Académique Documents
Professionnel Documents
Culture Documents
Procalcitonina en Pop Cardiovascular
Transféré par
darlingcarvajalduqueCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Procalcitonina en Pop Cardiovascular
Transféré par
darlingcarvajalduqueDroits d'auteur :
Formats disponibles
Diagnostic Value of Procalcitonin on Early
Postoperative Infection After Pediatric Cardiac
Surgery
Xia Li, MD1; Xu Wang, MD1; Shoujun Li, MD2; Jun Yan, MD2; Dan Li, PhD1
Objectives: Assess the diagnostic value of serial monitoring of concentration was always higher than 1.0 ng/mL within 7 days after
procalcitonin levels on early postoperative infection after pediatric surgery and/or procalcitonin variation between postoperative days 4
cardiac surgery with cardiopulmonary bypass. and 7 was positive in the infected patients. Best receiver operating
Design: Prospective, observational study. characteristics curves area under the curve were obtained for pro-
Setting: A pediatric cardiac surgical ICU (PICU) and pediatric calcitonin and procalcitonin variation from postoperative days 5 to 7.
cardiac surgery department at Fuwai Hospital, Chinese Academy WBC- and C-reactive protein–related receiver operating character-
of Medical Sciences, Peking Union Medical College. istics curves area under the curve revealed a very poor ability to pre-
Patients: Patients were 3 years old and below, underwent cardiac dict infection. Logistic regression found that only procalcitonin on
surgery involving cardiopulmonary bypass, the Aristotle Compre- postoperative day 7 and PICU stay was independently correlated
hensive Complexity score was 8 or higher and free from active to the infection status. There was no significant correlation between
preoperative infection or inflammatory disease. the absolute value of procalcitonin and timing of infection.
Interventions: Blood samples for measurement of procalcitonin, Conclusions: Procalcitonin was more accurate than C-reactive
C-reactive protein, and WBC were taken before surgery and daily protein and WBC to predict early postoperative infection, but the
for 7 days in postoperative period. Clinical, laboratory, and imag- diagnostic properties of procalcitonin could not be observed dur-
ing data were collected on enrollment. Procalcitonin, C-reactive ing the first 3 postoperative days due to the inflammatory process
protein, WBC levels, and procalcitonin variation were calculated related to cardiopulmonary bypass. The dynamic change of pro-
and compared between those with and without infection. calcitonin is more important than the absolute value to predict
Measurements and Main Results: Two hundred and thirty-eight chil- postoperative infection. The maintenance of a high level (procal-
dren were enrolled. Presence of infection within 7 days of surgery, citonin > 1.0 ng/mL) within 7 days after surgery and/or a second
length of intubation, and ICU stay were documented. Two indepen- increase in procalcitonin between the fourth and the seventh
dent experts in regard to the complete medical chart determined the postoperative day could be used as an indicator of postoperative
final diagnosis of postoperative infection. Infection was diagnosed in infection. Continuous procalcitonin monitoring might help to dis-
45 patients. Procalcitonin peaked on the first postoperative day. No cover infection earlier. (Pediatr Crit Care Med 2017; XX:00–00)
differences were found on procalcitonin within 3 days after operation Key Words: cardiac surgery; cardiopulmonary bypass; congenital
between the infected and the noninfected patients, and significant heart disease; postoperative infection; procalcitonin
correlation was found between procalcitonin on postoperative days
1–3 and cardiopulmonary bypass duration. Serum procalcitonin
P
1
Department of Pediatric Intensive Care Unit, National Center for rocalcitonin (PCT), initially described as a marker for
Cardiovascular Disease and Fuwai Hospital, Chinese Academy of
infection (1), has emerged as an early, sensitive, and
Medical Sciences, Peking Union Medical College, Beijing, The People’s specific indicator of bacterial infection during the last
Republic of China.
decade (2, 3). However, recent studies showed that PCT levels
2
Department of Surgery, Pediatric Cardiac Center,National Center for
Cardiovascular Disease and Fuwai Hospital, Chinese Academy of also increased in clinical situations without infections such as
Medical Sciences, Peking Union Medical College, Beijing, The People’s cardiopulmonary bypass (CPB), massive blood transfusion,
Republic of China. trauma, burns, shock, or major surgery (4–7).
The authors have disclosed that they do not have any potential conflicts Pediatric cardiac surgery with CPB is a major surgery, which
of interest.
can induce an acute inflammatory response (8). This inflam-
Address correspondence and requests for reprints to: Xu Wang, MD,
E-mail: fwpicu@163.com matory response is a result of several stimuli, such as exposure
Copyright © 2017 by the Society of Critical Care Medicine and the World of blood to nonphysiologic surfaces, surgical trauma, myo-
Federation of Pediatric Intensive and Critical Care Societies cardial ischemia-reperfusion, and endotoxin release (9, 10).
DOI: 10.1097/PCC.0000000000001118 Because of this response, conventional clinical and biologic
Pediatric Critical Care Medicine www.pccmjournal.org 1
Copyright © 2017 by the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies.
Unauthorized reproduction of this article is prohibited
Li et al
signs may be misleading in the diagnosis of early postoperative Tracheal extubation was performed when patients met all
infection, and the value of PCT remains a matter of debate in the following criteria: no severe arrhythmias, no bleeding,
the setting of pediatric cardiac surgery with CPB. hemodynamic stability, adequate muscle strength, full con-
Therefore, the primary aim of our study was to assess the sciousness, and adequate ventilation.
diagnostic value of serial monitoring of PCT levels on early
postoperative infection in children undergoing pediatric cardiac Biologic Measurement
surgery with CPB, and to compare it with those of C-reactive Blood samples for measurement of serum concentrations of
protein (CRP) and WBC count. The secondary objective PCT, CRP, and WBC were obtained separately after induction
included observing the normal profile of PCT, CRP, and WBC. of anesthesia (baseline) and daily until the seventh postopera-
tive day (POD).
