Académique Documents
Professionnel Documents
Culture Documents
Toxi Prelim To Finals 1
Transféré par
Raya Ibarra Lumogdang0 évaluation0% ont trouvé ce document utile (0 vote)
74 vues7 pagesToxi lec prelim to finals notes
Titre original
Toxi Prelim to Finals 1
Copyright
© © All Rights Reserved
Formats disponibles
DOCX, PDF, TXT ou lisez en ligne sur Scribd
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentToxi lec prelim to finals notes
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
0 évaluation0% ont trouvé ce document utile (0 vote)
74 vues7 pagesToxi Prelim To Finals 1
Transféré par
Raya Ibarra LumogdangToxi lec prelim to finals notes
Droits d'auteur :
© All Rights Reserved
Formats disponibles
Téléchargez comme DOCX, PDF, TXT ou lisez en ligne sur Scribd
Vous êtes sur la page 1sur 7
LESSON 1 o Testing or analysis of a toxicant or
agents in bodily fluids
What is TOXICOLOGY?
o LD50, LC50
“Branch of science that deals with o TLV - Threshold limit values
poisons” 4. Descriptive Toxicology
“The science of poisons and the effects o Conduct toxicity testing in order to
of chemicals on living organisms” gather product information on
“The medical science of studying product acceptance , safety and
poisons” regulation
5. Forensic Toxicology
POISON o Concerned with medico-legal cases
o e.g. crime scenes
Any substance that can cause injury,
disease and death. 6. Mechanistic Toxicology
o Deals with the MECHANISM OF
Any drug is poisonous if taken in
TOXIC ACTION (MOTA) of
sufficient quantities
substances
EX: Luana Suares 2013 Died of Water
Intoxication LESSON 2 INTRODUCTION TO POISONS
INTOXICATION Toxicity associated with any SOURCES OF POISONS
substance
1) INDUSTRIAL
HAZARD Likelihood that an injury may occur
POLLUTANTS
RISK Frequency that a harmful effect may HYDROCYANIC ACID
happen CARBON DIOXIDE/MONOXIDE
CHLOROFLUOROCARBONS
OVERDOSE Intentional exposure to toxic agent
2) HOUSEHOLD
POISONING Accidental exposure to toxic agent INSECTICIDES/PESTICIDES
Branches of Toxicology CLEANING AGENTS
3) ENVIRONMENTAL
LEAD
SULFUR DIOXIDE
NITROGEN
OZONE
4) PHARMACOLOGIC/MEDICINAL
CLINICALLY USED SUBSTANCE
1. Clinical Toxicology SUBSTANCES FOR ABUSE
o The analysis and assessment of
KINDS OF POISONS
overdose and poisoning effects to
the patient ACCORDING TO PROPERTY
2. Environmental Toxicology A. CORROSIVES
o The study of the impact of Local destruction of parts but not
pollutants to human health poisonous if diluted.
3. Experimental Toxicology ACIDS , BASES
B. TRUE POISONS
Highly toxic Subcutaneous
No medicinal value Absorption through the skin
C. CUMULATIVE POISONS Inhalation
Increases the intensity of a poison as
the dose increase Quantitative Toxicity
ACCORDING TO MODE OF ACTION Median Lethal Dose (LD5)
A. LOCAL Median Lethal Concentration (LC50)
Destroy or cause serious injury to Threshold Limit Value (TLV)
mucous membrane or tissues TYPES OF POISONING
Corrosives (e.g. Acids & Bases) A. ACUTE
KINDS OF LOCAL EFFECTS Taken in excess in a single dose or small
CORROSION doses with high frequency resulting to
IRRITATION death or injury over a short span of
SPECIFIC EFFECT time.
