Académique Documents
Professionnel Documents
Culture Documents
NCCN Rectal Cancer Guidelines 2018 Benson 874 901
Transféré par
Nikos PapaioannouCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
NCCN Rectal Cancer Guidelines 2018 Benson 874 901
Transféré par
Nikos PapaioannouDroits d'auteur :
Formats disponibles
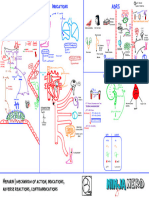
Dual Role of Immune Cells in the Tumor Microenvironment
The balance between anti- and pro-tumor activities shapes the fate of the tumor
Elimination Escape
ILC2 Immature DC
FcR
αβ TCR
IL-2 Mature DC αβ TCR
IL-4
KIR
IL-12 Plasma cell B cell (Be1) ILC1 Naïve CD4+Th1 cell γδ TCR IL-5
SIRPα
IFNγ Vα24 TCR IL-6
γδ Treg cell Bregcell Tregcell Naïve CD4+Th2 cell HLA Class I/peptide
HLA Class I/peptide M2-like TAM
TNF IL-10
HLA Class II/peptide MDSC HVEM
Granzymes IL-13
PD-1
FasL
IL-17
Perforin
M1-like TAM γδ T cell NKT cell NK cell Fas
PD-L1
IL-35
NO
BTLA
CD8+ T cell TRAIL
TGF-β
Tolerogenic DC
ROS
Death receptor CD80/86
VEGF
Glycolipid
M1-like TAM γδ T cell NKT cell NK cell CD8+ T cell
CD80/86 CD28
Amphiregulin
IPP
CD28 CTLA-4
PGE2
TAA NKG2D 02 CD47
Glucose Lactate
NO
MICA/B TRP KYN NKG2A
Antibody
ATP Adenosine
ROS
CD1d CD94
Adenosine
HLA-E/peptide
Lymphatic Vessel
Lymphatic Vessel
Extracellular Matrix
Extracellular Matrix
Fibroblast
Pericyte
Pericyte
Cancer Associated Fibroblast
Blood Vessel
Tumor Cells Blood Vessel
Tumor Cells
Anti-tumor activity Pro-tumor activity
In the early stage of tumor growth, the innate and adaptive immune responses co-operate to identify and eliminate transformed cells. The immune system is alerted of the presence of tumor cells CD4+ Th1 cell Derived from naïve CD4+ T cells upon antigen recognition and IL-12 stimulation, CD4+ Th1 If the tumor is not completely eradicated in the elimination phase, the remaining tumor and immune cells enter a dynamic equilibrium phase in which new tumor variants continue to arise Tregcell Treg cells are a heterogeneous population of immunosuppressive lymphocytes, primarily
cells are defined by the expression of the transcription factor T-bet and production of the defined by expression of FoxP3 and CD25 that play critical roles in maintaining immune
by the presence of danger signals, such as type I interferons, damage-associated molecular patterns and by the expression of stress-induced ligands such as MICA/B and ULBP1 by transformed cells. pro-inflammatory cytokines IL-2, IFNγ and TNF.
and be eliminated. This phase lasts until the tumor develops mutations that allow it to escape immune detection and elimination, eventually resulting in tumor progression (escape phase). homeostasis and self-tolerance.
Inflammatory signals recruit innate immune cells such as macrophages, NK cells, NKT cells and γδ T cells that recognize and kill tumor cells via different mechanisms, including secretion of Changes in tumor cells that result in immune escape include loss of tumor antigen expression, down-regulation of MHC class I molecules, induction of immune cell exhaustion through
At the tumor site, CD4+Th1 cells recruit, retain and activate CTLs, NK cells and macrophages. Treg cell suppressive activity involves secretion of immunosuppressive cytokines (TGF-β,
pro-inflammatory cytokines and cytotoxic molecules, antibody-dependent cell cytotoxicity and phagocytosis and FasL- and TRAIL-induced apoptosis. Dendritic cells loaded with tumor debris persistent activation, expression of ligands for co-inhibitory receptors (PD-L1/PD1, CD80/CTLA-4, HLA-E/NKG2A-CD94, MHC class I/KIR, HVEM/BTLA) and inhibition of phagocytosis through IL-10 and IL-35) and the consumption of IL-2 that is required by effector T cells.
migrate to lymph nodes, where they activate tumor-specific CD4+ Th1 and cytotoxic CD8+ T cells. The activated CD4+ and CD8+ T cells then migrate to the tumor site, where they function Th1 cytokines induce upregulation of MHC molecules on tumor cells leading to enhanced CTL expression of the do not eat me signaling molecule CD47.