PCT was measured by an immunoluminometric assay
METHODS whose detection limit ranging from 0.05 to 25 ng/mL and nor-
This was a prospective and observational study. The study was mal value was less than 0.5 ng/mL. CRP was measured by auto-
approved by Institutional Review Board of Fuwai Hospital. matic lasernephelometry with normal value less than 8 mg/L.
Written informed consents for research were obtained from WBC was determined by using an automatic counter with a
caretakers of all enrolled patients. normal value between 4,000 and 10,000 cells/mm3. The coef-
ficient of variation of the measurements was less than 5%.
Study Setting and Patient Characteristics
The study setting is a pediatric cardiac surgical ICU (PICU; 22 Diagnosis of Postoperative Infection and Grouping
beds) and pediatric cardiac surgery department (120 beds) at Postoperative infections were defined as: 1) pneumonia (12):
Fuwai Hospital (1,500 beds), Chinese Academy of Medical Sci- a) One of the following symptoms occurs: purulent sputum,
ences, Peking Union Medical College, Beijing, China. auscultation findings suspicious of pneumonia or hypoxemia,
All children admitted to our PICU after pediatric cardiac body temperature higher than 38°C; b) Infiltrate on chest radio-
surgery involving CPB from March 2015 to June 2015 were graph; c) Leukocytosis (> 12,000 cells/mm3); and d) Microor-
screened for study eligibility, and finally 238 patients met ganism isolated in bronchial secretions. 2) Deep sternal wound
the inclusion criteria: 1) Patients were 3 years old and below; infection and mediastinitis (13): a) Body temperature greater
2) Patients underwent cardiac surgery involving CPB; 3) The than 38°C; b) Leukocytosis (> 12,000 cells/mm3); and c) Pres-
Aristotle Comprehensive Complexity (ACC) score (11) was 8 ence of pus, bacterial growth, or both, identified in mediastinal
or higher; and 4) Patients were free from active preoperative tissue samples obtained during surgical reexploration. 3) Sep-
infection or inflammatory disease (all of the following criteria sis (14) (according to American College of Chest Physicians/
were achieved at study entry: WBC count < 12 × 109/L, PCT < Society of Critical Care Medicine Consensus Conference).
0.5 ng/mL, body temperature < 37.5°C). The final diagnosis of postoperative infection was determined
by two independent experts in regard to the complete medical
Anesthesia, CPB, and Perioperative Management chart. In cases of disagreement between the two experts, a third
Anesthesia was induced with midazolam (0.05 mg/kg) and expert reached a consensus. Each final diagnosis was classified as
fentanyl (5–10 µg/kg), maintained with continuous infusion certain (high probability), possible, low probability (unlikely),
of fentanyl (0.05–0.1 µg/kg/min). Trachea intubation was per- or absent. The final diagnosis was reached when it was classi-
formed after adequate muscular relaxation had been obtained fied as certain or possible by the experts and ruled out when the
with pancuronium (0.1 mg/kg). Monitoring included electro- experts classified it as absent or unlikely. Experts were blinded
cardiography, pulse oximetry, end-tidal carbon dioxide, and for PCT but not for WBC and CRP, which are routinely used.
invasive arterial blood pressure using a radial artery cath- Patients were divided into two groups: the noninfection
eter. Prophylactic antibiotics consisted of cefuroxime-sodium group, who did not develop any postoperative infection within
15–20 mg/kg after induction and maintained q8h within 2 days 7 days after surgery, and the infection group, who developed
after operation. postoperative infection within 7 days after surgery.
Heparin (300 UI/kg) was administrated before CPB for
anticoagulant in every patient. Myocardial protection during Diagnosis of Noninfectious Complications
CPB was performed with intermittent infusion of cold crystal- Because postoperative infection could also be combined with
loid cardioplegia and moderate hypothermia (32°C). other noninfectious complications, which interfered with PCT
After surgery, body temperature, microbiological and radio- level, we also assessed postoperative noninfectious complica-
logic examinations, were performed daily, and a blood gas analy- tions. In this study, postoperative noninfectious complications
sis was performed every 4 hours when the patients were in the were defined as: 1) low cardiac output syndrome (LCOS) char-
PICU. After transferring to general ward, blood gas analysis, acterized by clinical signs and symptoms of low cardiac output
microbiological, and radiologic examinations were performed (oliguria, tachycardia, poor perfusion, and cardiac arrest) that
when deemed necessary by the physicians. Blood culture was required inotropic support greater than or equal to 100% above
performed when body temperature was above 38.5°C, and a baseline, administration of a new inotropic agent, or malignant
secretion sample for microbiological examination was per- ventricular arrhythmia, high output failure necessitating use of
formed when the wound was swelling. delayed sternal closure/extracorporeal membrane oxygenation
2 www.pccmjournal.org XXX 2017 • Volume XX • Number XXX
Copyright © 2017 by the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies.
Unauthorized reproduction of this article is prohibited
Cardiac Intensive Care
support or other maneuvers used to improve cardiac output recorded daily until POD7. PCT variation was defined by the
(i.e., cardiac pacing); 2) renal insufficiency needs peritoneal equation ([PCTdelayed – PCTinitial]/PCTinitial) × 100%. PCTinitial is
dialysis or continuous venovenous hemofiltration treatment; PCT concentration on POD1; PCTdelayed is blood PCT concen-
3) neurologic complication (stroke, ischemic injury); and 4) tration measured at POD2 to POD7. A negative value indicates
gastrointestinal complication (ischemia, bleeding). a decrease in PCT concentration. VIS is calculated as dopa-
mine dose (μg/kg/min) + dobutamine dose (μg/kg/min) + 100
Data Collection × epinephrine dose (μg/kg/min) + 100 × norepinephrine dose
At study entry, data regarding patient demographics, anatomic (μg/kg/min) + 15 × milrinone dose (μg/kg/min) + 10,000 ×
diagnosis, and ACC score were collected. The CPB time, aor- vasopressin dose (U/kg/min) (15).
