Académique Documents
Professionnel Documents
Culture Documents
Maternal Infectious Diseases, Antimicrobial Therapy or Immunizations: Very Few Contraindications To Breastfeeding
Transféré par
Valdis SuryanTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Maternal Infectious Diseases, Antimicrobial Therapy or Immunizations: Very Few Contraindications To Breastfeeding
Transféré par
Valdis SuryanDroits d'auteur :
Formats disponibles
PIDnote_Oct.
qxd 10/16/2006 3:23 PM Page 270
PAEDIATRIC INFECTIOUS DISEASE NOTES
Maternal infectious diseases, antimicrobial
therapy or immunizations: Very few
contraindications to breastfeeding
he Canadian Paediatric Society recommends exclusive breastfeeding, provided the mother is not contagious or she
T breastfeeding as the optimal method of infant feeding
for the first six months of life for healthy, term infants (1).
has received two weeks of appropriate TB treatment (7-9).
Continuing breastfeeding while on TB therapy is not a
There are many benefits associated with breastfeeding, problem, as these drugs appear to be safe for use with breast-
including nutritional, immunological, psychological, devel- feeding (8,10,11). Breastfed neonates of women on isoni-
opmental, environmental, social, economic and health (eg,
azid therapy should receive a multivitamin supplement,
decrease in infectious diseases) (2-4). To promote, protect
and support breastfeeding, every effort must be made to including pyridoxine (12). If both mother and infant are
minimize contraindications to breastfeeding, particularly taking isoniazid, then there are concerns about possible
unnecessary ones. The present article summarizes the excessive drug concentration in the infant (12).
maternal infectious diseases in which continuing breast- Consultation with an expert is indicated.
feeding is recommended, the very few infectious diseases in With parasitic infections such as malaria, breastfeeding
which it is not recommended, the rare instances in which should be continued provided the mother’s clinical condi-
maternal antimicrobial therapy indicates a caution for tion allows for it. While the antimalarials chloroquine,
breastfeeding, and the continuation of breastfeeding when a hydroxychloroquine and quinine are found in variable
mother or her infant is receiving a routine recommended quantities in breast milk, all three are regarded as compat-
immunization. ible with breastfeeding (10) unless the infant has glucose-
6-phosphate dehydrogenase (G6PD) deficiency, in which
MATERNAL INFECTIOUS DISEASES case withdrawal of quinine is advised (11). Similarly, pri-
AND BREASTFEEDING maquine should not be used unless both the mother and
Human breast milk is not sterile; it frequently contains infant have normal G6PD levels. Precautions to minimize
organisms found in the mother’s microbial skin flora (5). insect-borne infections should be encouraged. Insect
Normal healthy breastfeeding infants become colonized repellents help to reduce mosquito bites, which may trans-
with their mother’s flora over time (6). While breast milk mit malaria or viruses such as West Nile. There are no
can be a source of maternally derived commensal and path- reported adverse events following use of repellents con-
ogenic microorganisms, there are very few maternal infec- taining diethyltoluamide or picaridin in breastfeeding
tious diseases for which cessation or interruption of mothers (13).
breastfeeding is indicated (2,7-9). While maternal fungal infections such as candidal
When a nursing mother presents with symptoms of an vaginitis can lead to infant colonization, this is not a con-
infectious disease, she has already exposed her infant to the traindication to breastfeeding, nor is maternal treatment
pathogen. Cessation of breastfeeding does not prevent with topical or systemic antifungal agents such as
exposure, and may instead decrease the infant’s protection fluconazole (8,11).
that comes through specific maternal antibodies and other For most maternal viral infections, ongoing breastfeed-
protective factors found in human milk. Therefore, com- ing is recommended with few exceptions (Table 1) (7,8).
mon maternal bacterial, fungal and viral infections in With maternal HIV infection, in resource-rich settings
which the mother’s health is not compromised are not con- such as Canada, where a safe and culturally accepted
traindications to breastfeeding (Table 1). replacement is available, breastfeeding is not recommended
Maternal bacterial infections are rarely complicated by because HIV transmission to the infant has been well doc-
transmission to the infant through breastfeeding. Mothers umented (8,9,14-16). Emotional support for the mother to
with mastitis or breast abscesses should be encouraged to not breastfeed may be required; in some instances, finan-
continue breastfeeding (5,7,9). In instances of breast cial support for formula purchase may be necessary as well.
