Académique Documents
Professionnel Documents
Culture Documents
Honey Hydrogel Dressing To Treat Burn Wound in Rats - A Preliminary Report
Transféré par
Farhana AnuarTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Honey Hydrogel Dressing To Treat Burn Wound in Rats - A Preliminary Report
Transféré par
Farhana AnuarDroits d'auteur :
Formats disponibles
ISSN: 1511-3701
Pertanika J. Trop. Agric. Sci. 35 (1): 67 - 74 (2012) © Universiti Putra Malaysia Press
Honey Hydrogel Dressing to Treat Burn Wound in Rats -
A Preliminary Report
Rozaini Mohd. Zohdi1, Md. Zuki Abu Bakar@Zakaria1,3*, Norimah Yusof4,
Noordin Mohamed Mustapha1, Muhammad Nazrul Hakim Somchit2
and Asnah Hasan3
1
Faculty of Veterinary Medicine,
2
Faculty of Medicine and Health Sciences,
3
Laboratory of Molecular Biomedicine, Institute of Bioscience,
Universiti Putra Malaysia, 43400 Serdang,
Selangor Darul Ehsan, Malaysia
4
Division of Agrotechnology & Bioscience,
Malaysian Nuclear Agency, Bangi, 43000 Kajang,
Selangor Darul Ehsan, Malaysia
*
E-mail: zuki@vet.upm.edu.my
ABSTRACT
Various studies have shown that honey is effective in healing burns and wounds. In this study, Malaysian
honey was incorporated into hydrogel dressing formulation using electron beam irradiation technique and
introduced as Honey Hydrogel dressing. The wound healing efficacy of Honey Hydrogel dressing on deep
partial thickness burns was monitored on the basis of gross appearances, rate of wound contraction and
histopathological changes. Deep partial thickness burns were created by applying an aluminium template
preheated to 85°C to the backs of rats for 5 s and randomly treated with Honey Hydrogel or hydrogel while
control group received no treatment. Wound appearance was photographed and the rate of wound contraction
was calculated at 7, 14, and 21 days post burn. Rats were euthanized after 21 days of treatment and skin samples
were taken for histopathological examination. The wounds treated with Honey Hydrogel dressing showed
better gross appearances and significantly (p<0.05) enhanced the rate of wound contraction as compared to
the control group at 21 days post burn. Faster epithelialization was also seen in the Honey Hydrogel treated
group as compared to the other groups, although this was not statistically significant. The results substantiate
the potential efficacy of Honey Hydrogel in accelerating burn wound healing.
Keywords: Honey, hydrogel, burn wound healing, wound contraction, rats
INTRODUCTION (Branski et al., 2009). Recently, however,
Major injuries such as in thermal burns there has been a surge of interest in the use of
resulting in extensive damage to the skin alternative therapies and natural remedy among
necessitate immediate coverage to aid repair modern societies, mainly due to its potential to
and regeneration to restore normal skin function improve healing and reduce the financial burden
(Cuttle et al., 2006). Different therapies that at the same time (Salmah & Sidik, 2005; Davis
affect burn wound repair have been proposed & Perez, 2009).
over the last few decades due to technology Honey is the nectar and saccharine
and strategic advances in the biomedical field exudation of plants gathered, modified and
*
Corresponding Author
Rozaini Mohd. Zohdi et al.
stored by the honey bee (Molan, 2000). It is Preparation of Honey Hydrogel Dressing
one of the oldest and most enduring materials Polyvinyl pyrolidone (PVP) with a molecular
to be used in managing wound (Molan, 1998). weight of 1.2 x 10 6 (Kollidon 90) and
It may be used alone or in combination with Polyethylene glycol (PEG) with molecular
other substances (Salmah & Sidik, 2005) weight of 400 were obtained from BASF,
and has been administered both topically and Ludwigshafen, Germany. Technical grade agar
systemically (Suguna et al., 1992). Much of the was supplied by Oxoid. The mixture, containing
effectiveness of honey in many of its medicinal 15% PVP (Kollidon 90), 1% Protein Free Agar
uses is attributed to the antibacterial activity and solution, and 1% PEG, was added with 6%
antioxidant properties (Molan, 1999). honey (Yusof et al., 2007). The mixture was
Topical application of Malaysian honey poured into plastic molds (5 cm in diameter;
has also been reported to be effective to treat 3-4 mm in thickness), and left to set at room
burn and wound in rats (Rozaini et al., 2005; temperature (37°C) before it was covered with
Aljady et al., 2000). However, rapid clearance polyethylene sheet and individually packed. The
from the wound site occurred as honey tends gels were cross-linked and sterilized by electron
to flow out from the wound area, making it beam at 25 kGy at Alutron Irradiation Facility,
difficult to maintain therapeutic concentration Malaysian Nuclear Agency (Model EPS-3000,
over prolonged period of time. In order to conveyer speed of 4.4m/minute, beam current of
further enhance the use of honey in wound 10mA and energy of 3MeV).
management and for easy handling, local
honey was incorporated into hydrogel dressing
formulation, cross-linked and sterilized using Study Design
irradiation technique. The present study A complete randomized design was used to
reports on the preliminary evaluation of Honey determine the efficacy of Honey Hydrogel
Hydrogel dressing in improving the outcome of dressing to treat deep partial thickness burns in
burn wound by monitoring the morphological rats. The experimental protocol was approved
changes of the burn wound tissue healing after by the Animal Care and Use Committee (ACUC)
the treatment with Honey Hydrogel. at the Faculty of Veterinary Medicine, Universiti
Putra Malaysia (UPM) (Reference No: 08R36/
MATERIALS AND METHODS July 08-Jun09).