tic cross clamp time, vasoactive-inotropic scores (VIS) at 24
hours, the levels of serum aspartate aminotransferase (AST), Statistical Analysis
alanine aminotransferase (ALT), creatinine and blood urea Quantitative variables are presented as mean ± sd or median
nitrogen (BUN) on POD1, the duration of mechanical ventila- (95% CI) in nonnormally distributed variables (Kolmogorov-
tion, the length of PICU stay, mortality, presence of infection Smirnov test), and qualitative data are given as number and
within 7 days of surgery, and noninfectious complications were percentage. The values results were not normally distributed
recorded. Serum PCT, CRP, and WBC concentrations were also and thus were analyzed nonparametrically. Noninfection and
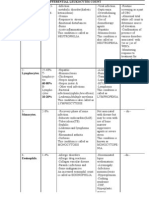
Table 1. Clinic Characteristics of Patients in the Noninfection and Infection Groups
Infection Group Noninfection Group
Variable (n = 45) (n = 193) p
Age (mo) 8 (0.6–32) 9 (0.7–34) 0.608
Body weight (kg) 7.58 ± 3.01 8.21 ± 2.93 0.149
Male sex (n, %) 29 (64.4) 120 (62.2) 0.417
Aristotle Comprehensive Complexity score 9.47 ± 1.47 9.51 ± 1.53 0.783
Cardiac diagnose 0.586
Tetralogy of Fallot 12 52
Total anomalous pulmonary venous connection 5 20
Double-outlet of right ventricular 6 31
Total endocardial cushion defect 7 33
Pulmonary arterial atresia 5 19
Coarctation of the aorta + ventricular septal defect 4 16
Transposition of great arteries 6 22
Cardiopulmonary bypass duration (min) 126.3 ± 49.9 121.6 ± 42.5 0.665
Aortic cross clamp (min) 85.7 ± 34.1 81.6 ± 38.7 0.639
Vasoactive-inotropic scores at 24 hr 14.2 ± 6.5 13.9 ± 5.9 0.488
Aspartate aminotransferase (U/L) 152.9 ± 63.1 151.4 ± 59.2 0.606
Alanine aminotransferase (U/L) 28.8 ± 10.5 25.8 ± 8.8 0.281
Creatinine (µmol/L) 44.6 ± 13.2 43.1 ± 12.1 0.329
Blood urea nitrogen (mmol/L) 8.2 ± 2.5 8.1 ± 2.6 0.815
Mechanical ventilation duration (hr) 22 (6–126) 18 (5–54) 0.136
PICU stay (d) 5 (3–15) 3 (1–5) 0.013
Death (n, %) 1 (2.22) 0 0.050
Noninfectious complications (n, %) 5 (11.1) 18 (9.3) 0.554
Low cardiac output syndrome 3 11
Renal insufficiency (peritoneal dialysis/continuous 2 7
venovenous hemofiltration)
Data are expressed as mean ± sd, median (95% CI), or number (%).
Pediatric Critical Care Medicine www.pccmjournal.org 3
Copyright © 2017 by the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies.
Unauthorized reproduction of this article is prohibited
Li et al
infection were compared by the Mann-Whitney U test or t 9 months (0.6–34 mo) and weight of 8.08 ± 2.96 kg. Cardiac
test for continuous variables and by chi-square test, and when diagnoses were all complex malformation with an average
appropriate, Fisher exact test for categorical variables. Linear ACC score of 9.50 ± 1.51.
regression analysis was performed to describe the relationship Forty-five patients were categorized into the infection
between serum PCT concentration and CPB duration. Correla- group, 37 patients (82.2%) had pneumonia, one (2.2%) had
tion and scatterplots were calculated and constructed between mediastinitis, and seven (15.6%) had sepsis, and there was an
the infected patient’s timing of infection and the absolute value excellent agreement between experts for the diagnosis of infec-
of PCT on the day of infection. tion (98%).
Because WBC, CRP, PCT, and PCT variation are numerical Characteristics of the patients in the two groups are pre-
data, receiver operating characteristics (ROC) curves and area sented in Table 1. No significant differences were found
under the curve (AUC) were computed. For infection predic- regarding age, body weight, sex, ACC score, cardiac diagnose,
tion, cutoff values for WBC, CRP, and PCT were chosen to cor- duration of CPB and aortic cross clamp, VIS at 24 hours, the
respond to the best respective Youden’s index calculated as follows: levels of AST, ALT, creatinine and BUN on POD1, the duration
Youden’s index = sensitivity + specificity − 1. Results are expressed of mechanical ventilation, and noninfectious complications.
for area under the ROC curves (AUC) as mean (95% CI). The length of PICU stay was longer in the infection group (5 vs
Logistic regression was performed to discriminate if PICU 3 d; p = 0.013). One patient (2.22%) in infection group devel-
stay, PCT on POD4 to POD7, PCT variation of POD4 to oped LCOS necessitating use of extracorporeal membrane
POD7–POD1, and WBC on POD2 were independently cor- oxygenation support and died (1/45 vs 0/173; p = 0.05).
related to the infection status.
A p value of less than or equal to 0.05 was considered signif- WBC, CRP, PCT, and the Value of PCT Variation in the
icant. All analyses were conducted using SPSS version 20 (IBM Infected and Noninfected Patients
Corporation, New York, NY). Baseline WBC (8.32 ± 1.71 vs 8.66 ± 2.16 mm–6; p = 0.546),
CRP (7.9 ± 2.1 vs 8.1 ± 2.4 mg/L; p = 0.449), and PCT (0.34
[0.16–0.48] vs 0.26 [0.12–0.38] ng/mL; p = 0.328) were not
RESULTS
significantly different between the infection and noninfection
Patient Characteristics groups. All preoperative WBCs were less than 12 × 109/L, and
Nine hundred and seventy-six patients were admitted to the serum PCT concentration was less than 0.5 ng/mL.
