Académique Documents
Professionnel Documents
Culture Documents
ATOTW 136 Major Haemorrhage Part 1 2009
Transféré par
viaereaCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
ATOTW 136 Major Haemorrhage Part 1 2009
Transféré par
viaereaDroits d'auteur :
Formats disponibles
Sign up to receive ATOTW weekly – email worldanaesthesia@mac.
com
MANAGEMENT OF MAJOR HAEMORRHAGE
PART ONE: INITIAL RESPONSE
ANAESTHESIA TUTORIAL OF THE WEEK 136
1ST JUNE 2009
Katrina Webster (Senior Registrar in Anaesthesia)
Royal Hobart Hospital, Tasmania, Australia.
Correspondence to katrina.webster@dhhs.tas.gov.au
CLINICAL CASE
A 26 year old female presents to the emergency department (ED) with sudden onset severe abdominal pain.
She is also feeling generally unwell and dizzy.
The patient states she is 8 weeks pregnant.
On arrival in ED her blood pressure (BP) is 80/60 mmHg and heart rate (HR) is 85 bpm. Fluid
resuscitation with 4 litres of crystalloid solution begins immediately.
‘FAST’ ultrasound scan (focused abdominal sonography in trauma) shows a large amount of free fluid in
the peritoneal cavity. Bedside pelvic ultrasound performed by the obstetrician is suggestive of ectopic
pregnancy although an intrauterine pregnancy is also seen (Heterotropic ectopic pregnancy).
The patient is booked for an urgent laparotomy, and arrives in theatre 15 minutes later.
On arrival in the OT her BP is 65/45 mmHg and her HR is 125 bpm. SaO2 99% 2L O 2. The patient is
pale, drowsy and difficult to rouse.
• Anaesthetic given: RSI Induction (40mg propofol, 80mg suxamethonium), 3mg midazolam,
metaraminol infusion to maintain mean arterial pressure.
• Routine monitoring (pulse oximetry, non-invasive blood pressure, capnography, ECG and gas
analysis).
• Forced air warmer, blood warmer and constant temperature monitoring are used.
• An arterial line is placed for continuous invasive BP monitoring.
• Massive transfusion: 8 units (cross matched) RBC, 4 FFP, 8 cryoprecipitate. Transfusion begun
within 5 minutes of anaesthesia induction.
Surgical findings are: a gestational sac in right fallopian tube (eroded through a blood vessel) with 3 litres
of blood in the pelvis. The ectopic pregnancy is removed and surgery is complete within 40 minutes.
The patient is transferred to Intensive Care and is ventilated for 12 hours. She is extubated, then transferred
to the ward the next day and discharged home two weeks later with a viable intrauterine pregnancy.
QUESTIONS
Before continuing, try to answer the following questions.
The answers can be found at the end of the article.
1. What is hypovolaemic shock?
2. What is the normal blood volume for an 80kg man? What about for a 60kg woman?
3. What clinical signs are used to assess the degree of blood loss?
4. What are the main goals of initial management of massive haemorrhage?
5. What blood products can be used in severe haemorrhage?
ATOTW 136. Management of major haemorrhage –Part 1, 01/06/2009 Page 1 of 6
Sign up to receive ATOTW weekly – email worldanaesthesia@mac.com
6. What are the main complications from massive haemorrhage?
ASSESSING DEGREE OF BLOOD LOSS: PHYSIOLOGICAL RESPONSE
• Shock: inadequate tissue perfusion for metabolic requirements and the associated physiological response.
• Hypovolaemic shock: inadequate tissue perfusion due to reduced circulating blood volume.
• Normal blood volume is 70mls/kg. That is 4-5L total blood volume (TBV) for an average sized adult
female and 5-6L for an average sized adult male.
• Loss of over 40% of blood volume is immediately life threatening1.
• Massive transfusion (commonly used definitions include): 1. An entire blood volume within a 24 hour
period. 2. >50% of blood volume within 3 hours.
• Assessment is a combination of clinical signs and measured blood loss.
• Tachycardia and pallor are key early signs of significant haemorrhage. Severe haemorrhage is indicated
by hypotension, altered consciousness and oliguria. Clinical signs are a very important indicator of
volume status.
• Blood loss can be observed and measured. Visible blood loss is often overestimated and non-visible
blood loss such as retroperitoneal or long bone bleeding can be difficult to quantify2. In the operating
theatre blood loss is monitored by close observation of blood in suction equipment and on drapes, and is
measured by collection and weighing of blood soaked swabs.
• Keep in mind that medications can cause alteration from normal response patterns. For example β-
adrenoceptor antagonists can make heart rate an unreliable sign, while vasodilator drugs including ACE
inhibitors and calcium channel antagonists can lead to an exaggerated hypotensive response.
