Académique Documents
Professionnel Documents
Culture Documents
Peerj Reviewing 13867 v0
Transféré par
Drima EdiDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Peerj Reviewing 13867 v0
Transféré par
Drima EdiDroits d'auteur :
Formats disponibles
Manuscript to be reviewed
Testing decision-making competency of schizophrenia
participants in clinical trials. A meta-analysis and meta-
regression
Sorin Hostiuc Corresp., 1
, Mugurel Constantin Rusu 2
, Ionuț Negoi 3
, Eduard Drima 4
1
Medicine, University of Medicine and Pharmacy of Bucharest, Bucharest, Romania
2
Dental Medicine, Carol Davila University of Medicine and Pharmacy, Bucharest, Romania
3
Medicine, Carol Davila University of Medicine and Pharmacy, Bucharest, Romania
4
Medicine, Galați University of Medicine and Pharmacy, Galați, Romania
Corresponding Author: Sorin Hostiuc
Email address: soraer@gmail.com
Aim. The primary purpose of this article is to evaluate the degree of impairment in each
dimension of decision-making capacity in schizophrenia patients compared to non-
mentally-ill controls, as quantified by the MacCAT-CR instrument. Secondary objectives are
(1) to see whether enhanced consent forms are associated with a significant increase in
decision-making capacity in schizophrenia patients, and (2) if decision-making capacity in
schizophrenia subjects is dependent on the age, gender, or the inpatient status of the
subjects. Materials and Methods. We analyzed the results obtained from three databases:
ISI Web of Science, Pubmed, Scopus. Each database was scrutinized using the following
keywords: “MacCAT-CR + schizophrenia”, “decision-making capacity + schizophrenia”,
and “informed consent + schizophrenia.” Results and Discussions. We included ten studies
in the analysis. Even if schizophrenia patients has a significantly decreased decision-
making competence compared to non-mentally-ill controls, they should be considered as
competent unless very severe changes are identified during the clinical examination. Using
enhanced informed consent techniques significantly decreased the difference between
schizophrenia patients and non-mentally-ill controls (except for the reasoning dimension),
and should be employed whenever the investigators want to include more severe patients
in their clinical trials. Older age, an increased percentage of men gender or inpatient
status tend to escalate the score difference of decision-making competence compared to
non-mentally-ill subjects in various dimensions of the decision-making capacity.
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
Manuscript to be reviewed
1 Testing decision-making competency of schizophrenia
2 participants in clinical trials. A meta-analysis and meta-
3 regression
5 Authors: Sorin Hostiuc1*, Mugurel Constantin Rusu2, Ionuț Negoi3, Eduard Drima4
1
6 MD, Ph.D., (1) Carol Davila University of Medicine and Pharmacy, Bucharest, Romania, (2)
7 National Institute of Legal Medicine, Bucharest, Romania
2
8 MD, Ph.D., (1) Carol Davila University of Medicine and Pharmacy, Bucharest, Romania
3
9 MD, Ph.D., Carol Davila University of Medicine and Pharmacy, Bucharest, Romania
4
10 MD, Ph.D., niversity of Medicine and Pharmacy, Galați, Romania
11 Running title: Decision-making competence in schizophrenia subjects
12
13
14
15 Corresponding author, Sos.Vitan Barzesti 9, 042122 Sector 4 Bucuresti, Romania, tel
16 0040723791072, email: soraer@gmail.com, sorin.hostiuc@umf.ro
17
18
19
20
21 Abstract
22 Aim. The primary purpose of this article is to evaluate the degree of impairment in each
23 dimension of decision-making capacity in schizophrenia patients compared to non-mentally-
24 ill controls, as quantified by the MacCAT-CR instrument. Secondary objectives are (1) to see
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
1
Manuscript to be reviewed
1 whether enhanced consent forms are associated with a significant increase in decision-
2 making capacity in schizophrenia patients, and (2) if decision-making capacity in
3 schizophrenia subjects is dependent on the age, gender, or the inpatient status of the subjects.
4 Materials and Methods. We analyzed the results obtained from three databases: ISI Web of
5 Science, Pubmed, Scopus. Each database was scrutinized using the following keywords:
6 “MacCAT-CR + schizophrenia”, “decision-making capacity + schizophrenia”, and “informed
7 consent + schizophrenia.”
8 Results and Discussions. We included ten studies in the analysis. Even if schizophrenia
9 patients has a significantly decreased decision-making competence compared to non-
10 mentally-ill controls, they should be considered as competent unless very severe changes are
11 identified during the clinical examination. Using enhanced informed consent techniques
12 significantly decreased the difference between schizophrenia patients and non-mentally-ill
13 controls (except for the reasoning dimension), and should be employed whenever the
14 investigators want to include more severe patients in their clinical trials. Older age, an
15 increased percentage of men gender or inpatient status tend to escalate the score difference of
16 decision-making competence compared to non-mentally-ill subjects in various dimensions of
17 the decision-making capacity.
18
19 Keywords: decision-making capacity; MACCAT-CR; inpatients; outpatients.
20
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
2
Manuscript to be reviewed
1
3 Introduction
4 The process of assessing the decision-making competence (DMC) of potential
5 subjects before their inclusion in clinical research is essential for respecting their right to self-
6 determination. DMC is a four-dimensional concept, which included (1) the understanding of
7 the disclosed information, (2) its appreciation to particular a setting, (3) reasoning associated
8 with that information and (4) the aptitude to express a choice(Appelbaum and Roth, 1982). In
9 adults, the presence of DMC is assumed; this is not the case in other groups of potential
10 research subjects including children, elderly, persons with psychiatric or neurological
11 disorders(Hein et al., 2014, Kim et al., 2002, Sessums et al., 2011).
12 Schizophrenia patients have quantitative and qualitative mental deficits, making them
13 at risk of incorrectly assessing a request to take part in a clinical trial(Wilson and Stanley,
14 2006). Howe et al., for example, found that DMC is inversely correlated with specific
15 positive symptom factor scores, especially those associated with cognition (poor attention,
16 difficulty in abstract thinking and conceptual disorientation)(Howe et al., 2005). Moser et al.
17 found that patients with positive symptoms did not have significant impairments on any
18 MacCAT-CR subscale while patients with negative and disorganized symptoms have a
19 decreased DMC(Moser et al., 2002). Overall, a larger proportion of people with
20 schizophrenia has a significant degree of decision-making impairment compared to non-
21 mentally-ill subjects(Jeste et al., 2006).
22 In recent years, the MacCAT-CR instrument was often used to assess the DMC for
23 taking part in clinical research of schizophrenia subjects. It is a 20- to 30-minute semi-
24 structured interview, which analyzes the four main dimensions of decision-making capacity,
25 each of them receiving a particular score – 0-26 points for understanding, 0-6 points for
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
3
Manuscript to be reviewed
1 appreciation, 0-8 points for reasoning and 0-2 points for expressing a choice(Appelbaum and
2 Grisso, 2001).
3 Most studies that compared DMC of schizophrenia subjects versus non-mentally-ill
4 controls, by using the MacCAT-CR instrument, found significant decreases in one or more of
5 its main dimensions(Anderson and Mukherjee, 2007, Candilis et al., 2008, Carpenter et al.,
6 2000, Harmell et al., 2012, Jeste et al., 2009, Kim et al., 2007, Kovnick et al., 2003, Moser et
7 al., 2002). The mean score for each dimension and the score difference between the
8 subgroups was variable.