Localization of Poisons e.g. Sleeping pills
The remote action of poison following B. CHRONIC
absorption on certain organs Produced by taking over the course of a
Factors Affecting Absorption of Poison long period of time producing gradual
Solubility of Poison but progressive deterioration of tissue
Character of the Surface to which functions.
the poison is applied e.g. Heavy metals
Quantity of blood in the blood CLASSIFICATION OF TOXIC EFFECTS
vessels A. PHARMACOLOGICAL – exaggeration of
Conditions which Modify the Action of Poisons effects
Physical state B. PATHOLOGICAL- injury to tissue
Age C. GENOTOXIC –damage to DNA
Sex D. CHRONIC
Idiosyncrasy E. ACUTE
Habit F. IMMEDIATE – rapid effects after
Mental & Physical State exposure
Condition of the stomach G. DELAYED – occurrence of effects over a
Character and amount of stomach period of time
contents H. DIRECT – caused directly by a specific
B. SYSTEMIC substance
Follow local action, absorbed into the I. INDIRECT – effects are only
bloodstream, furthermore, produces consequences of the direct effects.
harmful effects on vital organs. EVIDENCE OF POISONING
E.g. Heavy Metals CIRCUMSTANTIAL
Routes Circumstance or deduced from
Oral various consequences and facts
Intravenous SYMPTOMATIC
Exhibited by the patient • RIBOFLAVIN & RIFAMPICIN – YELLOW
CHEMICAL
Evidence by means of chemical LESSON 3 MOTA
analysis (e.g. tyrotoxin, A. RECEPTOR THEORY
tyrotoxicon) According to Paul Erlich
ANTE-MORTEM Specific or selective for a
Obtained right before death particular tissue or organ
POST-MORTEM Cell possess receptors
Examinations of organs or (proteins, cell membrane
tissues after death surface, nucleus) which forms
Blackening and severe complexes with poisons.
corrosion (corrosives) Cause physiologic change in the
Discoloured lips (caustic alkali) cell
Swollen lips (ammonia) B. CHANGE IN ENZYME SYSTEMS
Whitened mucous membrane Disruption of enzyme activity
(oxalic acid) Direct action on
Dessicated inflammation substrate or a cofactor
(cantharides) Inhibition of enzyme
EXPERIMENTAL Similar structure of enzyme acts
Obtained by administering a on a substrate
suspected substance to some Competitive inhibition
living animals and observing the Inactive enzymes
effects Alter enzyme structures
Discoloration of the feces C. CHANGE IN MEMBRANE STRUCTURE
Discoloration of the urine Interfere with the normal
FECAL EVIDENCE activities of the membrane:
• ANTACIDS – WHITISH SPECKS transport of nutrients,
• ANTICOAGULANTS – RED TO BLACK expulsion of toxic products
• BISMUTH AND IRON – BLACK COMMON PATHOPHYSIOLOGICAL
• PIRVINIUM PAMOATE – RED MECHANISMS
• RIFAMPICIN – RED A. INTERFERENCE OF OXYGEN
• SALICYLATES – RED TO BLACK B. DEPRESS OR STIMULATE CNS
URINARY EVIDENCE C. AFFECT ANS
• CASCARA SAGRADA – RED IN ALKALINE D. AFFECT THE LUNGS
URINE E. AFFECT CV
• CHLOROQUINE – YELLOW TO BROWN F. LOCAL DAMGE
• CHLORPROMAZINE – PINK TO RED G. DELAYED EFFECTS
• FURAZOLIDONE – YELLOW TO BROW ELIMINATIONOF POISONS
• METRONIDAZOLE – DARK A. SALIVA
• NITROFURANTOIN – YELLOW TO B. URINE
BROWN C. SWEAT
D. BILE Trade and generic name of the
E. PANCREATIC JUICE poisons
Route of exposure
F. FECES
Formulation and name of
G. RENAL IS USALLY THE ROUTE OF manufacturer
ELIMINATION Action taken to eliminate poison
H. GASEOUS POISONS MAY BE PROMPTLY Occupation and hobbies
REMOVED BY THE LUNGS WHEN?