Honey Sample
Animals
Local monofloral Apis mellifera honey from
In this study, a total of 18 male Sprague-Dawley
the floral source of Melaleuca spp. (Gelam)
rats (weight 200-300 g) were used and they were
trees was used in this study. The honey was
randomly divided into three experimental groups
supplied by the Department of Agriculture
of 6 rats each. The sample size was designed
Malaysia through Malaysian Nuclear Agency
to minimize the number of animals required,
(Nuclear Malaysia) and was irradiated with
which was still adequate to generate statistical
25 kGy gamma irradiation using radioactive
analysis. The animals were acclimatized to the
source Cobalt 60, with the dose rate of 2 kGy
laboratory conditions for one week prior to the
per hour for sterilization purposes at MINTec-
onset of experiment. The rats were individually
Sinagama, Malaysian Nuclear Agency (Model
caged and given commercial pellet and water ad
JS 8900). Dosimetry was performed using
libitum throughout the study.
ceric/cerous sulphate solution and analyzed by
potentiometrics.
68 Pertanika J. Trop. Agric. Sci. Vol. 35 (1) 2012
Honey Hydrogel Dressing to Treat Burn Wound in Rats - A Preliminary Report
Skin Preparation Treatment Protocol
Rats were anaesthetized with an intramascular Approximately 15 minutes after wound creation,
(IM) injection of ketamine (50 mg/kg) and all wounds in the treatment groups were dressed
xylazine (5 mg/kg) into the caudal thigh muscle. with Honey Hydrogel or hydrogel followed by
Under anaesthesia, the back and flank of both OpSite® film dressing (Smith and Nephew,
sides of the body were shaved. Following this Hull, England) as secondary dressing. The
procedure, rats were returned to their cages for dressings were held in place by wrapping the
24 hours to allow any oedema caused by the whole trunk with sterile gauze and plastered
shaving procedure to recede. with Leukoplast® (BSN Medical, Pinetown,
SA). Leukoplast® was applied to firmly affix
the dressings to the animal’s skin. Every 7 days,
Thermal Source
wounds were redressed with fresh hydrogel or
A method described by Kaufman et al. (1990) Honey Hydrogel, while the rats were under
was used with modification. Cylindrical anaesthesia. The secondary dressing and the
aluminium templates (2.5 cm diameter × 3 cm hydrogels were removed and the wounds were
length, a handle measuring 24 cm, and total flushed with sterile saline to remove debris and
weight 400 g) were heated in a water bath at a to clean the wound area. Sterile techniques
constant temperature of 85°C for 3 hours prior were utilized when changing the dressings to
to inflicting burn areas on the skin of the rats. minimize infection by pathogens to the wound
Five templates were heated simultaneously, used site. Once the wounds have been analyzed, fresh
alternately, and then returned to the water bath to dressings were placed on the wounds. Control
ensure maintenance of the desired temperature of group did not receive any treatment.
the template surface. There was approximately 5
minutes elapsed between each use of a template.
Assessment of the Wound
The progress of burn wound healing was
Burn Lesions
recorded at 0, 7, 14 and 21 days post-burn.
Rats were again anaesthetized with an IM All the wounds were digitally photographed
injection of ketamine (50 mg/kg) and xylazine in the presence of a standard reference ruler.
(5 mg/kg). The anaesthetized rat was positioned The wound area was measured immediately
in sternal recumbency, restrained and stretched by placing a transparent tracing paper over
on a metal stage. The location of the burn was the wound and tracing it. The tracing paper
marked between the last ribs and the horizontal was placed on a 1 mm2 graph sheet and traced
line of the sacroiliac joints. Deep partial accordingly. The squares were counted and the
thickness burn was inflicted on the dorsal part of area was recorded. The wound area was assessed
the rat between the last thoracic vertebra and the by the same blinded observer.
first sacrum by placing the heated and moistened
template at the right angles perpendicular to the
dorsum of the rat on the pre-marked location Histopathological Analysis
for 5 seconds, using an analogue stopwatch. Rats were euthanized at day 21 post-burn by
Minimal and constant pressure was applied to halothane inhalation and the skin samples were
ensure a perfect contact between the template taken for histopathological examination. The skin
surface and the skin. The shaved skin was samples were fixed in 10% formalin solution and
smoothened to ensure sufficient contact and embedded in paraffin. Tissue sections of 4-5 mm
uniform pressure over the entire lesion. thickness were cut, stained with haematoxylin
and eosin (H&E), and examined under light
microscope. Digital photomicrographs were
Pertanika J. Trop. Agric. Sci. Vol. 35 (1) 2012 69
Rozaini Mohd. Zohdi et al.
captured at representative locations using a RESULTS
digital camera attached to a Nikon Eclipse FX-
35DX microscope. Measurement of the Wound Size
On days 7 and 14 post-burn, there were no
significant differences (p>0.05) observed in
Statistical Analysis the wound area measurement between all the
Data are expressed as mean ± Standard Deviation experimental groups (Table 1). On day 21 post-
(S.D). The statistical analysis of data was burn, nevertheless, the wound area measurement
performed using two-way ANOVA using the showed a significant (p<0.05) reduction in the
SPSS® Statistical package (SPSS, Version wound size of the treated group as compared
10.0, Chicago, Illinois, USA). The effects with to the control with Honey Hydrogel dressing,
P<0.05 were considered statistically significant. showing the lowest mean of the wound size
(60.8±2.2), followed by the hydrogel treated
wound (80.8±2.6 ). In addition, the wound size
of the untreated control group was significantly
Honey Hydrogel Hydrogel Control
Fig. 1: General appearance of the wound sites in all the experimental groups at day 7
post-burn. Burned skin started to exhibit moist, intact, soft and supple yellow-brown
discoloration in the treated groups, while the control group exhibited dry, intact, light-
dark brown discolouration.
