Académique Documents
Professionnel Documents
Culture Documents
406-01. Manuscript (Article Text) - 1308-1-10-20130405
Transféré par
Jeffrey RamosTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
406-01. Manuscript (Article Text) - 1308-1-10-20130405
Transféré par
Jeffrey RamosDroits d'auteur :
Formats disponibles
J Nep Med Assoc 2006; 45: 291-294
Serum Urea, Creatinine and Electrolyte Status
in Patients Presenting with Acute Gastroenteritis
KC M*, Gurubacharya D L*, Lohani R*, Rauniyar A*
* KMC Teaching Hospital, Sinamangal, Kathmandu, Nepal
abstract
The present study was undertaken to estimate the serum urea, creatinine and electrolyte status
of patients presenting with acute gastroenteritis. Sixty patients who presented to Kathmandu
Medical College and Teaching hospital from 15 June to 15 July 2005 with acute diarrhea with or
without associated vomiting, causing dehydration severe enough to require hospital admission
were investigated for serum urea, creatinine and electrolyte level. Out of 60 patients investigated,
serum sodium and potassium level were available for 34 patients. Only one (2.9%) patients had
sodium level below 135mEq/l, thirty two (94.11%) had sodium level between 135-146 mEq/l and
one (2.9%) had sodium level above 146mEq/l. Similarly 9 (26.47%) patients had potassium level
below 3.5mEq/l, 22 (64.70%) patients had potassium level between 3.5-5 mEq/l and 3 (8.82%)
patients had level above 5 mEq/l. Serum urea and creatinine level were available for 47 patients.
36 (76.59%) patients had serum urea level between 15-45mg/dl and 11 (23.40%) patients had urea
level above 45 mg/dl. 35 (74.46%) patients had serum creatinine level between 0.5-1.4 mg/dl and
12 (25.53%) had serum creatinine level above 1.4 mg/dl. In this study hypokalaemia was noticed
more than hyponatremia and significant number of patients also showed increased level of serum
urea and creatinine. Therefore, serum urea, creatinine and electrolytes should be closely monitored
in patients with acute gastroenteritis.
Key Words: Acute gastroenteritis, urea, creatinine, electrolyte.
Address for correspondence :
Dr. Mathura KC
KMC Teaching Hospital, Sinamangal, Kathmandu, Nepal
Email: kcmathura@wlink.com.np
Received Date : 5th May, 2005
Accepted Date : 11th Jul, 2006
JNMA, Jul - Sep, 2006, 45
KC et al. Serum Urea, Creatinine and Electrolyte Status ... 292
Introduction admission were included in the study. All patients were
assessed clinically and blood samples were sent to labora-
Despite reductions in mortality worldwide, diarrhea still tory for serum level of urea, creatinine and electrolytes at
accounts for more than 2 million deaths annually1 and is the time of admission before patients were hydrated with
associated with impaired physical and cognitive develop- intravenous isotonic saline.
ment in resource-limited countries.2 In the United States
an estimated 211 million to 375 million episodes of acute Results
diarrhea occur each year (91.4 episodes per person per
year); such episodes are responsible for more than 900,000 Out of sixty patients investigated for acute diarrhea, 38
hospitalization and 6000 deaths annually.3,4 (63.3%) were male and 22 (36.67%) were female. Out of
60 patients investigated, serum sodium and potassium level
Acute diarrhea, defined as an increase frequency of defeca- were available for 34 patients. Only one (2.9%) patients
tion (three or more times per day or at least 200 grams of had sodium level below 135mEq/l, thirty two (94.11%) had
stool per day) lasting less than 14 days, may be accompa- sodium level between 135-146 mEq/l and one (2.9%) had
nied by nausea, vomiting, abdominal cramping, clinically sodium level above 146mEq/l. Similarly 9 (26.47%) patients
significant symptoms, or malnutrition.5 Acute diarrhea is had potassium level below 3.5mEq/l, 22 (64.70%) patients
among the most common problems encountered by the had potassium level between 3.5-5 mEq/l and 3 (8.82%)
physician in the developing countries. Serum electrolytes patients had level above 5 mEq/l as shown in Table I.
