Académique Documents
Professionnel Documents
Culture Documents
AJO - Review of Common Clinical Conditions of The Proximal Tibiofibular Joint - 2018-12-12
Transféré par
pnalamatiTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
AJO - Review of Common Clinical Conditions of The Proximal Tibiofibular Joint - 2018-12-12
Transféré par
pnalamatiDroits d'auteur :
Formats disponibles
Review of Common Clinical Conditions of the Proximal
Tibiofibular Joint
Publish date: December 11, 2018
Authors:
Christian M. Curatolo, BS Gregory Bach, MD Christopher E. Mutty, MD John M. Marzo, MD
Author Affiliation | Disclosures
Mr. Curatolo is a medical student at The Jacobs School of Medicine and Biomedical Sciences, University at
Buffalo, Buffalo, New York. Dr. Mutty is Clinical Assistant Professor, Department of Orthopaedics, Jacobs School
of Medicine and Biomedical Sciences, University at Buffalo, Buffalo, New York. Dr. Marzo is Clinical Professor,
Department of Orthopaedics, Jacobs School of Medicine and Biomedical Sciences, University at Buffalo, Buffalo,
New York. Dr. Bach is a resident, Department of Surgery, University of South Florida Morsani College of
Medicine, Tampa, Florida.
Authors’ Disclosure Statement: The authors report no actual or potential conflict of interest in relation to this
article.
Address correspondence to: John Marzo, MD, The Jacobs School of Medicine and Biomedical Sciences, 955
Main St, Buffalo New York, 14203 (tel, 716-829-2982; fax, 716-829-3945; email jmmarzo@buffalo.edu).
Am J Orthop. 2018;47(12). Copyright Frontline Medical Communications Inc. 2018. All rights reserved.
Take-Home Points
Problems of the proximal tibiofibular joint (PFTJ) should be considered in the differential diagnosis when a
patient presents with complaints in the lateral aspect of the knee.
The primary function of the PTFJ is to transmit and absorb axial loads from weight bearing on the
extremity, and to dissipate torsional loads applied to the leg and ankle.
The most common instability pattern is anterolateral fibular displacement.
Most proximal tibiofibular joint instabilities can be treated with closed reduction and conservative care, but
some require internal fixation or soft-tissue reconstruction.
Arthritic conditions of the PTFJ are treated similar to those of any diarthrodial joint, with additional option
of surgical arthrodesis or resection arthroplasty.
Clinical conditions of the proximal tibiofibular joint (PTFJ) are an uncommon source of lateral knee complaints and
are often overlooked in the differential diagnosis as a source of the knee complaint. The most common conditions
of the PTFJ include traumatic dislocations, fractures, chronic instability, and osteoarthritis. This article reviews
the most common diseases affecting this joint and discusses both diagnostic and treatment strategies in an
attempt to raise awareness of this joint as a source of lateral knee complaints.
www.amjorthopedics.com Dec 2018 The American Journal of Orthopedics © 1
Anatomy
The PTFJ is an arthrodial synovial joint between the posterolateral surface of the tibia and the proximal fibular
head.1 Surrounding the synovial membrane of the articulation is a fibrous joint capsule with distinct anterior and
posterior tibiofibular ligaments.2,3 The anterior tibiofibular ligament has been described as 1 or 2 bands whereas
the posterior ligament consists of 1 band.3 The anterior ligament attaches anteroinferiorly to the fibular styloid
and posteriorly to Gerdy’s tubercle on the tibia. It runs linearly from posterior to anterior, and the fibular footprint
is immediately anterior to the insertion of the biceps femoris. The posterior ligament is located inferior to the
lateral joint space, and the fibular footprint is posterior to the insertion of the biceps femoris.3 Anatomy of the
PTFJ is shown schematically in Figure 1.
Both the lateral collateral ligament (LCL) and the tibiofibular interosseous membrane add stability to the PTFJ.
The LCL travels from the lateral femoral epicondyle to the lateral side of fibula head, anterior to the fibular
styloid. The interosseous membrane extends obliquely between the borders of the tibia and fibula. Additionally,
the short head of the biceps femoris, fibular collateral ligament, fabellofibular ligament, popliteofibular ligament,
and popliteus muscle all attach to the PTFJ and provide additional stability to the joint.
It is important to note that the common peroneal nerve passes posteriorly over the fibula neck, can be involved in
the clinical presentation, and is a potential source of concern with any injury to or surgery on the joint.4
Many studies have demonstrated that a communication with the tibiofemoral joint exists through the subpopliteal
recess, but the rate of communication has varied widely.5-8 Most recently, Bozkurt and colleagues5 found the rate
of communication between the PTFJ and lateral femorotibial space to be 57.9%. When distinct communication
exists, the PTFJ must be considered as a fourth compartment of the knee and is subject to any process that affects
the knee joint proper.
Ogden1 described 2 types of PTFJs, horizontal and oblique, with the latter being considered less stable because of
less rotational mobility. The horizontal configuration is defined as <20° of inclination of joint surface in relation to
the horizontal plane, and the oblique variation is defined as >20° of inclination of the joint surface in relation to
the horizontal plane.1
Biomechanics and Function
The primary function of the PTFJ is to dissipate torsional loads applied to the ankle, attenuate lateral tibial
bending moments, and transmit axial loads from weight bearing on the extremity.1 The degree of knee flexion,
ankle dorsiflexion, and tibial rotation all play an important role in PTFJ biomechanics. In knee flexion, the proximal
fibula moves anteriorly because of the relative laxity of the LCL and biceps femoris tendons. In knee extension, the
LCL and biceps femoris tighten, pulling the proximal fibula posteriorly.1 Because the LCL and biceps tendon are
both relaxed and less supportive during knee flexion, the PTFJ is more prone to injury with a flexed knee. The
ankle plays an important role in the biomechanics of the PTFJ because it contains the distal syndesmosis, where
both the tibia and fibula are firmly attached distally. During ankle dorsiflexion, the fibula must externally rotate to
accommodate a wider anterior talus.1 In regard to tibia rotation, Scott and colleagues9 demonstrated the
relationship between tibial rotation and fibular translation. With internal tibial rotation, the fibular head
translated posteriorly and with external tibial rotation, the fibula translated anteriorly. The greatest translational
motion was seen during loading of the knee into varus and during external tibial rotation at all flexion angles.