abscess where pain interferes with breastfeeding, the infant In more resource-limited settings, the optimal feeding
can continue to breastfeed on the nonabscessed breast. method for infants whose mothers are HIV positive is still
Similarly, maternal tuberculosis (TB) is compatible with unclear (16). Breastfeeding is also not advised for mothers
Department of Paediatrics, IWK Health Centre, Halifax, Nova Scotia
Correspondence: Dr Noni E MacDonald, IWK Health Centre, 5850/5980 University Avenue, PO Box 9700, Halifax, Nova Scotia B3K 6R8.
Telephone 902-470-8799, fax 902-470-7232, e-mail noni.macdonald@dal.ca
270 Can J Infect Dis Med Microbiol Vol 17 No 5 September/October 2006
PIDnote_Oct.qxd 10/16/2006 3:23 PM Page 271
PID Notes
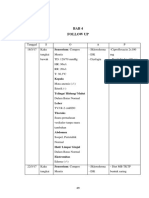
TABLE 1
Selected maternal infections and corresponding breastfeeding management for healthy term infants
Maternal infection/disease Microbial agent(s) Breastfeeding recommendation
Bacteria
Mastitis and breast abscesses Staphylococcus aureus Continue breastfeeding unless there is obvious pus, in which
Streptococcus species case pump and discard from the infected breast and continue
Gram negatives: Escherichia coli breastfeeding with the other breast
Rarely: Salmonella species,
mycobacteria, candida, Cryptococcus
TB Mycobacterium tuberculosis Main route of transmission is airborne. With active TB, delay
breastfeeding until mother has received 2 weeks of
appropriate anti-TB therapy; provide TB prophylaxis for infant
Urinary tract infection Gram negatives: E coli, etc Continue breastfeeding
Bacterial infection abdominal wall Skin microbes Continue breastfeeding
postcesarean section
Diarrhea Salmonella, Shigella, E coli, Campylobacter Continue breastfeeding; good hand hygiene
Other bacterial infections in which Wide range of bacterial microbes Continue breastfeeding
the mother’s physical condition and
general health is not compromised
Parasites
Malaria Plasmodium species Continue breastfeeding
Fungi
Candidal vaginitis Candida Continue breastfeeding; good hand hygiene
Viruses
Cytomegalovirus Continue breastfeeding
Hepatitis Hepatitis A virus Continue breastfeeding; immunoglobulin prophylaxis for the
infant; good hand hygiene
HBV Continue breastfeeding; routine prevention of infant HBV
infection with HBIG at birth; immunization with HBV vaccine
Hepatitis C virus Continue breastfeeding
Herpes HSV-1, HSV-2 Continue breastfeeding; good hand hygiene. If there are lesions
on breasts, interrupt until lesions are healed (crusted)
Chicken pox, shingles Varicella Continue breastfeeding; for perinatal VZV, give VZIG;
for postpartum, consider VZIG
Enterovirus Continue breastfeeding; good hand hygiene
HIV Contraindicated; see text for details
HTLV-1, HTLV-2 Contraindicated
Parvovirus Continue breastfeeding
West Nile virus Continue breastfeeding
Data from references 7 to 9 and 12 to 15. HBIG Hepatitis B immune globulin; HBV Hepatitis B virus; HSV Herpes simplex virus; HTLV Human T-lymphotropic virus;
TB Tuberculosis; VZIG Varicella-zoster immune globulin; VZV Varicella-zoster virus
with human T-lymphotropic virus type 1 or 2 infection. MATERNAL ANTIMICROBIAL THERAPY
(7,8). In mothers with latent cytomegalovirus (CMV) AND BREASTFEEDING
infection, the virus reactivates in breast milk during the There are very few instances in which maternal therapy with
postpartum period and can be transmitted to the infant commonly used antimicrobial agents precludes continuation
with breastfeeding (9). This does not pose a risk to the of breastfeeding (8,10,11) (Table 2). Even maternal therapy
term infant because serious disease is prevented by placen- with tetracycline, aminoglycosides or quinolones is not an
tally transferred maternal antibody. For premature infants, indication to withhold breastfeeding.
