Académique Documents
Professionnel Documents
Culture Documents
NAG Gastrointestinal Infections As of Nov 2017
Transféré par
Rhod Bernaldez EstaTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
NAG Gastrointestinal Infections As of Nov 2017
Transféré par
Rhod Bernaldez EstaDroits d'auteur :
Formats disponibles
GASTROINTESTINAL TRACT INFECTIONS
I. ACUTE DIARRHEA AND GASTROENTERITIS
A. Acute Diarrhea in Children
Acute diarrhea is defined as diarrhea lasting less than 14 days. Mainstay of
treatment is to give fluids, zinc supplements, and food.
Classification of dehydration status of children 2 months to 5 years of age (IMCI
2014):
• Severe dehydration (when 2 of the following signs are present)
- Lethargic or unconscious
- Sunken eyes
- Not able to drink or drinking poorly
- Skin pinch goes back very slowly
• Some dehydration (when 2 of the following signs are present)
- Restless, irritable
- Sunken eyes
- Drinks eagerly, thirsty
- Skin pinch goes back slowly
• No dehydration (when there are not enough signs to classify patient’s
status as some or severe)
Etiology:
Community and hospital-based based studies in children < 5 years (Saniel et al
1982-84, Lucero et al 1982-83, Carlos et al 1989):
Salmonella: 10-15%, ETEC: 9-15%, Rotavirus: 7-17%
Etiology of acute diarrheas in developing countries expressed in weighted
annual incidence per 100 child years (Nelson’s Textbook of Pediatrics, 20th
edition, 2015):
<12 months: Rotavirus: 2.1-10.1, Enterotoxigenic Escherichia coli (ETEC): 0.7-
3.6, Cryptosporidium: 0.7-5.4
12-23 months: Rotavirus: 1.6-12.4, ETEC: 0.7-2.8, Shigella: 0.5-8.5
24-59 months: Rotavirus: 0.3-3.5, Shigella: 0.2-3.1, Vibrio cholera 01: 0.2-1.8
Preferred Regimen:
IMCI protocol Neonate up to 2 months: Child 2 months to 5 years:
Suspected Ciprofloxacin 30mg/kg/d PO Ciprofloxacin 30 mg/kg/d
dysentery: div 2 doses x 3d div 2 doses x 3d
Suspected Erythromycin 250mg PO qid
cholera: _____ x 3d OR Tetracycline 250mg
PO qid x 3d
National Antibiotic Guidelines 1
GASTROINTESTINAL TRACT INFECTIONS
Recommendations of Feigin and Cherry:
Indication Preferred Regimen:
Suspected antibiotic-associated Metronidazole 30mg/kg/d IV or PO div 4
colitis presenting as severe doses x 10-14d OR
disease or with prolonged Vancomycin 40mg/kg/d PO div 4 doses
symptoms especially for patients with severe disease
Suspected nontyphoidal Ciprofloxacin 30mg/kg/d IV div 2 doses x
Salmonella in the setting of 10-14d OR Azithromycin 6mg/kg/d PO qd x
severe diarrhea in infants less 5d OR Ceftriaxone 75-100 mg/kg/d IV q24h
than 6 months of age, x 14d
malnourished and
immunocompromised children
Campylobacter Azithromycin 10mg/kg/d PO x 3d OR
Erythromycin 40mg/kg/d PO div 4 doses x
5d
Entamoeba histolytica Metronidazole 35-50mg/kg/d PO div 3
doses x 7-10d
Giardia Metronidazole 15mg/kg/d PO div 3 doses x
5-7d
Cyclospora Trimethoprim-sulfamethoxazole 10 mg
TMP/50mg SMX/kg/d PO div 2 doses x 7-
10d
Comments:
For children with severe dehydration living in an area with reported cases of
cholera, give antibiotic for cholera. For cases of acute diarrhea with dysentery
(blood in the stool), give ciprofloxacin for 3 days. For suspected antibiotic-
associated colitis, mild disease does not warrant antibiotic treatment since
symptoms resolve within 7-10 days after discontinuing precipitating antibiotics.
Probiotic treatment of children with C. difficile diarrhea has not been well studied.
Immunization of infants starting at 6 weeks of age with either of 2 available live
attenuated rotavirus vaccines is recommended to afford protection against severe
rotavirus disease. The monovalent human rotavirus vaccine is given as a 2-dose
series and the pentavalent human bovine rotavirus vaccine is given as a 3-dose
series. Oral vancomycin is not available locally.
B. Gastroenteritis (infectious diarrhea) In adults
MILD DIARRHEA (≤3 unformed stools/day; minimal associated symptomatology)
Preferred Regimen: Oral Hydration
2 National Antibiotic Guidelines
GASTROINTESTINAL TRACT INFECTIONS
MODERATE DIARRHEA (3 - 4 unformed stools/day; with or without systemic
symptoms)
Preferred Regimen: Oral or Parenteral Hydration
Comments:
Try to make specific diagnosis, especially in patients with severe diarrhea or
systemic symptoms.
