Académique Documents
Professionnel Documents
Culture Documents
Acute Kidney Injury An Update
Transféré par
karol fernandezTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Acute Kidney Injury An Update
Transféré par
karol fernandezDroits d'auteur :
Formats disponibles
See
discussions, stats, and author profiles for this publication at: https://www.researchgate.net/publication/280092445
EMJ EUROPEAN MEDICAL JOURNAL ACUTE
KIDNEY INJURY -AN UPDATE
Article · August 2015
CITATIONS READS
0 65
3 authors, including:
Matt Varrier Marlies Ostermann
Guy's and St Thomas' NHS Foundation Trust Guy's and St Thomas' NHS Foundation Trust
10 PUBLICATIONS 59 CITATIONS 200 PUBLICATIONS 5,206 CITATIONS
SEE PROFILE SEE PROFILE
Some of the authors of this publication are also working on these related projects:
Timely Initiation of Renal Replacement Therapy View project
Angiotensin II View project
All content following this page was uploaded by Marlies Ostermann on 16 July 2015.
The user has requested enhancement of the downloaded file.
ACUTE KIDNEY INJURY - AN UPDATE
Matt Varrier, Richard Fisher, *Marlies Ostermann
Department of Critical Care & Nephrology, Guy’s & St Thomas’ NHS Foundation Hospital, London, UK
*Correspondence to Marlies.Ostermann@gstt.nhs.uk
Disclosure: The authors have declared no conflicts of interest.
Received: 05.02.15 Accepted: 16.04.15
Citation: EMJ Nephrol. 2015;3[1]:75-82.
ABSTRACT
The syndrome of acute kidney injury (AKI) occurs frequently in hospitalised patients, leading to increased
morbidity, mortality, and healthcare expenditure. In the context of a precipitating insult, disturbances
in both global and microcirculatory renal blood flow, tubular cell damage, and activation of pro-
inflammatory pathways lead to impairment of numerous elements of renal function. Classification
systems, including the recent ‘Kidney Disease: Improving Global Outcomes’ (KDIGO) classification,
typically define and stage AKI in terms of the magnitude of rise in serum creatinine (SCr) and the
presence of oliguria. At present there is no cure for AKI and the key principles of its management include
early recognition, haemodynamic optimisation, correction of hypovolaemia, ceasing and avoidance of
nephrotoxic medications, and treatment of the underlying cause. Recent data show that the type and
volume of fluid therapy can affect renal function and that further guidance is required. In the future it is
hoped that novel technologies, including biomarkers and real-time measurement of glomerular filtration
rate will allow the earlier identification of patients with AKI, whilst a greater understanding of the
pathogenesis of AKI will lead to the identification of new therapeutic targets. Despite SCr usually
recovering after an episode of AKI, there is growing recognition that survivors of AKI are at an increased
risk of subsequent chronic kidney disease, including end-stage renal failure and premature death.
Keywords: Acute kidney injury (AKI), fluid therapy, AKI biomarkers, AKI e-alert.
INTRODUCTION magnitude and nature of the insult. Traditional
diagnostic tools to diagnose AKI include SCr,
Acute kidney injury (AKI) is a frequent complication blood urea nitrogen, urine output, urine chemistry,
in hospitalised patients. It is associated with serious urine microscopy, and histology. The need for a
short and long-term morbidities, an increased risk standardised definition culminated in the ‘Kidney
of dying, and significant healthcare costs. Even Disease: Improving Global Outcomes’ (KDIGO)
small rises in serum creatinine (SCr) independently AKI classification,2 which evolved from the ‘Risk,
predict poor outcome.1 This review focuses on Injury, Failure, Loss of kidney function, and End-
recent developments in AKI that are of interest to stage kidney disease’ (RIFLE) and AKI Network
the general physician. criteria (Table 1).3,4
DEFINITION Although SCr is readily available in clinical practice,
it is affected by muscle mass and fluid status,
AKI is a syndrome encompassing many different can change in response to certain drugs without
aetiologies and is characterised by an acute change in renal function, is not reliable in patients
deterioration of renal function. The most common with liver disease, and may take 24–36 hours to
causes are sepsis, volume depletion, haemodynamic rise after a definite renal insult. Conversely, patients
instability, and nephrotoxic injury. AKI comprises with advanced chronic kidney disease (CKD) may
simultaneous impairment of nitrogenous waste have a SCr rise as part of natural progression or
excretion, fluid balance and electrolyte regulation, a relatively small decrease in glomerular filtration
and acid-base homeostasis, which occur to rate (GFR), which may bias them towards a
varying degrees and reversibility according to the diagnosis of AKI. Epidemiological studies have
NEPHROLOGY • July 2015 EMJ EUROPEAN MEDICAL JOURNAL 75
also shown that some patients have a slow but and post-discharge patient-care costs. The cost of
persistent (creeping) rise in SCr but do not fulfil AKI-related inpatient care in England consumes 1%
the criteria for AKI. The term ‘acute kidney disease’ of the entire healthcare budget, and is estimated
has been suggested to describe this scenario.2 to be higherthan that of the four most common
cancers combined.13
Accurate measurement of urine output is
challenging in patients without a urinary catheter
EARLY RECOGNITION
and oliguria may be missed, especially outside
of critical care areas. Urine output can be
The best chance of ameliorating the severity of
manipulated by diuretics and may persist until
AKI is through early recognition and intervention.
renal function almost ceases. Importantly, oliguria
The majority of AKI develops in the context of an
may be an appropriate response in the setting
acute medical or surgical illness outside renal or
of hypovolaemia reflecting under-resuscitation
critical care units. The UK National Confidential
rather than kidney injury. The use of weight-based
Enquiry into Patient Outcomes and Death
urine output criteria for AKI may be misleading in
(NCEPOD) report in 2009 – ‘AKI - adding insult to
obesity and result in the overdiagnosis of AKI. The
injury’ – was a retrospective case analysis of
European Renal Best Practice Guidelines (2012)
patients who had died and been coded as having
recommend using the ideal weight rather than
AKI.14 In only 50% of cases was care considered
the true weight when calculating urine output in
to be ‘good’. In 30% of cases, AKI was deemed to
ml/min/kg to avoid a misdiagnosis of AKI.5
have been both predictable and avoidable.
