Académique Documents
Professionnel Documents
Culture Documents
Ca Treatment Phyllodes Web Algorithm PDF
Transféré par
Muhammad SubhiTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Ca Treatment Phyllodes Web Algorithm PDF
Transféré par
Muhammad SubhiDroits d'auteur :
Formats disponibles
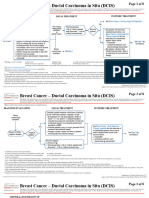
Phyllodes Tumor Page 1 of 4
This practice algorithm has been specifically developed for MD Anderson using a multidisciplinary approach and taking into co nsideration circumstances particular to MD Anderson,
including the following: MD Anderson’s specific patient population; MD Anderson’s services and structure; and MD Anderson’s clinical information. Moreover, this algorithm is not
intended to replace the independent medical or professional judgment of physicians or other health care providers . This algorithm should not be used to treat pregnant women.
Note: Consider Clinical Trials as treatment options for eligible patients.
PATIENT INITIAL TREATMENT
PRESENTATION EVALUATION
Fibroadenoma Close clinical follow-up
Review final pathology
Clinical suspicion of
Phyllodes tumor ● If benign or borderline, observe
phyllodes tumor: ● History and
includes benign3, Wide excision3 without ● If malignant, consider radiation therapy
4,5,6
● Palpable mass physical exam
borderline and axillary staging ● If greater than 5 cm with stromal
● Rapid growth ● Ultrasound
Core needle malignant4,5 overgrowth, refer to Adult Soft – Tissue
● Imaging with ultrasound ● Mammogram for
biopsy1,2 Sarcoma for Clinical Stage III Algorithm
suggestive of fibroadenoma women greater
except for size (greater than than or equal to
2 cm) and/or history of 30 years of age
rapid growth Invasive or in situ
See Breast cancer - Invasive or Noninvasive Algorithm
breast cancer
Phyllodes, including benign,
Fibroepithelial borderline and malignant
Excisional Review final
lesion or
biopsy7 pathology
indeterminate
pathology2 Fibroadenoma Observation
1
Fine needle aspiration will not, and core biopsy may not, distinguish fibroadenoma from phyllodes tumor in most cases (tumor heterogenity may not allow for a definitive diagnosis as some phyllodes arise in a background of fibroadenoma )
2
It is recommended that the review of the pathology material be performed by a pathologist who is experienced in phyllodes tumor
3
If initially excised with negative margin, wide local excision not required
4
Referral to a multidisciplinary sarcoma center for treatment recommendations is appropriate for malignant phyllodes tumor or one with stromal overgrowth
5
For patients with malignant phyllodes tumor on pathology review, refer to Adult Soft - Tissue Sarcoma for Clinical Stage III algorithm
6
There is no prospective randomized data supporting the use of radiation treatment (XRT) with phyllodes tumor. If the phyllodes tumor of the breast is benign or borderline histology, radiation therapy not routinely recommended after excision.
If the tumor has malignant features (i.e., stromal overgrowth, cellular atypia, high number of mitoses) radiotherapy can be considered as follows:
● If mastectomy is performed and margins negative, do not recommend XRT
● If mastectomy was performed and margins were concerning/close, tumor involved the fascia or chest wall, or tumor was very large (greater than 5 centimeters), consider XRT to chest wall
● If partial mastectomy only is performed, consider adjuvant XRT to breast, especially if margins are less than 1 cm
7
Excisional biopsy includes complete mass removal, but without the intent of obtaining widely negative surgical margins
Department of Clinical Effectiveness V7
Approved by Executive Committee of the Medical Staff 10/31/2017
Phyllodes Tumor Page 2 of 4
This practice algorithm has been specifically developed for MD Anderson using a multidisciplinary approach and taking into co nsideration circumstances particular to MD Anderson,
including the following: MD Anderson’s specific patient population; MD Anderson’s services and structure; and MD Anderson’s clinical information. Moreover, this algorithm is not
intended to replace the independent medical or professional judgment of physicians or other health care providers . This algorithm should not be used to treat pregnant women.
Note: Consider Clinical Trials as treatment options for eligible patients.
