Académique Documents
Professionnel Documents
Culture Documents
Nursing Care Plan For Myocardial Infarction
Transféré par
jamieboyRN88%(8)88% ont trouvé ce document utile (8 votes)
13K vues7 pagesThe client reports of chest pain radiating to the left arm and neck and back. Within 1 hour of nursing interventions, the client had improved comfort in chest. Assisting the client in quantifying pain may differentiate pre-existing and current pain patterns as well as identify complications.
Description originale:
Titre original
Nursing Care Plan for Myocardial Infarction
Copyright
© Attribution Non-Commercial (BY-NC)
Formats disponibles
DOC, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentThe client reports of chest pain radiating to the left arm and neck and back. Within 1 hour of nursing interventions, the client had improved comfort in chest. Assisting the client in quantifying pain may differentiate pre-existing and current pain patterns as well as identify complications.
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme DOC, PDF, TXT ou lisez en ligne sur Scribd
88%(8)88% ont trouvé ce document utile (8 votes)
13K vues7 pagesNursing Care Plan For Myocardial Infarction
Transféré par
jamieboyRNThe client reports of chest pain radiating to the left arm and neck and back. Within 1 hour of nursing interventions, the client had improved comfort in chest. Assisting the client in quantifying pain may differentiate pre-existing and current pain patterns as well as identify complications.
Droits d'auteur :
Attribution Non-Commercial (BY-NC)
Formats disponibles
Téléchargez comme DOC, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 7
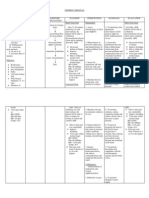
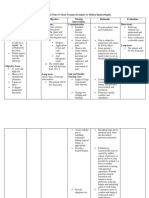
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
Subjective: Acute (Chest) STG: INDEPENDENT: STG:
Within 1 hour 1. assess 1. pain is indication of Within 1 hour of
The client Pain r/t
of nursing characteristics of MI. assisting the nursing
reports of chest myocardial chest pain, including
interventions, client in quantifying intervention, the
pain radiating to ischemia resulting location, duration,
the client will pain may differentiate client had improved
the left arm and from coronary have improved quality, intensity, pre-existing and comfort in chest, as
neck and back. artery occlusion comfort in chest, presence of radiation, current pain patterns evidenced by:
with as evidenced precipitating and as well as identify • States a
loss/restriction of by: alleviating factors, complications. decrease in the
blood flow to an • States a and as associated rating of the chest
Objective: decrease in symptoms, have pain.
area of the client rate pain on a
Restlessness myocardium and the rating of • Is able to rest,
the chest pain. scale of 1-10 and displays reduced
• Facial necrosis of the • Is able to document findings in tension, and
grimacing myocardium. nurse’s notes.
rest, displays sleeps
• Fatigue reduced 2. obtain history of 2. this provides comfortably.
• Periphera tension, and previous cardiac pain information that may • Requires
l cyanosis sleeps and familial history of help to differentiate decrease
comfortably. cardiac problems. current pain from analgesia or
• Weak
• Requires previous problems nitroglycerin.
pulse and complications.
decrease Goal was met.
• Cold and analgesia or
clammy skin nitroglycerin. 3. assess respirations, 3. respirations may LTG:
• Palpitatio BP and heart rate with be increased as a The client had an
LTG: each episodes of result of pain and improved feeling of
ns chest pain.
The client will associate anxiety. control as evidenced
• Shortnes have an 4. maintain bedrest 4. to reduce oxygen by verbalizing a
s of breath improved feeling during pain, with consumption and sense of control
• Elevated of control as position of comfort, demand, to reduce over present
maintain relaxing competing stimuli and
temperature evidenced by situation and future
verbalizing a environment to reduces anxiety. outcomes within 2
• Pain promote calmness.
sense of control days of nursing
scale of 8/10 over present intervention.
situation and Goal was met.
future outcomes 5. prepare for the 5.pain control is a
within 2 days of administration of priority, as it
nursing medications, and indicates ischemia.
interventions. monitor response to
drug therapy. Notify
physician if pain does
not abate.
6.istruct patient in 6. to decrease
nitroglycerin SL myocardial oxygen
administration after demand and workload
hospitalization. on the heart.
Instruct patient in
activity alterations
and limitations.
