Académique Documents
Professionnel Documents
Culture Documents
Diabetic Ulcer Severity Score
Transféré par
Dwi Hm HsbCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Diabetic Ulcer Severity Score
Transféré par
Dwi Hm HsbDroits d'auteur :
Formats disponibles
International Surgery Journal
Kumar ST et al. Int Surg J. 2016 Aug;3(3):1606-1610
http://www.ijsurgery.com pISSN 2349-3305 | eISSN 2349-2902
DOI: http://dx.doi.org/10.18203/2349-2902.isj20162756
Research Article
Diabetic ulcer severity score: clinical validation and outcome
Shiva Kumar T.*, Srinivas Arava, Pavan B. M., Guru Kiran C. S.,
Chandan G. B., Naveen Kumar M.
Department of General Surgery, Sri Siddharatha Medical College, Agalakote, Tumkur, Karnataka, India
Received: 14 June 2016
Accepted: 15 July 2016
*Correspondence:
Dr. Shiva Kumar T.,
E-mail: shiva123kumar.sk2@gmail.com
Copyright: © the author(s), publisher and licensee Medip Academy. This is an open-access article distributed under
the terms of the Creative Commons Attribution Non-Commercial License, which permits unrestricted non-commercial
use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
Background: Foot ulcers are a common complication of diabetes and represent a major source of morbidity.
Variation in the clinical presentation of this disease has resulted in the paucity of evidence to guide optimal clinical
management. A validated scoring system might help the clinicians and researchers in everyday assessment and
management of patients or the development and assessment of new therapies. Diabetic ulcer severity score (DUSS) is
one of the latest wound based system of classification which needs to be validated. The objective of this study was to
clinically validate diabetic ulcer severity score with patient outcome.
Methods: 100 patients were prospectively assessed from October 2012 to March 2014 for four clinical parameters -
palpable pedal pulses absence (score 1) or presence (score 0), probing to bone yes (score 1) or no (score 0). The site
of ulcer- toe (score 0) or foot (score 1) ulcer. Multiple ulcers scored as 1, single ulcers scored as 0. The DUSS was
calculated by adding these to a maximum of 4. Wounds were followed-up until healing or amputation .Kaplan-Meier
analysis; Chi- Square tests were used for statistical analysis.
Results: Analyses showed a significantly higher probability of healing for patients with palpable pulses, no probing
to bone, toe ulcers, and single ulcer. A decreasing probability of healing for absent pedal pulses, probing to bone, foot
ulcers and multiple ulcers with increasing amputation rates.
Conclusions: Lower DUSS score was strongly associated with healing and higher score with amputation.
Keywords: DUSS, Diabetic Ulcer, Healing, Amputation
INTRODUCTION depth, and presence/absence of neuropathy, infection and
peripheral arterial disease and have been used to compare
Foot ulcers are a common complication of diabetes and the outcomes.
represent a major source of morbidity. Fifteen percent of
diabetics develop foot ulcers during their life time with DUSS (diabetic ulcer severity score) is one of the latest
significant health related decrease in quality of life and wound based system of classification which needs to be
consumption of a great deal of healthcare resources.1 validated.2
A number of foot ulcer classification systems for METHODS
example, the Meggit-Wagner system and the University
of Texas systems have been devised in an attempt to Method of collection of data
categorize ulcers more effectively and thereby allow
effective comparison of the outcome of routine Total of 100 diabetic patients with diabetic foot ulcers
management in different centers and treatment strategies. attending surgical department in Sri Siddharatha Medical
These systems are variously based on the site of ulcer, its College and Hospital were recruited. The baseline
International Surgery Journal | July-September 2016 | Vol 3 | Issue 3 Page 1606
Kumar ST et al. Int Surg J. 2016 Aug;3(3):1606-1610
demographic data which included age, sex, occupation, Healing was defined as complete epithelialisation.
education status, habits, socioeconomic status and Amputation rate was defined as the percentage of patients
treatment history were taken. undergoing minor or major amputation within the
observation period. Toe or forefoot amputations were
Ulcers were labeled infected if a purulent discharge was taken as minor amputation and below or above knee
present with two other local signs (warmth, erythema, amputation were taken as major amputation.
lymphangitis, lymphadenopathy, edema, pain).
