Académique Documents
Professionnel Documents
Culture Documents
1 Congestive Heart Failure - An Uncommon Presentation of Pheochromocytoma
Transféré par
Lisandro KoyamaTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
1 Congestive Heart Failure - An Uncommon Presentation of Pheochromocytoma
Transféré par
Lisandro KoyamaDroits d'auteur :
Formats disponibles
nical Cas
Cli EI Hage et al., J Clin Case Rep 2015, 5:4
DOI: 10.4172/2165-7920.1000524
e
f Journal of Clinical Case Reports
Journal o
Re
ports
ISSN: 2165-7920
Case Report Open Access
Congestive Heart Failure: An Uncommon Presentation of
Pheochromocytoma
Halim El Hage*, Boutros Karam, Julie Zaidan and Elie El Charabaty
Staten Island University Hospital, 475 Seaview Avenue, Staten Island, New York, USA
Abstract
Introduction: Pheochromocytomas are rare catecholamine secreting tumors that arise from the chromaffine
tissue of the adrenal medulla. Rarely, these tumors are associated with cardiomyopathy. We herein present a patient
with pheochromocytoma presenting initially with congestive heart failure and hypertensive emergency.
Case presentation: A 62-year-old female with no past medical history presented to the emergency department
for dyspnea and lower extremity edema of 2 weeks duration. The patient was tachycardic at 120 BPM, hypertensive
at 197/90 mmHg. She had decreased breath sounds bilaterally. Electrocardiogram showed sinus tachycardia. Chest
x-ray revealed bilateral pulmonary infiltrates and effusions. Laboratory testing demonstrated a white blood cell count
of 18.06 TH/mm3, platelet count of 693 TH/mm3, D-dimer of 540 ng/ml, and a brain natriuretic peptide of 888pg/ml.
A lower extremity duplex was negative for venous thromboembolism. Computed tomography scan of the chest ruled
out pulmonary embolism. An Echocardiogram showed diffuse hypokinesis, and an estimated ejection fraction of 35
percent. Thyroid stimulating hormone, Urine and plasma metanephrines and renal artery duplex were done as part
of the workup. Renal ultrasound and arterial Doppler were negative for renal artery stenosis, but revealed a right
upper pole partially solid mass. An MRI of the abdomen confirmed a mass in the upper pole of the right kidney. Initial
laboratory tests showed elevated plasma Metanephrines at 8065 pg/ml and urine metanephrines at 1594 mcg/g.
The patient was started on Phenoxybenzamine. Surgical resection with histo-pathological examination performed 4
weeks later confirmed the diagnosis of pheochromocytoma.
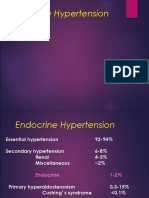
Discussion: Pheochromocytomas are rare tumors, associated with a number of cardiovascular complications.
The acute onset of severe congestive heart failure secondary to catecholamine overproduction is a rare entity, and is
associated with a poor prognosis.This case teaches us, that in patients presenting with heart failure with no obvious
cause, the diagnosis of pheochromocytoma should always be contemplated.
Keywords: Cardiomyopathy; Phechromocytoma blood tests showed white blood cell count of 18.06 TH/mm3 (reference
range 4.8-10.8 TH/mm3), platelets of 693 TH/mm3 (reference range 130-
Introduction 400 TH/mm3), D-dimer of 540 ng/ml (reference range: 0-230 ng/ml), and
Pheochromocytomas are rare catecholamine secreting tumors that BNP of 888 pg/ml (reference range 0-99 pg/ml). Her blood urea nitrogen,
arise from the chromaffine tissue of the adrenal medulla. The classic
triad of episodic headache, sweating, and tachycardia is frequently
absent [1,2]. Sustained or paroxysmal hypertension is the most common
sign, but approximately 5 to 15 percent of patients present with normal
blood pressure [3]. Rarely, pheochromocytomas are associated with
cardiomyopathy [4]. Patients may present with pulmonary edema and
may deteriorate with initiation of beta-adrenergic blockade [5]. We
herein present a patient with pheochromocytoma presenting initially
with pulmonary edema and hypertensive emergency.
Case Presentation
A 62 year old female, with no significant past medical or surgical
history presented to the emergency department for worsening
shortness of breath, orthopnea and lower extremity edema that have
Figure 1: Sinus tachycardia, with signs of left ventricular hypertrophy according
been ongoing for 2 weeks. This was preceded by an episode of upper
to the Sokolow-Lyon index: S in V1 + R in V5 or V6 ≥ 35 mm (≥7 large squares)
respiratory tract infection accompanied by myalgia and arthralgia. on 12 lead electrocardiogram.