are commonly ordered in the evaluation of patients with
acute diarrhea. Complications develop exclusively from Serum urea and creatinine level were available for 47 pa-
the effect of volume and electrolyte depletion and include tients. 36 (76.59%) patients had serum urea level between
renal failure due to acute tubular necrosis in some cases. 15-45mg/dl and 11 (23.40%) patients had urea level above
45 mg/dl. 35 (74.46%) patients had serum creatinine level
The aim of this clinical study was to evaluate prospectively between 0.5-1.4 mg/dl and 12 (25.53%) had serum creati-
serum level of urea, creatinine and electrolytes in patients nine level above 1.4 mg/dl as shown in Table II.
presenting with acute gastroenteritis.
Discussion
Materials and methods
Although differential diagnosis of infectious diarrhea is
Sixty patients who presented to Kathmandu Medical Col- broad, the clinical history can help guide the clinician
lege and Teaching hospital from 15 June to 15 July, 2005 towards the appropriate evaluation. Viruses are the major
with acute diarrhea with or without associated vomiting,
causing dehydration severe enough to require hospital
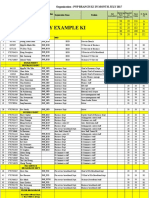
Table I: Serum sodium and potassium level of patients (n=34)
JNMA, Jul - Sep, 2006, 45
293 KC et al. Serum Urea, Creatinine and Electrolyte Status ...
Table II: Serum urea and creatinine level of patients (n=47)
cause of diarrhea worldwide. When diarrhea is a result of
infection, invasive bacteria is the most likely cause with References
features of large volume watery stool and diffuse abdomi-
nal cramps.6 Patients with severe dehydration should have 1. Kosek M, Bern C, Guerrant RL. The global burden of diarrhoeal
blood drawn for complete blood count, serum urea, creati- disease, as estimated from studies published between 1992-2000.
nine and electrolytes, Extreme dehydration can be evalu- Bull World health Organ 2003; 81; 197-204.
ated by serum electrolytes. Serum urea and bicarbonate
can be helpful in estimation of fluid deficit independently 2. Guerrant RL, Kosek M, Lima AA, Lorntz B, Guyatt HL. Updating
from serum sodium.7 Quantification of serum electrolytes the DALYs for diarrhoeal disease. Trends Parasitol 2002; 18:191-3.
in severely dehydrated children or whose history and physi-
cal findings are inconsistent with pure diarrheal episode is 3. Herikstad H, Yang S, Van Gilder TJ, Vugia D, Hadler J, Blake P,
helpful, though most diarrheal episode in well nourished Deneen V, Shiferaw B, Angulo FJ. A population-based estimate
infants leads to isotonic dehydration.8 of the burden of diarrhoeal illness in the United States: FoodNet,
1996-7. Epidemiol Infect 2002; 129:9-17.
Stool routine examination and microscopic examination
can support empirical antibiotic therapy9-11 and is cost ef- 4. Mead PS, Slutsker L, Dietz V, McCaig LF, Bresee JS, Shapiro C,
fective.12-15 Stool culture and sensitivity is recommended Griffin PM, Tauxe RV. Food-related illness and death in the United
but not necessary as yield is only 2%.6,9,10,11,16 Primary States. Emerg Infect Dis 1999; 5:607-25.
therapy is oral rehydration solution (ORS). But patient
should be hydrated with intravenous isotonic saline or 5. Thielman NM, Guerrant RL. Clinical practice. Acute infectious
ringer lactate solution in severe dehydration, as oral intake diarrhea. N Engl J Med. 2004; 350:38-47.
in severe dehydration will not be adequate to overcome
dehydration because the profuse watery diarrhea represents 6. Caceres VM, Ball RT, Somerfeldt SA, Mackey RL, Nichols SE,
impairment of normal interstitial absorption. MacKenzie WR, Herwaldt BL. A foodborne outbreak of cyclospo-
riasis caused by imported raspberries. J Fam Pract 1998; 47:231-4.
