Académique Documents
Professionnel Documents
Culture Documents
A Cross-Sectional Study of The Prevalence of
Transféré par
Kurnia pralisaTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
A Cross-Sectional Study of The Prevalence of
Transféré par
Kurnia pralisaDroits d'auteur :
Formats disponibles
ORIGINAL CONTRIBUTIONS 1
see related editorial on page x
A Cross-Sectional Study of the Prevalence of
COLON/SMALL BOWEL
Gastrointestinal Symptoms and Pathology in Patients
With Common Variable Immunodeficiency
Silje F. Jørgensen, MD1, 2, 3, Henrik M. Reims, MD, PhD4, Didrik Frydenlund, MD, PhD4, Kristian Holm, MSc1, 5, Vemund Paulsen, MD6,
Annika E. Michelsen, PhD1, 9, Kristin K. Jørgensen, MD, PhD5, 7, Liv T. Osnes, MD, PhD8, Jorunn Bratlie, BLS1, Tor J. Eide, MD, PhD4, 9,
Christen P. Dahl, MD, PhD1, Ellen Holter, MD10, Rune R. Tronstad, MD11, 12, Kurt Hanevik, MD, PhD11, Hans-Richard Brattbakk, PhD11, 13,
Fatemeh Kaveh, PhD14, Torunn Fiskerstrand, PhD11, 13, Anne-Marte B. Kran, MD, PhD9, 15, Thor Ueland, PhD1, 16,
Tom H. Karlsen, MD, PhD1, 3, 5, 9, Pål Aukrust, MD, PhD1, 2, 3, 9, Knut E.A. Lundin, MD, PhD6, 9, 17 and Børre Fevang, MD, PhD1, 2, 9
OBJECTIVES: The objective of this study was to study the prevalence of gastrointestinal (GI) symptoms and
histopathology in patients with common variable immunodeficiency (CVID) as well as linking the
findings to GI infections and markers of systemic immune activation.
METHODS: In this cross-sectional study, we addressed GI symptoms in 103 patients and GI histopathological
findings in 53 patients who underwent upper and lower endoscopic examination. The most frequent
histopathological findings were linked to GI symptoms, B-cell phenotype, and markers of systemic
immune activation (soluble (s)CD14, sCD25, and sCD163). Microarray analysis compared “celiac-
like disease” in CVID to celiac disease. Screening for selected bacterial and viral infections in fecal
samples and gut mucosal biopsies was performed.
RESULTS: The main findings of this study were as follows: most common GI symptoms were bloating (34%),
pain (30%), and diarrhea (26%). The most frequent histopathological findings were increased
intraepithelial lymphocytes in the descending part of the duodenum, i.e., “celiac-like disease”
(46% of patients), decreased numbers of plasma cells in GI tract mucosa (62%), and lymphoid
hyperplasia (38%), none of which were associated with GI symptoms. Reduced plasma cells in GI
mucosa were associated with B-cell phenotypic characteristics of CVID, and increased serum levels
of sCD14 (P=0.025), sCD25 (P=0.01), and sCD163 (P=0.04). Microarray analyses distinguished
between CVID patients with “celiac-like disease” and celiac disease. Positive tests for bacterial and
viral infections were scarce both in fecal samples and gut mucosal biopsies, including PCR test for
norovirus in biopsy specimens (0 positive tests).
CONCLUSIONS: In conclusion, GI pathology is common in CVID, but does not necessarily cause symptoms. However,
reduced plasma cells in GI mucosa were linked to systemic immune activation, “celiac-like disease”
in CVID and true celiac disease appear to be different disease entities, as assessed by gene
expression, and infections (including norovirus) are rarely a cause of the CVID enteropathy.
SUPPLEMENTARY MATERIAL is linked to the online version of the paper at http://www.nature.com/ajg
Am J Gastroenterol advance online publication, 16 August 2016; doi:10.1038/ajg.2016.329
1
Research Institute of Internal Medicine, Oslo University Hospital, Rikshospitalet, Oslo, Norway; 2Section of Clinical Immunology and Infectious Diseases, Oslo
University Hospital Rikshospitalet, Oslo, Norway; 3K. G. Jebsen Inflammation Research Centre, Institute of Clinical Medicine, University of Oslo, Oslo, Norway;
4
Department of Pathology, Oslo University Hospital, Rikshospitalet, Oslo, Norway; 5Norwegian PSC Research Center, Oslo University Hospital Rikshospitalet,
Oslo, Norway; 6Department of Transplantation Medicine, Section of Gastroenterology, Oslo University Hospital Rikshospitalet, Oslo, Norway; 7Department of
Gastroenterology, Akershus University Hospital, Lørenskog, Norway; 8Department of Immunology, Oslo University Hospital, Rikshospitalet, Oslo, Norway; 9Institute
of Clinical Medicine, University of Oslo, Oslo, Norway; 10Department of Microbiology, Oslo University Hospital, Rikshospitalet, Oslo, Norway; 11Department of
Clinical Science, University of Bergen, Bergen, Norway; 12Department of Pediatrics, Haukeland University Hospital, Bergen, Norway; 13Center for Medical
Genetics and Molecular Medicine, Haukeland University Hospital, Bergen, Norway; 14Medical Genetics Department, Oslo University Hospital, Ullevål, Oslo,
Norway; 15Department of Microbiology, Oslo University Hospital, Ullevål, Oslo, Norway; 16K.G. Jebsen Thrombosis Research and Expertise Center, University
of Tromsø, Tromsø, Norway; 17Centre for Immune Regulation, University of Oslo, Oslo, Norway. Correspondence: Silje F. Jørgensen, MD, Research Institute of
Internal Medicine, Oslo University Hospital, Rikshospitalet, postbox 4950, Nydalen, Oslo 0424, Norway. E-mail: s.f.jorgensen@medisin.uio.no
Received 29 February 2016; accepted 6 July 2016
© 2016 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
2 Jørgensen et al.
INTRODUCTION defined as decreased serum levels of immunoglobulin (Ig)G, IgA,
Common variable immunodeficiency (CVID) is the most com- and/or IgM by at least two standard deviations below the mean
mon symptomatic primary immunodeficiency in adults, with a for age, and exclusion of other causes of hypogammaglobuline-
prevalence of 1 in 25,000 in Caucasians. CVID patients are char- mia (13,14). The actual concentration used as cutoff levels were
COLON/SMALL BOWEL
acterized by a B-cell defect with reduced antibody production for IgG≤5 g/l (15) and for IgA<0.7 g/l. For males and females <50
as the immunological hallmark. However, other immunological years the lower IgM cutoff value was 0.4 g/l and 0.6 g/l, respec-
abnormalities including T-cell deficiency, monocyte/macrophage tively. The study included an upper and lower endoscopy (GIF-
hyperactivity, and signs of low-grade systemic inflammation are HQ190, Olympus, Hamburg, Germany), and the completion of
also described (1). a GI-symptoms questionnaire. Patients undergoing endoscopy
Most of the patients suffer from recurrent bacterial infections in also had blood tests and fecal samples taken prior to endoscopy.
the respiratory tract. A large proportion (68–71%) (2,3) of CVID In addition, duodenal biopsies from 17 healthy adults without
patients, however, also have various forms of autoimmune and abdominal symptoms and 10 patients with untreated celiac dis-
inflammatory disorders; such as immune-mediated cytopenia, ease (16) were obtained for gene-expression profiling analyses.
sarcoid-like granulomas, immune-mediated hepatitis, and various These biopsies were compared with duodenal biopsies from 12
forms of non-malignant and malignant lymphoid disorders (2,4). CVID patients with increased intraepithelial lymphocytes (IEL),
These non-infectious complications in CVID also include various and 8 CVID patients with normal number of IEL in the duode-
forms of inflammatory and autoimmune manifestations of the num (pars descendens).
intestine (5). The study was approved by the Regional Committee for Medical
Intermittent or persistent diarrhea has been described as the and Health Research Ethics and conforms to the principles out-
most common gastrointestinal (GI) symptom in CVID patients, lined in the “Declaration of Helsinki”. Written informed consent
reported in 20–60% of cases, depending on the study (6–10). was obtained from all participants.
