Académique Documents
Professionnel Documents
Culture Documents
Nursing Assessment Form For LTC - revidedEE
Transféré par
Krystel WilkinsTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Nursing Assessment Form For LTC - revidedEE
Transféré par
Krystel WilkinsDroits d'auteur :
Formats disponibles
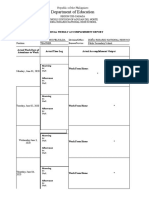
NEW YORK UNIVERSITY COLLEGE OF NURSING
NURSING ASSESSMENT FROM – For Adult-Elder I Clinical (LTC/Nursing Home)
STUDENT’S NAME: ___________________________ CLINICAL UNIT: ____________________________
DATE OF PATIENT CARE ______________________ CLINICAL INSTRUCTOR _____________________
I. DEMOGRAPHIC DATA:
Patient Initials: _______ Age: _____ Gender: ______ Date of Admission __________ Advance Directives ______________
HISTORY OF PRESENT ILLNESS:
Reason for admission to the LTC facility - (“what brought you to the Nursing Home?” – must include “What happened, where,
when, how long prior to admission)
DIAGNOSIS: –
ALLERGY: – DESCRIBE REACTION(S): ________________________
I. PAST MEDICAL/ PSYCHIATRIC HISTORY (Include date condition was diagnosed, if known):
II. PAST SURGICAL HISTORY (include dates of surgery, if known):
III: PSYCHOSOCIAL HISTORY:
Spiritual/ Cultural Assessment: Religion_______________ Cultural/Ethnic background ____________ Marital status________
Smoking – yes cigarettes/day ____ no
Influenza Vaccination – yes Date: _______ no Pneumovax – yes Date_________ no Reason _____________
Discharge Planning:
Support Systems: _________________________________________________________________________________________
Living arrangements_______________________ Caregiver______________ Referral Needs___________________________
Medication Compliance Issues (literacy/language barrier etc.): _____________________________________________________
LTC/Nursing Home Page 1
IV. VITAL SIGNS and PAIN ASSESSMENT
BP ________ Apical Heart Rate (rhythm) ______________ Radial (rate/rhythm) _____________ Resp. Rate and Pattern __________
Temperature ________ Pulse Oximetry _______ Height __________ Weight ___________ BMI____________
Time Location of Pain Scale Interventions Scale Comments
(Pre) (Post)
V. PHYSICAL ASSESSMENT / SYSTEMS REVIEW
1. Neurological System:
Subjective Data: __________________________________________________________
[ ] Alert [ ] Confused [ ] Lethargic [ ] Restless [ ] Aphasic Orientation [ ] Time [ ] Place [ ] Person
Other neurological findings: _____________________________________________________________________________
2. Neuromuscular System:
Subjective Data___________________________________________________________
[ ] Intact motor & sensory function [ ] Weakness – [ ] right, [ ] left [ ] Paralysis – [ ] right, [ ] left
Gait: [ ] steady [ ] Unsteady Use of Assistive device: [ ] Cane [ ] Walker [ ] Wheelchair
Other neuromuscular findings___________________________________________________________________________
3. Cardiovascular:
Subjective Data: ______________________________________________________________________
[ ] Chest Pain (describe) _________________________________________________________ [ ] Palpitations
Peripheral Pulses Dorsalis Pedis [ ] Present [ ] Weak [ ] Absent Posterior Tibialis [ ] Present [ ] Weak [ ] Absent
Other cardiovascular findings: ___________________________________________________________________________
4. Respiratory:
Subjective Data: ______________________________________________________________________
RR _________ Pattern: [ ] Regular [ ] Irregular Use of accessory muscles [ ]
Breath sounds [ ] Clear, bilateral [ ] Abnormal/ Presence of adventitious sounds [ ]
LTC/Nursing Home Page 2
[ ] O2 therapy _____________[ ] Cough productive yes [ ]describe ____________ no [ ]
Other: _____________________________________________________________________________
5. Gastrointestinal:
Subjective Data: _____________________________________________________________________
Abdomen: [ ] Soft [ ] Firm [ ] Distended [ ] Tenderness [ ] Bowel sounds: [ ] Present [ ] Diminished [ ] Absent
[ ] Nausea [ ] Vomiting [ ] Anorexia [ ] NGT/OGT/PEG feeding formula/rate ___________________________________
Residuals (color/Amount) ___________________________
[ ] Last BM (Date) __________ [ ] Constipation [ ] Diarrhea # times________ Type of Stool ________ Onset________
[ ] Ostomy (specify ________________________ Dental/Oral Health (describe) ___________________________________
Other GI findings: ______________________________________________________________________________________
6. Genitourinary:
Subjective Data: ________________________________________________________________________________________
Urine Color_________ Character_____________ [ ] Voiding [ ] Foley catheter – date inserted ____________________
[ ] Incontinence [ ] Dysuria Other GU findings: ____________________________________________________________
7. Integumentary:
Subjective Data: ________________________________________________________________________________________
Skin quality: Temperature [ ] cool, [ ] warm [ ] Dry [ ] Moist [ ] Ecchymosis [ ] Hematoma [ ] Petechiae
[ ] Edema (indicate location) _______________________________________ [ ] Rash [ ] Scar _________
[ ] Pressure ulcer site____________________________________________________________________________________
Braden Scale Score ________ [ ] Operative wound (describe) ___________________________________________________
Other Integumentary findings_______________________________________________________________________________
VI- List of Medications the resident is taking each day.
