Académique Documents
Professionnel Documents
Culture Documents
Makalah Oma Edited
Transféré par
Daniel Sukmadja0 évaluation0% ont trouvé ce document utile (0 vote)
31 vues12 pagesTitre original
makalah oma edited.docx
Copyright
© © All Rights Reserved
Formats disponibles
DOCX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
31 vues12 pagesMakalah Oma Edited
Transféré par
Daniel SukmadjaDroits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 12
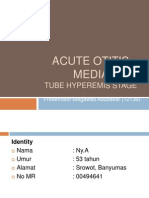
CASE REPORT
ACUTE OTITIS MEDIA
Presented by:
Audiza Luthffia 13/350442/KU/16009
Ayu Larasati Sukarno 13/346237/KU/15698
Dian Rahmawati 13/346688/KU/15860
Joshepine Debora Uli 13/352456/KU/16058
Joshua Andrew 13/348775/KU/15922
Patria Aditya Arimukti 13/346366/KU/15761
Stephani Novia Wijaya 13/349279/KU/15945
Moderated by:
dr. Ashadi Prasetyo, M.Sc, Sp.THT-KL
Departement of Otorhinolaryngology, Head and Neck Surgery
Faculty of Medicine Universitas Gadjah Mada
Dr Sarjito Hospital
2017
INTRODUCTION of all culture-positive cases),
Haemophylus influenzae (40–45%),
Acute otitis media (AOM) is one
Streptococcus pyogenes (1–5%) and
of the most commonly occurring
Moraxella catarrhalis (1–5%).6
inflammatory diseases of infancy and
childhood and the third most frequent The pathogenesis of AOM
reason for prescription of antibiotics in begins with eustachian tube
this age group.1 More than 50% of the dysfunction. The Eustachian tube
children will have at least one episode preserves normal middle ear
of AOM by the age of one year. The conditions through three primary
disease is most frequent between 6 functions: clearance of middle ear
and 13 months of age.2 fluid, ventilation, and protection from
nasopharyngeal reflux. The
Acute otitis media is
mucociliary wave transports middle
inflammatory diseases of the middle
ear secretions toward the
ear with particular involvement of the
nasopharing. When a precipitating
tympanic cavity.3 The risk factor of
event, such as viral URTI or allergic
AOM are genetic predisposition,
rhinitis, triggers nasal mucosal
premature birth, male gender, family
inflammation, obstruction of the tubal
history of recurrent otitis media,
orifice leads to fluid stasis. Individuals
presence of siblings in the household,
with narrower and horizontally
young age, day care attendance,
oriented anatomy, cleft palate, or
exposure to smoking, lack of breast
tensor veli palatini deficiency have
feeding, supine feeding position, use
impaired drainage and are at higher
of pacifiers, family history of recurrent
risk for tubal dysfunction. Tubal
AOM, craniofacial abnormalities and
dysfunction induces a negative
low socioeconomic status.4 AOM is
pressure in middle ear resulting in
related to upper respiratory infection
tympanic membrane retraction and
(URTI); in 94% of patient URTI
transudation into tympanic cavity.
proceeds AOM, one in three children
Middle ear effusion caused by
will develop AOM after URTI.5
transudation becomes a favorable
The most frequent bacterial media for bacterial growth resulting in
pathogens causing AOM are infection of bacteria in timpanic cavity.