PICU after pediatric cardiac surgery during the study period. After CPB, serum PCT concentration increased signifi-
Of these, 238 patients (24.4%) were included in this study, cantly, peaked on the first POD, and began to decrease from
149 (62.6%) male and 89 (37.4%) female, with a mean age of POD2. In the noninfection group, serum PCT concentration
Table 2. Serum Procalcitonin Concentrations and Procalcitonin Variation of Patients in
the Noninfection and Infection Groups
Infection Group Noninfection Group
Variable (n = 45) (n = 193) p
Baseline PCT (ng/mL) 0.34 (0.16–0.48) 0.26 (0.12–0.38) 0.328
POD1 PCT (ng/mL) 12.69 (1.3–25) 12.09 (1.3–25) 0.928
POD2 PCT (ng/mL) 8.80 (0.5–25) 7.92 (0.9–25) 0.859
POD3 PCT (ng/mL) 4.45 (0.3–25) 3.83 (0.23–25) 0.534
POD4 PCT (ng/mL) 3.35 (0.44–16.3) 1.23 (0.31–8.7) 0.015
POD5 PCT (ng/mL) 2.59 (0.37–6.5) 0.44 (0.1–3.8) < 0.001
POD6 PCT (ng/mL) 2.15 (0.25–4.7) 0.35 (0.05–2.2) < 0.001
POD7 PCT (ng/mL) 1.35 (0.28–3.7) 0.22 (0.05–1.2) < 0.001
Variation PCT POD2 to POD1 (%) –0.28 (–0.89 to 1.58) –0.40 (–0.77 to 1.19) 0.729
Variation PCT POD3 to POD1 (%) –0.51 (–0.98 to 1.47) –0.74 (–0.98 to 0.02) 0.194
Variation PCT POD4 to POD1 (%) –0.66 (–0.98 to 2.36) –0.88 (–0.98 to –0.07) 0.006
Variation PCT POD5 to POD1 (%) –0.75 (–0.96 to 1.52) –0.93 (–0.99 to –0.56) 0.002
Variation PCT POD6 to POD1 (%) –0.81 (–0.97 to 0.04) –0.96 (–0.99 to –0.74) < 0.001
Variation PCT POD7 to POD1 (%) –0.87 (–0.98 to 0.10) –0.97 (–1.0 to –0.84) < 0.001
PCT = procalcitonin, POD = postoperative day.
Data are expressed as median (95% CI).
4 www.pccmjournal.org XXX 2017 • Volume XX • Number XXX
Copyright © 2017 by the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies.
Unauthorized reproduction of this article is prohibited
Cardiac Intensive Care
decreased progressively and returned to baseline values on The value of PCT variation was significantly higher in the
POD5, whereas in the infection group, PCT remained elevated noninfected patients than in the infected ones between POD4
thereafter. No differences were found on PCT value within and POD7; from the 95% CI, we can see there were some
3 days after operation between the infected and noninfected positive values in the infection group that indicates a second
patients (p > 0.05), but there were significant differences increase in PCT, whereas in the noninfection group, all values
on PCT level from POD4 to POD7 between the two groups of PCT variation were negative (Table 2).
(p < 0.05) (Table 2 and Fig. 1). Significant correlation Of the 45 infected patients, 19 patients maintain a high level
was found between PCT on POD1 to 3 and CPB duration of PCT (> 1 ng/mL) during the first 7 PODs, whereas in other
(r2 = 0.76, 0.68, and 0.59, respectively). 26 infected patients, the PCT levels showed a different trend,
descended to normal range
within 3 days after surgery, but
appeared a secondary increase
on the fourth and seventh PODs.
WBC and CRP peaked on
POD2 and remained elevated
after the seventh POD in the
two groups (Fig. 1). There
were significant differences of
WBC on POD2 (12.98 ±
2.28
vs 15.79 ± 4.72 mm–6; p = 0.019)
while the CRP level was not sig-
nificantly different between the
two groups on each POD (Fig. 1).
Diagnostic Value of
WBC, CRP, PCT, and PCT
Variation
ROC curves, AUC for WBC
on POD2, CRP on POD2 (the
maximum value), PCT and PCT
variation from POD4 to 7 were
calculated, and the most accu-
rate cutoff values to distinguish
infection and noninfection were
evaluated. Best ROC curves
AUC were obtained for PCT
and PCT variation from POD5
to POD7 (Table 3). WBC- and
CRP-related ROC curves AUC
revealed a very poor ability to
predict infection (Table 3 and
Fig. 2). When comparing the
ROC curves, PCT and PCT
variation were more accurate
than CRP and WBC for the
diagnosis of postoperative infec-
tion (Fig. 2). The diagnostic vari-
ables of each biologic marker are
depicted in Table 3: PCT was
better than CRP and WBC.
Multivariate Analysis
Between the Infection and
Figure 1. Comparison of (A) WBC count, (B) C-reactive protein (CRP), and (C) procalcitonin (PCT) in the Noninfection Patients
noninfection (circles and dotted line; n = 193) and infection (square and unbroken line; n = 45) groups.
Data are expressed as mean or median. * p < 0.05 (between-group comparisons, Mann-Whitney U test with Logistic regression found that
Bonferroni correction). only PCT on POD7 and PICU
Pediatric Critical Care Medicine www.pccmjournal.org 5
Copyright © 2017 by the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies.
