Académique Documents
Professionnel Documents
Culture Documents
Laryngeal Complications After Thyroidectomy: Is It Always The Surgeon?
Transféré par
Prabjot SehmiTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Laryngeal Complications After Thyroidectomy: Is It Always The Surgeon?
Transféré par
Prabjot SehmiDroits d'auteur :
Formats disponibles
ORIGINAL ARTICLE
Laryngeal Complications After Thyroidectomy
Is It Always the Surgeon?
Matthias Echternach, MD; Christoph Maurer, MD; Thomas Mencke, MD;
Martin Schilling, MD; Thomas Verse, MD; Bernhard Richter, MD
Hypothesis: Laryngeal dysfunction after thyroidec- Results: The overall rate of laryngeal complications was
tomy is a common complication. However, few data are 42.0% (320 patients). Complications from an injury to
available to differentiate whether these complications re- the vocal folds occurred in 31.3% of patients. Weakness
sult from injury to the recurrent nerve or to the vocal or paresis of the recurrent nerve was initially present in
folds from intubation. 6.6% and was related to the nerves at risk. This rate was
higher in revision thyroidectomies than in primary sur-
Setting: University medical center. gical interventions (6.2% vs 11.6%; P=.04). The rate of
laryngeal injuries was higher in patients older than 65
Patients: Seven hundred sixty-one patients who years (39.8% vs 30.8%; P =.03).
underwent surgery to the thyroid gland from 1990 to
Conclusions: These data suggest that laryngeal compli-
2002. Of these patients, 8.4% underwent a revision
cations after thyroidectomies are primarily caused by in-
thyroidectomy. jury to the vocal folds from intubation and to a lesser ex-
tent by injury to the laryngeal nerve. We recommend
Intervention: Preoperative and postoperative laryngo-
documentation of informed consent, especially for pa-
stroboscopic examination. tients who use their voice professionally, such as sing-
ers, actors, or teachers.
Main Outcome Measure: Laryngostroboscopic evalu-
ation of laryngeal complications. Arch Surg. 2009;144(2):149-153
L
ARYNGEAL COMPLICATIONS AF- going thyroidectomy, the descriptions of
ter thyroidectomy are a com- vocal fold injury are missing. In smaller
mon problem.1-5 The leading groups of patients undergoing thyroidec-
cause of the problem is in- tomy, laryngeal dysfunction was noted by
jury to the recurrent nerve. Stojadinovic et al16 in 2 of 15 symptomatic
Studies performed on large groups of pa- and 2 of 30 asymptomatic patients and by
tients show a prevalence for permanent palsy de Pedro Netto et al17 in 28 of 100 patients.
of the recurrent nerve ranging from 0% In the present study, we sought to deter-
mine the incidence and characteristics of in-
tubation-related vocal fold injuries after thy-
Author Affiliations: Institute See Invited Critique roidectomy in a large group of patients.
for Musicians’ Medicine, at end of article
Freiburg University Medical
Center, Freiburg
METHODS
after primary surgery to 20% after revision
(Drs Echternach and Richter),
Department of Anaesthesiology,
surgery.1-5 Tracheal intubation can lead to A total of 1001 patients were included in the
Rostock University, Rostock hoarseness as well.6,7 The incidence of la- study between 1990 and 2002. All patients
(Dr Mencke), Department of ryngeal injuries caused by intubation is con- scheduled for thyroidectomy underwent pre-
Surgery, Saarland University sidered to be about 6% to 70% after surgi- operative evaluation of the vocal folds. Over-
Medical Center, Homburg cal procedures not adjacent to the larynx.6,8-13 all, 240 patients failed to appear for postop-
(Dr Schilling), and Department To date, there are few data concerning in- erative examination of the vocal folds at our
of Otorhinolaryngology, juries to the vocal folds after surgery in university medical center (reasons included re-
Asklepios Hospital Harburg, fusal of reexamination, subjective rejection of
Hamburg (Dr Verse), Germany;
close relationship to the larynx. Although reevaluation because of good vocal quality, or
and Department of Surgery, Musholt et al14 and Lombardi et al15 report reevaluation by an otolaryngologist at an-
Liestal Hospital, Liestal, that hoarseness is increased and videolaryn- other institution) and were excluded from the
Switzerland (Dr Maurer). goscopy was performed in patients under- analysis.
(REPRINTED) ARCH SURG/ VOL 144 (NO. 2), FEB 2009 WWW.ARCHSURG.COM
149
©2009 American Medical Association. All rights reserved.
Downloaded From: on 05/16/2018
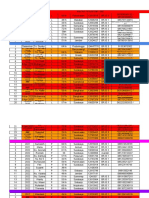
Table 1. General Data for 761 Study Patients Table 3. Preoperative and Postoperative
Laryngostroboscopic Findings in 761 Patients
Variable No. (%)
Diagnosis No. (%)
Sex
Female 528 (69.4) Preoperative findings a
Male 233 (30.6) Laryngitis 52 (6.8)
Age, y Edema 21 (2.8)
Median 51 Cyst 1 (0.1)
Range 7-87 Granuloma 1 (0.1)
ⱕ64 600 (78.8) Polyp 6 (0.8)
ⱖ65 161 (21.2) Leukoplakia 2 (0.3)
Lateralization of surgery Sulcus vocalis 1 (0.1)
Total bilateral 46 (6.0) Hyperfunction 15 (2.0)
Total unilateral 70 (9.2) Hypofunction 21 (2.8)
Subtotal bilateral 413 (54.3) Hyperplasia of ventricular folds 5 (0.7)
Subtotal unilateral 77 (10.1) Palsy of recurrent nerve 14 (1.8)
Total on one side, subtotal on the other side 115 (15.1) Postoperative findings b
Bilateral node extirpation 32 (4.2) Hematoma 70 (9.2)
Unilateral node extirpation 6 (0.8) Granuloma 68 (8.9)
Resection at the isthmus 2 (0.3) Thickening of mucosa 104 (13.7)
First thyroidectomy 697 (91.6) Edema 29 (3.8)
Revision thyroidectomy 64 (8.4) Subluxation of arytenoid cartilage 1 (0.1)
Recurrent nerve palsy 84 (11.0)
a Two patients had 2 different kinds of laryngeal changes.
b Three hundred fifty-six alterations were noted in 320 patients.