Time of exposure
DIAGNOSIS OF POISONING
Differential diagnosis as to the
Dependent on: onset of the poison
Consciousness of the patient Routines
Physical examination HOW MUCH?
Past history Amount of exposure and strength
Chemical identification of poison
Quantification of compound in Place of exposure
question WHY?
CONSCIOUSNESS Poisoning
Overdosing
Admittance
PHYSICAL FINDING
Poisoning
Vital signs
SIGNS
Heart rate
Vomiting
Respiration rate
Convulsions
Temperature
Coma
Blood pressure
Pupilodilation/pupilocostriction
Documents and Pertinent
Slow/rapid respiration
Evidence
Delirium
Dyspnea
MANAGEMENT OF POISONING: GENERAL
Cyanosis
PRINCIPLES
IDENTIFICATION OF PATIENT AND
A. Separation of patient from the poison
TOXIC AGENT Remove the patient from contaminated
WHO IS THE PATIENT? area
HOW IS THE PATIENT? Remove clothing, if the area of
Obtaining the history (for non life exposure is local
threatening cases) Induce vomiting for non-corrosives
Symptomatic patients are B. Provide supportive therapy
transferred to the nearest health Use of ventilator
care facility Use of cardiovascular support
Asymptomatic patients: C. Give antidotes
Age Give universal antidotes
Medication taken Give specific antidotes
Past history
Last meal MANAGEMENT OF POISONING: PREVENTING
Events that lead to the ABSORPTION
poisoning/overdose
A. Induce vomiting
WHAT?
stimulation of medullary
chemoreceptor trigger zone (CTZ) LESSON 4
Syrup of Ipecac (Cephalis ipecacuanha) ANTIDOTES
Contraindicated for corrosives,
agents which neutralize or counteract
hydrocarbons
the effects of poisons
unconscious or altered consciousness
Kinds of Antidotes
convulsive
B. Gastric Lavage Mechanical
large-bore tube through the mouth, into Remove poisons or prevent absorption
the esophagus and stomach by coating or suspending the poison
Pumped in with 250mL aliquots of saline or Examples:
water
Stomach pump or tube
Less effective
employment of emetics,
Alternative for emesis
cathartics
C. Activated Charcoal
A. EMETICS
Adsorption of poison or toxin
Delay GI absorption 1. LOCAL EMETICS
stimulation or irritation of terminal
D. Cathartics
enhances the transit of materials through
nerve filaments, reflex stimulation of
the GIT the vomiting center of the medulla
generally, utilized after specific antidotes oblongata
are given Example:
FIRST AID TREATMENT FOR POISONING Mustard (Brassica nigra and Sinapis
alba)
A. Removal of poison from point of
2. SYSTEMIC EMETICS
contact
produce effects through circulation
1. Eyes - wash with saline, milk
Example:
2. Skin - wash with running water Ipecac syrup
3. Mouth - remove contents of mouth Emetine
B. Removal of victim from poisonous Apomorphine hydrochloride
fumes B. CATHARTICS
1. Allow the victim to have fresh air agents which produce intestinal
2. Loosen all tight-fitting clothing evacuation, generally used after a
3. If breathing is not detected, start chemical antidote
artificial respiration Castor Oil - contraindicated for
4. Use oxygen if available cantharides, copper salts, phosphorus
C. Inducing vomiting Magnesium sulfate (Epsom salt)
1. Give syrup of ipecac Sodium sulfate (Glauber’s salt)
Dosing:
Adults - 30mL
