Académique Documents
Professionnel Documents
Culture Documents
Biomarker Epilepsi
Transféré par
Fanel PutraTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Biomarker Epilepsi
Transféré par
Fanel PutraDroits d'auteur :
Formats disponibles
Review
Development of epilepsy after ischaemic stroke
Asla Pitkänen, Reina Roivainen, Katarzyna Lukasiuk
For about 30% of patients with epilepsy the cause is unknown. Even in patients with a known risk factor for epilepsy, Lancet Neurol 2015
such as ischaemic stroke, only a subpopulation of patients develops epilepsy. Factors that contribute to the risk for Published Online
epileptogenesis in a given individual generally remain unknown. Studies in the past decade on epilepsy in patients November 16, 2015
http://dx.doi.org/10.1016/
with ischaemic stroke suggest that, in addition to the primary ischaemic injury, existing difficult-to-detect microscale
S1474-4422(15)00248-3
changes in blood vessels and white matter present as epileptogenic pathologies. Injury severity, location and type of
Department of Neurobiology,
pathological changes, genetic factors, and pre-injury and post-injury exposure to non-genetic factors (ie, the exposome) A. I. Virtanen Institute for
can divide patients with ischaemic stroke into different endophenotypes with a variable risk for epileptogenesis. Molecular Sciences, University
These data provide guidance for animal modelling of post-stroke epilepsy, and for laboratory experiments to explore of Eastern Finland, Kuopio,
Finland (Prof A Pitkänen PhD);
with increased specificity the molecular `mechanisms, biomarkers, and treatment targets of post-stroke epilepsy in
Department of Neurology,
different circumstances, with the aim of modifying epileptogenesis after ischaemic stroke in individual patients Hyvinkää Hospital, Hyvinkää,
without compromising recovery. Finland (R Roivainen MD); and
The Nencki Institute of
Experimental Biology, Polish
Introduction arterial dissection.12 Ischaemic stroke can occur at any
Academy of Sciences, Warsaw,
In 2013, The Working Group of the International League time during life, with the greatest risk being during the Poland (K Lukasiuk PhD)
Against Epilepsy revised the terminology related to the first week after birth.13 Study results14,15 have shown that Correspondence to:
term epileptogenesis and provided recommendations although ischaemic stroke is more often associated with Prof Asla Pitkänen, A. I. Virtanen
for doing studies of antiepileptogenic treatments.1 elderly adults, it is not uncommon in young adults (aged Institute, University of Eastern
Finland, PO Box 1627,
Epileptogenesis refers to the development and extension 16–49 years), with an incidence of ten to 11 per
FIN-70 211 Kuopio, Finland
of tissue capable of generating spontaneous seizures, 100 000 people per year. The initiation and location of asla.pitkanen@uef.fi
resulting in the development of an epileptic disorder or epileptogenesis after ischaemic stroke can be accurately
progression after the disorder is established. Thus, the defined, allowing the mechanisms of the acquired
new definition takes into account evidence from epileptogenesis to be assessed at different stages of the
preclinical studies showing that epileptogenic epileptogenic process. Development of novel diagnostic
neurobiological processes can continue even after the methods and instruments will allow stroke to be
appearance of spontaneous recurrent seizures.2 In classified by subtype, cause, and confounding factors
addition to unprovoked seizures, epilepsy is often with improved accuracy and specificity, which will
associated with cognitive and behavioural comorbidities advance the accuracy of data collection and analysis.
that arise from the region of the epileptogenic network.3 Most of the experimental data from studies of post-stroke
Because the epileptogenic process seems to be largely epileptogenesis come from models of ischaemic stroke,
dependent on the underlying cause of epilepsy, which provide a scenario for the translation of preclinical
therapeutic approaches need to be tailored according to data to the clinic.
these causes.4 No antiepileptogenic treatments are Interpretation of the available data on human post-
available at present for patients at risk of epilepsy after stroke epileptogenesis is subject to several caveats,
brain injury, emphasising the need to understand cause- including the definitions of so-called early and late
specific mechanisms that can be targeted to combat seizures, which have been variable. The definitions are,
epileptogenesis in individual patients. however, crucial for data analysis and interpretation
Cerebrovascular diseases underlie about 11% of all because the occurrence of a late seizure is required for
cases of epilepsy5 and are heterogeneous with various diagnosis of PSE. An early seizure refers to a seizure
causes. Some cerebrovascular diseases are progressive, occurring during the first week after stroke—ie, the time
causing a spectrum of primary and secondary pathologies period during which seizures are regarded as acute
that can initiate the evolution of epileptogenic networks. symptomatic seizures that are not suggestive of an
Depending on the underlying cerebrovascular disease, enduring predisposition of the brain to generate epileptic
3% to 30% of patients who have had a stroke develop seizures.16,17 A late seizure occurs more than 1 week after
post-stroke epilepsy (PSE).6–10 the stroke.17 This definition is generally agreed to be
In this Review, we discuss the present understanding arbitrary. Other caveats to the interpretation of clinical
of the epileptogenic process after cerebrovascular post-stroke epileptogenesis studies are listed in the panel
diseases, focusing on arterial ischaemic stroke. Ischaemic and figure 1.
stroke is a common epileptogenic cause, accounting for Our aim is to describe new aspects emerging from
up to 9% of incident cases of epilepsy.11 In adults, the research into clinical and experimental PSE, which we
most common causal categories of ischaemic stroke are expect will affect experimental modelling, the
large artery atherosclerosis, cardiogenic emboli, small development of diagnostics, and the discovery of
vessel disease, and other, a diverse category that includes biomarkers and treatment strategies for post-stroke
inflammatory disease, hypercoagulable states, and epileptogenesis.
www.thelancet.com/neurology Published online November 16, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00248-3 1
Review
A
Epidemiology and clinical course of PSE
B
In adult populations, about 70–85% of cerebrovascular
diseases are ischaemic, and most cases of PSE are due to
arterial ischaemic stroke.18 The cumulative occurrence of
PSE after ischaemic stroke in different studies is
summarised in table 1.
The longest population-based follow-up study by
Graham and colleagues9 revealed that the 10-year estimate
of PSE after total anterior circulation infarct was 28·7%,
C D
partial anterior circulation infarct was 13·4%, and posterior
circulation infarct was 4·8%. After ischaemic stroke, the
greatest risk for the first unprovoked post-stroke seizure
was during the first follow-up year (table 1). In a 5-year
follow-up,20 the mean incremental risk of late seizures after
ischaemic stroke was 1·5% per year after the first year.20
Another study23 reported that the annual event risk of
seizures after the first-ever ischaemic stroke is 6·3% after
1 year, 2·4% after 2 years, 1·3% after 3 years, and 0·3%
thereafter. Registry-based data from a case-control study
also suggested that the risk of unprovoked seizure
incidence remains heightened for 7 years after cerebral
infarction, being highest during the first post-stroke year.11
Data from the past 10 years has drawn attention to the
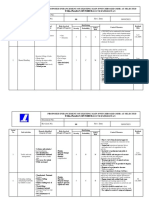
Figure 1: Epileptogenesis or atherogenesis?
(A, B) Magnetic resonance angiography and (C, D) fluid-attenuated inversion recovery MRI taken at 20-month
development of PSE in young adults (table 1).
intervals from a woman with her first ischaemic stroke in the right medial cerebral artery territory at age 54 years Additionally, in the Rochester ischaemic stroke
(A, C; orange arrows). The left side of the brain is shown on the right side of the images. She had a maternal family population, the absolute risk of late seizures after
history of ischaemic stroke, and at the time of the first ischaemic stroke she was treated for hypertension. An ischaemic stroke was similar between patients younger
episode of clonic movements in the left limbs was seen during treatment at hospital. Inter-ictal EEG recorded at
the acute phase was interpreted to show epileptiform focal disturbance. Post-stroke epilepsy was diagnosed and
than 55 years and those older than 75 years.19 The
treatment with oxcarbazepine was initiated. Additionally, she was given aspirin–dipyridamole combination. A year negligible effect of age on the risk of post-stroke
later, a short episode of left-sided numbness re-occurred and the oxcarbazepine dose was increased. 3 months epileptogenesis was also noted in two more recent
later, a third similar paroxysm occurred in the right arm, prompting reassessment of the symptom cause. A second studies.11,22 Caveats also exist regarding the recognition of
radiological assessment suggested rapid progression of atherosclerosis (B) and a new left medial cerebral artery
infarction (D; green arrows). Additionally, dental caries and periodontal disease were diagnosed as possible factors
seizures in elderly people (aged 60–75 years), in whom
contributing to ischaemic stroke. convulsive seizures might be less frequent and seizure
manifestations more difficult to recognise than in
Panel: Caveats to the interpretation of clinical data related younger people (aged <55 years).26 The diagnostic
to post-stroke epileptogenesis investigation is also likely to be more thorough in young
patients with ischaemic stroke than in elderly people,
Accuracy of stroke diagnosis and the higher survival rates of young people might
Prevalence of different types of stroke in a given study underlie the late seizure incidence.
population Children have a clearly enhanced risk of post-stroke
epileptogenesis (table 1).27 Although the causes and risk
Definitions of early and late seizures and epilepsy
factors for ischaemic stroke are different in children
Follow-up duration compared with adults, the molecular and cellular
Sample size environment in the immature brain at the time of stroke
seems to promote PSE development.24,25,27
Heterogeneity in study designs
Use of univariate versus multivariate statistics for data Epilepsy phenotype
analysis In a group of 20 patients with PSE, Lamy and
Availability and analysis of CT and MRI scans for diagnosis colleagues21 reported that the first late seizure was
and follow-up simple partial in ten patients, complex partial in two,
secondary generalised in six, undetermined in one, and
Accuracy regarding the location and type of primary lesion
status epilepticus in one, whereas Lossius and
Availability of EEG for detection of epileptiform activity colleagues22 reported simple or complex partial seizures
(seizures and status epilepticus) in three patients and secondarily generalised seizures
Use of antiepileptic drugs or other medications acutely or in 12 patients. In a study of 102 young adults, the first
during follow-up late seizure was a bilateral convulsive seizure in
79 (77%) patients, impairment of consciousness was
2 www.thelancet.com/neurology Published online November 16, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00248-3
Review
Study type Number Age group (mean age) Patients with PSE at Patients with PSE Length of
of 1 year at the end of follow-up
patients follow-up (years)
So et al (1996)19 Prospective 535 8–99 years (71·6) 3·0% 7·4% 5
Burn et al (1997)20 Retrospective 545 All adult (72·2 years) 4·2% 9·7% 5
Bladin et al (2000)*6 Prospective 1632 All adult (72·7 years) 3·8%; 9 months† ·· ··
Lamy et al (2003)21 Prospective 581 18–55 years (42·5) 3·1% 5·5% 3
Lossius et al (2005)†22 Prospective 484 >60 years (76·2) 2·5% 3·1% 7–8
Roivainen et al (2013)23 Retrospective 995 16–49 years (41·3) 6·9% 11·5% 10
Lee et al (2009)24 Retrospective 75 1 month to 18 years (4·2) ·· 20·0% 2‡
Hsu et al (2014)25 Prospective 94 1 month to 18 years (7·6) 15·0% 21·8% 4·5
The epileptogenic process is most active during the first year when more than 50% of patients who will eventually develop post-stroke epilepsy do so. PSE=post-stroke
epilepsy. *Seizures after 2 weeks from index stroke. †PSE defined as at least two unprovoked seizures. ‡Median follow-up time of total population.