PATIENT INITIAL TREATMENT
PRESENTATION EVALUATION
No metastatic Consider post-
Re-excision with histologically negative
disease operative radiation
margins without axillary staging
(category 2B)2
● History and physical exam
● Ultrasound
Locally recurrent breast
● Mammogram
mass following excision 1
● Core needle biopsy
of phyllodes tumor
● Consider chest imaging if
malignant phyllodes tumor
Metastatic disease management following principles of soft tissue
Metastatic disease
sarcoma (See Adult Soft - Tissue for Clinical Stage III Algorithm)
1
Pathology should be reviewed to assess for fibroadenoma versus phyllodes (phyllodes benign, borderline and malignant).
2
There is no prospective randomized data supporting the use of radiation treatment with phyllodes tumor . However, in the setting where additional recurrence would create significant morbidity (e.g., chest wall
recurrence following salvage mastectomy) radiation therapy may be considered, following the same principles that are applied to the treatment of soft tissue sarcoma. Radiotherapy is considered for malignant
phyllodes tumor after wide local excision lesions over 2 cm or after mastectomy for lesions over 5 cm based on the retrospective review of 478 patients analyzed by Pezner, et al., 2008.
Department of Clinical Effectiveness V7
Approved by Executive Committee of the Medical Staff 10/31/2017
Phyllodes Tumor Page 3 of 4
This practice algorithm has been specifically developed for MD Anderson using a multidisciplinary approach and taking into co nsideration circumstances particular to MD Anderson,
including the following: MD Anderson’s specific patient population; MD Anderson’s services and structure; and MD Anderson’s clinical information. Moreover, this algorithm is not
intended to replace the independent medical or professional judgment of physicians or other health care providers . This algorithm should not be used to treat pregnant women.
SUGGESTED READINGS
National Comprehensive Cancer Network. (2017). Breast Cancer V1.2017. Retrieved March 27, 2017 from https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf
Pezner, R. D., Schultheiss, T. E., & Paz, I. B. (2008). Malignant phyllodes tumor of the breast: Local control rates with surgery alone. International Journal of Radiation Oncology,
Biology, Physics, 71(3), 710-713. doi:10.1016/j.ijrobp.2007.10.051
Department of Clinical Effectiveness V7
Approved by Executive Committee of the Medical Staff 10/31/2017
Phyllodes Tumor Page 4 of 4
This practice algorithm has been specifically developed for MD Anderson using a multidisciplinary approach and taking into co nsideration circumstances particular to MD Anderson,
including the following: MD Anderson’s specific patient population; MD Anderson’s services and structure; and MD Anderson’s clinical information. Moreover, this algorithm is not
intended to replace the independent medical or professional judgment of physicians or other health care providers . This algorithm should not be used to treat pregnant women.
DEVELOPMENT CREDITS
This practice consensus algorithm is based on majority expert opinion of the Breast Faculty at the University of Texas MD Anderson Cancer Center.
