Académique Documents
Professionnel Documents
Culture Documents
Journal - Albumin in Critical Ill
Transféré par
Muhammad DickyCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Journal - Albumin in Critical Ill
Transféré par
Muhammad DickyDroits d'auteur :
Formats disponibles
TATM 2003;5(4):397-400
Should Albumin Be Used to )
(
Correct Hypoalbuminemia
in the Critically Ill? Yes
SUMMARY
Hypoalbuminemia is frequent in critically ill patients and is associated with worse
outcomes. From the limited clinical data available, it would seem that replenishing
J EAN -L OUIS V INCENT, MD , PhD
low albumin levels in hypoalbuminemic critically ill patients may be of benefit.
DEPARTMENT OF INTENSIVE CARE
ERASME HOSPITAL Nevertheless, deciding exactly which patients to treat and what level of serum
FREE UNIVERSITY OF BRUSSELS albumin to aim for remains uncertain. The results of prospective, randomized
BRUSSELS, BELGIUM
controlled trials are urgently needed to provide intensivists with sufficient, high-
grade evidence on which to base decisions regarding albumin use. In the meantime,
however, there is no reason to ban the use of albumin in the critically ill patient.
• Albumin
• Hypoalbuminemia
• Critically ill
• Safety
Transfusion Alternatives in Transfusion Medicine 397 ) VOLUME 5 NUMBER 4 OCTOBER 2003
( Page
Albumin in the Critically Ill: Pro J E A N -L O U I S V I N C E N T
Recent years have seen increasing debate and controversy over frequently occurs in the critically ill patient, passage of fluid into
the use of albumin in critically ill patients. Meta-analyses have the interstitial space increases considerably, and maintenance of
been published with apparently conflicting conclusions,1,2 oncotic pressure becomes relatively more important. In patients
moratoriums on the use of albumin have been called for by some3 with hypovolemic shock, colloid infusion, including albumin, is
while others have leapt honorably to its defense,4 and the associated with less edema formation than crystalloid infusion.10
intensivist is left trying to weigh up the evidence. Although some
questions had been raised earlier,5 the story really kick-started Substance Binding
with the publication in 1998 of a meta-analysis by the respected
In addition to the effects of albumin on COP, albumin has many
Cochrane group on the administration of albumin solutions.1 The
other physiological properties, which make it a valuable
authors concluded that the overall relative risk of death in patients
resuscitation fluid. Albumin functions as the principal binding
receiving albumin solutions was 1.68 compared with non-albumin
protein of various endogenous and exogenous substances,
recipients, suggesting that for every 17 critically ill patients treated
including drugs and metabolites. Albumin is also a secondary or
with albumin there is one additional death. This study attracted
tertiary carrier for some substances that have specific binding
considerable media attention with headlines such as “Burns
proteins, for example, steroids, including derivatives such as
treatment ‘kills thousands’” (Daily Telegraph, UK). However,
vitamin D and thyroxine.11 For drugs that are strongly linked to
albumin has been used widely around the world for more than
albumin and those with narrow therapeutic ranges,
60 years. Should we discard it on the basis of this one, highly
hypoalbuminemia will increase the free fraction of the drug,
criticized article? Let us briefly look at some of the evidence in
potentially leading to an increased or even toxic effect.12,13
support of albumin.