There remains debate about the definition of Failures of care included the non-institution of
baseline SCr.2,6 Extending the baseline assessment basic measures such as stopping nephrotoxins,
period to 3, 6, and 12 months prior to hospital prescribing supplemental fluids, and unacceptable
admission results in progressively more patients delays in recognition. Electronic alert systems
being classified as having AKI, but with decreasing use changes in SCr to identify AKI and alert
in-hospital mortality.6 Despite these limitations the clinical team with the aim of instituting a
and potential pitfalls it is recommended to review and management plan. A number of
use the KDIGO classification of AKI in clinical studies have suggested that electronic alerts
practice and research until more specific and can positively influence physician behaviour
sensitive tests are routinely available. The use of and improve outcomes.15-19 However, a recent
formulae to calculate an estimated GFR cannot be randomised controlled trial (RCT) showed no
recommended in AKI.2 difference in mortality or need for dialysis.20
EPIDEMIOLOGY PATHOPHYSIOLOGY
The incidence of AKI is increasing with time7-9 The kidneys receive around 20% of the cardiac
due to population changes (ageing/comorbidity), output, and renal oxygen extraction is low
changing healthcare behaviours (increasing use (approximately 10-15%), yet they are very
of potentially nephrotoxic drugs, contrast media, susceptible to tissue hypoxia, especially during an
high-risk interventions), and increased recognition. acute illness. In recent years, the previously held
AKI affects 7-22% of hospital inpatients. Older belief that AKI develops due to a global decrease
and critically ill patients are at particular risk. in renal perfusion associated with a state of shock
A large, multi-national meta-analysis identified has been called into question.21,22 For instance, AKI
154 cohorts published between 2004 and does not necessarily occur in survivors of cardiac
2012, including 3.4 million hospitalised adults arrest despite prolonged periods of hypotension.23
that allowed classification according to KDIGO In sepsis, animal models demonstrated that renal
criteria.10 The pooled incidence of AKI was 22%. blood flow (RBF) may be reduced, increased, or
The odds of death in the 2.2 million patients for unchanged, which implies that factors other than
whom data was available was five-times greater RBF play an important role.
for those with AKI than without. The annual
incidence in the community may be as high as 1%.11 Current evidence suggests that the origin of
The financial burden of AKI is huge as it greatly most cases of AKI is multifaceted rather than
increases length of stay in the intensive care unit the result of an individual insult. Several concurrent
(ICU) and in the hospital, and both in-hospital12 mechanisms contribute, including regional
76 NEPHROLOGY • July 2015 EMJ EUROPEAN MEDICAL JOURNAL
variations in perfusion and oxygen consumption, prescribed class of drug and increased prescribing
impaired autoregulation, distortion of peritubular may be responsible for 15% of the increase in
and glomerular microcirculation, tubular cell injury, admissions for AKI.28 Non-steroidal anti-
endothelial injury, microvascular thrombosis, inflammatory drugs are easily available and
and arteriovenous shunting, resulting in the commonly implicated too. Although evidence-
activation of inflammatory processes.24 AKI is based data from RCTs is missing, it makes sense
now considered a pro-inflammatory condition. to recommend that during an episode of AKI,
Numerous pro and anti-inflammatory mediators drugs with potential for nephrotoxic injury should
and pathways have been identified, which account be avoided or dose adjusted if possible.
for some of the clinical sequelae of AKI and may
also serve as therapeutic targets in the future.25-27 Haemodynamic Optimisation
Haemodynamic optimisation uses fluid therapy
TREATMENT and vasoactive drugs to achieve cardiac output
and perfusion pressures that will restore/maintain
The management of AKI is supportive with focus adequate oxygen delivery to tissues including the
on the optimisation of fluid and haemodynamic kidneys. Optimisation has three main components:
status, treatment of the underlying illness,
avoidance of further nephrotoxic insults, and renal i) Pre-load optimisation aims to maximise stroke
replacement therapy (RRT) if necessary. There is volume (and therefore cardiac output) by
no cure for AKI. Many pharmacological treatments augmenting left ventricular end-diastolic volume
have been tried with disappointing results. The with intravascular filling. The use of central
recent KDIGO expert group appraised and venous pressure to guide volume expansion is
summarised current evidence-based management not recommended.29
(Table 2).2 In cases where the necessary evidence
ii) Afterload optimisation aims to ensure adequate
was missing, recommendations were made based
perfusion of the kidneys and is especially
on expert opinion.
important in the management of distributive
Avoidance of Nephrotoxic Agents shock, where vasopressors can improve renal
haemodynamics.30
Nephrotoxic drugs often contribute to the
development of AKI during an acute illness. iii) Contractility optimisation aims to improve
For example, in the UK, angiotensin-converting oxygen delivery if shock persists, despite pre-
enzyme (ACE)-inhibitors and angiotensin II load and afterload optimisation. The most
receptor blockers are the second most commonly commonly used drugs are inotropes.
Table 1: KDIGO definition and classification of acute kidney injury.2
Definition AKI is diagnosed if SCr increases by at least 0.3 mg/dl (26.5 µmol/l) in 48 hours or rises to
at least 1.5-fold from baseline within 7 days.
Stage SCr rise Urine output
1 1.5–1.9 × baseline <0.5 ml/kg/h for 6–12 hours
OR
≥0.3 mg/dl (≥26.5 µmol/l) increase
2 2.0–2.9 × baseline <0.5 ml/kg/h for ≥12 hours
3 3.0 × baseline <0.3 ml/kg/h for ≥24 hours
OR OR
increase in SCr to ≥4.0 mg/dl (≥353.6 µmol/l) anuria for ≥12 hours
OR
initiation of renal replacement therapy
SCr: serum creatinine; KDIGO: Kidney Disease: Improving Global Outcomes; AKI: acute kidney injury.
NEPHROLOGY • July 2015 EMJ EUROPEAN MEDICAL JOURNAL 77
Table 2: Summary of guidelines for treatment of acute kidney injury from KDIGO.2
Do Do not
Discontinue all nephrotoxic drugs if possible. Restrict protein intake with the aim of preventing or
delaying initiation of RRT.
In the absence of haemorrhagic shock, use isotonic Use diuretics to prevent or treat AKI, except in the
crystalloids rather than colloids as initial management for management of volume overload.
expansion of intravascular volume.
Use vasopressors in conjunction with fluids in patients Use low-dose dopamine, fenoldopam, ANP, or rIGF-1 to
with vasomotor shock with or at risk of AKI. prevent or treat AKI.