Several types of GI infections seem to occur more commonly
in CVID patients, including Giardia, Campylobacter, certain GI symptoms questionnaire
Salmonella species (11), and Cytomegalovirus (CMV) (5), and in a We used the well-validated “GI symptoms” questionnaire Gas-
recent relatively small study (n=8) chronic norovirus infection was trointestinal Symptom Rating Scale IBS (GSRS-IBS); a 13-item
suggested as cause of severe CVID enteropathy (12). In addition, questionnaire to assess the presence of different GI symptoms
there is a wide spectrum of non-infectious GI pathology among using a 7-point Likert scale (17). We considered a few ques-
CVID patients, including nodular lymphoid hyperplasia, atrophic tionnaires suitable for the task of mapping the GI symptoms in
gastritis, inflammatory bowel disease, lymphocytic colitis, and CVID. The question regarding diarrhea was in our opinion, at
celiac-like findings in the duodenum (5,6,8). All of these condi- pre-analysis, the most important symptom to record and the
tions seem to share an abnormal immune response in the GI tract, GSRS-IBS addressed this symptom (as well as pain, bloating,
supported by the fact that many of the patients with GI abnormali- satiety, and constipation) in a way that was transportable to other
ties on endoscopic examination have autoimmune manifestations disease phenotypes (like CVID), however, the questionnaire is
in other organs (10). However, the true frequency of these mani- developed for irritable bowel syndrome (IBS) and is not CVID
festations in CVID, as well as their relation to GI symptoms, and specific.
other clinical and immunological characteristics of CVID patients The patients indicated from 1–7; where 1 was “no discomfort at
are largely undefined. all” and 7 was ”very severe discomfort”. The 13 questions could be
Here, we performed a cross-sectional study in unselected further sub-scaled into symptom clusters of: pain, bloating, con-
CVID patients addressing the prevalence of GI symptoms in stipation, diarrhea, and satiety. The patients with more than 3 on
103 patients and GI histopathological findings in 53 patients the Likert scale (more than “mild discomfort”) were considered
who agreed to undergo endoscopic examination. By including positive for the symptom.
patients irrespective of GI symptoms, we sought to reveal the
true prevalence of GI symptoms and pathology in CVID patients Histopathological assessment
as well as their link to clinical and immunological features in Intestinal biopsies were collected according to protocol (Supple-
these patients. mentary Figure 1 online) at the Section for Gastroenterological
Endoscopy at Oslo University Hospital, Rikshospitalet, Oslo,
Norway. Prior to endoscopy, fecal samples were analyzed for
METHODS pathogenic microbes (Supplementary Methods). Hematoxylin
Study design and eosin-stained slides were reviewed independently by two
All the adult CVID patients (n=112) registered at the Section of pathologists (H.M.R and D.F.) using a structured reporting sheet.
Clinical Immunology and Infectious Diseases at Oslo University The cutoff level for increased IEL in duodenal biopsies has var-
Hospital, Rikshospitalet, Oslo, Norway received a letter invit- ied over the years from 40 IEL/100 enterocytes (EC) to as low as
ing them to participate in the study. The Section functions as a 20 IEL/100 EC for different classification schemes (18–21). In
national center for diagnosis and treatment of primary immuno- this study, an increased number of IELs in the duodenal mucosa
deficiency diseases for adults in Norway. The CVID diagnosis was was defined by a number of IEL ≥25 per 100 EC based on the
The American Journal of GASTROENTEROLOGY www.nature.com/ajg
Gastrointestinal Disease in CVID 3
CVID patients
most recent European (16) and the American College of
Gastroenterology guidelines (22). See Supplementary Informa- 112
tion (online) for methods and further classification into diagnos-
COLON/SMALL BOWEL
tic categories. Endoscopy
Yes No
Gene expression by microarray analysis
Total RNA was extracted from the tissues and each sample was 53 59
biotin-labeled and amplified. The raw data were first imported
into GenomeStudio Data Analysis Software (Illumina, San Diego, Of which....
CA) and then to J-Express 2012 (Bergen, Norway) (23). Corres-
pondence analysis was applied to study global trends in the data
Gastroscopy Colonoscopy GI symptoms GI symptoms
(Supplementary Methods) (24). questionnaire questionnaire
50 52
Statistical analysis 103 total
Both 52 51
Univariate analyses were performed using parametric (t-tests)
or non-parametric methods (Mann–Whitney’s U- and Kruskal– 49
Wallis tests) for continuous variables, and χ2-tests and Fisher’s
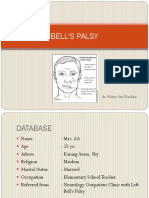
Figure 1. Overview of number of common variable immunodeficiency
exact test for categorical variables. Correlation analysis was (CVID) patients in the study.
performed using parametric (Pearson’s) or non-parametric
(Spearman’s) tests. P values are two-sided and considered signifi-
cant when <0.05.
Detection of norovirus, rotavirus, adenovirus, astrovirus, CMV,
Table 1. Patient characteristics
Epstein–Barr virus (EBV), and Helicobacter pylori in tissue speci-
mens by PCR and/or immunohistochemical assessment, blood Total No endoscopy Endoscopy P value
(n=104)a (n=51)b (n=53)
sampling protocol, measurements of soluble (s)CD14, sCD25,
and sCD163 in serum and The human leukocyte antigen (HLA) Male, n (%) 53 (51) 28 (53) 25 (47) 0.55c
analyses are described in Supplementary Methods. Age, mean 47.5 (19–83) 45.3 (20–83) 49.6 (19–81) 0.16d
years (range)
Splenomegaly, 47 (45) 23 (45) 24 (45) 1.00c
RESULTS n (%)
Study population Organ-specific 20 (19) 9 (17) 11 (21) 0.80c
In all, 112 adult CVID patients were invited to participate in autoimmunity,
n (%)
the study, of whom 53 underwent endoscopy and 103 patients
completed the GI symptom score questionnaire (the 13-item Autoimmune 22 (21) 12 (24) 10 (19) 0.64c
cytopenia,
GSRS-IBS; Figure 1). Forty-nine patients underwent both gas- n (%)
troscopy and colonoscopy, three patients colonoscopy only and
HLA DQ2.5e 34 (38) 19 (37) 15 (28) 0.39c
one patient gastroscopy only (based on the patient preferences).
e
In total, 50 gastroscopies and 52 colonoscopies were performed. HLA DQ8 26 (29) 12 (24) 14 (26) 0.81c
Of the 53 patients undergoing endoscopy, 52 were on Ig replace- Enteropathy, lymphoid hyperplasia, and therefore “Infection only” are not
included because these are influenced by the study. NRH liver (3), LIP (1), and
ment therapy (10 on intravenous IG, 37 on subcutaneous IG, 5 lymphoma (1) are not included due to low numbers.
on a combination thereof, and one refused to take IgG replace- a
The total include: 103 patients filling in the questionnaire plus 1 patient that
ment therapy). None were newly diagnosed CVID patients performed endoscopy but did not fill out the questionnaire.
b
Excluding 8 missing.
and except for IgG substitution, none of the patients were on c
Fisher’s exact test.
any immunomodulatory medication with relevance to the GI d
Independent t-test.
tract. Patient characteristics regarding age, sex, selected non- e
n=90 for the HLA data, 14 (13%) missing.
infectious complications, and the celiac disease-specific HLA
phenotype are presented in Table 1 for the whole cohort n=104
and separately for the group undergoing endoscopy, and the
group not undergoing endoscopy. The recruitment of patients Prevalence of GI symptoms in CVID patients
undergoing endoscopy was based on volunteerism and not The most prevalent symptom in our CVID cohort was bloating
stratified. There was therefore a risk that the cohort undergoing (34%) followed by pain (30%), and diarrhea (26%; Table 2). In
endoscopy would be biased in terms of the patient characteris- total, 48 patients (47%) suffered from one or more pre-defined
tics, but importantly, when comparing the patient characteristics GI symptoms (bloating, pain, diarrhea, satiety, and constipation)
between the patient who had undergone endoscopy and those with no significant difference between the “endoscopy group” and
patients who had not, there were no significant differences. the “no endoscopy group” (Table 2).
© 2016 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
4 Jørgensen et al.
Table 2. Symptoms from GI tract in the study group
Symptomsa CVID %, n (total)b CVID mean (95% CI Mean±s.d. Mean±s.d. no P value endoscopy/
for mean)c endoscopyc endoscopyc no endoscopy
COLON/SMALL BOWEL
Bloating 34%, 34 (99) 2.49 (2.25, 2.74) 2.56±0.18 2.40±0.17 0.52d
Diarrhea 26%, 26 (102) 2.19 (1.94, 2.44) 2.03±0.14 2.35±0.20 0.51e
Constipation 13%, 13 (102) 1.60 (1.37, 1.83) 1.73±0.20 1.51±0.14 0.63e
Pain 30%, 31 (103) 2.12 (1.85, 2.38) 1.99±0.29 1.95±0.16 0.68e
Satiety 14%, 14 (100) 1.55 (1.26, 1.84) 1.59±0.12 1.74±0.15 0.31e
CI, confidence interval; CVID, common variable immunodeficiency; GI, gastrointestinal.
a
GSRS-IBS.
b
≥3 on GSRS-IBS scale.
c
1=no discomfort at all, 2=minor discomfort, 3=mild discomfort, 4=moderate discomfort, 5=moderately severe discomfort, 6=severe discomfort, and 7=very severe
discomfort.
d
t-test.
e
Mann–Whitney’s test for CVID endoscopy patients compared with CVID no endoscopy.
