Académique Documents
Professionnel Documents
Culture Documents
Rev Infarct
Transféré par
flying highCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Rev Infarct
Transféré par
flying highDroits d'auteur :
Formats disponibles
REVIEWS
Heart regeneration and repair after
myocardial infarction: translational
opportunities for novel therapeutics
Thomas J. Cahill1,2, Robin P. Choudhury2,3 and Paul R. Riley1
Abstract | Current therapies for heart failure after myocardial infarction are limited and
non-curative. Although regenerative approaches are receiving significant attention, clinical
efforts that involve transplantation of presumed stem and progenitor cells have largely failed to
deliver. Recent studies of endogenous heart regeneration in model organisms, such as zebrafish
and neonatal mice, are yielding mechanistic insights into the roles of cardiomyocyte proliferation,
resident stem cell niches, neovascularization, the immune system and the extracellular matrix.
These findings have revealed novel pathways that could be therapeutically targeted to stimulate
repair following myocardial infarction and have provided lessons to guide future efforts towards
heart regeneration through cellular reprogramming or cardiomyocyte transplantation.
Heart failure is the consequence of cardiomyocyte death To date, clinical efforts towards cardiac regeneration
Heart failure
A pathological state that is or dysfunction, which is most commonly caused by have focused on cell-based therapies, including bone
defined by the inability of the myocardial infarction, hypertension, valve disease, infiltra- marrow-derived cells, mesenchymal stem cells and pre-
heart to pump blood to tion, infection, chemotherapy or genetic cardiomyopa- sumed cardiac progenitor cells9,10 (TABLE 1). Although these
support the requirements of thy1,2. Heart failure is a global disease challenge that affects studies have met safety end points, the effect on cardiac
the body. Typical symptoms
include shortness of breath,
an estimated 38 million people worldwide3. Despite strides function has been small or negligible, which has prompted
fluid retention and fatigue. forward in the management of acute myocardial infarction, a search for novel approaches. Insights from endogenous
heart failure remains common, and the incidence may be heart regeneration in animal models, such as zebrafish
increasing owing to improved early survival with primary (Danio rerio) and neonatal mice, are now yielding new
percutaneous coronary intervention4,5. Health care costs understanding of innate mechanisms for complex organ
associated with heart failure exceed US$30 billion annually repair. This includes the origins of new cardiomyocytes
in the United States alone and are projected to increase to after injury, control of cardiomyocyte proliferation in
almost $70 billion by 2030 (REF. 6). Heart failure is a leading development and ageing, and the roles of developmental
cause of hospitalization, adverse quality of life, and death, stem cell niches such as the epicardium11,12.
and a new diagnosis carries a worse prognosis than many In this Review, we describe recent insights into the
cancers, with a survival rate of only 50% at 5 years. biology of heart regeneration that have been gained from
1
Department of Physiology,
Current therapies to prevent or delay progression of preclinical animal models and extrapolate these to a next
Anatomy and Genetics,
University of Oxford, heart failure are limited. Conventional pharmacotherapy generation of regenerative strategies for heart failure,
Sherrington Building, Oxford targets the maladaptive counter-regulatory mechanisms including methods for augmentation of intrinsic repair,
OX1 3PT, UK. activated by left ventricular dysfunction (BOX 1). This cell reprogramming and extrinsic cardiomyocyte replace-
2
Division of Cardiovascular approach has yielded blockbuster agents over the past ment. The key steps that are needed to translate informed
Medicine, University of
Oxford, John Radcliffe
20 years, including inhibitors of the renin–angiotensin biology to novel therapeutic approaches and compounds,
Hospital, Oxford OX3 9DU, system, the mineralocorticoid receptor, the sympathetic adapt existing clinical trial design and enhance interac-
UK. nervous system and, most recently, the natriuretic sys- tions between scientists, clinicians and the pharmaceutical
3
Oxford Acute Vascular tem7,8 (FIG. 1). Although these drugs reduce mortality, they industry are outlined.
Imaging Centre, University of
fail to address the underlying loss of cardiomyocytes and
Oxford, John Radcliffe
Hospital, Oxford OX3 9DU, vasculature, and are intrinsically non-curative. Discovery of heart regeneration
UK. Regeneration of the heart by reconstitution of the Organ regeneration has long been recognized. In 1686,
Correspondence to P.R.R. cardiomyocyte substrate is a tantalizing and potentially lizard tail regeneration was demonstrated to the Paris
paul.riley@dpag.ox.ac.uk entirely disruptive approach to combat heart failure. Organ Academy of Sciences, and the first scientific reports of
doi:10.1038/nrd.2017.106 regeneration is seen widely across the animal kingdom regeneration in Hydra spp. were published by A. Trembley
Published online 21 Jul 2017 and can occur in humans, for example, after liver injury. in the mid‑18th century.
NATURE REVIEWS | DRUG DISCOVERY ADVANCE ONLINE PUBLICATION | 1
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Box 1 | Development of heart failure: pathophysiological mechanisms reports of functional regeneration after cardiac injury in
infants, and a lack of scarring in children after cardiac
Heart failure following acute myocardial infarction is a paradigm for failed surgery for congenital heart disease, support the concept
regeneration. Following coronary artery occlusion, ischaemic death of cardiomyocytes of age-dependent regeneration in the human heart 23,24.
begins within hours. Cell injury and death trigger the release of pro-inflammatory
cytokines, infiltration of neutrophils and mobilization of monocytes from the spleen204.
Mechanisms of heart regeneration
Opening of the occluded coronary artery by primary percutaneous coronary
intervention improves salvage of the injured myocardium but — in the short term — Regeneration is a finely orchestrated process that has
leads to a burst of oxidative stress and further cardiomyocyte death. Even after parallels to organ formation during embryonic develop-
reperfusion, microvascular obstruction (MVO) — caused by thrombotic and plaque ment, which requires control of cell division, differentia-
debris and by endothelial damage — persists in up to 50% of patients205. Over tion, migration, integration and maturation25. Compared
subsequent days, inflammation drives further infarct expansion at the border zones. A with development, regeneration from injury is com-
transition from inflammation to repair is characterized by activation of fibroblasts to plicated by the need to clear damaged or dead tissue,
myofibroblasts, which deposit collagen matrix that leads to scar formation206. regulate inflammation, suppress overactive fibrosis, and
Chronic remodelling of the damaged left ventricle subsequently occurs over weeks to reconstitute and integrate only a subsection of cardio
months, involving ventricular dilatation, scar thinning and activation of interstitial myocytes, extracellular matrix (ECM), blood vessel and
fibrosis207,208. Reduced cardiac output triggers activation of neurohormonal systems
lymphatic systems26. Studies of heart regeneration in key
that act to maintain the circulation209. Release of angiotensin II and aldosterone drive
sodium and fluid retention, and adrenergic system activation maintains blood pressure genetic model organisms, the zebrafish and the neonatal
through vasoconstriction210. These mechanisms are initially compensatory but become mouse, have heralded several insights into the underlying
maladaptive, driving fluid overload, myocardial hypertrophy and slow but ongoing biological mechanisms of these processes.
cardiomyocyte death, which leads to further deterioration in ventricular function211,212.
Incremental benefits may be gained by optimizing early salvage, reducing MVO and Cardiomyocyte regeneration
further inhibition of maladaptive physiology, but entirely novel approaches are required Replacement of cardiomyocytes to restore structural and
to address the fundamental issue of cardiomyocyte death. functional integrity is the sine qua non of heart regen-
eration. The identification of the source (or sources) of
new cardiomyocytes and the mechanisms that control
Regeneration of the injured heart was first recog- cardiomyocyte proliferation is crucial to understand the
nized in amphibians and has now been described in sev- mechanisms of regeneration and to direct therapeutic
eral teleost fish and amphibians13. The two-chambered strategies for humans.
heart of the zebrafish regenerates after damage caused
by surgical resection of the cardiac apex, cryoinjury, Sources of cardiomyocytes in endogenous regeneration.
cardiomyocyte ablation or hypoxia–reoxygenation14–17. In principle, new cardiomyocytes could be derived from
Urodele amphibians, including the axolotl (Ambystoma the existing cardiomyocyte pool (either directly from
mexicanum) and newt (Notophthalmus viridescens), are mature cardiomyocytes or from an intermediate cell
also capable of complete heart regeneration. In both fish type) or alternatively from a progenitor cell population,
and amphibians, functional cardiomyocytes repopulate either resident in the heart or located remotely. Seminal
the injury site, and the transient scar is resolved over a studies in zebrafish and mouse models have addressed
variable period of 60–180 days, depending on the injury this question through genetic lineage tracing, using the
mechanism13,18,19. tamoxifen-inducible Cre–loxP system to irreversibly
Although previously thought to be restricted to fish label cardiomyocytes with a fluorescent reporter protein
and amphibians, Porrello et al. reported heart regen- before injury 27. Once the label is activated, all cardio
eration in the neonatal mouse in 2011 (REFS 20,21). myocytes and their progeny express the fluorescent
After resection of the cardiac apex or surgical coro- reporter, which means that if new cardiomyocytes are
nary artery ligation (to induce myocardial infarction), labelled they have originated from the pre-existing pool.
regeneration occurred over a period of ~21 days, leav- If not, it can be deduced that they have been derived
ing only very minor residual scarring at the site of the from a non-cardiomyocyte progenitor. Two studies that
Myocardial infarction ligature. Interestingly, this capacity for regeneration was used this approach in zebrafish have shown that almost
An acute injury to the heart restricted to a temporally privileged window of the first all (~95%) new cardiomyocytes after injury are labelled,
that is caused by occlusion of 7 days after birth. which suggests that cells in the pre-existing cardio
the coronary blood supply, The revelation that regeneration can occur in the myocyte pool are capable of re‑entering the cell cycle,
usually due to atherosclerotic
plaque rupture. This process is
neonatal mouse has ignited the field and suggests that dividing and migrating to mediate regeneration28,29. In
also commonly known as regenerative repair is not a unique programme lost to mice, new cardiomyocytes formed during ageing and
a heart attack. mammals in evolution. Although regeneration in the neonatal heart regeneration are also derived from the
postnatal setting may involve repurposing of the ongoing pre-existing cardiomyocyte pool21,30. In the infarcted
Epicardium
growth response, it remains highly valuable as a means non-regenerating adult mouse heart, some data sup-
The outer layer of the heart;
also known as the visceral to identify trophic pathways to promote regeneration in port a minor contribution of a non-cardiomyocyte
pericardium. the adult. Furthermore, several intriguing (albeit low- progenitor population (for example, KIT + cells) to
evidence level) studies support the concept of a tempo- the development of new cardiomyocytes, but this
Fibrosis rally privileged period of regenerative repair in humans. remains controversial31,32.
A pathological process that
is characterized by deposition
These include a case report of a newborn infant with The concept of regeneration that is driven primarily
of interstitial fibrous or a large anterior myocardial infarction, which healed by by existing cardiomyocytes represents a paradigm shift.
scar tissue. regeneration with full functional recovery 22. Other case Many of the first-generation cell therapy trials (TABLE 1)
2 | ADVANCE ONLINE PUBLICATION www.nature.com/nrd
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
ICD therapy ESC-derived cardiomy-
(MADIT-II ocytes engraft the
study) macaque heart
First heart ACEI MRAs ARB
Organomercurial transplant (Consensus I (RALES (Val-HeFT CRT Sacubitril and Valsartan
diuretics in humans study) study) study) (MIRACLE (PARADIGM heart
study) failure study)
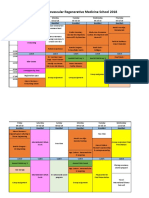
1920 1959 1967 1986 1987 1996 1999 2001 2002 2012 2014 2016
Thiazide Hydralazine Beta-blockers From 2001 onwards, In vivo iPSC-derived
diuretics and nitrate (Carvedilol heart cell therapy trials reprogramming cardiomyocytes
(V-HeFT I study) failure study) commence: of fibroblasts to engraft the
BMCs, MSCs and cardiomyocytes macaque heart
cardiac progenitors in the mouse
Figure 1 | Heart failure therapy timeline. Landmark breakthroughs in heart failure therapy NatureareReviews
indicated in green,
| Drug and
Discovery
progress in regenerative therapies for heart failure are shown in purple. Key trials in heart failure are shown in brackets.
ACEI, angiotensin-converting enzyme inhibitors; ARB, angiotensin receptor blockers; BMCs, bone marrow-derived cells;
ESC, embryonic stem cell; CRT, cardiac resynchronization therapy; ICD, implantable cardioverter defibrillator; iPSC,
induced pluripotent stem cell; MRAs, mineralocorticoid receptor antagonists; MSCs, mesenchymal stem cells.
were inspired by the concept of bone marrow-derived Control of cardiomyocyte proliferation. Environmental
progenitors, which had been reported to differentiate cues in the postnatal environment have been implicated
into cardiomyocytes, but this has been progressively dis- in proliferative arrest of mammalian cardiomyocytes.
credited33–35. The benefits of bone marrow mononuclear After birth, the heart transitions from the relatively
cells and mesenchymal stem cells seen in some clinical hypoxic intrauterine environment to normoxia, which is
studies (TABLE 1) are increasingly ascribed to paracrine associated with a shift from glycolysis to oxidative phos-
effects. Now, a major research focus is on understanding phorylation, increased mitochondrial mass and activity,
whether human mature cardiomyocytes can proliferate production of reactive oxygen species and cardiomyocyte
and the mechanisms by which this may be controlled. cell cycle arrest 39. Scavenging of reactive oxygen species
prolongs the neonatal regenerative window, whereas
Cardiomyocyte proliferation in development, ageing hyperoxia shortens it. During regeneration, reactivation
and injury. Cardiomyocytes in mice and humans pro- of cell cycle activity is associated with hypoxic activation of
liferate during heart development in utero and during hypoxia-inducible factor 1α (HIF1α)40. Other factors have
early postnatal life. After birth, most cardiomyocytes exit been implicated in the loss of proliferative capacity post-
the cell cycle, but a variable subset (~25% in humans) natally, including upregulation of p38 mitogen-activated
undergo a further cycle of nuclear division without cell protein kinase (MAPK) and MEIS1 (REFS 41,42). MEIS1,
separation (cytokinesis), which results in binucleation36. In which is a member of the three-amino-acid loop exten-
humans, the adult heart has thus traditionally been con- sion transcription factor family, promotes cell cycle arrest
sidered incapable of further cell division, with growth through activation of the cyclin-dependent kinase (CDK)
being achieved by hypertrophy. In fact, increasing evi- inhibitors p15 (encoded by CDKN2B), p16 (also known
dence suggests that cardiomyocytes do renew in the as INK4A; encoded by CDKN2A) and p21 (encoded by
human heart, albeit at a low level. Relying on integra- CDKN1A). Inhibition of MEIS1 extends the regenerative
tion of carbon‑14 into DNA during Cold War nuclear window in neonates and is capable of reactivating the cell
testing, Bergmann et al. estimated that cardiomyocyte cycle in adults.