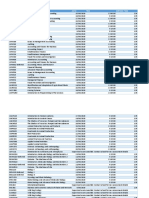
TABLE 1
Measurement of the wound sizes (mm2) of the control and the treated groups at 0, 7, 14
and 21 days post-burn. Results are shown in mean ± standard deviation (S.D). *P<0.05
compared with the control group.
Measurement of the wound area (mm2) (mean±S.D)
Groups 0 7 14 21
Control 430.4±3.26 400.4±3.2 285.6±1.3 149.6±3.6
Honey Hydrogel 427.2±1..03 388±1.33 258.8±5.4 60.8±2.2*
Honey 423.3±2.23 388.0±3.1 272.3±1.7 80.8±2.6*
70 Pertanika J. Trop. Agric. Sci. Vol. 35 (1) 2012
Honey Hydrogel Dressing to Treat Burn Wound in Rats - A Preliminary Report
(p<0.05) higher at day 21 post-burn with Histopathological Study
149.6±3.6 mm 2. No significant difference After 21 days of injury, epidermal regeneration
was observed in the treated groups at 21 days was observed in all experimental wounds.
post-burn, although there was a trend towards Histopathologic comparisons showed that on
improvement in the Honey Hydrogel treated day 21, Honey Hydrogel treated wounds resulted
group. in better re-epithelialization as compared to the
control and hydrogel treated rats. In addition,
General Appearance of the Wound the inflammatory cells were absent in both
treated wounds. In the untreated control wounds,
Gross changes in the general appearance and
though new epithelium was noted to regenerate,
the size of burn wounds were monitored at 7,
inflammatory cells particularly neutrophils
14 and 21 days post-burn by capturing digital
and macrophages were still present on the
images of each animal. Towards the end of
upper dermis. Less scab formation was seen
the first week (day 7 post-burn), the wounds in
in the wounds treated with Honey Hydrogel as
both the treated groups exhibited moist, soft and
compared to the hydrogel and untreated control
supple, yellow-brown discolouration, with red
wounds (Fig. 5).
rim around the lesion, while the control group
was covered with dry scab (Fig. 2). After 14
days, the treated groups still exhibited moist DISCUSSION
appearance with soft, yellow-brown lesions, Burn wounds lead to a loss of integrity of
while the control wounds were covered with the skin and have complex healing process.
dry, intact, dark brown-coloured scab (Fig. 3). Wound healing proceeds through an overlapping
The best healing was seen in Honey Hydrogel pattern of events consisting of inflammation,
treated wounds after 21 days of post-burn with proliferation and tissue remodelling. A number
the wounds getting considerably smaller, while of studies have indicated that honey is a potential
the control wound still exhibited dry appearance agent for wound healing, mainly due to its
with dark brown scab (Fig. 4). antibacterial, anti-inflammatory and antioxidant
Honey Hydrogel Hydrogel Control
Fig. 2: General appearances of the wound sites in all the experimental groups at day 14
of post-burn. The wound treated with Honey Hydrogel showed better healing with scab
started to slough off while hydrogel treated wound exhibited moist appearance with
soft, yellow-brown discolouration. However, the untreated control wound was covered
with dry, intact, dark brown discoloured scab.
Pertanika J. Trop. Agric. Sci. Vol. 35 (1) 2012 71
Rozaini Mohd. Zohdi et al.
Honey Hydrogel Hydrogel Control
Fig. 3: General appearance of the wound sites in all the experimental groups at day
21 post burn. Better sign of healing in the wound treated with Hydrogel Honey with
wound getting considerably smaller. However, the control wound still exhibited dry
appearance with dark brown scab.
Fig. 4: Representative micrographs of the histological sections at 21 days of post-burn
stained with H&E. Note the advanced epidermal regeneration in the wound treated
with (A) Honey Hydrogel. Marked inflammatory response still persists in (B) hydrogel
(C) control group. (E=epidermis, **=inflammatory cells; 40x mag.). Bars on the
photomicrograph represent 20 µm.
72 Pertanika J. Trop. Agric. Sci. Vol. 35 (1) 2012
Honey Hydrogel Dressing to Treat Burn Wound in Rats - A Preliminary Report
properties (Molan, 2000; Subrahmanyam, prolonged and the wounds had been followed
1998). Recent advances in radiation have longer, as there was clearly a trend to greater
resulted in the ability to incorporate honey into improvement in the Honey Hydrogel treatment
the hydrogel matrix for better handling. The compared to hydrogel. Further studies on the
present study showed that topical application of cellular and molecular mechanism of Honey
Honey Hydrogel accelerated the rate of wound Hydrogel were carried out.
healing as demonstrated by the increased rate of
wound closure and better cosmetic appearances.
