Académique Documents
Professionnel Documents
Culture Documents
Trans
Transféré par
Zllison Mae Teodoro MangabatTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Trans
Transféré par
Zllison Mae Teodoro MangabatDroits d'auteur :
Formats disponibles
(LECTURE)
2A PARASITOLOGY
P-04 Dr. Julius Capili | March 03, 2019
BABESIA
Maltese-cross formation Sheaters Flotation Gold standard for
often mistaken as Plasmodium falciparum technique identifying isospora
but differs in: Mod.Acid Fast Stain used to stain the
lacks pigments in the cytoplasm isopora
lacks of growing trophozoites
(sporozoites or merozoites) 2. Cryptosporidium parvum
the vector are Ticks--- Ixodes parasite that causes intestinal infection
scapularis among AIDS patients
Animals (ex: deer) is the usual definitive associated with watery, frothy, diarrhea
host with oocyst shed in feces
Man (incidental Host) is infected by the bite Detection: Sheath’s Sugar flotation,
of the intermediate host (Tick----IXODES) Modified Acid Fast Stain
and blood transfusion.
Causes: NOTE: ISOSPORA AND CRYPTOSPORIDIUM both
o Headache and fever causes Gastroenteritis, intestinal malabsorption
o Hemolytic anemia with among AIDS patient but MOST COMMON is
hemoglobinuria in immunocompetent Crystosporidium.
host
o Red water fever on cattles (can also 3. Toxoplasma gondii
become a definitive host) Associated with CNS disorder
Definitive Host: CAT
COCCIDIA
Intermediate host: MAN (source of
-literally refer to sporozoans which are infecting
trophozoites that has crescent
HIV/ AIDS patients
appearance in tissues)
o Schizogony (asexual) in variety of
nucleated cells of the definitive host.
Lifecycle:
o Sporogony (sexual) in intestinal
1. Toxoplasma divide in tissues of man as
mucosa of the definitive host----
TACHYZOITES (actively dividing
infective oocyst excreted in feces.
trophozoites),
*INFECTIVE STAGE: Oocyst
2. Pseudocysts (group of BRADYZOITES) are
also formed
Babesia vs Malaria vs Coccidia 3. Females who acquire infection during
Babesia: Man is Incidental host pregnancy may transit infection to embryo
Malaria: Man is Intermidiate host resulting in fetal death, mental retardation in
Coccidia: Man maybe Definitive or newborn or blindness in later life.
Intermediate (depends on the lifecycle)
Laboratory Diagnosis
1. Isospora belli a) Sabin fieldman dye test: Methylene blue
Definitive host: MAN staining of Tachyzoites inhibited by prior
Intermediate host: PIGS/CATTLES addition of patient serum containing
Transmission: ingestion of sporulated oocyst antibodies to toxoplasma
in contaminated food and water. Positive result: Colorless organisms
Lab dx: Stool exam and Modified Acid Fast over a blue background
Stain - Tachyzoites resist the dye.