Table 1: Cumulative risk of unprovoked seizure occurrence in ischaemic stroke populations
present in 13 (13%) patients, and motor or autonomic temporal gyrus seems to be associated with post-stroke
phenomena were reported in 10 (10%) patients.23 epileptogenesis.6,21,34,35
Convulsive seizures are the most frequent seizure type
in childhood PSE.25 Subcortical small vessel disease
On EEG, the most frequent finding is focal slowing Lacunar infarctions form about 11% of post-ischaemic
corresponding to the hemispheric side of the infarct.21,28 epilepsy.36 Lacunar infarcts are often discussed in the
De Reuck and colleagues28 reported diffuse slowing context of leukoaraiosis, which refers to “white matter
(n=15), intermittent rhythmic delta activity (n=17), or hyperintensity of presumed vascular origin”.37
periodic lateralised epileptic discharges (n=4) in Leukoaraiosis manifests as round-shaped, isolated, or
69 patients with subsequent early (n=12) or late (n=57) confluent lesions of variable size without cavitation.
seizures whereas similar disturbances in post-stroke Typically, leukoaraiosis is localised in the periventricular
EEG were seen in only 17 of 275 patients who did not areas or deep white matter, or both, and has become
develop post-stroke seizures. A normal post-stroke EEG easier to detect because of advances in imaging methods.37
was seen in only 6 (9%) of 69 patients who developed Gasparini and colleagues38 studied patients with epilepsy
epilepsy compared with 148 (54%) of 275 who did not with or without a clinically identified stroke event, but for
enter epileptogenesis.28 Notably, the data in large PSE whom the cause of epileptogenesis was probably vascular,
studies derives mainly from investigations done during dividing them into those with large vessel infarct (with or
routine clinical practice. EEG is usually done when the without leukoaraiosis) and those with leukoaraiosis only.
nature of the post-stroke paroxysmal event is uncertain. The leukoaraiosis group consisted of 51% of the
Additionally, interpretation of EEG results is challenging 117 patients investigated. Patients with leukoaraiosis
in patients after they have had a stroke because some frequently had clinical and EEG signs suggestive of
EEG disturbances, such as focal slowing, are often temporal lobe epilepsy. Patients with large vessel infarct,
recorded in patients with stroke21,29 and elderly people.30 however, had signs of frontal lobe epilepsy, corresponding
with a cortical or central localisation of the infarct.
Characteristics of epileptogenic ischaemic Hypothetical leukoaraiosis-induced damage to temporal
stroke lobe networks was discussed, but occult coexisting
Symptom severity and lesion size cortical microinfarcts could not be excluded. Accordingly,
Clinical stroke severity, irrespective of stroke scale used, a PET study39 revealed reduced cortical blood flow and
is a major factor in the development of PSE.6,9,10,31,32 Total oxygen consumption more frequently in patients with
anterior circulation infarct is a particularly strong risk late-onset epilepsy and leukoaraiosis than in patients with
factor for post-stroke epileptogenesis compared with leukoaraiosis who did not have epilepsy. Furthermore,
other ischaemic stroke subtypes.9,20,21,23 patients with leukoaraiosis and lacunar infarct with
impaired cognition had a greater risk for PSE than
Lesion location patients without cognitive impairment.40 Leukoaraiosis is
Extent of cortical involvement is a significant risk factor often associated with small vessel disease, which is more
for post-stroke epileptogenesis shared by different age frequent and more severe in patients with seizures
groups with ischaemic stroke.6,21,33 Some evidence beginning after age 60 years, with or without clinical
suggests that epileptogenicity also varies depending on stroke than in patients whose seizures began before age
the affected cortical area. Involvement of the parieto- 60 years, suggesting a role for small vessel disease in
temporal cortex, supramarginal gyrus, and superior epileptogenesis.41
www.thelancet.com/neurology Published online November 16, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00248-3 3
Review
Seizures as biomarkers for cerebrovascular environmental factors that interact with our own unique
disease characteristics, such as genetics, physiology, and
Epileptic seizures could be caused by ischaemic stroke, epigenetics, and affects our health and response to
or be a presenting symptom42,43 or biomarker for it (ie, a injury.
marker of subclinical vascular disease).44 The hypothesis Table 3 summarises the different components of the
that late-onset epilepsy is a precursor of impending exposome and comorbidities that are temporally related
stroke was presented as vascular heralding epilepsy.45 to the occurrence of stroke and have been investigated in
Accumulating data lend support to this hypothesis. the context of post-stroke epileptogenesis. These studies
A large study46 in the UK reported that late-onset epilepsy have shown that hyperglycaemia, type 1 or 2 diabetes,
is associated with triple the risk of later stroke. The dyslipidaemia, hypertension, cardiovascular morbidities,
study46 reported that vascular risk factors, including peripheral infections, early seizures, depression and use
history of myocardial infarction, peripheral vascular of antidepressants, use of statins, and pre-existing
disease, hypertension, total serum cholesterol, and left dementia might modulate post-stroke epileptogenesis.
ventricular hypertrophy, are related to late-onset epilepsy One important aspect of the peri-injury exposome is
through either silent infarcts or non-infarct mechanisms. the effect of acute treatments on post-stroke
The findings are lent support by a meta-analysis epileptogenesis. Acute symptomatic seizures occur in
published in 201444 showing that cerebrovascular disease 2–6% of patients after ischaemic stroke.19,21,23,74 Although
is often a cause of otherwise unexplained late-onset identified as a risk factor for late seizures, treatment and
epilepsy.44 Furthermore, 20% of seizures occurring in prevention of early seizures after stroke with antiepileptic
patients with a previous cerebral infarct are reported to drugs does not modulate post-stroke epileptogenesis.21,75,76
present clinically as a new stroke.47 Convulsive status epilepticus occurs in about 1% of
patients with ischaemic stroke, and 0·1–0·2% cases
Genetic factors occur during the first week after stroke.70,77,78 In a stroke-
About 30% of all epilepsy syndromes are believed to be of unit study79 applying video-EEG monitoring, non-
genetic origin and more than 500 loci are linked to convulsive status epilepticus was identified in 3·6% of
epilepsy in human beings and mice.48 However, only two patients admitted to hospital for stroke. Although status
studies49,50 have assessed the contribution of genetics to epilepticus is thought to be epileptogenic in both
the response to injury and consequent epileptogenesis in animals and man,80,81 it is not associated with the
patients with stroke (table 2). development of PSE.70,82 Use of antiepileptic drugs to
Yang and colleagues50 reported that allele A of the rs671 control seizures or status epilepticus in the acute phase
polymorphism in a gene encoding mitochondrial has raised concerns about their effect on stroke
aldehyde dehydrogenase 2 is associated with PSE and recovery.83 Nadeau and colleagues72 assessed the classes
increases the plasma concentration of aldehyde of α1-noradrenergic blockers, α2-noradrenergic agonists,
dehydrogenase 2 substrate, 4-hydrozynonenal. Zhang benzodiazepines, voltage-sensitive sodium-channel
and colleagues49 reported that a CD40-1C/T polymorphism anticonvulsants, and α2δ voltage-sensitive calcium-
might be associated with PSE susceptibility. The channel blockers on the recovery of functional walking,
proposed mechanisms included raised plasma and reported no significant effects on recovery in a 1-year
concentrations of sCD40L, which is involved in the follow-up. However, systematic studies with larger
inflammatory response.63 cohorts and assessments of different treatment regimens
Several other genes have been investigated in the are needed. Additionally, the effect of non-pharma-
context of ischaemic stroke outcome and the development cological treatment (eg, rehabilitation) on post-stroke
of comorbidities (table 2). The available data suggest epileptogenesis needs to be investigated.
