Académique Documents
Professionnel Documents
Culture Documents
4 Meningoencefalocele PDF
Transféré par
Omar Lopez ArbolayTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
4 Meningoencefalocele PDF
Transféré par
Omar Lopez ArbolayDroits d'auteur :
Formats disponibles
Hindawi Publishing Corporation
Case Reports in Medicine
Volume 2012, Article ID 763259, 4 pages
doi:10.1155/2012/763259
Case Report
Gigant Transethmoidal Meningoencephalocele Operated by
Full Endonasal Endoscopic Approach: Case Report
Omar Lopez Arbolay, Jorge Rojas Manresa,
Justo Gonzalez Gonzalez, and Jose Luis Bretón Rosario
Neurosurgery Department of Hermanos Ameijeiras Hospital, Havana 10348, Cuba
Correspondence should be addressed to Omar Lopez Arbolay, arbolay@infomed.sld.cu
Received 18 September 2011; Accepted 6 December 2011
Academic Editor: Mark E. Shaffrey
Copyright © 2012 Omar Lopez Arbolay et al. This is an open access article distributed under the Creative Commons Attribution
License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly
cited.
Intranasal meningoencephaloceles have historically been managed by neurosurgeons, although their main clinical manifestations
are rhinological. Recent advances in endoscopic skull base surgery has significantly improved the treatment of these lesions and
consequently diminished appreciable surgical morbidity. We report an ethmoidal meningoencephalocele case operated on by
endonasal endoscopic approach for removal of the lesion and reconstructing the associated skull base. From this experience, we
conclude that removal of the lesion and watertight closure of the skull base irrespective of the size of the mass and anterior skull
base defect are the operation’s most important aspects.
1. Introduction leading investigation because it is able to show the protruded
brain tissues and their relationship with neighboring struc-
Intranasal meningoencephaloceles are an infrequent condi- tures. A special useful test to demonstrate the bony defect
tion characterized by protrusion of meningeal and brain will be the CT scan with bone window [1].
tissue through a skull-base defect. Congenital anomalies are We present a case with transethmoidal meningoen-
the main cause [1], but they may have also a traumatic or cephalocele that was operated on by endonasal endoscopic
a spontaneous origin [2, 3]. According to the location, technique.
meningoencephaloceles are classified in: occipital, cranial
vault, posterior fosse, and basal. The incidence of this rare 2. Clinical Case
condition range between 0.1 to 0.5 of 1,000 birthrates. Basal
meningoencephalocele represents 1.5% of all these lesions, Our case is a 55-year-old female patient, who 23 years ago
and are classified as: transethmoidal, sphenoethmoidal, underwent transsphenoidal surgery for an intrasellar cyst.
transsphenoidal, and frontosphenoidal [4, 5]. In transeth- Five years after the surgery, hydrocephalus with cerebral
moidal type, a defect on the cribriform plate is observed, spinal fluid leakage occurred and it was resolved by the place-
commonly small and limited to one side [6]. Nasal CSF ment of a ventriculoperitoneal shunt. Computed tomogra-
leakage, headache, and nasal obstruction, are frequently the phy did not define the bone defect at the site of previous
chief complaints. Rarely, seizure is observed but meningitis is surgery at that time. The patient presented before us, two
common. years ago, with recurrent profuse rhinorrhea and nasal
On physical examination, it is possible to find an in- obstruction. She was admitted in Neurosurgical Department
tranasal mass, leakage of a clear liquid across the nose, with headache, fever and vomiting, and bacterial meningitis
olfaction lost, and other craniofacial defects in the congenital which was successfully treated with antibiotics was diag-
encephaloceles. Some studies may be performed to establish nosed. MRI revealed protrusion of the brain and meninges
the diagnosis, but magnetic resonance imaging (MRI) is the from the anterior cranial fossa to the upper right nasal cavity.
2 Case Reports in Medicine
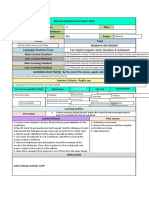
Figure 1: MRI, coronal view. Figure 3: CT scan.
Figure 4: Endoscopic view of big meningoencephalocele within
right nasal cavity.