self-renewal occurs at a rate of 1% per year for adults Many of the emerging ligands and signalling path-
aged 25 years, which decreases to 0.45% by 75 years37. ways that regulate cardiomyocyte proliferation in the
Histological analysis of the human heart has identi- context of regeneration are familiar from developmental
fied phosphorylated histone H3, which is a marker of biology (FIG. 2). Neuregulin 1 (NRG1), which is an ago-
mitosis, in adults up to the age of ~20 years38. However, nist for the ERBB2 and ERBB4 receptor tyrosine kinases
Cytokinesis despite the apparent capacity for renewal, myocardial of the epidermal growth factor receptor family, is a key
Division of the cell cytoplasm
infarction fails to activate effective proliferation. In the mitogen during heart development 43,44. It is reactivated
to complete the cell cycle and
create a membrane barrier adult mouse, using co‑registration of cardiomyocyte in perivascular cells during zebrafish heart regeneration,
between two daughter cells. fluorescent labelling and [15N]thymidine labelling of and overexpression enhances cardiomyocyte prolifera-
DNA replication, Senyo et al. reported that only 3% tion even in the uninjured heart 45. The transcription fac-
Binucleation of infarct zone cardiomyocytes initiate DNA replication tor heart and neural crest derivatives-expressed protein 2
Division of the nucleus that
leads to the formation of two
and nuclear division. Furthermore, although these cells (HAND2) is crucial to cardiomyocyte development from
nuclei within a cell but without became binucleated, almost none underwent cytokinesis the second heart field, an anterior progenitor pool that
division of the cytoplasm. to form a new daughter cell30. contributes extensively to the developing right ventricle
NATURE REVIEWS | DRUG DISCOVERY ADVANCE ONLINE PUBLICATION | 3
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Table 1 | Landmark studies from the infancy of regeneration: cell therapy trials in acute myocardial infarction and heart failure
Name Design Patient group Cell type, dose and Primary end Outcome Comment Refs
and number of delivery route point
patients
Menasche et al. Case report • Ischaemic • Skeletal myoblasts NA NA • First‑in‑man report 213
(2001) heart failure • 800 × 106 cells of skeletal myoblast
undergoing • Intramyocardial injection
CABG injection during • Improved wall
• n = 1 CABG motion and
perfusion on PET
Strauer et al. • Non-randomized • Acute • Autologous bone Not specified Reduced infarct First study of bone 214
(2002) • Open-label myocardial marrow-derived size in cell therapy marrow cells in acute
infarction cells‡ arm myocardial infarction
• n = 20 • 2.8 × 107 cells
• Intracoronary
delivery
Perin et al. • Non-randomized • Ischaemic • Autologous bone Safety • Improved left First study of bone 215
(2003) • Open-label heart failure marrow-derived ventricular marrow cells in heart
• n = 21 cells‡ function failure
• 25.5 × 106 cells • Reduced
• Transendocardial reversible
injection perfusion defect
BOOST • Randomized • Acute • Autologous bone Change in LVEF Improved global First randomized 216
(2004) • Non-placebo myocardial marrow-derived left ventricular study of bone marrow
controlled infarction cells‡ function cells
• n = 60 • 24.6 × 108 nucleated
cells
• Intracoronary
delivery
ASTAMI • Randomized • Acute • Autologous bone Change in LVEF No change in Negative trial 217
(2006) • Non-placebo myocardial marrow-derived left ventricular concurrent with
controlled infarction cells‡ function, REPAIR-AMI
• n = 100 • 68 × 106 cells end-diastolic
• Intracoronary volume or infarct
delivery size at 6 months
REPAIR-AMI • Randomized • Acute • Autologous bone Change in LVEF Significant Largest trial of bone 218
(2006) • Double-blind myocardial marrow-derived improvement marrow cells. Showed
• Placebo infarction cells‡ in global left reduction in clinical
controlled • n = 204 • 236 × 106 cells ventricular end point of death,
• Intracoronary function at recurrent myocardial
delivery 4 months infarction and
revascularization
Janssens et al. • Randomized • Acute • Autologous bone Change in LVEF Negative for Reduction in infarct 219
(2006) • Double-blind myocardial marrow-derived primary end point volume
• Placebo infarction cells‡
controlled • n = 67 • 304 × 106 nucleated
cells
• Intracoronary
delivery
MAGIC • Randomized • Heart failure • Skeletal myoblasts Change in regional Negative for • High-cell-dose 220
(2008) • Double-blind and previous • 400 × 106 cells (low and global left primary efficacy arm had reduced
• Placebo myocardial dose) – 800 × 106 ventricular end points left ventricular
controlled infarction cells (high dose) function remodelling with
undergoing • Surgical injection decreased left
CABG during CABG ventricular volumes
• n = 97 • Increased
arrhythmias in the
cell therapy arms
SCIPIO* • Randomized • Ischaemic • Autologous KIT+ Safety No adverse events Increase in LVEF and 221
(2011) • Open-label heart failure cardiac stem cells reported decrease in infarct
• Non-placebo • n = 23 • 1 × 106 cells size reported in cell
controlled • Intracoronary therapy recipients
delivery (secondary end
points)
CADUCEUS • Randomized • Acute • Cardiosphere- Safety: Met safety end Reduction in scar 222
(2012) • Non-placebo myocardial derived cells unexpected or point size and mass in cell
controlled infarction • 12.5–25 × 106 cells arrhythmia-related therapy arm
• n = 25 • Intracoronary death, myocardial
delivery infarction, tumour
formation or MACE
4 | ADVANCE ONLINE PUBLICATION www.nature.com/nrd
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Table 1 (cont.) | Landmark studies from the infancy of regeneration: cell therapy trials in acute myocardial infarction and heart failure
Name Design Patient group Cell type, dose and Primary end Outcome Comment Refs
and number of delivery route point
patients
FOCUS-CCTRN • Randomized • Ischaemic • Autologous bone • Change in left Negative for – 200
(2012) • Double-blind heart failure marrow-derived ventricular primary end
• Placebo • n = 92 cells‡ end-systolic points
controlled • 100 × 106 cells volume
• Transendocardial • Maximal O2
injection consumption,
• Reversibility on
SPECT
SWISS-AMI • Randomized • Acute • Autologous bone Change in LVEF Negative for – 223
(2013) • Open-label myocardial marrow-derived primary end point
• Non-placebo infarction cells‡
controlled (either early • 140–160 × 106
(5–7 days) nucleated cells
or late • Intracoronary
(3–4 weeks)) delivery
• n = 200
PROMETHEUS • Non-randomized • Ischaemic • Mesenchymal stem NA NA • Increased ejection 224
(2014) • Non-placebo heart failure cells fraction
controlled undergoing • 2 × 107 cells (low • Decreased scar
CABG dose) – 2 × 108 cells mass
• n = 6 (high dose)
• Intramyocardial
injection during
CABG
Menasche et al. Case report • Ischaemic • Human ESC‑derived NA NA • First-in-man study 225
(2015) heart failure cardiac progenitor • New-onset
undergoing cells on a fibrin contractility
CABG scaffold observed in the
• n = 1 • Surgical patch patched region
implantation
REGENERATE- • Randomized • Acute • Autologous bone Change in LVEF Negative for Large, 226
AMI (2016) • Double-blind myocardial marrow‑derived primary end point double-blinded study
• Placebo infarction cells‡ that failed to meet
controlled • n = 100 • 59.8 × 106 cells primary efficacy end
• Intracoronary point
delivery
CABG, coronary artery bypass grafting; ESC, embryonic stem cell; LVEF, left ventricular ejection fraction; MACE, major adverse cardiovascular events; NA, not
applicable; PET, positron emission tomography, SPECT, single-photon emission-computed tomography. *Subject to expression of concern. ‡See individual studies
for precise characteristics of bone marrow-derived cells used.
and atria, sequentially following linear heart tube forma- chromatin remodelling by BRG1, which controls prolif-
tion. Zebrafish with mutations in hand2 have a reduction eration through pro-proliferative bone morphogenetic
in the number of cardiomyocytes, and Hand2‑knockout protein 10 (BMP10) and inhibition of p57KIP2 (also
mice show abnormalities in the right ventricle and out- known as CDKN1C)53. Inhibition of BRG1, or other
flow tract region46,47. Hand2 is upregulated in the injured switch/sucrose non-fermentable (SWI/SNF) compo-
zebrafish ventricle, and its overexpression is sufficient to nents such as BRG1‑associated factor 60C (BAF60C;
drive cardiomyocyte proliferation48. Similarly, GATA4, also known as SMARCD3) and BAF180 (also known
which is a zinc finger transcription factor known to reg- as PBRM1), leads to blunted proliferation and failed
ulate cardiomyocyte differentiation, migration, hyper- regeneration54.
trophy and survival, is required for neonatal mouse Despite these insights, whether a mature mammalian
heart regeneration, acting via fibroblast growth factor cardiomyocyte can re‑enter the cell cycle and progress
16 (FGF16) to stimulate proliferation49. The Hippo path- through to cytokinesis is unclear. In zebrafish, cardio-
way, which comprises a series of proteins that regulate myocytes are mononuclear and relatively ‘primitive’,
the transcription factor YES-associated protein 1 (YAP1) and this seems to be a crucial factor that determines
and its co‑activator TAZ (also known as WWTR1), is an their ability to divide. Proliferation of the mononuclear
evolutionarily conserved regulator of cell proliferation, cardiomyocyte population can be induced by NRG1
growth, viability and organ size50. Forced expression of treatment after myocardial infarction in mice. Based on
YAP1 in development leads to hyperproliferation and nuclearity, the adult human heart might be more regen-
cardiac enlargement in mice, and in mouse heart regen- erative than that of the mouse, as it contains a higher
eration, YAP1 promotes proliferation by acting through proportion of mononuclear cardiomyocytes55. In addi-
insulin-like growth factor and WNT signalling path- tion, distinct subsets of cardiomyocytes may have dif-
ways51,52. Last, as in development, regeneration requires fering abilities to proliferate: in zebrafish, the outermost
NATURE REVIEWS | DRUG DISCOVERY ADVANCE ONLINE PUBLICATION | 5
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
• NRG1 sequencing approaches 58. The precise mechanisms
• FGF1 Periostin ECM stiffness OSM that direct cardiomyocytes to undergo cell division as
• WNTs opposed to polyploidization (which seems to suppress
• IGF1
• TWEAK further cell cycle entry) also remain poorly understood59.
In parallel, understanding the hierarchy, relative impor-
tance and overlap of extrinsic cues would help to pri-
oritize therapeutic targets. For example, alongside the
• HAND2
• GATA4 soluble ligands discussed above, the autonomic nerv-
• miRNAs Cell cycle re-entry Dedifferentiation ous system is emerging as a regulator of cardiomyocyte
• HIF1α proliferation and may therefore represent a potential
S
adjunctive target 60,61.
G1 G2
M Neovascularization: the epicardium
• p38 MAPK Although primary percutaneous coronary interven-
YAP–TAZ • MEIS1
• miR-15
tion (PPCI) is effective at restoring coronary blood
• Reactive flow in the major epicardial vessels following myocar-
oxygen species dial infarction, failure to perfuse the microcirculation
• Cell cycle
Binucleation regulators (also known as microvascular obstruction (MVO)) is
common and is associated with poor wound healing,
Cardiomyocyte ventricular remodelling, heart failure and reduced over-
all survival62. MVO is multifactorial and occurs owing
?
to endothelial cell death, inflammation and physical
Hippo pathway Cytokinesis plugging by thrombotic or plaque debris. Restoration of
antagonists effective myocardial perfusion by regeneration or repair
of the coronary microcirculation, which comprises the
Figure 2 | Endogenous mechanisms controlling cardiomyocyte
Nature Reviewsproliferation.
| Drug Discovery
vascular endothelium, smooth muscle, fibroblasts and
Initiation of cardiomyocyte proliferation is regulated by both intrinsic and extrinsic pericytes, will be essential to achieve heart regeneration.
factors. Several soluble ligands have been identified that promote cardiomyocyte
proliferation during development and in models of heart regeneration, including Coronary formation during development. Coronary
neuregulin 1 (NRG1), fibroblast growth factor 1 (FGF1), WNTs, insulin-like growth factor 1 formation during development is a blueprint for the for-
(IGF1) and tumour necrosis factor-related weak inducer of apoptosis (TWEAK; also mation of new vessels. Coronary endothelial cells arise
known as TNFSF12) pathways. Other soluble cues that are implicated in proliferation primarily from the sinus venosus, with an additional
include oncostatin M (OSM), which is a macrophage-derived cytokine that directs
contribution from the inner lining of the heart, the endo-
cardiomyocyte dedifferentiation. Downstream transcriptional regulators of
cardiomyocyte cell cycle re‑entry include heart and neural crest derivatives-expressed cardium, which generates the coronary endothelium for
protein 2 (HAND2), GATA4, YES-associated protein 1 (YAP1)–TAZ, hypoxia-inducible the interventricular septum63–65. The programme of cor-
factor 1α (HIF1α) and microRNAs (miRNAs). In the adult mammalian heart, onary vascular formation is directed by the epicardium,
cardiomyocytes exit the cell cycle postnatally and are resistant to cell cycle re‑entry, and also known as the visceral pericardium, which acts as
proliferation is inhibited by p38 mitogen-activated protein kinase (MAPK), MEIS1, miR‑15 a source of both trophic factors and progenitor cells66.
and reactive oxygen species. Structural and functional aspects of the extracellular matrix Formed at embryonic day 9.75 in the mouse (human
(ECM) also regulate cardiomyocyte proliferation: periostin and a lack of matrix rigidity Carnegie stage 11), the epicardium is an epithelial sheet
promote cardiomyocyte proliferation. Factors that promote cytokinesis following that envelops the growing heart 67. Epicardium-derived
binucleation, to generate new daughter cells, remain poorly defined. cells (EPDCs) invade the underlying myocardium and
undergo epithelial-to‑mesenchymal transition (EMT),
which gives rise to pericytes, smooth muscle cells and
‘cortical’ zone proliferates early and rapidly in regener- adventitial and interstitial fibroblasts63,68,69. The epi-
ation56. Cardiomyocyte proliferation requires cellular cardium also begins a signalling pas de deux with the
‘dedifferentiation’, which is defined by increased inter- myocardium, from which growth factors that support
cellular separation and loss of sarcomeric and Z‑disc vasculogenesis and mitogens that support cardio
structures28. Dedifferentiation has been observed in the myocyte proliferation are secreted66. Physical or genetic
mammalian heart and may be triggered by oncostatin ablation (through deletion of epicardial genes such as
Ploidy M, which is a macrophage-derived cytokine related to Wilms tumour homologue 1 (Wt1)) leads to defects in
The number of sets of interleukin‑6 (IL‑6), but is poorly characterized at a coronary vessel formation and impaired cardiomyocyte
chromosomes in a cell. molecular level57. proliferation70,71.
Research priorities in the mammalian heart include
Ventricular remodelling
A process that is characterized identifying and tracking the key cardiomyocyte subpop- Coronary revascularization following injury. The epi-
by a change in size, shape and ulation (or subpopulations) that are capable of division cardium is quiescent in the adult heart but is reactivated
structure of the ventricle. After in the adult based on ploidy or other discriminating and expands in response to injury 72,73. Reactivation is
myocardial infarction, features. The characterization of the markers and tran- associated with expression of an embryonic gene pro-
pathological remodelling
causes the ventricle to enlarge,
scriptional pathways of cardiomyocytes that undergo file and recapitulation of its developmental functions,
become spherical in shape and dedifferentiation, replication, migration and matura- supporting repair and neovascularization. Ablation
functionally deteriorate. tion would be valuable and is achievable with single-cell of transcription factor 21 (Tcf21)-positive cells in the
6 | ADVANCE ONLINE PUBLICATION www.nature.com/nrd
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
epicardium after ventricular resection in the zebrafish specialized clusters91. Improved markers for different
leads to a reduction in cardiomyocyte proliferation, subpopulations will be required to dissect their respec-
delays neovascularization and results in incomplete tive roles and to separate the paracrine and progenitor
regeneration at 30 days74. In adult mice, priming of cell components of the epicardial response. Recently, at
the epicardium before injury with the small peptide least three new subpopulations have been reported in
thymosin β4 (Tβ4), or treatment with epicardial cell- zebrafish, including a role for genes such as caveolin 1
conditioned media, improves neovascularization and (REF. 92). A key research requirement to optimally har-
functional outcomes after myocardial infarction75–77. ness therapeutic effects of the epicardial response is to
Similarly, stimulation of the epicardium with Tβ4 in understand how it is modulated in the setting of regen-
neonatal mice can extend the temporal window for eration compared with scar formation; for example, in
regeneration78. the repression of fibroblast formation.
The precise mechanisms of coronary revasculariza-
tion following injury are not well defined. There is evi- Inflammation and immune system activation
dence to support both local proliferation of endothelial Myocardial infarction leads to extensive cell death and is
cells and a contribution from a remote stem cell source, a potent activator of inflammation93. In mice and humans,
endothelial progenitor cells, which is a controversy that inflammation is linked to repair through a biphasic
is discussed in detail elsewhere79. In the neonatal mouse immune response: an early pro-inflammatory phase that
heart, neovascularization is achieved primarily by for- is characterized by release of cytokines and recruitment
mation of large collateral arteries that bypass the ligation of neutrophils and monocytes, which is followed by a
site. These derive from pre-existing arteries through a reparative phase with resolution of inflammation, activa-
process of arteriogenesis rather than arterialization of the tion of myofibroblasts and deposition of a collagen-based
pre-existing capillary network80. Clues from non-cardiac scar 94,95. This process is patterned and under tight spatio
injury models (for example, zebrafish fin) suggest that temporal regulation. Macrophages, for example, have
neovascularization during regeneration is dependent on diverse functions through the course of injury, including
classical angiogenic signalling mechanisms that involve pro-inflammatory cytokine production, phagocytosis of
vascular endothelial growth factor receptor 2 (VEGFR2), necrotic cell debris, pro-angiogenic signalling, activation
HIF1α and C-X-C motif chemokine 12 (CXCL12; also of fibroblasts and remodelling of the ECM96,97. Improved
known as SDF1)81–83. cell surface markers and transcriptional profiling are
Neovascularization is supported by the epicardium helping to define the identity and function of specific
through several secreted factors, including retinoic monocyte, macrophage, neutrophil and T cell subsets in
acid, fibroblast growth factors, VEGFA and CXCL12 the injured heart98–100.