It was developed using a multidisciplinary approach that included input from the following:
Constance Albarracin, MD Ashleigh Guadagnolo, MD, MPHŦ George Perkins, MD
Dejka Araujo, MD Karen Hoffman, MD Vinod Ravi, MD
Elsa Arribas, MD Gabriel Hortobagyi, MD Erika Resetkova, MD
Banu Arun, MD Kelly Hunt, MDŦ Geoffrey Robb, MD
Gildy Babiera, MD Rosa Hwang, MD Merrick Ross, MD
Robert Bast Jr., MD Nuhad Ibrahim, MD Aysegul Sahin, MD
Isabelle Bedrosian, MDŦ Kimberly Koenig, MD Lumarie Santiago, MD
Robert Benjamin, MD Savitri Krishnamurthy, MD Simona Shaitelman, MD
Shon Black, MD Henry Kuerer MD, PhDŦ Ben Smith, MD
Daniel Booser, MD Deanna Lane, MD Tanya Stephens, MD
Abenaa Brewster, MD Huong Le-Petross, MD Eric Strom, MD
Thomas Buchholz, MDŦ Jennifer Litton, MD Fraser Symmans, MD
Aman Buzdar, MD Anthony Lucci, MD Welela Tereffe, MDŦ
Abigail Caudle, MD Joseph Ludwig, MD Debu Tripathy, MDŦ
Janice Cormier, MD Funda Meric-Bernstam, MD Gloria Trowbridge, BSN, RN♦
Sarah DeSnyder, MD Lavinia Middleton, MD Naota Ueno, MD
Mark Dryden, MD Tamara Miner Haygood, MD Vincente Valero, MD
Barry Feig, MD Elizabeth Mittendorf, MD Ronald Walters, MD
Bruno Fornage, MD Stacy Moulder, MD Gary Whitman, MD
Michael Gilcrease, MD James Murray III, MD Anita M. Williams, BS♦
Sharon Giordano, MD Shreyaskumar Patel, MD Wendy Woodward, MD
Wei Yang, MD
Ŧ
Core Development Team
♦Clinical Effectiveness Development Team
Department of Clinical Effectiveness V7
Approved by Executive Committee of the Medical Staff 10/31/2017
Vous aimerez peut-être aussi
- Breast Disease: Diagnosis and Pathology, Volume 1D'EverandBreast Disease: Diagnosis and Pathology, Volume 1Adnan AydinerPas encore d'évaluation
- Ca Treatment Phyllodes Web Algorithm PDFDocument4 pagesCa Treatment Phyllodes Web Algorithm PDFtaufikolingPas encore d'évaluation
- Ca Treatment Breast Noninvasive Web AlgorithmDocument8 pagesCa Treatment Breast Noninvasive Web AlgorithmAgustin SierraPas encore d'évaluation
- Ca - Treatment-Breast-Inflammatory-Web-AlgorithmDocument19 pagesCa - Treatment-Breast-Inflammatory-Web-AlgorithmAgustin SierraPas encore d'évaluation
- Ca Treatment Paget S Web AlgorithmDocument4 pagesCa Treatment Paget S Web AlgorithmAgustin SierraPas encore d'évaluation
- Cancer de Mama y EmbarazoDocument5 pagesCancer de Mama y EmbarazoNicolás BertachiniPas encore d'évaluation
- Phyllodes TumorsDocument4 pagesPhyllodes TumorsNexi anessaPas encore d'évaluation
- J Janardhan, P Venkateshwar, K Sreedhar Rao, K Sreedhar RaoDocument5 pagesJ Janardhan, P Venkateshwar, K Sreedhar Rao, K Sreedhar RaoNatalindah Jokiem Woecandra T. D.Pas encore d'évaluation
- Ca Treatment Prostate Web AlgorithmDocument12 pagesCa Treatment Prostate Web AlgorithmCalvinPas encore d'évaluation
- Clinical Guideline Suspected Adrenal IncidentalomaDocument3 pagesClinical Guideline Suspected Adrenal IncidentalomaMica SaeronPas encore d'évaluation
- A Randomised Active - Controlled Trial For Vulvovaginal Atrophy in Patients With Breast Cancer On Endocrine TherapyDocument5 pagesA Randomised Active - Controlled Trial For Vulvovaginal Atrophy in Patients With Breast Cancer On Endocrine Therapyana.tocha.avtPas encore d'évaluation
- Giant Juvenil FAMDocument5 pagesGiant Juvenil FAMNatalindah Jokiem Woecandra T. D.Pas encore d'évaluation