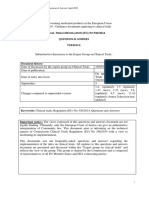
Table 1: Baskett’s classification of hypovolaemic shock3.
CLASS I CLASS II CLASS III CLASS IV
Blood Loss:
-% total blood volume (TBV) <15% TBV 15-30% TBV 30-40% TBV >40% TBV
-Absolute volume (70kg male) 750mls 800-1500mls 1500-2000mls >2000mls
Blood pressure:
Unchanged Normal Reduced Very low
-systolic
Unchanged Raised (narrow Reduced Very low
-diastolic
pulse pressure)
Mild 100-120 >120 (reduced >120 (very
Heart rate (bpm)
tachycardia volume) weak)
Normal Slow (> 2 sec) Slow (> 2 sec) Undetectable
Capillary refill
Normal Normal Tachypnoea Tachypnoea
Respiratory rate (>20/min) (>20/min)
>30 ml/hr 20-30 ml/hr 10-20 ml/hr 0-10 ml/hr
Urine output
Normal Pale Pale Pale and cold
Extremities
Normal Pale Pale Ashen
Colour
Alert Anxious/ Anxious, Drowsy,
Mental state aggressive aggressive or confused or
drowsy unconscious
ATOTW 136. Management of major haemorrhage –Part 1, 01/06/2009 Page 2 of 6
Sign up to receive ATOTW weekly – email worldanaesthesia@mac.com
ANAESTHETIC CONSIDERATIONS
• High concentration oxygen therapy ensures maximum oxygen saturation of haemoglobin and increased
plasma dissolved oxygen. Oxygen may also cause some constriction of peripheral vessels, which may
help maintain blood pressure.
• Fluid therapy is used to restore adequate circulating volume. It is important to understand the properties
of each fluid option and it’s relevant distribution after administration. For example 0.9% saline is a
common choice of crystalloid in resuscitation, however it can contribute to acidosis if large volumes are
given (hyperchloraemic acidosis). Start with 20mls/kg of crystalloid while the degree of blood loss is
assessed. Consider the use of further crystalloids, colloids, red blood cells and coagulation factors based
on clinical situation and potential complications.
• Hb/Hct levels do not fall for several hours after acute major blood loss.
• In haemorrhage, Hb concentration is strongly related to plasma volume. Care should be taken when
interpreting the Hb concentration, as it can be misleading if used to judge blood loss or the need for blood
replacement. For example, a healthy euvolaemic patient may have a normal Hb concentration of 13g/dl.
After 1 litre of blood loss (thus decreasing total volume of both haemoglobin and plasma) this patient
may maintain a Hb concentration of 13g/dl. After replacement of the 1 litre blood loss with crystalloid
solution this patient can have a restored circulating intravascular volume but their Hb concentration may
drop to 9g/dl. Hb concentrations can be misleadingly high prior to resuscitation and fall rapidly during
fluid therapy2.
• Evidence suggests that a Hb concentration of 7-9g/dl is acceptable for non-bleeding critically ill patients.
Transfusing to a Hb concentration of 8-10g/dl provides a safety buffer for further bleeding 2. Patients with
heart disease should be kept at the upper end of this range.
• Drugs which cause vasodilation or reduce cardiac output (eg. induction agents, neuraxial anaesthesia)
may worsen hypotension and further impair tissue oxygenation.
• Smaller doses of anaesthetic agents are required to produce the usual clinical effect due to a higher
proportion of blood flow going to vital organs.
• Hypothermia is avoided through use of warmed IV fluids/blood, forced air warmers, minimising patient
exposure, a warm theatre environment and warm surgical irrigation.
• Risk management needs to consider both the direct risk of hypovolaemia and the secondary risks of
massive transfusion.
• Source control is often important in minimising the blood loss. If haemorrhage is ongoing, there should
be no delay in achieving operative assessment and operative control of bleeding.
• Current evidence suggests the optimal blood pressure to achieve prior to source control is a mean arterial
pressure (MAP) of 60-70mmHg. This will maintain organ perfusion while avoiding unnecessary blood
loss from damaged vessels. More aggressive restoration of normal blood pressure is achieved after
source control is established2.
INITIAL MANAGEMENT OF MASSIVE HAEMORRHAGE
• Good management requires cooperation and communication between all team members (anaesthetist,
surgeon, haematologist, blood bank staff, and theatre assistants).
• Intraoperative management of hypovolaemia is coordinated by the anaesthetist.
Good clinical management involves understanding of the physiology of blood loss and appropriate
resuscitation, as well as good logistical organisation in a potentially stressful and chaotic environment.