Follow up
Wound depth was evaluated using a sterile blunt probe.
The ability to probe to bone with the presence of local or These patients were followed up in the surgical outpatient
systemic infection and suggestive radiological features clinic once in fortnight for 1st month, then once in a
provided a clinical diagnosis of osteomyelitis.3 month till the ulcer healed or for a minimum period of up
to 6 months. Ulcer healing was assessed.
Peripheral vascular disease was clinically defined by the
absence of both pedal pulses, patients were categorized as Inclusion criteria
having single or multiple ulcerations on the same foot. In
patients with multiple ulcers, the wound with the highest Age limit: 20-90 years.
grading were selected for analysis. For wounds with
identical grading, the larger wound was chosen. Grading All subjects suffering from diabetes mellitus as per World
of wounds is shown in Table 1. Health Organization criteria that have foot ulcers.
Table 1: Grades of ulcer. Symptoms of diabetes plus random blood sugars
>200 mg/dl.
Wound depth as measured by (A.) Fasting blood sugars >126 mg/dl. (B.) Two hour
Ulcer grades
sterile blunt probe plasma glucose levels >200 mg/dl.
G-1 Dermis
G-2 Subcutaneous tissue Exclusion criteria
G-3 Fascia
G-4 Muscle Venous stasis ulcers with diabetes mellitus
G-5 Bone All patients with less than two follow up visits
during observation period
Unhealed ulcers were followed up for a minimum period Non diabetic neuropathic ulcers
of 6 months. Once a patient’s ulcer had healed Ulcers above the ankle
completely either by primary healing or skin grafting or a All non-diabetics with foot ulcers.
lower-limb amputation was performed, the outcome was
noted and the patient was deemed to have completed the Statistical methods
study.
Data collected was entered in Microsoft Excel
Diabetic ulcer severity score (DUSS) Professional 2010, Microsoft corporation and analyzed
using statistical package for social sciences version 20.0,
Ulcers were classified by the below mentioned variables. IBM corporation, 2011.
Diabetic ulcer severity score (DUSS) was calculated by
adding these separate grading to a theoretical maximum Descriptive statistics such as mean, SD was calculated.
of 4. Parameters and scores are shown in Table 2. Chi-square test was used as test of significance. P-value
<0.001 is considered as statistically significant.
Table 2: Diabetic ulcer severity scoring system.
RESULTS
Parameter Score 0 Score 1
Palpable pedal pulses Presence Absence In our study out of 100 patients 81 were male and 19
Probing to bone No Yes female. Most common age group affected with diabetic
Ulcer site Toes Foot foot was 51-60 years followed by 41-50 years with mean
age of study group was 57±12 years.
Ulcer number Single Multiple
Most common DUSS among study population was 1(44
Standard treatment care was given to all these patients,
patients) followed by 2 (21 patients). Peripheral pulses
which included oral hypoglycemic/insulin, health
were absent in 24 patients while probe to bone test was
education, antibiotics if necessary and regular wound
positive in 43 patients. Gangrene was present in 28
care.
patients.
International Surgery Journal | July-September 2016 | Vol 3 | Issue 3 Page 1607
Kumar ST et al. Int Surg J. 2016 Aug;3(3):1606-1610
Primary healing occurred in 55 patients and total of 45 lee et al in a Scottish study reported a mean age of 67.4
patients underwent amputation as shown in Table 3. In years.10 National hospital discharge survey, looking at
amputation group 8 were female and 37 were male. 17 275,000 inpatient records from 500 hospitals since 1996
patients underwent major amputations among which 13 revealed that elderly diabetics had twice the risk of
male and 4 female. 29 patients underwent minor developing a foot ulcer, three times the risk of developing
amputation among which 25 were male and 4 female. a foot abscess and four times the risk of developing
Osteomyelitis.11
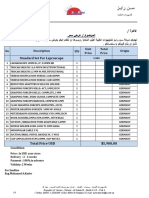
Table 3: DUSS versus clinical outcome.