Streptococcus pneumoniae (40–45% The pus formation in the middle ear
push the tympanic membrane (bulging The 2013 U.S. AOM Guidelines
appearance of tympanic membrane) . recommended features for the
Continuous pus formation increase definition of AOM which is the
tension in tympanic membrane results presence of moderate to severe
in ischemia and necrosis of tympanic bulging of the tympanic membrane or
membrane. Necrosis in tympanic new onset of otorrhea not due to acute
membrane appears as tympanic otitis externa, presence of mild bulging
membrane perforation, this of the tympanic membrane and an
perforation allows passage of pus to acute (within 48 hours) onset of
outer ear canal. Resolutions of earache (holding, tugging, rubbing of
perforation will occur if patient is the ear in a nonverbal child) or intense
immunocompetent and the bacterial erythema of the tympanic membran,
virulence is low.7 and presence of medial ear efussion
based on pneumatic otoscopy and/or
The clinical practice guideline for
tympanometry.9
diagnosis and management of AOM
reported by the American Academy of Clinical manifestations of acute
Pediatrics provides that a diagnosis of otitis media are different based on its
AOM requires signs and symptoms stage. The first stage is tubal
such as recent, usually abrupt, onset occlusion which manifests as
of signs and symptoms of middle-ear retracted tympanic membrane, dull or
inflammation and effusion; presence normal tympanic membrane,
of middle ear effusion, indicated by symptom of deafness may pass
any bulging of the tympanic unnoticed especially in children, pain,
membrane, limited or absent mobility if occur, not so severe and may
of the tympanic membrane, air-fluid described as fullness. Second, stage
level behind the tympanic membrane, of pre-suppuration/hyperemic,
and otorrhea; and signs or symptoms manifests as hyperemic/injection of
of middle-ear inflammation as tympanic membrane due to vessels
indicated by either distinct erythema of engorgement, at this stage fever and
the tympanic membrane or distinct restlessness may start, increase of
earache (discomfort results in earache and deafness. Third, stage of
precludes normal activity or sleep). 8 suppuration manifests as edema,
bulging of tympanic membrane due to
presence of pus in the middle ear, sensation, or hearing impairment were
severe earache that can precludes denied. Her parents stated that 1 week
normal activity or sleep, and fever may before the visit, the patient has history
reach 39,50C.10 of having upper respiratory tract
infection manifested as cough, sore
Fourth, stage of perforation, in
throat, runny nose, and nasal
this stage spontaneous rupture of
congestion. The cough and nasal
tympanic membrane results in fall in
symptoms has reduced by taking
temperature, earache decreases, and
some over the counter drugs, but the
discharge could be purulent,
parents forget the drugs name. There
mucopurulent or bloody. Last, stage
were no similar complaints prior to the
of resolution, discharge may stop
visit. The girl has no history of allergy
within two days, most of the symptoms
or atopic history in the family. There
resolve except for hearing impairment
were no family history related to the
due to residual effusion. The aim of
complaints as well as similar
acute otitis media therapy are opening
complaints in the family.
tubal occlusion using decongestant,
decreasing earache and discomfort Physical examination of the
using analgetic, and treating infection right ear was within the normal limit.
using antibiotic. Acute otitis media While for the physical examination of
stage perforation also needs frequent the left ear from inspection the
aural toilets/cleaning.10 anatomy of the auricula was normal,
no redness and swelling of the
CASE REPORT
auricula were seen. There were no
A six year-old girl presented to pain when auricula was retracted as
ENT clinic RSUD Banyumas on 25th well as when the tragus was palpated.
2017 with chief complain of pain in the Inspection of the ear canal was not
left ear since last night. Her parents hyperemic or edema. There were no
also complained of fever, irritable, discharge seen in the ear canal. The
difficult to fall asleep, and frequently tympanic membrane was still intact
waking up after falling asleep last but hyperemic upon inspection. Cone
night. No history of ear discharge. of light was not visible.
Other conditions such as dizzy, head
Physical examination of both
and face pain, buzzing sound
left and right nose showed no
anatomic abnormality, slight concha In this case, the patient has
edema, no hyperemic and minimal history of URTI. The patient suffered
discharge was seen. Physical from cough, runny nose, nasal
examination of the throat also within congestion, and mild fever a week
the normal limit, the pharyng was not before the ear symptoms appear.
hyperemic and no granule was seen.
As mention before, upper
The tonsil size was T1 in both right
respiratory infection has a relation with
and left tonsils, and also not
incidence of otitis media (OM). A
hyperemic.
research conducted by Chonmaitree
Based on history-taking and et al show relation between URTI
physical examination, patient was caused by virus infection with
then diagnosed with hyperemic stage incidence of OM. Rhinovirus and
of acute otitis media. Patient was adenovirus were among the most
prescribed with Amoxicilin forte syrup frequently detected causative agent
2 teaspoon 3 times daily, Rhinos found in patients with URI. The overall
Junior syurp 1 teaspoon 2 times daily, incidence of OM following was 61%,
Paracetamol syrup 1 ½ teaspoon 3 including a 37% incidence of AOM and
times daily as medications. Duration of a 24% incidence of otitis media
treatment is 7 days. effusion (OME). AOM occurred in
approximately one-half of children
Patient was given education to
with URTI due to adenovirus,
complete the antibiotic treatment
respiratory syncytial virus, or
course and to take all medications
coronavirus and in approximately one-
according to the recommendation.