9 The primary aim of this article is to test the impairment in each dimension of DMC in
10 schizophrenia patients compared to non-psychiatric controls, as appraised by the MacCAT-
11 CR instrument. Secondary objectives are (1) to see whether EIC is associated with a
12 significant increase in DMC in schizophrenia patients, and (2) if the DMC in schizophrenia
13 subjects depends on the age, gender, or their inpatient status.
14
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
4
Manuscript to be reviewed
1 Materials and methods
2 We performed the study by PRISMA and MOOSE guidelines for reporting systematic
3 reviews and meta-analyses of observational studies in epidemiology.
4 Selection criteria
5 Inclusion criteria: (1) observational studies that analyzed the DMC of schizophrenia subjects
6 compared to a control group comprising of non-mentally-ill subjects, with the aid of the
7 MacCAT-CR instrument. The main exclusion criteria were: (1) not fulfilling the inclusion
8 criteria, (2) not presenting enough information to reconstruct the data needed for the analysis,
9 (3) case-series studies and studies without a control group.
10 Search method.
11 We analyzed the results found in three databases: ISI Web of Science, Pubmed, Scopus. For
12 each, we used the following keywords: “MacCAT-CR + schizophrenia”, “decision-making
13 capacity + schizophrenia”, and “informed consent + schizophrenia”.
14 Data collection and analysis
15 SH and IN researched the databases independently, with an agreement rate for the added
16 articles of 83.3%. Data was then extracted separately by the two reviewers and listed in an
17 Excel file. When we found discrepancies between the obtained results, the issues were re-
18 analyzed by both examiners. We summarized the following data: study, year, total number of
19 cases, mean age and standard deviation, gender ratio for each group, ratio of in- versus
20 outpatients in the cases group, and mean and standard deviation of the values in the four main
21 dimensions of MacCAT-CR - understanding, appreciation, reasoning and expressing a
22 choice. If a particular article contained data regarding a potential intervention aimed at
23 improving the DMC, we added the data for both unenhanced and enhanced informed consent
24 techniques/forms.
25 The risk of bias was assessed separately for each case.
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
5
Manuscript to be reviewed
1 The quality assessment was performed by two researchers (SH and RMC) using the
2 Newcastle-Ottawa Scale for case-control studies (NOS). NOS was developed to address the
3 quality of non-randomized studies for systematic reviews/meta-analyses. Briefly, it comprises
4 of eight items, categorized into three main groups: (1) selection of the survey groups, (2)
5 comparability of the two groups and (3) evaluation of the exposure or outcome of interest.
6 The final quality score was computed as an average of the scores given by the two reviewers.
7 The agreement rate between reviewers was 90%.
9 Statistical analysis
10 We determined the effect size as the difference in means in all cases using a random effects
11 model computed in CMA software. To assess the odds for significant alterations of the
12 dimensions of the DMC, we calculated the Odds Ratio (OR). This was done by transforming
13 the difference in means in Cohen’s d (by dividing it by the standard deviation), converting
14 Cohen’s into ln(OR) through the following formula ln(OR)=dπ/sqrt(3), and then ln(OR) to
15 OR through the following equation OR=eln(OR). For each group and subgroup, we performed
16 a forest plot. We used Egger’s intercept technique for the analysis of publication bias, and I2
17 for measuring the heterogeneity. We used 95% confidence intervals and considered a p-value
18 of 0.05 or lower to be statistically significant. We rounded the obtained values to the second
19 decimal, except for (1) p-values below 0.05, case in which we included data until the 4th
20 decimal, and (2) when by rounding the OR, we obtained the value 1.
21
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
6
Manuscript to be reviewed
1 Results
2 Search synthesis
3 We obtained 2,496 results from which, after deleting duplicate and irrelevant studies, and
4 analyzing the type of paper and abstracts (if available), 53 articles were selected. They were
5 downloaded and examined further. Evaluating the references of these 53 articles, we
6 identified four more that were considered potentially relevant, which were also downloaded.
7 From the total number of 57 studies, we selected 10, which ultimately fulfilled the inclusion
8 criteria, and were added to the meta-analysis. We excluded 47 articles for not meeting the
9 inclusion criteria. Details regarding the selection algorithm are shown in Figure 1. The
10 studies included in the analysis are detailed in Table 1.
11
12 Quality assessment
13 The studies had quality scores ranging from 4.5 and 6.5 using the NOS Case Control scale.
14 The values for each study are given in Table 1.
15
16 Descriptive data
17 Within the ten included studies were 498 schizophrenia subjects (396 in simple consent
18 studies and 102 in enhanced consent studies), and 370 subjects in the control groups (301 in
19 simple consent studies and 69 in enhanced consent studies). The arithmetic mean values for
20 the four dimensions of the MacCAT-CR test are presented in Table 2.
21
22 Understanding
23 We included ten studies in the analysis. The effect size between the schizophrenia and
24 the control group was significant, with a difference in means of -4.18 (-5.49; -2.86), p<0.001.
25 The odds for a decreased understanding in schizophrenia patients was about five times higher
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
7
Manuscript to be reviewed
1 compared to control groups (OR=0.19, CI=0.14-0.28, p<0.001). See Figure 2 for details.
2 Publication bias was not statistically significant (Egger’s regression intercept = -1.86, p =
3 0.28). The heterogeneity of the understanding dimension was low (I2=30.9).
4 By running a meta-regression using mean age for the schizophrenia group as a
5 covariate, we found a slight decrease in understanding with growing age, but the result was
6 not statistically significant (B=-1.51, Z=-1.75, p=0.08). It was significantly affected when the
7 difference between men percentage of cases and control group increased (B=-1.64, Z=-9.68,
8 p<0.001), and when the proportion of inpatients increased (B=-3.74, Z=-3.65, p=0.0003). See
9 Figure 3.
10 Three studies contained information about enhanced informed consent. In them, we
11 found a decreased difference in means compared to controls (-2.73, with limits between -4.97
12 and -0.49). The odds for a decreased understanding in schizophrenia subjects using EIC was
13 about three times higher compared to the control groups (OR=0.28, CI=0.14-0.59, p=0.001).
14 Overall the use of EIC leads to a significant increase in understanding in
15 schizophrenia subjects compared to simple informed consent (OR=0.60, CI=0.37-0.98,
16 p=0.04).
17
18 Appreciation
19 We included ten studies in the analysis. The effect size was significant, with a
20 difference in means of -1.01 (-1.45, -0.75, p<0.001). The odds for a decreased appreciation in
21 schizophrenia patients was about five times higher compared to the control groups
22 (OR=0.206, CI=0.155-0.274, p<0.001). See Figure 4 for details. Publication bias was not
23 statistically significant (Egger’s regression intercept = -1.33, p = 0.37). The heterogeneity of
24 the appreciation dimension was very low (I2=0).
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
8
Manuscript to be reviewed
1 By running a meta-regression using mean age for the schizophrenia group as a
2 covariate, we found a significant decrease in appreciation with growing age (B=1.07, Z=-
3 2.78, p=0.005). Increasing the percentage of men between the comparison and the control
4 group (B=-0.87, Z=-10.30, p<0.001), and increasing the inpatient rate (B=-0.71 Z=-5.65,
5 p<0.001) also significantly decreased DMC in schizophrenia subjects. See Figure 5.