that both epileptogenesis and the development of Two studies84,85 reported an association between
comorbidities can be modulated by non-overlapping thrombolysis with recombinant tissue plasminogen
polymorphisms. At the transcriptomics level, a functional activator and an increased likelihood of acute sympto-
connectivity seems to exist between many of the genes matic seizures after ischaemic stroke. The risk of acute
that modulate post-ischaemic stroke outcomes (figure 2). seizures is not associated with haemorrhagic trans-
So far, no studies have been done to investigate whether formation or recanalisation and reperfusion injury, but it
a given polymorphism will increase the association of is related to the severity of stroke and the extent of cortical
PSE with a specific comorbidity. involvement.85 Irrespective of seizure occurrence, long-
term survival and outcome are improved in patients
Peri-injury exposome as a modulator of receiving thrombolysis.86,87 However, within the
epileptogenesis population of patients receiving thrombolysis, PSE is
The exposome is defined as a measure of all non-genetic associated with an unfavourable outcome due to an
exposures of an individual in a lifetime and how those unidentified mechanism.88,89 Experimental data suggest
exposures relate to health65 (table 3, figure 2). It is that mice with a deficiency in endogenous tissue
composed of environmental, dietary, lifestyle, and other plasminogen activator were less susceptible to
4 www.thelancet.com/neurology Published online November 16, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00248-3
Review
pharmacologically induced seizures and had less neuro- Post-injury cellular pathology
degeneration when exposed to excitotoxic epileptogenic Animal models
insults.90 However, the contribution of treatment with Since 2001, several video-EEG studies have reported the
tissue plasminogen activator on acquired post-stroke occurrence of seizures in various rodent models of
epileptogenesis remains to be explored. ischaemic stroke, including cortical photothrombosis,
Gene or locus Study participants Outcome measure Observation
PSE
CD40-1 C/T49 CD40 molecule, TNF 410 patients with ischaemic PSE Frequency of T allele higher in patients with PSE
receptor superfamily stroke without epilepsy,
member 5 389 patients with PSE
Rs67150 Mitochondrial aldehyde 240 patients with ischaemic PSE Allele A associated with PSE
dehydrogenase 2 stroke without epilepsy,
225 patients with PSE
Other stroke outcomes
ε4 status51 Apolipoprotein E 189 patients with acute BI and MRS at 1 and 3 months No association with performance in daily living activities or
ischaemic stroke degree of disability or dependence
ε4 status52 Apolipoprotein E 496 patients with ischaemic MRS within 1 year No association with degree of disability or dependence
stroke
ε4 status53 Apolipoprotein E 657 patients with ischaemic MRS within 1 year No association with degree of disability or dependence at 1 year;
stroke ε4 genotype is a positive predictor of death within 1 year in men
589C→T54 Interleukin 4 145 patients with ischaemic Disease relapses, deaths, and BI at 589 T allele associated with total ischaemic stroke recurrences;
stroke, 145 controls 1, 3, and 6 months no association with performance in daily living activities or death
589C→VT55 Interleukin 4 145 patients with ischaemic Disease relapses, deaths, and BI No association with performance in daily living activities, death,
stroke or ischaemic stroke recurrences
308G→A55 TNFα 145 patients with ischaemic Disease relapses, deaths, and BI GG genotype associated with reduced odds for impairment in
stroke daily living activities or death
174G→C55 Interleukin 6 145 patients with ischaemic Disease relapses, deaths, and BI No association with performance in daily living activities, death,
stroke or ischaemic stroke recurrences
174G→C56 Interleukin 6 100 patients with ischaemic MRS and BI at 7 days, 3 and GC genotype associated with impaired performance in daily
stroke, 120 controls 6 months living activities, degree of disability or dependence, and higher
mortality
1082G→A54 Interleukin 10 145 patients with ischaemic Disease relapses, deaths, and BI at 1082 GG genotype predicts early stroke progression and
stroke, 145 controls 1, 3, and 6 months impaired performance in daily living activities
1082G→A55 Interleukin 10 145 patients with ischaemic Disease relapses, deaths, and BI No association with performance in daily living activities,
stroke ischaemic stroke recurrences, or death
1188A→C55 Interleukin 12B 145 patients with ischaemic Disease relapses, deaths, and BI No association with performance in daily living activities,
stroke ischaemic stroke recurrences, or death
VNTR in intron 257 Interleukin 1 receptor 391 patients with ischaemic SSS, BI, and OHS at 7 days, 1 and IL1RN*2 homozygocity associated with reduced impairment in
antagonist stroke 3 months, 1 year performance in daily living activities, with lower disability or
dependence at 7 days and 1 year; IL1RN*2 allele increases risk of
death
2518A→G58 Monocyte 145 patients with ischaemic OHS at 1 months No association with degree of disability or dependence in daily
chemoattractant protein-1 stroke living activities
12 SNPs59 Insulin-like growth factor 1 844 patients with ischaemic MRS at 3 and 24 months rs7136446 allele associated with lower degree of disability or
stroke dependence in daily living activities at 24 months post stroke
SNPs in promoter MBL-low MBL2 135 patients with ischaemic or MRS and BI at 3 months MBL-sufficient genotype associated with increased disability and
and MBL-sufficient allele haemorrhagic stroke dependence
variants60
SNP D105→G60 MBL-associated serine 135 patients with ischaemic or MRS and BI at 3 months No association with performance in daily living activities or
protease haemorrhagic stroke degree of disability or dependence
196G→A and 270C→T61 Brain-derived growth 498 patients with ischaemic and BI and OHS at 1 month No association with performance in daily living activities or
factor 56 with haemorrhagic stroke degree of disability or dependence
196G→A and 270C→T61 Brain-derived growth 287 patients with ischaemic and BI and RS before and after Effect of 196 GA+AA genotypes on rehabilitation apparent only
factor 51 with haemorrhagic stroke rehabilitation in those aged ≤55 years and women
Val158Met62 Catechol-O- 78 patients with ischaemic stroke BI and RMA at the beginning and Val/Val alleles associated with improved motor functions and
methyltransferase after 4 weeks and 6 months of ability to do activities of daily living
rehabilitation
TNF=tumour necrosis factor. PSE=post-stroke epilepsy. BI=Barthel index. MRS=modified Rankin scale. VNTR=variable number tandem repeat. SSS=Scandinavian stroke scale. OHS=Oxford handicap scale.
IL1RN=interleukin 1 receptor antagonist. SNP=single nucleotide polymorphism. MBL=mannose-binding lectin. RS=Rankin score. RMA=Rivermead motor assessment.
Table 2: Polymorphisms associated with outcome after ischaemic stroke
www.thelancet.com/neurology Published online November 16, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00248-3 5
Review
A B Depression
Exposure to Alzheimer’s disease
Postmenopausal cigarette smoke Post-stroke Substance use
hormone therapy Hypertension epileptogensis
Chil3/Chil4
Inflammation Physical inactivity COMT CSF1R
Depression FAM49A
Alzheimer’s disease CLU FAP
Dyslipidaemia Cancer
diabetes CD40
GSR Diabetes
Obesity Substance use HIVEP3
Dementia CAMKK2 Alzheimer’s disease
Diabetes Diabetes
Depression Depression BDNF Myocardial
IGF1
Sickle cell Myocardial infarct infarct
disease Dementia Hyperlipidaemia APP IL10 Cancer
Carotid artery Post-stroke
stenosis epileptogenesis
IL1RN
Poor diet Myocardial
Atrial infarct APOE
fibrillation IL4
APBA2 Diabetes
IL6 Alzheimer’s
Tmsb4x disease
ITM2B
TNFAIP8L2
LOC728392
Diabetes TNF
MRC1
Cytokine or Transcription regulator TLR7
Kinase MT-ND4
growth factor
SOD1
Transmembrane SLC40A1 Mt1
Other Transporter
receptor SLC11A2
NCDN
SCG5 NFATC4
Ion channel Enzyme RYR3
Peptidase
Post-stroke epileptogenesis Diabetes, Alzheimer’s disease
ALDH2 MBL2
Figure 2: Post-stroke epilepsy and comorbidity interactome
(A) Post-stroke epilepsy is associated with several comorbidities that can precede or be caused by ischaemic stroke (comorbidities according to Goldstein and colleagues64). (B) Functional in-silico
analysis of genes investigated to assess the association of polymorphisms with various outcome measures after ischaemic stroke suggests a substantial number of interactions. Polymorphisms in
aldehyde dehydrogenase 2 and CD40 genes are associated with post-stroke epileptogenesis. Polymorphisms in several other genes are associated with stroke outcomes such as death, ischaemic stroke
recurrence, performance of daily living activities, and disability or dependence. Notably, functional in-silico analysis suggests that many of the investigated genes are associated with the
pathophysiology of comorbidities of post-stroke epilepsy shown in panel A. Amyloid precursor protein is a particularly prominent node for interactions. Red colour indicates the genes in which a
polymorphism affected the outcome. Solid lines indicate direct interactions between proteins encoded by the genes. Dashed lines indicate indirect interactions between proteins encoded by the genes.
Different shapes represent functions of gene products. Gene interactions were analysed using Ingenuity Pathway Analysis software (Qiagen, Venlo, Netherlands) with default settings.
transient medial cerebral artery occlusion, cortical the perilesional cortex, thalamus, or corpus callosum.94
application of endothelin-1, and hypoxia–ischaemia Two studies92,106 reported changes in inhibitory networks
models of stroke (table 4). In accordance with human in the perilesional cortex, including changes in the
studies, PSE in rodents can be most successfully produced staining intensity of neuropeptide Y neurons and
by ischaemic lesions involving the cerebral cortex. As GABAA receptor subunits (α1, β1, and γ2S). However,
summarised in table 4, post-stroke epileptogenesis seems the contribution of these molecular changes to post-
to depend more on the type of stroke induction than the stroke epileptogenesis remains uncertain. A study by
age of the animal at the time of stroke. Paz and colleagues95 suggested that epileptiform activity
Cellular changes associated with epileptogenesis, caused by photothrombotic stroke in the S1 cortex
such as neurodegeneration, axonal and synaptic can be controlled by optogenetic stimulation of the
sprouting, neurogenesis, gliogenesis, blood–brain thalamocortical pathways.
barrier damage, and inflammatory response, have been
extensively investigated after experimental ischaemic Human PSE
stroke.104,105 However, very few of these changes have A CT study by Awada and colleagues107 suggested the
been linked to increased excitability or epileptogenesis. existence of viable islands of spared tissue within the
Cellular changes in the hippocampus, such as hilar cell cortical infarct region associated with PSE. Accordingly, a
loss or mossy fibre sprouting, do not differentiate PET study47 reported that seizures originate from regions
animals with or without epilepsy after photothrombotic that are only partly destroyed, with borderline critically
stroke,94 and neither does the amount of iron deposits in decreased cerebral regional blood flow, a low regional
6 www.thelancet.com/neurology Published online November 16, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00248-3
Review
cerebral metabolic rate for oxygen, and no changes in the
Association with
regional oxygen extraction fraction. These observations post-stroke
are interesting in view of a study published in 2015108 epileptogenesis
suggesting that patchy microlesions could be indicative Life-style factors
of epileptogenic areas. Smoking10,66 No
On the basis of epidemiological studies, haemorrhagic Alcohol use*10,23,35,66 Yes/no
stroke seems to be more epileptogenic than ischaemic Acute metabolic disturbances
stroke, with about 10–20% of patients developing PSE Acid–base imbalance66 No
after haemorrhagic stroke compared with 2–14% after Electrolyte imbalance35,66 No
ischaemic stroke;7,20,32 however, this difference was not
Hyperglycaemia*23,35 Yes
confirmed by a meta-analysis published in 2014.10
Non-CNS morbidities
Haemorrhagic transformation of ischaemic stroke is an
Diabetes 1 or 2*11,35,66 Yes/no
independent risk factor for both acute symptomatic
Dyslipidaemia66 No
seizures and epileptogenesis.23,109 The epileptogenic
Renal insufficiency35,66 No
potential of haemorrhagic transformation might also
Hypertension35,66,67,68 Yes/no
relate to the associated blood–brain barrier disruption.110,111
Coronary heart disease or myocardial infarction*11,35,66 Yes/no
Experimental studies provide convincing evidence that
Peripheral infections*23,66 Yes/no
increased blood–brain barrier permeability makes the
CNS morbidities
brain prone to seizures.112,113 Gilad and colleagues114
Early seizures*21,23,33,69 Yes
reported a prospective study of 28 patients aged
Status epilepticus within 2 weeks post stroke70 No
38–90 years with cortical stroke who developed PSE, and
imaged them about 1 year after the index stroke with Depression or use of antidepressants*23,66 Yes
⁹⁹mTc-diethylene triamine penta-acetic acid SPECT. Dementia71 Yes
Imaging was done within 72 h after the last seizure. In Pharmacotherapy
86% of patients with PSE, the blood–brain barrier was Antiepileptic drugs72 No
disrupted in the known cortical stroke region. This study α1-noradrenergic blockers72 No
also included a historic control group of patients with α2-noradrenergic agonists72 No
stroke without seizures; of these, only 29% had blood– benzodiazepines72 No
brain barrier disruption in the cortical stroke region. α2δ voltage-sensitive calcium-channel blockers72 No
Importantly, the study114 reported no difference between Statins*73 Yes
groups with and without PSE for the latency between *Because data derived from ischaemic stroke only are meagre, cohorts reported in
stroke and imaging, or for stroke localisation and size. studies shown also include other stroke types.