- Ca Treatment Breast Invasive Web AlgorithmDocument27 pagesCa Treatment Breast Invasive Web AlgorithmAgustin SierraPas encore d'évaluation
- Myoma UteriDocument8 pagesMyoma UteriFaraida Arvilla100% (1)
- Cystosarcoma Phyllodes Rapidly Growing Tumours WitDocument4 pagesCystosarcoma Phyllodes Rapidly Growing Tumours WitWinarti RimadhaniPas encore d'évaluation
- Ca Treatment Breast Noninvasive Web AlgorithmDocument6 pagesCa Treatment Breast Noninvasive Web Algorithmmarcelo chavez diazPas encore d'évaluation
- CA Treatment Phyllodes Web AlgorithmDocument4 pagesCA Treatment Phyllodes Web AlgorithmNurul Ramadhani IslamiPas encore d'évaluation
- Breast "Case-Based Optional"Document18 pagesBreast "Case-Based Optional"eiuj497Pas encore d'évaluation
- CA Treatment Leptomeningeal Web AlgorithmDocument5 pagesCA Treatment Leptomeningeal Web Algorithmsugoiman100% (1)
- Tumor PhyloidesDocument5 pagesTumor Phyloidesflor gonzalezPas encore d'évaluation
- FNAC Male BreastDocument5 pagesFNAC Male BreastDima PathPas encore d'évaluation
- Marfan'sDocument39 pagesMarfan'sRavin DebiePas encore d'évaluation
- Signs & Symptoms: NeoplasmDocument2 pagesSigns & Symptoms: NeoplasmKath RubioPas encore d'évaluation
- Primary Fibrosarcoma of Breast: A Rare Case Presentation: Cash ReportDocument4 pagesPrimary Fibrosarcoma of Breast: A Rare Case Presentation: Cash ReportBastiaanPas encore d'évaluation
- Breast Cancer Histologic SubtypesDocument24 pagesBreast Cancer Histologic Subtypesgaby andreaPas encore d'évaluation
- Fibroadenoma PDFDocument2 pagesFibroadenoma PDFAthika Dwi Sofiana100% (1)
- Regression of Fibroadenoma in Response To Centchroman Therapy-A R Andomized Control TrialDocument4 pagesRegression of Fibroadenoma in Response To Centchroman Therapy-A R Andomized Control TrialRahmawati JuliaPas encore d'évaluation
- Screening Endometrial Web AlgorithmDocument3 pagesScreening Endometrial Web AlgorithmKadir GümüşPas encore d'évaluation
- 3 - NCM112Document6 pages3 - NCM112Edthel IniegoPas encore d'évaluation
- PCOS GP Tool 20180815 Henry, Dr.Document4 pagesPCOS GP Tool 20180815 Henry, Dr.Mitaa CikawaiPas encore d'évaluation
- Practice Parameter 2003 Prophylactic MastectomyDocument3 pagesPractice Parameter 2003 Prophylactic MastectomyGabriela AlexaPas encore d'évaluation
- Fam 1Document3 pagesFam 1novaPas encore d'évaluation
- Cap 17Document37 pagesCap 17Saul RivasPas encore d'évaluation
- ScabiesDocument1 pageScabiesAnsor PratamaPas encore d'évaluation
- JurnalDocument4 pagesJurnalDini Mardiana UsmanPas encore d'évaluation
- Granulomatous Lobular Mastitis: Original ArticlesDocument5 pagesGranulomatous Lobular Mastitis: Original ArticlesFirdillaQonitaFirodiyaRobbyPas encore d'évaluation
- Cancer of The Endometrium PDFDocument6 pagesCancer of The Endometrium PDFYanita BetraPas encore d'évaluation
- 1097-0142 (19860115) 57 2 320 Aid-Cncr2820570221 3.0.co 2-C PDFDocument4 pages1097-0142 (19860115) 57 2 320 Aid-Cncr2820570221 3.0.co 2-C PDFم.محمدولدعليPas encore d'évaluation
- MED2 5.01A Treatment Modalities in Cancer (Part 1) - Dr. F. AdefuinDocument3 pagesMED2 5.01A Treatment Modalities in Cancer (Part 1) - Dr. F. AdefuinAra DiocosPas encore d'évaluation
- Block 10 A: Tindoc, Tugano, Urquiza, Uy, Velasco, Ventigan, Ventura, VerdolagaDocument32 pagesBlock 10 A: Tindoc, Tugano, Urquiza, Uy, Velasco, Ventigan, Ventura, VerdolagaNatalliaPas encore d'évaluation