6 Three studies contained information about EIC. In them, we found a decreased
7 difference in means compared to controls (-0.46, with limits between -0.76 and -0.15). The
8 odds for a decreased understanding in schizophrenia subjects EIC was about two and a half
9 times higher compared to the control groups (OR=0.42, CI=0.24-0.74, p=0.003).
10 Overall the use of EIC leads to a significant increase in appreciation in schizophrenia
11 subjects compared to simple informed consent (OR=0.60, CI=0.36-0.98, p=0.04).
12
13 Reasoning
14 We included ten studies in the analysis. The effect size was highly significant, with a
15 difference in means of -0.99 (-1.44, -0.56, p<0.001). The odds for a decreased reasoning in
16 schizophrenia patients was about three times higher compared to the control groups
17 (OR=0.33, CI=0.22-0.51, p<0.001). See Figure 6 for details. Publication bias was not
18 statistically significant (Egger’s regression intercept = -2.01, p = 0.35). The heterogeneity of
19 the reasoning dimension was moderate (I2=52.9).
20 By running a meta-regression using mean age for the schizophrenia group as
21 covariate we found a slight decrease in reasoning with increasing age, but the result was not
22 statistically significant B=-1.30, Z=-1.72, p=0.21). The parameter was significantly affected
23 when the difference in the percentage of men in cases versus control group increased (B=-
24 1.00, Z=-5.15, p<0.001), and when the proportion of inpatients increased (B=-0.77, Z=-2.36,
25 p=0.01). See Figure 7.
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
9
Manuscript to be reviewed
1 Three studies contained information about EIC. In them, we found a non-statistically
2 significant decrease in the difference in means compared to controls (-0.830, with limits
3 between –2.28 and 0.57). The odds for a decreased reasoning in schizophrenia subjects using
4 EIC was four times higher compared to the control groups (OR=0.258, CI=0.03-2.60,
5 p=0.250), but the result was not statistically significant.
6 Overall the use of EIC leads to a significant increase in reasoning in schizophrenia
7 subjects compared simple informed consent (OR=0.56, CI=0.34-0.92, p=0.02).
9 Expressing a choice
10 We included nine studies in the analysis (Kovnick et al. did not analyze specifically
11 expressing a choice). The effect size was significant, with a difference in means of -0.05 (-
12 0.9, -0.01, p=0.022). See Figure 8 for details. The odds for a decreased aptitude to express a
13 choice in schizophrenia patients was about 66% higher compared to the control groups
14 (OR=0.61, CI=0.46-0.80, p<0.001). Publication bias was not statistically significant (Egger’s
15 regression intercept = 0.26, p = 0.84). The heterogeneity of the aptitude to express a choice
16 was very low (I2=0).
17 By running a meta-regression using mean age for the schizophrenia group as
18 covariate we found a slight decrease in the aptitude to express a choice with increasing age,
19 but the result was not statistically significant (B=-1.10, Z=-1.66, p=0.10). This parameter was
20 significantly affected when the differential between men percentage in cases and control
21 group increased (B=-0.53, Z=-3.67, p=0.0002), and when the proportion of inpatients
22 increased (B=-0.08, Z=-2.23, p=0.02).
23 Three studies contained information about EIC. In them, we found a non-statistically
24 significant increase in the difference in means compared to controls (0.01, with limits
25 between –0.03 and 0.05). The odds for a decreased capacity to express a choice in
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
10
Manuscript to be reviewed
1 schizophrenia subjects using the EIC was similar to the one found in the control groups
2 (OR=1.09, CI=0.62-1.91, p=0.76).
3 Overall the use of EIC forms leads to a significant increase in the aptitude to express a
4 choice compared to simple informed consent (OR=0.58, CI=0.35-0.95, p=0.03).
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
11
Manuscript to be reviewed
1 Discussions
2 Our study showed that when using non-enhanced informed consent procedures,
3 schizophrenia subjects tend to have highly significant decreased values for all dimensions of
4 DMC, the highest effect sizes being encountered for the understanding and appreciation sub-
5 scales.
6 To include subjects in clinical trials, the investigators must make a categorical
7 decision about the presence/absence of DMC. Some studies are suggesting various threshold
8 values for some or all DMC parameters(Stroup and Appelbaum, 2003, Kim et al., 2007). For
9 example, in the Clinical Antipsychotic Trials of Intervention Effectiveness – Schizophrenia
10 (CATIE)(Stroup et al., 2005) study was established a threshold value of 15 for the
11 understanding scale, a value that was proven to be a little too conservative(Kim et al., 2007).
12 Our study showed that there is a circa 4-point difference between schizophrenia and control
13 subjects in the understanding scale. If we were to take into account the mean value for
14 understanding (20.82, see Table 2) and add to this the average difference obtained in the
15 meta-analysis (-4.18), we would see that the mean theorized value for the schizophrenia
16 subjects [20.82-(4.18/2)=18.72] is well above this threshold. Similarly, the lower limit with a
17 95%CI (-5.49, corresponding to a lower limit for the schizophrenia group of 18.06) is well
18 above the 15 points threshold. By also taking into account the results of Kim et al. (Kim et
19 al., 2007), our analysis supports the idea that schizophrenia patients should be considered, per
20 prima facie, as being able to make informed decisions regarding the participation to clinical
21 trials. By assuming decision-making incompetence in these patients, we might discriminate
22 them based on their disease; therefore, by trying to obey the bioethical principle of autonomy
23 fully, we might breach the principle of justice.
24 Jeste et al. suggested the presence of a high inter-group heterogeneity in DMC in
25 patients with schizophrenia, with a standard deviation often increased twofold compared to
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
12
Manuscript to be reviewed
1 the control groups, and hinted as one of its leading sources the variable inclusion of in- and
2 outpatients in the cases groups(Jeste et al., 2006). Our analysis confirmed his hypothesis, as
3 all four dimensions of decision-making capacity were significantly affected by the percentage
4 of inpatients included in the initial studies. However, between studies our analysis showed a
5 little heterogeneity (except for the reasoning subscale where it was moderate), suggesting an
6 excellent reliability of the studies.
7 The scores on every subscale decreased once the percentage of men in the
8 schizophrenia group increased. This result is in agreement with other studies suggesting a
9 better social adaptability of women with schizophrenia to the disease. Hintikka et al. found
10 that women with schizophrenia have significantly better independent skills and domestic
11 activities compared to men with the same illness. For example, 11% of men lacked skills
12 regarding personal hygiene compared to only 4% of the women; 32% of men lacked skills
13 regarding financial affairs compared to 20% in women; 25% of men lacked decision-making
14 capacity compared to only 19% in women(Hintikka et al., 1999). Hambrecht et al. showed
15 that maladaptive social behaviors (including negative symptoms or inappropriate illness
16 behaviors) were more often found in men with schizophrenia(Hambrecht et al., 1992). Palmer
17 and Jeste revealed that understanding is correlated with the severity of negative
18 symptoms(Palmer and Jeste, 2006).