Perilesional EEG findings do not differ between patients
Table 3: Peri-injury exposome and risk of epileptogenesis after cerebral
with and without blood–brain barrier damage,114 and the
stroke
reason that seizures do not occur in all patients with
blood–brain barrier damage remains unknown.
Hippocampal sclerosis is a pathological hallmark of timepoint of sampling, occurrence of seizures and status
different types of acquired epilepsies, which presents epilepticus, and the exposome (particularly drug
either as a primary or dual pathology.115 A histological treatment)—and the difficulty obtaining representative
assessment of hippocampal infarcts revealed that control samples. Transcriptomic profiling in animal
150 (12%) of 1245 patients who had been autopsied had models of stroke provides an unbiased insight into
hippocampal infarcts; however, after exclusion of cases ongoing molecular pathologies that could be exploited
with co-existing extrahippocampal pathologies, the for clinical benefit—eg, for optimisation of treatment of
number of patients with hippocampal infarcts who had comorbidities such as status epilepticus—according to
epilepsy (5 [4%] of 116) did not differ from those without target expression.
hippocampal infarcts (5 [5%] of 96).116 So far, no studies Most available data on transcriptome profiling in
have specifically assessed hippocampal changes in adult animal models of ischaemic stroke describe alterations
PSE. Some studies suggest the existence of a critical in gene expression during the acute phase—ie, within
time window for the development of hippocampal 24 h of stroke. This is the time window when most of
sclerosis after childhood cortical infarction,117,118 but the the seizures and status epilepticus occur clinically, and
contribution of hippocampal changes to childhood PSE the patient is being actively treated. Only a few
remains to be explored. experimental datasets cover a longer post-stroke time
period that would allow for the assessment of the
Post-injury molecular pathology temporal sequence of post-stroke molecular
Molecular analysis of the outcomes of stroke in man is pathologies. Lu and colleagues119 investigated time-
challenging because of the many patient-related specific alterations in gene expression patterns in the
variables—such as injury subtype, brain areas affected, injured hemisphere after transient middle cerebral
www.thelancet.com/neurology Published online November 16, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00248-3 7
Review
Age Lesion Age at the end Percentage Seizure frequency Seizure
of follow-up with epilepsy duration
Photothrombosis91 2–30 months Motor cortex, S1 4–8 months 50–75% Multiple 10–90 s
Photothrombosis92 “Young adult” S1 4 months 100% Daily recurrent About 10 s
Photothrombosis93 2 months Sensorimotor cortex 6 months 50% 1/4·6 h 2–3 s
Photothrombosis94 3 months S1 10 months 19% 0·39/day 117 s
Photothrombosis95 P25–30 S1 11 months 60% ·· 10–120 s
Photothrombosis96 P7 Sensorimotor cortex P12, P25 ·· At P25 seizure ··
susceptibility to
pentylenetetrazol
increases
Transient MCAO97 3 months Cortex 12 months 0% NA NA
Transient MCAO98 2·5 months Cortex 6 months 0% NA NA
Transient MCAO99 4 months Cortex 6 months 0% NA NA
Transient MCAO99 20 months Cortex 22 months 100% 1–2/week 6 s to 1 min
Endothelin-1100 8–9 months Cortex, striatum 12 months 3% 0·21/day 78–174 s
Endothelin-1101 P12 Hippocampus 3 months 71% 2·3/24 h 6–18 s
Endothelin-1101 P25 Hippocampus 3 months 92% 1·8/24 h 5–9 s
Unilateral carotid ligation P7 Ipsilateral hemisphere 2–12 months 100% 0·09–0·96/24 h 10–240 s
with hypoxia102
Global hypoxia103 P10 Mossy fibre sprouting in P175 95% 5·8/h 3–37 s
CA3
S1=primary somatosensory cortex. P=postnatal day. MCAO=medial cerebral artery occlusion. NA=not applicable.
Table 4: Epilepsy phenotype in animal models of ischaemic stroke or hypoxia-ischaemia based on in-vivo EEG recordings
artery occlusion in rats. The data revealed clear dynamic have described miRNA expression at timepoints later
and coordinated post-stroke transcriptional changes. than 1 day after stroke. Gubern and colleagues121 reported
For example, transcription factors and heat-shock changes in several miRNAs in the cortical ischaemic
proteins were already upregulated at 30 min post tissue at 7 days and 14 days after middle cerebral artery
stroke. Upregulation of genes mediating inflammation, occlusion, suggesting that regulated miRNAs participate
cell death, cytoskeletal functions, and metabolism was in brain damage, neuroprotection, synaptic plasticity,
evident at 1 day post stroke. Increased expression of regulation of neuronal excitability, or glial scar formation.
heat-shock proteins and neurotrophic growth factors As with mRNA, alterations in miRNA expression are
persisted until 7 days post stroke. Downregulation of dynamic after injury.121
ion channels and receptors began at 1 day post stroke, Taken together, the findings suggest some similarities
but some genes remained suppressed for up to 7 days. between changes in gene expression after stroke and
Importantly, differentially expressed genes have a those after other brain injuries that trigger
limited overlap at more than one timepoint.119 This epileptogenesis, especially the dynamic nature of the
finding was confirmed in a permanent middle cerebral alterations and the functional characteristics of genes
artery occlusion model in rats, as largely different sets whose expression level changes at different timepoints.4,122
of genes were upregulated or downregulated at 1 day Because analyses were done at early post-stroke
and 3 days post stroke.120 Ramos-Cejudo and colleagues120 timepoints, whether some of the animals developed
added another level of complexity by showing epilepsy and whether the molecular changes in those
differential alterations in gene expression between the animals differed from those in non-epileptogenic
lesion core and peri-infarct area. These data suggest animals are unknown. Additionally, many of the studies
that molecular mechanisms induced by ischaemic were done in models of ischaemic stroke that have not
stroke have specific spatiotemporal dynamics, starting been shown to result in PSE (adult rats with medial
with pronounced changes in the regulation of cerebral artery stroke). Even with these caveats, these
transcription and culminating in an immune response data have implications for the design of treatment
and neuronal plasticity. strategies for stroke and its acute manifestations
The regulation mechanisms of mRNA expression after (eg, seizures and status epilepticus) and chronic
stroke are not well described. In the past decade studies comorbidities (eg, memory impairment) since the given
have revealed the epigenetic mechanisms involved in the drug, applied at different post-injury timepoints,
regulation of post-stroke gene expression, including that encounters a totally different molecular landscape (target
of miRNAs (short non-coding RNAs involved in mRNA expression), and therefore the treatment effects might
silencing and degradation). Only a few profiling studies vary accordingly (figure 3).
8 www.thelancet.com/neurology Published online November 16, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00248-3
Review
Outstanding questions and future directions with brain injury such as stroke. Moreover, the highest
In the past decade, approaches to elucidate the risk of epileptogenesis after status epilepticus is in
mechanisms of epileptogenesis have focused on patients with acute symptomatic status epilepticus.80
revealing cause-specific mechanisms.4,126 Despite detailed Afsar and colleagues128 studied the timing of status
cellular analyses of the infarcted cortex in experimental epilepticus in patients with stroke and reported that 5 of
models, almost no attempts have been made to link 30 episodes of status epilepticus occurred at stroke onset,
the penumbral cellular reorganisation or molecular 15 of 30 within 2 weeks, and 10 of 30 after 2 weeks from
pathology with the development of epileptogenic foci, the index stroke. Whether investigators should induce
even though the limited number of clinical studies point status epilepticus in a clinically relevant context (ie, after
to the cortex as an epileptogenic area.94,104–106 To identify stroke taking into account the timing of status epilepticus
the endophenotypes with the highest risk of epilepto- after stroke) remains to be discussed. In view of data on
genesis, improved accuracy of the documentation of the the occurrence of PSE after ischaemic stroke at any age,
injury itself and patient-related factors, including use of animals with different ages seems relevant in
genetics, is needed. In view of the interplay between the preclinical research. Additionally, assessment of the
periphery and the CNS, detailed exploration of the effect effect of genetic modulators or variable exposomes (eg,
of the peri-injury exposome on post-stroke epilepto- early seizures, status epilepticus, treatments, and
genesis is needed, both in experimental and clinical nutrition) should be systematically assessed (figure 3).
studies. Achieving statistical power in endophenotyping About 30 preclinical proof-of-concept pharmacological
studies will require detailed and accurate data collection studies have provided favourable antiepileptogenesis
and documentation, often from multiple study sites.