7. to promote
7. instruct knowledge and
patient/family in compliance with
medication effects, therapeutic regimen
side-effects, and to alleviate fear
contraindications and of unknown.
symptoms to report.
DEPENDENT: 1. serial ECG and stat
1. obtain a 12-lead ECGs record changes
ECG on admission, that can give
then each time chest evidence of further
pain recurs for cardiac damage and
evidence of further location of MI.
infarction as
prescribed.
2. Morphine is the
2. administer drug of choice to
analgesics as ordered, control MI pain, but
such as morphine other analgesics may
sulfate, meferidine of be used to reduce
Dilaudid N. pain and reduce the
workload on the
heart.
3. administer beta-
blockers as ordered. 3. to block
sympathetic
stimulation, reduce
heart rate and lowers
4. administer calcium- myocardial demand.
channel blockers as 4. to increase
ordered. coronary blood flow
and collateral
circulation which can
decrease pain due to
ischemia.
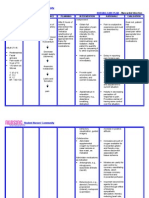
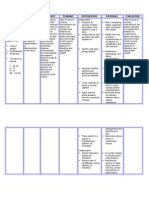
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
INDEPENDENT:
Subjective: Activity STG: 1. monitor heart rate, 1.changes in VS assist STG:
rhythm, respirations with monitoring
The client Intolerance Within 3 days and blood pressure for physiologic responses to
Within 3 days of
reports of r/t cardiac of nursing abnormalities. Notify increase in activity. nursing
increased dysfunction, interventions, physician of significant interventions,
work of changes in the client will be changes in VS. the client tolerated
breathing oxygen able to tolerate 2. Alleviation of factors activity without
2. Identify causative that are known to create
associated supply and activity without factors leading to intolerance can assist with
excessive dyspnea
with feelings consumption excessive intolerance of activity. development of an and had been able
of weakness as dyspnea and will activity level program. to utilize breathing
and tiredness. evidenced be able to utilize 3. encourage patient to 3. to help give the patient techniques and
by shortness breathing assist with planning a feeling of self-worth and energy
activities, with rest well-being.
Objective: of breath. techniques and periods as necessary. conservation
Increased energy 4. instruct patient in 4. to decrease energy techniques
heart rate conservation energy conservation expenditure and fatigue. effectively.
Increased techniques techniques. Goal was met.
effectively. 5. assist with active or 5.to maintain joint
blood pressure
passive ROM exercises mobility and muscle tone.
Dyspnea with at least QID. LTG:
exertion LTG: 6.to improve respiratory Within 5 days of
Pallor Within 5 days 6. turn patient at least function and prevent skin nursing
Fatigue and of nursing every 2 hours, and prn. breakdown. interventions, the
weakness interventions, client increased
7. instruct patient in 7. to improve breathing
Decreased the client will be isometric and breathing and to increase activity and achieved
oxygen able to increase exercises. level. desired activity
saturation and achieve level,
Ischemic ECG desired activity 8. provide 8. to promote self-worth progressively, with
patient/family with and involves patient and
changes level, no intolerance
exercise regimen, with his family with self-care.
progressively, written instructions. symptoms noted,
with no such as respiratory
intolerance DEPENDENT: compromise.
symptoms 1.Assisst patient with 1. to gradually increase Goal was met.
ambulation, as ordered, the body to compensate
noted, such as
with progressive for the increase in
respiratory increases as patient’s overload.
compromise. tolerance permits.
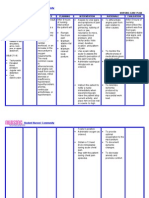
ASSESSMENT DIAGNOSIS PLANNING INTERVENTION RATIONALE EVALUATION
INDEPENDENT:
Subjective: Deficient STG: 1. monitor patient’s 1. to promote optimal STG:
readiness to learn and learning environment
The client Knowledge r/t The client will determine best methods
The client
when patient show
verbalizes new diagnosis be able to to use for teaching. willingness to learn.
verbalized and
questions and lack of verbalize and 2. provide time for 2. to establish trust. demonstrated
regarding understanding demonstrate individual interaction with understanding of
problems and of medical understanding patient. information given
3. instruct patient on 3. to provide information regarding condition,
misconceptions condition. of information procedures that may be to manage medication
about his given regarding performed. regimen and to ensure
medications, and
condition. condition, Instruct patient on compliance. treatment regimen
medications, medications, dose, within 3 days of
Objective: and treatment effects, side effects, nursing
contraindications, and
• Lack of regimen within signs/symptoms to report interventions.