especially those less than 32 weeks gestation, breastfeed-
ing from a CMV-positive mother is controversial. MATERNAL IMMUNIZATION AND
However, recent studies suggest that that the relative inci- BREASTFEEDING
dence and severity of CMV disease in such premature Breastfeeding is not a contraindication to the administration of
infants are low, and that the rate of CMV acquisition is routine recommended vaccines to the infant or the mother (20).
not much different from the rate of acquisition in prema-
ture infants fed CMV-negative breast milk (17,18), pro- ACKNOWLEDGEMENT: This document was reviewed by the
Canadian Paediatric Society Drug Therapy and Hazardous
viding further support for fresh breast milk feeding even if
Substances Committee.
the mother is CMV positive (19).
Can J Infect Dis Med Microbiol Vol 17 No 5 September/October 2006 271
PIDnote_Oct.qxd 10/16/2006 3:23 PM Page 272
PID Notes
TABLE 2
Selected maternal antimicrobial therapies and corresponding breastfeeding management for healthy term infants
Maternal antimicrobial therapy Breastfeeding recommendation
Antibiotics
Group 1: Penicillins, cephalosporins, carbapenams, macrolides, Continue breastfeeding
aminoglycosides, quinolones
Group 2: High-dose metronidazole Discontinue breastfeeding for 12 h to 24 h to allow excretion of dose
Group 3: Chloramphenicol Caution: Possible idiosyncratic bone marrow suppression
Group 4: Trimethoprim/sulfamethoxazole, sulfisoxazole, dapsone Proceed with caution if nursing infant has jaundice or G6PD deficiency, and also if
ill, stressed or premature
Antitubercular drugs
Isoniazid, rifampin, streptomycin, ethambutol Continue breastfeeding. While mother is taking isoniazid, administer pyridoxine for
the nursing infant
Antiparasitics
Group 1: Chloroquine, quinidine, ivermectin; Continue breastfeeding
maternal topical diethyltoluamide or picaridin
Group 2: Primaquine, quinine Contraindicated during breastfeeding unless both mother and baby have normal
G6PD levels
Antifungals
Fluconazole, ketoconazole Continue breastfeeding
Antivirals
Acyclovir, valacyclovir, amantadine Continue breastfeeding. If considering prolonged use of amantadine,
observe for milk suppression, as it can suppress prolactin production
Data from references 8,10,11 and 13. G6PD Glucose-6-phosphate dehydrogenase
REFERENCES
1. Canadian Paediatric Society, Nutrition Committee. [Principal author: 12. American Academy of Pediatrics. Perinatal Infections. In: Gilstrap LC,
Margaret Boland] Exclusive breastfeeding should continue to six Oh W, eds. Guidelines for Perinatal Care, 5th edn. Illinois: American
months. Paediatr Child Health 2005;10:148. Academy of Pediatrics, 2002:285-329.
2. Gartner LM, Morton J, Lawrence RA, et al; American Academy of 13. Centers for Diseases Control and Prevention. Updated Information
Pediatrics Section on Breastfeeding. Breastfeeding and the use of human regarding Insect Repellents <www.cdc.gov/ncidod/dvbid/westnile/
milk. Pediatrics 2005;115:496-506. RepellentUpdates.htm> and West Nile Virus, Pregnancy and
3. Ogundele MO. A viewpoint of mucosal immunity in relation to early Breastfeeding <www.cdc.gov/ncidod/dvbid/westnile/qa/
feeding method. Intern J Food Sci Tech 2001;36:341-55. breastfeeding.htm> (Version current at September 17, 2006).
4. Heinig MJ. Host defense benefits of breastfeeding for the infant. Effect 14. Canadian Paediatric Society, Infectious Diseases and Immunization
of breastfeeding duration and exclusivity. Pediatr Clin North Am Committee. [Principal author: Susan King] Evaluation and treatment of
2001;48:105-23. the human immunodeficiency virus-1-exposed infant. Paediatr Child
5. Michie C, Lockie F, Lynn W. The challenge of mastitis. Arch Dis Child Health 2004;9:409-17.
2003;88:818-21. 15. Read JS; American Academy of Pediatrics, Committee on Pediatric AIDS.
