Académique Documents
Professionnel Documents
Culture Documents
Medical Diseases of The Retina
Transféré par
Nurul WijayantiTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Medical Diseases of The Retina
Transféré par
Nurul WijayantiDroits d'auteur :
Formats disponibles
The Continuously Expanding and Updated Electronic Ophthalmology Textbook
Magdy A Nofal
MB, ChB, FRCSEd, FRCOphth
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
Introduction
My goal of writing “The Really Current Ophthalmology” book is to provide the reader with an
ophthalmology textbook that will continuously be expanded and up-dated to meet the rapid developments in
Ophthalmology and Ophthalmic research. Nowadays, when medical knowledge is changing with such an
alarming speed, it would be much easier and more practical to produce books in an electronic format which
can be updated and expanded much faster and easier. This will also enable me to produce the book in a very
economic way to keep the cost to a minimum, which will be reflected on its price. Any part or the whole of
the book can be printed if the reader wishes to read it on paper rather than on a computer screen.
Magdy Nofal
The Author
Magdy Nofal is an ophthalmic surgeon in Torbay general hospital, Torquay, Devon, UK. He was born in Egypt
and qualified in medicine in Cairo university in 19975 (MB ChB). He has been working in the UK since 1980.
He passed his FRCS Diploma examination from the Royal College of Surgeons in Edinburgh in 1983, and was
also awarded the fellowship of the College of Ophthalmologists of the UK in 1990. The author’s main
interest in Ophthalmology is anterior segment, oculoplastic and lacrimal surgery.
Address
Mr. Magdy A Nofal FRCS, FRCOphth
The Eye Clinic, Level 2, Torbay General Hospital,
Lawe’s Bridge, Torquay TQ 2 7 AA
Devon, UK
Tel. number
Work: “UK” 01803655192.
E-mail address
magdynofal@hotmail.co.uk
For the latest information about the whole book; see the website:
www.medicalebooks.co.uk
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
MEDICAL DISEASES OF THE RETINA
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
Central and Branch Retinal Vein Occlusion
Pathogenesis and Aetiology
Central and branch retinal vein occlusion are multi-factorial conditions. The pathogenesis of central retinal
vein occlusion is not completely understood. The following mechanisms have been implicated in the
pathogenesis of the disease:
1. Venous thrombus formation
2. Venous stasis
3. Inflammation
Anatomical factors appear to be more crucial in second order branch retinal vein occlusion than in more
peripheral occlusions. Narrowing of retinal veins at the A/V crossing may induce haemodynamics changes
that lead to thrombus formation and venous occlusion. Among the other anatomical factors that play a role
in the mechanism of the disease, is the axial length of the eye. The axial length in eyes with central or
branch retinal vein occlusion appears to be shorter than controls. Branch retinal vein occlusion typically
occurs at the arteriovenous crossings with the retinal arteriole crossing over the vein in 70-85% of the
intersections. At these locations the retinal arterioles share a common adventitial sheath with the venules.
Central retinal vein occlusion may result from thrombus formation at the cribriform plate. Thrombus
formation may also result as a secondary phenomenon due to obstruction of the central retinal vein. The
scleral outlet is a confined space occupied by the optic nerve, central retinal artery and vein. Pressure in
the scleral outlet may be increased by vascular thickening, persistent myelin sheath, and connective tissue
and collagen changes. Increased pressure in the confined scleral outlet may lead to compression of the
central retinal vein or artery (a bottleneck effect).
A prospective study examined 1090 patients with retinal vein occlusion to assess the prevalence of
associated systemic diseases. The study showed a significantly higher prevalence of hypertension,
peripheral vascular diseases, venous diseases, peptic ulceration, thyroid disease, chronic obstructive airway
diseases and cerebrovascular diseases in patients with branch occlusion than in those with central retinal
vein occlusion. Patients with ischaemic central retinal vein occlusion were more likely to have hypertension
and diabetes than those with non ischaemic occlusion. The study also showed no relationship with smoking.
When compared against the general population, patients with vein occlusion are more likely to die from
myocardial infarction.
Measuring plasma homocysteine levels is important in the evaluation of patients with retinal vascular disease
for hyper-coagulable state. Retinal vascular occlusion is associated with elevated plasma homocysteine
levels and low serum folate levels, but not with serum vitamin B12 levels. It is thought that plasma
homocysteine levels and serum folate levels should be determined in patients with retinal vascular
occlusions, and dietary supplementation with low doses of folate and vitamin B12 should be considered for
affected persons. Fluorescein administered in angiographic studies may interfere with blood tests using
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
fluorescein-labeled reagents, as well as other methods, measuring near its 493.5-nm absorption maximum or
525-nm emission wavelengths or involving fluorescence quenching.
There is a close correlation between aqueous Vascular Endothelial Growth Factor (VEGF) levels and the
onset, persistence, and regression of iris new vessels; extent of retinal capillary non-perfusion; and vascular
permeability in human ischaemic central retinal vein occlusion indicating that increased aqueous Vascular
Endothelial Growth Factor level may predict the need for treatment, and that anti-VEGF therapy at an
early stage of ischaemic central retinal vein occlusion may be therapeutically beneficial.
Clinical Features
CRVO is divided into 2 clinical types, ischaemic and non-ischaemic. Non-ischaemic CRVO is the milder form
of the disease. It may present with good vision, few retinal hemorrhages and cotton-wool spots, no relative
afferent pupillary defect, and good perfusion to the retina. Non-ischaemic CRVO may resolve fully with
good visual outcome or may progress to the ischemic type. Ischaemic CRVO is the severe form of the
disease. CRVO may present initially as the ischaemic type, or it may progress from non-ischaemic. Usually,
ischaemic CRVO presents with severe visual loss, extensive and deep retinal hemorrhages and cotton-wool
spots, presence of relative afferent pupillary defect, poor perfusion to retina, and presence of severe ERG
changes. Patients with ischaemic CRVO may end up with neovascular glaucoma and a painful blind eye.
The natural history of branch retinal vein occlusion is variable. Some patients may notice spontaneous
improvement in visual acuity and clinical features. Visual loss in this disease may be caused by several
factors:
1. Macular oedema.
2. Retinal ischaemia with or without neovascularisation of the disc, the retina or the iris.
3. Vitreous haemorrhage.
4. Traction retinal detachment involving the fovea.
5. Epiretinal membrane.
o Patchy ischaemic retinal whitening is a useful fundus sign that has been described in younger patients
with non-ischaemic central retinal vein occlusion. This sign seems to be associated with better visual
outcomes. The patchy ischaemic retinal whitening has a perivenular distribution in the macula, has no
fluorescein angiographic correlate in milder cases, can occur before any retinal haemorrhages or macular
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
oedema, and resolves in 2 to 4 weeks. Cilioretinal arteriolar insufficiency is a common finding associated
with patchy ischaemic retinal whitening.
o In a prospective study, 874 cases of retinal vein occlusion were classified into three groups depending
on the sites of occlusion:
1. Arteriovenous crossing retinal vein occlusion,
2. Optic cup retinal vein occlusion, and
3. Optic nerve retinal vein occlusion.
o The study looked at different risk factors associated with these different sites, and optic nerve head
swelling was used to separate the optic nerve sited retinal vein occlusions into two groups. A high
prevalence of hypertension and smoking was seen in arteriovenous crossing retinal vein occlusion, roughly
correlating to the old classification of branch retinal vein occlusion. Association of primary open-angle
glaucoma was seen only for those cases of central retinal vein occlusion, or optic nerve sited retinal vein
occlusion without optic nerve head swelling. Optic cup retinal vein occlusion was associated with raised
intraocular pressure.
o There is higher prevalence of abnormal haematocrit value, haemoglobin and blood urea nitrogen in
ischaemic central retinal vein occlusion than non-ischaemic vein occlusion. On the other hand, non-
ischaemic central retinal vein occlusion has a higher incidence of abnormal antinuclear antibody (ANA).
Uric acid levels were highest in the branch retinal vein occlusions. There is also a higher prevalence of
abnormal glucose and ANA in central retinal vein occlusion and hemi-central retinal vein occlusion than in
branch retinal vein occlusion.
Management
The main aims of management are:
1. Identification of the main risk factor and prompt referral for treatment
2. Treatment of sight threatening ophthalmic complications
1. Identification of the main risk factor and prompt referral for treatment
Identifying and treating the main risk factors are likely to result in less recurrence (estimated to affect
about 15% of patients over a 5 years period), protection of the other eye and also in reduction of
cardiovascular events rate. The main risk factors known to be associated with retina vein occlusion include:
i. Hypertension
ii. Hyperlipidaemia
iii. Diabetes
iv. Thrombophilia
v. Myloproliferative diseases
vi. Glaucoma
vii. Other inflammatory eye disease e.g. Behcet’s disease, sarcoidosis and others.
The following table summarises the basic investigations needed in patients with retinal vein occlusion:
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
Routine Investigation Special Investigation
1. FBC and plasma viscosity (or ESR) 1. Thrombophilia screening
2. Blood glucose level 2. Anti-cardiolipin antibodies
3. Blood cholesterol and HDL cholesterol (the 3. Lupus antibodies
cholesterol level should be interpreted with 4. C reactive protein
relation to the thyroid function tests) 5. Serum ACE
4. Electrolytes and creatinine levels 6. Antibodies profile
5. Plasma protein electrophoresis 7. Chest X ray
8. Fasting homocysteine level
o A previous study of 588 patients with branch or central retinal vein occlusion showed that taking anti-
platelets treatment protects against death.
2. The recognition and the treatment of sight threatening ophthalmic complications
Until recently, treatment of central and branch retinal vein occlusion has been directed at treatment of the
sequelae of the disease such as macular oedema and disc, retinal or iris neovascularisation by laser
photocoagulation. Recently, there have been some laser and surgical techniques that can lead to improved
perfusion and circulation in the occluded veins.
Argon Laser Photocoagulation
Major recommendations of the branch retinal vein occlusion study
1. Wait for sufficient clearing of retinal haemorrhages to obtain a good and reliable Fluorescein
angiography.
2. Determine whether visual loss is due to macular oedema or due to macular ischaemia and non-perfusion.
3. If the visual loss is due to macular oedema, wait for spontaneous improvement in about 3 months.
4. If there is no spontaneous improvement in 3 months, recommend grid laser photocoagulation.
5. If visual loss is considered to be due macular ischaemia, no laser treatment will be needed.
6. If there are more than 5 disc diameters of retinal non-perfusion, follow up every 4 months watching for
the development of retinal/disc neovascularisation.
7. If retinal/disc neovascularisation develops, recommend sector retinal laser photocoagulation.
Major recommendations of the central retinal vein occlusion study
1. About one third of eyes judged to be perfused at the onset of the disease become non-perfused by 3
years.
2. Grid laser photocoagulation for macular oedema may result in drying of the oedema but does not result
in improvement in vision and is not recommended.
3. Prophylactic laser retinal photocoagulation before the development of retinal/disc neovascularisation
does not prevent the development of retinal/disc neovascularisation and is not recommended.
4. Prompt regression of neovascularisation is more likely to occur in eyes that had not undergone
prophylactic pan retinal laser photocoagulation.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
5. Prompt pan retinal laser photocoagulation, when neovascularisation develops (on the disc, retina, iris or
anterior chamber angle), appears to diminish the risk of developing neovascular glaucoma and should be
undertaken.
Surgical Technique: Laser Photocoagulation for Branch Retinal Vein Occlusion
Laser photocoagulation for macular oedema secondary to branch retinal vein occlusion
Macular oedema (represented with the grey colour) is treated with 100-200 micron laser burns
(represented with the black colour) placed in the area of retinal thickening up to the foveal avascular zone
(the 100 micron burns are placed nearer to the boundary of the FAZ).
Avoid treatment over collateral vessels and retinal haemorrhages.
Sector retinal laser photocoagulation for peripheral or disc neovascularisation secondary to branch
retinal vein occlusion
200 micron laser burns of moderate intensity (represented with the grey colour) placed in the retinal
quadrant supplied with the occluded retinal vein
Pan retinal laser photocoagulation for central retinal vein occlusion
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
Intense 200 micron laser burns of 0.1 second duration (represented with the grey colour) are placed all
over the whole retina excluding the macular area.
o Retinal photocoagulation in patients with branch vein occlusion has a vasoconstrictive effect on occluded
veins. The correlation between the change in visual acuity and the change in vessel diameter indicates
that constriction of the branch retinal vein after photocoagulation may be an early indicator of the
success of laser treatment.
o Patients with retinal-choroidal collateral are unlikely to develop anterior segment ischaemia, and
patients with collateral vessels may safely be followed up with conservative treatment instead of laser
photocoagulation.
Laser-assisted chorioretinal anastomosis
The aim of this technique is to create an anastomosis between the retinal circulation and the choroidal
circulation to enable the obstructed venous blood to enter the choroidal circulation and bypass the site of
venous obstruction.
Surgical Technique
o Blue/green argon laser is used with setting of 50 micron spot size, 0.1 second duration and a power of
1.5 to 2.5 W
o The site of the attempted anastomosis is often selected in the lower half of the retina three disc
diameters away from the optic disc. In branch retinal vein occlusion the laser is applied within one disc
diameter peripheral to the site of occlusion. The horizontal meridian is avoided to minimise the risk of
damage to the long posterior ciliary arteries.
o Laser shots are directed to the edge of a tributary vein of the inferior temporal or inferior nasal
branches of the central retinal vein. High power shots are used aiming to disrupt the vein wall and also
the Bruch’s membrane.
o Rapid sequence fluorescein angiography can be used to determine the success of failure of the
anastomosis.
Treatment of BRVO (left), and CRVO (right)
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
o The technique has been shown, in a previous study, to produce a successful anastomosis in 33% of
patients. In all cases with successful anastomosis there was a resolution of the clinical features and
improvement in the visual acuity. 31% of eyes, in which anastomosis creation was not possible, developed
ischaemic changes and 50% developed various degrees of macular damage and reduced visual acuity.
o This technique can also be employed for the treatment of branch retinal vein occlusion. In a
retrospective study of 24 eyes with central retinal vein occlusion and 6 eyes with branch retinal vein
occlusion, creation of a successful anastomosis was possible in 38% of eyes with central retinal vein
occlusion and in 50% of eyes with branch retinal vein occlusion. The same study reported an
improvement in the visual acuity in successful case of central retinal vein occlusion of 6 lines or more (in
8% of cases) within two months after treatment and no improvement in 8% of cases. In eyes with
branch retinal vein occlusion visual acuity improved 6 lines in 16% of patients (one eye), and 1 to 3 lines
in 33% (two eyes).
o This procedure is not without complications. The efficacy and safety of this technique was described in
a case series study of 8 patients with central retinal vein occlusion. The study reported only two
successful attempts at creating an anastomosis in a twenty attempts in all eyes. However, the successful
cases demonstrated no improvement in the visual acuity, while two cases showed improvement in the
visual acuity despite having a failed anastomosis creation. Three patients in the study developed
rubeosis and retinal neovascularisation at the laser sites and vitreous haemorrhage. Additionally,
traction retinal detachment occurred twice and neovascular glaucoma once.
o McAllister and Constable reported a large retrospective study of 91 eyes with non-ischaemic central
retinal vein occlusion with a mean duration of 15 weeks and visual acuity of 20/100 or less with a
minimum of 12 months follow up. In 54% of cases creation of a successful anastomosis was possible.