www.amjorthopedics.com Dec 2018 The American Journal of Orthopedics © 2
Clinical Conditions
Ogden10 classified instability of the PTFJ into 4 main groups: anterolateral dislocation, posteromedial dislocation,
superior dislocation, and atraumatic subluxation. Injury to the PTFJ usually occurs in younger, athletic patients
during sports that require violent twisting motions such as soccer, basketball, dance, skiing, horseback riding,
parachute jumping, jet skiing, and judo. Patients with generalized ligamentous laxity have been described as at
increased risk for joint instability.10,11
Acute Dislocation
The most common injury to the PTFJ is an anterolateral dislocation and involves injury to both the anterior and
posterior capsular ligaments, and occasionally the LCL.10 Anterolateral dislocation is usually the result of a fall on
a hyperflexed knee with the foot inverted and plantarflexed.11 While most anterolateral dislocations are the result
of indirect sports trauma, several have been associated with other types of skeletal injuries such as fracture-
dislocation of the hip, crush injury of the proximal and distal ends of the tibia, fracture-dislocation of the ankle,
proximal tibial fracture, and fracture-dislocation of the distal femoral epiphysis.10 Ogden10 described the
mechanism as follows: (1) sudden inversion and plantar flexion of the foot causing tension in the peroneal muscle
group, extensor digitorum longus, and extensor halluces longus, which applies a forward dislocating force to the
proximal end of the fibula; (2) simultaneous flexion of the knee, relaxing the biceps tendon and LCL; and (3)
twisting of the body over the knee, transmitting energy along the femur to the tibia, exerting a relative external
rotatory torque of the tibia on the foot, which is already fixed in inversion. Steps (2) and (3) spring the proximal
end of the fibula laterally while the contracting muscles of (1) pull the fibula anteriorly.
Posteromedial dislocation is the second most common type of acute PTFJ dislocation. Posteromedial dislocations
usually involve direct trauma and are associated with peroneal nerve injuries.1,2,10 The mechanism of dislocation
results in tearing of the anterior and posterior PTFJ capsular ligaments, followed by injury to the LCL and other
surrounding ligaments. This allows the biceps femoris to draw the unsupported proximal part of the fibula
posteromedially along the posterolateral tibial metaphysis.7
Superior dislocations are the least frequent form of acute PTFJ dislocations and are associated with high-energy
ankle injuries.2,10,12 Superior dislocation results in injury to the interosseous membrane between the tibia and
fibula and is frequently associated with tibial shaft fracture.10,11 Atraumatic, acquired superior dislocation of the
PTFJ has also been associated with congenital dislocation of the knee.10,11
Subluxation/Chronic Instability
Subluxation of the PTFJ classically involves excessive and symptomatic anterior-posterior motion without actual
dislocation of the joint.11 Subluxations of the PTFJ typically occur without any known trauma or injury and are
most frequently associated with benign hyperlaxity syndrome, Ehlers-Danlos syndrome, or muscular dystrophy.4,10
Semonian and colleagues13 suggest that subluxation of the PTFJ is not given enough recognition in the literature
and that instability should not be considered a rare condition. They hypothesize that many patients have joints
that do not tolerate increases in fibula rotation secondary to subclinical trauma, repetitive overuse, or
biomechanical variation of the joint. Semonian and associates13 state that the condition begins with the anterior
capsule and anterior tibiofibular ligament attenuation as a result of excessive fibular rotation. Once stretched, the
functional pull of the biceps femoris and soleus maintain the fibula in a relatively posterior and externally rotated
www.amjorthopedics.com Dec 2018 The American Journal of Orthopedics © 3
position. Furthermore, Ogden10 found that 70% of the dislocations and subluxations he studied were of the oblique
variant compared with that of the horizontal variant. Many authors suggest that the oblique variant is more at risk
for injury because of its decreased joint surface area causing decreased rotational mobility.1,2,10
Early recognition is extremely important in dislocations and subluxations of the PTFJ as undiagnosed acute trauma
can turn into chronic subluxation, and chronic subluxation may lead to dislocation.13 Additionally, chronic
subluxation or dislocation are thought result in osteoarthritis of the PTFJ.14
Osteoarthritis
The literature on osteoarthritis of the PTFJ is limited. Eichenblat and Nathan7 studied the PTFJ in cadavers and
dry bones and found that 28% had evidence of osteoarthritis. Clinically, however, osteoarthritis of the PTFJ is a
rare primary diagnosis, suggesting that involvement of the PTFJ is either asymptomatic or that symptoms are
associated with osteoarthritis of the knee joint. Boya and colleagues15 and Eichenblat and Nathan7 both found a
high correlation between the presence of osteoarthritis of the PTFJ and osteoarthritis of the tibiofemoral joint in
cadavers. The authors suggest this correlation may be related to the presence of anatomical communication
between the 2 joints. Theoretically, inflammatory mediators flow freely between the joint spaces and contribute to
arthritis in both joints. The possibility of degenerative arthritis of the PTFJ accompanying degenerative arthritis of
the knee warrants evaluation, especially in patients considering total knee arthroplasty. Unrecognized arthritis of
the PTFJ might influence outcome scores and be an unsolved source of lateral knee pain post-knee replacement.16
Clinical Presentation
Acute Dislocation
Patients with acute PTFJ dislocation present with pain, tenderness, swelling, and asymmetry of the lateral side of
the knee, while the knee joint is not swollen and range of knee motion is not limited.17 A bony prominence might
be felt, and the biceps femoris tendon can often appear to be tense.13 Active or passive ankle movements often
exacerbate the lateral knee pain.11 It is also important to examine the peroneal nerve, as transient peroneal palsy
has been described in all types of PTFJ dislocations but most often with posteromedial dislocations. Sensory
disturbance in the peroneal nerve distribution is more common than motor loss, but foot drop is also a potential
presenting sign.11 On examination, palpation of the fibular head illustrates tenderness and aggravates the pain.
Subluxation/Chronic Instability
Subluxation of the PTFJ can be difficult to recognize because the history, signs, and symptoms of lateral knee pain
can be subtle and sometimes misleading. In addition, current literature provides little information on specific
tests, measurements, signs, or subjective information regarding subluxation. Patients rarely reveal a history of
trauma or mechanism of injury. Subluxations are often associated with patients participating in repetitive sports
requiring running, jumping, or twisting movements, and can be present bilateral. Instability has also been
described in patients with osteomyelitis, rheumatoid arthritis, septic arthritis, pigmented villonodular synovitis,
below-knee amputations, osteochondroma, and in runners who recently increased mileage (especially during the
first 2-3 miles and during downhill running).11,13 Patients normally do not have difficulty with activities of daily
living, but symptoms may arise when making movements with a sudden change of direction.11
www.amjorthopedics.com Dec 2018 The American Journal of Orthopedics © 4
These patients usually complain of instability of the knee and pain along the lateral aspect of the knee. Pain
radiating proximally into the region of the iliotibial band and medially into the patellofemoral joint can be seen.13
Patients may also report clicking, popping, or catching of the lateral knee; while others will report a sense of
giving way of the knee joint.11,13 Progressive peroneal nerve symptoms are usually seen in older patients; however,
they are more common with acute PTFJ dislocations as discussed.13
A clinical method for examining a PTFJ with possible subluxation or chronic instability has been described by
Sijbrandij.18 With the patient in the supine position, the knee is flexed to 90° to relax the LCL and biceps femoris
tendon. The fibular head is then held between the thumb and index finger, and moved anteriorly and laterally.