Consider protocol-based management of haemodynamic Use aminoglycosides if a non-nephrotoxic alternative
and oxygenation parameters in high-risk patients in the is available (close monitoring of trough levels if
perioperative setting or in patients with septic shock. unavoidable).
Consider alternatives to radiocontrast procedures. Use oral fluids, theophylline, fenoldopam, or RRT for
prophylaxis of CIN.
In critically ill patients, use insulin therapy targeting Use conventional formulations of amphotericin B (lipid
plasma glucose 110-149 mg/dl (6.1-8.3 mmol/l). preparations are less nephrotoxic).
Achieve a total energy intake of 20-30 kcal/kg/day.
Provide nutrition preferentially via the enteral route.
Use lipid formulations of amphotericin B rather than
conventional.
Use intravenous 0.9% saline or isotonic sodium
bicarbonate and oral NAC in patients at high risk of CIN.
Initiate RRT emergently when life-threatening changes in
fluid, electrolyte, and acid-base balance exist.
When considering RRT, consider the presence of
conditions that can be modified with RRT, and trends of
laboratory tests, rather than single urea and creatinine
thresholds.
AKI: acute kidney injury; ANP: atrial natriuretic peptide; CIN: contrast induced nephropathy; rIGF:
recombinant insulin growth factor; RRT: renal replacement therapy; NAC: N-acetylcysteine; KDIGO:
Kidney Disease: Improving Global Outcomes.
Fluid Therapy 2.9%) and need for RRT compared to patients
treated with Plasma-Lyte.35 After correction for
i) Type of fluid: The optimal type of fluid for confounders, the increased rate of RRT remained
prevention and management of AKI is not known. significant. Based on animal models the underlying
However, there is increasing evidence that starch- mechanism is believed to be chloride-induced
based colloids can cause or worsen AKI if given in renal vasoconstriction and decrease of renal
large volumes and should be avoided in critically artery blood flow and GFR.36-38 It is important to
ill patients.31-33 Use of chloride-rich solutions like note that all data suggesting that balanced
0.9% saline is associated with hyperchloraemic solutions may be superior to 0.9% saline are based
metabolic acidosis and an increased risk of AKI.34 on observational studies. An RCT is still awaited.
There is some evidence that balanced crystalloid
solutions such as Ringer’s Lactate, Hartmann’s ii) Volume of fluid: Classically, in volume-depleted
solution, or Plasma-Lyte may have benefits patients with intact tubular function, avid retention
over saline. of sodium is reversible with fluid therapy and
oliguria improves. Prolonged volume depletion is
Analysis of a large US database of patients harmful to kidney function; fluid administration
undergoing major abdominal surgery showed that beyond the resuscitation phase in patients with
patients who received 0.9% saline had a higher AKI is not only ineffective but also harmful
unadjusted in-hospital mortality (5.6% versus and associated with reduced chances of renal
78 NEPHROLOGY • July 2015 EMJ EUROPEAN MEDICAL JOURNAL
recovery and an increased mortality.39 Fluid of improving the processes of care and patient
overload results in tissue oedema, obstruction outcomes through a small set of evidence-based
of capillary blood flow and lymphatic drainage, practices that, when performed collectively,
impaired diffusion of oxygen, and disturbed cell– improve patient outcomes.45 Care bundles have
cell interactions.40 Progressive organ dysfunction been successfully integrated into the management
may result. The effects are pronounced in of potentially life-threatening conditions like
encapsulated organs such as the kidneys, which sepsis or ventilator associated pneumonia. The
cannot accommodate extra volume without an initial treatment of AKI may benefit from a similar
increase in interstitial pressure and compromised approach but evidence from RCTs is lacking.46
organ blood flow. Although both inadequate and
Prevention of Contrast-Induced Nephropathy
overzealous fluid resuscitation are harmful in AKI,
there are currently no reliable tools to diagnose Iodinated contrast media can cause AKI by several
euvolaemia. The decision of when to stop fluid mechanisms including direct tubular toxicity and
therapy is mainly based on the regular clinical renal vasoconstriction. It is uncommon in stable
assessment of the patient. patients without risk factors44 but frequently
contributes to AKI in patients with an acute illness
Blood Pressure Management or pre-existing CKD, especially if procedures which
Hypotension and low cardiac output are necessitate high contrast volumes are necessary.
deleterious for kidney function but the optimal Other risk factors are advanced age, diabetes
haemodynamic targets for patients with early AKI with CKD, heart failure, and concurrent use of
are unknown. Data in the literature are conflicting. nephrotoxic drugs. The only proven effective
A large Finnish study showed that septic preventative strategy is to optimise volume status
patients who developed AKI within 5 days of ICU with saline or isotonic sodium bicarbonate before
admission had a significantly lower mean arterial the procedure whilst addressing any treatable
pressure (MAP) (74 mmHg) compared to septic components of the acute illness (Table 2).47 The
patients without AKI (MAP: 79mmHg).41 In contrast, use of oral N-acetylcysteine is a weak KDIGO
Bourgoin et al.42 reported that raising MAP to recommendation2 that has been dropped from
>85 mmHg in patients with shock did not result in the recent guideline by the National Institute for
Health and Care Excellence UK.44
an improvement of urine output or SCr. Similarly,
an RCT comparing a target MAP of 80-85 mmHg Renal Replacement Therapy
versus 65-70 mmHg in patients with septic shock
showed no difference in mortality (although RRT should be considered when the benefits
both groups achieved MAPs greater than their outweigh any potential risks, independent of
target resulting in a less pronounced difference specific urea and creatinine results, but before
between both groups).43 Interestingly, patients the development of any uraemic emergencies.2
with chronic hypertension randomised to the high Continuous RRT is recommended for patients who
MAP group needed RRT less often. The current are haemodynamically unstable or have conditions
recommendation is to tailor MAP targets to the associated with increased intracranial pressure.2
individual. It is reasonable to aim for a higher Peritoneal dialysis is an option but is rarely used in
MAP in patients with chronic hypertension with adults in developed countries.48
persistent oliguria or rising SCr.