ACKNOWLEDGEMENTS
Meanwhile, the histopathological evaluation
of the wound site also provided evidence that The authors wish to express their appreciation
Honey Hydrogel stimulated the healing process to Dr Jennifer Eddy from the University of
by reducing the inflammatory response and Wisconsin (USA) for her kindness in reviewing
enhancing re-epithelialization. the paper. Thanks are also due to Mrs. Asnah
One of the goals of wound therapy is to Hassan from Malaysian Nuclear Agency for her
reduce excess inflammatory responses (Cho et conscientious technical assistance.
al., 2003). Honey has been reported to reduce
inflammation when it is applied to wounds REFERENCES
(Subrahmanyam, 1998); its anti-inflammatory
Aljadi, A. M., & Kamaruddin M. Y. (2004). Evaluation
activity may be associated with the antioxidant
of the phenolic contents and antioxidant
property of honey which is responsible to capacities of two Malaysian floral honeys. Food
scavenge free radicals involved in various Chemistry, 85, 513-518.
aspects of inflammation. Aljadi and Kamaruddin
(2004) reported that honey has antioxidative and Aljadi, A. M., Kamaruddin, M. Y., Jamal, A.
M., & Mohd.Yassim, M. Y. (2000).
radical scavenging properties, which are mainly
Biochemical study on the efficacy of Malaysian
due to its flavonoids and phenolic constituents.
Honey on inflicted wounds: an animal
Re-epithelialization was also found to model. Medical Journal of Islamic Academy of
have remarkably advanced in the Honey Sciences, 13(3), 125-132.
Hydrogel treated wounds as compared to other
groups. Meanwhile, the nutrient contents Branski, L. K., Gauglitz, G. C., Herndon, D. N., &
Jeschke, M. G. (2009). A review of gene and
of honey, such as laevulose and fructose,
stem cell therapy in cutaneous wound healing.
improved the local substrate supply and helped
Burns 35, 171-180.
in promoting epithelialization and tissue growth
(Subrahmanyam, 1998). The application of Cho, M. K., Sung, M. A., Kin, D. S., Park, H.
Honey Hydrogel also kept the wounds moist and G., Jew, S. S., & Kim, S. G. (2003). 2-
it has been proven that keratinocytes migrated Oxo-3,23-isopropylidene-asiatate (AS2006A), a
wound-healing - asiatate derivative, exerts anti-
more easily over a moist wound surface than that
inflammatory effect by apoptosis of macrophages
underneath a dry scab (Winter and Scales 1963).
International Immunopharmacology, 3, 1429-
Furthermore, Honey Hydrogel dressings may be 1437.
clinically easier to use, maintaining shape and
consistency on or within the wound cavity. Corsetti, G., D’Antona, G., Dioguardi, F. S., &
Rezzani, R. (2010). Topical application of
dressing with amino acids improves cutaneous
CONCLUSION wound healing in aged rats. Acta Histochemica,
The current study has shown that Honey 112(5), 497-507.
Hydrogel is effective in healing burns, although Cuttle, L., Kempf, M., Philips, G. E., mill, J., Hayes,
not statistically more effective than hydrogel. M. T., Fraser, J. F., Wang, X. Q., & Kimble, R. M.
Nonetheless, perhaps statistical significance (2006). A porcine deep dermal partial thickness
would be reached if the study period was burn model with hypertrophic scarring. Burns,
32, 806-820.
Pertanika J. Trop. Agric. Sci. Vol. 35 (1) 2012 73
Rozaini Mohd. Zohdi et al.
Davis, S. C., & Perez, R. (2009). Cosmeceuticals and Salmah, I., Mahmood, A. A., & Sidik, K. (2005).
natural products: wound healing. Clin Dermatol, Synergistic effects of alcoholic extract of sweet
27(5), 502-506 basil (Ocimum basilicum L.) leaves and honey on
cutaneous wound healing in rats. International
Kaufman, T., Lusthaus, S. N., Sagher, U., & Wexler,
Journal of Molecular Medicine and Advance
M. R. (1990). Deep partial skin thickness burns: a
Sciences, 1, 220-224.
reproducible animal model to study burn wound
healing, Burns, 16(1), 13-16. Subrahmanyam, M. (1998). A prospective randomized
clinical and histological study of superficial
Molan, P. C. (1998). The evidence for honey
burn wound healing with honey and silver
promoting wound healing. Primary intention
sulphadiazine. Burns, 24, 157-161.
(The Australian Journal of wound management),
6, 148-158. Suguna, L., Chandrakasan, G. and Thomas Joseph,
K. (1992). Influence of honey on collagen
Molan, P. C. (1999). The role of honey in the
metabolism during wound healing in rats.
management of wounds. Journal of Wound Care.
Journal of Clinical Biochemical Nutrition, 13,
8, 423-426.
7-12.
Molan, P. C. (2000). Establishing honey as
Yusof, N., Ainul Hafiza, A. H., Zohdi, R. M., &
a recognized medicine. The Journal of the
Bakar, M. Z. A. Development of honey hydrogel
American Apitherapy Society, 7, 7-9.
dressing for enhanced wound healing. Radiation
Rozaini, M. Z, Zuki, A. B. Z., Noordin, M. M., Physics and Chemistry, 76(11-12), 1767-1770.
Norimah, Y., & Nazrul Hakim, A. (2005).
Macroscopic evaluation of burn wounds healing
progress treated with different types of honey.
Pakistan Journal of Biological science, 8(5),
672-678.