1 AYANG ANG, CASTRO, LABUGUEN, VALEROZO
P-04
**Principle: INHIBITION MECHANISM (trophozoites a. Wheatley’s trichrome stain
don’t absorb dye) b. Iron Hematoxylin stain
c. Modified Acid fast stains
(Cryptosporidium, cyclospora, Isospora)
b) IFA
Positive result: Fluorescence (emission of C. Concentration methods for protozoa cysts and
light) helminthes eggs and larva
Ex of Dye used: 1. Sedimentation techniques
Phycocyanin RED a. Acid ether concentration
Texas Red fluorescence b. formalin ether concentration
FITC Green Gold -dissolves debris, lipid and CHOs
fluorescence 2. Flotation technique
a. Brine flotation (NaCl)
c) TORCH Test b. Zinc sulfate centrifugal flotation techniques
Toxoplasma, Rubella, CMV, Herpes (specific gravity of 1.18)
c. Sheathers sugar flotation
LABORATORY METHOS -best for Cryptosporidium
A. Examination of blood
1. Detects agents of malaria, babesiosis, D. Culture methods for protozoa
trypanosomiasis, leishmanasis and 1. Culture media for intestinal amoeba
filariasis a. Boeck Dorbohlav’s Diphasic medium
2. Include thick and thin blood films (modified by Dobell and Laidlaw)
3. Concentration techniques (Quantitative b.Las’s Casein Hydrolysate serum medium
Buffy Coat/QBC) c. Balamuth’s Aqueous Egg Yolk infusion
a. Preparation of buffy coat d. Cleveland Colliers medium
smears (L. donovani, e. Feinberg medium
trypanosomes, microfilaria) f. Whittington medium
b. Knott’s concentration g. Modified Diamond’s medium
membrane filtration h. PYGC medium with antibiotics
(detects microfilaria) i. Nove McNeal Nicolle (NNN) medium for
c. Fluorochrome acridine Teismania and Trypanosoma
orange in microhematocrit j. Hockmeyer;s medium- visceral leishmania
centrifuge format (QBC k.Weinman’s medium-Trypanosoma
blood parasite detection gambiense
method) l.Toboes Diphasic medium- hemoflagellates
B. Examination of Fecal Specimen E. Additional techniques for examination of
1. Specimens maybe submitted to the ecterice parasites
laboratory either fresh or in appropriate a. Cellulose tape technique for pinworm
preservative (Scoth tape method)
2. Stool fixatives: b. Egg studies
a. 10% formalin 1. direct smear method of Beaver
b. Scaudinn’s solution 2. Stoll dilution egg count
c. Polyvinyl alcohol 3. Kato Thick smear
d. Merthiolate-Iodine formalin (MIF) c. Nematode culture and recovery techniques
e. Sodium acetate formlain (SAF) 1. Harda-Mori filter paper culture
3. Direct Wet mount 2. Baermann funnel technique
a. Saline mount (strongloides)
b. Iodine mount
4. Permanent stains
2 AYANG ANG, CASTRO, LABUGUEN, VALEROZO
P-04
F. Examination of other specimens 2. PVA (Polyvinyl Alcohol-fixative)
1. Vaginal and urethral discharges, prostatice -preserves tropozoites and cysts for
sections and urine subsequent permanent staining
2. skin biopsy (Onchorera, Mansonella) , muscle 3. MIF (Methiolate-iodine-formaldehyde)
biopsy (Trichinella) -preserves all stages for wet mount
examinations
COLLECTION OF SPECIMENS 4. PAF (Phenol-alcohol-formaldehyde)
-preserves all stages for wet mount
Containers examinations
Contaminants and Drugs Permanent stains cannot be made from feces
Size of Specimen preserved in MIF and PAF solutions;
Age of Specimen therefore, a portion of the specimen should
1. Size also be preserved in PVA-fixative
-entire fecal passage, if possible, or at least 20 Fecal specimens: normally passes fecal
to 30 grams or about 1 to 2 tablespoonful specimens, 2-3 days intervals
2. Contaminants or Interfering substances
a. Urine- destroys protozoan trophozoites Container: plastic cups; defecate directly on
b. Water-destroys protozoan trophozoites the cup or in a cardboard (karton) to avoid
c. Dirt-interferes with examinations; may contamination
introduce free-living organisms that Conduct stool examination before prescribing
might be confused with parasites drugs especially antibiotics
Label of the specimen (eg name of patient)
Oily Interfere with examination; may should be placed on the side of the cup, not on
laxatives cause inaacurate or ineffective the top (takip)
performance of techniques
Bismuth Crystals in feces which interfere NEMATODES