LONG-TERM PROGNOSIS
Exclusion of Obstruction
Several large epidemiological studies have
Ultrasound imaging of the urinary tract is shown that the prognosis of AKI (even with good
recommended in patients at high risk of obstruction recovery of SCr) is not entirely benign. Survivors
or where there is no obvious cause of AKI.44 It will of AKI are at an increased risk of death and
also identify important pre-existing anatomical CKD including progression to end-stage renal
variations, like a single kidney or small kidneys in failure, which has a major impact on the patient’s
the case of CKD. life expectancy and contributes to healthcare
AKI Care Bundles costs.49-51 Patients with diabetes, chronic vascular
disease, and CKD are particularly at risk. There
There has been a trend in critical care towards the are several reasons for this, including common
use of care ‘bundles’, which are a structured way comorbidities as well as factors directly related
NEPHROLOGY • July 2015 EMJ EUROPEAN MEDICAL JOURNAL 79
to repair processes following AKI. A single-centre avoid during sick days.44 This is particularly
observational study in Pennsylvania, USA found relevant for patients with CKD.
that patients with AKI were 50% more likely to
die and nearly twice as likely to develop CKD FUTURE DEVELOPMENTS
following hospital discharge compared with
matched controls without AKI.51 Proteinuria has There is an ongoing search for more sensitive
recently been identified as more common in AKI tests to diagnose AKI before elevations in SCr
survivors than controls and is associated with occur, which may also facilitate the discovery of
CKD progression.52 Other studies have found an potential therapies.
association between AKI and subsequent risk of
coronary events,53 strokes,54 fractures,55 and reduced Novel Biomarkers
quality of life.56 There have been calls for regular
Novel biomarkers of AKI vary in their origin,
follow-ups for patients who survive a hospital
function, distribution, and time of release following
admission complicated by AKI in order to improve
renal injury.61,62 They can be divided into:
their long-term prognosis, but the most effective
strategy has not yet been identified.57 i) Markers of glomerular function: Small molecular
weight molecules that are present in the
The assessment of residual renal function after
systemic circulation and undergo glomerular
an acute illness is challenging. SCr results may be
filtration (i.e. cystatin C). In the case of reduced
misleading due to changes in muscle mass and
metabolism, clearance of excess tissue water, and GFR their plasma concentration rises.
temporary discontinuation of drugs that affect ii) Markers of tubular function: Molecules that are
GFR, such as ACE-inhibitors.58 This ‘pseudo- filtered and undergo tubular reabsorption (i.e.
normalisation’ may become apparent only if a retinol-binding protein) and may appear in the
repeat SCr is measured after recovery from critical urine in the case of tubular injury.
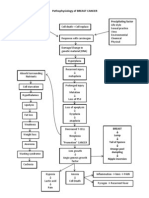
illness. AKI and CKD are complex, interconnected
syndromes (Figure 1). Prospective longitudinal iii) Markers of tubular injury, damage, or repair:
studies in AKI survivors are in progress and will Molecules that are released into urine or
be valuable to guide decision making.59,60 plasma as a result of direct renal cell damage,
inflammatory activation, or following gene
Self-Management
upregulation, i.e. kidney injury molecule-1
It is recommended that patients at risk of AKI (KIM-1), interleukin-18 (IL-18), tissue
are informed of the conditions that may cause metalloproteinase-2, and insulin-like growth
AKI (i.e. diarrhoea and vomiting) and the drugs to factor-binding protein 7.
Structural damage, nephron-loss, glomerular hyperfiltration, and
promoters of tubulointerstitial fibrosis such as TGF-β
Factors which
predispose to an
CKD tends to progress
episode of AKI may
with time. The mainstay
persist leading to
of treatment is control
recurrent bouts, e.g. AKI CKD of blood pressure and
diuretic-dependent
proteinuria with priority
heart failure or a long-
to RAAS inhibition
term catheter, which
led to urosepsis
CKD is a major risk factor for AKI. There is a lack of functional
renal reserve and greater vulnerability to haemodynamic stress
Figure 1: Relationships between acute kidney injury and chronic kidney disease.
Underpinning all these relationships are a large number of potential factors that increase risk for both
AKI and CKD e.g. advanced age, hypertension, coronary artery disease, diabetes, heart failure,
proteinuria, etc.
AKI: acute kidney injury; CKD: chronic kidney disease; TGF-β: transforming growth factor β; RAAS: rennin
angiotensin aldosterone system.
80 NEPHROLOGY • July 2015 EMJ EUROPEAN MEDICAL JOURNAL
The most-studied biomarkers are neutrophil Curative Therapies
gelatinase-associated lipocalin, cystatin C, KIM-1,
and IL-18. Studies have shown that the use Novel strategies including mesenchymal stem cell
of novel biomarkers in certain situations may therapy, anti-inflammatory agents, and treatment
indicate the onset of AKI earlier than SCr or urine with alkaline phosphatase are currently being
output, correlate with severity of AKI, and/or investigated and the results of these studies
prognosticate the need for RRT. However, the results are awaited.
are variable and depend on the case-mix, cause
of AKI, clinical setting, associated comorbidities, CONCLUSION
and timing of biomarker measurements.63 To date,
The mainstay of AKI management remains prompt
novel AKI biomarkers have not been integrated
recognition followed by early optimisation of
into routine clinical practice.
haemodynamics, correction of volume depletion,
Real-Time GFR Measurement avoidance of nephrotoxins, and treatment of
the underlying cause. The development of new
Knowing the actual GFR would not only define diagnostic tools, including biomarkers and
and stage AKI earlier and more accurately, it techniques to measure GFR in real time, offers new
may also improve clinical management, for opportunities and the prospect of diagnosing AKI
instance facilitating correct drug dosing.62 Some earlier and more accurately. Until then, strategies
investigators have made progress in real-time GFR to improve AKI care are likely to include a
techniques. For instance, external whole-tissue co-ordinated approach to education, electronic
radioactivity measured after intravenous injection alerts, and care bundles. Increasing recognition of
of Tc-labelled diethylenetriaminepentaacetic acid the long-term complications confirms that AKI
allowed an accurate, fast, and convenient way is no longer just an acute illness and deserves
to measure total and individual kidney GFR.64 long-term follow-up.
Several commercial companies are in the process
of developing rapid, sensitive, reproducible, and
affordable techniques to measure real-time GFR.