SEVERE DIARRHEA (≥ 6 unformed stools/day ± fever, tenesmus, blood or fecal
leukocytes)
Etiologies: Bacterial: Shigella sp., Salmonella sp., C. jejuni, C. difficile (Toxin
positive) E. coli (enterotoxigenic, enteroaggregative, Shiga-toxin producing) K.
oxytoca (Toxin producer); Parasitic: Giardia lamblia, E. histolytica,
Cryptosporidium
Preferred Regimen:
Empiric therapy: Specific therapy:
Ciprofloxacin 500mg PO q12h OR Entamoeba histolytica:
Levofloxacin 500mg PO q24h x 3–5d Metronidazole 500-750mg PO tid x 7-
OR Azithromycin 500mg PO q24h for 10d OR Tinidazole 2g PO qd x 3d
3d (preferred for Campylobacter) Vibrio cholera:
OR Cotrimoxazole DS PO bid x 3–5d Doxycycline 300mg x 1 dose OR
Tetracycline 500mg qid X 3d OR
Cotrimoxazole DS PO bid X 3d
Shigella species:
Cotrimoxazole DS PO bid X 3d OR
Ciprofloxacin 500mg PO bid X 3d
C. Primary spontaneous bacterial peritonitis (SBP)
Characterized by a patient with cirrhosis, ascites, fever, and ≥ 250 neutrophils/μl
of ascitic fluid.
Etiology:
P: S. pneumoniae (30-50%; most common), E. coli (25-40%), Staphylococci (2-4%),
Group A Streptococcus, Enterococci, Klebsiella pneumoniae
A: Enterobacteriaceae, S. pneumoniae, Enterococcus sp., Anaerobes, Extended
spectrum β-lactamase (ESBL) positive Klebsiella sp. reported
National Antibiotic Guidelines 3
GASTROINTESTINAL TRACT INFECTIONS
Preferred Regimen:
PEDIATRICS ADULTS
S. pneumoniae: 1st line:
Cefotaxime 200mg/kg/d IV div 4 or 6 Cefotaxime 2g IV q8h (q4h, if life-
doses OR Ceftriaxone 100mg/kg/d IV threatening infection) OR
div 1-2 doses Ampicillin-sulbactam 3g IV q6h OR
If penicillin sensitive S. pneumoniae: Piperacillin-tazobactam 4.5g IV q6h
aqueous Penicillin G 200,000-300,000 (or 4-hour infusion of 4.5g q8h) OR
U/kg/d IV in 6 div doses x 10-14d Ceftriaxone 2g IV q24h OR
Gram-negative bacilli: Ertapenem 1g IV q24h
Cefotaxime 200mg/kg/d IV div 4 or 6
doses x 10d to 3 weeks OR 2nd line:
Ceftriaxone 100mg/kg/d IV div 1-2 If resistant E. coli, Klebsiella species
doses x 10d to 3 weeks WITH or (e.g., ESBL): Meropenem 1g IV q8h
WITHOUT DOT: Unclear. Treat at 5 days and
Gentamicin 3-7.5mg/kg/d IV div 3 perhaps longer if documented
doses OR Monotherapy with the bacteremia
following:
Piperacillin tazobactam 300mg/kg/d IV
div 3 doses (piperacillin component) or
Ampicillin-sulbactam 100-200mg/kg/d
div 4 doses (ampicillin component
Comments:
Perform analysis (check bleeding parameters first), Gram stain and culture of
peritoneal fluid to distinguish primary from secondary peritonitis. Ceftriaxone may
cause bile sludge in patients with jaundice or cirrhosis. Maintain fluid and
electrolyte balance. Do surgical consult. Start antimicrobials as soon as possible.
Generally managed medically. Duration of antibiotic therapy depends on clinical
course of the patient. Probiotics have no use in the adjunctive treatment.
Antibiotic Prophylaxis: Indications:
1. Patients with cirrhosis Variceal or upper GI bleeding
Norfloxacin 400mg PO q12h x
7d OR Ceftriaxone 1g IV qd x 7d
2. Prophylaxis of SBP
Norfloxacin 400mg/d PO OR • Low protein ascites (< 15 g/L)
Ciprofloxacin 500 mg/d PO • Advanced liver failure (Child-Pugh
score > 9 points with serum bilirubin >
DOP for SBP: 3 mg/dL) and/or renal dysfunction
Until liver transplantation, death, (serum creatinine > 1.2 mg/dL, BUN >
resolution of ascites or 25 mg/dL and/or serum sodium < 130
mEq/L)
4 National Antibiotic Guidelines
GASTROINTESTINAL TRACT INFECTIONS
improvement in liver function to • Prior episode of SBP
a compensated state.
D. Secondary peritonitis
Etiology: Usually polymicrobial consisting of anaerobes and facultative gram-
negative bacilli: Bacteroides fragilis group, Peptostreptococcus, E. coli, Klebsiella,
P. aeruginosa, Enterococcus
Preferred Regimen:
Metronidazole 22.5-40mg/kg/d IV div 3 doses PLUS Cefotaxime 200mg/kg/d IV
div 4 or 6 doses OR
Monotherapy with the following antibiotics:
Piperacillin tazobactam 300mg/kg/d IV div 3 doses (piperacillin component) OR
Meropenem 30-60mg/kg/d IV div 3 doses
DOT: Antibiotics are generally given for 5-10d but the primary basis for duration
of antibiotic treatment is the patient’s clinical course.