Advance warning where possible is very valuable, as this allows for adequate preparation. It is important
to maximise staffing levels and to delegate roles. Good communication is essential.
If there is more that one anaesthetist and two or more anaesthetist assistants, the role delegation might
include the following:
ATOTW 136. Management of major haemorrhage –Part 1, 01/06/2009 Page 3 of 6
Sign up to receive ATOTW weekly – email worldanaesthesia@mac.com
1. Principal anaesthetist to coordinate resuscitation
2. Second anaesthetist to focus on the anaesthetic (specifically airway, anaesthesia drug
administration, and monitor progress of vital signs).
3. First anaesthetic assistant to aid airway management, provision of required drugs, provision of
equipment for venous/arterial access, double checking blood products prior to transfusion.
4. Second anaesthetic assistant to supervise delivery of blood products (including warming devices,
transfusion machines, and documentation of blood products administered).
5. A hospital orderly (where available) is very useful for collecting blood products and delivering
them to the theatre as required.
• Goals of management are: haemostasis, restoration of circulating blood volume, and blood component
replacement.
Table 2: Guideline for management of massive blood loss (adapted from reference 1).
GOALS INTERVENTIONS
Initial Restore Insert wide bore cannula(s), consider central venous pressure
management circulating blood monitoring, consider swan sheath or other large volume infusion
volume. catheter.
Keep patient warm, give oxygen at high FiO2.
Give adequate volumes of crystalloid solution, give blood
Organise an replacement (up to 2 units O neg blood if extreme emergency and
effective team. cross match not available).
Maintain MAP > 60mmHg and urine output > 30mls/hr.
Contact appropriate personnel (senior anaesthetist, clinician/surgeon
Stop the bleeding. responsible for the patient, haematologist and blood transfusion
service).
Urgent surgical, radiological or obstetric intervention to stop the
bleeding.
Blood Order lab FBC, PT, APTT, fibrinogen.
replacement investigations. Blood cross match sample.
therapy Request Electrolytes and blood gases (arterial line is helpful).
appropriate red Repeat FBC, PT, APTT and fibrinogen every 4 hours or after 1/3
cells. blood volume replacement.
Request platelets. Ensure correct sample and correct blood product for correct patient.
Request FFP. Use cell salvage, blood warmer and rapid infusion device if
Request available.
cryoprecipitate. Use O neg, group specific, or fully cross matched blood depending
on the urgency of transfusion and time to delivery of the blood.
Platelets and FFP used to minimize coagulopathy, aim for PT and
APTT <1.5 x control mean. Cryoprecipitate used to replace factor
VIII and fibrinogen, aim for fibrinogen >1.0g litre-1.
Other Minimise Monitor for DIC and treat underlying cause if possible.
considerations complications Treat acidosis, hypothermia, and hypocalcaemia.
from massive
transfusion
ATOTW 136. Management of major haemorrhage –Part 1, 01/06/2009 Page 4 of 6
Sign up to receive ATOTW weekly – email worldanaesthesia@mac.com
BLOOD PRODUCTS
Best practice will consider use of RBC, platelets, FFP and cryoprecipitate to achieve Hct above 24%,
platelets above 50 x109 litre-1 and fibrinogen above 0.5-1.0g litre-1.
Packed Red Blood Cells
Packed red cells are produced by removing 150-200ml citrated plasma from a whole unit of blood, and
have a shelf life of approximately 35 days. In extreme emergencies O Rh negative blood may be used
while awaiting a cross matched blood supply (in males and post menopausal females O Rh positive or
negative blood may be used as risk of sensitisation and haemolytic disease of the newborn does not apply).
Blood group specific transfusion should be given at the earliest opportunity.
Whole Blood
This is blood prior to fractionation into individual components and it has a shelf life of 35 days. 70ml of
citrate preservative is added to 420ml of blood. Whole blood for transfusion is generally only used in
centres where blood fractionation into component products is not possible.
Platelets
Platelets are removed from the plasma component of whole blood and they have a shelf life of 3-5 days.
Platelets above 50 x109 litre-1 are required to prevent excessive bleeding risk and a higher level of 100 x10 9
litre-1 has been recommended in patients with high energy trauma or central nervous system injury. Platelet
count should be measured at least every 4 hours or after 1/3 blood volume replaced. Initial dose is 4-8
platelet concentrates. Six units usually increases the platelet count by 20-30 x109 litre-1. Anticipating
platelet requirement and advance platelet request may be necessary to ensure availability when required.