4. client may need to
improvement 3 days of to physician. increase dietary Goal was met.
of previous nursing 4. instruct in dietary potassium if placed on
regimen interventions. needs and restrictions, diuretics; sodium should LTG:
such as limiting sodium be limited because of The client had
• Inadequa
or increasing potassium. the potential for fluid
te follow-up LTG: been able to
retention.
on The client will 5. provide printed 5. to provide reference correctly perform all
instructions able to correctly materials when possible for the patient and tasks prior to
given. perform all for patient/family to family to refer. discharge.
tasks prior to reviews. Goal was met.
• Anxiety
6. have patient 6. to frovide information
• Lack of discharge. demonstrate all skills that that patient has gained
understan- will be necessary for a full understanding of
ding. postdischarge. instruction.
7. instruct exercises to be 7. these are helpful in
performed, and to avoid improving cardiac
overtaxing activities. function.
DEPENDENT:
1. refer patient to cardiac 1. to provide further
rehabilitation as ordered improvement and
rehabilitation
postdischarge.
.
Vous aimerez peut-être aussi
- NCP Myocardial InfarctionDocument1 pageNCP Myocardial InfarctionjamieboyRN88% (8)
- Nursing Care Plan For Myocardial InfarctionDocument7 pagesNursing Care Plan For Myocardial Infarctionmariejo95% (125)
- Nursing Assessment and Interventions for Acute Chest PainDocument3 pagesNursing Assessment and Interventions for Acute Chest PainAjay SupanPas encore d'évaluation
- NURSING CARE PLAN For Myocardial InfarctionDocument13 pagesNURSING CARE PLAN For Myocardial Infarctionbanyenye2593% (14)
- Nursing Care Plan For Myocardial Infarction NCPDocument8 pagesNursing Care Plan For Myocardial Infarction NCPderic87% (15)
- NURSING CARE PLAN For Myocardial InfarctionDocument16 pagesNURSING CARE PLAN For Myocardial InfarctionFreisanChenMandumotan100% (1)
- MI Chest Pain AssessmentDocument5 pagesMI Chest Pain AssessmentDharline Abbygale Garvida AgullanaPas encore d'évaluation
- NURSING CARE PLAN - Myocardial Infarction Assessment Diagnosis Inference Planning Intervention Rationale EvaluationDocument4 pagesNURSING CARE PLAN - Myocardial Infarction Assessment Diagnosis Inference Planning Intervention Rationale Evaluationsweethoney220% (1)
- NCP MiDocument4 pagesNCP MiPitaca Madiam Annabehl PaulPas encore d'évaluation
- Acute Myocardial InfarctionDocument35 pagesAcute Myocardial Infarctionvirnzrobz80% (10)
- Nursing Care Plan (Septick Shock)Document6 pagesNursing Care Plan (Septick Shock)REMILYN ROSE ASUNCION67% (9)
- NCP - AnxietyDocument1 pageNCP - AnxietyNovie Carla100% (1)
- NCP for Acute Coronary Syndrome AssessmentDocument3 pagesNCP for Acute Coronary Syndrome Assessmentsarahtot67% (3)
- NCP Lung CancerDocument4 pagesNCP Lung CancerShizuen Mn83% (12)
- Care Plan Unstable AnginaDocument4 pagesCare Plan Unstable Anginaالغزال الذهبي50% (6)
- NCP For AnginaDocument5 pagesNCP For Anginacarizza_bernas100% (1)
- Nursing Care Plan - Myocardial InfarctionDocument3 pagesNursing Care Plan - Myocardial Infarctionderic80% (10)
- Myocardial Infarction NCPDocument3 pagesMyocardial Infarction NCPlapistolero33% (3)
- "Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" Nursing Care PlansDocument21 pages"Acute Coronary Syndrome Non ST Elevation Myocardial Infarction, Hypertensive Cardiovascular Disease, Diabetes Mellitus Type 2, and Community Acquired Pneumonia" Nursing Care PlansCarl Elexer Cuyugan Ano100% (1)