Comments:
Patient may require either immediate surgery to control the source of
contamination and to remove necrotic tissue, blood and intestinal contents from
the peritoneal cavity or a drainage procedure if a limited number of large
abscesses can be shown.
E. CAPD-associated peritonitis
Infectious complication of chronic ambulatory peritoneal dialysis (CAPD)
PEDIATRICS:
Etiology: Preferred Regimen:
Gram-positive organisms, Vancomycin 45-60mg/kg/d IV or
coagulase negative intraperitoneal in 3-4 doses PLUS Gentamicin
staphylococci, S. aureus (30- 3-7.5mg/kg/d IV div 3 doses
45%), Enterobacteriaceae
(20-30%)
Ventriculo-peritoneal shunt Vancomycin 45-60mg/kg/d IV or
peritonitis: intraperitoneal div 3-4 doses
Coagulase-positive/negative PLUS for Gram-negative infections
Staphylococci Cefotaxime 200mg/kg/d IV div 4 or 6 doses
• Gram-negative bacilli OR
Ceftriaxone 100mg/kg/d IV div 1 or 2 doses
OR
National Antibiotic Guidelines 5
GASTROINTESTINAL TRACT INFECTIONS
Ceftazidime 200-300mg/kg/d div 3 doses OR
Meropenem 30-60mg/kg/d div 3 doses
DOT: generally, 10d but the primary basis for DOT is the patient’s clinical course.
ADULTS:
Etiology: Preferred Regimen:
Gram-positive cocci For Gram-positive cocci:
(45%), Vancomycin added to the dialysis fluid.
Gram-negative bacilli For Gram-negative bacilli:
(15%), Cefepime 2g IV q8–12h OR
Mixture (1%), Ceftazidime 3g loading dose intraperitoneal (IP),
Fungi (2%), then 1-2g IP q24h or 2g IP q48h OR
M. tuberculosis (0.1%) Meropenem 1g IV q8h OR
Aztreonam 1–2g IV q6–8h OR
Ciprofloxacin 400mg IV q12h OR
Amikacin 15–20mg/kg IV q24h
Add an antifungal only if yeast seen on Gram stain.
Comments:
A positive Gram stain will help guide initial therapy. If polymicrobic gram-negative
flora is cultured, consider possibility of catheter-induced bowel perforation,
and/or concomitant underlying GI pathology (e.g., dead bowel). Infection almost
always limited to abdominal cavity; complicating bacteremia is rare. Hence,
usually treat by adding drugs to dialysis fluid; if bacteremia documented or likely,
treat via IV route.
The following are the recommendations based on the Consensus Guidelines for
Prevention and Treatment of Catheter-related infections and peritonitis in
pediatric patients receiving peritoneal dialysis (2012 update):
• Empiric diagnosis of PD-related peritonitis can be made if the effluent WBC
count > 100/mm3 and at least 50% of the WBCs are polymorphonuclear
leukocytes. Effluent should be centrifuged and sediment should be cultured.
• Antibiotics for the treatment of bacterial peritonitis should be administered by
the intraperitoneal route. Beta lactam antibiotics should be administered
continuously.
• Center-specific antibiotic susceptibility patterns should guide selection of
empiric antibiotic therapy although the ISPD recommends cefepime as empiric
treatment. Refer to a specialist for co-management.
Higher cure rate is achieved with VP shunt removal.
6 National Antibiotic Guidelines
GASTROINTESTINAL TRACT INFECTIONS
F. Hepatitis A
Etiology: Hepatitis A virus
Preferred Regimen:
PEDIATRICS ADULTS
No antiviral treatment is No antiviral treatment is recommended.
recommended Give supportive measures.
Comments:
P: Hepatitis A vaccine is given intramuscularly as a 2-dose series at a minimum age
of 12 months. A second dose is given at least 6 months from the first dose.
A: If within 2 weeks of exposure, Hepatitis A vaccination:
• Monovalent Hepatitis A vaccine
a. 720 ELISA units/ml IM - 2doses 1 month apart
b. 1440 ELISA units/ml IM single dose
• Booster dose between 6 & 12 months after initiation of primary course is
recommended to ensure long term antibody titers.
(Handbook on Adult Immunization for Filipinos, 2012)
A single dose of immunoglobulin 0.02 mL/kg IM is protective if administered
within 2 weeks of exposure, but is not locally available. Immunoglobulin might be
preferred over Hepatitis A vaccination among seronegative individuals with
significant underlying liver disease (Sanford Guide to Antimicrobial Therapy,
2016).
G. Hepatitis B
• Patients with Hepatitis B (HBV) are usually asymptomatic.
• When symptomatic, common complaints include: fatigue, nausea, anorexia,
myalgias, arthralgias, asthenia, weight loss (except where ascites).
• There is poor correlation between symptoms and disease stage or
transaminase elevation
Etiology: Hepatitis B virus
PEDIATRICS
Preferred Regimen: Refer to a specialist.