recognition and killing. Tumor infiltrating Treg cells express the ectonucleotidases CD39 and CD73 that function in
synergistically to effectively eliminate tumor cells. CD4+ T helper cells, together with their innate counterparts ILC1s, support the activity of cytotoxic cells and macrophages by secreting Th1 tandem to convert ATP into adenosine, a highly immunosuppressive molecule that binds
Tumor cells can also escape immune responses by remodeling the tumor microenvironment. High expression of VEGF-A induces aberrant angiogenesis characterized by disorganized and
effector cytokines such as IFNγ, TNF and IL-12. Tumor-infiltrating B cells also play key roles in tumor elimination. They can present tumor-specific antigens and acquire an effector phenotype to A2aR expressed on effector T cells. Adenosine inhibits the PI3K-AKT pathway and the
leaky blood vessels resulting in hypoxia, whereas high expression of VEGF-C/D promotes lymphangiogenesis that favors tumor progression and dissemination. The tumor also promotes stromal downstream glycolysis, required for effector T-cell function.
(Be1) that is characterized by secretion of Th1 cytokines and cytotoxic molecules. Differentiation of B cells into antibody-secreting plasma cells contributes to antibody-mediated cytotoxicity CD8+ T cell response is stimulated by soluble factors released by CD4+ Th cells, and by dendritic
CD8+ T cell remodeling, primarily through secretion of TGF-β, PDGF-BB and VEGF, that causes transformation of normal fibroblasts into CAFs, detachment of pericytes from blood vessels, alterations of
and phagocytosis of cells expressing specific tumor antigens. cells that present antigenic epitopes from captured tumor-derived peptides on MHC class I
together with co-stimulatory molecules CD80, CD86 and CD40, and secreted IL-12. blood vessel and lymphatic endothelial cells. The abnormal stromal components secrete immunosuppressive molecules such as PGE2, TGF-β and IL-6 that directly inhibit cytotoxic cell activity,
while recruiting and activating immunosuppressive cells, together with chemokines secreted by tumor cells (CCL2, CCL5, CCL22). Infiltrating regulatory cells (Treg, Breg and γδ Treg cells), M2-like γδ Treg cell The tumor microenvironment can polarize γδ T cells toward different immunosuppressive
Tumor elimination is mediated by the release of granules containing perforin and granzymes, phenotypes.
which induce apoptosis of tumor cells. FasL and TRAIL signaling also contribute to tumor TAMs, immature DCs, ILC2s and CD4+ Th2 cells contribute to the switch from a pro-inflammatory Th1 response to an immunosuppressive Th2 response mediated by the secretion of IL-10,
cell death. IL-35, TGF-β, IL-4, IL-5 and IL-13. Vδ1 γδ Treg cells can be recruited by breast cancer cells through secreted IP-10 and are able to
M1-like TAM M1-like TAMs derive from macrophage polarization induced by IFNγ, M-CSF or LPS. NKT cell NKT cells are innate lymphocytes that express a limited repertoire of αβ TCRs which recognize suppress DC maturation and CTL functions.
lipid antigens presented by CD1d on APCs and tumor cells. CD8+ T cells also produce TNF and IFNγ contributing to the generation of a pro-inflammatory,
M1-like TAMs directly promote tumor elimination through secretion of TNF, generation of anti-tumorigenic microenvironment. Tumor cells further inhibit CTLs through metabolic exhaustion. Tumor cells outcompete T cells for oxygen, glucose and amino acids. Expression of IDO, arginase-1, ectonucleotidases CD39 γδ T17 cells represent another group of γδ Treg cells. These cells are induced by IL-6 and TGF-β
high levels of NO and ROS and antibody-dependent cell phagocytosis mediated by FcR. Type I NKT cells (also called iNKT cells) express a semi-invariant TCRα chain (Vα24-Jα18 in and CD73 by tumor cells, Treg cells, MDSCs or immature DCs further contributes to T-cell nutrient deprivation and inhibition by decreasing the levels of tryptophan and increasing the concentration and able to secrete IL-17. In the context of an altered tumor microenvironment, IL-17 can play
human, Vα14-Jα18 TCR in mice), while Type II NKT cells display a more diverse TCR repertoire. an immunosuppressive function by promoting angiogenesis and recruiting MDSCs.