In our study we have clinically validated the DUSS score
Clinical Clinical based on the eventual outcome of the wound similar to as
DUSS
outcome outcome Total shown by the study conducted by Beckert et al. They
score
Healing Amputation noted that a lower DUSS score was strongly associated
0 14 0 14 with healing.
1 37 7 44
2 4 17 21 In our study according to the Kaplan Meier analysis the
3 0 14 14 probability of healing with score 0 was 100%, 84%
4 0 7 7 probability of healing for score 1 while that of score 2
had 19 % probability of healing. Patient with DUSS 3
Total 55 45 100
and 4 had 0% probability of healing.
DUSS score was significantly associated with clinical
Beckert et al reported primarily healing of 74% (n =
outcome (P<0.001) as shown in Table 4. With every unit
1,000), Prompers et al, 77% (n = 1,229), Oyibo et al, 65%
increase in DUSS proportion of patient healing decreased
(n = 194), Jeffcoate et al, 66% (n = 449), and Gul et al,
significantly.
72% (n = 200).6,12-14
Table 4: Chi-Square tests for significance of DUSS
In our study the results showed that presence of gangrene
with clinical outcome.
in diabetic foot carries a hazard ratio of 0.351 (95% CI
0.171 - 0.718) of amputation or has a 64.9 % hazard of
Value df P value
amputation. Prompers L et al observed that peripheral
Pearson Chi- Square 63.133 4 <0.001
arterial disease and infection has a major impact on
Likelihood ratio 78.619 4 <0.001 healing rates. Armstrong et al. (University of Texas
classification system) accordingly, upon analysis of the
Kaplan Meier analysis showed that patient with DUSS of odds of non-healing per PAD × infection status, it was
0 have 100% probability of healing. DUSS of 1 had 16% only in those patients with both PAD and infection that
probability of amputation while that of 2 had 81% the odds of non-healing were markedly increased
probability of amputation. Patient with DUSS 3 and 4 had compared with those without PAD or infection.6 Jan
100% probability of amputation. Apelqvist suggested that there is a need to introduce and
recognize decreased perfusion or impaired circulation as
DISCUSSION indicator for the need of re-vascularisation in the diabetic
foot to achieve healing.15 Karthikesalingam A et al in his
Diabetic foot is a serious complication of diabetes and review of various scoring system found that infection and
also has significant socioeconomic impact.4 Diabetic foot ischemia contribute to impaired healing of ulcer.16
ulcers will complicate the disease in more than 15% of Graham lee et al in his study proved that non-infected
the people with diabetes during their lifetime.5 Prompers ulcers were more likely to heal than infected ulcers (81
L et al have reported that the lifetime risk of developing a versus 69%; P <0.02). The rate of healing for patients
foot ulcer in diabetic patients may be as high as 25%.6 In with absent pulses was similar to those with neuropathy
India, diabetic foot infection is a common cause for (89.7 versus 91.7%), but in patients who had both clinical
hospital admission among diabetic patients. Prevalence of criteria, the healing rate was significantly lower (61.2%;
foot infection in diabetic patients in India is 26%-34% P < 0.0001)10, but however Maria candida Persis using
and is caused by a number of sociocultural practices.7 the SAD classification, found that there was no difference
in outcome in presence of ischaemia.17
Most common age group affected with diabetic foot was
between 51-60 years, Second group being between 41-50 In our study, presence of probe to bone carried a hazard
years. Mean age group was 57±12 years. Range of the ratio of 0.024 (95% CI 0.005 - 0.111) of amputation or
age was 27-90 years. Similar results in various studies had 97.6% hazard of amputation (95% CI 88.9% -
conducted by Viswanathan et al where mean age was 99.5%) than absence of probe to bone. Karthikesalingam
60.6 years, Prompers L et al, a mean age of 64.7 years, A et al also in assessment of various scoring system
Deribe B et al a mean age of 50.7 years, was seen.6-8 showed that depth of ulcer had an impact on healing
Paul, et al in a multicenter trial over three continents, ofulcer.16 lee G et al suggested that depth of ulcer as one
found similar finding of mean age of 66.7 years.9 Graham of the major predictors in healing of ulcer, Maria candida
International Surgery Journal | July-September 2016 | Vol 3 | Issue 3 Page 1608
Kumar ST et al. Int Surg J. 2016 Aug;3(3):1606-1610
Persis proved that there is significant differences in terms Early Minor amputation can prevent a later major
of healing were observed for depth of ulcer amputation.20 Seven (15.90%) of 44 patients with score 1
(p<0.002).10,17 had minor amputation, 14 (66.66 %) of 21 patients with
score 2 had minor amputation, 10 (71.42 %) of 14
Diabetes related lower limb major amputation rates patients with score 3 had minor amputations, 3 (42.85 %)
reported by Prompers L et al was 5%. Jeffcoate et al also of 7 patients with score 4 had minor amputations. Minor
reported an amputation rate of 5%. In a German cohort, amputations were more common in patients with DUSS
Beckert et al found major amputation rates of 3%, Score of 2 in our study.
