Académique Documents
Professionnel Documents
Culture Documents
12.anaesthesia MSQ
Transféré par
vamshidhTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
12.anaesthesia MSQ
Transféré par
vamshidhDroits d'auteur :
Formats disponibles
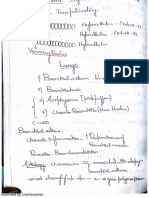
TOPIC 1: LOCAL ANESTHETIC ANAESTHESIA 1
TOPIC 1: LOCAL ANESTHETIC • Remember that while most local anaesthetics cause
vasdilatation,
1. True about EMLA: Cocaine is one of the rare examples of local
A. Can be used for intubation anaesthetic which causes vasoconstriction’
B. Mixture of local anesthesia • Pocaine, Chlorprocaine and Lidocaine all cause varodilation.Q
C. Faster acting
D. Used in children 6. Longest acting L.A
B&D A. Bupivacaine
..........(PGI - DEC 2006) B. Tetracaine
C. Xylocaine
• EMLA (Eutectic mixture of 2.5% Lidocaine base and 2.5%. D. Procaine
Prilocaine base) is a topial anaesthetic B
formulation, widely used for cutaneous analgesia ..........(AIPGMEE - 1994)
through intact skin.
• The preparation should be applied under an occlusive 7. Nerve Fibre affected by local anesthesia first
bandage for 45-60 minutes to obtain A. Type A
effective cutaneous anaesthesia. B. TypeB
• Uses : C. Type C
to decrease pain a/w percutaneous insertion of I:V. needles D. Type
and cannulas. C
- Skin grafting procedures. .........(AIPGMEE - 1995)
- in neonates or in needle phobics.
- Newborn circumcision. Susceptibility Most Intermediate Least
to susceptible susceptible
2. Which of the following is not an amide:
A. Lidocaine Hypoxia B A C
B. Procaine Pressure A B C
C. Prilocaine
D. Etidocaine Local C B A
B Anesthetics
..........(AIIMS PGMEE NOV - 2003)
Amide linked Local anaesthetics 8. Shortest acting local anaesthetic agent is:
Lidocaine A. Procaine
Bupivacaine B. Leidocaine
Dibucaine C. Tetracaine
Prilocaine D. Bupivacaine
Ropivacaine A
Ester linked local anaesthetics ..........(AIPGMEE - 1997)
Cocaine
Procaine Procaine
Chlorprocaine Duration of action of v arious anaesthetic agents in
Tetracaine descending order are :
Benzocaine Dibucaine (Cinchocaine)>Tetracaine (amethocaine) >
Bupivacaine > Lidocaine > Procaine
3. Which one of the following local anesthetics belongs Amongst the choices provided procaine is the shortest acting.
to the ester group?
A. Procaine Other commonly asked questions on local anaesthesea :
B. Bupivacaine • Safest LA agent – Prilocaine
C. Lignocaine • Longest acting LA – Dibucaine (Cinchocaine)
D. Mepivacaine • Shortest acting LA – Chlorprocaine
A • Best L.A. for Regional block – Bupivacaine
..........(AIPGMEE - 2006), AIPGMEE - 2007 • Only naturally occurring LA-Cocaine
• Only LA agent which causes vasoconstriction – Cocaine
5. Which of the following local anaesthetics causes (Rest are vasodilators)
vasoconstriction:
A. Procaine 9. All of the following are example of amide linked local
B. Lidocaine anaesthetics except:
C. Cocaine A. Lidocaine
D. Chlorprocaine B. Procaine
C C. Bupivacaine
..........(AIPGMEE - 1999), AIPGMEE – 1998 D. Mepivacaine
PGI - 1997 – Dec, AIIMS PGMEE - DEC 1997 B
Cocaine ..........(AIPGMEE - 1998)
HELP LINE NO. 9391567707
TOPIC 1: LOCAL ANESTHETIC ANAESTHESIA 2
12. About lidocatne, all are true except: - Restoration of haemodynamics with IVF & cardiac
A. LA effect massage if required.
B. Cardiac arrhythmia - Prevention of metabolic acidosis with sodium bicarbonate.
C. Ester - Prevention or early treatment of seizure activity
D. Acts on mucous membrances with Benzodiazepines.
C - Inotropic support with Atropine, Epinephrine, Dopamine
..........(PGI - 1998 - Dec) & Calcium chloride.
Defibrillation, Antiarrythmic agents like Amiodarone.
• Lidocaine is AMIDE linked LA
good for both surface application and injections. 16. True about local anaesthetic agents
• Lidocaine has little effect on contractility and conductivity, A. Duration depends on protein binding
it abbreviates ERP, and is used as ANTI- ARRHYTHMIC. B. Potency depends upon lipid solubility
Overdose of lidocaine can cause-cardiac arrhythmias, - C. LA with low PK is more active
Decrased BP, convulsion, resp.arrest, coma etc. D. Higher dose produces more block
E. Signal transduction blockade
13. True statements about local anaesthesia: ALL
A. It inhibits the generation of action potential. ..........(PGI - JUNE 2004)
B. Unmyelinated thin fiber are most susceptible than
myelinated large fibers. • Local anaesthetics are chemical compounds which are
C. Toxicity is reduced by addition of vasoconstrictor. capable of reversibly inhibiting the propagation of
D. Blocks all modalities of sensation at the same time impulses in nerve cells.
A • Three major factors determine the conduction-blocking
..........(.PGI - DEC 2003) profile of a LA in an isolated nerve preparation :
Lipid solubility, protein binding & PK.
• Local anesthesia (LA) produce conduction blockade of
neural impulses by preventing passage of sodium ions LA agents which are highly lipid-soluble are able to penetrate
through ion selective sodium channels in nerve membranes the neuronal membrane & gain access to their site of
thus inhibiting generation of Action potential. It do not action more readily than less lipid-soluble agents & is
alter the resting transmembrane potential or threshold reflected biologically in their increased potency.
potential. Duration of action of LA appear to be influenced primarily by
• Myelin increases conduction velocity and makes the nerve their protein-binding capacity, agents with the longest
membrane more susceptible to LA. duration of action (Bupivacaine & Ropivacaine) are
• Large myelinated fibers are more sensitive to LA than small highly protein bound.
unmyelinated fibers.
• Preganglionic type ‘B’ fibers are more readily blocked by • LA with PK closer to physiological PH will have more
LA than any fiber. rapid onset than those with higher PK.
• In practice, the sequence of nerve block by LA are : • Onset of conduction block by LA depends on the dose or
Autonomic -> Sensony -» Motor concentration of LA.
• Addition of vasoconstrictors like adrenaline to LA • The physiological changes during laryngoscopy & intubation
- Produces : decreased absorption and reduces toxicity are :
- Prolongs analgesic activity. CVS :
Hypertension, Tachycardia & dysrhythemias & bradycardia
14. Local anaesthesia acts by in children.
A. Na+ channel inhibition Respiratory :
B. Ca+ channel inhibition Increased a irway reactivity & lar yngospasm &
C. Mg*4 channel inhibition bronchospasm.
D. K+ channel inhibition CNS : Stimulates CNS activity with Increased in EEG activity,
A CMR (cerebral metabolic rate), cerebral blood flow, &
..........(PGI - JUNE 1997) thus ICP & IOP.
Abdomen : Increased in intraabdominal pressure with
Local anaesthetic drugs exert their effect by binding to increased risk of aspiration in patients with full stomach.
the internal mouth of the sodium channel.
17. Short acting L.A:
15. Drugs used in case of local anesthetic toxicity: A. Procaine
A. Antiarrhythmic B. Lignocaine
B. IV fluids C. Bupivacaine
C. Anticonvulsant D. Tetracaine
D. O2 A
A ..........(PGI - June -2000)
..........(PGI - JUNE 2006)
Procaine, is a short acting local anaesthetic duration of nerve
Emmergency treatment of local anaesthetic toxicities are: block is 30-60 minutes
- Facemask oxygenation.
HELP LINE NO. 9391567707
TOPIC 2: KETAMINE ANAESTHESIA 3
18. True about local anaesthetic: Ester linked local aneasthetics produce allergic reaction
A. Cocaine acts by decreasing norepinephrine because they are first metabolized to PABA derivative.
B. Act by decreasing sodium entry into the cell These metabolites are responsible for the allergic reaction
C. Lignocaine is a amide caused by ester linked local anaesthetics.
D. Dibucaine is drug of choice for epidural anaesthesia Out of the given options only Benzocaines is an ester
B&C linked local anaesthetic,
..........(PGI - June -2001)
22. L.A. causing Methaemoglobinemia
19. Order of sensitivity of nerve fibres to Local A. Procaine
anaesthetic in decreasing order: B. Prilocaine
A. Pain (C and A-delta), Preganglionic sympathetic B., motor C. Bupivacaine
B. Preganglionic sympathetic B., Pain (C and A- delta), sensory, D. Cocaine
motor B
C. Pain (C and A-delta), sensory, motor, Preganglionic ..........(AIPGMEE - 1994)
sympathetic B
D. Preganglionic sympathetic B. sensory, motor, Pain (C and • Prilocaine is an amide linked local anaesthetic.
A-delta) • Methamoglobinemia may be seen sometimes with use of
B
prilocaine.
..........(AIIMS PGMEE - MAY 2008)
• One of the degrading products of prilocaine has potential
of causing methamoglobirumia Congenital or acquired
Fiber Sensory Modality Diamete Condu Local Myelinat methamoglobinumia are thus contraindications to the use
Type Classifi Served r (mm) ction Anestheti ion of Prilocaine
cation {mis) c
Sensitivit
y TOPIC 2: KETAMINE
Aa Motor 12-20 70-120 + Yes
Aa T ype la Proprio 12-20 70-120 ++ Yes 23. Which of the following increases intracranial tension
ception A. Thiopentone
Aa T ypelb Proprio 12-30 70-120 ++ Yes B. Ketamine
ception
C. Halothane
AP T ype II T ouch 5-12 30-70 ++ Yes
pressur
D. Propofol
e B
Proprio ..........(AIIMS PGMEE - SEP 1996)
ception
Ay Motor 3-6 15-30 ++ Yes
(muscle 24. Which of the following causes hallucination ;
spindle) A. Ether
A5 T ype-III Pain 2-5 12-30 +++ Yes B. Halothane,
Cold C. Ketamine
tempera
ture D. Thiopentone
T ouch C
B Pregang <3 3-14 ++++ Some ......(AIIMS PGMEE - SEP 1996), AIIMS PGMEE - DEC 1997
lionic
autono
mic 25. Best anaesthesia for status Asthmaticus is
fibers A. Thiopentone
C T ype IV Pain 0.4-1-2 05-2 ++++ No B. Ether
Dorsal Warm
root and
C. Ketamine
cold D. N2O
tempera C
ture
T ouch
..........(AIIMS PGMEE - FEB - 1997)
C Postgan 0.3-1.3 07-2.3 ++++ No
Sympat glionic Ketamine
hetic sympat • Ketamine causes Sympathetic stimulation which leads to
hetic
fibers Bronchodilatation so it is the anaesthetic of choice
for Status Asthmaticus.
• It is more potent Bronchodilator than Halothane
21. Which of the following local anesthetic is most likely • Muscle Relaxant of Choice in Asthma —Pancuronium
to produce an allergic reaction • Muscle Relaxant to be avoided in Asthma
A. Prilocaine • Metacurine & Succinyl choline (d/t secretion of histamine)
B. Ropivacaine
C. Etidocaine 26. Anaesthetic agent causing raised intracranical tension
D. Benzocaine is:
D A. Etoruidal
..........(AIIMS PGMEE - MAY 2004)
HELP LINE NO. 9391567707
TOPIC 2: KETAMINE ANAESTHESIA 4
B. Ketamine • Ketamine is used as anaesthetic where maintenance
C. Ether of blood pressure is important e.g. in states of shock
D. Nitrous Oxide
B Ketamine produces profound analgesia
..........(AIIMS PGMEE - JUNE - 1997)
Ketamine
• Ketamine is an analogue of phencyclidine and therefore it
causes hallucinations.
• Ketamine.
• It causes Dissociative Anaesthesia*.
It causes sympathetic stimulation which leads to
• Cardiac stimulation —increase O2 demand*
• Bronchodilation —
• it is anesthetic of choice for Bronchial Asthma
• Increase all pressure
• B.P.,I.C.T. ,I.O.P.
• It causes muscular rigidity*
Ketamine
• It increases salivation so Atropine is always given with
• Ketamine causes an increase in all pressure viz
it*. intracranial pressure
Intraocular pressure
27. An unconscious pt. of head injury comes in casualty. Blood pressure
Examination shows raised intracranial pressure. It does not cause muscle Relaxation
Which anesthetic agent is contra- indicated: Ketamine induces dissociative anaesthesia : profound
A. Propofol analgesia, immobility, amnesia with light sleep and
B. Ketamine felling of dissociation Q from ones own body and the
C. Etomidate surrounding.
D. Thiopentone sodium
B It forms the answer to a set of questions. A quick revision
..........(AIIMS PGMEE JUNE - 1999) therefore :
AIPGMEE - 2000 , AIPGMEE – 1998 • Anaeshesia of choice in shock/hypotension : Ketamine
PGI - JUNE 1997, PGI - June –1999 • Anesthetic associated with increase in muscle tone :
AIIMS PGMEE - MAY 2006, AIIMS PGMEE - DEC 1998 ketamine
• Anaesthetic which does not abolish reflexes : Ketamine
Ketamine • Profound analgesia is seen with : Ketamine
• Ketamine causes increase in all pressure of body fluids - • Anaesthetic which increases cardiac oxygen demand :
• Increased ICT Ketamine
• Increased IOT • Anaesthetic of choice in Bronchial Asthma : Ketamine
• Increased B.P. • Anaesthetic which is associated with emergence delerium
• Therefore it is not used in raised ICT and IOT as it may and hallucinations : ketamine
increase the pressure to morbid levels.
• K etamine, like Phencyclidine, is primarily a non- Anaesthetic causing increased CT Anaesthetic which increase
IOT
competitive antagonist of the NMDA receptor,which
• Ketamine • ketamine
opens in response to binding of the neurotransmitter
• Halothane • Nitrous oxide
glutamate . This NMDA receptor mediates the
• Scoline
analgesic (reduction of pain ) effects of ketamine at
• Cyclopropane
low doses
Anaesthetics causing decreased ICT Anaesthetic which
• Ketamine causes bronchodilation decreased IOT
• It is primarily used for the induction and maintenance of • Theopentone • Morphine
general anesthesia, usually in combination with some • Droperidol • Thiopentone
sedative drug. • Althesin • Halothane
• Other uses include sedation in intensive care, analgesia 29. Dissociative anesthesia is
(particularly in emergency medicine), and treatment of A. Ketamine
bronchospasm. B. Halothane
• Ketamine C. SCH
• The injection of a therapeutic dose of Ketamine produces D. d-TC
dissociative anaesthesia A
• Ketamine is a phenycyclidine analogue, it produces ..........(AIPGMEE - 1996)
Hallucinations AIIMS PGMEE - NOV 2006
HELP LINE NO. 9391567707
TOPIC 2: KETAMINE ANAESTHESIA 5
30. Maximum analgesic action is seen with: maintained i.e. - Systemic vascular resistance should be
A. Catecholamine increased pulmonary vascular resistance should be
B. Propofol decreased.
C. Ketamine
D. Thiopentone • This will help to reduce the shunt in cyanotic heart
C diseases.
..........(AIPGMEE - 1997) , PGI - 2001 - Dec • Therefore the goal of anaesthetic management in patients
with cyanotic heart disease is to maintain
Ketamine intravascular volume or systemic vascular resistance.
Ketamine is a rapidly acting parenteral anaesthetic, causing
Sedation and Profound analgesia besides other features. • Anaesthetic drugs and procedures which increase
Analgesia is a marked feature and extends into the systemic vascular resistance and decrease pulmonary
postoperative period. vascular resistance should be preferred.
32. Which drug of anaesthetics causes hallucination: Ketamine (intramuscular or intravenous) is commonly used
A. Ketamine as an induction agent in cyanotic heart disease because it
B. Trilene
maintains or increases systemic vascular resistance and it
C. Halothane
does not appear to increase pulmonary vascular resistance
D. Trichloroethylene
(PVR) in children.
A
So the use of ketamine will decreased right to left shunting.
..........(AIPGMEE - 1998)
“Dreaming, Hallucinations and delerium are seen with • Halothane’s safety in patients with cyanotic heart disease
ketamine” - and good cardiac reserve is well established
• Patients with milder degrees of Right to left shunting can
37. With regard to Ketamine, all of the following are also tolerate inhalational induction with halothane
true except - because Halothane tends to maintain systemic vascular
A. It is a direct myocardial depressant resistance (systemic arterial vasodilation is minimal
B. Emergence phenomena are more likely if anticholinergic with halothane).
premedication is used • But Remember, that halothane induction is not used in
C. It may induce cardiac dysarrythmias in patients receiving very young patients (because it is pungent and it is slow
tricyclic antidepressants acting).
D. Has no effect on intracranial pressure • Halothane is also not preferred for patients with low CO.
D
..........(AIIMS PGMEE - NOV 2005) Important facts which should always be taken care of while
anaesthetizing a patient with right to left shunt.
38. A 5 year old child is suffering from cyanotic heart • The right to left shunting tends to slow the uptake of
disease. He is planned for corrective surgery. The inhalational anaesthetics.
induction agent of the choice would by - • In contrast it may accelarate the onset of intravenous
A. Thiopentone agents.
B. Ketamine
Nitrous oxide is usually used with inhalational induction (does
C. Halothane
not increase PVR)
D. Midazolam
B
41. Which of the following increases cerebral oxygen
..........(AIIMS PGMEE - NOV 2005)
consumption
• Cyanotic heart disease have predominantly Right to left A. Propofol
shunt i.e. blood flows directly from right ventricle to left B. Ketamine
ventricle bypassing the pulmonary circulation. C. Thiopentone
• This produces cyanosis as the systemic blood coming to D. Alfentanyl
the right ventricle cannot be oxygenated by the lung. B
• Note that in right to left shunting , the fixed ..........(AIIMS PGMEE - NOV 2007)
component is determined by the severity of the right
ventricular obstruction while the variable component • This has been discussed so many times that ketamine
depend upon difference between systemic vascular increases cerebral oxygen consumption. It increases
resistance (SVR) and pulmonary vascular resistance (PVR) the intracranial tension too.
• Thiopentone and propofol decrease cerebral oxygen
• If the right ventricular obstruction remains same greater consumption.
the systemic vascular resistance the lesser the shunt, Alfentanyl is an opioid and opioids in general reduce cerebral
• So in right to left shunts a favourable ratio of systemic oxygen consumption, cerebral blood flow and
vascular resistance to pulmonary resistance should be intracranial pressure.
HELP LINE NO. 9391567707
TOPIC 3: SUCCINYLCHOLINE ANAESTHESIA 6
TOPIC 3: SUCCINYLCHOLINE
44. Malignant hyperthermia is seen with
A. Gallamine
B. Lignocaine
C. Succinylcholine (Sch)
D. Bupivacaine
C
..........(AIIMS PGMEE - MAY - 1993)
• Drug causing malignant hyperthermia 47. Administration of Scoline produces dangerous
1) Sucinyl choline (Most common) hyperkalemia in:
2) Halothane A. Paraplegia
3) Lidocaine B. Fracture Femur
4) Mepivacaine C. Raise intracranial pressure
5) Methoxyflurane D. Acute renal failure
6) Gallamine A
7) Ethylene ..........(AIIMS PGMEE JUNE - 1999)
8) Ethyl chloride
9) Trichlorethylene
45. Post anaesthetic muscle soreness is caused by
A. Gallamine
B. d-Tubocurarine
C. Suxamethonium
D. Xylocaine
C
..........(.AIIMS PGMEE - NOV - 1993)
• Suxamethonium causes muscle pain -
• This pain is influenced by age, sex and physical fitness.
i) Pain is more common in women
Paraplegia
ii) More common in middle age than extreme age.
• “Hyperkalemia caused by Scoline is insignificant except
iii) Less common in muscularly fit
after—>
• The longer the interval b/w injection of barbiturate and • paraplegia
suxamethonium the more intense the pain. • burns &
• tetanus”
Prevention of muscle pain caused by suxamethonium • Other adverse effect of Scoline:
1) Precurairzation - Nondepolarizing relaxants are given 3 1. Malignant Hyperthermia
minutes before suxamethonium injection 2. Muscle Fasciculations
2) lignocaine injection before suxamethonium
48. Hyperkalemia due to Scoline is seen in all except:
Other adverse effects of Suxamethonium - A. Muscular Dystrophy
1) Hyperkalemia B. Crush injury
2) Raised intraocular pressure C. Abdominal Sepsis
3) Malignant hyperpyrexia D. Burns
4) Dystrophia myotonica none
..........(AIIMS PGMEE JUNE - 2000)
5) CVS - Bradycardia and cardiac arrest
None of the above
46. Regarding myasthenia, what is true about sensitivity • Hyperkalemia d/f Scoline is seen in following
to curare and succinylcboline Curare - Succinylcholine: conditions:
A. Decreased Increased • Trauma
B. Decreased Normal • Burns
C. Increased Increased • Muscle disease such as myopathy
D. Increased Decreased • Motor neuron disease
D • Muscular Dystrophy
..........(AIIMS PGMEE - NOV - 1993) • denervation
• Spinal Cord transection
In myaesthenia gravis the muscles affected by myaesthenia • Tetanus
gravis are hypersensitive to non depolarizing relaxants • Congenital cerebral palsy
like curare but they are resistant to succinyl choline • Chronic Arterial insufficiency
and decamethonium (depolarizing blockers) • Severe Intra Abdominal infection
HELP LINE NO. 9391567707
TOPIC 3: SUCCINYLCHOLINE ANAESTHESIA 7
Suxamethonium –ADVERSE EFFECTS Succinyl choline is short acting muscle relaxant as it is rapidly
• Side effects include fasciculations, muscle pains, acute metabolized by pseudocholinestrase secreted both by liver
rhabdomyolysis with hyperkalemia, transient ocular and plasma.
hypertension, and changes in cardiac rhythm In liver failure ,this enzyme is reduced ,so succinylcholine
including bradycardia, cardiac arrest, and ventricular concentration is increase during liver failure and is also
dysrhythmias. maintained for greater periods.
• In children with unrecognized neuromuscular diseases, a
single injection of suxamethonium can lead to massive The duration of paralysis produced by succinylcholine is
release of potassium from skeletal muscles with cardiac increased during liver failure but this does not require
arrest. Succinylcholine to be contraindicated in liver failure.
• Suxamethonium does not produce unconsciousness or
anesthesia, and its effects may cause considerable Conditions where succinyl choline use is contra
psychological distress while simultaneously making it indicated due to hyperkalemia caused by succinyl choline
impossible for a patient to communicate. are-
• For these reasons, administration of the drug to a (a) Tetanus (h) Massive trauma
conscious patient is strongly contraindicated , except (b) Stroke (i) Prolonged body immobilization
in necessary emergency situations. (c) Closed head injury (j) GB. syndrome
(d) Myopathy (k) Spinal cord injury
49. In a young patient who had extensive soft tissue (e) Burn (L) Paraplegia
and muscle injury, which of these muscle relaxants (f) Acidosis (M) Severe intraabdominal infection
used for endotracheal intubation might lead to
cardiac arrest: 52. A six-year old boy is scheduled for examination of
A. Atracurium. the eye under anaesthesia. The father informed that
B. Suxamethonium. for the past six months the child is developing
C. Vecuronium. progressive weakness of both legs. His elder sibling
D. Pancuronium had died at age of 14 years. Which drug would you
B definitely avoid during the anaesthetic management
..........(.AIIMS PGMEE MAY - 2003) ?
A. succinylcholine
Hyperkalemia produced due to suxamethonium is B. thiopentone
aggravated in muscular diseases. The hyperkalemia so C. nitrous oxide
produced causes cardiac arrest. D. vecuronium
A
..........(AIIMS PGMEE NOV - 2002)
Weakness of the legs indicate that the boy is suffering from
myopathy {most probably Duchenes muscular dystrophy).
Succinyl choline use is contra indicted in myopathy due to
increased risk of hyperkalamia.
50. Which muscle relaxant increases intra cranial
pressure?
A. Mivacurium
B. Atracurium
C. Suxamethonium
D. Vecuronium
C
..........(AIIMS PGMEE NOV - 2002)
Succinylcholine (or Suxamethonium) causes increase in -
(a) Intracranial pressure
(b) Intraocular pressure 53. A young boy undergoes eye surgery under day case
(c) Intragastric pressure anesthesia with succinyl choline and propofol and
after 8 hours he starts walking and develops muscle
51. The use of succinylcholine is not contraindicated in pain. What is the likely cause?
A. tetanus A. Early mobilization
B. closed head injury B. Due to the effects of eye surgery
C. cerebral stroke C. Succinyl choline
D. hepatic failure D. Propofol
D C
..........(AIIMS PGMEE NOV - 2002) ..........(AIPGMEE - 2007)
HELP LINE NO. 9391567707
TOPIC 3: SUCCINYLCHOLINE ANAESTHESIA 8
Muscle pain or Myalgia is a common adverse effect of succinyl Phase I block :• results from persistant depolarizatin of
choline muscle end plate.
It is common in women and young to middle aged adults and • preceded by muscle fasciculation
in those who are ambulant shortly after surgery • potentiated by isoflur ane,
The young adult in question has recieved succinylcholine and antichlinesterase, magnesium an lithium.
is now ambulant after surgery. Phase IIblock:• results from desensitization of receptor
He is classically presenting with myalgia secondary to Ach
to succinyl choline use. • resemble block produced by TC and is
partially reversed by anticholinesterases.
Myalgia (Muscle Pain after succinyl chnline
• The incidence of muscle pain after administration of succinyl 56. Muscle pain after anaesthesia is caused by:
choline varies from 0.2 % to 89% A. Vecuronium
B. D tubocurare
It occurs more frequently in : C. Suxamethonium
• Women /young to middle aged adults D. All
• After minor surgery (day case) C
..........(PGI - 1999 - Dec)
In those who are ambulatory shortly after surgery
(rather than bedridden patients) • Muscle pain after anaesthesia i s caused by
• Pain is believed to be secondary to damage produced in SUXAMETHONIUM- pain is influenced by age, sex and
muscle by unsynchronized contraction of adjacent muscle physical fitness.
fibres just prior to the onset of paralysis.
• Myalgia may be prevented (or attenuated) by a small dose Important side effects of suxamethonium
of non depolarizing neuro muscular block few minutes - Prolonged Apnea
before succinylcholine administration - Increased K+
- Increased IOP
54. Agent causing malignant hyperthermia - Muscle pain
A. Succinyl Choline - Malignant hyperpyrexia
B. Dantroline - Dystrophia Myotonica
C. gallamine Bradycardia, cardiac arrest P-K reaction.
D. Ketamine
A 57. Drugs metabolized by cholinesterase:
..........(AIPGMEE - 1995) A. Succinycholine
B. Mivacurium
Malignant hyperthermia is an autosomal dominant genetic C. Esmolol
disorder of skeletal muscle that occurs in susceptible D. Remifentanyl
individuals. It is precipitated by drug administeration, E. Ketamine
particularly: A
1. Succinyl choline ..........(PGI - DEC 2004)
2. Halothane
3. Fluoranes : sevofluorane, isofluorane etc 58. True about scoline are following except:
4. Amide local analgesics eg lignocaine A. Fasciculations
5. Phenothiazines B. ICT increases
6. Tricyclic antidepressant C. Non Depolarising neuro muscular blocker
7. Monoamine oxidase inhibitors D. Short acting muscle relaxant
A&B
The drug of choice for treatment of malignant hyperthermia ..........(PGI - JUNE 1997)
is Dantrolene
59. Myaesthenics are resistant to following muscle
55. Fasciculation are known to be caused by: relaxant:
A. Suxamethonium
A. Suxamethonium
B. Pancurium
B. Vecuronium
C. Atracuronium
C. Pancuronium
D. Vecuronium
D. Atracumium
A
A
..........(PGI - June -2000)
..........(AIPGMEE - 1997)
• Myasthenic patients are resistant to decamethonium and
Suxamethonium
suxamethonium.
Suxamethanium or other depolarizing blockers depolarize
Muscles affected by myasthenia gravis are hypersensitive to
muscle end plates by opening Na+ channels and initially
non depolarizing muscle relaxants.
produce twitching and fasciculations because in the
focally innervated mammalian muscle stimulation is
60. Which of the following is the neuromuscular blocking
transient.
agent with the shortest onset of action?
Neuro muscular blockage by depolarizing agents can be divided
A. Mivocurium
into two phases:
B. Vecuronium
HELP LINE NO. 9391567707
TOPIC 3: SUCCINYLCHOLINE ANAESTHESIA 9
C. Rapacuronium
D. Succinylcholine
D
..........(AIIMS PGMEE - MAY 2006)
* Shortest acting muscle relaxant (both depolarizing and
non depolarizing) -
• Shortest acting non depolarizing muscle relaxant
Succinylcholine --> Mivacurium
Muscle relaxants Onset (min.) Duration (min.)
Succinyl choline 1-1.5 3-6
Mivacurium 2-4 12-20
Rocuronium 1-2 25-40
Vecuronium 2-4 30-60
Atracurium 2-4 20-35
Cisatracurium 3-6 20-40
Piperacuronium 2-4 50-100
d-Tubocurarine 4-6 30-60 • Succinylcholine rele ases a metabolite —>
Pancuronium 4-6 40-80 Succinvlmonocholine
Doxacurium 4-8 60-120 This metabolite causes excitation of the cholinergic
receptors in the sinoatrial node, resulting in bradycardia.
61. All of the following statements are incorrect about • Children are particularly susceptible to succinylcholine
the treatment of prolonged suxamethonium apnoea induced bradycardia.
due to plasma cholinesterase deficiency (after a single • In adults bradycardia is commonly seen when second dose
dose of suxamethonium) except- of succinylcholine is administered.
A. Reversal with incremental doses of neostigmine Prevention against succinvlchol ine induced
B. Continue anaesthesia and mechanical ventilation till bradvcardia.
recovery “Intravenous atropine is often given prophylactically in
C. Transfusion of fresh frozen plasma children an d always before a sec ond dose of
D. Plasmapheresis succinychotine”.
B
..........(AIIMS PGMEE - NOV 2004) 63. Phase II block is seen in
A. Halothane
Suxamethonium is a very short acting muscle relaxant. B. Ether
It has very rapid onset of action and very short duration of C. D-tubocurare
action D. Suxamethonium
Reason D
Rapid onset of action ..........(AIIMS PGMEE - DEC 1998)
---> It is highly lipid soluble
Short duration of action Suxamethonium
---> It is rapidly metabolized by pseudocholinesterase • Suxamethonium causes Biphasic Block.
But sometimes suxamethonium intake is associated with • With dose more than 500mg.
prolonged apnoea. The reason are - • Phase I block ---> Features of classical depolarization
- Atypical serum cholinesterase block
- Low level of serum cholinesterase • Phase II block ---> Results from desensitization of
- Dehydration and electrolyte imabalance receptor to a ctylcholine and
resembles competitive block and
An overdose of relaxant drug partially antagonized by anticholinesterase.
Excessive formation of succinylcholine monocholine phase II
block
There are tw o phases to the blocki ng effect of
- Managemen t of prolonged ap nea after
suxamethonium
suxamethonium.
Phase 1 block
- The best man agement in this case i s to provide
The first is due to the prolonged stimulation of the
mechanical ventilation, maintain anaesthesia and
acetylcholine receptor results first in disorganized muscle
continue monitoring till muscle function returns to normal.
contractions (fasciculations, considered to be a side
- Transfusion of fresh frozen plasma is beneficial (It
effect), as the acetylcholine receptors are stimulated .
will provide pseudocholinesterase)
On stimulation, the acetylcholine receptor becomes a
62. Bradycardia is common after injection of - general ion channel, so there is a high flux of potassium
A. Midazolam out of the cell, and of sodium into the cell, resulting
B. Succinyl choline in an endplate potential less than the action potential.
C. Dopamine So, after the initial firing, the cell remains refractory.
D. Isoprenaline
B • Phase 1 blockade is potentiated by anticholinesterases
..........(AIIMS PGMEE - NOV 2005) and antagonized by competitive blockers.
HELP LINE NO. 9391567707
TOPIC 4: SPINAL ANAESTHESIA ANAESTHESIA 10
Phase 2 block The manifestation of total spinal analgesia are-
• If the duration of blockade is prolonged however, or if 1. Marked hypotension
the concentration of the blocker is excessive, then phase 2. Apnoea
two blockade occurs in which the pharmacological 3. Dilated pupils
characteristic is that of a competitive inhibition.
