Psychiatry 43, 332340 (2004).
attention-deficit hyperactivity disorder are Psychiatry 49, 82. Greven,C.U. etal. Developmentally stable whole
preferentially associated with neurodevelopmental 10201030 (2008). brain volume reductions and developmentally
genes. Mol. Psychiatry 15, 637646 (2010). 62. Willcutt,E.G., Doyle,A.E., Nigg,J.T., Faraone,S.V. sensitive caudate and putamen volume alterations
42. Williams,N.M. etal. Rare chromosomal deletions and &Pennington,B.F. Validity of the executive function inparticipants with attention-deficit/hyperactivity
duplications in attention-deficit hyperactivity disorder: theory of attention-deficit/hyperactivity disorder: disorder and their unaffected siblings.
a genome-wide analysis. Lancet 376, 14011408 ameta-analytic review. Biol. Psychiatry 57, JAMAPsychiatry 72, 490499 (2015).
(2010). 13361346 (2005). 83. Hoogman,M. etal. Current self-reported symptoms
43. Williams,N.M. etal. Genome-wide analysis of copy 63. Sergeant,J.A. Modeling attention-deficit/ of attention deficit/hyperactivity disorder are
number variants in attention deficit/hyperactivity hyperactivity disorder: a critical appraisal of the associated with total brain volume in healthy adults.
disorder confirms the role of rare variants and cognitive-energetic model. Biol. Psychiatry 57, PLoS ONE 7, e31273 (2012).
implicates duplications at 15q13.3. Am. J.Psychiatry 12481255 (2005). 84. Stoodley,C.J. & Schmahmann,J.D. Functional
169, 195204 (2012). 64. Sonuga-Barke,E.J. & Fairchild,G. Neuroeconomics topography in the human cerebellum: a meta-analysis
44. Elia,J. etal. Genome-wide copy number variation ofattention-deficit/hyperactivity disorder: differential of neuroimaging studies. Neuroimage 44, 489501
study associates metabotropic glutamate receptor influences of medial, dorsal, and ventral prefrontal (2009).
gene networks with attention deficit hyperactivity brain networks on suboptimal decision making? 85. Frodl,T. & Skokauskas,N. Meta-analysis of structural
disorder. Nat. Genet. 44, 7884 (2011). Biol.Psychiatry 72, 126133 (2012). MRI studies in children and adults with attention
45. Lesch,K.P. etal. Genome-wide copy number variation 65. Luman,M., Tripp,G. & Scheres,A. Identifying the deficit hyperactivity disorder indicates treatment
analysis in attention-deficit/hyperactivity disorder: neurobiology of altered reinforcement sensitivity effects. ActaPsychiatr. Scand. 125, 114126
association with neuropeptide Y gene dosage in an inADHD: a review and research agenda. (2012).
extended pedigree. Mol. Psychiatry 16, 491503 Neurosci.Biobehav. Rev. 34, 744754 (2010). 86. van Ewijk,H., Heslenfeld,D.J., Zwiers,M.P.,
(2011). 66. Scheres,A., Lee,A. & Sumiya,M. Temporal reward Buitelaar,J.K. & Oosterlaan,J. Diffusion tensor
46. Neale,B.M. etal. Meta-analysis of genome-wide discounting and ADHD: task and symptom specific imaging in attention deficit/hyperactivity disorder:
association studies of attention-deficit/hyperactivity effects. J.Neural Transm. 115, 221226 (2008). a systematic review and meta-analysis.
disorder. J.Am. Acad. Child Adolesc. Psychiatry 49, 67. Toplak,M.E. & Tannock,R. Time perception: modality Neurosci.Biobehav. Rev. 36, 10931106 (2012).
884897 (2010). and duration effects in attention-deficit/hyperactivity 87. Shaw,P. etal. Mapping the development of the basal
47. Gizer,I.R., Ficks,C. & Waldman,I.D. Candidate gene disorder (ADHD). J.Abnorm. Child Psychol. 33, ganglia in children with attention-deficit/hyperactivity
studies of ADHD: a meta-analytic review. Hum. Genet. 639654 (2005). disorder. J.Am. Acad. Child Adolesc. Psychiatry 53,
126, 5190 (2009). 68. Tomblin,J.B. & Mueller,K.L. How can the 780789.e11 (2014).
48. Franke,B. etal. Multicenter analysis of the SLC6A3/ comorbidity with ADHD aid understanding of 88. Shaw,P. etal. Attention-deficit/hyperactivity disorder
DAT1 VNTR haplotype in persistent ADHD suggests language and speech disorders? Top. Lang. Disord. ischaracterized by a delay in cortical maturation.
differential involvement of the gene in childhood 32, 198206 (2012). Proc.Natl Acad. Sci. USA 104, 1964919654
andpersistent ADHD. Neuropsychopharmacology 35, 69. Kuntsi,J. & Klein,C. Intraindividual variability in (2007).
656664 (2010). ADHD and its implications for research of causal links. 89. Shaw,P. etal. Development of cortical surface area
49. Bralten,J. etal. Candidate genetic pathways for Curr.Top. Behav. Neurosci. 9, 6791 (2012). andgyrification in attention-deficit/hyperactivity
attention-deficit/hyperactivity disorder (ADHD) show 70. Fair,D.A., Bathula,D., Nikolas,M.A. & Nigg,J.T. disorder. Biol. Psychiatry 72, 191197 (2012).
association to hyperactive/impulsive symptoms Distinct neuropsychological subgroups in typically 90. Dreisbach,G. etal. Dopamine and cognitive control:
inchildren with ADHD. J.Am. Acad. Child Adolesc. developing youth inform heterogeneity in children the influence of spontaneous eyeblink rate and
Psychiatry 52, 12041212.e1 (2013). with ADHD. Proc. Natl Acad. Sci. USA 109, dopamine gene polymorphisms on perseveration
50. Poelmans,G., Pauls,D.L., Buitelaar,J.K. & Franke,B. 67696774 (2012). anddistractibility. Behav. Neurosci. 119, 483490
Integrated genome-wide association study findings: 71. Fliers,E.A. etal. Undertreatment of motor problems (2005).
identification of a neurodevelopmental network inchildren with ADHD. Child Adolesc. Ment. Health 91. Makris,N. etal. Cortical thinning of the attention and
forattention deficit hyperactivity disorder. 15, 8590 (2009). executive function networks in adults with attention-
Am.J.Psychiatry 168, 365377 (2011). 72. Coghill,D.R., Seth,S. & Matthews,K. deficit/hyperactivity disorder. Cereb. Cortex 17,
51. Skoglund,C., Chen,Q., DOnofrio,B.M., A comprehensive assessment of memory, delay 13641375 (2007).
Lichtenstein,P. & Larsson,H. Familial confounding aversion, timing, inhibition, decision making and 92. Clerkin,S.M. etal. Thalamocortical activation and
ofthe association between maternal smoking during variability in attention deficit hyperactivity disorder: connectivity during response preparation in adults
pregnancy and ADHD in offspring. J.Child Psychol. advancing beyond the three-pathway models. withpersistent and remitted ADHD. Am. J.Psychiatry
Psychiatry 55, 6168 (2014). Psychol.Med. 44, 19892001 (2014). 170, 10111019 (2013).
52. Milberger,S., Biederman,J., Faraone,S. V., Chen,L. 73. Sonuga-Barke,E., Bitsakou,P. & Thompson,M. 93. Mattfeld,A.T. etal. Brain differences between
&Jones,J. Is maternal smoking during pregnancy Beyond the dual pathway model: evidence for the persistent and remitted attention deficit
arisk factor for attention deficit hyperactivity disorder dissociation of timing, inhibitory, and delay-related hyperactivitydisorder. Brain 137, 24232428
inchildren? Am. J.Psychiatry 153, 11381142 impairments inattention-deficit/hyperactivity (2014).
(1996). disorder. J.Am. Acad. Child Adolesc. Psychiatry 49, 94. Francx,W. etal. White matter microstructure
53. Harold,G.T. etal. Biological and rearing mother 345355 (2010). anddevelopmental improvement of hyperactive/
influences on child ADHD symptoms: revisiting the 74. Cortese,S. etal. Toward systems neuroscience impulsivesymptoms in attention-deficit/
developmental interface between nature and nurture. ofADHD: a meta-analysis of 55 fMRI studies. hyperactivitydisorder. J.Child Psychol. Psychiatry
J.Child Psychol. Psychiatry 54, 10381046 (2013). Am.J.Psychiatry 169, 10381055 (2012). http://dx.doi.org/10.1111/jcpp.12379 (2015).
