Académique Documents
Professionnel Documents
Culture Documents
Sore Throat: High Risk For Rheumatic Fever
Transféré par
Syahidatul Kautsar NajibTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Sore Throat: High Risk For Rheumatic Fever
Transféré par
Syahidatul Kautsar NajibDroits d'auteur :
Formats disponibles
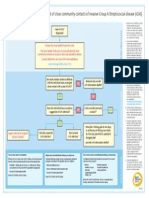
Sore throat
Aim: All group A streptococcal (GAS) pharyngitis
Aim: Reduce unnecessary antibiotic use
in high rheumatic fever risk patients are treated
High Risk for Rheumatic Fever
High risk if personal, family or household history of rheumatic fever or have 2 or more criteria:
• Māori or Pacific
Low Risk for Rheumatic Fever
• Aged 3–35 years Assess severity of symptoms and occupational risk
• Living in crowded circumstances or lower socioeconomic area of spreading GAS.
If only 1 criterion see green box.
1. Unwell patients have potential to develop local
suppurative complications.
2. Throat swabbing and/or antibiotic treatment* may not be
routinely required for mild symptoms unless the patient is
Primary Care or School Sore Throat Clinics at increased risk of spreading GAS e.g. healthcare and
Emergency Departments Throat swab residential care workers, food handlers, school and early
Throat swab if follow up possible Wait for result before starting antibiotics4 childhood teachers and students. Instead consider analgesia.
Start 10 days of empiric penicillin or amoxicillin If GAS positive: *10 days of empiric penicillin or amoxicillin or single dose of IM benzathine penicillin.
or single dose of IM benzathine penicillin Start 10 days of antibiotics
If group A streptococci (GAS) positive:
• Consider swabbing all symptomatic household Reasons to Throat Swab in Those at High Risk Footnotes
members.1 of Rheumatic Fever 1. In family households, more than half of secondary cases of serologically proven
GAS pharyngitis were in 5–12 year old children. Risk of secondary GAS infection
• Consider isolating at home for 24 hours after starting • To identify GAS pharyngitis in index case
was 1.8 times greater than that of primary infection in the community.a
• To discontinue antibiotics in GAS negative cases3
10 days of antibiotics.2 • To initiate antibiotic therapy (check and reinforce
Adults are at lesser risk of developing rheumatic fever but given their household
contact status, they may spread GAS.
10 day adherence) in following up GAS positive results
• Swab all household members (symptomatic or not), if: 2. The Writing Group recommends that for workers who are at increased risk of
• To allow household contact tracing and initiate
spreading GAS (healthcare workers, food handlers, teachers and childcare
appropriate treatment
-- ≥ 3 cases of GAS pharyngitis in household • To reduce unnecessary antibiotic prescribing
workers) isolation should be considered for 24 hours after starting antibiotics.
in the last 3 months, or Legislation allows Medical Officers of Health to enforce 7 days isolation for
• To allow for surveillance of GAS pharyngitis resistant
pupils, teachers and food handlers.b
-- Personal, family or household history of rheumatic to antibiotics
3. >70% of sore throats will be viral and do not need antibiotic treatment.c
• To provide education when following up throat
fever and promptly treat all GAS positive cases swab results.
4. Start empiric antibiotics if results of throat swab are likely to be delayed.
See Algorithm in Guideline for Household References
Consider not throat swabbing and instead start empiric a. Danchin M et al. Burden of acute sore throat and group A streptococcal
Sore Throat Management. antibiotics if follow-up may be problematic. pharyngitis in school-aged children and their families in Australia.
Pediatrics. 2007; 120: 950-957.
If GAS negative: b. Health (Infectious and Notifiable Diseases) Regulations 1966. Amended and
reprinted 2013: http://www.legislation.govt.nz/regulation/public/1966/0087/
• Stop antibiotics.3 latest/whole.html#DLM24238
c. Shaikh N et al. Prevalence of streptococcal pharyngitis and streptococcal
carriage in children: A meta-analysis. Pediatrics. 2010; 126: 557–564.
http://www.heartfoundation.org.nz Printed August 2014
Antibiotics for Routine Group A Streptococcal (GAS) Pharyngitis
Standard treatment for a patient’s first or second case of confirmed group A streptococcal (GAS) pharyngitis.