Phase 2 blockade is antagonized by anticholinesterases, Management
and potentiated by competitive blockers. Patient should be immediately intubated and 100% O2
should be given I.V. fluids and vasopressors should be given
Why does Acetylcholine cause Hyperkalemia
• The side effect of hyper kalaemia is because the 65. In high spinal anaesthesia what is seen
acetylcholine receptor is propped open, allowing continued A. Hypertension and Bradycardia
flow of potassium ions into the extracellular fluid. B. Hypertension and Tachycardia
• A typical increase of potassium io n serum C. Hypotension and Bradycardia
concentration on administration of suxamethonium is 0.5 D. Hypotension and Tachycardia
mmol per litre, whereas the normal range of potassium is C
3.5 to 5 mmol per litre: a significant increase which results ..........(AIIMS PGMEE MAY - 2001)
in the other side-effects of ventricular fibrillation due to
reduced to action potential initiation in the heart. Hypotension and Bradycardia
• Phase 1 block potentiated by anticholinesterases and Effect of spinal block on cardiovascular system
antagonized by competitive blockers.
• Phase 2 block antagonized by anticholinesterases and
potentiated by competitive blockers.
Vessels Heart
Drug interactions
1. Potentiation of the neuromuscular blockade caused by Vasodilation of arterioles, resistance Decrease inotropic Action
the aminoglycoside antibiotics , and tetracyclines. vessels and venous capacitance Decrease chronotropic Action
2. Do not potentiate the effects of the halogenated vessels (This causes Hypotension)
Increase effective Refractory period
hydrocarbon anesthetics -halothane
Decrease automaticity decrease
3. Lithium in therapeutic concentrations used in the level of catecholamine
treatment of manic disorders can slow the onset and
(This causes Bradycardia)
increase the duration of action of succinylcholine.
66. Following spinal subarachnoid block a patient
TOPIC 4: SPINAL ANAESTHESIA develops hypotension. This can be managed by the
following means except.
64. A patient was administered epidural anaesthesia with A. Lowering the head end
15ml of 1.5% lignocaine with adrenaline for hernia B. Administration of 1000 ml of Ringers lacate before the
surgery. He developed hypotension and respiratory block
depression within 3 minutes after administration of C. Vasopressor drug like methoxamine
block. The commonest cause would be. D. Use of ionotrope like dopamine
A. Allergy to drug administered. A
B. Systemic toxicity to drug administered. ..........(.AIIMS PGMEE MAY - 2003)
C. Patient got vasovagal shock.
D. Drug has entered the sub arachnoid space For spinal subarchnoid block, the anaesthetic agent is injected
D into the subarchnoid space.
..........(.AIIMS PGMEE MAY - 2003) The subarchnoid space contains CSF.
If the head end is lowered, the anaesthetic drug will
Sometimes during epidural analgesia, due to inadvertent move towards the cephalic direction (being heavier than
suparachnoid injection (i.e. the injection enters the CSF). This will increase the level of spinal block and may
subarachnoid space) a condition termed ‘total spinal lead to cardiac & ventilatory failure.
analgesia” is produced. It is produced because large dose (Sympathetic supply of heart comes from T3 to T4; phrenic
of drug which is used in epidural anaesthesia enters the nerve supplying diaphragm arise from C3 to C5)
subarachnoid space.
“Hyperbaric solution of bupivacaine are injected as a ‘single
shot’ into the cerebrospinal fluid, to produce rapidly an
intense blockade, usually within 5 minutes.
Autonomic sympathetic blockade results in hypotension,
necessitating prior intravenous fluid loading and titration
of vasoconstrictor drugs.
If the hyperbaric solution is allowed to ascend too
high, severe hypotension and ventilatory failure occur.
This factor limits the use of spinal anaesthesia to surgery
below the segmental level of T10.”
67. Centrineuraxial (spinal and epidural) anaesthesia is
not contraindicated in-
A. Platelets < 80,000
B. Patient on aspirin
HELP LINE NO. 9391567707
TOPIC 4: SPINAL ANAESTHESIA ANAESTHESIA 11
C. Patient on oral anticoagulants Caudal anaesthesia may be used for perenial operations.
D. Raised intracranial pressure It is not indicated in Lower segment caesarian section.
B Further it is associated with potential risk of penetrating
..........(AIPGMEE - 2007) the fetal head in obstetric practice.
Centrineuraxial anesthesia is not associated with increased
risk with most antiplatelet agents (eg. aspirin Q & NSAJDs).
Contraindications of Centrineuraxial (Spinal /Epidural)
Anesthesia
69. A patient undergoing caesarean section following
prolonged l abour under subarach noid block
developed carpopedal spasm. Lignocaine was used
as anesthetic agent. The most likely diagnosis is:
A. Amniotic fluid embolism
B. Lignocaine toxicity
C. Hypocalcemia
D. Hypokalemia
C
..........(AIPGMEE - 2004)
Absolute Contraindications During prolonged labour, pain from episodic uterine
- Patient’s refusal contractions produces an increase in minute ventilation.
- Patient’s inability to maintain stillness during the needle Hyperventilation thus produced results in development of
puncture (eg. dementia, psychosis) hypocarbia and respiratory alkalosis.
- Raised intra cranial pressure Resulting acute respiratory alkalosis causes intracellular shift
(papilledema, cerebral edema, tumors in posterior fossa, of K+, Na+ & PO4" and reduces free Ca +2 by increasing
suspected subarachnoid Hemorrhage) the protein bound fraction and precipitates
- Severe hypovolemia hypocalcemia.
- Severe stenotic valvular heart disease, the patient may
be unable to compensate for vasodilation because of a Respiratory alkalosis secondary to hvperventilation following
fixed cardiac output. prolonged labour may result in :
- Marked skin sepsis & marked spinal deformity
- Marked coagulopathy, blood dyscariasis or full anticoagulant Neurological Symptoms Symptoms
therapy symptoms secondary to secondary to
hypophosphatemia
secondary to hypocalcemia
Relative contraindications cerebral Muscle weakness
Paraesthesias
- Un coperative patient (may be performed in conjuction vasoconstriction Carpopedal
with GA)
Dizziness Visual spasm
- Pre existing neurological deficit (eg demyelinating lesions).
symptoms Tetany
- All severe & marked diseases in lesser degree i.e. spinal
Syncope Seizure
deformity, sepsis etc.
- Pre eclamptic toxaemia - epidural block has been used Lignocaine toxity is likely to cause hypercalcemia by
with great benefit in this condition, but a platelet count releasing Ca into the blood and hence corpopedal
of less than 100 xlO9 L”1 usually preclude epidural or spasm as a manifestation is unlikely.
subarachnoid block.
- Mildly impaired coagulation 70. Concentration of Lidocaine used in spinal anaesthesia
- Patients with platelet <80000 /ml A. 5%
B. 3%
C. 2%
68. A Lower Segment Caesarean section (LSCS) can be
D. 1%
carried out under all the following techniques of
A
anaesthesia except:
..........(AIPGMEE - 1994)
A. General anaesthesia
B. Spinal anaesthesia Lignococine
C. Caudal anaesthesia
D. Combined Spinal Epidural anaesthesia 5% 4% 0.5%
C Spinal Topically in Eye Epidural
..........(.AIPGMEE - 2005) Anesthesia Anesthesia
HELP LINE NO. 9391567707
TOPIC 4: SPINAL ANAESTHESIA ANAESTHESIA 12
71. Post Spinal Headache can last for • Severe Hypovolemia
A. upto 10 min • Raised ICT
B. upto 10 hours • Infection at site of injection
C. 7-10 days Severe stenotic valvular Heart disease & fixed cardiac output
D. upto 10 months states
C
..........(AIPGMEE - 1994) 75. Spinal anaesthesea should be injected into the space
between:
Post spinal Headache starts in 1st 3 days and lasts for 1- A. T12 – L1
2 weeks B. L1-L2
C. L3 – L4
72. Best way to prevent hypotension during spinal D. L5 – S1
anesthesia C
A. preloading with crystalloids ..........(AIPGMEE - 1997)
B. Mephentermine
C. Dopamine The LA is injected in the subarachnoid space between L 2_3orL
D. Tredelenbug’s position _ , i.e. below the lower end of spinal cord.
3 4
A • The primary site of action is the nerve root in the cauda
..........(AIPGMEE - 1995) equina rather than the spinal cord.
• The level of anaesthesia depends on volume and speed
Hypotension following spinal anaesthesia is due to of injection, specific gravity of drug solution & posture of
blockage of sympathetic vasoconstrictor outflow the patient.
to blood vessels, venous pooling and decreased return • Duration of spinal anaesthesia depends on drug used
to heart. Prevention is by preloading with crystalloids. and its concentration. e
73. Post sipnal headache is due to
A. Meningitis • Autonomic pre-ganglionic fibres are more sensitive
B. Encephaletics and somatic motor fibres less sensitve than somatic sensory
C. CSF leak fibres.
D. Increased ICT (Sympathetic block occurs before para-sympathetic and
C somatic block).
..........(AIPGMEE - 1995)
76. Which is the true statement regarding post-dural
‘Headache is due to seepage of CSF and can be minimized anesthetic headache:
by use of smaller bore needle’ A. Blood patch is the first line of treatment
B. Occurs due to low CSF pressrue
74. In all of the following conditions neuraxial blockade C. Increased incidence with early mobilization of patient.
is absolutely contraindicated, except: D. Use of small guage needle prevents hea
A. Patient refusal A
B. Coagulopathy ..........(PGI - 2001 - Dec)
C. Severe hypovolemia
D. Pre-existing neurological deficits 77. True about epidural anaesthesia in pregnancy:
D A. Given through subarachnoid space.
..........(AIPGMEE - 2003) B. Increases cardiac output.
C. Decreases venous return.
• Neuraxial block is combined name given to spinal, Epidural D. Venous pooling.
and Caudal Blocks. E. Decreased placental circulation
Principal site of action for neuroaxial block is Nerve root C
..........(PGI - DEC 2003)
Absolute contra indications are -
• Patient Refusal • In epidural anesthesia, the anesthetic drug is injected in
• Bleeding Diathesis a potential space within the bony cavity of the spinal canal
and outside the dural sac.
HELP LINE NO. 9391567707
TOPIC 4: SPINAL ANAESTHESIA ANAESTHESIA 13
In spinal anesthesia, only the drug is injected in the DEFINITIVE
subarachnoid space. - Full hydration maintenance
- Simple analgesics
• CVS changes that occurs after epidural anaesthesia : - Maintain supine position
Epidural Anesthesia - Continuous drip of Hartman’s solution in extradural space
• Loss of sympathetic vasomotor tone with a catheter
• Vasodilatation Epidural blood patch with 10-20ml of venous blood.
• Peripheral pooling of blood
• Reduced venous return 80. Trendelenberg position produces decrease in all of
• Reduced cardiac output the following except-
A. Vital capacity
Hypotension B. Functional residual capacity
• In the absence of hypotension, neither epidurals nor
C. Compliance
spinal have any effect on the progress of labor nor
D. Respiratory rate
do they affect uterine blood flow.
Brief episode of hypotension do not appear to affect D
the clinical condition of the neonates, the duration ..........(AIIMS PGMEE - NOV 2004)
seems more important than the degree.
Hypotension during epidural is usually said to occur if blood Trendelenburg position or head down position causes a
pressure falls 20-30 mm Hg below the preepidural level or cephalad shift in the abdominal viscera and the
systolic pressure drops below 100 Hg. diaphragm.
78. Vasopressor of choice in hypotension produced during
sub-arachroid block:
A. Ephedrine
B. Mephentermine
C. Adrenaline
D. Dopamine
E. Steroids
C&D
..........(PGI - DEC 2004)
79. Post dural puncture headache, true about
A. Common in elderly
B. Small bore needle prevents it
C. Early ambulation increases incidence
D. Occurs immediately after spinal anaesthesia
E. Blood patch is the first line of treatment This effects the lung volume in the following way
B Functional residual capacity -----> Decreases
..........(PGI - JUNE 2004) Total lung volume -----> Decreases
Vital capacity -----> Decreases
• Postdural puncture headache (PDPH) may occur after Lung compliance -----> Decreases
deliberate or accidental dural puncture, or even after
Although these changes are usually well tolerated by healthy
uncomplicated block.
patients, it may cause hypoxemia in obese patients
• Typically it comes on within an hour or two of the
anaesthesia & may be delayed for some days & may last and patients with preexisting lung disease.
for weeks or even months.
• Pain usually occurs in the occipital region & a/w pain &
stiffness in neck.
It is worsened by sitting up & relived by lying down or by
abdominal compression.
Factors affecting PDPH :
• Increasing
- Younger age
- Females> male
The above mentioned changes also lead to increased
• Larger needle
- Dural fibres cut transversely ventilation/perfusion mismatching and atelactasis.
- Pregnant females There is also increased likelihood of regurgitation.
- Multiple punctures
81. Site of action in epidural analgesia
• Treatment: A. Cortex
PROPHYLACTIC B. SubstantiaGelatinosa
- Avoided in pts with h/o frequent severe headache C. Ventral horn
- Use of smaller sized needle D. Sensory nerve ending
- Whitacre needle or sprotte needle should be used B
- Prevention of dehydration, ..........(AIIMS PGMEE - DEC 1998)
HELP LINE NO. 9391567707
TOPIC 5: ANAESTHESIA COMPLICATIONS ANAESTHESIA 14
• The epidural space is situated between the dura mater
and the vertebral canal . It extends from the cranium
to the sacrum and contains loose connective tissue, fat,
lymph vessels, blood vessels and nerves. Drugs can be
administered into the epidural space.
• They diffuse across the dura and the subarachnoid
space and b ind to receptors loc ated in the
substantia gelatinosa in the dorsal horn of the spinal
cord. They also exert an effect on the nerve roots outside
the dura mater, are absorbed systemically from the epidural 84. Mendelson syndrome is due to:
blood vessels and may be distributed through the A. Aspiration pneumonitis
subarachnoid space in the cerebrospinal fluid (CSF). B. Chemical pneumonitis
C. Oesophagitis
D. Oesophageal spasm
Substantia Gelatinosa
A
..........(PGI - 1998 - Dec)
• Mendelson’s syndrome is acid aspiration syndrome.
Aspiration of acid gastric contents cause a chemical trauma
to bronchial and alveolar epithelia i.e. acute exudative
pneumonitis
Mendelson’s syndrome usually occur with material (gastric
acid) at a PH of 2.5 or below, but known to occur with
fluid of a neutral PH as well.
85. Diffusion hypoxia is seen during:
A. Induction of anaesthesia
B. Recovering anaesthesia
C. Preoperatively
D. Postoperatively
B
..........(PGI - 1998 - Dec)
TOPIC 5: ANAESTHESIA COMPLICATIONS
Diffusion hypoxia is seen during recovering anaesthesia. It is
82. Which d oes not cause broncho spasm after seen with N2O.
anaesthesia Mechanism
A. Regurgitation After prolonged N2 O anaesthesia when discontinued N2O
B. Aspiration having low Solubility rapidly diffuses to alveoli and dilutes
C. Postintubation alveolar air PP of oxygen in alveoli is reduced: Resulting
D. Halothane hypoxia is called DIFFUSION HYPOXIA
D
..........(AIIMS PGMEE - DEC 1994) 86. Incubator heat is delivered by except:
A. Conduction
Halothane causes dilatation of Bronchi and is preferred in B. Convection
Asthma C. Radiation
Causes of Bronchospam D. Evaporation
The patients lower airways are excessively responsive to the D
following – ..........(PGI - 1998 - Dec)
1) Surgical stimulation
a) Intubation under light aneasthesia • Incubator heat is delivered by radiation and convection.
b) Carinal stimulation by a tube that is too long Some incubators have humidifiers which will produce an
2) Respiratory infection ambient relative humidity within the canopy of 90% or
3) Pulmonary edema more (compared with 30—40% hunidity without
4) Severe r eduction in lung volume as in tension humidifier).
pneumothorax, Drugs.
83. Mismatc hed blood transfusio n manifests
intraoperatively as:
A. Rise in B. P.
B. Excessive bleeding
C. Dyspnoea
D. Hematuria
B
..........(PGI - 1999 - Dec)
Mismatched blood transfusion manifests intraoperatively as
EXCESSIVE BLEEDING.
HELP LINE NO. 9391567707
TOPIC 5: ANAESTHESIA COMPLICATIONS ANAESTHESIA 15
At such humidity infants evaporative heat loss is very low. • Sodium Nitroprusside can sometimes cause toxicity due
Also sometimes wall of the incubator is doubled which to its conversion to cyanide and thiocyanate, when its
also helps to prevent evaporative loss of heat from infant. infused for longer duration.
In infant heat loss through conduction is very small as infants • “Toxic accumulation of cyanide leading to severe lactic
are not usually in direct contact with structure of acidosis, can occur usually if sodium nitroprusside is infused
high thermal capacity. at a rate greater than 5 microgm/kg.”
• Short-term side-effects of nitroprusside are d/t excessive
87. During intra operative anesthesia mismatched blood vasodilation with hypotension and its consequences
by transfusion is manifested by:
A. Hypotension 92. The most common cause of morbidity and mortality
B. Increase Bleeding in patients undergoing major vascular surgery is:
C. Bonchospasm A. Renal complications
D. Movement of limbs B. Thrombo embolic phenomenon
E. Rash C. Coagulopathies
A & B, C D. Cardiac complications
..........(PGI - JUNE 2006) Ans d
..........(AIIMS PGMEE - MAY 2005)
* Mismatched blood transfusion in anaesthetic patient
present as : 93. The most common rhythm disturbance during early
Immediate rapid severe and progressive hypotension. postoperative period is:
Tachycardia A. Bradycarida
General oozing from wound. B. Ventricular fibrillation
Urticarial rash. C. Tachycardia
Bronchospasm, raising airway pressures on intermittent positive D. Complete heart block
pressure ventilation. Later jaundice and oliguria in 5-10% Ans c
of these patient. ..........(AIIMS PGMEE - MAY 2005)
88. Cause of post-operative hypertension The most common acute post-operative arrhythmias
A. Pre-operative hypertension were junctional ectopic tachycardia
B. inadequate analgesia
C. Phaeochromocytoma 94. Most common cause of postoperative renal failure:
D. Hypoxaemia A. Decreased renal perfusion
E. Hypercarbia B. Toxicity of anesthetic drugs
All C. Toxicity of antibiotics
..........(PGI - JUNE 2004) D. ——
A
89. True about aspiration pneumonia ..........(AIIMS PGMEE - MAY 2008)
A. Affected by volume of aspiration
B. Affected by PH of aspiration fluid • Most common cause of postoperative renal failure
C. Increased incidence during induction is decreased renal perfusion due to hypovolemia.
D. Inflammation Hypovolemia usually results from inadequate intraoperative
E. Infection fluid replacement, continuing fluid sequestration by
All tissues {third spacing) or wound drainage or postoperative
..........(PGI - JUNE 2004) bleeding.
• Factors affecting Acid aspiration pneumonia: 95. Which of the following does not represent a
- Aspirate volume > 25ml significant anaesthetic problem in the morbidly obese
- PH of aspirate <2.5 patient?
- Aspiration of partially digested food A. Difficulties in endotracheal intubation
• Conscious level of patients (e.g. alcoholics, drug B. Suboptimal arterial oxygen tension
abusers, seizures, strokes or general anaesthesia) C. Increased metabolism of volatile agents
- Mechanical impediments (e.g. nasogastric or D. Decreased cardiac output relative to total body mass
endotracheal tubes) D
• Pure acid a spiration producing aspiration ..........(AIIMS PGMEE - NOV 2004)
pneumonitis or chemical pneumonitis (inflammation)
& aspiration of oropharyngeal secretion produces
severe bacterial pneumonitis.
91. Sodium nitroprusside infusion may result in:
A. Hypertension
B. Pulmonary oedema
C. Cyanide toxicity
D. Heart block
C
..........(AIIMS PGMEE - MAY 2005)
• Sodium Nitroprusside is an effective antihypertensive agent
(dilates both arteries and veins)
HELP LINE NO. 9391567707
TOPIC 6: HALOTHANE ANAESTHESIA 16
Problems faced by obese patient during anaesthesia • Hemodynamic monitoring - It is done by
Perioperative
These patients are often difficult to intubate as a result Central venous or pulmonary artery pressure monitoring.
of limited mobility of temperomandibular and atlantoccipital The most sensitive hemodynamic correlates are derived
joints, a narrowed airway and a shortened distance from pulmonary artery pressure monitoring -
between mandible and sternal fat pads. Ischemia is frequently but not always associated with an
Increased risk of developing aspiration pneumonia, abrupt increase in pulmonary capillary wedge pressure.
therefo re routine t/t with H 2 antago nists an d
metoclopromide is given. The most common hemodynamic abnormalities observed
during ischemic episodes are hypertension and
Intraoperative tachycardia.
Volatile anaesthetics are metabolized more rapidly while
the action of nonvolatile agents are prolonged. 97. Sallick’s manouvere is used
Risk of aspiration A. To reduce dead space
Difficulties in regional anaesthesia B. To prevent alveolar collapse
C. To prevent gastric aspiration
Postoperative D. To facilitate assisted respiration
Respiratory failure is the major problem C
postoperatively ..........(AIIMS PGMEE - DEC 1997)
There is risk of postoperative hypoxia, so extubation should
be delayed until the effects of neuromuscular blocker is • Sallick’s manoeuvre is application of backward pressure
completely reversed. on Cricoid cartilage to prevent gastric aspiration.
Cardiovascular changes in obesity TOPIC 6: HALOTHANE
• High Blood volume
• High Cardiac output 98. Hepatoxic anaesthetic agent is:
• Hypertension (Systemic and pulmonary) A. Ketamine
• High Workload on heart B. Ether
• High Stroke volume C. Nitrous Oxide
• Cardiomegaly D. Halothane
Respiratory changes in an obese patient D
• Decrease in vital capacity and functional residual capacity ..........(AIIMS PGMEE - JUNE - 1997)
• Hypoxemia
• Decrease compliance • Halothane is hepatoxic. It is “contraindicated” in liver
• Decrease respiratory drive diseases.
These patients require high FiO2 to achieve adequate • Other Important side effects of Halothane
oxygenation, the ratio of Nitrous Oxide by O2 is kept at 2/ • Arrythmia (Max Arrythmogenic)*
3 Malignant Hyperthermia*
Gastrointestinal changes in obesity
Hiatal hernia 99. Least analgesic gas used is
Gastroesophageal reflux A. N20
Poor gastric emptying B. Ether
Hyper acidic gastric fluid C. Halothane
D. Cyclopropane
96. The most sensitive and practical technique for C
detection of myocardial ischemia in the perioperative ..........(AIIMS PGMEE - MAY - 1994)
period is -
A. Magnetic Resonance Spectroscopy
• Halothane is a potent anaesthetic but poor analgesic
B. Radio labeled lactate determination
All the other agents mentioned in the question are good
C. Direct measurement of end diastolic pressure
analgesics
D. Regional wall motion abnormality detected with the help
Nitrous Oxide - It is good analgesic but poor anaesthetic.
of 2D transoesophagealechocardiography
Ether - It is potent anaesthetic as well as good analgesic
D
Cyclopropane - It is a good anaesthetic and a good analgesic
..........(AIIMS PGMEE - NOV 2005)
100. Which one of the following agents sensitizes the
Two dimensional transesophageal echocardiography is the
myocardium to catecholamines?
most sensitive method to detect myocardial ischemia in
A. Isoflurane
the perioperative period.
B. Ether
C. Halothane
D. Propofol
C
..........(AIPGMEE - 2006)
Halothane sensitize the heart to adrenaline (both
exogenous as well as endogenous, more prominently
exogenous) producing severe ventricular arrhythmias‘.
HELP LINE NO. 9391567707
TOPIC 6: HALOTHANE ANAESTHESIA 17
101. Repeated use of halothane causes: 104. Anesthesia agent with least analgesic property
A. Hepatitis A. N2O
B. Encephalitis. . B. Halothane
C. Pancreatitis C. Ether
D. Bronchitis D. Propane
A B
..........(AIPGMEE - 1999), PGI - JUNE 1997 ..........(AIPGMEE - 1994)
Hepatitis Halothane is a potent anaesthetic but provides poor analgesia.
Massive hepatic necrosis has been seen following halothane
Best/Maximum Trilene
anesthesia.
analgesia
Subclinical ‘Halothane Hepatitis1 with lesser degree of liver
impairment, and a hepatocellular pattern of elevated Profound Analgesia Ketarnine
transferases may also occur. Only analgesia N2O
The most susceptible ones are middle-aged females and obese.
Analgesic Halothane
102. Anatomical dead space is increased by all of the 105. Post operative jaundice is because of use of:
following except: A. Isoflurane
A. Atropine B. NO
B. Halothane C. Melhoxyflurane
C. Massive pleural effusion D. Halothane
D. Inspiration D
C ..........(PGI - 1999 - Dec)
..........(AIPGMEE - 1999)
• Post operative jaundice can be cause by halothane. It
can cause massive hepatic necrosis, subclinical one is called
Anatomical dead space means those areas in the tracheo-
‘Halothane hepatitis.’
bronchial tree, where the gaseous exchange between
the lung and capillaries is not possible.
Note : Other causes of post. Operative jaundice
This area starts from the nasal cavity and includes,
- Phenothiaziges
larynx, trachea, bronchii and ends in the terminal - MAO inhibitors
bronchiole. - Blood. Transfusion
- Sepsis
Pleural effusion, normally tends to compress on the alveoli Coincidental viral infection.
and thus interferes with the physiological dead space
(space where gaseous exchange is occurring). 106. True about halothane:
However, with a massive effusion, atleast some of the structure A. 1% Thymol is used as preservative.
comprising the anatomical dead space may be compressed B. It sensitizes heart to catecholamines at 1 MAC.
thereby decreasing the anatomical dead space. C. 20% metabolized.
D. It is not usually given in same patient within 3 months.
103. All of the following are true except: E. It forms compound-A with sodalime,
A. Halothane is good as an analgesic agent B
B. Halothane sensitises the heart to action of catacholamines ..........(PGI - DEC 2003)
C. Halothane relaxes brochi & is preferred in anaes thetics
D. Halothane may cause Liver cell necrosis • Halothane is a volatile, liquid with sweet odour, nonirritant
A and noninflammable anaesthetic.
..........(AIPGMEE - 2001) • It contains 0.01% thymol for stability and decomposed
by light, but is stable when stored in amber-lime and the
Halothane is good as an analgesic agent vapour is absorbed by rubber.
• Halothane is a potent anaesthetic but not a good analgesic • An estimated 15-20% of absorbed halothane undergoes
or muscle relaxant. metabolism.
• Halothane sensitizes the heart to arrythmogenic action of • Sevoflurane reacts with soda-lime and thus produces
Adrenaline compound-i.e., pentafluoroisopropenyl fluromethyl ether.
• P ethidine is recommended in the management of
• R emember dr ugs which sensitizes the heat to
Halothane shakes.
arrythmogenic action of adrenaline include
• Halothane may persist in the liver for as long as 12 days
- Halothane
after administration.
- Methoxyflurance
- Trichloroethylene 107. True about halothane:
-
Cyclopropane A. Causes bronchodilation
B. Anti-arrhythmic
- Chloroform C. Ted cardiac index
- Halothane causes bronchodilation. Thus it is preferred in D. Uterine contraction occurs
asthmatics (also Ketamine) E. Causes hepatitis
• Massive hepatic necrosis is following halothane A&E
anaesthesia has been reported ..........(PGI - DEC 2002)
HELP LINE NO. 9391567707
TOPIC 7: THIOPENTONE ANAESTHESIA 18
108. True about Halothane: While Intra arterial injection causes Vasospasm
A. Non-irritant intravenous injection causes Vasodilatation.
B. Antiarrhythmic
C. It antagonises bronchospasm 113. Thiopentone is contraindicated in:
D. Vasodilator A. Acute intermitent porphyria
A &C
B. Induction of GA
..........(PGI - DEC 2006)
C. CHF
• Halothane is a colourless, relatively non-irritant vapour. D. GI disease
It is non-flammable non-explosive when mixed with O2 in A
any concentrations used clinically. ..........(AIIMS PGMEE - FEB - 1997)
Effects on organs : • Acute intermitent porphyria
CVS : - Myocardial depression, fall of arterial pressure. • Barbitur ates (Thiopentone) ppt acute intermitent
- Vasodilatation, dilates coronary arteries porphyria
- Bradycardia.
- Increased myocardial excitability, ventricular extrasystoles.
Arrythmia after I.V. infusion of Adrenaline > 10 micro g/
min.
110. Which of the are the following contraindication for
halothane used:
A. Male sex
B. Middle age
C. Recent halothane use
D. Associated liver pathology
Safe drugs in porphyria
E. Obesity
C&D
Local Anaesthesia Drugs used in anaesthesia
..........(PGI - June -2001)
Amethocaine Adrenaline
111. Which of the following fluorinated anaesthetics Bupivacaine Atropine
corrodes metal in vaporizers and breathing systems? Lignocaine 2 Cyclopropane
A. Sevoflurane Prilocaine Epinephrine
B. Enflurane Procaine Ether
C. Isoflurane T etracaine Isoflurane
D. Halothane Neostigmine
D Nitrous oxide
..........(AIIMS PGMEE - MAY 2006) Pancuronium
Phentolamine
• Halothane causes corrosion of metals in vaporizers and Propofol
breathing system Suxamethonium
TOPIC 7: THIOPENTONE Safe anticonvulsants in porphyria
112. Intra arterial injection of thiopentone causes: Anticonvulsants
A. Hypotension Clobazam
B. Necrosis of vessel wall Clonazepam
C. Vasodilation Gabapentin
D. Vasospasm Sodium
D valporate
..........(AIIMS PGMEE - Dec - 1995) Valporate3
Vigabatrin
Vasospasm
When thiopentone is given intra arterial it results in ppt of Safe drugs in porphyria
solid crystals of Thiopentone
Analgesics
↓
Alfentanil
These solid crystal block small vascular channels at Arteriolar Aspirin
and capillary levels Buprenorphine
↓ Codeine Phosphate
Vasospasm Dextromethorphan
(d/t irritant properties of solid crystals) Dextromoramide
Diamorphine
• Morbidity due to Intra arterial injection of Thiopentone is Dihydrocodeine
also d/t Fenbufen
– Thrombosis & Endothelial damage Fentanyl
HELP LINE NO. 9391567707
TOPIC 7: THIOPENTONE ANAESTHESIA 19
(b) Prostacycline
Flurbiprofen Antidepressants (c) Dexamethaethasone
Ibuprofen Fluoxetine (d) Tolazoline
(e) Phenoxybenzamine
Indometacin Mianserin (f) Urokinase
Ketoprofen Antipsychotics
Meloxicam Chlorpromazine • Cancel the operation
Methadone Fluphenazine • Possibly continue volatile anesthesia as an effective
Morphine Haloperidol method of securing vasodilatation
• Perform a Brachical plexus or stellae ganglion block to
Naproxen Olanzapine remove all vasoconstrictor impulses
Paracetamol Pipotiazine • I. V. lignocaine is a vasoditator
Pethidine Trifluoperazine – (all local anesthetics are vasoditator except cocaine) and
Piroxicam can help overcome the vasoconstriction caused by
Sulindac thiopentone.
114. Intraarterial Thiopentone injection causes 116. During surgery for aortic arch aneurysm under deep
A. Cardiac arrest hypothermic circulatory arrest which of the following
B. Respiratory arrest anaesthetic agent administered prior to circulatory
C. Convulsion arrest that also provides cerebral protection ?
D. Pain A. Etomidate
D B. Thiopental Sodium
..........(AIIMS PGMEE - NOV - 1993) C. Propofal
D. Ketamine
Signs and symptoms of intra arterial injection of B
thiopentone ..........(AIIMS PGMEE NOV - 2002)
a) Immediate -
i) Pain • During the surgery for aortic arch all the blood supply to
ii) White hand with cyanosed fingers the br ain has to be stopped so that proper arch
iii) Patches of skin discolouration anastomosis can be performed. This carries great risk for
iv) Onset of unconsciousness is delayed beyond the usual the brain. So the surgery for aortic arch aneurysm is
time performed now days using deep hypothermia and
b) Late circulatory arrest method.
i) Ulcers or blisters • It is based on the principle that brain can safely tolerate
ii) Edema of forearm and hand circulatory arrest for periods of upto 45minutes, if the
iii) Gangrene - rare temperature is carefully lowered to 15-17°C wide surgery.
So during surgery for aortic arch aneurysm temperature is
115. A pt. Selected for surgery who was induced with lowered till the temperature of the body is lowered up to
thiopentone i.v. through one of the antecubital veins 15-17°c and then surgery is performed.
complains of severe pain of whole hand. The next
line of management is: • During this process we need an anaesthetic agent which
A. Give I.V. Ketamine through same needle lowers the metabolic demands of the brain, so that the
B. Give I.V. propofol through same needle brain can sustain longer periods of circulatory arrest.
C. Leave it alone Thiopentone sodium is one such drug, which lowers
D. Give I.V. lignocaine through same needle the metabolic demands of brains and provides it
D added protection, when its blood supply it reduced
..........(AIIMS PGMEE MAY - 2001), AIPGMEE - 1997 during surgery.