although the data as presented in that report cannot be
easily compared because of their unique classification When the DUSS score was compared with the proportion
system. Oyibo et al also found similar rates of major of individuals undergoing amputation it was noted that a
amputation of 5% in their cohort, Jan Apelqvist total of 3 (14.28 %) of 21 people with score 2, 4
suggested that an infection in the diabetic foot is a limb- (28.57%) of 14 people with score 3, 4 (57.14%) of 7
threatening condition and was the immediate cause for people with score 4 had major amputations in our study.
amputation in 25-50% of diabetic patients.6,15 None of the patients with score 0, 1 had major
Karthikesalingam A, in his systematic review of scoring amputation.
systems for diabetic foot ulcers he found that surgical
removal of bone is required in up to 27% of these patients In the original study by Beckert et al patients with a score
with 0.5-5 per 1000 progressing to major amputation16. of 0 had no risk of major amputation, while patients with
Graham lee et al in a Scottish study found 12% of a score of 1 had a 2.4%, patients with a score of 2 had a
patients required major or minor amputation10 Maria 7.7%, patients with a score of 3 had an 11.2%, and
candida Persis in a Brazilian study reported that 12% of patients with a score of 4 had a 3.8%.In comparison in
patients underwent amputation.17 our present study none of the patients with score 0, 1 and
2 had major amputation, 16 (30.2%) of 53 people with
Margolis et al conducted a cohort study of 24,616 score 3 had major amputations; 19 (55.9%) out of 34
individuals with a diabetic neuropathic foot ulcer treated people with score 4 had major amputations.
within a multicenter wound care network.18 Total of 1653
(6.7%) individuals had an amputation and 46.3% of these CONCLUSION
amputations were of a toe or ray (minor amputation). In
the more than 10-year follow-up period, the percentage of DUSS scoring system provides an easy diagnostic tool
those who had an amputation varied between 5.6% and for predicting probability of healing or amputation by
8.4%. Of those who had an amputation, the percentage combining four clinically assessable wound based
that had a minor amputation increased over time from parameters. Study groups can be stratified depending on
4.0% in the earliest years to more than 60% in the later severity of ulcers and thus can help provide a simple,
years of observation. streamlined approach in clinical setting without need of
any advanced investigative tool, but it does not alter the
Overall 45 (45.0%) of 100 people had amputations in our procedure of wound management.
study. Major amputation (below - or above-knee
amputation) was done for 11.0 % and minor Amputation Lower DUSS score was strongly associated with healing
(toe or forefoot amputations) was done in 34.0 % of and higher score with amputation. Any lasting medical
patients which is higher as compared to previous studies. treatment or healing course is doomed without patient
This can be attributed to lower socio- economic status of involvement. Regular foot examinations are important in
majority of patients included in our study, which is detecting co-morbid pre-ulcerative calluses. Surgeon
supported by Kington and Smith theory that economics practices, techniques, team work, care strategies still
may play a role in list of complications.19 Wachtel MS demonstrate the best results.
has also found in his study that comparisons of
amputation rates have not been fully performed with ACKNOWLEDGEMENTS
specific regard to family poverty and diet, proper
footwear, appropriate assessment of foot injuries and Authors would like to thank heartfully all our patients
timely medical interventional impact the probability of a without whom this study could not be done. Authors also
lower-extremity amputation.19 thank Mr. Prakash for his clerical work. I thank the
librarian for his co-operation.
