Académique Documents
Professionnel Documents
Culture Documents
APH
Transféré par
wedishaDescription originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
APH
Transféré par
wedishaDroits d'auteur :
Formats disponibles
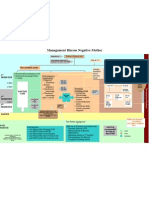
Management of antepartum haemorrage
NB - Emergency
NON- SPECIALIST HOSPITAL trolley ready at all
times (Checked by
sister at every shift &
• History by doctor daily)
• Vital signs/Pain assessment
The serious causes of APH are: • Estimate blood loss
Placenta Praevia • Abdominal palpation (gentle)
Placenta Abruption • *Emergency trolley
Vass Praevia (rare) • IV Cannula (16g)
• Collect blood for: Hb, Group & cross Match
• IV Fluids if necessary
Is there danger to mother or fetal distress?
YES NO
• Resuscitate
• Communicate and transfer to specialist • 24 hours observation of mother and baby in hospital
hospital promptly • Refer to Specialist Hospital for further assessment and care
• Accompanied by doctor / Midwife • Advise patients regarding;
9 Importance of further investigation in Specialist Hospital (E.g.: Ultrasound examination)
9 Warning signs-
Decrease fetal movements.
Further bleeding
Abdominal pain
NB - Emergency trolley
SPECIALIST HOSPITAL ready at all times
(Checked by sister at
every shift & by doctor
Assessment daily)
History
Vital signs/Pain assessment
The serious causes of APH are: Estimate blood loss
Placenta Praevia Abdominal palpation (gentle) o *Emergency trolley
Placenta Abruption o IV Cannula (16g)
Vass Praevia (rare) o Collect blood for: Hb, Group & X Match
o FMH test in Rh neg (Ideal)
Is there danger to mother or fetal distress?
Yes NO
YES
Summon help Management –according to gestation and diagnosis
Obstetrician /Registrar Clinical history and examination
Blood bank officer/Haematologist Consider analgesia
Anaesthetist Ultrasound to confirm placental site
ICU Speculum (If no Placenta Praevia)
Pediatrician If RH negative: *FMH test (Ideal) /Anti D if required
*NB: Kleihauer now Different diagnosis:
known as: Assessment
o Placenta praevia
of Feto-Maternal
Resuscitation (Concurrent management) Haemorrhage (FMH) o Placental abruption
IV cannula16G; Saline, or Hartman Use 9ml EDTA blood o Other causes
Collect blood: collection tube.
o Full blood count Ongoing management is individualized according to gestation,
o Group & Cross-match diagnosis and patient condition.
o Coagulation profile Principles may include:
o *FMH test (Ideal) for Rh negative women-Anti-D if required 20-24 Weeks
o If significant blood loss- increase fluid/blood/blood products Admission
o Oxygen Rest in bed
o Indwelling urinary catheter Maternal monitoring
o Monitor fetal heart rate (available)/continuous Paediatric consultation
Cardiotocography (CTG) 24-36Weeks
o Ongoing maternal monitoring: vital signs, blood loss Consider corticosteroids (usually 24-34 weeks)
Continued fetal surveillance
Confirm diagnosis/gestation Anti D if RH negative
Ultrasound Paediatric consultation
Speculum examination (If no
praevia) 36 weeks
Praevia
Expectant management
Mother & Fetus stable? Yes Elective C.S.