Conclusion
7. Yilmaz K, Karabocuoglu M, Citak A, Uzel N. Evaluation of laboratory
In this study hypokalaemia was noticed more than hypo- tests in dehydrated children with acute gastroenteritis. J Paediatr
natremia and significant number of patients also showed Child Health 2002; 38:226-8.
increased level of serum urea and creatinine. Therefore,
serum urea, creatinine and electrolytes should be closely 8. Holliday M. The evolution of therapy for dehydration: should deficit
monitored in patients with acute gastroenteritis. therapy still be taught? Pediatrics 1996; 98:171-7.
JNMA, Jul - Sep, 2006, 45
KC et al. Serum Urea, Creatinine and Electrolyte Status ... 294
30:3213-6.
9. Harris JC, Dupont HL, Hornick RBFecal leukocytes in diarrheal
illness. Ann Intern Med 1972; 76:697-703. 14. Meropol SB, Luberti AA, De Jong AR. Yield from stool testing of
pediatric inpatients. Arch Pediatr Adolesc Med 1997; 151:142-5.
10. McNeely WS, Dupont HL, Mathewson JJ, Oberhelman RA, Erics-
son CD. Occult blood versus fecal leukocytes in the diagnosis of 15. Mayer CL, Palmer CJ. Evaluation of PCR, nested PCR, and fluo-
bacterial diarrhea: a study of U.S. travelers to Mexico and Mexican rescent antibodies for detection of Giardia and Cryptosporidium
children. Am J Trop Med Hyg 1996; 55:430-3. species in wastewater. Appl Environ Microbiol 1996; 62:2081-5.
11. Bardhan PK, Beltinger J, Beltinger RW, Hossain A, Mahalanabis 16. Keusch GT, Waldor MK. Cholera and other vibrioses, in Harrison’s
D, Gyr K. Screening of patients with acute infectious diarrhoea: Principal of Internal Medicine, 15th edition, Braunwald, Fauci, et
evaluation of clinical features, faecal microscopy, and faecal occult al (eds). Mc Graw-Hill, Inc, 2001, 980-89.
blood testing. Scand J Gastroenterol 2000; 35:54-60.
12. Siegel DL, Edelstein PH, Nachamkin I. Inappropriate testing for
diarrheal diseases in the hospital. JAMA 1990; 263:979-82.
13. Morris AJ, Wilson ML, Reller LB. Application of rejection criteria
for stool ovum and parasite examinations. J Clin Microbiol 1992;
JNMA, Jul - Sep, 2006, 45
Vous aimerez peut-être aussi
- Diabetic Ketoacidosis in A Hospital Based Population in PakistanDocument6 pagesDiabetic Ketoacidosis in A Hospital Based Population in Pakistanhasnainhamid668Pas encore d'évaluation
- Complementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderD'EverandComplementary and Alternative Medical Lab Testing Part 6: Liver and GallbladderPas encore d'évaluation
- Bellomo 2006Document7 pagesBellomo 2006Manal regraguiPas encore d'évaluation
- Jurnal GEADocument5 pagesJurnal GEARian KurniawanPas encore d'évaluation
- Frequency of Hyponatraemia and Hypokalaemia in Malnourished Children With Acute DiarrhoeaDocument4 pagesFrequency of Hyponatraemia and Hypokalaemia in Malnourished Children With Acute DiarrhoeaRaja Bajak LautPas encore d'évaluation
- Manjuck 2005Document5 pagesManjuck 2005Alejandro PerezPas encore d'évaluation
