Académique Documents
Professionnel Documents
Culture Documents
Stages of Labor
Transféré par
myer pasandalanTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Stages of Labor
Transféré par
myer pasandalanDroits d'auteur :
Formats disponibles
1
STAGES OF LABOR
1st Stage: CERVICAL STAGE
a. Latent phase
b. Active phase
c. Transition phase
2nd Stage: EXPULSIVE STAGE
3rd Stage: PLACENTAL STAGE
4th Stage: IMMEDIATE POSTPARTUM
1st Stage: CERVICAL STAGE
Begins with true labor contractions & ends with complete effacement & full dilatation of
the cervix
Cervical effacement/obliteration
Shortening of the cervical canal from a length of 1-2 cm until it is paper thin
Expressed in percentage (100%)
Cervical dilatation
Enlargement / widening of the cervical opening
Expressed in cm (10 cm)
During labor, the uterus is gradually differentiated into 2 distinct portions
1. Upper uterine segment – becomes thick & active to expel out the fetus
2. Lower uterine segment - becomes thin-walled, supple & passive so that fetus can be pushed
out easily
3 Phases of the cervical stage:
a. Latent phase – early in labor
Cervical dilatation: 0-3 cm
Contractions:
Duration : 20-40 sec.
Interval : 5-10mins.
Takes up to 8 of the 12 hour first stage
b. Active / accelerated
Cervical dilatation : 4-7 cm
Contractions:
Duration : 40-60 secs
Interval : 3-5 mins
Mother should be brought to the hospital
Nursing care:
Hospital admission:
a. Obtain personal data & obstetrical data
EDC; GPA
Amount & character of show
Whether or not membranes have ruptured
b. General PE, IE, Leopold’s maneuver
c. Monitor progress of labor using the PARTOGRAPH
Assess start of labor
Monitor maternal status: BP, PR, T, uterine contractions, urine voided, vaginal bleeding
Fetal status: FHR, color of amniotic fluid
2
Facilitates early identification of delayed progress of labor
Blood Pressure: Should not be taken during a contraction (tends to increase)
Fetal Heart Rate:
Uterine soufflé - synchronizes maternal heartbeat
Location of FHS:
Vertex: R or L lower quadrant of abdomen
Breech: At or above the level of the umbilicus
FHR should not be taken during a contraction (will ↓)
For any abnormality in FHR, the first nursing action: change the mother’s position
Signs of fetal distress:
Fetal bradycardia
Tachycardia
Meconium stained Amniotic Fluid
Fetal trashing
Danger signs of labor maternal:
Blood pressure of > 140/90 or decreasing
Abnormal pulse
Inadequate or prolonged contractions
Pathologic retraction ring
Abnormal lower abdominal contour
Apprehension
d. Emotional support
Keep the patient constantly informed of the progress of labor
e. Health teachings
1. Bathing: if contractions are still tolerable
2. Mobility and position of choice
3. Allow woman to eat and drink easy to digest foods
4. Encourage the woman to void every 2-3 hours by offering a bedpan:
A full bladder retards fetal descent
Urinary stasis can lead to UTI
A full bladder may be traumatized during delivery
5. Perineal preparation: Perineal flushing; NO routine perineal shaving
6. Encourage Sim’s position (left lateral decubitus)
It favors anterior rotation of the fetal head
It prevents supine hypotensive syndrome
It promotes relaxation between contractions.
Woman in labor should not bear down unnecessarily to prevent exhaustion and cervical
edema
Relief of Pain and Discomfort during Labor
Communication - explain, inform, respect, praise, encourage, reassure
Mobility- move freely, choice of position
Urination- encourage every 2 hrs.
Breathing technique
Birth companion
When to transfer to the DR?
Primigravidas: when cervix is fully dilated or when there is bulging of the perineum
Multigravidas: 7-8 cm dilatation
3
c. Transition Phase of the cervical stage
Maximum cervical dilatation occurs
Contraction:
Intensity : Peak
Interval : 2-3 mins.
Duration : 60-90 sec.
Sudden gush of Amniotic Fluid
Show is prominent
Second Stage (Expulsive Stage)
Begins with full dilatation of the cervix & ends with delivery of the infant
Surest sign that the baby is about to be born:
o Bulging of the perineum or Crowning
THIRD STAGE: Placental Stage
Begins with the birth of the infant and ends with the delivery of the placenta
Duration:
50% of placental deliveries occur w/in 5 mins.
90% are delivered w/in 15 mins.
Mean delivery time of 8.3 mins. (WHO)
Longer that 18 mins. is asso. w/ a significant risk of postpartum hemorrhage
Longer than 30 mins., PPH occurs 6x more often
Approaches in the Management of the Third Stage of Labor:
PMSTL - Physiologic Management of the third stage of labor
AMSTL - Active Management of the third stage of labor
• Oxytocin 10 “iu” IM after delivery of the baby (exclude the possibility of a 2nd baby)
• Controlled cord traction with counter traction on the uterus
• Uterine massage
Fourth stage of Labor: Immediate Postpartum Period
- The period from delivery of the placenta until the condition of the woman has stabilized
(1-4 hours after delivery).
