Académique Documents
Professionnel Documents
Culture Documents
Pediatric CAP Guideline
Transféré par
John Vincent Dy OcampoDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Pediatric CAP Guideline
Transféré par
John Vincent Dy OcampoDroits d'auteur :
Formats disponibles
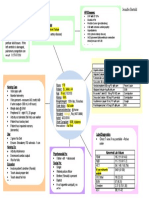
PEDIATRIC COMMUNITY-ACQUIRED PNEUMONIA CLINICAL GUIDELINE
Guideline Eligibility Criteria: Assessment: Respiratory status (rate for age,
Age 3 months to 17 years WOB, crackles, decreased or abnormal breath
Previously healthy children with no underlying conditions sounds), AMS, apnea, pulse ox < 90% on room
Clinical findings of CAP air, Immunization Status (DTaP, Pneumoccocal,
influenza, HiB), Exposure to TB
Guideline Exclusion:
Aspiration Intervention: oxygen to keep sats >92%, IVF if
Immunocompromised children clinically indicated.
Recent hospitalization (<7days before the onset of
illness)
Underlying lung disease or other chronic condition *Tachypnea*
Meets inpatient criteria: Age 0-2mo: >60
Age 2-12mo: >50
Outpatient Management O2 sats < 90% Age 1-5 yrs: >40
Influenza: oseltamivir (or NO Not tolerating PO Age >5 yrs: >20
zanamivir for children ≥7) Age 3 to 6 mo
Presumed bacterial: Respiratory distress WHO Criteria for severe illness
Not able to drink
Preferred: amoxicillin
persistent vomiting
(Alternative: augmentin) YES convulsions
PCN allergic: CTX, cefotaxime, lethargic or unconscious
or clindamycin Severely ill? stridor in a calm child
Presumed atypical: Azithromycin
NO YES
>5years old: Consider empiric
Inpatient Management:
addition of azithromycin
Severe or concern for Complicated CAP
Repeat CXR in 4-6 wks if concern Inpatient Management: CXR at admission
for lung collapse to r/o mass, Uncomplicated CAP Labs to consider: Flu/RSV if <3yrs, Flu if >3
anatomic anomaly CXR at admission yrs, (RVP only if Flu/RSV negative), Blood culture
No labs required x1, CRP/ESR (only to trend improvement)
Start therapy CBC is not helpful in trending disease or
determining viral vs bacterial cause
Start therapy
ANTI-MICROBIAL THERAPY
Continued Considerations Immunized
D/c antibiotics if RVP positive Ampicillin or penicillin G
D/c IVF when tolerating PO Alternatives (PCN allergic): ceftriaxone, cefotaxime, clindamycin
Change to oral antibiotics upon Not Fully Immunized for H. flu and S. pneumo
clinical improvement Ceftriaxone or cefotaxime
Repeat CXR if no clinical Resistant organism
improvement in 48 to 72 hrs
Ceftriaxone 100 mg/kg/day divided q12-24h
Discharge Criteria **Add macrolide only if M. pneumonia or C. pneumonia are
Tolerating PO significant considerations
No supplemental O2 for 12-24h
Respiratory rate normal for age **Start oseltamivir if influenza + or if high suspicion for influenza
even if test negative
If severely Ill consider:
Empiric influenza treatment
Created 6/2015. Based on IDSA CAP guidelines 2011.
CA-MRSA, add vancomycin or clindamycin
Temp>39? WBC >15,00Suspician for CA-MRSA?