Table 2. Histopathologic Findings at Thyroidectomy
ralysis of the recurrent nerve were considered separately because
Finding No. (%) a their origin after thyroidectomy (because of the surgical pro-
Malignant lesion 59 (7.8)
cedure or intubation) is still unclear.
Follicular 21 (35.5)
In all patients, age, sex, histopathologic diagnosis, and re-
Papillary 19 (32.2) port of the surgical procedure were analyzed (Table 1 and
Lindsay tumor b 6 (10.2) Table 2). For comparison between groups, the 2 test and Ken-
Anaplastic 1 (1.7) dall -b rank correlation were used. Statistical significance was
Medullary 9 (15.3) defined with a 95% confidence interval (P⬍.05).
Paraganglioma 1 (1.7)
Metastasis 2 (3.4)
RESULTS
Benign lesion 702 (92.2)
Nodular goiter and adenoma 576 (82.1)
Thyroiditis 70 (10.0) At preoperative stroboscopic examination, we found 139
Hyperparathyroidism 54 (7.7) alterations of the vocal folds in 137 patients (18.0%;
Oncocytoma 2 (0.3) Table 3). Fourteen patients (1.8%) had preexisting palsy
a The percentages for the main categories “Malignant lesion” and “Benign
of the recurrent nerve. Eight of these patients had pre-
lesion” are based on the entire cohort of 761 patients; the percentages for
viously undergone a surgical procedure with a nerve at
the subcategories are based on 59 and 702 patients, respectively. risk (thyroid gland [n=7] or transcervical approach to
b Also known as follicular differentiated papillary thyroid carcinoma.
the spinal cord [n = 1]). In 2 patients, the paresis was
caused by a malignant lesion and, in 4 patients, the cause
was unknown.
In each of the remaining 761 patients (Table 1), preop- The total number of nerves at risk was 1365. In 2 pa-
erative and postoperative endoscopic laryngostroboscopy
tients, only resection in the area of the thyroid isthmus
(Timcke Elektromedizinische Geräte, Hamburg, Germany) was
performed by an experienced otolaryngologist. Compared with was performed, without any risk of damage to the laryn-
laryngoscopy, laryngostroboscopy provides more detailed in- geal recurrent nerve.
formation about vocal fold oscillations such as amplitudes and The histopathologic findings revealed a malignant le-
mucosa waves and the glottic closure18 and is more sensitive sion in 59 patients (7.8%) (Table 2). Two patients had
for detection of even small alterations. The postoperative ex- thyroid metastasis from primary tumors in a kidney and
amination was performed on day 3 or 4 after surgery. in the stomach. In 21 patients (2.8%), surgical compli-
Laryngeal complications were defined as newly discovered cations during or after thyroidectomy were cited in the
findings at the vocal folds after surgery compared with the pre- surgical reports, with the most prevalent complication
operative status. Specific attention was placed on findings de- being bleeding in the surgical area in 10 patients (47.6%
scribed in the literature6,9-14,16,19 such as edema, granulations,
of surgical complications). No descriptions of injury to
hematomas, dislocation of the arytenoid cartilage, and fibrin-
ous laryngitis or thickening of the vocal folds. All of these con- the recurrent nerve were noted in the surgical reports.
ditions resulted in incomplete closure of the rima glottidis or The overall rate of postoperative laryngeal complica-
changes in the amplitude of the vocal fold vibration or move- tions after surgery was 42.0%. Thirty-six patients exhib-
ments of the mucosa wave and, therefore, caused hoarse- ited 2 different kinds of laryngeal complications. The rate
ness.6,9-14,16,19 Apart from these complications, weakness and pa- of vocal fold injury was estimated at 31.3% (Table 3). Only
(REPRINTED) ARCH SURG/ VOL 144 (NO. 2), FEB 2009 WWW.ARCHSURG.COM
150
©2009 American Medical Association. All rights reserved.
Downloaded From: on 05/16/2018
1 patient experienced subluxation of the arytenoid car-
A
tilage, which was repositioned in a subsequent surgical
procedure that resulted in good improvement in vocal
function. No statistically significant occurrence of later-
alization of granulomas occurred (P = .63) (Figure, A).
Although edema was more unilateral than bilateral (n=20
vs n=9; P=.04), there was no dominance of one side over
the other (P=.37). Only hematomas (Figure, B) were more
prevalent unilaterally (left side, n = 46; right side, n=20;
bilateral, n=4; P ⬍.001).
Patients with preoperative alteration of the vocal folds
did not demonstrate a statistically significant higher rate
of postoperative vocal fold injury compared with pa-
tients without any alterations (P=.06). Patients with pre-
operative superficial laryngitis, characterized by injec-
tion of vessels, did not have a statistically significant higher
rate of postoperative hematoma (P= .31). There was no
significant difference associated with the patients’ sex B
(P=.15). Older patients (ⱖ65 years) exhibited more al-
terations in the vocal folds than did younger patients
(39.8% vs 30.8%; P = .03).
Overall weakness or paralysis of the recurrent nerve
was noted in 78 patients unilaterally and in 6 patients
bilaterally. There was no injury to the superior laryn-
geal nerve. For the 1365 nerves at risk, the rate of recur-
rent nerve palsy was 6.6%. No significant difference was
noted in the rate of recurrent nerve palsy associated with
malignant lesions (P = .13) or age (P= .23). According to
the surgical reports, there were descriptions of prepara-
tion of the recurrent nerves in 1345 nerves at risk (98.5%).
In our data, the kind of dissection (total dissection, par-
tial dissection, or no dissection) compared with the nerves
at risk had no significant influence on the rate of recur-
rent nerve palsy (P = .10). Only revision surgery was as- Figure. Indirect laryngoscopic views of a granuloma on the left vocal fold at
sociated with higher rate of impairment of the recurrent the vocal process (A) and a hematoma on the right vocal fold (B).
nerve (6.2% vs 11.6%; P = .04).