- NCP AnginaDocument3 pagesNCP AnginaShie LA100% (1)
- NCP - Acute Pain Related Myocardial IschemiaDocument2 pagesNCP - Acute Pain Related Myocardial IschemiaKian HerreraPas encore d'évaluation
- Angina PectorisDocument12 pagesAngina Pectorismardsz93% (14)
- NCP Acute Pain Related To Tissue Ischemia As Manifested by Changes in Level of Consciousness PDFDocument3 pagesNCP Acute Pain Related To Tissue Ischemia As Manifested by Changes in Level of Consciousness PDFOGNTVPas encore d'évaluation
- Decrease Cardiac OutputDocument6 pagesDecrease Cardiac OutputGerardeanne ReposarPas encore d'évaluation
- CP Intestinal Obstruction Nursing Care PlanDocument7 pagesCP Intestinal Obstruction Nursing Care PlanShiella Heart MalanaPas encore d'évaluation
- NCP - Tissue Perfusion (Cerebral)Document2 pagesNCP - Tissue Perfusion (Cerebral)moodlayers50% (6)
- Cues Nursing Diagnosis Scientific Rationale Goals Nursing Interventions Rationale EvaluationDocument3 pagesCues Nursing Diagnosis Scientific Rationale Goals Nursing Interventions Rationale EvaluationIngrid Nicolas100% (1)
- Coronary Artery Disease - Case StudyDocument19 pagesCoronary Artery Disease - Case StudyJulieteeySarania100% (3)
- Myocardial InfarctionDocument16 pagesMyocardial InfarctionCay Sevilla100% (4)
- Coronary Artery Disease Care PlanDocument2 pagesCoronary Artery Disease Care PlanDanelle Harrison, RN100% (2)
- Coronary Artery Diseases Case StudyDocument20 pagesCoronary Artery Diseases Case StudyPyka Izzaty67% (3)
- Nursing Care Plan For Coronary Artery DiseaseDocument3 pagesNursing Care Plan For Coronary Artery DiseaseLorraineAnneSantiagoCandelario91% (22)
- Nursing Care Plan For Myocardial InfarctionDocument7 pagesNursing Care Plan For Myocardial InfarctionRocelyn CristobalPas encore d'évaluation
- Assessment Diagnoses: Planning Intervention Rationale EvaluationDocument13 pagesAssessment Diagnoses: Planning Intervention Rationale EvaluationdaleaimeePas encore d'évaluation
- Case Study Myocardial InfarctionDocument23 pagesCase Study Myocardial InfarctionJester GalayPas encore d'évaluation
- Nursing Care Plan For Myocardial Infarction NCPDocument8 pagesNursing Care Plan For Myocardial Infarction NCPRhomyrose CampanaPas encore d'évaluation
- Assessment Diagnosis Planning Intervention Rationale EvaluationDocument6 pagesAssessment Diagnosis Planning Intervention Rationale EvaluationBalloonsRus PHPas encore d'évaluation
- ACUTE PAIN BSN III KOLCABA NCP 8th ROTATIONDocument4 pagesACUTE PAIN BSN III KOLCABA NCP 8th ROTATIONKrisheille Amano MirandaPas encore d'évaluation
- NCP - Baby Final PDFDocument11 pagesNCP - Baby Final PDFCindy MariscotesPas encore d'évaluation
- Cues and Objectives Explanation of The Problem Goals and Objectives Interventions Rationale EvaluationDocument4 pagesCues and Objectives Explanation of The Problem Goals and Objectives Interventions Rationale EvaluationShaina Fe RabaneraPas encore d'évaluation
- NCPDocument4 pagesNCPfairwoods90% (10)
- Principles of Pathophysiology - Bullock, ShaneDocument2 pagesPrinciples of Pathophysiology - Bullock, ShaneMel Izhra N. MargatePas encore d'évaluation
- College of Health Sciences Nursing Care Plan for Acute Myocardial InfarctionDocument4 pagesCollege of Health Sciences Nursing Care Plan for Acute Myocardial InfarctionLouise GudmalinPas encore d'évaluation
- NCP-Septic Shock (Acute Pain)Document3 pagesNCP-Septic Shock (Acute Pain)Ted anadiloPas encore d'évaluation
- Escoton, Kate Angel P (NCP)Document4 pagesEscoton, Kate Angel P (NCP)Kate EscotonPas encore d'évaluation