Antibiotic Route Dose Duration IDSA GRADE 2012*,a
Penicillin V† PO Children <20kg: 250mg two or three times daily 10 days Strong, high
Adolescents & Adults ≥20kg: 500mg two or three times daily
Amoxicillin† PO Once daily: 50mg/kg dose once daily (Max daily dose 1000mg) 10 days Strong, high
OR: Weight <30kg: 750mg once daily
Weight ≥30kg: 1000mg once daily
Twice daily: 25mg/kg dose twice daily (Max daily dose 1000mg)
Benzathine penicillin‡ IM Children <30kg: 450mg (600,000 U) Single dose Strong, high
Adults & Children ≥30kg: 900mg (1,200,000 U)
If concern about allergic (IgE mediated§ or anaphylactic) response to beta lactams, use:
RoxithromycinII PO Children: 2.5mg/kg dose twice daily 10 days Unavailable in the USA
Pending Pharmac Adults: 300mg once daily
decision OR: 150mg twice daily
Erythromycin PO Children & Adults: 40mg/kg/day in 2–3 divided doses 10 days **
ethyl succinateII, ¶ (Max adult daily dose 1000mg)
For people on benzathine penicillin IM prophylaxis who are GAS positive:
Treat with a 10 day course of oral penicillin or amoxicillin.
Check adherence to prophylaxis programme. Serum penicillin levels will be falling by week three and four post IM long acting benzathine penicillin injection.h
Source: Modified from Table Two in the 1DSA Guideline 2012a. © by permission of Oxford University Press, 2014.
Footnotes References
* The Infectious Diseases Society of America (IDSA) used the GRADE (Grading of Recommendations Assessment, a. Shulman S et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis:
Development and Evaluation) system (see Guideline Update 2014 for description)a 2012 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2012; 55:1279–1282.
† Amoxicillin can be taken with food whereas oral penicillin V is best absorbed on an empty stomach. b. Lennon DR et al. Once-daily amoxicillin versus twice-daily penicillin V in group A beta-haemolytic streptococcal
Both are equally effective in eradicating GAS.b,c Lower frequency of antibiotic dosing has been shown to improve pharyngitis. Arch Dis Child. 2008; 93: 474-478.
adherence.d,e Amoxicillin is relatively palatable.f c. Clegg HW et al. Treatment of streptococcal pharyngitis with once-daily compared with twice-daily amoxicillin:
‡ Benzathine penicillin can be given with lignocaine to reduce injection site pain (see Guideline Update 2014). a noninferiority trial. Pediatr Infect Dis J. 2006; 25: 761-767.
It may be marginally more effective than oral penicillin or amoxicillin in eradicating GAS pharyngitis.g d. Llor C et al. The higher the number of daily doses of antibiotic treatment in lower respiratory tract infection the
§
IgE-mediated reactions include ANY bronchospasm, angioedema, hypotension, urticarial or pruritic rash. worse the compliance. J Antimicrob Chemother. 2009; 63: 396-399.
II
Always check for drug interactions before prescribing. In particular, care should be taken when prescribing e. Kardas P. Comparison of patient compliance with once-daily and twice-daily antibiotic regimens in respiratory
macrolides to patients taking warfarin and carbamazepine. tract infections: results of a randomized trial. J Antimicrob Chemother. 2007; 59: 531-536.
¶
The erythromycin currently funded by Pharmac is erythromycin ethyl succinate. There are other erythromycins f. Steele RW et al. Compliance issues related to the selection of antibiotic suspensions for children.
available with different pharmacokinetic profiles. Pediatr Infect Dis J. 2001; 20: 1-5.