M1-like TAMs upregulate the IRF5 transcription factor that is required for induction of Both types of NKT cells can play a role in tumor immunity. of its immunosuppressive catabolite kynurenine, by limiting the availability of arginine and by hydrolysing ATP into highly immunosuppressive adenosine. Moreover, Treg cells sequester IL-2,
cytokines (IL-12, IL-23 and TNF) involved in eliciting anti-tumor Th1 and Th17 responses. γδ T cells recognize unconventional antigens (phosphoantigens, heat shock proteins) in an required for T-cell survival and function, through high expression of IL-2 receptor alpha-chain (CD25). Understanding the different mechanisms by which tumor cells escape immune surveillance
γδ T cell
Upon recognition of CD1d-expressing tumor cells, NKT cells can directly kill tumor cells through MHC-unrestricted manner and can rapidly induce IFNγ and TNF secretion and target cell lysis.
the secretion of IFNγ, the release of granzymes and perforin and/or through FasL-induced has driven the development of immunotherapy strategies aimed at manipulating T-cell and tumor metabolism, and blocking, for example, inhibitory checkpoints (PD-1 and CTLA-4 axes), CD4+ Th2 cell Derived from naïve CD4+ T cells upon antigen recognition and IL-4 stimulation, Th2 cells
apoptosis. Recognition of the tumor and activation of γδ T cell anti-tumor functions also involve the immunosuppressive modulators TGF-β and IDO, CD47 signaling and CCL2-mediated recruitment of immunosuppressive cells. are defined by the expression of the transcription factor GATA3 and production of the anti-
Mature DC Mature DCs process and present tumor antigens to naïve T cells. binding of NKG2D to the stress ligands MICA/B or ULBP1. inflammatory cytokines IL-4, IL-5 and IL-13.
NKT cells can specifically stimulate DCs through the CD1d-TCR complex and CD40–CD40L
T-cell antigen presentation and activation is mediated by high expression of MHC class interaction which induces DC maturation and IL-12 secretion. γδ T cells can also kill tumor cells through release of granules containing perforin and granzymes, GATA3 suppresses Th1 cells development and ultimately disrupts Th1-mediated anti-tumor
I or II, co-stimulatory molecules CD80 and CD86 and secretion of IL-12. and through antibody-dependent cell cytotoxicity mediated by FcR such as CD16. M2-like TAMs are derived from macrophage polarization primarily induced by IL-4 and IL-13; immune responses.
M2-like TAM Tolerogenic DC Tolerogenic dendritic cells are partially mature DCs that express high levels of MHC class I
tumor-secreted CCL2 plays a key role in M2-like TAM recruitment. and class II, CD80 and CD86 and inhibit T cells through secretion of IL-10 and TGF-β. Th2 cells promote the differentiation and accumulation of immunosuppressive M2-like TAMs
NK cells express cell-surface receptors that deliver either activating or inhibitory signals. M2-like TAMs promote tumor escape by inducing an anti-inflammatory Th2 response Tolerogenic DCs also express high levels of IDO that inhibits CTLs by reducing the availability and MDSCs, leading to T cell suppression and loss of CTL activity.
NK cell
NKG2D activation, for instance, induces cytotoxic lysis of tumor cells upon binding with B cell (Be1) The pro-inflammatory milieu promotes polarization of B cells into effector B cells (Be1) that through secretion of IL-10 and TGF-β. of tryptophan and by increasing the concentration of its immunosuppressive catabolite Th2 cells at tumor sites can facilitate angiogenesis, tumor cell growth and invasion.
MICA/B or ULBP1. produce Th1 cytokines and enhance CTL activity and NK-meditated tumor cell killing. kynurenine.
M2-like TAMs express high levels of arginase-1 and inhibit CTLs by limiting arginine
ILC1s are innate immune cells that are derived from a common lymphoid progenitor NK cells produce cytokines, especially IFNγ and TNF, and release granules containing perforin B cells also promote direct tumor cell killing by secreting granzyme B or by triggering TRAIL availability. Expression of IDO further promotes the activity of immunosuppressive Treg cells.