NATURE REVIEWS | DISEASE PRIMERS VOLUME 1 | 2015 | 19
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
95. Shaw,P. etal. Trajectories of cerebral cortical criteria for ADHD (for example, age of onset, 133. Antshel,K.M., Zhang-James,Y. & Faraone,S.V.
development in childhood and adolescence and symptoms causing impairment in at least two Thecomorbidity of ADHD and autism spectrum
adultattention-deficit/hyperactivity disorder. settings and reduction in the number of symptoms disorder. Expert Rev. Neurother. 13, 11171128
Biol.Psychiatry 74, 599606 (2013). required for individuals 17years of age) alter the (2013).
This paper provides an excellent example of the prevalence estimates of ADHD in a 134. Wilens,T.E. etal. Does ADHD predict substance-use
type of longitudinal neuroimaging we can expect community-based sample of school-aged children. disorders? A 10year followup study of young adults
inthe future. Participants were evaluated for 112. Valo,S. & Tannock,R. Diagnostic instability of DSMIV with ADHD. J.Am. Acad. Child Adolesc. Psychiatry
persistence or remission of ADHD symptoms in ADHD subtypes: effects of informant source, 50, 543553 (2011).
adulthood. Cortical thinning, especially in the instrumentation, and methods for combining symptom 135. Bernardi,S. etal. The lifetime impact of attention
prefrontal cortex, was associated with persistence reports. J.Clin. Child Adolesc. Psychol. 39, 749760 deficit hyperactivity disorder: results from the National
of ADHD symptoms into adulthood. As such, this (2010). Epidemiologic Survey on Alcohol and Related
paper shows the power of longitudinal research in 113. Feldman,H.M. & Reiff,M.I. Clinical practice. Conditions (NESARC). Psychol. Med. 42, 875887
ADHD to identify the correlates of persistence, Attention deficit-hyperactivity disorder in children and (2012).
which may provide predictive biomarkers for adolescents. N.Engl. J.Med. 370, 838846 (2014). 136. Nigg,J.T., Willcutt,E.G., Doyle,A.E. &
disease outcome. 114. Becker,A., Rothenberger,A. & Sohn,A. Six years Sonuga-Barke,E. J. Causal heterogeneity in ADHD:
96. Almeida,L.G. etal. Reduced right frontal cortical ahead: a longitudinal analysis regarding course dowe need neuropsychological subtypes?
thickness in children, adolescents and adults with andpredictive value of the Strengths and Difficulties Biol.Psychiatry 57, 12241230 (2005).
ADHD and its correlation to clinical variables: a cross- Questionnaire (SDQ) in children and adolescents. 137. Sjowall,D., Roth,L., Lindqvist,S. & Thorell,L.B.
sectional study. J.Psychiatr. Res. 44, 12141223 Eur.Child Adolesc. Psychiatry 24, 715725 (2015). Multiple deficits in ADHD: executive dysfunction, delay
(2010). 115. Halperin,J.M., Berwid,O.G. & ONeill,S. Healthy aversion, reaction time variability, and emotional
97. Almeida Montes,L.G. etal. Brain cortical thickness body, healthy mind? The effectiveness of physical deficits. J.Child Psychol. Psychiatry 54, 619627
inADHD: age, sex, and clinical correlations. J.Atten. activity to treat ADHD in children. Child Adolesc. (2013).
Disord. 17, 641654 (2013). Psychiatr. Clin. N.Am. 23, 899936 (2014). 138. Cortese,S. etal. Cognitive training for attention-
98. Faraone,S.V. & Biederman,J. Neurobiology of 116. Plueck,J. etal. Effectiveness of a teacher-based deficit/hyperactivity disorder: meta-analysis of clinical
attention-deficit hyperactivity disorder. indicated prevention program for preschool children and neuropsychological outcomes from randomized
Biol.Psychiatry 44, 951958 (1998). with externalizing problem behavior. Prev. Sci. 16, controlled trials. J.Am. Acad. Child Adolesc.
99. Makris,N., Biederman,J., Monuteaux,M.C. 233241 (2015). Psychiatry 54, 164174 (2015).
&Seidman,L.J. Towards conceptualizing a neural 117. Biederman,J. etal. Gender effects of attention 139. Nussey,C., Pistrang,N. & Murphy,T. How does
systems-based anatomy of attention-deficit/ deficithyperactivity disorder in adults, revisited. psychoeducation help? A review of the effects of
hyperactivity disorder. Dev. Neurosci. 31, 3649 Biol.Psychiatry 55, 692700 (2004). providing information about Tourette syndrome and
(2009). 118. Faraone,S.V. etal. Attention deficit hyperactivity attention-deficit/hyperactivity disorder. Child Care
100. Sonuga-Barke,E.J. Causal models of attention-deficit/ disorder in adults: an overview. Biol. Psychiatry 48, Health Dev. 39, 617627 (2013).
hyperactivity disorder: from common simple deficits 920 (2000). 140. Fiks,A.G., Mayne,S., Debartolo,E., Power,T.J.
tomultiple developmental pathways. Biol. Psychiatry 119. Kooij,S.J. etal. European consensus statement &Guevara,J.P. Parental preferences and goals
57, 12311238 (2005). ondiagnosis and treatment of adult ADHD: regarding ADHD treatment. Pediatrics 132, 692702
101. Castellanos,F.X. & Tannock,R. Neuroscience of TheEuropean Network Adult ADHD. BMC Psychiatry (2013).
attention-deficit/hyperactivity disorder: the search for 10, 67 (2010). 141. Atkinson,M. & Hollis,C. NICE guideline: attention
endophenotypes. Nat. Rev. Neurosci. 3, 617628 This article was the first European consensus deficit hyperactivity disorder. Arch. Dis. Child Educ.
(2002). aboutADHD in adults. It provides an excellent Pract. Ed. 95, 2427 (2010).
102. Kuntsi,J. etal. Separation of cognitive impairments review of the neurobiology, diagnosis and 142. Faraone,S.V. & Glatt,S.J. A comparison of the
inattention-deficit/hyperactivity disorder into 2 treatment of adults with ADHD. efficacy of medications for adult attention-deficit/
familial factors. Arch. Gen. Psychiatry 67, 11591167 120. The Express Scripts Lab. Turning attention to ADHD. hyperactivity disorder using meta-analysis of effect
(2010). An Express Scripts Report. U. S. Medication Trends sizes. J.Clin. Psychiatry 71, 754763 (2010).
103. Biederman,J. etal. Deficient emotional self-regulation forAttention Deficit Hyperactivity Disorder. The Lab This study is among the most comprehensive
and pediatric attention deficit hyperactivity disorder: Express Scripts [online], http://lab.express-scripts. meta-analytic efforts in reviewing the efficacy
a family risk analysis. Psychol. Med. 42, 639646 com/insights/industry-updates/report-turning- ofstimulants and non-stimulants in adults
(2012). attention-to-adhd (2014). withADHD.
104. Epstein,J.N. & Weiss,M.D. Assessing treatment 121. Barkley,R. A., Murphy,K. R. & Fischer,M. ADHD in 143. Faraone,S.V. & Buitelaar,J. Comparing the efficacy of
outcomes in attention-deficit/hyperactivity disorder: Adults: What the Science Says (Guildford, 2007). stimulants for ADHD in children and adolescents using
a narrative review. Prim. Care Companion CNS Disord. 122. Epstein,J.N. & Kollins,S.H. Psychometric properties meta-analysis. Eur. Child Adolesc. Psychiatry 19,
14, PCC.11r01336 (2012). of an adult ADHD diagnostic interview. J.Atten. 353364 (2010).
105. Seixas,M., Weiss,M. & Muller,U. Systematic review Disord. 9, 504514 (2006). 144. Wolraich,M. etal. ADHD: clinical practice guideline
ofnational and international guidelines on attention- 123. Adler,L.A. etal. Validity of pilot adult ADHD Self- forthe diagnosis, evaluation, and treatment of
deficit hyperactivity disorder. J.Psychopharmacol. 26, Report Scale (ASRS) to rate adult ADHD symptoms. attention-deficit/hyperactivity disorder in children
753765 (2012). Ann. Clin. Psychiatry 18, 145148 (2006). andadolescents. Pediatrics 128, 10071022 (2011).
106. Miller,T.W., Nigg,J.T. & Miller,R.L. Attention deficit 124. Antshel,K.M. etal. Is adult attention deficit 145. Faraone,S.V., Biederman,J., Spencer,T.J. &
hyperactivity disorder in African American children: hyperactivity disorder a valid diagnosis in the Aleardi,M. Comparing the efficacy of medications
what can be concluded from the past ten years? presence of high IQ? Psychol. Med. 39, 13251335 forADHD using meta-analysis. MedGenMed. 8, 4
Clin.Psychol. Rev. 29, 7786 (2009). (2009). (2006).
107. Klimkeit,E. etal. Children should be seen and heard: 125. Barkley,R.A. Deficient emotional self-regulation: 146. Fredriksen,M., Halmoy,A., Faraone,S.V. & Haavik,J.
self-report of feelings and behaviors in primary-school- a core component of attention-deficit/hyperactivity Long-term efficacy and safety of treatment with
age children with ADHD. J.Atten. Disord. 10, disorder. J.ADHD Related Disord. 1, 537 (2010). stimulants and atomoxetine in adult ADHD:
181191 (2006). 126. Biederman,J. etal. Stability of executive function a review ofcontrolled and naturalistic studies.