third of those with URI due to influenza
Patient was also told to prevent
virus, parainfluenza virus, enterovirus,
recurrency of the upper respiratory
or rhinovirus. AOM and OME was
infection, and avoid manipulating the
diagnosed on days 1–24 in the course
ear. The patient was advised to be
of URI, with the peak occurring on
follow up in the following week, after 7
days 3–5, the median time was day 4
days of treatment.
for AOM and day 3 for OME.11
While for the bacterial studies,
DISCUSSION Revai et al published a research that
show nasopharyngeal cultures were
85.6% positive for pathogenic bacteria disrupts the mucociliary system and
in URTI. S. Pneumoniae was isolated impairs the ear’s primary mechanical
alone or combination with another barrier from bacterial invasion. In
bacterial in 34% of the cases, H. addition, eustachian-tube dysfunction
influenzae was isolated in 34%, and can lead to reduced middle-ear
M. catarrhalis was isolated in 69%.12 pressure, which forces mucus,
nasopharyngeal secretions, and
Thirty five percent of URTI
bacteria into the middle ear; this
episodes were complicated by AOM.
creates an ideal milieu for bacterial
AOM diagnosis peaked on day 3, and
superinfection.13
85% of AOM episodes were
diagnosed within 7 days after URTI The highest incidence of AOM
onset. The Odd Ratio showed after URTI to be between 6 and 11
increased risk of AOM when the months of age.13 The increased
nasopharynx was colonized with susceptibility to AOM in younger
pathogenic bacteria (S. pneumoniae, children has been postulated to be
NT H. influenzae, or M. catarrhalis), secondary to inadequate immunologic
compared with no pathogen. The 3 response and a shorter, straighter,
pathogenic bacteria, either alone or in and narrower Eustachian tube. The
combination, were more likely to be anatomical features of eustachian
isolated from samples from children tube in pediatrics makes the
with AOM than from samples from progession of the infection at upper
children without AOM. Compared with respiratory tract to the middle ear
a child with no bacteria in the more possible than those in adults.
nasopharynx, a child with 2 types of The horizontal direction of drainage
bacteria in the nasopharynx was 2.6 into throat in pediatrics makes the
times as likely to have AOM.12 migration of pathogen to the middle
ear easier than the gravity assisted
Bacteria colonized in the
vertical direction of drainage in adults.
nasopharing enter the middle ear via
The shorter tube length in pediatrics
the eustachian tube. Normally,
also gives the pathogen a shorter
bacteria are prevented from entering
pathway to reach the middle ear. It
the middle ear by the ciliated
stands to reason that the taller
epithelium that lines the eustachian
children are protected from exposure
tube. Respiratory virus infection
to known avoidable otitis media risk effective for moderate or severe pain.
factors, the later the onset of AOM and But the use of narcotics requires
the lower their lifetime incidence.14 prescription, and consideration of the
side effects, such as risk of respiratory
In this case, the patient
depression, altered mental status,
recieved amoxicilin forte syrup,
gastrointestinal upset, and
Rhinos Junior syrup, and Paracetamol
constipation.15 The route of
syrup as medications.
administration is more preferred in oral
Based on American Academy route rather than ear drop because the
of Family Physicians (AAFP), there administration analgesic ear drops
are three recommendations for AOM should be delayed until examination
treatment which are the use of the whole tympanic membrane is
analgesics, observational protocol, performed. Administration of
and antibiotics. analgesic ear drops is not
First recommendation, the use recommended in children under 3
of analgesics. The goal of analgesic years old without a previous tympanic
administration is to relieve pain in membrane visualization because
patients with AOM since pain is one of there is not a solid evidence of
the most troublesome complain in efficacy, it is not safe in case of
AOM. Ramakrishnan et al stated that spontaneous perforation, and may
acetaminophen or ibuprofen are alter the otoscopic assessment
effective analgesics to treat mild to because of cerumen fluidification.17
moderate pain.15 Bertin et al conduct The second recommendation is
a multicenter randomized double-blind the observational treatment. This
controlled study and conclude that the protocol has been proved to reduce
analgesics effect of ibuprofen was the use of antibiotics in 56% 6 months-
significant compared to a placebo, but 12 years old patient.18 Observation
no significant analgesic effect of without use of antibacterial agents in a
acetaminophen was observed.16 But child with uncomplicated AOM is an
recent study stated that option for selected children based on
acetaminophen can be used for diagnostic certainty, age, illness
treating pain in AOM. Narcotic severity, and assurance of follow-up.
