Académique Documents
Professionnel Documents
Culture Documents
1 s2.0 S0022391316305108 Main
Transféré par
Novita RTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
1 s2.0 S0022391316305108 Main
Transféré par
Novita RDroits d'auteur :
Formats disponibles
RESEARCH AND EDUCATION
Three-dimensional finite element analysis of implant-assisted
removable partial dentures
Ju-Won Eom, DDS, MS,a Young-Jun Lim, DDS, MS, PhD,b Myung-Joo Kim, DDS, MS, PhD,c and
Ho-Beom Kwon, DDS, MS, PhDd
Various treatment options have ABSTRACT
been developed using dental Statement of problem. Whether the implant abutment in implant-assisted removable partial
implant systems, including dentures (IARPDs) functions as a natural removable partial denture (RPD) tooth abutment is
implant-retained overden- unknown.
tures, implant-supported
Purpose. The purpose of this 3-dimensional finite element study was to analyze the biomechanical
overdentures, and implant- behavior of implant crown, bone, RPD, and IARPD.
supported fixed prostheses.1,2
Recently implant-supported Material and methods. Finite element models of the partial maxilla, teeth, and prostheses were
generated on the basis of a patient’s computed tomographic data. The teeth, surveyed crowns, and
fixed restorations have been
RPDs were created in the model. With the generated components, four 3-dimensional finite
used in combination with element models of the partial maxilla were constructed: tooth-supported RPD (TB), implant-
removable partial dentures supported RPD (IB), tooth-tissue-supported RPD (TT), and implant-tissue-supported RPD (IT)
(RPDs) as an alternative treat- models. Oblique loading of 300 N was applied on the crowns and denture teeth. The von Mises
ment for patients with partial or stress and displacement of the denture abutment tooth and implant system were identified.
3
complete edentulism. The Results. The highest von Mises stress values of both IARPDs occurred on the implants, while those
benefits of implant-assisted of both natural tooth RPDs occurred on the frameworks of the RPDs. The highest von Mises stress of
RPDs have been described by model IT was about twice that of model IB, while the value of model TT was similar to that of model
several authors.3-7 An implant- TB. The maximum displacement was greater in models TB and TT than in models IB and IT. Among
assisted removable partial den- the 4 models, the highest maximum displacement value was observed in the model TT and the
lowest value was in the model IB.
ture (IARPD) is different from
an implant-retained RPD in Conclusions. Finite element analysis revealed that the stress distribution pattern of the IARPDs was
that the implant provides different from that of the natural tooth RPDs and the stress distribution of implant-supported RPD
an RPD abutment in an was different from that of implant-tissue-supported RPD. When implants are used for RPD
abutments, more consideration concerning the RPD design and the number or location of the
IARPD.7-10 The implant in an
implant is necessary. (J Prosthet Dent 2017;117:735-742)
IARPD provides retention and
support, which improves
masticatory efficiency and patient comfort and satisfac- IARPDs is also cost-effective as the number of implants is
tion.11 In addition, the implants protect the remaining reduced.15 Furthermore, by transforming Kennedy class I
natural teeth and preserve bone.12,13 Clasp arms can be RPDs to Kennedy class III through the placement of distal
replaced by retentive attachments to the implant abutment, implants, IARPDs can provide better support and increased
improving patients’ appearance.13,14 Treatment with masticatory force.16,17
Supported by grant 2015R1D1A1A01060940 from the National Research Foundation of Korea.
a
Graduate student, Dental Research Institute and Department of Prosthodontics, School of Dentistry, Seoul National University, Seoul, Republic of Korea.
b
Professor, Dental Research Institute and Department of Prosthodontics, School of Dentistry, Seoul National University, Seoul, Republic of Korea.
c
Associate Professor, Dental Research Institute and Department of Prosthodontics, School of Dentistry, Seoul National University, Seoul, Republic of Korea.
d
Associate Professor, Dental Research Institute and Department of Prosthodontics, School of Dentistry, Seoul National University, Seoul, Republic of Korea.
THE JOURNAL OF PROSTHETIC DENTISTRY 735
736 Volume 117 Issue 6
structures.22-27 It provides useful information that is
Clinical Implications difficult to measure intraorally, including the results of
When implants were used as abutments for the different component sizes and material changes, the
calculation of preload, the effect of implant-abutment
removable partial denture (RPD) design, the highest
connections, and the influence of parafunctional
stress was concentrated on the implants in
habits.22,24,25,28 Although several studies have described
implant-assisted removable partial dentures. To
the use of RPDs in conjunction with implant prostheses,
avoid possible implant complications such as
few studies have used 3D finite element analysis to
prosthesis fracture, marginal bone loss, or implant
evaluate the use of implant prostheses as abutments for
failure related to this stress concentration, it might
RPDs.19,29,30 Therefore, the purpose of this 3D finite
be necessary to consider the placement of multiple
implants, splinted prostheses, or the extension of element analysis study was to analyze the biomechanical
behavior of implant, bone, and RPD in different types of
the RPD base to cover the maximum supporting
IARPDs.
area.