Fresh Frozen Plasma
FFP is produced by freezing plasma and it lasts for one year. It requires thawing prior to use. FFP contains
all the coagulation factors. Coagulation factor depletion is the primary cause of coagulopathy in the setting
of major haemorrhage. Fibrinogen falls first (reaching the critical level of 1.0 g litre -1 after 150% blood
loss) and later there is a fall in other clotting factors to 25% activity after 200% blood loss1. Use of FFP
should be considered after approximately one blood volume has been lost. Aim for PT and APTT <1.5 x
control mean. The recommended initial dose is 10-15mls/kg. Sufficient quantity of FFP will correct
fibrinogen and most coagulation factor deficiencies but large volumes are often required. If fibrinogen
levels remain critically low (below 1.0 g litre-1) after FFP has been given, cryoprecipitate infusion should be
considered.
Cryoprecipitate
Cryoprecipitate is obtained by rapidly thawing FFP and separation of cryoprecipitate from albumin/factor
IX/immunoglobulins. It is then stored frozen and thawed immediately prior to use. Cryoprecipitate is rich
in factor VIII and fibrinogen. In acute haemorrhage, aim for fibrinogen >1.0g litre-1.
Recombinant activated factor VII (rFVIIa)
rFVIIa was originally developed to treat bleeding in haemophiliacs with antibodies to factor VIII and IX..
Factor VIIa enhances thrombin generation on the surfaces of platelets. It is a very expensive product and is
not licensed for use in acute traumatic haemorrhage. There have been several case reports demonstrating
dramatic improvements in the setting of acute haemorrhage, however no randomized controlled trial has yet
been published to investigate this application5. While clinical use may be promising, the dosing and
clinical indications for use are currently under examination4.
Antifibrinolytics
A large amount of evidence supports the use of antifibrinolytics to treat bleeding in elective general and
cardiac surgery4 and they may also be useful in trauma patients. This includes tranexamic acid, ε-
aminocaproic acid and aprotinin. The risk of precipitated thrombosis and other complications must be
considered.
ATOTW 136. Management of major haemorrhage –Part 1, 01/06/2009 Page 5 of 6
Sign up to receive ATOTW weekly – email worldanaesthesia@mac.com
CONCLUSION
The outcome from massive transfusion has improved over time. This is likely due to active warming
measures, aggressive correction of coagulopathy, and decreased operative times for initial surgery. New
drugs such as recombinant factor VIIa have increased pharmacologic control over ongoing bleeding,
although data is conflicting regarding the long term effect on outcome.
Prevention and management of later complications of massive haemorrhage such as coagulopathy, acidosis,
hypothermia and death are important considerations, and will be discussed in detail in a later tutorial of the
week.
IMPORTANT POINTS
• Loss of over 40% of total blood volume is immediately life
threatening.
• Clinical signs can give a good indication of degree of blood
loss.
• The main management goals in major haemorrhage are:
haemostasis, restoration of circulating volume, and blood
volume replacement.
ANSWERS TO QUESTIONS
1. Hypovolaemic shock is inadequate tissue perfusion due to reduced circulating blood volume.
2. Normal blood volume is 70mls/kg. That is 5600ml total blood volume for an 80kg person and
4200ml for a 60kg person.
3. Clinical signs to assess extent of blood loss include; blood pressure, heart rate, capillary refill,
respiratory rate, urine output, mental state, colour of extremities and complexion.
4. The main goals of initial management of massive haemorrhage are haemostasis, restoration of
circulating blood volume, and blood component replacement.
5. Blood products used in severe haemorrhage include red blood cells, fresh frozen plasma, and
cryoprecipitate. Albumin, antifibrinolytics and recombinant Factor VIIa are sometimes used.
6. The main complications from massive haemorrhage include coagulopathy, acidosis, hypothermia
and death.
REFERENCES and FURTHER READING
1. Stainsby D, MacLennan S, Hamilton PJ. Management of massive blood loss: a template guideline. Br. J.
Anaesth. 2000;85;487-491.
2. Marcela C. ABC of transfusion. 4th ed. Wiley-Blackwell; 2009.
3. Baskett PJ. ABC of major trauma. Management of hypovolaemic shock. BMJ. 1990;300;1453-1457.
4. Spahn DR, Cerny V, Coats TJ, et al. Management of bleeding following major trauma: a European
guideline. Crit Care. . 2007;11;R17.
5. Spahn DR, Tucci MA, Makris M. Editorial: Is recombinant FVIIa the magic bullet in the treatment of
major bleeding? Br. J. Anaesth. 2005;94;553-555.