Comments:
Hepatitis B vaccine is given intramuscularly. The first dose is given at birth or within
the first 12 hours of life. The minimum interval between doses is 4 weeks. The final
dose is administered not earlier than age 24 weeks. Another dose is needed if the
last dose was given at age < 24 weeks.
National Antibiotic Guidelines 7
GASTROINTESTINAL TRACT INFECTIONS
For preterm infants, if born to HBsAg (-) mothers and medically stable, the first
dose of HBV may be given at 30 days of chronological age regardless of weight,
and this can be counted as part of the 3 dose primary series. Another dose of HBV
is needed for those < 2 kg whose 1st dose was received at birth.
For infants born to HBsAg (+) mothers, administer HBV and HBIG (0.5ml) within
12hours of life. HBIG should be administered not later than 7 days of age, if not
immediately available.
For infants born to mothers with unknown HBsAg status, if birth weight is >2 kg,
administer HBV within 12h of birth and determine mother’s HBsAg status as soon
as possible. If HBsAg (+), administer HBIG not later than 7 days of age. If with birth
weight of <2 kg, administer HBIG in addition to HBV within 12h of life.
Referral to a specialist is recommended for management of hepatitis cases.
ADULTS
Preferred Regimen: Refer to a specialist.
The following are key indicators for treatment: HBeAg status, HBV viral load (HBV
DNA), elevated liver enzymes (ALT level), cirrhosis. For HBeAg+ patients treatment
is typically deferred for 3-6 months to observe spontaneous seroconversion from
HBeAg+ to negative. [Sanford]
Comments:
Vaccination:
Recombinant Hepatitis B Vaccine (20μg/mL) IM 3 doses at 0,1,6 months
Combined Hepatitis A (720 ELISA units) & B (20 μg/mL recombinant) – 3 doses IM
at 0, 1, 6 months (Handbook on Adult Immunization for Filipinos, 2012)
H. Hepatitis C
• Usually asymptomatic (elevated transaminases).
• When symptomatic, common complaints include fatigue, nausea, anorexia,
myalgias, arthralgias, asthenia, weight loss (except where ascites).
• If symptomatic, usually abates in days to weeks; rarely associated with
hepatic failure.
• 75-85% of persons with acute infection progress to chronic HCV.
Etiology: Preferred Regimen:
Hepatitis C virus Specialist referral RECOMMENDED.
Comments: No recommended prophylaxis; immune serum globulin not effective.
8 National Antibiotic Guidelines
GASTROINTESTINAL TRACT INFECTIONS
I. Liver Abscess
• Fever, right upper quadrant tenderness
• Findings consistent with single or multiple abscesses on abdominal ultrasound
or CT
PEDIATRICS
Etiology: Preferred Regimen:
50% polymicrobial Ampicillin-sulbactam 100-200mg/kg/d IV div 4
S. aureus doses (ampicillin component) (Max: 8g) or
Streptococcus sp. Piperacillin-tazobactam 300mg/kg/d IV div 3
E. coli doses (piperacillin component) (Daily adult dose 9-
K. pneumoniae, 16 g) or
Salmonella Ceftriaxone 100mg/kg/d IV in 1-2 doses (daily
Anaerobic organisms adult dose: 2-4 g)
(Nelson’s Textbook of PLUS
Pedia, 2015) Metronidazole 30-50 mg/kg/d IV div 3 doses (daily
In developing countries, adult dose: 0.75-2.25 g) for 2-3 weeks then shift to
may consider E. oral to complete 4-6 weeks.
histolytica and Toxocara For hepatic abscess secondary to E. histolytica:
canis Metronidazole 30-50mg/kg/d IV div 3 doses x 10d
FOLLOWED BY
Intraluminal amoebicides such as Diloxanide (2nd
line agent) to cure luminal infection
ADULTS
Etiology: Preferred Regimen:
Enterobacteriaceae Pending determination of bacterial versus
(esp. Klebsiella sp.) amoebic liver abscess:
Bacteroides sp. Metronidazole 30-40mg/kg/d div 3 doses IV q8h
Enterococcus sp. or 500mg PO q6-8h
E. histolytica PLUS
Fusobacterium Ceftriaxone 1-2g q24h IV or
necrophorum Piperacillin-tazobactam 4.5g IV q4-6h or
(Lemierre's) Ciprofloxacin 400mg IV q12h OR 750 mg PO or
Levofloxacin 750mg PO/IV q24h or
Ertapenem 1g IV q24h
If amoeba serology is positive:
Metronidazole 750mg IV/PO tid x 10d
National Antibiotic Guidelines 9
GASTROINTESTINAL TRACT INFECTIONS
Comments:
If MRSA is suspected, start on anti-MRSA regimen (refer to section on treatment
of MRSA infections). Ceftriaxone may cause bile sludge in patients with jaundice
or cirrhosis. Serological tests for amebiasis should be done on all patients. For
anaerobic or mixed infections piperacillin-tazobactam, ertapenem (or other
carbapenem) are sufficiently active alone and metronidazole may be
discontinued.