- Nursing Care Plan: Defining The Assessment Diagnosis Scientific Explanation Objectives Interventions Rationale EvaluationDocument2 pagesNursing Care Plan: Defining The Assessment Diagnosis Scientific Explanation Objectives Interventions Rationale EvaluationLovella Gonzales LimPas encore d'évaluation
- Acute Pain Management After EpisiotomyDocument3 pagesAcute Pain Management After EpisiotomyJheanAlphonsineT.MeansPas encore d'évaluation
- Final Zollinger-Ellison SyndromeDocument9 pagesFinal Zollinger-Ellison SyndromeGLYDEL CORDEROPas encore d'évaluation
- Nursing Care Plan for Labor Pain ManagementDocument3 pagesNursing Care Plan for Labor Pain ManagementFc CrisostomoPas encore d'évaluation
- St. Paul University PhilippinesDocument3 pagesSt. Paul University PhilippinesMia Grace GarciaPas encore d'évaluation
- No Data Problem Etiology Diagnosis: 1.pain Control 1. Pain ManagementDocument6 pagesNo Data Problem Etiology Diagnosis: 1.pain Control 1. Pain ManagementArjuna AnggaraPas encore d'évaluation
- Managing Acute Chest PainDocument3 pagesManaging Acute Chest PainRachelle Ann DomingoPas encore d'évaluation
- Typhoid Fever NCPDocument46 pagesTyphoid Fever NCPLyra Lustre RN67% (3)
- Diagnostic TestsDocument5 pagesDiagnostic TestsKathleen DimacaliPas encore d'évaluation
- Nursing Care for Acute Migraine PainDocument3 pagesNursing Care for Acute Migraine PainJan Lianne BernalesPas encore d'évaluation
- Ccu Cad NCPDocument5 pagesCcu Cad NCPheyyymeeePas encore d'évaluation
- NCP FormatDocument2 pagesNCP Formatheartberroya1721Pas encore d'évaluation
- Nursing Care Plans for Postpartum ClientDocument3 pagesNursing Care Plans for Postpartum ClientPauline AñesPas encore d'évaluation
- Labor Pain NCPDocument4 pagesLabor Pain NCPBea Dela Cena60% (5)
- Assessment Diagnosis Planning Intervention Rationale Evaluation Subjective Data: Short Term Goal: Independent Independent Goal MET Short Term GoalDocument2 pagesAssessment Diagnosis Planning Intervention Rationale Evaluation Subjective Data: Short Term Goal: Independent Independent Goal MET Short Term GoalHazel Mae ConcepcionPas encore d'évaluation
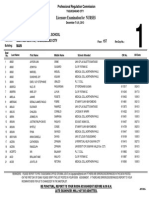
- Top 10 NLE Passers (May 2014)Document2 pagesTop 10 NLE Passers (May 2014)Coolbuster.NetPas encore d'évaluation
- December 2013 NLE Room Assignments - Iloilo CityDocument131 pagesDecember 2013 NLE Room Assignments - Iloilo CityjamieboyRNPas encore d'évaluation
- 2013 December Passers NURS1213seDocument220 pages2013 December Passers NURS1213seHarley Justiniani Dela CruzPas encore d'évaluation
- Top Schools For May 2014 NLEDocument17 pagesTop Schools For May 2014 NLECoolbuster.NetPas encore d'évaluation
- December 2013 NLE Room Assignments - ManilaDocument503 pagesDecember 2013 NLE Room Assignments - ManilajamieboyRNPas encore d'évaluation
- Dec 2013 NLE Rooms Cebu (Removal)Document1 pageDec 2013 NLE Rooms Cebu (Removal)Coolbuster.NetPas encore d'évaluation
- December 2013 NLE Room Assignments - Davao CityDocument150 pagesDecember 2013 NLE Room Assignments - Davao CityjamieboyRNPas encore d'évaluation
- List of Successful Examinees in The May 2014 Nurse Licensure ExaminationDocument225 pagesList of Successful Examinees in The May 2014 Nurse Licensure ExaminationofwwatchPas encore d'évaluation
- Nursing Care Plan - HemodialysisDocument2 pagesNursing Care Plan - HemodialysisjamieboyRN100% (2)
- December 2013 NLE Room Assignments - Examinees From Tacloban CityDocument22 pagesDecember 2013 NLE Room Assignments - Examinees From Tacloban CityjamieboyRNPas encore d'évaluation