** Erythromycin is not recommended in 2012 The Infectious Diseases Society of America (IDSA) Guideline.a g. Shulman ST et al. Streptococcal pharyngitis. In: Stevens DL, Kaplan EL (Eds). Streptococcal infections:
In 2002 the IDSA recommended erythromycin based on a different grading system for clinical guideline Clinical Aspects, microbiology and molecular pathogenesis. 2000. New York, Oxford University Press.
recommendations (see Guideline Update 2014) h. Kaplan EL et al. Pharmacokinetics of benzathine penicillin G: Serum levels during the 28 days after intramuscular
injection of 1,200,000 units. J Pediatr. 1989; 115: 146-150.
http://www.heartfoundation.org.nz Printed August 2014
Vous aimerez peut-être aussi
- Pharyngitis: Patient Population. ObjectivesDocument10 pagesPharyngitis: Patient Population. ObjectivesjumiPas encore d'évaluation
- Management of Infection in Primary Care Adapted For Local UseDocument15 pagesManagement of Infection in Primary Care Adapted For Local UseWizri SuharianiPas encore d'évaluation
- Faring It IsDocument10 pagesFaring It IsjavlafPas encore d'évaluation
- نموذج تعليمات المضادات الحيوية (أطفالDocument9 pagesنموذج تعليمات المضادات الحيوية (أطفال5n7qd7fjjjPas encore d'évaluation
- Tetanus Immune Globulin (Human) : Revision Date: May 27, 2013Document3 pagesTetanus Immune Globulin (Human) : Revision Date: May 27, 2013DrscottmccallPas encore d'évaluation
- Summary Antimicrobial Prescribing Guidance - July 21 For BNFDocument31 pagesSummary Antimicrobial Prescribing Guidance - July 21 For BNFbarcanbiancaPas encore d'évaluation
- Diagnosis Treatment and Prevention of Typhoid Fever in Adults 2017Document11 pagesDiagnosis Treatment and Prevention of Typhoid Fever in Adults 2017Khayla Ray RondobioPas encore d'évaluation
- Antibiotic Prescribing in Primary Care - Therapeutic Guidelines Summary Table 2019Document2 pagesAntibiotic Prescribing in Primary Care - Therapeutic Guidelines Summary Table 2019RL100% (1)
- Universiti Teknologi Mara (Uitm) Puncak Alam Campus Faculty of Health SciencesDocument9 pagesUniversiti Teknologi Mara (Uitm) Puncak Alam Campus Faculty of Health SciencesMOHD MU'IZZ BIN MOHD SHUKRIPas encore d'évaluation
- Igas Flow ChartDocument1 pageIgas Flow ChartYi Wei KoPas encore d'évaluation
- PharingitisDocument17 pagesPharingitisFirman AlAshfaPas encore d'évaluation
- Antimicrobial Prescribing GuidanceDocument24 pagesAntimicrobial Prescribing GuidanceJason Merari PeranginanginPas encore d'évaluation
- Influenza More InfosDocument3 pagesInfluenza More InfosincognitoPas encore d'évaluation
- Primary Prevention of Acute Rheumatic FeverDocument3 pagesPrimary Prevention of Acute Rheumatic FeverJoe LuPas encore d'évaluation
- Guideline URTI in South Africa 2008Document9 pagesGuideline URTI in South Africa 2008Febbe Nadia Okky LucianaPas encore d'évaluation
- Respiratory Tract Infections - Med DidacticsDocument59 pagesRespiratory Tract Infections - Med Didacticsapi-649060644Pas encore d'évaluation
- Tetanus Immune Globulin (TIG) : IndicationsDocument5 pagesTetanus Immune Globulin (TIG) : IndicationsShams JailaniPas encore d'évaluation
- Assessment Nursing Diagnosis Scientific Explanation Objectives Interventions Rationale Expected OutcomeDocument3 pagesAssessment Nursing Diagnosis Scientific Explanation Objectives Interventions Rationale Expected OutcomeRammiel Saylo CarlosPas encore d'évaluation
- Acute Otitis Media in ChildrenDocument7 pagesAcute Otitis Media in ChildrensssscePas encore d'évaluation