J. Gallbladder infection
Etiology: Preferred Regimen:
Acute acalculous Piperacillin tazobactam 300mg/kg/d IV div 3
cholecystitis is uncommon in doses (piperacillin component) OR
children and usually caused Ampicillin-sulbactam 100-200mg/kg/d div 4
by an infection secondary to doses (ampicillin component) OR
Groups A and B Streptococci, Cefotaxime 200mg/kg/d IV div 4-6 doses
Gram-negative bacilli (like WITH or WITHOUT
Salmonella) and Gentamicin 3.75mg/kg/d IV div 3 doses x 14-
Leptospirosis interrogans. 21d OR
Amikacin 15-22.5mg/kg/d div 3 doses x 14-21d
Antibiotic therapy should
cover for gut luminal flora
(E. coli, Klebsiella,
Enterococcus).
Comments:
Laparoscopic cholecystectomy is the most common surgical treatment for acute
calculous or acalculous cholecystitis in over 95% of pediatric cases. Other
treatment options when laparoscopic or open cholecystectomy is not feasible
include cholecystostomy.
II. COMPLICATED INTRA-ABDOMINAL INFECTIONS
• Complicated intra-abdominal infection extends beyond the hollow viscus of
origin into the peritoneal space and is associated with either abscess
formation or peritonitis.
• Contamination of peritoneal cavity by bowel flora due to bowel perforation,
ruptured appendix, ruptured diverticula, ischemic bowel, leaking surgical
anastomosis, intra-abdominal abscess or other like conditions.
• Common pathogens: Escherichia coli, Klebsiella pneumoniae, Pseudomonas
aeruginosa, Enterobacter cloacae, Acinetobacter baumannii
(Antibiotic management of complicated intra-abdominal infections in adults:
The Asian perspective, Annals of Medicine and Surgery, 2014)
10 National Antibiotic Guidelines
GASTROINTESTINAL TRACT INFECTIONS
A. Biliary complicated intra-abdominal infections
Clinical Setting: Preferred Regimen:
Community-acquired acute Cefazolin 1–2g IV q8h OR
cholecystitis of mild-to- Cefuroxime 1.5g IV q8h OR
moderate severity Ceftriaxone 1–2g IV q12–24h
Community-acquired acute 1st line: Piperacillin-tazobactam 4.5g IV q6h
cholecystitis of severe 2nd line: Metronidazole 500mg IV q8–12h
physiologic disturbance, PLUS Ciprofloxacin 400mg IV q12h or
advanced age, or Levofloxacin 750mg IV q24h or
immunocompromised state Cefepime 2g IV q8–12h
Acute cholangitis following 1st line: Meropenem 1g IV q8h
bilio-enteric anastamosis of 2nd line: Metronidazole 500mg IV q8–12h
any severity. PLUS Ciprofloxacin 400mg IV q12h or
Health care–associated Levofloxacin 750mg IV q24h or
biliary infection of any Cefepime 2g IV q8–12h
severity (IDSA, 2010).
Comments:
Obtain surgical consult for possible gallbladder removal. Patients undergoing
cholecystectomy for acute cholecystitis should have antimicrobial therapy
discontinued within 24 hours unless there is evidence of infection outside the wall
of the gallbladder (IDSA Complicated Intra-abdominal Infection Guidelines, CID
2010:50).
B. Extra-biliary complicated intra-abdominal infections
Etiology: Preferred Regimen:
Mild-to-moderate 1st line:
severity: perforated or Cefoxitin 2g IV q6h OR
abscessed appendicitis and Ertapenem 1g IV q24h
other infections of mild-to- 2nd line:
moderate severity Metronidazole 500mg IV q8–12h
PLUS
Cefazolin 1–2g IV q8h or
Cefuroxime 1.5g IV q8h or
Ceftriaxone 1–2g IV q12–24h or
Cefotaxime 1–2g IV q6–8h or
Ciprofloxacin 400mg IV q12h or
Levofloxacin 750mg IV q24h
High risk or severity: 1st line:
severe physiologic Piperacillin-tazobactam 4.5g IV q6h OR
disturbance, advanced age, Meropenem 1g IV q8h
National Antibiotic Guidelines 11
GASTROINTESTINAL TRACT INFECTIONS
or immunocompromised 2nd line:
state Metronidazole 500mg IV q8–12h
PLUS
Cefepime 2g IV q8–12h or
Ceftazidime 2g IV q8h or
Ciprofloxacin 400mg IV q12h or
Levofloxacin 750mg IV q24h
Comments:
Antimicrobial therapy of established infection should be limited to 4–7 days,
unless it is difficult to achieve adequate source control. Longer durations of
therapy have not been associated with improved outcome. (IDSA Complicated
Intra-abdominal Infection Guidelines, CID 2010:50)
Duration of therapy is variable and clinical trial data, especially for severe disease
is sparse:
• Mild or moderate peritonitis: clinical trial found comparable clinical outcomes
in patients treated for 4 days vs those treated until vital signs and GI continuity
had returned (mean of 8 days). All patients had "source control". Normalization
of serum procalcitonin concentration may assist in customizing the duration of
therapy.