with examinations - referred as ASCALMINTHES
Barium Abrasive action, which may destroy - they are round and embossed
organisms; interferes with
- they are huge parasites and multicellular
examinations
Kaolin Abrasive action may affect
compounds appearance of organisms. Wait for Characteristics:
7-10 days after these compounds 1. System of the parasite
have been given before collecting
specimens for parasitologic A. Integumentary system
examinations - known as SYNCYTIUM / CUTICLE
Antibiotics Cause decrease in numbers of Composed of 3 muscle bands/layers:
protozoa in intestinal tract; wait 1 to 1. INNERMOST- longitudinal
2 weeks after termination of therapy 2. MIDDLE LAYER- oblique
before collecting specimens 3. OUTER LAYER- circular
3. Age Movement:
- unpreserved specimens should reach the Adult parasite - Figure of 8
laboratory within 1-2 hours after passage Larva- Purposely motion (they can go anywhere)
-time and date of passage should be recorded
PRESERVATIVES B. Nervous System
1. Formalin (5-10%) - has a nerve center referred to as the ganglia
-preserves eggs, larvae and cysts for wet seen in the esophageal area or the CIRCUM
mount examinations ESOHAGEAL RING
3 AYANG ANG, CASTRO, LABUGUEN, VALEROZO
P-04
Difference between Male and Female
MALE FEMALE
Curved tails Pointed tails
Smaller Larger - for procreation
Male Reproductive Organ
Basic Unit structure: Gubernaculum
- seen at the posterior most portion
Parts of gubernaculum
1. Bursa – lobed part of gubernaculum
2. Bursal rays – inside the bursa
- nerve center transmit nerve impulses or a. Bipartile: 2 lobes (ex. Necator
senses to the different parts of the parasites americanus)
through TRANSVERSE COMMISURE b. Tripartile: 3 lobes (ex. Ancylostoma
- Parasite would access into one organ referred spp.)
to as CHEMORECEPTOR 3. Cleft or the cleavage
Caudal Chemoreceptors: Phasmids 4. Spicule- most important because it is the
Other Chemoreceptors: Aphasmids penis of the parasite
- It is the copulatory organ
C. Circulatory System - For nematodes it contains one spicule and
- It is considered to be absent, the fluid inside other parasite contain multiple spicules
the parasite works the function of the blood - Some of the spicules are barbed or fused (ex.
N. americanus), Ancylostoma is plenty or
D. Digestive System unfused
- known as a Complete system:
Mouth or Buccal capsule Female Reproductive Organ
Esophagus Organ: Genital primordium/ Gynecophoral canal
Alimentary canal - Found/ along one side of the parasite,
Anus (female parasite)/Cloaca (male probably ¼ to ½ anterior to the body
parasite)
- Referring to the mouth or the buccal capsule Sexual position: inverted Y position
of the parasite it is accessorized.
Dorsal Cutting Plates- ex. Necator The central dogma of the life cycle of
americanus nematodes:
Teeth- ex. Ancylostoma spp.
1. Ova
3 lips (trilobe)- ex. Ascaris
2. Larva
Papilated lips- ex. Trichuris
3. Adult
E. Reproductive System
- Males separate from Female Ova Stage
Ex. Ascaris lumbricoides male and Ascaris -Ova of the parasites would have 3 types
lumbricoides female 1. Unfertile ova- cannot proceed to the next
developmental life cycle stages.
2. Mature ova- potential ova, that needs to get to
the embryonated stage.
4 AYANG ANG, CASTRO, LABUGUEN, VALEROZO
P-04
3. Embryonated ova- INFECTIVE stage. Causes Embryonation requirements:
infection
1. Soil
Larva stage: - Ascaris
1. Rhabditiform larva - Trichuris
- early stage. - Hookworm
- Feeding/ vegetative stage 2. Water
- Open mouth - Capillaria philipinensis
- Shorter but broader 3. None
2. Filariform Larva - Enterobius vermicularis
- Non-feeding/ non-vegetative stage
When the infective stage is the filariform larva, the
- Closed mouth
mode of transmission would be skin penetration.
- INFECTIVE stage(e.g. hookworms)
- Slender but longer If the infective stage is the embryonated ova, MOT
would be ingestion.
Larval stage of development will always be the same
among the nematodes 2 CLASSES OF NEMATODES
Adult Stage: 1. Aphasmids/amphids/adenophorea
- Stage where parasites can be sexually - lack caudal chemoreceptors but have
differentiated. cephalic chemoreceptors.