19 Various studies have suggested that age could alter decision-making capacity in
20 schizophrenia patients(Palmer and Jeste, 2006). Our study showed that there is an age-related
21 deterioration in various MacCAT-CR subscales, but they are not statistically significant
22 (except for the appreciation subscale), a possible cause being that prevalence of
23 schizophrenia tends to increase in women with increasing age(Mitter et al., 2005), and they,
24 as shown above, have better decision-making capacity compared to men(Hintikka et al.,
25 1999).
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
13
Manuscript to be reviewed
1 Using EICs various authors proved a significant increase in DMC(Moser et al., 2002,
2 Harmell et al., 2012, Jeste et al., 2009). Our study shows that, compared to the control group,
3 using EICs decreased the deficits in the understanding and appreciation subscales. When
4 compared to simple consent studies, EICs significantly increased the values for all four
5 MacCAT-CR subscales. Corroborated with our previous results, we recommend using EICs
6 only for studies that require subjects with severe cognitive deficits.
7 Kim et al. found that understanding sub-scale from MacCAT-CR was more important
8 as a predictor of a categorical capacity status compared to appreciation or reasoning(Kim et
9 al., 2007). Most instruments used for assessing decision-making capacity are testing the
10 understanding (for details see Palmer et al(Palmer et al., 2005)). Our study shows that
11 appreciation, together with understanding are the most affected dimensions of decision-
12 making capacity in schizophrenia subjects, and therefore, tasks directed specifically toward
13 increasing them might be the best approach in optimizing the tasks directed toward
14 decreasing decision-making incompetence for potential subjects with schizophrenia and
15 decision-making incapacity.
16
17 Limits
18 The number of studies included in the analysis is small (10); however, if we were to
19 include studies in which decision-making competence was evaluated using other scales, the
20 results would have been more heterogeneous. Moreover, only three studies included data
21 about enhanced ways of informing potential subjects. Even if the number was small, the
22 results reached statistical significance in most scales, suggesting that they did profoundly
23 improve the DMC.
24
25 Conclusions
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
14
Manuscript to be reviewed
1 Even if schizophrenia patients have a significantly decreased DMC compared to non-
2 mentally-ill controls, they should be considered as competent unless very severe alterations
3 are identified during the clinical examination. EICs tend to reduce the difference between
4 schizophrenia patients and non-mentally-ill controls (except for the reasoning dimension),
5 and should be used whenever the investigators want to include more severe patients in their
6 clinical trials. Age, men gender and the percentage of inpatients tend to increase the
7 differential of decision-making incompetence compared to non-mentally-ill subjects in
8 various dimensions of the decision-making competence as analyzed by the MacCAT-CR
9 scale.
10
11
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
15
Manuscript to be reviewed
1 References
2 ANDERSON, K. K. & MUKHERJEE, S. D. 2007. The need for additional safeguards in the
3 informed consent process in schizophrenia research. J Med Ethics, 33, 647-50.
4 APPELBAUM, P. S. & GRISSO, T. 2001. MacArthur competence assessment tool for clinical
5 research (MacCAT-CR), Professional Resource Press/Professional Resource Exchange.
6 APPELBAUM, P. S. & ROTH, L. H. 1982. Competency to consent to research: A psychiatric
7 overview. Archives of General Psychiatry, 39, 951.
8 CANDILIS, P. J., FLETCHER, K. E., GEPPERT, C. M., LIDZ, C. W. & APPELBAUM, P. S. 2008. A
9 direct comparison of research decision-making capacity:
10 schizophrenia/schizoaffective, medically ill, and non-ill subjects. Schizophr Res, 99,
11 350-8.
12 CARPENTER, W. T., JR., GOLD, J. M., LAHTI, A. C., QUEERN, C. A., CONLEY, R. R., BARTKO, J. J.,
13 KOVNICK, J. & APPELBAUM, P. S. 2000. Decisional capacity for informed consent in
14 schizophrenia research. Arch Gen Psychiatry, 57, 533-8.
15 HAMBRECHT, M., MAURER, K. & HÄFNER, H. 1992. Gender differences in schizophrenia in
16 three cultures. Social psychiatry and psychiatric epidemiology, 27, 117-121.
17 HARMELL, A. L., PALMER, B. W. & JESTE, D. V. 2012. Preliminary study of a web-based tool
18 for enhancing the informed consent process in schizophrenia research. Schizophr
19 Res, 141, 247-50.
20 HEIN, I. M., TROOST, P. W., LINDEBOOM, R., BENNINGA, M. A., ZWAAN, C. M., VAN
21 GOUDOEVER, J. B. & LINDAUER, R. J. 2014. Accuracy of the MacArthur competence
22 assessment tool for clinical research (MacCAT-CR) for measuring children’s
23 competence to consent to clinical research. JAMA pediatrics, 168, 1147-1153.
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
16
Manuscript to be reviewed
1 HINTIKKA, J., SAARINEN, P., TANSKANEN, A., KOIVUMAA-HONKANEN, H. & VIINAMÄKI, H.
2 1999. Gender differences in living skills and global assessment of functioning among
3 outpatients with schizophrenia. Australian and New Zealand Journal of Psychiatry,
4 33, 226-231.
5 HOWE, V., FOISTER, K., JENKINS, K., SKENE, L., COPOLOV, D. & KEKS, N. 2005. Competence
6 to give informed consent in acute psychosis is associated with symptoms rather than
7 diagnosis. Schizophr Res, 77, 211-4.
8 JESTE, D. V., DEPP, C. A. & PALMER, B. W. 2006. Magnitude of impairment in decisional
9 capacity in people with schizophrenia compared to normal subjects: an overview.
10 Schizophr Bull, 32, 121-8.
11 JESTE, D. V., PALMER, B. W., GOLSHAN, S., EYLER, L. T., DUNN, L. B., MEEKS, T., GLORIOSO,
12 D., FELLOWS, I., KRAEMER, H. & APPELBAUM, P. S. 2009. Multimedia consent for
13 research in people with schizophrenia and normal subjects: a randomized controlled
14 trial. Schizophr Bull, 35, 719-29.
15 KIM, S. Y., APPELBAUM, P. S., SWAN, J., STROUP, T. S., MCEVOY, J. P., GOFF, D. C., JESTE, D.
16 V., LAMBERTI, J. S., LEIBOVICI, A. & CAINE, E. D. 2007. Determining when impairment
17 constitutes incapacity for informed consent in schizophrenia research. Br J
18 Psychiatry, 191, 38-43.
19 KIM, S. Y., KARLAWISH, J. H. & CAINE, E. D. 2002. Current state of research on decision-
20 making competence of cognitively impaired elderly persons. The American journal of
21 geriatric psychiatry, 10, 151-165.
22 KOVNICK, J. A., APPELBAUM, P. S., HOGE, S. K. & LEADBETTER, R. A. 2003. Competence to
23 consent to research among long-stay inpatients with chronic schizophrenia.
24 Psychiatr Serv, 54, 1247-52.
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
17
Manuscript to be reviewed
1 MITTER, P., REEVES, S., ROMERO-RUBIALES, F., BELL, P., STEWART, R. & HOWARD, R. 2005.
2 Migrant status, age, gender and social isolation in very late-onset schizophrenia-like
3 psychosis. International journal of geriatric psychiatry, 20, 1046-1051.