Unauthorized reproduction of this article is prohibited
Li et al
Table 3. Comparison of Area Under the Receiver Operating Characteristic Curve and
Efficiency of WBC, C-Reactive Protein, Procalcitonin and Procalcitonin Variation in the
Diagnosis of Postoperative Infection
Area Under
the Receiver
Operating Positive Positive Negative Negative
Characteristic Predictive Likelihood Predictive Likelihood
Variable Threshold Curve Sensitivity Specificity Value Ratio Value Ratio
POD2 WBC 14.1 × 109/L 0.64 0.68 0.67 0.68 2.05 0.67 0.48
(0.48–0.77) (0.45–0.86) (0.43–0.85) (0.45–0.86) (1.3–3.1) (0.43–0.85) (0.2–1.1)
POD2 C-reactive 73.5 mg/L 0.49 0.67 0.47 0.27 1.29 0.84 0.68
protein (0.41–0.58) (0.50–0.83) (0.38–0.57) (0.18–0.37) (1.0–1.7) (0.73–0.92) (0.4–1.1)
POD4 PCT 1.9 ng/mL 0.69 0.63 0.71 0.76 2.11 0.56 0.53
(0.56–0.79) (0.46–0.77) (0.50–0.86) (0.58–0.89) (1.5–3.0) (0.38–0.73) (0.3–1.1)
POD5 PCT 0.97 ng/mL 0.81 0.89 0.71 0.85 3.13 0.79 0.15
(0.68–0.90) (0.75–0.97) (0.48–0.89) (0.70–0.94) (2.3–4.2) (0.54–0.94) (0.05–0.5)
POD6 PCT 0.86 ng/mL 0.85 0.81 0.79 0.85 2.91 0.81 0.12
(0.73–0.93) (0.65–0.92) (0.54–0.94) (0.70–0.94) (2.1–4.0) (0.54–0.96) (0.03–0.4)
POD7 PCT 0.80 ng/mL 0.86 0.70 0.89 0.93 6.68 0.61 0.33
(0.74–0.94) (0.53–0.84) (0.67–0.98) (0.77–0.99) (5.1–8.7) (0.41–0.79) (0.08–1.3)
Variation PCT
POD4 to POD1 –0.77 0.73 0.64 0.71 0.80 2.16 0.58 0.51
(0.61–0.83) (0.45–0.77) (0.50–0.86) (0.61–0.92) (1.5–3.0) (0.41–0.75) (0.2–1.0)
POD5 to POD1 –0.92 0.77 0.84 0.67 0.82 2.51 0.70 0.24
(0.64–0.87) (0.68–0.94) (0.43–0.85) (0.66–0.92) (1.8–3.5) (0.46–0.88) (0.09–0.6)
POD6 to POD1 –0.91 0.82 0.89 0.79 0.89 4.24 0.79 0.14
(0.69–0.91) (0.75–0.97) (0.54–0.94) (0.75–0.97) (3.3–5.5) (0.54–0.94) (0.04–0.5)
POD7 to POD1 –0.95 0.80 0.89 0.63 0.83 2.42 0.75 0.17
(0.67–0.89) (0.75–0.97) (0.38–0.84) (0.67–0.93) (1.7–3.5) (0.48–0.93) (0.06–0.5)
PCT = procalcitonin, POD = postoperative day.
Data are expressed as value
(95% CI).
stay were independently correlated to the infection status with be affected by longer duration of CPB time, and the inflammatory
a p value equals to 0.013 (odds ratio [OR] =3.23 [95% CI, response induced by CPB is stronger. All congenital heart disease
1.28–8.14]) and p value equals to 0.046 (OR = 1.52 [95% CI, (CHD) patients enrolled in this study were complicating complex
1.01–2.29]), respectively (Table 4). malformation (ACC score ≥ 8), which was also a common pre-
disposing factor for pneumonia in children with CHD. Although
The Absolute Value of PCT and the Timing of patients might be free from active preoperative infection or inflam-
Infection matory disease, they were still a high-risk population of postop-
The average time of infection in the 45 infected patients was erative infection. For them, it is difficult to distinguish the higher
5.6 ± 0.9 days after operation, and the average absolute value level of PCT arises mainly from inflammatory response induced
of PCT on the day of infection was 3.7 ± 1.8 ng/mL. Figure 3 by CPB or/and infection. We believe that the study about dynam-
shows the scatterplot of infected patient’s timing of infection ics of PCT levels of this special population will help us discover
and the absolute value of PCT on the day of infection, and no and diagnose infection earlier, so as to promote the recovery and
significant correlation was found between them (r2 = 0.147). improve prognosis. In our study, we observed that the absolute
value of PCT was higher and the value of PCT variation was lower
DISCUSSION in patients with postoperative infection after pediatric cardiac sur-
Very few pediatric studies have analyzed the serial PCT measure- gery and that PCT was more accurate than WBC and CRP to pre-
ments and the value of PCT variation as indicators for postopera- dict postoperative infection. Furthermore, the dynamic change of
tive infection after cardiac surgery. To our knowledge, this was the PCT permitted an early diagnosis. The persistent high level of PCT
first study about correlating PCT variation with infection in pedi- (> 1.0 ng/mL) within 7 days after surgery and/or a second increase
atric patients with complex congenital heart disease. In contrast to in PCT between the fourth and the seventh PODs could be used as
adults, children with complex congenital heart disease are easier to an indicator of postoperative infection.
6 www.pccmjournal.org XXX 2017 • Volume XX • Number XXX
Copyright © 2017 by the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies.
Unauthorized reproduction of this article is prohibited
Cardiac Intensive Care
reported to rise earlier than
WBC and CRP after the
onset of bacterial infection
and to decrease earlier dur-
ing the course of controlled
infection (7, 19).
In our study, the diagnostic
value of PCT was higher than
WBC and CRP to predict post-
operative infection (Table 3).
PCT has already been postu-
lated to be superior to CRP
or WBC, and to even correlate
with the severity of bacterial
infection (20−21). The superi-
ority of PCT may be explained
by its more specific increase
in case of bacterial infection
but also by its perioperative
kinetics after CPB. Indeed,
PCT was only transiently
increased after CPB, whereas
the increase in WBC and CRP
was more prolonged and CRP
occurs similarly in infected
Figure 2. Comparison of the receiver operating characteristic curves showing the relation between sensitivity and noninfected patients
(true positive) and 1-specificity (true negative) in determining the predictive value of procalcitonin (PCT) (value (Fig. 1). Therefore, PCT might
on postoperative day [POD] 7), PCT variation (values of POD6 to POD1), C-reactive protein (CRP) (maximum be useful in the early recogni-
value on POD2), and WBC (value on POD2) for the diagnosis of postoperative infection.
tion of an infection after CPB.