Child over 1 year - 15mL
Child less than 1 year – 10ml Physiological
2. Contraindications: agents which act by opposing the
o Unconscious patients
effects of the poison combat symptoms
o Convulsive
Example:
o Ingested corrosives
o Ingested hydrocarbons
Atropine to morphine
Barbiturate to cocaine A product of hydrolysis of penicillin
Caffeine to morphine Usually for the removal of copper and
Chemical Antidotes lead
agents which acts chemically to form 4. DEFEROXAMINE
non-toxic compounds chelates iron to FERRIOXAMINE
given aif the Iron serum levels exceeds
action is usually by precipitation,
400mcg/Dl
neutralization, oxidation or chelation
5. SUCCIMER
1. Acids & corrosives - antacids
also known as Dimercaptosuccinic acid
2. Barium salts - sodium sulfate, magnesium
or DMSA
sulfate
analog of dimercaprol
3. Alkaloids - potassium permanganate
Isolated from Streptomyces pilosus
4. Heavy metals - milk, egg white A/E: Anorexia, N&V, diarrhea
5. Mercury – dimercaprol
6. TRIENTINE
Also known as
A. CHELATION TRIETHYLENETETRAMINE
CHELATE for copper chelation, second line
formation of a large compound treatment
containing a ligand bonded to acentral
metal atom LESSON 5
1. DIMERCAPROL Specific Poisons
Also known as British Anti-Lewisite Corrosives
(BAL) Maybe referred as acids
Metal acceptor to prevent or MOTA:
reverse activation Direct chemical reaction, the tissue protein
A/E: is converted to acid proteinate (e.g.
3mg/Kg dose: Anorexia, restlessness, Hemoglobin to Hematin) and is
body malaise, itching, salivation, elevated BP precipitated. The action to the tissue will
cause reflex loss of vascular tone
5mg/Kg dose: Vomiting, convulsions,
Caustics
stupor or coma
Contraindications: Maybe referred as bases
MOTA:
Not for Iron or selenium poisoning
combine with proteins to form proteinates
Not for patients with hepatic and renal
and form soap, produce soft liquefactive
issues
necrosis, can also cause loss of vascular
2. CALCIUM EDETATE tone
Also known as Calcium disodium Corrosives and Caustics
versenate Principal Manifestation: CORROSION
Only for metals that cannot be Ingested: severe burning pain in the tissues
displaced by calcium that come into contact
(e.g.) Lead, iron, zinc, manganese, Evidence: Brown to yellow stains
beryllium, copper Probable cause of death: Asphyxia from the
3. PENICILLAMINE edema of the glottis
Also known as Cuprimine
Inhaled: coughing to choking, dizziness,
weakness, cyanosis, hemoptysis
Evidence: shortness of breath for several
weeks
Probable cause of death: Asphyxia from the
vapor
Skin Contact: penetrating burns, necrosis
Evidence: yellow to brown stains
Eye Contact: penetrating burns,
conjunctival edema, corneal destruction,
pain
Evidence: redness of the eyes, blindness
TREATMENT: Corrosives and Caustics
General Measures:
Dilution with milk (100x)
Gastric lavage is not the first option
Relieve pain with morphine
Prevent edema of the glottis
Maintain blood pressure
EYE - Dilute with milk for at least 15 minutes
SKIN - Flowing water for at least 15 minutes
INHALATION - Artificial respiration
Vous aimerez peut-être aussi
- Clinical Chemistry: ToxicologyDocument9 pagesClinical Chemistry: ToxicologyChristine BadilloPas encore d'évaluation