4 MOSER, D. J., REESE, R. L., HEY, C. T., SCHULTZ, S. K., ARNDT, S., BEGLINGER, L. J., DUFF, K.
5 M. & ANDREASEN, N. C. 2006. Using a brief intervention to improve decisional
6 capacity in schizophrenia research. Schizophr Bull, 32, 116-20.
7 MOSER, D. J., SCHULTZ, S. K., ARNDT, S., BENJAMIN, M. L., FLEMING, F. W., BREMS, C. S.,
8 PAULSEN, J. S., APPELBAUM, P. S. & ANDREASEN, N. C. 2002. Capacity to provide
9 informed consent for participation in schizophrenia and HIV research. Am J
10 Psychiatry, 159, 1201-7.
11 PALMER, B. W., DUNN, L. B., APPELBAUM, P. S., MUDALIAR, S., THAL, L., HENRY, R.,
12 GOLSHAN, S. & JESTE, D. V. 2005. Assessment of capacity to consent to research
13 among older persons with schizophrenia, Alzheimer disease, or diabetes mellitus:
14 comparison of a 3-item questionnaire with a comprehensive standardized capacity
15 instrument. Arch Gen Psychiatry, 62, 726-33.
16 PALMER, B. W., DUNN, L. B., DEPP, C. A., EYLER, L. T. & JESTE, D. V. 2007. Decisional capacity
17 to consent to research among patients with bipolar disorder: comparison with
18 schizophrenia patients and healthy subjects. J Clin Psychiatry, 68, 689-96.
19 PALMER, B. W. & JESTE, D. V. 2006. Relationship of individual cognitive abilities to specific
20 components of decisional capacity among middle-aged and older patients with
21 schizophrenia. Schizophr Bull, 32, 98-106.
22 SESSUMS, L. L., ZEMBRZUSKA, H. & JACKSON, J. L. 2011. Does this patient have medical
23 decision-making capacity? Jama, 306, 420-427.
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
18
Manuscript to be reviewed
1 STROUP, S. & APPELBAUM, P. 2003. The subject advocate: protecting the interests of
2 participants with fluctuating decisionmaking capacity. IRB, 25, 9-11.
3 STROUP, S., APPELBAUM, P., SWARTZ, M., PATEL, M., DAVIS, S., JESTE, D., KIM, S., KEEFE, R.,
4 MANSCHRECK, T. & MCEVOY, J. 2005. Decision-making capacity for research
5 participation among individuals in the CATIE schizophrenia trial. Schizophrenia
6 research, 80, 1-8.
7 WILSON, S. T. & STANLEY, B. 2006. Ethical concerns in schizophrenia research: looking back
8 and moving forward. Schizophr Bull, 32, 30-6.
10
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
19
Manuscript to be reviewed
1
3 Table Legend
4 Table 1. Summary of studies included in the meta-analysis.
5 Table 2. Mean scores for the included studies computed as simple arithmetic means
7 Figure Legend
8 Figure 1. Selection algorithm for the included studies (PRISMA flow diagram)
9 PRISMA 2009 Flow Diagram
10
11
12
Identification
13 Records identified through Additional records identified
database searching through other sources
14 (n = 2496 (n = 53)
15
16
Records after duplicates removed
(n = 915)
17
Screening
18
19
Records screened Records excluded
(n = 788) (n = 731)
20
21
22 Full-text articles assessed Full-text articles excluded,
for eligibility with reasons
Eligibility
23 (n = 57) (n = 47 )
24
Studies included in
25
qualitative synthesis
(n = 10)
26
Included
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
Studies included in
20
quantitative synthesis
(meta-analysis)
(n = 10)
Manuscript to be reviewed
1
3 Figure 2. Understanding – Forest plot for ORs
5 Figure 3. Understanding – meta-regression, percentage of inpatients
7 Figure 4. Appreciation – Forest plot for ORs
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
21
Manuscript to be reviewed
2 Figure 5. Appreciation – meta-regression, proportion of inpatients
4 Figure 6. Reasoning – Forest plot for ORs
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
22
Manuscript to be reviewed
2 Figure 7. Reasoning – meta-regression, proportion of inpatients
4 Figure 8. Expressing a choice – Forest plot for ORs
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
23
Manuscript to be reviewed
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
24
Manuscript to be reviewed
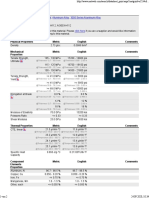
Table 1. Summary of studies included in the meta-analysis
Study Total No Schiz. Control Mean (st dev)* Men%* Description Quality
Subjects Subjects group ***
2008, Candillis(Candilis et 109 52 57 37.79(11.67), 76.9, 57.9 Subjects: 45 stable patients from a state hospital, seven outpatients 5
al., 2008) 41.04(13.16) Controls: patients from a diabetes clinic
Answers were given regarding the participation to a potential drug trial; payment of 10$ for
participation
2000, Carpenter(Carpenter 54 30 24 40.2(8.8), 56.7, 78.2 Subjects: inpatients and outpatients (20 and 10 respectively). 28 schizophrenia patients, 2 5
et al., 2000) 39.7(10.2) patients with schizoaffective disorder
Controls: recruited from community centers and a free medical clinic.
Answers regarding the participation to a randomized, double-blind trial of a novel anti-
psychotic medication for this study
2012, Harmell(Harmell et 17 9 8 57(10), 89, 50 Subjects: outpatients, recruited through a registry; randomly assigned for receiving either a 6.5
al., 2012) 52.2(12.1) normal or a web-media enhanced consent procedure
Controls: non-psychiatry patients, recruited through a registry
Answers: regarding a hypothetical clinical trial of an experimental cognition enhancing
medication
2012, Harmell**(Harmell 18 10 8 57.9(8.9), 40, 62.5
et al., 2012) 48.6(15.9)
2009, Jeste(Jeste et al., 95 66 29 51.2(6.5), 64, 52 Subjects: community-dwelling outpatients aged >40 years, with schizophrenia. Subjects 5
2009) 54.2(9.3) were randomly assigned to either a simple or a multimedia consent procedure
Controls: recruited through newspaper advertisements, flyers, and word of mouth
Answers: regarding a 14-week double-blind, placebo-controlled RCT to determine the
25
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
Manuscript to be reviewed
effectiveness of a cognition-enhancing drug for cognitive deficits associated with
schizophrenia or with normal aging
2009, Jeste(Jeste et al., 93 62 31 52.4(8), 65, 45
2009) 54.7(7.3)
2007, Kim(Kim et al., 131 91 40 42.2(10.2), Subjects: with severe mental illness consisted of two subgroups: 55 participants from a 6
2007) 39.9(10.9) schizophrenia study from six different sites across the US; 36 people from two outpatient
clinics serving individuals with severe and persistent mental illnesses, and from inpatient
units
Controls: recruited through advertisements from the community, in support staff work areas
of a general hospital and at an out-patient substance misuse recovery program
Answers: regarding participation in the CATIE study
2003, Kovnik(Kovnick et 51 27 24 39.1(7.1), 78, 79 Cases: 27 psychiatric inpatients, non-acutely ill 5
al., 2003) 39.7(10.2) Controls: individuals from the community, without known psychiatric pathologies
Answers regarding a hypothetical clinical trial of a new medication for schizophrenia that
was conducted in a randomized, double-blind fashion
2006, Moser(Moser et al., 60 30 30 34.1(10.65), 73, 87 Cases: 30 individuals with schizophrenia (6 outpatients, 24 inpatients) 4.5
2006) 30(11.46) Controls: healthy individuals, without significant psychiatric or medical pathologies
Answers regarding a possible double- blind, placebo-controlled trial of a cognitive-
enhancing agent called Synaptoclear
2006, Moser(Moser et al., 60 30 30 34.1(10.65), 73, 87
2006) 30(11.46)
2002, Moser(Moser et al., 50 25 25 31.56(9.77), 84, 76 Cases: 25 individuals with schizophrenia, 21 outpatients, and four inpatients, 18 of which 5.5
2002) 37.4(7.76) received antipsychotic medication
Controls: 25 infected individuals, 24 outpatients, one inpatient, 15 under psychotropic
26
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
Manuscript to be reviewed
medication (primarily for depression); none was under antipsychotic medication
Answers regarding a hypothetical 6-week, randomized, double-blind, placebo-con- trolled
study of a cognition-enhancing agent called Synaptoclear
2005, Palmer(Palmer et al., 71 35 36 65.7(5.2), 57.1, 97.2 Cases: 35 clinically stable outpatients with diagnoses of schizophrenia (30) or 5
2005) 70.9(6.2) schizoaffective disorder (5)
Controls: 36 outpatients with diabetes mellitus, recruited through clinical research programs
Answers regarding participation in a randomized controlled trial of an experimental
compound (“plakmin”), tested for cognitive-enhancing effects, which was modeled after one
used for a local study of cognitive benefits of a cholinomimetic agent
2007, Palmer(Palmer et al., 59 31 28 52.4(7), 48.4,46.4 Cases: 31 outpatients with schizophrenia 5.5
2007) 56.6(11.1) Controls: recruited from the community (28)
Answers regarding a longitudinal study of side effects, including tardive dyskinesia, of
FDA–approved second-generation antipsychotic medications among middle-aged and older
patients
* statistics for both schizophrenia patients and controls, separated by a comma.
