Académique Documents
Professionnel Documents
Culture Documents
Ijcem 0037903
Transféré par
riyanDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Ijcem 0037903
Transféré par
riyanDroits d'auteur :
Formats disponibles
Int J Clin Exp Med 2017;10(1):1325-1329
www.ijcem.com /ISSN:1940-5901/IJCEM0037903
Original Article
Correlation of retinopathy with serum levels of growth
hormones and insulin-like growth factor-1 in
patients with diabetic retinopathy
Jie Zhang1, Li Zhang2, Li Quan3, Wenxue Qi3, Yujie Jiang3, Sheng Jiang3
1
Department of Endocrinology, People’s Hospital of Xinjiang Uygur Autonomous Region, Urumqi 830000, Xinjiang,
China; 2Department of Ophthalmology, Armed Police Hospital of Xinjiang, Urumqi 830000, Xinjiang, China;
3
Department of Endocrinology, First Affiliated Hospital of Xinjiang Medical University, Urumqi 830000, Xinjiang,
China
Received August 14, 2016; Accepted October 19, 2016; Epub January 15, 2017; Published January 30, 2017
Abstract: Objective: This study aims to retrospectively analyze the correlation between levels of serum growth hor-
mones and insulin-like growth factor-1 (IGF-1) and severity of retinopathy in type 2 diabetes patients reaching the
goal of blood glucose control. Method: A retrospective analysis was adopted for 112 type 2 diabetes patients reach-
ing the goal of blood glucose control in the past 3 years. All patients received fundus fluorescein angiography, based
on which the patients were divided into normal fundus group, non-proliferative diabetic retinopathy (DR) group
and proliferative DR group. The three groups were compared with regard to the levels of serum growth hormones
and IGF-1. Their correlation with severity of DR was assessed using multivariate unconditional logistic regression.
Result: In the proliferative DR group, the levels of low density lipoprotein cholesterol (LDL-C), urine micro albumin
(UmALB), serum growth hormones and IGF-1 were all significantly higher than those of the normal group and the
non-proliferative DR group (P<0.05); however, no significant difference was found between the non-proliferative DR
group and the normal group (P>0.05). The C-peptide (C-P) level in the proliferative DR group was markedly lower
than that of the other two groups (P<0.05); but no significant difference was found between the non-proliferative
DR group and the normal group (P>0.05). As indicated by correlation analysis, course of disease, UmALB, IGF-1
and fasting C-P levels were correlated to the severity of DR. Conclusion: The common factors of DR are course of
diabetes, systolic pressure, LDL-C, fasting C-R risk and UmALB. In addition to these, higher levels of serum growth
hormones and IGF-1 may also contribute to DR, which is speculated to be one mechanism for the progression of
DR in type 2 diabetes.
Keywords: Diabetic retinopathy, serum growth hormones, insulin-like growth factor-1
Introduction and IGF-1 for type 2 diabetes (T2DM) patients
combined with different severity of DR, so as to
Diabetic retinopathy (DR) is a common type of identify other potential risk factors of DR.
microvascular complication in diabetes and
also among the main causes of blindness. The Materials and methods
risk factors believed to be associated with DR
include course of diabetes, glycated hemoglo- Subjects
bin (HhA1c), blood pressure, low density lipo-
protein cholesterol (LDL-C), urine micro albu- From January 2012 to June 2015, 128 T2DM
min (UmALB), and possibly vascular endot- patients treated at our hospital with complete
helial growth factors (VEGF) [1]. However, they data were included. The diagnosis was based
cannot explain every aspect of pathogenesis on 1999 WHO criteria [3]. The patients included
of DR. According to the latest report, growth 78 males and 50 females with an average age
hormones (GH) and insulin-like growth factor-1 of 57.4 ± 11.2 years and course of 12.7 ± 3.2
(IGF-1) may be also involved [2]. The present years. The inclusion criteria were as follows:
study assessed the correlation between GH Confirmed T2DM and having received treat-
Analysis of diabetic retinopathy
_
Table 1. Comparison of clinical characteristics among three groups of patients ( x ± s)
Case Course of Waist
Group Age (years) BMI (Kg/M2) SBP (mmHg) DBP (mmHg)
(n) disease (years) circumference (cm)
PDR group 23 56.9 ± 10.42 13.45 ± 4.22 91.54 ± 4.94 23.89 ± 3.86 129.69 ± 13.87 85.55 ± 8.94
NPDR group 31 57.42 ± 9.24 11.63 ± 5.38* 90.15 ± 6.86 24.15 ± 5.14 125.65 ± 10.34 83.83 ± 7.82
N group 74 56.9 ± 13.55 10.81 ± 6.95* 93.25 ± 8.26 24.83 ± 4.82 127.43 ± 9.32 84.51 ± 8.43
F value - 0.168 11.671 0.285 0.310 0.547 0.675
P value - 0.506 0.004 0.753 0.734 0.073 0.531
*Compared with the PDR group, the difference was statistically significant (P<0.05).