ILC1 signaling.
and lack a rearranged antigen receptor on the cell surface. and granzymes that eliminate tumor cells. CAF CAFs can derive from normal fibroblasts, endothelial cells, pericytes or tumor cells through
differentiation, transdifferentiation or epithelial-to-mesenchymal transition mediated by TGF-β
Similar to their CD4+ Th cell counterparts, ILC1s produce Th1 cytokines (IFNγ, TNF) that and PDGF-BB.
promote the activity of CTLs, NK cells and macrophages. MDSC Myeloid-derived suppressor cells are immature cells endowed with potent immunosup- Immature DC Immature dendritic cells are unable to properly present antigen to naïve T cells due to low
Plasma cell Differentiation into plasma cells and generation of antibodies against tumor antigens promote pressive activity. expression of MHC class I and class II, CD80 and CD86. CAFs directly inhibit cytotoxic cells through secretion of PGE2 and TGF-β.
tumor elimination through antibody-dependent mechanisms, including cell cytotoxicity and
Chronic inflammation induced by cytokines (IL-4, IL-5, IL-6, IL-10) in the tumor Similar to tolerogenic DCs, immature DCs inhibit CTLs through secretion of IL-10 and TGF-β CAFs promote Th2 polarization through expression of TSLP, and M2-like TAM polarization through
phagocytosis, and complement-mediated lysis of tumor cells.
microenvironment promotes MDSC recruitment and expansion. and high expression of IDO. secretion of IL-6, TGF-β and FGF.
MDSCs express high levels of arginase-1 and IDO which results in high consumption of IL-6 expression is also responsible for the inhibition of dendritic cell maturation and recruitment
arginine and tryptophan, and T-cell inhibition via nutrient deprivation. of immature dendritic cells.
ILC2 ILC2s are considered the innate counterpart of CD4+ Th2 cells.
MDSCs also express high levels of iNOS that synthesizes NO from arginine using an
alternative pathway than the one used by arginase-1. The combination of NO and ROS Upon activation by IL-33, IL-25 and TSLP, ILC2s secrete Th2 cytokines IL-4 and IL-13 that
generates peroxynitrite that nitrosylates and alters the function of the TCR, thus inhibiting contribute to the generation of an immunosuppressive milieu. Pericytes Detachment of pericytes from the tumor vasculature contributes to the formation of disorganized,
T-cell activation. leaky blood vessels that cannot meet the blood supply demand of highly proliferating tumor cells.
ILC2s also promote T-cell inhibition by producing amphiregulin, an EGFR ligand that regulates
Abbreviations: MDSCs recruit immature DCs and inhibit their maturation through secretion of VEGF, IL-6 and maintain Treg cell’s suppressive function.
This results in a hypoxic and acidic tumor microenvironment that attracts immunosuppressive
immune cells and inhibits CTLs.
and IL-10.
A2aR, adenosine receptor A2a; AKT, aka protein kinase B; AMP, adenosine monophosphate; APC, antigen-presenting cell; ATP, adenosine triphosphate; Be1, B cell effector 1; Breg cell, regulatory B cell; BTLA, B and T lymphocyte attenuator; CAF, cancer associated fibroblast; CCL, chemokine (C-C motif) ligand; CD40L, CD40 Pericytes directly inhibit cytotoxic cells through the secretion of PGE2 and TGF-β, and the expression
ligand, CD154; CTL, cytotoxic T lymphocyte; CTLA-4, cytotoxic T-lymphocyte-associated protein 4, CD152; DC, dendritic cell; EGFR, epithelial growth factor receptor; Fas, first apoptosis signal receptor, CD95; FasL, Fas ligand, CD95L; FcR, crystallizable fragment receptor; FGF, fibroblast growth factor; GATA3, GATA Bregcell Tumor infiltrating Breg cells play pivotal roles in the suppression of anti-tumor immunity. of the inhibitory ligand PD-L1.
binding protein 3; γδ Treg cell, gamma delta regulatory T cell; HLA, human leukocyte antigen; HVEM, herpesvirus entry mediator; IDO, indoleamine 2,3-dioxygenase; ILC, innate lymphoid cell; IFNγ, interferon gamma; IL, interleukin; iNOS, inducible nitric oxide synthase; IP-10, IFNγ-inducible protein 10; IPP, Breg cells’ suppressive activity is mostly attributed to the production of the anti-inflammatory Pericytes promote M2-like TAM polarization through secretion of IL-6.
isopentenyl pyrophosphate; IRF5, interferon regulatory factor 5; KIR, killer-cell immunoglobulin-like receptors; KYN, kynurenine; LPS, lipopolysaccharides; M-CSF, macrophage colony-stimulating factor; MDSC, myeloid-derived suppressor cells; MHC, major histocompatibility complex; MICA/B, major histocompatibility cytokine IL-10, TGF-β and IL-35.