Dislocation or subluxation will be felt and visualized as the fibular head translates, and should be compared with
the uninjured PTFJ. On release, the fibular head will return to its normal position, often with a click. Asking the
patient if this subluxation/reduction maneuver reproduces the symptoms or causes apprehension or pain may also
be helpful.18 Another method for examination is eliciting the Radulescu sign.11,13 While the patient lies prone, the
examiner stabilizes the thigh with 1 hand while the knee is flexed to 90°. The examiner then applies an internal
rotation force on the lower leg. Observing an abnormal excursion of the fibular head in an anterior and lateral
direction represents a positive test.11,13
Osteoarthritis
Clinical evaluation for osteoarthritis in the PTFJ is not well described in the literature. A single report describes
applying manual pressure over the fibular head during active ankle motion.16 A test known as the grinding test is
used as a sign to detect the involvement of the PTFJ as a component of osteoarthritis of the knee. A positive test
will elicit pain and/or tenderness of the joint.16
Diagnostic Imaging
Plain radiographs in the anteroposterior (AP) and true lateral views are useful as first-line investigations in
suspected PTFJ dislocation. Comparable AP and lateral radiographs of each knee are highly recommended to
detect findings that suggest dislocation.2 Abnormal findings include increased interosseous space, medial or
lateral displacement of the fibula on the anteroposterior view, and anterior or posterior displacement of the fibula
head on lateral view as shown in Figure 2.19,20
Resnick and colleagues2 proposed the use of the linear sloping radiodensity that defines the posteromedial corner
of the lateral tibial condyle as an indicator of anterolateral or posteromedial PTFJ dislocation. However, this
application is limited because of the PTFJ’s highly variable morphology.8 In a recent study conducted by Hey and
colleagues,21 5968 (2984 patients) knee radiographs were retrospectively collected and subjected to
radiographical measurements and statistical analysis. The tibiofibular overlap method had a specificity of 94.1%
and 84.5% when diagnosing PTFJ dislocations on the AP and lateral views, respectively.21
If a diagnosis of PTFJ is suspected but not clearly established based on radiography, computed tomography with
comparison views of the contralateral knee are recommended to confirm the diagnosis.17,22 This becomes more
critical in cases of suspected subluxation/chronic PTFJ instability. Additionally, magnetic resonance imaging (MRI)
can be used to assess chronic PTFJ instability. Recently, Burke and colleagues23 performed a 10-year retrospective
case series that included 7 patients with chronic PTFJ instability and included MRI as part of their evaluation. The
MRI abnormalities in these patients included periarticular soft tissue edema, including in the proximal soleus
muscle (n = 5), periarticular ganglion or ganglia (n = 4), tibiofibular ligament edema (n = 4), subchondral marrow
www.amjorthopedics.com Dec 2018 The American Journal of Orthopedics © 5
edema (n = 3), posterior tibiofibular ligament thickening (n = 2), subcortical cyst at a ligament insertion (n = 2),
partial-thickness tear of the anterior tibiofibular ligament (n = 1), and tibiofibular joint effusion (n = 1).
Osteoarthritis
Routine knee radiographs can show PTFJ joint space narrowing, sclerosis, marginal osteophytes, and local
osteopenia as conventional components of osteoarthritis of any joint. Serial radiographs have also been described
as effective in evaluating progressive degenerative changes of the PTFJ.14 An MRI will show osteophyte formation,
subchondral cysts, subchondral sclerosis, joint effusion, joint space narrowing, and is highly sensitive for detecting
degenerative changes in cartilage, as well as identifying other possible pathologies such as synovial cysts or
pigmented villonodular synovitis. Chronic PTFJ instability appears to predispose to tibiofibular osteoarthritis as
reported by Burke and colleagues,23 who found a particularly high incidence (42.9%) of osteoarthritis in patients
with chronic PTFJ instability. Additionally, Veth and colleagues14 found degenerative changes in 8 of 19 patients
presenting with PTFJ dislocations.
Treatment
Acute Dislocation
Prompt recognition and treatment of any acute PTFJ dislocation are necessary to avoid long-term instability and
other possible sequelae.11 Treatment consists of reduction followed by restriction of weight-bearing.11
Traditionally, the knee is immobilized with a cast in extension for 3 to 4 weeks followed by knee mobilization and
progressive range of motion exercises,24 but there is some controversy regarding complete immobilization.11,25,26
Initially, closed reduction is advised as the treatment for acute PTFJ dislocation.11,19,24 It involves placing the knee
in 80°to 110° of flexion to relax the biceps femoris and LCL, then applying an appropriate force to the fibular head
in a direction opposite the displacement.11,24 An audible pop is often heard as the fibula reduces back into normal
alignment. Stability of the reduction and stability of the knee should be determined with respect to both
posterolateral structures and the LCL after reduction.11 Anterolateral dislocations are usually easier to reduce, as
a posteromedial or superior dislocation can result in the fibular head being perched on the lateral tibial ridge, and
held by the LCL.11
Calabró and colleagues27 described a new, simple, and safe alternative technique of closed reduction of an anterior
dislocation if the classical method fails. This technique relies on ligamentotaxis and a dynamic counteraction
between muscles and ligaments to reduce the joint. The patient flexes the knee >90° while the physician applies a
counterforce to the heel with the palm. Simultaneously, gentle direct pressure should be applied to the fibular
head to move it toward the lateral tibial ridge. With a relaxed LCL, the biceps femoris tendon will actively reduce
the proximal fibular head back into its correct anatomic orientation.27
When a closed reduction in an awake patient has failed, a reduction under sedation or anesthesia should be
performed. If that fails, an open reduction should be performed. Following an open reduction, the joint is
stabilized with Kirschner wires, bioabsorbable pins, or cortical screws.24-26,28 The torn capsule and any injured
ligaments should also be primarily repaired. After approximately 6 weeks, the stabilization hardware may be
removed.24,25
Acute posteromedial dislocations are treated similarly to anterolateral dislocations; however, open reduction and
www.amjorthopedics.com Dec 2018 The American Journal of Orthopedics © 6
repair of the capsule and ligaments are more frequently required.10 Superior dislocations are also more frequently
reduced by open methods, sometimes dictated by open treatment of associated tibia or ankle fracture.10 Damage
to any structure of the posterolateral knee as a result of acute PTFJ injury should be repaired, as this has been
associated with better outcomes.14
PTFJ dislocation and tibia fracture can occur together, and in a retrospective study conducted by Herzog and
colleagues29 the authors recorded the incidence of PTFJ dislocation as 1.5% of operative tibial shaft fractures and
1.9% of operative tibial plateau fractures. Haupt and colleagues30 also conducted a retrospective study in which
the authors recorded the incidence of PTFJ dislocations in 1.06% of all tibial shaft fractures in their series. In both
studies combined, all except 1 PTFJ dislocation had been caused by high-energy trauma.29,30 In the case of PTFJ
dislocation with tibial shaft fracture, intramedullary nailing of the tibial shaft fracture followed by open reduction
of the PTFJ with 1 or 2 positioning screws just below the PTFJ has yielded satisfactory results.30 The positioning
screw should be removed 6 weeks post-operation to prevent PTFJ arthrodesis and patients should be supported in
full weight-bearing.30 An illustrative case report from our institution is shown in Figure 3.