The most frequent histopathological findings in CVID Table 3. Percentage of patients with histopathological finding
The most frequent findings were increased IEL (n=32), reduced
number of plasma cells (n=33), and lymphoid hyperplasia (n=20; Histopathological finding Number of patients, n (%)
Table 3 and Figure 2). In addition, gastric metaplasia of the duo- Increased IEL total 32 (60%)
denal bulb (n=13) and other findings in the stomach (n=19; i.e., Descending part of duodenum 23 (46%)
intestinal metaplasia (n=6), atrophic gastritis (n=9), and fibrosis
Reduced number of plasma cells 33 (62%)
(n=13); Table 3) were frequently present. Inflammation was noted
in 24 patients, representing a heterogeneous group with regard Lymphoid hyperplasia 20 (38%)
to localization and type of inflammation and was therefore not Gastric metaplasia in duodenal bulb 13 (26%)
ranked as a distinct group (Table 3 and Supplementary Table S1). Fibrosis in the gastric mucosa 13 (26%)
Supplementary Table S2 (online) shows the positive findings in Intestinal metaplasia in gastric mucosa 6 (12%)
relation to anatomical localization. The prevalence of increased
Subacute inflammation 2 (4%)
IELs was highest in biopsies taken from the descending part of
the duodenum. Chronic/chronic active inflammation, total 24 (45%)
For the three most common histopathological findings in CVID; Stomach 20 (40%)
increased IEL in the duodenum (pars descendens), reduced num- Colon 11 (22%)
ber of plasma cells. and lymphoid hyperplasia, we looked for asso- Atrophic gastritis 9 (18%)
ciations with certain characteristics of CVID: GI symptoms, B-cell
GVHD-like 1 (2%)
parameters in blood according to the Euro classification (25), and
markers of systemic immune activation, i.e., serum levels of sCD14 Eosinophilic inflammation 4 (8%)
and sCD163 as markers of monocyte activation and sCD25 as a Lymphocytic enteritis/colitis 4 (8%)
marker of T-cell activation. The results are represented below and Collagenous enteritis/colitis 3 (6%)
in Table 4.
Granulomatous inflammation 3 (6%)
GVHD, graft-vs.-host disease; IEL, intraepithelial lymphocytes.
Increased IEL in duodenal biopsies without villous blunting
Text in bold relates to percentage of patients at each anatomical site.
An increased number of IELs was found in one or more biopsy
sites in 32 patients (60%). The presence of increased IEL was most
frequent in duodenal biopsies pars descendens (46%) and bul-
bus (28%), and to a lesser extent in the stomach, ileum, colon, constipation), B-cell phenotype, or markers of systemic inflam-
and rectum (Supplementary Table S2). Of the 23 patients who mation (Table 4).
had IEL≥25 (three patients had IEL above 40), only one had vil-
lous atrophy (Marsh grade 3a. IEL 56). This patient had been on Gene profiling shows little overlap between celiac disease
a gluten-free diet for several years at the time of the biopsy, was and CVID patients with increased IEL
HLADQ2.5 positive, and negative to celiac-specific autoantibod- On the basis of the findings of increased IEL in duodenal biopsies
ies (as one would expect in a patient with antibody deficiency). in CVID, an overlap with celiac disease has been suggested
The finding of increased IEL in pars descendens was not asso- (26). We therefore examined the gene-expression profile in pars
ciated with GI symptoms (diarrhea, bloating, satiety, pain, or descendens of duodenum in CVID patients with increased IEL
The American Journal of GASTROENTEROLOGY www.nature.com/ajg
Gastrointestinal Disease in CVID 5
COLON/SMALL BOWEL
Figure 2. The most common histopathological findings in common variable immunodeficiency (CVID) (a–c) compared with normal histopathological findings
in the same tissue (d–f). (a) Duodenal mucosal villi with an increased number of intraepithelial lymphocytes (arrows). (b) Colonic mucosa with a reduced
number of plasma cells in the lamina propria. (c) Duodenal mucosa with a lymphoid aggregate (arrows). (d) Normal duodenal mucosal villi illustrating nor-
mal number of intraepithelial lymphocytes. (e) Normal colonic mucosa with a plasma cells (arrows) in the lamina propria. (f) Normal duodenal mucosa.
2.0
Table 4. Comparing the most common histopathological finding CVID
CVID
in CVID with GI symptoms, B-cell phenotype, and systemic CVID
CVID CVID
inflammation H
1.0 CVID
H
CVID
CVID
CVID
CVID
CVID
Marsh 3a
CVID subtypes Histopathological findings H
CVID CVID
CVID
CVID CVID
H H H
H
Reduced plasma Lymphoid Increased IEL in H H
CVID
CVID
CVIDH
cells hyperplasia pars descendens 0.0 H
H
CD
CDCD
GI symptoms No No No H Marsh 1
H
B-cell phenotype ↓switched memory, ↑B-cells No –1.0
H
CD
CVID
(Euroclass) ↑CD21low, H
CD
CD
Systemic inflam- ↑sCD14, ↑sCD163, No No CD CDCD
mation (sCD14, ↑sCD25
sCD163, sCD25) –2.0
H
CVID, common variable immunodeficiency; GI, gastrointestinal. Celiac disease CVID-IEL
CVID-normal Healthy CD
–3.0
–3.0 –2.0 –1.0 0.0 1.0 2.0
(n=12, IEL mean 33 (range 25–56) IEL/100 EC), CVID with nor-
Figure 3. Principal component plot showing the difference in gene expres-
mal levels of IEL (n=8), untreated celiac disease (n=10, Marsh sion between common variable immunodeficiency (CVID) patients with
grade 3a or above), and healthy controls (n=17) by cDNA micro- increased intraepithelial lymphocytes (IEL), CVID patients with normal
array assessment. With regard to the gene-expression profile, IEL, patients with celiac disease, and healthy controls. In the CA plot, the
CVID patients with increased IEL were more similar to CVID microarray data for samples are projected onto a two-dimensional plane
patients with normal IEL than to celiac disease patients (Figure 3). defined by the first and second principal components. The first principal
component (along the x-axis) explains most of the total χ2 (6.9%), the
Even the CVID patient with Marsh grade 3a did not cluster second principal component explains second most of the total χ2 (6.1%).
with the other celiac disease patients (Figure 3). This difference Samples that are close together in the plot are more similar than samples
between CVID and celiac disease was also confirmed by dis- further apart. The lines drawn from the origin and through the group mean
criminating pathways analyses (Supplementary Figure 2a–d and gives the direction of the sample group.
Supplementary Table S3a–h). In fact, 544 genes (q=0) are signifi-
cantly different expressed between CVID with increased IEL and
celiac disease (Supplementary Table 4; see URL). (Table 1). Forty-two patients who underwent gastroscopy had
We also investigated the occurrence of two HLA genotypes com- HLA DQ2.5 and HLA DQ8 data available. Of these, 13 patients
mon in celiac disease: HLA DQ2.5 and HLA DQ8 in our cohort carried the HLA DQ2.5 genotype (26%) of which 7 had increased
© 2016 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
6 Jørgensen et al.
IEL in duodenal pars descendens and 6 did not, showing no asso- remaining 11 patients with diarrhea, but without chronic inflam-
ciation with increased IEL in duodenal pars descendens (Fisher’s mation of the colon, were difficult to pin-point with two excep-
exact test, P=0.75; Supplementary Table S5). Also, HLA DQ8 was tions; one patient with infection with Cryptosporidium (found
present in 14 CVID patients (26%) and was not associated with on fecal screening) and one patient with collagenous enteritis
COLON/SMALL BOWEL
increased IEL in duodenal pars descendens (Fisher’s exact test, (antrum; Supplementary Table S6).
P=0.76). Compared with patients without any histological inflamma-
tion, those categorized in the heterogeneous inflammation group,
Reduced numbers of plasma cells are associated with an irrespective of site, were associated with increased level of sCD25
inflammatory phenotype (1.93 ng/ml (0.96–2.24) vs. 0.78 ng/ml (0.62–1.34); P=0.03),
A paucity or lack of plasma cells was found in 33 of the patients and inflammation of the antrum (stomach) was associated with
(62%), most frequently in the colon (56%) followed by rectum increased sCD14 (3,816 ng/ml (3,332–5,354) vs. 3,281 ng/ml
(50%), ileum (42%), duodenum (42%), and—to a much lesser (2,785–3,964); P=0.02), and sCD25 (2.02 ng/ml (0.91–2.24) vs.
extent—in the stomach (16%). Reduced number of plasma cells 0.90 ng/ml (0.63–1.37); P=0.03), given as median and (25–75) per-
at one or more site were associated with the B-cell characteristics centiles, with and without inflammation, respectively.
in peripheral blood, i.e., decreased switched memory (P=0.0004)
and CD21low B-cells (P=0.045), but not with percentage of CD19+ Malignancy and acute inflammation
B-cells (P=0.47), or total number of circulating B-cells (P=0.24; None of the biopsies showed malignancy, acute infection, or
Table 4). Patients with reduced plasma cells in GI mucosa, had inflammation. However, intestinal metaplasia in the gastric
increased serum levels of sCD14 (3,620 ng/ml (3,185–4,282) vs. mucosa was present in 6 (12%) patients.