Metabolic and Antioxidant Activities
Properties of Albumin Albumin is involved in the metabolism of endogenous
substances such as lipids and eicosanoids. Albumin can stabilize
Maintenance of Oncotic Pressure some eicosanoids during metabolism, such as prostaglandin I2
and thromboxane A2; it can increase the release of arachidonate
Albumin accounts for about 80% of the normal oncotic
from macrophages; and it seems to favor lipo-oxygenase over
pressure.6 Critically ill patients have a lowered COP, and this is
cyclo-oxygenase.11 Albumin also has important oxygen free radical
associated with worsened outcome.7 When capillary permeability
scavenging properties, with albumin able to inhibit the production
is normal, a decreased COP is associated with an increased
of oxygen free radicals by polymorphonuclear leucocytes14 and
filtration rate across the capillaries, resulting in edema in most
in septic patients albumin administration can increase plasma
tissues, although the lung is relatively insensitive to extravascular
thiol levels,15 thiols, themselves, being scavengers of reactive
fluid shifts caused by lowering of the COP, due to the efficacy of
oxygen and nitrogen species. Although the clinical significance
the pulmonary lymph drainage and the high pulmonary interstitial
of these effects remains untested, hypoalbuminemic patients may
protein concentration.8 The main determinant of fluid exchange
thus have reduced potential for oxygen free scavenging and
in the lung is the hydrostatic force, and when pulmonary
increased susceptibility to the effects of these toxic agents.
hydrostatic pressure is normal, a fall in oncotic pressure is of little
importance;9 however, when hydrostatic pressure increases, as
Antithrombotic Properties
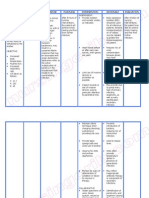
Table 1.
Albumin influences coagulation in a similar way to heparin,
Suggested Beneficial and Harmful Effects of Albumin possibly related to the similarity in the structure of the two
Potentially beneficial molecules.11 Albumin decreases platelet aggregation16 and has
• Decreased edema antithrombotic effects.17 There is an intimate connection between
– improved gas exchange
– improved wound healing the coagulation system and the inflammatory response, supported
– earlier mobilization by the fact that the only immunomodulating therapy so far shown
– improved tolerance to feeding to be effective in treating sepsis is drotrecogin alfa (activated), a
• Anti-platelet effects
• Anti-thrombotic effects recombinant form of the natural anticoagulant, activated protein
• Improved microcirculation C.18 The effects of albumin on this interaction may be important.
Potentially harmful
• Fluid overload – pulmonary edema Effects of Albumin on the Microcirculation
• Altered myocardial contractility (decreased calcium availability)
• Worsening of edema (leakage of larger molecules in the interstitium) There is evidence that albumin might beneficially influence the
• Increased blood losses (anti-hemostatic and anti-platelet effects)
microcirculation, although this remains controversial. Albumin
• Impaired water and sodium excretion/renal failure
• Altered immune response seems to reduce increases in capillary permeability; the
Transfusion Alternatives in Transfusion Medicine 398 ) VOLUME 5 NUMBER 4 OCTOBER 2003
( Page
Albumin in the Critically Ill: Pro J E A N -L O U I S V I N C E N T
mechanisms behind these effects are unclear but may be related beneficial, and indeed this approach has been evaluated in a
to the size of the albumin molecule simply blocking the channels, number of studies.34-39 However, these studies focused on specific
or some effect of the strong negative charge repelling other populations and extrapolation to the general ICU patient may be
negatively charged particles in the capillary membrane.11 In a rat difficult. Nevertheless, a recent randomized controlled trial of
model of hemorrhagic shock, Horstick et al. noted markedly albumin administration in critically ill hypoalbuminemic patients
reduced rolling and adherent leukocytes, maximum velocity, and does support a beneficial effect of albumin replacement,40 and a
shear rate in the mesenteric microcirculation after administration recent meta-analysis assessed the effects of correcting
of albumin.19 hypoalbuminemia as reported in 9 prospective studies involving
535 patients.27 Analysis of dose-dependency in these controlled
Anti-Apoptotic Effects trials of albumin therapy suggested that complication rates may
be reduced when the serum albumin level attained during
Some of the effects on the microcirculation may be related to
albumin administration exceeds 30 g/L. In addition, if correction
the anti-apoptotic effects of albumin. Apoptosis is a normal
of hypoalbuminemia is considered, the optimal albumin
phenomenon involved in vascular remodeling, but it may be
concentrations to which therapy should be targeted by have not
disturbed in certain situations. Several studies have demonstrated
been clearly defined.