Chronic Instability
Chronic instability is commonly the result of untreated or misdiagnosed subluxation of the PTFJ. Ogden10 reported
that 57% of patients with acute proximal tibiofibular dislocations required surgery for ongoing symptoms after
treatment failure with closed reduction and 3 weeks of immobilization. The first step in the management of
chronic instability of the PTFJ is usually a nonoperative approach. Immobilization, activity level modification,
utilization of a supportive strap placed 1 centimeter below the fibular head for pain relief, and participation in a
strength-training program of the lower leg are initial treatment recommendations.10,11,13 Many patients with
chronic PTFJ instability do not respond to conservative treatment and may pursue surgical intervention. Surgical
treatment options include permanent arthrodesis, resection of the fibular head, soft tissue reconstruction, and
temporary fixation.10,13,26,31 Given the rare nature of the injury and lack of data on varying treatments, there is no
clear consensus on the optimal surgical procedure.
Arthrodesis and fibular head resection are 2 traditional methods of surgically addressing the PTFJ, but both have
limitations that need to be recognized. Arthrodesis involves clearing the PTFJ of all articular cartilage, bone
grafting, and then reducing the joint using screw fixation.11 Rigid fixation prevents rotation of the fibula which
puts additional stress on the ankle, frequently causing pain and instability of the ankle joint.10,11 The other
traditional surgical option, fibular head resection, involves excision of the head and neck of the fibula while
preserving the fibular styloid and LCL.4 Fibular head resection is indicated when peroneal nerve symptoms or
palsy occur in PTFJ injuries.4,10 Unfortunately, resection may disrupt the posterolateral corner structures of the
knee and result in pain and instability.3,13 As a general rule, it is advisable to avoid arthrodesis and fibular head
resection in children and athletes because of the length of time during which complications can develop.11
Van den Bekerom and colleagues26 suggest that their technique of temporary fixation of the PTFJ using a
cancellous screw yields satisfactory outcomes in treating chronic PTFJ instability. The method entails having the
ankle dorsiflexed and the head of the fibula slightly externally rotated and reduced into the most stable position. A
hole is drilled in the anteromedial direction from posterior fibula head into the tibia. A non-tapped cortical screw
is used to fix the fibula head in the reduced position.26 The screw is removed after 3 to 6 months. Seven of 8
patients treated with this technique by Van den Bekerom and colleagues26 have had alleviation of symptoms,
although the screws broke in 2 cases before their planned removal.
Soft tissue reconstruction of the PTFJ has been an evolving area of treatment. Several techniques using a variety
www.amjorthopedics.com Dec 2018 The American Journal of Orthopedics © 7
of tissue grafts and fixation methods have been described. Giachino32 proposed a reconstruction in which the
fibular head is stabilized with a strip of ipsilateral biceps femoris tendon still attached distally to the fibular head
and deep fascia of the leg. Drill holes are made in the tibia, and the tissue is secured anteriorly to the fascia with a
suture. Shapiro and colleagues33 performed a stabilization using a strip of the iliotibial band still connected to its
insertion on Gerdy’s tubercle. The graft was tunneled through a tibial drill hole from anterior to posterior and
through the fibular head from posterior to anterior before suturing back onto itself. Another technique described
by Mena and colleagues34 uses a split biceps tendon autograft, harnessing the strong attachments of the tendon to
the fibular head to stabilize the reduced PTFJ.
More recently, Miller35 employed elements of the techniques described by Gianchino,32 Shapiro and colleagues,33
and Mena and colleagues34 to develop a method involving the biceps femoris tendon and iliotibial band in a soft
tissue reconstruction. The technique involves harvesting the biceps femoris tendon while preserving the distal
insertion and harvesting the iliotibial band while leaving the distal insertion at the Gerdy’s tubercle intact.35 The
biceps tendon is passed from posterior to anterior through a tibial bone tunnel, and the iliotibial band graft is
passed through the same tunnel but in the anterior to posterior direction. A bioabsorbable interference screw is
placed into the tibial tunnel from anterior to posterior. The remaining biceps tendon graft is sewn into the soft
tissue of the anterior tibia. The tail of the iliotibial band graft is passed through the fibular bone tunnel in the
posterior to anterior direction and looped around the fibular head and under the LCL before being sewn back onto
itself.35 Kobbe and colleagues36 described a surgical technique using the ipsilateral semitendinosis tendon while
Maffulli and colleagues37 and Morrison and colleagues38 presented techniques using the ipsilateral gracilis tendon.
These techniques do not jeopardize lateral knee or fibular head stability by avoiding the use of the biceps femoris
and iliotibial band, as well as local knee stabilizers. Warner and colleagues31 proposed a similar technique to the
aforementioned using a semitendinosus tendon; however, they do not reconstruct the anterior ligamentous
structures, as seen in Figures 4A and 4B.39 The authors have concerns that a 2-limb reconstruction as described
by Kobbe and colleagues36 and Morrison and colleagues38 may be prone to overconstraint or other errors in
tensioning because it does not allow for differential tension to be applied to each limb.31 According to Warner and
colleagues,31 the anterior structures of their patients with chronic PTFJ instability have appeared normal, and
isolated posterior ligamentous reconstruction has been adequate for the restoration of stability. Camarda and
colleagues28 proposed a technique very similar to that of Warner and colleagues;31 however, the tibial tunnel is
reamed from posterolateral to the anteromedial aspect of the tibia, exploiting the skin incision previously used for
tendon harvest.
Arthritis
The management options for secondary arthritis due to chronic PTFJ instability have rarely been discussed in the
literature. Arthrodesis or fibular head resection are options for the treatment of arthritis, and the above discussion
applies here as well. Yaniv and colleagues40 describe a technical procedure for addressing both instability and
secondary joint arthritis. The authors performed a ligament reconstruction of the PTFJ using the anterior part of
the biceps femoris combined with interpositional joint arthroplasty using a vascularized fascia lata strip. Two
weeks post-operation, the patient was walking with full weight-bearing and 6 weeks post-operation the first sports
activities were allowed.40
Conclusion
Conditions affecting the PTFJ, their diagnosis, and treatment are infrequent topics of discussion in the literature.
While PTFJ injury, instability, and other disease states are admittedly rare, clinicians need to include them in the
www.amjorthopedics.com Dec 2018 The American Journal of Orthopedics © 8
differential diagnosis of patients presenting with lateral knee complaints. Diagnostic imaging is a critical
component in early identification of PTFJ conditions to prevent long-term complications. Most injuries are treated
first with conservative methods, reserving surgery as an option when first-line measures are unsuccessful.