2,939 ng/ml (2,482–3,945), P=0.025) and sCD163 (1,055 ng/
ml (825–1,314) vs. 581 ng/ml (420–1,382), P=0.04) as mark- Gastrointestinal infections in CVID
ers of monocyte activation and sCD25 (1.49 ng/ml (0.87–2.05) Screening for GI infections prior to endoscopy revealed the fol-
vs. 0.61 ng/ml (0.52–1.29), P=0.01) as marker of T-cell activa- lowing outcomes: one patient with Clostridium difficile (positive
tion, with and without reduced plasma cells, respectively, given PCR for toxin A and B and culture), one had Cryptosporidium
in median (25–75 percentiles; Table 4). We found no association (rapid immunoassay and positive microscopy including Ziehl–
with reduced plasma cells (at one or more site in the GI tract) Neelsen), and one had Campylobacter jejuni infection (stool cul-
and GI symptoms (i.e., pain, bloating, constipation, diarrhea, and ture). The patients with infections generally had few pathological
satiety). findings on endoscopy (data not shown) and only the patient with
Cryptosporidium had significant symptoms (i.e., diarrhea).
Lymphoid hyperplasia is associated with increased number of In all, 3 out of 50 patients were found positive for H. pylori rapid
circulating B-cells test directly on the biopsy at the time of endoscopy. In addition,
Lymphoid hyperplasia was present in one or more biopsy sites in immunohistochemical staining for H. pylori was performed in
20 patients (38%; Table 3), being most frequent in the duodenum biopsies from gastric corpus and antrum on all patients (n=50),
(26%, Supplementary Table S2). Lymphoid hyperplasia was asso- detecting only one patient with positive staining (also positive
ciated with increased numbers of circulating B-cells (238 cells/μ l rapid test).
(105–408) vs. 104 cells/μ l (31–221), P=0.019, with and without In the light of the recent publication (12) of the potentially prom-
lymphoid hyperplasia, respectively, given in median (25–75 per- inent role of chronic norovirus infection leading to GI enteropathy
centiles)), but not with GI symptoms or signs of systemic inflam- in CVID patients, we investigated the presence of norovirus RNA
mation (i.e., sCD14, sCD25, and sCD163; Table 4). and other viruses with a potential to cause GI infection (i.e., rotavi-
rus, adenovirus, and astrovirus) in biopsies from 52 CVID patients
Chronic inflammation in GI biopsies from CVID patients is from three different sites (stomach (n=40), duodenum (n=49),
associated with systemic inflammation and immune activation and colon (n=46) by PCR (Supplementary Methods). None of
In total, 24 (45%) CVID patients had chronic/chronic active the biopsies were positive for norovirus, adenovirus, or astrovirus.
inflammation on histological examination (Table 3 and Supple- One patient had positive rotavirus PCR both in the duodenal and
mentary Table S1), of which 11 had chronic active or chronic colon biopsy. He suffered from diarrhea, pain, bloating, and satiety
inflammation of the colon. In our study, 17 CVID patients had syndrome, and histopathology showed increased IEL in the duode-
diarrhea syndrome (>3 on the GSRS-IBS scale), and in only 6 of nal biopsy and GVHD-like finding in the colon (Supplementary
these, diarrhea was associated with inflammatory manifestation Table S6, patient 13). The healthy controls from the microarray
in the colon (“GVHD (graft-vs.-host disease)-like” (n=1), eosino- analysis (duodenal biopsies, n=17) were used as controls and were
philic inflammation (n=1), collagenous colitis (n=2), lympho- negative for all the above enteropathogenic viruses.
cytic colitis (n=1), and unspecified chronic active inflammation We also investigated the presence of EBV and CMV from the
(n=1); Table 3 and Supplementary Table S1). Of the five other same three sites in the GI tract. Twelve (10 patients) of a total of
patients with chronic inflammation of the colon, but not diarrhea 127 biopsies (41 in the duodenum, 40 in the stomach, and 46 in the
syndrome, two had “IBD-like” findings, two had granulomas, colon) had positive PCR test for EBV; six positives from stomach,
and one patient had eosinophilic inflammation. The causes of the five positives from duodenum (including two positives in both
The American Journal of GASTROENTEROLOGY www.nature.com/ajg
Gastrointestinal Disease in CVID 7
stomach and duodenum), and one positive in the colon biopsy. Six common pathogenic mechanism of celiac disease and “celiac-like”
(4 patients) out of 127 biopsies were positive for CMV PCR, two disease findings in CVID patients. The unreliable auto-antibody
at each site of stomach, duodenum, and colon. However, none of tests owing to B-cell deficiency, inconsistent response to gluten-
COLON/SMALL BOWEL
these positive specimens were positive on immunohistochemistry free diet (31,32), and inconsistency in the HLA profile in CVID
(CMV) or in situ hybridization (EBV). There was no association patients with celiac-like disease contribute to making the diagno-
between histopathological findings or symptoms with positive sis of concomitant celiac disease challenging in CVID. This is also
CMV and/or EBV by PCR. illustrated for the patient with increased IEL and villous atrophy
in our study were the histopathology and HLA phenotype sup-
ports the diagnosis of celiac disease, whereas the lack of response
DISCUSSION to gluten-free diet and the unreliable interpretation of the autoan-
In the present study, 103 CVID patients were screened for GI tibodies weakens the likelihood that this is a true celiac disease.
symptoms and 53 unselected CVID patients underwent endo- It is in fact difficult in all CVID patients to truly confirm or rule
scopic examination. Our major findings were as follows: (i) out if they have celiac disease or if the histopathological finding is
bloating (34%), pain (30%), and diarrhea (26%) were the most part of the immunodeficiency syndrome representing an immune-
common gastrointestinal symptoms. (ii) The most frequent histo- mediated complication as seen at other sites in the GI tract and in
pathological findings were increased IEL in the descending parts other organs in CVID. The large difference in gene-expression data
of the duodenum, decreased plasma cells in GI tract mucosa, and shown in this study supports that celiac disease and CVID with
lymphoid hyperplasia. (iii) Decreased number of plasma cells was increased IEL are different disease entities. Other possible triggers
associated with immunological features of the CVID patients. for the increased IEL than gluten may be infectious, but as shown
(iv) The heterogeneous inflammation group, irrespective of site, in this study, the rate of infection is low and therefore the trigger is
was associated with signs of systemic immune activation. (v) The unlikely to be infectious. In our opinion the celiac-like findings in
CVID patients with increased IEL in pars descendens of duode- CVID most probably reflect an immune-dysregulated phenotype
num showed little or no overlap with celiac disease, as assessed in these patients with immunodeficiency co-existing with persis-
by gene-expression microarray analyses and HLA typing. (vi) GI tent immune activation and inflammation. On the basis of this
tract infection, such as H. pylori, was seen only in one patient and hypothesis, the treatment approach could be immunomodulatory
none of the patients had evidence of chronic norovirus infection. rather than a gluten-free diet. Notwithstanding, systematic studies
The strengths of this study lie in the cross-sectional design that explore the role of gluten-free diets in CVID with increased
within a given time frame, standardized biopsy procedure, the IEL, in particular randomized intervention trial, could be
structured reporting questionnaire, the dual endoscopy (gastros- warranted.
copy and colonoscopy) investigation in the majority of patients, A reduced number of plasma cells in mucosal tissue were found
and the inclusion of patients with and without GI tract symptoms. to be associated with signs of increased systemic inflammation
Moreover, the CVID patients who underwent endoscopy were rep- (i.e., increased serum levels of sCD14 and sCD163) and immune
resentative for our total CVID cohort at our hospital with regard activation (sCD25), but not with GI symptoms. Moreover, this
to clinical characteristics and GI symptoms. Previous studies have histological feature was significantly associated with certain B-cell
been inconsistent in the reporting of GI disease in CVID, mainly phenotypes in peripheral blood, i.e., decreased class-switched
due to inadequate investigation of the GI tract, biased study popu- memory and increased CD21low B-cells, the latter is known to be
lation in terms of symptoms, retrospective study design, and low associated with non-infectious complications in CVID (33). The
number of participants in each study (5,27–29). Based on our reason for these associations is at present not clear, but underscore
study design, we believe that our data give a good indicator of the that reduced plasma cells in GI tract mucosa is not an “obligate”
prevalence of GI disease and symptoms in the CVID population finding in all patients with B-cell deficiency. The finding of reduced
representing a disease model of the interaction between immuno- plasma cells in mucosal tissue could therefore potentially be used
deficiency, autoimmunity, and the GI tract. as an indicator of a “systemic” phenotype, (a state of low-grade
Herein, we showed increased IEL in a large proportion (i.e., systemic inflammation and immune activation) which in turn is
46%) of biopsies from duodenum. With one exception, however, related to inflammatory and autoimmune complication (2).