VII - LIST THREE (POTENTIAL AND ACTUAL) PATIENT CARE NEEDS/CONCERNS:
1.
2.
3.
LTC/Nursing Home Page 3
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5782)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (587)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (72)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (119)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Mapeh 6 - 1st Periodical TestDocument4 pagesMapeh 6 - 1st Periodical TestMAY ANN GRACE SAMPUTONPas encore d'évaluation
- Raita Puro 2016Document16 pagesRaita Puro 2016Enamul Hoque TauheedPas encore d'évaluation
- 2gi19cv418 Pratik-PatilDocument1 page2gi19cv418 Pratik-PatilDIVYA MAHALSEKAR-2GI18CV026Pas encore d'évaluation
- Psy219 Intro to Research Methods SyllabusDocument4 pagesPsy219 Intro to Research Methods SyllabusNick WeberPas encore d'évaluation
- ConnectorsDocument2 pagesConnectorsAlejandra BejaranoPas encore d'évaluation
- Permanent Present Tense The Unforgettable Life of The Amnesic Patient, H. M. by Suzanne CorkinDocument401 pagesPermanent Present Tense The Unforgettable Life of The Amnesic Patient, H. M. by Suzanne CorkinIngrid DíazPas encore d'évaluation
- Iwar and Idlar - DRNHSDocument10 pagesIwar and Idlar - DRNHSWilliam FelisildaPas encore d'évaluation
- Unit Test 7ADocument2 pagesUnit Test 7ACamilaPas encore d'évaluation
- Makalah Modul 1Document49 pagesMakalah Modul 1gadisestiPas encore d'évaluation
- Reading Comprehension Worksheet Have Got and Has GotDocument2 pagesReading Comprehension Worksheet Have Got and Has GotAnalía M Figueredo Vogel88% (17)
- Philos Intro PageDocument3 pagesPhilos Intro PageRed StohlPas encore d'évaluation
- RAHUDocument3 pagesRAHUmrinalini kotaPas encore d'évaluation
- Acceptance of The ChallengeDocument1 pageAcceptance of The Challengejennifer gonzalesPas encore d'évaluation
- Positives and Negatives of Virtue EthicsDocument1 pagePositives and Negatives of Virtue EthicsVarun Smile SPas encore d'évaluation
- OPT B2 Unit Test 9 StandardDocument7 pagesOPT B2 Unit Test 9 Standards.belka100% (1)
- Assignment of Material DevelopmentDocument18 pagesAssignment of Material DevelopmentEnglicanRoxiiRockxPas encore d'évaluation
- Personaldevelopment q1 Mod16 Demonstrateandcreatewaystomanagevariousemotions v2Document19 pagesPersonaldevelopment q1 Mod16 Demonstrateandcreatewaystomanagevariousemotions v2Crusher 14oPas encore d'évaluation
- How Much How Many WorksheetDocument1 pageHow Much How Many WorksheetAarronPas encore d'évaluation
- Basics of Tour GuidingDocument3 pagesBasics of Tour GuidingJanelle CerveraPas encore d'évaluation
- MSU Marketing Plan 11-07-2013Document25 pagesMSU Marketing Plan 11-07-2013sheref_hamadyPas encore d'évaluation
- 2009, AVEN - On Risk Defined As An Event Where Theoutcome Is UncertainDocument12 pages2009, AVEN - On Risk Defined As An Event Where Theoutcome Is UncertainDanielPas encore d'évaluation
- Existential TherapyDocument8 pagesExistential TherapytinPas encore d'évaluation
- Mini-Historiographical Essay InstructionsDocument2 pagesMini-Historiographical Essay InstructionsBarbara WaltersPas encore d'évaluation
- Modern children suffering adult diseases like obesityDocument1 pageModern children suffering adult diseases like obesityNgọc Thảo0% (1)
- Organizational Culture Impacts Innovation Culture in Auto CompaniesDocument25 pagesOrganizational Culture Impacts Innovation Culture in Auto CompaniesHoàng ThànhPas encore d'évaluation
- LKCDocument2 pagesLKCGlenden KhewPas encore d'évaluation
- Synthesis Chapter 2 First HalfDocument6 pagesSynthesis Chapter 2 First HalfPrincess EngresoPas encore d'évaluation
- Native Colonialism by Yirga GelawDocument246 pagesNative Colonialism by Yirga Gelawbirhane gebreegziabiher100% (4)
- Abhishek Pantha Bio Data and ResumeDocument4 pagesAbhishek Pantha Bio Data and ResumeSudarshan SharmaPas encore d'évaluation
- Jan 3-4 DLL TLE 102Document2 pagesJan 3-4 DLL TLE 102Jeh Ubaldo100% (6)