- December 2013 NLE Room Assignments - Legazpi CityDocument53 pagesDecember 2013 NLE Room Assignments - Legazpi CityjamieboyRNPas encore d'évaluation
- PRC Room Assignment For December 2013 Nursing Board Exam - For Removals (Manila)Document1 pagePRC Room Assignment For December 2013 Nursing Board Exam - For Removals (Manila)PhilippineNursingDirectory.comPas encore d'évaluation
- PRC Program of Examination For The December 2013 Philippine Nursing Board Exam (NLE)Document2 pagesPRC Program of Examination For The December 2013 Philippine Nursing Board Exam (NLE)PhilippineNursingDirectory.comPas encore d'évaluation
- PRC Room Assignment For December 2013 Nursing Board Exam (Cebu)Document150 pagesPRC Room Assignment For December 2013 Nursing Board Exam (Cebu)PhilippineNursingDirectory.comPas encore d'évaluation
- December 2013 NLE Room Assignments - Pagadian CityDocument41 pagesDecember 2013 NLE Room Assignments - Pagadian CityjamieboyRNPas encore d'évaluation
- PRC Room Assignment For December 2013 Nursing Board Exam (Cagayan de Oro)Document103 pagesPRC Room Assignment For December 2013 Nursing Board Exam (Cagayan de Oro)PhilippineNursingDirectory.comPas encore d'évaluation
- Guidelines Nurse Deployment Project 2014Document4 pagesGuidelines Nurse Deployment Project 2014jamieboyRNPas encore d'évaluation
- December 2013 NLE Room Assignments - Zamboanga (Removal)Document1 pageDecember 2013 NLE Room Assignments - Zamboanga (Removal)jamieboyRNPas encore d'évaluation
- June 2013 NLE ResultsDocument325 pagesJune 2013 NLE ResultsjamieboyRNPas encore d'évaluation
- PRC 2014 Exam ScheduleDocument7 pagesPRC 2014 Exam ScheduleCoolbuster.NetPas encore d'évaluation
- PRC Room Assignment For December 2013 Nursing Board Exam (Tuguegarao)Document68 pagesPRC Room Assignment For December 2013 Nursing Board Exam (Tuguegarao)PhilippineNursingDirectory.comPas encore d'évaluation
- December 2013 NLE Room Assignments - PampangaDocument40 pagesDecember 2013 NLE Room Assignments - PampangajamieboyRNPas encore d'évaluation
- DOH Nurse Deployment Project 2014 Application FormDocument1 pageDOH Nurse Deployment Project 2014 Application FormjamieboyRNPas encore d'évaluation
- June 2013 NLE Topnotchers and Top SchoolsDocument19 pagesJune 2013 NLE Topnotchers and Top SchoolsCoolbuster.NetPas encore d'évaluation
- June 2013 Pharmacist Board Exam Results - Performance of SchoolsDocument2 pagesJune 2013 Pharmacist Board Exam Results - Performance of SchoolsjamieboyRNPas encore d'évaluation
- June 2013 NLE TopnotchersDocument3 pagesJune 2013 NLE TopnotchersNoypistuffPas encore d'évaluation
- June 2013 Pharmacist Board Exam Results - TopnotchersDocument1 pageJune 2013 Pharmacist Board Exam Results - TopnotchersjamieboyRNPas encore d'évaluation
- Special Professional Licensure Board Examination (SPLBE) October 2013Document2 pagesSpecial Professional Licensure Board Examination (SPLBE) October 2013jamieboyRNPas encore d'évaluation
- June 2013 Pharmacist Board Exam ResultsDocument28 pagesJune 2013 Pharmacist Board Exam ResultsjamieboyRN0% (1)
- New Sched Filing of NLE 2013 - Resolution No. 2013-14Document2 pagesNew Sched Filing of NLE 2013 - Resolution No. 2013-14jamieboyRNPas encore d'évaluation
- Cencus Thrombo Baru 2020Document14 pagesCencus Thrombo Baru 2020Wan ooPas encore d'évaluation
- Heart Disease Thesis StatementDocument6 pagesHeart Disease Thesis StatementHelpWithPaperCanada100% (2)
- Mitral StenosisDocument48 pagesMitral StenosiskornbergwiPas encore d'évaluation