ATOTW 136. Management of major haemorrhage –Part 1, 01/06/2009 Page 6 of 6
Vous aimerez peut-être aussi
- Defining Autism PDFDocument266 pagesDefining Autism PDFTihomir Rajčić100% (3)
- Disruptive Mood Dysregulation Disorder: Florian Daniel Zepf, Caroline Sarah Biskup, Martin Holtmann, & Kevin RunionsDocument17 pagesDisruptive Mood Dysregulation Disorder: Florian Daniel Zepf, Caroline Sarah Biskup, Martin Holtmann, & Kevin RunionsPtrc Lbr LpPas encore d'évaluation
- Lymphbuster Version 1.0 PDFDocument395 pagesLymphbuster Version 1.0 PDFDiana MariaPas encore d'évaluation
- Vasopressor & InotropesDocument44 pagesVasopressor & InotropesArun KumarPas encore d'évaluation
- High Yield Surgery Compatible VersionDocument77 pagesHigh Yield Surgery Compatible VersionManish K100% (1)
- Hypertensiveemergencies RullDocument60 pagesHypertensiveemergencies RullagustinaPas encore d'évaluation
- Mrs. Bagent 1-9 BWAKANANG SHETDocument5 pagesMrs. Bagent 1-9 BWAKANANG SHETaaron tabernaPas encore d'évaluation
- Combat Anesthesia - The First 24 Hours 1st Edition PDFDocument608 pagesCombat Anesthesia - The First 24 Hours 1st Edition PDFviaerea100% (1)
- Cardiovascular Nursing NotesDocument17 pagesCardiovascular Nursing NotesLucky GomezPas encore d'évaluation
- Antenatal & Postnatal Care: 1. General InformationDocument7 pagesAntenatal & Postnatal Care: 1. General InformationanishnithaPas encore d'évaluation
- ShockDocument53 pagesShockHassan Ahmed100% (3)
- Bls - Fbao - First AidDocument172 pagesBls - Fbao - First AidMaria Regina Castro Gabriel100% (1)
- Anand's Human Anatomy For Dental Students, 3rd EditionDocument762 pagesAnand's Human Anatomy For Dental Students, 3rd Editionviaerea100% (4)
- Hypovolemic ShockDocument8 pagesHypovolemic ShockLyka Flores100% (1)
- Past Years SNQ Answer by RCSIDocument47 pagesPast Years SNQ Answer by RCSIhelamahjoubmounirdmo100% (1)
- PK of Drug OverdoseDocument32 pagesPK of Drug OverdoseviaereaPas encore d'évaluation
- HypertensionDocument57 pagesHypertensionmers puno100% (5)
- Nursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Document9 pagesNursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Gayu Patel100% (2)
- Sepsis: Pathophysiology and Management in The ICUDocument38 pagesSepsis: Pathophysiology and Management in The ICUprashsubbuPas encore d'évaluation
- MedicalDocument456 pagesMedicalSri Sakthi Sumanan100% (1)
- Cerebrospinal Fluid: Physical Characteristic and Composition of The Cerebrospinal FluidDocument5 pagesCerebrospinal Fluid: Physical Characteristic and Composition of The Cerebrospinal FluiderickPas encore d'évaluation
- 1-And 2-Rescuer Adult BLS With AED Skills Testing Sheet: BLS For Healthcare Providers CourseDocument2 pages1-And 2-Rescuer Adult BLS With AED Skills Testing Sheet: BLS For Healthcare Providers CoursefjnPas encore d'évaluation
- Hemodynamics Basic Concepts 1204053445109897 4Document115 pagesHemodynamics Basic Concepts 1204053445109897 4valeriesolidum100% (1)
- Medical Education A History in 100 ImagesDocument236 pagesMedical Education A History in 100 ImagesviaereaPas encore d'évaluation
- Nursing Care Plan for Fluid Volume DeficitDocument9 pagesNursing Care Plan for Fluid Volume DeficitGayu Patel0% (1)
- IV Fluid TherapyDocument28 pagesIV Fluid Therapyansuh2250% (2)
- Acute Trauma Care:: ShockDocument45 pagesAcute Trauma Care:: ShockGeoffrey100% (1)
- 136 Management of Major Haemorrhage Part 1Document6 pages136 Management of Major Haemorrhage Part 1fitrah fajrianiPas encore d'évaluation
- Konsep Dasar Dan Prinsip Resusitasi Cairan Pada SyokDocument28 pagesKonsep Dasar Dan Prinsip Resusitasi Cairan Pada SyokraraPas encore d'évaluation
- What Is Fluid Therapy?Document42 pagesWhat Is Fluid Therapy?Mirel YdianPas encore d'évaluation
- What Is Fluid Therapy?Document42 pagesWhat Is Fluid Therapy?Mirel YdianPas encore d'évaluation