ment at department of endocrinology of ter- using multivariate unconditional logistic regres-
tiary hospitals with regular follow-up. The treat- sion, and P<0.05 was considered significant
ment protocol conformed to China Guideline difference.
for Type 2 Diabetes (2013) [4]; Receiving detec-
tion of HbA1c 1 levels in the past 3 years for at Results
least once a year and the result being below
7.5%; without contraindications for fundus fluo- According to the result of fundus fluorescein
rescein angiography. Exclusion criteria: grade 2 angiography, 128 T2DM patients were divided
hypertension or above; abnormalities of the into 3 groups. PDR group had 23 cases (16 ma-
pituitary gland and thyroid; liver diseases or les and 7 females). NPDR group had 31 cases
aminotransferase levels two times higher than (19 males and 12 females). Normal group (N
the normal levels; abnormalities of major org- group) had 74 cases (43 males and 31 fem-
ans, including heart, lung, kidney and brain, ales). Of all baseline indicators, the three
had been treated with drugs that may affect groups only differed significantly in the course
GH; average number of hypoglycemia onset of disease (P<0.05) (Table 1).
more than once weekly. All cases signed the
informed consent. Blood marker tests of 3 groups indicated that
C-P and 2hC-P levels of PDR group were signifi-
Method cantly lower than those of NPDR and N groups
(P<0.05); however, NPDR group and N group
All cases received fundus fluorescein angiogra- were not significantly different (P>0.05). The
phy. Diagnosis of proliferative DR (PDR) or non- levels of LDL-C, UA, GH and IGF-1 were consid-
proliferative DR (NPDR) was made according erably higher in PDR group than in NPDR and
to China Guideline for Type 2 Diabetes (2013). N group (P<0.05). But no significant differe-
Baseline indicators were measured for all pati- nce was found between NPDR and N groups
ents: height, weight, waist circumference (WC), (P>0.05) (Table 2).
body mass index (BMI), systolic blood pressure
(SBP), diastolic blood pressure (DBP), fasting Logistic regression
plasma glucose (FPG), C-peptide (C-P), plasma
glucose 2 h (2hPG) and C-P (2hC-P) after 100 g Taking DR as dependent variable and age,
steamed bun diet, LDL-C, triglyceride (TG), high course of disease, WC, BMI, LDL-C, HDL-C, TG,
density lipoprotein cholesterol (HDL-C), total TC, C-P, 2hC-P, UA, GH and IGF-1 as indepen-
cholesterol (TC), urine albumin (UA), GH and dent variables, multivariate logistic regression
IGF-1. All indicators were measured at the analysis was performed. The result showed
Center for Clinical Laboratory of our hospital. that as far as the 128 T2DM patients were
concerned, course of DM, UA, IGF-1 and fasting
Statistical process C-P correlated independently to DR (P<0.05)
(Table 3).
Statistical analysis was conducted using SPSS
18.0 software. Measurements were expressed Discussion
as x ± s and the difference of the three groups
was compared by analysis of variance. t-test DR is a microvascular complication highly spe-
was used for comparing the means of the two cific to DM. In developing countries, DR is the
groups. Risk factors of DR were identified by leading cause of blindness in adults, affecting
1326 Int J Clin Exp Med 2017;10(1):1325-1329
Analysis of diabetic retinopathy
_
Table 2. Comparison of blood markers among three groups of patients ( x ± s)
FPG LDL-C HDL-C PPG
Group GH (ng/ml) IGF-1 (ng/ml) C-P (ng/ml) PC-P (ng/ml) TG (mmol/L) TC (mmol/L) UA (mg/L)
(mmol/L) (mmol/L) (mmol/L) (mmol/L)
PDR group 2.61 ± 1.32 158.5 ± 41.42 0.68 ± 0.41 1.43 ± 0.91 7.38 ± 1.54 4.85 ± 1.13 4.15 ± 1.79 5.16 ± 1.31 1.06 ± 0.39 262 ± 49.61 10.14 ± 2.45
NPDR group 1.83 ± 1.14* 132. ± 33.81* 0.93 ± 0.56* 2.66 ± 1.04* 7.85 ± 2.63 3.0 ± 1.10* 3.95 ± 1.31 5.01 ± 1.22 1.11 ± 0.65 221 ± 37.91* 9.96 ± 3.78
N group 1.75 ± 1.06* 129. ± 38.25* 0.99 ± 0.47* 3.11 ± 1.12* 6.93 ± 1.22 3.1 ± 1.24* 3.77 ± 1.21 4.91 ± 0.92 1.13 ± 0.82 218 ± 29.53* 9.63 ± 4.48
F value 12.822 32.762 5.068 6.048 2.206 12.823 0.445 2.207 0.056 12.820 0.057
P value 0.002 0.013 0.014 0.005 0.063 0.008 0.643 0.065 0.946 0.012 0.944
*Compared with the PDR group, the difference was statistically significant (P<0.05).