** italic lines – decision-making capacity after enhancement procedure
*** Newcastle-Ottawa Scale for case-control studies
27
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
Manuscript to be reviewed
Table 2. Mean scores for the included studies computed as simple arithmetic means
Parameter Simple Informed Consent, Simple Informed Consent, Mean values Enhanced Informed Consent, Enhanced Informed Consent,
Cases Controls Cases Controls
Understanding 18.3 24.12 20.82 22.29 25.13
Appreciation 4.17 5.44 4.72 5.03 5.61
Reasoning 5.34 6.08 5.66 5.46 5.63
Expressing a choice 1.89 1.98 1.93 1.99 1.99
Total No. of Subjects 396 301 102 69
28
PeerJ reviewing PDF | (2016:10:13867:0:0:NEW 12 Oct 2016)
Vous aimerez peut-être aussi
- Dimensional PsychopathologyD'EverandDimensional PsychopathologyMassimo BiondiPas encore d'évaluation
- Finding the Path in Alzheimer’s Disease: Early Diagnosis to Ongoing Collaborative CareD'EverandFinding the Path in Alzheimer’s Disease: Early Diagnosis to Ongoing Collaborative CarePas encore d'évaluation
- Apatia y Riesdo de PDD CIDDocument15 pagesApatia y Riesdo de PDD CIDGustavo PestanaPas encore d'évaluation
- ndt-18-891Document7 pagesndt-18-891Julio DelgadoPas encore d'évaluation
- Cognitive Insight As An Indicator of Competence To Consent To Treatment in SchizophreniaDocument4 pagesCognitive Insight As An Indicator of Competence To Consent To Treatment in SchizophreniaJulio DelgadoPas encore d'évaluation
- HuntintingDocument8 pagesHuntintingJose Bryan GonzalezPas encore d'évaluation
- Decisional Capacity of Patients With Schizophrenia To Consent To Research Taking StockDocument4 pagesDecisional Capacity of Patients With Schizophrenia To Consent To Research Taking StockJulio DelgadoPas encore d'évaluation
- General Hospital Psychiatry: Review ArticleDocument10 pagesGeneral Hospital Psychiatry: Review Articlehevi_tarsumPas encore d'évaluation
- The Clinically Important Difference On The Unified Parkinson's Disease Rating ScaleDocument7 pagesThe Clinically Important Difference On The Unified Parkinson's Disease Rating Scale143 lutfiana azzahraPas encore d'évaluation
- CIA 47367 Assessment of Cognitive Impairment in Patients With Parkinso 021214Document7 pagesCIA 47367 Assessment of Cognitive Impairment in Patients With Parkinso 021214ziropadjaPas encore d'évaluation
- A Study of Co-Morbidity in Mental RetardationDocument9 pagesA Study of Co-Morbidity in Mental RetardationijhrmimsPas encore d'évaluation
- 36 - Decision-Making and Risk-Taking in Forensic and Non-Forensic Patients With Schizophrenia Spectrum Disorders A Multicenter European StudyDocument8 pages36 - Decision-Making and Risk-Taking in Forensic and Non-Forensic Patients With Schizophrenia Spectrum Disorders A Multicenter European Studygabri93bioPas encore d'évaluation
- Prevalence of ADD-ADHD in Older AdultsDocument8 pagesPrevalence of ADD-ADHD in Older AdultsRyan BPas encore d'évaluation
- Meta-Analysis of Neuropsychological Functioning in Euthymic Bipolar Disorder: An Update and Investigation of Moderator VariablesDocument9 pagesMeta-Analysis of Neuropsychological Functioning in Euthymic Bipolar Disorder: An Update and Investigation of Moderator VariablesIcaroPas encore d'évaluation
- Escala Ansietat Parkinson (PAS)Document55 pagesEscala Ansietat Parkinson (PAS)Mar BatistaPas encore d'évaluation
- Diagnostics 09 00131Document8 pagesDiagnostics 09 00131lors93Pas encore d'évaluation
- Descriptive Analysis of The Autism Spectrum Quotient (AQ) in A Sample of Brazilian AdultsDocument6 pagesDescriptive Analysis of The Autism Spectrum Quotient (AQ) in A Sample of Brazilian AdultsBruno PontesPas encore d'évaluation
- Systematic Review and Meta-Analysis: The Prevalence of Mental Illness in Child and Adolescent Refugees and Asylum SeekersDocument10 pagesSystematic Review and Meta-Analysis: The Prevalence of Mental Illness in Child and Adolescent Refugees and Asylum SeekersdsfsdgfdgfdgPas encore d'évaluation
- WNL 0000000000009400Document8 pagesWNL 0000000000009400Hans MaulwurfPas encore d'évaluation
- Caye - Life Span Studies of ADHD Predictors of Persistence - Curr Psychiatry Rep - 2016Document11 pagesCaye - Life Span Studies of ADHD Predictors of Persistence - Curr Psychiatry Rep - 2016Karla GarzaPas encore d'évaluation
- 10 1002@acn3 51102Document12 pages10 1002@acn3 51102chemistpl420Pas encore d'évaluation
- 134 FullDocument10 pages134 FullJulio DelgadoPas encore d'évaluation
- 1 s2.0 S0890856714004079 MainDocument10 pages1 s2.0 S0890856714004079 MainPar DoPas encore d'évaluation
- Neurocognitive Impairmente Defecit Subtype SchizophreniaDocument11 pagesNeurocognitive Impairmente Defecit Subtype SchizophreniaLeandro FornésPas encore d'évaluation
- Prevalence of Dementia and Cognitive Impairment After Stroke: An Epidemiological StudyDocument12 pagesPrevalence of Dementia and Cognitive Impairment After Stroke: An Epidemiological StudylydiaPas encore d'évaluation
- The Impact of Machine Learning Techniques in The Study of Bipolar DisorderDocument17 pagesThe Impact of Machine Learning Techniques in The Study of Bipolar DisorderDiego Librenza GarciaPas encore d'évaluation
- 2017 - Clinical and Demographic Predictors of Conversion To Dementia in Mexican Elderly With Mild Cognitive ImpairmentDocument7 pages2017 - Clinical and Demographic Predictors of Conversion To Dementia in Mexican Elderly With Mild Cognitive ImpairmentRaúl VerdugoPas encore d'évaluation
- NP Borderline PersonalityDocument30 pagesNP Borderline PersonalityMaria Beatriz JuradoPas encore d'évaluation