However, 18% of patients had neovascular complications such as intravitreal, intra-retinal and sub-
retinal neovascular membranes. Fibrous tissue proliferation also occurred at 9% of cases. The creation
of successful anastomosis was associated with improved visual acuity. 84% of eyes had an average
improvement of between 2 to 20 lines.
o The efficacy and safety of the technique of laser-induced chorioretinal anastomosis in the treatment of
non-ischaemic central retinal vein occlusion is still unproved. Complications’ rate and severity are still
unacceptable taking in consideration that spontaneous improvement in the clinical features and visual
acuity in some of these cases is possible. Further refinement in the technique is needed before it can be
used in clinical practice.
A new modification of laser-assisted chorioretinal anastomosis
A new study showed that puncture of the vein wall is not required to form a functioning anastomosis and
that puncture of the adjacent Bruch's membrane alone is sufficient. In this study treatment sites were
selected adjacent to engorged first-order or second-order venous tributaries, avoiding direct treatment
through intra-retinal haemorrhage. The immediate peripapillary area and the horizontal meridian are
avoided to minimize the risk of striking a branch of the posterior ciliary arterial circulation. Medium
intensity long-duration laser photocoagulation spots were applied to a focal area at the selected site using
green or blue-green wavelength. The evolution of functioning anastomosis sites occurred over a 4-week to
8-week period. Treatment complications were limited to localized pre-retinal fibrosis, which developed at
treatment sites in 26% of patients.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
Old technique (left), and new modification (right)
Surgical Treatment
Arteriovenous crossing decompression (sheathotomy)
The retinal arteries and veins share a common connective tissue sheath at their crossing sites. It has been
postulated that arteriolar sclerosis presses on the venule causing narrowing of the venous lumen, blood flow
turbulence, damage to the vascular endothelium and possibly thrombus formation. Therefore, surgical
decompression of the venule by separating the arteriole from the venule should, theoretically, result in
improvement of the retinal perfusion.
Surgical decompression of branch retinal vein occlusion via sheathotomy of the arteriovenous crossing has
been proven to be technically possible in eyes with branch retinal vein occlusion. The procedure appears to
result in rapid reperfusion of the retina. Retinal reperfusion leads to resolution of macular haemorrhage,
oedema, and ischaemia and may lead to improvement in the visual acuity.
Surgical principle:
o A conventional 3-port Pars plana vitrectomy is performed.
o A modified micro-vitreoretinal blade with a bent tip is used to separate the arteriole from the venule.
o An inner retinal incision parallel to the retinal arteriole is then performed.
o A gentle lifting action of the arteriole is applied until the common sheath is identified.
o The sheath is divided by the blade and the arteriole is separated from the underlying venule.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
o A recent article reviewed the long term results of arteriovenous sheathotomy in 5 cases (a mean of 6.5
years) with branch retinal vein occlusion. The visual acuity in 4 out of the 5 cases improved after
surgery from preoperative visual acuity of 20/200 to visual acuity of between 20/30 and 20/70 after
surgery. Poor preoperative visual acuity in these cases was mainly caused by macular oedema. The visual
acuity in the fifth case stayed the same at counting finger.
o A recent prospective, non randomised comparative trial compared this technique in 20 eyes to no
treatment or laser photocoagulation for macular oedema in another 20 eyes. In the 20 eyes that had
sheathotomy 75% halved the visual angle, and the average improvement of vision was 4.55 lines. In the
other 20 eyes that had observation or grid laser treatment, only 40% halved the visual angle, and the
average improvement of vision was 1.55 lines.
Radial Optic Neurotomy
o It has been hypothesised that central retinal vein occlusion may be caused by a neuro-vascular
compression mechanism similar to carpal tunnel and thoracic inlet syndrome (bottleneck effect).
Relaxation of the compression at the scleral outlet ring, should therefore, lead to improvement of the
retinal circulation and the clinical features of central retinal vein occlusion.
Increased pressure in the confined scleral outlet may lead to compression of the central retinal vein
(bottleneck effect).
o Radial optic neurotomy is a new technique designed to test this theory. In this technique the scleral
outlet is decompressed via an internal vitreoretinal approach. A retrospective pilot study of 11 patients
with severe central retinal vein occlusion demonstrated that this technique is technically possible and
can be successful in improving the outcome of central retinal vein occlusion.
Patients’ selection criteria are:
o Non-randomised selection with an average age of 60 (35-86)
o The average duration of the disease before surgery was 4 months (1-7 months)
o All 11 patients had severe haemorrhagic central retinal vein occlusion with initial visual acuity of 20/400
or less
o Six patients had RAPD, and pre-proliferative retinal changes
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
o Four patients had iris neovascularisation and two had vessels in the angle
o Patients were followed up at 1 day, 1 week, 1 month, 2 months and at the last visit
o The average follow up was 9 months (5-12 months)
Surgical principle
o The goal of the procedure is to make a relaxing incision at the level of the cribriform plate, scleral ring
and the adjacent sclera.
o Three-port vitrectomy, the intraocular pressure is raised during surgery to avoid intraocular bleeding.
o The optic neurotomy incision is performed on the nasal side of the optic disc to avoid injury to the
papillomacular bundle. The clock hour site of the incision is selected preoperatively to avoid damage to
the main retinal vessels.
o One or more incisions are performed in a radial fashion to avoid transection of and minimise damage to
the nerve fibre layer. The tip of a micro-vitreoretinal blade is placed at the edge of the optic disc and
directed posteriorly into the optic nerve for a depth just beyond the widest part of the blade. Great
care should be taken to avoid any contact with the major retinal vessels on the disc.
o Laser photocoagulation or gas tamponade was not used.
The optic neurotomy incision is performed on the nasal side of the optic disc to avoid injury to the
papillomacular bundle.
The results of this study are summarised in the following table:
1. All patients had improvement in the clinical and angiographic fundus features.
2. Equal or better visual acuity was noticed in 82% of patients (9/11 patients).
3. 73% of patients (8/11) had an average of five lines improvement in the Snellen visual acuity.
4. 73% of patients (7/11) had final visual acuity of 20/200 or better.
5. 45% (5/11) had visual acuity equal or better than 20/70, and two patients achieved visual acuity of
20/40 at the final follow up examination.
6. The visual acuity in two patients deteriorated by one line. These two patients had iris neovascularisation
prior to surgery.
7. Resolution of retinal haemorrhage and venous dilatation occurred relatively rapidly (by two months after
surgery).
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
8. The improvement in the visual acuity did not correlate with the duration of the central retinal vein
occlusion or with the associated systemic disease.
o A new study evaluated the effects of radial optic neurotomy on retinal circulation in patients with
central retinal vein occlusion by Indocyanine Green videoangiography and a computer-assisted image
analysis. The study showed that there is a degree of retinal circulation improvement in approximately
half of the eyes. The improvement appears to be correlated with the development of chorioretinal
anastomosis.
o Another study showed that radial optic neurotomy may be complicated with choroido-vitreal
neovascularization from the neurotomy site.
Endovascular Therapy
o Endovascular re-canalisation of the retinal vessels can help establish retinal blood flow by both
mechanical and pharmacological means. Several attempts aiming at restoring blood flow in the retinal
vessels have been described. Recently, it has been demonstrated, in cadaver eye models, that
cannulation of branch retinal arterioles and central retinal artery and branch retinal venules and central
retinal vein can be achieved. The introduction of a catheter through the retinal blood vessels and
navigating it to the desired site where the obstruction lies has also been proved possible and feasible.
o In an experimental study in cadaver eyes Tang, et al, showed that, by using two 20 gauge micro-
vitreoretinal blades it is possible to create a longitudinal incision in the retinal vessels wall after
elevating the retinal vessels from the retinal surface. They also showed that such an incision can be
created in the first order retinal arteriole/venule immediately distal to the central bifurcation and also
in the second order retinal arteriole/venule about 3 or 4 disc diameters away from the optic disc.
Cannulation of the retinal blood vessels, through the longitudinal incision, was also possible using a 10/0
black nylon suture. The nylon suture could be advanced only till the optic disc in cases of branch retinal
vessels. In cases of cannulation of the central retinal vessels the nylon sutures could easily be advanced
in the optic nerve emerging from the retrobulbar part of the nerve. In their study, unsuccessful
cannulation was due to insufficient blood fill in the retinal vessels, poor view caused by bleeding, false
passage, folding and distortion of the retina. The authors reported that new technology and technical
advances may lead to the production of better cannulation devices. Histological studies of the
successfully cannulated vessels, in this study, demonstrated no damage to the vascular endothelium
caused by the nylon suture.
The use of fibrinolytic agents
o Histopathological studies showed that central retinal vein occlusion may be associated with thrombosis
at the lamina cribrosa. Systemic administration of fibrinolytic agents (such as tissue plasminogen
activator) has, therefore, been investigated for the treatment of this disease. Treatment by systemic
administration of the drug seems to have a beneficial effect on the retinal circulation in some cases. In
a pilot study, 42% of patients treated with IV 100 mg of t-PA had improvement in the visual acuity of at
least three lines. However, systemic administration of tissue plasminogen activator may be associated
with higher morbidity and mortality rate caused by ocular and cerebral haemorrhage.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
o Intravitreal administration of fibrinolytic substances appears to be simpler and safer than systemic
administration. Intravitreal administration does not however appear to modify the natural history of the
disease and does not significantly improve the final visual acuity in most patients.
o It has been proven that cannulation and injection of tissue plasminogen activator in the retinal vein is
practically possible and safe procedure.
o In 1988, Weiss reported a case of 81 years old women who developed a central retinal vein occlusion
following a similar problem in the other eye few years previously. Conventional treatment and
chorioretinal laser anastomosis was unsuccessful in her case. The author reported improvement in the
venous filling time (from 33 seconds to 24 seconds) and also improvement in the clinical features after
injection of tissue plasminogen activator in a branch retinal vein in the recently affected eye. The visual
acuity, however, stayed stable for one year after treatment.
o In 2001 the same author published a prospective non-comparative study of this technique applied in 28
eyes with central retinal vein occlusion. The author concluded that vitrectomy with vain cannulation and
infusion of tissue plasminogen activator is a safe procedure that may improve vision in eyes with central
retinal vein occlusion.
Surgical principle
o A conventional 3-port vitrectomy technique is used + fashioning an additional sclerotomy for the
introduction of 33 gauge needle that is introduced parallel to the branch retinal vein selected for the
injection. Initially the author used a 33 gauge needle, but later on he designed a glass cannula specially
made for that purpose.
o The IOP is then lowered and the injection is made in the selected retinal vein.
o A bolus of an average 3.4 mg of t-PA is then injected in the vein very slowly over few minutes.
o The IOP may or may not be increased after the injection to prevent vitreous haemorrhage.
Results of cannulation and tissue plasminogen activator injection in central retinal vein occlusion:
1. The visual acuity improved in 54% of patients for three lines or more within 6 months.
2. 7 patients developed vitreous haemorrhage.
3. 1 patient developed retinal detachment which was repaired by pneumatic retinopexy.
o Recent advances in neuro-radiology have made possible the selective catheterisation of small
intracranial vessels. A recent retrospective non-controlled study investigated the possibility of
selective ophthalmic artery infusion of urokinase in the treatment of central retinal vein occlusion,
combined central retinal vein occlusion and artery occlusion, and combined central retinal vein occlusion
and celioretinal artery occlusion. Treatment in this study was carried out in a neuro-radiological
department under local anaesthesia by a neuro-radiologist.
o 26 eyes of 26 patients were included in this study. Six patients experienced what the authors
described as a striking improvement in the visual acuity in the first 24 hours after treatment. Four out
of these six patients had combined central artery and central retinal vein occlusion. Intravitreal
haemorrhage occurred in 2 eyes. No patient developed any extraocular complications related to the
procedure. The authors suggested that patients with duration of visual loss of less than 8 days, and
those without macular oedema should be subjected to this treatment. Additionally, they also suggested
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
that this method of treatment might be particularly useful in patients with suspected combined artery
and vein occlusion as most of these cases has a poor outcome. They concluded that more prospective
controlled studies are needed to fully evaluate this technique.
Surgical principle
o The internal carotid is catheterised via the femoral artery.
o An internal carotid cerebral angiogram is carried out to identify the carotid artery siphon.
o A 5 Fr guide catheter is then placed inside the proximal extracranial part of the internal carotid artery.
o A 1.8 Fr or 1.5 Fr flow guide micro-catheter is advanced through the guide catheter into the opening of
the ophthalmic artery.
o A super-selective ophthalmic angiogram is then performed to assess the correct placement of the
micro-catheter.
o 300000 IU of urokinase pre-diluted with 0.9% normal saline is used to perfuse the ophthalmic artery
for 40 minutes using an electric pump.
Surgical treatment of complications
o Surgical treatment may also be indicated for complications of central and branch retinal vein occlusion.
The main indications of surgical treatment are:
1. Persistent vitreous haemorrhage
2. Traction retinal detachment involving the macula and rhegmatogenous retinal detachment
3. Epiretinal membrane
o Vitrectomy for complications of branch retinal vein occlusion results in improvement in the visual acuity
in the majority of patients. About 74% of eyes with non-clearing vitreous haemorrhage and about 59%
of patients with traction retinal detachment are expected to benefit from surgical treatment.
o Visual outcome of treatment for epiretinal membrane seems to be poorer in this group of patients than
in the idiopathic type. This may be due the presence of macular ischaemia and or oedema. Vitrectomy in
this group of patients may be complicated with retinal detachment, vitreous haemorrhage, epiretinal
membrane, choroidal haemorrhage, central retinal vein occlusion and central retinal artery occlusion.
Better preoperative visual acuity, absence of RAPD, absence of preoperative macular oedema are
associated with better visual results.
o Rhegmatogenous retinal detachment occurs in about 2-3% of patients with branch retinal vein occlusion.
The detachment may be associated with two different types of retinal breaks, retinal break caused by
vitreous traction or retinal break without vitreous traction After vitrectomy operation about 32% of all
eyes with rhegmatogenous retinal detachment achieve visual acuity of 20/400 or better and 80% of
eyes achieve visual acuity of 20/200 or better. Eyes with retinal breaks without vitreous traction
achieve better visual results than eyes with retinal breaks associated with vitreous traction. In a study
of 25 eyes that underwent vitrectomy for rhegmatogenous retinal detachment after branch retinal vein
occlusion, 100% of eyes with retinal holes without traction and 77% of eyes with retinal breaks with
vitreous traction achieved successful anatomical outcome at final examination. 100% of eyes with retinal
holes not caused by vitreous traction achieved visual acuity equal to or better than 20/200 compared to
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
62% of eyes associated with retinal breaks caused by vitreous traction. Higher rate of preoperative
macular detachment and a higher rate of recurrences of the detachment are factors associated with
poor final visual acuity in eyes associated with retinal breaks caused by vitreous traction.
o The outcome of vitrectomy for retinal detachment also depends on whether disc new vessels are
present or absent. In a retrospective study of 22 patients with branch retinal vein occlusion and retinal
detachment, eyes without disc new vessels achieved better visual results after vitrectomy than eyes
with disc new vessels. The authors of the study speculated that the difference in the visual results is
probably due to difference in retinal perfusion and difference in the presence of angiogenic factors
between the two groups.
o Optic disc traction and secondary localized retinal detachment can develop after ischaemic central
retinal vein occlusion and may contribute to the poor visual acuity.