1327 Int J Clin Exp Med 2017;10(1):1325-1329
Analysis of diabetic retinopathy
Table 3. Logistic regression analysis of DR-related factors usually accompanied by increased
Wald X
2 plasma protein levels, with red blood
Variable β value P value OR value (95% CI) cell and platelet aggregation and thic-
value
Course of DM 0.483 12.181 0.001 1.811 (1.270-2.632) kened basement membrane of capil-
IGF-1 0.229 7.843 0.033 1.211 (1.121-1.380) laries. As a result, capillary leakage
UA 1.420 7.037 0.008 4.137 (1.455-11.211) increases, and retinal ischemia, mic-
roaneurysm and angiogenesis take
C-P 0.186 6.577 0.044 1.049 (1.012-1.098)
place. In the present study, DM pati-
ents reaching the goal of blood glu-
2-5% of total population. DR is seen in about cose control still had obviously higher serum
20-40% of T2DM patients, with 8% of them GH levels when combined with PDR, as com-
suffering from severe vision loss. By severity, pared with NPDR group and N group. However,
DR is classified into 6 grades consisting of the difference between NPDR group and N
NPDR and PDR [5]. The pathogenesis of DR group was insignificant. From this it can be
is very complex and the contributing factors inferred that GH plays a role in PDR, as is also
of DR include pericyte loss, endothelial cell indicated by many other researches [9]. GH lev-
proliferation, basement membrane thickening, els showed a significantly positive correlation
lumen stenosis and occlusion, retinal ische- to the severity of DR, but whether GH levels
mia and hypoxia, angiogenesis and traction and severity of DR are causally related or not
retinal detachment. Each of the above proc- is unknown. We failed to prove that GH was a
esses involves assorted array of cytokines. risk factor of DR.
Some researchers believe that activation of
VEGF, angiopoietins and specific receptors as IGF-1 originates in the liver. GH acts through
well as GH and IGF-1 play a role in DR [6]. IGF-1 and regulates IGF-1, and the latter is used
as an indicator of GH levels. As to the correla-
Under normal conditions, high blood glucose tion between DM and IGF-1, many opposing
can inhibit the secretion of GH. But for DM opinions have appeared. Studies based on
patients, persistent high blood glucose leads to larger populations seem to indicate that with
an increase of serum GH, which further aggra- the factors of HbAlc, age and course of disease
vates insulin resistance and glucose metabo- controlled, IGF-1 does not significantly corre-
lism disorder. Changes of GH levels may con-
late to the occurrence and progression of DR
tribute to the occurrence of microvascular
in either teenage or adult DM patients [10]. In
lesions. It has been demonstrated by clinical
other studies, serum levels of IGF-1 increase as
trials that GH levels in DR patients are obvi-
DR deteriorates, which agrees with our result.