Routinely inspect the vulva, vagina, perineum and anus to identify genital lacerations.
Inspect the placenta and membranes.
DO NOT DO routine manual exploration of the uterine cavity.
Evaluate if the uterus is well contracted and massage the uterus at regular intervals.
Teach the woman to massage her own uterus to keep it firm. DO NOT put ice pack on
the mother’s abdomen.
Signs of readiness for BF: crawling, tonguing, rooting, sucking
Signs of good attachment:
Chin touching the breast
Mouth is wide-open
Lower lip turned upward
More areola seen above than below the mouth.
Vous aimerez peut-être aussi
- Complaint For Damages SampleDocument4 pagesComplaint For Damages SampleJubelee Anne Patangan100% (2)
- Anatomy of The Urinary System: Patient's Name / Room No. - 1Document2 pagesAnatomy of The Urinary System: Patient's Name / Room No. - 1myer pasandalanPas encore d'évaluation
- Student Assignment LoadDocument2 pagesStudent Assignment Loadmyer pasandalanPas encore d'évaluation
- Student Assignment LoadDocument2 pagesStudent Assignment Loadmyer pasandalanPas encore d'évaluation
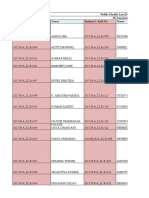
- Summary of Drugs and IVDocument2 pagesSummary of Drugs and IVmyer pasandalanPas encore d'évaluation
- Complaint For Damages SampleDocument4 pagesComplaint For Damages Samplemyer pasandalanPas encore d'évaluation
- Summary of Meds New FormatDocument2 pagesSummary of Meds New Formatmyer pasandalanPas encore d'évaluation
- Nursing Assessment IIDocument5 pagesNursing Assessment IImyer pasandalanPas encore d'évaluation
- Nursing Care Plan: Cues Nursing Diagnosis Objective Intervention Rationale EvaluationDocument3 pagesNursing Care Plan: Cues Nursing Diagnosis Objective Intervention Rationale Evaluationmyer pasandalanPas encore d'évaluation
- Risperidine: Disturbed Thought Process Related To Neurological DisturbancesDocument3 pagesRisperidine: Disturbed Thought Process Related To Neurological Disturbancesmyer pasandalanPas encore d'évaluation
- Nursing Care Plan: Cues Nursing Diagnosis Objective Intervention Rationale EvaluationDocument3 pagesNursing Care Plan: Cues Nursing Diagnosis Objective Intervention Rationale Evaluationmyer pasandalanPas encore d'évaluation
- Review of SystemDocument2 pagesReview of Systemmyer pasandalanPas encore d'évaluation
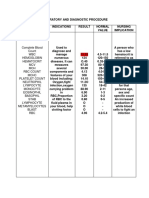
- Laboratory and Diagnostic ProcedureDocument5 pagesLaboratory and Diagnostic Proceduremyer pasandalanPas encore d'évaluation
- Diagnostic and Laboratory ProceduresDocument6 pagesDiagnostic and Laboratory Proceduresmyer pasandalanPas encore d'évaluation
- Nursing Care Plan: Cues Nursing Diagnosis Objective Intervention Rationale EvaluationDocument2 pagesNursing Care Plan: Cues Nursing Diagnosis Objective Intervention Rationale Evaluationmyer pasandalanPas encore d'évaluation
- Group F DXDocument2 pagesGroup F DXmyer pasandalanPas encore d'évaluation
- Discharge Plan: Drug/S Indication/S Dosage Route FrequencyDocument3 pagesDischarge Plan: Drug/S Indication/S Dosage Route Frequencymyer pasandalanPas encore d'évaluation
- Case Management 1Document5 pagesCase Management 1myer pasandalanPas encore d'évaluation
- Narrative PathophysiologyDocument5 pagesNarrative Pathophysiologymyer pasandalanPas encore d'évaluation
- Hemorrhagic StrokeDocument4 pagesHemorrhagic Strokemyer pasandalanPas encore d'évaluation
- Drug StudyDocument2 pagesDrug Studymyer pasandalanPas encore d'évaluation
- DKKDNDDocument14 pagesDKKDNDmyer pasandalanPas encore d'évaluation
- ConstipationDocument3 pagesConstipationmyer pasandalanPas encore d'évaluation
- Schizophrenia: I. IdentificationDocument3 pagesSchizophrenia: I. Identificationmyer pasandalanPas encore d'évaluation
- Personality DisordersDocument2 pagesPersonality Disordersmyer pasandalanPas encore d'évaluation
- Anatomy and PhysioDocument2 pagesAnatomy and Physiomyer pasandalanPas encore d'évaluation
- Drug StudyDocument2 pagesDrug Studymyer pasandalanPas encore d'évaluation
- Somatoform Disorders: I. IdentificationDocument1 pageSomatoform Disorders: I. Identificationmyer pasandalanPas encore d'évaluation