Intravitreal triamcinolones “see elsewhere under Vitreoretinal surgery”
Intravitreal injection of triamcinolone appears to be effective in reducing cystoid macular oedema
associated with central retinal vein occlusion. This reduction often corresponded to an improvement in visual
acuity.
Hyperviscosity Syndromes
Hyperviscosity syndromes are caused by an increase in the serum or whole blood viscosity. They are caused
as the result of either proliferation of abnormal immunoglobulins in serum (multiple myeloma or
Waldenstroms macroglobulinaemia), or an excess of white cells or red blood cells, (leukaemia or
polycythaemia).
Causes
1. Multiple myeloma: Multiple myeloma is caused by the production of a monoclonal immunoglobulin (IgG,
IgA, or IgD) from a single clone of plasma cells (large with an eccentric nucleus and perinuclear halo).
Hyperviscosity syndrome is rarely seen until the serum viscosity exceeds 4.0 Cp units relative to normal
saline (for more details, see below).
2. Waldenstroms macroglobulinaemia: Waldenstroms macroglobulinaemia is characterized by the
production of a single b-cell line (plasmacytoid lymphocytes) with high intravascular concentration of
IgM. The B lymphocytes densely infiltrate the bone marrow, lymph nodes and spleen, and the excess
IgM leads to the elevated intravascular volume that results in dilated capillary beds. The IgM also coats
platelets and binds with clotting factors leading to a bleeding tendency.
3. Leukaemia: in leukaemia with a grossly elevated white cell count patients may develop features of the
hyperviscosity syndrome. Leukaemic blast cells and mature leukocytes are less deformable than
erythrocytes. This in combination with the increase in whole blood viscosity and the high oxygen
consumption rate of the leukaemic blast cells will impair flow in the microcirculation.
4. Polycythaemia: Primary (polycythaemia rubra vera) is a clonal, neoplastic proliferation of myeloid stem
cells. Polycythaemia is an increase in red cells, usually with a corresponding increase in haemoglobin level.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
Systemic Features Retinal Features Investigation
fatigue, headaches, weakness, Venous dilation, beading and tortuosity, Full blood count, electrolytes,
dizziness, cardiac failure, anorexia, retinal haemorrhages (dot and blot), glucose, LFTs, ESR, Protein
epistaxis or bleeding gums, and visual retinal and disc oedema, retinal venous electropheresis and urine for Bence
impairment occlusion, and rarely retinal artery Jones proteins, CT scan. Refer to
occlusions, vitreous haemorrhage and haematologists for further
serous retinal detachment. investigation – (bone marrow
Fluorescein angiography shows micro- aspirate/biopsy),
vascular changes, microaneurysms and
discrete areas of capillary non-
perfusion.
Management
o Depend on the underlying cause for the hyperviscosity disorder
o Reducing the viscosity
Prognosis
o The visual prognosis is generally good if there is no central retinal vein occlusion.
o Permanent reduction of vision if there is capillary occlusion of the perifoveal network or chronic serous
detachment
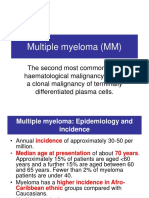
Multiple myeloma
Multiple myeloma develops from plasma cells. In myeloma, a single plasma cell multiplies out of control. This makes the
immune system much less effective. Myeloma cells produce excessive amounts of a single type of antibody, which is
known as paraprotein, or monoclonal spike. Myeloma usually develops at a number of different sites within the body.
The most common sites for multiple myeloma are the pelvis, spine, rib cage, skull, shoulders and hips. Multiple myeloma
seems to commoner in 50 years old or older patients, people who have been exposed to high doses of radiation, people
with a disease called monoclonal gammopathy, and in people of African descent.
Multiple myeloma may not cause symptoms in its early stages. Symptoms can include: bone pain, bleeding/bruising
problems, anaemia, tiredness and weakness, shortness of breath and infection. The excessive production of antibody,
or paraprotein, in multiple myeloma can lead to kidney damage.
Diagnostic tests include: Blood tests (very high ESR, FBC, protein electrophoresis, and electrolytes for kidney
damage), urine test (Bence-Jones protein), X-rays (bone damage) and bone marrow tests.
Chemotherapy is the main treatment for multiple myeloma. Radiotherapy is commonly used to treat localized areas
where there is bone destruction and pain. Doctors may give radiotherapy as a treatment on its own, or in addition to
chemotherapy.
Retinal Vein Occlusion in Young Patients
Central retinal vein occlusion in young patients is rare. The disease is rarely associated with systemic
disease. The presenting visual acuity does not appear to be predictive of visual or anatomic outcome in
younger patients with central retinal vein occlusion. A significant number of patients with good vision at
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
presentation develop legal blindness. It often undergoes a slow spontaneous resolution over a period of 4-6
months. Good visual recovery often occurs in most patients. Some studies on the other hand demonstrated
poor visual outcome. The final visual results largely depend on the degree of retinal ischaemia as well as the
presence of complications e.g. cystoid macular oedema.
The cause and pathogenesis of the disease is unknown. It is thought that the disease, in most cases, is
caused by a mild non-specific vasculitis of the retinal or disc capillary vessels. Other investigators believe
that vitreous traction may play an important role in the pathogenesis of the disease. Routine examination
should be directed at excluding possible causes. The following systemic and local conditions have previously
been described in association with central retinal vein occlusion in young adults:
Systemic causes Local causes
1. Hypertension 1. Glaucoma
2. Diabetes 2. Congenital arteriovenous malformation
3. Hyperlipidaemia 3. Anterior and posterior uveitis
4. Hypercoagulability conditions (e.g. smoking, 4. Optic nerve disease (e.g. drusen and
abnormal platelets function and blood diseases papilloedema)
associated with increased viscosity) 5. Trauma
5. Migraine
6. Mitral valve prolapse (it is thought to be due to
abnormal platelets function)
7. Collagen vascular diseases
8. AIDS
9. Carotid artery disease (possibly due to the
presence of atherosclerotic vascular changes in
both the carotid and the retinal vessels)
10. Medications (e.g. oral contraceptives, diuretics).
Antiphospholipid antibodies syndrome
Antiphospholipid antibodies syndrome is a rare syndrome characterised by the presence of lupus
anticoagulant and antiphospholipid antibodies. Antiphospholipid antibodies may be primary, or secondary to
other disease (e.g. SLE, lymphoma, dysglobulinaemia and some infections such as Q-fever).
The syndrome is characterised by:
1. Recurrent venous and / or arterial thrombosis.
2. Recurrent spontaneous abortion.
3. Thrombocytopenia.
o Primary antiphospholipid syndrome is a thrombophilic state characterized by recurrent arterial and
venous thrombosis, recurrent pregnancy loss, and the presence of circulating antiphospholipid antibodies
that may be responsible for thrombophilia and pregnancy morbidity. Several prospective studies show an
increased risk of thrombosis in the presence of medium to high antibody level. Antiphospholipid
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
antibodies syndrome may occur in patients as young as 6 years of age. A recent report described this
condition in a 6 years old girl with poor vision caused by retinal vein thrombosis.
o Ophthalmologic features are present in 15–88% of the patients with primary antiphospholipid syndrome.
Diagnosis of antiphospholipid syndrome should be considered in all patients with recurrent systemic or
ocular thrombosis in the absence of known risk factors. An accurate diagnosis may save the patient from
recurrent, potentially life-threatening thrombosis. Patients with occlusive retinal diseases have a
significantly high prevalence of antiphospholipid antibodies. Posterior segment disease such as vasculitis,
vitritis, retinal vascular occlusion and retinal detachment are commonly associated with antiphospholipid
antibodies. Anterior segment disease may also occur. Screening of these antibodies is indicated in
patients who do not have any of the common risk factors e.g. hypertension, cardiovascular diseases or
diabetes. A study of 39 patients with primary antiphospholipid syndrome demonstrated that permanent
pathological ocular features are rare. The study also demonstrated that there is a high prevalence of
visual disturbances among patients. Most of these disturbances are transient and mainly caused by
central nervous system ischaemia.
o Systemic clinical features, such as chorea, transverse myelitis, cardiac valve lesions, and accelerated
atherosclerosis, are hypothesized to be due to a direct tissue-antibody interaction and cannot be
explained purely by thrombosis.
o Management of these patients must be a multi-disciplinary effort with either a rheumatologist or a
haematologist. Recurrent thrombosis appears to be significantly reduced with treatment with warfarin
as compared with systemic prednisolone or with no treatment at all. A prothrombin ratio of 1.5/2.0 is
recommended. It is also recommended that treatment should be continued for at least 6 months after
the disappearance of the antibodies. Recurrent branch artery occlusion has, however, been reported in
some patients after the disappearance of the antibodies, despite treatment with aspirin and steroids.
Treatment of isolated ocular thrombophilia in the presence of moderate to high titres of
antiphospholipid antibodies should be on the same principles as patients with antiphospholipid syndrome
to prevent recurrent ocular or cerebral thrombosis.
Resistance to activated protein C
o Retinal vein occlusion may also be associated with other abnormalities in the coagulation system.
o More than 90% of resistance to protein C is caused by a mutation in factor V (R 506Q), which renders
activated factor V relatively resistant to its degradation by activated protein C. The prevalence of this
mutation is high in white patients but very rare in blacks.
o Mutation of factor V has been identified in many patients with retinal vein occlusions as well as deep
venous thrombosis. Screening for this mutation, in patients with retinal vein occlusion, is recommended
by some authorities in order to identify patients at risk of developing deep vein thrombosis.
Other causes
o Hyper-homocysteinemia is a risk factor for central retinal vein occlusion and may suggest a poor
prognosis in patients with central retinal vein occlusion. This is an important cause of the disease as it
can be treated by dietary measures.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
o Thrombophilia, hypofibrinolysis and raised thrombin-anti-thrombin III complex are other abnormalities
with the coagulation system that have been reported with retinal vein occlusion. These abnormalities
may be more important in retinal vein occlusion near the main vein trunk rather than in the retinal
periphery.
o Factor VII (FVIIa) is a newly identified thrombophilia factor. Elevation of FVIIa level may play a part in
the patho-physiology of both central retinal vein occlusion and branch retinal vein occlusion
o In young patients, retinal vein occlusion may be secondary to retinal congenital arteriovenous
communication. It is proposed that a turbulent flow, high intra-vascular volume and arteriolar pressure
in the venous side of the malformation may lead to vessel wall damage, thrombosis and occlusion of the
blood vessel.
o Recent reports indicate that the incidence of retinal vascular diseases may also be slightly increased in
recent contraceptive pills users.
Treatment
o Systemic steroids may be used in cases with other local or systemic features of inflammation. It may
also be used when there severe bilateral involvement or if the vision in the fellow eye is poor. If
steroids are successful in improving vision, they may need to be continued for long periods of time. If
they are not successful, they should be stopped quickly.
o Anticoagulants have also been suggested by some clinician in order to promote collateral development.
o Plasmapheresis and haemodilution may also be effective in causing regression in the clinical findings and
improvement in the visual acuity in some patients with mixed connective tissue diseases.
o Vitrectomy may also be indicated to relieve vitreous traction or to treat vitreous haemorrhage or
traction retinal detachment.
o There is a controversy about the role played by contraceptive pills in the risk of developing
cardiovascular diseases. Case control and cohort studies suggest that taking norethisterone or
levonorgestrel-containing pills (second generation pills) increases risk of developing venous thrombo-
embolism from 5 cases per 100,000 per year to about 15 cases per 100,000 per year. Taking pills
containing a desogestrel or gestodene (third generation pills) increases the risk, on the other hand, from
5 to 25 cases per 100,000 per year. There does not appear to be any data to show that the risk of
having myocardial infarction is increased with any of these medications. Most authorities suggest that
the contraceptive pill should be stopped in patients with retinal vein occlusions.
o It is thought that the use of estrogens-containing HRT is not associated with any significant
cardiovascular risks, or retinal vascular occlusion. However, there are recent reports and case
presentations that highlight the possibility of an association between retinal vein occlusion and the use
of HRT. Central retinal vein occlusion may also be associated with celioretinal artery occlusion. The
mechanism of this condition is not completely understood. A recent case report documented this
condition in patients who had started hormone replacement therapy 6 weeks previously. The authors
believe that the celioretinal artery occlusion followed the central retinal vein occlusion.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
Central and Branch Retinal Artery Occlusion
Aetiology
o Significant carotid artery stenosis is a major cause for transient monocular blindness, retinal artery
occlusion and ocular ischaemic syndrome. Patient with retinal artery disease, at any age, should have
carotid ultrasound examination to investigate the status of the carotid artery. The presence of emboli
does not appear to be necessary for the pathogenesis of these conditions. Embolic acute retinal artery
occlusion has, however, a higher mortality rate than non-embolic disease. The presence of a retinal
embolus does not necessarily indicate the presence of a significant carotid stenosis, but their presence
has 39% sensitivity and 68% specificity for the presence of a significant carotid artery stenosis.
Patients with retinal emboli, even if asymptomatic, are at increased risk of having strokes, hypertension,
and cardiovascular disease. Medical referral for assessment may be beneficial.
o Selection for treatment should be based on the morphology of the lesion as well as the degree of
stenosis. Complex heterogeneous carotid lesions are known to be associated with more vascular lesions
than simple heterogeneous or homogenous lesions. In patients with severe carotid artery stenosis (70-
99% reduction in carotid artery diameter), associated with symptoms (e.g. amaurosis fugax, transient
ischaemic attacks, or minor ischaemic strokes), carotid endarterectomy appears to be beneficial in
reducing subsequent stroke rate. Carotid endarterectomy may also change the haemodynamics in the
circulation of the ophthalmic artery, central retinal artery, and some posterior ciliary vessels.
o In a retrospective, observational case series of 29 patients with central retinal artery occlusion, in
whom no evidence of emboli was detected; all patients underwent neuro-ophthalmic examination and
investigation with orbital colour Doppler imaging. In nine of the 29 patients a hyper-acoustic area was
noted in the retrobulbar area; which was presumed to be emboli. These hyper-acoustic plaques were
seen within the central retinal artery in its course in the orbit or the nerve, and the suggestion is that
they are embolic in nature because carotid Doppler images were abnormal in five of the nine patients.
The colour Doppler portion of the ultrasound imaging confirmed a reduced central retinal artery flow
consistent with central artery occlusion.