- Male parasites are smaller and curved - Trichinella spiralis small
tails while females are bigger and have intestines
pointed tails. - Capillaria
- Diocophyma renale- kidneys
Classification Female adults according to ova laid: - Trichuris trichuria- large intestines
1. Oviparous- lay immature ova 2. Phasmids/Sercentea
2. Oviviparous- lay readily infective ova (e.g. - Hookworms
Enterobius vermicularis) - Ascaris small intestines
3. Viviparous/Larviparous- doesn’t lay ova, they - Stongyloides
lay larva. - Enterobius vermicularis- large
intestines
Classification Female adults depending on the - Filarial worms- tissues
uterine orientation:
1. Single- 1 ovary and oviduct(e.g. Trichuris
trichuria and Trichinella spiralis)
2. Bifurcated 2 pairs of ovary and oviduct (e.g.
Hookworms, Ascaris, Enterobius)
Molting
transition period of the larva going to adult stage.
Ascaris lumbricoides- 3 moltings from
rhabditiform to filariform and 1 molting from
filariform to adult.
5 AYANG ANG, CASTRO, LABUGUEN, VALEROZO
P-04
6 AYANG ANG, CASTRO, LABUGUEN, VALEROZO
Vous aimerez peut-être aussi
- Integrated Science NotesDocument115 pagesIntegrated Science Notesserene munga100% (1)
- Threadfins of The World (Family Polynemidae)Document8 pagesThreadfins of The World (Family Polynemidae)cavrisPas encore d'évaluation
- CSEC Biology June 2012 P2Document17 pagesCSEC Biology June 2012 P2Joy BoehmerPas encore d'évaluation
- Introduction To ParasitologyDocument79 pagesIntroduction To ParasitologyLeeShauran100% (7)
- Parasitology Exam (HELMINTHS)Document7 pagesParasitology Exam (HELMINTHS)Tony DawaPas encore d'évaluation
- Balantidium Coli: B. Coli - Is The Only Ciliate Known To Parasitize HumansDocument2 pagesBalantidium Coli: B. Coli - Is The Only Ciliate Known To Parasitize HumansMichael Vincent P.Pas encore d'évaluation
- Cabison - Mycology ReviewerDocument10 pagesCabison - Mycology ReviewerPatricia Cabison100% (1)
- Biology A Level PaperDocument24 pagesBiology A Level Papermegaordinaryday100% (1)
- Super Parasitology TableDocument11 pagesSuper Parasitology Tablesleepyhead archerPas encore d'évaluation
- Ultimate Final CoachingDocument79 pagesUltimate Final CoachingCarlo Montejo100% (1)
- Sleep Apnea and Disorders GuideDocument117 pagesSleep Apnea and Disorders GuideZllison Mae Teodoro MangabatPas encore d'évaluation
- Parasitic AmoebaDocument23 pagesParasitic AmoebaJethrö MallariPas encore d'évaluation
- Systemic and Opportunistic MycosesDocument5 pagesSystemic and Opportunistic Mycosesmiguel cuevasPas encore d'évaluation
- Sleep Apnea Sleep DisordersDocument11 pagesSleep Apnea Sleep DisordersZllison Mae Teodoro MangabatPas encore d'évaluation
- Sleep Apnea Sleep DisordersDocument11 pagesSleep Apnea Sleep DisordersZllison Mae Teodoro MangabatPas encore d'évaluation
- ParasitologyDocument30 pagesParasitologypk 77Pas encore d'évaluation
- Pre 1 MibrobiologyDocument3 pagesPre 1 MibrobiologyDeannise AnnPas encore d'évaluation
- Medtech ReviewerDocument4 pagesMedtech ReviewerLyudmyla Gillego100% (4)
- Dams Lastlook Microbiology PDFDocument27 pagesDams Lastlook Microbiology PDFChauhan Monika100% (1)