REFERENCES
1. Kao SS et al. Variability in inpatient acute kidney injury in database studies: Dial Transplant. 2014;29(7):1362-8.
serum creatinine: its impact upon the effects of varying the baseline 14. NCEPOD. Adding insult to injury –
short- and long-term mortality. QJM. kidney function assessment period and a review of care of patients who died
2015;pii:hcv020. [Epub ahead of print]. considering CKD status. Am J Kidney Dis. in hospital with a primary diagnosis of
2. KDIGO Clinical Practice Guideline for 2010;56(4):651-60. acute kidney injury (acute renal failure).
Acute Kidney Injury. Kidney International. 7. Hsu RK et al. Temporal changes in June 2009. http://www.ncepod.org.
2012;suppl.(2):1-138. incidence of dialysis-requiring AKI. J Am uk/2009report1/Downloads/AKI_report.
3. Bellomo R et al. Acute renal failure - Soc Nephrol. 2013;24(1):37-42. pdf. 10 January 2015.
definition, outcome measures, animal 8. Hsu CY et al. Community-based 15. McCoy AB et al. A computerized
models, fluid therapy and information incidence of acute renal failure. Kidney provider order entry intervention for
technology needs: the Second Int. 2007;72(2):208-12. medication safety during acute kidney
International Consensus Conference of 9. Lewington AJ et al. Raising awareness injury: a quality improvement report. Am
the Acute Dialysis Quality Initiative (ADQI) of acute kidney injury: a global J Kidney Dis. 2010;56(5):832-41.
Group. Crit Care. 2004;8(4):R204-12. perspective of a silent killer. Kidney Int. 16. Rind DM et al. Effect of computer-
4. Mehta RL et al. Acute Kidney Injury 2013;84(3):457-67. based alerts on the treatment and
Network: report of an initiative to improve 10. Susantitaphong P et al. World outcomes of hospitalized patients. Arch
outcomes in acute kidney injury. Crit Care. incidence of AKI: a meta-analysis. Clin J Intern Med. 1994;154(13):1511-7.
2007;11(2):R31. Am Soc Nephrol. 2013;8(9):1482-93. 17. Colpaert K et al. Implementation of a
5. Fliser D et al. A European Renal Best 11. Xu G et al. Identifying acute kidney injury real-time electronic alert based on the
Practice (ERBP) position statement on in the community - a novel informatics RIFLE criteria for acute kidney injury
the Kidney Disease Improving Global approach. J Nephrol. 2015;pii:hcv020. in ICU patients. Acta Clin Belg Suppl.
Outcomes (KDIGO) clinical practice [Epub ahead of print]. 2007;(2):322-5.
guidelines on acute kidney injury: part 1: 12. Chertow GM et al. Acute kidney injury, 18. Selby NM et al. Use of electronic
definitions, conservative management mortality, length of stay, and costs in results reporting to diagnose and monitor
and contrast-induced nephropathy. hospitalized patients. J Am Soc Nephrol. AKI in hospitalized patients. Clin J Am
Nephrol Dial Transplant. 2012;27(12): 2005;16(11):3365-70. Soc Nephrol. 2012;7(4):533-40.
4263-72. 13. Kerr M et al. The economic impact of 19. Selby NM. Electronic alerts for
6. Lafrance JP, Miller DR. Defining acute kidney injury in England. Nephrol acute kidney injury. Curr Opin Nephrol
NEPHROLOGY • July 2015 EMJ EUROPEAN MEDICAL JOURNAL 81
Hypertens. 2013;22(6):637-42. intravenous fluid administration strategy to chronic dialysis in survivors of severe
20. Wilson FP et al. Automated, and kidney injury in critically ill adults. acute kidney injury: a competing risk
electronic alerts for acute kidney injury: JAMA. 2012;308(15):1566-72. study. BMC Nephrol. 2014;15:114.
a single-blind, parallel-group, randomised 35. Shaw AD et al. Major complications, 50. Coca SG et al. Chronic kidney disease
controlled trial. Lancet. 2015;doi:10.1016/ mortality, and resource utilization after after acute kidney injury: a systematic
S0140-6736(15)60266-5. [Epub ahead of open abdominal surgery: 0.9% saline review and meta-analysis. Kidney Int.
print]. compared to Plasma-Lyte. Ann Surg. 2012;81(5):442-8.
21. Prowle J et al. Renal blood flow, 2012;255(5):821-9. 51. Bucaloiu ID et al. Increased risk of
fractional excretion of sodium and acute 36. Hansen PB et al. Chloride regulates death and de novo chronic kidney disease
kidney injury: time for a new paradigm? afferent arteriolar contraction in following reversible acute kidney injury.
Curr Opin Crit Care. 2012;18(6):585-92. response to depolarization. Hypertension. Kidney Int. 2012;81(5):477-85.
22. Gomez H et al. A unified theory 1998;32(6):1066-70. 52. Horne KL et al. The effects of acute
of sepsis-induced acute kidney 37. Chowdhury AH et al. A randomized, kidney injury on long-term renal function
injury: inflammation, microcirculatory controlled, double-blind crossover study and proteinuria in a general hospitalised
dysfunction, bioenergetics, and the on the effects of 2-L infusions of 0.9% population. Nephron Clin Pract.
tubular cell adaptation to injury. Shock. saline and plasma-lyte(R) 148 on renal 2014;128(1-2):192-200.
2014;41(1):3-11. blood flow velocity and renal cortical 53. Wu VC et al. Long-term risk of
23. Chua HR et al. Acute kidney injury tissue perfusion in healthy volunteers. coronary events after AKI. J Am Soc
after cardiac arrest. Resuscitation. Ann Surg. 2012;256(1):18-24. Nephrol. 2014;25(3):595-605.
2012;83(6):721-7. 38. Wilcox CS. Regulation of renal blood 54. Wu VC et al. The impact of acute
24. Togel F, Westenfelder C. Recent flow by plasma chloride. J Clin Invest. kidney injury on the long-term risk of
advances in the understanding of acute 1983;71(3):726-35. stroke. J Am Heart Assoc. 2014;3(4):
kidney injury. F1000Prime Rep. 2014;6:83. 39. Grams ME et al. Fluid balance, diuretic e000933.
25. Kinsey GR, Okusa MD. Role of use, and mortality in acute kidney injury. 55. Wang WJ et al. The impact of acute
leukocytes in the pathogenesis of acute Clin J Am Soc Nephrol. 2011;6(5):966-73. kidney injury with temporary dialysis on
kidney injury. Crit Care. 2012;16(2):214. 40. Prowle JR et al. Fluid management the risk of fracture. J Bone Miner Res.