Give I.V. lignocaine through same needle 117. Which of the following anesthetic agents does not
• Injection . has gone into the Artery which lies adjacent trigger malignant hyperthermia?
to the antecubital vein. A Halothane
• Immediate symptoms and sign of intra arterial B. Isoflurane
thiopentone C. Suxamethonium
1. Pain during injection D. Thiopentone
2. A white hand with cyanosed fingers d/t arterial spasm D
which may be accompanied or followed by arterial ..........(AIPGMEE - 2006)
thrombosis
3. Patches of skin discoloration in the limb ‘Muscle relaxant succinylcholine is the most commonly
4. Onset of unconsciousness may be delayed beyond the implicated agent. Halothane and isoflurane have also been
usual, time. implicated.
Barbiturates (thiopentone sodium) are safe drugs for
Treatment gener al anae sthesia in patients sus ceptible for
• Leave the canula in site malignanthyperthermia
• Heparin 1000 units is given via cannula in the Artery Malignant Hyperthermia
• Through Canula in the Artery inject Malignant hyperthermia is a familial syndrome characterized
(a) Papavarine 40 -80 mg in 10- 20 ml of Saline clinically by arise of temperature of at least 2DC/hour
Inheritance
HELP LINE NO. 9391567707
TOPIC 7: THIOPENTONE ANAESTHESIA 20
Autosomal dominant inhe ritance with incomplete * Ketamine is having profound analgesic property.
penetration .Defect in gene on chromosome * Fentanyl is a synthetic opioid having intense analgesia.
Pathology 123. Intravenous thiopentone, produces
Abnormality of Ryanodine Receptor: calcium releasing A. Rash
channel of sarcoplasmic reticulum. Sudden rise in B. Pain
intracellular calcium2 leads to hypermetabolic state. C. Spasm
D. Hypotension
118. Not intravenous Anasthetic agent E. Muscular excitation (locally)
A. Ketamine A&B&D
B. Thiopantone ..........(PGI - JUNE 2003)
C. Etomidate
D. Cyclopropane • Thiopentone is an ultra short acting barbiturate used for
D induction of anaesthesia.
..........(AIPGMEE - 1995) • The different effects produced by thiopentone are :
Classification of Anaesthe tic agents: CNS & Respiratory system : Sedation, hypnosis, anaesthesia
& respiratory depression.
Inhalation Intravenous - Increased cerebral blood flow, decrease I C pressure,
Cerebral metabolism & O2 consumption leading to cerebral
Gas Liquid Inducing agent Slower Acting
protection..
• N 2O • Ether • Propofol • Ketamine - CVS : hypotension due to vasodilatation in skin & muscle.
• Halothane • (dissociative Larynx : Increased sensitivity to stimuli producing laryngeal
Methohexitone anesthesia) spasm.
• Cyclopropane • Thiopentone • Fentanyl Eye : - pupils first dilate then constrict.
• Fluranes • Etomidate Droperidol - Loss of eyelash reflex is an excellent sign of adequate
(Neurolept induction.
analgesia) Allergic reaction : Rarely manifests as scarlantiniform rash,
- Enflurane angioneurotic edema & photosensitivity.
- Iso flurane Injection effects : - The incidence of pain on injection is
1-2% when injected into small veins & essentially none
- Desmoflurane when injected into larger veins.
- Sevoflurane - Perivenous injection produces pain, redness & swelling,
haematoma formation, bruising, rarely ulceration.
119. Sodium Thiopentone is ultra short acting d/t - Accidental intraarterial injection produces intense arterial
A. Rapid absorption spasm & excruciating pain that can be felt from the
B. Rapid metabolism injection site to the hand & fingers.
C. Rapid redistribution Musculo skeletal : Besides producing unconsciousness, it
D. Rapic excretion can cause mild muscular excitatory movements such as
C hypertonus, tremor or twitching & respiratory excitatory
..........(AIPGMEE - 1996) effects including cough & hiccup. These are dose
dependent effects.
121. Uses of thiopentone:
A. Seizure 124. Regarding thiopentone all are true except
B. Truth spell A. Sodium carbonate is added to improve its solubility
C. Reduction of I.C.P. B. Cerebro protective
D. Cerebral protection C. Contraindicated in porphyria
E. Maintanance of Anesthesia D. Induction agent of choice in shock
Ans a,b,c,d,e D
..........(PGI - DEC 2004) ..........(AIIMS PGMEE - NOV 2007)
122. Which of the following is not analgesic • Thiopentone is a short acting barbiturate used in the
A. N2O induction of anaesthesia.
B. Thiopentone • Anaesthetic barbiturates are derivatives of Barbituric acid
C. Methohexitone with an oxygen or sulfur at 2 position.
D. Ketamine • The three barbiturates commonly used for clinical
E. Fentanyl anaesthesia are :
B • Sodium thiopental
..........(PGI - DEC 2005) • Thiamylal
• Methohexital
* N2O (nitrous oxide) is a weak anaesthetic agent having Barbiturates are formulated as the sodium salts with
potent analgesic property. 6% sodium carbonate and reconstituted in water or
* Thiopentone & Methohexitone, both are barbiturate group isotonic saline to produce alkaline solutions with pH of 10-
of induction agent without analgesic properties. 11.
Thiopentone having ant-analgesic property only i.e. • Once reconstituted these are stable in solutions for
it decreases the pain threshold. upto 1 week.
HELP LINE NO. 9391567707
TOPIC 8: PAEDIATRIC ANESTHESIA ANAESTHESIA 21
• Thiopentone is used for the induction of anaesthesia Other drugs used are -
because it has a very rapid onset of action. 1) Methohexitone
• The typical induction dose (3-5 mg/kg) of thiopentone 2) Propofol
produces unconsciousness in 10-30 seconds with a peak 3) Etomidate
effect in 1 minute and duration of anaesthesia of 5-8 4) Ketamine
minutes.
• Action of this drug terminates quickly because of rapid 126. The ideal muscle relaxant used for a neonate
redistribution. undergoing porto-enterostomy for biliary atresia is:
• Thiopentone is highly lipid soluble, therefore its A. Atracurium.
redistribution is very rapid and this accounts for its short B. Vecuronium
duration of action. C. Pancuronium.
• Sulphur is added to increase the lipid solubility of D. Rocuronium
thiopentone. A
• Thiopentone is given intravenously. ..........(.AIIMS PGMEE MAY - 2003)
• It produces little to no pain on injection.
• Venoirritation can be reduced by injection into larger non In this case a muscle relaxant is required whose metabolism
hand veins and by prior intravenous injectionof lidocaine. has nothing to do with liver (because liver is damaged in
• If sometimes thiopentone inadverten tly enter biliary atresia)
intraarterial circulation it causes severe inflammatory
and potentially necrotic reaction. • So Atracurium is the muscle relaxant of choice as it is
inactivated in plasma by spontaneous non enzymatic
Effects on system C.N.S.
degradation. (Hoffman elimination) so its duration of
• Besides producing a general anaesthesia, barbiturates
action will not be affected in patients with hepatic
reduce the cerebral metabolic rate, as measured by
insufficiency.
cerebr al oxygen consumpti on (CMR0 2 ) in a dose
dependent manner.
127. In a 2 months old infant undergoing surgery for
• As a consequence of the decrease in (CMRO2) cerebral
biliary atresia, you would avoid one of the following
blood flow and intracranial pressure are similarly reduced.
anaesthetic
• Because it markedly lowers cerebr al metabolism,
A. Thiopentone
thiopentone has been used as a protectant against
cerebral ischemia. B. Halothane.
• Thiopentone also reduces intraocular pressure. C. Propofol.
• Presumbaly in part due to their CNS depressant activity D. Sevoflurane
barbiturates are effective anticonvulsants. B
• Thiopentone in particular is a proven medication in the t/ ..........(.AIIMS PGMEE MAY - 2003)
t of status epilepticus.
halothane is known to cause liver toxicity. So Halothane
C.V.S should be avoided in a patient undergoing surgery for
• Thiopentone produces dose dependent decrease in Biliary atresia (as the liver is already damaged)
blood pressure.
• The effect is primarily due to vasodilation particularly
venodilation.
Respiratory
• Theiopentone is respiratory depressants.
• It causes dose dependent decrease in minute ventilation
and tidal volume with a smaller and inconsistent decrease
in respiratory rate.
Other adverse effects
• Thiopentone has no clinically significant effect on hepatic,
renal or endocrine systems.
• Thiopentone (Barbiturates) can induce fatal attacks of
porphyria in patients with acute intermittent porphyria 128. Regarding neonatal circumcision, which one of the
and are contraindicated in such patients. following is true:
A. It should be done without anaesthesia, as it is hazardous
TOPIC 8: PAEDIATRIC ANESTHESIA to give anaesthesia.
B. It should be done without anesthesia, as neonates do not
125. Method of anaesthetic induction in children is by perceive pain as adults.
A. Intramuscular C. It should be done under local anaesthesia only.
B. Inhalation D. General anaesthesia should be given to neonate for
C. Intravenous circumcision as they also feel pain as adults
D. Oxygen tent D
C ..........(.AIIMS PGMEE MAY - 2003)
..........(AIIMS PGMEE - NOV - 1993)
Circumcision anaesthesia.
• In children intravenous induction of anaesthesia is the “A general anaesthetic is preferable in children, but in
most common method used for induction of anaesthesia. adults local infiltrative anaesthesia, or regional anaesthesia
• The drug most commonly used is thiopentone with a caudal or subpubic block is also satisfactory
HELP LINE NO. 9391567707
TOPIC 8: PAEDIATRIC ANESTHESIA ANAESTHESIA 22
• Its main development has been as a monitoring tool
for use during anaesthesia and intensive care .
• It is usually presented as a graph of expiratory CO2
plotted against time, or, less commonly, but more
usefully, expired volume. The plot may also show the
inspired CO2, which is of interest when rebreathing
systems are being used.
129. Which of the following inhalational agents is the
induction agent of choice in children:
A. Methoxyflurane
B. Sevoflurane
C. Desflurane
D. Isoflurane
B
..........(AIPGMEE - 2006) • The capnogram is a direct monitor of the inhaled and
exhaled concentration or partial pressure of CO2,
Faster, pleasant, and smooth in duction with no significant and an indirect monitor of the CO2 partial pressure
systemic toxity makes sevoflurane the agent of choice in the arterial blood. In healthy individuals, the difference
for induction, especially in children between arterial blood and expired gas CO2 partial
pressures is very small, and is probably zero in children. In
130. A two-month-old infant has undergone a major the presence of most forms of lung disease, and some
surgical procedure. Regarding postoperative pain forms of congenital heart disease (the cyanotic lesions)
relief which one of the following is recommended: the difference between arterial blood and expired gas
A. No medication is needed as infant does not feel pain after increases and can exceed 1 kPa.
surgery due to immaturity of nervous system
B. Only paracetamol suppository is adequate • During anaesthesia, there is interplay between two
C. Spinal narcotics via intrathecal route components: the patient and the anaesthesia
D. Intravenous narcotic infusion is lower dosage administration device (which is usually a breathing circuit
Ans c and a ventilator or respirator). The critical connection
between the two components is either an endotracheal
..........(AIPGMEE - 2006) tube or a mask, and CO2 is typically monitored at this
junction. Capnography directly reflects the elimination of
• Bupivacaine has, until recently, been the drug of choice CO2 by the lungs to the anaesthesia device. Indirectly, it
for postoperative epidural infusions in children. Despite a reflects the production of CO2 by tissues and the
reasonable safety profile, bupivacaine is currently being circulatory transport of CO2 to the lungs.
replaced by many anesthesiologists with new local
anesthetics: levobupivacaine and ropivacaine. These 132. All of the following agents can be given for
local anesthetics are associated with less risk for cardiac induction of anaesthesia in children except:
and central nervous system toxicity and are also less likely A. Halothane
to result in unwanted postoperative motor blockade B. Servoflurane
C. Morphine
131. A non ventilated preterm baby in incubator is under D. Nitrous oxide
observation. Which is the best way to monitor the C
baby’s breathing and detect apnea? ..........(AIPGMEE - 2001)
A. Capnography
B. Impedence pulmonometry Morphine
C. Chest movement monitoring Morphine should not be used in infants specially those
D. Infrared End Tidal CO 2mesurement less than 6 months of age.
A Morphine is also not commonly recommended in older children
..........(AIPGMEE - 2007) (3-10 years) of age
• Capnography is the monitoring of the concentration or
Most commonly used method for inducing gaseous anaesthesia
partial pressure of carbon dioxide (CO2) in the
is with O2, with or without N2O and either halothane
respiratory gases .
or sevoflurane.
HELP LINE NO. 9391567707
TOPIC 9: VENTILATOR ANAESTHESIA 23
• What happens when such a person holds his
breath.
• Soon his blood O2 level will fall (hypoxia) but his blood CO2
level will be normal or below normal (as he was hypocapnic
due to hyperventilation)
• His blood O2 level will continue to fall, but his CO 2 level
will still be not high enough to stimulate the brain for
respiratory drive.
• The person will continue to hold his breath and his
• Halothane is well tolerated in children , in which the O2 level may fall to lethal levels without any respiratory
risk of halo thane induced hepatitis on repeated drive (his brain is still unaware that he is in danger
administration is small. of dying from hypoxia.)
• Enflurane and isoflurane are more pungent and not
recommended 137. In volume cycled ventilation the inspiratory flow
• Sevoflurane, if available is the agent of choice rate is set at
A. 140-160L/min
• Nitrous oxide is particularly useful because of the B. 110-130 L/min
speed of induction, absence of cardiovascular and C. 60-100 L/min
respiratory depression, its rapid onset and offset, and its D. 30-50 L/min
powerful analgesic action. Ans : C
..........(AIIMS PGMEE NOV - 2002)
135. Upper respiratory tract infection is a common
problem in children. All the following anesthetic • Ventilators are devices which are used to provide warm
complications can occur in children with respiratory and humidified gas to the airway opening according to
infections, except: specific volume pressure and time patterns. The ventilator
A. Bacteremia serves as energy source only during inspiration
B. Halothane granuloma replacing the muscles of chest wall and diaphragm.
C. Increased mucosal bleeding • Expiration is passive driven by the recoil of the lung and
D. Laryngospasm chest wall.
B
..........(AIPGMEE - 2002) There are various modes of mechanical ventilation such as
(1) Assist control mode ventilation
• Due to local infection there is hyperemia of the local area (2) Continuous positive airway pressure
& trauma can result in mucosal bleeding (3) Pressure control ventilation
• Due to local edema & inflammation laryngospasm can be a (4) Pressure support ventilation
complication (5) Open lung ventilation
• Systemic infection can lead to Bacteremia • These various modes of ventilation specifies the manner
in which ventilator breaths are triggered, cycled and
TOPIC 9: VENTILATOR limited.
Lets see the meaning of these terms.
136. After Hyperventilating for some time holding the Trigger- It defines what the ventilator senses to initiate
breath is dangerous because: an assisted cycle.
A. Decrease CO2 shift the O2 dissociation curve to the left In volume-assist control, the patient can receive
B. Alkalosis can lead to tetany controlled or assisted breaths – all identical
C. It can lead to CO2 Narcosis
D. Due to lack of stimulation by CO2, anoxia can go into
dangerous levels
D
..........(AIIMS PGMEE NOV - 2000)
Due to lack of stimulation by CO2, anoxia can go into dangerous
levels
• In our body its not O2, but CO 2 that maintains the
respiratory drive (though main function of respiration is
to maintain adequate oxygen level in the body)
• Thus its not hypoxia but hypercarbia that is required • One has to be careful with triggering devices: if the trigger
to inform the brain that respiration is inadequate. is too sensi tive the patient “overt riggers” and
• If normally a person holds his breath he will soon hyperventilates, if it is not sensitive enough, the patient
have decrease O 2 level (hypoxia) and increase CO 2 becomes dysynchronous.
level (hypercarbia)
• Hypercarbia will stimulate the brain and increase the Cycle- Refers to the factors that determine the end of
respiratory drive, forcing the person to take breath. inspiration
• What happens when a person hyperventilates ? For e.g., in volume cycle ventilation inspiration ends
• decreased PaCO2 of blood when a specified volume is delivered to the patient
• normal O2 saturation (despite hyperventilation arterial Limiting factors-are operator specified values such as
O2 saturation remains same as blood is almost fully airway pressure that are monitored by transducer’s
saturated at normal ventilation rate ) internal to the ventilatory circuit.
HELP LINE NO. 9391567707
TOPIC 9: VENTILATOR ANAESTHESIA 24
• Volume cycle ventilation and Assist control mode of Pressure support ventilation (PSV)
ventilation. • For the spontaneously breathing patient, pressure
Every breath whether triggered by patient or timer is a support ventilation (PSV) has been advocated to
volume cycled breath and the inspiratory flow rate is limit barotrauma and to decrease the work of
maintained at 60 L/ min breathing.
• Pressure support differs from A/C and IMV in that a
Methods of Ventilatory Support level of support pressure is set (not TV) to assist
Continuous mandatory ventilation every spontaneous effort.
• Breaths are delivered at preset intervals, regardless of • Airway pressure support is maintained until the patient’s
patient effort. inspiratory flow falls below a certain cutoff (eg, 25% of
• This mode is used most often in the paralyzed or apneic peak flow). With some ventilators, there is the ability to
patient because it can increase the work of breathing set a back-up IMV rate should spontaneous
if respiratory effort is present. respirations cease.
• Continuous mandatory ventilation (CMV) has given
way to assist-control (A/C) mode because A/C with the • PSV is frequently the mode of choice in patients
apneic patient is tantamount to CMV. Many ventilators do whose respiratory failure is not severe and who have an
not have a true CMV mode and offer A/C instead. adequate respiratory drive. It can result in improved
patient comfort, reduced cardiovascular effects,
Assist-control ventilation reduced risk of baro trauma, and improved
• The ventilator delivers preset breaths in coordination distribution of gas.
with the respiratory effort of the patient .
• With each inspiratory effort, the ventilator delivers a full Noninvasive ventilation
assisted tidal volume. • The application of mechanical ventilatory support through
• Spontaneous breathin g independent of the a mask in place of endotracheal intubation is
ventilator between A/C breaths is not allowed. becoming increasingly accepted and used in the
• As might be expected, this mode is better tolerated emergency department. Considering this modality for
than CMV in patients with intact respiratory effort. patients with mild-to-moderate respiratory failure is
appropriate. The patient must be mentally alert enough
Intermittent mandatory ventilation to follow commands. Clinical situations in which it has
• With intermittent mandatory ventilation (IMV), proven useful include acute exacerbation of chronic
breaths are delivered at a preset interval, and obstructive pulmonary disease (COPD) or asthma,
spontaneous breathing is allowed between ventilator- decompensated congestive heart failure (CHF) with
administered breaths. mild-to-moderate pulmonary edema, and pulmonary
• Spontaneous breathing occur s agains t the edema from hypervolemia.
resistance of the airway tubing and ventilator • It is most commonly applied as continuous positive
valves, which may be formidable. This mode has given airway pressure (CPAP) and biphasic positive airway
way to synchronous intermittent mandatory pressure (BiPAP).
ventilation (SIMV). • BiPAP is commonly misunderstood to be a form of pressure
support ventilation triggered by patient breaths; in
Synchronous intermittent mandatory ventilation actuality, BiPAP is a form of CPAP that alternates
• The ventilator delivers preset breaths in between high and low positive airway pressures,
coordination with the respiratory effort of the
permitting inspiration (and expiration) throughout.
patient. Spontaneous breathing is allowed between
breaths. Synchronization attempts to limit barotrauma that
• Indications For Mechanical Ventilation
may occur with IMV when a preset breath is delivered to
Clinical criteria
a patient who is already maximally inhaled (breath stacking)
• Apnea or hypopnea
or is forcefully exhaling.
• Respiratory distress with altered mentation
• The initial choice of ventilation mode (eg, SIMV, A/C) is
• Clinically apparent increasing work of breathing
institution and practitioner dependent. A/C ventilation,
unrelieved by other interventions
as in CMV, is a full support mode in that the ventilator
• Obtundation and need for airway protection
performs most, if not all, of the work of breathing. These
Other criteria
modes are beneficial for patients who require a high
• Controlled hyperventilation (eg, in head injury).
minute venti lation. Full support re duces oxygen
• Severe circulatory shock
consumption and CO2 production of the respiratory
Laboratory Criteria for Mechanical Ventilation
muscles. A potential drawback of A/C ventilation in the
patient with obstructive airway disease is worsening of air Blood gases PaO2 <55 mm Hg
trapping and breath stacking.
PaCO2 >50 mm Hg and pH <7.32
• When full respiratory support is necessary for the Pulmonary function tests Vital capacity <10 mL/kg
paralyzed p atient following neu romuscular Negative inspiratory force <25
blockade, no difference exists in minute ventilation cm H2O
or airway pressures with any of the above modes
of ventilation.
FEV1 < 10mL/KG
Guidelines for Ventilator Settings
• In the apneic patient, A/C with a respiratory rate Mode of ventilation
(RR) of 10 and a TV of 500 mL delivers the same • The mode of ventilation should be tailored to the needs
minute ventilation as SIMV with the same parameters. of the patient. In the emergent situation, the practitioner
HELP LINE NO. 9391567707
TOPIC 9: VENTILATOR ANAESTHESIA 25
may need to order initial settings quickly. SIMV and A/C • One obvious beneficial effect of PEEP is to shift lung water
are versatile modes that can be used for initial from the alveoli to the perivascular interstitial space. It
settings. does not decrease the total amount of extravascular lung
• In patients with a good respiratory drive and mild- water. This is of clear benefit in cases of cardiogenic as
to-moderate respiratory failure , PSV is a good initial well as noncardiogenic pulmonary edema. An additional
choice. benefit of PEEP in cases of CHF is to decrease venous
return to the right side of the heart by increasing
Tidal volume intrathoracic pressure.
• Observations of the adverse effects of barotrauma and
volutrauma have led to recommendations of lower tidal
• Applying physiologic PEEP of 3-5 cm H2 O is common
volumes than in years past, when tidal volumes of 10-15
to prevent decreases in functional residual capacity
mL/kg were routinely used.
• An initial TV of 5-8 mL/kg of ideal body weight is generally in those with normal lungs. The reasoning for increasing
indicated, with the lowest values recommended in the levels of PEEP in critically ill patients is to provide acceptable
presence of obstructive airway disease and ARDS. The oxygenation and to reduce the FiO2 to nontoxic levels
goal is to adjust the TV so that plateau pressures are less (FiO2 <0.5). The level of PEEP must be balanced such
than 35 cm H2 O. that excessive intrathoracic pressure (with a resultant
decrease in venous return and risk of barotrauma) does
Respiratory rate not occur.
• A respiratory rate (RR) of 8-12 breaths per minute is
recommended for patients not requiring hyperventilation Sensitivity
for the treatment of toxic or metabolic acidosis, or • With assisted ventilation, the sensitivity typically is set
intracranial injury. High rates allow less time for exhalation, at -1 to -2 cm H2 O. The development of iPEEP
increase mean airway pressure, and cause air trapping in increases the difficulty in generating a negative
patients with obstructive airway disease. The initial rate inspiratory force sufficient to overcome iPEEP and
may be as low as 5-6 breaths per minute in the set sensitivity. Newer ventilators offer the ability to
asthmatic patients when using a permissive hypercapnic sense by inspiratory flow instead of negative force. Flow
technique.
sensing, if available, may lower the work of breathing
associated with ventilator triggering.
Supplemental oxygen therapy
• The lowest FiO2 that produces an arterial oxygen
saturation (SaO2) greater than 90% and a PaO2 Initial ventilator settings in various disease states.
greater than 60 mm Hg is recommended. No data Tidal volume RR I/E ratio PEEP FIO2
indicate that prolonged use of an FiO2 less than 0.4
damages parenchymal cells. Normal lungs 8 mL/kg 10-12 1:2 4 1.0
Asthma/copd 6 mL/kg 5-8 1:4 4 1.0
Inspiration/expiration ratio
ARDS 6 mL/kg 10-12 1:2 4-15 1.0
• The normal inspiration/expiration (I/E) ratio to start
is 1:2. This is reduced to 1:4 or 1:5 in the presence Hypovolemia 8 mL/kg 10-12 1:2 0-4 1.0
of obstructive airway disease in order to avoid air- 138. Laryngeal mask Airway (LMA) is used for;
trapping (breath stacking) and auto-PEEP or intrinsic PEEP A. Maintenance of the airway
(iPEEP). Use of inverse I/E may be appropriate in certain B. Facilitating laryngeal surgery
patients with complex compliance problems in the setting C. Prevention of aspiration
of ARDS. D. Removing oral secretions
A
Inspiratory flow rates ..........(AIIMS PGMEE NOV - 2003)
• Inspiratory flow rates are a function of the TV, I/E
ratio, and RR and may be controlled internally by the Laryngeal mask is used for maintenance of airway in patients
ventilator via these other settings. If flow rates are set in whom tracheal intubation is difficult or impossible.
explicitly, 60 L/min is typically used. This may be It is a cuffed mask designed to fit closely over the
increased to 100 L/min to deliver TVs quickly and laryngeal aperture. It forms a seal around the larynx.
allow for prolonged expiration in the presence of
obstructive airway disease.
Positive end-expiratory pressure
• PEEP has several beneficial effects and may be clinically
underutilized. Research underway is examining the utility
of high (>10 cm H2 O) PEEP in disease states
ranging from COPD/asthma to ARDS . PEEP has been
found to reduce the risk of atelectasis trauma and increase
the number of “open” alveoli participating in ventilation,
thus minimizing V/Q mismatches. However, note that in
disease states such as ARDS, the degree to which alveoli
function has been compromised varies tremendously within - Laryngeal mask airway is also called as Bain Mask (after
the lungs and there is no single “ideal” PEEP the name of its inventor)
appropriate for all alveoli; rather, a compromise PEEP - It provides relatively safe anaesthesia for adults and
must be selected. children in place of tracheal intubation.
HELP LINE NO. 9391567707
TOPIC 9: VENTILATOR ANAESTHESIA 26
Contraindications Oropharyngeal abscess or mass.
• Full stomach patients
• Hiatus hernia
• Pregnancy (where chances of aspiration are high).
• Patients who are vulnerable to go in bronchospasm.
It should be remembered that it is only an adjunct to airway
management but not a substitute for tracheal intubation.
Moreover it does not protect the airway from pulmonary
aspiration.
140. The following modes of ventilation may be used
139. The laryngeal mask airway used for securing the for weaning off patients from mechanical ventilation
airway of a patient in all of the following conditions except:
except: A. Controlled Mechanical ventilation (CMV).
A. In a difficult intubation. B. Synchronized intermittent mandatory ventilation (SIMV).
B. In cardiopulmonary resuscitation. C. Pressure support ventilation (PSV).
C. In a child undergoing an elective/routine eye surgery. D. Assist-control ventilation (ACV)
D. In a patient with a large tumour in the oral cavity A
D ..........(AIPGMEE - 2005)
..........(.AIPGMEE - 2005)
In controlled mode ventilation (CMV) patients own effort
Oropharyngeal abscess or mass is a contraindication to the is nil.
use of laryngeal mask airway. (LMA) Only ventilator is delivering the present tidal volume. This
mode therefore will play no role in weaning a patient from
mechanical ventilation.
Laryngeal Mask Airway
It is a special type of airway useful in difficult intubation.
It is placed blindly in the oropharynx and the cuff is 141. In apatient with fixed respiratory obstruction
inflated with large volume of air inflated cuff seals Helium is used along with Oxygen instead of plain
the lateral and posterior pharyngeal walls and patient can oxygen because
be ventilated through ventilation parts. A. It decreases oxygenation
B. It decreases turbulence
Indications C. It decreases the dead space
1) As an alternative to intubation where difficult intubation D. It provides analgesia
is anticipated. D
2) Securing airway in emergency where intubation and mask ..........(AIPGMEE - 2002)
ventilation is not possible.
3) As a elective method for minor surgeries where It increases oxygenation
anaesthetist wants to avoid intubation. • Helium is given as Heliox [HeO2], a mixture of 20% to
4) As a conduit for bronchoscopes, small size tubes, gum 80% He and 80% to 20% O 2 [usually 80% He with
elastic bougies. 20% O2]. It has about 1/3rd the density of O2 or air.
Advantages • Because helium is highly diffusible , the use of the
Easy to insert (even paramedical staff can insert). mixture greatly reduces the work of breathing in a patient
Does not require any laryngoscope and muscle relaxants with narrowed airways and thus lead to improved aerosol
Does not require any specific position of cervical spine so delivery and increased oxygenation in severe
can be used in cervical injuries asthma.
• It may also reduce the risk of barotrauma.
Disadvantages • Airway resistance is dictated by the diameter of the
• It does not prevent aspiration so should not be used airways and by the density of the inspired gas. Therefore
for full stomach patients. when nitrogen (of air) is replaced by helium, airway
• High incidence of laryngospasm and bronchospasm resistance is reduced due to the lower density of
HELP LINE NO. 9391567707
TOPIC 9: VENTILATOR ANAESTHESIA 27
the inspired gas. This means that when one breathes It’s value’ is increased when there are :
Heliox, airway resistance is less, and therefore the - Increased CO2 production e.g. in malignant hyperpyrexia.
mechanical energy required to ventilate the lungs, - Depression of respiratory center with concomitant
or the Work of Breathing (WOB) is decreased . reduction of total ventilation and ExCO2.
- Reduction of effective ventilation induced by paralysis,
• Heliox is used mainly in the alleviation of many medical neurologic disease, high spinal anaesthesia,
conditions that involve a decrease in airway diameter weakened respiratory musculature or respiratory
(and consequently increased airway resistance), disease.
such as upper airway obstruction, asthma, chronic
obstructive pulmonary disease (COPD), bronchiolitis Abnormally low end-tidal values (< 35 mm of Hg)
and croup. Patients with these conditions may suffer a most often reflect hyperventilation but may be also be
range of symptoms including dyspnea (breathlessness), caused by increased dead space with normal PaCO2 i.e.
hypoxemia (below-normal oxygen content in the arterial
alveolar gas emanating from a lung region with no
blood) and eventually a weakening of the respiratory
blood flow (and no local CO 2 relative to PaCO 2. So,
muscles due to exhaustion, which can lead to respiratory
in pul. embolism it is decreased).
failure and require intubation and mechanical ventilation -
Heliox may reduce all these effects, making it easier for
the patient to breathe, and as it will reduce work of 144. The physiological dead space is decreased by:
breathing, Heliox can help to prevent this respiratory A. Upright position
failure. Heliox has also found utility in the weaning of B. Positive pressure ventilation
patients off mechanical ventilation, and in the nebulization C. Neck flexion
of inhalable drugs. D. Emphysema
A
• It decreases turbulence. In COPD, Helium is used along ..........(AIIMS PGMEE - MAY 2005)
with O2 to decrease the viscosity of gaseous mixture
which increases its linearity & decreases resistance in The PaCO2 will be greater than or equal to end-ridal PaCO2
pathway. (PET CO 2 ) unles s the patient inspires or r eceives
exogenous ca rbon dioxide (e.g., fro m peritoneal
insufflation). The difference between PETCO2) is because
of dead space ventilation. The most common reason for
an acute increase in dead space ventilation is decreased
cardiac output. Measurement of this difference-which is
simple, readily obtainable, and fairly inexpensive-yields
reliable information relative to the degree of dead space
ventilation. Clinical situations that change pulmonary blood
flow sufficiently to increase dead space ventilation can be
detected by comparing PET CO 2 with temper ature
corrected PaCO 2. Yamanaka and Sue52 found that the
142. All are true about PEEP except: PETCO2 in ventilated patients varied linearly with the dead
A. Useful in situations where PO2 is low space to tidal volume ratio (VD/VT) and that PETCO2
B. Decreased Cardiac output correlated poorly with PaCO 2. Thus, in the critically ill,
C. Impaired renal function mechanically ventilated patient, and in anesthetized
D. Decreased ICT patients, monitoring PETCO2 gives far more information
D about ventilatory efficiency or dead space ventilation than
..........(PGI - June -1999) it does about the absolute value of PaCO2.
• When PEEP (Positive End Expiratory Pressure) is applied,
145. Placement of a double lumen tube for lung surgery
there is rise in cerebral venous and intracranial pressures
is best confirmed by -
in parallel with the increase in mean intrathroacic pressure.
A. EtCO2
• Cardiac output and venous return is reduced Rt. Atrial
B. Airway pressure measurement
pressure - rises.
• Useful in conditions where PO2 is low and also easier if C. Clinically by auscultation
PCO2 is lowered. D. Bronchoscopy
D
143. End-tidal CO2 is increased to maximum level in: ..........(AIIMS PGMEE - NOV 2005)
A. Pulmonary. Embolism
B. Malignant hyperthermia
C. Extubation
D. Blockage of secretion
B
..........(PGI - June -2000)
• The PCO2 value at the end of exhalation is referred to as
End-tidal PCO2 (PETCO2).
The normal end-expiratory CO 2 partial pressure ranges
between 35 and 45 mm of Hg.