Nevertheless, it should be
After CPB, activation of inflammatory cascades may occur, pointed out that the diagnostic properties of PCT could not be
and this reaction shows strong similarity to those observed in observed during the first 3 PODs (Fig. 1 and Table 2).
sepsis (16). In our study, we described the postoperative PCT, After CPB, the cutoff value of PCT as a marker of infection
CRP, and WBC kinetics after cardiac surgery with CPB (Fig. 1) remains a matter of debate. Aouifi et al (22) showed that, in the
and observed that they were all significantly increased after CPB. presence of fever, PCT was reliable for diagnosis of infection
The postoperative rise observed in the noninfected patients after cardiac surgery, with sensitivity and specificity, respec-
is in agreement with previous studies (8, 11, 17). Indeed, an tively, at 0.85 and 0.95, and with a cutoff value of 1 ng/mL.
increase in PCT after CPB in the absence of postoperative Using a cutoff value of 0.5 ng/mL, Al Nawas et al (23) found
infection has already been noted by Minami et al (18). Our sensitivity and specificity of 60% and 79%, respectively. In
study observed an elevated PCT greater than 3 ng/mL within our study, for prediction of infection by PCT, the sensitiv-
3 days after CPB, and no differences between the infected and ity and specificity were 89% and 71%, and with a cutoff value
noninfected patients. This increase interferes with the diag- of 0.97 ng/mL on the POD5, whereas sensitivity and specific-
nosis of infection during the immediate postoperative period. ity on POD6 were 81% and 79% with a threshold of 0.86 ng/
However, in contrast to WBC and CRP that remain elevated mL, and a threshold of 0.80 ng/mL on POD7 had a sensitivity
for up to 1 week after surgery even in the absence of infection, of 70% and a specificity of 89%. However, it should be pointed
PCT has a transient rise and decreased progressively to nor- out that this threshold could be modified by the clinical condi-
mal value by POD5 in the absence of infection. PCT has been tions of the patient. Indeed, we observed high PCT values (>
Table 4. Multivariate Analysis Between the Infection and the Noninfection Groups
95% CI
Variable p OR Inferior Superior
Postoperative day 7 procalcitonin 0.013 3.23 1.28 8.14
PICU stay 0.046 1.52 1.01 2.29
OR = odds ratio.
Pediatric Critical Care Medicine www.pccmjournal.org 7
Copyright © 2017 by the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies.
Unauthorized reproduction of this article is prohibited
Li et al
infections (24). Conversely,
we noted that the diagnosis of
infected patients could occur
earlier with continuous PCT
monitoring, allowing an ear-
lier administration of antibi-
otics in infected patients, and
it should be emphasized that
an earlier therapeutic inter-
vention may improve the
prognosis in sepsis and severe
sepsis (3).
Several limitations should
be considered to interpret this
study. First, it was an observa-
tional analysis whose results
support an association and not
necessarily causation. Second,
data come from a single cen-
ter and institution-specific
variables may have influenced
the present results. Therefore,
our results must be further
validated by other multicenter
studies. Third, there were many
Figure 3. Correlation between the infected patient’s timing of infection and the absolute value of procalcitonin manipulations of the PCT data
(PCT) on the day of infection. POD = postoperative day.
and its clinical utility is thus
decreased. A more straightfor-
1 ng/mL) during the first 7 PODs in 19 infected patients, and a
ward data analysis without manipulation could improve the
second increase of PCT between the fourth and seventh PODs
generalizability and utility of the findings. And how to improve
in the other 26 infected patients, and at this time, no clinical
the generalizability and utility of the findings will be the direc-
sign of an infection was evident. There was no significant cor-
tion of our research work in the future.
relation between timing of infection and the absolute value of
PCT (Fig. 3). In summary, the dynamic change of PCT is more
important than the absolute value to predict postoperative CONCLUSIONS
infection, and the maintenance of a high level and/or a delayed PCT was more accurate than CRP and WBC to predict early
increase in PCT beyond the first 3 PODs could be used as an postoperative infection, but the diagnostic properties of PCT
indicator of postoperative infection. could not be observed during the first 3 PODs due to the
Our study provides some interesting information regard- inflammatory process related to CPB. The dynamic change of
ing the kinetics of PCT that is important for conducting future PCT is more important than the absolute value to predict post-
research. First, it is obvious that, because of the inflammatory operative infection. The maintenance of a high level (PCT >
process related to CPB, all biomarkers increased during the first 1.0 ng/mL) within 7 days after surgery and/or a second increase
3 PODs, thus precluding any diagnostic usefulness (Fig. 1). At in PCT between the fourth and the seventh PODs could be
least in pediatric cardiac surgery, only the maintenance of a high used as an indicator of postoperative infection. Continuous
level and/or a delayed increase in PCT beyond the early period PCT monitoring might help to discover infection earlier and
could be used as an indicator of postoperative infection. This to know in whom there is a need for intensified monitoring.
has several important consequences: 1) timing of the dosage is
an important issues; 2) the early postoperative period, during ACKNOWLEDGMENTS
which the diagnostic value of the biomarker is expected to be We would like to thank the nurses and staff of the PICU and
null because of the inflammatory process, should be precisely pediatric cardiac surgery department at Fuwai Hospital for
defined; and 3) beyond that early period, any maintenance of a their valuable contributions to our project.
high level or further increase in the biomarker should be con-
sidered for the diagnosis of postoperative infection.
From our study, we thought the diagnostic value of PCT REFERENCES
1. Laffey JG, Boylan JF, Cheng DC: The systemic inflammatory
would help to decide which patients should be treated with anti- response to cardiac surgery: Implications for the anesthesiologist.
biotics, as already shown in patients with lower respiratory tract Anesthesiology 2002; 97:215–252
8 www.pccmjournal.org XXX 2017 • Volume XX • Number XXX
Copyright © 2017 by the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies.
Unauthorized reproduction of this article is prohibited
Cardiac Intensive Care
2. Abraham E, Matthay MA, Dinarello CA, et al: Consensus confer- 13. El Oakley RM, Wright JE: Postoperative mediastinitis: Classification
ence definitions for sepsis, septic shock, acute lung injury, and acute and management. Ann Thorac Surg 1996; 61:1030–1036
respiratory distress syndrome: Time for a reevaluation. Crit Care Med 14. Hanley JA, McNeil BJ: A method of comparing the areas under
2000; 28:232–235 receiver operating characteristic curves derived from the same cases.