- FREQUENCY - OF - NEPHROPATHY - AND - ITS - RELATION - TO - METAB (Diskusi)Document5 pagesFREQUENCY - OF - NEPHROPATHY - AND - ITS - RELATION - TO - METAB (Diskusi)lusiyanaPas encore d'évaluation
- Indeks Diastase 2 PDFDocument5 pagesIndeks Diastase 2 PDFddew indahPas encore d'évaluation
- Complementary and Alternative Medical Lab Testing Part 8: UrologyD'EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyÉvaluation : 3 sur 5 étoiles3/5 (1)
- Fluidmanagement PDFDocument8 pagesFluidmanagement PDFJAMAL HUDAPas encore d'évaluation
- PIIS240545772100245XDocument5 pagesPIIS240545772100245Xsulemi castañonPas encore d'évaluation
- Jcem 2743Document4 pagesJcem 2743Yaser MPas encore d'évaluation
- ERC PotasioDocument10 pagesERC PotasioAbrilPas encore d'évaluation
- 11 134 v12n4 2013 PredictingPortalDocument11 pages11 134 v12n4 2013 PredictingPortalDevy Widiya GrafitasariPas encore d'évaluation
- Fluid ResuscitationDocument81 pagesFluid Resuscitationmaya_fitrianaPas encore d'évaluation
- Reliability of Mini Nutritional Assessment in Hemodialysis Compared With Subjective Global AssessmentDocument6 pagesReliability of Mini Nutritional Assessment in Hemodialysis Compared With Subjective Global AssessmentyafanitaizzatiPas encore d'évaluation
- Manuscript 1Document4 pagesManuscript 1maryPas encore d'évaluation
- Letters: Serum and Ascitic Fluid CA-125 Level in Patients With AscitesDocument8 pagesLetters: Serum and Ascitic Fluid CA-125 Level in Patients With AscitespudjoPas encore d'évaluation
- Ebsco ContentServerDocument7 pagesEbsco ContentServerHailey LapinePas encore d'évaluation
- Autoimmune Hepatitis in Children: Giorgina Mieli-Vergani, MD, PHD, FRCP, FRCPCH, Diego Vergani, MD, PHD, Frcpath, FRCPDocument12 pagesAutoimmune Hepatitis in Children: Giorgina Mieli-Vergani, MD, PHD, FRCP, FRCPCH, Diego Vergani, MD, PHD, Frcpath, FRCPFildzah DheaPas encore d'évaluation
- Concentrations Ascorbic Acid in Plasma and White Blood Patients With Cancer and Noncancerous Chronic DiseaseDocument7 pagesConcentrations Ascorbic Acid in Plasma and White Blood Patients With Cancer and Noncancerous Chronic DiseaseDharmaMaya ChandrahasPas encore d'évaluation
- (Doi 10.1007/978!1!4020-9646-4 - 41) Shirahata, Sanetaka Ikura, Koji Nagao, Masaya Ichikawa, Akira - Animal Cell Technology - Basic & Applied Aspects  - Nordenau Phenomenonâ -  - Application of NaDocument7 pages(Doi 10.1007/978!1!4020-9646-4 - 41) Shirahata, Sanetaka Ikura, Koji Nagao, Masaya Ichikawa, Akira - Animal Cell Technology - Basic & Applied Aspects  - Nordenau Phenomenonâ -  - Application of NaAndry SudhariandiPas encore d'évaluation
- Thesis Final University Copy 25.09.2013 SubmissionDocument173 pagesThesis Final University Copy 25.09.2013 SubmissionAmit GoelPas encore d'évaluation
- Rhabdomyolysis AbstractDocument1 pageRhabdomyolysis Abstractapi-284057899Pas encore d'évaluation
- Clinical Profile, Degree of Severity and Underlying Factors of AcuteDocument5 pagesClinical Profile, Degree of Severity and Underlying Factors of AcuteHumayera KabirPas encore d'évaluation
- Hiperspenisme 2Document6 pagesHiperspenisme 2anakfkubPas encore d'évaluation