The reason for this might be the earlier performance of
laryngostroboscopy. Compared with recent prospective
COMMENT
studies in smaller patient groups, our data reflect a simi-
lar frequency of intubation-related laryngeal inju-
To our knowledge, in the present study, we demon- ries.10,12 However, these studies excluded patients who
strated for the first time in a large group of patients that underwent an operation performed close to the larynx.
damage to the recurrent nerve is not the most prevalent The comparable number of laryngeal injuries led the au-
cause of laryngeal complications after thyroidectomy. Ap- thors to believe that, compared with intubation and ex-
proximately 40% of our patients had impairment in vo- tubation, thyroidectomy causes minor risk to the lar-
cal function overall; however, 3 to 4 days after surgery, ynx.10-12 Similar findings were reported in a smaller group
injury to the vocal folds was noted about 3 times more of patients undergoing thyroidectomy.17
often than palsy of the recurrent nerve. Among many risk factors for injury to the vocal folds
We found injury to the vocal folds, presumably caused caused by intubation are cuff pressure, size of the tube,
by intubation or extubation, in 31% of our patients. Com- movement of the tube, physical trauma, intubation envi-
pared with findings in older studies that found laryn- ronment, duration of intubation, gastroesophageal reflux,
geal injuries of 6.2% to 16.3%, our data suggest a much and mucociliary mechanism.10,21 However, previous stud-
higher rate for these complications.9,13,20 Previous au- ies found no significant influence of the drug used for re-
thors who examined intubation-related complications laxation after rapid-sequence induction and no reduction
chose a longer interval after surgery and used laryngos- in vocal fold injury using neuromuscular monitoring.11,12
copy or mirror stroboscopy rather than endoscopic laryn- In contrast to our findings, Weymuller22 found higher rates
gostroboscopy. Endoscopic laryngostroboscopy is a more of hoarseness in women. Other authors were unable to con-
sensitive method for detecting small alterations in the vo- firm a relationship between the size of the tube and changes
cal folds. Pröschel and Eysholdt,6 who investigated short- in the acoustic signal.23 We found more vocal fold injuries
term alterations of the larynx after intubation, exam- in older patients, presumably due to a decrease in flexibil-
ined the vocal folds 1 to 2 days after surgery and found ity and atrophy of the vocal tissues.24 In this study, other
an even higher rate of complications (73%) than we did. potential risk factors such as nicotine use, ethanol abuse,
(REPRINTED) ARCH SURG/ VOL 144 (NO. 2), FEB 2009 WWW.ARCHSURG.COM
151
©2009 American Medical Association. All rights reserved.
Downloaded From: on 05/16/2018
and gastroesophageal reflux were not evaluated. It is pos- we preoperatively found idiopathic recurrent nerve
sible that these potential risk factors increase the risk of in- palsy. It is presumed that recurrent nerve palsy would
tubation-related complications. be considered a surgical complication after thyroidec-
Similar to other studies,6,10,12 the most common find- tomy without any preoperative laryngologic examina-
ing in our study was thickening of the mucosa in the pos- tion. This emphasizes the need for preoperative laryn-
terior parts of the vocal folds, followed by hematoma. goscopy before thyroidectomy, at least for medicolegal
Whether these alterations are caused by laceration or by reasons.
gastroesophageal reflux remains unclear. However, al- Our data suggest that laryngeal complications caused
terations in the posterior part of the vocal folds have been by injury to the vocal folds occur much more frequently
thought to be induced by the tube or by an adduction than impairment of the recurrent nerve function, thus
reaction of the vocal folds caused by superficial anesthe- confirming findings in smaller patient groups. We rec-
sia.6 Subluxation of the arytenoid cartilage was found in ommend documentation of informed consent, espe-
only 1 patient, and only rarely has dislocation of the ary- cially for patients who use their voice professionally, such
tenoid cartilage been reported.25 Similar to our findings, as singers, actors, or teachers.
Kambic and Radsel9 found such dislocation in only 1 of
1000 patients. To avoid ankylosis of the cricoarytenoid
joint, early surgical mobilization is recommended.19 Accepted for Publication: February 1, 2008.
Our data confirm findings in the subgroup of hema- Correspondence: Matthias Echternach, MD, Institute for
tomas in which a higher rate of laryngologic complica- Musicians’ Medicine, Freiburg University Medical
tions was found on the left side, presumably due to the Center, Breisacher Str 60, 79106 Freiburg, Germany
anesthesiologist being right-handed.9,13 Granulations and (matthias.echternach@uniklinik-freiburg.de).
thickening were primarily found bilaterally in the pos- Author Contributions: Dr Echternach had full access to
terior part of the vocal folds, presumably more the re- all of the data in the study and takes responsibility for
sult of chronic irritation by the endotracheal tube. the integrity of the data and the accuracy of the data analy-
It has been suggested that vocal fold injuries are fre- sis. Study concept and design: Echternach, Maurer, and
quently noted in the first days after surgery but that they Mencke. Acquisition of data: Echternach and Schilling.
heal quickly.6,8 Peppard and Dickens13 described heal- Analysis and interpretation of data: Echternach, Maurer,
ing of glottal hematomas within 4 weeks in 21 of 22 pa- Mencke, Verse, and Richter. Drafting of the manuscript:
tients. Analysis of hoarseness with acoustic or percep- Echternach, Verse, and Mencke. Critical revision of the
tive measurements14-17 cannot be offered because of the manuscript for important intellectual content: Echternach,
large number of patients. However, because of the risk Maurer, Mencke, Schilling, Verse, and Richter. Statisti-
of persisting alterations with long-term impairment of the cal analysis: Echternach, Mencke, and Verse. Adminis-
voice, we recommend laryngologic follow-up examina- trative, technical, and material support: Echternach, Maurer,
tions for patients who use their voice professionally (eg, Verse, and Richter. Study supervision: Maurer, Mencke,
professional singers, actors, or teachers). Schilling, Verse, and Richter.