Types of emboli
Type Features Systemic associations
Platelet/fibrin Dull grey and elongated Carotid disease
Cholesterol Sparkling yellow + usually at an arterial Carotid disease
bifurcation
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
Calcium Dull white + typically around or on the disc Cardiac disease
Cardiac myxoma Often occludes the ophthalmic or central In young patients and particularly in the left
retinal artery behind the globe and is not eye
seen
Talc Small yellow/white glistening particles in Intravenous drug abuse
macular arterioles + may produce peripheral
retinal neovascularization
Lipid or air No emboli. Cotton-wool spots are often seen Chest trauma (Purtscher's retinopathy) +
fracture of long bones
o Amaurosis fugax is typically associated with carotid artery diseases. Abnormal haematological factors
may also cause occlusive retinal vascular diseases, and amaurosis fugax. It accounts for 25% of all
transient ischaemic attacks involving the anterior circulation. The North American symptomatic carotid
endarterectomy trial (NASCET) and European carotid surgery trial (ECST) have demonstrated the
benefit of carotid endarterectomy in symptomatic stenosis of more than 70%. In the NASCET sub-
group analysis of 1583 patients with TIAS (including 496 patients with amaurosis fugax), the risk of
ipsilateral stroke following amaurosis fugax was found to be half that for other forms of hemispheric
TIA. For patients who had had an episode of amaurosis fugax, factors that increased the risk of stroke
were:
Age > 75 years,
Male sex,
History of other hemispheric TIA/stroke,
Intermittent claudication,
Stenosis 80-94% and absence of collateral circulation
o The three-year risk of stroke (with medical treatment) varied from 1.8% for < 1 risk factor to 24.2%
for > 3 risk factors. Frequency, number and duration of episodes of amaurosis fugax bore no relation to
the degree of stenosis or the risk of subsequent stroke. Endarterectomy was only of benefit in reducing
three-year risk of stroke if two or more risk factors were present.
o Central retinal artery occlusion is rare in young adults. Systemic evaluation is necessary to rule out any
life threatening conditions. Cardiac valve diseases are the most commonly diagnosed cause in this age
group. The prevalence of cardiac valve diseases in patients presenting with occlusive vascular retinal
diseases is about 25%. Investigations to rule out the presence of emboli e.g. by trans-thoracic or by,
the even better, approach of trans-oesophageal echocardiography is recommended for the evaluation
of the heart condition in these patients, even in the absence of retinal emboli. Tailoring the
investigations according to the type of emboli (calcific, cholesterol, or platelets) does not seem to be
reliable as there is inter- and intra-observer disagreement in the diagnosis of the type of the embolus.
Trans-thoracic echocardiography is the most widely used cardiac imaging procedure. It is a non-invasive
technique that displays the left ventricle such that changes and filling defects can be detected easily.
Trans-oesophageal echocardiography is another technique that allows detection of posteriorly and
deeply located structures beyond the scope of the trans-thoracic method. This technique has increased
the detection of potential cardiac sources of emboli by two to ten folds. The main difficulty with TOE is
its invasive nature. Many elderly stroke patients are unable to tolerate it and sedation is undesirable.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
o Other diseases causing hyper-coagulation or systemic emboli (e.g. atrial myxoma, sub acute bacterial
endocarditis, smoking, internal carotid artery disease, oral contraceptives and leukaemia) may also cause
the disease. Trauma, sickle cell haemoglobinopathy (even if not associated with any contributing
factors), intravenous drug abuse, SLE, varicella-zoster infection and T cell lymphoma may also cause
retinal artery occlusion in children. Activated protein C resistance should also be considered in patients
with retinal arterial occlusion when the usual embolic or thrombotic diseases are ruled out.
o Hyper-homocysteinaemia has been identified as a general vascular risk factor. Homocysteinaemia has a
toxic effect on the vascular endothelium which may result in arteriosclerosis and arterial and venous
thrombo-embolism at a younger age. Patients with Hyper-homocysteinaemia have increased risk of
vascular occlusive diseases, strokes and myocardial infarction. The disease may also lead to the
development of retinal artery and retinal vein occlusion and also non-arteritic anterior ischaemic optic
neuropathy in young patients. This condition should be excluded in these patients who are otherwise
healthy, or patients with bilateral or recurrent disease. Diagnosis is important as the high serum level of
homocysteine can be lowered by high doses of vitamin B6, folic acid or betaine.
Gazed Evoked Amaurosis
Gazed evoked amaurosis has been previously described in patients with cavernous haemangiomas, optic
nerve sheath meningioma, osteoma, and neurofibroma. Amaurosis fugax in certain directions of gaze may
also be associated with intra-orbital mass lesions (e.g. intra-orbital foreign body) in young patients. These
cases share certain characteristics including good vision in primary position with deterioration of vision in
eccentric gaze; objective pupillary abnormalities in eccentric gaze; stereotypic onset and recovery of vision;
and fundus abnormalities of disc oedema and chorioretinal folds. This condition has also been reported
after extra-orbital lesion such as orbital fracture, and sinus tumours. Treatment of the associated
problems often leads to improvement in symptoms.
Management
o Patient with central retinal artery occlusion, central retinal vein occlusion, or anterior ischaemic optic
neuropathy are at increased risk of developing macro-vascular diseases (e.g. myocardial infarction and
cerebrovascular accidents). Hypertension, hypercholesterolemia and hypertriglyceridaemia appear to be
associated with vascular retinal diseases e.g. central and branch retinal artery occlusion and anterior
ischaemic optic neuropathy. Many studies demonstrated clinical benefit from treating blood pressure
higher than 160 systolic and 95 diastolic in patients under the age of 65 with vascular retinal diseases.
Other studies proved this benefit in older patients as well.
o It is suggested that the combined treatment of hypertension, hypercholesterolemia and the use of anti-
platelets drugs would reduce recurrence in the fellow eyes. In high risk patients it has also been shown
that anti-platelets therapy (aspirin 75-325 mg daily) reduces the risk of vascular death, myocardial
infarction and stroke. In view of the increased mortality noticed in patient with central retinal vein or
artery occlusion it seems appropriate to treat patients with anti-platelets drugs.
o It is also recommended that patient taking combined oral contraceptive pills should discontinue the
treatment if they develop retinal artery or retinal vein occlusion to avoid recurrence in the fellow eye.
Patients with retinal artery or retinal vein occlusion, on the other hand, should continue treatment with
HRT to avoid macro-vascular diseases.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
o Re-breathing into a bag produces hypercapnea (which increases the retinal blood flow) and hypoxia
(which causes vasodilatation). Both hypercapnea and hypoxia increases the cardiac output, systemic
blood pressure and also increases the ocular perfusion pressure and produce a large increase in the
macular leukocyte velocity. Re-breathing into a bag might be useful in the immediate treatment of
retinal arterial obstructive diseases, but they should be used with caution in elderly patients with
cardiovascular diseases.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
Ocular Ischaemic Syndrome (OIS)
Carotid Artery Disease
Carotid occlusive disease (originally termed venous stasis retinopathy) is not due to outflow obstruction but
due to decreased arterial perfusion, and is better termed hypotensive retinopathy. Ocular ischaemic
syndrome or hypotensive retinopathy occurs in 5-40% of patients with carotid artery occlusion. Carotid
occlusive disease may be accompanied by disease affecting small orbital arteries (which would be consistent
with the multiple risk factors seen in these patients). The retinopathy has some features similar to retinal
vein occlusion and is an important differential diagnosis in patients with vein occlusion.
The retinal circulation is auto-regulated so a moderate reduction in perfusion pressure does not reduce the
retinal blood flow. However the choroid does not show evidence of auto-regulation so that reduction in
perfusion pressure causes concomitant reduction in choroidal blood flow. Animal studies also show that only
5% of ocular blood flow is to the retina, 80% serves the choroid. Therefore choroidal perfusion is of great
importance in vascular disease of the eye. Accordingly it is reasonable to think that the first site of
damage in ocular ischaemia is the choroid. It has therefore been suggested that choroidal or ciliary body
ischaemia rather than retinal ischaemia is responsible for neovascularisation in some cases of OIS.
Hypo-perfusion of the eye has long been recognized as the major cause of OIS. It is unclear why some
patients with carotid occlusive disease develop OIS and others show no signs of ocular ischaemia at all. One
suggestion is related to the development of ophthalmic artery collaterals.
Significant carotid stenosis may result in changes in the ophthalmic artery blood flow. If there is
inadequate cross-flow in the circle of Willis from the contralateral internal carotid, reversal of flow occurs
in the ophthalmic artery as a consequence of a collateral circulation from branches of the external carotid
artery. This reversal of flow sustains cerebral blood flow at the expense of blood flow to the eye. A recent
study of 110 patients with symptomatic carotid artery occlusion found reversal of blood flow in the
ophthalmic artery in 94% with and 84% without hypotensive retinopathy. However in the cases of reversed
flow the patients with hypotensive retinopathy had on average lower pulsatility indexes in the ophthalmic
artery and lower cerebropetal blood flow than patients without hypotensive retinopathy. They could not
demonstrate that hypotensive retinopathy in these patients indicated worse atherosclerosis.
Causes
1. Carotid disease (the commonest cause, usually > 90% stenosis)
2. Ophthalmic artery disease (less common)
Clinical features
o Typically occurs in patients who are aged 50 to 80 years.
o Commonest symptom is amaurosis fugax, or CRAO
o If initial VA is better than 6/18 patients are more likely to maintain that level visual acuity.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
Posterior segment changes:
o Unilateral decreased vision + ocular or periorbital pain + after images + amaurosis fugax + dilated non-
tortuous retinal veins + narrow retinal arterioles + mid-peripheral retinal haemorrhages, and
microaneurysms + cotton wool spots, disc and macular oedema + cobblestone degeneration + iris/retina
or disc neovascularization
o The retinopathy may be confused with non-ischaemic CRVO and diabetic retinopathy.
o A swollen disc is typical of CRVO but not OIS. Diabetic retinopathy is usually bilateral and symmetric
with haemorrhages and microaneurysms located throughout the fundus, whereas the haemorrhages are
mid peripheral in carotid occlusive disease.
o Marked asymmetry in a patient with diabetic retinopathy should suggest ipsilateral carotid artery
disease or CRVO.
o Central retinal artery occlusion may occur.
Anterior segment changes:
Corneal oedema + mild anterior uveitis +/- glaucoma/iris atrophy or cataract, dilated episcleral veins, mid
dilated and poorly reactive pupil, cataract, neovascularisation of the iris and development of secondary
glaucoma
Chronic ocular ischaemia:
Chronic ocular ischaemia has chronic low perfusion pressure resulting in diffuse retinal ischaemia
(manifested as prolonged circulation time), dilation and irregular calibre and tortuosity of retinal veins
Fluorescein angiography:
FA abnormalities found in 67% of cases with carotid occlusion or stenosis
1. Increased retinal arteriovenous transit time
2. Patchy, delayed, irregular choroidal filling, Areas of retinal non perfusion
3. Microaneurysms
4. Venous dilation and beading
5. Diffuse late leakage from retinal vessels
6. Leakage at arterial bifurcations (suggesting emboli damage) and from retinal neovascularisation
Electroretinography:
There is a decrease in both the a and b waves in eyes that are affected by OIS, in contrast to sparing of
the a wave in CRAO. This is related to the choroidal and outer retinal ischaemia of eyes with OIS
Other causes of neovascularization
1. Diabetes
2. Central retinal vein occlusion
3. Aortic arch disease
Aortic arch disease
o Caused by atherosclerosis, syphilis, or Takayasu’s arteritis
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
o Clinical picture is identical to ocular ischaemic syndrome, but is often bilateral.
o Arm and neck pulses are absent + cold hands + spasm of the arm muscles with exercise.
Investigations
1. Exclude vascular risk factors and other causes of stroke by FBC, ESR, U + E's, blood sugar, serum
cholesterol, serology for syphilis, ECG and CXR.
2. Carotid artery ultrasound
3. Ophthalmo-dynamometry (ophthalmic artery pressure is low in carotid disease but is normal to increased
in central retinal vein occlusion)
4. Cardiology consultation
Treatment
1. Control hypertension + diabetes + stop smoking
2. Laser photocoagulation in the presence of neovascularization. Laser photocoagulation is not as effective
at reducing the ischaemic stimulus in this situation compared with diabetic retinopathy. Pan retinal laser
photocoagulation alone causes new vessels at the iris to regress in only 36% of eyes. There is no
scientific rationale for pan retinal laser photocoagulation when the fluorescein angiography shows no
retinal ischaemia in the form of capillary non-perfusion.
3. Carotid end-arterectomy for significant stenosis
Referral of Patients for medical assessment
o In a recent retrospective study of 52 patients with OIS seen over 7 years, it was found that there is a
higher prevalence of certain risk factors for atherosclerosis (such as diabetes and hypertension) than
the control group, and a dramatic difference in mortality.
o The following medical problems are associated with OIS:
1. 73% hypertensive
2. 56% diabetic
3. 48% ischaemic heart disease
4. 27% history of previous CVA
5. Stroke rate of 4% per year
6. 5 year mortality was 40%. Most deaths were cardiac related (63%), 19% stroke, 12% cancer
related.
Role of Carotid end-arterectomy
o The benefit of carotid end-arterectomy in patients with OIS is unknown
o The risk of stroke is low in patients with stenosis less than 30% and does not justify surgery. The
diagnosis of stenosis by angiography itself carries a risk of stroke (from 1-4 %.)
o The European Carotid Surgery Trial (ECST) and North American Symptomatic Carotid Endarterectomy
Trial (NASCET) showed clear decreases in the overall risk of stroke in operated patients with recently
symptomatic (non-disabling severe ischaemic stroke, or retinal infarct) severe (70-99%) carotid
stenosis. Surgery for less stenosis was shown to be harmful.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
o The ECST showed that there was an initial risk following surgery of 7.5% suffering stroke or dying in
the first 30 days. However over the next 3 years the total risk of surgical death, or any stroke was
12.3% for those who had surgery and 21.9% for controls
o The NASCET found 8% of patients who underwent end-arterectomy vs. 18% of patients in the medical
group had suffered a major stroke or death at 2 years, including the operative complication rate of
5.8%.
o The Asymptomatic Carotid Surgery trial shows a highly significant reduction in the 5 year risk of stoke
or perioperative death following surgery. 3120 patients with substantial carotid artery narrowing (70%
or more) but no recent neurological symptoms (stroke or transient ischaemia in the previous 6 months)
were randomized to immediate end-arterectomy or indefinite deferral. The risk of death or stroke
within 30 days of end-arterectomy was 3.1%. Combining perioperative and non perioperative strokes the
5 year risks were 6.4% (immediate end-arterectomy) vs. 11.8% (deferral) for all strokes.
o Another trial (3120 patients) investigated the use of immediate carotid endarterectomy in patients with
unilateral or bilateral carotid artery stenosis (more than or equal to 60%) but no stroke or ischaemia in
the previous 6 months showed that in patients younger than 75 years of age with carotid diameter
reduction about 70% or more on ultrasound immediate carotid endarterectomy halved the net 5-year
stroke risk from about 12% to about 6% (including the 3% perioperative hazard). Half this 5-year
benefit involved disabling or fatal strokes. Note also that the authors stated that outside trials,
inappropriate selection of patients or poor surgery could obviate such benefits
o The National Clinical Guidelines for Stroke provide the following recommendations about carotid
endarterectomy:
1. Any patient with a carotid area stroke and minor or absent disability should be considered for
carotid endarterectomy. Carotid ultrasound should be undertaken on all patients who would be
considered for carotid endarterectomy
2. Carotid endarterectomy should only be undertaken if the stenosis is measured at greater than 70%
3. Patients with a carotid stenosis of less than 70% or who have a totally occluded carotid artery do
not benefit from carotid artery surgery and are best treated medically. Medical treatment for
symptomatic patients includes aspirin and antihypertensive agents and statin.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
Diabetic Retinopathy
Medical Background
Blood glucose concentrations are normally tightly regulated. Fasting values lie between 3.5 and 5.5 mmol/l
and even large carbohydrate loads do not raise the concentration above 8 mmol /l.