anti-apoptotic effects of albumin,20,21 possibly mediated in part by
Liver disease, and particularly cirrhosis, is frequently associated
its effects on calcium metabolism.20
with hypoalbuminemia. In a study of 126 patients with cirrhosis
and spontaneous bacterial peritonitis, Sort et al.41 randomized
patients to receive treatment with cefotaxime or cefotaxime plus
Adverse Events intravenous albumin. The results showed a reduced incidence of
renal impairment and reduce mortality rates in the group treated
Albumin solutions have an excellent long-term safety profile.22,23
with intravenous albumin in addition to the antibiotic. In 126
A recent study covering 1.62 x 107 albumin doses noted that
patients with cirrhosis and ascites, albumin was shown to be
despite likely increased reporting of adverse events since the
effective in improving the rate of response to diuretic therapy and
Cochrane meta-analysis,1 the incidence of all serious adverse
preventing recurrence of ascites.42
events was 5.28 per 106 doses, and no patient death was classified
The use of albumin as a general resuscitation fluid in all critically
as probably related to albumin administration.23
ill patients is less obvious and results of randomized controlled
studies, such as that recently completed in Australasia (the Saline
versus Albumin Fluid Evaluation [SAFE] study) where saline was
Use of Albumin in Critically Ill Patients compared with albumin in the fluid resuscitation of critically ill
patients, are urgently awaited, although this may not provide all
Hypoalbuminemia is frequent in the critically ill patient,24 and
the answers as it studied albumin as a resuscitation fluid rather
may be the result of a variety of factors including decreased
than specifically to correct hypoalbuminemia.
synthesis or increased catabolism, renal or gut losses, dilution
secondary to fluid infusion, and redistribution secondary to
increased vascular permeability.25 Hypoalbuminemia is associated
with worse outcomes in intensive care unit patients. In a review
Conclusion
of the literature, mortality was reported to increase by 24 to 56%
Albumin has well-established, unique and wide-ranging
for each 2.5 g/L decrease in albumin concentration,26 and more
properties, and hypoalbuminemia is associated with poorer
recently, in a meta-analysis of 90 cohort studies including a total
outcomes. From the limited clinical data available, it would seem
of 291,433 patients, for each 10 g/L decrease in albumin, the
that replenishing low albumin levels in hypoalbuminemic critically
mortality was increased by 137%, morbidity by 89%, and ICU
ill patients may be of benefit. Nevertheless, deciding exactly which
and hospital lengths of stay by 28% and 71%, respectively.27 In
patients to treat and what level of serum albumin to aim for
this study, the association between hypoalbuminemia and poor
remains uncertain. The results of prospective, randomized
outcome was independent of the patient’s nutritional and
controlled trials are urgently needed to provide intensivists with
inflammatory status. Other studies have also demonstrated a link
sufficient, high-grade evidence on which to base decisions
between hypoalbuminemia and various outcome measures
regarding albumin use. In the meantime, however, there is no
including mortality,28-30 ICU length of stay,31 ventilator
reason to ban the use of albumin in the critically ill patient
dependency,31,32 and the development of acute respiratory distress
syndrome (ARDS) in patients with sepsis.33
The poor prognosis associated with hypoalbuminemia suggests
that raising serum albumin levels back towards normal may be
Transfusion Alternatives in Transfusion Medicine 399 ) VOLUME 5 NUMBER 4 OCTOBER 2003
( Page
Albumin in the Critically Ill: Pro J E A N -L O U I S V I N C E N T
R E F E R E N C E S
1. Cochrane Injuries Group. Human albumin administration in 16. Jorgensen KA, Stoffersen E. On the inhibitory effect of 32. Sapijaszko MJ, Brant R, Sandham D, Berthiaume Y.
critically ill patients: systematic review of randomized albumin on platelet aggregation. Thromb Res 1980;17:13-8. Nonrespiratory predictor of mechanical ventilation
controlled trials. BMJ 1998;317:235-40. 17. Joorgensen KA, Stoffersen E. Heparin like activity of dependency in intensive care unit patients. Crit Care Med
2. Wilkes MM, Navickis RJ. Patient survival after human albumin. Thromb Res 1979;16:569-74. 1996;24:601-7.
albumin administration. A meta-analysis of randomized, 18. Bernard GR, Vincent JL, Laterre PF, et al. Efficacy and 33. Mangialardi RJ, Martin GS, Bernard GR, et al.