- NR 23 Strictly Anaerobic Beer Spoilage Bacteria With Special Emphasis On New and Emerging Species Riikka JuvonenDocument37 pagesNR 23 Strictly Anaerobic Beer Spoilage Bacteria With Special Emphasis On New and Emerging Species Riikka JuvonenIvana NikolicPas encore d'évaluation
- Structure and Classification of Bacteria: Morpho DifferencesDocument8 pagesStructure and Classification of Bacteria: Morpho DifferencesJaz CPas encore d'évaluation
- Experimental Biology with Micro-Organisms: Students' ManualD'EverandExperimental Biology with Micro-Organisms: Students' ManualPas encore d'évaluation
- Free Living Amoeba and CoccidiansDocument33 pagesFree Living Amoeba and CoccidiansGlanela ManalotoPas encore d'évaluation
- The Intestinal Protozoa: Classification and Identification of Medically Important SpeciesDocument15 pagesThe Intestinal Protozoa: Classification and Identification of Medically Important SpeciesWasilla MahdaPas encore d'évaluation
- Emerging Parasitic InfectionDocument6 pagesEmerging Parasitic Infectionmiguel gaquitPas encore d'évaluation
- Gram Positive Bacilli: A. Bacillus SpeciesDocument9 pagesGram Positive Bacilli: A. Bacillus SpeciesOddly SatisfyingPas encore d'évaluation
- Dracunculus Medinensis and Filarial WormsDocument19 pagesDracunculus Medinensis and Filarial WormsAnastasiaPas encore d'évaluation
- TRANS NOTES For CH16Document5 pagesTRANS NOTES For CH16Patricia CabisonPas encore d'évaluation
- Blood Smear Results Falciparum MalariaDocument4 pagesBlood Smear Results Falciparum MalariaMaria Micaela CabarlesPas encore d'évaluation
- (Microbiology and Parasitology) Basic and Clinical ParasitologyDocument33 pages(Microbiology and Parasitology) Basic and Clinical ParasitologyMa. Pia Lorein JacintoPas encore d'évaluation
- AmebaDocument53 pagesAmebaapi-19916399Pas encore d'évaluation
- TRANS GROUP 2Document8 pagesTRANS GROUP 2Alanah JanePas encore d'évaluation
- UntitledDocument2 pagesUntitledGlaiza BolanoPas encore d'évaluation
- Apicomplexa (Sporozoa) 5.1general Future and ClassificationDocument10 pagesApicomplexa (Sporozoa) 5.1general Future and Classificationtedela gulumaPas encore d'évaluation
- BABESIOSISDocument34 pagesBABESIOSISRoderick83% (6)
- CitosesqueletoDocument11 pagesCitosesqueletoIvanAntonioVilchezPas encore d'évaluation
- Cryptosporidium and Giardia, Fact or FictionDocument12 pagesCryptosporidium and Giardia, Fact or FictionwiwienPas encore d'évaluation
- Lesson 6 - Coccidian PDFDocument11 pagesLesson 6 - Coccidian PDFAnya IgnacioPas encore d'évaluation
- The Intestinal ProtozoaDocument15 pagesThe Intestinal ProtozoaKHURT MICHAEL ANGELO TIUPas encore d'évaluation
- 4 ProtozoaDocument2 pages4 Protozoareaj.jumsaliPas encore d'évaluation
- Am Positive Rods-1Document73 pagesAm Positive Rods-1temesgensemahegn55Pas encore d'évaluation
- Opportunistic Mycoses: Portal of Entry: Respiratory, Mucocutaneous Infectious Particles: Conidia, MyceliaDocument4 pagesOpportunistic Mycoses: Portal of Entry: Respiratory, Mucocutaneous Infectious Particles: Conidia, MyceliaPinay YaunPas encore d'évaluation
- B. Anserine, Toricotae, Parkeri: Dammini/deer TicksDocument4 pagesB. Anserine, Toricotae, Parkeri: Dammini/deer TicksPia Rose BaguioPas encore d'évaluation