- Psychological MeasuresDocument6 pagesPsychological MeasuresvaneschkPas encore d'évaluation
- Cognitive Impairment and Associated Risk Factors in Older Adult Hemodialysis Patients: A Cross Sectional SurveyDocument9 pagesCognitive Impairment and Associated Risk Factors in Older Adult Hemodialysis Patients: A Cross Sectional Surveyre septian IlhamsyahPas encore d'évaluation
- Patients SchizofreniaDocument3 pagesPatients SchizofreniaArinaDogaruPas encore d'évaluation
- Alves, 2022 - AQ Norms BrazilDocument5 pagesAlves, 2022 - AQ Norms BrazilKathleen LimaPas encore d'évaluation
- Progression and Predictors of Mild Cognitive Impairment in Chinese Elderly: A Prospective Follow-Up in The Shanghai Aging StudyDocument9 pagesProgression and Predictors of Mild Cognitive Impairment in Chinese Elderly: A Prospective Follow-Up in The Shanghai Aging StudyCristina SavaPas encore d'évaluation
- Good For QualitativeDocument9 pagesGood For QualitativeWassie TsehayPas encore d'évaluation
- Keefe. The Schizophrenia Cognition Rating ScaleDocument7 pagesKeefe. The Schizophrenia Cognition Rating ScaleRosarioBengocheaSeco0% (1)
- The Presence of Behavioural and Psychological Symptoms and Progression To Dementia in The Cognitively Impaired Older PopulationDocument11 pagesThe Presence of Behavioural and Psychological Symptoms and Progression To Dementia in The Cognitively Impaired Older PopulationCeci_SunshinePas encore d'évaluation
- Missed Opportunities For DiagnosisDocument7 pagesMissed Opportunities For DiagnosisEduardo SemblanoPas encore d'évaluation
- Middleton 2006Document8 pagesMiddleton 2006Nagy DaherPas encore d'évaluation
- HSR 2179Document13 pagesHSR 2179Lisa SariPas encore d'évaluation
- Estimating The Prevalence of Dementia and Mild Cognitive Impairment in The US - PMCDocument19 pagesEstimating The Prevalence of Dementia and Mild Cognitive Impairment in The US - PMCveronicalovirgenPas encore d'évaluation
- Evidence-Based Treatment in The Field of Child andDocument2 pagesEvidence-Based Treatment in The Field of Child andRayén F. HuenchunaoPas encore d'évaluation
- Prevalence of Mental Disorders in Elderly People: The European Mentdis - Icf65+ StudyDocument7 pagesPrevalence of Mental Disorders in Elderly People: The European Mentdis - Icf65+ StudyToqa DiaaPas encore d'évaluation
- 130 494 1 PB PDFDocument9 pages130 494 1 PB PDFhfathiardiPas encore d'évaluation
- Epidemiology of Apathy in Older Adults. The Cache County StudyDocument11 pagesEpidemiology of Apathy in Older Adults. The Cache County StudyJuanPas encore d'évaluation
- Research Paper:: Cognitive Process in Patients With Obsessive-Compulsive Disorder: A Cross-Sectional Analytic StudyDocument10 pagesResearch Paper:: Cognitive Process in Patients With Obsessive-Compulsive Disorder: A Cross-Sectional Analytic StudyTrifan DamianPas encore d'évaluation
- The Incremental Value of Neuropsychological Assessment: A Critical ReviewDocument33 pagesThe Incremental Value of Neuropsychological Assessment: A Critical ReviewJose Alonso Aguilar ValeraPas encore d'évaluation
- Dementia q6Document21 pagesDementia q6Rachel GabrielaPas encore d'évaluation
- Article Psychological MedicineDocument12 pagesArticle Psychological MedicineAnnita triyanaPas encore d'évaluation
- Teste Faux PasDocument5 pagesTeste Faux PasAdriano FerrazPas encore d'évaluation
- Acta Neuro Scandinavica - 2018 - Mani - Efficacy of Group Cognitive Rehabilitation Therapy in Multiple SclerosisDocument9 pagesActa Neuro Scandinavica - 2018 - Mani - Efficacy of Group Cognitive Rehabilitation Therapy in Multiple Sclerosismadalena limaPas encore d'évaluation
- Sleep Characteristics in Diabetic Patients Depending On The Occurrence of Neuropathic Pain and Related FactorsDocument13 pagesSleep Characteristics in Diabetic Patients Depending On The Occurrence of Neuropathic Pain and Related FactorsderisonmarsinovabakaraPas encore d'évaluation
- Neurologist Communicationg The Diagnosis of ELADocument9 pagesNeurologist Communicationg The Diagnosis of ELAHabib G. Moutran BarrosoPas encore d'évaluation
- Heterogenitate BPDocument8 pagesHeterogenitate BPCarmen CiursaşPas encore d'évaluation
- (C1C2) Herpertz (2017)Document13 pages(C1C2) Herpertz (2017)sydhpzsb7dPas encore d'évaluation
- Clinical Applicability and Cutoff Values For AnDocument9 pagesClinical Applicability and Cutoff Values For AnDayanne SilvaPas encore d'évaluation
- Impact of Cognitive Impairment On MildDocument12 pagesImpact of Cognitive Impairment On MildCristina MPPas encore d'évaluation
- Articulo 3 Sesión 1 Visión General Reed Et Al 2018Document13 pagesArticulo 3 Sesión 1 Visión General Reed Et Al 2018manuel ñiquePas encore d'évaluation
- Jurnal 1Document15 pagesJurnal 1utin putiPas encore d'évaluation
- Xu 2011Document6 pagesXu 2011GanellPas encore d'évaluation
- 1 s2.0 S0010440X15302169 MainDocument4 pages1 s2.0 S0010440X15302169 Mainlidia torres rosadoPas encore d'évaluation
- Conjugare - Traducere To Be To Have., To DoDocument4 pagesConjugare - Traducere To Be To Have., To DoDrima EdiPas encore d'évaluation
- Conjugarea Verbului A Face La Toate TimpurileDocument4 pagesConjugarea Verbului A Face La Toate TimpurileDrima EdiPas encore d'évaluation
- Scor WaterlowDocument1 pageScor WaterlowDrima EdiPas encore d'évaluation
- Lista Verbelor RegulateDocument7 pagesLista Verbelor RegulateDrima EdiPas encore d'évaluation
- Conjugare - Traducere To Be To Have., To DoDocument5 pagesConjugare - Traducere To Be To Have., To DoDrima EdiPas encore d'évaluation