controlled trials. Ann Intern Med 2001;135:149-64. safety of recombinant human activated protein C for severe Hypoproteinemia predicts acute respiratory distress syndrome
3. Offringa M. Excess mortality after human albumin sepsis. N Engl J Med 2001;344:699-709. development, weight gain, and death in patients with sepsis.
administration in critically ill patients. Clinical and Ibuprofen in Sepsis Study Group. Crit Care Med
19. Horstick G, Lauterbach M, Kempf T, et al. Early albumin 2000;28:3137-45.
pathophysiological evidence suggests albumin is harmful. BMJ infusion improves global and local hemodynamics and reduces
1998;317:223-4. inflammatory response in hemorrhagic shock. Crit Care Med 34. Brown RO, Bradley JE, Bekemeyer WB, Luther RW. Effect
4. Allison SP, Lobo DN. Debate: Albumin administration should 2002;30:851-5. of albumin supplementation during parenteral nutrition on
not be avoided. Crit Care 2000;4:147-50. hospital morbidity. Crit Care Med 1988;16:1177-82.
20. Zoellner H, Hofler M, Beckmann R, et al. Serum albumin is
5. AF, van Wilgenburg MG, de Laat PH, van der Hoven B. a specific inhibitor of apoptosis in human endothelial cells. 35. Foley EF, Borlase BC, Dzik WH, Bistrian BR, Benotti PN.
Albumin abuse in intensive care medicine. Intensive Care Med J Cell Sci 1996;109(Pt 10):2571-80. Albumin supplementation in the critically ill. A prospective,
1988;14:554-7. randomized trial. Arch Surg 1990;125:739-42.
21. Zoellner H, Hou JY, Lovery M, et al. Inhibition of
6. Weil MH, Henning RJ, Puri VK. Colloid oncotic pressure: microvascular endothelial apoptosis in tissue explants by 36. Wojtysiak SL, Brown RO, Roberson D, Powers DA, Kudsk
clinical significance. Crit Care Med 1979;7:113-6. serum albumin. Microvasc Res 1999;57:162-73. KA. Effect of hypoalbuminemia and parenteral nutrition on
free water excretion and electrolyte-free water resorption. Crit
7. AS, Gabel JC, McLeavey CA. Relation between lowered 22. von H, I, Waller C. Safety of human albumin based on Care Med 1992;20:164-9.
colloid osmotic pressure, respiratory failure, and death. Crit spontaneously reported serious adverse events. Crit Care Med
Care Med 1977;5:239-40. 2001;29:994-6. 37. Golub R, Sorrento JJ Jr, Cantu R Jr, Nierman DM,
Moideen A, Stein HD. Efficacy of albumin supplementation
8. Van der Linden P. [Clinical practice interpretation of oncotic 23. Vincent JL, Wilkes MM, Navickis RJ. Safety of human in the surgical intensive care unit: a prospective, randomized
pressure, serum albumin and protein determination and their albumin: Serious adverse events reported worldwide in 1998- study. Crit Care Med 1994;22:613-9.
ability for guiding therapeutics in cases of disturbances of 2000. Br J Anaesth 2003; in press.
capillary exchanges]. Ann Fr Anesth Reanim 1996;15:456-63. 38. Rubin H, Carlson S, DeMeo M, Ganger D, Craig RM.
24. Herrmann FR, Safran C, Levkoff SE, Minaker KL. Serum Randomized, double-blind study of intravenous human
9. Guyton AC, Granger HJ, Taylor AE. Interstitial fluid albumin level on admission as a predictor of death, length of albumin in hypoalbuminemic patients receiving total
pressure. Physiol Rev 1971;51:527-63. stay, and readmission. Arch Intern Med 1992;152:125-30. parenteral nutrition. Crit Care Med 1997;25:249-52.