- Plasma Leptin Levels in Rats With PancreatitisDocument6 pagesPlasma Leptin Levels in Rats With PancreatitisAndykaYayanSetiawanPas encore d'évaluation
- Factors Predicting Malnutrition in Hemodialysis Patients: A Cross-Sectional StudyDocument10 pagesFactors Predicting Malnutrition in Hemodialysis Patients: A Cross-Sectional StudyMarco TolentinoPas encore d'évaluation
- ACPN AbstractsDocument21 pagesACPN AbstractsPediatric NephrologyPas encore d'évaluation
- Ojsadmin, 176Document4 pagesOjsadmin, 176Signor 2019Pas encore d'évaluation
- Negative Impact of Hypocaloric Feeding and Energy Balance On Clinical Outcome in ICU PatientsDocument8 pagesNegative Impact of Hypocaloric Feeding and Energy Balance On Clinical Outcome in ICU PatientsDaniela HernandezPas encore d'évaluation
- RL Vs NS Dalam KADDocument7 pagesRL Vs NS Dalam KADIkek StanzaPas encore d'évaluation
- Fmed 07 603725Document8 pagesFmed 07 603725Rskg PpniPas encore d'évaluation
- Prevalence and Potential Risk Factors of Hypokalemia in Pediatric Patients With Diabetic KetoacidosisDocument2 pagesPrevalence and Potential Risk Factors of Hypokalemia in Pediatric Patients With Diabetic KetoacidosisAti Rahmi PurwandariPas encore d'évaluation
- Complementary and Alternative Medical Lab Testing Part 16: HematologyD'EverandComplementary and Alternative Medical Lab Testing Part 16: HematologyPas encore d'évaluation
- ALF 418RLE Group1Document22 pagesALF 418RLE Group1PAOLA LUZ CRUZPas encore d'évaluation
- Evaluation of Protein-Energy Wasting and Inflammation On Patients Undergoing Continuous Ambulatory Peritoneal Dialysis and Its CorrelationsDocument8 pagesEvaluation of Protein-Energy Wasting and Inflammation On Patients Undergoing Continuous Ambulatory Peritoneal Dialysis and Its CorrelationsnuvitaPas encore d'évaluation
- ALF 418RLE Group1Document21 pagesALF 418RLE Group1PAOLA LUZ CRUZPas encore d'évaluation
- Diarrhea Associated With Typhoid Fever: ParatyphiDocument6 pagesDiarrhea Associated With Typhoid Fever: ParatyphiNadya Ayu AnanditaPas encore d'évaluation
- Adult Minimal-Change Disease: Clinical Characteristics, Treatment, and OutcomesDocument9 pagesAdult Minimal-Change Disease: Clinical Characteristics, Treatment, and OutcomesMutiara RizkyPas encore d'évaluation
- Ariceta, 2021Document13 pagesAriceta, 2021ValentinaPas encore d'évaluation
- Cancer Antigen-125 As A Marker of Ascites in Patients With Liver CirrhosisDocument4 pagesCancer Antigen-125 As A Marker of Ascites in Patients With Liver CirrhosiselisasusantiPas encore d'évaluation
- DR T Dinesh Guide DR Baba YelkeDocument27 pagesDR T Dinesh Guide DR Baba YelkeDinesh AshwinPas encore d'évaluation
- Protein Energy Malnutrition in CKD PatientsDocument4 pagesProtein Energy Malnutrition in CKD PatientsEditor IJTSRDPas encore d'évaluation
- Jurnal DWIDocument6 pagesJurnal DWIDwi Asti Lestari PandePas encore d'évaluation
- Clinical Course of Diabetic Ketoacidosis in Hypertriglyceridemic Pancreatitis Pancreas 2015Document4 pagesClinical Course of Diabetic Ketoacidosis in Hypertriglyceridemic Pancreatitis Pancreas 2015América FloresPas encore d'évaluation