complex class I chain-related protein A and B; NK cell, natural killer cell; NKG2A, natural killer group 2 A, CD159a; NKG2D, natural killer group 2 D, CD314; NKT cell, natural killer T cell; NO, nitric oxide; 02, oxygen; PD-1, programmed cell death protein 1, CD279; PD-L1, programmed death-ligand 1, CD274; PDGF-BB, The inhibitory effects of IL-10 producing Bregs include dampening of CTL activity and blocking
platelet-derived growth factor isoform BB; PI3K, phosphatidylinositide 3-kinase; PGE2 prostaglandin E2; ROS, reactive oxygen species; SIRPα, signal regulator protein alpha; TAA, tumor-associated antigen; TAM, tumor-associated macrophage; T-Bet, T-cell-specific T-box transcription factor; TCR, T-cell receptor; IFNγ and IL-17 production by Th1 and Th17 cells, respectively. They can also impair Th17 cell
TGF-β, transforming growth factor beta; Th cell, T helper cell; TNF, tumor necrosis factor; TRAIL, tumor necrosis factor-related apoptosis inducing ligand; Treg cell, regulatory T cell; TRP, tryptophan; TSLP, thymic stromal lymphopoietin; ULBP1, UL16-binding protein 1; VEGF, vascular endothelial growth factor differentiation and induce the conversion of T cells into Tregs.
Class 1 Laser Product.
For Research Use Only. Not for use in diagnostic or therapeutic procedures.
23-20563-00
BD Life Sciences, San Jose, CA, 95131, USA | Visit bdbiosciences.com
© 2018 BD. All rights reserved. Unless otherwise noted, BD, the BD Logo, and all other trademarks are property of Becton, Dickinson and Company.
Vous aimerez peut-être aussi
- Cellular Communication POGILDocument5 pagesCellular Communication POGILJiwon Shin60% (5)
- Essay On Long-Term PotentiationDocument8 pagesEssay On Long-Term PotentiationJayPas encore d'évaluation
- POGIL KeyDocument2 pagesPOGIL KeyfiuePas encore d'évaluation
- Schematic - BMW M50 ProDocument1 pageSchematic - BMW M50 ProEstang Da ViePas encore d'évaluation
- Gigabyte Ga-H110m-H-Ddr3-1.0 (PDF Boardview)Document2 pagesGigabyte Ga-H110m-H-Ddr3-1.0 (PDF Boardview)RicardoPas encore d'évaluation
- Chemokine ReceptorDocument1 pageChemokine ReceptorSPas encore d'évaluation
- OSLD With Time GradingDocument1 pageOSLD With Time GradingDarshit VyasPas encore d'évaluation
- ETAP Direct2D PrintingDocument1 pageETAP Direct2D PrintingDarshit VyasPas encore d'évaluation
- Ga H61M DS2V R2.1Document1 pageGa H61M DS2V R2.1sỹ QuốcPas encore d'évaluation
- Plano PydDocument1 pagePlano PydJohann Nuñez VasquezPas encore d'évaluation
- Cardiovascular Pharmacology) 03 Heparin - KeyDocument1 pageCardiovascular Pharmacology) 03 Heparin - Keyhasanatiya41Pas encore d'évaluation
- Ga H61M DS2V R2.0Document2 pagesGa H61M DS2V R2.0sỹ QuốcPas encore d'évaluation
- Beko bkl19 LWDocument2 pagesBeko bkl19 LWcioargaPas encore d'évaluation
- Placa Mae LGA1151 v2Document2 pagesPlaca Mae LGA1151 v2paranozjpcPas encore d'évaluation
- CU1 LU1 VGA: Cec8 Cec4 Cec9 Cec7 Cec5 Cec2 Cec3Document1 pageCU1 LU1 VGA: Cec8 Cec4 Cec9 Cec7 Cec5 Cec2 Cec3謝紳泳Pas encore d'évaluation
- 03-120000-4800000522-Amt-Sec-Drg-100012 - Control Room ArrangementDocument1 page03-120000-4800000522-Amt-Sec-Drg-100012 - Control Room ArrangementRiazuddinPas encore d'évaluation
- DM - DQ1 DB - DQ1 DA - DQ1: Daq2 Daq5Document2 pagesDM - DQ1 DB - DQ1 DA - DQ1: Daq2 Daq5Huỳnh Văn ĐôngPas encore d'évaluation
- GA B75M-D3V-Rev.1.1 ăÎÍDocument1 pageGA B75M-D3V-Rev.1.1 ăÎÍsỹ QuốcPas encore d'évaluation