ously higher than those in diabetic patients
Many scholars hold that IGF-1 levels and sev-
without DR. PDR can be prevented or delayed
erity of DR positively correlate to the course of
by resection of the anterior lobe of pituitary
DM and persistent high blood glucose leads
gland [7]. In diabetic dwarf with GH deficiency,
microvascular lesions may be absent. Merime to an increase of IGF-1 levels. This becomes
(1973) studied a population of pituitary dwarf- more conspicuous with prolonged course of
ism (caused by GH deficiency) combined with disease. According to Chante-lau et al. [11],
reduced glucose tolerance. As compared with proper blood glucose control does not always
DM patients (increased blood glucose and lead to the delay of DR and the opposite may
GH) of the same age, the incidence of DR was occur, especially for simple DR. Before deterio-
0% vs. 40%, indicating close connection bet- ration of DR, the serum level of IGF-1 in these
ween DR and GH. Higher GH levels will aggra- DM patients increased by over 100%. Thus it
vate glucose metabolism disorder, enhancing was concluded that the deterioration of sim-
the activity of glucosidase and galactosidase ple DR correlated to reduced retinal tolerance
and thus promoting the synthesis of glycopro- to IGF-1. So IGF-1 is presumed to be one cause
teins. With more glycoproteins deposited to the of PDR. As found by our study, IGF-1 levels in
basement membranes of capillaries, diabetic PDR group were much higher than those in
microvascular lesions may be induced. This NPDR group and N group and IGF-1 levels cor-
constitutes one major pathogenesis of DR [8]. related to DR, which coincides with the findings
Moreover, changes of GH and insulin levels are of foreign literature.
1328 Int J Clin Exp Med 2017;10(1):1325-1329
Analysis of diabetic retinopathy
Though the pathogenesis of DR is still unclear, [4] Chinese Medical Association Diabetes Branch.
several risk factors have been reported, includ- Chinese type 2 diabetes prevention guide
ing course of DM, systolic pressure, blood glu- (2013 Edition). Chinese Journal of Diabetes
cose control status and urine albumin. These Mellitus 2014; 88: 26-89.
[5] Long QY and Yu LH. Risk factors associated
factors are already attended to in clinics [12].
with diabetic retinopathy progression in pa-
According to our result, DM patients combined
tients with type 2 diabetes. Chinese Journal of
with PDR still had higher GH and IGF-1 levels Prevention and Control of Chronic Diseases
in spite of good blood glucose control status. 2014; 22: 411-413.
IGF-1 is a risk factor of DR. For these patients, [6] Muir KW, Grubber J, Mruthyunjaya P, McCant F
inhibiting IGF-1 may be one pathway for pre- and Bosworth HB. Progression of diabetic reti-
venting and treating DR. nopathy in the hypertension intervention nurse
telemedicine study. JAMA Ophthalmol 2013;
Acknowledgements 131: 957-958.
[7] Du YJ, Zhao ZY, Li XJ and Ma LX. Diabetic reti-
This work was supported by the Natural fund nopathy and serum growth hormone (analysis
project in Xinjiang (Name of the fund: The study of 31 cases). Chinese Journal of Gerontology
about Xinjiang uygur people’s osteocalcin level 1992; 12: 218-220.
difference and its relationship with insulin resi- [8] Ringholm L, Vestgaard M, Laugesen CS, Juul A,
stance. No. 2013ZRZD05) and the fund proj- Damm P and Mathiesen ER. Pregnancy-in-
duced increase in circulating IGF-I is associat-
ect of Hospital to Xinjiang Uygur Autonomous
ed with progression of diabetic retinopathy in
Region, NO. 20140102.
women with type 1 diabetes. Growth Horm IGF
Res 2011; 21: 25-30.
Disclosure of conflict of interest
[9] Bonfig W, Molz K, Woelfle J, Hofer SE, Hauffa
BP, Schoenau E, Golembowski S, Wudy SA and
None. Holl RW. Metabolic Safety of Growth Hormone
in Type 1 Diabetes and Idiopathic Growth Hor-
Address correspondence to: Sheng Jiang, Depart-
mone Deficiency. J Pediatr 2013; 163: 1095-
ment of Endocrinology, First Affiliated Hospital of 1098.e4.
Xinjiang Medical University, No.134 Liyushan South [10] Gokulakrishnan K, Velmurugan K, Ganesan S
Road, Urumqi 830000, Xinjiang, China. Tel: +86- and Mohan V. Circulating levels of insulin-like
18999936571; Fax: +86-18999936571; E-mail: growth factor binding protein-1 in relation to
jsheng_a@163.com insulin resistance, type 2 diabetes mellitus,and
metabolic syndrome (Chennai Urban Rural Epi-
References demiology Study 118). Metabolism 2012; 61:
43-46.
[1] Das A, Stroud S, Mehta A and Rangasamy S. [11] Chantelau E. Evidence that upregulation of se-
New treatments for diabetic retinopathy. Dia- rum IGF-I concentra-tion can trigger accelera-
betes Obes Metab 2015; 17: 219-230 tion of diabetic retinopathy. Br J Ophthalmol
[2] Wu YK, Zhang LM, Ge WL and Yang JK. The re- 1998; 82: 725-730.
lationship between growth hormone and insu- [12] Yang Y, Tian M and Lv HB. Recent advances in
lin like growth factor I and diabetic retinopathy. treatment of diabetic retinopathy. Recent Ad-
Zhong Hua Yan Di Bing Za Zhi 2000; 16: 30- vances in Ophthalmology 2015; 35: 497-500.