- Pediatric Treatment RecDocument5 pagesPediatric Treatment RecGrace Noviyanthi SinambelaPas encore d'évaluation
- Corticosteroids For Sore Throat: A Clinical Practice GuidelineDocument7 pagesCorticosteroids For Sore Throat: A Clinical Practice GuidelineAmelia 'amek' RahayuPas encore d'évaluation
- Calf PneumoniaDocument2 pagesCalf PneumoniaNeniPas encore d'évaluation
- Acute PharyngitisDocument3 pagesAcute Pharyngitisdr_dediet1Pas encore d'évaluation
- JurnalDocument3 pagesJurnalMmama HakimahPas encore d'évaluation
- Guidelines On MGT of Animal BitesDocument44 pagesGuidelines On MGT of Animal BitesTinea nigraPas encore d'évaluation
- Childhood Immunization & Catch Up Immunization-2Document53 pagesChildhood Immunization & Catch Up Immunization-2Haters ExterminatorPas encore d'évaluation
- NICE - UKHSA APG Summary Table Content Only - 29 June 2023Document28 pagesNICE - UKHSA APG Summary Table Content Only - 29 June 2023Stacey WoodsPas encore d'évaluation
- Gentamicin in NeonatusDocument9 pagesGentamicin in NeonatusSalsabila RaniahPas encore d'évaluation
- Advisory - Pertussis 2024.03.22Document3 pagesAdvisory - Pertussis 2024.03.22Jenevive PaurongPas encore d'évaluation
- Treatment of Acute PharyngitisDocument4 pagesTreatment of Acute PharyngitisZafira Ananda RaishaPas encore d'évaluation
- Ofelia L. Mendoza - Drug StudyDocument3 pagesOfelia L. Mendoza - Drug StudyMaenard JavierPas encore d'évaluation
- Flow Chart Management of Dog or Cat Bite 17.1.23 (V4)Document5 pagesFlow Chart Management of Dog or Cat Bite 17.1.23 (V4)leo89azman100% (1)
- INFORMATION SHEET 1. - Risk Categorisation Guidelines: Protection Against The Specified Infectious Diseases Is RequiredDocument4 pagesINFORMATION SHEET 1. - Risk Categorisation Guidelines: Protection Against The Specified Infectious Diseases Is RequiredjacksonzchenPas encore d'évaluation
- Antibiotics Guide 2017Document32 pagesAntibiotics Guide 2017Josef SosPas encore d'évaluation
- Allergic RhinitisDocument8 pagesAllergic RhinitisJuanPas encore d'évaluation
- Atopic Dermatitis Complicated by Severe Impetigo in A Syrian Refugee InfantDocument4 pagesAtopic Dermatitis Complicated by Severe Impetigo in A Syrian Refugee InfantbillyPas encore d'évaluation
- Acute Respiratory Infections: Streptococcus PneumoniaeDocument9 pagesAcute Respiratory Infections: Streptococcus Pneumoniaesunma09082001Pas encore d'évaluation
- Bpacnz Antibiotics GuideDocument40 pagesBpacnz Antibiotics GuideBulborea MihaelaPas encore d'évaluation
- BarnardDocument4 pagesBarnardSina SoltaniPas encore d'évaluation
- Acute Otitis MediaDocument27 pagesAcute Otitis MediasssscePas encore d'évaluation
- Pharyngitis: Approach To Diagnosis and TreatmentDocument9 pagesPharyngitis: Approach To Diagnosis and Treatmentraudhatul muttaqinPas encore d'évaluation
- Infections in Primary CareDocument5 pagesInfections in Primary CareAtta Muhammad Memon100% (1)
- TonsillitisDocument5 pagesTonsillitisyosefPas encore d'évaluation
- Mongardini 1999Document14 pagesMongardini 1999Anita PrastiwiPas encore d'évaluation
- Pharyngitis (Strep Throat) : Group A Streptococcal (GAS) DiseaseDocument7 pagesPharyngitis (Strep Throat) : Group A Streptococcal (GAS) DiseasegiselPas encore d'évaluation
- Acute Pharyngitis GuidelineDocument7 pagesAcute Pharyngitis GuidelineRezki AnurPas encore d'évaluation
- Revised Guidelines For Homoeopathy Practitioners For Prophylaxis and Symptomatic Management of COVID-19 Patients in Home IsolationDocument6 pagesRevised Guidelines For Homoeopathy Practitioners For Prophylaxis and Symptomatic Management of COVID-19 Patients in Home IsolationBABUPas encore d'évaluation