- Conjugarea Verbului A Fi La Toate TimpurileDocument4 pagesConjugarea Verbului A Fi La Toate TimpurileDrima Edi100% (1)
- Behavioral Activation Strategies For The Treatment of PTSDDocument41 pagesBehavioral Activation Strategies For The Treatment of PTSDDrima Edi100% (1)
- Alphabet and PronunciationDocument11 pagesAlphabet and PronunciationDrima Edi100% (2)
- N I "M T ?": Ewer Typical NtipsychoticsDocument15 pagesN I "M T ?": Ewer Typical NtipsychoticsDrima EdiPas encore d'évaluation
- Aids To Examination of The Peripheral Nervous System 4th 2000 PDFDocument67 pagesAids To Examination of The Peripheral Nervous System 4th 2000 PDFDrima EdiPas encore d'évaluation
- Personality Dimensions 1: Gsaucier@uoregon - EduDocument47 pagesPersonality Dimensions 1: Gsaucier@uoregon - EduDrima EdiPas encore d'évaluation
- Anticholinergics Study Drug ListDocument1 pageAnticholinergics Study Drug ListDrima Edi100% (1)
- Ch.1 Psychiatric AssesDocument35 pagesCh.1 Psychiatric AssesDrima Edi0% (1)
- An Atlas of Infant Polysomnography PDFDocument186 pagesAn Atlas of Infant Polysomnography PDFDrima EdiPas encore d'évaluation
- New Psychiatric MedicationsDocument60 pagesNew Psychiatric MedicationsDrima EdiPas encore d'évaluation
- Psychopharmacologic Drugs: - Antipsychotic Agents - Antimanic Drugs - Antidepressant DrugsDocument18 pagesPsychopharmacologic Drugs: - Antipsychotic Agents - Antimanic Drugs - Antidepressant DrugsDrima EdiPas encore d'évaluation
- Atlas of Alzheimer's Disease PDFDocument159 pagesAtlas of Alzheimer's Disease PDFDrima EdiPas encore d'évaluation
- Antidepresive Sedative ActivatoareDocument2 pagesAntidepresive Sedative ActivatoareDrima EdiPas encore d'évaluation
- CA Inter Group 1 Book November 2021Document251 pagesCA Inter Group 1 Book November 2021VISHAL100% (2)
- STM - Welding BookDocument5 pagesSTM - Welding BookAlvin MoollenPas encore d'évaluation
- Bajaj Allianz InsuranceDocument93 pagesBajaj Allianz InsuranceswatiPas encore d'évaluation
- Basic of An Electrical Control PanelDocument16 pagesBasic of An Electrical Control PanelJim Erol Bancoro100% (2)
- How To Control A DC Motor With An ArduinoDocument7 pagesHow To Control A DC Motor With An Arduinothatchaphan norkhamPas encore d'évaluation
- Environmental Auditing For Building Construction: Energy and Air Pollution Indices For Building MaterialsDocument8 pagesEnvironmental Auditing For Building Construction: Energy and Air Pollution Indices For Building MaterialsAhmad Zubair Hj YahayaPas encore d'évaluation
- Seminar On Despute Resolution & IPR Protection in PRCDocument4 pagesSeminar On Despute Resolution & IPR Protection in PRCrishi000071985100% (2)
- 7 TariffDocument22 pages7 TariffParvathy SureshPas encore d'évaluation
- Banjara EmbroideryDocument34 pagesBanjara EmbroideryKriti Rama ManiPas encore d'évaluation
- Cdi 2 Traffic Management and Accident InvestigationDocument22 pagesCdi 2 Traffic Management and Accident InvestigationCasanaan Romer BrylePas encore d'évaluation
- An RambTel Monopole Presentation 280111Document29 pagesAn RambTel Monopole Presentation 280111Timmy SurarsoPas encore d'évaluation
- On CatiaDocument42 pagesOn Catiahimanshuvermac3053100% (1)
- Multispan LC 2046 Length Counter PDFDocument2 pagesMultispan LC 2046 Length Counter PDFvinod kumarPas encore d'évaluation
- Condition Monitoring of Steam Turbines by Performance AnalysisDocument25 pagesCondition Monitoring of Steam Turbines by Performance Analysisabuhurairaqazi100% (1)
- CH 1 India Economy On The Eve of Independence QueDocument4 pagesCH 1 India Economy On The Eve of Independence QueDhruv SinghalPas encore d'évaluation
- Powerpoint Presentation: Calcium Sulphate in Cement ManufactureDocument7 pagesPowerpoint Presentation: Calcium Sulphate in Cement ManufactureDhruv PrajapatiPas encore d'évaluation
- Aluminum 3003-H112: Metal Nonferrous Metal Aluminum Alloy 3000 Series Aluminum AlloyDocument2 pagesAluminum 3003-H112: Metal Nonferrous Metal Aluminum Alloy 3000 Series Aluminum AlloyJoachim MausolfPas encore d'évaluation
- BSCSE at UIUDocument110 pagesBSCSE at UIUshamir mahmudPas encore d'évaluation
- Specialty Arc Fusion Splicer: FSM-100 SeriesDocument193 pagesSpecialty Arc Fusion Splicer: FSM-100 SeriesSFTB SoundsFromTheBirdsPas encore d'évaluation
- WEEK6 BAU COOP DM NextGen CRMDocument29 pagesWEEK6 BAU COOP DM NextGen CRMOnur MutluayPas encore d'évaluation
- 09 WA500-3 Shop ManualDocument1 335 pages09 WA500-3 Shop ManualCristhian Gutierrez Tamayo93% (14)
- Employees' Pension Scheme, 1995: Form No. 10 C (E.P.S)Document4 pagesEmployees' Pension Scheme, 1995: Form No. 10 C (E.P.S)nasir ahmedPas encore d'évaluation
- BluetoothDocument28 pagesBluetoothMilind GoratelaPas encore d'évaluation
- Resume Jameel 22Document3 pagesResume Jameel 22sandeep sandyPas encore d'évaluation
- Shubham Tonk - ResumeDocument2 pagesShubham Tonk - ResumerajivPas encore d'évaluation
- COOKERY10 Q2W4 10p LATOJA SPTVEDocument10 pagesCOOKERY10 Q2W4 10p LATOJA SPTVECritt GogolinPas encore d'évaluation
- Notifier AMPS 24 AMPS 24E Addressable Power SupplyDocument44 pagesNotifier AMPS 24 AMPS 24E Addressable Power SupplyMiguel Angel Guzman ReyesPas encore d'évaluation
- CSEC Jan 2011 Paper 1Document8 pagesCSEC Jan 2011 Paper 1R.D. KhanPas encore d'évaluation
- Methodical Pointing For Work of Students On Practical EmploymentDocument32 pagesMethodical Pointing For Work of Students On Practical EmploymentVidhu YadavPas encore d'évaluation
- Tradingview ShortcutsDocument2 pagesTradingview Shortcutsrprasannaa2002Pas encore d'évaluation