HELP LINE NO. 9391567707
TOPIC 10: ATRACURIUM ANAESTHESIA 28
• During thoracic surgery there is a need for one lung to be What is the use of end tidal CO2 determination (EtCO2) in
deflated and or isolated. This offers the surgeon easier intubuation ?.
and better acess within the designated hemothorax. • The EtCO2 can be used to confirm the position of
In order to achieve this double lumen endobronchial the endotracheal tube, (whether the tube is in
tubes are used that allow the anaesthetist to oesophagus or trachea)
selectively deflate one lung while maintaining • The persistent detection of CO2 by a capnograph is the
standard ventilation of the other. best confirmation of tracheal placement of an
endotracheal tube (EtCO 2).
Capnography can detect whether the tube is in trachea
or oesophagus but can not differentiate between
tracheal intubation and endobronchial intubation
because in both these cases there will be persistent
detection of COr
146. The most common cause of hypoxia during one
lung ventilation is -
Components of Double lumen tube A. Malposition of the double lumen tube
• Double lumen endobronchial tube has two separate colour B. Increased shunt fraction
coded lumen each with its own bevel. C. Collapse of one lung
• One lumen ends in the trachea and the other lumen D. Soiling of lung by secretions
ends in either the left or right main bronchus B
• Each lumen has its own cuff (tracheal an bronchial cuffs) ..........(AIIMS PGMEE - NOV 2005)
and colour coded pilot balloons.
• The proximal end of these tubes is connected to a Malpositioning of the double lumen endo-bronchial tube
breathing system. used to be the most common cause of hypoxia during
one lung ventilation.
However during last 2 decades, with the use of fiber-
optic bronch oscopes or bronchial bl ockers, this
complication has declined and no longer remains the
most common cause of hypoxemia in these procedures.
The common cause is pulmonary AV shunt in the non-
ventilated lung and the ventilated lung.
How does this shunt develops during one lung
ventilation
• Intentional collapse of the lung on the operative side
facilitates most thoracic procedures but complicates
anaesthetic management.
Mechanism of action
• Because of the differing anatomy of the main bronchi and
their branches, both right and left versions of any particular
double lumen tube must exist.
• Once correctly positioned the anaesthetist can
selectively ventilate one lung, so for operations
requiring that the right lung is deflated , a left sided
double lumen tube would be used that enables selective
ventilation of the left lung alone and vice versa.
• The position of the tubes should b e checked by Since the collapsed lung continues to be perfused
auscultation immediately after intubutation and after and is deliberately no longer ventilated, the patient
positioning the patient for operation. develops a large right to left intrapulmonary shunt (20-
• The auscultatorv method for checking the correct 30%).
placement of tube is hist a clinical method for ensuring Mixing of the unoxygenated blood from the still ventilated
correct placement of the tube and the confirmation of dependent lung widens the PA-a (alveolar to arterial) O2
correct placement of the tube should be the done by gradient and can result in hypoxemia.
flexible fibreoptic bronchoscopy.
TOPIC 10: ATRACURIUM
147. Which of the following is the muscle relaxant of
choice in renal failure?
A. Rapacurium
B. Pancuronium
C. Atracurium
D. Rocuronium
C
..........(AIPGMEE - 2006), PGI - 1997 – Dec, AIIMS PGMEE -
NOV 2004
HELP LINE NO. 9391567707
TOPIC 10: ATRACURIUM ANAESTHESIA 29
‘The unique feature of Atracurium is inactivation in plasma Atracurium gets inactivated in plasma by spontaneous
by spontaneous nonenzymatic degradation (Hoffman non-enzymatic Hoffman’s elemination.
elemination) consequently its duration of action is not It is short acting and reversal is mostly not required
altered in patients with renal / hepatic insufficiency, or
hypodynamic circulation. Hemodynamically it is almost The concept of Balanced anaesthesia was introduced by
neupal Lundy and consist of
Preferred relaxants Thiopental For Induction
In renal failure : Vecuronium or Atracurium. N2O For Amnesia
In hepatic failure : Atracurium. Mepiridine (or other opioid) For Analgesia
In Myasthenia gravis : if relaxants are essential, one-tenth
Curare For Muscle relaxation
of the normal dose of atracurium
In short cases: atracurium, rapacurium, or mivacurium. Atracurium:
In obstetrics any relaxant except gallamine. Gets inactivated in plasma by spontaneous non-
In arterial surgery: to maintain art erial pressure enzymatic Hoffman’s elimination.
pancuronium. Short acting
To deliberately reduce BP: tubocurarine. Reversal is mostly not required
For rapid sequen ce induction: without using Vecuronium:
suxamethonium, Rocuronium or rapacurium. R ecovery is gener ally spon taneous not ne eding
neostigmine reversal unless repeated doses are
148. An elderly male on ventilator has received atracurium given.
infusion for 3 days. He now develops epileptic • Longterm administration of vecuronium to patients in ICU
fits.Probable cause for his epilepsy is: has resulted in prolonged neuro muscular blockade (upto
A. Allergy to drug sever al days) d/t accumulation of 3-Hydroxy
B. Accumulation of Atracurium metabolite, or development of polyneuropathy.
C. Accumulation of Laudanosine
D. Ventilator failure • Gallamine:
C Long acting
..........(AIPGMEE - 2007) Needs reversal
• Pancuronium:
Laudanosine is a metabolite of Atracurium and has CNS
Long acting
stimulating properties.
Needs reversal
Laudonosine may produce convulsions from its CNS
stimulating action, when high plasma concentration of
Laudanosine are reached. 152. Hoffman’s elimination is seen with:
In clinical practice, in the operating room and ICU setting, A. Gallamine
such high concentrations are usually not reached, but B. Atracurium
the patient in question has been on atracurium for 3 C. Succinyl choline
consequestive days before he develops epilepsy and hence D. Tubocurare
high plasma concentration of Laudanosine could well be a B
probable cause for epilepsy. ..........(PGI - June -1998), PGI - June -1999
149. Shortest acting non-depolarising skeletal muscle 153. Muscle relaxant used In renal failure:
relaxant is: A. Ketamine
A. Mivacurium B. Atracurium
B. Vecuronium C. Pancuronium
C. Atracurium D. Fentanyl
D. Succinyl choline B
A ..........(PGI - June -1999)
..........(AIPGMEE - 2000)
Muscle relaxant of choice in renal failure is Atracurium. It is
Mivacurium also suitable :
• Shortest acting depolarization agent is succinyl choline — For liver disease.
(duration = 3 to 6mm) — For patients with atypical cholinesterase.
• Shortest acting non-depolarization agent is – Mivacurium — For organophosphorous poisoning,
(duration = 12-20 min) - Myasthenia Gravis.
150. At the end of a balanced anaesthesia technique
156. A 21-year-old lady with a history of hypersensitivity
with non-depolarizing muscle relaxant, a patient
to Neostigmine is posted for an elective caesarean
recovered spontaneously from the effect of muscle
section under general anesthesia. The best muscle
relaxant without any reversal. Which is the most
relaxant of choice in this patient should be
probable relaxant the patient had received.
A. Pancuronium A. Pancuronium
B. Gallamine B. Atracurium
C. Atracurium C. Rocuronium
D. Vecuronium D. Vecuronium
C B
..........(AIPGMEE - 2003) ..........(AIIMS PGMEE - MAY 2004)
HELP LINE NO. 9391567707
TOPIC 11: INTUBATION ANAESTHESIA 30
Neostigmine is given for reversal of action of non- Using upper incisors as lever to lift the laryngoscope will cause
depolarizing muscle relaxants damage to the upper incisors (in fact it will break the
Neostigmine is an anticholinesterase. Its action prevents upper incisors)
the metabolism of acetylcboline by the enzyme
acetylcholinesterase. This increases the concentration During endotracheal intubation a small pillow should be placed
of Acetylcholine in the synaptic cleft and leads to under the occiput to flex the neck and extend the atlanto-
development of action potential. occipital joint. This straightens the path from upper
This causes the muscles paralysed by the muscle rerlaxants incisors to the larynx.
to return back to their normal contractile state.
In both straight blade laryngoscope and curved blade
Neostigmine is usually required after long acting muscle laryngoscope the tip of the laryngoscope is inserted firmly
relaxants have been used, to hasten recovery at the end into the vallecula and is used to lift the base of epiglottis.
of operation.
Among the muscle relaxants given in the option Atracurium 159. The narrowest part of larynx in infants is at the
has the shortest duration of action and so it usually cricoid level. In administering anesthesia this may
does not require neostigmine for the reversal of its lead to all except.
action. A. Choosing a smaller size endotracheal tube.
B. Trauma to the subglottic region.
Mivacurium is the shortest acting competitive blocker C. Post operative stridor
therefore it does not need reversal. D. Laryngeal oedema
D
TOPIC 11: INTUBATION ..........(AIIMS PGMEE MAY - 2003)
157. Endotracheal intubation is contraindicated in: The narrowest part of larynx in infants is at the cricoid level
A. Fracture mandible (below the vocal cords), hence endotracheal tube
B. Short neck which passes through the vocal cords may not pass
C. CSF rhinorrhoea through the cricoid-hence a smaller size of tube is
D. Fracture cervical spine chosen.
C
..........(AIIMS PGMEE - Dec - 1995) Because cricoid (subglottic area) area is the narrowest - it
may get traumatized during intubation.
CSF rhinorrohoea
“Endotracheal intubation can be done in patients with
fracture of cervical spine. It may be difficult and may
require fibreoptic intubation”.
Postoperative stridor after extubation occurs due to
mucosal edema in subglottic area resulting after intubation.
Laryngeal edema is unlikely because small size of tube
used in infants does not cause trauma to larynx, however
it may cause trauma to subglottic area leading to subglottic
edema.
160. Which of the following is not an indication for
endotracheal intubation?
A. Maintenance of a patent airway
B. To provide positive pressure ventilation
158. During laryngoscopy and endo-tracheal intubation C. Pulmonary toilet
which of the maneuver is not performed: D. Pneumo thorax
A. Flexion of the neck. D
B. Extension of Head at the atlanto-occipital joint. ..........(AIPGMEE - 2006)
C. The laryngoscope is lifted upwards levering over the upper
incisors. Pneumothorax requires urgent needle thoracocentesis
D. In a straight blade laryngoscope, the epiglottis is lifted by and/or Intercostal drainage .
the tip Pneumothorax is a known complication of endotracheal
C intubation and mechanical ventilation and is certainly not
..........(.AIIMS PGMEE MAY - 2003) an indication for the same.
HELP LINE NO. 9391567707
TOPIC 11: INTUBATION ANAESTHESIA 31
INDICATIONS FOR ENDOTRACHERAL INTUBATION 162. True about endotracheal intubation is:
Indications for Endotrachea! Intubation in the A. It reduces the normal anatomical dead space
operating room include : B. It produces resistance to respiration
• The need to deliver positive pressure ventilation C. Sub-glottic oedema is the most common complication
• Protection of the respiratory tract from aspiration of gastric D. All of the above
contents A
• Surgical procedure involving the head and neck or in non- ..........(AIPGMEE - 1999)
supine positions that preclude manual airway support
• Endotracheal intubation decreases the normal anatomical
• Almost all situations involving neuromuscular paralysis dead space (150ml) to as less as 25ml, and thus provides
• Surgical procedures involving the cranium, thorax, or a distinct advantage.
abdomen • Endotracheal intubation increases the resistance to
• Procedures that may involve intracranial hypertension respiration.
To keep resistance at a minimum, use of widest internal
Some non-operative indications are: diameter endotrachal tube that will fill in the larynx is
• Profound disturbance in consciousness with the inability recommended.
to protect the airways • Subglotic edema, though a complication, is not the most
• Tracheobronchial toilet (pulmonary toilet) common one.
• Severe pulmonary or multisystem injury associated with
respiratory failure, such as sepsis, airway obstruction 163. True about endotracheal cuff:
hypoxemia, and hypercarbia A. Low-volume, high pressure
B. Low-volume, low pressure
161. Malampatti Grading is for: C. High-volume, low pressure
A. To assess mobility of cervical spine D. High volume, high pressure
B. To assess mobility if atlantotaxial joint E. Equal volume and pressure
C. For assessment of free rotation of neck before intubation. A&C
D. Inspection of oral cavity before intubation ..........(PGI - DEC 2002)
D
..........(AIPGMEE - 2000) Large volume, low pressure endotracheal tube cuffs
are claimed to have less deleterious effect on tracheal
Inspection of oral cavity before intubation mucosa than high pressure, low volume cuffs
Malampatti grading is to assess the ‘size of tongue’, ‘pharyngeal
pillars’, ‘uvula’ etc. prior to endotracheal intubation.
Malampatti grading for assessment of air way :
Grade Structures visible on opening mouth
I Faucial pillars / soft palate / uvula
II Faucial pillars / soft palate / uvula masked by base of tounge
III Only soft palate
IV Hard palate
164. Indications of tracheostomy are:
A. Flail chest
B. Head injury
C. Tetanus
D. Cardiac tamponade
E. Foreign body
A, B, C & E
..........(PGI - JUNE 2003)
Indications for tracheostomy
To relieve upper airway obstruction
HELP LINE NO. 9391567707
TOPIC 12: MUSCLE RELAXANT ANAESTHESIA 32
• Foreign body 165. True about Laryngoscopy & intubation except
• Trauma A. Hypertension
• Acute infection - acute epiglottitis, diphtheria B. Tachycardia
• Glottic oedema C. Decreased ICT
• Bilateral abductor paralysis of the vocal cords D. Decreased Intra ocular pressure
• Tumours of the larynx E. Increased lower oesophageal sphincter tone
• Congenital web or atresia Ans c,d,e
To improve respiratory function ..........(.PGI - JUNE 2004), PGI - June -2001
• Fulminating bronchopneumonia
• Chronic bronchitis and emphysema
Application of cricoid pressure reduces LES tone and may
• Chest injury and flail chest
Respiratory paralysis cause the esophagus to be displaced to the side rather
• Unconscious head injury than to be compressed. Compression in the backward
• Bulbar poliomyelitis and upward direction improves laryngoscopy.
• Tetanus
Advantages of tracheostomy over endotracheal intubation rise in intraocular pressure during laryngoscopy and
• Reduces patient discomfort intubation is a matter of concern in patients of acute
• Reduces need for sedation glaucoma
• Improves ability to maintain oral and bronchial hygiene
• Reduces risk of glottic trauma Topical anesthesia of oropharynx with lidocaine aerosol
• Reduces dead space and reduces work of breathing (6 ml of 4% for 5 min) prevented hypertension and
• Augments process of weaning from ventilatory tachycardia during laryngoscopy
support
TOPIC 12: MUSCLE RELAXANT
Tracheostomy technique
• Patient positioned supine with sandbag between scapulae
167. Train of four fade is a characteristic feature of:
• Transverse cervical skin incision 1 cm above sternal notch
A. Depolarizing block
• Incision should extend to the sternomastoid muscles
• Dissect through fascial planes and retract anterior jugular B. Non depolarizing block
veins C. Both depolarizing and non-depolarizing block
• Retract the strap muscles D. Malignant hyperthermia
• Divide thyroid isthmus and oversew to prevent bleeding B
• Place cricoid hook on 2 nd tracheal ring ..........(AIPGMEE - 2008)
• Stoma fashioned between 3 rd and 4 th tracheal rings
• Anterior portion of tracheal ring removed Train of four fade is a characteristic of a non-depolarizing
• No advantage in creating a tracheal flap block
• Endo-tracheal tube withdrawn to sub-glottis
• Tracheostomy tube inserted using obturator What is a Train of Four Stimulation and Fade
• When confirmed that in correct position the ET tube • Train-of-four stimulation denotes administration of four
removed successive 200|is stimuli in 2 seconds (2 Hz)
• Tube secured with tapes • The pattern seen with a depolarizing block differs from
that of a non-depolarizing block
With a non depolarizing block there is progressive
depression of height with each twitch (fade)
With a depolarizing block there is equal depression of all
four twitches
Complications of tracheostomy
Immediate
• Haemorrhage
• Surgical trauma - oesophagus, recurrent laryngeal nerve
• Pneumothorax
Intermediate
• Tracheal erosion
• Tube displacement Train-of-Four
• Tube obstruction
• Subcutaneous emphysema With 2-Hz stimulation, the mechanical or electrical response
• Aspiration & lung abscess decreases little after the fourth stimulus, and the degree
Late of fade is similar to that found at 50 Hz. 43 Thus, applying
• Persistent tracheo-cutaneous fistula train-of-Four stimulation at 2 Hz provides more sensitivity
• Laryngeal and tracheal stenosis than single twitch and approximately the same sensitivity
• Tracheomalacia as tetanic stimulation at 50 Hz. In addition, this relatively
• Tracheo-oesophageal fistula low frequency allows the response to be evaluated manually
HELP LINE NO. 9391567707
TOPIC 12: MUSCLE RELAXANT ANAESTHESIA 33
or visually. Moreover, the presence of a small number of
impulses (four) eliminates the problem of posttetanic
facilitation. Train-of-four stimulation can be repeated every
12 to 15 seconds. There is a fairly close relationship
between single-twitch depression and train-of-four
response, 116 and no control is required for the latter. During
recovery, the second twitch reappears at 80 to 90% single-
twitch block, the third at 70-80%, and when blockade is
65-70%, all four twitches become visible. 117 Then, the
train-of-four ratio, the height of the fourth twitch to that
of the first twitch, is linearly related to first twitch height.
When blockade is <70%. When single-twitch height has
recovered to 100%, the train-of-four ratio is approximately
70%.
169. Drug causing anaphylactoid reaction:
A. Propotol
B. Alcuronium
C. Thiopentone
D. Glycopyrrolate
B
..........(PGI - 1998 - Dec)
• Development of true allergy or antibody formation may of
course occur in days or weeks following exposure to any
Posttetanic count (PTC). During profound blockade, no of non depolarising muscle relaxants (i.e. ALCURONIUM)
response is seen to train-of-four (TOF) or tetanus. • They also cause TACHYPHYLAXIS.
However, because there is posttetanic facilitation, some
twitches can be seen after tetanic stimulation. In this 170. Neostigmine is used for reversing the adverse effect
example, the PTC is 9. of:
A. d - TC + pancuronium
168. Phase -II blocker is: B. d TC only
A. D - TC C. Alcuronium only
B. Cocaine D. Ketamine complication
C. Scoline A
D. Vencuronium ..........(PGI - JUNE 1997)
C
..........(PGI - 1998 - Dec) • By interfering with the breakdown of acetylcholine ,
neostigmine indirectly stimulates both nicotinic and
• Phase - II blocker is scoline muscarinic receptors.
Depolarising muscle relaxants have dual mechanism of • Unlike physostigmine, neostigmine has a quarternary
action (NM Blockade) : nitrogen; hence, it is more polar and does not enter
— Phase - I : Persistent depolarisation of muscle end the CNS. its effect on skeletal muscle is greater than
plate and is rapid onset. that of physostigmine, and it can stimulate contractility
— Phase -II : Slow onset, desensitization of the receptor before it paralyzes.
to acetvlcholine • Neostigmine has short duration of action , usually
• Decamethonium and suxamethonium have these actions. thirty minutes to two hours.
D - TC, Vecuronium are non-depolarising, competitively
block at NM junction on nicotinic (NM)cholinergic receptors, • Neostigmine binds to the anionic site of cholinesterase.
The drug blocks the active site of acetylcholinesterase so
Succinylcholine Tubocuraine the enzyme can no longer break down the acetylcholine
Phase I Phase II molecules before they reach the postsynaptic membrane
Administration of Antagonistic Augmented Additive
receptors. This allows for the threshold to be reached so
tubocuraine a new impulse can be triggered in the next neuron.
Administration of Additive Augmented Antagonistic
Succinylcholine • In myasthenia gravis there are too few acetylcholine
receptors so with the acetylcholinesterase blocked,
Effect of neostigmine Augmented1 Antagonistic Antagonistic
acetylcholine can bind to the few receptors and trigger a
Initial excitatory effect Fasciculations None None muscular contraction.
on skeletal muscle
Response to a tetanic Sustained2 Unsustained Unsustained • It is used to improve muscle tone in people with myasthenia
stimulus
gravis and routinely, in anesthesia at the end of an
Posttetanic facilitation No Yes Yes operation, to reverse the effects of non-depolarizing
Rate of recovery 4-8 min > 20 min 3 30-60 min 3 muscle rel axants such as rocu ronium and
vecuronium.
HELP LINE NO. 9391567707
TOPIC 12: MUSCLE RELAXANT ANAESTHESIA 34
• It can also be used for urinary retention resulting from
general anaesthesia and to treat curariform drug • Shortest acting competitive(non Mivacurium (duration
toxicity. depolarizing) neuromuscular of action 12-18
blocker minutes)
• Another indication for use is the Ogilvie syndrome which
is a pseudoobstruction of the colon in critically ill patients. • Fastest acting non-depolarizing Rocuronium
blocker
• Historically, it has been used as a test for early pregnancy.
In a non-pregnant female whose menstrual period is • Shortest and fastest acting Succinylcholine
delayed, administration of neostigmine can provoke neuromuscular blocker (overall)
menstrual bleeding. Modern tests which rely on detecting • Longest acting neuromuscular Pancuronium
hCG in urine have rendered this application obsolete. blocker
• Neostigmine will cause slowing of the heart rate
(bradycardia), for this reason it is usually given along • Histamine release is d-TC maximum tendency,
with a parasympatholytic drug such as atropine or caused by Succinylcholine, Mivacurium,
glycopyrrolate. • Virtually no histamic Pancuronium
release
171. True about Non-depolarizing muscle relax ants: • Maximal vagal block and Pancuronium
A. Competitive inhibitor of acetylcholine T achycardia
B. Metabolised by pseudocholinesterase • Vagal stimulation is caused Succinylcholine
C. Mg2+ predisposes the block by
D. Ca2+ antagonizes the block • Maximal ganglion blockade d-TC
is caused by
E. Hypothermia prolongs the block
• Ganglion stimulation is Sucinylcholine
A, C, D & E
caused by
..........(PGI - JUNE 2005)
* Char acteristics features of Nondepol arizing • Most commonly used muscle relaxant Vecuronium
neuromuscular blocking drugs : for routine surgery
- They are competitive blockers & compete with Ach for • Most potent skeletal muscle relaxant Doxacurium
the end plate r eceptors but without causing • Least potent skeletal muscle relaxant Succinycholine
depolarization. • Least potent non-depolarizing skeletal Rocuronium
muscle relaxant
- Acts by preventing the access of Ach to the cholinergic
receptor, which are responsible for muscular tone & 173. Muscle relaxant excreted exclusively by kidney is:
contraction. A. Scoline
- Do not cause muscular fasciculation. B. Atracurium
- Relatively slow onset (1-5 min). C. Vecuronium
- Among all the non-depo larizing relaxants, on ly D. Gallamine
D
Mivacurium is metabolized by pseudocholinesterase. ’
..........(AIIMS PGMEE - JUNE 1998)
- Reversed by neostigmine & other anticholinesterases.
- Effects reduced by adrenaline & Ach. Gallamine
- The relaxed muscles still responsive to other (mechanical
& electrical ) stimuli. • “Urinary Excretion of Gallamine is > 95%.
- Block is potentiated by volatile agents, Mg 2+ & • Its billiary excretion is < 1%”.
hypokalemia. • Gallamine
- Ca 2+ enhances the release of Ach from the motor nerve • It is nephrotoxic so C/I in Renal Failure*.
terminal & enhances excitation-contraction coupling in • It crosses placenta so C/I in Pregnancy*.
muscles thus partially antagonizing the block
- mild cooling antagonizing the block, but greater cooling • M.R. undergone Hoffman’s elimination —-Atracurium
(<33° c) potentiates the block. • M.R. of choice in Renal failure & Hepatic failure
• Atracurium
- Acidosis increases duration & degree of the block.
• Atracurium is a neuromuscular-blocking drug or
172. Shortest acting NDMR: skeletal muscle relaxant in the category of non-
A. Succinyl choline depolarising neuromuscular blocking agents, used
B. Rapacuronium adjunctively in anaesthesia to facilitate endotracheal
C. Atracurium intubation and to provide skeletal muscle relaxation
D. Pancuronium during surgery or mechanical ventilation.
B • Side effects owing to histamine liberation are rash,
..........(AIIMS PGMEE - MAY 2008) reflex increase in heart rate, low blood pressure and
bronchospasm.
• Rapacuronium is the shortest ating drug.
• Rapacuronium has been withdrawn from the market • M.R. causing maximum Histamine release
• —d-TC*
because it produces intense bronchospasm in a
• M.R. causing minimum Histamine release —
significant number of patients.
Vecuronium*
• Alcuronium is a relatively short acting muscle relaxant.
HELP LINE NO. 9391567707
TOPIC 12: MUSCLE RELAXANT ANAESTHESIA 35
• M.R. C/I in Hepatic failure They binds to ach receptors like acetycholine but are
• d-TC, Pancuronium, Scoline* incapable of inducing ion channel opening.
Since acetycholine is prevented from binding to its receptors
no end plate potential develops.
In this way they act as competitive antagonist of
acetycholine.
• M.R. used in Bronchial Asthma
• Atracurium & Vecuronium
Non depolarizing muscle relaxants are -
Long acting Intermediate Short acting
acting
Tubocurarine Atracurium Mivacurium
Metocurine Cisatracurium Rapacuronium
Doxacurium Vecuronium
Pancuronium Rocuronium
Pipecuronium
Gallamine
A summary of the pharmacology of nondepolarizing Depolarizing muscle relaxant
muscle relaxants. These drugs physically resemble Ach and therefore bind
to Ach receptors generating a muscle action potential
Relaxant Chemical Metabolism Primary Onset2 Duration3 Histamine Vagal but unlike Ach these drugs are not metabolized by
Structure1 Excretion Release4 Blockade5
Atracurium B +++ Insignificant ++ ++ + 0
acetylcholinesterase and their concentration in the
Cisatracurium B +++ Insignificant ++ ++ 0 0 synaptic cleft does not fall as rapidly . This results in
Mivacurium B +++ Insignificant ++ + + 0 continuous prolonged depolarization of muscle end phase.
Doxacurium B Insignificant Renal + +++ 0 0
Pancuronium S + Renal ++ +++ 0 ++
Pipecuronium S + Renal ++ +++ 0 0
V ecuronium S + Billary ++ ++ 0 0
Rocuronium S Insignificant Billary +++ ++ 0 +
1B, benzylisoquinoline; s, steroidal.
Drug ED95 for Intubation Onset of Duration Maintenance Maintenance
Adductor Pollicis Dose Action for of Dosing by Dosing by
During N2/O2 (mg/kg) intubating Intubating Boluses Infusion
Anesthesia Dose Dose (mg/kg) (mg/kg/min)
(mg/kg) (min) (min)
Succinylcholine 0.5 1.0 0.5 5-10 0.15 2-15 mg/min
Rocuronium 0.3 0.8 1.5 35-75 0.15 9-12
Mivacurium 0.08 0.2 2.5-3.0 15-20 0.05 4-15
Atracurium 0.2 0.5 2.5-3.0 30-45 0.1 5-12
Cisatracurium 0.05 0.2 2.0-3.0 40-75 0.02 1-2
175. Cardiovascular side effects are minimal with
A. Pancuronium
Vecuronium 0.05 0.12 2.0-3.0 40-90 0.01 1-2
Pancuronium 0.07 0.12 2.0-3.0 60-120 0.01 -
Pipecuronium 0.05 0.1 2.0-3.0 80-120 0.01 - B. Rocuronium
Doxacurium 0.025 0.07 4.0-5.0 90-150 0.05 - C. Doxacurium
D. Vecuronium
174. The neuromuscular blocking action of Curare is E. Mivacurium
brought about by B,C & D
A. Blocking Acetylcholine synthesis ..........(PGI - DEC 2002)
B. Preventing the release of Acetylcholine
C. Causing persistent depolarization 176. Which one of the following muscle relaxant has
D. Competitive inhibition the maximum duration of action?
D A. Atracurium
..........(AIIMS PGMEE - MAY 2004) B. Vecuronium
C. Rocuronium
Curare are also called non depolarizing muscle relaxants. D. Doxacurium
Non depolarizing muscle relaxants competitively inhibit D
acetylcholine ..........(AIPGMEE - 2006)
HELP LINE NO. 9391567707
TOPIC 13: PROPOFOL ANAESTHESIA 36
TOPIC 13: PROPOFOL 179. Which of the following statements about propofol
is not true?
A. It is contraindicated in porphyria
B. It does not trigger malignant hyperthermia
C. Commercial preparations contains egg
D. It is a suitable agent for day care surgery
A
..........(AIPGMEE – 2008)
Propofol can be used safely in porphyria & malignant
hyperthermia
• Propofol is an oil based preparation containing egg
177. The following combination of agents are the most lecithin
preferred for short day care surgeries It is an alkylphenol, 2, 6-Disopropylphenol.
A. Propofol, fentanyl, isoflurane It is highly soluble in lipid but insoluble in water so it is presented
B. Thiopentone sodium, morphine, halothane
as a 1 or 2 percent emulsion in 10 percent soyabean oil
C. Ketamine, pethidine, halothane
with 1.2 percent egg phosphatide as the emulsifying
D. Propofol, morphine, halothane
agent
A
The addition of disodium edetate (0.005%) supresses
..........(AIIMS PGMEE MAY - 2003), AIPGMEE – 2006
bacterial growth.
AIPGMEE – 2004, AIPGMEE - 2003
• Propofol is considered the agent of choice for day
For day care surgery patients are sent back home the same
care anaesthesia.
day. Therefore you need agents which are rapidly
Smooth induction, rapid onset of action , easy
eliminated so that no after effects are left. The agents
used are- titration to effect, short clinical duration of action and
- Propofol demonstr able antiemetic effect make propofol an
- Alfentanil induction agent of choice for day care anaesthesia.
- Remifentanil
- N 20 • Propofol is non contraindicated in porphyria
- Isoflurane Propofol is considered safe in porphyria -
- Sevoflurane
- Desflurane • Propofol does not trigger Malignant Hyperthermia
Propofol has been recommended as the agent of choice
‘Propofol is the intravenous induction agent of choice ’ for induction is susceptible individuals for malignant
because of its early induction and smooth recovery. hyperthermia
Patients remain clear headed and have low incidence of
post operative nausea and vomiting. 182. A 38 year old man is posted for extraction of last
molar tooth under general anaesthesia as a day care
case. He wishes to resume his work after 6 hours.
Which one of the following induction agents is
preferred:
A. Thiopentone sodium
B. Ketamine
C. Diazepam
D. Propofol
D
..........(AIPGMEE - 2003)
The patient in question wishes to resume his work after
Day case surgery Agent of choice 6 hours and hence needs a day care anaesthetic agent
Intravenous induction Propofol that has the advantage of rapid recovry and little incidence
agent of post recovery compilations. Propofol as described above
Desflurane >Isoflurane is such an agent of choice.
Inhalation induction
agent Alfentanyl Remifentanyl
Intravenous opioid 183. True about Propofol
analgesia
Mivacurium A. It suppress adrenocortical hormone
B. I.M. injection is not painful
Muscle relaxants C. Hepatic metabolism
D. Di-isopropyl phenol
Agents used in day care anaesthesia include : E. Cerebral protector
1. Propofol B, C, D & E
2. Alfentanyl, Remifentanyl ..........(PGI - DEC 2005)
3. Isoflurane, Sevoflurane, Desflurane
4. Methohexitone
* Propofol (2, 6 - diisopropyl phenol) is an intravenous
5. Thiopentone
anaesthetic agent.
6. Etomidale
HELP LINE NO. 9391567707
TOPIC 14: ISOFLURANE ANAESTHESIA 37
* The main disadvantage in the use of propofol is the age; maintenance of general anesthesia in adult patients
production of pain on its injection into small veins. and pediatric patients older than 2 months of age; and
This can be decreased by selecting larger veins or by prior sedation in medical contexts, such as intensive care
administration of 1% Lidocaine or a potent short-acting unit (ICU) sedation for intubated, mechanically
opioid. ventilate d adults , and in proce dures such as
* Propofol metabolism in the liver is rapid & extensive. colonoscopy.
* Propofol reduces cerebral metabolic rate of oxygen • It provides no analgesia
(CMRO2) without reduction of cerebral perfusion
pressure (CPP), producing cerebral protection. • 20 ml ampoule of 1% propofol emulsion
• A common hospital-worker slang term for Propofol is “Milk
• Etomidate is also an anaesthetic agent which of Amnesia/Milk of Anesthesiologists
suppresses the secretion of cortisol.
184. A 20-year-old patient presented with early
pregnancy for Medical Termination of Pregnancy
(MTP) in day care facility. What will be the anesthetic
induction agent of choice?
A. Thiopentone
B. Ketamine
C. Propofol
D. Diazepam
C
..........(AIIMS PGMEE - MAY 2006)
Rapid induction of propofol is due to its high Iipid solubility
and rapid recovery is due to very short distribution.