- Risk Factors Associated With Diarrhea in Danish Commercial Mink (Neovison Vison) During The Pre-Weaning PeriodDocument8 pagesRisk Factors Associated With Diarrhea in Danish Commercial Mink (Neovison Vison) During The Pre-Weaning PeriodardytawaradaniPas encore d'évaluation
- DocumentDocument5 pagesDocumentPRECIOUS LOVE LAGRIMASPas encore d'évaluation
- Pfizer Vaccine Explainer Version 2Document6 pagesPfizer Vaccine Explainer Version 2Samanta SlanaPas encore d'évaluation
- Summary Guide To Tetanus Prophylaxis in Routine Wound ManagementDocument1 pageSummary Guide To Tetanus Prophylaxis in Routine Wound ManagementmwaPas encore d'évaluation
- Singular in Infant WheezerDocument31 pagesSingular in Infant Wheezerwawa chenPas encore d'évaluation
- ImmunizationDocument20 pagesImmunizationsarguss14100% (2)
- Cough and ColdsDocument3 pagesCough and ColdsKarl-Ren Lacanilao100% (1)
- Diagnosis and Treatment of Group A Streptococcus PharyngitisDocument2 pagesDiagnosis and Treatment of Group A Streptococcus Pharyngitiselite9491Pas encore d'évaluation
- GAS CarriersDocument2 pagesGAS CarriersRahaf AbughoshPas encore d'évaluation
- Guideline/Drug Updates: 2020 Rxprep Course Book: Update Type DescriptionDocument5 pagesGuideline/Drug Updates: 2020 Rxprep Course Book: Update Type Descriptionsyed100% (1)
- 5 Cefuroxime Drug StudyDocument4 pages5 Cefuroxime Drug Studyshadow gonzalezPas encore d'évaluation
- Health Advice and Immunizations for TravelersD'EverandHealth Advice and Immunizations for TravelersPas encore d'évaluation
- Pathophysiology and Treatment of Motion Sickness: ReviewDocument6 pagesPathophysiology and Treatment of Motion Sickness: ReviewSyahidatul Kautsar NajibPas encore d'évaluation
- Critical Review JurnalDocument34 pagesCritical Review JurnalSyahidatul Kautsar NajibPas encore d'évaluation
- Faktor PrognostikDocument8 pagesFaktor PrognostikSyahidatul Kautsar NajibPas encore d'évaluation
- Venugopalan2016 PDFDocument7 pagesVenugopalan2016 PDFSyahidatul Kautsar NajibPas encore d'évaluation
- Perioperative Management of The Patient With A Coronary Artery StentDocument6 pagesPerioperative Management of The Patient With A Coronary Artery StentSyahidatul Kautsar NajibPas encore d'évaluation
- 07945Document55 pages07945Tri RachmadijantoPas encore d'évaluation
- Primary Care Guidelines VertigoDocument1 pagePrimary Care Guidelines VertigoSyahidatul Kautsar NajibPas encore d'évaluation
- Assessment of Hemophilic Arthropathy by Ultrasound Where Do We StandDocument9 pagesAssessment of Hemophilic Arthropathy by Ultrasound Where Do We StandSyahidatul Kautsar NajibPas encore d'évaluation
- Liswity 2016Document14 pagesLiswity 2016Syahidatul Kautsar NajibPas encore d'évaluation
- How Should We Manage Vitamin D Deficiency Rickets?: Editorial Editorial Editorial Editorial Editorials S S S SDocument2 pagesHow Should We Manage Vitamin D Deficiency Rickets?: Editorial Editorial Editorial Editorial Editorials S S S SSyahidatul Kautsar NajibPas encore d'évaluation
- E202 Medical Assessment PDFDocument1 pageE202 Medical Assessment PDFSyahidatul Kautsar NajibPas encore d'évaluation
- Methodology Checklist 2: Randomised Controlled Trials: Pages)Document6 pagesMethodology Checklist 2: Randomised Controlled Trials: Pages)Syahidatul Kautsar NajibPas encore d'évaluation
- PNP Orders Oplan KatokDocument2 pagesPNP Orders Oplan Katokgwen furrowPas encore d'évaluation