- Miscellaneous Protozoa1Document5 pagesMiscellaneous Protozoa1Haki TozakiPas encore d'évaluation
- Topnotch Parasitology Super Table by DR - Yns PereyraDocument50 pagesTopnotch Parasitology Super Table by DR - Yns PereyraRochelle Joyce AradoPas encore d'évaluation
- Biostat PP 9-10Document4 pagesBiostat PP 9-10medtedcgPas encore d'évaluation
- Enfermedades Por Protozoos Criptosporidiosis, Giardiasis y Otras Enfermedades Por Protozoos IntestinalesDocument18 pagesEnfermedades Por Protozoos Criptosporidiosis, Giardiasis y Otras Enfermedades Por Protozoos IntestinalesCarol VelezPas encore d'évaluation
- Significance of Commensal Amebae in StoolDocument12 pagesSignificance of Commensal Amebae in StoolNicolle PanchoPas encore d'évaluation
- Chapter 41 - 42 - Anaerobic OrganimsDocument4 pagesChapter 41 - 42 - Anaerobic OrganimsKoarie Frae ZulePas encore d'évaluation
- BZ Lab 4.0Document7 pagesBZ Lab 4.0Alexa Jean D. HonrejasPas encore d'évaluation
- 2. Amoebae Final 2Document23 pages2. Amoebae Final 2theonlinegeekhubPas encore d'évaluation
- Micro by DR - Hesham (GIT)Document65 pagesMicro by DR - Hesham (GIT)abcde990075Pas encore d'évaluation
- 5 CorynebacteriumDocument41 pages5 Corynebacterium01. Akhmad Gilang R - XII MIPA 4Pas encore d'évaluation
- Nonpathogenic Amoebae - FlagellatesDocument20 pagesNonpathogenic Amoebae - FlagellatesHend AtijaniPas encore d'évaluation
- Mycobacteria 1Document46 pagesMycobacteria 1Sajjal AliPas encore d'évaluation
- Birao Sas 15 Microbiology and ParasitologyDocument8 pagesBirao Sas 15 Microbiology and ParasitologyFrancis Jacob Dejecacion GarcesPas encore d'évaluation
- Medical Biology 3 - BR - 2020Document70 pagesMedical Biology 3 - BR - 2020Yusuf Yağız TimurPas encore d'évaluation
- (PROTOZOANS) Phylum ApicomplexaDocument8 pages(PROTOZOANS) Phylum ApicomplexaEunice AndradePas encore d'évaluation
- P3 Basil Gram (+) Rev2016Document50 pagesP3 Basil Gram (+) Rev2016AuliaPas encore d'évaluation
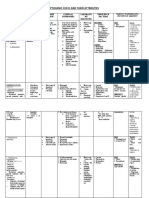
- PYOGENIC COCCI AND THEIR ATTRIBUTESDocument5 pagesPYOGENIC COCCI AND THEIR ATTRIBUTESJesette KhoPas encore d'évaluation
- Medmicronotes 3Document66 pagesMedmicronotes 3Lethal BaconPas encore d'évaluation
- Bacterial Cultivation Microbial CultureDocument4 pagesBacterial Cultivation Microbial CulturePatricia CuaPas encore d'évaluation
- COCCIDIADocument12 pagesCOCCIDIACheska Marie SalvaPas encore d'évaluation
- Aust Clinical Parasitology CLS 450: Dr. Renée Zakhia Rzakhia@aust - Edu.lbDocument33 pagesAust Clinical Parasitology CLS 450: Dr. Renée Zakhia Rzakhia@aust - Edu.lbChristine KamaleddinePas encore d'évaluation
- Acid (Acts As Antigenic Determinant-Impo For Serologic ID)Document5 pagesAcid (Acts As Antigenic Determinant-Impo For Serologic ID)qwertier2Pas encore d'évaluation
- Protozoan Parasite E. histolytica Life CycleDocument6 pagesProtozoan Parasite E. histolytica Life CyclePrimo GeorgePas encore d'évaluation
- Airway-management-for-interns (2)Document2 pagesAirway-management-for-interns (2)Zllison Mae Teodoro MangabatPas encore d'évaluation
- PAPASA KA NA A REVALIDADocument1 pagePAPASA KA NA A REVALIDAZllison Mae Teodoro MangabatPas encore d'évaluation