6. Kawada M, Okuzumi K, Hitomi S, Sugishita C. Transmission of Human milk, breastfeeding, and transmission of human immunodeficiency
Staphylococcus aureus between healthy, lactating mothers and their virus type 1 in the United States. Pediatrics 2003;112:1196-2003.
infants by breastfeeding. J Hum Lact 2003;19:411-7. 16. Bulterys M, Fowler MG, Van Rompay KK, Kourtis AP. Prevention of
7. American Academy of Pediatrics. Transmission of infectious agents via mother-to-child transmission of HIV-1 through breast-feeding: Past,
human milk. In: Pickering LK, ed. Red Book: 2003 Report of the present, and future. J Infect Dis 2004;189:2149-53.
Committee on Infectious Diseases, 26th edn. Illinois: American 17. Yasuda A, Kimura H, Hayakawa M, et al. Evaluation of cytomegalovirus
Academy of Pediatrics, 2003:118-21. infections transmitted via breast milk in preterm infants with a real-
8. Lawrence RM, Lawrence RA. Breast milk and infection. Clin Perinatol time polymerase chain reaction assay. Pediatrics 2003;111:1333-6.
2004;31:501-28. 18. Miron D, Brosilow S, Felszer K, et al. Incidence and clinical
9. Lamounier JA, Moulin ZS, Xavier CC. [Recommendations for breastfeeding manifestations of breast milk-acquired Cytomegalovirus infection in low
during maternal infections]. J Pediatr (Rio J) 2004;80(Suppl):S181-8. birth weight infants. J Perinatol 2005;25:299-303.
10. American Academy of Pediatrics, Committee on Drugs. The transfer of 19. Schanler RJ. CMV acquisition in premature infants fed human milk:
drugs and other chemicals into breast milk. Pediatrics 2001;108:776-89. Reason to worry? J Perinatol 2005;25:297-8.
11. Mathew JL. Effect of maternal antibiotics on breast feeding infants. 20. Health Canada, National Advisory Committee on Immunization.
Postgrad Med J 2004;80:196-200. Canadian Immunization Guide, 6th edn. Ottawa: Health Canada, 2002:19.
INFECTIOUS DISEASES AND IMMUNIZATION COMMITTEE
Members: Drs Simon Richard Dobson, BC Children’s Hospital, Vancouver, British Columbia; Joanne Embree, University of Manitoba, Winnipeg, Manitoba (chair); Joanne
Langley, IWK Health Centre, Halifax, Nova Scotia; Dorothy Moore, The Montreal Children’s Hospital, Montreal, Quebec; Gary Pekeles, The Montreal Children’s Hospital,
Montreal, Quebec (board representative); Élisabeth Rousseau-Harsany, Sainte-Justine UHC, Montreal, Quebec (board representative); Lindy Samson, Children’s Hospital of
Eastern Ontario, Ottawa, Ontario
Consultant: Dr Noni MacDonald, Department of Pediatrics, IWK Health Centre, Halifax, Nova Scotia
Liaisons: Drs Upton Allen, The Hospital for Sick Children, Toronto, Ontario (Canadian Pediatric AIDS Research Group); Scott Halperin, IWK Health Centre, Halifax,
Nova Scotia (IMPACT); Monica Naus, BC Centre for Disease Control, Vancouver, British Columbia (Health Canada, National Advisory Committee on Immunization);
Larry Pickering, Centers for Disease Control and Prevention, Atlanta, Georgia, USA (American Academy of Pediatrics, Committee on Infectious Diseases)
Principal author: Dr Noni E MacDonald, IWK Health Centre, Halifax, Nova Scotia
The recommendations in this statement do not indicate an exclusive course of treatment or procedure to be followed. Variations, taking
into account individual circumstances, may be appropriate. Internet addresses are current at time of publication. This article also appears in
the October 2006 issue of Paediatrics & Child Health [Paediatr Child Health 2006;11(8):489-491].