Most commonly ulcers were of DUSS Score of 1
followed by Score 2. Mean score was 1.56±1.113. 7 Funding: No funding sources
(9.4%) out of 44 people with score 1 had amputations, 17 Conflict of interest: None declared
(25.5%) out of 21 people with score 2 had amputations, Ethical approval: The study was approved by the
14 (90.6%) out of 14 people with score 3 had institutional ethics committee
amputations, 7 (100.0%) out of 7 people with score 4 had
amputations.
International Surgery Journal | July-September 2016 | Vol 3 | Issue 3 Page 1609
Kumar ST et al. Int Surg J. 2016 Aug;3(3):1606-1610
REFERENCES specialist foot clinic. Diabetes care.
2007;30(8):2064-9.
1. The Expert Committee on the diagnosis and 11. Reed JF. An audit of lower extremity complication in
management of diabetes mellitus. Report of the patients with diabetes mellitus. International Journal
expert committee on the diagnosis and management Lower Extremity Wounds. 2004;3:161-4.
of diabetes mellitus. Diabetes Care. 12. Oyibo SO, Jude EB, Tarawneh I, Nguyen HC,
1997;20(7);1183-97. Armstrong DG, Harkless LB, et al. The effects of
2. Beckert S, Witte M, Wicke C, Königsrainer A, ulcer size and site, patient’s age, sex and type and
Coerper S. A new wound-based severity score for duration of diabetes on the outcome of diabetic foot
diabetic foot ulcers. Diabetes Care. 2006;29:988-92. ulcers. Diabet Med. 2001;18:133-8.
3. Petrova NL, Foster AV, Edmonds ME. Difference in 13. Jeffcoate WJ, Chipchase SY, Ince P, Game FL.
presentation of Charcot osteoarthropathy in type 1 Assessing the outcome of the management of
compared with type 2 diabetes. Diabetes Care. diabetic foot ulcers using ulcer-related and person-
2004;27:1235-6. related measures. Diabetes Care. 2006;29:1784-7.
4. Kleopatra A, Doupis J. Management of diabetic foot 14. Gul A, Basit A, Ali SM, Ahmadani MY. Role of
ulcers. Diabetes Therapy. 2012:(3)1:4. wound classification in predicting the outcome of
5. Kalaivani V, Vijay Kumar HM. Short diabetic foot ulcer. J Pak Med Assoc. 2006;56:444-7.
communication diabetic foot in India. Reviewing the 15. Apelqvist, Jan. Diagnostics and treatment of the
Epidemiology and the Amit Jain’s. Sch Acad J diabetic foot. Endocrine. 2012;41(3):384-97.
Biosci. 2013;1(6):305-8. 16. Karthikesalingam A, Holt PJ, Moxey P, Jones KG,
6. Prompers L, Schaper N, Apelqvist J, Edmonds M, Thompson MM, Hinchliffe RJ. A systematic review
Jude E, Mauricio D, et al. Prediction of outcome in of scoring systems for diabetic foot ulcers. Diabetic
individuals with diabetic foot ulcers: focus on the Medicine. 2010;57(5):544-9.
differences between individuals with and without 17. Parisi MC, Zantut-Wittmann DE, Pavin EJ, Machado
peripheral arterial disease. The Eurodiale Study. H, Nery M, Jeffcoate WJ. Comparison of three
Diabetologia. 2008;51(5):747-55. systems of classification in predicting the outcome of
7. Viswanathan V, Madhavan S, Rajasekar S, diabetic foot ulcers in a Brazilian population.
Chamukuttan S, Ambady R. Urban-rural differences European Journal of Endocrinology.
in the prevalence of foot complications in South- 2008;159(4):417-22.