- Cec6 Cec9 Cec2 Cec1: Daec2 Daec3 Daec4Document2 pagesCec6 Cec9 Cec2 Cec1: Daec2 Daec3 Daec4rick martinsPas encore d'évaluation
- WWW - Vinafix.vn: Usb - RcaDocument1 pageWWW - Vinafix.vn: Usb - RcaNam NhiPas encore d'évaluation
- Gigabyte Ga-B85m-D3v Rev 1.11 (PDF Boardview)Document1 pageGigabyte Ga-B85m-D3v Rev 1.11 (PDF Boardview)Carlos GomesPas encore d'évaluation
- Level 3 Repair: 8-1. Block DiagramDocument79 pagesLevel 3 Repair: 8-1. Block DiagramAli UnlockPas encore d'évaluation
- Bitmaps H110M-DS2-DDR3-1.0Document2 pagesBitmaps H110M-DS2-DDR3-1.0Rin 193Pas encore d'évaluation
- P4 SLD 2019 PLIRE - Recover-ModelDocument1 pageP4 SLD 2019 PLIRE - Recover-ModelMd Shamim RezaPas encore d'évaluation
- Detail Buttress (4X) Section 4 - 4 Detail Buttress (4X) Section 5 - 5Document1 pageDetail Buttress (4X) Section 4 - 4 Detail Buttress (4X) Section 5 - 5joselito navarroPas encore d'évaluation
- Afs Gigabyte Ga-H110m-S2h-Ddr3-1.0 (PDF Boardview)Document2 pagesAfs Gigabyte Ga-H110m-S2h-Ddr3-1.0 (PDF Boardview)Евгений КуценкоPas encore d'évaluation
- Eurocontrol Erc04h 27012022Document1 pageEurocontrol Erc04h 27012022AlexPas encore d'évaluation
- Plano 2 Parte 2 - 3 de 4Document1 pagePlano 2 Parte 2 - 3 de 4pelaoonePas encore d'évaluation
- Kimball Et Al 2018, Figure 9Document1 pageKimball Et Al 2018, Figure 9Abby KimballPas encore d'évaluation
- Gigabyte GA-H61M-S1 r3.0 BoardviewDocument2 pagesGigabyte GA-H61M-S1 r3.0 Boardviewsỹ QuốcPas encore d'évaluation
- Gigabyte GA-H61M-S1 r3.0 BoardviewDocument2 pagesGigabyte GA-H61M-S1 r3.0 BoardviewANH TUANPas encore d'évaluation
- Gigabyte GA-H61M-S1 r3.0 BoardviewDocument2 pagesGigabyte GA-H61M-S1 r3.0 Boardviewsỹ QuốcPas encore d'évaluation
- H61M-S1 Rev.3.0 BVDocument2 pagesH61M-S1 Rev.3.0 BVĐức Hòa Điện Thoại - Máy TínhPas encore d'évaluation
- GA-H61M-S1 Rev.3.0Document2 pagesGA-H61M-S1 Rev.3.0Đức Hòa Điện Thoại - Máy TínhPas encore d'évaluation
- GA-H61M-S1 Rev.3.0Document2 pagesGA-H61M-S1 Rev.3.0Đức Hòa Điện Thoại - Máy TínhPas encore d'évaluation
- Electrical Schematic DiagramDocument1 pageElectrical Schematic DiagramMary CindyPas encore d'évaluation
- A320 Family Maintenance Concept2019Document1 pageA320 Family Maintenance Concept2019br213Pas encore d'évaluation
- Showing Part Plan at Showing Part Plan at Foundation Level Deck Level (For Prop. Rob)Document1 pageShowing Part Plan at Showing Part Plan at Foundation Level Deck Level (For Prop. Rob)PratikPas encore d'évaluation
- GLJ30-ELET-BM-SD-100 To 103-GLJ30-ELET-GF-SD-101Document1 pageGLJ30-ELET-BM-SD-100 To 103-GLJ30-ELET-GF-SD-101Omer SharifPas encore d'évaluation
- Cell Biology) 9. DNA Transcription - KeyDocument1 pageCell Biology) 9. DNA Transcription - Keysaranya sankarPas encore d'évaluation
- 17pw15 SemaDocument10 pages17pw15 Semabehzat gülerPas encore d'évaluation
- Etaa Tps Schematic v1Document1 pageEtaa Tps Schematic v1Spwebconnect Website developerPas encore d'évaluation
- Offerx313640x1 O HDocument2 pagesOfferx313640x1 O HArnaldo EspejoPas encore d'évaluation
- COPIER (B264/B265) Point To Point Diagram: Bicu PCB 1Document14 pagesCOPIER (B264/B265) Point To Point Diagram: Bicu PCB 1josdavisPas encore d'évaluation
- B737NG-v1 3Document1 pageB737NG-v1 3Akshay KharatPas encore d'évaluation
- Shell Asgard 1f Security LayoutDocument1 pageShell Asgard 1f Security Layoutbharathayyappa1806Pas encore d'évaluation