33.
[3] Alberti KG and Zimmet PZ. Definition, diagno-
sis and classification of diabetes mellitus and
its complications. Part 1: diagnosis and classi-
fication of diabetes mellitus provisional report
of a WHO consultation. Diabet Med 1998; 15:
539-553.
1329 Int J Clin Exp Med 2017;10(1):1325-1329
Vous aimerez peut-être aussi
- Complementary and Alternative Medical Lab Testing Part 8: UrologyD'EverandComplementary and Alternative Medical Lab Testing Part 8: UrologyÉvaluation : 3 sur 5 étoiles3/5 (1)
- JDR2019 7825804Document9 pagesJDR2019 7825804Anonymous Xc7NwZzoPas encore d'évaluation
- Nihms 82233Document10 pagesNihms 82233LeonardoPas encore d'évaluation
- Abstracts: Nephrology Dialysis TransplantationDocument1 pageAbstracts: Nephrology Dialysis TransplantationrezkyfikriPas encore d'évaluation
- Mertoglu and Gunay 2017Document5 pagesMertoglu and Gunay 2017Via MeysaPas encore d'évaluation
- The Relationship Between Hba1C and Lipid Profile in Type 2 Diabetic Saudi PatientsDocument6 pagesThe Relationship Between Hba1C and Lipid Profile in Type 2 Diabetic Saudi PatientsnaxxxPas encore d'évaluation
- Effect of Variability of Hemoglobin Value On Type and Severity of Diabetic Retinopathy in Adult Type II Diabetes Mellitus PatientsDocument11 pagesEffect of Variability of Hemoglobin Value On Type and Severity of Diabetic Retinopathy in Adult Type II Diabetes Mellitus PatientsInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- Can Non-Alcoholic Fatty Liver Disease (NAFLD) As A Marker For Microalbuminuria in Prediabetes Group?Document4 pagesCan Non-Alcoholic Fatty Liver Disease (NAFLD) As A Marker For Microalbuminuria in Prediabetes Group?BinaNuraeniPas encore d'évaluation
- Serial Measurement of Lipid Profile in Patients With Acute Myocardial InfarctionDocument4 pagesSerial Measurement of Lipid Profile in Patients With Acute Myocardial InfarctionMJSPPas encore d'évaluation
- Assessment of Prevalence and Associated Risk Factors of NAFLD in Indian Diabetes Patients 03jan2020 Final PDFDocument27 pagesAssessment of Prevalence and Associated Risk Factors of NAFLD in Indian Diabetes Patients 03jan2020 Final PDFrasika bhatPas encore d'évaluation
- Original Article Evaluation of Dyslipidaemia in Type 2 Diabetes Mellitus PatientsDocument6 pagesOriginal Article Evaluation of Dyslipidaemia in Type 2 Diabetes Mellitus PatientsEnvhy AmaliaPas encore d'évaluation
- Case Based Discussion: Department of Internal Medicine Sultan Agung Islamic UniversityDocument177 pagesCase Based Discussion: Department of Internal Medicine Sultan Agung Islamic UniversityRobby GumawanPas encore d'évaluation
- Fendo 13 885516Document7 pagesFendo 13 885516adri20121989Pas encore d'évaluation
- Markers in Various Clinical Stages of Type 2 Diabetic Nephropathy" Merupakan Hasil SebuahDocument6 pagesMarkers in Various Clinical Stages of Type 2 Diabetic Nephropathy" Merupakan Hasil Sebuahkwon hyukPas encore d'évaluation
- Comparison of Inflammatory Markers in HTNDocument6 pagesComparison of Inflammatory Markers in HTNDan JohnstonPas encore d'évaluation
- 2016 Article 69Document10 pages2016 Article 69Rhowy Al-mu'izzahPas encore d'évaluation
- Glycemic Index, Glycemic Load, and Blood Pressure: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsDocument15 pagesGlycemic Index, Glycemic Load, and Blood Pressure: A Systematic Review and Meta-Analysis of Randomized Controlled TrialsLisiane PerinPas encore d'évaluation