• Severe peritonitis: need source control and resolution of fever, leukocytosis and
ileus. Some centers continue antibiotics until the serum procalcitonin serum
concentration is <0.25 mg/ml or has decreased by 90% from its peak
concentration. (Sanford Guide to Antimicrobial Therapy 2016)
An appropriate source control procedure to drain infected foci, control ongoing
peritoneal contamination by diversion or resection, and restore anatomic and
physiological function to the extent feasible is recommended for nearly all patients
with intra-abdominal infection.
C. Acute pancreatitis
• Patients with necrotizing pancreatitis who develop gas in the area of necrosis,
rising inflammatory markers or persistent fever may be suspected of having
infected pancreatic necrosis and would be candidates for antibiotic therapy.
• Post-Necrotizing pancreatitis, infected pseudocyst or pancreatic abscess
Etiology: Enterobacteriaceae, Enterococcus sp., S. aureus, Staphylococcus
epidermidis, Anaerobes, Candida sp.
Preferred Regimen:
1st line 2nd line
Piperacillin-tazobactam 4.5g IV q4- Ciprofloxacin 400mg IV q12h OR
6h OR Meropenem 1g IV q8h Levofloxacin 750mg IV q24h
12 National Antibiotic Guidelines
GASTROINTESTINAL TRACT INFECTIONS
PLUS Metronidazole 500 mg IV q8–
12h
Comments:
Current consensus is that use of prophylactic antibiotics is not advisable in
pancreatitis, but that they should be employed when clinical factors point to
infected pancreatic necrosis. Those with necrosis involving 30% or more of the
pancreas are at greatest risk of developing infection.
REFERENCES:
• Carlos C, Saniel M. Etiology and epidemiology of diarrheas. Philipp J Microbiol Infect Dis
1990;19(2): 51-53.
• Cherry J, et al. Feigin and Cherry's Textbook of Pediatric Infectious Diseases, 7th Edition.
Philadelphia: Elsevier; 2015.
• Cherry JD, Harrison GJ, Kaplan SL, Steinbach WJ, Hotez PJ. Feigin and Cherry's Textbook of
Pediatric Infectious Diseases. Philadelphia: Elsevier Inc., 2014.
• Integrated Management of Childhood Illness Chart Booklet. Geneva: World Health
Organization; March 2014
• Jalan R, et al. Bacterial infections in cirrhosis; A position statement based on the EASL
Special Conference 2013. J Hepatol 2014; 60:1310-1324.
• Kliegman RM, et al. Nelson’s Textbook of Pediatrics, 20th edition, 2015. Philadelphia:
Elsevier; 2015.
• Kliegman RM, Stanton B, St. Geme J, Schor N. Nelson Textbook of Pediatrics, 20th edition,
Philadelphia, Pennsylvania: Elsevier Inc, 2016.
• Kurup A, et al. Antibiotic management of complicated intra-abdominal infections in adults:
The Asian perspective, Annals of Medicine and Surgery 3 (2014) 85-91
• Lucero M, Saniel M, Geronimo J, Ang C, Leano F, Mate R, Trajano E, Sanvictores E, Forbes
Z, Tupasi T. Etiology of diarrhea in hospitalized children. Philipp J Microbiol Infect Dis 1984.
• Nagel JL, Rarus RE, Crowley AW, Alaniz C, Pogue JM. Retrospective analysis of azithromycin
versus fluoroquinolones for the treatment of legionella pneumonia. PT. 2014; 39:204-205.
• Philippine Foundation for Vaccination and the Philippine Society for Microbiology and
Infectious Diseases. Handbook on Adult Immunization for Filipinos 2012. Manila: Philippine
Foundation for Vaccination; 2012.
• Saniel M, Moriles R, Monzon O, Salazar N, Leano F, Trajano B, Sombrero L, Mat R,
Villanueva J, Geronimo J, Balis A. The relative importance of various enteropathogen in the
etiology of acute diarrhea: a hospital-based study in urban Philippines. SEAMIC Publication
(1987).
• Solomkin JS, et al. Diagnosis and Management of Complicated Intra-abdominal Infection in
Adults and Children: Guidelines by the Surgical Infection Society and the Infectious
Diseases Society of America. Clin Infect Dis. 2010;50(2):133-164.
• The Sanford Guide to Antimicrobial Therapy 2016. Available at:
http://webedition.sanfordguide.com/.