this was not accompanied by villous atrophy. This may seem in In this study we show that a large proportion of the CVID
contrast to previous publications where villous atrophy was pre- patients had chronic inflammation of the GI tract, associated
sent in duodenal biopsies in 31–42% of CVID patients (26,27,30). with signs of systemic immune activation in both monocytes and
However, these studies give no indication of the true prevalence of T cells. Perreau et al. (34) have reported that increased systemic
villous atrophy in CVID due to their retrospective study design, endotoxin levels are associated with systemic T-cell pathology in
and that the individuals studied were patients with severe GI CVID, and our findings herein may suggest a link between GI
symptoms. On the other hand, Maarschalk et al. (29) found in inflammation and T-cell as well as monocyte pathology. GI inflam-
their cross-sectional study only 1 patient out of 30 (3%) with vil- mation may contribute to microbial translocation with subsequent
lous atrophy, but unfortunately, this study lacked information on systemic immune activation as seen in other diseases like HIV
IEL. The apparent co-existence of CVID and celiac disease has pre- infection (35). We have recently shown that lipopolysaccharide (a
viously been described (31), but it is not clear if this represents a marker of microbial translocation) is increased in plasma in CVID
© 2016 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
8 Jørgensen et al.
patients—associated with altered gut microbiota in these patients Rune R. Tronstad, Hans-Richard Brattbakk, and Torunn Fiskerstrand;
(36). It is tempting to hypothesize that altered gut microbiota and performed the pathway analysis: Fatemeh Kaveh; analyzed the data
GI tract inflammation, causing a breach in the mucosal surface and performed statistical analysis: Silje F. Jørgensen, Kristian
of the GI tract results in a “leaky gut” where lipopolysaccharide
COLON/SMALL BOWEL
Holm, Hans-Richard Brattbakk, Annika E. Michelsen, and Thor
leaks into the blood stream, could contribute to the inflammatory Ueland; coordinated and supervised the project: Silje F. Jørgensen,
phenotype seen in a large proportion of CVID patients. Børre Fevang, Tor J. Eide, Pål Aukrust, and Tom H. Karlsen; and
Of particular interest with regard to the unexplained diarrhea, drafted the manuscript Silje F. Jørgensen, Henrik M. Reims, Didrik
we were not able to replicate the recently shown association of Frydenlund, Børre Fevang, and Pål Aukrust. All authors revised the
CVID enteropathy and chronic norovirus infection in our cohort. manuscript for critical content and approved the final version.
The difference in results may be due to patient selection and that Financial support: S.F.J. was funded by a grant from the South-East-
Woodward et al. (12) did a more detailed investigation. However, ern Norway Regional Health Authority (project number 2012063).
although Woodward et al. (12) examined 8 patients, we analyzed Potential competing interests: None.
samples from 52 patients, and the fact that we are not able to Data and material availability: Microarray data are deposited in
identify any patients with norovirus in our cohort suggests that the GEO archives with data accession number: GSE72625 URL:
norovirus is unlikely to be a common cause of the GI enteropathy http://www.ncbi.nlm.nih.gov/geo/query/acc.cgi?acc=GSE72625.
of unknown etiology in CVID.
H. pylori infection has previously been associated with gastritis
in CVID (37), but none of the patients with atrophic gastritis or intes- Study Highlights
tinal metaplasia in our study had positive H. pylori tests, nor did the
WHAT IS CURRENT KNOWLEDGE
✓ Gastrointestinal symptom and histopathology in common
single patient with positive H. pylori test have atrophic gastritis. This
suggests another or an additional trigger of atrophic gastritis in CVID.
variable immunodeficiency (CVID) patients varies greatly
In summary, GI pathology is common in CVID, but all patho- between studies, potentially reflecting that a low number of
logy does not necessarily correspond with symptoms. However, patients have been included.
certain findings (i.e., reduced plasma cells in mucosa and GI tract ✓ There is a wide spectrum of non-infectious gastrointestinal
inflammation) were associated with increased levels of sCD25 (GI) pathology among CVID patients, but neither their fre-
and sCD14, suggesting a link between GI pathology, and systemic quency in an unbiased CVID cohort in terms of symptoms,
inflammation and immune activation in CVID. Although similari- nor their relationship to other clinical and immunological
characteristics is established.
✓ The apparent co-existence of CVID and celiac disease
ties between patients with celiac disease and CVID patients with
increased IEL on duodenal biopsies, our findings suggest that these
has previously been described, but it is not clear if this
two groups represent different disease entities. Moreover, very few represents a common pathogenic mechanism of true celiac
patients had positive tests for microbes associated with GI patho- disease and “celiac-like” disease findings in CVID patients.
logy including norovirus and H. pylori. Future studies should aim ✓ A recent study suggests chronic norovirus as the cause of
to identify the triggers for CVID enteropathy as well as to charac- severe CVID enteropathy.
terize the molecular mechanisms for increased IEL and lymphoid WHAT IS NEW HERE
hyperplasia in GI mucosa of CVID patients. ✓ In the largest study of GI symptoms and GI histopathology,
performing upper and lower endoscopies in CVID patients
ACKNOWLEDGMENTS with and without GI symptoms, we found that the most
Mona Bjørnstad, Liv Wenche Thorbjørnsen, Hege Dahlen Sollid, frequent histopathological findings in GI mucosa of CVID
patients were increased intraepithelial lymphocytes (IEL)
and other members of the Norwegian PSC Research Center are
in descending duodenum—celiac-like disease—(46%
acknowledged for support on sample collection and logistics. We of patients), decreased plasma cells in GI tract mucosa
acknowledge the technical support and service from the Genomics (62%), and lymphoid hyperplasia (38%).
Core Facility at the Department of Clinical Science, the University of ✓ Reduced plasma cells in GI mucosa were associated with
Bergen. Anusha Aravinthan and the Department of Microbiology at B-cell phenotypes and signs of low-grade systemic immune
Oslo University Hospital are acknowledged for technical assistance. activation and inflammation reflecting phenotypic charac-
teristics of CVID.
CONFLICT OF INTEREST ✓ CVID patients with “celiac-like disease” and true celiac disease
are different disease entities as assessed by gene-expression
Guarantor of the article: Silje F. Jørgensen, MD.
analysis and The human leukocyte antigen (HLA) genotyping.
Specific author contributions: Recruited subjects, obtained human
samples, and clinical data collection: Silje F. Jørgensen, Børre
✓ Norovirus infection was not found as a cause of CVID
enteropathy in our cohort.
Fevang, Kurt Hanevik, Jorunn Bratlie, Christen P. Dahl, Kristin K.
Jørgensen, and Pål Aukrust; reviewed the pathology slides: Henrik
M. Reims and Didrik Frydenlund; performed the endoscopies: Knut
E.A. Lundin and Vemund Paulsen; performed the flow cytometry REFERENCES
1. Yong PF, Thaventhiran JE, Grimbacher B. "A rose is a rose is a rose," but
analysis: Liv T. Osnes; performed PCR analysis: Anne-Marte B. Kran CVID is not CVID common variable immune deficiency (CVID), what do
and Ellen Holter; contributed to the microarray analysis: we know in 2011? Adv Immunol 2011;111:47–107.
The American Journal of GASTROENTEROLOGY www.nature.com/ajg
Gastrointestinal Disease in CVID 9
2. Resnick ES, Moshier EL, Godbold JH et al. Morbidity and mortality in com- 19. Mahadeva S, Wyatt J, Howdle P. Is a raised intraepithelial lymphocyte count
mon variable immune deficiency over 4 decades. Blood 2012;119:1650–7. with normal duodenal villous architecture clinically relevant? J Clin Pathol
3. Chapel H, Lucas M, Lee M et al. Common variable immunodeficiency 2002;55:424–8.
disorders: division into distinct clinical phenotypes. Blood 2008;112: 20. Hayat M, Cairns A, Dixon M et al. Quantitation of intraepithelial lympho-
277–86. cytes in human duodenum: what is normal? J Clin Pathol 2002;55:393–4.