- Assessment of Creactive Protein Lpid Profile and Body Mass Index in Type2 Diabetes Mellitus in Sudanese PatientsDocument9 pagesAssessment of Creactive Protein Lpid Profile and Body Mass Index in Type2 Diabetes Mellitus in Sudanese PatientsMotasem Sirag Mohmmed othmanPas encore d'évaluation
- PDML Article1Document4 pagesPDML Article1kingdeyPas encore d'évaluation
- Labmed31 0383Document4 pagesLabmed31 0383ushakPas encore d'évaluation
- 7 FFCDocument8 pages7 FFCHow to youPas encore d'évaluation
- Association of Diabetic Retinopathy in Type II Diabetes Mellitus With Hba1c Levels: A StudyDocument6 pagesAssociation of Diabetic Retinopathy in Type II Diabetes Mellitus With Hba1c Levels: A StudyYoga TDPas encore d'évaluation
- Sindrom NefrotikDocument7 pagesSindrom NefrotikDania SaraswatiPas encore d'évaluation
- Diabetes Care Glucosa Promedio EstimadaDocument6 pagesDiabetes Care Glucosa Promedio EstimadaGemeneza GonzalesPas encore d'évaluation
- Jurnal TerbaruDocument5 pagesJurnal TerbaruSuci Ramadhani PutriPas encore d'évaluation
- Research Journal of Pharmaceutical, Biological and Chemical SciencesDocument9 pagesResearch Journal of Pharmaceutical, Biological and Chemical SciencesMuhammad ZubaidiPas encore d'évaluation
- 12.glycemia Reduction in Type 2 DiabetesDocument14 pages12.glycemia Reduction in Type 2 DiabetesEdilberto Pérez ManturanoPas encore d'évaluation
- Reconfirmation of Newly Discovered Risk Factors of Diabetic Peripheral Neuropathy in Patients With Type 2 Diabetes: A Case-Control StudyDocument10 pagesReconfirmation of Newly Discovered Risk Factors of Diabetic Peripheral Neuropathy in Patients With Type 2 Diabetes: A Case-Control Studychrisna dewiPas encore d'évaluation
- Sodium and Potassium Intake in Overweight And.596Document2 pagesSodium and Potassium Intake in Overweight And.596jackie funtanillaPas encore d'évaluation
- Tidak Di Include KanDocument7 pagesTidak Di Include KanKeperawatan LawangPas encore d'évaluation
- Journal of SGPTDocument3 pagesJournal of SGPTEric GibsonPas encore d'évaluation
- Clinical Study: Steroid-Induced Diabetes: Is It Just Unmasking of Type 2 Diabetes?Document6 pagesClinical Study: Steroid-Induced Diabetes: Is It Just Unmasking of Type 2 Diabetes?inaagustinpPas encore d'évaluation
- Reducción de La Glucemia en La Diabetes Tipo 2 Resultados Microvasculares y CardiovascularesDocument14 pagesReducción de La Glucemia en La Diabetes Tipo 2 Resultados Microvasculares y CardiovascularesEdwin Fabian Paz UrbanoPas encore d'évaluation
- Reljanovic Et Al. - 1999 - Treatment of Diabetic Polyneuropathy With The Antioxidant Thioctic Acid (Alpha-Lipoic Acid) A Two Year Multi Center Randomized DoubleDocument9 pagesReljanovic Et Al. - 1999 - Treatment of Diabetic Polyneuropathy With The Antioxidant Thioctic Acid (Alpha-Lipoic Acid) A Two Year Multi Center Randomized DoubleJay LawPas encore d'évaluation
- Is There Any Correlation Between Vitamin D Insufficiency and Diabetic Retinopathy?Document6 pagesIs There Any Correlation Between Vitamin D Insufficiency and Diabetic Retinopathy?MsharaniaPas encore d'évaluation
- Retinal Nerve Fiber Layer and Ganglion Cell Complex Thickness in Patients With Type 2 Diabetes Mellitus Original ArticleDocument2 pagesRetinal Nerve Fiber Layer and Ganglion Cell Complex Thickness in Patients With Type 2 Diabetes Mellitus Original ArticledrblurryfacePas encore d'évaluation
- Paper13 PDFDocument6 pagesPaper13 PDFSekar MentariPas encore d'évaluation
- Randomized Placebo-Controlled EPPIC Trials of AST-120 in CKDDocument15 pagesRandomized Placebo-Controlled EPPIC Trials of AST-120 in CKDPROF. ERWIN M. GLOBIO, MSITPas encore d'évaluation
- PIIS1098301518308854Document1 pagePIIS1098301518308854Angga PratamaPas encore d'évaluation