185. The following anaesthetic drug causes pain on • The elimination half-life of propofol has been estimated
intravenous adminstration: to be between 2–24 hours. However, its duration of clinical
A. Midazolam effect is much shorter because propofol is rapidly
B. Propofol distributed into peripheral tissues , and its effects
therefore wear off considerably within even a half
C. Ketamine
hour of injection.
D. Thiopentone sodium
• This, together with its rapid effect (within minutes of
B
injection) and the moderate amnesia it induces makes
..........(AIIMS PGMEE - MAY 2006) it an ideal drug for IV sedation .
• Aside from the hypotension (m ainly through
• it is intraarterial (not intravenous) injection of vasodilatation) and transient apnea following
thiopentone, that causes intense pain. induction doses
• Intraarterial injection of thiopentone induces severe • one of propofol’s most frequent side effects is pain on
inflammatory and potentially necrotic reaction and injection, especially in smaller veins. This pain can be
should be avoided. Its intravenous injection does not mitigated by pretreatment with lidocaine.
produce pain. • Patients tend to show great variability in their
• Intravenous injection of propofol frequently response to propofol , at times showing profound
produces pain. sedation with small doses.
• Propofol has been known to cause an adverse reaction in
186. Induction agent for Day care Surgery is: some patients, known cases include myoclonia and
A. Ketamine dystonia. Note this is extremely rare.
B. Diazepam • Propofol appears to be safe for use in porphyria , and
C. Thiopentone has not been known to trigger malignant hyperpyrexia.
D. Propofol • A recently described rare but serious side effect is
D propofol infusion syndrome . This potentially lethal
..........(AIIMS PGMEE - DEC 1998) metabolic derangement has been reported in critically-
ill patients after a prolonged infusion of high-dose
propofol in combination with catecholamines and/
Propofol
or corticosteroids
• “Propofol is used as in inducing agent for day care
TOPIC 14: ISOFLURANE
surgery because residual impairment is less marked and
incidence of post operative nausea and vomiting is low.” 187. In raised intracranial tension, anaesthetic agent
used is
• Day care anaesthesia −−− Isoflurane A. Nitrous oxide (N2O)
• Day care analgesic −−− Alfentanyl B. Trichloroethylene
C. Enflurane
• Propofol is a short-acting intravenous anesthetic D. Isoflurane
agent used for the induction of general anesthesia in D
adult patients and pediatric patients older than 3 years of ..........(AIIMS PGMEE - MAY - 1994)
HELP LINE NO. 9391567707
TOPIC 14: ISOFLURANE ANAESTHESIA 38
“All inhalational agents are cerebral vasodilators this • Isoflurane may cause coronary steal phenomenon , it is
vasodilation causes increase in blood flow which powerful caronary dilator
causes increase in intracranialpressure.”
Among the inhalational agents Isoflurane causes the least
increase in cerebral blood flow. Therefore it is most
suitable inhalational agents in increased intracranial
pressure.
Isoflurane -
- It has got least effect on heart
- Agent of choice in renal and hepatic failure
- It has got rapid induction and recovery
- Pupils do not dilate and light reflex in not lost even at
deeper levels.
- It does not provoke seizures
• Isoflurane is the preferred agent for neuro surgical
It produces profound respiratory depression
anaesthesia as in Low concentration it does not cause
any increase in cerebral blood flow.
188. Which of the following statements about inhalation
anesthetic agents is wrong?
A. Sevoflurane is more potent than isoflurane
B. Sevoflurane is less cardiodepressant than isoflurane
C. Desflurane has lower blood-gas partition coefficient than
sevoflurane
D. Sevoflurane has a higher MAC than isoflurane
A&D
..........(AIPGMEE - 2008)
Compared with isoflurane, sevoflurane is less potent
and lacks coronary vasodilating properties’
189. Which anaesthetic agent ha s the least
cardiovascular effect: • Isoflurane is used is day care surgery.
A. Isoflurane
B. Enflurane
C. Tnlene
D. Ketamine
A
..........(AIPGMEE - 2000)
Isoflurane
• Of the various inhalation agents available, isoflurane has
the advantage of providing stability to cardiac rhythm and
the lack of sensitization of heart to exogenous or • Isoflurane is always administered in conjunction with
endogenous adrenaline air and/or pure oxygen . Often nitrous oxide is also used.
• It causes less myocardial depression than halothane on
enflurane. Isoflurane for maintainence not induction
It thus causes the least alternation of cardiovascualar • Although its physical properties means that anaesthesia
status. can be induced more rapidly than with halothane ,
its pungency can irritate the respiratory system, negating
this theoretical advantage conferred by its physical
properties.
• It is usually used to maintain a state of general anesthesia
that has been induced with another drug, such as
thiopentone or propofol.
• It vaporizes readily, but is a liquid at room temperature.
• It is completely non-flammable.
• Isoflurane reduces pain sensitivity (analgesia) and
relaxes muscles
190. Anaesthetic agent of choice in renal failure is:
A. Methoxyflurane
B. Isoflurane
C. Enflurane
D. None of the above
B
..........(AIPGMEE - 2001)
HELP LINE NO. 9391567707
TOPIC 15: OPIOIDS ANAESTHESIA 39
Isoflurane ‘Of the various inhalation agents available, isoflurane
• Methoxyflurane has a high nephrotoxic potential has the advantage of providing stability of cardiac
• Enflurane is best avoided as nephrotoxic levels of rhythm and lack of sensitization of the heart to
fluoride ions have been seen just after 3.5 MAC-hours. exogenous and endogenous adrinaline.’ -
• Isoflurane, sevoflurane, desflurane and halothane result Isoflurane is stable and unlikely to be toxic.
in little or no increase in fluoride levels and are
preferred. 194. Fluoride content is least:
A. Methoxyflurane
191. A man with alcoholic liver failure requires general B. Enflurane
anesthesia for surgery. Anaesthetic agent of choice C. Isoflurane
is: D. Sevoflurane
A. Ether C
B. Halothane ..........(PGI - 1997 - Dec)
C. Methoxyflurane
D. Isoflurane Among all the fluorinated anesthetic agents mentioned here,
D isoflur ane is having the least fluori de content &
..........(AIPGMEE - 2001) methoxyflurane is having the highest amount of fluoride
content.
Isoflurane The higher the fluoride content, the more the side effect
of the drug.
Anaesthesia in chronic alcoholism :
Chronic alcoholism damages the liver but also induces drug TOPIC 15: OPIOIDS
metablism enzymes so the response to drugs is not
always predictable. 195. Neurolept analgesia all are true except:
A. Can be used along with N2 0 oxygen
Common agent employed include : B. Causes focal dystonia
• Midazolam is useful for sedation. C. Fentanyl - droperidol
• Regional analgesia should be considered D. Causes hypotension
• Isoflurane or sevoflurane are suitable anaesthesitc NONE
agents. ..........(PGI - 1998 - Dec)
• The perioperative use of certain narcotic opioids such as • ‘Neurolept analgesia’ is Fentanyl and droperidol combination
morphine and oxycodone should be avoided in and when 65% N2 O + 35% O 2 is adminstered it is
patients with cirrhosis, because their bioavailability is converted to ‘Neurolept anaesthesia’.
markedly increased and their half-life prolonged.[6] By • Muscle dystonia, abnormal movements can occur as an
contrast, metabolism of fentanyl does not seem to extrapyramidal side effect of droperidol .
be affected by hepatic dysfunction . • Fall in BP (due to a—adrenergic blocking action of
droperidol) is generally slight unless hypovolemia is
• The metabolism of certain benzodiazepines (such as present or patient’s posture is changed .
midazolam and diazepam) can also be slowed in patients Heart rate often decreases (fentanyl stimulates vagus)
with cirrhosis, whereas oxazepam and temazepam but heart is not sensitized to adrenaline.
undergo conjugation without hepatic metabolism • Droperidol sometimes cause hypotension.
and their clearance rate is, therefore, not affected .
196. Best antagonist of Morphine
•
In patients with hepatic dysfunction, the increased A. Pentazocine
duration of action of benzodiazepines and narcotics B. Buprenorphi ne
can lead to prolonged depression of the central C. Naloxone
nervous system and hepatic encephalopathy ; these D. Nalorphine
agents should, therefore, be used with caution in the C
perioperative setting. ..........(AIIMS PGMEE - JUNE - 1997)
• Of the volatile anesthetics, isoflurane is generally
recommended as it undergoes the least amount of Naloxone
hepatic metabolism and does not impair hepatic blood
flow. • T/t of choice for morphine poisoning is Naloxone (6
• By contrast, halothane undergoes significant hepatic mg.IV) repeated every 3 min till respiration picks up)
metabolism and reduces hepatic blood flow. Halothane • It is preferred due to no agonistic action and no
anesthesia carries with it a significant risk of drug-induced respiratory depression.
hepatitis • Nalorphine is given only when Naloxone not available
192. Least Cardiotoxic anaesthetic agent 197. Which of the following opioids is not given
A. Enfluranc intrathecally
B. Isoflurane A. Remifentanil
C. Sevoflurane B. Morphine
D. Halothane C. Sufentanil
B D. Fentanyl
..........(AIPGMEE - 1996), AIPGMEE - 1998 A
..........(AIPGMEE - 2007)
HELP LINE NO. 9391567707
TOPIC 15: OPIOIDS ANAESTHESIA 40
Remifentanil is not used intrathecatly because glycine in the 201. Which one of the following is the description used
drug vehicle can cause temporary motor paralysis. It is for the term allodynia during pain management?
generally given by continuous, intravenous infusion, A. Absence of pain perception
Opioids such as Morphine, Diamorphine, P ethiden B. Complete lack of pain sensation
(Meperidene), Fentanyl and Sufentanil may all be used C. Unpleasant sensation with or without a stimulus
intra thecally D. Perception of an ordinarily nonnoxious sitmulus as severe
pain
198. Drug with Ceiling effect D
A. Morphine ..........(.AIIMS PGMEE - MAY 2006)
B. Buprenorphine
C. Fentanyl Terms used in pain management
D. Mfentanyl Allodynia Perception of an ordinarily nonnoxious
B stimulus as pain
..........(AIPGMEE - 1994) Analgesia Absence of pain perception
Anaesthesia Absence of all sensations
Buprenorphine is most potent opoid used for epidural
Analgesia. Dysesthesia Unpleasant or abnormal sensation with or
without a stimulus
Because of its ceiling effect and poor bioavailability,
buprenorphine is safer in overdose than opioid full agonists Hypalgesia Diminished response to noxious
stimulation
• Advantages of buprenorphine in the treatment of chronic Hyperalgesia Increased response to noxious stimulation
pain are, from a clinical perspective, its relatively long half- Hyperaesthesia Increased response to mild stimulation
life, the option of sublingual and transdermal application Hyperpathia Presence of hyperaesthesia, allodynia and
and the excellent safety profile (ceiling effect for hyperalgesia usually associated with
respiratory depression, lack of immunosuppressive overreaction and persistence of sensation
effect, low pharmacokinetic interaction potential, after the stimulus
no accumulation in renal impairment Hypoaesthesia Reduced cutaneous sensation (e.g. light
touch, pressure or temperature)
199. 0.5 mg Buprenorphine equivalent of: Neuralgia Pain in the distribution of a nerve or a
A. 10 mg tramadol group of nerves.
B. 6 mg morphine Paresthesia Abnormal sensation perceived without an
C. 75mg of pentazocine apparent stimulus
C Radiculopathy Functional abnormality of one or more
..........(PGI - JUNE 2006) roots
• The potency of opioids in mg, relative to lOmg of 202. A 52 year old male diagnosed as triple vessel
morphine are: coronary artery disease with poor left ventricular
Pentazocine = 30 mg function. Coronary artery bypass grafting surgery
Nalbuphine = 10 mg was decided. During maintenance of anaesthesia
Butorphanol = 2 mg which one of the following agents should be
Buprenorphine = 0.2 mg preferred?
Dezocine =10 mg A. IV Opioids
Meptazinol = 100 mg B. Isoflurane
Pethidine (Meperidine) = 75 mg C. Halothane
Fentanyl =0.1 mg D. Nitrous oxide
Sufentanil = 0.01 mg A
Alfentanil = 1 mg ..........(AIIMS PGMEE - NOV 2004)
Methadone = 10 mg
Tramadol = 100 mg Maintenance anaesthesia in patients with coronary
So, 0.5 mg of Buprenorphine = 25 mg of Morphine = 250mg heart disease.
of Tramadol = 75mg of Pentazocine. - Isoflurane is the most common maintenance anaesthesia
used in these cases, but doubts have been raised regarding
200. Which one of the common side effects is seen with its safety in patients with coronary artery disease.
fentanyl?
A. Chest wall rigidly - Isoflurane causes vasodilatation of coronary
B. Tachycardia arteries, so it is feared that it can cause coronary
C. Pain in abdomen steal phenomenon.
D. Hypertension - Isoflurane also causes minimal cardiac depression.
A Many anaestheists believe that opioids are better in these
..........(AIIMS PGMEE - MAY 2006) cases, opioids do not have any direct depressant on heart
and are also helpful in cases of heart failure.
Opioids (particularly Fentanyl, Sufentanil and
Alfentanil) can induce chest wall rigidity severe The major disadvantage with the use of opioids is patient
enough to prevent adequate ventilation. awareness and respiratory depression.
This centrally medicated muscle contraction is most frequent The prospective clinical trials on isoflurane have not been
after large drug boluses and is effectively treated with able to prove that it causes coronary steal.
neuromuscular blocking drugs.
HELP LINE NO. 9391567707
TOPIC 16: BUPIVACAINE ANAESTHESIA 41
Coronary heart disease patients is 205. Cholinesterase metabolizes following except:
Pts with poor Left ventricular function A. Propanidid
“Maintenance anaesthesia of choice is — I.V. opioids B. Procaine
Pts with good Left ventricular function C. Acetyl choline
Maintenance anaesthesia of choice is — Isoflurane
D. Bupivacaine
Advantages of Isoflurane in patients with CHD D
• They reduce myocardial O2 requirement ..........(PGI - 1997 - Dec)
• Protective role in reperfusion injuries Disadvantages of
Isoflurane in patients with CHD Bupivacaine is not metabolized by cholinesterase. Rest of the
• Negative inotropic effect drugs are metabolized by cholinester ase & causes
• Cause coronary vasodilatation that can lead to coronary
hydrolysis.
steal
• Tachycardia and hypotension
207. Which of the following is long acting local anesthetic
Advantage of i.v. opioids in patients with CHD > 2 hrs
• They do not have any direct depressant effect on heart A. Bupivacaine
• There is no effect on Contractility Automaticity Conduction B. Prilocaine
sensitivity to catecholamines
Due to these advantage, i.v. opioids have become the C. Etidocaine
mainstay of anaesthesia in pts with poor left ventricular D. Lignocaine
function. A&C
..........(PGI - DEC 2005), PGI - 2000 - Dec
Disadvantages of i.v. opioids
• Patient awareness Procaine 30-60
• Prolonged respiratory depression, postoperatively
• Opioids also fail to consistently control the hypertensive Lignocaine 60-120
response to stimulation. T etracaine 180-480
203. Which one of the following is the shortest acting Bupivacaine 180-600
intravenous analgesic:
A. Remifantanil. Repivacaine 180-360
B. Fentanyl. Etidocaine 240-480
C. Alfentanil.
D. Sufentanil • Bupivacaine
A
..........(.AIIMS PGMEE MAY - 2003) Metabolism Hepatic
All of these are included in short acting narcotic analgesics.
Half life 3.5 hours (adults)
This shortest acting among them is Remifentanil. 8.1 hours (neonates)
Onset Duration Excretion Renal, 4-10%
Remifentanil 30s - 60s 5-5 minutes
* Prilocaine is having intermediate duration of action like
Alfentanil 0.5 m 5-10 minutes
lignocaine.
Fentanyl 1-4 min 30 min
Sufentanil 1-4 min 30 min
208. Bupivacaine
TOPIC 16: BUPIVACAINE A. Less cardiotoxic than prilocine
B. It is an amide
204. The topical use of following local anesthetic is not
C. The max dose tolerable is 8 mg/kg/ body wt
recommended
D. Duration more than 2 hrs
A. Lignocaine
B. Bupivacaine B&D
C. Cocaine ..........(PGI - DEC 2005)
D. Dibucaine
B • Bupivacaine is an amide type local anaesthetic drug.
..........(AIIMS PGMEE NOV - 2002) – It is reputed to be four times as potent as both Mepivacaine
& Lignocaine.
Local anaesthetics * It is more cardiotoxic than other local anaesthetics & is
Used as surface Can not be used as surface made worse by hypoxia, hypercapnia & by pregnancy.
anaesthetics anaesthetics So, it is not used for I.V. regional anaesthesia (Bier’s block)
(a) Cocaine (a) Bupivacaine .
(b) Lidocaine (b) Procaine * It causes more sensory than motor block & its duration
(c) Dibucaine (c) Mepivacaine of effect is between 5 & 16 hr.
(d) T etracaine Maximum safe dose that can be used is 2 mg/kg.
(e) Benzocaine
HELP LINE NO. 9391567707
TOPIC 17: PIN INDEX ANAESTHESIA 42
209. Levo-bupivacaine is administered by which of ; TOPIC 17: PIN INDEX
following routes
A. Nasogastric
B. Epidural
C. Intra-venous
D. Intra-theccal
E. Oral
B
..........(PGI - JUNE 2004)
• Commercial bupivacaine is a racemic mixture of both ‘R’ &
‘S’ isomers.
Levobupivacaine is as effective as racemic one & being ‘S’
isomer has the potential for reduced toxicity.
It can be used by the following routes.: 212. Pin index system is a safety feature adopted in
- Intrathecal anaesthesia. Machines to prevent:
A. Incorrect attachment of anaesthesia machines.
- Epidural
B. Incorrect attachment of anaesthesia face masks.
- Peripheral nerve blocks C. Incorrect inhalation agent delivery.
• Bupivacaine is more prone to induce cardiac arrythymia & D. Incorrect gas cylinder attachment
should not be used for IV regional anaesthesia. D
..........(.AIIMS PGMEE MAY - 2003)
210. Which one of the following local anaesthetics is
highly cardio-toxic: To understand this and the next question you are required
A. Lignocaine to have a preliminary knowledge of Boyle anaesthesia
B. Procaine machine.
C. Mepivacaine Boyle anaesthesia machine is a continuous flow type of
machine used for administration of inhalational anaesthesia.
D. Bupivacaine
It is equipped with two oxygen cylinders, two nitrous
D oxide cylinders, one carbondioxide cylinder and one
..........(AIIMS PGMEE - MAY 2005) cyclopropane cylinder.
211. A 30-year-old lady is to undergo surgery under These cylinders are locked to Boyle apparatus in metal
intravenous regional anesthesia for her left ‘trigger yoke with two pins and fiting holes on the cylinder
finger’. Which of the following should not be used head.
for this patient Each cylinder has a particular pin code and unless the
A. Lignocaine correct cylinder valve is attached the pins and holes will
not coincide. Thus it is practically impossible to fit any
B. Bupivacaine
cylinder to wrong yokes.
C. Prilocaine
D. Lignocaine + Ketorolac
B
..........(AIIMS PGMEE - MAY 2004)
Intravenous regional anaesthesia or Bier’s block is used
for producing intense surgical anaesthesia for short surgical
procedures of the forearm and hand.
An esmarch bandage or an orthopaedic pneumatic splint
is used to compress the arm or the forearm.
213. The Pin index code of Nitrous oxide is:
The anaesthetic is inserted on the dorsum of the hand through A. 2,5.
an intravenous catheter. B. 1,5.
This techqnique is most commonly used for carpal tunnel C. 3,5.
release. D. 2,6
C
..........(.AIIMS PGMEE MAY - 2003)
Local aneasthetics used are –Lidocaine ,Prilocaine
Local anaesthetic contraindicated - Bupivacaine
Pin index for the following gases are-
{because of its potential side effects). • Nitrous oxide -> 3 and 5
• Oxygen -> 2 and 5
Bupivacaine prolongs QTC and cause ventricular • Cyclopropane -> 3 and 6
tachycardia or cardiac depression. • Carbondioxide -> 1 and 6
The site of action of drug in this technique is peripheral International colour code for cylinders
nerve ending. • Oxygen* -> black with white shoulders
• Nitrous oxide* -> Blue
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 43
• Carbon dioxide* -> Gray • N2O is a colourles, odourless, heavier than air, non-
• Cyclopropane* -> Orange inflammable gas supplied under pressure in steel cylinders
• Colour of cylinder is blue
214. For High Pressure Storage of compressed gases, • Pressure of cylinder is 750 Ib/sq. inch (Psi)
Cynlinders are made up of: • Pin-index is 3, 5
A. Molybdenum steel MAC-value between 100% and 105%
B. Iron + molybedenum
C. Cooper + steel
D. Iron
A
..........(AIPGMEE - 2000)
Molybdenum steel
“Cylinders are made of molybdenum steel”
• Comparison of different medical gases commonly used are
:
Gas Colour Of Pin Index State In Pressure Volume Filling
Cylinder Cylinder Density
Oxygen White 2,5 Gas 1900 660l ' 68%
Psig
Nitrous Blue 3,5 Gas
Oxide Liquid < 745 Psig 1590
98°f
218. All of the following are used to maintain proper
215. An anaesthetist orders a new attenant to bring oxygen flow to the patient except:
the oxygen cylinder. He will ask the attendant to A. Placement of nitrogen flowmeter downstream of the
identify the correct cylinder by following color code: oxygen flowmeter
A. Black cylinders with white shoulders B. A proportionater between N2 and O2 control valve
B. Black cylinders with grey shoulders- C. Different pin index for nitrogen and oxygen
C. White cylinders with black shoulders D. Calibrated oxygen concentration analyses
D. Grey cylinder with white shoulders C
A ..........(AIIMS PGMEE - MAY 2008)
..........(AIPGMEE - 2003)
• Pin index safety system for cylinders prevents incorrect
cylinder attachments.
Gas Colour of Cylinder
Oxygen Black body, white It is a safeguard introduced to eliminate cylinder
shoulder interchanging and the possibility of accidently
placing the incorrect gas on a yoke designed to
Air Grey body, black and
accomodate another gas.
white shoulder It has nothing to do with hypoxia.
N2O Blue
The systems used to prevent
Entonox (O2 and N2O Blue body, white and hypoxia:-
mixture in equal blue quartered shoulder Low oxygen pressure alarm It detects oxygen supply failure at
volume) the common gas inlet that activates
a gas whistle or electric alarm
Cyclopropane Orange Minimum oxygen/nitrous oxide Prevent delivery of less than 21 %
Carbondioxide Grey ratio controller device (hypoxic oxygen
guard)
Thiopentone Y ellow Oxygen must enter the common Prevent hypoxia in event of
manifold down-stream to other proximal gas leak
Halothane Amber (Purple - Red) gases
Oxygen concentration monitor Prevents administration of hypoxic
217. True about N2O cylinder and alarm gas mixtures in event of a low
A. Pressure is 2200 PSI pressure system leak; precisely
B. Blue in colour regulate oxygen concentration
C. Gas in liquid form
D. Pin index 3.5 TOPIC 18: MAC
E. It is flammable
B,D 219. Partition coefficient of gas:
..........(PGI - JUNE 2004), (PGI - 2000 - Dec) A. Measure of potency
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 44
B. Directly proportional to potency response to a painful stimulus (surgical incision) in 50%
C. Measures solubility individuals. It is accepted as a valid measure of potency
D. All of the above of inhalational GAs because it remain fairly constant for
C a given species even under varying conditions.
..........(PGI - June -1998)
222. Characteristic of an ideal gas is:
• Blood/Gas partition co-efficient is the ratio (at equillibrium) A. Volume is directly proportional to change in pressure
of concentration in blood to that in Gas. B. Volume is inversely proportional to change in temperature
• It measures the solubility of the gas. C. At absolute temp, volume of gas is 1
The MAC (minium alveolar concentration) measures the D. Obeys charles, boyles and avagadro’s laws
potency of inhalational anaesthetics. D
The MAC of a no. of GAS shows excellent correlation ..........(PGI - June -1998)
with their oil/gas partition co-efficient.
• An ideal gas obeys charle’s, boyle’s and avogadro’s law.
For a highly soluble gas-alveolar concentration can rise Boyle’s Law :- Volume (V) is inversely proportional to the
SLOWLY where as a low soluble gas-the alveolar pressure.
concentration rises RAPIDLY so, there is an inverse Charles’s Law :- Volume of a given mass of gas is proportional
relationship. to its^absolute Temperature if pressure remains constant.
220. All of the following factors decrease the Minimum 223. The potency of an Inhalational anesthetic depends
Alveolar Concentration (MAC) of an inhalation on:
anaesthetic agent except. A. Blood gas partition co-efficient
A. Hypothermia B. Oil-gas partition co-efficient
B. Hyponatremia C. Gas pressure
C. Hypocalcemia D. Blood pressure
D. Anemia B
C ..........(PGI - June -1999)
..........(AIIMS PGMEE MAY - 2003)
• The physical property of anaesthetic that correlates best
Minimum alveolar concentration with anaesthetic potency is the lipid solubility (i.e., oil-gas
- Is the concentration of anaesthetic gas needed to partition co-efficient), whereas the best estimate of
eliminate movements among 50% of patients challenged anaesthetic potency is the minimum alveolar concentration
by standardized skin incision. The MAC is usually expressed (MAC) (at 1 atm) of an agent that produces immobility in
as percentage of gas in a mixture required to achieve the 50% of those subjects exposed to a noxious stimulus.
effect. The MAC of a number of GAs partion coefficient shows
excellent correlation with their oil-gas. partition coefficient
Factors causing decrease in MAC. The blood-gas partition coefficient is the ratio of the
1. Hypothermia concentration of anaesthetic in blood to that in the gas
2. Anaemia phase. It is an index of solubility of the GA in blood. The
3. Hyponatremia uptake of anaesthetics depends on blood-gas coefficient.
4. Pregnancy
5. Hypoxemia 224. Lowest concentration of Anaesthetic agent in
6. Cholinesterase inhibitors pulmonary alveoli needed to produce immobility in
7. Reserpine, a methyldopa response to painful stimulus in 50% individual is
8. Severe hypotension termed as:
A. Minimal alveolar concentration
Factors causing increase in MAC: B. Maximum alveolar concentration
1. Hyperthermia C. Maximum analgesic concentration
2. Hyperthyroidism D. Minimum analgesic concentration
3. Alcoholism A
4. Hypernatremia ..........(AIIMS PGMEE - JUNE 1998)
Remember, numerically MAC is small fo r potent
anaesthetics, such as halothane and large for less potent Minimal alveolar concentration
anaesthetics such as nitrous oxide. • Minimal alveolar concentration (MAC)
Therefore the inverse of MAC is an index of potency “is the lowest concentration of the anaesthetic in
of the anaesthetic. pulmonary alveoli needed to produce immobility in
response to a painful stimulus in 50% individuals.
221. Index of potency of general anaesthesia It is accepted as a valid measure of potency of
A. Minimum alveolar concentration inhalational general anesthetics.”
B. Diffusion coefficient
C. Dead space concentration Meyer-Overton hypothesis
D. Alveolar blood concentration • The MAC of a volatile substance is inversely proportional
A to its lipid solubility (oil:gas coefficient) , in most
..........(PGI - 1997 - Dec) cases.
• This is the Meyer-Overton hypothesis. MAC is inversely
• MAC is the lowest concentration of the anaesthetic in related to potency i.e. high mac equals low potency.
pulmonary alveoli needed to produce immobility in
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 45
TOPIC 19: MC GILL CIRCUIT
228. In Magil circuit, Airflow is:
A. Equal to Minute Alveolar Ventilation
B. Half of the Minute Volume
C. Equal to Minute Volume
D. Twice the Minute Volume
C
..........(AIPGMEE - 2000)
• In gener al anaesthesia, recovery and emergency
resuscitation procedures involve the use of a breathing
Mapleson D
system. The principle of anaesthetic systems is to
(Coaxial Bain)
efficiently eliminate exhaled carbon dioxide, without greatly
• This system is mainly used with spontaneous respiration.
increasing dead space or resistance.
• The Fresh Gas Flow is close to the patient and the
• In 1954 Mapleson classified breathing systems based on
APL valve is placed away from the patient . The risk
their efficiency in eliminating carbon dioxide during
of rebreathing in this circuit will be high especially in
spontaneous respiration.
patients who have a short expiratory pause or do not
• The breathing systems are classified in order of
have an expiratory pause (infants). To overcome this
increased requirement of fresh gas flow (FGF) to
problem a high FGF of 2 - 4 times of the patient’s Minute
prevent re breathing during s pontaneous
Volume is required. If Mapleson D is used with controlled
respiration.
or assisted ventilation a high FGF is required to prevent
• System A requires 0.8 - 1 times, B and C require 1.5-2
all rebreathing. In practice some rebreathing is tolerated
times and D, E and F require 2-4 times of the patient’s
and in an adult an FGF of 6 - 7 litres/minute will maintain
minute volume.
a normal arterial C02 tension.
Equal to Minute alveolar Ventilation
‘Mapleson system A is also known as Magill system’ :
This is the most efficient system with spontaneous
respiration
Mapleson E
(Infant T-piece, and Ayres T-Piece without Bag)
A flow of about 5 L/min (equal to minute ventilation) • This system is primarily for use in neonates and paediatrics,
is required in young healthy patients to flush Co2 from where low resistance is of great importance . There
the system) is no APL valve (to reduce resistance) and a high FGF, 2 -
4 times of the patient’s Minute Volume (with a minimum
Mapleson B flow of 3 litres/minutes) is required to eliminate rebreathing
• In this system the Reservoir bag, fresh gas supply risk during spontaneous ventilation.
and APL valve are closer to the patient . This will cause
mixing of inspiratory and expiratory gases and therefore a
higher flow rate (1.5 - 2 times of the patient’s minute
volume, i.e. 12 - 16 litres/min) is required to prevent
rebreathing during spontaneous respiration. Due to the
risk of rebreathing and reduced delivery of oxygen
rich gases to the patient this system is no longer
used.
• This system is recommended for up to 22kg (approximate
tidal volume of 140ml).
• This system recommends that total fresh gas flow should
be about twice the minute volume of the patient (and
volume of the reservoir tube equal to about 1/3 rd of
• Mapleson C the tidal volume)
(Waters Bag, Bagging System (Adult, Direct and Paediatric) The main advantage of a ‘T’ piece is the absence of Resistance
and Resuscitation Bag) to Expiration a factor of crucial importance to children.
This system is similar to Mapleson B , however, the bag is
positioned very close to the patient. This system is used Jackson Rees made a great improvement to T-Pieces
for manual ventilation during resuscitation. A flow rate of (Mapleson E) by adding an open tail 0.5 litre reservoir
1.5 - 2 times of the Minute Volume is required to avoid bag to the end of expiratory (reservoir) limb .
rebreathing
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 46
This allows manual ventilation and the application of Positive • Mapleson C
End Expiratory Pressure (PEEP) to help maintain open Used in postoperative recovery room
airways. • Mepleson D
Most efficient in assisted and controlled ventilation
Mapleson F • Mepleson E
• Jackson Rees Modification (Infant T-piece, and Ayres T- Used in infants and children (flow rate = 2x minute volume)
Piece with open end Bag) It is as efficient as Mepleson D in assisted and controlled
Jackson Rees made a great improvement to T-Pieces ventilation
(Mapleson E) by adding an open tail 0.5 litre reservoir Also known as Ayre ‘s tube.
bag to the end of expiratory (reservoir) limb .
This allows manual ventilation and the application of Positive 227. The most appropriate circuit for ventilating a
End Expiratory Pressure (PEEP) to help maintain open spontaneously breathing infant during anaesthesia
airways. is:
• For controlled ventilation, normocapnia can be maintained A. Jackson Rees’ modification of Ayres’ T Piece.
with a FGF of 1000ml + 100ml/kg body weight. B. Mapleson A or Magill’s circuit.
C. Mapleson C or Waters’ to and fro canister.
D. Bains circuit
A
..........(.AIPGMEE - 2005)
The most appropriate circuit advocated/or use in
infants is the Ayre’s T piece (Mapleson E).
Type E is basically a circuit for spontaneous respiration,
as it does not contain a breathing bag .
Efficiency of system with spontaneous Respiration :
A>D&E>C>B
Efficiency of systems with IPPV :
D&E>B>C>A
225. Regarding rebreathing prevention valve, incorrect
is
A. Should be as far as possible from the patient
B. Should be light
C. Suitably designed
D. Installed at expiratory end of the tube Being incomplete it was classically modified by Jackson
A Rees who added a bag for monitoring and IPPV.
..........(AIIMS PGMEE - DEC 1994) Jackson’s Rees modification of Ayre’s T piece has thus
become the most appropriate circuit for ventilating
226. All of the following are suitable anaesthetic circuits a spontaneously breathing infant.
for both controlled and assisted ventilation except
A. MaplesonA
B. MaplesonB&C
C. MaplesonD
D. MaplesonE
A
..........(AIIMS PGMEE NOV - 2003)
Mapleson A system is most useful in spontaneous
respiration and least useful in assisted and controlled
ventilation.