analgesia with codeine or analogs is This option should be limited to
otherwise healthy children 6 months to >39oC).15 If antibiotics is indicated, the
2 years of age with non-severe illness first line is amoxicillin 80-
at presentation and an uncertain 90mg/kg/day. In patient with severe
diagnosis, and to children 2 years of infection and if the patient is infected
age and older without severe beta lactamase producing
symptoms at presentation or with an Haemophillus influenza and Moraxella
uncertain diagnosis. In these catarrhalis, the regimen should start
situations observation provides an with high dose Amoxicillin clavulanat
opportunity for the patient to improve (90mg/kg/day Amoxicillin dan
without antibacterial treatment. The 6,4mg/kg/day clavulanat divided in 2
indications of observational protocol doses). If the patient is allergic to
are absent of fever or vomit, parents penicillin, and the reaction is not type I
and patient agreed to delay antibiotics hypersensitivity (urticarial or
administration. While the relative anaphylactic reaction), the patient can
contraindications are history of be given cefdinir (14 mg/kg/day in 1 or
antibiotic treatment within the last 2 2 doses), cefpodoxime (10 mg/kg/day
weeks and present of otorrhea. The once daily), or cefuroxime (30
use of this protocol refer to delay in mg/kg/day in 2 divided doses) can be
antibiotic treatment for selected used. In cases of Type I reactions,
patients with no complications for 72 azithromycin (10 mg/kg/day on day 1,
hours or more. During the followed by 5 mg/kg/day x 4 days as a
observational period, the patients only single daily dose) or clarithromycin (15
receive symptomatic treatment mg/kg/day in 2 divided doses) can be
including analgesics. Antibiotic used in an effort to select an
treatment should be initiate if antibacterial agent of an entirely
symptoms of AOM persist until the different class. Other possibilities
third day.19 include erythromycin-sulfisoxazole
(50 mg/kg/day of erythromycin) or
Antibiotics are recommended
sulfamethoxazole-trimethoprim (6–10
for all children under 6 months, 6
mg/kg/day trimethoprim). Alternative
months – 2 years with certain
therapy in the penicillin-allergic patient
diagnosis, and for children above 2
who is being treated for infection that
years old with severe infection
is known or presumed to be caused by
(moderate to severe otalgia or fever
penicillin-resistant S pneumoniae is
clindamycin at 30 to 40 mg/kg/day in 3 Histamine interacts with
divided doses. In the patient who is histamin receptors such as H1, H2,
vomiting or cannot otherwise tolerate H3, H4. H1 receptor is responsible for
oral medication, a single dose of allergic reaction. Interaction of
parenteral ceftriaxone (50 mg/kg) has histamine with H1 receptor causes
been shown to be effective for the vasodilatation, thus increasing
initial treatment of AOM.15 vascular permeability. This condition
could lead to congestion.
If the patient fails to respond to
Antihistamine works by binding to H1
the initial management option within
receptor competitively. It will prevent
48 to 72 hours, the clinician must
the interaction between histamine and
reassess the patient to confirm AOM
H1 receptor.20
and exclude other causes of illness. If
AOM is confirmed in the patient Decongestan stimulates alpha-
initially managed with observation, the adrenergic receptor resulting in
clinician should begin antibacterial vasoconstriction of dilated arteries,
therapy. If the patient was initially decreasing the edema and mucus
managed with an antibacterial agents, formation.21
the clinician should change the
However, the use of
antibacterial agents.
antihistamine and/or decongestant
Since the patient is already 6 only have a little clinical effect, thus
years old (more than 2 years old) and are not recommended for routine in
the diagnosis of AOM is already AOM treatment.22 In this case, the
established, the patient fulfil the patient was given antihistamine and
criteria for antibiotic therapy. decongestant to relieve the nasal
symptom.
As for the symptomatic
treatment for this case, the patient CONCLUSION
were given Rhinos Junior syrup
A 6-year-old girl patient was
containing 15 mg pseudoefedrin and 1
diagnosed with hyperemic stage of
mg chlorpheniramine maleate / 5ml
acute otitis media. Patient was
and Paracetamol (acetaminophen
prescribed with Amoxicilin forte syrup,
class which act as analgetic as well as
Rhinos Junior syurp, Paracetamol
antipyretic).
syrup as medications for 7 days.
REFERENCES 7. Coticchia JM, Chen M,
Sachdeva L, Mutchnick S. New
Paradigms in the Pathogenesis
1. Agrawal S, Husein M, MacRae
of Otitis Media in Children.
D: Complications of otitis
Frontiers in Pediatrics.
media: an evolving state. J
2013;1:52.