- Classification of PoisonsDocument18 pagesClassification of Poisonslucy2 kasongi100% (1)
- PCOL3011Document5 pagesPCOL3011Jack AultPas encore d'évaluation
- The Integumentary System Development: Biene, Ellen Angelic Flores, Andrie BonDocument29 pagesThe Integumentary System Development: Biene, Ellen Angelic Flores, Andrie BonMu Lok100% (3)
- Clinical ToxicologyDocument25 pagesClinical ToxicologyMark Steven Garlitos100% (1)
- Pink Simple School NewsletterDocument4 pagesPink Simple School NewsletterCarla Flor LosiñadaPas encore d'évaluation
- 2 Toxicokinetics & ToxicodynamicsDocument32 pages2 Toxicokinetics & ToxicodynamicsLaura RodriguezPas encore d'évaluation
- Environmental Toxicology: Universidad Manuela Beltran Ingenieria Ambiental 2018Document16 pagesEnvironmental Toxicology: Universidad Manuela Beltran Ingenieria Ambiental 2018Daniel Salas OjedaPas encore d'évaluation
- Toxicology: WEEK 6-8Document29 pagesToxicology: WEEK 6-8Cariza Anda0% (1)
- Unit 2 Poisons and PoisoningDocument16 pagesUnit 2 Poisons and PoisoningKhar Mel GoPas encore d'évaluation
- Occupational Safety and Health: Chemical Hazards Outline: TeamDocument30 pagesOccupational Safety and Health: Chemical Hazards Outline: TeamNeoPas encore d'évaluation
- ToxicologyDocument13 pagesToxicologyCed OlmonPas encore d'évaluation
- Casarett & Doulls Essentials of Toxicology - 3E PDFDocument15 pagesCasarett & Doulls Essentials of Toxicology - 3E PDFwhothehellisarcticmonkeysPas encore d'évaluation
- Intro To Toxi 2019 2020 PDFDocument70 pagesIntro To Toxi 2019 2020 PDFJerson Aizpuro SuplementoPas encore d'évaluation
- B - Kelompok 1 - RECOGNITIONDocument29 pagesB - Kelompok 1 - RECOGNITIONAlya RosaliPas encore d'évaluation
- Tujuan: Efek Toksik Tumbuhan RacunDocument10 pagesTujuan: Efek Toksik Tumbuhan RacunCatherina AileenPas encore d'évaluation
- Forensic ToxicologyDocument12 pagesForensic ToxicologyRenalyn EllicaPas encore d'évaluation
- TOXICOLOGYDocument106 pagesTOXICOLOGYbhag singh dhaked100% (1)
- Chapter 8 ToxicologyDocument9 pagesChapter 8 Toxicologyminessweeper23Pas encore d'évaluation
- Pharmacology: Incidentally Atmosphere Contact During Occupation or Recreational Activities Ingestion As Food AdditivesDocument4 pagesPharmacology: Incidentally Atmosphere Contact During Occupation or Recreational Activities Ingestion As Food AdditivesSelena MoonPas encore d'évaluation
- PHCT311 Week 1Document32 pagesPHCT311 Week 1jdrancap0746qcPas encore d'évaluation
- Chapter 18-ToxicologyDocument25 pagesChapter 18-ToxicologyBARCELON, CHRISTOPHER JAMESPas encore d'évaluation
- Toxicology (Lecture 1)Document42 pagesToxicology (Lecture 1)yousernamePas encore d'évaluation
- CORE Part 1 - ToxicityDocument10 pagesCORE Part 1 - ToxicityDigitalGeeksPas encore d'évaluation
- Lecture 10 - Toxicology of Hazardous ChemicalsDocument7 pagesLecture 10 - Toxicology of Hazardous ChemicalsSyafiq AzizPas encore d'évaluation
- T o X I C o L o G yDocument7 pagesT o X I C o L o G yDennis ValdezPas encore d'évaluation
- ToxicologyDocument8 pagesToxicologybernalhoneylethjhoy06Pas encore d'évaluation