History was also positive for a 20 pounds weight loss, and moderate
night sweats. The patient had taken antibiotics during the previous
week, with no improvement of respiratory symptoms. *Corresponding author: Halim El Hage, Staten Island University Hospital, 475
Seaview Avenue, Staten Island, New York, USA, Tel: 347-896-3584; E-mail:
On presentation the patient was afebrile, tachycardic at 120 halim.hage@gmail.com
BPM, and hypertensive at 197/90 mmHg. The physical exam showed
Received April 17, 2015; Accepted April 28, 2015; Published April 30, 2015
decreased breath sounds bilaterally, crackles in the lower lung fields
and bilateral pitting lower extremity edema. The rest of the exam was Citation: El Hage H, Karam B, Zaidan J, Charabaty EEl (2015) Congestive Heart
Failure: An Uncommon Presentation of Pheochromocytoma. J Clin Case Rep 5:
unremarkable. 524. doi:10.4172/2165-7920.1000524
Electrocardiogram on admission showed sinus tachycardia, with Copyright: © 2015 El Hage H, et al. This is an open-access article distributed under
signs of left ventricular hypertrophy, and no ischemic changes (Figure 1). the terms of the Creative Commons Attribution License, which permits unrestricted
use, distribution, and reproduction in any medium, provided the original author and
Chest x-ray revealed bilateral pulmonary effusions (Figure 2). Patient’s source are credited.
J Clin Case Rep Volume 5 • Issue 4 • 1000524
ISSN: 2165-7920 JCCR, an open access journal
Citation: El Hage H, Karam B, Zaidan J, Charabaty EEl (2015) Congestive Heart Failure: An Uncommon Presentation of Pheochromocytoma. J Clin
Case Rep 5: 524. doi:10.4172/2165-7920.1000524
Page 2 of 3
Figure 3: Kidney ultrasound showing a partially solid mass in right upper pole
of the kidney (arrow).
Figure 2: Portable chest X-ray showing bilateral pleural effusions (arrows),
and increased interstitial markings.
creatinine and electrolytes were within normal limits. A lower extremity
duplex at the bedside was negative for venous thromboembolism.
A computed tomography scan of the chest with contrast ruled out
pulmonary embolism, but showed bilateral moderate pleural effusions
and partially visualized ascites. An Echocardiogram then performed at
the bedside, showed moderate diffuse hypokinesis, with wall hypertrophy
and an estimated ejection fraction of 35-40 percent. The patient had no
previous history of heart disease. Antinuclear antibodies, erythrocyte
sedimentation rate, thyroid stimulating hormone, urine and plasma
metanephrines and renal artery duplex were done as part of the workup.
The patient was placed on a nitroglycerin infusion, loop diuretics, an
ACE inhibitor and transferred to the intensive care unit.
During her stay, her respiratory symptoms improved; however, she
had an episode of syncope while trying to get out of bed, and was found
to have orthostatic hypotension. A diagnostic cardiac catheterization
was performed and ruled out obstructive coronary disease. Renal artery
duplex was negative for renal artery stenosis, whereas ultrasound of the
abdomen revealed an incidental right upper pole partially solid mass
measuring 6.9 × 5.6 × 6.2 cm (Figure 3). This was completed by an
MRI of the abdomen, which confirmed the finding (Figure 4). Initial
laboratory workup done on admission showed a thyroid stimulating
hormone level of 1.4 uIU/ml (reference range 0.27-4.2 uIU/ml), plasma
total metanephrines of 8065 pg/ml (reference range ≤205 pg/ml),
Figure 4: MRI of the abdomen with a 6.9 × 5.6 × 6.2 cm enhancing mass in the
urine metanephrines of 1594 mcg/g (reference range 21-153 mcg/g), upper pole of the right kidney/adrenal gland (arrows).
erythrocyte sedimentation rate of 40 mm/hr (reference range 0-20
mm/hr), and a normal antinuclear antibodies titer <1:80. The patient
was started on Phenoxybenzamine. She was then discharged from an estimated ejection fraction of 60%. The patient was completely
the hospital in stable condition with planned surgical intervention in asymptomatic and was taken off her anti-hypertensive medications.
4 weeks. The tumor was resected surgically under general anesthesia
without significant complications. Histo-pathological examination Discussion
was positive for chromogranin, synaptophysin, S-100 (sustentacular Pheochromocytomas are rare tumors, affecting about 1 in 2500-
cells) without capsular invasion, significant mitotic activity, necrosis, or 6500 individuals, with 500-1600 cases diagnosed annually in the United
atypical histological features. The diagnosis of pheochromocytoma was States [6]. However, their true incidence may be higher owing to the
confirmed. Follow up at an outpatient clinic one-month later, revealed lack of diagnosis until post-mortem [7,8].
normalization of the blood pressure, and a repeat echocardiogram
showed improvement of the left ventricular systolic function with Pheochromocytomas are either sporadic or hereditary due to
J Clin Case Rep Volume 5 • Issue 4 • 1000524
ISSN: 2165-7920 JCCR, an open access journal
Citation: El Hage H, Karam B, Zaidan J, Charabaty EEl (2015) Congestive Heart Failure: An Uncommon Presentation of Pheochromocytoma. J Clin
Case Rep 5: 524. doi:10.4172/2165-7920.1000524
Page 3 of 3
underlying genetic mutations. Hereditary pheochromocytoma occurs 2. Baguet JP, Hammer L, Mazzuco TL, Chabre O, Mallion JM, et al. (2004)
Circumstances of discovery of phaeochromocytoma: a retrospective study of
with neurofibromatosis, multiple endocrine neoplasias (MEN 1 and 2),
41 consecutive patients. Eur J Endocrinol 150: 681-686.