• Warady BA, et al. Consensus guidelines for the prevention and treatment of catheter-
related infections and peritonitis in pediatric patients receiving peritoneal dialysis: 2012
update. Perit Dial Int. 2012 Jun;32 Suppl 2: S32-86
National Antibiotic Guidelines 13
Vous aimerez peut-être aussi
- HGVSJDocument2 pagesHGVSJRhod Bernaldez EstaPas encore d'évaluation
- Statistics PDFDocument54 pagesStatistics PDFRhod Bernaldez EstaPas encore d'évaluation
- Patient Safety Culture in Primary Care: Natasha VerbakelDocument176 pagesPatient Safety Culture in Primary Care: Natasha VerbakelRhod Bernaldez EstaPas encore d'évaluation
- NursingDocument1 pageNursingRhod Bernaldez EstaPas encore d'évaluation
- Carrebean SeaDocument7 pagesCarrebean SeaRhod Bernaldez Esta100% (1)
- Perceive/observe It. Please Answer All Items On This Sheet. If An Item Is Irrelevant, or IfDocument3 pagesPerceive/observe It. Please Answer All Items On This Sheet. If An Item Is Irrelevant, or IfRhod Bernaldez EstaPas encore d'évaluation
- Grenada History, Geography, Politics and EconomyDocument2 pagesGrenada History, Geography, Politics and EconomyRhod Bernaldez EstaPas encore d'évaluation
- Official Receipt PDFDocument1 pageOfficial Receipt PDFRhod Bernaldez EstaPas encore d'évaluation
- 2nd Patient Safety Congress RegistrationDocument1 page2nd Patient Safety Congress RegistrationRhod Bernaldez EstaPas encore d'évaluation
- Erastus Perceptions 2018 PDFDocument105 pagesErastus Perceptions 2018 PDFRhod Bernaldez EstaPas encore d'évaluation
- RHOD Seniority Complex Semi FinalDocument39 pagesRHOD Seniority Complex Semi FinalRhod Bernaldez EstaPas encore d'évaluation
- Radically Redesigning: Patient SafetyDocument9 pagesRadically Redesigning: Patient SafetyRhod Bernaldez EstaPas encore d'évaluation
- Sops Hospital Survey: Language: EnglishDocument6 pagesSops Hospital Survey: Language: EnglishNoviyanti LindaPas encore d'évaluation
- Leadership DevelopmentDocument2 pagesLeadership DevelopmentRhod Bernaldez EstaPas encore d'évaluation
- AHRQ Patient Safety Culture Improvement PlanDocument4 pagesAHRQ Patient Safety Culture Improvement PlanRhod Bernaldez EstaPas encore d'évaluation
- Patient Safety in Primary Healthcare A Review of The Literature August 2015Document160 pagesPatient Safety in Primary Healthcare A Review of The Literature August 2015Rhod Bernaldez EstaPas encore d'évaluation
- Facil Scan FormDocument7 pagesFacil Scan FormJoe ThesecondmonthPas encore d'évaluation
- Patient Safety Incident Reporting - Canadian Health SystemDocument13 pagesPatient Safety Incident Reporting - Canadian Health SystemRhod Bernaldez EstaPas encore d'évaluation
- Relationship Between Patient Safety Culture and Safety Outcome Measures Among NursesDocument80 pagesRelationship Between Patient Safety Culture and Safety Outcome Measures Among NursesRhod Bernaldez EstaPas encore d'évaluation
- MHD Mission VisionDocument1 pageMHD Mission VisionRhod Bernaldez EstaPas encore d'évaluation
- Fallpxtool 1 BDocument2 pagesFallpxtool 1 BRhod Bernaldez EstaPas encore d'évaluation
- Gardner-Webb University Digital Commons at Gardner-Webb UniversityDocument132 pagesGardner-Webb University Digital Commons at Gardner-Webb UniversityRhod Bernaldez EstaPas encore d'évaluation
- Control of Documented Information Procedure SampleDocument4 pagesControl of Documented Information Procedure Sampleingventor0% (1)
- Nurses' Perceptions of Patient Safety Culture in Oman: Fatma Al Dhabbari MSC, Pgd. BSC (Hons), R.G.NDocument3 pagesNurses' Perceptions of Patient Safety Culture in Oman: Fatma Al Dhabbari MSC, Pgd. BSC (Hons), R.G.NRhod Bernaldez EstaPas encore d'évaluation
- Objectives 2. Scope 3. Responsibilities 4. Records and References 5. Procedure Details Page No. Rev. No. Effectivity Nature of ChangeDocument8 pagesObjectives 2. Scope 3. Responsibilities 4. Records and References 5. Procedure Details Page No. Rev. No. Effectivity Nature of ChangeRhod Bernaldez EstaPas encore d'évaluation
- NursingDocument1 pageNursingRhod Bernaldez EstaPas encore d'évaluation
- Perceived Safety Culture of Healthcare Providers in Hospitals in The PhilippinesDocument14 pagesPerceived Safety Culture of Healthcare Providers in Hospitals in The PhilippinesRhod Bernaldez EstaPas encore d'évaluation
- Icrd Vawc-1Document1 pageIcrd Vawc-1Rhod Bernaldez EstaPas encore d'évaluation
- Implementing Rules and Regulations of The Lending Company Regulation Act of 2007 Ra9474Document19 pagesImplementing Rules and Regulations of The Lending Company Regulation Act of 2007 Ra9474Lance DionelaPas encore d'évaluation