MATERIAL AND METHODS
Implant placement on the maxillary or mandibular Three-dimensional finite element models of an IARPD
posterior regions is sometimes restricted by anatomic or and a tooth-supported RPD were constructed based on a
financial limitations. Some patients with complete patient’s computed tomography (CT) image. Four 3D
edentulism are unwilling to have extensive surgical pro- finite element models of an implant-supported RPD (IB), a
cedures. In these situations, anterior implant-supported tooth-supported RPD (TB), an implant-tissue-supported
fixed restorations in conjunction with RPDs can be an RPD (IT), and a tooth-tissue-supported RPD (TT) were
effective treatment option.18 Chronopoulos et al3 constructed to simulate RPDs combined with implant
described a patient with RPDs in which Kennedy class I prostheses or natural teeth as abutments on the partially
RPDs were used on the maxilla and mandible in combi- edentulous maxilla. An oblique load of 300 N was applied
nation with anterior fixed implant prostheses with semi- on the crowns and denture teeth. The maximum von
precision attachments. The authors concluded that the use Mises stresses and the displacements of the denture
of a dental implant as an abutment for a mandibular abutment teeth, implants, bone, and RPDs were identi-
extension RPD was an effective clinical solution. fied. This study was approved by the institutional review
Cunha et al19 demonstrated that the placement of a board of Seoul National University Dental Hospital.
dental implant diminished the tendency for intrusion of The geometry of the maxilla was extracted from CT
RPDs. The authors constructed a 2-dimensional (2D) data. The individual was healthy and had normal
finite element model of a partially edentulous mandible craniofacial structures. The left side of the maxilla was
and RPD models combined with an implant and used to build a finite element model. The CT scans were
concluded that locating the implant near the abutment segmented using an image processing software (Amira;
tooth positively influenced the distribution of stresses on FEI) and then exported into a meshing program (Visual-
the analyzed structures. Pellizzer et al20 studied the Mesh; ESI Group), which produced the tetrahedral
association between a distal extension RPD and an volumetric meshes of the partial maxilla.
osseointegrated implant using 2D finite element analysis. Four 3D finite element models representing half of
The authors reported that implants associated with a the maxilla, abutments, and half of the RPD were con-
healing abutment, Sterngold ERA overdenture attach- structed. Two models had natural teeth, and the other 2
ment (Sterngold), or a ball attachment exhibited favorable models had implant-supported surveyed crowns. The
stresses with an RPD. In contrast, distal extension RPDs model TB consisted of 2 surveyed crowns supported by
associated with a single implant-supported prosthesis in natural teeth in the area of the maxillary first premolar
the posterior area were not favorable. Shahmiri et al21 and the second molar combined with the RPD. A
analyzed a Kennedy class I implant-assisted removable partially edentulous maxilla was created by removing the
prosthesis using finite element analysis. They constructed second premolar and the first molar in the original model
a 3-dimensional (3D) human mandible model with an and by replacing the first premolar and second molar
RPD and an implant and analyzed the maximum defor- with the scan data of artificial teeth in the replica model
mation and stress distribution of a framework and acrylic (Nissin D50-555; Nissin). The final model TB was
resin in the RPD, cortical or cancellous bone, and implants. composed of palatal mucous membrane, cortical bone
The authors reported the deformation that might lead to and cancellous bone, periodontal ligaments, abutments,
acrylic resin fracture in the prosthesis. surveyed crown, and RPD. The surveyed crowns had rest
Finite element analysis has frequently been used in seats and were modeled on the properties of a gold alloy.
dentistry to analyze the biomechanical behavior of The RPD had 2 Akers clasps.
THE JOURNAL OF PROSTHETIC DENTISTRY Eom et al
June 2017 737
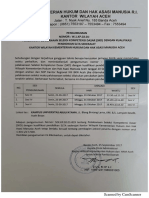
Figure 1. Structure of finite element models. A, Implant-supported RPD (IB). B, Tooth-supported RPD (TB). C, Implant-tissue-supported RPD (IT).
D, Tooth-tissue-supported RPD (TT). RPD, removable partial denture.
The model TT was created by removing the second Table 1. Finite element models
molar of the model TB and by covering edentulous area Removable
Partial No. of No. of
with denture base. Except for the difference in the second Model Abutment Denture Nodes Elements
molar region, all of the components of the model TT were TB Maxillary first premolar and maxillary Tooth 34 120 114 197
identical to those of the model TB. In the model IB, the second molar supported
natural tooth abutments of the model TB were replaced TT Maxillary first premolar Implant tissue 33 024 111 110
supported
with implants. In the model IT, the first premolar of the IB Implant-supported maxillary first Implant 39 902 140 223
model TT was replaced with an implant (Fig. 1). The premolar and implant-supported supported
maxillary second molar
models are summarized in Table 1.