108. Biederman,J., Keenan,K. & Faraone,S.V. Parent deficits into young adult years: a prospective Eur.Neuropsychopharmacol. 23, 508527 (2013).
based diagnosis of attention deficit disorder predicts longitudinal followup study of grown up males with 147. Shaw, M. etal. A systematic review and analysis of
adiagnosis based on teacher report. J.Am. Acad. ADHD. Acta Psychiatr. Scand. 116, 129136 (2007). long-term outcomes in attention deficit hyperactivity
Child Adolesc. Psychiatry 29, 698701 (1990). 127. Sonuga-Barke,E.J. & Taylor,E. in Rutters Child & disorder: effects of treatment and non-treatment.
109. Biederman,J., Faraone,S. V., Monuteaux,M. & Adolescent Psychiatry (eds Thapar,A. etal.) BMCMed. 10, 99 (2012).
Grossbard,J. How informative are parent reports 738756 (Wiley Blackwell, 2015). 148. Langberg,J.M. & Becker,S.P. Does long-term
ofADHD symptoms for assessing outcome in clinical 128. Nigg,J.T., Tannock,R. & Rohde,L.A. What is to be medication use improve the academic outcomes of
trials of long-acting treatments? A pooled analysis the fate of ADHD subtypes? An introduction to the youth with attention-deficit/hyperactivity disorder?
ofparents and teachers reports. Pediatrics 113, special section on research on the ADHD subtypes Clin. Child Fam. Psychol. Rev. 15, 215233 (2012).
16671671 (2004). and implications for the DSMV. J.Clin. Child Adolesc. 149. van de Loo-Neus,G.H., Rommelse,N. &
110. Sayal,K. & Goodman,R. Do parental reports of child Psychol. 39, 723725 (2010). Buitelaar,J.K. To stop or not to stop? How long
hyperkinetic disorder symptoms at school predict 129. Staller,J. & Faraone,S.V. Attention-deficit should medication treatment of attention-deficit
teacher ratings? Eur. Child Adolesc. Psychiatry 18, hyperactivity disorder in girls: epidemiology and hyperactivity disorder be extended?
336344 (2009). management. CNS Drugs 20, 107123 (2006). Eur.Neuropsychopharmacol. 21, 584599 (2011).
This large-scale epidemiological study of 130. Pingault,J.B. etal. Childhood trajectories of 150. MTA Cooperative Group. National Institute of Mental
516years olds in the United Kingdom provides inattention and hyperactivity and prediction of Health Multimodal Treatment Study of ADHD
empirical evidence that parental reports about educational attainment in early adulthood: a 16year followup: 24month outcomes of treatment strategies
ADHD symptoms at school have limited use in longitudinal population-based study. Am. J.Psychiatry for attention-deficit/hyperactivity disorder. Pediatrics
predicting teacher ratings, thereby highlighting the 168, 11641170 (2011). 113, 754761 (2004).
importance of obtaining information directly from 131. Biederman,J., Newcorn,J. & Sprich,S. Comorbidity 151. Rostain,A., Jensen,P.S., Connor,D.F., Miesle,L.M.
teachers for the diagnosis of ADHD in childhood. ofattention deficit hyperactivity disorder with conduct, &Faraone,S.V. Toward quality care in ADHD: defining
111. McKeown,R.E. etal. The impact of case definition on depressive, anxiety, and other disorders. the goals of treatment. J.Atten Disord. 19, 99117
attention-deficit/hyperactivity disorder prevalence Am.J.Psychiatry 148, 564577 (1991). (2015).
estimates in community-based samples of school-aged 132. Cortese,S., Faraone,S.V., Konofal,E. & 152. Ermer,J. etal. Lisdexamfetamine dimesylate: linear
children. J.Am. Acad. Child Adolesc. Psychiatry 54, Lecendreux,M. Sleep in children with attention- dose-proportionality, low intersubject and intrasubject
5361 (2015). deficit/hyperactivity disorder: meta-analysis of variability, and safety in an open-label single-dose
This large-scale USbased study demonstrates how subjective andobjective studies. J.Am. Acad. Child pharmacokinetic study in healthy adult volunteers.
case definition and inclusion of changes in DSM5 Adolesc. Psychiatry 48, 894908 (2009). J.Clin. Pharmacol. 50, 10011010 (2010).
20 | 2015 | VOLUME 1 www.nature.com/nrdp
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
153. Bendz,L.M. & Scates,A.C. Melatonin treatment trend in pediatric psychopharmacology. hyperactivity disorder. J.Clin. Child Adolesc. Psychol.
forinsomnia in pediatric patients with attention- J.Am.Acad.Child Adolesc. Psychiatry 34, 110112 40, 519531 (2011).
deficit/hyperactivity disorder. Ann. Pharmacother. 44, (1995). 190. Ghuman,J.K. & Ghuman,H.S. Pharmacologic
185191 (2009). 171. Schoenfelder,E.N., Faraone,S.V. & Kollins,S.H. intervention for attention-deficit hyperactivity disorder
154. Cortese,S. etal. Practitioner review: current best Stimulant treatment of ADHD and cigarette smoking: in preschoolers: is it justified? Paediatr. Drugs 15,
practice in the management of adverse events during ameta-analysis. Pediatrics 133, 10701080 (2014). 18 (2013).
treatment with ADHD medications in children 172. Biederman,J. etal. Stimulant therapy and risk for 191. Sonuga-Barke,E.J. etal. Nonpharmacological
andadolescents. J.Child Psychol. Psychiatry 54, subsequent substance use disorders in male adults interventions for ADHD: systematic review and meta-
227246 (2013). with ADHD: a naturalistic controlled 10year followup analyses of randomized controlled trials of dietary
155. Maldonado,R. Comparison of the pharmacokinetics study. Am. J.Psychiatry 165, 597603 (2008). andpsychological treatments. Am. J.Psychiatry 170,
and clinical efficacy of new extended-release This study is among the largest longitudinal studies 275289 (2013).
formulations of methylphenidate. Expert Opin. Drug documenting the absence of increased risk of This comprehensive article uses meta-analysis
Metab. Toxicol. 9, 10011014 (2013). substance use disorders associated with stimulants todocument the relative efficacy of non-
156. Kimko,H. etal. Population pharmacodynamic in ADHD. pharmacological interventions for ADHD. It shows
modeling of various extended-release formulations 173. Faraone,S.V. & Wilens,T. Does stimulant treatment that efficacy measures from poorly blinded studies
ofmethylphenidate in children with attention deficit lead to substance use disorders? J.Clin. Psychiatry markedly overestimate the efficacy of treatments.
hyperactivity disorder via meta-analysis. 64, 913 (2003). 192. Faraone,S.V. & Antshel,K.M. Towards an evidence-
J.Pharmacokinet. Pharmacodyn. 39, 161176 174. Groenman,A.P. etal. Stimulant treatment for ADHD based taxonomy of nonpharmacologic treatments
(2012). reduces risk for developing substance use disorder. forADHD. Child Adolesc. Psychiatr. Clin. N.Am. 23,
157. Wilens,T.E. ADHD: Prevalence, diagnosis, and issues Br.J.Psychiatry 203, 112119 (2013). 965972 (2014).
of comorbidity. CNS Spectr. 12 (Suppl. 6), 15 175. Chang,Z. etal. Stimulant ADHD medication and risk 193. Stevenson,J. etal. Research review: the role of diet
(2007). for substance abuse. J.Child Psychol. Psychiatry 55, inthe treatment of attention-deficit/hyperactivity
158. Faraone,S.V., Biederman,J., Morley,C.P. 878885 (2014). disorder an appraisal of the evidence on efficacy
&Spencer,T.J. Effect of stimulants on height and 176. Wilens,T. etal. Misuse and diversion of stimulants and recommendations on the design of future studies.
weight: a review of the literature. J.Am. Acad. Child prescribed for ADHD: a systematic review of the J.Child Psychol. Psychiatry 55, 416427 (2014).
Adolesc. Psychiatry 47, 9941009 (2008). literature. J.Am. Acad. Child Adolesc. Psychiatry 47, 194. Nigg,J.T. & Holton,K. Restriction and elimination
159. Dalsgaard,S., Kvist,A.P., Leckman,J.F., 2131 (2008). diets in ADHD treatment. Child Adolesc. Psychiatr.
Nielsen,H.S. & Simonsen,M. Cardiovascular safety 177. Bangs,M.E. etal. Efficacy and safety of atomoxetine Clin. N.Am. 23, 937953 (2014).
ofstimulants inchildren with attention-deficit/ in adolescents with attention-deficit/hyperactivity 195. Pfiffner,L.J. & Haack,L.M. Behavior management
hyperactivity disorder: a nationwide prospective disorder and major depression. J.Child Adolesc. forschool-aged children with ADHD. Child Adolesc.
cohort study. J.Child Adolesc. Psychopharmacol. 24, Psychopharmacol. 17, 407420 (2007). Psychiatr. Clin. N.Am. 23, 731746 (2014).