Advancements in surgical options for dislocation and subluxation/chronic instability of the joint have been made,
but further research on their effectiveness and long-term outcomes is needed before a gold-standard treatment
can be determined.
Key Info
Figures/Tables
Figures / Tables:
curatolomarzo1218_f1.jpg
curatolomarzo1218_f2.jpg
www.amjorthopedics.com Dec 2018 The American Journal of Orthopedics © 9
curatolomarzo1218_f3.jpg
www.amjorthopedics.com Dec 2018 The American Journal of Orthopedics © 10
curatolomarzo1218_f4.jpg
www.amjorthopedics.com Dec 2018 The American Journal of Orthopedics © 11
www.amjorthopedics.com Dec 2018 The American Journal of Orthopedics © 12
References
References
1. Ogden JA. The anatomy and function of the proximal tibiofibular joint. Clin Orthop Relat Res.
1974(101):186-191.
2. Resnick D, Newell JD, Guerra J, Jr., Danzig LA, Niwayama G, Goergen TG. Proximal tibiofibular
joint: anatomic-pathologic-radiographic correlation. AJR Am J Rroentgenol. 1978;131(1):133-138.
doi: 10.2214/ajr.131.1.133.
3. See A, Bear RR, Owens BD. Anatomic mapping for surgical reconstruction of the proximal
tibiofibular ligaments. Orthopedics. 2013;36(1):e58-63. doi: 10.3928/01477447-20121217-19.
4. Ogden JA. Subluxation of the proximal tibiofibular joint. Clin Orthop Relat Res. 1974(101):192-197.
doi: 10.2106/00004623-197456010-00015
5. Bozkurt M, Yilmaz E, Akseki D, Havitcioglu H, Gunal I. The evaluation of the proximal tibiofibular
joint for patients with lateral knee pain. Knee. 2004;11(4):307-312. doi: 10.1016/j.knee.2003.08.006
6. Dirim B, Wangwinyuvirat M, Frank A, et al. Communication between the proximal tibiofibular joint
and knee via the subpopliteal recess: MR arthrography with histologic correlation and stratigraphic
dissection. AJR Am J Roentgenol. 2008;191(2):W44-W51. doi: 10.2214/AJR.07.3406.
7. Eichenblat M, Nathan H. The proximal tibio fibular joint. An anatomical study with clinical and
pathological considerations. Int Orthop. 1983;7(1):31-39. doi: 10.1007/bf00267557
8. Espregueira-Mendes JD, da Silva MV. Anatomy of the proximal tibiofibular joint. Knee Surg Sports
Traumatol Arthrosc. 2006;14(3):241-249. doi: 10.1007/s00167-005-0684-z.
9. Scott J, Lee H, Barsoum W, van den Bogert AJ. The effect of tibiofemoral loading on proximal
tibiofibular joint motion. J Anat. 2007;211(5):647-653. doi: 10.1111/j.1469-7580.2007.00803.x.
10. Ogden JA. Subluxation and dislocation of the proximal tibiofibular joint. J Bone Joint Surg Am.
1974;56(1):145-154. doi: 10.2106/00004623-197456010-00015
11. Sekiya JK, Kuhn JE. Instability of the proximal tibiofibular joint. J Am Acad Orthop Surg.
2003;11(2):120-128. doi: 10.5435/00124635-200303000-00006
12. Horan J, Quin G. Proximal tibiofibular dislocation. Emerg Med Jl : EMJ. 2006;23(5):e33. doi:
10.1136/emj.2005.032144.
13. Semonian RH, Denlinger PM, Duggan RJ. Proximal tibiofibular subluxation relationship to lateral
knee pain: a review of proximal tibiofibular joint pathologies. J Orthop Sports Phys Ther.
1995;21(5):248-257. doi: 10.2519/jospt.1995.21.5.248.
14. Veth RP, Kingma LM, Nielsen HK. The abnormal proximal tibiofibular joint. Arch Orthop Trauma
Surg. 1984;102(3):167-171. doi: 10.1007/bf00575227
15. Boya H, Ozcan O, Oztekin HH. Radiological evaluation of the proximal tibiofibular joint in knees
with severe primary osteoarthritis. Knee Surg Sports Traumatol Arthrosc. 2008;16(2):157-159. doi:
10.1007/s00167-007-0442-5.
16. Öztuna V, Yildiz A, Özer C, Milcan A, Kuyurtar F, Turgut A. Involvement of the proximal tibiofibular
joint in osteoarthritis of the knee. The Knee. 2003;10(4):347-349. doi:
10.1016/s0968-0160(03)00004-8
17. Milankov M, Kecojević V, Gvozdenović N, Obradović M. Dislocation of the proximal tibiofibular
joint. Med Pregl. 2013;66(9-10):387-391. doi: 10.2298/mpns1310387m
18. Sijbrandij S. Instability of the proximal tibio-fibular joint. Acta Orthop Scand. 1978;49(6):621-626.
doi: 10.3109/17453677808993250
19. Aladin A, Lam KS, Szypryt EP. The importance of early diagnosis in the management of proximal
www.amjorthopedics.com Dec 2018 The American Journal of Orthopedics © 13
tibiofibular dislocation: a 9- and 5-year follow-up of a bilateral case. Knee. 2002;9(3):233-236. doi:
10.1016/S0968-0160(02)00012-1
20. Turco VJ, Spinella AJ. Anterolateral dislocation of the head of the fibula in sports. Am J Sports Med.
1985;13(4):209-215. doi: 10.1177/036354658501300401.
21. Hey HW, Ng LW, Ng YH, Sng WZ, Manohara R, Thambiah JS. Radiographical definition of the
proximal tibiofibular joint - A cross-sectional study of 2984 knees and literature review. Injury.
2016;47(6):1276-1281. doi: 10.1016/j.injury.2016.01.035.
22. Voglino JA, Denton JR. Acute traumatic proximal tibiofibular joint dislocation confirmed by
computed tomography. Orthopedics. 1999;22(2):255-258.
23. Burke CJ, Grimm LJ, Boyle MJ, Moorman CT, 3rd, Hash TW, 2nd. Imaging of Proximal Tibiofibular
Joint Instability: A 10 year retrospective case series. Clin Imaging. 2016;40(3):470-476. doi:
10.1016/j.clinimag.2015.12.011.
24. Parkes JC II, Zelko RR. Isolated acute dislocation of the proximal tibiofibular joint. Case report. J
Bone Joint Surg Am. 1973;55(1):177-183. Doi: 10.2106/00004623-197355010-00019
25. Gvozdenović N, Gvozdenović K, Obradović M, Stanković M. Modified technique of the treatment for
proximal tibiofibular joint dislocation. Vojnosanitetski Pregled. 2017;74(3):282-286. doi:
10.2298/VSP150318177G
26. van den Bekerom MP, Weir A, van der Flier RE. Surgical stabilisation of the proximal tibiofibular
joint using temporary fixation: a technical note. Acta Orthop Belg. 2004;70(6):604-608.