Otolaryngol. 2005; 34 Suppl 1:
8. American Academy of
33–39.
Pediatrics Subcommittee on
2. Kershner JE. Otitis media. In:
Management of Acute Otitis
Kliegman RM, Stanton BF,
Media 2004. Diagnosis and
Schor NF, St. Geme III JW,
management of acute otitis
Behrman RE, editors. Nelson
media. Subcommittee on
textbook of pediatrics. 19th ed.
Management of Acute Otitis
Philadelphia, PA: WB
Media: Pediatrics. 2004; 113:
Saunders; 2011 :p 2199–213.
1451-65.
3. Thomas JP, Berner R, Zahnert
9. Lieberthal AS, Carroll AE,
T, Dazert S: Acute otitis media:
Chonmaitree T, Ganiats TG,
a structured approach. Dtsch
Hoberman A, Jackson MA,
Arztebl Int 2014; 111(9): 151–
Joffe MD, Miller DT, Rosenfeld
60.
RM, Sevilla XD, Schwartz RH,
4. Uhari M, Mantysaari K,
Thomas PA, Tunkel DE: The
Niemela M. A meta-analytic
diagnosis and management of
review of the risk factors for
acute otitis media. Pediatrics
acute otitis media. Clin Infect
2013; 131:e964-e99
Dis. 1996;22:1079–1083
10. Djaafar ZA, Helmi, Restuti RD.
5. Shawabkeh MA, Larem H,
Kelainan Telinga Tengah. In
Albu-Mahmood Z, Alsaadi A,
Soepardi.E.A, N.Iskandar,
Alqahtani A. Acute Otitis
J.Bashiruddin, R.D.Restuti.
Media- An Update. Journal of
Buku Ajar Ilmu Kesehatan
Otolaryngology-ENT
Telinga Hidung Tenggorok
Research. 2017; 8 (4)
Kepala dan Leher. Edisi VII(7).
6. Hendley JO. Clinical practice.
Jakarta : Fakultas Kedokteran
Otitis media. N Engl J Med.
Universitas Indonesia. 2012; p.
2002;347:1169–74.
57-69
11. Chomnmaitree T, Revai K, G. A randomized, double-blind,
Grady J J, et al. Viral Upper multicentre controlled trial of
Respiratory Tract Infection and ibuprofen versus
Otitis Media Complication in acetaminophen and placebo
Young Children. Clinical for symptoms of acute otitis
Infectious Diseases. 2008; media in children. Fundam Clin
46:825-823 Pharmacol 1996; 10:387-92.
12. Revai K, Mamidi D, 17. Chiappini E, Bortone B, Doria
Chonmaitree T. Assosiation of M, et al. What not to do in acute
Nasopharyngeal Bacterial otitis media: the top five
Colonization during Upper recommendations proposed by
Respiratory Tract Infection and the Italian Society of Preventive
the Development of Acute and Social Pediatrics. Expert
Otitis Media. Clinical Infectious Review of Anti-infective
Diseases. 2008;. 46: 825-823 Therapy. 2017; p 1-6
13. Revai K, Dobbs LA, Nair S, et 18. Spiro DM, Tay, KY, Arnold DH,
al. Incidence of Acute Otitis Dziura JD, Baker MD, Shapiro
Media and Sinusitis ED. Wait and see prescription
Complicating Upper for the treatment of acute otitis
Respiratory Tract Infection: media. A randomized
The Effect of Age. Pediatrics. controlled trial. JAMA
2006; 119:e1408 2006;296(10):1235-41
14. Paradise JL. Otitis Media in 19. Helmi. Diagnosis dan
Infant and Children. Pediatrics. penatalaksanaan otitis media.
1980; 65:p 917 Dalam: Satelit symposium.
15. Ramakrishnan K, Sparks RA, Penanganan mutakhir kasus
Berryhill WE. Diagnosis and telinga hidung tenggorok,
treatment of otitis media. Am Jakarta; 2003.