Figure 2: MRI, sagital view.
3. Discussion
A multidisciplinary management is recommended in the
diagnosis and treatment of meningoencephalocele. Surgi-
cal procedures include removal and anterior fossa defect
The T1-weighted sequences showed downward herniation of reconstruction by craniotomy and more recently endonasal
the ethmoidal roof on the right nasal cavity and T2-weighted endoscopic resection and repair or combination of these two
coronal, and sagital imaging confirmed a liquid-filled mass in techniques to remove the lesion and repair the defect [7–14].
the right ethmoidal sinus and nasal cavity projecting through Endonasal endoscopic procedures and special develop-
a defect in the ethmoidal roof (Figures 1 and 2). Computed ment of extended endonasal endoscopic approaches have
tomography confirmed these findings (Figure 3). increased the interest on treating this kind of lesion. That
An extended endonasal endoscopic approach to the ante- is why the treatment of meningoencephaloceles has become
rior cranial base was practiced. A big meningoencephalocele more popular.
within right nasal cavity was found (Figure 4). By using As the first step in the surgery, meningoencephalocele
bipolar forceps the lesions were reduced. Middle turbinate is carefully and gradually removed using bipolar cauterizing
was atrophic and middleward displaced. When the lesion up to the level of the skull base. Then, mucosa surrounding
was completely removed, a bony defect at the junction of skull-base defect is removed and the defect is prepared for
ethmoidal sinus and posterior wall of the frontal bone were the graft.
observed (Figure 5). This was reconstructed inlaying a free Selection of the graft material depends on the defected
intradural fat graft and an epidural layer of bone, which size and configuration, underlying pathophysiology and the
was then covered with a nasoseptal flap. This was supported surgeon’s preference [15]. A multilayer repair is preferred not
with balloon of 12 French Foley catheter in order to press only to stop the CSF leak, but to reinforce the thin skull base
the multilayer reconstruction against the defect. The patient and prevent meningoencephalocele recurrence [16, 17].
had an uneventual recovery. There were no cerebrospinal Autologous-free or pedicellate mucoperichondrial grafts,
rhinorrhea or any other complications and the patient was fascia, turbinate grafts, cartilage grafts, pericranial-galeal,
discharged six days after the surgery. and bone grafts have all been used successfully. Heterologus
Case Reports in Medicine 3
meningoencephaloceles,” Indian Pediatrics, vol. 42, no. 10, pp.
1033–1036, 2005.
[2] S. Badiane, K. Kalangu, Y. Kato, and G. Dechambenoit, “En-
cephaloceles,” in Essential Practice of Neurosurgery, pp. 1282–
1289, Access Publishing Co., 2009.
[3] T. H. Yang, S. Y. Jeong, and S. Y. Oh, “Recurrent Strepto-
coccus Pneumoniae Meningoencephalitis in a patient with a
Transethmoidal Maningoencephalocele,” The Journal of Clini-
cal Neurology, vol. 4, no. 1, pp. 40–44, 2008.
[4] J. T. Rutka, C. Carlotti, and M. Iantoska, “Development and
acquired anomalies,” in Youmans Neurological Surgery, W. H.
Richard, Ed., pp. 3198–3213, 5th edition, 2004.
[5] M. S. Greenberg, Handbook of Neurosurgery, Thieme, New
Figure 5: Endoscopic view of bony defect at the junction of eth-
York, NY, USA, 6th edition, 2006.
moidal sinus and posterior wall of the frontal bone.
[6] A. Kubo, K. Sakata, J. Maegawa, and I. Yamamoto, “Transeth-
moidal meningoencephalocele in an elderly woman: case re-
port,” Neurologia Medico-Chirurgica, vol. 45, no. 6, pp. 322–
materials have also been used subdural as collagen matrix 326, 2005.