- NOVEMBER 24transDocument3 pagesNOVEMBER 24transZllison Mae Teodoro MangabatPas encore d'évaluation
- servicesDocument23 pagesservicesZllison Mae Teodoro MangabatPas encore d'évaluation
- Pediatric Infectious Diseases GuideDocument6 pagesPediatric Infectious Diseases GuideZllison Mae Teodoro MangabatPas encore d'évaluation
- LabdxheartDocument2 pagesLabdxheartZllison Mae Teodoro MangabatPas encore d'évaluation
- Basic Examinations of The Blood: 0.5G SHB/DL of Blood O Hemoglobin Concentration DeterminationDocument14 pagesBasic Examinations of The Blood: 0.5G SHB/DL of Blood O Hemoglobin Concentration DeterminationZllison Mae Teodoro MangabatPas encore d'évaluation
- OB TVS Transabdominal UltrasoundDocument8 pagesOB TVS Transabdominal UltrasoundZllison Mae Teodoro MangabatPas encore d'évaluation
- Cummings Otolaryngology Chapter 201Document14 pagesCummings Otolaryngology Chapter 201Zllison Mae Teodoro MangabatPas encore d'évaluation
- CSF Analysis GuideDocument12 pagesCSF Analysis GuideZllison Mae Teodoro MangabatPas encore d'évaluation
- IgA Vasculitis - Differentials - EditedDocument2 pagesIgA Vasculitis - Differentials - EditedZllison Mae Teodoro MangabatPas encore d'évaluation
- Embryology of Urinary SystemDocument4 pagesEmbryology of Urinary SystemZllison Mae Teodoro MangabatPas encore d'évaluation
- NEUROLOGY MULTIPLE-CHOICE QUIZDocument11 pagesNEUROLOGY MULTIPLE-CHOICE QUIZzhai bambalanPas encore d'évaluation
- Marriage: Ethics IiDocument2 pagesMarriage: Ethics IiZllison Mae Teodoro MangabatPas encore d'évaluation
- Uti VurDocument5 pagesUti VurZllison Mae Teodoro MangabatPas encore d'évaluation
- RecallDocument1 pageRecallZllison Mae Teodoro MangabatPas encore d'évaluation
- RRL JordanDocument6 pagesRRL JordanZllison Mae Teodoro MangabatPas encore d'évaluation
- Mangabat Ethics3MIdtermsDocument7 pagesMangabat Ethics3MIdtermsZllison Mae Teodoro MangabatPas encore d'évaluation
- 2 3 Platelet ProductsDocument4 pages2 3 Platelet ProductsKartika ParamitaPas encore d'évaluation
- Mark M Calban MD MPM-HSDDocument58 pagesMark M Calban MD MPM-HSDZllison Mae Teodoro Mangabat100% (1)
- Infectious Diseases Part I 2Document65 pagesInfectious Diseases Part I 2Zllison Mae Teodoro MangabatPas encore d'évaluation
- Patho Lab1Document118 pagesPatho Lab1Zllison Mae Teodoro MangabatPas encore d'évaluation
- Multiple page document scanned by CamScannerDocument30 pagesMultiple page document scanned by CamScannerZllison Mae Teodoro MangabatPas encore d'évaluation
- Labdxtransfinals PDFDocument16 pagesLabdxtransfinals PDFSubhan Souda MangalasseryPas encore d'évaluation
- 2 3 Platelet ProductsDocument4 pages2 3 Platelet ProductsKartika ParamitaPas encore d'évaluation
- Activity PharmaDocument1 pageActivity PharmaZllison Mae Teodoro MangabatPas encore d'évaluation
- Markus Kalkum 2017Document352 pagesMarkus Kalkum 2017joão costaPas encore d'évaluation
- A Double-Strain TM (gp45) Polypeptide Antigen and Its Application in The Serodiadnosis of Equine Infectius AnemiaDocument8 pagesA Double-Strain TM (gp45) Polypeptide Antigen and Its Application in The Serodiadnosis of Equine Infectius AnemiaFredy MoralesPas encore d'évaluation
- Anaplastic meningioma diagnosisDocument1 pageAnaplastic meningioma diagnosisBhavik ChavdaPas encore d'évaluation