Vous aimerez peut-être aussi
- Heal Yourself-The Natural WayDocument489 pagesHeal Yourself-The Natural Waygemoregold100% (18)
- History and Mental Status Exam GuideDocument17 pagesHistory and Mental Status Exam Guideyeney armenterosPas encore d'évaluation
- Pneumonia Cheat Sheet: by ViaDocument3 pagesPneumonia Cheat Sheet: by ViaGayle MariePas encore d'évaluation
- Concept Map HypertensionDocument1 pageConcept Map Hypertensiongeorge pearson0% (1)
- Completed Concept MapDocument4 pagesCompleted Concept Mapapi-607361848Pas encore d'évaluation
- System Disorder: Renal CalculiDocument1 pageSystem Disorder: Renal CalculiHolly DeckelmanPas encore d'évaluation
- Physical AssessmentDocument3 pagesPhysical AssessmentHyacinth ExmundoPas encore d'évaluation
- Basic Tools in NutritionDocument23 pagesBasic Tools in NutritionSeanmarie Cabrales0% (1)
- Concept MapDocument5 pagesConcept Mapapi-546509005Pas encore d'évaluation
- Quotes NursingDocument14 pagesQuotes NursingFreddy ÁlvaroPas encore d'évaluation
- Description: Congestive Heart FailureDocument22 pagesDescription: Congestive Heart FailurePinklet Arleena CubianPas encore d'évaluation
- 5P Handoff SheetDocument1 page5P Handoff SheetBarry SeeboPas encore d'évaluation
- Nursing AssessmentDocument16 pagesNursing AssessmentJihan Novita100% (1)
- Head to-Toe-Assessment Complete Guide - Nightingale CollegeDocument1 pageHead to-Toe-Assessment Complete Guide - Nightingale CollegeDabon RusselPas encore d'évaluation
- Fluidsandelectrolytes 090224074347 Phpapp02Document102 pagesFluidsandelectrolytes 090224074347 Phpapp02IsaacJ22Pas encore d'évaluation
- Stroke Signs, Risks, and Nursing CareDocument1 pageStroke Signs, Risks, and Nursing CareMariel Febreo MerlanPas encore d'évaluation
- Case Simu 101Document5 pagesCase Simu 101Princess Levie CenizaPas encore d'évaluation
- Legal/Forensic Medicine: Atty. Tony D. Rebosa, MD, BscrimDocument30 pagesLegal/Forensic Medicine: Atty. Tony D. Rebosa, MD, BscrimAlpana Laisom75% (4)
- Concept Map 2Document1 pageConcept Map 2lanrevoicePas encore d'évaluation
- Medical Surgical Nursing IIDocument52 pagesMedical Surgical Nursing IItwinkle143Pas encore d'évaluation
- Appendix 10 Patient Profile TemplateDocument6 pagesAppendix 10 Patient Profile TemplateAL Rizwan AsifPas encore d'évaluation
- Diabetes Mellitus Complte LONG 2Document56 pagesDiabetes Mellitus Complte LONG 2John Vincent Dy OcampoPas encore d'évaluation
- Diabetes Mellitus Complte LONG 2Document56 pagesDiabetes Mellitus Complte LONG 2John Vincent Dy OcampoPas encore d'évaluation
- Prof. Sandra M. Covarrubias - September 24, 2021: 5.2fluid & Electrolytes ImbalancesDocument5 pagesProf. Sandra M. Covarrubias - September 24, 2021: 5.2fluid & Electrolytes ImbalancesIvy VillalobosPas encore d'évaluation
- Educational Strategies For Children With Emotional and Behavioral ProblemsDocument74 pagesEducational Strategies For Children With Emotional and Behavioral Problemsmaeydel50% (2)
- Pediatric Concept MapDocument12 pagesPediatric Concept Mapapi-352157080Pas encore d'évaluation
- Care of Pediatric Client With Dermatologic DisorderDocument3 pagesCare of Pediatric Client With Dermatologic DisorderAraw GabiPas encore d'évaluation