27. Calabró T, Cevolani L, Chehrassan M, Gasbarrini A. A new technique of reduction for isolated
proximal tibiofibular joint dislocation: a case report. Eur Rev Med Pharmacol Sci. 2014;18(1):93-95.
28. Camarda L, Abruzzese A, D'Arienzo M. Proximal tibiofibular joint reconstruction with autogenous
semitendinosus tendon graft. Tech Orthop. 2013;28(3):269-272. doi.
10.1097/BTO.0b013e31827b7182
29. Herzog GA, Serrano-Riera R, Sagi HC. Traumatic Proximal Tibiofibular Dislocation: A Marker of
Severely Traumatized Extremities. J Orthop Trauma. 2015;29(10):456-459. doi:
10.1097/BOT.0000000000000348.
30. Haupt S, Frima H, Sommer C. Proximal tibiofibular joint dislocation associated with tibial shaft
fractures - 7 cases. Injury. 2016;47(4):950-953. doi: 10.1016/j.injury.2016.01.037.
31. Warner BT, Moulton SG, Cram TR, LaPrade RF. Anatomic Reconstruction of the Proximal
Tibiofibular Joint. Arthrosc Tech. 2016;5(1):e207-e210. doi: 10.1016/j.eats.2015.11.004
32. Giachino AA. Recurrent dislocations of the proximal tibiofibular joint. Report of two cases. J Bone
Joint Surg Am. 1986;68(7):1104-1106. doi: 10.2106/00004623-198668070-00023
33. Shapiro GS, Fanton GS, Dillingham MF. Reconstruction for recurrent dislocation of the proximal
tibiofibular joint. A new technique. Orthop Rev. 1993;22(11):1229-1232.
34. Mena H, Brautigan B, Johnson DL. Split biceps femoris tendon reconstruction for proximal
tibiofibular joint instability. Arthroscopy. 2001;17(6):668-671. doi: 10.1053/jars.2001.22359.
35. Miller T. New technique of soft tissue reconstruction for proximal tibiofibular joint instability using
iliotibial band and biceps femoris longhead autograft. Tech Orthop. 2014;29(4):243-247. doi:
10.1097/BTO.0000000000000046
36. Kobbe P, Flohe S, Wellmann M, Russe K. Stabilization of chronic proximal tibiofibular joint
instability with a semitendinosus graft. Acta Orthop Belg. 2010;76(6):830-833.
37. Maffulli N, Spiezia F, Oliva F, Testa V, Capasso G, Denaro V. Gracilis autograft for recurrent
posttraumatic instability of the superior tibiofibular joint. Am J Sports Med. 2010;38(11):2294-2298.
doi: 10.1177/0363546510373472.
38. Morrison TD, Shaer JA, Little JE. Bilateral, atraumatic, proximal tibiofibular joint instability.
Orthopedics. 2011;34(2):133. doi: 10.3928/01477447-20101221-28.
39. Horst PK, LaPrade RF. Anatomic reconstruction of chronic symptomatic anterolateral proximal
www.amjorthopedics.com Dec 2018 The American Journal of Orthopedics © 14
tibiofibular joint instability. Knee Surg Sports Traumatol Arthrosc. 2010;18(11):1452-1455. doi:
10.1007/s00167-010-1049-9.
40. Yaniv M, Koenig U, Imhoff AB. A technical solution for secondary arthritis due to chronic
proximal tibiofibular joint instability. Knee Surg Sports Traumatol Arthrosc. 1999;7(5):334-336. doi:
10.1007/s001670050173.
Multimedia
Product Guide
Product Guide
STRATAFIX™ Symmetric PDS™ Plus Knotless Tissue Control Device
STRATAFIX™ Spiral Knotless Tissue Control Device
BioComposite SwiveLock Anchor
BioComposite SwiveLock C, with White/Black TigerTape™ Loop
×
×
Citation
Christian M. Curatolo, BS Gregory Bach, MD Christopher E. Mutty, MD John M. Marzo, MD . Review of Common
Clinical Conditions of the Proximal Tibiofibular Joint. Am J Orthop.
Publish date: December 11, 2018
Christian M.
Curatolo, BS
www.amjorthopedics.com Dec 2018 The American Journal of Orthopedics © 15
Vous aimerez peut-être aussi
- Orthopaedic Physical Examination General PrinciplesDocument13 pagesOrthopaedic Physical Examination General Principlesdokterrynaldi100% (4)
- Diaphragm Sparing Brachial Plexus Blocks A.12Document7 pagesDiaphragm Sparing Brachial Plexus Blocks A.12FIA SlotPas encore d'évaluation
- Low Back Pain Guidelines-Reduced2Document26 pagesLow Back Pain Guidelines-Reduced2ranggadr100% (1)
- ManualDocument95 pagesManualcristina_c_43Pas encore d'évaluation
- Cervical Spine - Minimally Invasive and Open SurgeryDocument338 pagesCervical Spine - Minimally Invasive and Open Surgerymohamed lamrana jallohPas encore d'évaluation
- Clinical and Radiological ExaminationDocument201 pagesClinical and Radiological ExaminationSllavko KallfaPas encore d'évaluation
- Low Back DisorderDocument160 pagesLow Back DisordernetshidoPas encore d'évaluation
- Functional Anatomy of The Lumbar SpineDocument7 pagesFunctional Anatomy of The Lumbar Spinealejo_buitragoPas encore d'évaluation
- Spinal Instability Neoplastic ScoreDocument9 pagesSpinal Instability Neoplastic ScoreJacklyn YekPas encore d'évaluation
- Jospt 2018 0301 PDFDocument51 pagesJospt 2018 0301 PDFMónica Sabogal JaramilloPas encore d'évaluation
- History of Spine BiomechanicsDocument13 pagesHistory of Spine BiomechanicsLeopoldo AguayoPas encore d'évaluation
- Gallstone Pancreatitis - CST PDFDocument5 pagesGallstone Pancreatitis - CST PDFDaniel Rosero CadenaPas encore d'évaluation
- Different Orthotic Management of Stroke & Brain Injury Patients With Its Biomechanical Efficiency - DevadriDocument34 pagesDifferent Orthotic Management of Stroke & Brain Injury Patients With Its Biomechanical Efficiency - DevadriDevadri DeyPas encore d'évaluation
- Iliopsoas Stretches GuideDocument2 pagesIliopsoas Stretches GuideGordana LakicPas encore d'évaluation
- MPT Orthopaedics 2019Document76 pagesMPT Orthopaedics 2019syed imranPas encore d'évaluation
- Chapter 12: Musculoskeletal Disorders: Multiple ChoiceDocument5 pagesChapter 12: Musculoskeletal Disorders: Multiple ChoiceJamiePas encore d'évaluation
- Unifying Neuro-Fasciagenic Model ofDocument18 pagesUnifying Neuro-Fasciagenic Model ofTasiaFerreiraPas encore d'évaluation
- Cataplasmas de CayceDocument30 pagesCataplasmas de CayceYarisa YanisaPas encore d'évaluation