IT Implant-supported maxillary first Implant tissue 36 048 124 373
The geometries of the dental implant system (Osstem premolar supported
US system; Osstem Implant Co) of all models were
provided by the manufacturer. The implant was 10 mm
long and 4 mm in diameter. The abutments and the Meshes of teeth, surveyed crowns, and RPDs were
abutment screws were designed independently and were created with 3D computer-aided design software (Visual-
assembled. The abutment screw was simplified and was Mesh; ESI Group) (Fig. 2). The meshes for the roots of the
in contact with the implant screw hole. The inferior teeth were surrounded by meshes of the periodontal liga-
surface of the abutment was in contact with the top of the ment that were 0.5 mm thick. The RPD model was composed
implant. The preload on the abutment screw was of a metal framework, acrylic resin base, and denture teeth.
generated to simulate screw tightening by using the bolt- The acrylic resin base was considered to be completely
pretension mechanism, which is included in the finite bonded with the denture tooth and metal framework.
element analysis software (ANSYS 14.5; Swanson Anal- All materials were assumed to be linearly elastic,
ysis Systems Inc).31 The preload used was 825 N.25 The homogenous, and isotropic to simplify the calculations.
implant was considered to be bonded with cancellous The elastic modulus and the Poisson ratio for each ma-
and cortical bone to simulate complete osseointegration. terial are summarized in Table 2.
Eom et al THE JOURNAL OF PROSTHETIC DENTISTRY
738 Volume 117 Issue 6
Figure 2. Coronal section of meshes. A, Coronal section of implant-supported removable partial denture (model IB). B, Coronal section of model TB.
C, Coronal section of model IT. D, Coronal section of model TT.
Finite element analysis was performed with software Table 2. Material properties of finite element models31,32
(ANSYS 14.5; Swanson Analysis Systems Inc). The inter- Material Elastic Modulus (GPa) Poisson Ratio
faces between the surveyed crowns and the clasps of the Titanium 110 0.33
RPDs were modeled as frictional contacts with appropriate Acrylic resin 2.2 0.31
friction coefficients (m=0.10).8 Contact analysis was also RPD framework (cobaltechromium) 211 0.3
applied to the interfaces between implant components. Tooth dentin 41 0.3
The coefficient of friction value between the abutment and Gold alloy 91 0.33
Periodontal ligament 3×10−5 0.45
implant was 0.16, and that between the abutment and
Cortical bone 13.7 0.3
abutment screw was 0.2.8 On the basis of previous studies,
Cancellous bone 1.37 0.33
oblique loading of 300 N was applied on the crown and
Mucosa 0.001 0.37
denture tooth to simulate masticatory loading.23,33 Oblique
RPD, removable partial denture.
force was directed at 14.04 degrees to the long axis of the
crown from the buccal to the lingual direction and
distributed to the central fossa and the lingual slopes of the Table 3. Highest von Mises stress values for each finite element model
Model IB TB IT TT
buccal cusps of all maxillary premolars and molars in the
Von Mises stress value (MPa) 120.6 279.7 252.5 307.4
models.34 All nodes of the most medial and most distal
surfaces in the models were constrained in all directions.
The von Mises stress value was used for the analysis, investigated. Maximum displacement of the finite element
appropriate for predicting failure of ductile materials such model was used to verify which compartments moved.
as titanium, cobalt-chromium, and gold alloy.24 Higher
RESULTS
von Mises stress values represent higher risk of fail-
ure.22,34,35 The von Mises stress values of the cortical bones, The highest von Mises stress values were observed on
cancellous bones, RPD frameworks, and implants in the different positions and compartments of each model
different types of IARPDs or natural tooth RPDs were (Table 3). The maximum von Mises stress values of the
THE JOURNAL OF PROSTHETIC DENTISTRY Eom et al
June 2017 739
Figure 3. Von Mises stress (GPa) of removable partial denture framework of finite element models. Red arrows indicate area of maximum von Mises
stress. A, Framework of model IB. B, Framework of model TB. C, Framework of model IT. D, Framework of model TT.
Table 4. Highest von Mises stress values (MPa) in each compartment
With regard to the IARPDs, the maximum von Mises
Model IB TB IT TT
stress values of the cancellous bone and cortical bone,
Cortical bone 33.5 6.5 61.4 6.1
RPD framework, and implant were about twice as high in
Cancellous bone 3.2 0.8 7.5 0.7
model IT as in model IB. For the tooth-supported RPDs,
RPD framework 72.7 279.7 163.1 307.4
Implant 120.6 - 252.4 -
the maximum von Mises stress values of the cortical bone
and cancellous bone were slightly higher in model TB
RPD, removable partial denture.
than those in model TT, while the maximum von Mises
stress value of the RPD framework was higher in model
Table 5. Highest maximum displacement value (mm) for each finite TT (307.4 MPa) than that in model TB (279.7 MPa)
element model (Table 4).