- Pubdoc 3 1364 6020Document9 pagesPubdoc 3 1364 6020محمدأميندماجPas encore d'évaluation
- Review Poison N ToxicologyDocument10 pagesReview Poison N ToxicologyAceAsabuPas encore d'évaluation
- Iadt03i5p402 PDFDocument10 pagesIadt03i5p402 PDFRakesh PrasadPas encore d'évaluation
- ZOOL609 Lecture 1 - 128234Document35 pagesZOOL609 Lecture 1 - 128234Malaika javedPas encore d'évaluation
- Forensic ToxicologyDocument27 pagesForensic ToxicologyMarkus WolfePas encore d'évaluation
- Toxicology: CH153 Q3 AY2021Document11 pagesToxicology: CH153 Q3 AY2021Astra BeckettPas encore d'évaluation
- En (Entry) Ef (Effect) El (Eliminate) Av (Avoid)Document3 pagesEn (Entry) Ef (Effect) El (Eliminate) Av (Avoid)Ng SiewminPas encore d'évaluation
- Effects of ToxicDocument1 pageEffects of ToxicPutri SaidatinaPas encore d'évaluation
- Chap8 ToxicologyDocument9 pagesChap8 ToxicologySharon GabrielPas encore d'évaluation
- PoisoningDocument2 pagesPoisoninggoyaPas encore d'évaluation
- Chemical Toxicology ChapterDocument20 pagesChemical Toxicology ChapterarushiPas encore d'évaluation
- Chemical and Nuclear DisasterDocument79 pagesChemical and Nuclear DisasterArchana MadpathiPas encore d'évaluation
- 1 Introduction PDFDocument20 pages1 Introduction PDFAll Furqaniya ChannelPas encore d'évaluation
- Fundamentals of Toxicology: Sri Hainil, S.Si, M.farm, AptDocument39 pagesFundamentals of Toxicology: Sri Hainil, S.Si, M.farm, AptlyanaPas encore d'évaluation
- Clinical ToxicologyDocument36 pagesClinical ToxicologyMuhammad FawadPas encore d'évaluation
- 1 Principles of Toxicology PDFDocument85 pages1 Principles of Toxicology PDFMariefe BlayaPas encore d'évaluation
- 01 Introduction To ToxicologyDocument32 pages01 Introduction To ToxicologyGendis SabrinaPas encore d'évaluation
- Toxicology 1Document32 pagesToxicology 1Evan Jane GacottPas encore d'évaluation
- Mechanism of Toxicity I: Dr. Nadia Mohamed SharafDocument30 pagesMechanism of Toxicity I: Dr. Nadia Mohamed SharafAstutePas encore d'évaluation
- TOXICOLOGY1Document80 pagesTOXICOLOGY1Wynli.AncogPas encore d'évaluation
- A - Look - Into - The - World - of - ToxicologyDocument29 pagesA - Look - Into - The - World - of - ToxicologyGustavo Calderon EliasPas encore d'évaluation
- Toxicology IDocument30 pagesToxicology IMohamed SHPas encore d'évaluation
- Environmental ToxicologyDocument65 pagesEnvironmental ToxicologyZulaikatu MustaphaPas encore d'évaluation
- Esther AssignmentDocument17 pagesEsther Assignmentsani sundayPas encore d'évaluation
- General Principles of ToxicologyDocument8 pagesGeneral Principles of ToxicologyJarot MangkubumiPas encore d'évaluation
- Basic Concept On Toxicology PDFDocument40 pagesBasic Concept On Toxicology PDFmefav7778520Pas encore d'évaluation
- Basic Concept On ToxicologyDocument40 pagesBasic Concept On Toxicologyadel santosPas encore d'évaluation
- Environmental Toxicology L1 L2Document7 pagesEnvironmental Toxicology L1 L2prasad sanjayaPas encore d'évaluation
- Lesson 13Document10 pagesLesson 13JASPER PENALBAPas encore d'évaluation
- Toxicology (Effects of Toxic) : Che 135 - Plant Safety and Occupational HealthDocument18 pagesToxicology (Effects of Toxic) : Che 135 - Plant Safety and Occupational Healthmuhammad izzulPas encore d'évaluation