302310 (2014). 178. Kratochvil,C.J. etal. Atomoxetine alone or combined 196. Wells,K.C. etal. Parenting and family stress
160. Cooper,W.O. etal. ADHD drugs and serious with fluoxetine for treating ADHD with comorbid treatment outcomes in attention deficit hyperactivity
cardiovascular events in children and young adults. depressive or anxiety symptoms. J.Am. Acad. Child disorder (ADHD): an empirical analysis in the MTA
N.Engl. J.Med. 365, 18961904 (2011). Adolesc. Psychiatry 44, 915924 (2005). study. J.Abnorm. Child Psychol. 28, 543553
This article is among the more-informative studies This study is among the first to document the use (2000).
documenting the cardiac safety of stimulants. ofatomoxetine in the management of children with 197. Evans,S.W., Langberg,J.M., Egan,T. & Molitor,S.J.
161. Mazza,M. etal. Drugs for attention deficit- ADHD and co-morbid anxiety. Middle school-based and high school-based
hyperactivity disorder do not increase the mid-term 179. Rizzo,R., Gulisano,M., Cali,P.V. & Curatolo,P. interventions for adolescents with ADHD.
risk of sudden death in children: a meta-analysis of Tourette syndrome and comorbid ADHD: current ChildAdolesc. Psychiatr. Clin. N.Am. 23, 699715
observational studies. Int. J.Cardiol. 168, pharmacological treatment options. Eur. J.Paediatr. (2014).
43204321 (2013). Neurol. 17, 421428 (2013). 198. Faraone,S.V. & Antshel,K.M. ADHD: non-
162. American Academy of Pediatrics/American Heart 180. Maneeton,N., Maneeton,B., Srisurapanont,M. pharmacologic interventions. Child Adolesc. Psychiatr.
Association. American Academy of Pediatrics/ &Martin,S.D. Bupropion for adults with attention- Clin. N.Am. 23, xiiixiv (2014).
American Heart Association clarification of statement deficit hyperactivity disorder: meta-analysis of This issue reviews the clinical methodology
on cardiovascular evaluation and monitoring of randomized, placebo-controlled trials. Psychiatry Clin. anddata that support efficacy for the following
children and adolescents with heart disease receiving Neurosci. 65, 611617 (2011). non-pharmacological interventions for ADHD:
medications for ADHD: May 16, 2008. J.Dev. Behav. 181. Connor,D.F., Glatt,S.J., Lopez,I.D., Jackson,D. cognitivebehavioural therapy, family therapy,
Pediatr. 29, 335 (2008). & Melloni,R.H.Jr. Psychopharmacology and psychotherapy, social skills training, behavioural
163. Warren,A.E. etal. Cardiac risk assessment before aggression. I: a meta-analysis of stimulant effects on management, working memory training,
theuse of stimulant medications in children and overt/covert aggression-related behaviors in ADHD. neurofeedback, lifestyle interventions, traditional
youth: a joint position statement by the Canadian J.Am. Acad. Child Adolesc. Psychiatry 41, 253261 Chinese medicine, restriction and food colour
Paediatric Society, the Canadian Cardiovascular (2002). exclusion diets and herbal and nutritionalproducts.
Society, and the Canadian Academy of Child and 182. Connor,D.F. etal. Effects of guanfacine extended 199. Daley,D. etal. Behavioral interventions in attention-
Adolescent Psychiatry. Can. J.Cardiol. 25, 625630 release on oppositional symptoms in children aged deficit/hyperactivity disorder: a meta-analysis of
(2009). 612years with attention-deficit hyperactivity randomized controlled trials across multiple outcome
164. Tanaka,Y., Rohde,L.A., Jin,L., Feldman,P.D. disorder and oppositional symptoms: a randomized, domains. J.Am. Acad. Child Adolesc. Psychiatry 53,
&Upadhyaya,H.P. A meta-analysis of the consistency double-blind, placebo-controlled trial. CNS Drugs 24, 835847.e5 (2014).
of atomoxetine treatment effects in pediatric patients 755768 (2010). 200. Mikami,A.Y., Jia,M. & Na,J.J. Social skills training.
with attention-deficit/hyperactivity disorder from 183. Newcorn,J.H., Spencer,T.J., Biederman,J., Child Adolesc. Psychiatr. Clin. N.Am. 23, 775788
15clinical trials across four geographic regions. Milton,D.R. & Michelson,D. Atomoxetine treatment (2014).
J.Child Adolesc. Psychopharmacol. 23, 262270 in children and adolescents with attention-deficit/ 201. Abikoff,H. etal. Remediating organizational
(2013). hyperactivity disorder and comorbid oppositional functioning in children with ADHD: immediate and
165. Jain,R., Segal,S., Kollins,S.H. & Khayrallah,M. defiant disorder. J.Am. Acad. Child Adolesc. longterm effects from a randomized controlled trial.
Clonidine extended-release tablets for pediatric Psychiatry 44, 240248 (2005). J.Consult. Clin. Psychol. 81, 113128 (2013).
patients with attention-deficit/hyperactivity disorder. 184. Simonoff,E. etal. Randomized controlled double-blind 202. DuPaul,G.J., Gormley,M.J. & Laracy,S.D.
J.Am. Acad. Child Adolesc. Psychiatry 50, 171179 trial of optimal dose methylphenidate in children and Schoolbased interventions for elementary school
(2011). adolescents with severe attention deficit hyperactivity students with ADHD. Child Adolesc. Psychiatr. Clin.
166. Biederman,J. etal. Long-term, open-label extension disorder and intellectual disability. J.Child Psychol. N.Am. 23, 687697 (2014).
study of guanfacine extended release in children and Psychiatry 54, 527535 (2013). 203. Antshel,K.M. & Olszewski,A.K. Cognitive behavioral
adolescents with ADHD. CNS Spectr. 13, 10471055 185. Levin,H. etal. Symptoms of attention-deficit/ therapy for adolescents with ADHD. Child Adolesc.
(2008). hyperactivity disorder following traumatic brain injury Psychiatr. Clin. N.Am. 23, 825842 (2014).
167. Faraone,S.V., McBurnett,K., Sallee,F.R., Steeber,J. in children. J.Dev. Behav. Pediatr. 28, 108118 204. Safren,S.A. Cognitivebehavioral approaches to
& Lopez,F.A. Guanfacine extended release: a novel (2007). ADHD treatment in adulthood. J.Clin. Psychiatry
treatment for attention-deficit/hyperactivity disorder 186. Shaywitz,B.A., Williams,D.W., Fox,B.K. 67(Suppl. 8), 4650 (2006).
inchildren and adolescents. Clin. Ther. 35, &Wietecha,L.A. Reading outcomes of children 205. Knouse,L.E. & Safren,S.A. Current status of
17781793 (2013). andadolescents with attention-deficit/hyperactivity cognitive behavioral therapy for adult attention-deficit
168. Treuer,T. etal. A systematic review of combination disorder and dyslexia following atomoxetine hyperactivity disorder. Psychiatr. Clin. North Am. 33,
therapy with stimulants and atomoxetine for attention- treatment. J.Child Adolesc. Psychopharmacol. 24, 497509 (2010).
deficit/hyperactivity disorder, including patient 419425 (2014). 206. Seidman,L.J. Neuropsychologically informed
characteristics, treatment strategies, effectiveness, 187. Biederman,J. etal. Effects of stimulant medication strategic psychotherapy in teenagers and adults with
andtolerability. J.Child Adolesc. Psychopharmacol. onneuropsychological functioning in young adults ADHD. Child Adolesc. Psychiatr. Clin. N.Am. 23,
23, 179193 (2013). withattention-deficit/hyperactivity disorder. J.Clin. 843852 (2014).
169. Maneeton,N., Maneeton,B., Intaprasert,S. & Psychiatry 69, 11501156 (2008). 207. Robin,A.L. Family therapy for adolescents with
Woottiluk,P. A systematic review of randomized 188. Faraone,S. V. etal. Atomoxetine and Stroop task ADHD. Child Adolesc. Psychiatr. Clin. N.Am. 23,
controlled trials of bupropion versus methylphenidate performance in adult attention-deficit/hyperactivity 747756 (2014).
in the treatment of attention-deficit/hyperactivity disorder. J.Child Adolesc. Psychopharmacol. 15, 208. Arns,M., de Ridder,S., Strehl,U., Breteler,M.
disorder. Neuropsychiatr. Dis. Treat. 10, 14391449 664670 (2005). &Coenen,A. Efficacy of neurofeedback treatment
(2014). 189. Langberg,J.M. etal. Patterns and predictors of inADHD: the effects on inattention, impulsivity and
170. Wilens,T.E., Spencer,T., Biederman,J., Wozniak,J. & adolescent academic achievement and performance hyperactivity: a meta-analysis. Clin. EEG Neurosci. 40,
Connor,D. Combined pharmacotherapy: an emerging ina sample of children with attention-deficit/ 180189 (2009).