• Efficiency of the systems with spontaneous
respiration
A>D&E>C>B
• Efficiency of systems with IPPV (assisted and
controlled ventilation) Efficacy of Mapleson’s systems for spontaneous
D&E>B>C>A respiration
A>D&E>C>B
Mapleson A system - Although the most efficacious system for spontaneous
Also known as Magill system respiration is Mapleson A, in the context of infants and
Most satisfactory with spontaneous respiration small children ,Ayre’s T tube with Jackson Rees modification
Flow of about 5 L/min is maintained becomes the answer of choice.
‘The main advantage of the T piece technique is the
• Mapleson B absence of resistance to expiration, a factor of crucial
Not in common clinical use importance in small children.’
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 47
229. A 25 year old male is undergoing incision and determines the induction and recovery, induction and
drainage of abscess under general anaesthesia with recovery will be fast with agent with less B/G
spontaneous respiration. The mos t efficient partition coefficient and induction and recovery with
anaesthetic circuiit is: be slower with agents with high B/G partition
A. Maplelson A coefficients.
B. Mapleson B
C. Mapleson C Agent Blood gas partition
D. Mapleson coefficient
A Desflurane 0.42
.........(AIPGMEE - 2003)
Cyclopropane 0.44
CO2 will be exhaled into B. tube or directly vented through Nitrous oxide 0.47
an open pop off valve Sevoflurane 0.69
Before inhalation occurs if the fresh gas flow exceeds alveolar
minute volume the inflow of fresh gas will force the Isoflurane 1.38
remaining alveolar gas in B. tube to exit from valve and Enflurane 1'.8
inspiration will only contain fresh gas.
Halothane 2.4
Because a fresh gas flow equal to minute volume is sufficient
to prevent rebreathing of exhaled air ,Mapleson A is Chloroform 8
the most efficient circuit for spontaneous ventilation Trielene 9
Ether 12
Methoxyflurane 15
It can be concluded from the table that induction will be
fastest with desflurane with B/G coefficient of 0.42 and
slowest with methoxyflurane with B/G coefficient
of 15.
232. Which one of the following anaesthetic agents
230. Magill circuit air flow is: causes a rise in the Intracranial pressure:
A. Equal to minute volume A. Sevoflurane.
B. Twice to minute volume B. Thiopentone sodium.
C. Half to minute volume C. Lignocaine.
D. Equal to alveolar volume D. Propofol
A A
..........(AIPGMEE - 1998) ..........(AIPGMEE - 2005)
Equal to minute volume ‘Intracranial pressure increases at high inspired
- Magil system is synonymous with Mapelson system A concentrations of sevoflurane‘
- This is the most satisfactory system for spontaneous
respiration In the given options only sevoflurane causes rise in
- Gas flow here needs to be maintained at flow rates of 5- intracranial pressure while other cause fall in I.C.P.
6 l/min which is approximately equal to the minute volume.
Increased Decreased IOP Increased BP Bronchodilat Branchospas
TOPIC 20: SEVOFLURANE IOP ors tnodics
• Ketamine ■ Halothane • Ketamine (Preferred in (Contraindica
asthmatics) ted in
231. Which one of the following is the fastest acting Asthmatics)
inhalational agent? • N2O • Morphine • Pentazocin • Ketamine • Ether
A. Halothane. (most dilators)
B. Isoflurane. • Etomidate ■ Decreased BP • • Halothane • N2O
C. Ether. Pancuronium
D. Sevoflurane • Thiopental • Halothane • • Thiopentone
D Promethazine
• • Morphine
..........(.AIPGMEE - 2005) Hexamathonium
• Trimethaphan • d-Tc
The fastest induction is seen with sevoflurane
Blood Gas Partition Coefficient (B/G Coff.) 233. Which of the following volatile anaesthetic agents
This is the most important factor determining the uptake should be preferred for induction of anaesthesia in
of agent and so the speed of induction and recovery. children ?
A. Enflurane
Agents will low blood gas partition coefficient will B. Isoflurane
have high alveolar concentration e.g., nitrous oxide C. Sevoflurane
with blood gas partition coefficient of 0.47 means D. Desflurane
concentration (or partial pressure) in blood is 47% of C
alveolar concentration. Since alveolar concentration ..........(AIPGMEE - 2004)
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 48
Induction in Pediatric Patient A. Sevoflurane
B. Methoxyflurane
Inhalation Intravenous Intramuscular C. Desflurane
(Preferred (reserved method) D. Isoflurane
method) A
Sevoflurane Rapid acting Ketamine ..........(AIIMS PGMEE - MAY 2004)
Barbiturate
Children become very anxious at the mere sight of a needle
(Thiopental)
so intravenous induction is difficult in children.
propofol
So inhalational anaesthetics are used to induce anaesthesia
followed, by non
in children.
depolarizing MR
Sevoflurane is commonly used to induce anaesthesia in
234. True about sevoflurane: children.
A. Isopropyl ether (Halothane can also be used)
B. MAC is 2%
C. Good to use in old age Desflurane and isoflurance can also induce aneasthesia but
D. Blood gas partition coefficient is more they are not used because of the following side effects.
E. Formation of compound ‘A with Baralyme - They are pungent
A,B,C & E - Cause coughing
..........(PGI - DEC 2004) - Breath holding
- Produce laryngospasm
235. A 6 month old child is suffering from patent ductus
arteriosus (PDA) with congestive cardiac failure. Agents used if i.v. induction is done in children
Ligation of ductus arteriosus was decided for surgical Thiopentone
management. The most appropriate inhalational
anaesthetic agent of choice with minimal Used in children are -» non depolarizing muscle relaxants (e.g.)
haemodynamic alterat ion fro induction of Rapacuronium
anaesthesia is - Rocuronium
A. Sevoflurane Atracurium
B. Isoflurane Miva curium
C. Enfiurane Sometimes succinyl choline can also be used
D. Halothane
A TOPIC 21: AIRWAY
..........(AIIMS PGMEE - NOV 2005)
237. Oxygen delivery is regulated by all, EXCEPT
• Sevoflurane is the agent of choice for inhalational A. Oxygen tent
induction of anaesthesia in pediatric procedures. B. Nasal catheter
• It is an excellent choice for smooth and rapid inhalational C. Venti mask
induction in pediatric procedures because D. Polymask
- It has sweet odour, so induction is smooth B
- Rapid increase in alveolar anaesthetic concentration ..........(AIIMS PGMEE - NOV - 1993)
(therefore rapid onset of action)
Its low blood solubility results in rapid fall in alveolar O2 is delivered through the following devices
anaesthetic concentration upon discontinuation and 1) Nasal catheter
results in quicker emergence when compared to other 2) BIB mask
inhalational agents. 3) Polymask
4) Vent mask
Cardiovascular effects of sevoflurane 5) Oxygen tent
• Sevoflurane has minimal effect on cardiovascular system, 6) Oxygen apparatus
it causes minimal hemodynamic alterations therefore it can
be easily used as an induction agen in patients with PDA.
The cardiovascular effects are
- Minimal cardiac depression
- Slight decrease in systemic vascular resistance
- Minimal decrease in cardiac output
Halothane and isoflurane are usually avoided in children
because they have a pungent adour and so the induction 238. In a patient with multiple injuries, first thing to be
is not smooth. done is:
A. Patency of airway
236. A 6-year-old child is posted for elective urology B. Maintenance of B. P
surgery under general anesthesia. He refuses to allow C. Immobilize cervical spine
the anesthe siologist an IV acces s. The best D. Lateral position with mouth gag
inhalational agent of choice for induction of A
anesthesia is ..........(PGI - 1999 - Dec), PGI - 2000 - Dec
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 49
• In a patient with multiple injuries, first thing to be done is A. Nasal Cannula
the care of the airway. B. Venturi mask
- The first step in cardio-pulmonary resuscitation is AIRWAY C. O2 by T-piece
MAINTAINANCE D. Edinburgh mask
- The intention for CPR is maintain O2 perfusion until definite B
interventions instituted. ..........(AIIMS PGMEE - MAY 2005)
- The elements of CPR
TOPIC 22: CPR
• Maintainance of airway (A)
• Breathing (B) 242. In a patient with cardiorespiratory arrest, basic life
• Circulation (C) support is given to support which of the following
systems:
240. Laryngeal mask airway is indicated In: A. Respiratory system
A. To prevent aspiration of stomach contents B. Cardiovascular system
B. Short surgical procedure C. Renal system
C. Where endotracheal intubation is contra-indicated D. Gastrointestinal system
D. Difficult airway E. CNS
E. Facilitate endotracheal intubation A
B&D ..........(PGI - 2001 - Dec)
..........(PGI - 2001 - Dec)
243. During cardiac resuscitation, the following can occur
except:
A. Rupture of Lungs
B. Rupture of liver
C. Rupture of Stomach
The Laryngeal mask airway is an alternative airway device
D. Rupture of Spleen
used for anesthesia and airway support. it consists of an
E. Disseminated intravascular coagulation occurs
inflatable silicone mask and rubber connecting tube. it is
None
inserted blindly into the pharynx, forming a low-pressure
..........(PGI - 2001 - Dec)
seal around the laryngeal inlet and permitting gentle
positive pressure ventilation. all parts are latex-free.
244. In a 10 year old child presented anaphylactic shock,
drug of choice is:
The laryngeal mask airway is an appropriate airway choice
A. I/V adrenaline
when mask ventilation can be used but endotracheal
B. S.C. adrenaline
intubation is not necessary.
C. Anti histamine
contraindications:
D. Corticosteroids
Non-fasted patients
A
Morbidly obese patients
..........(PGI - JUNE 1997)
Obstructive or abnormal lesions of the oropharynx
Status epilepticus is said to occur when a seizure lasts beyond
Advantages:
30 minutes or seizures are repetitive, prolonged & the
- Allows rapid access
patient remains unconscious in between the seizures.
- Does not require laryngoscope
Best drug to use in status epilepticus is lorazepam
- Relaxants not needed
in a dose of 0.l mg/kg b.w by I.V. route. This may be
- Provides airway for spontaneous or controlled ventilation
repeated after 5 minutes. Lorazepam effect lasts longer
- Tolerated at lighter anesthetic planes
than diazepam. If lorazepam is not available, immediately
Disadvantges:
diazepam is given in a dose of 0.3 mg/kg by IV route.
Does not fully protect against aspiration in the non – fasted
Seizures may recur after 15-30 minutes since half life of
patient standard LMA does not allow high positive pressure
diazepam is short. Hence, diazepam should be followed
ventilation Requires re - sterilization
by phenytoin in a dose of 10-15 mg/kg IV. If the fits are
not controlled even with this, 20 mg/kg of phenobarbitone
241. Which one of the following device provides fixed
may be given I.V, at a rate of 1 mg/kg/ minute.
performance oxygen therapy:
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 50
245. True about adrenaline in CPR: C. Need for inotropic support
A. Can be given intratracheally D. Rate of intravenous fluid replacement
B. I.V. route better than intracardiac E. Assess need for plasma transfusion
C. Intracardiac route better than IV A
D. Converts coarse fibrillation into fine ones ..........(PGI - 2001 - Dec)
E. The dose used is 2ml. containing 1 in 1000 concentration
NO ANSWER CVP is a useful means of assessing the circulating blood volume
..........(PGI - June -2001) and therefore appropriate for rate of intravenous fluid
replacement.
• During CPR, adrenaline is given every 3 –5 min – this • So, CVP has importance in — assessing need for blood
reflects its half-life. When switching from the non-shockable and plasma transfusion.
to the shockable side of the algorithm, the next dose of • CVP is not a good guide for daily fluid requirements e.g. A
adrenaline will be given before the first or the second pt. can easily be waterloaded or dehydrated in presence
shock depending on when adrenaline was last given of a normal CVP.
248. In an injured patient with hypovoiemia intravenous
fluid administered is guided by:
A. Central venous pressure.
B. Blood pressure.
C. Urine output.
D. Pulse rate
A, B, C & D
..........(.PGI - DEC 2003)
• In a hypovolemic patient, the adequacy of IVF replacement
can be assessed by :
- Clinical pulse, BP
- Urine output
246. The outcome following resuscitation of a cardiac - Invasive CVP and PCWP
arrest is worsened if during resuscitation patient is
given - • Normal PCWP = 8-12 mm Hg
A. Ringer’s lactate Pulmonary artery pressure = 25 mm Hg-Systolic ; 10 mm
B. Colloids Hg- Diastolic.
C. 5% Dextrose
D. Whole blood transfusion Interpretation of CVP and PCWP in various
C conditions :
..........(AIIMS PGMEE - NOV 2005)
CONDITION CVP PCWP
• While performing cardiopulmonary resuscitation for cardias Hypovolemic shock Low Low
arrest, therapy with hyperglycemic intravenous fluid Right heart failure High N
should be avoided.
• Therapy with intravenous glucose solutions results in Left heart failure N High
worse neurological outcome. Cardiogenic shock (Rt and Lt heart N/High High
• Increase in blood and thus brain glucose during global failure)
cerebral ischemia will profoundly affect outcome of the Cardiac tamponade High High
patient
• In high risk patients, intravenous glucose solutions should Pulmonary embolism N/High High
be avoided or used judiciously and blood glucose 249. ‘C wave in JVP tracing seen in:
concentr atio ns should be maintaine d within the A. Ventricular systole
normoglycemic range until the patients have passed the B. Ventricular diastole
period of high risk for hemodynamic compromise. C. Atrial systole
• Most critically ill patients do not need acute glucose D. Protodiastole
supplementations. A
• In patients who require glucose, however we recommend ..........(PGI - DEC 2006)
administering it in a manner (e.g. mini drip devices, infusion
pumps) that will avoid large infusions at the time of an • The different waves of JVP :
ischemic event. ‘a’ wave : Positive, produced by venous distention due to
• Specifically, glucose containing solutions should not be used right atrial contraction and is dominant wave in JVP.
in intravenous lines that will facilitate volume expansion
and drug administrations during t/t of shock or ‘c’ wave : Positive, produced by the bulging of the tricuspid
cardiac arrest. valve into the right atrium during Rt. ventricular
isovolumetric systole.
TOPIC 23: CVP
‘x’ descent : due to both atrial relaxation and to the
247. Importance of CVP measurements is: downward displacement of the tricuspid valve during
A. Need for blood transfusion ventricular systole.
B. Assess amnount of fluid to be given
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 51
fibreoptics for determination of mixed venous O2
saturation, and miniaturized electronics located on the
catheter for measurement of pulmonary flow.
251. While introducing the Swan-ganz catheter, its
placement in the pulmonary artery can be identified
by the following pressure tracing -
A. Diastolic pressure is lower in PA than in RV.
B. Diastolic pressure is higher in PA than in RV
C. PA pressure tracing has diacrotic notch from closure of
pulmonary valve
D. RV pressure tracing for plateau and sharp drop in early
diastole
B
..........(AIIMS PGMEE - NOV 2005)
Pulmonary artery catherization
As the catheter passes via Superior Low pressure waves (mean of 3-8
venacava mmHg)
to right atrium (Right A trial
pressure)
V wave : Positive ; produced by increasing volume of blood
Now the catheter enters Right Tall pressure waves
in the Rt. atrium during ventricular systole when the ventricle through tricuspid valve (RV are displayed (15-25 systolic and
tricuspid valve is closed. pressure) 0-l0 diastolic)
‘y ; decent : Produced mainly by the opening of the tricuspid
Catheter advances Systolic pressure
valve and the subsequent rapid inflow of blood into the
into pulmonary artery remains same as in
right atrium.
through the pulmonary right ventricle but the diastolic
valve (Pulmonary Artery pressure
250. Swan Ganz catheter measure: pressure) increases (10-20 mm Hg)
A. PCWP Dicrotic notch caused bv closure of
B. CO. pulmonary
C. Mixed venous 02 saturation valve can also be noted
D. Pulm. capillary pressure Now the catheter advances ◊ into A dampened pressure
A a branch of pulmonary waveform
..........(PGI - DEC 2006) artery (where it wedges) mean pressure of
Pulmonary capillary 4 -12mmHg
• Swan-Ganz pulmonary artery catheter is the mainstay for wedge pressure
assessment of cardiac function in the critical care and This reflects the left atrial
perioperative settings. It is used to measure : Pressure.
- direct pressure of Rt. atrium, Rt. ventricle and pulmonary
artery (PAWP). TOPIC 24: INTRAOPERATIVE MANAGEMENT
- indirect pressure in Ieft. atrium.
- cardiac output by indicator dilution 252. Which of the following agents is not used to
- Rt. ventricular ejection fraction, provide induced hypotension during surgery?
A Sodium nitroprusside
B. Hydralazine
C. Mephenterrnine
D. Esmolol
C
..........(AIPGMEE - 2006)
Mephentermine acts directly on both a and beta
receptors to cause cardiac stimulation and vasoconstriction.
It increases the cardiac output and both systolic and
diastolic BP.
It is used not to induce but to prevent hypotension.
Hvpotensive Anaesthesia :
This is a technique of deliberately reducing the systolic blood
pressure to 8O-9OmrnHg or mean arterial pressure to 50-
65mmHg in order to reduce the intra operative bleeding.
The clinical criteria is to reduce the blood pressure by one
• Recent refinements have included the addition of fast-
third of preoperative value.
response thermistors, high fidelity pressure transducers,
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 52
Techniques include the following : • Using this property, carbon dioxide concentration can
be measured directly and continuously throughout the
Vasodilators Inhaled Other respiratory cycle.
Sodium Anaesthetics Spinal tepidural • The gradient observed during end tidal CO2 measurement
nitroprusside Isoflurane (Agent of block in healthy individuals is
Nitroglycerine choice) Halothane Ganglion blockers
Enfiurane (Trimethophan) a End tidal CO 2 < alveolar CO 2 < arterial CO\
blocker
(phenotolaraine) p
blocker
(Esmolol/prop
analol) a+P blocker
(Lobetalol) Calcium
channal blocker
Prostaglandin PG5
253. Which of the following is not used in controlling
heart rate intraoperatively.
A. Propanolol/Metoprolol
B. Verapamil
C. Esmolol
D. Procainamide Why is End tidal CO2 less than alveolar COr ?
A • Because the end tidal carbon di oxide is always diluted
..........(AIPGMEE - 2007) with alveolar dead space gas from unperfused alveoli.
These alveoli do not take part in gas exchange and so
Non selective long acting b blockers are avoided for contain no carbon di oxide.
controlling arrythmias (or heart rate) during surgery .
Why is alveolar CO2 less than arterial CO2?
254. Use of Intraarterial cannula in major surgery • Because the blood from the unvetilated alveoli and lung
A. Measurement of direct intra arterial BP parenchyma (both have higher CO2 contents) mixes with
B. Sample for ABG the blood from ventilated alveoli.
C. Drug injection
D. BT • In healthy adults with normal lungs end tidal CO2 is 3 to
A,B,C & D .6 kPa less than arterial CO 2.
..........(PGI - June -2001) • This difference is reduced if the lungs are ventilated with
large tidal volumes.
255. All the following drugs are recommended for
treatment of beta blocker induced excessive Uses of End tidal CO2 (Et CO,). Capnographv
bradycardia and/or decrease in cardiac output, • To detect correct placement in tracheal intubation.
except: Persistent detection of CO 2 by a caphograph is best
A. Dopamine confirmation of tracheal placement of endotracheal
B. Dobutamine tube. If the tracheal tube goes into the oesophagus no,
C. Glucagon or very little CO2 is detected.
D. Calcium chloride
B • To diagnose lung embolism as a sudden decrease in
..........(AIIMS PGMEE - MAY 2005) end tidal carbon di oxide, assuming that the arterial blood
pressure remain stable.
256. Which of the following is not a cardiovascular • To diagnose malignant hyperpyrexia as a gradual
monitoring technique - increase in end tidal carbon di oxide.
A. Transesophageal echocardiography • As a disconnection alarm for a ventilator or breathing
B. Central venous pressure monitoring system. There is sudden absence of end tidal CO2.
C. Pulmonary artery catheterization
D. Capnography Cardiovascular monitoring techniques.
D Non invasive mathods
..........(AIIMS PGMEE - NOV 2005) (1) ECG
(2) Blood pressure
Capnography is a respiratory monitor system (not a (3) Transesophageal echocardiography
cardiovascular)
Capnography - Invasive
• It is the determination of End tidal CO 2 (Et COj) (1) Invasive blood pressure
concentration to confirm adequate ventilation.
• It is useful during all anaesthetic procedures TOPIC 25: DESFLURANE
Principal of End tidal CO 2 determination (capnography) 257. Rapid induction of anaesthesia occurs with which
• Gases with molecules that contain at least two dissimilar of the following inhalational anesthetics?
atoms absorb radiation in the infrared region of the A. isoflurane
spectrum. B. halothane
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 53
C. desflurane Metabolism of Desflurane - Desflurane undergoes minimal
D. sevoflurane metabolism in humans therefore serum and urine
C inorganic fluoride levels following anaesthesia are essentially
..........(AIIMS PGMEE NOV - 2002) unchanged from preanaesthetic levels.
• Rapid induction of anaesthesia is seen with both Desflurane Cardiovascular effects of Desflurane
& Sevoflurane but Desflurane is the anwer as it causes The cardiovascular effects of desflurance appear to be
more rapid induction of anaesthesia then similar to that of isoflurane i.e., it also causes minimal cardiac
Sevoflurane. depression like isoflurane.
• The speed of induction by inhalational anaethestics The specific effects are: -
in descending order is: Blood pressure ----> decrease
(a) Nitrous oxide Heart rate ----> No change or increase
(b) Desflurane Systemic vascular resistance -----> Decrease
(c) Sevoflurane Cardiac output -----> No change or decrease
(d) Isoflurane
(e) Halothane 260. A 70-year-old male is posted for a surgery, which is
• Rate of indu ction of anaesthesia by inhalational likely to last for 4-6 hours. The best inhalational agent
anaesthetics is inversly proportional to its blood gas of choice for maintenance of anesthesia in such a
partition coefficient i.e. the agents with low blood gas case is
partition coefficient eg. Nitrous oxide will have faster rate A. Methoxyflurane
of induction. B. Ether
C. Trichloroethylene
258. Which of the following ihalational agents has the D. Desflurane
minimum blood gas solubility coefficient? D
A. Isoflurane ..........(AIIMS PGMEE - MAY 2004)
B. Sevoflurane
C. Desflurane In a geriatric patient the normal physiological functions
D. Nitrous oxide are already compromised so pros and cons of an
C anaesthetic must be carefully weighed against before
..........(AIIMS PGMEE - MAY 2006) giving an anaesthetic.
Blood gas partition coe fficient in ascending order Methoxyflurane-
- It is highly nephrotoxic and this limits its use.
Agent Blood gas partition - In old patients the G.F.R. is already low so any nephrotoxic
coefficient agent shold be avoided.
• Desflurane .42
Ether-
• Nitrous oxide .47 - Ether was very popular in the past but it is not used now
• Sevoflurane .68 because of its inflammable and unpleasant properties.
• Isoflurane 1.4
Trichlorethylene
• Enflurane 1.9 - It forms explosive mixtures and should not be used in
• Halothane 2.3 closed circuit
Desflurane-
259. Which one of the following statements regarding - Desflurane is a recently developed, fluorinated congener
desflurane is correct? of isoflurane which is quiet safe like isoflurane.
A. It causes severe myocardial depression - It can serve as a good alternative to isoflurane for
B. It is a structural analogue of isoflurane routine surgery as well as prolonged operations
C. It has very high blood and tissue-gas partition coefficients (Here operation is long and lasts for 4-6 hrs).
D. It is metabolically unstable
B Properties of Desflurane-
..........(AIIMS PGMEE - NOV 2004) - No renal and hepatic toxicity has no arrythmogenic action
- Coronory circulation is mantained
Desflurane’s structure is very similar to that of - Very low solubility in blood and tissues because of which
isoflurane induction and recovery are very fast.
It is a recently developed all fluorinated congener of - Agent of choice for induction of anaesthesia in Geriatric
isoflurane (The only difference is substitution of a fluorine patients —> Etomidate, thiopentone
atom for isoflurane’s chlorine atom). - Inhalational agent of choice for ma intenance of
Its special properties are It is highly volatile anaesthesia in Geriatric patient - Isoflurane.
Extremely low oil gas partition coefficient Very low solubility TOPIC 26: MUSCULAR DYSTROPHY/MYASTHENIA
in blood and tissues i.e., very low blood and tissue-gas
partition coefficients Because of these unique properties 261. A 5 year old boy suffering from Duchenne Muscular
it’s induction and recovery are very fast. Dystrophy and Polymyositis has been fasting for 8
Due to this short action it is commonly used as hour and has to undergo tendon lengthening
anaesthesia for out patient departments. procedure, which Anaesthetics should be used
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 54
A. Induction by I.V. scol ine and N2O halothane for dysarrhythmias, conduction abnormalities and finally
maintenance cardiac arrest. The most likely cause is:
B. Induction by I.V. propofol, N2O and O2for maintenance A. Hypercalcemia
C. Induction by I.V. thiopentone and HL.O and halothane for B. Hyperkalemia
maintenance C. Anaphylaxis
D. Inhalational N2O, halothane and O2 for maintenance D. Hypermagnesemia
B
B
..........(.AIIMS PGMEE JUNE - 2000). AIPGMEE - 2003
..........(AIIMS PGMEE MAY - 2003)
• In this boy with duchene muscular dystrophy, there is
high risk of malignant hyperthermia It has been repeated several times before that succinylcholine
• The earliest signs are masseter muscle rigidity causes hyperkalemia in par aplegic patients. This
(MMR), Tachycardia, and hypercarbia due to increased hyperkalemia is responsible for cardiac complications such
CO2 production as dysarrythmias, conduction abnormalities and cardiac
arrest.
Malignant Hyperthermia (MHS) is a pharmacogenetic
predisposition leading to adverse reactions to commonly
“Suxamethonium may be dangerous in the period b/w
used anaest hetic drugs (e.g. halo thane,
succinycholine). Patients respond to these drugs by about 3 days and 6 months or perhaps longer after onset
excessive release of intracellular calcium which triggers a of paraplegia. It releases more potassium than usual from
potentially lethal muscle hypermetabolism Central Core muscles and the extreme hyperkalemia can cause
Disease (CCD) is a chronic muscle weakness and arrythmias or cardiac arrest.”
degeneration due to leakage of intracellular calcium
stores. Both conditions share a common genetic cause: 264. In myasthcnia gravis, which druges should not be
Mutations in the muscle calcium release channel RYR1. used:
A. Gallamine
B. Noestigmine
C. Aminoglycosides
D. Metronidazole
E. Ampicillin
A&C
..........(PGI - June -2002)
• The muscles affected by MG are hypersensitive to non-
depolarizing muscle relaxants.
Even myasthenics successfully treated with steroids
and not requiring anticholinesterases may still show
this hypersensitivity. So they should be avoided, but
small doses of short-acting relaxants like Mivacurium,
with monitoring of the neuromuscular block may
be used.
Induction by I.V. propofol, N2O and O2 for maintenance
• This boy has chances of developing malignant hyperthermia • Myasthenics are resistant to the effects of depolarizing
because muscular diseases (duchene muscular dystrophy muscle relaxants like Suxamethonium and Decamethonium.
and polymyositis) predispose to malignant hyperthermia.
• Drugs like Aminoglycoside antibiotics (neomycin,
Predisposing conditions streptomycin, gentamicin), tetr acycline, quinidine,
• Arthrogryposis multiplex congenita* procainamide, penicillamine and beta-blockers can worsen
• Osteogenesis imperfecta*
MG and so avoided.
• Congenital ptosis
Ampicillin & Metronidazole are not contraindicated in
• Strabismus
• Hernia, kyphoscoliosis MG.
• Cleft palate
• Duchenne muscular dystrophy* TOPIC 27: PREANESTHETIC MEDICATION
Drugs which precipitate malignant hyperthermia 265. Most potent antiemetic agent used in preoperative
• Anaesthetic ——> Succinylcholine*, (MC) Halothane* period:
• Monoamine oxidase inhibitor A. Glycopyrrolate
• Phenothiazines
B. Hyoscine
• Amide local anaesthetics
C. Atropine
• TCA’s
D. Metochlorpromide
262. The administration of succinylocholine to a B
paraplegic patient led to the ap pearance of ..........(AIIMS PGMEE - SEP 1996)
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 55
Hyoscine • It is also an antiemetic (prevents vomiting), antivertigo
(prevents dizziness), and antispasmodic (reduces smooth
muscle contr actions; although a der iv ate called
butylscopolamine, that does not cross the blood-brain
barrier, is used preferably).
• It can be used as a pre-anesthetic sedation, as an
antiarrhythmic during anesthesia, and for the prevention
of motion sickness.
• Transdermal patches, , are avail able for the
prevention of symptoms of travel sickness.
• Scopolamine, also known as hyoscine
• It acts as a competitive antagonist at muscarinic
acetylcholine receptor (M1); it is thus classified as an
anticholinergic or as an anti-muscarinic drug. 266. Atropine as preanesthesia has all effects except
Scopolamine hydrobromide. A. decrease secretion
– It can be used as a depressant of the central nervous B. Bronchoconstriction.
system, though it can cause excitement, restlessness, C. prevent bradycardia
hallucinations, or delirium in the presence of pain, mydriasis D. prevebt hypotension
(pupillary dilation), and cycloplegia (paralysis of the eye B
muscles). ..........(AIPGMEE - 1996)
– When combined with morphine, it produces amnesia
and a tranquilized state known as twilight sleep. Atropine is a bronchodialator and reduces air way resistance
Although originally used in obstetrics, it is now considered specially COPD and Asthma patients.
dangerous for that purpose. Sometimes side effects of
scopolamine can be mistaken for symptoms of cancer 267. Drugs commonly used in pre- anaesthetic
because of the nausea and anisocoria associated with brain medication:
tumors. However, scopolamine induced anisocoria clears A. Diazepam
up usually within 3 days. B. Scopolamine
C. Morphine
• It is used in ophthalmology to deliberately cause cycloplegia D. Succinylcholine
and mydriasis so that certain diagnostic procedures may E. Atracuronium
be performed. It is also used in the treatment of A, B, & C
iridocyclitis. ..........(PGI - DEC 2004)
• Scopolamine is the other name of Hyoscine hydrobromide
which is anticholinergic drug used as premedicant
Succinylcholine & Atracurium are skeletal muscle relaxants
used in intubation & maintenance of anaesthesia.
268. Preanesthetic medication is used to:
A. Decrease does of anesthetic
• In otolaryngology it has been used to dry the upper airway B. Decrease BP
(anti-sialogogue action) prior to instrumentation of the C. Prevent aspiration
airway D. Produce amnesia for peri-operative events
E. Relieve anxiety
A, D & E
..........(PGI - June -2002)
• Preanesthetic medication (PAM) refers to the use of drags
before anaesthesia to make it more pleasant and safe.
The aims are :
- To relief anxiety apprehension and to facilitate smooth
induction.
- Amnesia of pre and post operative events.
- Supplement analgesic action of anaesthetics and
potentiate them so that less anaesthetic is needed.
- DECREASE -Secretions and vagal stimulation caused by
anaesthetics.
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 56
- Antiemetic effects extending to the postoperative period.
- DECREASE -Acidity*and volume of gastric juice so that it
is less damaging if aspirated.
• The different drugs that are used as PAM are :
Opiods-Morphine
Antianxiety drugs-Diazepam
Sedative-Hypnotics-Barbiturates Anticholinergics-
Atropine or hyoscine Neuroleptics-chlorpromazine
H2 blockers-Ranitidine/Famotidine
Antiemetics-Metoclorpr amide, Domperidone, or
Ondansetron.
Left parasternal long axis view with air shadow in the aorta
TOPIC 28: AIR EMBOLISM
269. Quantitative estimation of air embolism is done by
A. ECG
B. End tidal CO2 estimation
C. Pulmonary capillary wedge pressure
D. Doppler study
B
..........(AIIMS PGMEE - NOV – 1993)
270. 5 year old child going for sitting craniotomy, while
positioning in O.T. developed end tidal CO2- Zero mm
Hg, PO2- 80mm Hg implies that: ‘
Treatment
A. Venous air embolism
• irrigate operative site with fluid
B. Left lung collapse
• apply occlusive material to bone edges
C. Endotracheal tube in Oesophagus
• gently compress internal jugular veins
D. Endotracheal tube blocked with secretions
• head down position
A
• aspirate air through right atrial catheter (best if tip is at
..........(AIIMS PGMEE JUNE - 2000)
SVC-RA junction)
• discontinue N2O
Venous air embolism
• inotropes may be needed
• BEWARE: PEEP, by reversing RA-LA pressure
• The cranial sinuses have negative air pressure .
gradient, may lead to paradoxical air emboli via PFO
– So, it is possible that if the pt. is in wrong position while
operation, the sinuses may suck some air d/t their negative
271. About diagnosing air emb olism with
pressure which can cause venous embolism
transesophageal echocardiography, which of the
• The given value for the gases can occur only in Venous air
following is false:
embolism.