COLON/SMALL BOWEL
4. Chapel H, Cunningham-Rundles C. Update in understanding common 21. Veress B, Franzén L, Bodin L et al. Duodenal intraepithelial lymphocyte-
variable immunodeficiency disorders (CVIDs) and the management of count revisited. Scand J Gastroenterol 2004;39:138–44.
patients with these conditions. Br J Haematol 2009;145:709–27. 22. Rubio-Tapia A, Hill ID, Kelly CP et al. ACG clinical guidelines: diagnosis
5. Daniels JA, Lederman HM, Maitra A et al. Gastrointestinal tract pathology and management of celiac disease. Am J Gastroenterol 2013;108:656–76.
in patients with common variable immunodeficiency (CVID): a clinico- 23. Dysvik B, Jonassen I. J-Express: exploring gene expression data using Java.
pathologic study and review. Am J Surg Pathol 2007;31:1800–12. Bioinformatics 2001;17:369–70.
6. Cunningham-Rundles C, Bodian C. Common variable immunodeficiency: 24. Fellenberg K, Hauser NC, Brors B et al. Correspondence analysis applied to
clinical and immunological features of 248 patients. Clin Immunol 1999;92: microarray data. Proc Natl Acad Sci USA 2001;98:10781–6.
34–48. 25. Wehr C, Kivioja T, Schmitt C et al. The EUROclass trial: defining subgroups
7. Hermans PE, Diaz-Buxo JA, Stobo JD. Idiopathic late-onset immuno- in common variable immunodeficiency. Blood 2008;111:77–85.
globulin deficiency: clinical observations in 50 patients. Am J Med 1976;61: 26. Luzi G, Zullo A, Iebba F et al. Duodenal pathology and clinical-immuno-
221–37. logical implications in common variable immunodeficiency patients. Am J
8. Hermaszewski R, Webster A. Primary hypogammaglobulinaemia: a survey Gastroenterol 2003;98:118–21.
of clinical manifestations and complications. QJM 1993;86:31–42. 27. Malamut G, Verkarre V, Suarez F et al. The enteropathy associated with
9. Quinti I, Soresina A, Spadaro G et al. Long-term follow-up and outcome of common variable immunodeficiency: the delineated frontiers with celiac
a large cohort of patients with common variable immunodeficiency. J Clin disease. Am J Gastroenterol 2010;105:2262–75.
Immunol 2007;27:308–16. 28. Khodadad A, Aghamohammadi A, Parvaneh N et al. Gastrointestinal
10. Washington K, Stenzel TT, Buckley RH et al. Gastrointestinal pathology manifestations in patients with common variable immunodeficiency.
in patients with common variable immunodeficiency and X-linked Dig Dis Sci 2007;52:2977–83.
agammaglobulinemia. Am J Surg Pathol 1996;20:1240–52. 29. Maarschalk-Ellerbroek LJ, Oldenburg B, Mombers IM et al. Outcome of
11. Oksenhendler E, Gérard L, Fieschi C et al. Infections in 252 patients with screening endoscopy in common variable immunodeficiency disorder and
common variable immunodeficiency. Clin Infect Dis 2008;46:1547–54. X-linked agammaglobulinemia. Endoscopy 2013;45:320–3.
12. Woodward JM, Gkrania-Klotsas E, Cordero-Ng AY et al. The role of 30. Teahon K, Webster AD, Price AB et al. Studies on the enteropathy associ-
chronic norovirus infection in the enteropathy associated with common ated with primary hypogammaglobulinaemia. Gut 1994;35:1244–9.
variable immunodeficiency. Am J Gastroenterol 2015;110:320–7. 31. Venhoff N, Emmerich F, Neagu M et al. The role of HLA DQ2 and DQ8
13. International Union of Immunological Societies. Primary immunodefi- in dissecting celiac-like disease in common variable immunodeficiency.
ciency diseases. Report of an IUIS Scientific Committee. Clin Exp Immunol J Clin Immunol 2013;33:909–16.
1999;118:1–28. 32. Biagi F, Bianchi PI, Zilli A et al. The significance of duodenal mucosal
14. Al-Herz W, Bousfiha A, Casanova JL et al. Primary immunodeficiency atrophy in patients with common variable immunodeficiency: a clinical
diseases: an update on the classification from the international union of and histopathologic study. Am J Clin Pathol 2012;138:185–9.
immunological societies expert committee for primary immunodeficiency. 33. Mouillot G, Carmagnat M, Gerard L et al. B-cell and T-cell phenotypes in
Front Immunol 2014;5:162. CVID patients correlate with the clinical phenotype of the disease. J Clin
15. Ameratunga R, Woon ST, Gillis D et al. New diagnostic criteria for com- Immunol 2010;30:746–55.
mon variable immune deficiency (CVID), which may assist with decisions 34. Perreau M, Vigano S, Bellanger F et al. Exhaustion of bacteria-specific CD4
to treat with intravenous or subcutaneous immunoglobulin. Clin Exp T cells and microbial translocation in common variable immunodeficiency
Immunol 2013;174:203–11. disorders. J Exp Med 2014;211:2033–45.
16. Ludvigsson JF, Bai JC, Biagi F et al. Diagnosis and management of adult 35. Vazquez-Castellanos JF, Serrano-Villar S, Latorre A et al. Altered metabo-
coeliac disease: guidelines from the British Society of Gastroenterology. Gut lism of gut microbiota contributes to chronic immune activation in HIV-
2014;63:1210–28. infected individuals. Mucosal Immunol 2015;8:760–72.
17. Wiklund IK, Fullerton S, Hawkey CJ et al. An irritable bowel syndrome- 36. Jorgensen SF, Troseid M, Kummen M et al. Altered gut microbiota profile
specific symptom questionnaire: development and validation. Scand J in common variable immunodeficiency associates with levels of lipopoly-
Gastroenterol 2003;38:947–54. saccharide and markers of systemic immune activation. Mucosal Immunol;
18. Oberhuber G, Granditsch G, Vogelsang H. The histopathology of coeliac advance online publication, 16 March 2016; doi:10.1038/mi.2016.18.
disease: time for a standardized report scheme for pathologists. Eur J 37. Zullo A, Romiti A, Rinaldi V et al. Gastric pathology in patients with com-
Gastroenterol Hepatol 1999;11:1185–94. mon variable immunodeficiency. Gut 1999;45:77–81.