NATURE REVIEWS | DISEASE PRIMERS VOLUME 1 | 2015 | 21
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
209. Holtmann,M., Sonuga-Barke,E., Cortese,S. ADHD across seven countries: a qualitative study. 248. Edden,R.A., Crocetti,D., Zhu,H., Gilbert,D.L.
&Brandeis,D. Neurofeedback for ADHD: a review Health Qual. Life Outcomes 10, 47 (2012). &Mostofsky,S.H. Reduced GABA concentration
ofcurrent evidence. Child Adolesc. Psychiatr. Clin. 229. Caci,H. etal. Daily life impairments associated with inattention-deficit/hyperactivity disorder. Arch. Gen.
N.Am. 23, 789806 (2014). childhood/adolescent attention-deficit/hyperactivity Psychiatry 69, 750753 (2012).
210. Sonuga-Barke,E., Brandeis,D., Holtmann,M. disorder as recalled by adults: results from the 249. Oades,R.D., Slusarek,M., Velling,S. & Bondy,B.
&Cortese,S. Computer-based cognitive training European Lifetime Impairment Survey. CNS Spectr. Serotonin platelet-transporter measures in childhood
forADHD: a review of current evidence. Child 20, 112121 (2015). attention-deficit/hyperactivity disorder (ADHD):
Adolesc. Psychiatr. Clin. N.Am. 23, 807824 230. Coghill,D. The impact of medications on quality of life clinical versus experimental measures of impulsivity.
(2014). in attention-deficit hyperactivity disorder: WorldJ.Biol. Psychiatry 3, 96100 (2002).
211. Klingberg,T. etal. Computerized training of working asystematic review. CNS Drugs 24, 843866 (2010). 250. Faraone,S.V. & Zhang-James,Y. Can sodium/
memory in children with ADHD a randomized, 231. Barbaresi,W.J., Katusic,S.K., Colligan,R.C., hydrogen exchange inhibitors be repositioned for
controlled trial. J.Am. Acad. Child Adolesc. Weaver,A.L. & Jacobsen,S.J. Modifiers of long-term treating attention deficit hyperactivity disorder?
Psychiatry 44, 177186 (2005). school outcomes for children with attention-deficit/ An insilico approach. Am. J.Med. Genet. B
212. Bogels,S.M., de Bruin,E.L. & van der Oord,S. hyperactivity disorder: does treatment with stimulant Neuropsychiatr. Genet. 162B, 711717 (2013).
inCognitive Behaviour Therapy for Children and medication make a difference? Results from a 251. Adler,L.D. & Nierenberg,A.A. Review of medication
Families 3rd edn (eds Graham, P. & Reynolds,S.) population-based study. J.Dev. Behav. Pediatr. 28, adherence in children and adults with ADHD.
371384 (Cambridge Univ. Press, 2013). 274287 (2007). Postgrad.Med. 122, 184191 (2010).
213. Groenman,A.P. etal. Substance use disorders 232. Ljung,T., Chen,Q., Lichtenstein,P. & Larsson,H. 252. Lurie,J.D. & Morgan,T.S. Pros and cons of
inadolescents with attention deficit hyperactivity Common etiological factors of attention-deficit/ pragmatic clinical trials. J.Comp. Eff. Res. 2, 5358
disorder: a 4year followup study. Addiction 108, hyperactivity disorder and suicidal behavior: (2013).
15031511 (2013). apopulation-based study in sweden. 253. Biederman,J., Petty,C.R., OConnor,K.B.,
214. Lichtenstein,P. etal. Medication for attention deficit- JAMAPsychiatry 71, 958964 (2014). Hyder,L.L. & Faraone,S.V. Predictors of persistence
hyperactivity disorder and criminality. N.Engl. 233. Man,K.K. etal. Methylphenidate and the risk of in girls with attention deficit hyperactivity disorder:
J.Med. 367, 20062014 (2012). trauma. Pediatrics 135, 4048 (2015). results from an11year controlled followup study.
This very large population study found an 234. Perwien,A.R. etal. Atomoxetine treatment in Acta Psychiatr. Scand. 125, 147156 (2012).
association of ADHD with criminal behaviour and children and adolescents with attention-deficit 254. Holmes,J. etal. The child attention-deficit
that medications for ADHD reduce such behaviour. hyperactivity disorder: what are the long-term health- hyperactivity disorder teacher telephone interview
215. Cortese,S., Faraone,S.V., Bernardi,S., Wang,S. related quality-oflife outcomes? J.Child Adolesc. (CHATTI): reliability and validity.Br. J.Psychiatry
&Blanco,C. Adult attention-deficit hyperactivity Psychopharmacol. 16, 713724 (2006). 184, 7478 (2004).
disorder and obesity: epidemiological study. 235. Hechtman,L. etal. Academic achievement and 255. Ward,M.F., Wender,P.H. & Reimherr,F.W. The
Br.J.Psychiatry 203, 2434 (2013). emotional status of children with ADHD treated Wender Utah Rating Scale: an aid in the retrospective
216. Biederman,J. & Faraone,S.V. The effects of withlong-term methylphenidate and multimodal diagnosis of childhood attention deficit hyperactivity
attention-deficit/hyperactivity disorder on psychosocial treatment. J.Am. Acad. Child Adolesc. disorder. Am. J.Psychiatry 150, 885890 (1993).
employment and household income. MedGenMed 8, Psychiatry 43, 812819 (2004).
12 (2006). 236. Banaschewski,T. etal. Health-related quality of life Acknowledgements
217. Chang,Z., Lichtenstein,P., DOnofrio,B.M., and functional outcomes from a randomized- The authors thank M. Mehta for help with incorporating the
Sjolander,A. & Larsson,H. Serious transport withdrawal study of long-term lisdexamfetamine default mode network into Figure 4.S.V.F. is supported by the
accidents in adults with attention-deficit/hyperactivity dimesylate treatment in children and adolescents with K.G. Jebsen Centre for Research on Neuropsychiatric
disorder and the effect of medication: a population- attention-deficit/hyperactivity disorder. CNS Drugs Disorders, University of Bergen, Bergen, Norway, the
based study. JAMA Psychiatry 71, 319325 (2014). 28, 11911203 (2014). European Commissions Seventh Framework programme
218. James,A., Lai,F.H. & Dahl,C. Attention deficit 237. Collins,P.Y. etal. Grand challenges in global mental (FP7/20072013) under grant agreement no. 602805 and
hyperactivity disorder and suicide: a review of health. Nature 475, 2730 (2011). National Institute of Mental Health (NIMH) grants
possible associations. Acta Psychiatr. Scand. 110, 238. Gelernter,J. Genetics of complex traits in psychiatry. R13MH059126 and R01MH094469. J.B. is supported by
408415 (2004). Biol. Psychiatry 77, 3642 (2015). grants from the Netherlands Organization for Health Research
219. Biederman,J. etal. Patterns of psychiatric 239. Sagvolden,T., Russell,V.A., Aase,H., Johansen,E.B. and Development (ZonMw 606060097193), the
comorbidity, cognition, and psychosocial functioning & Farshbaf,M. Rodent models of attention-deficit/ Netherlands Organization for Scientific Research (NWO;
inadults with attention deficit hyperactivity disorder. hyperactivity disorder. Biol. Psychiatry 57, grants 1750102007010, 43309242 and 05613015), and
Am. J.Psychiatry 150, 17921798 (1993). 12391247 (2005). by the European Commissions Seventh Framework
220. Barkley,R.A., Fischer,M., Smallish,L. & Fletcher,K. 240. Norton,W.H. Toward developmental models of programme (FP7/20072013) under grant agreement no.