A. It can quantify the volume of air embolised
B. It is a very sensitive investigation
Venous Air Embolism (VAE)
C. Continuous monitoring is needed to detect venous
• consider whenever head > 5 cm above heart
embolism
• transected veins in cut edge of bone or dura may not
D. Interferes with doppler when used together
collapse
A
• air -> RV -> pulmonary circulation
..........(AIIMS PGMEE MAY - 2002)
• decreased pulmonary blood flow, pulmonary edema,
bronchoconstriction, cardiovascular collapse, hypoxemia
A “four-chamber” view. The right atrium is in the upper left
• paradoxical (air) embolism
corner of the picture.
• coronary or cerebral circulations
The central venous catheter can be seen as a small dot in
• via patent foramen ovale (PFO) (20-30% of adults have
the center of the atrium
probe-patent foramen ovale) detection
• precordial Doppler ultrasound near right upper
sternal border is most sensitive non-invasive
monitor (detects 0.25 ml)
• trans-esophageal echocardiography is more
sensitive, but more invasive and cumbersome
• sudden decrease in ETCO2, incease in ETN2
• gasping, hypotension, dysrhythmias, cyanosis, “mill-wheel”
murmur
• Apical four chamber view with air shadows in both right
and left ventricle
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 57
four-chamber view recorded during dissection of a vascular Oxygen
tumor. Air bubbles are visible as a “snow-storm” • I ncrease in oxygen causes a low amplitude, fast
appearance in the right atrium . Note that no air is frequency EEG pattern characteristics of cerebral
crossing into the left atrium excitation.
• Decreased brain oxygenation initially causes increased
cerebral excitability as a result of peripheral
chemoreceptor stimulation and its attendant effects on
brains reticular activating system.
If hypoxia persists and overwhelms compensatory system
diffuse EEG slowing occurs eventually, leading to EEG
silence as anoxia appears.
Carbon dioxide
• Hypocarbia causes slowing of the E.E.G.
• Small increase in pCO2 (5-20% above normal) causes
decreased cerebr a l excitabili ty and an in creased
electroshock seizure threshold.
• Higher levels of CO2 (30% above normal) result in
TOPIC 29: HYPOTHERMIA increased cerebral excitability and epileptiform
discharges.
272. Hypothermia is used in all except: • High levels (50% above normal) produce E.E.G.
A. Neonatal asphyxia depressions.
B. Cardiac surgery
C. Hyperthermia Effects of anaesthetic drugs on electroencephalograms
D. Arrythmia • Most anaesthetics produce a biphasic pattern on the
D E.E.G. consis ting of an initial activation (a t
..........(PGI - 1998 - Dec) subanaesthetic doses) follows by dose dependent
depression.
• There is substantial protection against ischemia and hypoxia
is provided by. just 1—3° C hypothermia Inhalational anaesthetics
Hypothermia reduces the tissue metabolic rate about • Halothane produces a typical biphasic pattern.
8%/°C. • Isoflurane is the only volatile anaesthetic that produces
• It decreases the cerebr al metabolic r ate and is isoelectric E.E.G.
cerebroprotective during episode of cerebral ischemia. • Desflurane and sevoflurane produces a burst suppression
pattern at high does but not electrical silence.
The protection afforded by mild hypothermia is so great that Nitrous oxide increases both frequency and amplitude.
reduced core temperature — 34° C is probably indicated
in : Intravenous agent
- Carotid artery surgery • Benzodizeapenes produce a typical biphasic pattern
- tieurosurgery on E.E.G.
- Procedures where tissue ischemia can be anticipated • Barbiturates, etomidate and propofol produces a
- Traumatic brain injury ARDS typical bipha sic pattern and are the only
intravenous agents capable of producing burst
273. Hypothermia is used in: suppression and electrical silence at high dose.
A. Hyperpyrexia • Opioids produce monophasic dose dependent
B. Prolonged surgeries depression of the E.E.G.
C. Massive blood transfusion Ketamine produces an unusual activation consisting of
D. Hypertension rhythmic high amplitude theta activity followed by very
A&B high amplitude gamma and low amplitude beta activities.
..........(PGI - June -2000)
Electroencephalographic changes during anaesthesia
274. Which of the following in anaesthesia will produce Activation Depression
decreased EEG activities • Inhalational agents (1-2 MAC)
• Inhalational agent
A. Hypothermia • Barbiturates
(subanaesthetic) •
B. Early hypoxia • Opioids
Barbiturates (small doses)•
C. Ketamine Benzodiazepenes (small • Propofol
D. N2O doses) • Etomidate
A • Hypocapnia
• Etomidate (small doses)•
..........(AIIMS PGMEE - NOV 2006) • Marked hypercapnia
Nitrous oxide
• Hypothermia
Effect of various conditions on E.E.G. Body temperature • Ketamine
• Hypothermia causes progressive slowing of the brain • Mild hypercapnia
activity. • Sensory stimulation
At core temperature below 35°C complete electrical • Hypoxia (early) • Hypoxia (late) ischemia
silence occurs with profound hypothermia.
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 58
TOPIC 30: NITRIC OXIDE TOPIC 31: POSTOPERATIVE COMPLICATIONS
275. Which of the following inhaled gases is used to 278. Which of the following agents is used for the
decrease pulmonary artery pressure in adults & treatment of postoperative shivering?
infants A Thiopentone
A. nitrous oxide B. Suxamethonium
B. nitrogen dioxide C. Atropine
C. nitric oxide D. Pethidine
D. nitrogen D
C ..........(AIPGMEE - 2006)
..........(AIIMS PGMEE NOV - 2002)
Treatment of postoperative shivering involves the use
Nitric oxide causes decrease in pulmonary artery of Tramadol, pethidine or pentazocine and oxygen
pressure in both adults and infants. inhalation.
It is the most effective agent used to decrease in • Shivering occurs as a protective mechanism as inhalational
pulmonary artery hypertension. It is an endothelium agents, spinal/epidural blocks cause vasodilatation leading
derived vasodilator to heat loss.
• Shivering can be abolished by inhibition of hypothalamus.
276. At the end of anaesthesia after discontinuation of • Most commonly shivering is seen after halothane.
nitrous oxide and removal of endotracheal tube,
100% oxygen is administered to the patient to Treatment of shivering
prevent: Oxygen inhalation: O2 consumption may increase upto 4
A. Diffusion Hypoxia times (400%) during shivering and hence oxygen inhalat
B. Second gas effect ion during shivering is mandatory. . . :
C. Hyperoxia
D. Bronchospasm Drugs:
A Tramadol is the drug of choice
. Pethidine/pentazocine may be used.
..........(AIIMS PGMEE NOV - 2003)
279. A 25 year old male with roadside accident
N2O has low blood solubility. So when N2O is discontinued
underwent debridement and reduction of fractured
after prolonged anaesthesia, due to its low blood solubility
both bones right forearm under axillary block. On
it rapidly diffuses into the alveoli and dilutes the alveolar
the second postoperative day the patient complained
air.
of persistent numbness and paresthesia in the right
This causes excess of N2O in alveoli so the partial pressure
forearm and hand) The commonest cause of this
of oxygen in the alveoli is reduced.
neurological dysfunction could be all of the following
except:
• This results in hypoxia and it is known as diffusion A. Crush injury to the hand and lacerated nerves
hypoxia B. A tight cast or dressing
If the cardiac reserve is normal diffusion hypoxia is not of C. Systemic toxicity of local anaesthetics
much significance but if cardiac reserve is low, diffusion D. Tounriqet pressure
hypoxia can be very dangerous. C
..........(AIPGMEE - 2004)
• Prevention: -
It can be prevented by continuing 100% O2 inhalation for a Systemic toxicitv of LA include
few minutes after discontinuing N2O • CNS toxicity
• Cardiovascular system
Diffusion hypoxia is not significant with other anaesthetics • Methemoglobinemia
because the y are administered a t very low • Allergies
concentrations (2 - 4%) and so they cannot dilute But the involvement of the peripheral nerve is characterized
alveolar air by more than 1-2% by parathesies, numbness, hypaesthesia, pain are
indication of local peripheral nerve injury.
277. Which of the following statements is true regarding
Nitric oxide: 280. When a patient develops supra ventricular
A. Used in pulmonary hypertension tachycardia with hypotension un der general
B. Decreases the dose of anaesthetics anaesthesia, all of the following treatments may be
C. Sympathomimetic action instituted except:
D. Causes systemic hypotension A. Carotid sinus massage
E. Used as a vasoconstrictor B. Adenosine 3-12 mg IV
Ans a,c C. Direct current cardioversion
..........(PGI - 2001 - Dec) D. Verapamil 5 mg IV
D
• It is reasonable to expect that inhalation of(NO) could be ..........(AIPGMEE - 2004)
beneficial as a long-term therapy for pulmonary arterial
hypertension (PAH) Verapamil should not be used in presence of SVT with
adverse factors such as hypotension. It can cause
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 59
prolonged hypotension and depression of ventricular • TC causes hypotension by :
function, especially in the presence of anaesthetic agents - Ganglion blockade.
that cause myocardial depression. - Histamine release.
- decreased venous return.
Supraventicular tachycardia (SVT) can occur at any time during • It cause vagal ganglionic blockade - so t ed HR.
the preoperative period in susceptible patients. Duration of action is 30— 60 minutes.
• Vagal manoeuvers in the form of carotid sinus massage
can terminate supraventicular arrythmias in about 80% of TOPIC 33: VECURONIUM
cases and thus these should be tried initially.
If attempts to increase vagal tone and terminate the SVT 284. Which of the following statement is not correct
by carotid sinus message are unsuccessful, the treatment for Vecuronium ?
of choice is adenosine by fast IV injection. This is safe and A. It has high incidence of cardiovascular side effects.
effective during haemodynamic intability because B. It has short duration of neuro muscular block
adenosine has duration of action of less than 60 seconds. C. In usual doses the dose adjustment is not required in kidney
It blocks AV conduction without compromising ventricular disease
function. Adenosine should not be given to patients wi D. It has high lipophilic property
th asthma or AV conduction block. A
..........(AIIMS PGMEE NOV - 2002)
• If adenosine is unavailable and the patient is
normotensive, IV verapamil can be given. However, Properties of Vecuronium.
verapamil can cause prolonged hypotension and depression (1) It is non depolarising muscle relaxant
of ventricular function, especially in the presence of (2) It is highly lipophilic
anaesthetic agents that cause myocardial depression. (3) It has dual excretory pathway i. e.,Itis excreted through
• Cardioversion is indicated if the SVT is associated with both liver and kidney.
hypotension or other adverse risk factors Kidney accounts for of the elimination of Vecuronium
so in renal failure, Vecuronium persists for a longer
TOPIC 32: TUBOCURARINE duration. Still Vecuronium is not contraindicted in
renal failure.
281. d-TC (d-Tubocurarine) is a The advantage of Vecuronium is that its side effects are
A. Ganglion blocker very few.
B. Depolarizing blocker It does not have any cardiovascular side effects.
C. Competitive neuromuscular block
D. a + c both 285. Skeletal muscle relaxant having no CVS side effects:
D A. Vecuronium
..........(AIIMS PGMEE - MAY - 1993) B. Doxacurium
C. Pancuronium
282. Which one of the following antibacterials should D. Rocuronium
not be used with d-tubocurarine? E. Mivacurium
A. Norfloxacin A, B & D
B. Streptomycin ..........(PGI - DEC 2006)
C. Doxycycline
D. Cefotaxime 286. Bradycardia during anaesthesia seen in
B A. Pancuronium
..........(AIPGMEE - 2006) B. Vecuronium
C. Atracurium
Use of Strep tomycin along with com petitive non D. Propofol
depolarizing blockers like d-tubocurarine can potentiate E. Succinylcholine
its action and produce prolonged apnea . B, C , D & E
..........(PGI - JUNE 2004)
Streptomycin should therefore not be used with d-
tubocurarine. • Pancuronium causes a moderate increase in heart rate.
• Vecuronium is about 20 times weaker as a vagolytic
Streptomycin and Neomyein have higher propensity substance than pancuronium.
than other aminoglyco sides. Tobramycin is least • Bradycardia seen after adminstration of vecuronium &
likely to produce these effects . atracurium.
• Propofol produces bradycardia due to central vagal
283. True about d TC is: activity.
A. Excreted unchanged by kidney Succinylcholine produces bradycardia & cardiac arrest on
B. Causes hypotension by ganglion blocking action the second on even after the first injection.
C. Vagolytic action
D. Effect lasts for 2-3 hours TOPIC 34: ABG
B
..........(PGI - June -1998) 287. Heparin interferes with which of the following
results of ABG:
Tubocurarine is partly metabolized in body. The unchanged A. PO2
drug is excreted in urine as well as in bile. B. PCo2.
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 60
C. PH. • Stage of Anaesthesia are as follows *
D. HCO3. • Stage I —> Analgesia
E. An ion gap • Stage II —> Delirium or excitement, partially dilated pupil
C • Stage III —> Stage of Surgical Anaesthesia
..........(.PGI - DEC 2003) It is divided in 4 stages
1. Moving eye to fixed age
288. Pulse oxymetry detects inaccurately in presence of: 2. Corneal & laryngeal reflex lost
A. Hyperbilirubinemia 3. Light reflex lost
B. Nail polish 4. Intercotsal paralysis,
C. Methernoglobinemia Abdominal respiration,
D. Skin pigmentation Pupils widely dilated*
B, C & D • Stage IV —> Stage of Medullary Paralysis
..........(PGI - JUNE 2005)
TOPIC 36: ATROPINE
* Pulse oxymeter is accurate in detecting oxygen saturation,
but there are many sources of error: 291. In belladona poisoning, antidote is:
- Different Hemoglobins: A. Physostigmine
B. Neostigmine
Methemoglobin : It absorbs light at equal wave lengths used C. Ami histamine
by pulse oxymeters, so there might be erroneously high D. Atropine
values of saturation. A
Carboxyhemoglobin:
..........(PGI - JUNE 1997)
Pulse oxymeters overread by the presence of HbCO.
Fetal hemoglobin: Only very high level can cause some
• Belladona poisoning may occur due to drug overdose or
inaccuracy.
Hemoglobin S: Controversial. consumption of seeds & berries of belladona/datura plant.
- Bilirubin : Children are highly susceptible. Manifestations are due to
Severe hyperbilirubinemia does not affect pulse oxymetry exaggerated pharmacological actions.
readings.
- Malposition of sensor Physostigmine 1-3 mg. S.C or i.v. antagonizes both central
- Poor peripheral pulsation & peripheral effects. It may be repeated 4-6 hourly.
- Skin pigmentation : Pulse oxymeter readings are Neostigmine is less satisfactory.
erroneously high in patients with dark skin color.
- Dyes: Like methylene blue, indocyanine green can cause 292. Atropine is used in following except:
large transient decrease in saturation without actual A. Glaucoma
decrease in the same. B. Mushroom poisoning
- Optical interferance : Sunlight, operating room light, C. Malathion poisoning
infrared heating lamps results in erratic readings. D. Organophosphorous poisoning
- Electrical interferance : A
Electrical interferance from an electrosurgical unit can ..........(PGI - JUNE 1997)
cause the oxymeter to give an incorrect pulse count.
- Nail polish & coverings :
• Topical instillation of atrepine cause mydriasis, abolition of
Black, blue & green (but not red or purple) nail polish may
light reflex & cycloplegia lasting 7-10 days. This results in
cause significantly lower saturation readings.
photophobia & blurring of near vision. The ciliary muscles
TOPIC 35: ANAESTHESIA STAGES recover somewhat earlier than sphincter pupillae. The
intraocular tension tends to rise, especially in narrow angle
289. Visual analogue scale (VAS) most widely used to glaucoma; conventional systemic doses produce minor
measure ocular effects.
A. Sleep
B. Sedation Atropine is also used to awtegonise muscarinic effects of drugs
C. Pain intensity & poisons. It is the specific antidote for anti ChE &
D. Depth of Anaesthesia early mushroom poisoning. It is also given to block
C muscarinic action of neostigmine used for rnyasthenia
..........(AIIMS PGMEE MAY - 2003) gravis, decurarization or cobra envenomation.
290. Stages of Anaesthesia were established by: TOPIC 37: CALCIUM CHANNEL BLOCKERS
A. Ether
B. Nitrous Oxide 293. Drugs which interfere with anesthesia are:
C. Cyclopropane
A. Calcium channel blocker nifedipine
D. Chloroform
B. Beta blockers
A
..........(AIIMS PGMEE - JUNE - 1997) C. Aminoglycosides
D. Steroid administration
Ether E. D-tubocurarine
• Guedel’s staging of Anaesthesia was given for Ether A, B, & C
..........(PGI - 2001 - Dec)
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 61
294. Ca2 + channel blockers In anesthesia. True is: Brief clonic seizures occur with the use of enflurane. Therefore
A. Needs to be decreased as they augment hypotension & enflurane is contraindicated.
muscle relaxation
B. withheld because they lower LES pressure Enflurane
C. Should be given in normal doses as they prevent MI & - Though it can give rise to fluoride as a metabolite, the
angina quantity is insufficient to cause renal toxicity.
D. All of the above - Bronchodilation and uterine relaxation is similar to
C halothane but it is better skeletal muscle relaxant
..........(PGI - June -2000) - It stimulates salivary and respiratory secretions slightly, but
they generally do not pose any problem.
• Calcium channel blockers (CCB) at therapentic doses have - It does not sensitize the heart to adrenaline (Arrythmias
no significant role in the release of normal Ach or on the are rare)
strength of normal neuromuscular (NM) transmission/There - Fall in B.P. is similar to that caused by halothane as it also
have been a few reports, however, that CCB may block decreases peripheral resistance to some extent.
of NM transmission induced by non-depolarising relaxants.
• CCBs relaxes the smooth muscles of esophagus thus TOPIC 39: ETOMIDATE
causing lowering of LES, but there is no such indication
of stoppage of this drug during anaesthesia for the same 297. Which of the following statements is not true about
complications. etomidate?
• The use of CCBs have several important implication for A. It is an intravenous anesthetic
anaesthetic management. B. It precipitates coronary insufficiency
C. It inhibits cortisol synthesis
They are : D. It causes pain at site of injection
(i) Along with inhalational and narcotic anesthetics, nifedipine B
causes decreased systemic vascular resistance, BP, and ..........(AIPGMEE - 2006)
contractility may be additive and alongwith verapamil, they
decrease the AV conduction times and additively decrease Etomidate does not precipitate coronary insufficiency.
BP, systemic vascular resistance and contractility. Cardiovascular & respiratory depression do not occur with
(ii) Verapamil and presumably the other CCBs have been found etomidate.
to decrease anesthetic requirement by 25%. Etomidate:
(iii) Because slow channel activation of Ca2+ is necessary to P otent ultrashort acting non barbiturate®
cause spasm of of cerebral and coronary vessels, broncho- intravenous anaesthetic.
constriction and normal platelet aggregation, these drugs
may have a role in treating ischemia of the CNS and 298. Induction agent that may cause adrenal cortex
CVS, bronchoconstriction and untoward clotting suppression is:
disorders perioperatively. A. Ketamine
B. Etomidate
TOPIC 38: ENFLURANE C. Propofol
D. Thiopentione
295. Which of the following is contraindicated in epilepsy B
A. Isoflurane ..........(AIPGMEE - 2003)
B. Halothane
C. Enflurane • Induction doses of etomidate transiently inhibit
D. Ether enzymes involved in cortisol and aldosterone
C synthesis.
..........(AIIMS PGMEE - MAY - 1994) Long term i nfusions lead to adr enocortical
suppression.
• Enflurane precipitates generalized tonic clottic • It is suitable for day care anaesthesia but less preferred
seizures therefore it is contraindicated in epileptics. than propofol
Its use is contraindicated in porphyria6, adrenal insufficiency.
• Other questions on Enflurane
It slighty stimulates salivary and respiratoxy secretions TOPIC 40: GALLAMINE
It causes fall in B.P. due to decrease in peripheral resistance.
It does not sensitize the heart to adrenaline (Arrythmias are 299. Muscle relaxant contraindicated in Renal failure is:
rare). A. Atracurium
It causes bronchodilation B. D-tubocurare
It is contraindicated in renal failure. C. Vecuronium
D. Gallamine
296. Which of the following inhalational agent is D
contraindicated in a patient with history of epilepsy; ..........(AIIMS PGMEE - Dec - 1995), (AIPGMEE - 1999)
A. Isoflurance
B. Enflurane • Gallamine is a muscle relaxant C/I in Renal failure as it is
C. Halothane almost exclusively excreted by kidney.
D. Sevoflurane
B • Gallamine (as gallamine triethiodide) is a non-depolarising
..........(AIIMS PGMEE NOV - 2003) muscle relaxant. It acts by combining with the cholinergic
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 62
receptor sites in muscle and competitively blocking the B. Dose needs to be altered in renal failure
transmitter action of acetylcholine. Gallamine has a C. It is very little affected by pH and heat
parasympatholytic effect on the cardiac vagus nerve which D. Loading dose before continuous infusion
causes tachycardia and occasionally hypertension. Very high B
doses cause histamine release. ..........(AIIMS PGMEE - MAY - 1994)
• Gallamine is commonly used to stabilize muscle
contractions during surgical procedures . Effect of lidocaine on refractory period
i) In normal cells - It decreases refractory period
Gallamine ii) In depolarized cells - It increases the refractory period
- Gallamine is excreted entirely unchanged in the Kidney, iii) AV Nodal refractory period –
so it is contraindicated in patients with Renal failure – It has no effect on AV nodal refractory period
• The important point about lidocaine is that it has no
Preferred relaxants: electrophysiologycal effects on normal cardiac tissue while
• In hepatic failure: Atracurium it has marked electrophysiologial effect on depolarized
• In Myaesthenia Gravis : one tenth of normal of Atracurium tissue.
(ifrelaxants are essential).
• In Obstretrics : any relaxant except Gallamine 304. Lignocaine in high doses produces
• In Arterial surgery (to maintain BP): Pancuronium A. Convulsion
To deliberately reduce blood pressure : Tubocurarine B. Respiratory depression
C. Hypotension
TOPIC 41: LAPROSCOPY D. Cardiac arrest
E. Hypothermia
301. Which gas is most commonly used in laparoscopy: A,B,C & D
A. O2 ..........(PGI - JUNE 2004)
B. CO,
C. N2O • The maximum safe dose of Lignocaine for a 70 kg man
D. N, with adrenaline (epinephrine)- 500mg i.e. 7 mg/kg;
B without adrenaline (epinephrine)- 200 mg i.e. 3 mg/
..........(AIIMS PGMEE - MAY 1995) kg body weight.
CO2 Higher doses produces toxicities like :
• The gas used is CO2 , as it is common to the human CNS : Stimulation followed by depression, restlessness,
body and can be removed by the respiratory system if it hysterical behaviour, vertigo, tremor, convulsions, and
absorbs through tissue. respiratory failure.
• It is also non-flammable, which is important due to the
fact that electrosurgical devices are commonly used CVS : Hypotension, primary cardiac failure, feeble pulse,
in laparoscopic procedures. cardiovascular collapse, bradycardia, pallor & sweating.
Respiratory depression : Apnoea from medullarly depression
or respiratory muscle paralysis.
Allergic :
Rare, bronchospasm, urticaria or angioneurotic oedema.
* Factors influencing local anaesthetic toxicity : . - Quantity
of’solution
- Concentration- of drug
- Presence or absence of adrenaline
- Vascularity of site of injection
- Rate of absorption of drug
- Rate of destruction of drug Hypersensitivtty of patient
- Age, physical status & weight, of patient
TOPIC 43: MALIGNANT HYPERTHERMIA
302. The gas used create pneumoperationeum is:
A. CO2 305. Hyperthermia is caused by:
B. N2 A. Anticholinergics
C. O2 B. MAO inhibitors
D. Room air C. Lithium
E. N2O D. Chlorpromazine
A, C, & D E. Carbimazole
..........(PGI - 2001 - Dec) NONE
..........(PGI - DEC 2002)
TOPIC 42: LIDOCAINE
306. Malignant hyperthermia is caused by:
303. All are true about Lidocaine, except A. Halothane
A. Prolongs refractory period B. Cyclopropane
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 63
C. Suxamethonium • Methoxyflurane has a high nephrotoxic potential and its
D. Ether use has been discontinued.
A&C • Eflur ane is also nephrotoxic, though lesser than
..........(AIIMS PGMEE - DEC 1997) Methoxyflurane and is also not recommended.
• Isoflurane, sevoflurane and halothane result in little or no
Halothane & Suxamethonium increase in fluoride levels and are preferred.
• C/f of Malignant Hyperthermia :
• Heat production exceeds the heat loss in the body to TOPIC 45: MIVACURIUM
cause a rise of temperature of at least 2 c/h.
• It is characterized by 309. Mivacurium false is
• Hypercapnia A. Hypertension
• Hyperventilation B. Increasing the dose produces rapid onset of action
• Hyperkalemia* C. Bronchospasm
• Metabolic Acidolis* D. Flushing RADIOLOGY
• Arrhythmia A
• Diffuse intravascular coagulation ..........(AIIMS PGMEE - NOV 2007)
• Pyrexia
• • Mivacurium belongs to non depolarizing blocker or
• There is – increased hemolysis* competitive skeletal muscle relaxants.
- increased Creatine phosphtinase* • This class of drugs acts by competitively inhibiting the
- increased Transaminase NM receptors and thus causing relaxation.
• Management : • The action of these dr ugs can be reversed by
• Early withdrawal of the volatile anaesthetic agent is of anticholinesterase like neostigmine.
utmost importance • Mivacurium is the only nondepolarising neuromuscular
• Cool the patient blocker that is metabolised by plasma cholinesterase.
• Acidosis corrected • Mivacurium is the shortest acting non depolarizing
• Administer Dantrolene muscle relaxant.
• Correction of Hyperkalemia • The usual intubuting dose is 1.5—2 mg/kg.
• Promote diuresis • Mivacurium causes histamine, release but it generally
• Give Dexamethasone does not cause serious side effects except for small degree
of hypotension. But when mivacurium is given in
TOPIC 44: METHOXYFLURANE large doses to increase the onset of action it causes
increased release of histamine which leads to
307. Nephrotoxic anaesthetic agent is: hypotension, flushing and bronchospasm.
A. Halothane • Mivacurium causes histamine release due to direct action
B. Isoflurane on mast cells.
C. Methoxyflurane • On increasing the dose, the onset of action is increased.
D. Nitrous Oxide
C 310. Shortest acting non depolarising muscle relaxant:
..........(AIIMS PGMEE - JUNE - 1997), AIPGMEE - 1998 A. Vecuronium
B. Atracurium
Methoxyflurane C. Succinylcholine
• Methoxyflurane has the highest fluoride content so it D. Mivacurium
is highly Nephrotoxic D
• There is high output renal failure and high chances ..........(AIIMS PGMEE - JUNE 1998)
of Oxalate stone.
• Its minimum alveolar concentration (MAC) is 0.2,
Shortest acting non depolarising muscle relaxant is ---->
hence it is extremely potent.
Mivacurium
• It has a high lipid solubility (oil:gas coefficient around Longest acting non depolarising muscle relaxant is ---->
950) giving it a very slow onset/offset, thus undesirable Pipecuronium*
for anesthetic purposes. Most potent N.D muscle relaxant ----> Doxacurium*
• Methoxyflurane has a high nephrotoxic potential and its Least potent N.D muscle relaxant ----> Gallamine*
use has been discontinued. Shortest acting depolarising M.R. ----> Succinylcholine*
• Eflur ane i s also nephrotoxic, thoug h lesser than Overall shortest acting M.R. ----> Succinylcholine*
Methoxyflurane and is also not recommended. • Most potent N.D muscle relaxant
Isoflurane, sevoflurane and halothane result in little or no – Doxacurium
increase in fluoride levels and are preferred.
• Least potent N.D muscle relaxant
– Gallamine
308. Nephrotoxicity is caused by:
A. Seroflurane
B. Methoxyflurane TOPIC 46: OXYGEN CONCNTRATOR
C. Isoflurane
D. Halothane 311. True about oxygen concentrator:
B A. Zeolite activation
..........(AIPGMEE - 1998) B. Delivers O2
C. Requires power supply
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 64
D. Gives O2 at 100 % Hematological advantages of Membrane oxygenators vs Bubble
A, B & C oxygenators.
..........(PGI - JUNE 2005) i) Less trauma to red blood cells
ii) Less trauma to platelets
• Oxygen concentrators are devices that extracts O2 from iii) Less trauma to white blood cells
atmospheric air for which a zeolite molecular sieve is used. iv) Less protein denaturation.
– The atmospheric air is exposed to the zeolite sieve at a Due to these advantages membrane oxygenators have
certain pressure which selectively retains the N2 & other largely replaced bubble oxygenators .
constituents of air & thus O2 of about 95% can be The oxygenators which were used in past Vertical screens
achieved. Disc oxygenators
312. Which of the following produces the least damage TOPIC 47: PERIBULBAR BLOCK
to blood elements -
A. Disc oxygenator 313. Complication of peribulbar block:
B. Membrane oxygenator A. Retrobulbular haemorrhage
C. Bubble oxygenator B. Globe rupture
D. Screen oxygenator C. Optic neuritis
B D. Local anaesthetic solution can migrate to brain
..........(AIIMS PGMEE - NOV 2004) E. Vasovagal syncope
ALL
Oxygenators are devices used in cardiopulmonary bypass ..........(PGI - DEC 2004)
surgeries.
Currently only two types of oxygenators i.e. membrane and 314. In general, the last muscle to be rendered akinetic
bubble oxygenators are in use. with a retrobulbar anesthetic block is:
Membrane oxygenators (Pump oxygenerators) are more A. Superior rectus
commonly used because they have improved the efficiency B. Superior oblique
of gas exchange while minimizing the trauma to the C. Inferior oblique
blood elements. D. Levator palpebral superioris
B
..........(AIIMS PGMEE - MAY 2006)
Retrobulbar anaesthesia -
• Retrobulbar block is regional anaesthesia for eye surgery.
• In this technique local anaesthetic is injected behind
the eye into the cone formed by extraocular
muscles.
• Retrobulbar injection is given with a special needle which
is having a rounded tip.
This lid penetrates the lower lid at the junction of the
middle and lateral one third of the orbit (usually. 5 cm
medial to the lateral canthus).
• Choice of local aneasthetic varies, but lidocaine 2% and
bupivacaine .75% are most common.
• To enhance the retrobulbar spread of local anaesthetic
Membrane oxygenators imitate the natural lung by
Hyaluronidase, a hydrolyzer of connective tissue
interspersing a thin membrane between gas and blood
polysaccharide is frequently added.
phases.
This eliminates gaseous microemboli formation and
• A properly placed retrobulbar injection is effective within
minimizes blood trauma.
seconds and blocks all extraocular muscles except the
superior oblique muscle, affects the ciliary ganglion
(resulting in pupillary dilatation) and anesthetizes the entire
globe.
A successful retrobulbar block is accompanied by anaesthesia,
akinesia, and abolishment of the oculocephalic reflex
(i.e. a blocked eye does not move during head turning).
Complications of retrobulbur anaesthesia -
• Retrobulbar hemorrhage
• Globe perforation
• Optic nerve atrophy
• Frank convulsion
• Oculocardiac reflex
• Acute neurogenic pulmonary edema
• Trigeminal nerve block
• Respiratory arrest
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 65
TOPIC 48: PORPHYRIA
315. Drugs contraindicated in acute intermittent
porphyria:
A. Thiopentone
B. Etomidate
C. Ketamine
D. Propofol
E. Midazolam
A&B
..........(PGI - DEC 2004)
Drugs Recommendati
on
Inhaled anaesthetics Safe
Nitrous oxide & volatile anaesthetics
Intravenous anaesthetics
Propofol, ketamine, Midazolam Safe
Thiopental, thiamylal, methohexital & Unsafe
Etomidate
Analgesics
Aspirin, Morphine Safe • onset of Horner’s syndrome indicates a successful stellate
Ketorolac, phenacetin & pentazocine Unsafe block.
Muscle relaxants
Succinylcholine, pancuronium, Safe
atracurium, vecuronium
Anticholinergics
• Stellate ganglion block (cervicothoracic sympathetic
Atropine & glycopyrrolate Safe block)
Anticholinestenase Indications
Neostigmine safe Pain syndromes
Complex regional pain syndrome type I and II
316. The drug which is not suitable for patients with Refractory angina
acute porphyria for intravenous induction is: Phantom limb pain
A. Thiopentone sodium Herpes zoster
B. Propofol Shoulder/hand syndrome
C. Midazolam Angina
D. Etomidate Vascular insufficiency
NONE Raynaud’s syndrome
..........(AIIMS PGMEE - MAY 2005) Scleroderma
Frostbite
TOPIC 49: STELLATE GANGLION BLOCK Obliterative vascular disease
Vasospasm
317. A pt. in the ICU was on invasive monitoring with Trauma
intra arterial cannulation through the right radial Emboli
artery. For the last 3 days later he developed swelling Contraindications
and discoloration of the right hand. The next line of – Coagulopathy
management is: Recent myocardial infarction
A. Brachial block Pathological bradycardia
B. Stellate ganglion block Glaucoma
C. Application of lignocaine jelly over the site
D. Radial nerve block on the same side • Chassaignac’s tubercle
B This is the anterior tubercle of the transverse process of
..........(AIIMS PGMEE MAY - 2001) the sixth cervical vertebra, which lies lateral to and at a
slightly higher level than the posterior tubercle, and against
Stellate ganglion block which the carotid artery may be compressed by the finger.