(REFS 77,84). Blockade of Fgf signalling in zebrafish leads Inflammation is not a barrier to tissue regeneration
to a failure of EMT and neovascularization (discussed and, in fact, may provide the initial pro-regenerative
further below), in turn leading to failed regeneration73. cues. In zebrafish, for example, brain injury activates
In mice, reactivation of epicardial EMT following myo- acute inflammation, which is sufficient to drive neu-
cardial infarction contributes several cell lineages to ral proliferation via leukotriene C4 (REF. 101). The cel-
support repair. By inducible labelling of the Wt1+ popu- lular immune response to injury has also been directly
lation, EPDCs have been shown to contribute to fibro- implicated in healing by regeneration102. In regenerat-
blast, myofibroblast, smooth muscle cell and adipocyte ing muscle, infiltrating cells — including macrophages,
populations77,85. Whether the reactivated epicardium eosinophils and Treg cells — influence activation of sat-
can contribute other cell types, specifically cardiomyo- ellite cells and fibroadipogenic progenitors to specify
cytes or endothelial cells, is debated. When pre-primed production of new myofibres103–105. Macrophages also
with exogenous Tβ4, the epicardium in mice can gener- direct endothelial progenitors to form capillary vessels,
ate extremely limited numbers of cardiomyocytes, but which suppresses an alternative EMT pathway 106. After
this does not occur without priming and is not seen in liver injury, macrophage secretion of WNT3A con-
zebrafish regeneration75,86–88. Last, an emerging mecha- trols lineage differentiation of hepatic progenitor cells
nism relates to crosstalk of epicardial cells and immune to produce hepatocytes107. Similarly, macrophage pro-
cells. The epicardium is required for populating the duction of WNT7B in the injured kidney is required for
heart with tissue-resident macrophages during embry- regeneration108.
onic development, and macrophages colocalize with the Inflammation and the immune response have
epicardium following injury 89. Recently, the epicardium also been linked to heart regeneration. Activation of
has been shown to mediate an immunosuppressive inflammation stimulates cardiomyocyte proliferation
response to myocardial infarction through modula- in the neonatal heart, and blockade of IL‑6 or signal
tion of cytokines that promote regulatory T (Treg) cell transducer and activator of transcription 3 (STAT3), its
recruitment to the heart 90. In mice, genetic knockout of downstream effector, blocks heart regeneration after
epicardial Yap1 or Wwtr1 led to persistent inflammation, apical resection109. In the neonatal mouse model of myo-
widespread fibrosis, heart failure and death following cardial infarction, macrophages are actively recruited to
myocardial infarction90. the heart, and treatment with clodronate liposomes
The epicardium is increasingly recognized to be to ablate macrophages blocks regeneration through
a highly heterogeneous cell population that consists inhibition of angiogenesis110. Divergent roles for distinct
of both mesenchymal and haematopoietic cells within macrophage subsets are emerging — notably between
NATURE REVIEWS | DRUG DISCOVERY ADVANCE ONLINE PUBLICATION | 7
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
tissue-resident macrophages, which are seeded to vis- directly influences the ability of cardiomyocytes to
ceral organs during embryonic development, compared undergo proliferation and cytokinesis119. Interestingly,
with those that derive from circulating monocytes — if the failing human heart is offloaded by implantation
during acute inflammation. Using a cardiomyocyte of a left ventricular assist device, cell cycle re‑entry is
ablation model, Lavine et al. found that depletion of observed, which is an effect that could be mediated by
resident macrophages in the neonatal heart leads to permissive ECM changes120.
reduced cardiomyocyte and endothelial cell prolifer- The ECM also has direct biological effects on cardio
ation, and increased interstitial fibrosis and chamber myocytes. The decellularized zebrafish ECM can induce
dilatation111. By contrast, inhibition of C-C chemokine cardiomyocyte proliferation and cardioprotection in
receptor type 2 (CCR2)-positive macrophages, which the mouse heart, an effect that is mediated by ERBB2
are derived from monocytes, preserves embryonic (REF. 121). Functional ECM components are emerg-
subsets and improves myocardial repair 111. ing from candidate approaches and unbiased screens.
Multiple injury models suggest that inflammatory Fibronectin, which is derived from the epicardium after
signalling is required as a trigger to induce cell pro- injury, stimulates zebrafish heart regeneration122,123.
liferation or differentiation of progenitors to restore Periostin, which is a matricellular protein, promotes
the lost tissue substrate. However, the precise mecha- cell cycle activation in mononucleated cardiomyocytes
nisms behind the divergent outcome of inflammation but also activates fibroblasts124. Small and large ani-
in regeneration and scar-forming models remain to be mal studies of periostin have shown improved heal-
fully elucidated. The capacity for tissue regeneration ing after myocardial infarction but at the expense of
seems to be inversely correlated with evolutionary com- increased fibrosis125,126. Hyaluronic acid and its receptor
plexity of the immune system, which has led to the sug- hyaluronan-mediated motility receptor are required for
gestion that a component of the mammalian immune EMT and heart regeneration in zebrafish127.
response might be a barrier to regeneration112. Detailed The roles of the ECM during regeneration and scar
comparisons of immune cell signalling in regenerative formation are still emerging, and thus much of the
and scar-forming models will be required to distinguish work is descriptive and at an early stage. The compo-
pro-regenerative signals from those that drive fibrosis sitional differences in the ECM during regeneration
or scar deposition, or the mechanisms by which the and scar formation, and the biological activity of these
same signals drive divergent healing. In addition, fur- proteins on downstream cell types, are not yet fully
ther characterization of the interplay between immune defined. Transcriptional profiling of fibroblasts, which
cell subsets, fibroblasts, endothelial cells and cardio are the major source of ECM components, and mass
myocytes is required. Potential therapeutic approaches spectrometry of the ECM in regeneration compared
to harness the regenerative potential of inflammation with scar formation would begin to address these ques-
are discussed below. tions. It remains unclear to what extent ECM compo-
nents can drive regeneration in vivo in an otherwise
Role of the extracellular matrix non-regenerative environment, and whether the ECM
The ECM consists of an organized and dynamic mesh- represents a standalone therapeutic target in endo
work of proteins113. Previously thought of as an inert genous regeneration. Harnessing the biological effects
structural scaffold, the ECM is now recognized to have of the ECM is also of value to cell therapy strategies in
complex biological effects and influences cell prolif- which survival, localization and engraftment of cells
eration, migration, lineage specification, intercellular may be augmented using patches or bioscaffolds with
signalling and growth factor presentation114. Control of engineered matrix properties128.
the ECM is a crucial component of regeneration. In the
newt limb, upregulation of ECM-remodelling matrix Scar formation and degradation
metalloproteinases occurs within hours of injury, and Regeneration and scar formation lie at opposite ends of
inhibition of those proteins blocks regeneration115. This the spectrum of repair. From an evolutionary perspec-
is associated with early deposition of a primitive ECM tive, it is unclear whether regenerative capacity was lost
that consists of hyaluronic acid, fibronectin and tenas- accidentally as a neutral trait, or whether it was selected
cin C, and downregulation of collagen116. Production against. Although it seems intuitive that regeneration
and remodelling of ECM components also occurs in would confer a survival and reproductive advantage,
scar-based healing, but this ‘scarring ECM’ is compo- costs associated with energy, time or interim function
sitionally distinct and seems to be directed by immune (for example, electrical stability) may have made it
cell control of fibroblasts to produce collagen117. advantageous to heal by rapid scar formation129,130.
In the heart, differences in ECM structure may be an Following acute myocardial infarction, scar tissue
important aspect that underlies the interspecies capacity is rapidly laid down in the mammalian heart by acti-
for regeneration. Although fish have a non-compacted, vated myofibroblasts. In the short term, this scar is cru-
spongy myocardium that is designed to function at low cial to providing mechanical strength and preventing
arterial blood pressure, the four‑chambered adult mam- ventricular rupture. Fibroblasts are originally derived
malian heart is highly compacted in a rigid matrix 118. In from the epicardium and endocardium during embry-
the neonatal mouse model, stiffening and maturation onic development through EMT131. Using a periostin-
of the ECM is correlated with cardiomyocyte cell cycle inducible Cre genetic mouse model for lineage tracing,
arrest, and in vitro, modulation of ECM compliance Kanisicak et al. showed that activated myofibroblasts
8 | ADVANCE ONLINE PUBLICATION www.nature.com/nrd
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
derive from tissue-resident TCF21+ fibroblasts, which interference, are effective at inducing DNA replication
produce large quantities of ECM components such as in vitro137. In vivo, overexpression of cyclin A2, cyclin D1
collagen and deactivate following resolution of injury 132. or cyclin D2 stimulates DNA synthesis, and cyclin D2
In the reparative phase, fibroblast activation following overexpression leads to improved repair following myo-
myocardial infarction is multifactorial but intricately cardial infarction138,139. Other approaches have included
linked to cytokine regulation by macrophages, for exam- knockout of tumour suppressor genes RB1 and RBL2,
ple, by transforming growth factor-β (TGFβ) and con- and direct targeting of the E2F transcription factor fam-
nective tissue growth factor (CTGF). Interestingly, TGFβ ily 140. Combinatorial reprogramming of cardiomyocytes
has been identified as a key pro-regenerative cytokine based on unbiased microarray approaches to define the
in the axolotl, but the mechanisms by which fibroblast proliferative state have proved to be more effective at
activation are suppressed are not clear 133. achieving improved repair 141. In general, however, these
The relationship between scar deposition and regen- approaches have triggered relatively modest DNA rep-
eration is complex. It has been proposed that these two lication, very limited cytokinesis and consequently little
events are diametrically opposed and compete to achieve new cardiomyocyte mass.
organ repair, with collagen deposition directly inhibitory Therapeutic targeting of upstream signalling path-
to regeneration134. However, knockdown of factors that are ways that regulate proliferation may reduce the risk
involved in scar formation in astrocytes following spinal of teratogenicity, which is inherent in directly target-
cord injury is not sufficient to induce axonal regrowth135. ing the cell cycle. For example, exogenous injection of
Furthermore, in the cryoinjury model in the zebrafish NRG1 activates proliferation of mononucleated cardio
heart, despite extensive scar deposition during the first myocytes via ERBB4 and phosphatidylinositol 3‑kinase
3 weeks following injury, regeneration still occurs, and is (PI3K), which leads to improved repair following exper-
characterized by progressive scar removal and replace- imental myocardial infarction55. Similarly, delivery of
ment with cardiomyocytes over time19. The finding that FGF1 with blockade of the p38 MAPK pathway, which
scar formation is not necessarily a barrier to regeneration is a key mediator of cardiomyocyte differentiation, pro-
has enormous therapeutic implications and suggests that motes myocardial repair following injury 142. A recent
the regenerative programme does not necessarily need to porcine myocardial infarction study showed that percuta-
be established in the early injury phase. neous intramyocardial injection of microparticles loaded
with NRG1 and FGF1 is effective at inducing improve-
Strategies for therapeutic regeneration ment in left ventricular function following myocardial
Efforts towards heart regeneration encompass a broad infarction, with increased angiogenesis and reduced
spectrum of approaches, including cell therapy, bio ventricular remodelling143 (TABLE 2). However, the growth
materials, tissue engineering, reprogramming and response is exquisitely regulated: in zebrafish, Notch
modulation of endogenous repair (FIG. 3a). This section pathway activation is required for cardiomyocyte prolifer-
focuses primarily on therapeutic strategies that exploit ation, but hyperactivation of Notch inhibited rather than
insights from developmental biology, including specifi- promoted heart regeneration144. A phase I study of recom-
cation or programming of the cardiomyocyte lineage, binant NRG1β3 (also known as cimaglermin alfa; Acorda
and endogenous regeneration. Therapeutics) in patients with chronic heart failure has
It should be noted that distinct approaches will be recently shown early promise, with evidence for safety
required for patients with recent myocardial infarction and preliminary findings that suggest an improvement
and for patients with established chronic heart failure. in left ventricular function at 90 days145 (TABLE 3).
Myocardial infarction provides a dynamic environ- Therapeutic cardiomyocyte proliferation can also be
ment of repair in which endogenous pathways can be induced by microRNA (miRNA) targeting. Screening
modulated towards regeneration. By contrast, in the of a whole-genome miRNA library identified 40 miR-
setting of stable heart failure, strategies to directly pro- NAs that increased both DNA synthesis and cytokinesis
vide new cardiomyocytes should be the focus. Current in vitro, two of which, miR‑590 and miR‑199a, stimulated
and future strategies for the production of new cardio cardiac regeneration in adult mice after experimental
myocytes and targeting of endogenous repair are myocardial infarction146. Similarly, overexpression of the
discussed in turn (FIG. 3a,b). miR‑302–367 cluster is sufficient to improve regener-
ation following adult myocardial infarction, which acts
Cardiomyocyte replacement via repression of the Hippo pathway 147. By contrast, the
Activation of cardiomyocyte proliferation. Initial miR‑15 family is upregulated postnatally, which correlates
attempts to reactivate cardiomyocyte proliferation with the shutdown of cardiomyocyte proliferative capacity.
were inspired by insights into cell cycle regulation by Delivery of anti‑miR‑15 leads to increased proliferation in
the cyclin–CDK system136. Cyclin–CDK complexes both the cardiomyocyte and non-myocyte compartments
modulate members of the retinoblastoma gene family after myocardial infarction at day 21, which results in
— retinoblastoma-associated protein (RB), p107 (also significant improvement in functional outcome21.
known as RBL1) and p130 (also known as RBL2) — A major outstanding challenge in the field is that reac-
which in turn lead to release of E2F transcription factors tivation of the cardiomyocyte cell cycle is frequently not
that activate genes for DNA synthesis. Overexpression followed by completion of cytokinesis to generate new
of CDK1, or knockdown of the CDK inhibitors p21, daughter cells. The identification of therapeutic factors,
p27KIP1 (also known as CDKN1B) and p57KIP2 by RNA miRNAs or small compounds that can drive bona fide
NATURE REVIEWS | DRUG DISCOVERY ADVANCE ONLINE PUBLICATION | 9
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
a
Exogenous ligands:
NRG1, FGF1, IGF1 and periostin
Activation of
cardiomyocyte
proliferation Intrinsic pathways: GATA4, MEIS1, YAP–TAZ, p38 MAPK,
Cardiomyocyte
miR-590, miR-199a, miR-302–367 and anti-miR-15
Epicardial stimulation
Activation and/or
transplantation of
progenitor populations Cardiac progenitor cells
Progenitor cell
GHMT
In vivo
reprogramming
Fibroblast • miRNAs (miR-1, miR-133, miR-208 and miR-499)
• Small molecules
Autologous: iPSC-derived
Exogenous
cardiomyocyte
replacement Exogenous mature Allogeneic: iPSC and/or ESC-derived
cardiomyocyte
Tβ4 WNT inhibitors,
for example, SFRP2
1
Epicardial cells
PDGFR
NRG1 WNTs blockade
• FGF2
• VEGFA
• FSTL1 • GATA4
• HAND2 4
• MEF2C
FSTL1 • TBX5
2 Angiogenesis
Lymphangiogenesis
Cardiomyocytes
Fibroblasts
VEGFA VEGFC
3
CCL2–CCR2 Relaxin HDAC Chymase
Macrophages blockade inhibitors inhibitors
Pro-fibrotic signals
10 | ADVANCE ONLINE PUBLICATION www.nature.com/nrd
Nature Reviews | Drug Discovery
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
◀ Figure 3 | Therapeutic strategies for heart regeneration. a | Strategies for which was first recognized in the newt lens more than
replacement of cardiomyocytes. Reactivation of cardiomyocyte proliferation is the 100 years ago150. Zebrafish use transdifferentiation of
major mechanism by which endogenous regeneration occurs in zebrafish and neonatal α-cells to β-cells to regenerate islets, and in the heart,
mouse models. It has been achieved in preclinical models by targeting upstream reprogramming of atrial to ventricular cardiomyocytes
ligands, such as neuregulin 1 (NRG1) and fibroblast growth factor 1 (FGF1), and
occurs after injury 151,152. Reprogramming of hepatocytes
downstream cell cycle pathways such as those mediated by MEIS1, YES-associated
protein 1 (YAP1)–TAZ, p38 mitogen-activated protein kinase (MAPK), and microRNAs
to biliary endothelial cells has been described in liver
(miRNAs), including miR‑590, miR‑199a and the miR‑302–367 cluster. Stimulation of regeneration in mice153.
progenitor populations, such as the epicardium or cardiac progenitor cells, leads to Large numbers of human cardiomyocytes can be pro-
pleiotropic effects to support cardiomyocyte survival and proliferation, but current duced by differentiation of ESCs. Chong et al. demon-
strategies do not seem to directly lead to new cardiomyocytes in significant numbers. strated that transplanted human ESC cardiomyocytes (at a
In vivo reprogramming of fibroblasts to produce cardiomyocytes has been achieved in dose of 1 × 109 per heart) survive and contribute new myo-
preclinical models using defined transcription factor cocktails — for example, GHMT, cardium to macaque hearts after direct injection 2 weeks
which consists of GATA4, heart and neural crest derivatives-expressed protein 2 following myocardial infarction154. Although a powerful
(HAND2), myocyte-specific enhancer factor 2C (MEF2C) and T-box protein 5 (TBX5) — proof of concept, evidence of functional improvement was
and microRNAs (miRNAs), and in vitro by using small molecules. Replacement of
lacking, and ventricular arrhythmias were recorded in all
cardiomyocytes by transplantation of exogenous mature cardiomyocytes, derived from
induced pluripotent stem cells (iPSCs) or embryonic stem cells (ESCs), has shown proof
animals, which suggests that significant hurdles with elec-
of concept in large animal studies. b | Therapeutic targeting of the non-cardiomyocyte trical integration remain before human trials could safely
compartment for cardiac regeneration. Epicardial activation (mechanism 1): during be undertaken (TABLE 2). Furthermore, ethical concerns
cardiac development and after injury, soluble factors derived from the activated exist regarding the use of embryonic tissue, and as it is
epicardium support angiogenesis, cardiomyocyte proliferation and survival, including an allogeneic product, recipients would require lifelong
follistatin-related protein 1 (FSTL1), FGF2 and vascular endothelial growth factor A immunosuppression to prevent rejection of the cells.