26. Fenhammar J et al. Toll-like receptor for the prevention and attenuation of 2014;29(3):676-84.
4 inhibitor TAK-242 attenuates acute acute kidney injury. Nat Rev Nephrol. 56. Johansen KL et al. Predictors of health
kidney injury in endotoxemic sheep. 2014;10(1):37-47. utility among 60-day survivors of acute
Anesthesiology. 2011;114(5):1130-7. 41. Poukkanen M et al. Hemodynamic kidney injury in the Veterans Affairs/
27. Grams ME, Rabb H. The distant organ variables and progression of acute National Institutes of Health Acute Renal
effects of acute kidney injury. Kidney Int. kidney injury in critically ill patients with Failure Trial Network Study. Clin J Am Soc
2012;81(10):942-8. severe sepsis: data from the prospective Nephrol. 2010;5(8):1366-72.
observational FINNAKI study. Crit Care. 57. Goldstein SL et al. AKI transition of
28. Tomlinson LA et al. ACE inhibitor
2013;17(6):R295. care: a potential opportunity to detect
and angiotensin receptor-II antagonist
prescribing and hospital admissions 42. Bourgoin A et al. Increasing mean and prevent CKD. Clin J Am Soc Nephrol.
with acute kidney injury: a longitudinal arterial pressure in patients with septic 2013;8(3):476-83.
ecological study. PLoS One. 2013;8(11): shock: effects on oxygen variables 58. Prowle JR et al. Serum creatinine
e78465. and renal function. Crit Care Med. changes associated with critical illness
2005;33(4):780-6. and detection of persistent renal
29. Marik PE, Cavallazzi R. Does the
central venous pressure predict fluid 43. Asfar P et al. High versus low blood- dysfunction after AKI. Clin J Am Soc
responsiveness? An updated meta- pressure target in patients with septic Nephrol. 2014;9(6):1015-23.
analysis and a plea for some common shock. N Engl J Med. 2014;370(17): 59. Go AS et al. The assessment, serial
sense. Crit Care Med. 2013;41(7):1774-81. 1583-93. evaluation, and subsequent sequelae of
30. Di Giantomasso D et al. Intrarenal 44. NICE. Acute kidney injury: Prevention, acute kidney injury (ASSESS-AKI) study:
blood flow distribution in hyperdynamic detection and management of acute design and methods. BMC Nephrol.
septic shock: Effect of norepinephrine. kidney injury up to the point of renal 2010;11:22.
Crit Care Med. 2003;31(10):2509-13. replacement therapy. NICE guidelines 60. ISRCTN - ISRCTN25405995:
[CG169]. 2013. Available at: http:// The Aki Risk In Derby (ARID) study.
31. Haase N et al. Hydroxyethyl starch
www.nice.org.uk/guidance/CG169. Last Available at: http://www.isrctn.com/
130/0.38-0.45 versus crystalloid or
accessed: 14 May 2015. ISRCTN25405995. Last accessed:
albumin in patients with sepsis: systematic
review with meta-analysis and trial 45. Horner D. Care bundles in intensive 16 April 2015.
sequential analysis. BMJ. 2013;346:f839. care. Contin Educ Anaesth Crit Care Pain. 61. Ostermann M et al. Clinical review:
2012;12(4):199-202. Biomarkers of acute kidney injury: where
32. Zarychanski R et al. Association
of hydroxyethyl starch administration 46. Hoste EA, De Corte W. Implementing are we now? Crit Care. 2012;16(5):233.
with mortality and acute kidney injury the Kidney Disease: Improving Global 62. Ostermann M. Diagnosis of acute
in critically ill patients requiring volume Outcomes/acute kidney injury guidelines kidney injury: Kidney Disease Improving
resuscitation: a systematic review and in ICU patients. Curr Opin Crit Care. Global Outcomes criteria and beyond.
meta-analysis. JAMA. 2013;309(7): 2013;19(6):544-53. Curr Opin Crit Care. 2014;20(6):581-7.
678-88. 47. McCullough PA. Contrast-induced 63. Ostermann M, Joannidis M. Biomarkers
33. Perel P et al. Colloids versus acute kidney injury. J Am Coll Cardiol. for AKI improve clinical practice: no.
crystalloids for fluid resuscitation in 2008;51(15):1419-28. Intensive Care Med. 2015;41(4):618-22.
critically ill patients. Cochrane Database 48. Chionh CY et al. Use of peritoneal 64. Rabito C et al. Accurate, fast, and
Syst Rev. 2013;2:CD000567. Dialysis in AKI: A Systematic Review. Clin convenient measurement of glomerular
34. Yunos NM et al. Association between J Am Soc Nephrol. 2013;8:1649-60. filtration rate in potential renal transplant
a chloride-liberal vs chloride-restrictive 49. Harel Z et al. Predictors of progression donors. Transplantation. 2010;90(5):510-7.