Young adult outcome of hyperactive children: adaptive psychiatric disorders in zebrafish. Front. Neural 278948 (TACTICS), 602450 (IMAGEMEND), 602805
functioning in major life activities. J.Am. Acad. Child Circuits 7, 79 (2013). (AGGRESSOTYPE) and 603016 (MATRICS); and Horizon
Adolesc. Psychiatry 45, 192202 (2006). 241. van der Voet,M., Harich,B., Franke,B. & Schenck, A. 2020 research programme (grant agreement no. 643051
221. Biederman,J. etal. Young adult outcome of attention ADHD-associated dopamine transporter, latrophilin (MiND) and 642996 (BRAINVIEW)). His research also receives
deficit hyperactivity disorder: a controlled 10year and neurofibromin share a dopamine-related funding from the US NIH Consortium grant no. U54
followup study. Psychol. Med. 36, 167179 (2006). locomotor signature in Drosophila. Mol. EB020403, supported by a cross-NIH alliance that funds Big
222. Ramos Olazagasti,M.A. etal. Does childhood Psychiatryhttp://dx.doi.org/10.1038/mp.2015.55 Data to Knowledge Centers of Excellence. B.F. is supported by
attention-deficit/hyperactivity disorder predict risk- (2015). grants from NWO (grants no. 43309229 and 016130669),
taking and medical illnesses in adulthood? J.Am. This paper suggests that the fruitfly, Drosophila from the European Commissions Seventh Framework
Acad. Child Adolesc. Psychiatry 52, 153162.e4 melanogaster, can clarify biological pathways from programme (grant agreement no. 278948 (TACTICS),
(2013). gene to disease in ADHD. As this animal model 602450 (IMAGEMEND) and 602805 (Aggressotype)); and
223. Klein,R.G. etal. Clinical and functional outcome enables fast, cheap and scalable investigations of Horizon 2020 research programme (grant agreement no.
ofchildhood attention-deficit/hyperactivity disorder gene function at several levels from molecule to 643051 (MiND)). Her research also receives funding from the
33years later. Arch. Gen. Psychiatry 69, cell to behaviour, and is also amenable to drug NIH Consortium grant no. U54 EB020403, supported by a
12951303 (2012). testing, it may provide a powerful model for the cross-NIH alliance that funds Big Data to Knowledge Centers
224. Dalsgaard,S., Ostergaard,S.D., Leckman,J.F., evaluation of gene-to-disease pathways and new of Excellence. J.A.R.-Q. is supported by grants from and
Mortensen,P.B. & Pedersen,M.G. Mortality in candidate pharmacological treatments for ADHD. Departament de Salut, Government of Catalonia, Spain,
children, adolescents, and adults with attention deficit Such high-throughput models will be needed to Instituto de Salud Carlos III-FIS (PI12/01139), Plan Nacional
hyperactivity disorder: a nationwide cohort study. discover new treatments. Sobre Drogas (PNSD2011/0080) and the European
Lancet 385, 21902196 (2015). 242. Brennand,K.J. etal. Modelling schizophrenia using Commissions Seventh Framework programme. R.T. is
225. Danckaerts,M. etal. The quality of life of children human induced pluripotent stem cells. Nature 473, supported by grants from the Canadian Institutes for Health
with attention deficit/hyperactivity disorder: 221225 (2011). Research (CIHR #245899) and the Institute of Education
asystematic review. Eur. Child Adolesc. Psychiatry 243. Thompson,P.M. etal. The ENIGMA Consortium: Sciences (R305A120184). L.A.R. is supported by a grant
19, 83105 (2010). large-scale collaborative analyses of neuroimaging from the National Counsel of Technological and Scientific
This review of 36 studies found that ADHD is andgenetic data. Brain Imaging Behav. 8, 153182 Development CNPq (grant no. 304678/20104). E.J.S.S.B.
associated with lower HRQOL across a broad (2014). is supported by grants from the Economic Social Research
range of psychosocial, achievement and 244. Kooij,J.J. etal. Internal and external validity of Council (ES/I037970/1), Medical Research Council (MR/
self-evaluation domains. The effect of ADHD on attention-deficit hyperactivity disorder in a K022474/1), National Institute for Health Research (NIHR
HRQOL was similar to that of other mental health population-based sample of adults. Psychol. Med. PGfAR RPPG010810061), MQ Transforming Mental
conditions and severe physical disorders. Higher 35, 817827 (2005). Health (MQ14PP_83), European Commissions Seventh
numbers ofADHD symptoms and impairments 245. Sanislow,C.A. etal. Developing constructs for Framework programme (20072013) under grant agreement
predicted poorer HRQOL. psychopathology research: research domain criteria. no. 260576 and an unrestricted programme grant from Shire
226. Riley,A.W. etal. Factors related to health-related J.Abnorm. Psychol. 119, 631639 (2010). Pharmaceuticals.
quality of life (HRQoL) among children with ADHD 246. Thome,J. etal. Biomarkers for attention-deficit/
inEurope at entry into treatment. Eur. Child Adolesc. hyperactivity disorder (ADHD). A consensus report Author contributions
Psychiatry 15 (Suppl. 1), I38I45 (2006). ofthe WFSBP task force on biological markers and Introduction (S.V.F.); Epidemiology (L.A.R.); Mechanisms/
227. Agarwal,R., Goldenberg,M., Perry,R. & the World Federation of ADHD. World J.Biol. pathophysiology (P.A., J.K.B. and S.V.F.); Diagnosis, screening
WilliamIshak,W. The quality of life of adults with Psychiatry 13, 379400 (2012). and prevention (R.T., J.A.R.-Q., S.V.F. and E.J.S.S.B.);
attention deficit hyperactivity disorder: a systematic 247. Peng,X., Lin,P., Zhang,T. & Wang,J. Extreme Management (J.B. and E.J.S.S.B.); Quality of life (T.B.);
review. Innov. Clin. Neurosci. 9, 1021 (2012). learning machine-based classification of ADHD using Outlook (B.F. and S.V.F.); Overview of Primer (S.V.F.). Aside
228. Brod,M., Pohlman,B., Lasser,R. & Hodgkins,P. brain structural MRI data. PLoS ONE 8, e79476 from the first and last author, authorship is alphabetical.
Comparison of the burden of illness for adults with (2013). Allauthors extensively commented on each others sections.
22 | 2015 | VOLUME 1 www.nature.com/nrdp
2015 Macmillan Publishers Limited. All rights reserved
PRIMER
Competing interests authorship royalties from Springer and Cambridge University scale used for ADHD diagnoses, paid by Ingenix, Prophase,
S.V.F. has received income, travel expenses and/or research Press. E.J.S.S.B. has received speaker fees, consultancy, Shire, Bracket Global, Sunovion and Theravance; these
support from, and/or has been on an advisory board for, and/ research funding and/or conference support from: Shire, royalties were paid to the Department of Psychiatry at MGH.
or participated in continuing medical education programmes Janssen-Cilag, Neurotech solutions, Medice and the J.A.R.Q. has been on the speakers bureau for, acted as
sponsored by: Pfizer, Ironshore, Shire, Akili Interactive Labs, Universities of Leuven, Aarhus and Copenhagen. He has consultant for and/or received travel awards from: Eli Lilly,
CogCubed, Alcobra, VAYA Pharma, Neurovance, Impax, received book royalties from Oxford University Press and Janssen-Cilag, Novartis, Shire, Lundbeck, Ferrer and Rubi in
NeuroLifeSciences, Otsuka, McNeil, Janssen, Novartis, Jessica Kingsley, the latter related to the New Forest the past 3years. The ADHD Program chaired by him received
EliLilly and the US NIH. With his institution, S.V.F. has US Parenting Programme. T.B. has served in an advisory or unrestricted educational and research support from the
patent US20130217707 A1 for the use of sodiumhydrogen consultancy role for, received conference support from, following pharmaceutical companies in the past 3years:
exchange inhibitors in the treatment of ADHD. He receives received speakers fees from, and/or been involved in clinical EliLilly, Janssen-Cilag, Shire, Rovi and Rubi. B.F. has
royalties for books published by Guilford Press: Straight Talk trials sponsored by: Hexal Pharma, Eli Lilly, Medice, Novartis, received speaker fees from Merz. L.A.R. has been on the
about Your Childs Mental Health; Oxford University Press: Otsuka, Oxford outcomes, PCM Scientific, Shire and Vifor speakers bureau for, on the advisory board for, received
Schizophrenia: The Facts; and Elsevier: ADHD: Non- Pharma. The present work is unrelated to the above grants travel grants from and/or acted as a consultant for: Eli Lilly,
Pharmacologic Treatments. J.K.B. has been a consultant to, and relationships. J.B. has received research support or Janssen-Cilag, Novartis and Shire in the past 3years.
amember of an advisory board for, and/or speaker for: honoraria from: The US Department of Defense, American Hereceives authorship royalties from Oxford University Press
Janssen-Cilag BV, Eli Lilly, Shire, Lundbeck, Roche and Academy of Child and Adolescent Psychiatry (AACAP), and ArtMed. The ADHD and Juvenile Bipolar Disorder
Servier. He receives research support from the NIH, the Alcobra, Forest Research Institute, Ironshore, Lundbeck, Outpatient Programs chaired by him received unrestricted
European Commissions Seventh Framework programme, the Magceutics Inc., Merck, PamLab, Pfizer, Shire, SPRITES, educational and research support from the following
Marie Curie programme and the Netherlands Organization Sunovion, Vaya Pharma/Enzymotec, Massachusetts General pharmaceutical companies in the past 3years: Eli Lilly,
for Scientific Research (NWO). R.T. is an advisory board Hospital (MGH) Psychiatry Academy, American Professional Janssen-Cilag, Novartis and Shire. P.A. has been on the
member for, has served as consultant for, received travel Society of ADHD and Related Disorders (APSARD), ElMindA, speakers bureau for, on the advisory board for and/or has
awards from, and/or received software licenses from: the McNeil and the NIH. He has a US patent application pending received unrestricted educational and research awards from:
Canadian ADHD Resource Alliance (CADDRA), Shire, Purdue, (Provisional number #61/233,686) through MGH corporate Janssen-Cilag, Novartis, Shire, Qbtech, Vifor Pharma,
the Ministry of Education of Newfoundland and Labrador, licensing on a method to prevent stimulant abuse. He has GWPharmaceuticals, PCM Scientific and Eli Lilly. All fees
BioMed Central and Pearson-Cogmed. She receives received departmental royalties from a copyrighted rating related to these activities are paid to Kings College London.