(VEGFA). The use of factors (such as thymosin β4 (Tβ4)) that activate or direct the Reprogramming of fibroblasts to cardiomyocytes
epicardium to promote repair, or delivery of specific recombinant factors identified offers potential advantages: a non-immunogenic cell
from the epicardium, are unexploited therapeutic strategies. Angiogenesis and product, derived from the patient’s own cells, and no
lymphangiogenesis (mechanism 2): replacement of damaged vasculature will be vital to
requirement for embryonic tissue. Inspired by the rev-
support new survival of transplanted, reprogrammed or proliferated cardiomyocytes.
Delivery of recombinant VEGFC, which is a macrophage-derived cytokine that
olutionary description of induced pluripotency by
promotes lymphangiogenesis, improves healing and functional outcome following Yamanaka, reprogramming approaches were initially
myocardial infarction in mice. Immunomodulation (mechanism 3): inhibition of C-C undertaken ex vivo, which relied on an intermediate
motif chemokine ligand 2 (CCL2)–C-C chemokine receptor type 2 (CCR2) signalling in induced pluripotent stem cell (iPSC) stage155. By trans-
monocyte–macrophages by delivery of small interfering RNA (siRNA) nanoparticles planting iPSC-derived cardiomyocytes in a non-human
reduces monocyte infiltration and infarct size in mice. Signals from the epicardium have primate model, Shiba et al. showed improvement in
recently been identified that recruit regulatory T (Treg) cells to dampen inflammation function following cell transplant, but also a significant
following injury. Fibrosis (mechanism 4): harnessing endogenous antifibrotic pathways ventricular arrhythmia rate156 (TABLE 2). However, produc-
mediated by NRG1 or relaxin may be used to halt progression of cardiac remodelling tion of an autologous cell product is expensive, subject to
and heart failure. The targeting of pro-fibrotic pathways with inhibitors of
variability and has restricted commercial opportunity. In
platelet-derived growth factor receptor (PDGFR), WNTs, chymase or histone
deacetylases (HDACs) has shown promise in small-animal models. Last, in vivo
addition to biological hurdles, the logistical and finan-
reprogramming of fibroblasts into cardiomyocytes, using GATA4, HAND2, MEF2C and cial barriers to clinical use of autologous cell therapies
TBX5, may allow replacement of cardiomyocytes, restoration of function and prevent are extremely challenging. Current cell numbers in the
fibrosis. Current therapeutic strategies are shown in blue boxes, and endogenous macaque trials have been in the order of 108–109 cells,
signalling pathways are shown in orange boxes. IGF1, insulin-like growth factor 1; but cell numbers of at least an order of magnitude higher
SFRP2, secreted frizzled-related protein 2. would be required for humans. The infrastructure and
running costs of good manufacturing production at this
scale, ideally embedded within or close to clinical cardiac
centres, seem prohibitive.
cytokinesis would benefit greatly from improved read- The discovery that delivery of three cardiac develop-
Embryonic stem cells
(ESCs). Pluripotent stem cells outs of completed cell division. Efforts towards this mental transcription factors — GATA4, myocyte-specific
that are derived from the inner include the anillin–GFP model, which provides a poten- enhancer factor 2C (MEF2C) and T-box protein 5
cell mass of embryos. tial mechanism for discriminating cytokinesis from (TBX5) — could drive direct reprogramming of fibro-
endoreduplication148. Despite these recent advances, blasts into cardiomyocytes, without an intermediate
Allogeneic
Derived from genetically
accurately quantifying dividing cardiomyocytes within cell stage, has opened the door to the concept of repro-
different individuals from the the adult mammalian heart is extremely difficult and gramming in vivo157,158. Several additional factors that
same species. would greatly benefit from further research focus. improve the efficiency of reprogramming have now
been identified, most notably HAND2 (REF. 159). This
Induced pluripotent stem
De novo cardiomyocytes by cellular reprogramming. approach requires no cell product, which eliminates the
cell
(iPSC). Pluripotent stem cells Production of de novo cardiomyocytes by directed dif- need for complex manufacturing. Proof of concept for
that are reprogrammed from ferentiation of embryonic stem cells (ESCs), or repro- in vivo reprogramming has now been demonstrated in
somatic cells by introducing gramming of differentiated non-myocyte cells (for mouse models in which transdifferentiated cells express
pluripotency factors. example, fibroblasts) to a cardiomyocyte fate, has revo- sarcomeric proteins, form gap junctions and drive
Autologous
lutionized therapeutic approaches to regeneration26,149. sustained improvement in ventricular function160–163.
Derived from cells or tissues of Interestingly, reprogramming by transdifferentiation Substantial challenges remain, including achieving
the same individual. is a strategy deployed in endogenous regeneration, selectivity of targeting to the heart, reprogramming
NATURE REVIEWS | DRUG DISCOVERY ADVANCE ONLINE PUBLICATION | 11
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Table 2 | Translational pipeline: preclinical large-animal regeneration studies in heart failure following myocardial infarction
Drug or therapy Mechanism Model and delivery Outcome Comment Refs
Allogeneic Direct cardiomyocyte • Heart failure (2 weeks Significant improvement in • Proof-of-principle study 156
iPSC-derived replacement post‑ischaemia–reperfusion) LVEF (~10%) at 12 weeks • All transplanted animals
cardiomyocytes • Surgical intramyocardial experienced sustained
injection ventricular tachycardia
peaking at day 14
post-transplantation
FGF1‑loaded and • Angiogenesis • Heart failure (4 weeks Approximately 8–10% Reduced ventricular 143
NRG1‑loaded • Reversal of fibrosis post‑ischaemia–reperfusion) improvement in fractional remodelling observed
microparticles • Catheter-based shortening with both NRG1
transendocardial injection and FGF1 microparticles
Human Direct cardiomyocyte • Heart failure (2 weeks • Successful transplantation, First study to demonstrate 154
ESC‑derived replacement post‑ischaemia–reperfusion) electromechanical regeneration by
cardiomyocytes • Surgical intramyocardial integration and partial transplantation of
injection maturation of ESC‑derived cardiomyocytes. All
cardiomyocytes transplanted animals
• No significant change experienced ventricular
in LVEF arrhythmias
IGF1 and HGF • Stimulation of • Heart failure (4 weeks • Small improvement in • Overall small functional 227
within hydrogel cardiomyocyte post‑ischaemia–reperfusion) LVEF effects observed
proliferation • Catheter-based • Reduced scar formation • Trend towards reduced
• Angiogenesis transendocardial injection fibrosis
MR‑409 • Pleiotropic effects • Heart failure (2 weeks Reduced scar size after Not accompanied by 228
(GHRH agonist) • Activation of the post‑ischaemia–reperfusion) 4 weeks improved cardiac function
growth hormone– • Subcutaneous injection
IGF1 axis
Recombinant • Pleiotropic effects • Heart failure (1 week Approximately 10% – 167
FSTL1 in patch • Stimulation of post-ischaemia–reperfusion) improvement in LVEF
cardiomyocyte • Surgical patch implantation
proliferation
• Arteriogenesis
ESC, embryonic stem cell; FGF1, fibroblast growth factor 1; FSTL1, follistatin-related protein 1; GHRH, growth hormone-releasing hormone; HGF, hepatocyte
growth factor; IGF1, insulin-like growth factor 1; iPSC, induced pluripotent stem cell; LVEF, left ventricular ejection fraction; NRG1, neuregulin 1.
human cells that have stable epigenetic modifications factor that promotes myocardial regeneration after
and achieving maturation of structure and function in injury. Application of a patch that contains recombinant
reprogrammed cells. human FSTL1 improved long-term cardiac function in
mice following surgically-induced myocardial infarction
Neovascularization and lymphangiogenesis and in a swine model of ischaemia–reperfusion injury167
Strategies aimed at neovascularization in myocardial (TABLE 2). Furthermore, Zangi et al. have shown that intra
infarction have been somewhat frustrated in recent years cardiac injection of a modified RNA (in which one or
by the failed promise of VEGFA. Despite several ani- more nucleotides is replaced by modified nucleotides)
mal studies that showed efficacy from the recombinant encoding VEGFA led to enhanced epicardial progenitor
protein or gene therapy with VEGFA, the double-blind activation and improved functional outcome after myo-
EUROINJECT-ONE and NORTHERN clinical trials cardial infarction168. The modified RNA of VEGFA pro-
failed to show therapeutic benefit 164,165. The reactivation motes differentiation of EPDCs towards an endothelial
of more comprehensive developmental programmes of (and, to a lesser extent, cardiomyocyte) cell fate168.
coronary vessel formation, such as targeting retained Clinical translation would greatly benefit from the
adult cell types that previously contributed to the devel- ability to image the epicardium in vivo, and emerging
oping coronaries — including the coronary sinus (sinus technologies using positron emission tomography (PET),
venosus-derived cells), the endocardium and the epi- single-photon emission-computed tomography (SPECT)
cardium — is a more attractive strategy for invoking and molecular imaging to demonstrate angiogenesis
neovascularization post‑myocardial infarction. will guide future trials169. The endocardium continues
The epicardium in particular has emerged as a viable to provide further endothelium for vessel formation
target, and the development of in vitro systems for cul- for a short period during postnatal growth and might
turing human epicardium that is derived from human be reactivated in adulthood to enhance neovasculariza-
pluripotent stem cells will facilitate both biological tion170. Interestingly, experimental myocardial infarction
understanding of its heterogeneity and small-molecule in mice has recently been shown to activate endothelial
screening for activating compounds166. Recently, epi- remodelling on the endocardial surface, which leads to
cardial follistatin-related protein 1 (FSTL1) has been outgrowth of pre-existing coronary vessels and de novo
identified as a key anti-apoptotic and proliferative arteriogenesis171.
12 | ADVANCE ONLINE PUBLICATION www.nature.com/nrd
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Table 3 | Recent clinical trials targeting cardiac injury and repair after acute myocardial infarction
Trial Drug Mechanism Phase and patient Primary end Outcome Refs
cohort point
Lenihan et al. (2016) Cimaglermin Recombinant • Phase I Safety/ • No severe adverse effects 145
alfa (Acorda full-length • 40 patients with tolerability • Improvement in LVEF in
Therapeutics) neuregulin 1β3 symptomatic heart the high-dose groups
failure and LVEF ≤40% (~7–9%) lasting for study
• Heart failure aetiology duration (90 days)
not reported
LATITUDE-TIMI 60 Losmapimod p38 MAPK inhibitor • Phase III Major adverse No significant difference in 229
(2016) (GSK) • 3503 patients with ACS cardiovascular primary end point or heart
events at failure events
24 weeks
TIPTOP Doxycycline Oral MMP inhibitor • Phase II Change in Significant reduction in 230
(2013) • 110 patients with STEMI LVEDVI at LVEDVI and infarct size with
6 months doxycycline
VCU‑ART2 Anakinra IL‑1R antagonist • Phase II Change in • No signficant change in 231
(2013) (Amgen; • 30 patients with STEMI LVESVI at LVESVI, LVEDVI or LVEF
Swedish ~3 months • Combined data from
Orphan VCU‑ART2 and VCU-ART
Biovitrum) studies suggested a
reduction in heart failure
events in the anakinra arm
• Recruitment for a larger
trial (VCU‑ART3) is
currently ongoing
Gullestad et al. IVIG (Bayer Immunomodulation • Phase II Change in LVEF No significant difference in 232
(2013) HealthCare) • 62 STEMI patients at 6 months change in LVEF or scar size
REVEAL Erythropoietin Pleiotropic effects on • Phase II Infarct size • No significant difference in 233
(2011) injury and repair • 222 patients with STEMI infarct size
• Increased rate of adverse
events with erythropoietin
VCU-ART Anakinra IL‑1R antagonist • Phase II pilot Change in Significant improvement in 234
(2010) (Amgen; • 10 patients with STEMI LVESVI at LVESVI on cardiac MRI
Swedish ~3 months
Orphan
Biovitrum)
Gao et al. (2010) Neucardin Recombinant • Phase II Change in LVEF, Non-significant trend 235
(Zensun epidermal growth • 44 patients with end-systolic towards improved LVEF
Shanghai) factor-like domain of symptomatic heart volume, or and reduced left ventricular
neuregulin 1β failure and LVEF ≤40%. end-diastolic remodelling in the
Heart failure aetiology volume at neuregulin arms
not reported 90 days
APEX AMI Pexelizumab Humanized • Phase III All-cause No significant difference in 236
(2007) (Alexion) monoclonal antibody • 5,745 patients with mortality at mortality, or in secondary
neutralizing C5 STEMI 30 days composite end point of
component of the death, shock or heart failure
complement system at 30 and 90 days
PREMIER PG 116800 Oral MMP inhibitor • Phase II Change in No significant difference in 237
(2006) (Procter & • 253 patients with LVEDVI at LVEDVI after 30 or 90 days
Gamble) STEMI and impaired 90 days
left ventricular function
(LVEF 15–40%)
ACS, acute coronary syndrome; GSK, GlaxoSmithKline; IL‑1R, interleukin‑1 receptor; IVIG, intravenous immunoglobulin; LVEDVI, left ventricular end-diastolic volume
index; LVEF, left ventricular ejection fraction; LVESVI, left ventricular end-systolic volume index; MAPK, mitogen-activated protein kinase; MMP, matrix
metalloproteinase; MRI, magnetic resonance imaging; STEMI, ST-segment elevation myocardial infarction.
Stimulation of lymphangiogenesis is another emerg- In rodents, augmentation of lymphangiogenesis by
ing strategy to augment repair. The cardiac lymphat- stimulation of VEGFC signalling, which is the princi-
ics remain poorly understood but are important for pal cytokine mediator of lymphatic formation during
transport of interstitial fluid and trafficking of immune development, improves healing, reduces fibrosis and
cells172. Following myocardial infarction, endogenous preserves myocardial function174,175. The precise mech-
Lymphangiogenesis
repair mechanisms activate lymphangiogenesis in mice anisms underlying this process are poorly understood
The growth of new lymphatic and humans, which is a response that is required for but may relate to clearance of oedema and resolution of
vessels. clearance of oedema and resolution of inflammation173. inflammation.