Fam Physician. 20. Pohan SS. Mekanisme
2007;76(11):1650-58 Antihistamin pada Pengobatan
16. Bertin L, Pons G, d’Athis P, Penyakit Alergi : Blokade
Duhamel JF, Maudelonde C, Reseptor - Penghambatan
Lasfargues G, Guillot M, Aktivasi Reseptor. Majalah
Marsac A, Debregeas B, Olive
Kedokteran Indonesia. 2007;
57 : p 113
21. Corboz MR, Rivelli MA, Mingo
GG, et al. Mechanism of
Decongestant Activity of Alpha
2-adrenoceptor Agonists. Pulm
Pharmacol Ther. 2008;21(3):p
449-54
22. Coleman C, Moore M.
Decongestants and
Antihistamine for Acute Otitis
Media in Children. Cocharane
Database of Systematic
Review. 2008; 3
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- IMCI QuizDocument7 pagesIMCI QuizAndrea Yoo86% (22)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Final ExamDocument4 pagesFinal ExamLyka AndayogPas encore d'évaluation
- Pap 0106Document31 pagesPap 0106Bogdan PraščevićPas encore d'évaluation
- ENT TransDocument7 pagesENT TransanonymousPas encore d'évaluation
- MCQSDocument258 pagesMCQSmuhannedPas encore d'évaluation
- Infections of The EarDocument9 pagesInfections of The Earrumaisyah alkatiriPas encore d'évaluation
- Common Health Problems of Infancy PowptDocument78 pagesCommon Health Problems of Infancy PowptCiella Dela CruzPas encore d'évaluation
- Prevention and Control of Cough - Colds, FeverDocument11 pagesPrevention and Control of Cough - Colds, FeverAriannaPas encore d'évaluation
- Osce Notes in OtolaryngologyDocument94 pagesOsce Notes in OtolaryngologyDr. T. Balasubramanian92% (39)
- Cod Liver Oil - Setting The Record Straight - The Weston A. Price FoundationDocument5 pagesCod Liver Oil - Setting The Record Straight - The Weston A. Price FoundationRicardo BritoPas encore d'évaluation
- Perforated EardrumDocument5 pagesPerforated EardrumElvinPas encore d'évaluation
- Intercollegiate Surgical Curriculum ENTDocument98 pagesIntercollegiate Surgical Curriculum ENTMendhi Ashish AnilPas encore d'évaluation
- Otogenic MeningitisDocument15 pagesOtogenic Meningitisadam Nohe100% (1)
- Medical Abbreviations and Acronyms For Medical TermsDocument123 pagesMedical Abbreviations and Acronyms For Medical Termspenitentexclusi27Pas encore d'évaluation
- Operation Manual: Impedance Audiometer AT235/AT235hDocument117 pagesOperation Manual: Impedance Audiometer AT235/AT235hCarlos Eduardo Mendez AlvarezPas encore d'évaluation
- 10 Besar 1 TH 2017Document356 pages10 Besar 1 TH 2017dartosPas encore d'évaluation
- SleDocument893 pagesSleAsma Sikander100% (4)
- Ear Nose and Throat Assessment AdultDocument6 pagesEar Nose and Throat Assessment AdultProfit Street100% (2)
- Gradenigos Syndrome A ReviewDocument5 pagesGradenigos Syndrome A ReviewPaola SanchezPas encore d'évaluation
- Pharmacotherapy of Infectious Disease URTIDocument44 pagesPharmacotherapy of Infectious Disease URTIDigafe TolaPas encore d'évaluation
- Alawiya, Jamal Tango P.Document18 pagesAlawiya, Jamal Tango P.Jamal P. AlawiyaPas encore d'évaluation
- Sindrom GradenigoDocument5 pagesSindrom GradenigoKelompok F8 CoasPas encore d'évaluation
- Handbook of Specimen Collection and Handling in MicrobiologyDocument72 pagesHandbook of Specimen Collection and Handling in MicrobiologyMiguel MataPas encore d'évaluation
- (APJ) Common ENT CasesDocument31 pages(APJ) Common ENT CasesApryl Phyllis JimenezPas encore d'évaluation
- Diseases ListDocument49 pagesDiseases ListChandra Sekhar GajulaPas encore d'évaluation
- Acute Otitis MediaDocument71 pagesAcute Otitis MediaMegawati Abubakar0% (1)
- ENT in A Nutshell 2Document28 pagesENT in A Nutshell 2Gyleen ElegioPas encore d'évaluation
- Describe The Four Main Symptoms of ImciDocument2 pagesDescribe The Four Main Symptoms of ImciMartha JulyPas encore d'évaluation
- Respiratory Disorders of Pediatric Clients - NCLEX - HPMDocument35 pagesRespiratory Disorders of Pediatric Clients - NCLEX - HPMNadesPas encore d'évaluation
- Myringotomy PET PT INFODocument3 pagesMyringotomy PET PT INFOdhiahabsyiPas encore d'évaluation