- Journal of Microscopy and Ultrastructure: Nora Nasir Al HassanDocument4 pagesJournal of Microscopy and Ultrastructure: Nora Nasir Al HassanAnis RanisPas encore d'évaluation
- Kuthiroly2021 Article LipoproteinLipaseDeficiencyDocument7 pagesKuthiroly2021 Article LipoproteinLipaseDeficiencybrajendra singhPas encore d'évaluation
- Asam BasaDocument7 pagesAsam BasaRabiatul 'raney' AdawiyahPas encore d'évaluation
- 1 s2.0 S168719792100040X MainDocument4 pages1 s2.0 S168719792100040X MainfelipethePas encore d'évaluation
- Bahan CKD Jurnal ProposalDocument6 pagesBahan CKD Jurnal ProposalArjunaPamungkasPas encore d'évaluation
- 10.1007@s10157 020 01867 yDocument6 pages10.1007@s10157 020 01867 yGin RummyPas encore d'évaluation
- Nutrients: Nutritional Adequacy and Latent Tuberculosis Infection in End-Stage Renal Disease PatientsDocument8 pagesNutrients: Nutritional Adequacy and Latent Tuberculosis Infection in End-Stage Renal Disease PatientsMarwa AmrangPas encore d'évaluation
- 163696-Article Text-423267-1-10-20171205Document6 pages163696-Article Text-423267-1-10-20171205Eric MurithiPas encore d'évaluation
- JGH 15535Document7 pagesJGH 15535Dolly JazmiPas encore d'évaluation
- Clinical Features and Outcomes of Children Admitted To The PICU Due To Rotavirus Infection GUNDocument5 pagesClinical Features and Outcomes of Children Admitted To The PICU Due To Rotavirus Infection GUNRoxana Ștefania DrăganPas encore d'évaluation
- Potassium Level Changes - Arrhythmia Contributing Factor in Chronic Kidney Disease PatientsDocument4 pagesPotassium Level Changes - Arrhythmia Contributing Factor in Chronic Kidney Disease PatientssigitPas encore d'évaluation
- AnemiaDocument9 pagesAnemiaJhonatan David Diaz IdarragaPas encore d'évaluation
- Clinical Sequelae From Overfeeding in Enterally FedDocument12 pagesClinical Sequelae From Overfeeding in Enterally FedKarla LapendaPas encore d'évaluation
- 1 Ajaz 2012Document4 pages1 Ajaz 2012Olivia Valentine LekiPas encore d'évaluation
- Higher Functions of The Nervous System - FasdfadsfDocument6 pagesHigher Functions of The Nervous System - FasdfadsfJeffrey RamosPas encore d'évaluation
- Biochemnistry Lab Module 1 Case 1 Number 3Document1 pageBiochemnistry Lab Module 1 Case 1 Number 3Jeffrey RamosPas encore d'évaluation
- RCOG Guidelines - Gestational Trophoblastic DiseaseDocument12 pagesRCOG Guidelines - Gestational Trophoblastic Diseasemob3100% (1)
- FasdfdasfDocument5 pagesFasdfdasfJeffrey RamosPas encore d'évaluation
- Digestive System Cont PDFDocument10 pagesDigestive System Cont PDFJeffrey RamosPas encore d'évaluation
- Geriatric PHSDFDSFDocument4 pagesGeriatric PHSDFDSFJeffrey RamosPas encore d'évaluation
- POGS CPG Abnormal Uterine BleedineDocument36 pagesPOGS CPG Abnormal Uterine Bleedinejandale57% (7)
- Issues On HIV and STI Among Pregnant Women: DR Helen Madamba, MD MPH-TM Fpogs FpidsogDocument32 pagesIssues On HIV and STI Among Pregnant Women: DR Helen Madamba, MD MPH-TM Fpogs FpidsogJeffrey RamosPas encore d'évaluation