- Anthropology Syllabus (Paper 1) : S.no Syllabus Reference BooksDocument6 pagesAnthropology Syllabus (Paper 1) : S.no Syllabus Reference BooksBhaskar NPas encore d'évaluation
- Endogenous Notch Signaling in Adult Kidneys.13Document17 pagesEndogenous Notch Signaling in Adult Kidneys.13Arista RachmaPas encore d'évaluation
- Molecular Biology (Sars-Cov-2) CT Value Result Test DescriptionDocument1 pageMolecular Biology (Sars-Cov-2) CT Value Result Test DescriptionVenkat Reddy AvulaPas encore d'évaluation
- Body Diagram2Document6 pagesBody Diagram2mmtruffautPas encore d'évaluation
- Allergy and Allergic Diseases - The New Mechanisms and Therapeutics (PDFDrive) PDFDocument588 pagesAllergy and Allergic Diseases - The New Mechanisms and Therapeutics (PDFDrive) PDFDora DodigPas encore d'évaluation
- (ObstetricsA) Implantation and Formation of Placenta and Fetal Membranes - Dr. Marinas (Lea Pacis) PDFDocument6 pages(ObstetricsA) Implantation and Formation of Placenta and Fetal Membranes - Dr. Marinas (Lea Pacis) PDFCristina Marie BarrugaPas encore d'évaluation
- Ch1 Kitabcd Class 8 MSBHSE Science NotesDocument8 pagesCh1 Kitabcd Class 8 MSBHSE Science NotesONE CLICK COMPUTERPas encore d'évaluation
- Chapter 22Document91 pagesChapter 22YuoMatsukiPas encore d'évaluation
- CH 10 Lecture PresentationDocument159 pagesCH 10 Lecture PresentationBrian Mathieu Jr.Pas encore d'évaluation
- 7 DvariationandclassificationDocument34 pages7 DvariationandclassificationKomalesh TheeranPas encore d'évaluation
- (Q1) Wu2019Document7 pages(Q1) Wu2019Salma FahimaPas encore d'évaluation
- Photosynthesis Lessons Student NotesDocument12 pagesPhotosynthesis Lessons Student NoteslinaPas encore d'évaluation
- BSbioDocument2 pagesBSbioMDreamerPas encore d'évaluation
- Classification of A PoisonDocument6 pagesClassification of A PoisonCake ManPas encore d'évaluation
- Mini Review Beyond pUC: Vectors For Cloning Unstable DNADocument7 pagesMini Review Beyond pUC: Vectors For Cloning Unstable DNAdiego jaraPas encore d'évaluation
- Photosynthesis PDFDocument30 pagesPhotosynthesis PDFhumble happyPas encore d'évaluation
- Formation of root & shoot from callus cultureDocument40 pagesFormation of root & shoot from callus cultureKiran KurhadePas encore d'évaluation
- Experiment No. 2 Amino Acids and Proteins (Part I)Document12 pagesExperiment No. 2 Amino Acids and Proteins (Part I)Anne GelliePas encore d'évaluation
- An Introduction To Plant Development: (Because Plants Are The Best)Document40 pagesAn Introduction To Plant Development: (Because Plants Are The Best)jesusrgffPas encore d'évaluation
- COVID Thrombosis: Mitochondria, The Endothelial Glycocalyx and Platelets Are KeyDocument10 pagesCOVID Thrombosis: Mitochondria, The Endothelial Glycocalyx and Platelets Are KeyMercedes BouterPas encore d'évaluation
- New Insights in Dialysis Membrane BiocompatibilityDocument7 pagesNew Insights in Dialysis Membrane BiocompatibilityDani ursPas encore d'évaluation
- Platelet-Rich Plasma (PRP) : What Is PRP and What Is Not PRP?Document4 pagesPlatelet-Rich Plasma (PRP) : What Is PRP and What Is Not PRP?Amanda PutriPas encore d'évaluation