Common data elements have been used in clinics for Ischaemic
many years, and preclinical researchers have recently stroke
Seizure focus
taken initiatives to develop common data elements for
harmonising data collection.127 Change in brain metabolism, structure, and connectivity
The inherent difficulty in the molecular analysis of
epileptogenesis in human beings is the availability and
sampling of tissue, since the available epileptogenic brain Injury-induced temporally
Contributing factors orchestrated changes in transcriptomics
tissue typically originates from patients who are drug-
refractory and undergoing epilepsy surgery. Additionally, Chronic exposome
Diabetes
high-quality control tissue from the corresponding brain Coronary heart disease
region that has not been affected pathologically is not Statins
available. Sampling of representative tissue from well Depression or use of
antidepressants
characterised relevant animal models of PSE is therefore
indispensable. Another challenge is the dilution of Temporary exposome
molecular changes in the epileptogenic microcircuitry by Alcohol use
changes in the surrounding non-epileptogenic tissue. Early seizures
Peripheral infections
A combination of electrophysiological methods, such as
high-density EEG arrays accompanied by in-vivo imaging, Polymorphism
will allow for more accurate in-vivo characterisation of ALDH2
epileptogenic regions, increasing the accuracy of CD40
Acute Subacute Chronic
sampling of epileptogenic changes. New approaches to
the sampling and analysis of molecular changes in Pre-stroke Post-stroke 24 h 1 week 1 year
epileptogenic microcircuitries, even in human beings, Epileptogenesis and development of comorbidities over time since index stroke
were recently presented.108
Another question is the extent to which refinement of Figure 3: Evolution of epileptogenesis and the development of comorbidities after an index stroke and
animal models is needed. At present, most studies on the contribution of genetic factors and the exposome
Components of the exposome deemed to have an effect on epileptogenesis after ischaemic stroke on the basis of
mechanisms of epileptogenesis or proof-of-concept trials univariate or multivariate analyses are listed in table 4. Exposure to a given factor can precede, co-occur, or follow
testing novel antiepileptic drugs are done in status the stroke. Additionally, the duration of exposures can vary and differ between patients. For example, on the one
epilepticus models, in which epilepsy develops in almost hand, depression and the use of antidepressants might span over the entire peri-injury period (dotted line
all animals within a period of days to weeks, and seizure expanding throughout the epileptogenic process). On the other hand, 40–98% of acute seizures occur within the
first 48 h post stroke,6,10,21,77,123,124 thus providing the opportunity for short-lasting (minutes) modulation of the
frequency is several per day. These status epilepticus post-injury outcome (short dotted lines represent short-lasting duration). 75% of peripheral infections occur
models are remarkably advantageous compared with within the first 3 days post stroke, which can also have a temporary acute-phase modulatory effect on the
PSE rodent models, in which typically only a few animals outcome.125 Because the exposome varies largely between individuals, its accurate description during data
develop epilepsy during the course of weeks to months, collection is crucial to reveal the contribution of different factors to the outcome. Moreover, ischaemic stroke
triggers temporally orchestrated waves of molecular changes that can be modulated by the exposome.
and seizure frequency is low. Although the use of status Consequently, depending on the timing of administration in a given patient, treatments encounter different
epilepticus models is time efficient and cost efficient, molecular environments within the recipients, which can affect the target expression, and consequently, treatment
notably, in man, status epilepticus is often associated effectiveness (eg, treatment of status epilepticus in patients).
www.thelancet.com/neurology Published online November 16, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00248-3 9
Review
Declaration of interests
Search strategy and selection criteria We declare no competing interests.
We searched all PubMed articles published up to Aug 1, 2015, Acknowledgments
This study was supported by the Academy of Finland (AP), ERA-NET
with the terms “cerebrovascular disease”, “cerebral stroke”, NEURON: TBI Epilepsy (AP), FP7-HEALTH project 602102
“ischemic stroke”, “post-stroke epilepsy”, “epilepsy”, “seizure”, (EPITARGET) (AP, KL), PMSE grant W19/7.PR/2014 (KL), and statutory
“epileptogenesis”, “antiepileptogenesis”, and their funds of the Nencki Institute (KL).
combinations. We included data from studies of adults and References
children. For genetics, we used the search terms 1 Pitkanen A, Nehlig A, Brooks-Kayal AR, et al. Issues related to
development of antiepileptogenic therapies. Epilepsia 2013;
“polymorphism and post-stroke epilepsy” and 54 (suppl 4): 35–43.
“polymorphism and stroke and outcome”. For 2 Pitkänen A ST. Is epilepsy a progressive disease? Prospects for new
transcriptomics in epileptogenesis, we used the search terms therapeutic approaches in temporal lobe epilepsy.
Lancet Neurol 2002; 1: 73–81.
“microarrays and epileptogenesis” and “transcriptome and
3 Kanner AM, Mazarati A, Koepp M. Biomarkers of epileptogenesis:
epileptogenesis”. For epigenetics, we used the search term psychiatric comorbidities (?). Neurotherapeutics 2014; 11: 358–72.
“epigenetic and epilepsy”. For preclinical treatment trials, we 4 Pitkanen A, Lukasiuk K. Mechanisms of epileptogenesis and
searched only for studies in which therapy was initiated after potential treatment targets. Lancet Neurol 2011; 10: 173–86.
5 Hauser WA, Annegers JF, Kurland LT. Incidence of epilepsy and
the epileptogenic insult. We also identified articles through unprovoked seizures in Rochester, Minnesota: 1935–1984.
searches of the authors’ own article collections. We only Epilepsia 1993; 34: 453–68.
reviewed articles published in English. 6 Bladin CF, Alexandrov AV, Bellavance A, et al. Seizures after stroke:
a prospective multicenter study. Arch Neurol 2000; 57: 1617–22.
7 Menon B, Shorvon SD. Ischaemic stroke in adults and epilepsy.
Epilepsy Res 2009; 87: 1–11.
data.129 However, none of these preclinical trials were done 8 Jungehulsing GJ, Heuschmann PU, Holtkamp M, Schwab S,
in PSE models. Furthermore, no attempts have been made Kolominsky-Rabas PL. Incidence and predictors of post-stroke
to identify biomarkers for post-stroke epileptogenesis. epilepsy. Acta Neurol Scand 2013; 127: 427–30.
9 Graham NSN, Crichton S, Koutroumanidis M, Wolfe CD, Rudd AG.
Even when the data become available, a major concern is Incidence and associations of poststroke epilepsy the prospective
that the successful preclinical trials will not translate to the South London stroke register. Stroke 2013; 44: 605–11.
clinic.130 To address this concern, the International League 10 Zhang C, Wang X, Wang Y, et al. Risk factors for post-stroke
seizures: a systematic review and meta-analysis. Epilepsy Res 2014;
Against Epilepsy and the American Epilepsy Society task 108: 1806–16.
force for advancing preclinical methodology in epilepsy 11 Adelow C, Andersson T, Ahlbom A, Tomson T. Prior hospitalization
research published recommendations in 2013 for doing for stroke, diabetes, myocardial infarction, and subsequent risk of
unprovoked seizures. Epilepsia 2011; 52: 301–07.
antiepileptogenesis studies aimed at overcoming the
12 Adams HP, Biller J. Classification of subtypes of ischemic stroke:
challenges related to statistically powered assessment of history of the trial of org 10 172 in acute stroke treatment
novel antiepileptogenesis therapies.1,127 classification. Stroke 2015: 114–18.
Nevertheless, treatments tested in the clinic have not 13 Nelson KB. Is it HIE? And why that matters. Acta Paediatr 2007;
96: 1113–14.
been vigorously assessed in preclinical models.76 Criteria
14 Jacobs BS, Boden-Albala B, Lin I-F, Sacco RL. Stroke in the young
for progressing from the laboratory to clinic have been in the northern Manhattan stroke study. Stroke 2002; 33: 2789–93.
proposed,1 but the high cost of clinical studies without 15 Putaala J, Curtze S, Hiltunen S, Tolppanen H, Kaste M,
available biomarkers to identify the most susceptible Tatlisumak T. Causes of death and predictors of 5-year mortality in
young adults after first-ever ischemic stroke: the Helsinki Young
individuals for epileptogenesis and to predict the therapy Stroke Registry. Stroke 2009; 40: 2698–703.
response hinder antiepileptogenesis clinical studies.129,131 16 Teasdale G, Jennett B. Assessment of coma and impaired
Attempts have been made to develop algorithms to consciousness. A practical scale. Lancet 1974; 2: 81–84.
17 Beghi E, Carpio A, Forsgren L, et al. Recommendation for a
predict the risk of PSE after ischaemic or haemorrhagic definition of acute symptomatic seizure. Epilepsia 2010; 51: 671–75.
stroke on the basis of the clinical characteristics.132,133 18 Feigin VL, Lawes CMM, Bennett DA, Barker-Collo SL, Parag V.
Another possibility is that a successful clinical trial in Worldwide stroke incidence and early case fatality reported in 56
population-based studies: a systematic review. Lancet Neurol 2009;
patients with ischaemic stroke with treatment developed 8: 355–69.
for an indication other than antiepileptogenesis could 19 So EL, Annegers JF, Hauser W, O’Brien PC, Whisnant JP.
provide a so-called positive control, allowing basic Population-based study of seizure disorders after cerebral
scientists to verify whether any of the experimental infarction. Neurology 1996; 46: 350–55.
20 Burn J, Dennis M, Bamford J, Sandercock P, Wade D, Warlow C.
models predict favourable clinical data, possibly in a Epileptic seizures after a first stroke: the Oxfordshire Community
multi-centre standardised setting. Unfortunately, clinical Stroke Project. BMJ 1997; 315: 1582–87.
trials in patients with stroke have not included epilepsy 21 Lamy C, Domigo V, Semah F, et al. Early and late seizures after
cryptogenic ischemic stroke in young adults. Neurology 2003;
as an outcome measure. The epilepsy field would be 60: 400–04.
greatly benefited if present studies searching for 22 Lossius MI, Ronning OM, Slapo GD, Mowinckel P, Gjerstad L.
therapies and biomarkers for functional outcomes of Poststroke epilepsy: occurrence and predictors—a long-term
prospective controlled study (Akershus Stroke Study).
stroke included epilepsy in their design. Epilepsia 2005; 46: 1246–51.
Contributors 23 Roivainen R, Haapaniemi E, Putaala J, Kaste M, Tatlisumak T.
All authors contributed equally to the conception, design, scientific Young adult ischaemic stroke related acute symptomatic and late
literature search, and writing of this Review. seizures: risk factors. Eur J Neurol 2013; 20: 1247–55.
10 www.thelancet.com/neurology Published online November 16, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00248-3
Review
24 Lee J-C, Lin K-L, Wang H-S, et al. Seizures in childhood ischemic 50 Yang H, Song Z, Yang G-P, et al. The ALDH2 rs671 polymorphism
stroke in Taiwan. Brain Dev 2009; 31: 294–99. affects post-stroke epilepsy susceptibility and plasma 4-HNE levels.