The current diagnostic criteria for diagnosing diabetes have been approved by the World Health
Organization, these criteria are:
1. Fasting glucose: more than 7.0 mmol /l and/or a value exceeding 11.1 mmol /l, either at 2 hours during an
oral glucose tolerance test or in a random sample. (126 and 200 mg/dl respectively).
2. Impaired glucose tolerance: fasting glucose less than 7.0 mmol /l and 2-hours oral glucose tolerance test
value between 7.8 and 11.1 mmol /l.
3. Impaired fasting glucose: fasting glucose 6.1 to 6.9 mmol/l (110 to 124 mg/dl).
Types
Diabetes is traditionally classified into type-1 and type-2. Type-1 diabetes (insulin-dependent’ diabetes) is
an autoimmune, predominantly T-cell-mediated process. The autoimmune process leads to destruction of the
β cells of the pancreas. Susceptibility is multi-factorial (genetic factors explain only 30 to 40 % of the
susceptibility). Type 1 diabetes is considerably rarer than type-2, accounting for between 5 and 15 % of all
diabetes Type-2 diabetes accounts for 85 to 90 % of diabetes worldwide. Type-2 diabetes is most
commonly diagnosed in patients over 40 years of age and the incidence rises to a peak at 60 to 65 years.
Type-2 diabetes is due to the combination of insulin resistance and β-cell failure. These two components
vary in importance between different individuals. Many type-2 patients require insulin to control
hyperglycaemia.
Monitoring diabetes
Blood Glucose level: It is recommended that patients should keep blood glucose level between 4 and 10
mmol/litre for most of the time
The haemoglobin A1c (HbA1c) test is a useful long-term measure that tells how well diabetes is controlled.
Glucose sticks to haemoglobin to make glycosylated haemoglobin or HbA1c, the more glucose that sticks to
the RBCs the higher the HbA1c. HbA1c results are expressed as a percentage and not in the mmol /l.
Target HbA1c depends on the patient’s personal circumstances, but it should lie between 6 and 7.5 %. Blood
glucose monitoring shows glucose levels at that moment in time; but HbA1c shows levels over the previous
two to three months. As red blood cells only live for three to four months, there is no point in testing
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
HbA1c more often than twice or three times a year. Research shows that keeping HbA1c under 7 % helps
reduce the risks of some long-term complications of diabetes. Elevated haemoglobin HbA1c levels correlate
strongly with persistent clinically significant macular oedema in patients with type II diabetes. The United
Kingdom Prospective Diabetes Study showed that intensive control of blood glucose (reducing HbA1c to
7.0%) was associated with a decrease in micro-vascular complications in patients with type II diabetes. It
showed that a decrease 0f 0.9 in the HbA1c is associated with a 37% reduction in the micro-vascular
complications.
Blood Fructosamine level: This is simple and cheaper method of monitoring, but the HbA1c is more reliable.
Epidemiology of diabetic retinopathy “DR”
o Diabetic retinopathy is an important cause of visual loss in relatively younger patients. The presence of
severe diabetic retinopathy and poor vision is also considered as a risk factor for the development of
ischaemic heart disease and death.
o The prevalence of diabetic retinopathy in newly diagnosed non-insulin dependant diabetics is estimated
to be 39% in men and 35% in women. In a population based incidence study, of 634 insulin dependant
diabetics, 14 years rate of progression of diabetic retinopathy was estimated to be 86%, regression
17%, and progression to proliferative diabetic retinopathy was 37%. The incidence of macular oedema
was estimated to be 26%.
o Male sex, higher glycosylated haemoglobin, higher diastolic blood pressure, and proteinuria are factors
that may be associated with progression of diabetic retinopathy. A 10 mm Hg or more increase in the
systolic blood pressure is associated with an increased incidence of diabetic retinopathy in younger
onset diabetic patients. Reduction of hyperglycaemia and blood pressure may be associated with a
decrease in the progression of diabetic retinopathy to proliferative diabetic retinopathy.
o Recent epidemiologic and clinical trial data have shown an association of hyperglycemia and hypertension
with retinopathy in people with diabetes. Data from the ARIC study have also shown that plasma lipids
are associated with the presence of hard exudates and that carotid artery intima-media wall thickness
is associated with retinopathy. The study showed that serum glucose, systolic blood pressure, and type
of diabetes medications taken, and severity of retinopathy was associated with carotid artery intima-
media wall thickness. It also showed that severity of diabetic retinopathy was not associated with
coronary artery disease or stroke history. Controlling for age, gender, duration of diabetes, serum
glucose, and type of diabetes medications taken, the presence of retinal hard exudates was associated
with plasma low-density lipoprotein cholesterol
o The presence of gross proteinuria is associated with increased risk of developing macular oedema. The
risk of proliferative diabetic retinopathy in patients with gross proteinuria is also higher than in
patients without proteinuria. Micro-albuminuria (between 0.03 and 0.29 g/l) is also associated with
greater risk of developing retinopathy in diabetic patients and also with the presence of proliferative
diabetic retinopathy in younger onset patients.
Basic Science
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
o Hyperglycaemia, retinal blood flow, retinal capillary occlusion and non-perfusion, growth factors,
hormonal factors, and dietary factors play important role in the pathogenesis of the disease. High
concentrations of glucose can stimulate the transcription of genes coding for growth factors which may
influence the glucose regulatory mechanisms of the retina, and consecutively, affect progression of
diabetic retinopathy. Retinal blood flow and oxygen consumption appear to be increased during periods
of acute hyperglycaemia. It has been suggested that increased retinal blood flow, and increased ocular
perfusion pressure may play a role in the development of diabetic retinopathy and also a role in the
progression of the disease to proliferative diabetic retinopathy in the younger onset groups.
o Retinal capillary occlusion and non-perfusion is a common feature of diabetic retinopathy.
Haemodynamics factors, increased blood viscosity and decreased red blood cells deformability are
believed to be important factors in causing capillary occlusion and retinal non-perfusion. Both increased
and decreased blood flow have been described. In a recent study it was found that pulsatile choroidal
blood flow, but not the retinal blood flow, increases with the progression of diabetic retinopathy.
o Micro-displacement of the RBC cell membrane indicates the deformability of the cells, which is directly
related to its ability to pass through small retinal blood vessels and retinal capillaries. The RBC cell
membrane micro-displacement is reduced in eyes with advanced diabetic retinopathy. This indicates that
the RBC’s are unable to pass through small vessels causing capillary occlusion and areas of retinal non-
perfusion.
o Renin is a major vaso-active agent that is thought to play an important role in diabetic retinopathy.
There are evidences that there is an intraocular Renin-Angiotensin system independent of that in the
circulation. Vitreous levels of pro-renin in diabetic patients are higher than that in non-diabetic patients
suggesting an activation of the Renin Angiotensin system in diabetics. Intraocular synthesis of
angiotensin II may be involved in the blood supply and also in the pathogenesis of vascular processes e.g.
neovascularisation in diabetic retinopathy. Serum total renin concentration is elevated in patients with
active diabetic retinopathy, irrespective of the renal and the autonomic system functions. Diabetic
retinopathy appears to be the most important determinant of serum renin in patients with insulin
dependent diabetes. It is possible that serum total renin concentration could be used as a marker for
activity in diabetic retinopathy in patients with insulin dependent diabetes.
o Growth factors are likely to be involved in the pathogenesis of Proliferative diabetic retinopathy.
Vascular endothelial growth factor (VEGF) is a glycoprotein that is secreted by the endothelial cells and
pericytes in the retinal blood vessels. It plays an important role in the regulation of angiogenesis in the
developing eye and also in many pathological conditions (e.g. diabetic retinopathy, central retinal vein
occlusion, choroidal neovascular membrane, ROP, corneal neovascularisation and wound healing, and iris
neovascularisation). Vascular endothelial growth factor is also believed to be the most likely factor
responsible for the development of diabetic retinopathy, and proliferative diabetic retinopathy. Hypoxia
increases VEGF levels in the retina, and vitreous. The vitreous levels of vascular endothelial growth
factors are significantly higher in patient with proliferative diabetic retinopathy than in eyes without
proliferative diabetic retinopathy. Systemic hyperoxia can lower retinal VEGF gene expression and re-
oxygenate ischaemic retina. Other growth factors (e.g. Insulin-like growth factor 1 and fibroblast
growth factor), and chemical mediators, (e.g. Interleukin 8, and interferon-induced protein) are present
in the vitreous in eyes with active proliferative diabetic retinopathy more than controls, and may also
play an important part in the pathogenesis of the disease. It has been shown that the thiazolidinediones
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
inhibit experimental retinal neovascularisation with an effect that is primarily downstream of VEGF
expression.
o Capillary non-perfusion occurs in diabetic retinopathy and other ischaemic diseases associated with
over-expression of VEGF. Vascular lumen narrowing caused by endothelial cell hypertrophy occurs in the
deep retinal capillary plexus in VEGF-induced retinopathy in monkeys. This suggests a causal role of
endothelial cell hypertrophy in the pathogenesis of VEGF-induced retinal capillary closure. A similar
mechanism may operate in retinal conditions in humans associated with ischaemia and VEGF over-
expression. VEGF-induced endothelial cell hypertrophy may be causative for capillary closure in these
diseases.
o Vitreous levels of interleukin-6 and vascular endothelial growth factor are related to diabetic macular
oedema. The levels of both IL-6 and VEGF were found to be elevated in the vitreous fluid of subjects
with diabetic macular oedema. IL-6 and VEGF may promote an increase of vascular permeability in
macular oedema subjects without posterior vitreous detachment.
o High levels of serum Laminin (a glycoprotein) have been reported in patients with proliferative diabetic
retinopathy. It is thought that a substantial amount of this chemical is secreted by the retinal
basement membrane. Laminin levels reflect changes in the basement membrane in diabetic retinopathy.
It has also been proposed that Laminin may be considered as an indicator for diabetic retinopathy. It is
not however an early indicator of the disease. It should be mentioned that this chemical may be reduced
after pan-retinal laser photocoagulation.
o Diabetic retinopathy rarely occurs before puberty suggesting that sex hormones may play a role in its
pathogenesis. The blood retinal barrier appears to remain stable until puberty and then progressively
declines afterwards. There seems to be an association between puberty, decline of the blood retinal
barrier and the development of diabetic retinopathy. Increased androgen activity may also be
associated with progression of retinopathy in male subjects with type 1 diabetes.
o The effects of dietary factors on diabetic retinopathy are not completely known. In one study of 387
patients with type 2 diabetes, antioxidants nutrients (vitamin C, E and beta-carotene) had no protective
effects on diabetic retinopathy. It also appears that these nutrients may be associated with worsening
of the diabetic retinopathy in some patients depending on their insulin use.
Old Classification of Diabetic Retinopathy
Stage Features What to do?
Background Microaneurysms + blot retinal haemorrhage + hard exudates + retinal No treatment needed
oedema
Pre- As above + cotton wool spots + IRMA + venous dilatation or beading + No treatment + close follow
proliferative arteriolar narrowing + large dark retinal haemorrhages (retinal up
infarcts)
Proliferative As above + disc new vessels or peripheral new vessels + vitreous Pan retinal photocoagulation
haemorrhage
Focal Macular thickening + hard exudates + focal fluorescein leakage Focal laser photocoagulation
(exudative) when vision is better than
macular 6/60 to save vision
oedema
Diffuse Extensive macular oedema and thickening + little exudates + micro- Grid laser photocoagulation
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
(cystic) cystic spaces + diffuse fluorescein leakage with flower-petal (less satisfactory than the
macular appearance focal type) + control of the
oedema blood pressure and blood
sugar level.
Ischaemic Microaneurysms + haemorrhages + little exudates + mild thickening + No treatment + close follow
maculopathy capillary non-perfusion by fluorescein angiography. up for proliferative changes.
Advanced 1. Persistent vitreous haemorrhage Vitrectomy +/- retinal
disease 2. Retinal detachment (tangential, anterior-posterior traction, or detachment repair
bridging traction detachment)
3. Opaque membrane formation
4. Neovascular glaucoma
Definition of Clinically Significant Diabetic Macular Oedema
Clinically significant macular oedema may be present with any of the previous stages. Grid laser treatment
is indicated in the following conditions:
1. Retinal thickening within 500 micron (one third of disc diameter) of the macular centre (the fovea).
2. Hard exudate within 500 micron of the centre of the macula (if associated with thickening).
3. Retinal thickening greater than one disc diameter if part of it is within one disc diameter of the centre
of the macula.
Clinically Significant Macular Oedema
Any retinal thickening within 500 micron of the fovea (left), or any hard exudate within 500 micron of the
fovea when associated with adjacent retinal thickening (middle), or retinal thickening larger than 1 disc
diameter, part of it is within one disc diameter of the fovea (right).
(Notice that 500 micron is one third of a disc diameter)
New Classification of Diabetic Retinopathy
A. Non-proliferative diabetic retinopathy
Mild:
o Micro-aneurysms
o Intra-retinal haemorrhages in fewer than 4 quadrants
o Hard exudates
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
o Macular oedema
o Abnormal foveal avascular zone
o Needs follow up.
Moderate to severe:
o Cotton wool spots
o Intra-retinal haemorrhages in 4 quadrants
o Venous beading
o IRMA
o Needs follow up closely.
Severe:
Any two of the following:
o Severe intra-retinal haemorrhage in 4 quadrants
o Venous beading in 2 quadrants
o Moderately severe IRMA
o Needs follow up very closely.
B. Proliferative diabetic retinopathy
o Neovascularisation of the disc, the retina, the iris or the anterior chamber angle
o Pre-retinal or vitreous haemorrhage
o Tractional retinal detachment
o Needs pan retinal laser photocoagulation
Another new Classification based on the Severity of Diabetic Retinopathy
A recent report suggested the following classification system for diabetic retinopathy based on the
severity of the retinopathy:
Proposed Disease Severity Level Posterior segment Findings
No apparent retinopathy No abnormalities
Mild non-proliferative Microaneurysms only
diabetic retinopathy
Moderate non-proliferative More than just microaneurysms but less than severe
diabetic retinopathy non-proliferative diabetic retinopathy
Severe non-proliferative diabetic retinopathy Any of the following:
o More than 20 intra-retinal haemorrhages in each
of 4 quadrants
o Definite venous heading in 2 + quadrants
o Prominent intra-retinal micro-vascular
abnormalities in 1 + quadrant
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
And
o No signs of proliferative retinopathy
Proliferative diabetic retinopathy One or more of the following:
o Neovascularisation,
o Vitreous haemorrhage
o Pre-retinal haemorrhage
The same report classified diabetic maculopathy according to severity as follows:
No macular oedema o No apparent retinal thickening or hard exudates in posterior pole.
o Diabetic macular oedema is defined as retinal thickening
o Hard exudates can be sign of current or previous macular oedema.
o Diagnosis requires a three-dimensional assessment that is best performed by a
dilated examination using slit-lamp biomicroscopy and/or stereo fundus
photography.