- Blood and Blood Products: Presenter: TAN LI LIAN Supervisor: DR AMINDocument15 pagesBlood and Blood Products: Presenter: TAN LI LIAN Supervisor: DR AMINNur Amin MuhammadPas encore d'évaluation
- ShockDocument27 pagesShockyashmodi5555Pas encore d'évaluation
- 23 Anaesthesia For Emergency SurgeryDocument7 pages23 Anaesthesia For Emergency SurgeryAtuy NapsterPas encore d'évaluation
- Paradoxical Bradycardia in A Patient With HaemorrhDocument6 pagesParadoxical Bradycardia in A Patient With HaemorrhBÁCH NGUYỄN ĐẮCPas encore d'évaluation
- IV Fluid TherapyDocument28 pagesIV Fluid TherapyJacinta MaryPas encore d'évaluation
- Pemicu 1 KGD: Muhammad Fahmi Rosyadi 405140220Document137 pagesPemicu 1 KGD: Muhammad Fahmi Rosyadi 405140220fahmi rosyadiPas encore d'évaluation
- Definition of ShockDocument29 pagesDefinition of Shockrazan asadPas encore d'évaluation
- Fluid Management & Shock ResuscitationDocument35 pagesFluid Management & Shock ResuscitationAmel MelatiPas encore d'évaluation
- Pcol Cover To CoverDocument214 pagesPcol Cover To CoverJec OcampoPas encore d'évaluation
- داتا حيداشر محاضرة فسيولوجىDocument6 pagesداتا حيداشر محاضرة فسيولوجىMohaned MokhtarPas encore d'évaluation
- Cardio Genic ShockDocument6 pagesCardio Genic ShockDedy HartantoPas encore d'évaluation
- Stop BleedingDocument26 pagesStop BleedingANNEPas encore d'évaluation
- Angela Heithaus, MD, PS Internal Medicine Seattle Healing Arts CenterDocument32 pagesAngela Heithaus, MD, PS Internal Medicine Seattle Healing Arts CenterMarwan M.Pas encore d'évaluation
- Haemorrhagic Shock, Resuscitation and HaemodynamicsDocument31 pagesHaemorrhagic Shock, Resuscitation and HaemodynamicsNinaPas encore d'évaluation
- Cardiac Content WyattDocument90 pagesCardiac Content WyattAnni BarbaPas encore d'évaluation
- Upper Gastrointestinal Bleeding 2007Document43 pagesUpper Gastrointestinal Bleeding 2007Matthew ThompsonPas encore d'évaluation
- Anesthetic Consideration in Hypertensive PatientDocument11 pagesAnesthetic Consideration in Hypertensive PatientYosiAsmaraPas encore d'évaluation
- Shock: Principles of Management: Nathan W. Mick, MD Massachusetts General Hospital Brigham and Women's HospitalDocument21 pagesShock: Principles of Management: Nathan W. Mick, MD Massachusetts General Hospital Brigham and Women's Hospitalifan zulfantriPas encore d'évaluation
- Pleno Pakar Blok EmergencyDocument30 pagesPleno Pakar Blok EmergencyakhomanPas encore d'évaluation
- Emergency Fluid Therapy in Companion Animals - PPitneyDocument9 pagesEmergency Fluid Therapy in Companion Animals - PPitneyUmesh GopalanPas encore d'évaluation
- Note On Cardiopulmonary Physiotherapy PDFDocument16 pagesNote On Cardiopulmonary Physiotherapy PDFTsz Kwan CheungPas encore d'évaluation
- Shock PDFDocument15 pagesShock PDFWenny AgustinPas encore d'évaluation
- Blood Pressure: By: Saiyed Falakaara Assistant Professor Department of Pharmacy Sumandeep VidyapeethDocument26 pagesBlood Pressure: By: Saiyed Falakaara Assistant Professor Department of Pharmacy Sumandeep VidyapeethFalak AaraPas encore d'évaluation
- 5 - Hypovolaemic ShockDocument7 pages5 - Hypovolaemic ShockmksharmaaPas encore d'évaluation
- Hypertension: Margaret Xaira R. Mercado RNDocument36 pagesHypertension: Margaret Xaira R. Mercado RNMargaret Xaira Rubio MercadoPas encore d'évaluation
- Shock Pathophysiology: Basic Cardiac PhysiologyDocument4 pagesShock Pathophysiology: Basic Cardiac PhysiologyChynthea ParamithaPas encore d'évaluation
- M&m-Hypovolemic ShockDocument29 pagesM&m-Hypovolemic ShockAyen FornollesPas encore d'évaluation
- Nursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)Document9 pagesNursing Care Plan: Fluid Volume Deficit R/T Active Fluid Loss (Increased Urine Output)ghellersPas encore d'évaluation