74 Pertanika J. Trop. Agric. Sci. Vol. 35 (1) 2012
Vous aimerez peut-être aussi
- The Paper Doctor TEXTODocument101 pagesThe Paper Doctor TEXTOondasdeforma67% (3)
- Employment ContractDocument3 pagesEmployment ContractHASRET75% (4)
- Therapy PolarityDocument37 pagesTherapy PolarityNaina RavahitrarivoPas encore d'évaluation
- Contract of Employment GuideDocument8 pagesContract of Employment Guidesartika hutabaratPas encore d'évaluation
- Contract of Employment GuideDocument8 pagesContract of Employment Guidesartika hutabaratPas encore d'évaluation
- Keller & Schoenfeld (1950) - Principles of PsychologyDocument456 pagesKeller & Schoenfeld (1950) - Principles of PsychologyPablo StuartPas encore d'évaluation
- Demand Letter and Employment LetterDocument6 pagesDemand Letter and Employment LetterFarhana AnuarPas encore d'évaluation
- Somatic Embryogenesis for Micropropagation of Coconut (Cocos nucifera L.)D'EverandSomatic Embryogenesis for Micropropagation of Coconut (Cocos nucifera L.)Pas encore d'évaluation
- TVET 4.0 Framework 2018 - 2025Document50 pagesTVET 4.0 Framework 2018 - 2025Farhana Anuar100% (4)
- TVET 4.0 Framework 2018 - 2025Document50 pagesTVET 4.0 Framework 2018 - 2025Farhana Anuar100% (4)
- Q2 DLL SCIENCE COMPLETE QUARTER 2 Inkay PeraltaDocument24 pagesQ2 DLL SCIENCE COMPLETE QUARTER 2 Inkay PeraltaGlen GorgonioPas encore d'évaluation
- 03 N.A. NorfarizanDocument7 pages03 N.A. NorfarizanikameilianajohanPas encore d'évaluation
- Sea cucumber hydrogel treats burn wounds in ratsDocument8 pagesSea cucumber hydrogel treats burn wounds in ratsandi adrina amandaPas encore d'évaluation
- Zahraetal 3Document9 pagesZahraetal 3fuady faridPas encore d'évaluation
- Available Online Through: WWW - Jpronline.infoDocument2 pagesAvailable Online Through: WWW - Jpronline.infoNatarajan KPas encore d'évaluation
- Evaluation of Antihyperlipidemic, Anti-Inflammatory, and Analgesic Activities of Eurycoma Longifolia in Animal ModelsDocument4 pagesEvaluation of Antihyperlipidemic, Anti-Inflammatory, and Analgesic Activities of Eurycoma Longifolia in Animal Modelsmendal sciPas encore d'évaluation
- Immunomodulatory Properties of Ethanol Extract Of: Canarium Ovatum (Burseraceae) PulpDocument5 pagesImmunomodulatory Properties of Ethanol Extract Of: Canarium Ovatum (Burseraceae) PulpFranco TankPas encore d'évaluation
- Induksi AlergiDocument5 pagesInduksi AlergiBilly Shan LastKagerooboroPas encore d'évaluation
- A New Sterilization and Inoculation Method in Silage ResearchDocument6 pagesA New Sterilization and Inoculation Method in Silage ResearchWtf MomentsPas encore d'évaluation
- Azadirachtin Effects on Indian Meal MothDocument5 pagesAzadirachtin Effects on Indian Meal MothVitor AfonsoPas encore d'évaluation
- Evaluation of Gastroprotective Effects of The Ethanolic Extract of PeperomiaDocument9 pagesEvaluation of Gastroprotective Effects of The Ethanolic Extract of PeperomiaVinaNazaliaPas encore d'évaluation
- Amelioration of Carbon Tetrachloride Induced Hepatic Damage by Methanolic Rhizome Extract of Atropa Accuminata in Wistar RatsDocument7 pagesAmelioration of Carbon Tetrachloride Induced Hepatic Damage by Methanolic Rhizome Extract of Atropa Accuminata in Wistar RatsAlbeena NisarPas encore d'évaluation
- Use of Spray-Cooling Technology For Development of Micro Encapsulated Capsicum Oleoresin For The Growing Pig As An Alternative To In-Feed Antibiotics - A Study of Release Using in Vitro ModelsDocument14 pagesUse of Spray-Cooling Technology For Development of Micro Encapsulated Capsicum Oleoresin For The Growing Pig As An Alternative To In-Feed Antibiotics - A Study of Release Using in Vitro ModelssdhanupriyaPas encore d'évaluation
- Calendula 8Document7 pagesCalendula 8Zeila OmarPas encore d'évaluation
- International Journal of Pharma and Bio Sciences: Pharmacology Research ArticleDocument10 pagesInternational Journal of Pharma and Bio Sciences: Pharmacology Research ArticleRivanFirdausPas encore d'évaluation
- B - 06 - English JournalDocument3 pagesB - 06 - English JournalTazkia AuditaPas encore d'évaluation
- Food Chemistry: Xiaoyong Wang, Yan Jiang, Yu-Wen Wang, Mou-Tuan Huang, Chi-Tang Ho, Qingrong HuangDocument6 pagesFood Chemistry: Xiaoyong Wang, Yan Jiang, Yu-Wen Wang, Mou-Tuan Huang, Chi-Tang Ho, Qingrong HuangMichelle WangPas encore d'évaluation
- MMR 15 03 1109Document8 pagesMMR 15 03 1109SoniaPas encore d'évaluation