Mild macular oedema o Some retinal thickening or hard exudates in posterior pole but distant from the
centre of the macula
Moderate macular o Retinal thickening or hard exudates approaching the centre of the macula but not
oedema involving the centre
Severe macular o Retinal thickening or hard exudates involving the centre of the macula
oedema
Clinical Features and Screening
Screening programs
o Screening programs for diabetic retinopathy are proved to be cost effective. Screening reduces the
risk of blindness in diabetic patients by 50%. There is no agreement, however, on the best method of
screening for diabetic retinopathy.
o The performance of a computer vision system in diagnosing early retinal lesions is comparable with that
of human experts. Therefore, a mobile, electronically easily accessible and non-invasive computer system
could become a mass screening tool and a clinical aid in diagnosing early lesions of diabetic retinopathy.
Statistical measures indicate excellent agreement between an eye specialist and the computer system.
o Retinal micro-vascular abnormalities are fairly common in elderly population without diabetes. The
retinal abnormalities are related to hypertension and may be associated with stroke and carotid artery
disease.
o Tritan colour vision contrast sensitivity may be a useful sign in screening for diabetic sight threatening
diabetic retinopathy before actual visual loss. Tritan colour deficiency is observed in patients with sight
threatening retinopathy before actual visual loos.
Progression
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
o A new study determined whether a 1-step or more or 2-step or more progression on the Early
Treatment Diabetic Retinopathy Study retinopathy severity scale over a 4-year period is meaningful in
predicting the subsequent incidence of proliferative diabetic retinopathy and clinically significant
macular oedema over the following 6 years. It seems that 1 or more steps of progression of retinopathy
over a 4-year period strongly predict the development of PDR over the next 6 years. There is also an
association between retinopathy progression and incidence of clinically significant macular oedema.
Therefore, using these end points of progression would result in the need for fewer subjects or shorter
follow-up in some clinical trials.
o Pulse rate may be a clinical indicator of overall risk of diabetic retinopathy, but is not independently
associated with the condition. People with higher pulse rates are more likely to have 4 year progression
of retinopathy, progression to proliferative retinopathy, and incident macular oedema than those with
lower pulse rates. However, these associations are weaker after controlling for blood pressure,
glycosylated haemoglobin, and other risk factors.
Macular oedema
o Diabetic maculopathy seems to be associated with the duration of the disease, diabetic nephrology, and
diabetic neuropathy and also with atherosclerotic vascular changes. Diabetic macular oedema is seen in
both type I and II diabetes mellitus and is the most common cause of visual loss in the latter. Macular
oedema is estimated to develop in 20.1 % of the younger onset diabetics, 25.4% in the older onset
patient taking insulin, and 13.9% in non-insulin patient over a 10 years period. Macular oedema and hard
exudates are common in African Americans with type 1 diabetes, particularly in patients with evidence
of renal disease.
o Macular oedema can be divided into two subtypes focal and diffuse.
1. Focal macular oedema refers to localized areas of retinal thickening caused primarily by focal
leakage from microaneurysms, dilated retinal capillaries, and less commonly from intra-retinal micro
vascular abnormalities. Complete or partial rings of hard exudates often demarcate it. Clusters of
microaneurysms are seen in the centre of circinate exudates. Fluorescein angiography demonstrates
both their presence and their abnormal permeability. Infrequently a fibrous plaque may develop
beneath the macula, resulted from fibrous metaplasia of the retinal pigment epithelium stimulated
by the subretinal exudates.
2. In diffuse macular oedema there is generalized leakage from dilated capillaries. Occlusion of a
considerable portion of the capillary bed leads to widening of the inter-capillary spaces and
compensatory dilation of the patent capillaries that tend to leak diffusely and cause oedema. Diffuse
macular oedema is usually symmetric in both eves and without significant exudation. Systemic and
ocular risk factors associated with diffuse macular oedema are cardiovascular or renal disease,
severe systemic hypertension, adult-onset diabetes mellitus, increasing number of retinal
microaneurysms, advanced retinopathy and vitreomacular traction
o Vitreous abnormalities and vitreomacular adhesion may play a role in the pathogenesis of diabetic
macular oedema in some eyes. Eyes with diabetic retinopathy are more likely to develop macular oedema
if the posterior hyaloid membrane is attached to the macula. Vitreomacular separation either
spontaneously or by vitrectomy may result in reduced macular oedema and improved visual acuity after
laser photocoagulation.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
o Retinal thickness analyser, scanning laser ophthalmoscope and optical coherence tomography are new
tools that may be used in the diagnosis and evaluation of treatment of macular and retinal thickness in
diabetic patients. Optical coherence tomography seems to be less sensitive than the retinal thickness
analyzer in detecting localized increases in retinal thickness in the initial stages of diabetic retinal
disease. Optical coherence tomography studies show three patterns of structural changes in diabetic
macular oedema; a sponge-like retinal swelling (88%), cystoid macular oedema (47%), or serous retinal
detachment (15%). Visual acuity with best correction moderately correlated with retinal thickness
regardless of the different tomographic features.
o Fundus perimetry with scanning laser ophthalmoscope allows the creation of exact maps of retinal
dysfunction. It may help in making management decisions in diabetic and non-diabetic patients by
offering a sensitive parameter in addition to visual acuity. Retinal Thickness Analyser gives quantitative
and objective measurement of the retinal thickness. The technique is based on angular delivery of a
narrow green helium laser beam to the retina and detection of the intersection of the beam with the
retinal structures. Evaluation of the macula by the scanning laser ophthalmoscope is also accurate,
reliable and reproducible.
Proliferative diabetic retinopathy
o Proliferative diabetic retinopathy is often associated with poorer visual prognosis, due to recurrent
vitreous haemorrhage and also due to the higher incidence of thrombotic glaucoma. Spontaneous
regression of new vessels in proliferative diabetic retinopathy may rarely occur. Spontaneous regression
does not seem to be related to any improvement in the diabetic control, but it seems to be associated
with improvement in the blood-retinal barrier.
o Iris new vessels occasionally develop in the anterior chamber angle before the pupil margin. Screening
gonioscopy is valuable and important for the early detection of iris neovascularisation. Rubeosis iridis
may develop rapidly in eyes with non-proliferative diabetic retinopathy in patients with insulin dependant
diabetes or non-insulin dependant diabetes after ECCE with posterior camber IOL despite good diabetes
control.
Differential diagnosis of retinal neovascularization
Diabetes o Tends to have a more posterior retinal location + dot/blot haemorrhages + increased blood
sugar.
Retinal vein o Flame shaped haemorrhage + sclerosed vessels.
occlusion
Sarcoidosis o May produce peripheral sea-fan neovascularization in young black individuals + granulomatous
uveitis + vitritis with vitreous opacities + sheathing of retinal veins.
Sickle-Cell o Tortuosity of retinal veins + black mid-peripheral fundus lesions (black sunbursts) + intra-
Disease retinal and sub-retinal haemorrhage (salmon patch) + refractile (iridescent) intra-retinal
deposits + angioid streaks + comma-shaped capillaries of the conjunctiva (especially along the
inferior fornix).
o Peripheral retinal neovascularization in a fan (sea-fan sign) + sclerosed peripheral retinal
vessels + abnormal dull grey peripheral fundus background colour (caused by peripheral
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
arteriolar occlusions and ischaemia).
o Vitreous haemorrhage and traction bands + retinal detachment + central retinal artery
occlusion + macular arteriolar occlusions may develop.
o Patients often have painful crises with severe abdominal or musculoskeletal discomfort.
Patients are of African or Mediterranean extraction in most cases.
o Haemoglobin electrophoresis may help in the diagnosis
Ocular o Decreased vision + pain +/- amaurosis + after image + dilated non-tortuous veins + retinal
ischaemic haemorrhages + corneal oedema + mild iritis + cataract.
syndrome o Carotid artery or ophthalmic artery stenosis + low ophthalmic artery pressure by ophthalmo-
dynamometry.
o If bilateral consider aortic arch disease (caused by atherosclerosis, syphilis, or Takayasu’s
arteritis)
Talc History of intravenous drug abuse+ Refractile talc particles in the macular arterioles.
retinopathy
Idiopathic See elsewhere in the book for more details
juxta-foveolar
retinal
telangiectasis
Eales' disease o Eales’ disease occurs in young healthy adult males, initially presenting as retinal
periphlebitis and later as retinal ischaemia that may lead to vascular alterations and
neovascularization. Recurrent vitreous haemorrhage with or without retinal
detachment is the common sequelae.
o Its aetiology appears to be multi-factorial. In recent years, immunological, molecular
biological, and biochemical studies have indicated the role of human leukocyte antigen,
retinal autoimmunity, mycobacterium tuberculosis genome, and free radical mediated
damage in the pathogenesis of this disease.
o The management depends on the stage of the disease and consists of medical
treatment with oral corticosteroids in the active inflammatory stage and laser
photocoagulation in the advanced retinal ischaemia and neovascularization stages. The
results of vitreoretinal surgery have been found to be satisfactory in case of vitreous
haemorrhage with or without retinal detachment.
o A diagnosis of exclusion.
Diabetic papillopathy
Diabetic papillopathy is a syndrome of a relatively benign optic disc swelling that occurs not only in young
diabetics, but also in older patients with type 2 diabetes. Affected eyes often have macular oedema and
retinal vascular changes that commonly affect the final visual outcome. Small physiological cup may
represent an anatomical predisposition to this condition. The condition may be associated with rapid
progression of the diabetic retinopathy and the development of disc neovascularisation. Patients with
diabetic papillopathy should be monitored closely.
Diabetic ophthalmoplegia
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
Diabetic ophthalmoplegia most commonly involves the 3rd and 6th cranial nerves, with relative sparing of the
4th. Simultaneous multiple cranial nerves involvement occurs in 2.6% of cases, and consecutive involvement
occur in 3.9% of cases. Type II diabetics with ocular motor palsy have significantly less diabetic
retinopathy than controls. This may imply a different pathophysiological mechanism for these two micro-
vascular complications of diabetes.
Others
o The autonomic pupillary changes in type I and II diabetic patients without clinical evidence of diabetic
autonomic neuropathy were compared with age matched controls. Dark adapted pupil size is significantly
smaller in diabetic patients than controls. Except for type I diabetics with disease for less than 5 years,
most patients have significantly greater constriction in pupil size in response to dilute pilocarpine than
controls. Denervation hypersensitivity to diluted pilocarpine results from damage to the pupillary
parasympathetic supply of diabetic patients. This occurs before the pupillary sympathetic pathway is
affected, it can be detected early in the disease, and it may be a possible explanation for the small pupil
size seen in diabetic patients. Additionally, pupillary autonomic dysfunction occurs before cardiovascular
autonomic changes and detection of pupil denervation hypersensitivity to dilute pilocarpine is an
inexpensive way to detect early DAN.
o Patients with diabetes, with or without diabetic retinopathy, may suffer from visual loss, loss of
contrast sensitivity, and abnormalities in colour perception (tritan-like defect). Visual pathway
dysfunction may also occur in the absence of obvious diabetic retinopathy or hyperglycaemia. The
mechanism underlying this abnormality is unknown. The visual loss may be caused by reversible changes
in retinal function at the ganglion cell layer. Reduced retinal oxygenation seems to be contributing
factor.
Diabetic retinopathy in pregnancy
o There is a significant decrease in the retinal venous diameter and blood flow in diabetic pregnant women.
This fall in retinal blood flow may exacerbate retinal ischaemia and hypoxia and thus may be associated
with the progression of diabetic retinopathy.
o Pregnant women with moderate to severe retinopathy at conception are at greater risk of retinopathy
progression. Retinopathy progression is increased in patients with poor diabetic control and higher
systolic blood pressure.
o Women with diabetic retinopathy should have their diabetes and blood pressure well controlled when
they consider conception.
o In those patients with moderate background retinopathy, fundus examination should be performed at
each obstetric visit and if progression is detected the patient should be examined at 2 week intervals to
detect any high risk characteristics. If high risk characteristics develop photocoagulation should be
carried out.
Treatment
The following three tables summarise the conclusions of major diabetic retinopathy trials:
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
o Eyes with proliferative diabetic retinopathy and with high risk factors have a 35% risk of severe visual
loss after 2 years. These eyes have a 60% reduction of severe visual loss over a 2 years period after
laser photocoagulation treatment. Laser photocoagulation should strongly be recommended for those
patients.
o Eyes with proliferative diabetic retinopathy and without high risk factors have a 10% risk of severe
visual loss after 2 years, and a 60% reduction in the risk after laser photocoagulation. Laser
photocoagulation in this group of patients is recommended; alternatively close follow up should be
undertaken.
o Eyes with severe non-proliferative diabetic retinopathy have a 4 % risk of severe visual loss in 2 years.
Laser photocoagulation or close follow up should be recommended.
High risk factors
1. Disc new vessels or new vessels within 1 disc diameter from the disc
2. Vitreous or pre-retinal haemorrhage
3. Severe new vessels
o In eyes with severe active proliferative diabetic retinopathy with moderate or no vitreous haemorrhage,
vitrectomy may be used as a part of the treatment options. When complete laser photocoagulation fails
to control the proliferative process vitrectomy and removal of the fibrous membrane is a reasonable
option. Scatter laser photocoagulation before vitrectomy should be carried out.
o Eyes with traction retinal detachment not involving the fovea do not need surgery until the fovea is
involved in the detachment area.
o Focal laser photocoagulation is recommended for eyes with clinically significant macular oedema with or
without proliferative diabetic retinopathy.
o Intensive insulin treatment results in a significant reduction of the incidence and progression of
retinopathy; and also in the need for laser photocoagulation for macular oedema or for proliferative
diabetic retinopathy. However, intensive treatment may result in initial worsening in some eyes
o There is no benefit from aspirin is preventing progression of either cataract or diabetic retinopathy.
Aspirin use does not appear to be associated with any ocular side effects in patients with diabetic
retinopathy.