3. Rivers E, Nguyen B, Havstad S, et al; Early Goal-Directed Therapy Radiology 1983; 148:839–843
Collaborative Group: Early goal-directed therapy in the treatment of 15. Lacour-Gayet F, Clarke D, Jacobs J, et al; Aristotle Committee: The
severe sepsis and septic shock. N Engl J Med 2001; 345:1368–1377 Aristotle score for congenital heart surgery. Semin Thorac Cardiovasc
4. Assicot M, Gendrel D, Carsin H, et al: High serum procalcitonin Surg Pediatr Card Surg Annu 2004; 7:185–191
concentrations in patients with sepsis and infection. Lancet 1993; 16. Aouifi A, Piriou V, Blanc P, et al: Effect of cardiopulmonary bypass
341:515–518 on serum procalcitonin and C-reactive protein concentrations. Br J
5. Gendrel D, Assicot M, Raymond J, et al: Procalcitonin as a marker Anaesth 1999; 83:602–607
for the early diagnosis of neonatal infection. J Pediatr 1996;
17. Prat C, Ricart P, Ruyra X, et al: Serum concentrations of procalcitonin
128:570–573
after cardiac surgery. J Card Surg 2008; 23:627–632
6. Harbarth S, Holeckova K, Froidevaux C, et al; Geneva Sepsis
18. Minami E, Ito S, Sugiura T, et al: Markedly elevated procalcitonin in
Network: Diagnostic value of procalcitonin, interleukin-6, and inter-
early postoperative period in pediatric open-heart surgery: A prospec-
leukin-8 in critically ill patients admitted with suspected sepsis. Am J
Respir Crit Care Med 2001; 164:396–402 tive cohort study. J Intensive Care 2014; 2:38–42
7. Claeys R, Vinken S, Spapen H, et al: Plasma procalcitonin and 19. Oberhoffer M, Karzai W, Meier-Hellmann A, et al: Sensitivity and
C-reactive protein in acute septic shock: Clinical and biological cor- specificity of various markers of inflammation for the prediction of
relates. Crit Care Med 2002; 30:757–762 tumor necrosis factor-alpha and interleukin-6 in patients with sepsis.
Crit Care Med 1999; 27:1814–1818
8. Lecharny JB, Khater D, Bronchard R, et al: Hyperprocalcitonemia in
patients with perioperative myocardial infarction after cardiac surgery. 20. Gendrel D, Raymond J, Assicot M, et al: Measurement of procalcito-
Crit Care Med 2001; 29:323–325 nin levels in children with bacterial or viral meningitis. Clin Infect Dis
1997; 24:1240–1242
9. Dörge H, Schöndube FA, Dörge P, et al: Procalcitonin is a valuable
prognostic marker in cardiac surgery but not specific for infection. 21. BalcI C, Sungurtekin H, Gürses E, et al: Usefulness of procalcitonin
Thorac Cardiovasc Surg 2003; 51:322–326 for diagnosis of sepsis in the intensive care unit. Crit Care 2003;
10. Prat C, Ricart P, Ruyra X, et al: Serum concentrations of procalcitonin 7:85–90
after cardiac surgery. J Card Surg 2008; 23:627–632 22. Aouifi A, Piriou V, Blanc P, et al: Effect of cardiopulmonary bypass
11. Kallel S, Abid M, Jarraya A, et al: [Kinetics, diagnostic and prognostic on serum procalcitonin and C-reactive protein concentrations. Br J
value of procalcitonin after cardiac surgery]. Ann Biol Clin (Paris) Anaesth 1999; 83:602–607
2012; 70:567–580 23. Al Nawas B, Krammer I, Shah PM: Procalciltorin in diagnosis of
12. Society of Critical Care Medicine Consensus Conference Committee, severe infections. Eur J Med Res 1996; 1:331–333
American College of Chest Physicians/Society of Critical Care 24. Christ-Crain M, Jaccard-Stolz D, Bingisser R, et al: Effect of pro-
Medicine Consensus Conference: Definitions for sepsis and organ calcitonin-guided treatment on antibiotic use and outcome in lower
failure and guidelines for the use of innovative therapies in sepsis. Crit respiratory tract infections: Cluster-randomised, single-blinded inter-
Care Med 1992; 20:864–874 vention trial. Lancet 2004; 363:600–607
Pediatric Critical Care Medicine www.pccmjournal.org 9
Copyright © 2017 by the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies.