- System Disorder ADDocument1 pageSystem Disorder ADSariahPas encore d'évaluation
- Waiters Rhabdomyolysis PDFDocument1 pageWaiters Rhabdomyolysis PDFmp1757Pas encore d'évaluation
- Pico Question WatchornDocument5 pagesPico Question Watchornapi-301725567Pas encore d'évaluation
- POC and Concepts Maps Week 12Document23 pagesPOC and Concepts Maps Week 12Michelle CollinsPas encore d'évaluation
- ACTIVE LEARNING TEMPLATE: System DisorderDocument1 pageACTIVE LEARNING TEMPLATE: System DisorderDeo FactuarPas encore d'évaluation
- Immersion Physical Exam Final - ChecklistDocument2 pagesImmersion Physical Exam Final - ChecklistElizalde HusbandPas encore d'évaluation
- Concept Map Meningitis TheoryDocument3 pagesConcept Map Meningitis TheoryMia AuliaPas encore d'évaluation
- Week 7 - Rheumatoid ArthritisDocument1 pageWeek 7 - Rheumatoid ArthritisTuTitPas encore d'évaluation
- Renal Concept MapDocument1 pageRenal Concept MapShaira Ann CalambaPas encore d'évaluation
- Newborn Care PDFDocument8 pagesNewborn Care PDFZedrake CaraanPas encore d'évaluation
- Acute and Chronic GastritisDocument6 pagesAcute and Chronic GastritisAnn CanPas encore d'évaluation
- Potential Complications Signs and SymptomsDocument2 pagesPotential Complications Signs and SymptomsJessica GomezPas encore d'évaluation
- CHF Concept MapDocument1 pageCHF Concept MapChristy Wegner Cooper100% (4)
- Nursing Care Plan for Patient with Gastric CancerDocument7 pagesNursing Care Plan for Patient with Gastric CancerHilario. Hayascent.Reign.M.Pas encore d'évaluation
- Concept Map 360Document6 pagesConcept Map 360api-273469220Pas encore d'évaluation
- Leoprolide Drug StudyDocument2 pagesLeoprolide Drug Studyhappymee927Pas encore d'évaluation
- Vancomycin Dosing and Monitoring in AdultsDocument1 pageVancomycin Dosing and Monitoring in AdultsjulialeoPas encore d'évaluation
- ATI Medication TemplateDocument1 pageATI Medication Templatephoenix180Pas encore d'évaluation
- Generic and Trade Names, Mechanisms, InterventionsDocument4 pagesGeneric and Trade Names, Mechanisms, InterventionsSonia FernandesPas encore d'évaluation
- Community Health Nursing Lecture: Family Health AssessmentDocument7 pagesCommunity Health Nursing Lecture: Family Health AssessmentSofia ResolPas encore d'évaluation
- Abdominal Assessment VideoDocument4 pagesAbdominal Assessment VideoAmber Nicole HubbardPas encore d'évaluation
- IVY TECH NURSING LAB INFORMATIONDocument7 pagesIVY TECH NURSING LAB INFORMATIONSethPas encore d'évaluation
- Teamworks! Game: Summary ReportDocument2 pagesTeamworks! Game: Summary ReportAngela May Pustasa AllamPas encore d'évaluation
- Fluids Electrolytes Visual NotesDocument8 pagesFluids Electrolytes Visual NotesVin Lorenzo CampbellPas encore d'évaluation
- Idiopathic Thrombocytopenic Purpura: Overview With Report of A CaseDocument4 pagesIdiopathic Thrombocytopenic Purpura: Overview With Report of A CaseHernan GonzalezPas encore d'évaluation
- Part I: Emergency Department (ED) : SKINNY ReasoningDocument6 pagesPart I: Emergency Department (ED) : SKINNY ReasoningUzumaki KPas encore d'évaluation
- DRUG STUDY FINAL (Onco) PDFDocument14 pagesDRUG STUDY FINAL (Onco) PDFFrancis Anthony LoslosoPas encore d'évaluation