- Helminth Revision 2Document1 pageHelminth Revision 2FarlogyPas encore d'évaluation
- MDH BrochureDocument2 pagesMDH Brochurerahms79Pas encore d'évaluation
- Hand HygieneDocument6 pagesHand HygieneCarolWestinghousePas encore d'évaluation
- Determination Actual Value Normal Value Interpretation Nursing ResponsibilitiesDocument3 pagesDetermination Actual Value Normal Value Interpretation Nursing ResponsibilitiesHzlyn GauPas encore d'évaluation
- Antitubercular DrugsDocument22 pagesAntitubercular DrugsApurba Sarker ApuPas encore d'évaluation
- Literature ReviewDocument12 pagesLiterature Reviewapi-490525267Pas encore d'évaluation
- Pathogen Safety Data Sheet: Candida AlbicansDocument1 pagePathogen Safety Data Sheet: Candida AlbicansDila AngelikaPas encore d'évaluation
- Health Data - UnicefDocument18 pagesHealth Data - UnicefEvaluation ConclavePas encore d'évaluation
- 17th-Century Plague Doctors Were The Stuff of Nightmares HowStuffWorksDocument1 page17th-Century Plague Doctors Were The Stuff of Nightmares HowStuffWorkszxcvbn1313Pas encore d'évaluation
- Field Veterinarian Notes by DR CsDocument98 pagesField Veterinarian Notes by DR CsSanjay Kumar67% (3)
- Rosenberg, Disease in HistoryDocument16 pagesRosenberg, Disease in Historyhector3nu3ezPas encore d'évaluation
- ICD Dan Kategori Pengecualian DRAFTDocument132 pagesICD Dan Kategori Pengecualian DRAFTamita sindu kusuma100% (1)
- Orkin India BrochureDocument5 pagesOrkin India BrochureSameer KulshreshthaPas encore d'évaluation
- Penyakit MeniereDocument25 pagesPenyakit MeniereMuhammad Budiman Irpan BachtiarPas encore d'évaluation
- The Role of Social Media inDocument16 pagesThe Role of Social Media inSaba TahseenPas encore d'évaluation
- Prevention and Control of Noncommunicable Diseases in The European Region A Progress Report EngDocument62 pagesPrevention and Control of Noncommunicable Diseases in The European Region A Progress Report EngQuỳDướiChânPhậtPas encore d'évaluation
- 6bi04 Exam Paper SampleDocument20 pages6bi04 Exam Paper SampleAli AkramPas encore d'évaluation
- Vol 26 1 2018 15Document10 pagesVol 26 1 2018 15sind badPas encore d'évaluation
- Operative Vaginal DeliveryDocument26 pagesOperative Vaginal DeliveryZurya UdayanaPas encore d'évaluation
- Resp Cheat SheetDocument4 pagesResp Cheat SheetHassaid33Pas encore d'évaluation
- Vaccinations Argumentative Essay - Lyla AlmoninaDocument3 pagesVaccinations Argumentative Essay - Lyla Almoninaapi-4441503820% (1)
- Wong Et Al. (2007)Document25 pagesWong Et Al. (2007)Sammer Cañesares BurgosPas encore d'évaluation
- Philippine Integrated Disease Surveillance and Response (Pidsr) "PIDSR A Bedrock of Effective Disease Surveillance" - Secretary DuqueDocument4 pagesPhilippine Integrated Disease Surveillance and Response (Pidsr) "PIDSR A Bedrock of Effective Disease Surveillance" - Secretary DuqueRoel AbricaPas encore d'évaluation
- ข้อสอบติวม 1Document32 pagesข้อสอบติวม 1Kratai TanapornPas encore d'évaluation
- Bonus Task On Politics and GovernanceDocument3 pagesBonus Task On Politics and GovernanceVictorBaguilatPas encore d'évaluation
- CD ExamsDocument3 pagesCD ExamsGilbert SalacupPas encore d'évaluation
- PNEUMONIADocument13 pagesPNEUMONIAshenecajean carajay100% (1)
- Chapter06 LectureDocument40 pagesChapter06 Lecture7104Pas encore d'évaluation
- Bronchial Asthma Pulmonary Oedema (Cardiac Asthma) : Avoid .AvoidDocument1 pageBronchial Asthma Pulmonary Oedema (Cardiac Asthma) : Avoid .AvoidjincymariyamPas encore d'évaluation