NATURE REVIEWS | DISEASE PRIMERS VOLUME 1 | 2015 | 23
2015 Macmillan Publishers Limited. All rights reserved
Vous aimerez peut-être aussi
- Cat Q PDFDocument15 pagesCat Q PDFKrol Amafo100% (2)
- 36clinical Neuropsychology A Pocket Handbook For Assessment, 3 Edition PDFDocument768 pages36clinical Neuropsychology A Pocket Handbook For Assessment, 3 Edition PDFEstebanGira100% (2)
- Supporting Autistic People With Eating Disorders (Kate Tchanturia)Document281 pagesSupporting Autistic People With Eating Disorders (Kate Tchanturia)Dr. Chewie Silverblue-HolzPas encore d'évaluation
- The Incredible 5 Point ScaleDocument10 pagesThe Incredible 5 Point ScaleCintia Ferris LanteroPas encore d'évaluation
- Prepturtlecasestudysept 78 MilesdDocument6 pagesPrepturtlecasestudysept 78 Milesdapi-329950402Pas encore d'évaluation
- Gillberg 2007 Adult DISCO LongitudinalDocument9 pagesGillberg 2007 Adult DISCO LongitudinalSkymaker69Pas encore d'évaluation
- Guia de Buena Practica Autismo With Cover Page v2Document13 pagesGuia de Buena Practica Autismo With Cover Page v2Micaela Astudillo ParedesPas encore d'évaluation
- The Autism Spectrum QuotientDocument11 pagesThe Autism Spectrum QuotientIntellibrainPas encore d'évaluation
- Wisconsin Card SortingDocument16 pagesWisconsin Card SortingJenn Gooch100% (1)
- AQ ChildDocument3 pagesAQ ChildClaudia González MirandaPas encore d'évaluation
- Caars Obser (S) Int.Document7 pagesCaars Obser (S) Int.Farida LarryPas encore d'évaluation
- Handbook of Early Intervention For Autism Spectrum 2014 Chap 4Document27 pagesHandbook of Early Intervention For Autism Spectrum 2014 Chap 4api-544801662Pas encore d'évaluation
- From Anxiety To Meltdown: How Individuals On The Autism Spectrum Deal With Anxiety, Experience Meltdowns, Manifest Tantrums, and How You Can Intervene Effectively - PsychologyDocument4 pagesFrom Anxiety To Meltdown: How Individuals On The Autism Spectrum Deal With Anxiety, Experience Meltdowns, Manifest Tantrums, and How You Can Intervene Effectively - PsychologyfobisokaPas encore d'évaluation
- Declaracin Actualizada Del Consenso Europeo Sobre El Diagnstico y Tratamiento Del Tdah en AdultosDocument33 pagesDeclaracin Actualizada Del Consenso Europeo Sobre El Diagnstico y Tratamiento Del Tdah en AdultosolPas encore d'évaluation
- Pekka Louhiala - Preventing Intellectual Disability - Ethical and Clinical Issues (2004)Document184 pagesPekka Louhiala - Preventing Intellectual Disability - Ethical and Clinical Issues (2004)Andre BritoPas encore d'évaluation
- Gender Identity Differences in Autistic AdultsDocument9 pagesGender Identity Differences in Autistic Adultscolin capersPas encore d'évaluation
- Mental Health & Wellbeing For Children & Young People - Part TwoDocument24 pagesMental Health & Wellbeing For Children & Young People - Part Twomariya khanPas encore d'évaluation
- The Childhood Autism Spectrum Test (CAST) : Yes No Yes No Yes No Yes No Yes NoDocument4 pagesThe Childhood Autism Spectrum Test (CAST) : Yes No Yes No Yes No Yes No Yes NoZainub A KhanPas encore d'évaluation
- CC SR ProjectDocument11 pagesCC SR Projectapi-617045311100% (1)
- Camouflaging in Autism - A Systematic Review - Accepted ManuscriptDocument82 pagesCamouflaging in Autism - A Systematic Review - Accepted ManuscriptGemma Jones100% (1)
- About Autism: What You Need To KnowDocument10 pagesAbout Autism: What You Need To KnowMolnár AndreaPas encore d'évaluation
- KTEA Technical and Interpretive ManualDocument690 pagesKTEA Technical and Interpretive ManualVanity TrimblePas encore d'évaluation
- GARS 2 - ArticleDocument20 pagesGARS 2 - ArticleGoropadPas encore d'évaluation
- DSM5-Reflexion in AutismDocument7 pagesDSM5-Reflexion in AutismBianca NuberPas encore d'évaluation
- Ghid Adolescenti AutismDocument56 pagesGhid Adolescenti AutismDelia ManuelaPas encore d'évaluation
- Assessment Telepractice: Table of ContentsDocument2 pagesAssessment Telepractice: Table of ContentsShanthoshini BaskaranPas encore d'évaluation
- Environmental Curricular AdaptationsDocument2 pagesEnvironmental Curricular Adaptationsapi-544895801Pas encore d'évaluation
- EBP Report 2020.n PDFDocument143 pagesEBP Report 2020.n PDFcamila FuentesPas encore d'évaluation
- Escala en Ingles para Mutismo SelectivoDocument4 pagesEscala en Ingles para Mutismo SelectivoSilvana Ocando100% (1)
- Conductas Desafiantes en Personas Con TRDocument15 pagesConductas Desafiantes en Personas Con TRMyriamRozadaGonzalezPas encore d'évaluation
- 10 Neurodiversity Affirming Principles For TherapistsDocument1 page10 Neurodiversity Affirming Principles For TherapistsBelegan CrengutaPas encore d'évaluation
- Early Expression of Autism Spectrum DisordersDocument39 pagesEarly Expression of Autism Spectrum Disordersjyoti mahajanPas encore d'évaluation
- DASI EnglishDocument96 pagesDASI Englishfionachappell79100% (1)
- Faux Pas Recog TestDocument24 pagesFaux Pas Recog TestManuel G. SánchezPas encore d'évaluation
- Asdv 2Document51 pagesAsdv 2api-434818140Pas encore d'évaluation
- Sensory Processing and Autism Evidence Research Future Directions DR Roseann Schaaf PDFDocument59 pagesSensory Processing and Autism Evidence Research Future Directions DR Roseann Schaaf PDFKiyorPas encore d'évaluation
- Implementation of The Early Start Denver Model in An Italian CommunityDocument8 pagesImplementation of The Early Start Denver Model in An Italian CommunityLuis SeixasPas encore d'évaluation
- Repetitive Behaviour Questionnaire (RBQ-2) Scoring Final1Document3 pagesRepetitive Behaviour Questionnaire (RBQ-2) Scoring Final1catPas encore d'évaluation
- Wender Utah Rating Scale-25 WURS-25 Psychometric PDocument8 pagesWender Utah Rating Scale-25 WURS-25 Psychometric PUnoduetre StellaPas encore d'évaluation
- The Association Between Theory of Mind, Executive Function, and The Symptoms of Autism Spectrum DisorderDocument15 pagesThe Association Between Theory of Mind, Executive Function, and The Symptoms of Autism Spectrum DisorderRaúl VerdugoPas encore d'évaluation
- Attention Deficit/hyperactivity Disorder and Video Games: A Comparative Study of Hyperactive and Control ChildrenDocument8 pagesAttention Deficit/hyperactivity Disorder and Video Games: A Comparative Study of Hyperactive and Control ChildrenpriyaPas encore d'évaluation
- YES NO: Does The Client Consent To An Autism Spectrum Disorder (ASD) Assessment?Document1 pageYES NO: Does The Client Consent To An Autism Spectrum Disorder (ASD) Assessment?aspire centerPas encore d'évaluation
- ResumenDocument1 pageResumensaraPas encore d'évaluation
- CARS Autismo PDFDocument9 pagesCARS Autismo PDFEster BorgesPas encore d'évaluation
- Asperger Syndrome and AdultsDocument4 pagesAsperger Syndrome and AdultsAnonymous Pj6Odj100% (1)
- The Ritvo Autism Asperger Diagnostic Scale-Revised (RAADS-R) - A Scale To Assist The Diagnosis of Autism Spectrum Disorder in Adults. An International Validation StudyDocument14 pagesThe Ritvo Autism Asperger Diagnostic Scale-Revised (RAADS-R) - A Scale To Assist The Diagnosis of Autism Spectrum Disorder in Adults. An International Validation StudyTaNiTa TiKaRaNPas encore d'évaluation