- Estructuras-Losa AligeradaDocument1 pageEstructuras-Losa Aligeradahector vera dueñasPas encore d'évaluation
- Darlington: Silicon PNP Epitaxial Planar TransistorDocument1 pageDarlington: Silicon PNP Epitaxial Planar Transistorroberto carlos martinez narvaezPas encore d'évaluation
- DA - DQ1 DB - DQ1 DM - DQ1: Daq5 Daq2Document2 pagesDA - DQ1 DB - DQ1 DM - DQ1: Daq5 Daq2Huỳnh Văn ĐôngPas encore d'évaluation
- UENR63330001-so Do DDocument2 pagesUENR63330001-so Do DGiangDoPas encore d'évaluation
- B737 800 DigitalDocument1 pageB737 800 DigitalmohammedredhadjoudiPas encore d'évaluation
- Gigabyte Ga-H110m-S2v-Ddr3 Rev. 1.0 1.01 (PDF Boardview)Document3 pagesGigabyte Ga-H110m-S2v-Ddr3 Rev. 1.0 1.01 (PDF Boardview)juan luis san miguelPas encore d'évaluation
- H61M DS2 Rev.4.0 BitmapDocument2 pagesH61M DS2 Rev.4.0 BitmapHoàng Quốc Trung100% (2)
- Parish Council Districts MapDocument1 pageParish Council Districts MapClaire TaylorPas encore d'évaluation
- C32with EMCP3Document4 pagesC32with EMCP3أبو أنس المسلمPas encore d'évaluation
- Crest Audio PFA600Document9 pagesCrest Audio PFA600rzvPas encore d'évaluation
- Pfa600 Schematic Set1Document9 pagesPfa600 Schematic Set1Николай ИвановPas encore d'évaluation
- Long Line ExercisesDocument3 pagesLong Line ExercisesWetse menPas encore d'évaluation
- Delta+DPS-205CP TIVIDocument3 pagesDelta+DPS-205CP TIVINgoc Tuy NguyenPas encore d'évaluation
- Instant Assessments for Data Tracking, Grade 4: MathD'EverandInstant Assessments for Data Tracking, Grade 4: MathÉvaluation : 5 sur 5 étoiles5/5 (2)
- Instant Assessments for Data Tracking, Grade 2: MathD'EverandInstant Assessments for Data Tracking, Grade 2: MathPas encore d'évaluation
- Instant Assessments for Data Tracking, Grade 1: Language ArtsD'EverandInstant Assessments for Data Tracking, Grade 1: Language ArtsPas encore d'évaluation
- Gina Brown Pent MonDocument69 pagesGina Brown Pent MonNikos PapaioannouPas encore d'évaluation
- BloodCoagulFibrinol2011 01Document7 pagesBloodCoagulFibrinol2011 01Nikos PapaioannouPas encore d'évaluation
- Duration of Adjuvant Oxaliplatin-Based Therapy For Stage III Colon Cancer - The ASCO PostDocument1 pageDuration of Adjuvant Oxaliplatin-Based Therapy For Stage III Colon Cancer - The ASCO PostNikos PapaioannouPas encore d'évaluation
- Colostrum and CancerDocument8 pagesColostrum and CancerNikos PapaioannouPas encore d'évaluation
- Doctors Hail World First As Woman's Advanced Breast Cancer Is Eradicated - Science - The GuardianDocument1 pageDoctors Hail World First As Woman's Advanced Breast Cancer Is Eradicated - Science - The GuardianNikos PapaioannouPas encore d'évaluation
- NCCN Rectal Cancer Guidelines-2018-Benson-874-901 PDFDocument28 pagesNCCN Rectal Cancer Guidelines-2018-Benson-874-901 PDFNikos PapaioannouPas encore d'évaluation
- Renal Failure - The FactsDocument282 pagesRenal Failure - The FactsJosé RamírezPas encore d'évaluation
- ΛΟΙΜΩΔΗΣ ΔΙΑΡΡΟΙΑDocument62 pagesΛΟΙΜΩΔΗΣ ΔΙΑΡΡΟΙΑNikos PapaioannouPas encore d'évaluation
- IB Chemistry - How To Write A Lab Report: GeneralDocument3 pagesIB Chemistry - How To Write A Lab Report: GeneralNikos PapaioannouPas encore d'évaluation
- Cell SignalingDocument87 pagesCell SignalingZaw Linn PhyoPas encore d'évaluation
- Chemistry of Signals and ReceptorsDocument13 pagesChemistry of Signals and Receptorsour lecturePas encore d'évaluation