Model IB TB IT TT The maximum displacement values of each model are
Maximum displacement 0.05 1.05 0.36 1.08 summarized in Table 5. The maximum displacement of
models IT and TT occurred in the distal area of each RPD
(Fig. 4). The maximum displacement value that occurred
cancellous and cortical bone were higher in IARPDs (models
in the RPD framework of model TT was the highest
IB and IT) than in the tooth-supported RPDs (models TB and
among the models, while the maximum displace-
TT). However, the maximum von Mises stress values of the
ment value in the RPD framework of model IB was the
RPD framework were higher in the tooth-supported RPDs
lowest.
than in the IARPDs (Fig. 3). Both of the maximum stress
values of models TB (279.7 MPa) and TT (307.4 MPa)
DISCUSSION
occurred on the minor connector of the RPD, while both of
the maximum stress values of models IB (72.7 MPa) and IT The highest von Mises stress value in each IARPD model
(163.1 MPa) occurred on the distal side of the first thread of was located at the implant, and the implants were
the implant in the area of the first premolar in both models. assumed to bear most of the loading in models IB and IT.
Eom et al THE JOURNAL OF PROSTHETIC DENTISTRY
740 Volume 117 Issue 6
Figure 4. Maximum displacement of finite element models. Red arrows indicate area of maximum displacement. A, Maximum displacement of model
IB. B, Maximum displacement of model TB. C, Maximum displacement of model IT. D, Maximum displacement of model TT.
The highest von Mises stress of the implant was about those of model IT were no more than 40 mm. These
twice as great in model IT as in model IB, which might be values are within the normal range, which is about 10 to
explained by the absence of the distal implant in model 50 mm as lateral force is loaded.36 It was assumed that as
IT. This result indicates that the tissue underlying the the RPD in model IT moved downward to the tissue
RPD provided less support under loading than in model under occlusal loading the tissue underneath the RPD
IT and that the use of an implant affected the behavior of base resisted the occlusal loading.37 Thus, the IARPD in
the RPD. However, the models where implants were not model IT should have the maximum support-bearing
used showed different results. The highest von Mises area underneath the base to distribute the total load
stress values in the models TB and TT were observed on from the RPD abutment to the supporting tissue because
the RPD framework, and it was assumed that the RPD the stress around the implant and cortical bone was
framework, which had the highest elastic modulus, found to be higher in model IT than in any other model
experienced the greatest stress because the tooth abut- (Table 4). In addition, the use of multiple splinted im-
ments were mobile because of the presence of the peri- plants instead of a single implant as an RPD abutment
odontal ligament. These results are consistent with those might decrease loading to the implants and thus reduce
of a previous study in which the metal framework of a the risk of complications.38
mandibular RPD showed the highest strain patterns on The reason that the implant models and natural tooth
the major and minor connectors in a mandible model.21 models had different maximum displacement values was
Maximum displacement values varied for each model that the abutment teeth of the natural tooth RPDs were
depending on the presence or absence of the distal more displaceable than those of IARPDs because of the
implant. The maximum displacement value of model IT periodontal ligament, which had a much lower elastic
was 7 times larger than that of model IB. The maximum modulus than any other component in the model. The
displacement values of the implant and the abutment of displacement of model TT was about three times as large
the implant of model IB were no more than 25 mm, while as that of model IT. The displacement of model TT was
THE JOURNAL OF PROSTHETIC DENTISTRY Eom et al
June 2017 741
attributed to tooth-abutment mobility, the elasticity of 6. Mijiritsky E, Ormianer Z, Klinger A, Mardinger O. Use of dental implants to
improve unfavorable removable partial denture design. Compend Contin
the RPD framework, and slipping of the RPD framework Educ Dent 2005;26:744-6.
from the surveyed crown. The displacement of model IT 7. Yeung S, Chee WW, Torbati A. Design concepts of a removable partial dental
prosthesis with implant-supported abutments. J Prosthet Dent 2014;112:
was attributed to the elasticity of the RPD framework and 99-103.
slipping of the RPD framework from the surveyed crown. 8. Shahmiri R, Das R, Aarts JM, Bennani V. Finite element analysis of an
implant-assisted removable partial denture during bilateral loading: occlusal
In this study, a preload of 825 N in the implant system rests position. J Prosthet Dent 2014;112:1126-33.
was created by using the bolt-pretension mechanism in 9. Gharehchahi J, Asadzadeh N, Mirmortazavi A, Shakeri MT. Maximum dis-
lodging forces of mandibular implant-assisted removable partial dentures:
the ANSYS program.31 The 825-N preload was regarded in vitro assessment. J Prosthodont 2013;22:543-9.
as the optimum preload, which was 75% of the yield 10. Wismeijer D, Tawse-Smith A, Payne AG. Multicentre prospective evaluation
of implant-assisted mandibular bilateral distal extension removable partial
strength as recommended for the implant screwejoint dentures: patient satisfaction. Clin Oral Implants Res 2013;24:20-7.
assembly.25 Lang et al25 reported that 75% of the yield 11. Mijiritsky E. Implants in conjunction with removable partial dentures: a
literature review. Implant Dent 2007;16:146-54.
strength of the abutment screw was equal to using a 12. Werbitt MJ, Goldberg PV. The immediate implant: bone preservation and
torque of 32 Ncm applied to the abutment screws in bone regeneration. Int J Periodontics Restorative Dent 1992;12:206-17.