- GE15 - SIM Week 6-7Document4 pagesGE15 - SIM Week 6-7Althea Nicole QuindoPas encore d'évaluation
- ToxicologyDocument5 pagesToxicologys.alisufyaanPas encore d'évaluation
- TOXICOLOGYDocument4 pagesTOXICOLOGYIŋterŋatiioŋal ǷwįƞçǯzxPas encore d'évaluation
- Veterinary Toxicology: Basic and Clinical PrinciplesD'EverandVeterinary Toxicology: Basic and Clinical PrinciplesÉvaluation : 4 sur 5 étoiles4/5 (1)
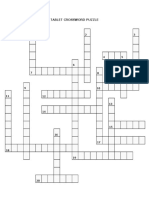
- Pcol2 CrossDocument1 pagePcol2 CrossRaya Ibarra LumogdangPas encore d'évaluation
- PCOL2 CrosswordDocument4 pagesPCOL2 CrosswordRaya Ibarra LumogdangPas encore d'évaluation
- Hard Copy Sublingual FinalDocument7 pagesHard Copy Sublingual FinalRaya Ibarra LumogdangPas encore d'évaluation
- States of Matter NotesDocument8 pagesStates of Matter NotesRaya Ibarra LumogdangPas encore d'évaluation
- Tablet PuzzleDocument3 pagesTablet PuzzleRaya Ibarra LumogdangPas encore d'évaluation
- CS2PDocument3 pagesCS2PRaya Ibarra LumogdangPas encore d'évaluation
- Organizational Chart of Quality Control LaboratoryDocument1 pageOrganizational Chart of Quality Control LaboratoryRaya Ibarra Lumogdang100% (1)
- ToxiiiiiiDocument6 pagesToxiiiiiiRaya Ibarra LumogdangPas encore d'évaluation
- Experiment 6 9 (Docu)Document1 pageExperiment 6 9 (Docu)Raya Ibarra LumogdangPas encore d'évaluation
- PCOGDocument1 pagePCOGRaya Ibarra LumogdangPas encore d'évaluation
- CholeraDocument1 pageCholeraRaya Ibarra LumogdangPas encore d'évaluation
- NailDocument7 pagesNailRaya Ibarra LumogdangPas encore d'évaluation
- Carbon Disulfide: Sulfocyanate Test Lead Acetate TestDocument1 pageCarbon Disulfide: Sulfocyanate Test Lead Acetate TestRaya Ibarra LumogdangPas encore d'évaluation
- A.M. P.M. Number Of: Name & Signature of Pharmacists-in-ChargeDocument4 pagesA.M. P.M. Number Of: Name & Signature of Pharmacists-in-ChargeRaya Ibarra LumogdangPas encore d'évaluation
- PLAN1Document3 pagesPLAN1Raya Ibarra LumogdangPas encore d'évaluation
- Lab Report Act 6Document6 pagesLab Report Act 6Raya Ibarra LumogdangPas encore d'évaluation
- Subjective and ObjectiveDocument2 pagesSubjective and ObjectiveRaya Ibarra LumogdangPas encore d'évaluation
- Pyra TBDocument6 pagesPyra TBRaya Ibarra LumogdangPas encore d'évaluation
- Urine PracticeDocument11 pagesUrine PracticeJack Eito NeoPas encore d'évaluation
- Defending A Dogma: Between Grice, Strawson and Quine: Elvis ImafidonDocument10 pagesDefending A Dogma: Between Grice, Strawson and Quine: Elvis ImafidonYang Wen-LiPas encore d'évaluation
- Analysis of Low-Frequency Passive Seismic Attributes in Maroun Oil Field, IranDocument16 pagesAnalysis of Low-Frequency Passive Seismic Attributes in Maroun Oil Field, IranFakhrur NoviantoPas encore d'évaluation
- Visual Rhetoric Music Video Comparison Essay - Abby MckellopDocument5 pagesVisual Rhetoric Music Video Comparison Essay - Abby Mckellopapi-597591424Pas encore d'évaluation
- Clinimetrics Single Assessment Numeric EvaluationDocument1 pageClinimetrics Single Assessment Numeric EvaluationNicol SandovalPas encore d'évaluation