- Echocardiographic Changes in The Shape and Size of The AorticDocument8 pagesEchocardiographic Changes in The Shape and Size of The AorticAristoteles Esteban Cine VelazquezPas encore d'évaluation
- Summary of High-Quality CPR Components For BLS ProvidersDocument1 pageSummary of High-Quality CPR Components For BLS ProvidersPhilippe Ceasar C. BascoPas encore d'évaluation
- Cardio Vascular System NursingDocument2 pagesCardio Vascular System NursingGade BalajiPas encore d'évaluation
- 2020 Focused Transesophageal Echocardiography During Cardiac Arrest ResuscitationDocument10 pages2020 Focused Transesophageal Echocardiography During Cardiac Arrest Resuscitationbogeg74816Pas encore d'évaluation
- Cvaa 116Document20 pagesCvaa 116elizaPas encore d'évaluation
- HypertensionDocument12 pagesHypertensionDr. PARMINDER NAINPas encore d'évaluation
- 200L FON PRESENTATION Group 1Document13 pages200L FON PRESENTATION Group 1jonaPas encore d'évaluation
- 2023 Atrial Fibrillation Guideline-at-a-Glance: Societal StatementDocument5 pages2023 Atrial Fibrillation Guideline-at-a-Glance: Societal StatementMiguel Limaylla ZapataPas encore d'évaluation
- Scientech 2351: FeaturesDocument2 pagesScientech 2351: FeaturesSudip KunduPas encore d'évaluation
- Atrial Fibrillation - Geeky MedicsDocument10 pagesAtrial Fibrillation - Geeky MedicsJahangir AlamPas encore d'évaluation
- ABPI-Ankle Brachial Pressure IndexDocument23 pagesABPI-Ankle Brachial Pressure IndexTamsi MahiPas encore d'évaluation
- 2020 Classic Lectures in Cardiac Imaging: Release Date: July 1, 2020 - 11.25 AMA PRA Category 1 Credit(s)Document4 pages2020 Classic Lectures in Cardiac Imaging: Release Date: July 1, 2020 - 11.25 AMA PRA Category 1 Credit(s)Muhammad Ahmad bin makruf syammakuPas encore d'évaluation
- Dr.T.Venkatachalam Professor of Anaesthesiology Madras Medical College, ChennaiDocument35 pagesDr.T.Venkatachalam Professor of Anaesthesiology Madras Medical College, ChennaiNailahRahmahPas encore d'évaluation
- Pi Is 0733862722000797Document12 pagesPi Is 0733862722000797Hames SeguraPas encore d'évaluation
- Algorithm For Cardiac TumorsDocument13 pagesAlgorithm For Cardiac TumorsPeter Paul PascualPas encore d'évaluation
- Excursion WorksheetDocument6 pagesExcursion Worksheetapi-348781812Pas encore d'évaluation
- Brugada Syndrome: ECG Changes and Treatment OptionsDocument34 pagesBrugada Syndrome: ECG Changes and Treatment OptionsMohammad Irfan100% (1)
- CASE STUDY PEDIA - SaavedraDocument15 pagesCASE STUDY PEDIA - SaavedraChryst Louise SaavedraPas encore d'évaluation
- Umj 1x Dovangiova 3330 1 ManuskripDocument8 pagesUmj 1x Dovangiova 3330 1 ManuskripNursaniahPas encore d'évaluation
- Module 4. Ebj. Pingul, MCDocument4 pagesModule 4. Ebj. Pingul, MCCharline PingulPas encore d'évaluation
- MCQ CvsDocument62 pagesMCQ CvsShihab AlmoliukiPas encore d'évaluation
- Protocolo FATE (Eco TT)Document4 pagesProtocolo FATE (Eco TT)darlingcarvajalduquePas encore d'évaluation
- Aortic Regurgitation PathophysiologyDocument1 pageAortic Regurgitation Pathophysiologydana100% (1)
- Clark Blue Book CARDIODocument181 pagesClark Blue Book CARDIOChristian SunurPas encore d'évaluation
- ALS Recertification CourseDocument64 pagesALS Recertification CoursePanagiotis Iliopoulos100% (1)
- Anaesthetic Crisis ManualDocument63 pagesAnaesthetic Crisis ManualkushishaPas encore d'évaluation
- How I Personalize Fluid Therapy in Septic Shock?: Review Open AccessDocument11 pagesHow I Personalize Fluid Therapy in Septic Shock?: Review Open AccessGian CarloPas encore d'évaluation