13. Keltjens HM, Kayser AF, Hertel R, Battistuzzi PG. Distal extension removable
implant assemblies with a coefficient friction of 0.12 be- partial dentures supported by implants and residual teeth: considerations and
tween the implant components. case reports. Int J Oral Maxillofac Implants 1993;8:208-13.
14. Budtz-Jorgensen E, Bochet G, Grundman M, Borgis S. Aesthetic consider-
In the present study, several assumptions were made ations for the treatment of partially edentulous patients with removable
to simplify the calculation. It was assumed that the dentures. Pract Proced Aesthet Dent 2000;12:765-72.
15. de Carvalho WR, Barboza EP, Caula AL. Implant-retained removable pros-
cortical and cancellous bones were isotropic, that the thesis with ball attachments in partially edentulous maxilla. Implant Dent
mucosa was linearly elastic, and that all the interfaces 2001;10:280-4.
16. Shahmiri RA, Atieh MA. Mandibular Kennedy Class I implant-tooth-borne
were bonded states except for the 2 frictional contact removable partial denture: a systematic review. J Oral Rehabil 2010;37:
interfaces between the surveyed crowns and the clasps of 225-34.
17. Ohkubo C, Kobayashi M, Suzuki Y, Hosoi T. Effect of implant support on
the RPDs and between implant components. Some distal-extension removable partial dentures: in vivo assessment. Int J Oral
components of the finite element models were simpli- Maxillofac Implants 2008;23:1095-101.
18. Pellecchia M, Pellecchia R, Emtiaz S. Distal extension mandibular removable
fied.22,28 In addition, only half of the maxilla and partial denture connected to an anterior fixed implant-supported prosthesis:
the partial RPD were generated and used in the a clinical report. J Prosthet Dent 2000;83:607-12.
19. Cunha LD, Pellizzer EP, Verri FR, Pereira JA. Evaluation of the influence of
present study. The contralateral side might have affected location of osseointegrated implants associated with mandibular removable
the results. Further studies on RPD design, other partial dentures. Implant Dent 2008;17:278-87.
20. Pellizzer EP, Verri FR, Falcon-Antenucci RM, Goiato MC, Gennari Filho H.
implanteabutment connection types, and the use of at- Evaluation of different retention systems on a distal extension removable
tachments with more sophisticated models are required. partial denture associated with an osseointegrated implant. J Craniofac Surg
2010;21:727-34.
21. Shahmiri R, Aarts JM, Bennani V, Atieh MA, Swain MV. Finite element
CONCLUSIONS analysis of an implant-assisted removable partial denture. J Prosthodont
2013;22:550-5.
22. Geng JP, Tan KB, Liu GR. Application of finite element analysis in
Within the limitation of this 3D finite element analysis, implant dentistry: a review of the literature. J Prosthet Dent 2001;85:
the following conclusions were drawn: 585-98.
23. Mericske-Stern R, Assal P, Mericske E, Burgin W. Occlusal force and oral
1. The highest stress was concentrated on the implants tactile sensibility measured in partially edentulous patients with ITI implants.
Int J Oral Maxillofac Implants 1995;10:345-53.
in both IARPDs. 24. Baggi L, Cappelloni I, Di Girolamo M, Maceri F, Vairo G. The influence of
2. Because the stress from the occlusal loading was implant diameter and length on stress distribution of osseointegrated im-
plants related to crestal bone geometry: a three-dimensional finite element
concentrated primarily on the implant when im- analysis. J Prosthet Dent 2008;100:422-31.
plants were used for the RPD abutments, more 25. Lang LA, Kang B, Wang RF, Lang BR. Finite element analysis to determine
implant preload. J Prosthet Dent 2003;90:539-46.
considerations concerning the RPD design and the 26. Anitua E, Tapia R, Luzuriaga F, Orive G. Influence of implant length,
number or location of the implant are necessary. diameter, and geometry on stress distribution: a finite element analysis. Int J
Periodontics Restorative Dent 2010;30:89-95.
27. Murakami N, Wakabayashi N. Finite element contact analysis as a critical
technique in dental biomechanics: a review. J Prosthodont Res 2014;58:
REFERENCES 92-101.
28. Torcato LB, Pellizzer EP, Verri FR, Falcón-Antenucci RM, Santiago Júnior JF,
1. Mentag PJ, Kosinski TF, Sowinski LL. Fabrication of a maxillary prosthesis de Faria Almeida DA. Influence of parafunctional loading and prosthetic
using dental implants and an “overdenture” attachment. A clinical report. connection on stress distribution: a 3D finite element analysis. J Prosthet
J Prosthet Dent 1991;65:331-5. Dent 2015;114:644-51.
2. Zitzmann NU, Marinello CP. Treatment plan for restoring the edentulous 29. Topkaya T, Solmaz MY. The effect of implant number and position on the
maxilla with implant-supported restorations: removable overdenture versus stress behavior of mandibular implant retained overdentures: a three-
fixed partial denture design. J Prosthet Dent 1999;82:188-96. dimensional finite element analysis. J Biomech 2015;48:2102-9.