- Somatic Dysfunction in FM PDFDocument25 pagesSomatic Dysfunction in FM PDFHailey0% (1)
- LisfrancDocument25 pagesLisfrancSamir AsmarPas encore d'évaluation
- Atlas of Nerve Conduction Studies and Electromyography (2 Ed.)Document12 pagesAtlas of Nerve Conduction Studies and Electromyography (2 Ed.)rodrigocorcino899959100% (1)
- Serratus Anterior Muscle InjuryDocument39 pagesSerratus Anterior Muscle Injuryandrea100% (2)
- Clinical Biomechanics - Basic Factors of Biodynamics and Joint StabilityDocument28 pagesClinical Biomechanics - Basic Factors of Biodynamics and Joint Stabilitymihaela_moldova9128Pas encore d'évaluation
- APA 7th Edition Template Student VersionDocument14 pagesAPA 7th Edition Template Student VersionAndrei ArtiedaPas encore d'évaluation
- MPFL ReconstructionDocument16 pagesMPFL ReconstructiondrjorgewtorresPas encore d'évaluation
- Lab Exercise No. 5: X-Ray Identification Activity: Name: Rocel Marie D. Lopez Section: BSN 1105Document11 pagesLab Exercise No. 5: X-Ray Identification Activity: Name: Rocel Marie D. Lopez Section: BSN 1105Rocel Marie Lopez100% (1)
- UveitisDocument90 pagesUveitisfranceseyemd89% (9)
- AACVPR Guidelines For Cardiac Rehabilitation and SDocument2 pagesAACVPR Guidelines For Cardiac Rehabilitation and SSergio Andres Chacon PedrazaPas encore d'évaluation
- Patellar InstabilityDocument16 pagesPatellar InstabilitydrjorgewtorresPas encore d'évaluation
- Como Identificar Dor NociplasticaDocument14 pagesComo Identificar Dor NociplasticaFranthesco CastroPas encore d'évaluation
- Rotator Cuff TendinopathyDocument7 pagesRotator Cuff TendinopathyMarcus Dos SantosPas encore d'évaluation
- 2018 Bernstein Levels MovementDocument23 pages2018 Bernstein Levels MovementjoaquinPas encore d'évaluation
- Clavicle AO Surgery Reference (2023)Document399 pagesClavicle AO Surgery Reference (2023)Wael GabrPas encore d'évaluation
- Rehabilitation and Return To Play Following Meniscal Repair PDFDocument14 pagesRehabilitation and Return To Play Following Meniscal Repair PDFYency AvilaPas encore d'évaluation
- Principles of Internal Fixation of The Craniomaxillofacial SkeletonDocument1 pagePrinciples of Internal Fixation of The Craniomaxillofacial SkeletonUmer HussainPas encore d'évaluation
- (Jean Oliver and Alison Middleditch (Auth.) ) Funct (B-Ok - CC)Document332 pages(Jean Oliver and Alison Middleditch (Auth.) ) Funct (B-Ok - CC)Lorena BurdujocPas encore d'évaluation
- Bioenergetics Nicholls 4th Ed. Intro To CHPT 1Document2 pagesBioenergetics Nicholls 4th Ed. Intro To CHPT 1MellyPas encore d'évaluation
- Un Modelo Sugerido para El Examen Físico y El Tratamiento Conservador de La Pubalgia AtléticaDocument14 pagesUn Modelo Sugerido para El Examen Físico y El Tratamiento Conservador de La Pubalgia AtléticaFernando Rojas LopezPas encore d'évaluation
- Pusher Syndrome A Frequent But Little-Known Disturbance of Body Orientation PerceptionDocument11 pagesPusher Syndrome A Frequent But Little-Known Disturbance of Body Orientation PerceptionKlgo Alex AyalaPas encore d'évaluation
- Women With Cronic Pelvic Pain. An Osteopathic Approach PDFDocument3 pagesWomen With Cronic Pelvic Pain. An Osteopathic Approach PDFHapplo82Pas encore d'évaluation
- (Douglas W. Zochodne) Neurobiology of Peripheral NDocument318 pages(Douglas W. Zochodne) Neurobiology of Peripheral NImmer Armendáriz BetancourtPas encore d'évaluation
- Common Entrapment NeuropathiesDocument11 pagesCommon Entrapment Neuropathiesrafael rocha novaesPas encore d'évaluation
- IASP 2016 Poster Abstracts - Wednesday PDFDocument731 pagesIASP 2016 Poster Abstracts - Wednesday PDFHendriik ViicarloPas encore d'évaluation
- Mechanics of Mandibular MovementDocument5 pagesMechanics of Mandibular MovementOpris PetruPas encore d'évaluation
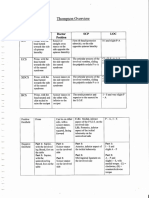
- 2016 Course Documentation Handbook VfinalDocument294 pages2016 Course Documentation Handbook VfinalctgruzalPas encore d'évaluation
- ICF-Ankle Trimalleolar (Cotton's) Fracture RehabDocument18 pagesICF-Ankle Trimalleolar (Cotton's) Fracture RehabdvenumohanPas encore d'évaluation
- ARTHROLOGYDocument10 pagesARTHROLOGYAlina MoisePas encore d'évaluation
- Kibler Et Al 2012 Scapula Dyskinesis and Its Relation To Shoulder Injury PDFDocument9 pagesKibler Et Al 2012 Scapula Dyskinesis and Its Relation To Shoulder Injury PDFPamela DíazPas encore d'évaluation
- Developmental Dysplasia of the Hip: Causes, Symptoms and TreatmentDocument28 pagesDevelopmental Dysplasia of the Hip: Causes, Symptoms and TreatmentSheilla RatnasariPas encore d'évaluation
- Hip Dislocation: Evaluation and Management: Review ArticleDocument11 pagesHip Dislocation: Evaluation and Management: Review ArticleFadhli Aufar KasyfiPas encore d'évaluation
- Women's Health Diploma ProgramDocument3 pagesWomen's Health Diploma ProgramMahmoud Abo AlfaPas encore d'évaluation
- Updates Clinical: International Association For The Study of PainDocument6 pagesUpdates Clinical: International Association For The Study of PainSuaeni Kurnia WirdaPas encore d'évaluation
- Digestion Enzymes Break Down Food into Absorbable NutrientsDocument12 pagesDigestion Enzymes Break Down Food into Absorbable NutrientsIvonneDiazPas encore d'évaluation
- Rehabilitation of LeprosyDocument72 pagesRehabilitation of LeprosyNur OctavianiPas encore d'évaluation
- Core Stability in Patellofemoral Pain SyndromeDocument8 pagesCore Stability in Patellofemoral Pain SyndromeInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- Biomechanics of MovementDocument17 pagesBiomechanics of Movements_chandrubioPas encore d'évaluation
- Ispo Self-Study DocumentDocument24 pagesIspo Self-Study DocumentFatima SanchezPas encore d'évaluation