- 1 PDFDocument5 pages1 PDFKhairul AlvaroPas encore d'évaluation
- Azitromicina y PiodermaDocument5 pagesAzitromicina y PiodermaCarlos Gerardo Castillo SosaPas encore d'évaluation
- 1 s2.0 S0093691X14002374 MainDocument6 pages1 s2.0 S0093691X14002374 MainElvis Jano Aviles MendozaPas encore d'évaluation
- Chemopreventive potential of Cassia fistula bark against skin cancerDocument4 pagesChemopreventive potential of Cassia fistula bark against skin cancerlinubinoiPas encore d'évaluation
- A Comparative Pharmacokinetic Analysis of Oral andDocument9 pagesA Comparative Pharmacokinetic Analysis of Oral andcandyPas encore d'évaluation
- Tungadi - 2018 - Transdermal Delivery of Snakehead Fish (Ophiocephalus Striatus) Nanoemulgel Containing Hydrophobic Powder For Burn WoundDocument12 pagesTungadi - 2018 - Transdermal Delivery of Snakehead Fish (Ophiocephalus Striatus) Nanoemulgel Containing Hydrophobic Powder For Burn Woundsibon M amrilPas encore d'évaluation
- Article1379775512 - Oluyemi Et AlDocument3 pagesArticle1379775512 - Oluyemi Et AlredityoPas encore d'évaluation
- Evaluation of Effectiveness of Honey-Based Alginate Hydrogel On Wound Healing in Rat ModelDocument5 pagesEvaluation of Effectiveness of Honey-Based Alginate Hydrogel On Wound Healing in Rat ModelAlief AkbarPas encore d'évaluation
- Effects of Methanol Leaf Extract of Dryopteris FilDocument4 pagesEffects of Methanol Leaf Extract of Dryopteris Filmobopubg7Pas encore d'évaluation
- Available Online Through: WWW - Jpronline.infoDocument7 pagesAvailable Online Through: WWW - Jpronline.infosafiraPas encore d'évaluation
- Investigation of Immunomodulatory Potential of Methanolic and Hexane Extract of Musa Acuminate Peel (Plantain) ExtractsDocument6 pagesInvestigation of Immunomodulatory Potential of Methanolic and Hexane Extract of Musa Acuminate Peel (Plantain) ExtractsDelyana Fitria DewiPas encore d'évaluation
- Research Paper: Indian J Pharmacol April 2005 Vol 37 Issue 2 103-110Document8 pagesResearch Paper: Indian J Pharmacol April 2005 Vol 37 Issue 2 103-110Prasanna BabuPas encore d'évaluation
- DNA Integrity, Acrosomal Integrity and Semen Characteristics Following Supplementation of Some Additives To Chilled and Frozen Rabbit SemenDocument7 pagesDNA Integrity, Acrosomal Integrity and Semen Characteristics Following Supplementation of Some Additives To Chilled and Frozen Rabbit SemenNa KhanPas encore d'évaluation
- Cicatrización Con Clavo en ConejosDocument12 pagesCicatrización Con Clavo en ConejosLoreto Rojas PeraltaPas encore d'évaluation
- Rivea HypocrateriformisDocument3 pagesRivea HypocrateriformisugoPas encore d'évaluation
- Evaluation of Anxiolytic Activity of Methanolic Extract of Sapindus Mukorossi Gaertn in MiceDocument8 pagesEvaluation of Anxiolytic Activity of Methanolic Extract of Sapindus Mukorossi Gaertn in MiceamritaryaaligarghPas encore d'évaluation
- BMC Complementary and Alternative Medicine: Antiinflammatory Evaluation of Leaves of Plumeria AcuminataDocument6 pagesBMC Complementary and Alternative Medicine: Antiinflammatory Evaluation of Leaves of Plumeria AcuminatadianapriyaniPas encore d'évaluation
- Liposomal Gel PropranololDocument7 pagesLiposomal Gel PropranololsacahePas encore d'évaluation
- Antibacterial, Cytotoxic and Neuropharmacological Activities of Cerbera odollam SeedsDocument6 pagesAntibacterial, Cytotoxic and Neuropharmacological Activities of Cerbera odollam SeedsMuhammad NaseerPas encore d'évaluation
- Nigella Sativa and Cimetidine Against AcetylsalicylicDocument6 pagesNigella Sativa and Cimetidine Against AcetylsalicylicTeguh D. WicaksonoPas encore d'évaluation
- Safety and Toxicological Evaluation of A Flap inDocument8 pagesSafety and Toxicological Evaluation of A Flap inamrutharajeshPas encore d'évaluation
- Comparison of Sugar Content, Mineral Elements and Antioxidant Properties of Heterotrigona Itama Honey From Suburban Forest in MalaysiaDocument9 pagesComparison of Sugar Content, Mineral Elements and Antioxidant Properties of Heterotrigona Itama Honey From Suburban Forest in Malaysiaasel ppPas encore d'évaluation
- Nanopartikel AseklofenakDocument9 pagesNanopartikel AseklofenakReski WahyuPas encore d'évaluation
- Revised Ph. BiologyDocument11 pagesRevised Ph. BiologyDibya Sundar PandaPas encore d'évaluation
- Hypoglycaemic Activity of Aerial Parts of Argemone Mexicana L. in Experimental Rat ModelsDocument9 pagesHypoglycaemic Activity of Aerial Parts of Argemone Mexicana L. in Experimental Rat ModelsSachin DatkhilePas encore d'évaluation