272 Can J Infect Dis Med Microbiol Vol 17 No 5 September/October 2006
Vous aimerez peut-être aussi
- Mat. Infxn & BF'G-ppt. (New)Document18 pagesMat. Infxn & BF'G-ppt. (New)Gayli De Lima BongyadPas encore d'évaluation
- Breast Milk and Vaccinations During A Pandemic: Rationalising The RisksDocument4 pagesBreast Milk and Vaccinations During A Pandemic: Rationalising The RisksAchmad RyandaPas encore d'évaluation
- Infectious Diseases Trans 2K2KDocument15 pagesInfectious Diseases Trans 2K2Kroselo alagasePas encore d'évaluation
- Maternal VaccinationDocument16 pagesMaternal VaccinationAnonymous l6Q1ROq2Pas encore d'évaluation
- Exclusive Breastfeeding Among HIV Exposed Infants From Birth To 14 Weeks of Life in Lira, Northern Uganda: A Prospective Cohort StudyDocument10 pagesExclusive Breastfeeding Among HIV Exposed Infants From Birth To 14 Weeks of Life in Lira, Northern Uganda: A Prospective Cohort StudyAjup SafarudinPas encore d'évaluation
- MCQ ImmunologyDocument79 pagesMCQ Immunologypriya009100% (2)
- Primary Health Care in Paediatric Hiv: Kenya National "Comprehensive Paediatric HIV Care Course". Nascop/Uon/Mu/Knh/GgchDocument82 pagesPrimary Health Care in Paediatric Hiv: Kenya National "Comprehensive Paediatric HIV Care Course". Nascop/Uon/Mu/Knh/GgchAlvin OmondiPas encore d'évaluation
- Lactmed. Drugs and Lactation Database (Lactmed) Since 2006 Till Now. Ncbi. Bethesda (MD) : National Library of Medicine (Us) 2006Document11 pagesLactmed. Drugs and Lactation Database (Lactmed) Since 2006 Till Now. Ncbi. Bethesda (MD) : National Library of Medicine (Us) 2006Anisa Aprilia AdhaPas encore d'évaluation
- Use of Specific Vaccines in Pregnancy: Bacillus Calmette - Gu - Erin (BCG)Document7 pagesUse of Specific Vaccines in Pregnancy: Bacillus Calmette - Gu - Erin (BCG)Saadia JavaidPas encore d'évaluation
- Reaction Paper (RLE)Document2 pagesReaction Paper (RLE)Princess VinluanPas encore d'évaluation
- Vaccines For Pregnant WomenDocument6 pagesVaccines For Pregnant WomenRodney LuceroPas encore d'évaluation
- Abm Clinical Protocol 4 MastitisDocument4 pagesAbm Clinical Protocol 4 MastitisFayrouz EssawiPas encore d'évaluation
- Antiinfective Properties of Human MilkDocument6 pagesAntiinfective Properties of Human Milkkiko arrojasPas encore d'évaluation
- The Vaginal Microbiome, Vaginal Anti-Microbial Defence Mechanisms and The Clinical Challenge of Reducing Infection-Related Preterm BirthDocument6 pagesThe Vaginal Microbiome, Vaginal Anti-Microbial Defence Mechanisms and The Clinical Challenge of Reducing Infection-Related Preterm BirthFelipe MPas encore d'évaluation
- 431 2019 Article 3563Document8 pages431 2019 Article 3563chindiaPas encore d'évaluation
- Questions and Answers On Enterobacter Sakazakii in Powdered Infant FormulaDocument3 pagesQuestions and Answers On Enterobacter Sakazakii in Powdered Infant FormulaDrashua AshuaPas encore d'évaluation
- Expanded Program ImmunizationDocument4 pagesExpanded Program ImmunizationLheiDanielMariellMonteroPas encore d'évaluation
- Vaccine Indication and ContraindicationDocument34 pagesVaccine Indication and ContraindicationMusa yohanaPas encore d'évaluation
- Varicella During Pregnancy: A Case ReportDocument3 pagesVaricella During Pregnancy: A Case ReportCosmin RăileanuPas encore d'évaluation
- Beneficial Effects of Probiotic Bacteria Isolated From Breast MilkDocument5 pagesBeneficial Effects of Probiotic Bacteria Isolated From Breast MilkHuan VuongPas encore d'évaluation