82 NEPHROLOGY • July 2015
View publication stats
EMJ EUROPEAN MEDICAL JOURNAL
Vous aimerez peut-être aussi
- Acute Kidney Injury: Current Concepts and New Insights: Key WordsDocument5 pagesAcute Kidney Injury: Current Concepts and New Insights: Key WordsIHPas encore d'évaluation
- AKI definition and use in practiceDocument12 pagesAKI definition and use in practicewelinPas encore d'évaluation
- Recognition and Management of Acute Kidney Injury: Thomas Oates and Shabbir MoochhalaDocument5 pagesRecognition and Management of Acute Kidney Injury: Thomas Oates and Shabbir MoochhalaIntan NoaPas encore d'évaluation
- AKI Perioperatif 2Document12 pagesAKI Perioperatif 2Kevin JohanesPas encore d'évaluation
- Periop AKIDocument12 pagesPeriop AKINavjot KaurPas encore d'évaluation
- Falla Renal 2011Document8 pagesFalla Renal 2011Mattya SalazarPas encore d'évaluation
- Síndrome Hepatorrenal Cirrosis Eur Gast J 2021Document9 pagesSíndrome Hepatorrenal Cirrosis Eur Gast J 2021Anabel GonzalezPas encore d'évaluation
- Global Epidemiology and Outcomes of Acute Kidney InjuryDocument19 pagesGlobal Epidemiology and Outcomes of Acute Kidney Injuryredouane bennaiPas encore d'évaluation
- ACS To AkiDocument9 pagesACS To AkiLink BuiPas encore d'évaluation
- Incidence and Characteristics of Acute Kidney Injury in Severe Diabetic KetoacidosisDocument6 pagesIncidence and Characteristics of Acute Kidney Injury in Severe Diabetic KetoacidosisMarcelliaPas encore d'évaluation
- Understanding Chronic Kidney Disease: A guide for the non-specialistD'EverandUnderstanding Chronic Kidney Disease: A guide for the non-specialistÉvaluation : 4 sur 5 étoiles4/5 (3)
- Acut Kidney InjuryDocument12 pagesAcut Kidney InjuryorriPas encore d'évaluation
- Does This Patient Have Acute Kidney Injury? An AKI ChecklistDocument4 pagesDoes This Patient Have Acute Kidney Injury? An AKI ChecklistOlga HMPas encore d'évaluation
- Management of Acute Kidney Injury: Core Curriculum 2018Document13 pagesManagement of Acute Kidney Injury: Core Curriculum 2018Kholida NabilaPas encore d'évaluation
- Essay 2.0Document25 pagesEssay 2.0Ahmed NassarPas encore d'évaluation
- Acute Kidney Injury - Final Draft (08 January 2011)Document58 pagesAcute Kidney Injury - Final Draft (08 January 2011)Mary-kate HengPas encore d'évaluation
- Acute Kidney Injury After Cardiac Surgery Chew2018Document54 pagesAcute Kidney Injury After Cardiac Surgery Chew2018Oğuz KayıkçıPas encore d'évaluation
- Acute Kidney Injury in Critically Ill PatientsDocument27 pagesAcute Kidney Injury in Critically Ill PatientsDeviana HidayatiPas encore d'évaluation
- WWW - Uwonephrology.ca Pdfs Academichalfday 20110308 AKIPart12011Document8 pagesWWW - Uwonephrology.ca Pdfs Academichalfday 20110308 AKIPart12011Ale Marques - TarólogoPas encore d'évaluation
- Joannidis Et Al-2023-Intensive Care MedicineDocument4 pagesJoannidis Et Al-2023-Intensive Care MedicineOmyRojasPas encore d'évaluation
- Kidneydiseaseandthe Nexusofchronickidney DiseaseandacutekidneyinjuryDocument33 pagesKidneydiseaseandthe Nexusofchronickidney DiseaseandacutekidneyinjuryMardauc AnaidPas encore d'évaluation
- Overview of The Management of Acute Kidney Injury in Adults - UpToDateDocument13 pagesOverview of The Management of Acute Kidney Injury in Adults - UpToDateDaniely FreitasPas encore d'évaluation
- Fluid and Electrolyte Problems in Renal DysfunctionDocument5 pagesFluid and Electrolyte Problems in Renal Dysfunctionfachrudin arPas encore d'évaluation
- Personalized Acute Kidney Injury TreatmentDocument8 pagesPersonalized Acute Kidney Injury TreatmentGabriela PachecoPas encore d'évaluation
- AKI PathogenesisDocument11 pagesAKI PathogenesisKaren RamPas encore d'évaluation
- Kdoki y KdigoDocument24 pagesKdoki y KdigoIsrael Armida SodanargPas encore d'évaluation
- Novel Aspects of Pharmacological Therapies For Acute Renal FailureDocument16 pagesNovel Aspects of Pharmacological Therapies For Acute Renal FailureproluvieslacusPas encore d'évaluation
- 16 PDFDocument8 pages16 PDFAkhileshPas encore d'évaluation
- The Definition of Acute Kidney Injury and Its Use in PracticeDocument12 pagesThe Definition of Acute Kidney Injury and Its Use in PracticeErwin SiahaanPas encore d'évaluation
- Management of Acute Kidney Injury - Core Curriculum 2018Document13 pagesManagement of Acute Kidney Injury - Core Curriculum 2018Enrique Aguilar MPas encore d'évaluation
- Global EpidemiologyDocument19 pagesGlobal EpidemiologySoniamartilovaPas encore d'évaluation
- Chew, Dennis - Acute - Kidney - Disease - Cats - STYLEDDocument7 pagesChew, Dennis - Acute - Kidney - Disease - Cats - STYLEDPatricia QueroPas encore d'évaluation
- Electrolyte Imbalance in CKD PatientsDocument4 pagesElectrolyte Imbalance in CKD PatientsEditor IJTSRDPas encore d'évaluation
- PAIM 20 00052 - RevDocument7 pagesPAIM 20 00052 - RevRiswanto RuslanPas encore d'évaluation
- 546 FullDocument3 pages546 FullAndreea GheorghiuPas encore d'évaluation
- AKI Case Discussion 2.0Document3 pagesAKI Case Discussion 2.0Mary Dominique RomoPas encore d'évaluation
- Hepatorenal SyndromeDocument14 pagesHepatorenal SyndromeVerónica Duménez JofréPas encore d'évaluation
- The Association Between Urine Output, Creatinine Elevation, and DeathDocument9 pagesThe Association Between Urine Output, Creatinine Elevation, and DeathTrahmono SrPas encore d'évaluation
- Article 1576845020 PDFDocument5 pagesArticle 1576845020 PDFFatima Habib JajjaPas encore d'évaluation
- Indicaciones AkiDocument8 pagesIndicaciones Akijair giancarlo villanueva arteagaPas encore d'évaluation
- Article AcuteKidneyInjuryInTheCriticalDocument16 pagesArticle AcuteKidneyInjuryInTheCriticalJoão João MendesPas encore d'évaluation
- Prevention and Management of Acute Kidney InjuryDocument30 pagesPrevention and Management of Acute Kidney InjuryIren DawsonPas encore d'évaluation