There is comprehensive literature about the preva- Financial Disclosure: None reported.
lence of recurrent nerve palsy after thyroidectomy. Stud- Additional Information: This study was performed at the
ies with a large number of patients show prevalence for Departments of Otolaryngology (Drs Echternach and
permanent paresis to be between 0% after primary sur- Verse), Surgery (Drs Maurer and Schilling), and Anes-
gery and 20% after revision surgery.1-5 Our findings are thesiology (Dr Mencke) at Saarland University Medical
within this range. Center, Homburg, Germany.
In the present study, no intraoperative monitoring of Additional Contributions: Volker Barth, MD, acquired
the laryngeal recurrent nerve was performed. There is still data and examined patients; Thomas Fuchs-Buder, MD,
controversy about the use of intraoperative recurrent nerve supervised the study; and Kenan Demiroglu performed
monitoring. Despite some publications recommending statistical analysis and acquired data.
monitoring, recent studies could not show lower inci-
dences of postoperative recurrent nerve palsy with moni- REFERENCES
toring.26,27 Similar to our data, Steurer et al28 showed that
surgical dissection of the recurrent nerve did not in- 1. Wagner HE, Seiler C. Recurrent laryngeal nerve palsy after thyroid gland surgery.
crease the total risk of temporary and permanent palsy. Br J Surg. 1994;81(2):226-228.
2. Thomusch O, Machens A, Sekulla C, et al. Multivariate analysis of risk factors
Furthermore, the risk of permanent impairment of re- for postoperative complications in benign goiter surgery: prospective multi-
current nerve function was reduced. Therefore, dissec- center study in Germany. World J Surg. 2000;24(11):1335-1341.
tion should be recommended. 3. Seiler CA, Glaser C, Wagner HE. Thyroid gland surgery in an endemic region.
Although there is much more risk of damaging the World J Surg. 1996;20(5):593-596.
4. Harness JK, Fung L, Thompson NW, Burney RE, McLeod MK. Total thyroidec-
nerve during thyroidectomy, it should be mentioned that tomy: complications and technique. World J Surg. 1986;10(5):781-786.
the nerve can be injured during intubation as well.29 Still, 5. Edis AJ. Prevention and management of complications associated with thyroid
it does not seem possible to differentiate between the dam- and parathyroid surgery. Surg Clin North Am. 1979;59(1):83-92.
age done by thyroid surgery and anesthesia in most cases. 6. Pröschel U, Eysholdt U. Short-term changes in the larynx and voice after intu-
Beyond the postoperative results, it was also interest- bation [in German]. Laryngorhinootologie. 1993;72(2):93-97.
7. Benjamin B. Laryngeal trauma from intubation: endoscopic evaluation and
ing that the incidence of preoperative laryngeal findings classification. In: Cummings CW, Fredrickson JM, Harker LA, Krause CJ, Rich-
was so high. Our patients did not see any reason to visit ardson MA, Schuller DE, eds. Otolaryngology-Head and Neck Surgery. St Louis,
an otolaryngologist because of their voice. In 4 patients, MO: Mosby; 1998:2013-2035.
(REPRINTED) ARCH SURG/ VOL 144 (NO. 2), FEB 2009 WWW.ARCHSURG.COM
152
©2009 American Medical Association. All rights reserved.
Downloaded From: on 05/16/2018
8. Chilla R, Gabriel P, Ilse H. The short-time–intubation as a cause of morphologi- general anaesthesia: anaesthesiological and laryngological aspects [in German].
cal and functional disorders of the larynx [in German]. Laryngol Rhinol Otol (Stuttg). Anaesthesist. 2007;56(2):177-192.
1976;55(2):118-123. 20. Zimmert M, Zwirner P, Kruse E, Braun U. Effects on vocal function and inci-
9. Kambic V, Radsel Z. Intubation lesions of the larynx. Br J Anaesth. 1978;50(6): dence of laryngeal disorder when using a laryngeal mask airway in comparison
587-590. with an endotracheal tube. Eur J Anaesthesiol. 1999;16(8):511-515.
10. Mencke T, Echternach M, Kleinschmidt S, et al. Laryngeal morbidity and quality 21. Loucks TM, Duff D, Wong JH, Finley-Detweiler R. The vocal athlete and endo-
of tracheal intubation: a randomized controlled trial. Anesthesiology. 2003; tracheal intubation: a management protocol. J Voice. 1998;12(3):349-359.
98(5):1049-1056. 22. Weymuller EA Jr. Laryngeal injury from prolonged endotracheal intubation.
11. Mencke T, Knoll H, Schreiber JU, et al. Rocuronium is not associated with Laryngoscope. 1988;98(8, pt 2)(suppl 45):1-15.
more vocal cord injuries than succinylcholine after rapid-sequence induction: 23. Horii Y, Fuller BF. Selected acoustic characteristics of voices before intubation
a randomized, prospective, controlled trial. Anesth Analg. 2006;102(3):943- and after extubation. J Speech Hear Res. 1990;33(3):505-510.
949. 24. Titze IR. Principles of Voice Production. Englewood Cliffs, NJ: Prentice-Hall In-
12. Mencke T, Echternach M, Plinkert PK, et al. Does the timing of tracheal intuba- ternational Inc; 1994.
tion based on neuromuscular monitoring decrease laryngeal injury? a random- 25. Rieger A, Hass I, Gross M, Gramm HJ, Eyrich K. Intubation trauma of the larynx: a
ized, prospective, controlled trial. Anesth Analg. 2006;102(1):306-312. literature review with special reference to arytenoid cartilage dislocation [in German].
13. Peppard SB, Dickens JH. Laryngeal injury following short-term intubation. Ann Anasthesiol Intensivmed Notfallmed Schmerzther. 1996;31(5):281-287.
Otol Rhinol Laryngol. 1983;92(4, pt 1):327-330. 26. Chan WF, Lang BH, Lo CY. The role of intraoperative neuromonitoring of recur-
14. Musholt TJ, Musholt PB, Garm J, Napiontek U, Keilmann A. Changes of the speak- rent laryngeal nerve during thyroidectomy: a comparative study on 1000 nerves
ing and singing voice after thyroid or parathyroid surgery. Surgery. 2006;140 at risk. Surgery. 2006;140(6):866-872.