25 Hsu C-J, Weng W-C, Peng SS-F, Lee W-T. Early-onset seizures are PLoS One 2014; 9: e109634.
correlated with late-onset seizures in children with arterial ischemic 51 McCarron MO, Muir KW, Nicoll JA, et al. Prospective study of
stroke. Stroke 2014; 45: 1161–63. apolipoprotein E genotype and functional outcome following
26 Cloyd J, Hauser W, Towne A, et al. Epidemiological and medical ischemic stroke. Arch Neurol 2000; 57: 1480–84.
aspects of epilepsy in the elderly. Epilepsy Res 2006; 52 Sarzynska-Dlugosz I, Gromadzka G, Baranska-Gieruszczak M,
68 (suppl 1): S39–48. Ciesielska A, Czlonkowska A. APOE does not predict poor outcome
27 Holmes GL, Milh MDM, Dulac O. Maturation of the human brain 1 year after ischemic stroke. Neurol Res 2007; 29: 64–69.
and epilepsy. Handb Clin Neurol 2012; 107: 135–43. 53 Gromadzka G, Baranska-Gieruszczak M, Sarzynska-Dlugosz I,
28 De Reuck J, Goethals M, Claeys I, Van Maele G, De Clerck M. Ciesielska A, Czlonkowska A. The APOE polymorphism and 1-year
EEG findings after a cerebral territorial infarct in patients who outcome in ischemic stroke: genotype-gender interaction.
develop early- and late-onset seizures. Eur Neurol 2006; 55: 209–13. Acta Neurol Scand 2007; 116: 392–98.
29 Horner S, Ni XS, Duft M, Niederkorn K, Lechner H. EEG, CT and 54 Marousi S, Ellul J, Antonacopoulou A, Gogos C,
neurosonographic findings in patients with postischemic seizures. Papathanasopoulos P, Karakantza M. Functional polymorphisms of
J Neurol Sci 1995; 132: 57–60. interleukin 4 and interleukin 10 may predict evolution and functional
30 McBride AE, Shih TT, Hirsch LJ. Video-EEG monitoring in the outcome of an ischaemic stroke. Eur J Neurol 2011; 18: 637–43.
elderly: a review of 94 patients. Epilepsia 2002; 43: 165–69. 55 Marousi S, Antonacopoulou A, Kalofonos H, Papathanasopoulos P,
31 Jungehulsing GJ, Heuschmann PU, Holtkamp M, Schwab S, Karakantza M, Ellul J. Functional inflammatory genotypes in
Kolominsky-Rabas PL. Incidence and predictors of post-stroke ischemic stroke: could we use them to predict age of onset and
epilepsy. Acta Neurol Scand 2013; 127: 427–30. long-term outcome? Stroke Res Treat 2011; 2011: 792923.
32 Arntz R, Rutten-Jacobs L, Maaijwee N, et al. Post-stroke epilepsy in 56 Chakraborty B, Chowdhury D, Vishnoi G, Goswami B, Kishore J,
young adults: a long-term follow-up study. PLoS One 2013; Agarwal S. Interleukin-6 gene -174 G/C promoter polymorphism
8: e55498. predicts severity and outcome in acute ischemic stroke patients
from north India. J Stroke Cerebrovasc Dis 2013; 22: 683–89.
33 Hsu C-J, Weng W-C, Peng SS-F, Lee W-T. Early-onset seizures are
correlated with late-onset seizures in children with arterial ischemic 57 Gromadzka G, Sarzynska-Dlugosz I, Czlonkowska A. IL1RN intron
stroke. Stroke 2014; 45: 1161–63. 2 polymorphism caused by variable number tandem repeats is
associated with 1-year outcome in patients with ischaemic stroke.
34 Heuts-van Raak L, Lodder J, Kessels F. Late seizures following a
J Neurol Neurosurg Psychiatry 2007; 78: 183–86.
first symptomatic brain infarct are related to large infarcts
involving the posterior area around the lateral sulcus. Seizure 58 Giannakopoulou E, Ragia G, Marousi S, Ellul J,
1996; 5: 185–94. Manolopoulos VG, Tavridou A. Association of monocyte
chemoattractant protein-1 -2518A>G polymorphism with
35 Leone MA, Tonini MC, Bogliun G, et al. Risk factors for a first
occurrence, severity, and outcome in ischemic stroke.
epileptic seizure after stroke: A case control study. J Neurol Sci 2009;
Neurol Sci Off J Ital Neurol Soc Ital Soc Clin Neurophysiol 2013;
277: 138–42.
34: 1315–20.
36 Benbir G, Ince B, Bozluolcay M. The epidemiology of post-stroke
59 Aberg ND, Olsson S, Aberg D, et al. Genetic variation at the IGF1
epilepsy according to stroke subtypes. Acta Neurol Scand 2006;
locus shows association with post-stroke outcome and to circulating
114: 8–12.
IGF1. Eur J Endocrinol 2013; 169: 759–65.
37 Wardlaw JM, Smith EE, Biessels GJ, et al. Neuroimaging standards
60 Cervera A, Planas AM, Justicia C, et al. Genetically-defined
for research into small vessel disease and its contribution to ageing
deficiency of mannose-binding lectin is associated with protection
and neurodegeneration. Lancet Neurol 2013; 12: 822–38.
after experimental stroke in mice and outcome in human stroke.
38 Gasparini S, Ferlazzo E, Beghi E, et al. Epilepsy associated with PLoS One 2010; 5: e8433.
Leukoaraiosis mainly affects temporal lobe: a casual or causal
61 Mirowska-Guzel D, Gromadzka G, Czlonkowski A, Czlonkowska A.
relationship? Epilepsy Res 2015; 109: 1–8.
BDNF -270 C>T polymorphisms might be associated with stroke
39 De Reuck JL. Evidence for chronic ischaemia in the pathogenesis of type and BDNF -196 G>A corresponds to early neurological deficit
vascular dementia: from neuroPATH to neuroPET. Acta Neurol Belg in hemorrhagic stroke. J Neuroimmunol 2012; 249: 71–75.
1996; 96: 228–31.
62 Liepert J, Heller A, Behnisch G, Schoenfeld A.
40 De Reuck J, De Clerck M, Van Maele G. Vascular cognitive Catechol-O-methyltransferase polymorphism influences outcome
impairment in patients with late-onset seizures after an ischemic after ischemic stroke: a prospective double-blind study.
stroke. Clin Neurol Neurosurg 2006; 108: 632–37. Neurorehabil Neural Repair 2013; 27: 491–96.
41 Maxwell H, Hanby M, Parkes LM, Gibson LM, Coutinho C, 63 Antoniades C, Bakogiannis C, Tousoulis D, Antonopoulos AS,
Emsley HC. Prevalence and subtypes of radiological cerebrovascular Stefanadis C. The CD40/CD40 ligand system: linking inflammation
disease in late-onset isolated seizures and epilepsy. with atherothrombosis. J Am Coll Cardiol 2009; 54: 669–77.
Clin Neurol Neurosurg 2013; 115: 591–96.
64 Goldstein LB, Adams R, Alberts MJ, et al. Primary prevention of
42 Giroud M, Gras P, Fayolle H, Andre N, Soichot P, Dumas R. Early ischemic stroke: a guideline from the American Heart Association/
seizures after acute stroke: a study of 1,640 cases. Epilepsia 1994; American Stroke Association Stroke Council: cosponsored by the
35: 959–64. Atherosclerotic Peripheral Vascular Disease Interdisciplinary
43 Chadehumbe MA, Khatri P, Khoury JC, et al. Seizures are common Working Group; Cardiovascular Nursing Council; Clinical Cardiology
in the acute setting of childhood stroke: a population-based study. Council; Nutrition, Physical Activity, and Metabolism Council; and
J Child Neurol 2009; 24: 9–12. the Quality of Care and Outcomes Research Interdisciplinary
44 Brigo F, Tezzon F, Nardone R. Late-onset seizures and risk of Working Group: the American Academy of Neurology affirms the
subsequent stroke: a systematic review. Epilepsy Behav 2014; 31: 9–12. value of this guideline. Stroke 2006; 37: 1583–633.
45 Cocito L, Favale E, Reni L. The frequency, characteristics and 65 Wild CP. The exposome: from concept to utility. Int J Epidemiol
prognosis of epileptic seizures at the onset of stroke. 2012; 41: 24–32.
J Neurol Neurosurg Psychiatry 1989; 52: 292. 66 Wang G, Jia H, Chen C, et al. Analysis of risk factors for first seizure
46 Cleary P, Shorvon S, Tallis R. Late-onset seizures as a predictor of after stroke in Chinese patients. Biomed Res Int 2013; 2013: 702871.
subsequent stroke. Lancet 2004; 363: 1184–86. 67 Ng SK, Hauser WA, Brust JC, Susser M. Hypertension and the risk
47 De Reuck JL. Stroke-related seizures and epilepsy. of new-onset unprovoked seizures. Neurology 1993; 43: 425–28.
Neurol Neurochir Pol 2007; 41: 144–49. 68 Forsgren L, Bucht G, Eriksson S, Bergmark L. Incidence and
48 Noebels J. Pathway-driven discovery of epilepsy genes. clinical characterization of unprovoked seizures in adults: a
Nat Neurosci 2015; 18: 344–50. prospective population-based study. Epilepsia 1996; 37: 224–29.
49 Zhang B, Chen M, Yang H, Wu T, Song C, Guo R. Evidence for 69 Fox CK, Glass HC, Sidney S, Lowenstein DH, Fullerton HJ. Acute
involvement of the CD40/CD40L system in post-stroke epilepsy. seizures predict epilepsy after childhood stroke. Ann Neurol 2013;
Neurosci Lett 2014; 567: 6–10. 74: 249–56.
www.thelancet.com/neurology Published online November 16, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00248-3 11
Review
70 Rumbach L, Sablot D, Berger E, Tatu L, Vuillier F, Moulin T. Status 95 Paz JT, Davidson TJ, Frechette ES, et al. Closed-loop optogenetic
epilepticus in stroke: report on a hospital-based stroke cohort. control of thalamus as a tool for interrupting seizures after cortical
Neurology 2000; 54: 350–54. injury. Nat Neurosci 2013; 16: 64–70.
71 Cordonnier C, Hénon H, Derambure P, Pasquier F, Leys D. 96 Brima T, Otáhal J, Mareš P. Increased susceptibility to
Influence of pre-existing dementia on the risk of post-stroke pentetrazol-induced seizures in developing rats after cortical
epileptic seizures. J Neurol Neurosurg Psychiatry 2005; 76: 1649–53. photothrombotic ischemic stroke at P7. Brain Res 2013;
72 Nadeau SE, Lu X, Dobkin B, Wu SS, Dai YE, Duncan PW. 1507: 146–53.
A prospective test of the late effects of potentially antineuroplastic 97 Karhunen H, Pitkänen A, Virtanen T, et al. Long-term functional
drugs in a stroke rehabilitation study. Int J Stroke 2014; 9: 449–56. consequences of transient occlusion of the middle cerebral artery in
73 Guo J, Guo J, Li J, et al. Statin treatment reduces the risk of rats: a 1-year follow-up of the development of epileptogenesis and
poststroke seizures. Neurology 2015; 85: 701–07. memory impairment in relation to sensorimotor deficits.