Indian diabetic patients. Diabetes care. 18. Margolis DJ, Allen-Taylor L, Hoffstad O. Diabetic
2006;29(3):701-3. neuropathic foot ulcers and amputation. Wound
8. Deribe BK, Michael W, Nemera G. Prevalence and Repair Regen. 2005;13:230-6.
factors influencing diabetic foot ulcer among diabetic 19. Wachtel MS. Family poverty accounts for
patients attending Arbaminch hospital, South differences in lower-extremity amputation rates of
Ethiopia. J Diabetes Metab. 2014;5(1):2-7. minorities 50 years old or more with diabetes. J Natl
9. Ince P, Abbas ZG, Lutale JK, Basit A, Ali SM, Med Assoc. 2005;97(3):334-8.
Chohan F, et al. Use of SINBAD classification 20. Buckley CM, Ali F, Roberts G, Kearney PM, Perry
System and score in comparing outcome of foot ulcer IJ, Bradley CP. Timing of access to secondary
management on three continents. Diabetes Care. healthcare services for diabetes management and
2008;31;964-7. lower extremity amputation in people with diabetes:
10. Leese G, Schofield C, McMurray B, Libby G, a protocol of a case–control study. BMJ open.
Golden J, MacAlpine R, et al. Scottish foot ulcer risk 2013;3(10):e003871.
score predicts foot ulcer healing in a regional
Cite this article as: Kumar ST, Arava S, Pavan
BM, Guru Kiran CS, Chandan GB, Kumar NM.
Diabetic ulcer severity score: clinical validation
and outcome. Int Surg J 2016;3:1606-10.
International Surgery Journal | July-September 2016 | Vol 3 | Issue 3 Page 1610
Vous aimerez peut-être aussi
- Tenis OpiniDocument2 pagesTenis OpiniDwi Hm HsbPas encore d'évaluation
- Absensi Retaker UKDIDocument14 pagesAbsensi Retaker UKDIDwi Hm HsbPas encore d'évaluation
- Thoracoabdominal WoundsDocument4 pagesThoracoabdominal Woundscahaya tinggiPas encore d'évaluation
- Extraction of Curcumin PDFDocument16 pagesExtraction of Curcumin PDFFranz Wensten100% (2)
- Infeccion Del Sitio Qx2017Document8 pagesInfeccion Del Sitio Qx2017Galo GarcìaPas encore d'évaluation
- ProcalcitoninDocument9 pagesProcalcitoninDwi Hm HsbPas encore d'évaluation
- Booklet Muktamar Xi Peraboi 2018Document9 pagesBooklet Muktamar Xi Peraboi 2018Dwi Hm HsbPas encore d'évaluation
- Booklet Muktamar Xi Peraboi 2018 PDFDocument4 pagesBooklet Muktamar Xi Peraboi 2018 PDFDwi Hm HsbPas encore d'évaluation
- Abstract DR Tommy Kuswara IndonesiaDocument1 pageAbstract DR Tommy Kuswara IndonesiaDwi Hm HsbPas encore d'évaluation
- Booklet Muktamar Xi Peraboi 2018Document4 pagesBooklet Muktamar Xi Peraboi 2018Dwi Hm HsbPas encore d'évaluation
- Extraction of Curcumin PDFDocument16 pagesExtraction of Curcumin PDFFranz Wensten100% (2)
- The Effect of A Separate Stream For Minor Injuries On Accident and Emergency Department Waiting TimesDocument3 pagesThe Effect of A Separate Stream For Minor Injuries On Accident and Emergency Department Waiting TimesDwi Hm HsbPas encore d'évaluation
- Effect of Extracts From Phyllanthus Watsonii Airy Shaw On Cell Apoptosis inDocument2 pagesEffect of Extracts From Phyllanthus Watsonii Airy Shaw On Cell Apoptosis inDwi Hm HsbPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5784)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Medical 1 PDFDocument5 pagesMedical 1 PDFsuresh balajiPas encore d'évaluation
- Anesthesia challenges in robotic surgeryDocument186 pagesAnesthesia challenges in robotic surgeryjaymebcPas encore d'évaluation