Protein kinase C inhibitors “PKC inhibitor”
The enzyme protein kinase C stimulates the formation of vascular endothelial growth factor and may be
essential for its action. Inhibition of this enzyme may be a promising way to treat diabetic retinopathy. By
interfering with the above biochemical pathways, protein kinase c inhibitors may retard or prevent the
development and progression of diabetic retinopathy. Because members of the PKC family are found
throughout the body, a generalized inhibitor is likely to be toxic. However, an inhibitor specific for PKC
beta may act effectively within the retina and have a favourable toxicity profile.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
Blood sugar control
Poor glycaemic control seems to be a cause of clinically significant macular oedema. The risk of developing
clinically significant macular oedema, in patients with type 1 diabetes, increases with poorer blood glycaemic
control. Some patients show progression of their diabetic retinopathy shortly after establishing a strict
diabetic control, which may be due to the increase in blood flow of the retinal circulation, or to an increase
in serum insulin-like growth factor. Metabolic control in the elderly diabetic patients with established
diabetic retinopathy should be instituted gradually. Insulin appears to have a more marked effect on the
choroidal blood flow more than on the retinal flow. Increased level of insulin significantly increase choroidal
blood flow and mean blood flow velocity in the ophthalmic artery, but not the retinal blood flow.
Hypertension
o Hypertension is now established as a major risk factor for the development and the progression of
diabetic retinopathy. Increased retinal capillary perfusion is a major part in the pathogenesis of
diabetic retinopathy. Factors that increases the retinal perfusion (e.g. hypertension, hyperglycaemia,
and pregnancy), may worsen the retinopathy, while other factors that decreases it, (e.g. carotid stenosis
and increased IOP), may protect the retina. Tight control on the blood pressure (less than 150/85) has
been shown to reduce the risk of developing complications in diabetic retinopathy in type 2 disease.
o In the UK prospective diabetic study, a 10 mm Hg reduction in systolic and a 5 mm Hg reduction in the
diastolic blood pressure was associated with a 47% fall in the risk of doubling the visual angle in 9 years.
The UK prospective diabetic study also showed that reducing the pressure is the main factor, no matter
what medications are used in achieving that. Anti-hypertension drugs, mainly the ACE inhibitor group,
have a primary role in reducing retinal capillary leak and hypo-perfusion. Reducing the blood pressure
also appears to be associated with further benefits to the cardiovascular system and the kidneys. The
evidence that tight blood pressure control is beneficial in type 1 diabetes is not as strong as in type 2
disease. The target blood pressure for patient with diabetic retinopathy is systolic and diastolic blood
pressure equal or less than 130/80.
o Recently, the UK Prospective Diabetes Study Group found that high blood pressure in patients with
type 2 diabetes mellitus is detrimental to each aspect of diabetic retinopathy. A tight BP control policy
reduces the risk of clinical complications from diabetic eye disease. The study found that By 4.5 year
after randomization, there was a highly significant difference in microaneurysms count with 23.3% in the
tight BP control group and 33.5% in the less tight BP control group. Hard exudates increased from a
prevalence of 11.2% to 18.3% at 7.5 years after randomization with fewer lesions found in the tight BP
control group. Additionally, patients allocated to tight BP control were less likely to undergo
photocoagulation treatment for the maculopathy.
o Pentoxifylline is a methyl xanthine derivative that has been used in the treatment of vascular
insufficiency diseases because of its ability to improve the blood flow. Oral administration of
Pentoxifylline in healthy volunteers produces a significant improvement in the retinal capillary blood flow
velocity and viscosity, and may be useful in the treatment of diabetic retinopathy, and other vascular
eye diseases.
Serum lipid
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
Elevated serum lipid levels in patients with diabetic retinopathy seem to be associated with increased risk
of having retinal hard exudate. Lowering serum lipids may be associated with decreased risk of hard
exudate development and visual loss. The association of lipid lowering agents with improvement of diabetic
retinopathy, on the other hand, is not known. Some recent reports indicate that lowering serum lipids and
cholesterol does not seem to affect the progression of retinopathy.
Laser photocoagulation
BACKGROUND
Photocoagulation is the most common laser-tissue interaction that is used in ophthalmic surgery. In this
technique ocular chromophores like haemoglobin, melanin and xanthophyll absorb the light energy and
convert the energy into heat causing denaturation and coagulation of the tissue proteins. The most
commonly used laser of this type is the argon laser used in the treatment of diabetic retinopathy.
Comparison of the common contact lenses used in retinal laser photocoagulation
Main uses Image Spot Field of view
magnification on (degrees)
the retina
Goldman Posterior pole and the periphery Virtual and 1.08 (i.e. 1.08 36
erect times the size of
the laser spot on
the laser
setting)
Mainster There are three types of lenses, Real and Depend on the Depends on the
the High, the standard and the inverted type of the lens lens (75, 90,
ultra-field. They can be used for 140)
macula, equator and the
periphery
Panfundoscopic The equator and the periphery Real and 1.41 120
inverted
Volk There are different types of Real and Depends on the Depends on the
lenses. Can be used for the inverted type of the lens lens (70, 82, 122,
macula, equator or the periphery 130, 160)
Laser photocoagulation for diabetic macular oedema
o Laser photocoagulation is the main method of treatment of clinically significant diabetic macular
oedema. It is not exactly known how laser photocoagulation works in reducing macular oedema. Reduction
in macular oedema may result from post-laser vasoconstriction, which occur secondary to the improved
retinal oxygenation caused by the laser treatment. Pre-treatment fluorescein angiography may improve
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
the accuracy of laser treatment. Quantitative retinal thickness measurements provide an objective
method of assessing and monitoring laser treatment in macula oedema.
o Krypton, argon, and micro-pulsed diode lasers can be used in the treatment of diabetic macula oedema.
The main advantage of krypton red over argon blue-green laser in diabetic retinopathy is the better
penetration of the red light through red blood or yellow lens nuclear sclerosis. Diode laser has the
advantage of being compact, portable, and easy to connect the main electrical supply and easier to cool
than Argon laser.
o Retinal laser photocoagulation is often carried out under topical anaesthesia. Occasionally peribulbar
injection may be needed in extensive or very peripheral treatment. The use of topical sodium diclofenac
0.1% eye drops may help in relieving pain during the treatment.
o Posterior sub-Tenon’s capsule application of Triamcinolone may improve early visual outcome in diffuse
diabetic macular oedema when combined with laser photocoagulation. The injection may be associated
with ptosis and orbital fat prolapse.
Technique of Laser Photocoagulation for macular oedema
In focal oedema (left) use 100 micron laser spots of 0.05-0.1 second duration to leaking spots and
microaneurysms as determined by Fluorescein angiography
In diffuse oedema (right) use 100 micron laser spots of 0.1 seconds placed up to the edge of the fovea
avascular zone
Laser power is titrated to give light grey retinal burns
Proliferative diabetic retinopathy
Proven benefit of laser photocoagulation in proliferative retinopathy
o Untreated eyes with severe disc new vessels have 40% risk of severe visual loss within 2 years. Treated
eyes have half this risk.
o Eyes with mild peripheral new vessels, with no vitreous haemorrhage, have 7% risk of severe visual loss
in 2 years. Treatment could be indicated, if the fellow eye is severely affected by the disease, or close
follow up might be enough if the fellow eye is mildly affected.
o Total detachment of the vitreous provides some protection against the progression of retinal or disc
new vessels.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
o Pregnancy may have a worsening effect on diabetic retinopathy. Laser photocoagulation may be needed
during pregnancy if the retinopathy worsens.
o Diabetic patients with proliferative diabetic retinopathy should be treated aggressively with pan-
retinal photocoagulation or cryotherapy or both. The mechanism of action is not completely understood.
It has been suggested that pan-retinal photocoagulation is associated with a local increase in the retinal
and the pre-retinal oxygen tension, in the treated areas, which causes vasoconstriction of the new
vessels. Pan-retinal photocoagulation is also thought to be associated by vascular narrowing which might
lead to the regression of the new vessels.
o Laser pulse of very short duration seems to affect the retinal pigment epithelium mainly with no or
little damage to the neuro-sensory retina or the choriocapillaris due to the reduced thermal effect
produced by this type of laser. The Iris Ocullight Micro-Pulse 810 nm diode laser is a new laser that has
the advantage of greater retinal pigment epithelium specificity and less damage to the inner retinal
layers. Visual field, and colour vision loss appear to be reduced with this type of laser treatment. Recent
studies showed that this laser is useful in the treatment of macular oedema in patients with diabetic
retinopathy and vascular retinal occlusive diseases.
o Regression of the proliferative diabetic retinopathy is known to occur in about 93% of all treated
patients. Regression appears to be significantly related to the cumulative total number of laser burns
applied to the retina. Renal disease and age (<50 years) are risk factors for non-regression of
retinopathy after pan retinal photocoagulation. Patients with diabetic nephropathy require considerably
more aggressive treatment than patients with no nephropathy. Hypertension, neuropathy, duration of
disease and insulin dependence seem to have no significant effect on outcome.
o Signs of regression after laser photocoagulation include:
1. Regression of the disc and retinal new vessels
2. Decrease in the venous dilatation
3. Decrease in the venous beading
4. Resolution of retinal haemorrhages
5. Improvement in the disc pallor
o Poor prognostic factors after pan retinal photocoagulation include the presence of disc
neovascularisation at base line, short interval between the diagnosis of diabetes and the need for pan
retinal photocoagulation, and earlier onset of diabetes. Patient with good visual acuity at presentation
seem to maintain a good visual acuity after one year, while patients with poor visual acuity at onset seem
to have poor visual outcome. Vitreous haemorrhage, traction retinal detachment may still occur after
pan retinal photocoagulation. Pan retinal laser photocoagulation may be associated with loss of the visual
field of vision.
o In eyes with PDR and normal vision, biweekly laser photocoagulation allows faster recovery of macular
thickness compared with weekly treatment.
o Several laser photocoagulation techniques have been described for the treatment of PDR. The following
diagrams demonstrate two of the commonly used techniques. In the first technique (left), laser is
applied firstly in the nasal quadrant, followed by the lower, upper and superior quadrants (about 500
shots for every quadrant, 200-500 micron with 0.1 to 0.05 second duration). The temporal quadrant is
left till last to avoid macular oedema. In the second technique (right), the posterior pole is treated
first, starting with the lower half of the retina (green) to avoid future difficulties in case there is
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
vitreous haemorrhage, followed by the nasal, upper and temporal quadrants. After finishing treatment
of the posterior pole, the retinal periphery is treated (dark blue).
Pre-macular haemorrhage
Pre-macular haemorrhage is common in patients with proliferative diabetic retinopathy. Most of these
haemorrhages occur in association with partial posterior vitreous detachment. The haemorrhages are often
slow to clear and may result in epimacular membrane or macular traction retinal detachment. Division of the
posterior cortical face by the YAG laser has been used to release the pre-retinal haemorrhage into the
vitreous to achieve rapid intravitreal drainage of the haemorrhage. Laser application allows the trapped
blood to enter the vitreous where it quickly gets absorbed. Complete intravitreal dispersion of the blood
can be achieved in most eyes within one week. The technique can be used instead of vitrectomy to allow an
early identification and treatment of any existing significant macular oedema.
Vitrectomy for the treatment of diabetic macular oedema
o Several studies have established the efficacy of laser in the management of patients with diabetic
macular oedema. However, visual improvement with laser only occurs in about 3% of patients with 25%
of patients losing two or more lines of acuity over a three year period despite laser treatment,
especially with diffuse rather than focal leakage. Laser treatment has to be repeated in approximately
one in three patients and has complications, such as visual field loss and choroidal neovascularisation. A
posterior vitreous detachment has been shown to be associated with both a lower prevalence and
increased rate of spontaneous resolution of diabetic macular oedema. These observations suggest that
the posterior vitreous might influence the course of diabetic macular oedema and provide a basis upon
which to consider the role of vitrectomy as a potential treatment modality in these patients. However; it
must be realized that the current position regarding the efficacy of vitrectomy for diabetic macular
oedema is very hard to conclude because there have not been randomized controlled studies.
o It has been suggested that there are four groups of patients with diabetic macular oedema in whom
there is some evidence regarding the role of vitrectomy:
1. Patients with clinically identifiable vitreoretinal traction: These patients have tractional retinal
detachment or clinically evident retinal striae. Most vitreoretinal surgeons agree that cystoid
macular oedema is prevalent when patients undergo vitrectomy for tractional complications such as
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
tractional detachment or vitreous haemorrhage. The oedema in such patients however tends to
resolve within a few months of surgery and macular laser is rarely required postoperatively.
2. Patients with a taut thickened posterior hyaloid: A taut thickened posterior hyaloid is a clinical
diagnosis based on the detection of an exaggerated pre-macular hyaloid reflex. This is usually due to
an increased glistening of the posterior hyaloid face, but the membrane is said to be occasionally
thick enough to preclude laser. The typical fluorescein appearance in these patients is a deep diffuse
late leak with prominent cystoid oedema. It has been hypothesized that a partial vitreous
detachment inducing focal vitreoretinal traction may be important in the aetiology of this condition.
The literature suggests that vitrectomy may be effective in this group with resolution of oedema in
61 % and improvement in acuity by two lines or more in 75%.
3. Patients with no evidence of a PVD but no TTPH: The commonest group. The results of
vitrectomy in this group of patients are encouraging in that surgery achieves a 45% improvement in
acuity by two or more Snellen lines. However, the rate of resolution of oedema is highly variable at
between 0% and 100% and in some series the oedema was found to recur. OCT studies showed
evidence of partial vitreomacular separation and signs of traction in approximately 10% of patients
with chronic diffuse diabetic macular oedema and no evidence of a taut or thickened posterior
hyaloid.
4. Eyes with a well defined PVD: There may be a modest benefit from vitrectomy.
Intravitreal triamcinolone for macular oedema
o Intravitreal 4 mg triamcinolone injection is a promising therapeutic method for diabetic macular oedema
that fails to respond to conventional laser photocoagulation. Treatment is followed by decrease in the
macular thickness and increase in the visual acuity. Complications may include rise in the IOP,
endophthalmitis or progression of cataract. They do not appear to be prohibitive.
o Acute postoperative endophthalmitis following intravitreal injection of triamcinolone can occur rapidly
(between 1–15 days) and may result in severe loss of vision.
o Pseudo-endophthalmitis after an intravitreal injection of triamcinolone acetonide is a distinct clinical
entity that may resolve without specific treatment. The condition is characterised by a dense vitreous
haze with severe reduction of fundus view; with no periorbital inflammation or pain. The condition seems
to be self limited. It may be appropriate to closely observe non-infectious, toxic endophthalmitis in
patients treated with intravitreal triamcinolone before assuming it to be infectious, especially in the
absence of eye pain.
Vitrectomy for proliferative diabetic retinopathy
o Pars plana vitrectomy for proliferative diabetic retinopathy may be followed by vitreous haemorrhage.
Fibro-vascular in-growth at the sclerotomy sites appears to be a common cause of recurrent vitreous
haemorrhage after diabetic vitrectomy. Careful examination to detect these in-growths is important.