- Removing Uterine FibroidsDocument4 pagesRemoving Uterine FibroidsAde Churie TanjayaPas encore d'évaluation
- Benign Breast DiseaseDocument48 pagesBenign Breast DiseaseNabighah ZukriPas encore d'évaluation
- Common Benign Chronic Vulvar DisordersDocument9 pagesCommon Benign Chronic Vulvar DisordersPriyaproject0003 goodgirlPas encore d'évaluation
- A Case of Left Mammary Fibroadenoma Successfully Cured by Homoeopathic Therapy1Document7 pagesA Case of Left Mammary Fibroadenoma Successfully Cured by Homoeopathic Therapy1Chandraja RathishPas encore d'évaluation
- Phyllodes Tumours: ReviewsDocument8 pagesPhyllodes Tumours: ReviewsMuhammad SubhiPas encore d'évaluation
- PDFsam ObGynDocument4 pagesPDFsam ObGynAlessandro ZadraPas encore d'évaluation
- Karsinoma EndometriumDocument7 pagesKarsinoma EndometriumIntan PermataPas encore d'évaluation
- Current Perspective inDocument9 pagesCurrent Perspective inMonik AlamandaPas encore d'évaluation
- Male Breast Cancer, Sarcomas of Breast, Pregnancy and Breast CancerDocument20 pagesMale Breast Cancer, Sarcomas of Breast, Pregnancy and Breast Cancerapi-3701915Pas encore d'évaluation
- Care For Women: With Ovarian, Cerviacl, Vulvar and Endometrial CancerDocument26 pagesCare For Women: With Ovarian, Cerviacl, Vulvar and Endometrial CancerAhmad JradeenPas encore d'évaluation
- Tiwari 2017Document3 pagesTiwari 2017Dewa OkaPas encore d'évaluation
- Ijcmr 1184 Dec 28Document3 pagesIjcmr 1184 Dec 28BayuHernawanRahmatMuhariaPas encore d'évaluation
- Clinicopathological Characteristics of Meningiomas Experience From A Tertiary Care Hospital in The Kashmir ValleyDocument6 pagesClinicopathological Characteristics of Meningiomas Experience From A Tertiary Care Hospital in The Kashmir ValleyHastrina MailaniPas encore d'évaluation
- Uterine Myoma - Surgical or Medical1.original.15615304794199696230846510162Document42 pagesUterine Myoma - Surgical or Medical1.original.15615304794199696230846510162Mi MaymdPas encore d'évaluation
- Cervical CancerDocument38 pagesCervical Cancerreema.saleh123Pas encore d'évaluation
- Study Nipple DischargeDocument10 pagesStudy Nipple DischargeIvana_998Pas encore d'évaluation
- A Review of Mastalgia in Patients With Fibrocystic Breast Changes Compairingeffectiveness of CentchromanDocument6 pagesA Review of Mastalgia in Patients With Fibrocystic Breast Changes Compairingeffectiveness of CentchromanIJAR JOURNALPas encore d'évaluation
- Contessa - Plante2019Document7 pagesContessa - Plante2019moises vigilPas encore d'évaluation
- If HP Cancer Guide Gu001 TesticularDocument23 pagesIf HP Cancer Guide Gu001 TesticularwidyaputraPas encore d'évaluation
- Phyllodes Tumor Review ArticleDocument11 pagesPhyllodes Tumor Review ArticleMuhammad SubhiPas encore d'évaluation
- Imaging of Spinal Metastatic DiseaseDocument13 pagesImaging of Spinal Metastatic DiseaseMuhammad SubhiPas encore d'évaluation
- Phyllodes Tumours: ReviewsDocument8 pagesPhyllodes Tumours: ReviewsMuhammad SubhiPas encore d'évaluation
- CA Treatment Phyllodes Web AlgorithmDocument4 pagesCA Treatment Phyllodes Web AlgorithmMuhammad SubhiPas encore d'évaluation
- Phyllodes Tumor Review ArticleDocument11 pagesPhyllodes Tumor Review ArticleMuhammad SubhiPas encore d'évaluation
- Summary of Guidelines For The Surgical Management of Traumatic Brain InjuryDocument3 pagesSummary of Guidelines For The Surgical Management of Traumatic Brain InjuryRidzky FirmansyahPas encore d'évaluation