- Upper GI Bleed by Wajid MunirDocument49 pagesUpper GI Bleed by Wajid MunirAtifPas encore d'évaluation
- Dr. Sunatrio - Management Hypovolemic ShockDocument59 pagesDr. Sunatrio - Management Hypovolemic ShockArga Putra SaboePas encore d'évaluation
- Curs Prim Ajutor 2023 - MG An V - Șocul Hemoragic - English-1Document18 pagesCurs Prim Ajutor 2023 - MG An V - Șocul Hemoragic - English-1hulia jokoPas encore d'évaluation
- Approach To ShockDocument40 pagesApproach To ShockDivesh NaiduPas encore d'évaluation
- Acute Myocardial InfarctionDocument13 pagesAcute Myocardial InfarctionSajjad KabirPas encore d'évaluation
- Haemorrhagic Shock: Kareena (Grp:45)Document33 pagesHaemorrhagic Shock: Kareena (Grp:45)ShivamPas encore d'évaluation
- Sepsis: Pathophysiology and Management in The ICU: Moderator: DR Kavita Rani Sharma Presenter: Dr. PrashanthDocument38 pagesSepsis: Pathophysiology and Management in The ICU: Moderator: DR Kavita Rani Sharma Presenter: Dr. Prashanthprashsubbu100% (1)
- SurgDocument8 pagesSurgJudi Townsend100% (1)
- Hypovolemic Shock: General Surgery Orientation Medical Student Lecture SeriesDocument33 pagesHypovolemic Shock: General Surgery Orientation Medical Student Lecture Seriesatdi777Pas encore d'évaluation
- Caso Clínico 4D Equipo 8Document14 pagesCaso Clínico 4D Equipo 8Raymundo Cisneros HernandezPas encore d'évaluation
- KGD 1 VivianDocument101 pagesKGD 1 VivianVivian SaputraPas encore d'évaluation
- Anaesthetic Management in Obstetric Haemorrhage: DR B.Srikanth Iindyrpg Dept. of AnaesthesiaDocument34 pagesAnaesthetic Management in Obstetric Haemorrhage: DR B.Srikanth Iindyrpg Dept. of AnaesthesiaEDI CPas encore d'évaluation
- Prediction of Lean Body Mass From Height and Weight 1966Document3 pagesPrediction of Lean Body Mass From Height and Weight 1966viaereaPas encore d'évaluation
- Structural Modifications of Human Albumin in Diabetes 2012Document8 pagesStructural Modifications of Human Albumin in Diabetes 2012viaereaPas encore d'évaluation
- Urgencias MetabolicasDocument11 pagesUrgencias MetabolicasviaereaPas encore d'évaluation
- Bleeding Is Out, Your Own Blood Is in 2014Document4 pagesBleeding Is Out, Your Own Blood Is in 2014viaereaPas encore d'évaluation
- Formulas de PesoDocument4 pagesFormulas de PesoviaereaPas encore d'évaluation
- Pharmacology of ShockDocument4 pagesPharmacology of ShockviaereaPas encore d'évaluation
- Crecimiento y Desarrollo PediaDocument369 pagesCrecimiento y Desarrollo PediaviaereaPas encore d'évaluation
- Understanding ASV Therapy - MorganDocument77 pagesUnderstanding ASV Therapy - MorganviaereaPas encore d'évaluation
- Lactancia - Materna en MéxicoDocument21 pagesLactancia - Materna en MéxicoviaereaPas encore d'évaluation
- Pharmacology of ShockDocument4 pagesPharmacology of ShockviaereaPas encore d'évaluation
- The Clinical Pharmacology of Intranasal L MethamphetamineDocument9 pagesThe Clinical Pharmacology of Intranasal L MethamphetamineviaereaPas encore d'évaluation
- Massive Haemorrhage PPT en PDFDocument18 pagesMassive Haemorrhage PPT en PDFviaereaPas encore d'évaluation
- Malignant Hyperthermia AlorithmDocument2 pagesMalignant Hyperthermia AlorithmviaereaPas encore d'évaluation
- Transfusion in Trauma SCARE 2012Document6 pagesTransfusion in Trauma SCARE 2012viaereaPas encore d'évaluation
- Physical Principles of Clinical Measurements 1966Document14 pagesPhysical Principles of Clinical Measurements 1966viaereaPas encore d'évaluation
- ATOTW 921 Major Haemorrhage in Paediatric SurgeryDocument3 pagesATOTW 921 Major Haemorrhage in Paediatric SurgeryviaereaPas encore d'évaluation
- ROBERTS Et Al 1988 AnaesthesiaDocument4 pagesROBERTS Et Al 1988 AnaesthesiaviaereaPas encore d'évaluation
- Statius Muller MCV RCT Arch 2003Document4 pagesStatius Muller MCV RCT Arch 2003viaereaPas encore d'évaluation