- Cyclophosphamide Versus Mycophenolate Versus Rituximab in Lupus Nephritis Remission InductionDocument8 pagesCyclophosphamide Versus Mycophenolate Versus Rituximab in Lupus Nephritis Remission InductionVh TRPas encore d'évaluation
- E131 FullDocument3 pagesE131 FullRahmanu ReztaputraPas encore d'évaluation
- Intradialytic Parenteral Nutrition Improves Protein and Energy Homeostasis in Chronic Hemodialysis PatientsDocument10 pagesIntradialytic Parenteral Nutrition Improves Protein and Energy Homeostasis in Chronic Hemodialysis PatientsBianca CheungPas encore d'évaluation
- Dialysis Induced Hypoglycemia in Non-Diabetic Chronic Kidney Disease PatientsDocument3 pagesDialysis Induced Hypoglycemia in Non-Diabetic Chronic Kidney Disease Patientsscience worldPas encore d'évaluation
- 313-Article Text-887-1-10-20180209Document7 pages313-Article Text-887-1-10-20180209stoicea catalinPas encore d'évaluation
- Predictors For Diabetic Retinopathy in Normoalbuminuric People With Type 2 Diabetes MellitusDocument6 pagesPredictors For Diabetic Retinopathy in Normoalbuminuric People With Type 2 Diabetes MellitusdrheriPas encore d'évaluation
- DiabetesDocument8 pagesDiabetesDanielValenciaPas encore d'évaluation
- Subclinical Hypothyroidism and Its Associated Complications in Type 2 Diabetes Mellitus PatientsDocument14 pagesSubclinical Hypothyroidism and Its Associated Complications in Type 2 Diabetes Mellitus PatientsIJAR JOURNALPas encore d'évaluation
- SUultima EvidenciaDocument8 pagesSUultima Evidenciasalvado moyanoPas encore d'évaluation
- Cardiovascular Outcomes StudiesDocument5 pagesCardiovascular Outcomes StudiesAnonymous LOeICSOqPas encore d'évaluation
- 2021 Journal of Personalized Medicine. 11 (8) 799Document14 pages2021 Journal of Personalized Medicine. 11 (8) 799Sofa ChaPas encore d'évaluation
- Translating The A1C Assay Into Estimated Average Glucose ValuesDocument6 pagesTranslating The A1C Assay Into Estimated Average Glucose ValuesFaryalBalochPas encore d'évaluation
- Correlation Between Fasting Blood Glucose and Hba1c With Vitamin D in Diabetes MellitusDocument4 pagesCorrelation Between Fasting Blood Glucose and Hba1c With Vitamin D in Diabetes MellitusErizal Dwi HandokoPas encore d'évaluation
- Makale Neo-Adma - Eng V2Document12 pagesMakale Neo-Adma - Eng V2Thomas LeonPas encore d'évaluation
- Austin Journal of Nephrology and HypertensionDocument4 pagesAustin Journal of Nephrology and HypertensionAustin Publishing GroupPas encore d'évaluation
- Dibacakan Oleh:: Achmad Nur Affendick Adriana Wulandari Dionisia I. Madin Ineke Lani Dimara Lis AmitasariDocument39 pagesDibacakan Oleh:: Achmad Nur Affendick Adriana Wulandari Dionisia I. Madin Ineke Lani Dimara Lis AmitasariMc'onethree BrownPas encore d'évaluation
- Cholesterol MS RADocument6 pagesCholesterol MS RATsamara YumnaPas encore d'évaluation
- JR 1-OliviaDocument9 pagesJR 1-OliviaVirginia EchoPas encore d'évaluation
- Jouyandeh - Metabolic Syndrome and Menopause - 2013Document4 pagesJouyandeh - Metabolic Syndrome and Menopause - 2013MIRIAM VIDURRIZAGAPas encore d'évaluation
- JPD Prepress/jpd 1 1 jpd181305/jpd 1 jpd181305Document7 pagesJPD Prepress/jpd 1 1 jpd181305/jpd 1 jpd181305Yan Hein TanawaniPas encore d'évaluation
- Checklist DRPDocument16 pagesChecklist DRPPutri Kusuma WardaniPas encore d'évaluation
- Hba1C Study: 51 Years /femaleDocument4 pagesHba1C Study: 51 Years /femalesangani.gayatriPas encore d'évaluation
- Family Nursing Care PlanDocument1 pageFamily Nursing Care PlanBhaby Che AserdnaPas encore d'évaluation