- Leadership DevelopmentDocument2 pagesLeadership DevelopmentRhod Bernaldez EstaPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Medicine List by AmirDocument39 pagesMedicine List by AmirNomAn JuTtPas encore d'évaluation
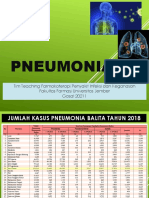
- Pneumonia: Tim Teaching Farmakoterapi Penyakit Infeksi Dan Keganasan Fakultas Farmasi Universitas Jember Gasal 20211Document67 pagesPneumonia: Tim Teaching Farmakoterapi Penyakit Infeksi Dan Keganasan Fakultas Farmasi Universitas Jember Gasal 20211Evie WulansariPas encore d'évaluation
- CPG Rational Antibiotic Utilisation in Selected Paediatric ConditionsDocument37 pagesCPG Rational Antibiotic Utilisation in Selected Paediatric ConditionsziggyshahdustPas encore d'évaluation
- Anti-Microbial USMLE Review: Active RecallDocument32 pagesAnti-Microbial USMLE Review: Active Recallmehrzi kamelPas encore d'évaluation
- Brain AbscessDocument13 pagesBrain Abscesskashim123Pas encore d'évaluation
- Cephalosporins GenerationDocument7 pagesCephalosporins GenerationSam SmileyPas encore d'évaluation
- Pharmacology Notes: EliminationDocument14 pagesPharmacology Notes: EliminationHaifa ibrahimPas encore d'évaluation
- Are Third Generation Cephalosporins Associated With A Bette - 2018 - Clinical MiDocument6 pagesAre Third Generation Cephalosporins Associated With A Bette - 2018 - Clinical MiRadia LachehebPas encore d'évaluation
- Acute Osteomyelitis: Diagnosis and ManagementDocument40 pagesAcute Osteomyelitis: Diagnosis and ManagementAnkit KarkiPas encore d'évaluation
- Antimicrobial Sensitivity of Most Commonly Isolated Bacteria From Feline Upper Respiratory Infection (URI)Document3 pagesAntimicrobial Sensitivity of Most Commonly Isolated Bacteria From Feline Upper Respiratory Infection (URI)KAREN LEE MEI FONGPas encore d'évaluation
- Community-Acquired Bacterial Meningitis in Adults: Review ArticleDocument10 pagesCommunity-Acquired Bacterial Meningitis in Adults: Review ArticleÁlvaro NBPas encore d'évaluation
- Rational Prescribing of Antibiotics in Infections in ChildrenDocument43 pagesRational Prescribing of Antibiotics in Infections in ChildrenVictor UmbuPas encore d'évaluation
- Cefotaxime 1g Powder For Solution For Injection or Infusion PL 14894 0397 Cefotaxime 2g Powder For Solution For Injection or Infusion PL 14894 0398Document48 pagesCefotaxime 1g Powder For Solution For Injection or Infusion PL 14894 0397 Cefotaxime 2g Powder For Solution For Injection or Infusion PL 14894 0398CongluanPas encore d'évaluation
- Beta Lactam AntibioticsDocument52 pagesBeta Lactam AntibioticsKaymie ReenPas encore d'évaluation
- Medication Guidelines Vol 1 Antimicrobial Prescribing v1.1 1Document77 pagesMedication Guidelines Vol 1 Antimicrobial Prescribing v1.1 1doodrillPas encore d'évaluation
- Hospital Antibiotic Policy: ST Helens and Knowsley Hospitals TrustDocument72 pagesHospital Antibiotic Policy: ST Helens and Knowsley Hospitals TrustDimas RfPas encore d'évaluation
- CeftriaxoneDocument7 pagesCeftriaxoneGreats HalomoanPas encore d'évaluation
- Pediatric Bacterial Meningitis in PhilippinesDocument27 pagesPediatric Bacterial Meningitis in Philippinesdranita@yahoo.comPas encore d'évaluation
- Indian JOurnal of PediatricsDocument8 pagesIndian JOurnal of Pediatricsliska ramdanawatiPas encore d'évaluation
- Pedia Care Study - Appendix B - Drug StudyDocument8 pagesPedia Care Study - Appendix B - Drug Studyryan100% (1)
- FormularyDocument123 pagesFormularyMuhammad Shakeel100% (3)
- Antibiotics: How Much Do You Know? Try Our Quiz For PrescribersDocument6 pagesAntibiotics: How Much Do You Know? Try Our Quiz For PrescribersSupratim SahaPas encore d'évaluation
- Pharmacy Training Book Topic GuideDocument355 pagesPharmacy Training Book Topic GuideHaneen HaneenPas encore d'évaluation
- Inhibitors of Bacterial Cell Wall Synthesis: Dr. Ndayisaba CorneilleDocument83 pagesInhibitors of Bacterial Cell Wall Synthesis: Dr. Ndayisaba CorneilleNdayisaba CorneillePas encore d'évaluation
- Christian Medical College Antimicrobial Therapy GuidelinesDocument43 pagesChristian Medical College Antimicrobial Therapy Guidelinesharshita guglaniPas encore d'évaluation
- Meningitis Pathophysiology PDFDocument59 pagesMeningitis Pathophysiology PDFpaswordnyalupa100% (1)
- Meningismus Vs MeningitisDocument19 pagesMeningismus Vs MeningitisRanna HertenizaPas encore d'évaluation
- Pediatric Drugs MKDDocument3 pagesPediatric Drugs MKDquixoticdreamer100% (7)
- Antibiotic Cross-Sensitivity Chart PDFDocument1 pageAntibiotic Cross-Sensitivity Chart PDFanareadsPas encore d'évaluation