- Medication - ALT-Template Polythene GlycolDocument1 pageMedication - ALT-Template Polythene GlycolNancyAmissahPas encore d'évaluation
- Care Plan FaringitisDocument63 pagesCare Plan FaringitisEnerolisa ParedesPas encore d'évaluation
- Case Study 101: Abdominal Aortic Aneurysm With Acute Kidney InjuryDocument8 pagesCase Study 101: Abdominal Aortic Aneurysm With Acute Kidney InjuryPatricia Ann Nicole ReyesPas encore d'évaluation
- IWU Nursing Care Plan for 81-Year-Old Female with CHF and PneumoniaDocument6 pagesIWU Nursing Care Plan for 81-Year-Old Female with CHF and PneumoniaclarimerPas encore d'évaluation
- Behavioral Health Care PlanDocument12 pagesBehavioral Health Care Planapi-520841770100% (1)
- Nursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument3 pagesNursing Care Plan: Assessment Diagnosis Inference Planning Intervention Rationale EvaluationJessa FabicoPas encore d'évaluation
- Data Collection and Patient DiagnosisDocument14 pagesData Collection and Patient DiagnosisJen CareyPas encore d'évaluation
- GRP 4 CLO 2 Concept Map PT 1 PDFDocument14 pagesGRP 4 CLO 2 Concept Map PT 1 PDFMaria Lyn Ocariza ArandiaPas encore d'évaluation
- ClindamycinDocument3 pagesClindamycinShaira TanPas encore d'évaluation
- Nursing Process Overview: Health Assessment NotesDocument40 pagesNursing Process Overview: Health Assessment NotesEliakim III InsongPas encore d'évaluation
- NANDA Nursing DiagnosesDocument8 pagesNANDA Nursing DiagnosesShreejana PrajapatiPas encore d'évaluation
- NURSING CARE OF ADULTS II: Passbooks Study GuideD'EverandNURSING CARE OF ADULTS II: Passbooks Study GuidePas encore d'évaluation
- COMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuideD'EverandCOMPREHENSIVE NURSING ACHIEVEMENT TEST (RN): Passbooks Study GuidePas encore d'évaluation
- Guidance on Evaluating and Treating UTIs and ASBDocument14 pagesGuidance on Evaluating and Treating UTIs and ASBJohn Vincent Dy OcampoPas encore d'évaluation
- Renal TuberculosisDocument43 pagesRenal TuberculosisPulse OfMedicoPas encore d'évaluation
- Pediatric Community-Acquired Pneumonia Clinical Guideline PDFDocument1 pagePediatric Community-Acquired Pneumonia Clinical Guideline PDFJohn Vincent Dy OcampoPas encore d'évaluation
- Manajemen Sepsis - SSCDocument8 pagesManajemen Sepsis - SSCDeborah Bravian TairasPas encore d'évaluation
- AcuteCoronary SyndromesDocument108 pagesAcuteCoronary SyndromesJohn Vincent Dy OcampoPas encore d'évaluation
- Chapter 95 Complications of Urologic Procedures and DevicesDocument39 pagesChapter 95 Complications of Urologic Procedures and DevicesJohn Vincent Dy OcampoPas encore d'évaluation
- Quality Sepsis Definitions SCCM ESICM Joint Session Critical Care CongressDocument88 pagesQuality Sepsis Definitions SCCM ESICM Joint Session Critical Care CongressSandritaAquinoPas encore d'évaluation
- Clinical Trials PhasesDocument2 pagesClinical Trials PhasespandabijoyPas encore d'évaluation
- Cap Guidelines Booklet 2010 UpdateDocument101 pagesCap Guidelines Booklet 2010 UpdateIcko DinopolPas encore d'évaluation
- Lower Respiratory Tract InfectionDocument21 pagesLower Respiratory Tract InfectionJohn Vincent Dy OcampoPas encore d'évaluation