- A Study To Assess Changes in The Hematological Profile in Chronic Kidney DiseaseDocument3 pagesA Study To Assess Changes in The Hematological Profile in Chronic Kidney Diseasemandhalanarshimlu48141Pas encore d'évaluation
- Acute Renal Failure in The ICU PulmCritDocument27 pagesAcute Renal Failure in The ICU PulmCritchadchimaPas encore d'évaluation
- Aki AcpDocument21 pagesAki AcpAndrés FelipePas encore d'évaluation
- Diagnosis and Treatment of Acute Kidney Injury in PediatricsDocument13 pagesDiagnosis and Treatment of Acute Kidney Injury in PediatricsagungPas encore d'évaluation
- Aetiology: Save Time & Improve Your PDP On Patient - Co.ukDocument9 pagesAetiology: Save Time & Improve Your PDP On Patient - Co.ukBaihaqi SaharunPas encore d'évaluation
- Acute Kidney InjuryDocument9 pagesAcute Kidney InjuryRobertPas encore d'évaluation
- Biomarcadores Post Aki A ErcDocument12 pagesBiomarcadores Post Aki A ErcGiss UrizarPas encore d'évaluation
- Jurnal Aki 2018Document13 pagesJurnal Aki 2018Arief TricahyonoPas encore d'évaluation
- Role of Kidney Injury in Sepsis: Review Open AccessDocument6 pagesRole of Kidney Injury in Sepsis: Review Open AccessnudhakoPas encore d'évaluation
- Management of Oliguria: Understanding The DiseaseDocument4 pagesManagement of Oliguria: Understanding The DiseaseJhosep SilvestrePas encore d'évaluation
- Definition and Classification of Kidney Diseases: EditorialDocument3 pagesDefinition and Classification of Kidney Diseases: EditorialdianaPas encore d'évaluation
- IradefDocument8 pagesIradefSimi-Deiu ZksiPas encore d'évaluation
- The Patient With Cirrhosis in TheDocument9 pagesThe Patient With Cirrhosis in TheJoseph Antonio Apaza GómezPas encore d'évaluation
- Risk of Seizures and Status Epilepticus in Older Patients With Liver Disease 2018Document6 pagesRisk of Seizures and Status Epilepticus in Older Patients With Liver Disease 2018Pablo Sebastián SaezPas encore d'évaluation
- Review Article: Epidemiology of Acute Kidney Injury in The Intensive Care UnitDocument10 pagesReview Article: Epidemiology of Acute Kidney Injury in The Intensive Care UnitmarinarizkyutamiPas encore d'évaluation
- Improving Recognition and Management of Acute Kidney Injury: Acute Medicine Journal September 2014Document6 pagesImproving Recognition and Management of Acute Kidney Injury: Acute Medicine Journal September 2014adil shabbirPas encore d'évaluation
- EssayDocument24 pagesEssayAhmed NassarPas encore d'évaluation
- CKD Classification and ManagementDocument20 pagesCKD Classification and ManagementAhmed AliPas encore d'évaluation
- Medico Legal Aspects of DeathDocument206 pagesMedico Legal Aspects of Deathrosana f.rodriguez83% (12)
- Pathophysiology of BREAST CANCERDocument1 pagePathophysiology of BREAST CANCERAlinor Abubacar100% (6)
- Understanding Meningitis: Causes, Symptoms and TreatmentDocument49 pagesUnderstanding Meningitis: Causes, Symptoms and TreatmentDrAbhilash RMPas encore d'évaluation
- How It Works Book of The HumanDocument180 pagesHow It Works Book of The Humanyassomelek100% (1)
- Drug 1Document2 pagesDrug 1Nicholas TaglePas encore d'évaluation
- The Ontogenetic Basic of Human AnatomyDocument18 pagesThe Ontogenetic Basic of Human AnatomymeseniaPas encore d'évaluation
- Traumatic Brain Injury PresentationDocument14 pagesTraumatic Brain Injury Presentationapi-413607178Pas encore d'évaluation
- Engebretsen2011, INSULINA EN B BLOQDocument7 pagesEngebretsen2011, INSULINA EN B BLOQFabiola Delia Rosas AlarcónPas encore d'évaluation
- FixationDocument3 pagesFixationficatPas encore d'évaluation
- ORAL BREATHINGDocument94 pagesORAL BREATHINGVivek Gaurav100% (1)
- Head Toe Physical AssessmentDocument2 pagesHead Toe Physical Assessmentzbestgurl100% (2)
- Sexual Precocity PDFDocument5 pagesSexual Precocity PDFmist73Pas encore d'évaluation
- Child Development A Thematic Approach 6th Edition Bukatko Test BankDocument36 pagesChild Development A Thematic Approach 6th Edition Bukatko Test Bankunframecizarsidquu100% (21)
- Arab Board Orthopedic Exam June 2013Document35 pagesArab Board Orthopedic Exam June 2013Nasser AlbaddaiPas encore d'évaluation
- Rhopalocera (Butterfly) : FunctionsDocument18 pagesRhopalocera (Butterfly) : FunctionsChris Anthony EdulanPas encore d'évaluation
- Dental Sedation TechniquesDocument28 pagesDental Sedation TechniquesRamesh CandyPas encore d'évaluation
- Essencial Phrasal VerbsDocument4 pagesEssencial Phrasal VerbsalverePas encore d'évaluation
- Effects of Cypermethrin and Diazinon On Haematology of Labeo Rohita (HDocument5 pagesEffects of Cypermethrin and Diazinon On Haematology of Labeo Rohita (Hkunalfcri09Pas encore d'évaluation
- Chapter 9 &10 - Gene ExpressionDocument4 pagesChapter 9 &10 - Gene ExpressionMahmOod GhPas encore d'évaluation
- F4D 24Document2 pagesF4D 24Ivan WongPas encore d'évaluation
- ADocument2 pagesAイ ロPas encore d'évaluation
- Kantor Cabang: BANJARMASIN - 1701 FKTP: Kertak Hanyar - 17040601Document6 pagesKantor Cabang: BANJARMASIN - 1701 FKTP: Kertak Hanyar - 17040601Ic-tika Siee ChuabbiePas encore d'évaluation
- Reaching and Being ReachedDocument18 pagesReaching and Being ReachedJoão Vitor Moreira Maia100% (1)
- Cancer DiseaseDocument7 pagesCancer Diseasenbs saraswathiPas encore d'évaluation
- Kidney PowerPoint Presentation TemplateDocument14 pagesKidney PowerPoint Presentation TemplateMedicinePPT100% (1)
- Arjun Chauhan (Bio)Document52 pagesArjun Chauhan (Bio)Sharad ChoudharyPas encore d'évaluation
- Lesson 1 Forensic 5Document7 pagesLesson 1 Forensic 5Marcos DmitriPas encore d'évaluation
- Types of Plant HormonesDocument6 pagesTypes of Plant HormonesKarren ReyesPas encore d'évaluation
- Herpes Zoster OphtalmicusDocument12 pagesHerpes Zoster OphtalmicusVicky LumalessilPas encore d'évaluation