- Operation Bigay Lunas: Mercury Drug FoundationDocument2 pagesOperation Bigay Lunas: Mercury Drug Foundationulanrain311Pas encore d'évaluation
- DiabetesDocument40 pagesDiabetesA RPas encore d'évaluation
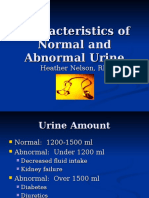
- Characteristics of Normal and Abnormal Urine 869Document12 pagesCharacteristics of Normal and Abnormal Urine 869RakeshSenwaliPas encore d'évaluation
- 1068 5615 2 PBDocument8 pages1068 5615 2 PBVicky AndriPas encore d'évaluation
- Diabetes Educators' Success Stories PDFDocument210 pagesDiabetes Educators' Success Stories PDFRavi V Potluri0% (1)
- Prediabetes Risk Test FinalDocument1 pagePrediabetes Risk Test FinalRafikPas encore d'évaluation
- Canine and Feline Endocrinology and Reproduction PARTE DIABETEDocument44 pagesCanine and Feline Endocrinology and Reproduction PARTE DIABETEmarparolaPas encore d'évaluation
- Diabetic Terhadap Nilai Ankle Brachial Index PadaDocument9 pagesDiabetic Terhadap Nilai Ankle Brachial Index PadaNesi HeryaniPas encore d'évaluation
- GLP 1Document10 pagesGLP 1Dayu GekPas encore d'évaluation
- Checklist Osce Blok 14Document2 pagesChecklist Osce Blok 14Agung Rizka PratamaPas encore d'évaluation
- Diabetic Nephropathy Pathophysiology 2Document38 pagesDiabetic Nephropathy Pathophysiology 2fabian ortizPas encore d'évaluation
- Diabetic EmergenciesDocument65 pagesDiabetic EmergenciesManmeet SPas encore d'évaluation
- Anita's PrescriptionDocument1 pageAnita's Prescriptionnitinvats.visioniasPas encore d'évaluation
- Type I Diabetes Mellitus Management in The Athletic PopulationDocument22 pagesType I Diabetes Mellitus Management in The Athletic PopulationRitesh NetamPas encore d'évaluation
- Information 13 00059 v2Document18 pagesInformation 13 00059 v2hendranatjPas encore d'évaluation
- A Review On Role of Plants Extracts and Its Phytochemicals For The Management of Diabetes 2155 6156 1000565Document38 pagesA Review On Role of Plants Extracts and Its Phytochemicals For The Management of Diabetes 2155 6156 1000565Opeyemi AriyoPas encore d'évaluation
- Blood Sugar Levels Blood Glucose Charts For Children and AdultsDocument1 pageBlood Sugar Levels Blood Glucose Charts For Children and Adultsyvess leyv ignacioPas encore d'évaluation
- FNCPDocument3 pagesFNCPNyj QuiñoPas encore d'évaluation
- Sglt2 Inhibitor - PDF 25Document7 pagesSglt2 Inhibitor - PDF 25JaganPas encore d'évaluation
- Module 9 ElaborateDocument6 pagesModule 9 ElaborateTrishaPas encore d'évaluation
- Variability in The Control of Type 2 Diabetes in Primary Care and Its Association With Hospital Admissions For Vascular Events. The APNA Study.Document12 pagesVariability in The Control of Type 2 Diabetes in Primary Care and Its Association With Hospital Admissions For Vascular Events. The APNA Study.franciscoPas encore d'évaluation
- SBAR ExampleDocument1 pageSBAR Examplekellymk2584100% (1)
- M1 Kamad - G26 NCPDocument3 pagesM1 Kamad - G26 NCPkkd nylePas encore d'évaluation
- Lesson Plan ContentDocument6 pagesLesson Plan ContentSrijana Gurung100% (2)
- Chavez Et Al - Final PaperDocument9 pagesChavez Et Al - Final PaperJed BellenPas encore d'évaluation
- Van Duyn May 11, 2021 InspectionDocument12 pagesVan Duyn May 11, 2021 InspectionJames MulderPas encore d'évaluation
- Cardiometabolic RiskDocument1 pageCardiometabolic RiskVaidya Priyanka SharmaPas encore d'évaluation
- Presentation and Character For Adult Patients With Diabetes in LibyaDocument8 pagesPresentation and Character For Adult Patients With Diabetes in LibyaMediterr J Pharm Pharm SciPas encore d'évaluation