- Press Release 06 2014 enDocument1 pagePress Release 06 2014 enPrashant SalviPas encore d'évaluation
- Appendicitis and Peritonitis 1Document21 pagesAppendicitis and Peritonitis 1chrisyenPas encore d'évaluation
- External Causes of Morbidity and MortalityDocument12 pagesExternal Causes of Morbidity and Mortalitynahna iPas encore d'évaluation
- General Surgery Lecture - 1Document18 pagesGeneral Surgery Lecture - 1lhundren santosPas encore d'évaluation
- Fusion of The Lumbar Spine. A Consideration of The IndicationsDocument12 pagesFusion of The Lumbar Spine. A Consideration of The IndicationsCristina Galvez PerezPas encore d'évaluation
- The Intraoperative Patient: by Lisa M. Dunn RN, MSN/ED, CCRNDocument52 pagesThe Intraoperative Patient: by Lisa M. Dunn RN, MSN/ED, CCRNrahmaya100% (1)
- Standard Set For LaproscopeDocument1 pageStandard Set For LaproscopewaleedalihamzahPas encore d'évaluation
- Test Bank Adult Health Nursing 7th Edition Cooper GosnellDocument15 pagesTest Bank Adult Health Nursing 7th Edition Cooper GosnellCarolina Chapman100% (29)
- Anesthesia Interest Group 4th Year AdviceDocument13 pagesAnesthesia Interest Group 4th Year Adviceadidassocr321Pas encore d'évaluation
- A Client With A Brain Tumor: Nursing Care PlanDocument1 pageA Client With A Brain Tumor: Nursing Care Planshabatat2002Pas encore d'évaluation
- Final List EMP 01.02.2022Document34 pagesFinal List EMP 01.02.2022Gulshan NaddaPas encore d'évaluation
- KUST Nursing Internship Logbook GuideDocument9 pagesKUST Nursing Internship Logbook Guidesarhang talebaniPas encore d'évaluation
- Kshara PDFDocument8 pagesKshara PDFVineet NavrangPas encore d'évaluation
- Rguhs Thesis Topics in OrthopaedicsDocument6 pagesRguhs Thesis Topics in Orthopaedicsjanetrobinsonjackson100% (1)
- Female To Male Gender Correction Surgery in IndiaDocument52 pagesFemale To Male Gender Correction Surgery in IndiaDr Narendra KaushikPas encore d'évaluation
- A Report On Clinical Rotation January 2023Document14 pagesA Report On Clinical Rotation January 2023charles juma100% (1)
- Patterns of Weight Change in Infants With Congenital Heart DiseasDocument152 pagesPatterns of Weight Change in Infants With Congenital Heart DiseasvaradanPas encore d'évaluation
- JCI HandbookDocument88 pagesJCI Handbookksbabar100% (10)
- Top 5 Complications of GonadectomyDocument7 pagesTop 5 Complications of GonadectomyCabinet VeterinarPas encore d'évaluation
- List of Empanelled HCOs - CGHS Meerut As On 29 July 2021Document11 pagesList of Empanelled HCOs - CGHS Meerut As On 29 July 2021delhidelhidubaiPas encore d'évaluation
- Iris Suture Set Hattenbach EDocument2 pagesIris Suture Set Hattenbach Eophtho india incPas encore d'évaluation
- Clpna Self-Assessment ToolDocument9 pagesClpna Self-Assessment Toolapi-306022321Pas encore d'évaluation
- IFIC BookDocument392 pagesIFIC BookMaria Santiniaratri100% (1)
- CB Insights - Industries Disrupted by AlphabetDocument71 pagesCB Insights - Industries Disrupted by AlphabetСергейPas encore d'évaluation
- The Preservation RhinoplastyDocument3 pagesThe Preservation RhinoplastyEvy Larousse33% (3)
- Cardiothoracic Products CatalogDocument24 pagesCardiothoracic Products Catalogmihalcea alinPas encore d'évaluation
- MS NeurosurgeryDocument60 pagesMS NeurosurgeryAdeel RaufPas encore d'évaluation
- Accomplishment Report orDocument1 pageAccomplishment Report orJESSIE MAE DAQUILPas encore d'évaluation