(Duragen, Integra Life Sciences) and no cells dermis grafts [7] F. Aderito, J. Minaret, S. Aidmar, and F. Medina, “Giant Eth-
(Alloderm, Lifecell Corp.) [15]. Recently, reconstruction moid Meningoencephalocele,” Journal of Otorhinolaryngology,
of skull base using vascularized pedicellar flap has been vol. 10, no. 2, 2009.
described. Nasoseptal and inferior turbinate flap seem to be [8] B. McCormack, P. R. Cooper, M. Persky, and S. Rothstein,
the most useful. Reconstruction of the cranial base using “Extracranial repair of cerebrospinal fluid fistulas: technique
vascularized tissue promotes fast and complete healing, pre- and results in 37 patients,” Neurosurgery, vol. 27, no. 3, pp.
venting complications caused by persistent communication 412–417, 1990.
between the cranial cavity and the sinonasal tract [18–21]. [9] E. E. Dodson, C. W. Gross, J. L. Swerdloff, and L. M. Gustafson,
We considered that best option for repairing the skull- “Transnasal endoscopic repair of cerebrospinal fluid rhinor-
base defect in this case was to use a multilayer grafts. rhea and skull base defects: a review of twenty-nine cases,”
Otolaryngology—Head and Neck Surgery, vol. 111, no. 5, pp.
We used a free inly fat graft (intradural), then an inlaid
600–605, 1994.
epidural bone graft, and, after that, we covered it with a
[10] M. Gjuric, H. Keimer, U. Goede, and M. E. Wigand, “En-
big vascular pedicellar nasoseptal flap to prevent a recurrent donasal endoscopic closure of cerebrospinal fluid fistulas at
brain herniation and CSF leakage. the anterior cranial base,” Annals of Otology, Rhinology and
Historically, lumbar drainage of CSF has been used after Laryngology, vol. 105, no. 8, pp. 620–623, 1996.
surgery as an adjoined action to surgical repair. Nevertheless, [11] S. Schmerber, C. Righini, J. P. Lavielle, J. G. Passagia, and
the indications for a postoperative lumbar drainage have E. Reyt, “Endonasal endoscopic closure of cerebrospinal fluid
been debated and are very controversial in the literature rhinorrhea,” Skull Base, vol. 11, no. 1, pp. 47–58, 2001.
[22, 23]. The lumbar drainage is used depending on the [12] C. Bachert, B. Verhaeghe, P. Van Cauwenberge, and J. Daele,
surgeon’s preference. We have adopted the use of the blown “Endoscopic Endonasal Surgery (EES) in skull base repairs
balloon to support the multilayer reconstruction because it and CSF leakage,” Acta Oto-Rhino-Laryngologica Belgica, vol.
counteracts gravity and the pulsations of the brain, mitigates 54, no. 2, pp. 179–189, 2000.
graft migration, and prevents development of a channel of [13] M. C. Noone, J. D. Osguthorpe, and S. Patel, “Pericranial
fluid. It is usually removed at the fifth day. flap for closure of paramedian anterior skull base defects,”
Surgical follow-up and postoperative care are always very Otolaryngology—Head and Neck Surgery, vol. 127, no. 6, pp.
494–500, 2002.
important; it includes bed rest with the head elevated 30◦ for
[14] A. Tabaee, T. L. Kassenoff, A. Kacker, and V. K. Anand, “The
2 weeks and the use of laxatives or stool softeners. In the
efficacy of computer assisted surgery in the endoscopic man-
absence of obvious infection the prevention with antibiotic agement of cerebrospinal fluid rhinorrhea,” Otolaryngology—
is fully justified but further studies are necessary to prove its Head and Neck Surgery, vol. 133, no. 6, pp. 936–943, 2005.
efficacy [24]. [15] B. George, P. Jamet, and P. Frerebeau, “Materials for osteo-
dural reconstruction in the cranium: an update,” Acta Neu-
4. Conclusions rochirurgica, vol. 35, pp. 145–151, 1989.
[16] V. K. Anand, R. K. Murali, and M. J. Glasgold, “Surgical deci-
Endonasal endoscopic approach makes it possible for a direct sions in the management of cerebrospinal fluid rhinorrhoea,”
work and total removal of ethmoidal meningoencephalo- Rhinology, vol. 33, no. 4, pp. 212–218, 1995.
celes. A nasoseptal flap allows repairing the defect and [17] B. A. Senior, K. Jafri, and M. Benninger, “Safety and efficacy of
practicing a watertight closure of the skull base reducing the endoscopic repair of CSF leaks and encephaloceles: a survey of
rate of postoperative CSF fistulae. the Members of the American Rhinologic Society,” American
Journal of Rhinology, vol. 15, no. 1, pp. 21–25, 2001.