© 2016 by the American College of Gastroenterology The American Journal of GASTROENTEROLOGY
Vous aimerez peut-être aussi
- Inflammatory Bowel Disease: Translating Basic Science into Clinical PracticeD'EverandInflammatory Bowel Disease: Translating Basic Science into Clinical PracticePas encore d'évaluation
- Complementary and Alternative Medical Lab Testing Part 5: GastrointestinalD'EverandComplementary and Alternative Medical Lab Testing Part 5: GastrointestinalPas encore d'évaluation
- [03241750 - Acta Medica Bulgarica] Extraintestinal Manifestations and Intestinal Complications in Patients with Crohn's Disease_ Associations with Some Clinico-Laboratory Findings, Immunological Markers and Therapy.pdfDocument6 pages[03241750 - Acta Medica Bulgarica] Extraintestinal Manifestations and Intestinal Complications in Patients with Crohn's Disease_ Associations with Some Clinico-Laboratory Findings, Immunological Markers and Therapy.pdfTeodorPas encore d'évaluation
- Human Leukocyte Antigen HLADRB1 Determinants Susceptibility To Gastroesophageal Reflux DiseaseDocument5 pagesHuman Leukocyte Antigen HLADRB1 Determinants Susceptibility To Gastroesophageal Reflux DiseaseThiago ThiagoPas encore d'évaluation
- Celiac DiseaseDocument11 pagesCeliac DiseaseXela AviàPas encore d'évaluation
- FFFFDocument11 pagesFFFFNejc KovačPas encore d'évaluation
- Background: Ormdl3 and of GSDMB Were Significantly Increased in Hrv-Stimulated PBMCSDocument6 pagesBackground: Ormdl3 and of GSDMB Were Significantly Increased in Hrv-Stimulated PBMCSSav GaPas encore d'évaluation
- Gastritis and Gastropathy Perspectives From The EndoscopistDocument4 pagesGastritis and Gastropathy Perspectives From The Endoscopisthenrique.uouPas encore d'évaluation
- WJG 20 Anniversary Special Issues (3) : Inflammatory Bowel DiseaseDocument10 pagesWJG 20 Anniversary Special Issues (3) : Inflammatory Bowel DiseaseDeril RidwanPas encore d'évaluation
- Inflamatory Bowel Disease: Dr. Samir IsmailDocument82 pagesInflamatory Bowel Disease: Dr. Samir IsmailGhadeer EbraheemPas encore d'évaluation
- Prevalence of Anemia and Iron Deficiency in Romanian Patients With Inflammatory Bowel Disease: A Prospective Multicenter StudyDocument6 pagesPrevalence of Anemia and Iron Deficiency in Romanian Patients With Inflammatory Bowel Disease: A Prospective Multicenter StudyOcha24 TupamahuPas encore d'évaluation
- P 219 HTLV 1 Infected Regulatory T Cell Expansion.255 PDFDocument2 pagesP 219 HTLV 1 Infected Regulatory T Cell Expansion.255 PDFNilo BarretoPas encore d'évaluation
- 05 - 203perkembangan Terkini Diagnosis Dan Penatalaksanaan Imflammatory Bowel Disease PDFDocument6 pages05 - 203perkembangan Terkini Diagnosis Dan Penatalaksanaan Imflammatory Bowel Disease PDFrisda aulia putriPas encore d'évaluation
- Systematic Review Gastrointestinal Infection and IncidentDocument11 pagesSystematic Review Gastrointestinal Infection and Incidentgrace liwantoPas encore d'évaluation
- Development of Type I Gastric Carcinoid in Patients With Chronic Atrophic GastritisDocument9 pagesDevelopment of Type I Gastric Carcinoid in Patients With Chronic Atrophic GastritisAbristaSeptikasariPas encore d'évaluation
- FOXP3 Variants Are Independently Associated With Transforming Growth Factor B1 Plasma Levels in Female Patients With Inflammatory Bowel DiseaseDocument9 pagesFOXP3 Variants Are Independently Associated With Transforming Growth Factor B1 Plasma Levels in Female Patients With Inflammatory Bowel DiseasePaula KikuchiPas encore d'évaluation
- 10 1111@hel 12741Document8 pages10 1111@hel 12741Catalina ChPas encore d'évaluation
- Primary Biliary Cholangitis in Patients With SysteDocument4 pagesPrimary Biliary Cholangitis in Patients With SysteOussama MouhPas encore d'évaluation
- Cvid Lancet 2008Document14 pagesCvid Lancet 2008Andre GarciaPas encore d'évaluation
- WJG 19 2612Document9 pagesWJG 19 2612Tanima BiswasPas encore d'évaluation
- Fecal Calprotectin in IBDDocument34 pagesFecal Calprotectin in IBDNathania Nadia Budiman100% (1)
- Fecal Calprotectin in IBDDocument34 pagesFecal Calprotectin in IBDNathania Nadia BudimanPas encore d'évaluation
- Nanoparticle-Mediated-Therapeutic-Approach-for-Ulcerative-Colitis-TreatmentDocument22 pagesNanoparticle-Mediated-Therapeutic-Approach-for-Ulcerative-Colitis-TreatmentAchudan JiiPas encore d'évaluation
- IgA Vasculitis (Henoch-Schönlein Purpura) Clinical Manifestations and DiagnosisDocument29 pagesIgA Vasculitis (Henoch-Schönlein Purpura) Clinical Manifestations and DiagnosisevecataneoPas encore d'évaluation
- Small Intestinal Contrast UltrasonographDocument5 pagesSmall Intestinal Contrast UltrasonographСергей СадовниковPas encore d'évaluation
- Helicobacter Species in The Intestinal Mucosa of Patients With Ulcerative ColitiDocument3 pagesHelicobacter Species in The Intestinal Mucosa of Patients With Ulcerative ColitiAlexandru CozmaPas encore d'évaluation
- Chronic Rhinosinusitis-An Update On Epidemiology, Pathogenesis and ManagementDocument5 pagesChronic Rhinosinusitis-An Update On Epidemiology, Pathogenesis and ManagementNaufal NrwPas encore d'évaluation
- S Stercoralis 30 Casos ClinicosDocument6 pagesS Stercoralis 30 Casos ClinicosYisellPas encore d'évaluation
- During The Coronavirus Disease 2019 (COVID-19) Pandemic, A New Phenomenon Manifesting As ADocument5 pagesDuring The Coronavirus Disease 2019 (COVID-19) Pandemic, A New Phenomenon Manifesting As APratiwiPas encore d'évaluation
- Proceedings of The 33rd World Small Animal Veterinary CongressDocument4 pagesProceedings of The 33rd World Small Animal Veterinary CongressJaviera Paz Rojas ÁlvarezPas encore d'évaluation
- 2003 Probiotic and IBDDocument5 pages2003 Probiotic and IBDsujata sharmaPas encore d'évaluation
- Coeliac Disease: John S. Leeds, Andrew D. Hopper, and David S. SandersDocument14 pagesCoeliac Disease: John S. Leeds, Andrew D. Hopper, and David S. Sandersbdalcin5512Pas encore d'évaluation
- Review: New Concepts in The Pathophysiology of Inflammatory Bowel DiseaseDocument11 pagesReview: New Concepts in The Pathophysiology of Inflammatory Bowel DiseaseReynalth Andrew Sinaga100% (1)
- 1471 230X 12 174 PDFDocument5 pages1471 230X 12 174 PDFAila HinlogPas encore d'évaluation
- Chronic Rhinosinusitis-An Update On Epidemiology, Pathogenesis and ManagementDocument6 pagesChronic Rhinosinusitis-An Update On Epidemiology, Pathogenesis and ManagementNaufal NrwPas encore d'évaluation
- Tuberculosis in Patients On DialysisDocument5 pagesTuberculosis in Patients On Dialysisvasarhely imolaPas encore d'évaluation
- Perkembangan Terkini Diagnosis Dan Penatalaksanaan in Ammatory Bowel Disease (IBD)Document7 pagesPerkembangan Terkini Diagnosis Dan Penatalaksanaan in Ammatory Bowel Disease (IBD)Kayyis FirzadiePas encore d'évaluation
- Histologic Diagnosis of Inflammatory Bowel DiseasesDocument14 pagesHistologic Diagnosis of Inflammatory Bowel DiseasesDiego Fernando Ortiz TenorioPas encore d'évaluation
- Enfermeda CeliacaDocument22 pagesEnfermeda CeliacaOmar CoroPas encore d'évaluation
- Asfari 2020 лактозаDocument6 pagesAsfari 2020 лактозаdr.martynchukPas encore d'évaluation
- Nihms 1688237Document20 pagesNihms 1688237Mohammed KhalidPas encore d'évaluation
- Lower Gastrointestinal Bleeding in Children: Experiences From Referral Center in Southern IranDocument4 pagesLower Gastrointestinal Bleeding in Children: Experiences From Referral Center in Southern IranFernandaPas encore d'évaluation
- Common Variable Immunodeficiency: Epidemiology, Pathogenesis, Clinical Manifestations, Diagnosis, Classification, and ManagementDocument21 pagesCommon Variable Immunodeficiency: Epidemiology, Pathogenesis, Clinical Manifestations, Diagnosis, Classification, and ManagementViviana LunaPas encore d'évaluation
- A Review of Crohn's Disease: Pathophysiology, Genetics, Immunology, Environmental Factors, Clinical Presentation, Diagnosis, ManagementDocument18 pagesA Review of Crohn's Disease: Pathophysiology, Genetics, Immunology, Environmental Factors, Clinical Presentation, Diagnosis, ManagementValentina RodriguezPas encore d'évaluation
- Endo 1Document7 pagesEndo 1Soulseller1983Pas encore d'évaluation
- Ijms 21 05223 PDFDocument42 pagesIjms 21 05223 PDFrohailPas encore d'évaluation
- Eosinophilic Colitis: A Rare Case Report and Review of The LiteratureDocument8 pagesEosinophilic Colitis: A Rare Case Report and Review of The LiteratureIJAR JOURNALPas encore d'évaluation