NATURE REVIEWS | DRUG DISCOVERY ADVANCE ONLINE PUBLICATION | 13
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
Immunomodulation myocardium184. Other prospective antifibrotic strategies
Components of functional pathways, which can loosely in early-stage studies include inhibitors of WNT signal-
be termed ‘inflammation’, are intricately linked to healing ling and histone deacetylases, and modulation of relaxin
following myocardial infarction. Several unsuccessful signalling 179 (FIG. 3b).
clinical trials of immunosuppressive agents (for exam- Before clinical trials in humans are carried out, an
ple, methylprednisolone, intravenous immunoglobulin improved understanding of the heterogeneity of human
(IVIG), pexelizumab (Alexion), anakinra (Amgen; post‑myocardial infarction healing is required to allow
Swedish Orphan Biovitrum); see TABLE 3) suggest that targeting of antifibrotic therapies to groups at highest
blunt inhibition of inflammation is not effective176. risk. For example, the use of advanced imaging and
Successful immunomodulation probably requires more novel biomarkers of inflammation and fibrosis in the
nuanced stratification of patients based on known acti- early phase of myocardial infarction may identify out-
vation (or inhibition) of specific pathways, coupled with lier patient subpopulations, who could then be targeted
identification and successful in vivo targeting of spe- with specific therapies.
cific immune cell subsets (or pathways), to bring about
beneficial repair. For example, inhibition of the CCR2+ Translational considerations
monocyte population that is mobilized after myocardial The past decade of clinical cell therapy trials has provided
infarction using nanoparticle-delivered CCR2‑targeting important lessons for the design and translation of future
small interfering RNA (siRNA) leads to reduced injury regenerative therapies185,186. Issues related to the use of ani-
and post-myocardial infarction left ventricular remod- mal models, drug discovery approaches, patient selection
elling in mice177. Transplantation of specific immune and clinical trial design will be discussed in turn.
cell populations is a strategy that is being tested in
other diseases: autologous macrophages are being tri- Limitations of animal models
alled for regression of liver fibrosis178, and infusion of Animal models have unquestionable value as a route to
Treg cells has shown efficacy in reduction of inflamma- novel biological insights, and there is extensive species
tion. Furthermore, understanding the differences of conservation in regenerative signalling pathways such
the immune response in the setting of scar formation as Notch, TGFβ and Janus kinase (JAK)–STAT path-
compared with regeneration will shed light on precise ways187. However, from a translational perspective, there
pathways that can be modulated to enhance regeneration is a pressing need to improve the filtering of therapeutic
without compromising repair. In patients with chronic targets and compounds before human studies. Many
heart failure, immunomodulation is unlikely to be suffi- recent clinical trials of compounds aimed at promoting
cient to induce regeneration. However, immunosuppres- cardiac repair have shown limited efficacy (TABLE 3), and
sion or induction of tolerance will be required to prevent this has led to questions regarding the validity of animal
rejection of allogeneic cardiomyocyte cell therapies or models for assessing novel therapeutic strategies.
vectors used to deliver a reprogramming cocktail. For regenerative therapies, a key problem inherent
in existing animal studies is the use of young, healthy,
Fibrosis inhibition homogeneous populations that lack the comorbidities
Inhibition of pro-fibrotic signalling in the setting of or drug confounders typically associated with human
chronic heart failure has been suggested to account patients. Age is inversely correlated with capacity for
for some of the existing benefits of beta-blockers, repair, with older mice demonstrating impaired wound
angiotensin-converting enzyme inhibitors, angioten- healing after myocardial infarction188. In young animals,
sin receptor blockers and statins. Several novel antifi- the ‘bar’ to improved repair is low, which leads to false
brotic compounds are emerging and have recently been positive results and subsequent failed large-animal or
reviewed in the context of cardiovascular disease179. human studies. Development of highly non-regenerative
Inhibition of scar formation after myocardial infarc- animal models, such as aged rodents or pigs, might help
tion may have a complementary role to stimulation of to reduce false-positive studies before human trials.
endogenous repair or cell therapy, but without effective
replacement of cardiomyocytes, it remains crucial to pre- Drug discovery
vent cardiac rupture. However, targeting late ‘reactive’ Focused drug discovery approaches to cardiac regenera-
fibrosis in the uninjured myocardium may reduce ven- tion are complicated by the breadth of therapeutic strate-
tricular remodelling and progression to heart failure180. gies that persist in the academic arena, which range from
For example, in addition to its effects on cardiomyocyte cell replacement and reprogramming to stimulation of
proliferation, NRG1 administered 7–35 days following endogenous regeneration (FIG. 3a; TABLE 2). To advance
myocardial infarction reduces fibrosis and remodelling drug discovery, a move towards the use of phenotypic
in a swine model through inhibition of myofibroblast screens, in vivo discovery and combination approaches
transdifferentiation and TGFβ signalling 181. Inhibition will be required, in which underlying biological insights
of chymase, which stimulates fibroblast activation are used for target deconvolution. For example, screen-
after injury, reduces fibrotic area and improves sur- ing for cardiomyocyte cell cycle reactivation in vivo using
vival following myocardial infarction in small-animal the fluorescent ubiquitylation-based cell cycle indicator
models 182,183. In rats, blockade of platelet-derived (FUCCI) reporter in zebrafish has been used to identify
growth factor receptor (PDGFR) signalling with imati- compounds targeting the Hedgehog, insulin-like growth
nib selectively inhibits fibrosis in the non-infarcted factor and TGFβ pathways, which effectively stimulate
14 | ADVANCE ONLINE PUBLICATION www.nature.com/nrd
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
cell cycle re‑entry 189. Furthermore, the ‘FunSel’ screen- size in cohorts at large, it remains difficult to accurately
ing approach, in which a cDNA library of the mouse predict future heart failure events for a given patient. In
secretome is targeted to cardiomyocytes in vivo using practice, this means that it may be difficult to justify the
an adenoviral vector, has been applied to identify cardio use of the highest-risk interventions (for example, cell
protective factors190. Targeted sequencing to identify fac- reprogramming) in this cohort of patients.
tors that are enriched after myocardial infarction have Better identification of patients at risk of heart fail-
revealed that cardiomyocytes transfected with ghrelin ure is required: emerging possibilities for enhanced
improved cell survival after injury. characterization derive from novel, mechanistically rel-
Once novel screening systems are established, evant biomarkers, including exosome characterization,
partnerships with pharmaceutical companies should miRNA profiling and cellular transcriptomics93. The goal
be established early to access screening libraries and is to develop diagnostics that provide quantifiable data
improve the process of lead generation and optimiza- on therapeutically relevant targets, which can be used to
tion. Many paradigms that are effective in vitro or in recruit patients to specific therapies. As noted in the can-
preclinical models may fail to translate into the clinic. cer field, it seems likely that optimal characterization will
Assessment of compounds across multiple assays, or require approaches that combine imaging and panels of
screening to assess the cumulative benefit of targeting biomarkers for mechanistic staging.
multiple parallel pathways for a given end point (for In patients with chronic heart failure, the disease
example, cardiomyocyte proliferation), may result in is established, and in those with severely impaired left
improved clinical efficacy downstream191,192. ventricular function and New York Heart Association
(NYHA) III–IV symptoms, the prognosis is extremely
Delivery systems poor. As such, regenerative strategies that carry higher
The targeting of the heart is achievable through a com- risk may be reasonable. Implantable cardioverter defibril-
bination of local delivery, biomaterial adjuncts and lators are already indicated in this patient group to pro-
biological selectivity. For delivery, advances in catheter tect from arrhythmia, and therefore cardiomyocyte cell
technology have made transendocardial injection, sub- therapy, reprogramming or cell patches, which may all
epicardial access and intracoronary injection available be arrhythmogenic, represent therapeutic strategies that
through a percutaneous, minimally invasive approach193. should be used in this cohort. The subgroup of patients
Surgical approaches by median sternotomy may be on left ventricular assist device therapy as a bridge to
reasonable for proof of principle but are not realistic for heart transplant could also be recruited, as cardiac tis-
the frail, comorbid heart failure population in general. sue may become available (at heart transplantation) to
Alongside delivery, major advances have been made in examine biological end points, such as cell engraftment.
the field of biomaterials and bioscaffolds128. Pre-seeded
scaffolds, patches or injectable hydrogels have been shown Clinical trial design
to improve retention and survival of transplanted cells194. Regenerative therapies require re‑evaluation of their
For non-cell-based approaches, delivery of factors within clinical trial paradigm197. Early trials of cell therapies
hydrogels or coated on microparticles can prevent rapid have been small, heterogeneous and subject to small-
clearance or degradation195. Local delivery and retention study effects, and subsequent studies have failed to
must be complemented with biological targeting (for reproduce an apparently large effect. Improvements
example, targeted liposomes, exosomes or viral vectors) in trial design, particularly at the phase II stage, have
or biological selectivity for cardiomyocyte pathways. The the potential to reduce this problem198. Whenever pos-
risks of off-target effects are greatest for pro-proliferative sible, phase II clinical studies should be designed to
or reprogramming approaches, which may disrupt remote demonstrate a defined biological effect as a surrogate
cell function or may be tumorigenic196. for efficacy. The biological effect could be angiogenesis,
evidence of engraftment or cell cycle re‑entry, and in
Patient selection turn needs development and validation of novel imag-
Targeting therapies to selected patient groups will be key ing strategies for regeneration199. This key step would
to the success of future regenerative therapy trials. Two allow biological insights to be correlated with clinical
distinct groups with separate biological and logistical outcomes, to prioritize some therapies for large-scale,
challenges are patients with acute myocardial infarction placebo-controlled trials. These should ideally be car-
and patients with chronic heart failure. ried out as part of consensus regenerative medicine net-
The acute myocardial infarction population is attrac- works, such as the Cardiovascular Cell Therapy Research
tive for regenerative therapies that modulate or harness Network, which has been instrumental in organizing
existing repair pathways; for example, factors to pro- large studies to show that bone marrow-derived mono-
mote cardiomyocyte proliferation or angiogenesis, epi- nuclear cells in acute myocardial infarction or ischaemic
cardial targeting, immunomodulation or inhibition of cardiomyopathy do not improve left ventricular func-
fibrosis. However, the identification of precisely which tion, for example, the FOCUS-CCTRN trial200 (TABLE 1).
patients with myocardial infarction to target is difficult, Furthermore, there is increasing recognition of report-
as accurate predictors of future heart failure are lacking. ing issues with cell therapy trials, and more than 600
Although age, diabetes, coronary physiology or infarct reporting discrepancies have been identified across 49
characteristics on cardiac MRI (for example, oedema, trials201. Of concern, the number of discrepancies cor-
haemorrhage or MVO) are predictors of final infarct relate with the reported effect size in the trial. There is
NATURE REVIEWS | DRUG DISCOVERY ADVANCE ONLINE PUBLICATION | 15
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
a need for standardization of cell characterization, han- a realistic first step and would have therapeutic value.
dling, methodology and reporting practice (akin to the The emerging biology of endogenous regeneration and
Preferred Reporting Items for Systematic Reviews and cardiomyocyte biology is exposing a multiplicity of
Meta-Analyses (PRISMA) or Consolidated Standards of therapeutic targets that could be exploited by conven-
Reporting Trials (CONSORT)) for trials. tional small-molecule approaches, recombinant factors,
miRNAs, reprogramming or cell transplantation.
Conclusions A closer partnership of scientists, spin-outs, the phar-
Novel regenerative therapies inspire great hope among maceutical industry and clinical trialists is required to
patients, scientists, physicians, the media and the public improve the commercialization of regenerative thera-
at large. Although this excitement can be warranted, it pies. There is a role for the pharmaceutical industry in
can easily lead to exaggeration of actual benefits. It is early partnership with scientists to test compound librar-
challenging to balance the needs of a desperate patient ies in novel in vitro or in vivo screens. Improved preclini-
population and the requirements for scientific rigour. cal models, patient selection and design of early clinical
Guidelines from the International Society for Stem Cell studies to establish biological efficacy in human subjects
Research specifically warn against the dangers of hype as will help to streamline the next generation of regenera-
novel therapies emerge202,203. Progress with regenerative tive therapy trials. At the national level, governmental
therapies is likely to be incremental and iterative rather support is required through facilitation of regulation and
than in the form of a quantum leap. funding for incubator and/or facilitator organizations,
Although complete regeneration of the infarcted such as the Cell and Gene Therapy Catapult (UK), the
heart is the end goal, marginal gains in cardiomyo- Centre for Commercialization of Regenerative Medicine
cyte number, neovascularization or scar reduction are and CellCAN (both in Canada).
1. Roger, V. L. Epidemiology of heart failure. Circ. Res. 18. Witman, N., Murtuza, B., Davis, B., Arner, A. & 34. Murry, C. E. et al. Haematopoietic stem cells do not
113, 646 (2013). Morrison, J. I. Recapitulation of developmental transdifferentiate into cardiac myocytes in myocardial
2. Cahill, T. J., Ashrafian, H. & Watkins, H. Genetic cardiogenesis governs the morphological and infarcts. Nature 428, 664–668 (2004).
cardiomyopathies causing heart failure. Circ. Res. 113, functional regeneration of adult newt hearts following This is a landmark study that refutes the concept
660–675 (2013). injury. Dev. Biol. 354, 67–76 (2011). of bone marrow-derived progenitor cells as
3. Braunwald, E. The war against heart failure: the 19. González-Rosa, J. M., Martín, V., Peralta, M., a source of new cardiomyocytes in the mouse.
Lancet lecture. Lancet 385, 812–824 (2015). Torres, M. & Mercader, N. Extensive scar formation 35. Balsam, L. B. et al. Haematopoietic stem cells adopt
4. Velagaleti, R. S. et al. Long-term trends in the and regression during heart regeneration after mature haematopoietic fates in ischaemic
incidence of heart failure after myocardial infarction. cryoinjury in zebrafish. Development 138, 1663 myocardium. Nature 428, 668–673 (2004).
Circulation 118, 2057 (2008). (2011). 36. Ahuja, P., Sdek, P. & MacLellan, W. R. Cardiac
5. Ezekowitz, J. A. et al. Declining in‑hospital mortality 20. Porrello, E. R. et al. Transient regenerative potential of myocyte cell cycle control in development, disease,
and increasing heart failure incidence in elderly the neonatal mouse heart. Science 331, 1078–1080 and regeneration. Physiol. Rev. 87, 521 (2007).
patients with first myocardial infarction. J. Am. Coll. (2011). 37. Bergmann, O. et al. Evidence for cardiomyocyte
Cardiol. 53, 13–20 (2009). This study is the first report of mammalian heart renewal in humans. Science 324, 98 (2009).
6. Heidenreich, P. A. et al. Forecasting the impact of regeneration. This study describes the identification and
heart failure in the United States. Circ. Heart Fail. 6, 21. Porrello, E. R. et al. Regulation of neonatal and adult quantification of cardiomyocyte replication in the
606 (2013). mammalian heart regeneration by the miR‑15 family. human heart using carbon‑14 dating.
7. Katz, A. M. The “modern” view of heart failure. Circ. Proc. Natl Acad. Sci. USA 110, 187–192 (2013). 38. Mollova, M. et al. Cardiomyocyte proliferation
Heart Fail. 1, 63 (2008). 22. Haubner, B. J. et al. Functional recovery of a human contributes to heart growth in young humans.
8. Jhund, P. S. & McMurray, J. J. V. The neprilysin neonatal heart after severe myocardial infarction. Circ. Proc. Natl Acad. Sci. USA 110, 1446–1451 (2013).
pathway in heart failure: a review and guide on the Res. 118, 216–221 (2016). 39. Puente, B. N. et al. The oxygen-rich postnatal
use of sacubitril/valsartan. Heart 102, 1342 23. Fratz, S. et al. Long-term myocardial scarring after environment induces cardiomyocyte cell-cycle arrest
(2016). operation for anomalous left coronary artery from the through DNA damage response. Cell 157, 565–579
9. Kloner, R. A. Current state of clinical translation of pulmonary artery. Ann. Thorac. Surg. 92, 1761–1765 (2014).
cardioprotective agents for acute myocardial (2011). 40. Kimura, W. et al. Hypoxia fate mapping identifies
infarction. Circ. Res. 113, 451 (2013). 24. Tsang, V. et al. Late donor cardiectomy after paediatric cycling cardiomyocytes in the adult heart. Nature
10. Nguyen, P. K., Rhee, J. & Wu, J. C. Adult stem cell heterotopic cardiac transplantation. Lancet 374, 523, 226–230 (2015).
therapy and heart failure, 2000 to 2016: a systematic 387–392 (2009). 41. Engel, F. B. et al. p38 MAP kinase inhibition enables
review. JAMA Cardiol. 1, 831–841 (2016). 25. Carlson, B. M. Some principles of regeneration in proliferation of adult mammalian cardiomyocytes.