References [18] F. S. G. Fortes, R. L. Carrau, C. H. Snyderman et al., “The
posterior pedicle inferior turbinate flap: a new vascularized
[1] P. Garg, V. Rathi, S. K. Bhargava, and A. Aggarwal, “CSF rhi- flap for skull base reconstruction,” Laryngoscope, vol. 117, no.
norrhea and recurrent meningitis caused by transethmoidal 8, pp. 1329–1332, 2007.
4 Case Reports in Medicine
[19] G. Hadad, L. Bassagasteguy, R. L. Carrau et al., “A novel recon-
structive technique after endoscopic expanded endonasal
approaches: vascular pedicle nasoseptal flap,” Laryngoscope,
vol. 116, no. 10, pp. 1882–1886, 2006.
[20] C. D. Pinheiro-Neto, D. M. Prevedello, R. L. Carrau et al.,
“Improving the design of the pedicled nasoseptal flap for skull
base reconstruction: a radioanatomic study,” Laryngoscope,
vol. 117, no. 9, pp. 1560–1569, 2007.
[21] C. H. Snyderman, A. B. Kassam, R. Carrau, and A. Mintz,
“Endoscopic reconstruction of cranial base defects following
endonasal skull base surgery,” Skull Base, vol. 17, no. 1, pp.
73–78, 2007.
[22] S. A. Shapiro and T. Scully, “Closed continuous drainage of
cerebrospinal fluid via a lumbar subarachnoid catheter for
treatment or prevention of cranial/spinal cerebrospinal fluid
fistula,” Neurosurgery, vol. 30, no. 2, pp. 241–245, 1992.
[23] R. R. Casiano and D. Jassir, “Endoscopic cerebrospinal
fluid rhinorrhea repair: Is a lumbar drain necessary?”
Otolaryngology—Head and Neck Surgery, vol. 121, no. 6, pp.
745–750, 1999.
[24] A. Kassam, A. J. Thomas, C. Snyderman et al., “Fully en-
doscopic expanded endonasal approach treating skull base
lesions in pediatric patients,” Journal of Neurosurgery, vol. 106,
supplement 2, no. 2, pp. 75–86, 2007.
Vous aimerez peut-être aussi
- Meningoencephalocele of The Temporal Bone-A Case Report: DR.B.V.N Muralidhar Reddy, DR K.V.V.RamjiDocument6 pagesMeningoencephalocele of The Temporal Bone-A Case Report: DR.B.V.N Muralidhar Reddy, DR K.V.V.RamjiNityaPas encore d'évaluation
- Transnasal Endoscopic Neochoanal TechniqueDocument4 pagesTransnasal Endoscopic Neochoanal TechniqueNalendra Tri WidhianartoPas encore d'évaluation
- Craniofacial DermoidsDocument7 pagesCraniofacial DermoidsParthiban BalaPas encore d'évaluation
- Anaesthetic Management of A Huge Occipital Meningoencephalocele in A 14 Days Old NeonateDocument4 pagesAnaesthetic Management of A Huge Occipital Meningoencephalocele in A 14 Days Old NeonateFahmil AgungPas encore d'évaluation
- An Atypical Esthesioneuroblastoma of The Sphenoid Sinus A Case ReportDocument4 pagesAn Atypical Esthesioneuroblastoma of The Sphenoid Sinus A Case ReportInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- Congenital Isolated Aplasia of Lower Lateral Cartilage and Reconstruction Using Dorsal Hump MaterialDocument3 pagesCongenital Isolated Aplasia of Lower Lateral Cartilage and Reconstruction Using Dorsal Hump MaterialDiego A. Cuadros TorresPas encore d'évaluation
- Frontoethmoidal Encephalomeningocele ChineseDocument6 pagesFrontoethmoidal Encephalomeningocele ChineseFritz TumanengPas encore d'évaluation
- Battaglia 2015Document6 pagesBattaglia 2015RathavishwarajPas encore d'évaluation
- Infection of Cranioplasty Seen Twenty Years LaterDocument3 pagesInfection of Cranioplasty Seen Twenty Years LaterGalan Budi PrasetyaPas encore d'évaluation