- Antioksidan Ic50Document13 pagesAntioksidan Ic50Prapti ChantiquePas encore d'évaluation
- Protective Effects of Saffron (Crocus Sativus Linn.) On Genotoxins-Induced Oxidative Stress in Swiss Albino MiceDocument4 pagesProtective Effects of Saffron (Crocus Sativus Linn.) On Genotoxins-Induced Oxidative Stress in Swiss Albino MiceArlaaPas encore d'évaluation
- Research Article Artemisia Kopetdaghensis: Evaluation of Cytotoxicity and Antifertility Effect ofDocument6 pagesResearch Article Artemisia Kopetdaghensis: Evaluation of Cytotoxicity and Antifertility Effect ofLinguumPas encore d'évaluation
- Wound Healing Potential of Aqueous Crude Extract of Stevia Rebaudiana in MiceDocument7 pagesWound Healing Potential of Aqueous Crude Extract of Stevia Rebaudiana in Micepankaj dagurPas encore d'évaluation
- Tocolytic and Toxic Activity of Papaya Seed Extract On Isolated Rat Uterus j.lfs.2003.06.035Document12 pagesTocolytic and Toxic Activity of Papaya Seed Extract On Isolated Rat Uterus j.lfs.2003.06.035proluvieslacusPas encore d'évaluation
- N Oculata in Choco SpreadDocument9 pagesN Oculata in Choco SpreadBabuskin SrinivasanPas encore d'évaluation
- Jurnal Falcourtia RukamDocument6 pagesJurnal Falcourtia RukamNorsarida AryaniPas encore d'évaluation
- Moringa LeavesDocument4 pagesMoringa LeavesKike PalaciosPas encore d'évaluation
- BH Chapter 5 Mice-IMI-Model (1) .EditedDocument16 pagesBH Chapter 5 Mice-IMI-Model (1) .EditedGifted MaggiePas encore d'évaluation
- Wound Healing1Document8 pagesWound Healing1basu68Pas encore d'évaluation
- Antioxidant Activity of Pink-Flesh Guava (Psidium Guajava L.) : Effect of Extraction Techniques and SolventsDocument8 pagesAntioxidant Activity of Pink-Flesh Guava (Psidium Guajava L.) : Effect of Extraction Techniques and SolventsVy Huynh Thi HaPas encore d'évaluation
- 55 110 1 SMDocument6 pages55 110 1 SMBadlina Fitrianisa YulianingrumPas encore d'évaluation
- Asian Elephant AnesthesiaDocument14 pagesAsian Elephant AnesthesiaJulissaPas encore d'évaluation
- Curcuma Anti KankerDocument4 pagesCurcuma Anti KankerTrisnawati AmaliaPas encore d'évaluation
- Carthamus Oxycantha Hepatoprotective EffectsDocument7 pagesCarthamus Oxycantha Hepatoprotective EffectsJavaria IkramPas encore d'évaluation
- Investigation of Microalgae For High Lipid Content Using Palm Oil Mill Effluent (Pome) As Carbon SourceDocument5 pagesInvestigation of Microalgae For High Lipid Content Using Palm Oil Mill Effluent (Pome) As Carbon SourceAmalinaArouraPas encore d'évaluation
- IJPhS 73 303Document4 pagesIJPhS 73 303Sunita GiriPas encore d'évaluation
- Hands On SessionDocument18 pagesHands On SessionFarhana AnuarPas encore d'évaluation
- Borang Progress Report 2013Document3 pagesBorang Progress Report 2013fsuhariPas encore d'évaluation
- Ijo 55 3 629 PDFDocument16 pagesIjo 55 3 629 PDFFarhana AnuarPas encore d'évaluation
- Hands On SessionDocument18 pagesHands On SessionFarhana AnuarPas encore d'évaluation
- MN Thesis Stream Progress ReportDocument4 pagesMN Thesis Stream Progress ReportFarhana AnuarPas encore d'évaluation
- Bertin - ICLS APS 004Document5 pagesBertin - ICLS APS 004Farhana AnuarPas encore d'évaluation
- Process Flow For Graduate StudiesDocument2 pagesProcess Flow For Graduate StudiesFarhana AnuarPas encore d'évaluation
- Genes 10 00479 v2Document14 pagesGenes 10 00479 v2Farhana AnuarPas encore d'évaluation
- 4 RTDocument3 pages4 RTFarhana AnuarPas encore d'évaluation
- Typodermic Fonts Inc. End User License Agreement (02-2014) : 1. InstallationDocument2 pagesTypodermic Fonts Inc. End User License Agreement (02-2014) : 1. InstallationOdóbùnmí AworeniPas encore d'évaluation
- Measuring Cancer Drug Sensitivity and Resistance in Cultured Cells: Cancer Drug Sensitivity and Resistance in CellsDocument21 pagesMeasuring Cancer Drug Sensitivity and Resistance in Cultured Cells: Cancer Drug Sensitivity and Resistance in CellsFarhana AnuarPas encore d'évaluation
- 安装说明Document1 page安装说明Farhana AnuarPas encore d'évaluation
- Prevalence of Job StressDocument4 pagesPrevalence of Job StressFarhana AnuarPas encore d'évaluation
- Digital Methods and Remote Sensing in ArDocument98 pagesDigital Methods and Remote Sensing in ArFarhana AnuarPas encore d'évaluation
- Accepted ManuscriptDocument33 pagesAccepted ManuscriptFarhana AnuarPas encore d'évaluation