11. Yester, J. W. & Kühn, B. Mechanisms of mammalian systems. Anat. Rec. B New Anat. 287, Genes Dev. 19, 1175–1187 (2005).
cardiomyocyte proliferation and differentiation in 4–13 (2005). 42. Mahmoud, A. I. et al. Meis1 regulates postnatal
development and regeneration. Curr. Cardiol. Rep. 26. Xin, M., Olson, E. N. & Bassel-Duby, R. Mending cardiomyocyte cell cycle arrest. Nature 497, 249–253
19, 13 (2017). broken hearts: cardiac development as a basis for (2013).
12. Karra, R. & Poss, K. D. Redirecting cardiac growth adult heart regeneration and repair. Nat. Rev. Mol. This study describes the identification of MEIS1 as
mechanisms for therapeutic regeneration. J. Clin. Cell Biol. 14, 529–541 (2013). an inhibitor of the cardiomyocyte cell cycle.
Invest. 127, 427–436 (2017). 27. Kretzschmar, K. & Watt, F. M. Lineage tracing. Cell 43. Lee, K.‑F. et al. Requirement for neuregulin receptor
13. Vivien, C. J., Hudson, J. E. & Porrello, E. R. 148, 33–45 (2012). erbB2 in neural and cardiac development. Nature
Evolution, comparative biology and ontogeny of 28. Jopling, C. et al. Zebrafish heart regeneration occurs 378, 394–398 (1995).
vertebrate heart regeneration. Regen. Med. 1, by cardiomyocyte dedifferentiation and proliferation. 44. Gassmann, M. et al. Aberrant neural and cardiac
16012 (2016). Nature 464, 606–609 (2010). development in mice lacking the ErbB4 neuregulin
14. Gonzalez-Rosa, J. M. & Mercader, N. Cryoinjury as 29. Kikuchi, K. et al. Primary contribution to zebrafish receptor. Nature 378, 390–394 (1995).
a myocardial infarction model for the study of cardiac heart regeneration by gata4+ cardiomyocytes. Nature 45. Gemberling, M., Karra, R., Dickson, A. L. & Poss, K. D.
regeneration in the zebrafish. Nat. Protoc. 7, 464, 601–605 (2010). Nrg1 is an injury-induced cardiomyocyte mitogen for
782–788 (2012). References 28 and 29 show that new cardiomyocytes the endogenous heart regeneration program in
15. Wang, J. et al. The regenerative capacity of zebrafish in the regenerating heart are derived from the zebrafish. eLife 4, e05871 (2015).
reverses cardiac failure caused by genetic existing cardiomyocyte pool. 46. Yelon, D. et al. The bHLH transcription factor
cardiomyocyte depletion. Development 138, 3421 30. Senyo, S. E. et al. Mammalian heart renewal by pre- hand2 plays parallel roles in zebrafish heart and
(2011). existing cardiomyocytes. Nature 493, 433–436 (2013). pectoral fin development. Development 127, 2573
16. Parente, V. et al. Hypoxia/reoxygenation cardiac injury 31. Ellison, G. M. et al. Adult c‑kit+ cardiac stem cells are (2000).
and regeneration in zebrafish adult heart. PLoS ONE necessary and sufficient for functional cardiac 47. Srivastava, D. et al. Regulation of cardiac mesodermal
8, e53748 (2013). regeneration and repair. Cell 154, 827–842 (2013). and neural crest development by the bHLH
17. Poss, K. D., Wilson, L. G. & Keating, M. T. Heart 32. van Berlo, J. H. & Molkentin, J. D. An emerging transcription factor, dHAND. Nat. Genet. 16,
regeneration in zebrafish. Science 298, 2188 consensus on cardiac regeneration. Nat. Med. 20, 154–160 (1997).
(2002). 1386–1393 (2014). 48. Schindler, Y. L. et al. Hand2 elevates cardiomyocyte
This study is the first definitive report of heart 33. Orlic, D. et al. Bone marrow cells regenerate infarcted production during zebrafish heart development and
regeneration. myocardium. Nature 410, 701–705 (2001). regeneration. Development 141, 3112 (2014).
16 | ADVANCE ONLINE PUBLICATION www.nature.com/nrd
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
49. Yu, W. et al. GATA4 regulates Fgf16 to promote heart 75. Smart, N. et al. De novo cardiomyocytes from within 100. Ma, Y. et al. Temporal neutrophil polarization following
repair after injury. Development 143, 936 (2016). the activated adult heart after injury. Nature 474, myocardial infarction. Cardiovasc. Res. 110, 51
50. Zhou, Q., Li, L., Zhao, B. & Guan, K.‑L. The hippo 640–644 (2011). (2016).
pathway in heart development, regeneration, and 76. Smart, N. et al. Thymosin β4 induces adult epicardial 101. Kyritsis, N. et al. Acute inflammation initiates the
diseases. Circ. Res. 116, 1431 (2015). progenitor mobilization and neovascularization. regenerative response in the adult zebrafish brain.
51. Heallen, T. et al. Hippo pathway inhibits Wnt signaling Nature 445, 177–182 (2007). Science 338, 1353 (2012).
to restrain cardiomyocyte proliferation and heart size. 77. Zhou, B. et al. Adult mouse epicardium modulates This study showed that inflammation is sufficient to
Science 332, 458 (2011). myocardial injury by secreting paracrine factors. initiate regeneration in the zebrafish brain.
This study describes the identification of the Hippo J. Clin. Invest. 121, 1894–1904 (2011). 102. Karin, M. & Clevers, H. Reparative inflammation takes
pathway as a key mediator of cardiomyocyte 78. Rui, L. et al. Extending the time window of charge of tissue regeneration. Nature 529, 307–315
proliferation. mammalian heart regeneration by thymosin beta 4. (2016).
52. Xin, M. et al. Hippo pathway effector Yap promotes J. Cell. Mol. Med. 18, 2417–2424 (2014). 103. Aurora, A. B. & Olson, E. N. Immune modulation of
cardiac regeneration. Proc. Natl Acad. Sci. USA 110, 79. Hagensen, M. K., Vanhoutte, P. M. & Bentzon, J. F. stem cells and regeneration. Cell Stem Cell 15, 14–25
13839–13844 (2013). Arterial endothelial cells: still the craftsmen of (2014).
53. Hang, C. T. et al. Chromatin regulation by Brg1 regenerated endothelium. Cardiovasc. Res. 95, 281 104. Burzyn, D. et al. A special population of regulatory T
underlies heart muscle development and disease. (2012). cells potentiates muscle repair. Cell 155, 1282–1295
Nature 466, 62–67 (2010). 80. He, L. et al. Genetic lineage tracing discloses (2013).
54. Xiao, C. et al. Chromatin-remodelling factor Brg1 arteriogenesis as the main mechanism for collateral 105. Heredia, J. E. et al. Type 2 innate signals stimulate
regulates myocardial proliferation and regeneration in growth in the mouse heart. Cardiovasc. Res. 109, 419 fibro/adipogenic progenitors to facilitate muscle
zebrafish. Nat. Commun. 7, 13787 (2016). (2016). regeneration. Cell 153, 376–388 (2013).
55. Bersell, K., Arab, S., Haring, B. & Kühn, B. 81. Bayliss, P. E. et al. Chemical modulation of receptor 106. Zordan, P. et al. Macrophages commit postnatal
Neuregulin1/ErbB4 signaling induces cardiomyocyte signaling inhibits regenerative angiogenesis in adult endothelium-derived progenitors to angiogenesis and
proliferation and repair of heart injury. Cell 138, zebrafish. Nat. Chem. Biol. 2, 265–273 (2006). restrict endothelial to mesenchymal transition during
257–270 (2009). 82. Eyries, M. et al. Hypoxia-induced apelin expression muscle regeneration. Cell Death Dis. 5, e1031
56. Gupta, V. & Poss, K. D. Clonally dominant regulates endothelial cell proliferation and (2014).
cardiomyocytes direct heart morphogenesis. Nature regenerative angiogenesis. Circ. Res. 103, 432 107. Boulter, L. et al. Macrophage-derived Wnt opposes
484, 479–484 (2012). (2008). Notch signaling to specify hepatic progenitor cell fate
57. Kubin, T. et al. Oncostatin M is a major mediator of 83. Xu, C. et al. Arteries are formed by vein-derived in chronic liver disease. Nat. Med. 18, 572–579
cardiomyocyte dedifferentiation and remodeling. Cell endothelial tip cells. Nat. Commun. 5, 5758 (2014). (2012).
Stem Cell 9, 420–432 (2011). 84. Kikuchi, K. et al. Retinoic acid production by 108. Lin, S.‑L. et al. Macrophage Wnt7b is critical for
58. Di Talia, S. & Poss, K. D. Monitoring tissue endocardium and epicardium is an injury response kidney repair and regeneration. Proc. Natl Acad. Sci.
regeneration at single-cell resolution. Cell Stem Cell essential for zebrafish heart regeneration. Dev. Cell USA 107, 4194–4199 (2010).
19, 428–431 (2016). 20, 397–404 (2011). 109. Han, C. et al. Acute inflammation stimulates
59. Walsh, S., Pontén, A., Fleischmann, B. K. & Jovinge, S. 85. Zangi, L. et al. An IGF1R‑dependent pathway drives a regenerative response in the neonatal mouse heart.
Cardiomyocyte cell cycle control and growth estimation epicardial adipose tissue formation after myocardial Cell Res. 25, 1137–1151 (2015).
in vivo — an analysis based on cardiomyocyte nuclei. injury. Circulation 135, 59–72 (2017). 110. Aurora, A. B. et al. Macrophages are required for
Cardiovasc. Res. 86, 365–373 (2010). 86. Zhou, B. et al. Thymosin beta 4 treatment after neonatal heart regeneration. J. Clin. Invest. 124,
60. White, I. A., Gordon, J., Balkan, W. & Hare, J. M. myocardial infarction does not reprogram epicardial 1382–1392 (2014).
Sympathetic reinnervation is required for mammalian cells into cardiomyocytes. J. Mol. Cell. Cardiol. 52, This study showed that macrophages are essential
cardiac regeneration. Circ. Res. 117, 990 (2015). 43–47 (2012). for regeneration in the neonatal mouse heart by
61. Mahmoud, A. I. et al. Nerves regulate cardiomyocyte 87. Kikuchi, K. et al. tcf21+ epicardial cells adopt non- modulation of neoangiogenesis.
proliferation and heart regeneration. Dev. Cell 34, myocardial fates during zebrafish heart development 111. Lavine, K. J. et al. Distinct macrophage lineages
387–399 (2015). and regeneration. Development 138, 2895–2902 contribute to disparate patterns of cardiac recovery
62. Regenfus, M. et al. Six-year prognostic value of (2011). and remodeling in the neonatal and adult heart. Proc.
microvascular obstruction after reperfused 88. González-Rosa, J. M., Peralta, M. & Mercader, N. Pan- Natl Acad. Sci. USA 111, 16029–16034 (2014).
ST‑elevation myocardial infarction as assessed by epicardial lineage tracing reveals that epicardium 112. Godwin, J. W. & Brockes, J. P. Regeneration, tissue
contrast-enhanced cardiovascular magnetic derived cells give rise to myofibroblasts and injury and the immune response. J. Anat. 209,
resonance. Am. J. Cardiol. 116, 1022–1027 (2015). perivascular cells during zebrafish heart regeneration. 423–432 (2006).
63. Red-Horse, K., Ueno, H., Weissman, I. L. & Dev. Biol. 370, 173–186 (2012). 113. Rienks, M., Papageorgiou, A.‑P., Frangogiannis, N. G.
Krasnow, M. A. Coronary arteries form by 89. Stevens, S. M., Gise, A.v., VanDusen, N., Zhou, B. & & Heymans, S. Myocardial extracellular matrix. Circ.
developmental reprogramming of venous cells. Nature Pu, W. T. Epicardium is required for cardiac seeding by Res. 114, 872 (2014).
464, 549–553 (2010). yolk sac macrophages, precursors of resident 114. Bonnans, C., Chou, J. & Werb, Z. Remodelling the
This study showed that coronary vessels originate macrophages of the adult heart. Dev. Biol. 413, extracellular matrix in development and disease. Nat.
from the sinus venosus during development. 153–159 (2016). Rev. Mol. Cell Biol. 15, 786–801 (2014).
64. Tian, X. et al. Subepicardial endothelial cells invade 90. Ramjee, V. et al. Epicardial YAP/TAZ orchestrate an 115. Vinarsky, V., Atkinson, D. L., Stevenson, T. J.,
the embryonic ventricle wall to form coronary arteries. immunosuppressive response following myocardial Keating, M. T. & Odelberg, S. J. Normal newt limb
Cell Res. 23, 1075–1090 (2013). infarction. J. Clin. Invest. 127, 899–911 (2017). regeneration requires matrix metalloproteinase
65. Zhang, H. et al. Endocardium minimally contributes to 91. Balmer, G. M. et al. Dynamic haematopoietic cell function. Dev. Biol. 279, 86–98 (2005).
coronary endothelium in the embryonic ventricular contribution to the developing and adult epicardium. 116. Calve, S., Odelberg, S. J. & Simon, H.‑G. A transitional
free walls. Circ. Res. 118, 1880–1893 (2016). Nat. Commun. 5, 4054 (2014). extracellular matrix instructs cell behavior during
66. Masters, M. & Riley, P. R. The epicardium signals the 92. Cao, J. et al. Single epicardial cell transcriptome muscle regeneration. Dev. Biol. 344, 259–271
way towards heart regeneration. Stem Cell Res. 13, sequencing identifies caveolin 1 as an essential factor (2010).
683–692 (2014). in zebrafish heart regeneration. Development 143, 117. Godwin, J. W. & Rosenthal, N. Scar-free wound
67. Risebro, C. A., Vieira, J. M., Klotz, L. & Riley, P. R. 232 (2016). healing and regeneration in amphibians:
Characterisation of the human embryonic and foetal 93. Ruparelia, N. et al. Acute myocardial infarction activates Immunological influences on regenerative success.
epicardium during heart development. Development distinct inflammation and proliferation pathways in Differentiation 87, 66–75 (2014).
142, 3630 (2015). circulating monocytes, prior to recruitment, and identified 118. Hu, N., Yost, H. J. & Clark, E. B. Cardiac morphology
68. Katz, T. C. et al. Distinct compartments of the through conserved transcriptional responses in mice and and blood pressure in the adult zebrafish. Anat. Rec.
proepicardial organ give rise to coronary vascular humans. Eur. Heart J. 36, 1923–1934 (2015). 264, 1–12 (2001).
endothelial cells. Dev. Cell 22, 639–650 (2012). 94. Frangogiannis, N. G. Regulation of the inflammatory 119. Yahalom-Ronen, Y., Rajchman, D., Sarig, R., Geiger, B.
69. Tian, X., Pu, W. T. & Zhou, B. Cellular origin and response in cardiac repair. Circ. Res. 110, 159–173 & Tzahor, E. Reduced matrix rigidity promotes
developmental program of coronary angiogenesis. (2012). neonatal cardiomyocyte dedifferentiation,
Circ. Res. 116, 515–530 (2015). 95. Nahrendorf, M. et al. The healing myocardium proliferation and clonal expansion. eLife 4, e07455
70. von Gise, A. et al. WT1 regulates epicardial epithelial sequentially mobilizes two monocyte subsets with (2015).
to mesenchymal transition through β‑catenin and divergent and complementary functions. J. Exp. Med. 120. Canseco, D. C. et al. Human ventricular unloading
retinoic acid signaling pathways. Dev. Biol. 356, 204, 3037–3047 (2007). induces cardiomyocyte proliferation. J. Am. Coll.
421–431 (2011). 96. Nahrendorf, M. & Swirski, F. K. Abandoning M1/M2 Cardiol. 65, 892–900 (2015).
71. Kwee, L. et al. Defective development of the for a network model of macrophage function. Circ. 121. Chen, W. C. W. et al. Decellularized zebrafish cardiac
embryonic and extraembryonic circulatory systems in Res. 119, 414–417 (2016). extracellular matrix induces mammalian heart
vascular cell adhesion molecule (VCAM‑1) deficient 97. Shiraishi, M. et al. Alternatively activated regeneration. Sci. Adv. 2, e1600844 (2016).
mice. Development 121, 489–503 (1995). macrophages determine repair of the infarcted adult 122. Mercer, S. E., Odelberg, S. J. & Simon, H.‑G. A
72. Huang, G. N. et al. C/EBP transcription factors murine heart. J. Clin. Invest. 126, 2151–2166 dynamic spatiotemporal extracellular matrix
mediate epicardial activation during heart (2016). facilitates epicardial-mediated vertebrate heart
development and injury. Science 338, 1599 (2012). 98. Zouggari, Y. et al. B lymphocytes trigger monocyte regeneration. Dev. Biol. 382, 457–469 (2013).