- Intracranial Epidermoid CystDocument3 pagesIntracranial Epidermoid CystWildaHanimPas encore d'évaluation
- Giant HyperostosisDocument6 pagesGiant Hyperostosissilvia erfanPas encore d'évaluation
- Cordom Clivus Case Report Plus Review 2017Document6 pagesCordom Clivus Case Report Plus Review 2017Ionela DumitriuPas encore d'évaluation
- Microsurgical Anatomy Brainstem Safe Entry Zones, Jns 2016Document18 pagesMicrosurgical Anatomy Brainstem Safe Entry Zones, Jns 2016Andrés SeguraPas encore d'évaluation
- Endoscopic Endonasal Reconstruction of Anterior Skull Base Defects What Factors Really Affect The OutcomesDocument8 pagesEndoscopic Endonasal Reconstruction of Anterior Skull Base Defects What Factors Really Affect The OutcomesSanooj SeyedPas encore d'évaluation
- 2021 Publication Case Report - Frontal MucoceleDocument3 pages2021 Publication Case Report - Frontal MucoceleMade RusmanaPas encore d'évaluation
- Treatment of TMJ Ankylosis in JordanianDocument7 pagesTreatment of TMJ Ankylosis in Jordanianshagun singhPas encore d'évaluation
- Medial Orbital Epidermoid Cyst: Case ReportDocument3 pagesMedial Orbital Epidermoid Cyst: Case ReportTeodorPas encore d'évaluation
- Ojolns-11 Issue-II F Color - P 11-14-Solitary Fibrous Tumors of The Nose and Paranasal Sinuses-Our ExperienceDocument4 pagesOjolns-11 Issue-II F Color - P 11-14-Solitary Fibrous Tumors of The Nose and Paranasal Sinuses-Our ExperienceDipak Ranjan NayakPas encore d'évaluation
- Annotated BibDocument19 pagesAnnotated Bibapi-252208553Pas encore d'évaluation
- External Fixation of Unstable, Flail Nasal FracturesDocument7 pagesExternal Fixation of Unstable, Flail Nasal FracturesAnonymous LnWIBo1GPas encore d'évaluation
- An Embedded Earring Backing in The Tragus: Otoscopic ClinicDocument3 pagesAn Embedded Earring Backing in The Tragus: Otoscopic Clinicxoleoni97Pas encore d'évaluation
- Bilateral Nasolabial Cyst MarcoviceanuDocument4 pagesBilateral Nasolabial Cyst MarcoviceanubamsusiloPas encore d'évaluation
- Impact of Corrective Rhinologic Surgery On Rhinogenic HeadacheDocument4 pagesImpact of Corrective Rhinologic Surgery On Rhinogenic HeadacheSinan Kadir AltunalPas encore d'évaluation
- Epidermoid Cysts TNEDocument10 pagesEpidermoid Cysts TNEbello_england_209552Pas encore d'évaluation
- Craniofacial Encephalocele: Updates On Management: Amelia Alberts, Brandon Lucke-WoldDocument13 pagesCraniofacial Encephalocele: Updates On Management: Amelia Alberts, Brandon Lucke-Woldhidayat adi putraPas encore d'évaluation
- Surgical Management of Meningioma en Plaque: January 1999Document6 pagesSurgical Management of Meningioma en Plaque: January 1999Bhisma D. SyaputraPas encore d'évaluation
- Transnasal Prelacrimal Approach To The Inferior Intraconal Space: A Feasibility StudyDocument6 pagesTransnasal Prelacrimal Approach To The Inferior Intraconal Space: A Feasibility Studythanh nguyenPas encore d'évaluation
- Transcranial EndosDocument4 pagesTranscranial EndosbenedettoPas encore d'évaluation
- Trifonia Astri Fergaus B - Eposter Frontoethmoidal Meningoencephalocele (Fullpaper) - EDITDocument6 pagesTrifonia Astri Fergaus B - Eposter Frontoethmoidal Meningoencephalocele (Fullpaper) - EDITtrifoniastriPas encore d'évaluation