74 Szaflarski JP, Rackley AY, Kleindorfer DO, et al. Incidence of Epilepsy Res 2003; 54: 1–10.
seizures in the acute phase of stroke: a population-based study. 98 Kelly KM, Jukkola PI, Kharlamov E a, et al. Long-term video-EEG
Epilepsia 2008; 49: 974–81. recordings following transient unilateral middle cerebral and
75 Temkin NR. Preventing and treating posttraumatic seizures: the common carotid artery occlusion in Long-Evans rats.
human experience. Epilepsia 2009; 50 (suppl 2): 10–13. Exp Neurol 2006; 201: 495–506.
76 Trinka E, Brigo F. Antiepileptogenesis in humans: disappointing 99 Kelly KM. Stroke. In: Pitkänen A, Schwarzkroin PA, Moshe SL, eds.
clinical evidence and ways to move forward. Curr Opin Neurol 2014; Models of seizures and epilepsy. Amsterdam: Elsevier, 2006: 501–19.
27: 227–35. 100 Karhunen H, Nissinen J, Sivenius J, Jolkkonen J, Pitkänen A.
77 Labovitz DL, Hauser WA, Sacco RL. Prevalence and predictors of A long-term video-EEG and behavioral follow-up after endothelin-1
early seizure and status epilepticus after first stroke. Neurology 2001; induced middle cerebral artery occlusion in rats. Epilepsy Res 2006;
57: 200–06. 72: 25–38.
78 Bateman BT, Claassen J, Willey JZ, et al. Convulsive status 101 Mátéffyová A, Otáhal J, Tsenov G, Mareš P, Kubová H.
epilepticus after ischemic stroke and intracerebral hemorrhage: Intrahippocampal injection of endothelin-1 in immature rats results
frequency, predictors, and impact on outcome in a large in neuronal death, development of epilepsy and behavioral
administrative dataset. Neurocrit Care 2007; 7: 187–93. abnormalities later in life. Eur J Neurosci 2006; 24: 351–60.
79 Belcastro V, Vidale S, Gorgone G, et al. Non-convulsive status 102 Kadam SD, White AM, Staley KJ, Dudek FE.
epilepticus after ischemic stroke: a hospital-based stroke cohort Continuous electroencephalographic monitoring with
study. J Neurol 2014; 261: 2136–42. radio-telemetry in a rat model of perinatal hypoxia-ischemia reveals
progressive post-stroke epilepsy. J Neurosci 2010; 30: 404–15.
80 Hesdorffer DC, Logroscino G, Cascino G, Annegers JF,
Hauser WA. Risk of unprovoked seizure after acute symptomatic 103 Rakhade SN, Klein PM, Huynh T, et al. Development of later life
seizure: effect of status epilepticus. Ann Neurol 1998; 44: 908–12. spontaneous seizures in a rodent model of hypoxia-induced
neonatal seizures. Epilepsia 2011; 52: 753–65.
81 Pitkanen A, Kharatishvili I, Karhunen H, et al. Epileptogenesis in
experimental models. Epilepsia 2007; 48 (suppl 2): 13–20. 104 Carmichael ST. Cellular and molecular mechanisms of neural
repair after stroke: making waves. Ann Neurol 2006; 59: 735–42.
82 Conrad J, Pawlowski M, Dogan M, Kovac S, Ritter MA, Evers S.
Seizures after cerebrovascular events: risk factors and clinical 105 Li S, Overman JJ, Katsman D, et al. An age-related sprouting
features. Seizure 2013; 22: 275–82. transcriptome provides molecular control of axonal sprouting after
stroke. Nat Neurosci 2010; 13: 1496–504.
83 Goldstein LB. Common drugs may influence motor recovery after
stroke. The Sygen In Acute Stroke Study Investigators. Neurology 106 Kharlamov EA, Kharlamov A, Kelly KM. Changes in neuropeptide Y
1995; 45: 865–71. protein expression following photothrombotic brain infarction and
epileptogenesis. Brain Res 2007; 1127: 151–62.
84 De Reuck J, Van Maele G. Acute ischemic stroke treatment and the
occurrence of seizures. Clin Neurol Neurosurg 2010; 112: 328–31. 107 Awada A, Omojola MF, Obeid T. Late epileptic seizures after
cerebral infarction. Acta Neurol Scand 1999; 99: 265–68.
85 Alvarez V, Rossetti AO, Papavasileiou V, Michel P. Acute seizures in
acute ischemic stroke: does thrombolysis have a role to play? 108 Dachet F, Bagla S, Keren-Aviram G, et al. Predicting novel
J Neurol 2013; 260: 55–61. histopathological microlesions in human epileptic brain through
transcriptional clustering. Brain 2015; 138: 356–70.
86 Schmitz ML, Simonsen CZ, Hundborg H, et al. Acute ischemic
stroke and long-term outcome after thrombolysis: nationwide 109 Alberti A, Paciaroni M, Caso V, Venti M, Palmerini F, Agnelli G.
propensity score-matched follow-up study. Stroke 2014; 45: 3070–72. Early seizures in patients with acute stroke: frequency, predictive
factors, and effect on clinical outcome. Vasc Health Risk Manag
87 Machado C, Pinho J, Alves JN, et al. Five-Year Outcome in Stroke
2008; 4: 715–20.
Patients Submitted to Thrombolysis. Stroke 2015; 46: 2312–14.
110 Renu A, Amaro S, Laredo C, et al. Relevance of blood–brain barrier
88 Couillard P, Almekhlafi MA, Irvine A, et al. Subacute seizure
disruption after endovascular treatment of ischemic stroke:
incidence in thrombolysis-treated ischemic stroke patients.
dual-energy computed tomographic study. Stroke 2015; 46: 673–79.
Neurocrit Care 2012; 16: 241–45.
111 Raabe A, Schmitz AK, Pernhorst K, et al. Cliniconeuropathologic
89 Gensicke H, Seiffge DJ, Polasek AE, et al. Long-term outcome in
correlations show astroglial albumin storage as a common factor in
stroke patients treated with IV thrombolysis. Neurology 2013;
epileptogenic vascular lesions. Epilepsia 2012; 53: 539–48.
80: 919–25.
112 Marchi N, Granata T, Ghosh C, Janigro D. Blood-brain barrier
90 Tsirka SE, Gualandris A, Amaral DG, Strickland S.
dysfunction and epilepsy: pathophysiologic role and therapeutic
Excitotoxin-induced neuronal degeneration and seizure are
approaches. Epilepsia 2012; 53: 1877–86.
mediated by tissue plasminogen activator. Nature 1995; 377: 340–44.
113 Van Vliet EA, Aronica E, Gorter JA. Blood–brain barrier
91 Kelly KM, Kharlamov A, Hentosz TM, et al. Photothrombotic brain
dysfunction, seizures and epilepsy. Semin Cell Dev Biol 2015;
infarction results in seizure activity in aging Fischer 344 and
38: 26–34.
Sprague Dawley rats. Epilepsy Res 2001; 47: 189–203.
114 Gilad R, Lampl Y, Eilam A, Boaz M, Loyberboim M. SPECT-DTPA
92 Liu J, Schmitt KL, Kharlamov EA, Stolarski CJ, Grayson DR,
as a tool for evaluating the blood–brain barrier in post-stroke
Kelly KM. Quantitative reverse transcription-polymerase chain
seizures. J Neurol 2012; 259: 2041–44.
reaction of GABA(A) alpha1, beta1 and gamma2S subunits in
epileptic rats following photothrombotic infarction of neocortex. 115 Blumcke I, Coras R, Miyata H, Ozkara C. Defining clinico-
Epilepsy Res 2002; 52: 85–95. neuropathological subtypes of mesial temporal lobe epilepsy with
hippocampal sclerosis. Brain Pathol 2012; 22: 402–11.
93 Kharlamov EA, Jukkola PI, Schmitt KL, Kelly KM. Electrobehavioral
characteristics of epileptic rats following photothrombotic brain 116 Rauramaa T, Pikkarainen M, Englund E, et al. Cardiovascular
infarction. Epilepsy Res 2003; 56: 185–203. diseases and hippocampal infarcts. Hippocampus 2011; 21: 281–87.
94 Karhunen H, Bezvenyuk Z, Nissinen J, Sivenius J, Jolkkonen J, 117 Squier W, Salisbury H, Sisodiya S. Stroke in the developing brain
Pitkänen A. Epileptogenesis after cortical photothrombotic brain and intractable epilepsy: effect of timing on hippocampal sclerosis.
lesion in rats. Neuroscience 2007; 148: 314–24. Dev Med Child Neurol 2003; 45: 580–85.
12 www.thelancet.com/neurology Published online November 16, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00248-3
Review
118 Salanova V, Markand O, Worth R. Temporal lobe epilepsy: analysis 127 Galanopoulou AS, Kokaia M, Loeb JA, et al. Epilepsy therapy
of patients with dual pathology. Acta Neurol Scand 2004; 109: 126–31. development: technical and methodologic issues in studies with
119 Lu X-CM, Williams AJ, Yao C, et al. Microarray analysis of acute and animal models. Epilepsia 2013; 54 (suppl 4): 13–23.
delayed gene expression profile in rats after focal ischemic brain 128 Afsar N, Kaya D, Aktan S, Sykut-Bingol C. Stroke and status
injury and reperfusion. J Neurosci Res 2004; 77: 843–57. epilepticus: stroke type, type of status epilepticus, and prognosis.
120 Ramos-Cejudo J, Gutierrez-Fernandez M, Rodriguez-Frutos B, et al. Seizure 2003; 12: 23–27.
Spatial and temporal gene expression differences in core and 129 Pitkanen A, Engel JJ. Past and present definitions of epileptogenesis
periinfarct areas in experimental stroke: a microarray analysis. and its biomarkers. Neurotherapeutics 2014; 11: 231–41.
PLoS One 2012; 7: e52121. 130 Green AR. Pharmacological approaches to acute ischaemic stroke:
121 Gubern C, Camos S, Ballesteros I, et al. miRNA expression is reperfusion certainly, neuroprotection possibly.
modulated over time after focal ischaemia: up-regulation of miR-347 Br J Pharmacol 2008; 153 (suppl): S325–38.
promotes neuronal apoptosis. FEBS J 2013; 280: 6233–46. 131 Engel JJ, Pitkanen A, Loeb JA, et al. Epilepsy biomarkers.