3. Chronopoulos V, Sarafianou A, Kourtis S. The use of dental implants in 30. Nakamura Y, Kanbara R, Ochiai KT, Tanaka Y. A finite element evaluation of
combination with removable partial dentures: a case report. J Esthet Restor mechanical function for 3 distal extension partial dental prosthesis designs
Dent 2008;20:355-64. with a 3-dimensional nonlinear method for modeling soft tissue. J Prosthet
4. Sato M, Suzuki Y, Kurihara D, Shimpo H, Ohkubo C. Effect of implant Dent 2014;112:972-80.
support on mandibular distal extension removable partial dentures: rela- 31. Montgomery J. Methods for modeling bolts in the bolted joint. Paper pre-
tionship between denture supporting area and stress distribution. sented at: ANSYS User’s Conference 2002. Available at: http://server2.docfoc.
J Prosthodont Res 2013;572:109-12. com/uploads/Z2015/12/22/nLEFnyDdtB/3f012e1c82f1b6f7f034b0c2fcd09d06.
5. Jang Y, Emtiaz S, Tarnow DP. Single implant-supported crown used as an pdf. Accessed November 7, 2016.
abutment for a removable cast partial denture: a case report. Implant Dent 32. Wang HY, Zhang YM, Yao D, Chen JH. Effects of rigid and nonrigid
1998;7:199-204. extracoronal attachments on supporting tissues in extension base partial
Eom et al THE JOURNAL OF PROSTHETIC DENTISTRY
742 Volume 117 Issue 6
removable dental prostheses: a nonlinear finite element study. J Prosthet 38. Sano M, Ikebe K, Yang TC, Maeda Y. Biomechanical rationale for six splinted
Dent 2011;105:338-46. implants in bilateral canine, premolar, and molar regions in an edentulous
33. O’Mahony AM, Williams JL, Spencer P. Anisotropic elasticity of cortical and maxilla. Implant Dent 2012;21:220-4.
cancellous bone in the posterior mandible increases peri-implant stress and
strain under oblique loading. Clin Oral Implants Res 2001;12:648-57.
34. Van Staden RC, Guan H, Loo YC. Application of the finite element method in Corresponding author:
dental implant research. Comput Methods Biomech Biomed Engin 2006;9:257-70. Dr Ho-Beom Kwon
35. Himmlova L, Dostalova T, Kacovsky A, Konvickova S. Influence of implant Dental Research Institute and Department of Prosthodontics
length and diameter on stress distribution: a finite element analysis. School of Dentistry
J Prosthet Dent 2004;91:20-5. Seoul National University
36. Kim Y, Oh TJ, Misch CE, Wang HL. Occlusal considerations in implant 101, Daehak-ro, Jongno-gu, Seoul 110-744
therapy: clinical guidelines with biomechanical rationale. Clin Oral Implants REPUBLIC OF KOREA
Res 2005;16:26-35. Email: proskwon@snu.ac.kr
37. LaVere AM, Krol AJ. Selection of a major connector for the extension-base
removable partial denture. J Prosthet Dent 1973;30:102-5. Copyright © 2016 by the Editorial Council for The Journal of Prosthetic Dentistry.
Noteworthy Abstracts of the Current Literature
Grinding damage assessment for CAD-CAM restorative materials
Curran P, Cattani-Lorente M, Anselm Wiskott HW, Durual S, Scherrer SS
Dent Mater 2017;33:294-308
Objectives. To assess surface/subsurface damage after grinding with diamond discs on five CAD-CAM restorative
materials and to estimate potential losses in strength based on crack size measurements of the generated damage.
Methods. The materials tested were: Lithium disilicate (LIT) glass-ceramic (e.max CAD), leucite glass-ceramic (LEU)
(Empress CAD), feldspar ceramic (VM2) (Vita Mark II), feldspar ceramic-resin infiltrated (EN) (Enamic) and a
composite reinforced with nano ceramics (LU) (Lava Ultimate). Specimens were cut from CAD-CAM blocs and
pair-wise mirror polished for the bonded interface technique. Top surfaces were ground with diamond discs of
respectively 75, 54 and 18 mm. Chip damage was measured on the bonded interface using SEM. Fracture mechanics
relationships were used to estimate fracture stresses based on average and maximum chip depths assuming these to
represent strength limiting flaws subjected to tension and to calculate potential losses in strength compared to
manufacturer’s data.
Results. Grinding with a 75 mm diamond disc induced on a bonded interface critical chips averaging 100 mm with a
potential strength loss estimated between 33% and 54% for all three glass-ceramics (LIT, LEU, VM2). The softer
materials EN and LU were little damage susceptible with chips averaging respectively 26 mm and 17 mm with no loss in
strength. Grinding with 18 mm diamond discs was still quite detrimental for LIT with average chip sizes of 43 mm and a
potential strength loss of 42%.
Significance. It is essential to understand that when grinding glass-ceramics or feldspar ceramics with diamond discs
surface and subsurface damage are induced which have the potential of lowering the strength of the ceramic. Careful
polishing steps should be carried out after grinding especially when dealing with glass-ceramics.