(6):978-988. 27. Shindo M, Chheda NN. Incidence of vocal cord paralysis with and without re-
15. Lombardi CP, Raffaelli M, D’Alatri L, et al. Voice and swallowing changes after current laryngeal nerve monitoring during thyroidectomy. Arch Otolaryngol Head
thyroidectomy in patients without inferior laryngeal nerve injuries. Surgery. 2006; Neck Surg. 2007;133(5):481-485.
140(6):1026-1032. 28. Steurer M, Passler C, Denk DM, Schneider B, Niederle B, Bigenzahn W. Advan-
16. Stojadinovic A, Shaha AR, Orlikoff RF, et al. Prospective functional voice assess- tages of recurrent laryngeal nerve identification in thyroidectomy and parathy-
ment in patients undergoing thyroid surgery. Ann Surg. 2002;236(6):823-832. roidectomy and the importance of preoperative and postoperative laryngo-
17. de Pedro Netto I, Fae A, Vartanian JG, et al. Voice and vocal self-assessment scopic examination in more than 1000 nerves at risk. Laryngoscope. 2002;
after thyroidectomy. Head Neck. 2006;28(12):1106-1114. 112(1):124-133.
18. Fleischer S, Hess M. The significance of videostroboscopy in laryngological prac- 29. Friedrich T, Hänsch U, Eichfeld U, Steinert M, Staemmler A, Schönfelder M.
tice [in German]. HNO. 2006;54(8):628-634. Recurrent laryngeal nerve paralysis as intubation injury [in German]? Chirurg.
19. Reber A, Hauenstein L, Echternach M. Laryngopharyngeal morbidity following 2000;71(5):539-544.
INVITED CRITIQUE
H oarseness is a dreaded complication after thy-
roidectomy. Even in the most experienced
hands, significant postoperative voice changes
occur in more than 5% to 10% of patients. Echternach
et al report that 42% of patients undergoing thyroidec-
of the gland? Is the incidence of vocal fold trauma in pa-
tients undergoing operations on the outside of the neck
similar? A control group such as this would have pro-
vided this information. Third, there are no data in this
article to suggest that recognizing laryngeal dysfunc-
tomy at their institution experienced a laryngeal com- tion preoperatively or postoperatively affects patient out-
plication. Most of these complications were unrelated to comes. Fourth, because only 23.8% of patients with la-
injury to the recurrent nerve by the surgeon but caused ryngeal injuries received long-term follow-up, we do not
by trauma to the vocal folds after intubation. While these know the long-term implications of these injuries. It is
finding are enlightening (and relieving!) to those of us hoped that additional data from this group and others
who perform thyroid operations, there are still unre- will shed light on these important issues.
solved issues and questions about the data in this study.
First, there are no data about patient symptoms associ- Herbert Chen, MD
ated with the laryngeal complications. If most patients
did not have symptoms, what is the clinical importance Correspondence: Dr Chen, Department of Surgery, Uni-
of the findings? Second, do we know for certain that most versity of Wisconsin Medical School, H4/750 Clinical Sci-
of the vocal fold injuries were caused by endotracheal ence Center, 600 Highland Ave, Madison, WI 53792 (chen
intubation rather than intraoperative abrasions or trauma @surgery.wisc.edu).
from pulling on the thyroid and trachea during removal Financial Disclosure: None reported.
(REPRINTED) ARCH SURG/ VOL 144 (NO. 2), FEB 2009 WWW.ARCHSURG.COM
153
©2009 American Medical Association. All rights reserved.
Downloaded From: on 05/16/2018
of air via the colonoscope to test the anastomosis, data though the data presented did not comment on details
supporting its use as a method of ensuring anastomotic such as the circumferential nature of the initial leak, the
integrity is, at best, inconclusive. This large study of left- percentage of the anastomosis that had to be primarily
sided colorectal anastomoses reveals that, indeed, anas- repaired (perhaps number of 3-0 silks used), or the pre-
tomotic leak testing is beneficial and that an airtight anas- existing comorbidities of these patients related to risk of
tomosis may be a reliable indicator of anastomotic an anastomotic leak, the data from this article proposes
integrity. Three very important conclusions are brought an algorithmic approach to the results of the intraopera-
to the forefront. First, an airtight anastomosis does not tive anastomotic leak testing following colorectal resec-
guarantee that anastomotic disruption will not occur post- tion and directs the surgeon to the need to repair, re-
operatively. Second, primary repair of a colorectal anas- resect, or divert.
tomosis that does not subsequently leak on testing also
does not guarantee a subsequent postoperative anasto- Walter E. Longo, MD
motic leak. Third, these data seem to suggest that an ini-
tial positive anastomotic leak test that either repair with Correspondence: Dr Longo, Yale School of Medicine, De-
fecal diversion or resecting the initial anastomosis and partment of Surgery, PO Box 208062, New Haven, CT
performing a new colorectal anastomosis will offer the 06520-8062 (walter.longo@yale.edu).
best chance of not encountering a postoperative leak. Al- Financial Disclosure: None reported.
Correction
Middle Initial Missing From Author Name. In the ar-
ticle titled “Laryngeal Complications After Thyroidec-
tomy: Is It Always the Surgeon?” by Echternach et al,
published in the February issue of the Archives (2009;
144[2]:149-153), the second author’s middle initial was
omitted from the byline on page 149. It should have read
as follows: Christoph A. Maurer, MD.
(REPRINTED) ARCH SURG/ VOL 144 (NO. 5), MAY 2009 WWW.ARCHSURG.COM
412
©2009 American Medical Association. All rights reserved.