- Eating DisordersDocument1 pageEating Disordersmyer pasandalanPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- KEMH Guidelines On Cardiac Disease in PregnancyDocument7 pagesKEMH Guidelines On Cardiac Disease in PregnancyAyesha RazaPas encore d'évaluation
- Target Heart Rate Lesson PlanDocument4 pagesTarget Heart Rate Lesson PlanEryn YeskePas encore d'évaluation
- Lecture in Geriatrics Physical Therapy 1Document27 pagesLecture in Geriatrics Physical Therapy 1S.APas encore d'évaluation
- Physiological Changes Postpartum PeriodDocument2 pagesPhysiological Changes Postpartum PeriodEurielle MiolePas encore d'évaluation
- Profile of Osteopathic Practice in Spain Results FDocument11 pagesProfile of Osteopathic Practice in Spain Results FBerenice LimarkPas encore d'évaluation
- ESI ER CompleteDocument45 pagesESI ER Completetammy2121Pas encore d'évaluation
- 2016 10 12 Members Letter-HHS OCR Organ Transplant DiscriminationDocument4 pages2016 10 12 Members Letter-HHS OCR Organ Transplant DiscriminationMike Honda100% (2)
- Feeds and Feedings - Margie EranDocument29 pagesFeeds and Feedings - Margie EranAlliah Dela RosaPas encore d'évaluation
- The Diagram Shows How A Company Called HB Office RDocument1 pageThe Diagram Shows How A Company Called HB Office RbugakPas encore d'évaluation
- Fasting and Low Carb InfoDocument4 pagesFasting and Low Carb InfoKatrin NovaPas encore d'évaluation
- Pres 2 PastpapersDocument190 pagesPres 2 PastpapersOdettePas encore d'évaluation
- Regional Victoria's RoadmapDocument12 pagesRegional Victoria's RoadmapTara CosoletoPas encore d'évaluation
- Coma ManagementDocument5 pagesComa ManagementElena DocPas encore d'évaluation
- Improving Lives of South Sudanese Communities Through Water and Sanitation: The Story of Salva DutDocument1 pageImproving Lives of South Sudanese Communities Through Water and Sanitation: The Story of Salva DutUNICEF South SudanPas encore d'évaluation
- Tcharestresumefinal 1009Document2 pagesTcharestresumefinal 1009tcharestPas encore d'évaluation
- Part 4abcDocument11 pagesPart 4abcMatthew Guevarra100% (1)
- Effects of Sprint Interval Training and Body.24Document8 pagesEffects of Sprint Interval Training and Body.24Maxwell MartinsPas encore d'évaluation
- Topic ListDocument6 pagesTopic ListEdwinPas encore d'évaluation
- Asthma Case StudyDocument39 pagesAsthma Case StudyDimitris TasiouPas encore d'évaluation
- Shaikh Sohail Shaikh KaleemDocument1 pageShaikh Sohail Shaikh KaleemMantra SriPas encore d'évaluation
- Safety Pocket Guide Web 061808Document534 pagesSafety Pocket Guide Web 061808hombre911100% (1)
- (Yabanci Dil Testi) : T.C. Millî Eğitim Bakanliği Ölçme, Değerlendirme Ve Sinav Hizmetleri Genel MüdürlüğüDocument22 pages(Yabanci Dil Testi) : T.C. Millî Eğitim Bakanliği Ölçme, Değerlendirme Ve Sinav Hizmetleri Genel Müdürlüğücem kayaPas encore d'évaluation
- Is Smartphone Addiction Really An AddictionDocument17 pagesIs Smartphone Addiction Really An AddictionHani HanoyyPas encore d'évaluation
- Antiinflammatorydrugs: Beatriz Monteiro,, Paulo V. SteagallDocument19 pagesAntiinflammatorydrugs: Beatriz Monteiro,, Paulo V. SteagallYohan Oropeza VergaraPas encore d'évaluation
- Test Bank For Pharmacology A Patient Centered Nursing Process Approach 9th EditionDocument16 pagesTest Bank For Pharmacology A Patient Centered Nursing Process Approach 9th EditionMichael Pupo73% (15)
- DebateDocument12 pagesDebate•Kai yiii•Pas encore d'évaluation
- DR Daniel Samadi MD PC - Pediatric ENT NJDocument7 pagesDR Daniel Samadi MD PC - Pediatric ENT NJPediatric ENT NJ by Dr Daniel SamadiPas encore d'évaluation
- Hazard Analysis in The WorkplaceDocument7 pagesHazard Analysis in The WorkplaceUghlahnPas encore d'évaluation
- The Impact of Longitudinal Studies On Understanding Development From Young Adulthood To Old AgeDocument11 pagesThe Impact of Longitudinal Studies On Understanding Development From Young Adulthood To Old AgeLana PeharPas encore d'évaluation
- Research Chapter 1 V Final Autosaved 2 1Document57 pagesResearch Chapter 1 V Final Autosaved 2 1Mirate JessPas encore d'évaluation