After pars plana diabetic vitrectomy ultrasound bio-microscopy is a useful tool in detecting fibro-
vascular in-growth at the sclerotomy sites.
o Intraoperative fluorescein angiography may be useful in disclosing unusual findings in the extreme
peripheral retina and pars plana which might lead to vitreous haemorrhage. The technique may aid
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
intraoperative evaluation and treatment of proliferative diabetic retinopathy. In eyes with persistent
vitreous haemorrhage, peripheral retinal cryotherapy stabilises the peripheral retina and vitreous and
also of the visual acuity in most patients. Trans-scleral cryotherapy is often possible even in eyes with
opaque media.
o A retrospective study reviewed the photographs of the maculae of 30 diabetic patients who had
undergone vitrectomy for proliferative diabetic vitreoretinopathy, with the aim of studying the
changes in diabetic maculopathy following surgery. The study showed a reduction in haemorrhages,
exudates and micro-aneurysms, and reduction in fluorescein leakage. In contrast, however, the foveal
avascular zone and extent of peri-foveolar ischaemia was increased. It is difficult therefore to know
whether vitrectomy is beneficial or otherwise; however, it was associated with changes in the macula.
o Intra and postoperative vitreous haemorrhage is a common problem after vitrectomy for proliferative
diabetic retinopathy occurring in about 17-30% of cases. A new study showed that in pseudophakic eyes
laser peripheral capsulotomy is safe and effective in treating post-vitrectomy haemorrhage.
Cataract Surgery in diabetic retinopathy
o Senile cataract is commoner in diabetic patients. Diabetic patients are also more likely to develop
cataract at an early age. Cataract surgery in patients with diabetic retinopathy is often associated with
good visual results, especially if the retinopathy is well controlled by laser photocoagulation before hand.
Patients with severe non-proliferative diabetic retinopathy or more advanced retinopathy have poor
results.
o A recent study showed that phacoemulsification surgery may be associated with a better visual acuity
and less postoperative inflammation than ECCE. The visual results and rate of retinopathy progression
after phacoemulsification surgery does not seem to differ significantly from those reported with other
techniques. The main causes of poor results after surgery are macular oedema or proliferative diabetic
retinopathy. It is thought that clinically significant macular oedema found at the time of surgery is
unlikely to resolve spontaneously and laser treatment should be carried out without delay. Macular
oedema appearing after surgery may however regress spontaneously, and conservative treatment may be
taken.
o A recent study looked at the effect of cataract surgery on the progression of diabetic retinopathy. In
75 patients the operated eyes were prospectively compared with the un-operated fellow eyes. Thirty
per cent of patients had progression of retinopathy, with statistically significantly more progression in
the operated than in the fellow un-operated eye. However, the authors were unable to find a significant
difference between patients with and without progression in terms of age, diabetes duration, surgical
method or hypertension. Pre-operative macular oedema and poor renal function were associated with
progression which is not strange. In another prospective study of 50 type-2 diabetics undergoing
uncomplicated phacoemulsification cataract surgery and in whom the other un-operated eye was used as
a control to compare the progression of retinopathy. There was no significant difference in progression
of retinopathy or maculopathy between the operated and fellow eyes. Some patients developed a
transient macular oedema, which had a benign course. Although the authors of the paper conclude that
uncomplicated cataract surgery does not cause acceleration of diabetic retinopathy, the relatively small
numbers of patients in this study may have given it insufficient power to detect the change of
progression in cataract eyes and non-operated eyes.
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
o Postoperative corneal oedema may also be a significant problem after cataract surgery in diabetic eyes.
Compared with non-diabetic eyes, eyes of patients with diabetes show more damage in corneal
endothelial cells due to cataract surgery and a delay in the postoperative recovery of corneal oedema
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
Age Related Maculopathy
Age related maculopathy is the leading cause of legal blindness among older people in the Western
countries. Blind and partially sighted registration rates, in the UK, because of cataract, glaucoma and optic
atrophy have decreased during the past 50 years. However, the incidence of registration due to age related
maculopathy seems to be increasing in the order of 30-40%. 26% of eyes with age related macular
degeneration (with unilateral extra-foveal choroidal neovascular membrane) develop choroidal neovascular
membrane in the fellow eyes 5 years after presentation and are associated with poor visual acuity at the
end of the 5 years period. In patients with a unilateral visual loss, the risk of visual loss in the second eye is
between 7-10%. Significant risk factors for the development of exudative or non-exudative lesions include
the degree of confluence of drusen within 1600 micron of the centre of the fovea, focal hyper-
pigmentation, slow choroidal filling, and focal extra foveal areas of atrophy of the retina pigment
epithelium.
Pathogenesis and Risk Factors
o The pathogenesis of age related maculopathy is not completely known. Some of the risk factors that
have been associated with age related maculopathy include:
Drusen
Hyperopia
High body mass index in men
Decreased stromal iris pigmentation
Serum high density lipoprotein
Alcohol (beer) consumption
Tobacco smoking
o Alcohol consumption (with the exception of beer), does not seem to be a risk factor for the incidence of
age related maculopathy. Beer consumption, especially in men, appears to be associated with a slightly
higher incidence of age related maculopathy and soft drusen development.
o Tobacco smoking also seems to have adverse effect on age related maculopathy. Previous smokers
appear to remain at higher risk. Combined data from racially similar communities across three continents
provided strong and consistent evidence that tobacco smoking is the principal known preventable
exposure associated with any form of age related maculopathy. A slower recovery from glare and more
extensive fundus changes in the affected eye also appear to be risk factors for the fellow eyes
involvement. A slower foveal ERG implicit time may also be an indicator of early stage choroidal
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
neovascular membrane development because of outer retina ischaemia. Recent data indicate that
smoking is related to an increased risk of the incident of AMD. Current smokers are at higher risk of
incident AMD than both past smokers and those who never smoked AMD (odds ratios relative to non
smokers: 2.83 and relative to past smokers: 2.80).
o Exposure to sunlight may be associated with the development of early ARM. Leisure time spent outdoors
while persons are teenagers (aged 13-19 years) and in their 30s (aged 30-39 years) appears to be
significantly associated with the risk of early ARM. There is non significant, protective effect
associated with use of hats and sunglasses while persons are teenagers and in their 30s. Additionally,
people with red or blond hair are slightly more likely to develop early ARM than people with darker hair.
o In a study of 4757 patients with age related maculopathy it was found that patients with intermediate
drusen are more likely to be women and to have arthritis but less likely to have angina. Patients with
large drusen are more likely to have arthritis. Neovascular disease was more likely in patients with
hypertension, hyperopia, and cataract. White race, geographic atrophy, and smoking were associated
with all three types of lesions and with the most severe and frequent lesions.
o Significantly higher malondialdehyde and lower Nitrous Oxide levels have been detected in plasma of
patients with age related maculopathy compared with controls. The results may support involvement of
oxidative damage and vascular theory in the pathogenesis of the disease as part of the ageing process
o A new study showed that pulsatile ocular blood flow in eyes with drusen was lower than their fellow
eyes with choroidal neovascular membrane, but higher than their fellow eyes with disciform scar. This
finding suggests that haemodynamics differences between fellow eyes in individuals are relevant to the
development of choroidal neovascular membrane and the formation of disciform scar.
o Recent data suggests that there might be an association between vascular endothelial growth factor,
hemorheologic factors, haemostasis, endothelial dysfunction, and age related maculopathy.
o Rod-mediated kinetic parameters of dark adaptation tests which reflect the rods function may be
abnormal in the early stages of the disease. This may prove useful in early diagnosis of the disease.
o There is intra-individual symmetry in eyes with bilateral geographic atrophy in the presence of a wide
range of inter-individual variability. Identical patterns of fundus auto-fluorescence are observed in 80%
of patients. The findings of intra-individual symmetry are in accordance with the view that age-related
macular degeneration is not merely the result of a non-specific ageing process. Symmetric
manifestations, rather, reflect specific individual determinants in the pathogenesis and manifestation of
the disease.
o Chlamydia pneumoniae is now emerging as possible risk factor for the development of cardiovascular
diseases. The hallmark of this disease is chronic inflammation. There is also an association between anti-
Chlamydia pneumoniae serum antibodies and the development of age related macular degeneration
indicating that this organism might play a role in the pathogenesis of age related macular degeneration
through mediating some of the pathological retinal and vascular changes associated with the disease.
o Chronic infection with cytomegalovirus may be a risk factor for the progression from dry to neovascular
AMD. A new experimental study showed that there is a significant association of high cytomegalovirus
IgG titre with neovascular AMD compared with dry AMD and control patients. The study also showed
that there is no major difference in the distribution of titres for Chlamydia pneumoniae IgG and
Helicobacter pylori IgG in wet and dry AMD patients.
Causes “Theories” of Age Related Macular Degeneration
The Really Current Ophthalmology. Magdy A Nofal. www.medicalebooks.co.uk. magdynofal@hotmail.co.uk
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Robbins Pathology Chapter 13 - White Blood CellsDocument7 pagesRobbins Pathology Chapter 13 - White Blood Cellsscorpiosphinx7980% (5)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Natural Herbs For Waldenstrom's MacroglobulinemiaDocument2 pagesNatural Herbs For Waldenstrom's MacroglobulinemiaJohn SmithPas encore d'évaluation
- MCQ MRCP Haematology-OncologyDocument149 pagesMCQ MRCP Haematology-OncologyHashim Ahmad100% (2)
- Birds Are Interesting Flying AnimalsDocument1 pageBirds Are Interesting Flying AnimalsNurul WijayantiPas encore d'évaluation
- Geriatric Nutrition UMMDocument33 pagesGeriatric Nutrition UMMNurul WijayantiPas encore d'évaluation
- Birds Are Interesting Flying AnimalsDocument1 pageBirds Are Interesting Flying AnimalsNurul WijayantiPas encore d'évaluation
- Derm CaseDocument6 pagesDerm CaseNurul WijayantiPas encore d'évaluation
- Scalp PDFDocument5 pagesScalp PDFNurul Hildayanti ILyasPas encore d'évaluation
- NMSC Kidney StonesDocument29 pagesNMSC Kidney StonesEdi KurniadiPas encore d'évaluation
- WHO 2015 - Mal TX Guidelines - 9789241549127 - Eng PDFDocument318 pagesWHO 2015 - Mal TX Guidelines - 9789241549127 - Eng PDFDody ChandraPas encore d'évaluation
- Jurnal Efek Dexametason Pada Anestesi SpinalDocument6 pagesJurnal Efek Dexametason Pada Anestesi SpinalNurul WijayantiPas encore d'évaluation
- Neutrophil Accumulation After Traumatic Brain Injury in RatsDocument8 pagesNeutrophil Accumulation After Traumatic Brain Injury in RatsNurul WijayantiPas encore d'évaluation
- Tyfoid PDFDocument121 pagesTyfoid PDFNurul WijayantiPas encore d'évaluation
- Medical ParasitologyDocument320 pagesMedical Parasitologymedtech_22m88% (26)
- Scalp PDFDocument5 pagesScalp PDFNurul Hildayanti ILyasPas encore d'évaluation
- Diaphragmatic HerniaDocument9 pagesDiaphragmatic HerniaFatimaPas encore d'évaluation
- History Taking and Clinical ExaminationDocument129 pagesHistory Taking and Clinical ExaminationYen ChouPas encore d'évaluation
- Immunoelectrophoresis (IEP), Serum Protein Electrophoresis (SPE) & Immunofixation (IFX)Document42 pagesImmunoelectrophoresis (IEP), Serum Protein Electrophoresis (SPE) & Immunofixation (IFX)kiedd_04100% (5)
- Monoclonal Gammopathy of Renal Significance: Review ArticleDocument11 pagesMonoclonal Gammopathy of Renal Significance: Review ArticleNoel Saúl Argüello SánchezPas encore d'évaluation
- Malignant LymphomaDocument3 pagesMalignant LymphomaKakaa KakaPas encore d'évaluation
- Plasma Cell Dyscrasias: Miten R. Patel, MD Cancer Specialists of North FloridaDocument41 pagesPlasma Cell Dyscrasias: Miten R. Patel, MD Cancer Specialists of North FloridaDr MonikaPas encore d'évaluation
- Waldenstrom MacroglobulinemiaDocument11 pagesWaldenstrom MacroglobulinemiaMr. LPas encore d'évaluation
- Bence Jones Protein-UrineDocument16 pagesBence Jones Protein-UrineDrashua Ashua100% (2)
- Quiz Hematology Oncology Part 2 of 2Document60 pagesQuiz Hematology Oncology Part 2 of 2MedShare100% (5)
- Sjogren's Syndrome, Vasculitis, and Cryoglobulinaemia Associated With (Kappa) Paraprotein With Rheumatoid ActivityDocument3 pagesSjogren's Syndrome, Vasculitis, and Cryoglobulinaemia Associated With (Kappa) Paraprotein With Rheumatoid ActivityGordana PuzovicPas encore d'évaluation
- Waldenstroms Macroglobulinemia (WM) FinalDocument57 pagesWaldenstroms Macroglobulinemia (WM) FinalnishPas encore d'évaluation
- Diagnosis of Monoclonal Gammopathy of RenalDocument14 pagesDiagnosis of Monoclonal Gammopathy of RenalConnie Alva GutierrezPas encore d'évaluation
- 1757 1626 1 333Document5 pages1757 1626 1 333Ade CandraPas encore d'évaluation
- ImmunofixationDocument36 pagesImmunofixationAstrianti Kusuma Wardani100% (1)
- Lecture 10 - Plasma Proteins - 18 Sep 2006Document34 pagesLecture 10 - Plasma Proteins - 18 Sep 2006api-3703352100% (3)
- Recognition of Monoclonal Proteins - UpToDateDocument33 pagesRecognition of Monoclonal Proteins - UpToDateEduardo Romero StéfaniPas encore d'évaluation
- Walden Strom SDocument60 pagesWalden Strom SsigitPas encore d'évaluation
- Poster ROICAM 2018Document1 pagePoster ROICAM 2018ibrahimPas encore d'évaluation
- Xavier Leleu 2012Document10 pagesXavier Leleu 2012monday125Pas encore d'évaluation
- Pathology 2 TND LiveDocument38 pagesPathology 2 TND Livepavan kumarPas encore d'évaluation
- Myeloma 2009 Nov 9Document59 pagesMyeloma 2009 Nov 9Hula HulahulagPas encore d'évaluation
- Tehreem - Recalls MODIFIED BY Me & AARAVDocument58 pagesTehreem - Recalls MODIFIED BY Me & AARAVRohini SelvarajahPas encore d'évaluation
- Hematology CLL, ММ tableDocument4 pagesHematology CLL, ММ tableShur .EPas encore d'évaluation
- GP Letter Example PV-ESRDocument6 pagesGP Letter Example PV-ESRRyan ChenPas encore d'évaluation
- Cold Agglutinin DiseaseDocument8 pagesCold Agglutinin Diseasehtunnm@gmail.comPas encore d'évaluation
- Monoclonal GammopathiesDocument70 pagesMonoclonal GammopathiesElisa Lincă100% (1)
- POEMS SyndromeDocument13 pagesPOEMS SyndromeFernando Suarez ChumaceroPas encore d'évaluation
- Cracking D' Boards Study & Review Center, Inc. Patho SecretsDocument10 pagesCracking D' Boards Study & Review Center, Inc. Patho SecretsKathryn KleinPas encore d'évaluation
- Plasma Cell DyscrasiasDocument6 pagesPlasma Cell DyscrasiasharideepPas encore d'évaluation