Downloaded From: on 05/16/2018
Vous aimerez peut-être aussi
- Postlaryngectomy voice rehabilitation with voice prosthesesD'EverandPostlaryngectomy voice rehabilitation with voice prosthesesPas encore d'évaluation
- Hoarseness After Thyroidectomy: Blame The Endocrine Surgeon Alone?Document11 pagesHoarseness After Thyroidectomy: Blame The Endocrine Surgeon Alone?ruthchristinawibowoPas encore d'évaluation
- Smooking MeriDocument6 pagesSmooking MeriarifPas encore d'évaluation
- 03 In-Office Endoscopic Laryngeal Laser ProceduresDocument7 pages03 In-Office Endoscopic Laryngeal Laser ProceduresG WPas encore d'évaluation
- Otolaryngol - Head Neck Surg - 2010 - Aynehchi - Systematic Review of Laryngeal Reinnervation TechniquesDocument11 pagesOtolaryngol - Head Neck Surg - 2010 - Aynehchi - Systematic Review of Laryngeal Reinnervation TechniquesAlejandra BenavidezPas encore d'évaluation
- Traumatic Perforations of Tympanic Membrane: Our Experience: Original Research ArticleDocument4 pagesTraumatic Perforations of Tympanic Membrane: Our Experience: Original Research ArticleXlr8zzPas encore d'évaluation
- A Comparison of Two Endoscopic Posterior Cordotomy Techniques: Laser Cordotomy Vs Diathermy-Assisted CordotomyDocument5 pagesA Comparison of Two Endoscopic Posterior Cordotomy Techniques: Laser Cordotomy Vs Diathermy-Assisted CordotomyGöksel TurhalPas encore d'évaluation
- 1808 8694 Bjorl 85 01 0003 PDFDocument8 pages1808 8694 Bjorl 85 01 0003 PDFruthchristinawibowoPas encore d'évaluation
- US Pulmón para Manejo de Atelectasias PerioperatoriasDocument11 pagesUS Pulmón para Manejo de Atelectasias PerioperatoriasJURAGOMAPas encore d'évaluation
- Difficult Intubation and Anesthetic Management in An Adult Patient With Undiagnosed Congenital Tracheal Stenosis: A Case ReportDocument6 pagesDifficult Intubation and Anesthetic Management in An Adult Patient With Undiagnosed Congenital Tracheal Stenosis: A Case ReportBianca CaterinalisendraPas encore d'évaluation
- Ultrasonography in Trauma: A Nation-Wide Cross-Sectional InvestigationDocument6 pagesUltrasonography in Trauma: A Nation-Wide Cross-Sectional InvestigationEdison HernandezPas encore d'évaluation
- Estudo 20 AnosDocument7 pagesEstudo 20 AnosLeonardo NóbregaPas encore d'évaluation
- JNS Role of Electrophysiology in Guiding Near Total Resection For Preservation of Facial Nerve Function in The Surgical Treatment of Large Vestibular SchwannomasDocument8 pagesJNS Role of Electrophysiology in Guiding Near Total Resection For Preservation of Facial Nerve Function in The Surgical Treatment of Large Vestibular SchwannomasAlejandro CheritPas encore d'évaluation
- 12th WINFOCUS World Congress On Ultrasound in Emergency and Critical CareDocument17 pages12th WINFOCUS World Congress On Ultrasound in Emergency and Critical CareVictor Euclides Briones MoralesPas encore d'évaluation
- Transient Gerstmann-SyndromeDocument3 pagesTransient Gerstmann-Syndromemuhammad fahrizaPas encore d'évaluation
- Oral Surgery Oral Medicine Oral PathologyDocument5 pagesOral Surgery Oral Medicine Oral PathologyDaniel ColesnicPas encore d'évaluation
- Medi 96 E8514Document4 pagesMedi 96 E8514Syd BarretPas encore d'évaluation
- Alterações Da Mobilidade Laríngea e Sintomas Após Cirurgia de Tireoide Acompanhamento de 6 Meses PDFDocument8 pagesAlterações Da Mobilidade Laríngea e Sintomas Após Cirurgia de Tireoide Acompanhamento de 6 Meses PDFGiovanna MartinsPas encore d'évaluation
- Dr. Zidan ProofDocument11 pagesDr. Zidan ProofDrMohmd ZidaanPas encore d'évaluation
- Lary 23467Document8 pagesLary 23467Dwi juliana DewiPas encore d'évaluation
- Evaluation of Prognostic Factors and Middle Ear RiskDocument5 pagesEvaluation of Prognostic Factors and Middle Ear RiskKye Hoon ParkPas encore d'évaluation
- A Preliminary Study of Computer Assisted EvaluatioDocument7 pagesA Preliminary Study of Computer Assisted Evaluatioabdullah al MamunPas encore d'évaluation
- Superiority of Continuous Over Intermittent Intraoperative Nerve Monitoring in Preventing Vocal Cord PalsyDocument9 pagesSuperiority of Continuous Over Intermittent Intraoperative Nerve Monitoring in Preventing Vocal Cord PalsyazharbattooPas encore d'évaluation
- Proceedings of The 2014 Spring Meeting of The Society of British 2014Document40 pagesProceedings of The 2014 Spring Meeting of The Society of British 2014rabiatul adawiyahPas encore d'évaluation
- Wa0011Document4 pagesWa0011PatrickNicholsPas encore d'évaluation
- Recent Key PublicationsDocument3 pagesRecent Key PublicationserdPas encore d'évaluation
- 29th International Symposium On Intensive Care and Emergency MedicineDocument209 pages29th International Symposium On Intensive Care and Emergency MedicineYOGIPas encore d'évaluation
- Diaphragmatic Laceration After Penetrating TraumaDocument5 pagesDiaphragmatic Laceration After Penetrating TraumajampogaottPas encore d'évaluation
- Daño Al RecurrenteDocument5 pagesDaño Al RecurrenteDaniel SuárezPas encore d'évaluation
- Puccinelli 2019Document8 pagesPuccinelli 2019RathavishwarajPas encore d'évaluation