- Microsoft Word - MediaRecipesForMCF10ACellsDocument1 pageMicrosoft Word - MediaRecipesForMCF10ACellsFarhana AnuarPas encore d'évaluation
- XTT Alamarbluemakalesi ToxicologyDocument6 pagesXTT Alamarbluemakalesi ToxicologyFarhana AnuarPas encore d'évaluation
- Digital Methods and Remote Sensing in ArDocument98 pagesDigital Methods and Remote Sensing in ArFarhana AnuarPas encore d'évaluation
- Euthanasia: A Muslim'S PerspectiveDocument13 pagesEuthanasia: A Muslim'S PerspectiveFarhana AnuarPas encore d'évaluation
- Digital Methods and Remote Sensing in Ar PDFDocument18 pagesDigital Methods and Remote Sensing in Ar PDFFarhana AnuarPas encore d'évaluation
- Digital Methods and Remote Sensing in ArDocument98 pagesDigital Methods and Remote Sensing in ArFarhana AnuarPas encore d'évaluation
- YouthCentral CoverLetter WorkExperience March15Document3 pagesYouthCentral CoverLetter WorkExperience March15lphounePas encore d'évaluation
- 2 CreamDocument1 page2 CreamFarhana AnuarPas encore d'évaluation
- Writing Good Abstracts APA FINAL NoFooter F10Document1 pageWriting Good Abstracts APA FINAL NoFooter F10Farhana AnuarPas encore d'évaluation
- Cbjescpl 02Document10 pagesCbjescpl 02Riya SharmaPas encore d'évaluation
- Activity 5 Type of Root SystemDocument2 pagesActivity 5 Type of Root SystemPreiy Julian De GuiaPas encore d'évaluation
- Physical Agents Used in The Management of Chronic Pain by Physical TherapistsDocument31 pagesPhysical Agents Used in The Management of Chronic Pain by Physical TherapistsMárcia MatosPas encore d'évaluation
- Snakes of The World A Supplement by Boundy Jeff WallachDocument284 pagesSnakes of The World A Supplement by Boundy Jeff WallachRoullienPas encore d'évaluation
- Manchester Ship Canal - Strategic Review of Fish PopulationsDocument139 pagesManchester Ship Canal - Strategic Review of Fish PopulationsSamyuktha PillaiPas encore d'évaluation
- Beckman ProtocolDocument34 pagesBeckman ProtocolIonut NeagaPas encore d'évaluation
- Facial Esthetics in FPDDocument8 pagesFacial Esthetics in FPDrayavarapu sunilPas encore d'évaluation
- Trimester 1 2020 Exam TimetableDocument11 pagesTrimester 1 2020 Exam TimetableBagus ArdiansyahPas encore d'évaluation
- GEN3051 Lecture 1: Human Genes and Human Genetic DisordersDocument5 pagesGEN3051 Lecture 1: Human Genes and Human Genetic DisordersAlessander Leyendecker JuniorPas encore d'évaluation
- A Conversation Explaining BiomimicryDocument6 pagesA Conversation Explaining Biomimicryapi-3703075100% (2)
- Kabole 2023Document12 pagesKabole 2023Omoding EmmanuelPas encore d'évaluation
- Clinical - Biochemistry 1Document45 pagesClinical - Biochemistry 1mqbljbr529Pas encore d'évaluation
- Frances Boa Methodology QuestionDocument39 pagesFrances Boa Methodology Questionmonday125Pas encore d'évaluation
- Dna ForensicsDocument40 pagesDna ForensicsMaybel NievaPas encore d'évaluation
- 3 5 18 950 PDFDocument3 pages3 5 18 950 PDFBang AthanPas encore d'évaluation
- Kung Et Al. (2018)Document14 pagesKung Et Al. (2018)Henry Daniel Ruiz AlbaPas encore d'évaluation
- Vitamin D in Hashimoto's Thyroiditis and Its Relationship With Thyroid Function and Inflammatory StatusDocument9 pagesVitamin D in Hashimoto's Thyroiditis and Its Relationship With Thyroid Function and Inflammatory StatusMedicina UNIDEP T3Pas encore d'évaluation
- Anisakis SPDocument15 pagesAnisakis SPLuis AngelPas encore d'évaluation
- Command Terms in IB BiologyDocument68 pagesCommand Terms in IB BiologyormattPas encore d'évaluation
- Science Raft-1Document5 pagesScience Raft-1api-271240315Pas encore d'évaluation
- SP4 Memes - UmaliDocument6 pagesSP4 Memes - UmaliSheryl Anne Benigno UmaliPas encore d'évaluation
- American Journal of Agricultural EconomicsDocument3 pagesAmerican Journal of Agricultural EconomicsRey DoankPas encore d'évaluation
- Evalution ReportDocument44 pagesEvalution ReportkamilPas encore d'évaluation
- Applied Malacology: A Different Approach To Teaching A Traditional TopicDocument16 pagesApplied Malacology: A Different Approach To Teaching A Traditional TopicGustavo DarrigranPas encore d'évaluation
- What Is The Lifespan of A Glofish - Google SearchDocument1 pageWhat Is The Lifespan of A Glofish - Google SearchaddisoncmoorePas encore d'évaluation
- Sticky Trap Monitoring of Insect Pests: Steve H. DreistadtDocument8 pagesSticky Trap Monitoring of Insect Pests: Steve H. DreistadtBryan AbarcaPas encore d'évaluation