- Central Coherence in Adults With A High-Functioning Autism Spectrum Disorder. in A Search For A Non-Self-Reporting Screening ToolDocument8 pagesCentral Coherence in Adults With A High-Functioning Autism Spectrum Disorder. in A Search For A Non-Self-Reporting Screening ToolNp Luis Gómez0% (1)
- Autism Spectrum DisorderDocument58 pagesAutism Spectrum DisorderPriscilla ChumrooPas encore d'évaluation
- DSM V Catherine Lord 2013 PDFDocument6 pagesDSM V Catherine Lord 2013 PDFmarikosvaPas encore d'évaluation
- Modified Coventry Model - Including PDA ProfileDocument13 pagesModified Coventry Model - Including PDA ProfileAliens-and-antsPas encore d'évaluation
- Assessment, Diagnosis and InterventionsDocument83 pagesAssessment, Diagnosis and InterventionsCristinaPas encore d'évaluation
- Autism 206 AymakelidesDocument44 pagesAutism 206 AymakelidesȘtefana StefiPas encore d'évaluation
- Adult DyslexiaDocument3 pagesAdult DyslexiareadalotbutnowisdomyetPas encore d'évaluation
- The Autism Checklist: A Practical Reference for Parents and TeachersD'EverandThe Autism Checklist: A Practical Reference for Parents and TeachersPas encore d'évaluation
- The Identification of Autistic Adults’ Perception of Their Own Diagnostic Pathway: A Research Dissertation Submitted for the Degree of Master of Autism at Sheffield Hallam UniversityD'EverandThe Identification of Autistic Adults’ Perception of Their Own Diagnostic Pathway: A Research Dissertation Submitted for the Degree of Master of Autism at Sheffield Hallam UniversityPas encore d'évaluation
- WJ III Clinical Use and Interpretation: Scientist-Practitioner PerspectivesD'EverandWJ III Clinical Use and Interpretation: Scientist-Practitioner PerspectivesPas encore d'évaluation
- Developmental Disorders of Language Learning and CognitionD'EverandDevelopmental Disorders of Language Learning and CognitionÉvaluation : 4 sur 5 étoiles4/5 (1)
- Essential Clinical Guide to Understanding and Treating AutismD'EverandEssential Clinical Guide to Understanding and Treating AutismPas encore d'évaluation
- Pebl 2 ManualDocument306 pagesPebl 2 ManualEstebanGiraPas encore d'évaluation
- Consciousness and Cognition: Dominique Makowski, Marco Sperduti, Serge Nicolas, Pascale PiolinoDocument9 pagesConsciousness and Cognition: Dominique Makowski, Marco Sperduti, Serge Nicolas, Pascale PiolinoEstebanGiraPas encore d'évaluation
- Willemsen 2012Document13 pagesWillemsen 2012EstebanGiraPas encore d'évaluation
- Electroencephalography Signatures of Attention-Deficit/hyperactivity Disorder: Clinical UtilityDocument15 pagesElectroencephalography Signatures of Attention-Deficit/hyperactivity Disorder: Clinical UtilityEstebanGiraPas encore d'évaluation
- The Mechanisms of Action of Commonly Used Antiepileptic DrugsDocument14 pagesThe Mechanisms of Action of Commonly Used Antiepileptic DrugsEstebanGiraPas encore d'évaluation
- Alteraciones Electroencefalográficas en NiñosDocument5 pagesAlteraciones Electroencefalográficas en NiñosEstebanGiraPas encore d'évaluation
- Cell Structure and FunctionsDocument23 pagesCell Structure and FunctionsMEOW41Pas encore d'évaluation
- Chapter 6 Advanced GeneticsDocument31 pagesChapter 6 Advanced GeneticsRochelleCasador180Pas encore d'évaluation
- Pathophysiology of Hiv and Aids: BY: DR Olasinde Abdulazeez Ayodeji Department of Community Medicine ABUTH ZariaDocument14 pagesPathophysiology of Hiv and Aids: BY: DR Olasinde Abdulazeez Ayodeji Department of Community Medicine ABUTH ZariaSalihu MustaphaPas encore d'évaluation
- Drexel BIOMED: School of Biomedical Engineering, Science & Health SystemsDocument35 pagesDrexel BIOMED: School of Biomedical Engineering, Science & Health SystemsBehnam Mirhashemi100% (1)
- MAKALAH BiokimiaDocument19 pagesMAKALAH BiokimiaGitha YaniPas encore d'évaluation
- PLANTS REviewerDocument3 pagesPLANTS REviewerJunie YeePas encore d'évaluation
- IMPORTANTVan de Ven and Poole (1995)Document32 pagesIMPORTANTVan de Ven and Poole (1995)stefi1234Pas encore d'évaluation
- Genetics Lab NotesDocument4 pagesGenetics Lab NotesJayar AguilarPas encore d'évaluation
- Fifth Edition Answers To End-Of-Chapter Questions: GCSE Biology For YouDocument1 pageFifth Edition Answers To End-Of-Chapter Questions: GCSE Biology For YouclydePas encore d'évaluation
- The Role of Micro-OrganismsDocument64 pagesThe Role of Micro-OrganismsAmit Singh50% (2)
- Real Time PCR: Pramod Bahadur K.CDocument14 pagesReal Time PCR: Pramod Bahadur K.CPramod KcPas encore d'évaluation
- Genetic Linkage, Recombination, Mapping - BIO231-FKDocument9 pagesGenetic Linkage, Recombination, Mapping - BIO231-FKmalik husnainPas encore d'évaluation
- Genetics in AquacultureDocument100 pagesGenetics in AquacultureDave DavePas encore d'évaluation
- Cold Spring Harb Perspect Med-2017-Long-a025577 PDFDocument17 pagesCold Spring Harb Perspect Med-2017-Long-a025577 PDFAurelia WetondiePas encore d'évaluation
- Glutamate Excitotoxicity in The Cerebellum Mediated by IL-1: Journal ClubDocument3 pagesGlutamate Excitotoxicity in The Cerebellum Mediated by IL-1: Journal ClubJar JarPas encore d'évaluation
- NeoplasiaDocument21 pagesNeoplasiaFreakyRustlee LeoragPas encore d'évaluation
- Rainsure Company, Instrument and Assays Introduction CLVDocument61 pagesRainsure Company, Instrument and Assays Introduction CLVMohammed H. KeshtaPas encore d'évaluation
- Haemogram: Blood CountsDocument3 pagesHaemogram: Blood CountsAbhi PrajapatiPas encore d'évaluation
- 7 week:: Microbial Growth (미생물의 성장)Document24 pages7 week:: Microbial Growth (미생물의 성장)MoonHoLeePas encore d'évaluation
- Class 9th Cell - The Unit of LifeDocument40 pagesClass 9th Cell - The Unit of LifeKabir RaiPas encore d'évaluation
- November 2006 MS - Paper 3 CIE Biology IGCSEDocument6 pagesNovember 2006 MS - Paper 3 CIE Biology IGCSEUzair ZahidPas encore d'évaluation
- Molecules Are DNA Molecules Formed by Laboratory Methods of Genetic RecombinationDocument2 pagesMolecules Are DNA Molecules Formed by Laboratory Methods of Genetic RecombinationMarygrace Broñola100% (2)
- Laboratory Manual and GuidelineDocument27 pagesLaboratory Manual and GuidelineFatih Rushdi100% (1)
- EBMT 2021 ProgramDocument288 pagesEBMT 2021 Programtirillas101Pas encore d'évaluation
- 13 2 A Biotic Abiotic Keystone SpeciesDocument12 pages13 2 A Biotic Abiotic Keystone Speciesapi-235225555Pas encore d'évaluation
- Axis Sumbu Tubuh (Materi 2)Document31 pagesAxis Sumbu Tubuh (Materi 2)Rizka MeisyPas encore d'évaluation
- Flavonoid ApplicationDocument8 pagesFlavonoid ApplicationAH SiddiquiPas encore d'évaluation
- Godbout, J. P., & Glaser, R. (2006) - Stress-Induced Immune Dysregulation. Implications For Wound Healing, Infectious Disease and CancerDocument7 pagesGodbout, J. P., & Glaser, R. (2006) - Stress-Induced Immune Dysregulation. Implications For Wound Healing, Infectious Disease and CancerFranco Paolo Maray-GhigliottoPas encore d'évaluation
- 7040 GCE O Biology MSC 20080807Document30 pages7040 GCE O Biology MSC 20080807Mehjabeen HossainPas encore d'évaluation