10. Rackow EC, Falk JL, Fein IA, et al. Fluid resuscitation in 25. Margarson MP, Soni N. Serum albumin: touchstone or 39. Martin GS, Mangialardi RJ, Wheeler AP, Dupont WD,
circulatory shock: a comparison of the cardiorespiratory totem? Anaesthesia 1998;53:789-803. Morris JA, Bernard GR. Albumin and furosemide therapy in
effects of albumin, hetastarch, and saline solutions in patients 26. Goldwasser P, Feldman J. Association of serum albumin and hypoproteinemic patients with acute lung injury. Crit Care
with hypovolemic and septic shock. Crit Care Med mortality risk. J Clin Epidemiol 1997;50:693-703. Med 2002;30:2175-82.
1983;11:839-50.
27. Vincent JL, Dubois MJ, Navickis RJ, Wilkes MM. 40. Dubois MJ, Orellana-Jimenez C, Melot C, et al.
11. Nicholson JP, Wolmarans MR, Park GR. The role of albumin Hypoalbuminemia in acute illness: is there a rationale for Administration of albumin in hypoalbuminemic patients. A
in critical illness. Br J Anaesth 2000;85:599-610. intervention? A meta-analysis of cohort studies and controlled prospective, randmized controlled, pilot study. Crit Care Med
12. Lindow J, Wijdicks EF. Phenytoin toxicity associated with trials. Ann Surg 2003;237:319-34. 2003;31:A108.
hypoalbuminemia in critically ill patients. Chest 28. Pollak AJ, Strong RM, Gribbon R, et al. Lack of predictive 41. Sort P, Navasa M, Arroyo V, et al. Effect of intravenous
1994;105:602-4. value of the APACHE II score in hypoalbuminemic patients. albumin on renal impairment and mortality in patients with
13. Tincani E, Mazzali F, Morini L. Hypoalbuminemia as a risk JPEN J Parenter Enteral Nutr 1991;15:313-5. cirrhosis and spontaneous bacterial peritonitis. N Engl J Med
factor for over-anticoagulation. Am J Med 2002;112:247-48. 29. Gibbs J, Cull W, Henderson W, Daley J, Hur K, Khuri SF. 1999;341:403-9.
14. Holt ME, Ryall ME, Campbell AK. Albumin inhibits human Preoperative serum albumin level as a predictor of operative 42. Gentilini P, Casini-Raggi V, Di Fiore G, et al. Albumin
polymorphonuclear leucocyte luminol-dependent mortality and morbidity: results from the National VA Surgical improves the response to diuretics in patients with cirrhosis
chemiluminescence: evidence for oxygen radical scavenging. Risk Study. Arch Surg 1999;134:36-42. and ascites: results of a randomized, controlled trial. J Hepatol
Br J Exp Pathol 1984;65:231-41. 30. Blunt MC, Nicholson JP, Park GR. Serum albumin and 1999;30:639-45.
15. Quinlan GJ, Margarson MP, Mumby S, et al. colloid osmotic pressure in survivors and nonsurvivors of
Administration of albumin to patients with sepsis syndrome: a prolonged critical illness. Anaesthesia 1998;53:755-61.
possible beneficial role in plasma thiol repletion. Clin Sci 31. Murray MJ, Marsh HM, Wochos DN, Moxness KE, Offord
(Lond) 1998;95:459-65. KP, Callaway CW. Nutritional assessment of intensive-care
unit patients. Mayo Clin Proc 1988;63:1106-15.