- Implementation of 7s Framenwork On RestuDocument36 pagesImplementation of 7s Framenwork On RestuMuhammad AtaPas encore d'évaluation
- Ministry of Truth Big Brother Watch 290123Document106 pagesMinistry of Truth Big Brother Watch 290123Valentin ChirilaPas encore d'évaluation
- RF Design MCQ-1Document16 pagesRF Design MCQ-1JeyavelPas encore d'évaluation
- (Durt, - Christoph - Fuchs, - Thomas - Tewes, - Christian) Embodiment, Enaction, and Culture PDFDocument451 pages(Durt, - Christoph - Fuchs, - Thomas - Tewes, - Christian) Embodiment, Enaction, and Culture PDFnlf2205100% (3)
- Final Paper IN MAJOR 14 EL 116 Life and Death: Fear Reflected in John Green's The Fault in Our StarsDocument12 pagesFinal Paper IN MAJOR 14 EL 116 Life and Death: Fear Reflected in John Green's The Fault in Our StarsMary Rose FragaPas encore d'évaluation
- 07 Lejano vs. People (95 PAGES!)Document95 pages07 Lejano vs. People (95 PAGES!)noonalawPas encore d'évaluation
- Moon and SaturnDocument4 pagesMoon and SaturnRamanasarmaPas encore d'évaluation
- Filipino HousesDocument4 pagesFilipino HousesjackPas encore d'évaluation
- GST 101 Exam Past QuestionsDocument6 pagesGST 101 Exam Past QuestionsBenjamin Favour100% (2)
- Ogayon Vs PeopleDocument7 pagesOgayon Vs PeopleKate CalansinginPas encore d'évaluation
- Lecture 6Document7 pagesLecture 6Shuja MirPas encore d'évaluation
- Number SystemsDocument165 pagesNumber SystemsapamanPas encore d'évaluation
- Context: Lesson Author Date of DemonstrationDocument4 pagesContext: Lesson Author Date of DemonstrationAR ManPas encore d'évaluation
- Olinger v. The Church of Jesus Christ of Latter Day Saints Et Al - Document No. 1Document4 pagesOlinger v. The Church of Jesus Christ of Latter Day Saints Et Al - Document No. 1Justia.comPas encore d'évaluation
- Darkness Points Reminder 2Document2 pagesDarkness Points Reminder 2Tata YoyoPas encore d'évaluation
- Soal Midtest + Kunci JawabanDocument28 pagesSoal Midtest + Kunci JawabanYuyun RasulongPas encore d'évaluation
- Bubble ColumnDocument34 pagesBubble ColumnihsanPas encore d'évaluation
- "Shiksha Se Hi Suraksha": Literacy Campaign WeekDocument4 pages"Shiksha Se Hi Suraksha": Literacy Campaign WeekVaishali100% (1)
- Confidential Recommendation Letter SampleDocument1 pageConfidential Recommendation Letter SamplearcanerkPas encore d'évaluation
- Ccounting Basics and Interview Questions AnswersDocument18 pagesCcounting Basics and Interview Questions AnswersAamir100% (1)
- Design of Experiments: I. Overview of Design of Experiments: R. A. BaileyDocument18 pagesDesign of Experiments: I. Overview of Design of Experiments: R. A. BaileySergio Andrés Cabrera MirandaPas encore d'évaluation
- Not For Profit Governance WeilDocument224 pagesNot For Profit Governance WeillkjhmnvbPas encore d'évaluation
- Music in The United KingdomDocument33 pagesMusic in The United KingdomIonut PetrePas encore d'évaluation
- Tugas, MO - REVIEW JURNAL JIT - Ikomang Aditya Prawira Nugraha (1902612010304)Document12 pagesTugas, MO - REVIEW JURNAL JIT - Ikomang Aditya Prawira Nugraha (1902612010304)MamanxPas encore d'évaluation
- Determining Rounding Common CoreDocument2 pagesDetermining Rounding Common Coreapi-3662903730% (1)