- MainDocument4 pagesMainarini ayukPas encore d'évaluation
- Mang of-HIV FINALDocument24 pagesMang of-HIV FINALemanPas encore d'évaluation
- Breastfeeding COVID 19Document1 pageBreastfeeding COVID 19valentinPas encore d'évaluation
- Breastfeeding Benefit From Mom Gives The Gift of A Lifetime To The Baby For Healthy FutureDocument7 pagesBreastfeeding Benefit From Mom Gives The Gift of A Lifetime To The Baby For Healthy FuturevallikaPas encore d'évaluation
- Breast FeedingDocument6 pagesBreast FeedingphobicmdPas encore d'évaluation
- Rusangu University: Name: Chalwe GivenDocument7 pagesRusangu University: Name: Chalwe Givenbright kaundaPas encore d'évaluation
- Guidance On Breastfeeding During The Covid-19 Pandemic: Review ArticleDocument6 pagesGuidance On Breastfeeding During The Covid-19 Pandemic: Review ArticleandctzgPas encore d'évaluation
- Child Health ProgrammeeDocument63 pagesChild Health ProgrammeeRam PokharelPas encore d'évaluation
- Breastfeeding and Autoimmunity - 2017Document11 pagesBreastfeeding and Autoimmunity - 2017Cláudia SilvaPas encore d'évaluation
- Helena Rabie - Infant Feeding Options For HIV-infected MothersDocument58 pagesHelena Rabie - Infant Feeding Options For HIV-infected Mothersprecious mudzingwaPas encore d'évaluation
- Breast-Feeding and Protection Against Infection: Lars A - HansonDocument3 pagesBreast-Feeding and Protection Against Infection: Lars A - Hansonocean329Pas encore d'évaluation
- Immunizations in PregnancyDocument47 pagesImmunizations in Pregnancymiss_izzniPas encore d'évaluation
- Kinder Impfen ENDocument3 pagesKinder Impfen ENcoleviper95Pas encore d'évaluation
- Kia 2Document19 pagesKia 2Ida ayu Krisna dewiPas encore d'évaluation
- Session 6 Infant Feeding and PMTCTDocument27 pagesSession 6 Infant Feeding and PMTCTMahad CaddePas encore d'évaluation
- Vaccines in PregnancyDocument40 pagesVaccines in Pregnancyboragam.saisharanyaPas encore d'évaluation
- Protecting Breastfeeding During The COVID-19 PandeDocument7 pagesProtecting Breastfeeding During The COVID-19 PandeRintha Aulia ParamithaPas encore d'évaluation
- Jurnal Mastitis 2Document6 pagesJurnal Mastitis 2Faizal DzikrullahPas encore d'évaluation
- Infant and Young Child Feeding: Dr. Malik Shahnawaz AhmedDocument71 pagesInfant and Young Child Feeding: Dr. Malik Shahnawaz AhmedRiyaz AhamedPas encore d'évaluation
- 3 Killers Infections BriefDocument2 pages3 Killers Infections BriefAraz MuhammadaminPas encore d'évaluation
- Early Human Development: Elizabeth Whittaker, Beate KampmannDocument5 pagesEarly Human Development: Elizabeth Whittaker, Beate KampmannTwhiePas encore d'évaluation
- Epi Brochure (Calalang)Document2 pagesEpi Brochure (Calalang)Nickaela CalalangPas encore d'évaluation
- Vaccine Friendly PlanDocument4 pagesVaccine Friendly PlanAna Sampaio89% (9)
- Breastfeeding QuestionsDocument3 pagesBreastfeeding QuestionsAgnimitra ChoudhuryPas encore d'évaluation
- Study Kasus 2 FIXDocument7 pagesStudy Kasus 2 FIXLis DWi MalmuTszPas encore d'évaluation
- Breastfeeding & ImmunizationDocument21 pagesBreastfeeding & ImmunizationShay YonniePas encore d'évaluation
- Immunization Presentation 3Document48 pagesImmunization Presentation 3Patrick ShibambuPas encore d'évaluation
- Sangita Shrestha Manisha Dhungana: Prepared byDocument37 pagesSangita Shrestha Manisha Dhungana: Prepared byBhawna JoshiPas encore d'évaluation