- 2008 Chest - The Blue ProtocolDocument9 pages2008 Chest - The Blue Protocoleduardo0% (1)
- Role of Swallowing Function of Tracheotomised Patients in Major Head and Neck Cancer SurgeryDocument3 pagesRole of Swallowing Function of Tracheotomised Patients in Major Head and Neck Cancer SurgeryAnonymous xvlg4m5xLXPas encore d'évaluation
- Vocal Cord Paralysis and Its Etiologies A Prospective StudyDocument4 pagesVocal Cord Paralysis and Its Etiologies A Prospective StudySheilla KhonadaPas encore d'évaluation
- Journal of Otolaryngology and Rhinology Jor 2 016Document5 pagesJournal of Otolaryngology and Rhinology Jor 2 016naveed gulPas encore d'évaluation
- A Comparative Study of Microscopic and Endoscopic Type I TympanoplastyDocument4 pagesA Comparative Study of Microscopic and Endoscopic Type I TympanoplastyPutraPas encore d'évaluation
- Hannan 1999Document8 pagesHannan 1999Rafael SchwingelPas encore d'évaluation
- Dmso TinnitusDocument7 pagesDmso TinnitusJoão FrancoPas encore d'évaluation
- Diaphragm Ultrasound As A New Method To Predict Extubation Outcome in Mechanically VentilaDocument7 pagesDiaphragm Ultrasound As A New Method To Predict Extubation Outcome in Mechanically VentilaSilvanaPas encore d'évaluation
- Contribution of Intraoperative Electroencephalogram Suppression To Frailty-Associated Postoperative Delirium: Mediation Analysis of A Prospective Surgical CohortDocument9 pagesContribution of Intraoperative Electroencephalogram Suppression To Frailty-Associated Postoperative Delirium: Mediation Analysis of A Prospective Surgical CohortSmith JanePas encore d'évaluation
- Efficacy of Sinusitis UltrasoundDocument7 pagesEfficacy of Sinusitis UltrasoundYazid MultazamPas encore d'évaluation
- Ultrasound in Emergency Medicine: Use of Ocular Ultrasound For The Evaluation of Retinal DetachmentDocument5 pagesUltrasound in Emergency Medicine: Use of Ocular Ultrasound For The Evaluation of Retinal DetachmentZarella Ramírez BorreroPas encore d'évaluation
- AngiofibromaDocument7 pagesAngiofibromaPandu DiputraPas encore d'évaluation
- Factors Of: Myringoplasty in Children: Predictive OutcomeDocument5 pagesFactors Of: Myringoplasty in Children: Predictive OutcomeAcoet MiezarPas encore d'évaluation
- Percutaneous Corticosteroid Injection For Vocal Fold Polyp: Yen-Bin Hsu, MD Ming-Chin Lan, MD Shyue-Yih Chang, MDDocument5 pagesPercutaneous Corticosteroid Injection For Vocal Fold Polyp: Yen-Bin Hsu, MD Ming-Chin Lan, MD Shyue-Yih Chang, MDFebi HaryadiPas encore d'évaluation
- Iatrogenia, Del Nervio TrigeminoDocument5 pagesIatrogenia, Del Nervio TrigeminoSpaceWord 369Pas encore d'évaluation
- Round and Oval Window Reinforcement For The Treatment of HyperacusisDocument5 pagesRound and Oval Window Reinforcement For The Treatment of HyperacusistonzmanojPas encore d'évaluation
- Surgical Treatment of Vestibular Schwannoma - Review of 420 CasesDocument11 pagesSurgical Treatment of Vestibular Schwannoma - Review of 420 CasesSa'Deu FondjoPas encore d'évaluation
- Trans Perineal Vs EndoanalDocument4 pagesTrans Perineal Vs Endoanalaziz fahrudinPas encore d'évaluation
- Juvenile Nasopharyngeal Angiofibroma - A Hospital-Based Retrospective StudyDocument3 pagesJuvenile Nasopharyngeal Angiofibroma - A Hospital-Based Retrospective StudyGiiszs AlvarezPas encore d'évaluation
- Pvul Terapia Voz Ingles PDFDocument6 pagesPvul Terapia Voz Ingles PDFGeral HernandezPas encore d'évaluation
- Congenital Middle Ear Anomalies: Anatomical and Functional Results of SurgeryDocument6 pagesCongenital Middle Ear Anomalies: Anatomical and Functional Results of SurgeryVali MocanuPas encore d'évaluation
- Articulo - Intubación en Inestabilidad de ColumnaDocument12 pagesArticulo - Intubación en Inestabilidad de ColumnaNFSOTPas encore d'évaluation
- Bjorl: Surgical Treatment of Severe Laryngomalacia: A Retrospective Study of 11 CasesDocument5 pagesBjorl: Surgical Treatment of Severe Laryngomalacia: A Retrospective Study of 11 CasesPutri HakimPas encore d'évaluation
- Comparing Erector Spinae Plane Block With Serratus Anterio - 2020 - British JourDocument9 pagesComparing Erector Spinae Plane Block With Serratus Anterio - 2020 - British JourtasyadelizaPas encore d'évaluation
- Goh 2019Document8 pagesGoh 2019Karol Y. Wilson LondoñoPas encore d'évaluation
- A Twin-Center Study of Nasal Tip Numbness Following Septorhinoplasty or RhinoplastyDocument4 pagesA Twin-Center Study of Nasal Tip Numbness Following Septorhinoplasty or RhinoplastySinan Kadir AltunalPas encore d'évaluation
- CWU and CWDDocument4 pagesCWU and CWDJanfeb DuasatuPas encore d'évaluation
- Tracheostomy in The Intensive Care Unit A University Hospital in A Developing Country StudyDocument5 pagesTracheostomy in The Intensive Care Unit A University Hospital in A Developing Country StudycendyjulianaPas encore d'évaluation
- Seguridad Del PacienteDocument14 pagesSeguridad Del PacienteTamara PricilaPas encore d'évaluation
- Estenosis Sub 5Document7 pagesEstenosis Sub 5Nicolás HenaoPas encore d'évaluation