- RECEPTORS Sexl MorigglDocument45 pagesRECEPTORS Sexl Morigglabhishek talokarPas encore d'évaluation
- Articulo de CancerDocument13 pagesArticulo de Cancer11249421Pas encore d'évaluation
- Lec - Chemical MessengersDocument5 pagesLec - Chemical MessengersSim QuiambaoPas encore d'évaluation
- NST110, Toxicology Department of Nutritional Sciences and Toxicology University of California, BerkeleyDocument29 pagesNST110, Toxicology Department of Nutritional Sciences and Toxicology University of California, BerkeleyAitheng LumPas encore d'évaluation
- Review FisiologíaDocument112 pagesReview FisiologíaDiego Bustamante HeinsohnPas encore d'évaluation
- 4.2 Mechanism of Action of Hormones-40Document39 pages4.2 Mechanism of Action of Hormones-40Namomsa W.Pas encore d'évaluation
- Endocrine Physiology: Felix E. Grissom, Ph.D. 2219 Adams Building Howard University Tel. (202) 806-4512Document30 pagesEndocrine Physiology: Felix E. Grissom, Ph.D. 2219 Adams Building Howard University Tel. (202) 806-4512Inis LeahyPas encore d'évaluation
- Apoptosis UsmleDocument2 pagesApoptosis Usmlelovelyc95100% (1)
- Cell SignallingDocument14 pagesCell SignallingWei JernPas encore d'évaluation
- Receptors: Types Structure FunctionsDocument44 pagesReceptors: Types Structure Functionsmaham1085Pas encore d'évaluation
- SS PChEMBL or PIC50 Prediction Based On QSAR Machine LearningDocument3 pagesSS PChEMBL or PIC50 Prediction Based On QSAR Machine LearningDiar RickiPas encore d'évaluation
- Role Histamine Mast Cell in AllergyDocument9 pagesRole Histamine Mast Cell in Allergycnh labPas encore d'évaluation
- Pharmacology Quizlet: Chapter 1 Intro To PharmacologyDocument18 pagesPharmacology Quizlet: Chapter 1 Intro To PharmacologyJerome ValerianoPas encore d'évaluation
- Cell Signalling Pathways: SynopsisDocument138 pagesCell Signalling Pathways: SynopsismariaPas encore d'évaluation
- Calcium Signalling in Cancer-Sh ErbetDocument382 pagesCalcium Signalling in Cancer-Sh ErbetGreen ViktorPas encore d'évaluation
- Exercise 15 Signal TransductionDocument4 pagesExercise 15 Signal TransductionTrina Rose AutidaPas encore d'évaluation
- Theories of Drug Receptor Interactions: by Lee Eun JinDocument42 pagesTheories of Drug Receptor Interactions: by Lee Eun Jinsky.bluePas encore d'évaluation
- Structure Activity Relationships of Phenylalkylamines As Agonist Ligands For 5 HT2ADocument11 pagesStructure Activity Relationships of Phenylalkylamines As Agonist Ligands For 5 HT2ALUCAS OYANEDERPas encore d'évaluation
- Cell Signaling PathwaysDocument18 pagesCell Signaling PathwaysJean Marcel Sousa LiraPas encore d'évaluation
- 2nd PPT Growth Factors and ReceptorsDocument31 pages2nd PPT Growth Factors and ReceptorsIndranil BanerjeePas encore d'évaluation
- Evolution of Cell SignalingDocument3 pagesEvolution of Cell SignalingkatakanPas encore d'évaluation
- Tumor Angiogenesis: Causes, Consequences, Challenges and OpportunitiesDocument26 pagesTumor Angiogenesis: Causes, Consequences, Challenges and OpportunitiesStella NoviaPas encore d'évaluation
- Signaling Pathways of EndocDocument1 pageSignaling Pathways of Endocashleighlong2014Pas encore d'évaluation
- In Ammation and Tumor Progression: Signaling Pathways and Targeted InterventionDocument46 pagesIn Ammation and Tumor Progression: Signaling Pathways and Targeted Interventionenkiyna archPas encore d'évaluation
- 001192187GS01Document33 pages001192187GS01radhoinezerellyPas encore d'évaluation