- 5398-Article Text-66016-1-10-20220526Document14 pages5398-Article Text-66016-1-10-20220526Zulaikha NAIMIPas encore d'évaluation
- TB Guideline PregnancyDocument8 pagesTB Guideline PregnancyErum KhanPas encore d'évaluation
- Neonatal InfectionDocument9 pagesNeonatal InfectionnishaPas encore d'évaluation
- Best Practive Clinical 2021Document17 pagesBest Practive Clinical 2021cdsaludPas encore d'évaluation
- 2021 Dawod Et AlDocument10 pages2021 Dawod Et Alpankaj27dataPas encore d'évaluation
- Chicken Pox in Pregnancy - A Challenge To The Obstetrician: Hem Kanta SarmaDocument2 pagesChicken Pox in Pregnancy - A Challenge To The Obstetrician: Hem Kanta SarmaDrDevdatt Laxman PitalePas encore d'évaluation
- Health Maintenance of InfantDocument59 pagesHealth Maintenance of InfantMohamed Na3eemPas encore d'évaluation
- Breastfeeding and HivDocument30 pagesBreastfeeding and HivbxrbxrPas encore d'évaluation
- Prevention of Mother-To-Child Transmission of HIV: Challenges For The Current DecadeDocument7 pagesPrevention of Mother-To-Child Transmission of HIV: Challenges For The Current DecadeHerry SasukePas encore d'évaluation
- Why Is Initial Bacterial Colonization of The IntestineDocument14 pagesWhy Is Initial Bacterial Colonization of The IntestineOlavo BenevenutoPas encore d'évaluation
- Health Advice and Immunizations for TravelersD'EverandHealth Advice and Immunizations for TravelersPas encore d'évaluation
- Old Diseases Are Coming Back:: Courtesy Of Anti-VaccinatorsD'EverandOld Diseases Are Coming Back:: Courtesy Of Anti-VaccinatorsÉvaluation : 1 sur 5 étoiles1/5 (1)
- (Medicuss) Soal To 2 Series Batch 2 2018Document18 pages(Medicuss) Soal To 2 Series Batch 2 2018Valdis SuryanPas encore d'évaluation
- (Medicuss) Soal To 3 Series Batch 2 2018Document17 pages(Medicuss) Soal To 3 Series Batch 2 2018Valdis SuryanPas encore d'évaluation
- (Medicuss) Soal To 1 Series Batch 2 2018Document20 pages(Medicuss) Soal To 1 Series Batch 2 2018Valdis SuryanPas encore d'évaluation
- JadwalDocument2 pagesJadwalValdis SuryanPas encore d'évaluation
- Bab Gizi FullDocument29 pagesBab Gizi FullValdis SuryanPas encore d'évaluation
- Adjustment Disorder - Epidemiology PDFDocument15 pagesAdjustment Disorder - Epidemiology PDFCristina ColoteloPas encore d'évaluation
- Periodontitis and DiabetesDocument17 pagesPeriodontitis and DiabetesValdis SuryanPas encore d'évaluation
- IFDEA Dental Anatomy Educational Teaching ResourceDocument38 pagesIFDEA Dental Anatomy Educational Teaching ResourceaerowongPas encore d'évaluation
- Scleroderma Chapter 4 (Indonesia Language) With The Indonesian Internist AgreementDocument7 pagesScleroderma Chapter 4 (Indonesia Language) With The Indonesian Internist AgreementValdis SuryanPas encore d'évaluation
- Power Point The Anatomy Physiology and Morphology of TeethDocument18 pagesPower Point The Anatomy Physiology and Morphology of TeethValdis SuryanPas encore d'évaluation
- IFDEA Dental Anatomy Educational Teaching ResourceDocument38 pagesIFDEA Dental Anatomy Educational Teaching ResourceaerowongPas encore d'évaluation
- K1 - Histology of Integument System - PPSXDocument47 pagesK1 - Histology of Integument System - PPSXValdis SuryanPas encore d'évaluation
- Breast Diseases BenignDocument34 pagesBreast Diseases BenignAhmad Uzair QureshiPas encore d'évaluation
- Mastitis Treatment Supporting FormulaDocument17 pagesMastitis Treatment Supporting FormulaPavan Kumar P N100% (1)