73. Lepilina, A. et al. A dynamic epicardial injury response mobilization and impair heart function after acute 123. Wang, J., Karra, R., Dickson, A. L. & Poss, K. D.
supports progenitor cell activity during zebrafish heart myocardial infarction. Nat. Med. 19, 1273–1280 Fibronectin is deposited by injury-activated epicardial
regeneration. Cell 127, 607–619 (2006). (2013). cells and is necessary for zebrafish heart regeneration.
74. Wang, J., Cao, J., Dickson, A. L. & Poss, K. D. 99. Weirather, J. et al. Foxp3+ CD4+ T cells improve Dev. Biol. 382, 427–435 (2013).
Epicardial regeneration is guided by cardiac outflow healing after myocardial infarction by modulating 124. Shimazaki, M. et al. Periostin is essential for cardiac
tract and Hedgehog signalling. Nature 522, 226–230 monocyte/macrophage differentiation. Circ. Res. 115, healingafter acute myocardial infarction. J. Exp. Med.
(2015). 55–67 (2014). 205, 295 (2008).
NATURE REVIEWS | DRUG DISCOVERY ADVANCE ONLINE PUBLICATION | 17
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
125. Kuhn, B. et al. Periostin induces proliferation of 150. Jopling, C., Boue, S. & Belmonte, J. C. I. 176. Ruparelia, N., Chai, J. T., Fisher, E. A. &
differentiated cardiomyocytes and promotes cardiac Dedifferentiation, transdifferentiation and Choudhury, R. P. Inflammatory processes in
repair. Nat. Med. 13, 962–969 (2007). reprogramming: three routes to regeneration. cardiovascular disease: a route to targeted therapies.
126. Ladage, D. et al. Stimulating myocardial regeneration Nat. Rev. Mol. Cell Biol. 12, 79–89 (2011). Nat. Rev. Cardiol. 14, 133–144 (2016).
with periostin peptide in large mammals improves 151. Thorel, F. et al. Conversion of adult pancreatic α-cells 177. Majmudar, M. D. et al. Monocyte-directed RNAi
function post-myocardial infarction but increases to β-cells after extreme beta-cell loss. Nature 464, targeting CCR2 improves infarct healing in
myocardial fibrosis. PLoS ONE 8, e59656 (2013). 1149–1154 (2010). atherosclerosis-prone mice. Circulation 127, 2038
127. Missinato, M. A., Tobita, K., Romano, N., Caroll, J. A. 152. Zhang, R. et al. In vivo cardiac reprogramming (2013).
& Tsang, M. Extracellular component hyaluronic acid contributes to zebrafish heart regeneration. Nature 178. ISRCTN registry. Macrophages therapy for liver
and its receptor Hmmr are required for epicardial 498, 497–501 (2013). cirrhosis. BioMed Central, http://www.isrctn.com/
EMT during heart regeneration. Cardiovasc. Res. 107, 153. Yanger, K. et al. Robust cellular reprogramming occurs ISRCTN10368050 (2016).
487–498 (2015). spontaneously during liver regeneration. Genes Dev. 179. Gourdie, R. G., Dimmeler, S. & Kohl, P. Novel
128. Hastings, C. L. et al. Drug and cell delivery for cardiac 27, 719–724 (2013). therapeutic strategies targeting fibroblasts and
regeneration. Adv. Drug Deliv. Rev. 84, 85–106 154. Chong, J. J. H. et al. Human embryonic-stem-cell- fibrosis in heart disease. Nat. Rev. Drug Discov. 15,
(2015). derived cardiomyocytes regenerate non-human 620–638 (2016).
129. Bely, A. E. & Nyberg, K. G. Evolution of animal primate hearts. Nature 510, 273–277 (2014). 180. Talman, V. & Ruskoaho, H. Cardiac fibrosis in
regeneration: re‑emergence of a field. Trends Ecol. This study showed that human ESC‑derived myocardial infarction — from repair and remodeling to
Evol. 25, 161–170 (2010). cardiomyocytes can engraft the macaque heart regeneration. Cell Tissue Res. 365, 563–581 (2016).
130. Goss, R. J. The evolution of regeneration: adaptive or following myocardial infarction. 181. Galindo, C. L. et al. Anti-remodeling and anti-fibrotic
inherent? J. Theor. Biol. 159, 241–260 (1992). 155. Takahashi, K. & Yamanaka, S. Induction of pluripotent effects of the neuregulin‑1β glial growth factor 2 in
131. Furtado, M. B., Nim, H. T., Boyd, S. E. & stem cells from mouse embryonic and adult fibroblast a large animal model of heart failure. J. Am. Heart
Rosenthal, N. A. View from the heart: cardiac cultures by defined factors. Cell 126, 663–676 (2006). Assoc. 3, e000773 (2014).
fibroblasts in development, scarring and regeneration. 156. Shiba, Y. et al. Allogeneic transplantation of iPS cell- 182. Kanemitsu, H. et al. Chymase inhibition prevents
Development 143, 387 (2016). derived cardiomyocytes regenerates primate hearts. cardiac fibrosis and dysfunction after myocardial
132. Kanisicak, O. et al. Genetic lineage tracing defines Nature 538, 388–391 (2016). infarction in rats. Hypertens. Res. 29, 57–64 (2006).
myofibroblast origin and function in the injured heart. 157. Efe, J. A. et al. Conversion of mouse fibroblasts into 183. Hoshino, F. et al. Chymase inhibitor improves survival
Nat. Commun. 7, 12260 (2016). cardiomyocytes using a direct reprogramming in hamsters with myocardial infarction. J. Cardiovasc.
133. Lévesque, M. et al. Transforming growth factor: strategy. Nat. Cell Biol. 13, 215–222 (2011). Pharmacol. 41, S11–S18 (2003).
β signaling is essential for limb regeneration in 158. Ieda, M. et al. Direct reprogramming of fibroblasts 184. Liu, C. et al. Platelet-derived growth factor blockade
axolotls. PLoS ONE 2, e1227 (2007). into functional cardiomyocytes by defined factors. Cell on cardiac remodeling following infarction. Mol. Cell.
134. Satoh, A., Hirata, A. & Makanae, A. Collagen 142, 375–386 (2010). Biochem. 397, 295–304 (2014).
reconstitution is inversely correlated with induction of This study demonstrated that fibroblasts can be 185. Menasche, P. Cardiac cell therapy: lessons from clinical
limb regeneration in ambystoma mexicanum. Zool. directly reprogrammed into cardiomyocytes in vitro trials. J. Mol. Cell. Cardiol. 50, 258–265 (2011).
Sci. 29, 191–197 (2012). by GATA4, MEF2C and TBX5. 186. Behfar, A., Crespo-Diaz, R., Terzic, A. & Gersh, B. J.
135. Anderson, M. A. et al. Astrocyte scar formation aids 159. Srivastava, D. & Yu, P. Recent advances in direct Cell therapy for cardiac repair — lessons from clinical
central nervous system axon regeneration. Nature cardiac reprogramming. Curr. Opin. Genet. Dev. 34, trials. Nat. Rev. Cardiol. 11, 232–246 (2014).
532, 195–200 (2016). 77–81 (2015). 187. Alvarado, A. S. & Tsonis, P. A. Bridging the
136. Bicknell, K. A., Coxon, C. H. & Brooks, G. Forced 160. Song, K. et al. Heart repair by reprogramming non- regeneration gap: genetic insights from diverse animal
expression of the cyclin B1–CDC2 complex induces myocytes with cardiac transcription factors. Nature models. Nat. Rev. Genet. 7, 873–884 (2006).
proliferation in adult rat cardiomyocytes. Biochem. J. 485, 599–604 (2012). 188. Bujak, M. et al. Aging-related defects are associated
382, 411 (2004). 161. Qian, L. et al. In vivo reprogramming of murine with adverse cardiac remodeling in a mouse model of
137. Di Stefano, V., Giacca, M., Capogrossi, M. C., cardiac fibroblasts into induced cardiomyocytes. reperfused myocardial infarction. J. Am. Coll. Cardiol.
Crescenzi, M. & Martelli, F. Knockdown of cyclin- Nature 485, 593–598 (2012). 51, 1384–1392 (2008).
dependent kinase inhibitors induces cardiomyocyte References 160 and 161 are key studies that 189. Choi, W.‑Y. et al. In vivo monitoring of cardiomyocyte
re‑entry in the cell cycle. J. Biol. Chem. 286, demonstrate in vivo reprogramming to form new proliferation to identify chemical modifiers of heart
8644–8654 (2011). cardiomyocytes. regeneration. Development 140, 660 (2013).
138. Chaudhry, H. W. et al. Cyclin A2 mediates 162. Jayawardena, T. M. et al. MicroRNA-mediated in vitro 190. Ruozi, G. et al. AAV-mediated in vivo functional
cardiomyocyte mitosis in the postmitotic myocardium. and in vivo direct reprogramming of cardiac fibroblasts selection of tissue-protective factors against
J. Biol. Chem. 279, 35858–35866 (2004). to cardiomyocytes. Circ. Res. 110, 1465 (2012). ischaemia. Nat. Commun. 6, 7388 (2015).
139. Pasumarthi, K. B. S., Nakajima, H., Nakajima, H. O., 163. Li, Y. et al. Tissue-engineered 3‑dimensional (3D) 191. Plowright, A. T., Engkvist, O., Gill, A., Knerr, L. &
Soonpaa, M. H. & Field, L. J. Targeted expression of microenvironment enhances the direct reprogramming Wang, Q.‑D. Heart regeneration: opportunities and
cyclin D2 results in cardiomyocyte DNA synthesis and of fibroblasts into cardiomyocytes by microRNAs. Sci. challenges for drug discovery with novel chemical and
infarct regression in transgenic mice. Circ. Res. 96, Rep. 6, 38815 (2016). therapeutic methods or agents. Angew. Chem. Int. Ed.
110 (2005). 164. Taimeh, Z., Loughran, J., Birks, E. J. & Bolli, R. 53, 4056–4075 (2014).
140. Ebelt, H. et al. E2F2 expression induces proliferation Vascular endothelial growth factor in heart failure. 192. Willems, E. et al. A chemical biology approach to
of terminally differentiated cardiomyocytes in vivo. Nat. Rev. Cardiol. 10, 519–530 (2013). myocardial regeneration. J. Cardiovasc. Transl Res. 4,
Cardiovasc. Res. 80, 219 (2008). 165. Giacca, M. & Zacchigna, S. VEGF gene therapy: 340–350 (2011).
141. Cheng, Y. Y. et al. Reprogramming-derived gene therapeutic angiogenesis in the clinic and beyond. 193. Campbell, N. G. & Suzuki, K. Cell delivery routes for
cocktail increases cardiomyocyte proliferation for heart Gene Ther. 19, 622–629 (2012). stem cell therapy to the heart: current and future
regeneration. EMBO Mol. Med. 9, 251–264 (2016). 166. Iyer, D. et al. Robust derivation of epicardium and its approaches. J. Cardiovasc. Transl Res. 5, 713–726
142. Engel, F. B., Hsieh, P. C. H., Lee, R. T. & Keating, M. T. differentiated smooth muscle cell progeny from (2012).
FGF1/p38 MAP kinase inhibitor therapy induces human pluripotent stem cells. Development 142, 194. Qian, L. et al. Hemodynamic contribution of stem cell
cardiomyocyte mitosis, reduces scarring, and rescues 1528–1541 (2015). scaffolding in acute injured myocardium. Tissue Eng.
function after myocardial infarction. Proc. Natl Acad. 167. Wei, K. et al. Epicardial FSTL1 reconstitution Part A 18, 1652–1663 (2012).
Sci. USA 103, 15546–15551 (2006). regenerates the adult mammalian heart. Nature 525, 195. Saludas, L., Pascual-Gil, S., Prósper, F., Garbayo, E. &
143. Garbayo, E. et al. Catheter-based intramyocardial 479–485 (2015). Blanco-Prieto, M. Hydrogel based approaches for
injection of FGF1 or NRG1‑loaded MPs improves 168. Zangi, L. et al. Modified mRNA directs the fate of cardiac tissue engineering. Int. J. Pharm. 523,
cardiac function in a preclinical model of ischemia- heart progenitor cells and induces vascular 454–475 (2017).
reperfusion. Sci. Rep. 6, 25932 (2016). regeneration after myocardial infarction. 196. Sarig, R. & Tzahor, E. The cancer paradigms of
144. Zhao, L. et al. Notch signaling regulates cardiomyocyte Nat. Biotechnol. 31, 898–907 (2013). mammalian regeneration: can mammals regenerate
proliferation during zebrafish heart regeneration. Proc. 169. Mandic, L. et al. Molecular imaging of angiogenesis in as amphibians? Carcinogenesis 38, 359–366
Natl Acad. Sci. USA 111, 1403–1408 (2014). cardiac regeneration. Curr. Cardiovasc. Imaging Rep. (2017).
145. Lenihan, D. J. et al. A phase I, single ascending dose 9, 27 (2016). 197. Rosen, M. R., Myerburg, R. J., Francis, D. P.,
study of cimaglermin alfa (neuregulin 1β3) in patients 170. Tian, X. et al. De novo formation of a distinct coronary Cole, G. D. & Marbán, E. Translating stem cell
with systolic dysfunction and heart failure. JACC Basic vascular population in neonatal heart. Science 345, research to cardiac disease therapies: pitfalls and
Transl Sci. 1, 576–586 (2016). 90–94 (2014). prospects for improvement. J. Am. Coll. Cardiol. 64,
146. Eulalio, A. et al. Functional screening identifies mi 171. Miquerol, L. et al. Endothelial plasticity drives arterial 922–937 (2014).
RNAs inducing cardiac regeneration. Nature 492, remodeling within the endocardium after myocardial 198. Hare, J. M. et al. Phase II clinical research design in
376–381 (2012). infarction. Circ. Res. 116, 1765 (2015). cardiology. Circulation 127, 1630 (2013).
This study reports that miRNAs are involved in 172. Norman, S. & Riley, P. R. Anatomy and development 199. Naumova, A. V., Modo, M., Moore, A., Murry, C. E. &
cardiac regeneration and have therapeutic effects of the cardiac lymphatic vasculature: its role in injury Frank, J. A. Clinical imaging in regenerative medicine.
to modulate repair in the mouse heart. and disease. Clin. Anat. 29, 305–315 (2016). Nat. Biotechnol. 32, 804–818 (2014).
147. Tian, Y. et al. A microRNA-hippo pathway that promotes 173. Ishikawa, Y. et al. Lymphangiogenesis in myocardial 200. Perin, E. C. et al. Effect of transendocardial delivery of
cardiomyocyte proliferation and cardiac regeneration in remodelling after infarction. Histopathology 51, autologous bone marrow mononuclear cells on
mice. Sci. Transl Med. 7, 279ra38 (2015). 345–353 (2007). functional capacity, left ventricular function, and
148. Hesse, M. et al. Direct visualization of cell division 174. Klotz, L. et al. Cardiac lymphatics are heterogeneous in perfusion in chronic heart failure: the FOCUS-CCTRN
using high-resolution imaging of M‑phase of the cell origin and respond to injury. Nature 522, 62–67 (2015). trial. JAMA 307, 1717–1726 (2012).
cycle. Nat. Commun. 3, 1076 (2012). 175. Henri, O. et al. Selective stimulation of cardiac 201. Nowbar, A. N. et al. Discrepancies in autologous bone
149. Srivastava, D. & DeWitt, N. In vivo cellular lymphangiogenesis reduces myocardial edema and fibrosis marrow stem cell trials and enhancement of ejection
reprogramming: the next generation. Cell 166, leading to improved cardiac function following myocardial fraction (DAMASCENE): weighted regression and
1386–1396 (2016). infarction. Circulation 133, 1484–1497 (2016). meta-analysis. BMJ 348, g2688 (2014).