- Management. Department of Surgery, Swiss HPB and Transplant Center, UniversityDocument1 pageManagement. Department of Surgery, Swiss HPB and Transplant Center, UniversityMuhammad SubhiPas encore d'évaluation
- 2011 CAP in ChildrenDocument52 pages2011 CAP in Childrenbebekdd22Pas encore d'évaluation
- Phyllodes Tumours: ReviewsDocument8 pagesPhyllodes Tumours: ReviewsMuhammad SubhiPas encore d'évaluation
- Glikemik IndeksDocument11 pagesGlikemik IndeksMuhammad SubhiPas encore d'évaluation
- Effectiveness of Herbal and Non-Herbal Toothpastes in Reducing Dental Plaque AccumulationDocument5 pagesEffectiveness of Herbal and Non-Herbal Toothpastes in Reducing Dental Plaque AccumulationMuhammad SubhiPas encore d'évaluation
- Glikemik IndeksDocument11 pagesGlikemik IndeksMuhammad SubhiPas encore d'évaluation
- 11 - 212tumor PhyllodesDocument3 pages11 - 212tumor PhyllodesRantangnasiPas encore d'évaluation
- F 2661 JCNSD Risperidone Long Acting Injection Safety and Efficacy in Elderly Pati - PDF 3577Document11 pagesF 2661 JCNSD Risperidone Long Acting Injection Safety and Efficacy in Elderly Pati - PDF 3577Richesio Sapata TomokumoroPas encore d'évaluation
- Homo Sapiens ChymotrypsinDocument9 pagesHomo Sapiens ChymotrypsinMuhammad SubhiPas encore d'évaluation
- TranslateDocument1 pageTranslateMuhammad SubhiPas encore d'évaluation
- TranslateDocument1 pageTranslateMuhammad SubhiPas encore d'évaluation
- Homo Sapiens ChymotrypsinDocument9 pagesHomo Sapiens ChymotrypsinMuhammad SubhiPas encore d'évaluation
- Glikemik IndeksDocument11 pagesGlikemik IndeksMuhammad SubhiPas encore d'évaluation
- F 2661 JCNSD Risperidone Long Acting Injection Safety and Efficacy in Elderly Pati - PDF 3577Document11 pagesF 2661 JCNSD Risperidone Long Acting Injection Safety and Efficacy in Elderly Pati - PDF 3577Richesio Sapata TomokumoroPas encore d'évaluation
- OUTPUT (Yang Dibuat Tabel)Document12 pagesOUTPUT (Yang Dibuat Tabel)Muhammad SubhiPas encore d'évaluation
- Glikemik IndeksDocument11 pagesGlikemik IndeksMuhammad SubhiPas encore d'évaluation
- Homo Sapiens KallikreinDocument8 pagesHomo Sapiens KallikreinMuhammad SubhiPas encore d'évaluation
- Chol Angio CarcinomaDocument12 pagesChol Angio CarcinomaMuhammad SubhiPas encore d'évaluation
- DASS21Document1 pageDASS21Ron LorenzoPas encore d'évaluation
- #Soal Jantung KEDUA CaronmntisDocument31 pages#Soal Jantung KEDUA CaronmntisMuhammad SubhiPas encore d'évaluation
- Anti-Streptolysin o (Asl)Document8 pagesAnti-Streptolysin o (Asl)Muhammad SubhiPas encore d'évaluation
- Bahan Kuliah Biologi 6Document83 pagesBahan Kuliah Biologi 6Muhammad SubhiPas encore d'évaluation
- Bahan Kuliah Biologi 6Document83 pagesBahan Kuliah Biologi 6Muhammad SubhiPas encore d'évaluation
- Hospital PlanningDocument8 pagesHospital PlanningadithiPas encore d'évaluation
- Anemia PPT 3 Nov 2014Document60 pagesAnemia PPT 3 Nov 2014Susi DesmaryaniPas encore d'évaluation
- Hovenia Dulcis - Scientific Review On Usage, Dosage, Side Effects - ExamineDocument5 pagesHovenia Dulcis - Scientific Review On Usage, Dosage, Side Effects - Examineozman blooriPas encore d'évaluation
- The FRCPath Exam - Paul BennettDocument130 pagesThe FRCPath Exam - Paul BennettVictor ChanPas encore d'évaluation