122 Lukasiuk K, Dabrowski M, Adach A, Pitkanen A. Epilepsia 2013; 54 (suppl 4): 61–69.
Epileptogenesis-related genes revisited. Prog Brain Res 2006; 132 Strzelczyk A, Haag A, Raupach H, Herrendorf G, Hamer HM,
158: 223–41. Rosenow F. Prospective evaluation of a post-stroke epilepsy risk
123 Olsen TS. Post-stroke epilepsy. Curr Atheroscler Rep 2001; 3: 340–44. scale. J Neurol 2010; 257: 1322–26.
124 Reith J, Jorgensen HS, Nakayama H, Raaschou HO, Olsen TS. 133 Haapaniemi E, Strbian D, Rossi C, et al. The CAVE score for
Seizures in acute stroke: predictors and prognostic significance. predicting late seizures after intracerebral hemorrhage. Stroke 2014;
The Copenhagen Stroke Study. Stroke 1997; 28: 1585–89. 45: 1971–76.
125 Vargas M, Horcajada JP, Obach V, et al. Clinical consequences of
infection in patients with acute stroke: is it prime time for further
antibiotic trials? Stroke 2006; 37: 461–65.
126 Stables JP, Bertram E, Dudek FE, et al. Therapy discovery for
pharmacoresistant epilepsy and for disease-modifying therapeutics:
summary of the NIH/NINDS/AES models II workshop.
Epilepsia 2003; 44: 1472–78.
www.thelancet.com/neurology Published online November 16, 2015 http://dx.doi.org/10.1016/S1474-4422(15)00248-3 13
Vous aimerez peut-être aussi
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Chapter 16 Magnetic Fields: Electricity and MagnetismDocument11 pagesChapter 16 Magnetic Fields: Electricity and MagnetismeltytanPas encore d'évaluation
- LADBS - Swimming PoolsDocument43 pagesLADBS - Swimming PoolsMichael James100% (1)
- ExtraDocument3 pagesExtraaman100% (1)
- Railway Engineering 3Document31 pagesRailway Engineering 3Sheikh UbaidPas encore d'évaluation
- Reading and Interpreting Product DesignDocument38 pagesReading and Interpreting Product DesignKate Adriano100% (2)
- (2014) Colour and Technology in Historic Decorated Glazes and Glasses PDFDocument117 pages(2014) Colour and Technology in Historic Decorated Glazes and Glasses PDFtariq.toffa4760Pas encore d'évaluation
- How To Use PathlossDocument32 pagesHow To Use Pathlosspathlossanwar100% (9)
- (John Zhang, Austin Colohan) Intracerebral Hemorrh (BookFi)Document470 pages(John Zhang, Austin Colohan) Intracerebral Hemorrh (BookFi)Fanel PutraPas encore d'évaluation
- Cardioembolic StrokeDocument13 pagesCardioembolic StrokeFanel PutraPas encore d'évaluation
- Calmodulin Levels in Blood Cells As A Potential Biomarker of Alzheimer 'S DiseaseDocument10 pagesCalmodulin Levels in Blood Cells As A Potential Biomarker of Alzheimer 'S DiseaseFanel PutraPas encore d'évaluation
- Calmodulin Levels in Blood Cells As A Potential Biomarker of Alzheimer 'S DiseaseDocument10 pagesCalmodulin Levels in Blood Cells As A Potential Biomarker of Alzheimer 'S DiseaseFanel PutraPas encore d'évaluation
- LiquorDocument8 pagesLiquorFanel PutraPas encore d'évaluation
- AkutDocument5 pagesAkutFanel PutraPas encore d'évaluation
- Calmodulin Levels in Blood Cells As A Potential Biomarker of Alzheimer 'S DiseaseDocument10 pagesCalmodulin Levels in Blood Cells As A Potential Biomarker of Alzheimer 'S DiseaseFanel PutraPas encore d'évaluation
- A Clinical Tool For Predicting Survival in ALSDocument8 pagesA Clinical Tool For Predicting Survival in ALSFanel PutraPas encore d'évaluation
- Selective Reminding For Analysis of Memory and Learning 1Document8 pagesSelective Reminding For Analysis of Memory and Learning 1Fanel PutraPas encore d'évaluation
- Article Nn. KranialisDocument5 pagesArticle Nn. KranialisFanel PutraPas encore d'évaluation
- Guideline Rehab StrokeDocument2 pagesGuideline Rehab StrokeFanel PutraPas encore d'évaluation
- MultipelDocument11 pagesMultipelFanel PutraPas encore d'évaluation
- Akut MigrainDocument15 pagesAkut MigrainFanel PutraPas encore d'évaluation
- Early Postoperative Tumor Progression Predicts Clinical Outcome in Glioblastoma-Implication For Clinical TrialsDocument6 pagesEarly Postoperative Tumor Progression Predicts Clinical Outcome in Glioblastoma-Implication For Clinical TrialsFanel PutraPas encore d'évaluation
- EpilepsiDocument8 pagesEpilepsiFanel PutraPas encore d'évaluation
- Internal MedicineDocument16 pagesInternal MedicineFanel PutraPas encore d'évaluation
- ArticleDocument11 pagesArticleFanel PutraPas encore d'évaluation
- Maju Jurnal MigrainDocument7 pagesMaju Jurnal MigrainRosyid PrasetyoPas encore d'évaluation
- Migraine and Body Mass Index Categories: A Systematic Review and Meta-Analysis of Observational StudiesDocument14 pagesMigraine and Body Mass Index Categories: A Systematic Review and Meta-Analysis of Observational StudiesRetno ManggalihPas encore d'évaluation
- 10 0000@cardiovascularultrasound Biomedcentral com@generic-5F05D17BCD6E PDFDocument8 pages10 0000@cardiovascularultrasound Biomedcentral com@generic-5F05D17BCD6E PDFFanel PutraPas encore d'évaluation
- ArticleDocument10 pagesArticleFanel PutraPas encore d'évaluation
- Article PDFDocument8 pagesArticle PDFFanel PutraPas encore d'évaluation
- 10 0000@cardiovascularultrasound Biomedcentral com@generic-5F05D17BCD6E PDFDocument8 pages10 0000@cardiovascularultrasound Biomedcentral com@generic-5F05D17BCD6E PDFFanel PutraPas encore d'évaluation
- Tremmel Horvath e ApheresisDocument26 pagesTremmel Horvath e ApheresisFanel PutraPas encore d'évaluation
- Sleep Disturbances and Quality of Life in Sub-Saharan African MigraineursDocument8 pagesSleep Disturbances and Quality of Life in Sub-Saharan African MigraineursFanel PutraPas encore d'évaluation
- Role of Magnesium Sulfate in Aneurysmal Subarachnoid Hemorrhage Management: A Meta-Analysis of Controlled Clinical TrialsDocument6 pagesRole of Magnesium Sulfate in Aneurysmal Subarachnoid Hemorrhage Management: A Meta-Analysis of Controlled Clinical TrialsFanel PutraPas encore d'évaluation
- JnsDocument8 pagesJnsFanel PutraPas encore d'évaluation
- 10 0000@cardiovascularultrasound Biomedcentral com@generic-5F05D17BCD6E PDFDocument8 pages10 0000@cardiovascularultrasound Biomedcentral com@generic-5F05D17BCD6E PDFFanel PutraPas encore d'évaluation
- Role of Magnesium in CVDDocument11 pagesRole of Magnesium in CVDFanel PutraPas encore d'évaluation
- Crepe Paper 2017-05-29-FINALDocument2 pagesCrepe Paper 2017-05-29-FINALPruthvi KrishnaPas encore d'évaluation
- AC 91-56 Amdt. 0 - Continuing Structural Integrity Program For Transport Category AirplaneDocument18 pagesAC 91-56 Amdt. 0 - Continuing Structural Integrity Program For Transport Category Airplaneyogaga100% (1)
- Assignment On Computer HardwareDocument9 pagesAssignment On Computer HardwareMuktadirhasan100% (1)
- Urban green-blue grids: Hammarby SjöstadDocument5 pagesUrban green-blue grids: Hammarby SjöstadAlejandra SusaPas encore d'évaluation
- Incepbio Project PPT - 080124Document21 pagesIncepbio Project PPT - 080124adminpunePas encore d'évaluation
- Raúl Edgardo Macchiavelli: Raul - Macchiavelli@upr - EduDocument53 pagesRaúl Edgardo Macchiavelli: Raul - Macchiavelli@upr - EduDhaval patelPas encore d'évaluation
- Acid Dissociation ConstantDocument4 pagesAcid Dissociation ConstantJair RangelPas encore d'évaluation
- A New Empirical System For Rock Slope Stability Analysis PDFDocument10 pagesA New Empirical System For Rock Slope Stability Analysis PDFJessie LeePas encore d'évaluation
- Precious Metals AlfaDocument83 pagesPrecious Metals AlfaPraveenPas encore d'évaluation
- Analysis of Caffeine Content in Kola Acuminate and Kola NitidaDocument50 pagesAnalysis of Caffeine Content in Kola Acuminate and Kola Nitidaebuka100% (1)
- Silo Surface Area CalculationDocument3 pagesSilo Surface Area CalculationVIC EngineersPas encore d'évaluation
- Compro Saj 2023 - 22052023Document58 pagesCompro Saj 2023 - 22052023Ahmad FauziPas encore d'évaluation
- Report on internship at JDS TransformersDocument50 pagesReport on internship at JDS TransformersSachinPas encore d'évaluation
- Your First ProgramDocument7 pagesYour First ProgramJosephat MugumbaPas encore d'évaluation
- Neem CofA 141019-4Document1 pageNeem CofA 141019-4Rahayuteuk Elf100% (1)
- CT AC 72A<INV=<90A 70A<REC=<135A Part SpecDocument7 pagesCT AC 72A<INV=<90A 70A<REC=<135A Part SpecEdwin Mosos RamosPas encore d'évaluation
- CBSE Class XII Mathematics - Inverse Trigonometric Functions Assignment 2 PDFDocument4 pagesCBSE Class XII Mathematics - Inverse Trigonometric Functions Assignment 2 PDFPooja KathuriaPas encore d'évaluation
- JSA - MergeDocument11 pagesJSA - MergeIzzuddin MustapaPas encore d'évaluation
- Balzac GaitDocument7 pagesBalzac Gaithieratic_headPas encore d'évaluation
- Central Sterile ServiceDocument75 pagesCentral Sterile ServiceSUBHENDU SIKDAR100% (1)
- Heat Transfer Through Extended SurfacesDocument16 pagesHeat Transfer Through Extended SurfaceschawarepPas encore d'évaluation
- LPVDDocument12 pagesLPVDPardha SaradhiPas encore d'évaluation