- L3 Award Introduction To Business Strategy and PlanningDocument18 pagesL3 Award Introduction To Business Strategy and PlanningPrabjot SehmiPas encore d'évaluation
- Margo Lick 2018Document6 pagesMargo Lick 2018Prabjot SehmiPas encore d'évaluation
- Original Contributions: Joa O Gonc Alves Filho, MD, and Luiz Paulo Kowalski, MD, PHDDocument6 pagesOriginal Contributions: Joa O Gonc Alves Filho, MD, and Luiz Paulo Kowalski, MD, PHDPrabjot SehmiPas encore d'évaluation
- The Epidemiology of Non-Alcoholic Fatty Liver Disease: Stefano BellentaniDocument4 pagesThe Epidemiology of Non-Alcoholic Fatty Liver Disease: Stefano BellentaniPrabjot SehmiPas encore d'évaluation
- Lecture 1 Wc25th Sept PT 1 CH 14 Base SlidesDocument16 pagesLecture 1 Wc25th Sept PT 1 CH 14 Base SlidesPrabjot SehmiPas encore d'évaluation
- NMS Physiology PDFDocument502 pagesNMS Physiology PDFPrabjot SehmiPas encore d'évaluation
- Textbook of Physiology, 3E (Chandramouli) (2010) (PDF) (UnitedVRG)Document436 pagesTextbook of Physiology, 3E (Chandramouli) (2010) (PDF) (UnitedVRG)Prabjot Sehmi67% (3)
- Acid Base PhysiologyDocument1 pageAcid Base PhysiologyPrabjot SehmiPas encore d'évaluation
- SUBASHINIDocument3 pagesSUBASHINIKB_mitPas encore d'évaluation
- A Discussion On Suture and LigatureDocument9 pagesA Discussion On Suture and LigatureKiran saiPas encore d'évaluation
- 49CDocument154 pages49Crudolfpetersson100% (2)
- Operation TheatreDocument22 pagesOperation TheatreAbirami100% (1)
- Lasik Eye Surgery Research PaperDocument7 pagesLasik Eye Surgery Research Paperwkzcoprhf100% (1)
- Mireille Varmuza Nursing ResumeDocument3 pagesMireille Varmuza Nursing Resumeapi-417947949Pas encore d'évaluation
- Synopsis DR ABCDocument8 pagesSynopsis DR ABCFiaz medicoPas encore d'évaluation
- Health Care Delivery SystemDocument21 pagesHealth Care Delivery SystemAyeza DuaPas encore d'évaluation
- UntitledDocument7 pagesUntitledmandla simelanePas encore d'évaluation
- Internet Case For Supplement 7Document3 pagesInternet Case For Supplement 7johnmia20Pas encore d'évaluation
- (GNUR 301) (Peri-Operative Nursing) : Lecturers: DR GLADYS DZANSI Gdzansi@ug - Edu.gh David Tenkorang-TwumDocument58 pages(GNUR 301) (Peri-Operative Nursing) : Lecturers: DR GLADYS DZANSI Gdzansi@ug - Edu.gh David Tenkorang-TwumNana Yaa PomaahPas encore d'évaluation
- Chapter 11 GastrointestinalDocument9 pagesChapter 11 GastrointestinalChyPas encore d'évaluation
- Batu Ren, Batu Ureter Dan Onko NewDocument29 pagesBatu Ren, Batu Ureter Dan Onko Newilham masdarPas encore d'évaluation
- Pre Anesthesia Assessment and PreparationDocument8 pagesPre Anesthesia Assessment and PreparationNoviantiPas encore d'évaluation
- Congenital Laryngomalacia: Symptom Duration and Need For Surgical InterventionDocument5 pagesCongenital Laryngomalacia: Symptom Duration and Need For Surgical InterventionNadia CeciliaPas encore d'évaluation
- Isjna Vol 17 2 Summer 2018Document72 pagesIsjna Vol 17 2 Summer 2018Nissa KurniaPas encore d'évaluation
- Anesthesia For Bariatric SurgeryDocument47 pagesAnesthesia For Bariatric Surgerydkhiloi100% (1)
- Kotak Group Accident Protect Policy WordingDocument12 pagesKotak Group Accident Protect Policy WordingVideshi BabuPas encore d'évaluation
- Narrative For Omar Durrani, MD Case NumberDocument5 pagesNarrative For Omar Durrani, MD Case NumberACDCPas encore d'évaluation
- Transversus Abdominis Plane Block For Laparoscopic SurgeryDocument2 pagesTransversus Abdominis Plane Block For Laparoscopic SurgeryFitri Kasmita SariPas encore d'évaluation
- NPT 0009 18 Website Announcement Final Awardation v3Document142 pagesNPT 0009 18 Website Announcement Final Awardation v3mohamed boufasPas encore d'évaluation
- BurnDocument30 pagesBurnMamata BeheraPas encore d'évaluation
- Pain Audit ToolsDocument10 pagesPain Audit ToolsIrmela CoricPas encore d'évaluation
- 20.pedagogy On PiezosurgeryDocument10 pages20.pedagogy On PiezosurgeryVishali RayapudiPas encore d'évaluation
- Hari Waktu Acara Narasumber Fasilitator/ Pengawas Pusat Senin, 26 April 2021Document2 pagesHari Waktu Acara Narasumber Fasilitator/ Pengawas Pusat Senin, 26 April 2021Larvahmir SpDVPas encore d'évaluation
- Disposable and Reusable Cannulas: CatalogDocument48 pagesDisposable and Reusable Cannulas: CatalogAdonias de OliveiraPas encore d'évaluation
- CPG Recommendations For Patient Safety and Minimal Monitoring Standards During Anaesthesia and Recovery PDFDocument21 pagesCPG Recommendations For Patient Safety and Minimal Monitoring Standards During Anaesthesia and Recovery PDFDzarrinPas encore d'évaluation
- 1 Introduction To CPT 2021 ModifierDocument7 pages1 Introduction To CPT 2021 ModifierChester FernandezPas encore d'évaluation
- Curriculum Vitae: Name Date of Birth Nationality GMC NumberDocument13 pagesCurriculum Vitae: Name Date of Birth Nationality GMC NumberRazor GGPas encore d'évaluation
- Daftar Harga Indosopha 2012 Bp. Edward Roy Palangkaraya PDFDocument5 pagesDaftar Harga Indosopha 2012 Bp. Edward Roy Palangkaraya PDFBoyke WinterbergPas encore d'évaluation