- (10920684 - Neurosurgical Focus) Surgical Management of Trigeminal Schwannomas - Defining The Role For Endoscopic Endonasal ApproachesDocument9 pages(10920684 - Neurosurgical Focus) Surgical Management of Trigeminal Schwannomas - Defining The Role For Endoscopic Endonasal ApproachesasiyazaidiaPas encore d'évaluation
- Variations - in - Lateral - Sphenoid - Sinus - Wall - DefectsDocument4 pagesVariations - in - Lateral - Sphenoid - Sinus - Wall - DefectsChiNdy AfiSaPas encore d'évaluation
- Cers Cadwell LucDocument3 pagesCers Cadwell LucVictorioStokPas encore d'évaluation
- Intracranial Anatomical Triangles A ComprehensiveDocument17 pagesIntracranial Anatomical Triangles A ComprehensiveYusuf BrilliantPas encore d'évaluation
- Ucoceles: of The Paranasal SinusesDocument3 pagesUcoceles: of The Paranasal SinusesYohana SimanjuntakPas encore d'évaluation
- Cancers 16 00169Document14 pagesCancers 16 00169hidayat adi putraPas encore d'évaluation
- CPC IndicationsDocument5 pagesCPC IndicationsCarlos Daniel Giménez MéndezPas encore d'évaluation
- J2011.Decompressive Craniectomy Technical NoteDocument6 pagesJ2011.Decompressive Craniectomy Technical NoteKysy CodonPas encore d'évaluation
- Neha CR Patho PDFDocument3 pagesNeha CR Patho PDFmanish agrawalPas encore d'évaluation
- Mucopyocele of The Maxillary Sinus A Case StudyDocument3 pagesMucopyocele of The Maxillary Sinus A Case StudyInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- Brain AbsesDocument4 pagesBrain Absesmuthiadewi31Pas encore d'évaluation
- 2012 - Frympas G.Document8 pages2012 - Frympas G.alejandra gonzalezPas encore d'évaluation
- Multiple-Suture Nonsyndromic Craniosynostosis: Early and Effective Management Using Endoscopic TechniquesDocument9 pagesMultiple-Suture Nonsyndromic Craniosynostosis: Early and Effective Management Using Endoscopic TechniquesKiky Martha A.Pas encore d'évaluation
- Case Report: Iatrogenic Intraspinal Epidermoid CystDocument3 pagesCase Report: Iatrogenic Intraspinal Epidermoid CystWilda HanimPas encore d'évaluation
- 2014 1 Focus13569 PDFDocument7 pages2014 1 Focus13569 PDFNovia AyuPas encore d'évaluation
- Using The Endoscopic Transconjunctival and Transcaruncular Approach To Repair Combined Orbital Floor and Medial Wall Blowout FracturesDocument4 pagesUsing The Endoscopic Transconjunctival and Transcaruncular Approach To Repair Combined Orbital Floor and Medial Wall Blowout Fracturesstoia_sebiPas encore d'évaluation
- A Bent Needle Tip During Irrigation For Enchondroma of The Distal Phalanx: A New Curettage ToolDocument9 pagesA Bent Needle Tip During Irrigation For Enchondroma of The Distal Phalanx: A New Curettage ToolusmandumassarPas encore d'évaluation
- 2012 VideoDocument4 pages2012 VideoNur LaelaPas encore d'évaluation
- Dr. Manjunath Rai, Dr. Sneha Ginimav, Dr. Padmaraj Hegde: Ginwalla's Technique RevisitedDocument6 pagesDr. Manjunath Rai, Dr. Sneha Ginimav, Dr. Padmaraj Hegde: Ginwalla's Technique Revisitedabhishekjha0082Pas encore d'évaluation
- Exemplu 8Document4 pagesExemplu 8Pavel SebastianPas encore d'évaluation
- 10 1016@s00uyttgDocument5 pages10 1016@s00uyttgAstri AmaliaPas encore d'évaluation
- Case Bezold AbscessDocument3 pagesCase Bezold AbscessCarimaGhaliePas encore d'évaluation