18 | ADVANCE ONLINE PUBLICATION www.nature.com/nrd
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
REVIEWS
202. International Society for Stem Cell Research. 220. Menasché, P. et al. The myoblast autologous grafting 232. Gullestad, L. et al. Intravenous immunoglobulin
Guidelines for Stem Cell Science and Clinical in ischemic cardiomyopathy (MAGIC) trial. Circulation does not reduce left ventricular remodeling
Translation (ISSCR, 2016). 117, 1189 (2008). in patients with myocardial dysfunction
203. Caulfield, T., Sipp, D., Murry, C. E., Daley, G. Q. & 221. Bolli, R. et al. Cardiac stem cells in patients with ischaemic during hospitalization after acute myocardial
Kimmelman, J. Confronting stem cell hype. Science cardiomyopathy (SCIPIO): initial results of a randomised infarction. Int. J. Cardiol. 168, 212–218
352, 776 (2016). phase 1 trial. Lancet 378, 1847–1857 (2011). (2013).
204. Swirski, F. K. et al. Identification of splenic reservoir 222. Makkar, R. R. et al. Intracoronary cardiosphere- 233. Najjar, S. S. et al. Intravenous erythropoietin in
monocytes and their deployment to inflammatory derived cells for heart regeneration after myocardial patients with ST‑segment elevation myocardial
sites. Science 325, 612–616 (2009). infarction (CADUCEUS): a prospective, randomised infarction: REVEAL: a randomized controlled trial.
205. Niccoli, G., Burzotta, F., Galiuto, L. & Crea, F. phase 1 trial. Lancet 379, 895–904 (2012). JAMA 305, 1863–1872 (2011).
Myocardial no‑reflow in humans. J. Am. Coll. Cardiol. 223. Sürder, D. et al. Intracoronary injection of bone 234. Abbate, A. et al. Interleukin‑1 blockade with
54, 281–292 (2009). marrow derived mononuclear cells, early or late after anakinra to prevent adverse cardiac remodeling
206. Van Linthout, S., Miteva, K. & Tschope, C. Crosstalk acute myocardial infarction: effects on global left after acute myocardial infarction (Virginia
between fibroblasts and inflammatory cells. ventricular function four months results of the SWISS- Commonwealth University Anakinra Remodeling
Cardiovasc. Res. 102, 258–269 (2014). AMI trial. Circulation 127, 1968–1979 (2013). Trial [VCU-ART] pilot study). Am. J. Cardiol. 105,
207. Pfeffer, M. A. & Braunwald, E. Ventricular remodeling 224. Karantalis, V. et al. Autologous mesenchymal stem 1371–1377.e1 (2010).
after myocardial infarction. Experimental observations cells produce concordant improvements in regional 235. Gao, R. et al. A phase II, randomized, double-blind,
and clinical implications. Circulation 81, 1161 (1990). function, tissue perfusion, and fibrotic burden when multicenter, based on standard therapy, placebo-
208. Sutton, M. G. S. J. & Sharpe, N. Left ventricular administered to patients undergoing coronary artery controlled study of the efficacy and safety of
remodeling after myocardial infarction. Circulation bypass grafting: the prospective randomized study of recombinant human neuregulin‑1 in patients with
101, 2981 (2000). mesenchymal stem cell therapy in patients undergoing chronic heart failure. J. Am. Coll. Cardiol. 55,
209. Packer, M. Pathophysiology of chronic heart failure. cardiac surgery (PROMETHEUS) trial. Circ. Res. 114, 1907–1914 (2010).
Lancet 340, 88–92 (1992). 1302–1310 (2014). 236. Armstrong, P. W. et al. Pexelizumab for acute
210. Lymperopoulos, A., Rengo, G. & Koch, W. J. Adrenergic 225. Menasché, P. et al. Human embryonic stem cell- ST‑elevation myocardial infarction in patients
nervous system in heart failure. Circ. Res. 113, 739 (2013). derived cardiac progenitors for severe heart failure undergoing primary percutaneous coronary
211. Narula, J., Haider, N., Arbustini, E. & treatment: first clinical case report. Eur. Heart J. 36, intervention: a randomized controlled trial. JAMA
Chandrashekhar, Y. Mechanisms of disease: apoptosis 2011–2017 (2015). 297, 43–51 (2007).
in heart failure — seeing hope in death. Nat. Clin. 226. Choudry, F. et al. A randomized double-blind control 237. Hudson, M. P. et al. Effects of selective matrix
Pract. Cardiovasc. Med. 3, 681–688 (2006). study of early intra-coronary autologous bone marrow metalloproteinase inhibitor (PG‑116800) to prevent
212. Packer, M. The neurohormonal hypothesis: a theory to cell infusion in acute myocardial infarction: the ventricular remodeling after myocardial infarction:
explain the mechanism of disease progression in heart REGENERATE-AMI clinical trial. Eur. Heart J. 37, results of the PREMIER (Prevention of Myocardial
failure. J. Am. Coll. Cardiol. 20, 248–254 (1992). 256–263 (2016). Infarction Early Remodeling) trial. J. Am. Coll.
213. Menasché, P. et al. Myoblast transplantation for heart 227. Koudstaal, S. et al. Sustained delivery of insulin-like Cardiol. 48, 15–20 (2006).
failure. Lancet 357, 279–280 (2001). growth factor‑1/hepatocyte growth factor stimulates
214. Strauer, B. E. et al. Repair of infarcted myocardium by endogenous cardiac repair in the chronic infarcted pig Acknowledgements
autologous intracoronary mononuclear bone marrow heart. J. Cardiovasc. Transl Res. 7, 232–241 (2014). T.J.C. is supported by the Wellcome Trust (grant
cell transplantation in humans. Circulation 106, 1913 228. Bagno, L. L. et al. Growth hormone–releasing 106334/Z/14/Z). R.P.C. is supported by the National
(2002). hormone agonists reduce myocardial infarct scar in Institute for Health Research (NIHR) Biomedical Research
215. Perin, E. C. et al. Transendocardial, autologous bone swine with subacute ischemic cardiomyopathy. J. Am. Centre, Oxford and the British Heart Foundation Centre for
marrow cell transplantation for severe, chronic Heart Assoc. 4, e001464 (2015). Research Excellence, Oxford. P.R.R. is supported by the
ischemic heart failure. Circulation 107, 2294 (2003). 229. O’Donoghue, M. L. et al. Effect of losmapimod on British Heart Foundation (grants CH/11/1/28798 and
216. Wollert, K. C. et al. Intracoronary autologous bone- cardiovascular outcomes in patients hospitalized with RG/13/9/303269).
marrow cell transfer after myocardial infarction: the acute myocardial infarction: a randomized clinical trial.
BOOST randomised controlled clinical trial. Lancet JAMA 315, 1591–1599 (2016). Competing interests statement
364, 141–148 (2004). 230. Cerisano, G. et al. Early short-term doxycycline The authors declare competing interests: see Web version for
217. Lunde, K. et al. Intracoronary injection of mononuclear therapy in patients with acute myocardial infarction details.
bone marrow cells in acute myocardial infarction. and left ventricular dysfunction to prevent the
N. Engl. J. Med. 355, 1199–1209 (2006). ominous progression to adverse remodelling: the
218. Schächinger, V. et al. Intracoronary bone marrow– TIPTOP trial. Eur. Heart J. 35, 184–191 (2013). FURTHER INFORMATION
derived progenitor cells in acute myocardial infarction. 231. Abbate, A. et al. Effects of interleukin‑1 blockade with Cell and Gene Therapy Catapult: https://ct.catapult.org.uk/
N. Engl. J. Med. 355, 1210–1221 (2006). anakinra on adverse cardiac remodeling and heart CellCAN: http://www.cellcan.com/en/home.aspx
219. Janssens, S. et al. Autologous bone marrow-derived failure after acute myocardial infarction [from the Centre for Commercialization of Regenerative Medicine:
stem-cell transfer in patients with ST‑segment elevation Virginia Commonwealth University-Anakinra http://ccrm.ca/
myocardial infarction: double-blind, randomised Remodeling Trial (2) (VCU‑ART2) pilot study].
ALL LINKS ARE ACTIVE IN THE ONLINE PDF
controlled trial. Lancet 367, 113–121 (2006). Am. J. Cardiol. 111, 1394–1400 (2013).
NATURE REVIEWS | DRUG DISCOVERY ADVANCE ONLINE PUBLICATION | 19
©
2
0
1
7
M
a
c
m
i
l
l
a
n
P
u
b
l
i
s
h
e
r
s
L
i
m
i
t
e
d
,
p
a
r
t
o
f
S
p
r
i
n
g
e
r
N
a
t
u
r
e
.
A
l
l
r
i
g
h
t
s
r
e
s
e
r
v
e
d
.
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Clinical Pathways Dan Sistem Drgs Casemix SMF Jantung & Kedokteran Vaskular Rsud Kota Cilegon 2018 Unstable Angina Pektoris (ICD 10: ..)Document3 pagesClinical Pathways Dan Sistem Drgs Casemix SMF Jantung & Kedokteran Vaskular Rsud Kota Cilegon 2018 Unstable Angina Pektoris (ICD 10: ..)flying highPas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Recent Advances in Pulmonary HypertensionDocument12 pagesRecent Advances in Pulmonary Hypertensionflying highPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Goland Et Al 2016 Angiogenic Imbalance and Residual Myocardial Injury in Recovered Peripartum Cardiomyopathy PatientsDocument7 pagesGoland Et Al 2016 Angiogenic Imbalance and Residual Myocardial Injury in Recovered Peripartum Cardiomyopathy Patientsflying highPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Incidence of Pulmonary Hypertension in Hyperthyroid PatientsDocument4 pagesIncidence of Pulmonary Hypertension in Hyperthyroid Patientsflying highPas encore d'évaluation
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- 47 PH in Patient With Hyperthyroidism-Dres - Niemeyer EN PDFDocument4 pages47 PH in Patient With Hyperthyroidism-Dres - Niemeyer EN PDFflying highPas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- Stem CellDocument22 pagesStem Cellflying highPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Takahashi2016Document11 pagesTakahashi2016flying highPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Educational Program Cardiovascular Regenerative Medicine School 2018Document3 pagesEducational Program Cardiovascular Regenerative Medicine School 2018flying highPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Hubungan Kelas Nyha Dengan Fraksi Ejeksi Pada Pasien Gagal Jantung Kronik Di Blu/Rsup Prof. Dr. R.D. Kandou ManadoDocument8 pagesHubungan Kelas Nyha Dengan Fraksi Ejeksi Pada Pasien Gagal Jantung Kronik Di Blu/Rsup Prof. Dr. R.D. Kandou Manadoflying highPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- hubungan Kadar Tnf-α Dengan Fraksi Ejeksi Pada Pasien Gagal Jantung Kronik Di Blu - rsup Prof. Dr. r.d. Kandou ManadoDocument6 pageshubungan Kadar Tnf-α Dengan Fraksi Ejeksi Pada Pasien Gagal Jantung Kronik Di Blu - rsup Prof. Dr. r.d. Kandou Manadoflying highPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Mesenchymal Stem Cells in Cardiac Regeneration: A Detailed Progress Report of The Last 6 Years (2010 - 2015)Document25 pagesMesenchymal Stem Cells in Cardiac Regeneration: A Detailed Progress Report of The Last 6 Years (2010 - 2015)flying highPas encore d'évaluation
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Anti-Inflammatory Nanomedicine For Cardiovascular DiseaseDocument13 pagesAnti-Inflammatory Nanomedicine For Cardiovascular Diseaseflying highPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Colloids and Surfaces B: Biointerfaces: Christina Mckee, G. Rasul ChaudhryDocument16 pagesColloids and Surfaces B: Biointerfaces: Christina Mckee, G. Rasul Chaudhryflying highPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Mesenchymal Stem Cell Paracrine Factors in Vascular Repair and RegenerationDocument9 pagesMesenchymal Stem Cell Paracrine Factors in Vascular Repair and Regenerationflying highPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Rupture of Vulnerable Atherosclerotic Plaques: Micrornas Conducting The Orchestra?Document8 pagesRupture of Vulnerable Atherosclerotic Plaques: Micrornas Conducting The Orchestra?flying highPas encore d'évaluation
- s2 2016 354560 BibliographyDocument4 pagess2 2016 354560 Bibliographyflying highPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Cover PageDocument10 pagesCover PageAvijit GhoshPas encore d'évaluation
- BraunDocument69 pagesBraunLouise Alyssa SazonPas encore d'évaluation
- Christine Remembered That Today Is The Birthday of Her BossDocument1 pageChristine Remembered That Today Is The Birthday of Her BossA.Pas encore d'évaluation
- WTSDA2021 TSDBlack Belt ManualDocument160 pagesWTSDA2021 TSDBlack Belt ManualJesus HernandezPas encore d'évaluation
- Discover India, January 2018Document51 pagesDiscover India, January 2018calebfriesenPas encore d'évaluation
- Lay Planning TypesDocument1 pageLay Planning TypesGaurav Shakya100% (1)
- Учебный предметDocument2 pagesУчебный предметorang shabdizPas encore d'évaluation
- Stamp 07 eDocument6 pagesStamp 07 eDumitru TuiPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Statistics For Criminology and Criminal Justice (Jacinta M. Gau)Document559 pagesStatistics For Criminology and Criminal Justice (Jacinta M. Gau)Mark Nelson Pano ParmaPas encore d'évaluation
- Po 4458 240111329Document6 pagesPo 4458 240111329omanu79Pas encore d'évaluation
- Zara Case StudyDocument26 pagesZara Case StudySeminarskiRadovi100% (2)
- A Software Architecture For The Control of Biomaterials MaintenanceDocument4 pagesA Software Architecture For The Control of Biomaterials MaintenanceCristian ȘtefanPas encore d'évaluation
- Alfa Laval Aalborg Os Tci Marine BoilerDocument2 pagesAlfa Laval Aalborg Os Tci Marine Boilera.lobanov2020Pas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Bluesil Ep 150 A3: Insulator Grade Silicone RubberDocument2 pagesBluesil Ep 150 A3: Insulator Grade Silicone RubberNagendra KumarPas encore d'évaluation
- Device InfoDocument3 pagesDevice InfoGrig TeoPas encore d'évaluation
- Federal Public Service CommissionDocument2 pagesFederal Public Service CommissionNasir LatifPas encore d'évaluation
- 32 Forms of God GaneshaDocument16 pages32 Forms of God Ganeshasudhakarpk2011100% (2)
- Lecture Planner - Chemistry - MANZIL For JEE 2024Document1 pageLecture Planner - Chemistry - MANZIL For JEE 2024Rishi NairPas encore d'évaluation
- Manual Daily Calorie Log: MyfitnesspalDocument4 pagesManual Daily Calorie Log: MyfitnesspalAzariah Burnside100% (2)
- UVEX - Helmets & Eyewear 2009Document19 pagesUVEX - Helmets & Eyewear 2009Ivica1977Pas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- MINDSET 1 EXERCISES TEST 1 Pendientes 1º Bach VOCABULARY AND GRAMMARDocument7 pagesMINDSET 1 EXERCISES TEST 1 Pendientes 1º Bach VOCABULARY AND GRAMMARanaPas encore d'évaluation
- South San Francisco Talks Plans For Sports Park ImprovementsDocument32 pagesSouth San Francisco Talks Plans For Sports Park ImprovementsSan Mateo Daily JournalPas encore d'évaluation
- Yazaki BrochureDocument4 pagesYazaki Brochureguzman_10Pas encore d'évaluation
- The Four Types of Gaps and How To Play Them PDFDocument17 pagesThe Four Types of Gaps and How To Play Them PDFshaikiftakar100% (2)
- My LH Cover LetterDocument3 pagesMy LH Cover LetterAkinde FisayoPas encore d'évaluation
- Ashfaque Ahmed-The SAP Materials Management Handbook-Auerbach Publications, CRC Press (2014)Document36 pagesAshfaque Ahmed-The SAP Materials Management Handbook-Auerbach Publications, CRC Press (2014)surajnayak77Pas encore d'évaluation
- Estocell - Data Sheet - 14-07-06Document2 pagesEstocell - Data Sheet - 14-07-06LeoRumalaAgusTatarPas encore d'évaluation
- Compal Confidential: Ziwb2/Ziwb3/Ziwe1 DIS M/B Schematics DocumentDocument56 pagesCompal Confidential: Ziwb2/Ziwb3/Ziwe1 DIS M/B Schematics DocumentSuhpreetPas encore d'évaluation
- Datasheet TBJ SBW13009-KDocument5 pagesDatasheet TBJ SBW13009-KMarquinhosCostaPas encore d'évaluation
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)D'EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Évaluation : 3 sur 5 étoiles3/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedD'EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedÉvaluation : 4.5 sur 5 étoiles4.5/5 (82)