Transfusion Alternatives in Transfusion Medicine 400 ) VOLUME 5 NUMBER 4 OCTOBER 2003
( Page
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- SAGO AdultObsDocument2 pagesSAGO AdultObsTim BrownPas encore d'évaluation
- Emergency Care Algorithms 2018 PDFDocument77 pagesEmergency Care Algorithms 2018 PDFFranklin Correa100% (2)
- Toxicology RecallDocument601 pagesToxicology RecallMuhammad Dicky100% (1)
- What Is SepticemiaDocument3 pagesWhat Is SepticemiaYhna Nesperos GelverioPas encore d'évaluation
- HeritageDocument116 pagesHeritageVarshaPas encore d'évaluation
- Highlights - ACLS - LinearizedDocument34 pagesHighlights - ACLS - LinearizedRayssaPas encore d'évaluation
- DSM 5 PTSDDocument2 pagesDSM 5 PTSDAnonymous Pj6Odj100% (1)
- Pediatric Septic ShockDocument24 pagesPediatric Septic ShockBRENDA AMAROPas encore d'évaluation
- Referat Wound HealingDocument60 pagesReferat Wound HealingMuhammad DickyPas encore d'évaluation
- Nursing Care Plan Neonatal SepsisDocument2 pagesNursing Care Plan Neonatal Sepsisderic100% (20)
- Infectious Diseases MCQDocument34 pagesInfectious Diseases MCQfrabziPas encore d'évaluation
- Sepsis: PathophysiologyDocument8 pagesSepsis: PathophysiologyDonald NashPas encore d'évaluation
- Lewiss Medical Surgical Nursing Assessment and Management of Clinical Problems 12Th Edition Mariann M Harding Full ChapterDocument68 pagesLewiss Medical Surgical Nursing Assessment and Management of Clinical Problems 12Th Edition Mariann M Harding Full Chapterroy.saunders943100% (8)
- Court County Death: Minnesota Hennepin GeegndjudicialDocument10 pagesCourt County Death: Minnesota Hennepin GeegndjudicialGoMNPas encore d'évaluation
- Sacral Fusion & Tarlov Cyst TreatmentDocument28 pagesSacral Fusion & Tarlov Cyst TreatmentMuhammad DickyPas encore d'évaluation
- TB/HIV A CLINICAL MANUAL (Second Edition 2004) World Health Organization WHODocument212 pagesTB/HIV A CLINICAL MANUAL (Second Edition 2004) World Health Organization WHOJulio Iñigo López100% (5)
- Gallstones: Gabriel E NjezeDocument7 pagesGallstones: Gabriel E NjezeMuhammad DickyPas encore d'évaluation
- Combat Associated Penetrating Spine InjuryDocument21 pagesCombat Associated Penetrating Spine InjuryMuhammad DickyPas encore d'évaluation
- Template Nama SertifikatDocument1 pageTemplate Nama SertifikatMuhammad DickyPas encore d'évaluation
- Am J Crit Care 2005 Futterman 438 40Document4 pagesAm J Crit Care 2005 Futterman 438 40Muhammad DickyPas encore d'évaluation
- Hand Hygiene Why How and When BrochureDocument7 pagesHand Hygiene Why How and When BrochureLeis FatwaPas encore d'évaluation
- Efektivitas Kelas Ibu Hamil Terhadap Deteksi Dini Tanda Bahaya KehamilanDocument5 pagesEfektivitas Kelas Ibu Hamil Terhadap Deteksi Dini Tanda Bahaya KehamilanIlalang GurunPas encore d'évaluation
- Morning Report Rsud Natuna: Sabtu, 9 Desember 2017 Minggu, 10 Desember 2017Document16 pagesMorning Report Rsud Natuna: Sabtu, 9 Desember 2017 Minggu, 10 Desember 2017Muhammad DickyPas encore d'évaluation
- Efektivitas Kelas Ibu Hamil Terhadap Deteksi Dini Tanda Bahaya KehamilanDocument5 pagesEfektivitas Kelas Ibu Hamil Terhadap Deteksi Dini Tanda Bahaya KehamilanIlalang GurunPas encore d'évaluation
- InstructionsDocument1 pageInstructionsMuhammad DickyPas encore d'évaluation