Unauthorized reproduction of this article is prohibited
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Httpswatermark Silverchair Com - Ezproxy.unbosque - edu.Copedsinreview.2022005642.Pdftoken AQECAHi208BE49Ooan9kkhW Ercy7Dm3ZL 9Document10 pagesHttpswatermark Silverchair Com - Ezproxy.unbosque - edu.Copedsinreview.2022005642.Pdftoken AQECAHi208BE49Ooan9kkhW Ercy7Dm3ZL 9darlingcarvajalduquePas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Early Progressive Mobility Protocol: Step 1: Screen For SafetyDocument2 pagesEarly Progressive Mobility Protocol: Step 1: Screen For SafetydarlingcarvajalduquePas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Nihms 1646158Document30 pagesNihms 1646158darlingcarvajalduquePas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Pediatric Pain AssessmentDocument10 pagesPediatric Pain AssessmentdarlingcarvajalduquePas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Post-Intensive Care Syndrome: Its Pathophysiology, Prevention, and Future DirectionsDocument14 pagesPost-Intensive Care Syndrome: Its Pathophysiology, Prevention, and Future DirectionsdarlingcarvajalduquePas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Early Progressive Mobility Protocol: Step 1: Screen For SafetyDocument2 pagesEarly Progressive Mobility Protocol: Step 1: Screen For SafetydarlingcarvajalduquePas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- De-Escalation of Critical Care and Prevention of Iatrogenicity Through PICU Liberation Rounding Process and A Daily Rounding ChecklistDocument1 pageDe-Escalation of Critical Care and Prevention of Iatrogenicity Through PICU Liberation Rounding Process and A Daily Rounding ChecklistdarlingcarvajalduquePas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Acutebrainfailure: Pathophysiology, Diagnosis, Management, and Sequelae of DeliriumDocument59 pagesAcutebrainfailure: Pathophysiology, Diagnosis, Management, and Sequelae of DeliriumdarlingcarvajalduquePas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- PALS Algorithms 2019 (Pediatric Advanced Life Support)Document1 pagePALS Algorithms 2019 (Pediatric Advanced Life Support)darlingcarvajalduquePas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Protocolo FATE (Eco TT)Document4 pagesProtocolo FATE (Eco TT)darlingcarvajalduquePas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Pals TachycardiaDocument1 pagePals TachycardiadarlingcarvajalduquePas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Pals Pediatric BradycardiaDocument1 pagePals Pediatric BradycardiadarlingcarvajalduquePas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Pediatric ShockDocument19 pagesPediatric ShockdarlingcarvajalduquePas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- SDOM Promising TherapiesDocument16 pagesSDOM Promising TherapiesdarlingcarvajalduquePas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Pediatric Dermatology MCQsDocument53 pagesPediatric Dermatology MCQsDr.Tawheed89% (18)
- Etextbook 978 0134019192 Microbiology With Diseases by TaxonomyDocument62 pagesEtextbook 978 0134019192 Microbiology With Diseases by Taxonomylashawn.fain938100% (49)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Preparedness For A High-Impact Respiratory Pathogen Pandemic PDFDocument84 pagesPreparedness For A High-Impact Respiratory Pathogen Pandemic PDFchinzsteelPas encore d'évaluation
- Differential Leukocytes CountDocument2 pagesDifferential Leukocytes CountSalmanPas encore d'évaluation
- SalmonellosisDocument26 pagesSalmonellosiscrazieelorraPas encore d'évaluation
- Q22019 CD Bulletin Vol 10 Issue 2 22 Dec 2019Document28 pagesQ22019 CD Bulletin Vol 10 Issue 2 22 Dec 2019Leo TrileoPas encore d'évaluation
- Ascaris LumbricoidesDocument15 pagesAscaris LumbricoidesJyoti DasPas encore d'évaluation
- Presentation DiarrheaDocument23 pagesPresentation DiarrheaVenkatesh KS 233Pas encore d'évaluation
- OIE Listed DiseaseDocument3 pagesOIE Listed DiseaseSamia KhanPas encore d'évaluation
- Neuromuscular Diseases in ChildrenDocument40 pagesNeuromuscular Diseases in ChildrenSven OrdanzaPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- BCG Hepatitisb Hexa1 Hexa2 Penta: Baby Immunization Schedule - QatarDocument3 pagesBCG Hepatitisb Hexa1 Hexa2 Penta: Baby Immunization Schedule - QatarKiran Kumar AkulaPas encore d'évaluation
- CAstV Biochek Slacum WVPA 2017 PDFDocument23 pagesCAstV Biochek Slacum WVPA 2017 PDFJimeno Franscisco de los pozosPas encore d'évaluation
- Vesicular Exanthema of Swine Virus VESVDocument9 pagesVesicular Exanthema of Swine Virus VESVAngelie OngPas encore d'évaluation
- 6 Epidemiology Public HealthDocument14 pages6 Epidemiology Public HealthPrince Marcos CortezPas encore d'évaluation
- The Respiratory System: Human AnatomyDocument47 pagesThe Respiratory System: Human AnatomyChelseaPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- 2009-10-16 Current Antiviral Recommendations For Influenza TreatmentDocument2 pages2009-10-16 Current Antiviral Recommendations For Influenza Treatmenttamiprior5294Pas encore d'évaluation
- Brugia MalayiDocument8 pagesBrugia MalayiROn Ace DancelPas encore d'évaluation
- Degradation Study of Metronidazole in Active and Different Formulation by Uv SpectrosDocument4 pagesDegradation Study of Metronidazole in Active and Different Formulation by Uv SpectrosEstefany LunaPas encore d'évaluation
- Anatomy and Physiology of BloodDocument10 pagesAnatomy and Physiology of Bloodaoi_rachelle100% (1)
- Disease Project Handout and RubricDocument1 pageDisease Project Handout and Rubricapi-409240655Pas encore d'évaluation
- Perinatal and Neonatal MortalityDocument40 pagesPerinatal and Neonatal MortalityDuncan Jackson0% (1)
- They Made Me Brave: Reflections On Women in LeadershipDocument36 pagesThey Made Me Brave: Reflections On Women in LeadershipOxfamPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Pandemic Expansion Guide v6Document5 pagesPandemic Expansion Guide v6jorgePas encore d'évaluation
- ABSTRACTBOOKMASTERforwebupdated20 3 14Document289 pagesABSTRACTBOOKMASTERforwebupdated20 3 14itaPas encore d'évaluation
- ImmunizationDocument50 pagesImmunizationDiscover APas encore d'évaluation
- Feline Pemphigus Foliaceus - A Retrospective Analysis of 57 Cases (Pages 313-321)Document9 pagesFeline Pemphigus Foliaceus - A Retrospective Analysis of 57 Cases (Pages 313-321)jenPas encore d'évaluation
- Food Code HaccpDocument37 pagesFood Code HaccpjucabrerasoPas encore d'évaluation
- The Pathogenic Basis of Malaria: InsightDocument7 pagesThe Pathogenic Basis of Malaria: InsightRaena SepryanaPas encore d'évaluation
- Lesson Plan AIDSDocument14 pagesLesson Plan AIDSS GPas encore d'évaluation
- Lecture 19 Notes - Mucosal ImmunityDocument5 pagesLecture 19 Notes - Mucosal ImmunityAlbert Mao LiPas encore d'évaluation
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)D'EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Évaluation : 3 sur 5 étoiles3/5 (1)