- Pindborg Tumor Presenting in Early Adolescent - A Rare Case ReportDocument7 pagesPindborg Tumor Presenting in Early Adolescent - A Rare Case ReportIJAR JOURNALPas encore d'évaluation
- 1 s2.0 S1878875018300159 MainDocument9 pages1 s2.0 S1878875018300159 MainAlexandrePas encore d'évaluation
- International Journal of Pediatric Otorhinolaryngology: Hesham Mohammad Eladl, Shawky M. ElmorsyDocument4 pagesInternational Journal of Pediatric Otorhinolaryngology: Hesham Mohammad Eladl, Shawky M. ElmorsyTuis PreviyantiPas encore d'évaluation
- Retromandibular Approach JournalDocument4 pagesRetromandibular Approach JournalAldo AguilarPas encore d'évaluation
- Mucoceles of The Paranasal Sinuses: Uncommon Location: September 1998, Vol. 112, Pp. 840-844Document5 pagesMucoceles of The Paranasal Sinuses: Uncommon Location: September 1998, Vol. 112, Pp. 840-844Yohana SimanjuntakPas encore d'évaluation
- PosterDocument1 pagePosterRaif RizqullahPas encore d'évaluation
- Extracapsular Dissection of Deep Lobe Parotid Mass Aided by Retromandibular Vein On Imaging: Case ReportDocument6 pagesExtracapsular Dissection of Deep Lobe Parotid Mass Aided by Retromandibular Vein On Imaging: Case Reportbasem.t.jamalPas encore d'évaluation
- An Endoscopic Technique For Endodontic Surgery: VOL. 25, NO. 2, FEBRUARY 1999Document4 pagesAn Endoscopic Technique For Endodontic Surgery: VOL. 25, NO. 2, FEBRUARY 1999DrdrPas encore d'évaluation
- Surgery of the Cranio-Vertebral JunctionD'EverandSurgery of the Cranio-Vertebral JunctionEnrico TessitorePas encore d'évaluation
- 7 Adenomas Hipofisarios PDFDocument5 pages7 Adenomas Hipofisarios PDFOmar Lopez ArbolayPas encore d'évaluation
- 5 Ensayo Clinico PDFDocument7 pages5 Ensayo Clinico PDFOmar Lopez ArbolayPas encore d'évaluation
- 7 Adenomas Hipofisarios PDFDocument5 pages7 Adenomas Hipofisarios PDFOmar Lopez ArbolayPas encore d'évaluation
- 1 Extended Endonasal Endoscopic Approach PDFDocument5 pages1 Extended Endonasal Endoscopic Approach PDFOmar Lopez ArbolayPas encore d'évaluation
- Write A Program in C To Check Whether A Entered Number Is Positive, Negative or ZeroDocument10 pagesWrite A Program in C To Check Whether A Entered Number Is Positive, Negative or ZeroSabin kandelPas encore d'évaluation
- UNIT 1 Previewing and PredictingDocument8 pagesUNIT 1 Previewing and PredictingRisa nurlailiPas encore d'évaluation
- Legend of September 2019 MagazineDocument40 pagesLegend of September 2019 MagazineAswathi ThatchinamoorthiPas encore d'évaluation
- Characteristics of Pop CultureDocument3 pagesCharacteristics of Pop Culturekhimamad02Pas encore d'évaluation
- Inph 13Document52 pagesInph 13kicaPas encore d'évaluation
- Albert Einstein's Riddle - With Solution Explained: October 19, 2009 - AuthorDocument6 pagesAlbert Einstein's Riddle - With Solution Explained: October 19, 2009 - Authorgt295038Pas encore d'évaluation
- 3RD Last RPHDocument5 pages3RD Last RPHAdil Mohamad KadriPas encore d'évaluation
- Indian School Bousher Final Term End Exam (T2) : Academic Session - 2021-22 Grade: 7Document7 pagesIndian School Bousher Final Term End Exam (T2) : Academic Session - 2021-22 Grade: 7Shresthik VenkateshPas encore d'évaluation