- Blood Gas InterpretationDocument36 pagesBlood Gas InterpretationMary Charmaine DivinagraciaPas encore d'évaluation
- Meuhedet Adif RegulationsDocument72 pagesMeuhedet Adif RegulationsEnglishAccessibilityPas encore d'évaluation
- Diabetes Mellitus Complicated PregnancyDocument21 pagesDiabetes Mellitus Complicated PregnancyanojanPas encore d'évaluation
- ASEAN Guideline On Stability of Drug ProductDocument8 pagesASEAN Guideline On Stability of Drug ProductSanjiv MenonPas encore d'évaluation
- NPI Reflects Spring 2013Document12 pagesNPI Reflects Spring 2013npinashvillePas encore d'évaluation
- Autocoid PharmacologyDocument29 pagesAutocoid PharmacologyLyadelou Fortu100% (1)
- Presented By: Bhagyashree KaleDocument58 pagesPresented By: Bhagyashree KaleSupriya JajnurkarPas encore d'évaluation
- Anaemia: by Swaathi R Final Year MbbsDocument33 pagesAnaemia: by Swaathi R Final Year MbbsGopi NathPas encore d'évaluation
- Tutorial Assignment Week 14 With AnswerDocument4 pagesTutorial Assignment Week 14 With AnswerCik Wynn100% (1)
- CAM101 Complete Course Notes Reduced SizeDocument174 pagesCAM101 Complete Course Notes Reduced SizehaydenfarquharPas encore d'évaluation
- Allergy Test PapersDocument5 pagesAllergy Test PapersDaniel MoncadaPas encore d'évaluation
- Colour Facts SheetDocument4 pagesColour Facts SheetChiranjaya HulangamuwaPas encore d'évaluation
- The 2015 OSDUHS Mental Health and Well-Being Report Executive SummaryDocument11 pagesThe 2015 OSDUHS Mental Health and Well-Being Report Executive SummaryCityNewsTorontoPas encore d'évaluation
- Facial Fat Grafting: Why, Where, How, and How MuchDocument20 pagesFacial Fat Grafting: Why, Where, How, and How MuchMade SetiadjiPas encore d'évaluation
- Post-Partum HemorrhageDocument15 pagesPost-Partum Hemorrhageapi-257029163Pas encore d'évaluation
- Argos SBR: A Compact SBR System Offering Process Flexibility and Major Capital SavingsDocument2 pagesArgos SBR: A Compact SBR System Offering Process Flexibility and Major Capital SavingsViorel HarceagPas encore d'évaluation
- Clinical QigongDocument5 pagesClinical QigongFlorin Iacob100% (1)
- Punjab Drugs Rules 2007Document33 pagesPunjab Drugs Rules 2007RphNaeemMalik75% (12)
- Modern Trends in Hypnosis Ed by David Waxman & Prem C Misra & Michael Gibson & M Anthony Basker (1985)Document404 pagesModern Trends in Hypnosis Ed by David Waxman & Prem C Misra & Michael Gibson & M Anthony Basker (1985)marcinlesniewicz100% (4)
- MZ 14Document68 pagesMZ 14Robert AndrejašPas encore d'évaluation
- Biowaiver Approaches For Solid Oral Dosage Forms in New Drug Applications - V8 - FinalDocument47 pagesBiowaiver Approaches For Solid Oral Dosage Forms in New Drug Applications - V8 - FinalSrinivas Reddy MaramPas encore d'évaluation
- Experiential Techniques and Therapeutic Relationship in The Treatment of Narcissistic Personality Disorder: The Case of LauraDocument14 pagesExperiential Techniques and Therapeutic Relationship in The Treatment of Narcissistic Personality Disorder: The Case of Lauraconsulta.nicolaslabbePas encore d'évaluation
- MHFW OrderDocument4 pagesMHFW OrderNavjivan IndiaPas encore d'évaluation
- ScabiesDocument5 pagesScabiespakemainmainPas encore d'évaluation
- Vmet DocumentDocument5 pagesVmet Documentapi-310904234Pas encore d'évaluation
- Nursing As A ProfessionDocument35 pagesNursing As A ProfessionAparna Aby75% (8)