Reprinted with permission of The Academy of Dental Materials.
THE JOURNAL OF PROSTHETIC DENTISTRY Eom et al
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- 1.1 Original ResearchDocument8 pages1.1 Original ResearchNovita RPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Jhfdbcsss TFVCBVC FFHGHDocument5 pagesJhfdbcsss TFVCBVC FFHGHNovita RPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- 1 s2.0 S0022391314003606 MainDocument4 pages1 s2.0 S0022391314003606 MainNovita RPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- KKJKKKDocument10 pagesKKJKKKNovita RPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- 1.1 Original ResearchDocument8 pages1.1 Original ResearchNovita RPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- JJHVBBDocument3 pagesJJHVBBNovita RPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- 1.1 Original ResearchDocument8 pages1.1 Original ResearchNovita RPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- 1.1 Original ResearchDocument8 pages1.1 Original ResearchNovita RPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Design of A Removable Partial Denture: by Taseef Hasan Farook, BDS (Final Year, University of Dhaka)Document70 pagesDesign of A Removable Partial Denture: by Taseef Hasan Farook, BDS (Final Year, University of Dhaka)Novita RPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- 96 130 1 SM PDFDocument6 pages96 130 1 SM PDFNovita RPas encore d'évaluation
- Aceh 2 PDFDocument1 pageAceh 2 PDFNovita RPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Podj 38Document4 pagesPodj 38Mohamed AliPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Biomechanics of Oral Mucosa: ReviewDocument20 pagesBiomechanics of Oral Mucosa: ReviewNovita RPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- 1.1 Original ResearchDocument8 pages1.1 Original ResearchNovita RPas encore d'évaluation
- HKGFDDocument4 pagesHKGFDNovita RPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Removable Prosthodontics: Complete Denture Fabrication MethodsDocument1 pageRemovable Prosthodontics: Complete Denture Fabrication MethodsNovita RPas encore d'évaluation
- OgfdgDocument4 pagesOgfdgNovita RPas encore d'évaluation
- Case Report: A Technique For Removing Implant-Retained Denture: Direct Relining ComplicationDocument4 pagesCase Report: A Technique For Removing Implant-Retained Denture: Direct Relining ComplicationNovita RPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- KkakakaDocument5 pagesKkakakaNovita RPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- KKJKKKDocument10 pagesKKJKKKNovita RPas encore d'évaluation
- VITA 1511GB A Guide To Complete Denture Prosthetics PS EN V00 PDFDocument150 pagesVITA 1511GB A Guide To Complete Denture Prosthetics PS EN V00 PDFLaizaEuniceT.Monte0% (1)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Fabrication of Combined Prosthesis With 6d86091e - 2 PDFDocument7 pagesFabrication of Combined Prosthesis With 6d86091e - 2 PDFNovita RPas encore d'évaluation
- V8I9A4Document5 pagesV8I9A4Novita RPas encore d'évaluation
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Analysis of Variability in The Manufacture of Cr-Co Fixed Partial Dentures by Geometric ComparisonDocument8 pagesAnalysis of Variability in The Manufacture of Cr-Co Fixed Partial Dentures by Geometric ComparisonNovita RPas encore d'évaluation
- Zaleske NC MC Article - 2Document2 pagesZaleske NC MC Article - 2Novita RPas encore d'évaluation
- 1 s2.0 S0022391314003606 MainDocument4 pages1 s2.0 S0022391314003606 MainNovita RPas encore d'évaluation
- Simplified Fabrication of An Implant-Supported Framework With Luted Abutment CylindersDocument5 pagesSimplified Fabrication of An Implant-Supported Framework With Luted Abutment CylindersNovita RPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Simplified Fabrication of An Implant-Supported Framework With Luted Abutment CylindersDocument5 pagesSimplified Fabrication of An Implant-Supported Framework With Luted Abutment CylindersNovita RPas encore d'évaluation
- Bgcse Physics Paper 1 2017Document17 pagesBgcse Physics Paper 1 2017Katlego LebekwePas encore d'évaluation
- Improvement of Soil Properties by Using Waste PlasticDocument6 pagesImprovement of Soil Properties by Using Waste PlasticnehamyaPas encore d'évaluation
- ECE 6123 Advanced Signal Processing: 1 FiltersDocument9 pagesECE 6123 Advanced Signal Processing: 1 FiltersJanaki KPas encore d'évaluation