- Circuits and SystemsDocument10 pagesCircuits and SystemsviaereaPas encore d'évaluation
- Carbon DioxideDocument9 pagesCarbon DioxideviaereaPas encore d'évaluation
- The Story of The GaugeDocument7 pagesThe Story of The GaugeviaereaPas encore d'évaluation
- 529 2527 1 PBDocument6 pages529 2527 1 PBviaereaPas encore d'évaluation
- AlgorithmACLS Tachycardia 200612Document1 pageAlgorithmACLS Tachycardia 200612YassarPas encore d'évaluation
- BurosumabDocument8 pagesBurosumabutamiprakosoPas encore d'évaluation
- ICU HandoverDocument2 pagesICU HandoverMark 'Mark Douglas' DouglasPas encore d'évaluation
- Sepsis Content Concepts MapDocument2 pagesSepsis Content Concepts Mapghodghod1230% (1)
- Laporan Ok Prof Budhi Jaya - Cory RettaDocument3 pagesLaporan Ok Prof Budhi Jaya - Cory RettaCory Monica MarpaungPas encore d'évaluation
- Iron Deficiency Anemia and Megaloblastic Anemia - Samson-Cruz MDDocument47 pagesIron Deficiency Anemia and Megaloblastic Anemia - Samson-Cruz MDMiguel Cuevas DolotPas encore d'évaluation
- Thallophytes 2Document32 pagesThallophytes 2Starnley TemboPas encore d'évaluation
- Reverse Optic Capture of The SingleDocument10 pagesReverse Optic Capture of The SingleIfaamaninaPas encore d'évaluation
- Rosemont Health Center Rev01Document7 pagesRosemont Health Center Rev01Amit VishwakarmaPas encore d'évaluation
- Femoral Fractures in Children: Surgical Treatment. Miguel Marí Beltrán, Manuel Gutierres, Nelson Amorim, Sérgio Silva, JorgeCoutinho, Gilberto CostaDocument5 pagesFemoral Fractures in Children: Surgical Treatment. Miguel Marí Beltrán, Manuel Gutierres, Nelson Amorim, Sérgio Silva, JorgeCoutinho, Gilberto CostaNuno Craveiro LopesPas encore d'évaluation
- Regulation5362014 Qa enDocument143 pagesRegulation5362014 Qa enmeiPas encore d'évaluation
- Balcom Rebecca Functional ResumeDocument2 pagesBalcom Rebecca Functional Resumeapi-360266135Pas encore d'évaluation
- Drug Study HydrocodoneDocument1 pageDrug Study HydrocodoneYlrenne DyPas encore d'évaluation
- Systematic Reviews of Interventions Following Physical Abuse: Helping Practitioners and Expert Witnesses Improve The Outcomes of Child Abuse, UK, 2009Document6 pagesSystematic Reviews of Interventions Following Physical Abuse: Helping Practitioners and Expert Witnesses Improve The Outcomes of Child Abuse, UK, 2009Beverly TranPas encore d'évaluation
- ns3360 Lesson Plans Spring2014Document11 pagesns3360 Lesson Plans Spring2014api-232466940Pas encore d'évaluation
- How To Make Your Own Starecta (Gelb Splint)Document18 pagesHow To Make Your Own Starecta (Gelb Splint)Martín T.Pas encore d'évaluation
- IP Sterility TestingDocument6 pagesIP Sterility TestingVarghese100% (3)
- Jubilant Life Sciences Receives ANDA Approval For Rosuvastatin Calcium Tablets (Company Update)Document3 pagesJubilant Life Sciences Receives ANDA Approval For Rosuvastatin Calcium Tablets (Company Update)Shyam SunderPas encore d'évaluation
- Toxic Metabolic Encephalopathy John W. Melton, M.DDocument17 pagesToxic Metabolic Encephalopathy John W. Melton, M.DabdalkhalidPas encore d'évaluation
- Procedure ListDocument20 pagesProcedure ListsoyrolandoPas encore d'évaluation
- Jobs Safety Analysis for Radiography WorkDocument4 pagesJobs Safety Analysis for Radiography WorkGan KusumaPas encore d'évaluation
- TEMPLATE-B-Master-list-of-Learners-for-the-Pilot-Implementation-of-F2F-Classes-for-S.Y.-2021-2022Document7 pagesTEMPLATE-B-Master-list-of-Learners-for-the-Pilot-Implementation-of-F2F-Classes-for-S.Y.-2021-2022Resa Consigna MagusaraPas encore d'évaluation
- Functional Abdominal Cramping Pain Expert Practical Guidance 2022Document9 pagesFunctional Abdominal Cramping Pain Expert Practical Guidance 2022Mohamad MostafaPas encore d'évaluation
- Rubbing Alcohol BrochureDocument2 pagesRubbing Alcohol BrochureShabab HuqPas encore d'évaluation