- GNL 6 172 PDFDocument16 pagesGNL 6 172 PDFAkh AdiibPas encore d'évaluation
- Hiv Staging 150307Document52 pagesHiv Staging 150307Taufan Prasetya AgungPas encore d'évaluation
- Applying Baldridge Organizational Effectiveness Model For Accreditation of Higher Education InstitutionDocument9 pagesApplying Baldridge Organizational Effectiveness Model For Accreditation of Higher Education InstitutionMuhammad DickyPas encore d'évaluation
- Penatalaksanaan Ketoasidosis Diabetik (Kad)Document13 pagesPenatalaksanaan Ketoasidosis Diabetik (Kad)Emir AfifPas encore d'évaluation
- Tugas Ujian Penyakit DalamDocument13 pagesTugas Ujian Penyakit DalamMuhammad DickyPas encore d'évaluation
- Pengenalan AnestesiDocument49 pagesPengenalan AnestesiMuhammad DickyPas encore d'évaluation
- Abstract Red Bettle InfusionDocument1 pageAbstract Red Bettle InfusionMuhammad DickyPas encore d'évaluation
- Icd 10Document4 pagesIcd 10mellyfr100% (1)
- Curiculum Vitae Iyere Faith-1Document4 pagesCuriculum Vitae Iyere Faith-1Halleluyah HalleluyahPas encore d'évaluation
- Medical Emergencies GuidebookDocument211 pagesMedical Emergencies GuidebookNadreen OsmanPas encore d'évaluation
- Indications and Hemoglobin Thresholds For Red Blood Cell Transfusion in The Adult - UpToDateDocument39 pagesIndications and Hemoglobin Thresholds For Red Blood Cell Transfusion in The Adult - UpToDateAhmed MostafaPas encore d'évaluation
- Compensated Shock Due To SepsisDocument5 pagesCompensated Shock Due To SepsisAlexandr SergeevichPas encore d'évaluation
- Perbedaan Pengaruh Parasetamol Dan Parecoxib Terhadap Aktivitas Agregasi Trombosit Pada Pasien SIRS Atau SepsisDocument10 pagesPerbedaan Pengaruh Parasetamol Dan Parecoxib Terhadap Aktivitas Agregasi Trombosit Pada Pasien SIRS Atau SepsisPratiwi IshakPas encore d'évaluation
- High-Flow Nasal Oxygen-The Pendulum Continues To Swing in The Assessment of Critical Care TechnologyDocument2 pagesHigh-Flow Nasal Oxygen-The Pendulum Continues To Swing in The Assessment of Critical Care TechnologyRodrigoSachiFreitasPas encore d'évaluation
- Septic ArthritisDocument8 pagesSeptic ArthritisLorebell100% (2)
- E PosterDocument1 pageE PosterIlham AjiPas encore d'évaluation
- Use of Vasopressors and InotropesDocument16 pagesUse of Vasopressors and InotropesIrving H Torres LopezPas encore d'évaluation
- Welcome To The Morning SessionDocument23 pagesWelcome To The Morning SessionGENERAL sharpPas encore d'évaluation
- Sri Rahayu PDFDocument14 pagesSri Rahayu PDFMoh RamliPas encore d'évaluation
- Shock Hipovolemico EnmascaradoDocument11 pagesShock Hipovolemico EnmascaradowiwiPas encore d'évaluation
- Anaesthesia: Update inDocument7 pagesAnaesthesia: Update inhabtishPas encore d'évaluation
- IV In-Line Filters CochraneDocument19 pagesIV In-Line Filters CochraneMarzuki Panji WijayaPas encore d'évaluation
- Past Paper - 221208 - 003047Document96 pagesPast Paper - 221208 - 003047Ashraf ShalbiPas encore d'évaluation
- Icu Antibiotic GuidelinesDocument4 pagesIcu Antibiotic GuidelinesTia MonitaPas encore d'évaluation
- Top 10 Pearls For The Recognition, Evaluation, And.246Document16 pagesTop 10 Pearls For The Recognition, Evaluation, And.246Vemuri SrinivasPas encore d'évaluation
- BucensDocument6 pagesBucensEmily GirardPas encore d'évaluation