- Professor Yaron Ilan - Oral Mixture of Autologous Colon-Extracted Proteins For The Crohn's Disease: A Double-Blind Trial.Document11 pagesProfessor Yaron Ilan - Oral Mixture of Autologous Colon-Extracted Proteins For The Crohn's Disease: A Double-Blind Trial.Prof. Yaron IlanPas encore d'évaluation
- The Role of Serum Calprotectin As A Novel Biomarker in Inflammatory Bowel Diseases: A Review StudyDocument7 pagesThe Role of Serum Calprotectin As A Novel Biomarker in Inflammatory Bowel Diseases: A Review StudyVid TiktokPas encore d'évaluation
- Pathophysiology of IBDDocument11 pagesPathophysiology of IBDOktarina Heni SunandarPas encore d'évaluation
- JESP - Volume 49 - Issue 1 - Pages 153-162Document10 pagesJESP - Volume 49 - Issue 1 - Pages 153-162Fathalla Fared MakhloufPas encore d'évaluation
- 539 FullDocument12 pages539 FullFadhel Jimmy AnugerahPas encore d'évaluation
- Di Lillo 2019Document7 pagesDi Lillo 2019putri permata SariPas encore d'évaluation
- Case Control StudyDocument4 pagesCase Control StudyPreeti SainiPas encore d'évaluation
- Prevalence of Helicobacter Pylori Infection and Its Association With Cardiovascular Risk Factors in Korean AdultsDocument7 pagesPrevalence of Helicobacter Pylori Infection and Its Association With Cardiovascular Risk Factors in Korean AdultsAlbert PapilayaPas encore d'évaluation
- Intestinal Host Response To Sars-Cov-2 Infection and Covid-19 Outcomes in Patients With Gastrointestinal SymptomsDocument50 pagesIntestinal Host Response To Sars-Cov-2 Infection and Covid-19 Outcomes in Patients With Gastrointestinal Symptomsmuhamad deniansyahPas encore d'évaluation
- Immunological Response in Diabetes MellitusDocument7 pagesImmunological Response in Diabetes MellitusparacuchoPas encore d'évaluation
- PraktLik 2013 4 8Document4 pagesPraktLik 2013 4 8mustafi28Pas encore d'évaluation
- Summary of Andrew J. Wakefield's Waging War On The Autistic ChildD'EverandSummary of Andrew J. Wakefield's Waging War On The Autistic ChildPas encore d'évaluation
- AACR 2022 Proceedings: Part A Online-Only and April 10D'EverandAACR 2022 Proceedings: Part A Online-Only and April 10Pas encore d'évaluation
- Budget Analysis Report Crs 2011-12-5Document44 pagesBudget Analysis Report Crs 2011-12-5Kurnia pralisaPas encore d'évaluation
- Sejarah Mikrobiologi - Pak Mahyarudin, S.Si, M.Si PDFDocument42 pagesSejarah Mikrobiologi - Pak Mahyarudin, S.Si, M.Si PDFKurnia pralisaPas encore d'évaluation
- Comparison and Analysis of Health Care Delivery Systems Pakistan Versus BangladeshDocument7 pagesComparison and Analysis of Health Care Delivery Systems Pakistan Versus BangladeshKurnia pralisa100% (1)
- 10 1016@j Amjmed 2017 12 024Document22 pages10 1016@j Amjmed 2017 12 024Kurnia pralisaPas encore d'évaluation
- CTG 201712 ADocument7 pagesCTG 201712 AKurnia pralisaPas encore d'évaluation
- Gastritis Staging in Clinical Practice: The OLGA Staging SystemDocument6 pagesGastritis Staging in Clinical Practice: The OLGA Staging SystemKurnia pralisaPas encore d'évaluation
- Research Article: Low Prevalence of Clinically Significant Endoscopic Findings in Outpatients With DyspepsiaDocument7 pagesResearch Article: Low Prevalence of Clinically Significant Endoscopic Findings in Outpatients With DyspepsiaKurnia pralisaPas encore d'évaluation
- Gupta Malhotra 2015Document9 pagesGupta Malhotra 2015Kurnia pralisaPas encore d'évaluation
- Mejdd 9 33Document6 pagesMejdd 9 33Kurnia pralisaPas encore d'évaluation
- Chapter IIDocument29 pagesChapter IIKurnia pralisaPas encore d'évaluation
- Association Between Noise Pollution and Prevalent Ischemic Heart DiseaseDocument9 pagesAssociation Between Noise Pollution and Prevalent Ischemic Heart DiseaseKurnia pralisaPas encore d'évaluation
- STAGING Lung CarcinomaDocument45 pagesSTAGING Lung CarcinomaKurnia pralisaPas encore d'évaluation
- Original Article: Comparative Evaluation of Iron Deficiency Among Obese and Non-Obese ChildrenDocument7 pagesOriginal Article: Comparative Evaluation of Iron Deficiency Among Obese and Non-Obese ChildrenKurnia pralisaPas encore d'évaluation
- So Boka 2017Document7 pagesSo Boka 2017Kurnia pralisaPas encore d'évaluation
- Tung 2016Document27 pagesTung 2016Kurnia pralisaPas encore d'évaluation
- Non-Alcoholic Fatty Liver DiseaseDocument15 pagesNon-Alcoholic Fatty Liver DiseaseKurnia pralisaPas encore d'évaluation
- Introduction To Pharmacology AntibioticDocument15 pagesIntroduction To Pharmacology AntibioticZaira Reine SantosPas encore d'évaluation
- Contemporary Chinese Pulse Diagnosis A Modern InteDocument8 pagesContemporary Chinese Pulse Diagnosis A Modern InteAnkit JainPas encore d'évaluation
- Bell''s PalsyDocument54 pagesBell''s Palsywahyu_sitaPas encore d'évaluation
- MCQ Anaethesia Posting Group 4 2014Document4 pagesMCQ Anaethesia Posting Group 4 2014Law YouPas encore d'évaluation
- Pulmonary Catheter Learning Package PDFDocument36 pagesPulmonary Catheter Learning Package PDFnisar khanPas encore d'évaluation
- 1 4927329208029413644 PDFDocument578 pages1 4927329208029413644 PDFWaseem UllahPas encore d'évaluation
- Application LetterDocument1 pageApplication LetterNina SatimbrePas encore d'évaluation
- LESSON 2-3 HealthDocument20 pagesLESSON 2-3 HealthKalabit PengePas encore d'évaluation
- Meniscus Injuries: Uhuebor David Mbbs (Lagos)Document23 pagesMeniscus Injuries: Uhuebor David Mbbs (Lagos)Uhuebor DavidPas encore d'évaluation
- Addendum Temocillin Breakpoints and AST 2020Document3 pagesAddendum Temocillin Breakpoints and AST 2020Marcelo UGPas encore d'évaluation
- Death & Dying: and How We Cope With Grief and LossDocument18 pagesDeath & Dying: and How We Cope With Grief and Losscarlos alemanPas encore d'évaluation
- Chapter 13Document6 pagesChapter 13Teehee Jones100% (1)
- Damage Control Orthopaedics, EvolvingDocument17 pagesDamage Control Orthopaedics, EvolvingAzmi Farhadi100% (1)
- ManilaDocument17 pagesManilaSarah Jean TraballoPas encore d'évaluation
- Prescribing For The ElderlyDocument8 pagesPrescribing For The ElderlykarladeyPas encore d'évaluation
- Hyperbaric Oxygen TherapyDocument7 pagesHyperbaric Oxygen Therapy18juni1995Pas encore d'évaluation
- Kesehatan Indonesia. 2016.: Daftar PustakaDocument2 pagesKesehatan Indonesia. 2016.: Daftar PustakaSiti Raudatus SolihahPas encore d'évaluation
- Health Psychology An Introduction To Behavior and Health 9th Edition Brannon Test BankDocument25 pagesHealth Psychology An Introduction To Behavior and Health 9th Edition Brannon Test BankJosephWilliamsinaom100% (9)
- Hipaa FillableDocument2 pagesHipaa FillableRameezNatrajanPas encore d'évaluation
- B32C08 Lab Report ProformaDocument13 pagesB32C08 Lab Report Proformajtoh22Pas encore d'évaluation
- AKI7Document14 pagesAKI7Kholida NabilaPas encore d'évaluation
- A Brief Sample Content of The " PACING THE PACES Tips For Passing MRCP and Final MBBS"Document24 pagesA Brief Sample Content of The " PACING THE PACES Tips For Passing MRCP and Final MBBS"Woan Torng100% (2)
- Daftar Atc DDD Antibiotik Who 2018Document14 pagesDaftar Atc DDD Antibiotik Who 2018tri tanayawatiPas encore d'évaluation
- Pharmaceutical Pakistan PPT 2019Document20 pagesPharmaceutical Pakistan PPT 2019Syed Haider Ali50% (2)
- Journal ReadingDocument3 pagesJournal ReadingRachelle Anne LetranPas encore d'évaluation
- TrepDocument50 pagesTrepMiguel Adrian GaonaPas encore d'évaluation
- Electrolyte Disturbances Causes and ManagementDocument19 pagesElectrolyte Disturbances Causes and Managementsuci triana putriPas encore d'évaluation
- Case Report: Severe Vitamin B12 Deficiency in Pregnancy Mimicking HELLP SyndromeDocument5 pagesCase Report: Severe Vitamin B12 Deficiency in Pregnancy Mimicking HELLP SyndromeSuci Triana PutriPas encore d'évaluation
- 2020 WHO Global Tuberculosis ReportDocument232 pages2020 WHO Global Tuberculosis Reportsana shakeelPas encore d'évaluation
- IMCI Q&A For Board ExamDocument12 pagesIMCI Q&A For Board Exammale nursePas encore d'évaluation


![[03241750 - Acta Medica Bulgarica] Extraintestinal Manifestations and Intestinal Complications in Patients with Crohn's Disease_ Associations with Some Clinico-Laboratory Findings, Immunological Markers and Therapy.pdf](https://imgv2-1-f.scribdassets.com/img/document/472637710/149x198/2a81753cb8/1597598960?v=1)