- WLP Creative WritingDocument12 pagesWLP Creative Writingsheena balaisPas encore d'évaluation
- Conduction A Long Simple BarDocument5 pagesConduction A Long Simple Bardiaa ibrahimPas encore d'évaluation
- GasCalc Module enDocument2 pagesGasCalc Module ensppramPas encore d'évaluation
- MALVINO & BATES Chapter 08Document29 pagesMALVINO & BATES Chapter 08Reece RevosaPas encore d'évaluation
- Supercritical PlantDocument71 pagesSupercritical PlantNitish KumarPas encore d'évaluation
- H Beam Weight-TWC PDFDocument1 pageH Beam Weight-TWC PDFSankar CdmPas encore d'évaluation
- IPT2020 Problem01 - CumulativeCannon MIPTDocument31 pagesIPT2020 Problem01 - CumulativeCannon MIPT林凱文Pas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Acara 4 GranulometriDocument63 pagesAcara 4 GranulometriHana Riwu KahoPas encore d'évaluation
- Bp8-Tension: User Defined Applied Forces at Interface Basic DimensionsDocument4 pagesBp8-Tension: User Defined Applied Forces at Interface Basic DimensionsMallesh NenkatPas encore d'évaluation
- List of Least Learned Competencies With Interventions ConductedDocument2 pagesList of Least Learned Competencies With Interventions ConductedGerry Chel-Nunez Awa-Laurente Aga100% (1)
- Life Cycle of Star LabDocument19 pagesLife Cycle of Star LabanicitoaPas encore d'évaluation
- Guide Du Soudage Des Aciers InoxydablesDocument92 pagesGuide Du Soudage Des Aciers InoxydablesFares Hayder100% (1)
- FMP-401 2021-Ag-8243Document4 pagesFMP-401 2021-Ag-8243ABdullah ButtPas encore d'évaluation
- PEX250í 1200 Instruction ManualDocument10 pagesPEX250í 1200 Instruction ManualSebastian Aguila RaipanPas encore d'évaluation
- MathsDocument2 pagesMathsAditya Singh PatelPas encore d'évaluation
- AC O& M City Mall Version 1.0Document12 pagesAC O& M City Mall Version 1.0yewminyun6098Pas encore d'évaluation
- Vib PDFDocument2 pagesVib PDFprasanna1990Pas encore d'évaluation
- NEXAFS Tutorial Review ArticleDocument12 pagesNEXAFS Tutorial Review ArticleAngelique LusuanPas encore d'évaluation
- Dry Gas Seal Systems - Part 2Document3 pagesDry Gas Seal Systems - Part 2Jai-Hong ChungPas encore d'évaluation
- JL Torero - Buoyancy Effects On Smoldering of Polyurethane FoamDocument229 pagesJL Torero - Buoyancy Effects On Smoldering of Polyurethane FoamIsraelPas encore d'évaluation
- UNU - Geothermal Well TestingDocument30 pagesUNU - Geothermal Well TestingZakariyaPas encore d'évaluation
- Earth and Life Science Copy (Repaired)Document39 pagesEarth and Life Science Copy (Repaired)Aaron Manuel MunarPas encore d'évaluation
- Leaded Receptacle Switch BrochureDocument18 pagesLeaded Receptacle Switch BrochureArturo De Asis SplushPas encore d'évaluation
- Report 3 Schlieren Visualisation of Over-Expanded NozzleDocument6 pagesReport 3 Schlieren Visualisation of Over-Expanded NozzleAbhishek DhaknePas encore d'évaluation
- Wopho 13 Prob7-Final PDFDocument3 pagesWopho 13 Prob7-Final PDFPeter JonesPas encore d'évaluation
- Method To Make Yttrium-Barium-Copper Oxide Superconductor (YBCO)Document2 pagesMethod To Make Yttrium-Barium-Copper Oxide Superconductor (YBCO)RUBYPas encore d'évaluation
- Performance Evaluation On Low-Crest Breakwater at North Coast of Java IslandDocument12 pagesPerformance Evaluation On Low-Crest Breakwater at North Coast of Java IslandSobariMuchlisPas encore d'évaluation
- 1,001 Questions & Answers for the CWI Exam: Welding Metallurgy and Visual Inspection Study GuideD'Everand1,001 Questions & Answers for the CWI Exam: Welding Metallurgy and Visual Inspection Study GuideÉvaluation : 3.5 sur 5 étoiles3.5/5 (7)
- The Laws of Thermodynamics: A Very Short IntroductionD'EverandThe Laws of Thermodynamics: A Very Short IntroductionÉvaluation : 4.5 sur 5 étoiles4.5/5 (10)
- Hyperspace: A Scientific Odyssey Through Parallel Universes, Time Warps, and the 10th DimensionD'EverandHyperspace: A Scientific Odyssey Through Parallel Universes, Time Warps, and the 10th DimensionÉvaluation : 4.5 sur 5 étoiles4.5/5 (3)
- Vibration Basics and Machine Reliability Simplified : A Practical Guide to Vibration AnalysisD'EverandVibration Basics and Machine Reliability Simplified : A Practical Guide to Vibration AnalysisÉvaluation : 4 sur 5 étoiles4/5 (2)
- Aerodynamics for Engineering StudentsD'EverandAerodynamics for Engineering StudentsÉvaluation : 5 sur 5 étoiles5/5 (5)
- Einstein's Fridge: How the Difference Between Hot and Cold Explains the UniverseD'EverandEinstein's Fridge: How the Difference Between Hot and Cold Explains the UniverseÉvaluation : 4.5 sur 5 étoiles4.5/5 (51)