- A LilingDocument3 pagesA LilingJohn Vincent Dy OcampoPas encore d'évaluation
- SCSD Application Summary Form PDFDocument2 pagesSCSD Application Summary Form PDFJoserie HernanePas encore d'évaluation
- Beat COVID-19 Situationer #004 (May 1)Document9 pagesBeat COVID-19 Situationer #004 (May 1)Glomarie Alyssa RacelisPas encore d'évaluation
- Basics of Critical Care.....Document34 pagesBasics of Critical Care.....XamanPas encore d'évaluation
- Physio Assess Form Oct 2022Document5 pagesPhysio Assess Form Oct 2022RishaadPas encore d'évaluation
- Handwashing NarrativeDocument9 pagesHandwashing NarrativeMaria Angelica BermilloPas encore d'évaluation
- Ovr New MohDocument2 pagesOvr New MohhyPas encore d'évaluation
- 243 471 1 SM PDFDocument6 pages243 471 1 SM PDFFia lutfiahPas encore d'évaluation
- En - 2316 9117 FP 26 04 380Document14 pagesEn - 2316 9117 FP 26 04 380Ana paula CamargoPas encore d'évaluation
- Estradiol 1mg + Norethisterone Acetate 0.5mg (Activelle)Document12 pagesEstradiol 1mg + Norethisterone Acetate 0.5mg (Activelle)asdwasdPas encore d'évaluation
- Faculty of Sport Science and Recreation Diploma in Sport Studies (Sr1132D) Sps220 - Nutrition For Health and ExerciseDocument6 pagesFaculty of Sport Science and Recreation Diploma in Sport Studies (Sr1132D) Sps220 - Nutrition For Health and ExerciseSyafiq MiqhaelPas encore d'évaluation
- INITIAL DATA BASE Form For Family 1Document5 pagesINITIAL DATA BASE Form For Family 1Reignallienn Inocencio MartinPas encore d'évaluation
- Efudix Leaflet With PicturesDocument2 pagesEfudix Leaflet With PicturesyehyaPas encore d'évaluation
- Database Clerk Vacancy in MawlamyineDocument3 pagesDatabase Clerk Vacancy in MawlamyineHein Min NaingPas encore d'évaluation
- 5ОМ англ ВОП 1Document22 pages5ОМ англ ВОП 1p69b24hy8pPas encore d'évaluation
- Renal Colic and Joint DeformitiesDocument19 pagesRenal Colic and Joint DeformitiesAhmad Syahmi YZ100% (1)
- Careers in Social Work: Outlook, Pay & MoreDocument9 pagesCareers in Social Work: Outlook, Pay & Morejoel lacayPas encore d'évaluation
- 4 Coercion in Mental Healthcare The Principle of Least Coercive CareDocument8 pages4 Coercion in Mental Healthcare The Principle of Least Coercive CarePedro Y. LuyoPas encore d'évaluation
- Mammograms and Other Breast Imaging Procedures: What Is A Mammogram?Document25 pagesMammograms and Other Breast Imaging Procedures: What Is A Mammogram?Marina StosicPas encore d'évaluation
- PHARMACOLOGY PrelimDocument26 pagesPHARMACOLOGY PrelimCrystal MiranaPas encore d'évaluation
- Dme Information Form Cms-10125 - External Infusion PumpsDocument2 pagesDme Information Form Cms-10125 - External Infusion PumpsSonof GoddPas encore d'évaluation
- STRDocument179 pagesSTRJatin AnandPas encore d'évaluation
- Konsult Sip ReportDocument72 pagesKonsult Sip ReportMohit AgarwalPas encore d'évaluation
- Cook 2009 Oropharyngeal DysphagiaDocument21 pagesCook 2009 Oropharyngeal DysphagiaDesiré MagalhãesPas encore d'évaluation
- Exams NAC Guideline Rating Scale PDFDocument2 pagesExams NAC Guideline Rating Scale PDFprakash13lPas encore d'évaluation
- HIV Testing and Management in IndonesiaDocument31 pagesHIV Testing and Management in IndonesiayurdiansyahPas encore d'évaluation