No Yes Abruption
Expectant management
Consider induction 37 weeks+, earlier if fetal
Timing and mode of delivery or maternal distress
determined by gestation and
maternal /fetal status
Sri Lanka College of Obstetrics and Gynaecology
Health sector development Project
Low Risk
Documentation at every step is mandatory Guidelines- Management of antepartum haemorrage
High Risk
Vous aimerez peut-être aussi
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- RhesusDocument1 pageRhesuswedishaPas encore d'évaluation
- Puerperal SepsisDocument1 pagePuerperal Sepsiswedisha100% (1)
- PromDocument1 pagePromwedishaPas encore d'évaluation
- Management of Normal Labour ChartDocument1 pageManagement of Normal Labour ChartwedishaPas encore d'évaluation
- Management of Abnormal Uterine Bleeding Peripheral Unit: Female Presenting To A With AUBDocument1 pageManagement of Abnormal Uterine Bleeding Peripheral Unit: Female Presenting To A With AUBwedishaPas encore d'évaluation
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Marine Science - Marine WormsDocument20 pagesMarine Science - Marine Wormssgw67Pas encore d'évaluation
- Bryonia Phosphorus Sepiaand MedorrhinumDocument39 pagesBryonia Phosphorus Sepiaand Medorrhinummihaipopescu0100% (1)
- Lacunar Infarct - Radiology Reference Article - RadiopaediaDocument8 pagesLacunar Infarct - Radiology Reference Article - RadiopaediaRismanto TorsioPas encore d'évaluation
- Legal Med. Report-QueenDocument61 pagesLegal Med. Report-QueenQuinnee VallejosPas encore d'évaluation
- Kulit Emergency in DermatologyDocument47 pagesKulit Emergency in DermatologyAulia Shabrina SyukharialPas encore d'évaluation
- Pathophysiology of Cyanotic Congenital Heart DefectsDocument16 pagesPathophysiology of Cyanotic Congenital Heart Defectsbonar46Pas encore d'évaluation
- Tibial Tuberosity Advancement For StabilDocument14 pagesTibial Tuberosity Advancement For StabilPaulina BieniaśPas encore d'évaluation
- Spina Bifida PresentationDocument11 pagesSpina Bifida Presentationapi-242435091Pas encore d'évaluation
- The Death of The Moth - Annie DillardDocument3 pagesThe Death of The Moth - Annie DillardjcfxPas encore d'évaluation
- Acute Coronary Syndrome: An Essential & Practical ApproachDocument35 pagesAcute Coronary Syndrome: An Essential & Practical ApproachGinawidiyastutiPas encore d'évaluation
- Hidden Pain: Ehlers-Danlos SyndromeDocument28 pagesHidden Pain: Ehlers-Danlos SyndromeVictoria67% (3)
- Assessment of The Ears Rev 4-2013Document8 pagesAssessment of The Ears Rev 4-2013alphabennydelta4468Pas encore d'évaluation
- Digestive System of GoatsDocument4 pagesDigestive System of Goatssoliun2556100% (2)
- We Are Fungi Ebook Christine NishiyamaDocument23 pagesWe Are Fungi Ebook Christine Nishiyamajeej00Pas encore d'évaluation
- Asuhan Keperawatan (Severe Acute Respiratory Syndrome) : Ns. Kristina., MSNDocument25 pagesAsuhan Keperawatan (Severe Acute Respiratory Syndrome) : Ns. Kristina., MSNMuhammad Sofyan NurPas encore d'évaluation
- Presented by Rasgas Medical Centre: Lowering Your CholesterolDocument22 pagesPresented by Rasgas Medical Centre: Lowering Your CholesterolNarasimhan PPas encore d'évaluation
- What Is EcgDocument5 pagesWhat Is EcgLeeyan MeePas encore d'évaluation
- Diagnostic MethodsDocument93 pagesDiagnostic MethodsSyukri La Ranti100% (3)
- AP Psychology Chapter 2 Study Guide (W/ Answers)Document24 pagesAP Psychology Chapter 2 Study Guide (W/ Answers)JeremiahUmalePas encore d'évaluation
- AppendicitisDocument8 pagesAppendicitisPhoebe Corazon Cercado100% (1)
- Model Test One Structure and Written ExpressionDocument10 pagesModel Test One Structure and Written ExpressionEka KurniatiPas encore d'évaluation
- EktropionDocument31 pagesEktropionapriliaPas encore d'évaluation
- Bmi Lab Viva QuestionDocument7 pagesBmi Lab Viva QuestionnijafancyPas encore d'évaluation
- 1-1 Animal Vaccine Business Opportunity With CavacDocument34 pages1-1 Animal Vaccine Business Opportunity With CavacFamar HivePas encore d'évaluation
- BeekeepingDocument17 pagesBeekeepingApollon Phebo0% (1)
- Class 11 Compiled Chintu Notes ..Document76 pagesClass 11 Compiled Chintu Notes ..Mohammed ArifuddinPas encore d'évaluation
- AQA Biol A Unit 1 Jan02Document20 pagesAQA Biol A Unit 1 Jan02Raymond RayPas encore d'évaluation
- Bowel Sounds: Jibran Mohsin Resident, Surgical Unit I SIMS/Services Hospital, LahoreDocument58 pagesBowel Sounds: Jibran Mohsin Resident, Surgical Unit I SIMS/Services Hospital, LahoreMariajanPas encore d'évaluation
- CDC Ebola Key Messages 10-30 14finalDocument24 pagesCDC Ebola Key Messages 10-30 14finalapi-232950579Pas encore d'évaluation
- Casos Clinicos de Hematopatología IiDocument5 pagesCasos Clinicos de Hematopatología IiRicardo LaraPas encore d'évaluation