• Anatomy
The stellate ganglion refers to the ganglion formed by • Stellate ganglion blocks have been traditionally performed
the fusion of the inferior cervical and the first blindly by palpating the transverse process of C6 and
thoracic ganglion as they meet anterior to the vertebral infiltrating a large volume (as much as 20 mL) of local
body of C7. It is present in 80% of subjects. It usually lies anesthetic. This technique is dependent on enough
on or above the neck of the first rib. volume reaching the stellate ganglion to result in an
effective block.
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 66
• Pain due to arterial insufficiency can be treated with a 320. The following are used for treatment of
stellate ganglion block, but this would have no effect on postoperative nausea and vomiting following squint
someone with venous insufficiency. surgery in children except:
A. Ketamine.
318. lnterscalene approach to brachial plexus block does B. Ondansetron.
not provide optimal surgical anaesthesia in the area C. Propofol.
of distribution of which of the following nerve D. Dexamethasone
A. Musculocutaneous A
B. Ulnar ..........(.AIPGMEE - 2005)
C. Radial
D. Median Ketamine is not used for treatment of postoperative
B nausea and vomiting. In fact ketamine use is itself
..........(AIPGMEE - 2003) associated with nausea and vomiting and requires
prophylaxis.
“Blockage of inferior trunk of brachial plexus may be incomplete ‘Nausea and vomiting occur and require prophylaxis’
requiring specific blockage ofulnar nerve at the elbow”
TOPIC 51: ASPIRIN
Brachial Plexus Block
Interscalene Axillary Approach Supra clavicular & 321. A pt. Who has on Aspirin for a long period was
Approach Infraclavicular
selected for an elective surgery what should be done:
approaches
A. Infusion of platelet concentrate
Most intense at C5 - C7 Most intense block in More even distribution
dermatomes and least C7-T, of local anaesthesia &
B. Infusion of fresh frozen plasma
intense at C8- T , (ulnar (ulnar can be used for C. Stop Aspirin for 7 days
nerve area) nerve).distribution least procedures on arm, D. Go ahead with surgery maintaining adequate hemostasis
Most optimal for intense in C5-C6 forearm and hand C
Procedures on dermatome ..........(AIIMS PGMEE MAY - 2001)
shoulder, arm and Most optimal for
forearm procedures from elbow
to hand Stop Aspirin for 7 days
TOPIC 50: STRABISMUS SURGERY • Aspirin inhibits TxA2 Synthesis by platelet’s even
in small doses.
319. A 5 Yr old child is scheduled for strabismus(squint)
correction .Induction of anae sthesia is
uneventful.After conjunctival incision as the surgeon This inhibits platelet aggregation
grasps the medial rectus, the anesthesiologists looks
at the cardiac monitor .Why do you think he did that Bleeding time prolonged nearly twice
?.
A. he wanted to check the depth of anesthesia
B. he wanted to be sure that the BP did not fall Effect lasts for about a week
C. he wanted to see if there was an oculocardiac (Turn over time for platelet is 7 days)
reflex
D. He wanted to make sure there was no ventricular if Aspirin is stopped for a week before Surgery
dysrhythmias which normally accompany incision =
C all platelet’s will be renewed
..........(AIIMS PGMEE NOV - 2002) =
bleeding time will become normal.
The anaesthesiologist looked at the cardiac monitor to check
for oculocardiac reflex. The Oculocardiac reflex is induced • Other measures will not help as Aspirin is irreversible
by inhibitor of Tx.A2.
(a) Pressure on the eyeball
(b) Traction on the extra ocular muscle TOPIC 52: BOYLE’S APPARATUS
(c) Orbital haematoma
(d) Ocular trauma 322. True about Boyle’s apparatus:
(e) Eye pain A. Continuous flow machine
B. Liquid anesthetic vapours not used
It is a trigeminovagal reflex. C. Resistance very high
The afferent pathway is through Trigeminal nerve and D. Resistance low
the efferent pathway is through Vagus nerve. A&D
..........(PGI - DEC 2006)
Manifestations-,
• Bradycardia ( most common) • Boyles apparatus was first developed for use in 1917. It
• Cardiac arrythmias was one of the most common types of anaesthetic
• Nodal rhythum equipment used in operating theatre.
• Ectopic beats • It operates on the continuous flow principle whereby
• Ventricular fibrillation gas flows all the time during the inspiratory and expiratory
• Asystole phase of patient respiration, being temporarily stored
during expiration in a reservoir bag.
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 67
• The basic principles of gas anaesthesia have been known section. Which of the following is the anaesthesia
for over a hundred years and are still used. An anaesthetising technique of choice -
agent is delivered to the patient via flow controllers and A. Spinal anaesthesia
mix controllers. B. Epidural anaesthesia
C. General anaesthesia
Normally a mixture of N2O and O2 would act as a carrier for D. Local anaesthesia with nerve blocks
the main agent (i.e. Halothane). C
Most gas apparatus used today is based on the Boyles ..........(AIIMS PGMEE - NOV 2005)
apparatus, and although dated, it is still used in many
hospitals. In coarctation of Aorta, Aorta narrows any where along its
course.
• In Boyles apparatus, the resistance offered by the bottles The most common site for coarctation of Aorta is
is overcome by the pressure of gases from the cylinders. • Just distal to origin of left subclavian artery
After leaving the bottles, the gases accumulate in the • Near the insertion of ligamentum arteriosus
reservoir bag. So, the common clinical presentation in coarctation of Aorta
The rubber tubing connecting this bag with the mask is
is of wide bore, thus minimal resistance to inspiration is • Hypotension, ischemia, distal to the obstruction,
presented to the patient. (circulation is usually diminished in obdominal organs and
pulses are absent in lower extremities)
TOPIC 53: CARBON MONOXIDE • Hypertension proximal to the site of obstruction
(the B.P. in upper extrenities and head and neck is
323. The gas which produces systemic toxicity without increased)
causing local irritation is:
A. Ammonia Effect of coarctation of Aorta on Pregnancy.
B. Carbon monoxide Coarctation of Aorta may lead to compromise of
C. Hydrocyanic acid placental circulation, because the placental circulation
D. Sulfur dioxide is derived from uterine artery, which is a branch of internal
D iliac artery
..........(AIPGMEE - 2002) (all the vessels originating distal to coarctation will
have diminished perfusion)
Carbon monoxide • So, the fetal circulation is in a compromised state in
Carbon monoxide is a colorless, tasteless, non-irritative coarctation of Aorta.
gas, which is produced due to incomplete combustion of
carbon. Anaesthetic considerations that should be taken into
account in case of coarctation of Aorta.
TOPIC 54: CHLORAL HYDRATE • In coarctation of Aorta, any decrease in cardiac output or
cardiac return is deleterious to the fetus because the
324. Which is safest to be used in asthmatic patients: placental circulation is already compromised on account
A. Nitrazepam of coarctation.
B. Phenobarbitone • So any anaesthetic procedure or drug which causes
C. Chloral hydrate hypotension should be avoided in these patients.
D. All hypnotics are safe Regional anaesthetic procedures such as spinal
E. Morphine anaesthesia and epidural anaesthesia should be avoided
C in these patients because hypotension is the most
..........(PGI - 2001 - Dec) common side effect of these procedures.
The consequence of decreased venous return and
• Benzodiazepines at usual hypnotic doses don’t affect decreased systemic vascular resistance as a result of
these procedures would be hazadrous to the
respiration or cardiovascular functions. They are now
patient.
popularly used as preanaesthetic medications because
they produce tranquility and smoothen induction
TOPIC 57: ETHER
with little respiratory depression.
327. All of the following are the disadvantages of
• Benzodiazepines are safe in asthmatics but these
anesthetic ether, except:
tranquilisers (also Nitrazepam), sedatives, opiates, should
A. Induction is slow.
be absolutely avoided in severely ill with asthma, as risk of
B. Irritant nature of ether increases salivary and bronchial
developing depression of alveolar ventilation is great and
secretions.
respiratory arrest may occur.
C. Cautery cannot be used
• Barbiturates cause respiratory and circulatory
D. Affects blood pressure and is liable to produce arrhythmias
depression.
D
Chloral hydrate, promethazine, diphenhydramine can be
..........(.AIPGMEE - 2005)
used satisfactorily.
BP & respiration are generally well maintained because of
TOPIC 55: COARCTATION OF AORTA
reflex stimulation and high sympathetic tone- kdt Cardiac
arrythmias occur rarely with ether and there is no
325. A 30 year old woman with coarctation of aorta is
sensitizatio n of the myocardium to circulating
admitted to the labour room for elective caesarean
catecholamines –
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 68
Induction with ether is very slow (blood gas coefficient • Endotracheal tube one-half size smaller than usual to
12.0) and very unpleasant maximize the chances of easy intubation
Slow induction and recovery • Firm pressure over cricoid cartilage prior to induction
Ether stimulates salivary and bronchial secretions and so (Sellick’s maneuver) e applied to make oesophagus
atropine premedication is given collapsed and prevent regurgitation
It should not be used when diathermy is needed in the • Thiopentone is used as induction agent
airways, because of risk of fire or explosion • The patient is not artificially ventilated to avoid filling
of stomach with gas and thereby increasing the risk of
TOPIC 58: FAT EMBOLISM emesis
• If intubation fails, spontaneous ventilation should be
328. Factors favouring fat embolism in a patient with allowed to return and awake intubation performed
major trauma: • After surgery , patient should remain intubated until
A. Mobility of # airway reflexes and consciousness has been regained.
B. Hypovolemic shock
C. Resp. failure TOPIC 61: TORNIQUET
D. Diabetes
A&D 331. Tourniquet pressure in lower limb surgery:
..........(PGI - June -2001) A. 50 mmHg above systolic
B. 100 mm Hg above systolic
TOPIC 59: OPIOIDS C. 200 mm Hg above systolic
D. Same as systolic BP
329. Best anaesthetic agent for outpatient anaesthesia E. Less than systolic BP
is B
A. Fentanyl ..........(PGI - JUNE 2006)
B. Morphine
C. Alfentanil * Tourniquet pressure is about 100 mm of Hg above the
D. Pethidine systolic blood pressure. The pressure for upper limb is =
C SBP+50mm of Hg & for lower limb is = 2 X SBP.
..........(AIIMS PGMEE - DEC 1994)
TOPIC 62: TRILENE
In outpatient anaesthesia the patients are sent back home
the same day. Therefore agents which are rapidly 332. Which is not compatible with Soda lime:
eleminated are used so that no after effects are left The A. Halothane
agents used are – B. Ether
• Propofol C. N2O
• Alfentanil D. Trilene
• Remifentanil D
• N 2O ..........(AIIMS PGMEE - FEB - 1997)
• Isoflurane • 90% Ca(OH)2*
• Sevofiurane Trilene • 5% Sodium
Hydroxide*
• Desflurane • Soda lime is a mixture of * —>
•1% Potassium
Hydoroxide*
TOPIC 60: RAPID SEQUENCE ANAESTHESIA • Silicates*
330. During rapid sequence induction of anaesthesia:
A. Sellick’s maneuver is not required
B. Pre-oxygenation is mandatory
C. Suxamethonium is contraindicated
D. Patient is mechanically ventilated before endotracheal
intubation
B
..........(AIPGMEE - 2003)
Rapid sequence Induction
This induction technique is used in patient with risk of
aspiration pneumonia (mendelson’ s syndrome) eg.
hiatus hernia or any emergency operation with full
stomach.
In this technique patient is intubated immediately after
induction to avoid vomiting, reguritation and aspiration of
gastric content.
Characteristic features - • Soda lime is used to absorb CO2. When it absorbs CO2
• Patient is always preoxygenated prior to induction it produces heat. All volatile anaesthetic agents are
• Prior Curarization with nondepolarization MR to prevent decomposed by the heat produced as a result of absortion
increase in intra abdominal pressure that accompanies use of CO2 by Soda lime.
of succinyl choline.
HELP LINE NO. 9391567707
MINOR TOPICS ANAESTHESIA 69
• Thermal decomposition of trilene (trichlor ethylene)
and Sevoflurane results in toxic compounds therefore • Xenon was discovered in 1898 and found to be the only
neither of them should be used with sodalime. noble gas to be anaesthetic under normobaric conditions.
• For anaesthetic purposes, it was found very close to the
• Function of soda lime ‘ideal agent”.
Soda lime is used in breathing systems to absorb
expired CO 2 during anaesthesia. Advantages of Xenon anaesthesia
• It can be incorporated in a Mapleson C system or a circle • Inert probably nontoxic with no metabolism
system. Exhaled gases are circled back to the canister, • Unlikely to be involved in any biochemical events in the
where CO2 absorption takes place and water and heat body, can be eliminated via lungs.
are produced. The warmed and humidified gas joins the • Minimal cardiovascular effects.
fresh gas flow to be delivered to the patient. • Low blood solubility.
• Rapid induction and recovery (lowest blood gas
The reaction: partition coefficient)
• Does not trigger malignant hyperthermia
CO2 + H2O leads to H2CO3 • Environmental friendly
2H2CO3 + 2NaOH leads to Na2CO3 + 4H2O + Heat • Non explosive
2Ca(OH)2 + Na2CO3 leads to 2CaCO3 + 2NaOH + Heat
Disadvantages
• In soda lime absorption, the carbon dioxide first reacts • High cost
with water to form carbonic acid , which then reacts • Low potency
with sodium hydroxide to form a soluble carbonate. The • No commercially available anaesthesia equipment
soluble sodium carbonate then reacts with calcium
hydroxide to form an insoluble carbonate and replenishes
the sodium hydroxide. Heat and water are produced
during the reaction. Exhaustion of its activity is indicated
by dyes; the most common one changes from pink to
white
• indicated by dyes; the most common one changes from
pink to white.
Size of granules
The size of the soda lime granules is 4-8 mesh (i.e. will pass
through a mesh of 4-8 strands per inch in each axis or
2.36–4.75 mm).
• Carbon monoxide production has occurred when
volatile agents containing the CHF2 moiety (enflurane/
isoflurane/desflurane) are passed over soda lime that
has become desiccated or dried out.
TOPIC 63: XENON
333. Which of the following is not true about Xenon
anaesthesia
A. Non explosive
B. Minimal cardiovascular side effects
C. Slow induction and slow recovery
D. Low blood gas solubility
C
..........(AIIMS PGMEE - NOV 2006
HELP LINE NO. 9391567707
Vous aimerez peut-être aussi
- CRQs and SBAs for the Final FRCA: Questions and detailed answersD'EverandCRQs and SBAs for the Final FRCA: Questions and detailed answersPas encore d'évaluation
- Graphic Anaesthesia, second edition: Essential diagrams, equations and tables for anaesthesiaD'EverandGraphic Anaesthesia, second edition: Essential diagrams, equations and tables for anaesthesiaPas encore d'évaluation
- Imm Mcqs Solved (Umer Hayat and DR RaliDocument129 pagesImm Mcqs Solved (Umer Hayat and DR RaliJaved GabaPas encore d'évaluation
- Physics and AnaesthesiaDocument6 pagesPhysics and AnaesthesiaSuresh Kumar100% (1)
- AnaesthesiaDocument5 pagesAnaesthesiaAnonymous 4jkFIRalKPas encore d'évaluation
- Physics principles for anesthesiologistsDocument97 pagesPhysics principles for anesthesiologistszeedansmPas encore d'évaluation
- 4 - Pharmacology of Anaesthesia (Updated)Document22 pages4 - Pharmacology of Anaesthesia (Updated)SivaPas encore d'évaluation
- Anesthesia Quiz PDFDocument2 pagesAnesthesia Quiz PDFUmmi Qorin0% (2)
- Anaesthesia and Sedation Outside TheatresDocument15 pagesAnaesthesia and Sedation Outside Theatresمحمد زينPas encore d'évaluation
- Local AnesthesiaDocument9 pagesLocal AnesthesiaSherry RamirezPas encore d'évaluation
- Physics of Anaesthesia Made Easy: Review ArticleDocument7 pagesPhysics of Anaesthesia Made Easy: Review ArticleEinstein A. MustafaPas encore d'évaluation
- Mechanism of Action of Local AnaestheticsDocument19 pagesMechanism of Action of Local AnaestheticsSumit Bhardwaj100% (1)
- Inhalational Anaesthesia McqsDocument35 pagesInhalational Anaesthesia McqsMohamed Saeed El Khayat100% (1)
- Anaesthesia Explained PDFDocument22 pagesAnaesthesia Explained PDFaksinu100% (1)
- Challenges of delayed awakening after anesthesiaDocument3 pagesChallenges of delayed awakening after anesthesiaaksinuPas encore d'évaluation
- Fred Rotenberg, MD Dept. of Anesthesiology Rhode Island Hospital Grand Rounds February 27, 2008Document53 pagesFred Rotenberg, MD Dept. of Anesthesiology Rhode Island Hospital Grand Rounds February 27, 2008lmjeksorePas encore d'évaluation
- Qbase Vol1 2Document209 pagesQbase Vol1 2Alexandra TokajiPas encore d'évaluation
- FINAL FRCA EXAM MCQS APRIL 2009Document16 pagesFINAL FRCA EXAM MCQS APRIL 2009Abouzr Mohammed ElsaidPas encore d'évaluation
- MCQ Anesthesiology Group 4Document3 pagesMCQ Anesthesiology Group 4Law YouPas encore d'évaluation
- Edward Hammond, Andrew McIndoe, Mark Blunt, John Isaac, Ravi Gill, Mike Herbertson, Sundeep Karadia, Elfyn Thomas, Gareth Wrathall - QBase Anaesthesia_ Volume 2, MCQs for the Final FRCA (v. 2)-Greenwi.pdfDocument249 pagesEdward Hammond, Andrew McIndoe, Mark Blunt, John Isaac, Ravi Gill, Mike Herbertson, Sundeep Karadia, Elfyn Thomas, Gareth Wrathall - QBase Anaesthesia_ Volume 2, MCQs for the Final FRCA (v. 2)-Greenwi.pdfFiaz medicoPas encore d'évaluation
- Final FRCA SyllabusDocument26 pagesFinal FRCA SyllabussteffmoPas encore d'évaluation
- Delayed Recovery From AnaesthesiaDocument15 pagesDelayed Recovery From AnaesthesiaSheldon OltonPas encore d'évaluation
- Anesthesia One Liner PDFDocument13 pagesAnesthesia One Liner PDFMinaz PatelPas encore d'évaluation
- Pediatric Anesthesiology Sample QuestionsDocument1 pagePediatric Anesthesiology Sample QuestionsJokevin Prasetyadhi100% (1)
- Anaesthesia On The MoveDocument244 pagesAnaesthesia On The MoveLucas ArenasPas encore d'évaluation
- General Anesthesia: Presented By: Shalakha Bhardwaj BDS Final Year (2007-2011)Document85 pagesGeneral Anesthesia: Presented By: Shalakha Bhardwaj BDS Final Year (2007-2011)KrishnaBihariShuklaPas encore d'évaluation
- Anesthesia NutshellDocument388 pagesAnesthesia NutshellMuhammad UmerPas encore d'évaluation
- Lippincott S Anesthesia Review 1001 Questions And.20Document1 pageLippincott S Anesthesia Review 1001 Questions And.20Reem Salem0% (1)
- ANESTHESIA-Pediatrics Airway SyndromesDocument12 pagesANESTHESIA-Pediatrics Airway SyndromeshollyuPas encore d'évaluation
- Exam ANS Report Final2022 1 PRVDocument18 pagesExam ANS Report Final2022 1 PRVtestingPas encore d'évaluation
- Anesthesiology Lectures - EditedDocument183 pagesAnesthesiology Lectures - EditedNoor Hazilla Waty100% (1)
- Obestetrics GynecologyDocument203 pagesObestetrics GynecologySwamynadh Gandhi ReddiPas encore d'évaluation
- Exm Sba July2012 PDFDocument5 pagesExm Sba July2012 PDFSuhas KapsePas encore d'évaluation
- ACE 2007 4A QuestionsDocument29 pagesACE 2007 4A QuestionsRachana GudipudiPas encore d'évaluation
- Prehospital Anesthesia HandbookDocument46 pagesPrehospital Anesthesia HandbookoscarPas encore d'évaluation
- Diploma Guide - EnglishDocument11 pagesDiploma Guide - EnglishAndra Victoria TitaPas encore d'évaluation
- Telegram Cloud Document 4 5893461163299045618 PDFDocument232 pagesTelegram Cloud Document 4 5893461163299045618 PDFAndreea FlorinaPas encore d'évaluation
- Report On The Constructed Response Question / Short Answer Question Paper - September 2019Document6 pagesReport On The Constructed Response Question / Short Answer Question Paper - September 2019cr7Pas encore d'évaluation
- Context Sensitive Half Time (CSHT) - The Lay Medical ManDocument3 pagesContext Sensitive Half Time (CSHT) - The Lay Medical Manpradeep danielPas encore d'évaluation
- Anesthesiology MCQ Sample Exam e PDFDocument5 pagesAnesthesiology MCQ Sample Exam e PDFOsob MohamudPas encore d'évaluation
- Anaesthesia Outside The Operating Theatre Update 2010Document5 pagesAnaesthesia Outside The Operating Theatre Update 2010Marcella AmadeaPas encore d'évaluation
- 1996 Ite ExamDocument72 pages1996 Ite Exampiano543Pas encore d'évaluation
- General Anesthesia - Induction - UpToDateDocument14 pagesGeneral Anesthesia - Induction - UpToDateTania Parra MoralesPas encore d'évaluation
- Arab-Board ExamDocument104 pagesArab-Board Examahmed.farag.ali2020Pas encore d'évaluation
- Exm Fficm MCQ Sba ExamplequestionsDocument1 pageExm Fficm MCQ Sba ExamplequestionsMuhammad Asim RanaPas encore d'évaluation
- Multiple Choice QuestionsDocument2 pagesMultiple Choice QuestionsChudaman Mahajan100% (1)
- ANZCA Primary Physiology QuestionsDocument34 pagesANZCA Primary Physiology Questionspriyavirdi100% (1)
- Conduct of AnaesthesiaDocument30 pagesConduct of AnaesthesiaAnirban PalPas encore d'évaluation
- Preparation For The Final FRCA 2014 Update1 PDFDocument4 pagesPreparation For The Final FRCA 2014 Update1 PDFSuhas Kapse0% (1)
- Appplied Physics AnesthesiaDocument38 pagesAppplied Physics AnesthesiaBogdan CarabasPas encore d'évaluation
- EMAC Course Handbook V2 3 July 2018Document13 pagesEMAC Course Handbook V2 3 July 2018bobbykrish0% (1)
- Electrolyte and Acid-Base Physiology ReviewDocument85 pagesElectrolyte and Acid-Base Physiology ReviewChee_Yeow_6172100% (1)
- Anesthesiology Examination and Board Review, 7E (2012) (PDF) (UnitedVRG)Document4 pagesAnesthesiology Examination and Board Review, 7E (2012) (PDF) (UnitedVRG)Gilberto GavarretePas encore d'évaluation
- Recent Final Frca Vascular Anaesthesia QuestionsDocument4 pagesRecent Final Frca Vascular Anaesthesia Questionslim sjPas encore d'évaluation
- Paediatric Anaesthesia PDFDocument33 pagesPaediatric Anaesthesia PDFMarcelitaTaliaDuwiriPas encore d'évaluation
- Final - 2018 CA-1 Tutorial Textbook - Smartphone or Tablet-3Document342 pagesFinal - 2018 CA-1 Tutorial Textbook - Smartphone or Tablet-3Nick-Hugh Wisdom100% (1)
- Anesthetic AgentsDocument7 pagesAnesthetic AgentsJan DacioPas encore d'évaluation
- Hong Kong College of Anaesthesiologists Final Fellowship Examination Report August - September 2002Document8 pagesHong Kong College of Anaesthesiologists Final Fellowship Examination Report August - September 2002Jane Ko100% (1)
- Anaesthesia MachineDocument51 pagesAnaesthesia Machinem07wwp100% (1)
- Anesthesiology Resident Manual of Procedures: A Step-by-Step GuideD'EverandAnesthesiology Resident Manual of Procedures: A Step-by-Step GuidePas encore d'évaluation
- Evolution of Mechanical Heart ValvesDocument5 pagesEvolution of Mechanical Heart ValvesvamshidhPas encore d'évaluation
- Evolution of Surgical ValvesDocument8 pagesEvolution of Surgical ValvesvamshidhPas encore d'évaluation
- Antibiotic Guidelines For Adults 2018Document58 pagesAntibiotic Guidelines For Adults 2018vamshidh100% (1)
- The Residency Towers: 15 - 16 SeptemberDocument10 pagesThe Residency Towers: 15 - 16 SeptembervamshidhPas encore d'évaluation
- Biventricular Assist Devices: A Technical Review: S D. G, D T, N G, D G. M, and J F. FDocument16 pagesBiventricular Assist Devices: A Technical Review: S D. G, D T, N G, D G. M, and J F. FvamshidhPas encore d'évaluation
- VIth Annual Cardiac CME 29th& 30th July 2017 RegistrationDocument1 pageVIth Annual Cardiac CME 29th& 30th July 2017 RegistrationvamshidhPas encore d'évaluation
- 9 Clinical Cardiology Update 2017: Institute of Cardio-Vascular DiseasesDocument3 pages9 Clinical Cardiology Update 2017: Institute of Cardio-Vascular DiseasesvamshidhPas encore d'évaluation
- Transplant IndicationsDocument9 pagesTransplant IndicationsvamshidhPas encore d'évaluation
- Azygous LobeDocument1 pageAzygous LobevamshidhPas encore d'évaluation
- Small Aortic RootDocument19 pagesSmall Aortic RootvamshidhPas encore d'évaluation
- The Residency Towers: 15 - 16 SeptemberDocument10 pagesThe Residency Towers: 15 - 16 SeptembervamshidhPas encore d'évaluation
- Are You Dreaming For A PG SEAT in First Attempt ???: Don't Just DreamDocument1 pageAre You Dreaming For A PG SEAT in First Attempt ???: Don't Just DreamvamshidhPas encore d'évaluation
- Challan For Thesis Fees PDFDocument2 pagesChallan For Thesis Fees PDFvamshidhPas encore d'évaluation
- 2 QuestionsDocument54 pages2 QuestionsvamshidhPas encore d'évaluation
- Renal PathologyDocument17 pagesRenal PathologyvamshidhPas encore d'évaluation
- Pamphlet For PrintingDocument1 pagePamphlet For PrintingvamshidhPas encore d'évaluation
- The Radiological Hallmark of Osteogenic SarcomaDocument16 pagesThe Radiological Hallmark of Osteogenic SarcomavamshidhPas encore d'évaluation
- Pamphlet For PrintingDocument1 pagePamphlet For PrintingvamshidhPas encore d'évaluation
- Ophthalmology MCQsDocument173 pagesOphthalmology MCQsvamshidh33% (3)
- Presentation 1 yDocument17 pagesPresentation 1 yvamshidhPas encore d'évaluation
- CTVS (Direct 6 Year)Document16 pagesCTVS (Direct 6 Year)one twoPas encore d'évaluation
- RadDocument66 pagesRadvamshidhPas encore d'évaluation
- Time Table LatestDocument2 pagesTime Table LatestvamshidhPas encore d'évaluation
- Lungs PDFDocument14 pagesLungs PDFvamshidhPas encore d'évaluation
- Fluid Therapy Selection Guide for Medical DisordersDocument4 pagesFluid Therapy Selection Guide for Medical DisordersSandip PatilPas encore d'évaluation
- 193Document76 pages193vamshidhPas encore d'évaluation
- Metro Rail Map Pictorial PDFDocument1 pageMetro Rail Map Pictorial PDFvamshidhPas encore d'évaluation
- SWT Microbiology DamsDocument80 pagesSWT Microbiology DamsvamshidhPas encore d'évaluation
- SWT Pharmacology DamsDocument84 pagesSWT Pharmacology DamsvamshidhPas encore d'évaluation
- Twins Bootcamp StudyDocument5 pagesTwins Bootcamp Studyandi dirhanPas encore d'évaluation
- The Management of Near DrowningDocument8 pagesThe Management of Near DrowningneddiantiseptikaPas encore d'évaluation
- Atomoxetine in ADHD in Children With and Without Comorbid Mood DisordersDocument10 pagesAtomoxetine in ADHD in Children With and Without Comorbid Mood DisordersNeuro GYMPas encore d'évaluation
- Anorectal MalformationDocument40 pagesAnorectal Malformationblessy83% (18)
- High Yield Step 2ckDocument4 pagesHigh Yield Step 2ckCesar_Palana_3832Pas encore d'évaluation
- Potential Long-Term Side Effects of Exposure To ChemoDocument21 pagesPotential Long-Term Side Effects of Exposure To ChemoMichael BublePas encore d'évaluation
- Adjuvant Analgesics (2015) PDFDocument177 pagesAdjuvant Analgesics (2015) PDFsatriomega100% (1)
- Rehab-U FreeMobilityEbook PDFDocument10 pagesRehab-U FreeMobilityEbook PDFTuteraipuni POTHIERPas encore d'évaluation
- BaytexDocument7 pagesBaytexArvind AkkPas encore d'évaluation
- E Stim PDFDocument6 pagesE Stim PDFAlvaro Toledo100% (1)
- Yakult ProfileDocument36 pagesYakult ProfileMubeen NavazPas encore d'évaluation
- 13 Other Blood Group SystemsDocument56 pages13 Other Blood Group SystemsCarinaJongLeePas encore d'évaluation
- Bastidas 2021Document13 pagesBastidas 2021ruben dario meza bertelPas encore d'évaluation
- Euro J of Neurology - 2021 - Van Den Bergh - European Academy of Neurology Peripheral Nerve Society Guideline On DiagnosisDocument28 pagesEuro J of Neurology - 2021 - Van Den Bergh - European Academy of Neurology Peripheral Nerve Society Guideline On DiagnosisSusana RochePas encore d'évaluation
- Full Mouth Rehabilitation: A Smooth Pathway For Complex JourneyDocument8 pagesFull Mouth Rehabilitation: A Smooth Pathway For Complex JourneySkAliHassanPas encore d'évaluation
- Jurnal 1 - Family Counseling in Malaysia Current Issues and PracticesDocument7 pagesJurnal 1 - Family Counseling in Malaysia Current Issues and PracticesMazlan D'GreatPas encore d'évaluation
- Spina Bifida OCCULTADocument1 pageSpina Bifida OCCULTArebelswanteddot_comPas encore d'évaluation
- Melatonina e EndometrioseDocument8 pagesMelatonina e EndometrioseFatima VieiraPas encore d'évaluation
- The Tuskegee Syphilis StudyDocument11 pagesThe Tuskegee Syphilis Studyapi-285171544Pas encore d'évaluation
- Sepsis: Signs and SymptomsDocument5 pagesSepsis: Signs and SymptomssujithasPas encore d'évaluation
- Gastrointestinal System Ppt.-NewDocument117 pagesGastrointestinal System Ppt.-NewFatima Syed100% (3)
- Bronchial Asthma Nursing Care PlansDocument2 pagesBronchial Asthma Nursing Care PlansdeincediannaPas encore d'évaluation
- Mycoplasma Genitalium A4Document1 pageMycoplasma Genitalium A4Nauli NasirPas encore d'évaluation
- Mental Health Act 1987Document35 pagesMental Health Act 1987P Vinod Kumar100% (1)
- Autocoid PharmacologyDocument29 pagesAutocoid PharmacologyLyadelou Fortu100% (1)
- Fear of IntimacyDocument9 pagesFear of IntimacyHelsi MayaPas encore d'évaluation
- The Nursing Process: Dr. Abdalkarim RadwanDocument62 pagesThe Nursing Process: Dr. Abdalkarim RadwanAngelique Ramos PascuaPas encore d'évaluation
- Professional Development of Obstetrician & GynaecologistDocument116 pagesProfessional Development of Obstetrician & GynaecologistDeepa YadavPas encore d'évaluation
- Post Operative Management After TAPVC RepairDocument36 pagesPost Operative Management After TAPVC RepairsreedeviPas encore d'évaluation
- Sarana Prasarana Pelayanan Terpadu (Pandu) Penyakit Tidak Menular Di FKTPDocument3 pagesSarana Prasarana Pelayanan Terpadu (Pandu) Penyakit Tidak Menular Di FKTPdion dqPas encore d'évaluation