- 6 VZDSFVDDocument2 pages6 VZDSFVDJeffrey RamosPas encore d'évaluation
- 胃腸科POMR範本fadfasdDocument11 pages胃腸科POMR範本fadfasdJeffrey RamosPas encore d'évaluation
- Issues On HIV and STI Among Pregnant Women: DR Helen Madamba, MD MPH-TM Fpogs FpidsogDocument32 pagesIssues On HIV and STI Among Pregnant Women: DR Helen Madamba, MD MPH-TM Fpogs FpidsogJeffrey RamosPas encore d'évaluation
- )Document11 pages)Jeffrey RamosPas encore d'évaluation
- Blueprints Pediatrics 6ed 2013 PDFDocument406 pagesBlueprints Pediatrics 6ed 2013 PDFGiorgos Gritzelas90% (10)
- Pathogenesis of Dengue Viral InfectionsDocument7 pagesPathogenesis of Dengue Viral InfectionsVenansius Ratno KurniawanPas encore d'évaluation
- Surgery AppendixqjjjjjjjjjjjjjjjjjjjjjDocument6 pagesSurgery AppendixqjjjjjjjjjjjjjjjjjjjjjJeffrey RamosPas encore d'évaluation
- OB Sample ReportsfdfadsDocument6 pagesOB Sample ReportsfdfadsJeffrey RamosPas encore d'évaluation
- Drug of ChoiceDocument2 pagesDrug of Choicetampupot90% (31)
- RADIO Liver and GallbladderDocument6 pagesRADIO Liver and GallbladderJeffrey RamosPas encore d'évaluation
- ABUSEDocument19 pagesABUSEJeffrey RamosPas encore d'évaluation
- Chronic Diarrhea in ChildrenDocument12 pagesChronic Diarrhea in ChildrenImanuel Far-FarPas encore d'évaluation
- Legal Med.: Archaeological Methods: Search and Recovery/Survey and ExcavationDocument2 pagesLegal Med.: Archaeological Methods: Search and Recovery/Survey and ExcavationJeffrey RamosPas encore d'évaluation
- RewaraewweDocument78 pagesRewaraewweJeffrey RamosPas encore d'évaluation
- RADIO Nuclear MedicineDocument8 pagesRADIO Nuclear MedicineJeffrey RamosPas encore d'évaluation
- Sample POMRDocument4 pagesSample POMRJeffrey RamosPas encore d'évaluation
- Philippines TB CP Guidelines 2006Document151 pagesPhilippines TB CP Guidelines 2006wiltechworksPas encore d'évaluation
- Leptospirosis CPG 2010 PDFDocument66 pagesLeptospirosis CPG 2010 PDFRogelio Junior RiveraPas encore d'évaluation
- Biochemnistry Lab Module 1 Case 1 Number 3Document1 pageBiochemnistry Lab Module 1 Case 1 Number 3Jeffrey RamosPas encore d'évaluation
- Anatomy PBL Lower Extremities 1Document2 pagesAnatomy PBL Lower Extremities 1Jeffrey RamosPas encore d'évaluation
- Adasds SDocument2 pagesAdasds SJeffrey RamosPas encore d'évaluation
- Ahmad Syihabudin: BiodataDocument2 pagesAhmad Syihabudin: BiodatabhjjqrgrwmPas encore d'évaluation
- Camless EnginesDocument4 pagesCamless EnginesKavya M BhatPas encore d'évaluation
- Operating Instructions: HTL-PHP Air Torque PumpDocument38 pagesOperating Instructions: HTL-PHP Air Torque PumpvankarpPas encore d'évaluation
- Xtype Power Train DTC SummariesDocument53 pagesXtype Power Train DTC Summariescardude45750Pas encore d'évaluation
- 1.161000 702010 New Perspectives 2ndedDocument43 pages1.161000 702010 New Perspectives 2ndedbimobimoprabowoPas encore d'évaluation
- MDI - Good Fellas - ScriptDocument20 pagesMDI - Good Fellas - ScriptRahulSamaddarPas encore d'évaluation