- Breast Lump History OSCE Guide Breast Cancer Geeky MedicsDocument1 pageBreast Lump History OSCE Guide Breast Cancer Geeky MedicsAnne Julia AgustinPas encore d'évaluation
- Mastitis Group 5Document14 pagesMastitis Group 5Michael Barfi OwusuPas encore d'évaluation
- Postpartum ComplicationsDocument42 pagesPostpartum ComplicationsElvisPas encore d'évaluation
- XII Breast and Nipple ConditionsDocument23 pagesXII Breast and Nipple ConditionsteabagmanPas encore d'évaluation
- Presentation On BreastfeedindDocument58 pagesPresentation On Breastfeedindcharanjit kaurPas encore d'évaluation
- Catatan Perkembangan PersalinanDocument7 pagesCatatan Perkembangan PersalinanLiman WijayaPas encore d'évaluation
- Streptococcus Agalactiae - A Practical Summary For Controlling Mastitis - VirginiaAg DASC-6P (2012)Document2 pagesStreptococcus Agalactiae - A Practical Summary For Controlling Mastitis - VirginiaAg DASC-6P (2012)userPas encore d'évaluation
- Kannaki (BREAST CARE)Document16 pagesKannaki (BREAST CARE)Jalajarani AridassPas encore d'évaluation
- Answer and Rationale MaternityDocument21 pagesAnswer and Rationale MaternityMark ElbenPas encore d'évaluation
- EMREE Q BANK - Edited and Revised Part 1Document101 pagesEMREE Q BANK - Edited and Revised Part 1Sandra Abboud100% (1)
- Engorgement Post Partum: Merry C.ODocument12 pagesEngorgement Post Partum: Merry C.OmerycoPas encore d'évaluation
- Rabbit Diseases: Disease Cause Symptoms Prevention TreatmentDocument3 pagesRabbit Diseases: Disease Cause Symptoms Prevention TreatmentAkinwumiPas encore d'évaluation
- Day 1. Mohd Sami 1Document67 pagesDay 1. Mohd Sami 1Baebee LouPas encore d'évaluation
- Updated NCM 107 Lecture Week 8Document46 pagesUpdated NCM 107 Lecture Week 8Quencee CalaycayPas encore d'évaluation
- Breastfeeding More Than Just Good Nutrition PDFDocument19 pagesBreastfeeding More Than Just Good Nutrition PDFAndini Pramono100% (1)
- Elca/Cspm Final Exam 2007 14 July, 2007Document23 pagesElca/Cspm Final Exam 2007 14 July, 2007Dr Atef Hadedy100% (3)
- INFLAMMATORY Breast CancerDocument20 pagesINFLAMMATORY Breast CancerbencleesePas encore d'évaluation
- A Survey of Mastitis On Dairy FarmsDocument20 pagesA Survey of Mastitis On Dairy FarmsBonnie BucquerouxPas encore d'évaluation
- Journal Homepage: - : Manuscript HistoryDocument5 pagesJournal Homepage: - : Manuscript HistoryIJAR JOURNALPas encore d'évaluation
- Honorhealth Therapeutic Breast MassageDocument1 pageHonorhealth Therapeutic Breast MassageRaja CangkangPas encore d'évaluation
- Group 9 Breast Engorgement BSN 2BDocument24 pagesGroup 9 Breast Engorgement BSN 2BChristine Joy MolinaPas encore d'évaluation
- Benign Breast DisordersDocument42 pagesBenign Breast DisordersBRI KUPas encore d'évaluation
- Aberrations of Normal Development and Involution (ANDI) : A Concept of Benign Breast Disorders Based On PathogenesisDocument16 pagesAberrations of Normal Development and Involution (ANDI) : A Concept of Benign Breast Disorders Based On PathogenesisSebastian PosadaPas encore d'évaluation
- 4 5814470955174463831Document45 pages4 5814470955174463831random personsaPas encore d'évaluation
- Puerperial PyrexiaDocument4 pagesPuerperial Pyrexiakutra3000Pas encore d'évaluation
- Bubbles HeDocument39 pagesBubbles HePerrilyn PereyPas encore d'évaluation
- Nutrition and Child DevelopmentDocument603 pagesNutrition and Child Developmentprinceej88% (32)
- BUBBLEHEBDocument13 pagesBUBBLEHEBJeffrey Viernes100% (1)