- Ankle Joints and Ligaments OverviewDocument8 pagesAnkle Joints and Ligaments OverviewkristinaPas encore d'évaluation
- Classification and Surgical Management of Spinal 22Document7 pagesClassification and Surgical Management of Spinal 22Mariana IugaPas encore d'évaluation
- Blood Flow Restriction Training in Rehabilitation: A Useful Adjunct or Lucy's Latest Trick?Document5 pagesBlood Flow Restriction Training in Rehabilitation: A Useful Adjunct or Lucy's Latest Trick?Arnold BarraPas encore d'évaluation
- Cementum (B. K. Berkovitz, Oral Anatomy, Histology & Embryology, 3rd Edition)Document12 pagesCementum (B. K. Berkovitz, Oral Anatomy, Histology & Embryology, 3rd Edition)Drsumit BahlPas encore d'évaluation
- Jakarta School of Prosthetics & Orthotics: Upper Limb Prosthetics Course Work Manual 2010Document84 pagesJakarta School of Prosthetics & Orthotics: Upper Limb Prosthetics Course Work Manual 2010Adinda Dinda100% (1)
- JB6 4 121 727Document3 pagesJB6 4 121 727Rhizka djitmauPas encore d'évaluation
- Medical Rehabilitation in Compression FractureDocument32 pagesMedical Rehabilitation in Compression FracturegloriaPas encore d'évaluation
- Contraindications in Malignancy Grid 2015Document1 pageContraindications in Malignancy Grid 2015Sharada NayakPas encore d'évaluation
- Prelegere Osteoarticular enDocument93 pagesPrelegere Osteoarticular enViorelVelenciucPas encore d'évaluation
- Manual Muscle TestingDocument13 pagesManual Muscle TestingPásztai ZoltánPas encore d'évaluation
- August2010CCLundenDocument15 pagesAugust2010CCLundenMariela CanovasPas encore d'évaluation
- A Novel TECHNIQUE For Isolated Weber B Ankle Fractures Surgical Treatment Using A Specialized Anatomical Locking PlateDocument6 pagesA Novel TECHNIQUE For Isolated Weber B Ankle Fractures Surgical Treatment Using A Specialized Anatomical Locking PlatepnalamatiPas encore d'évaluation
- The Cold, Hard Facts of Cryotherapy in Orthopedics and Sports MedicineDocument13 pagesThe Cold, Hard Facts of Cryotherapy in Orthopedics and Sports MedicinepnalamatiPas encore d'évaluation
- Safety and Efficacy of Percutaneous Injection of Lipogems Micro-Fractured Adipose Tissue For OA KneesDocument11 pagesSafety and Efficacy of Percutaneous Injection of Lipogems Micro-Fractured Adipose Tissue For OA KneespnalamatiPas encore d'évaluation
- Allergies in OrthopaedicsDocument7 pagesAllergies in OrthopaedicspnalamatiPas encore d'évaluation
- Ambulatory OrthopaedicsDocument8 pagesAmbulatory OrthopaedicspnalamatiPas encore d'évaluation
- Novumax Hospital Introduces India's First Bioflex Laser Therapy CentreDocument3 pagesNovumax Hospital Introduces India's First Bioflex Laser Therapy CentreKanika BhaskarPas encore d'évaluation
- Knee Strengthening Exercises Are One of The Best Ways To CureDocument10 pagesKnee Strengthening Exercises Are One of The Best Ways To CureRatnaPrasadNalamPas encore d'évaluation
- NCKH - Cải thiện độ tan và độ hòa tan của meloxicam với hệ phân tán rắnDocument9 pagesNCKH - Cải thiện độ tan và độ hòa tan của meloxicam với hệ phân tán rắnkamakaballestas87Pas encore d'évaluation
- Orthopedic Chanting: by Dr. ParasDocument15 pagesOrthopedic Chanting: by Dr. ParasSaravanan DevarajPas encore d'évaluation
- Aubf Synovial FluidDocument1 pageAubf Synovial FluidMaryPas encore d'évaluation
- Penyakit Sendi Degeneratif & Patologi TulangDocument38 pagesPenyakit Sendi Degeneratif & Patologi TulangSaddam ZakariyaPas encore d'évaluation
- Konsep Nyeri - Dr. SusiloDocument18 pagesKonsep Nyeri - Dr. Susilotendri ayuPas encore d'évaluation
- Rheumatoid ArthritisDocument45 pagesRheumatoid ArthritisThe AbyssinicansPas encore d'évaluation
- Essay 16Document1 pageEssay 16JEEMAIPas encore d'évaluation
- GINGEL Development and Evaluation of Anti-Arthritic Gel Containing Ginger (Zingiber Officinale)Document7 pagesGINGEL Development and Evaluation of Anti-Arthritic Gel Containing Ginger (Zingiber Officinale)International Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- Effectiveness of Physical Therapy Interventions For Gout Arthritis - Single Case Study ReportDocument11 pagesEffectiveness of Physical Therapy Interventions For Gout Arthritis - Single Case Study ReportLoubna AdnanePas encore d'évaluation
- Greater Trochanteric Bursitis Exercises New YorkDocument4 pagesGreater Trochanteric Bursitis Exercises New YorkJorge Gutierrez MozoPas encore d'évaluation
- Tugas Bahasa Inggris TK IiDocument5 pagesTugas Bahasa Inggris TK IiNurharwati WanthyPas encore d'évaluation
- Chitara Pentru ProstiDocument3 pagesChitara Pentru ProstimariodalPas encore d'évaluation
- Injury Hotspots: Swimming: Polytechnic University of The PhilippinesDocument13 pagesInjury Hotspots: Swimming: Polytechnic University of The PhilippinesMarcial VirayPas encore d'évaluation
- 1 s2.0 S0894113016300114 MainDocument13 pages1 s2.0 S0894113016300114 Mainwengi yipPas encore d'évaluation
- C Ebu Institute of Technology University: Plant VisitDocument5 pagesC Ebu Institute of Technology University: Plant VisitAdonis Cabingas ArponPas encore d'évaluation
- GO ON Knee LequesneDocument2 pagesGO ON Knee LequesnedgcrPas encore d'évaluation
- Management of OADocument50 pagesManagement of OADeni Mahisa PurbaPas encore d'évaluation
- MSK Viva Voce Lateral EpicondylitisDocument7 pagesMSK Viva Voce Lateral EpicondylitisTing ChenPas encore d'évaluation
- Assessing The Nuerologic, Musculoskeletal and Peripheral Vascular System RubricsDocument4 pagesAssessing The Nuerologic, Musculoskeletal and Peripheral Vascular System RubricsSamantha ZacharyPas encore d'évaluation
- Pinnacle Surgical Technique - 0Document36 pagesPinnacle Surgical Technique - 0Rigid EndoscopyPas encore d'évaluation