- Play ClawDocument2 pagesPlay ClawFrenda SeivelunPas encore d'évaluation
- Contemporary Philippine Arts From The Regions: Quarter 1Document11 pagesContemporary Philippine Arts From The Regions: Quarter 1JUN GERONAPas encore d'évaluation
- Manual de Operacion y MantenimientoDocument236 pagesManual de Operacion y MantenimientoalexPas encore d'évaluation
- RECYFIX STANDARD 100 Tipe 010 MW - C250Document2 pagesRECYFIX STANDARD 100 Tipe 010 MW - C250Dadang KurniaPas encore d'évaluation
- DN102-R0-GPJ-Design of Substructure & Foundation 28m+28m Span, 19.6m Width, 22m Height PDFDocument64 pagesDN102-R0-GPJ-Design of Substructure & Foundation 28m+28m Span, 19.6m Width, 22m Height PDFravichandraPas encore d'évaluation
- Operator'S Manual Diesel Engine: 2L41C - 2M41 - 2M41ZDocument110 pagesOperator'S Manual Diesel Engine: 2L41C - 2M41 - 2M41ZMauricio OlayaPas encore d'évaluation
- Ti05001 PDFDocument1 pageTi05001 PDFanggiePas encore d'évaluation
- Lenovo NotebooksDocument6 pagesLenovo NotebooksKamlendran BaradidathanPas encore d'évaluation
- European Construction Sector Observatory: Country Profile MaltaDocument40 pagesEuropean Construction Sector Observatory: Country Profile MaltaRainbootPas encore d'évaluation
- Vocabulary FceDocument17 pagesVocabulary Fceivaan94Pas encore d'évaluation
- Designing and Drawing PropellerDocument4 pagesDesigning and Drawing Propellercumpio425428100% (1)
- Vygotsky EssayDocument3 pagesVygotsky Essayapi-526165635Pas encore d'évaluation
- Nescom Test For AM (Electrical) ImpDocument5 pagesNescom Test For AM (Electrical) Impشاہد یونسPas encore d'évaluation
- Enrico Fermi Pioneer of The at Ted GottfriedDocument156 pagesEnrico Fermi Pioneer of The at Ted GottfriedRobert Pérez MartinezPas encore d'évaluation
- Green Dot ExtractDocument25 pagesGreen Dot ExtractAllen & UnwinPas encore d'évaluation
- Bubble Test Direct Pressure InserviceDocument3 pagesBubble Test Direct Pressure InserviceEdAlmPas encore d'évaluation
- Extract The .Msi FilesDocument2 pagesExtract The .Msi FilesvladimirPas encore d'évaluation
- DR S GurusamyDocument15 pagesDR S Gurusamybhanu.chanduPas encore d'évaluation
- PNP Ki in July-2017 AdminDocument21 pagesPNP Ki in July-2017 AdminSina NeouPas encore d'évaluation
- Women Are Better Managers Than MenDocument5 pagesWomen Are Better Managers Than MenCorazon ValdezPas encore d'évaluation
- Positive Psychology in The WorkplaceDocument12 pagesPositive Psychology in The Workplacemlenita264Pas encore d'évaluation
- KCG-2001I Service ManualDocument5 pagesKCG-2001I Service ManualPatrick BouffardPas encore d'évaluation
- An Eastern Orthodox Understanding of The Dangers of Modernity and TechnologyDocument10 pagesAn Eastern Orthodox Understanding of The Dangers of Modernity and TechnologyTimothy ZelinskiPas encore d'évaluation
- Sainik School Balachadi: Name-Class - Roll No - Subject - House - Assigned byDocument10 pagesSainik School Balachadi: Name-Class - Roll No - Subject - House - Assigned byPagalPas encore d'évaluation