- Due Books List ECEDocument3 pagesDue Books List ECEMadhumithaPas encore d'évaluation
- Duck 2019Document52 pagesDuck 2019Adrian BAGAYANPas encore d'évaluation
- UNIT VI. Gunpowder and ExplosivesDocument6 pagesUNIT VI. Gunpowder and ExplosivesMariz Althea Jem BrionesPas encore d'évaluation
- Assertiveness FinlandDocument2 pagesAssertiveness FinlandDivyanshi ThakurPas encore d'évaluation
- 211-05 Steering Column SwitchesDocument13 pages211-05 Steering Column SwitchesMiguel AngelPas encore d'évaluation
- ISO 9001 QuizDocument4 pagesISO 9001 QuizGVS Rao0% (1)
- Bed BathDocument6 pagesBed BathKristil ChavezPas encore d'évaluation
- Comparative Study of The Prison System in India, UK and USADocument12 pagesComparative Study of The Prison System in India, UK and USAHarneet Kaur100% (1)
- Ppivspiandpi G.R. No. 167715 November 17, 2010 Petitioner Respondents: Pfizer, Inc. and Pfizer (Phil.) Inc., TopicDocument26 pagesPpivspiandpi G.R. No. 167715 November 17, 2010 Petitioner Respondents: Pfizer, Inc. and Pfizer (Phil.) Inc., TopicMc Whin CobainPas encore d'évaluation
- Exeter: Durance-Class Tramp Freighter Medium Transport Average, Turn 2 Signal Basic Pulse BlueDocument3 pagesExeter: Durance-Class Tramp Freighter Medium Transport Average, Turn 2 Signal Basic Pulse BlueMike MitchellPas encore d'évaluation
- Research Methods in Accounting & Finance Chapter 5Document27 pagesResearch Methods in Accounting & Finance Chapter 5bikilahussenPas encore d'évaluation
- How To Format Your Business ProposalDocument2 pagesHow To Format Your Business Proposalwilly sergePas encore d'évaluation
- Child Health Services-1Document44 pagesChild Health Services-1francisPas encore d'évaluation
- AP Online Quiz KEY Chapter 8: Estimating With ConfidenceDocument6 pagesAP Online Quiz KEY Chapter 8: Estimating With ConfidenceSaleha IftikharPas encore d'évaluation
- Financial Accounting Theory Craig Deegan Chapter 7Document9 pagesFinancial Accounting Theory Craig Deegan Chapter 7Sylvia Al-a'maPas encore d'évaluation
- Effect of Perceived Work Environment On Employees' Job Behaviour and Organizational EffectivenessDocument10 pagesEffect of Perceived Work Environment On Employees' Job Behaviour and Organizational EffectivenessTanvee SharmaPas encore d'évaluation
- Chessboard PDFDocument76 pagesChessboard PDFAlessandroPas encore d'évaluation
- Snap Fasteners For Clothes-Snap Fasteners For Clothes Manufacturers, Suppliers and Exporters On Alibaba - ComapparelDocument7 pagesSnap Fasteners For Clothes-Snap Fasteners For Clothes Manufacturers, Suppliers and Exporters On Alibaba - ComapparelLucky ParasharPas encore d'évaluation
- Geotagging ManualDocument93 pagesGeotagging ManualAlthea AcasPas encore d'évaluation
- Global Slump: The Economics and Politics of Crisis and Resistance by David McNally 2011Document249 pagesGlobal Slump: The Economics and Politics of Crisis and Resistance by David McNally 2011Demokratize100% (5)
- CHP 11: Setting Goals and Managing The Sales Force's PerformanceDocument2 pagesCHP 11: Setting Goals and Managing The Sales Force's PerformanceHEM BANSALPas encore d'évaluation
- McEwan Pacific Student Scholarship 1374 RegulationsDocument2 pagesMcEwan Pacific Student Scholarship 1374 RegulationsHaitelenisia Hei'ululua KAMAPas encore d'évaluation