von Hippel-Lindau syndrome, and familial paraganglioma syndromes
[9]. In patients with an established mutation or underlying hereditary 3. Manger WM, Gifford RW (2002) Pheochromocytoma. J Clin Hypertens
(Greenwich). 4: 62-72.
syndrome, the condition may manifest at a younger age than in those
with sporadic disease [7]. 4. Kassim TA, Clarke DD, Mai VQ, Clyde PW, Mohamed Shakir KM (2008)
Catecholamine-induced cardiomyopathy. Endocr Pract 14: 1137-1149.
In the elderly, pheochromocytomas are usually sporadic and 5. Sibal L, Jovanovic A, Agarwal SC, Peaston RT, James RA, et al. (2006)
may present without typical signs and symptoms. Instead, they may Phaeochromocytomas presenting as acute crises after beta blockade therapy.
present unexpectedly with acute onset stroke, heart failure in absence Clin Endocrinol (Oxf) 65: 186-190.
of coronary artery or valvular disease, arrhythmias and ketoacidosis 6. Chen H, Sippel RS, O’Dorisio MS, Vinik AI, Lloyd RV, et al. (2010) The
[10]. The classic triad of headache, palpitations, and paroxysmal North American Neuroendocrine Tumor Society consensus guideline for the
hypertension is not always present. Therefore recognition requires a diagnosis and management of neuroendocrine tumors: pheochromocytoma,
paraganglioma, and medullary thyroid cancer. Pancreas 39: 775-783.
high index of suspicion [11].
7. McNeil A, Blok B, Koelmeyer T, Burke M, Hilton J (2000) Phaeochromocytomas
These tumors have been associated with a number of cardiovascular discovered during coronial autopsies in Sydney, Melbourne and Auckland.
complications that result from excessive catecholamine secretion Australian and New Zealand journal of medicine. 30: 648-652.
[6]. Although rare, myocardial involvement includes paroxysmal or 8. Beard CM, Sheps SG, Kurland LT, Carney JA, Lie JT (1983) Occurrence of
sustained hypertension, angina pectoris, acute heart failure, dilated pheochromocytoma in Rochester, Minnesota, 1950 through 1979. Mayo Clin
cardiomyopathy, myocardial infarction and arrhythmias. Patients with Proc 58: 802-804.
pheochromocytoma usually have normal or increased ventricular 9. Lenders JW, Eisenhofer G, Mannelli M, Pacak K (2005) Phaeochromocytoma.
systolic function on echocardiography with only around 10% presenting Lancet 366: 665-675.
with catecholamine-induced cardiomyopathy [12]. The acute onset 10. Cooper ME, Goodman D, Frauman A, Jerums G, Louis WJ (1986)
of severe congestive heart failure secondary to catecholamine Phaeochromocytoma in the elderly: a poorly recognised entity? Br Med J (Clin
overproduction is a rare entity [13], and is usually associated with Res Ed) 293: 1474-1475.
a poor prognosis [14,15]. In one report, 5 of 6 patients with acute 11. Steppan J, Shields J, Lebron R (2011) Pheochromocytoma presenting as acute
pulmonary edema caused by pheochromocytoma died within 24 hours heart failure leading to cardiogenic shock and multiorgan failure. Case Rep
Med 2011: 596354.
of the acute event [15].
12. Park JH, Kim KS, Sul JY, Shin SK, Kim JH, et al. (2011) Prevalence and
The diagnosis is established via biochemical confirmation of patterns of left ventricular dysfunction in patients with pheochromocytoma. J
hormonal excess with urine and plasma metanephrines, followed Cardiovasc Ultrasound 19: 76-82.
by anatomical localization of the catecholamine-secreting tumors 13. Kelley SR, Goel TK, Smith JM (2009) Pheochromocytoma presenting as acute
with imaging in the correct clinical setting. That being said, severe congestive heart failure, dilated cardiomyopathy, and severe mitral
pheochromocytomas are increasingly being diagnosed incidentally on valvular regurgitation: a case report and review of the literature. Journal of
surgical education. 66: 96-101.
imaging tests performed for different reasons [7].
14. Szakacs J, Cannon A (1958) L-Norepinephrine myocarditis. American journal
Once the diagnosis of pheochromocytoma has been established, of clinical pathology. 30: 425.
the mainstay treatment is complete surgical resection of the tumor [16]. 15. Sardesai SH, Mourant AJ, Sivathandon Y, Farrow R, Gibbons DO (1990)
Before surgical excision, patient’s hemodynamics should be optimized Phaeochromocytoma and catecholamine induced cardiomyopathy presenting
with pharmacological agents to avoid perioperative complications. as heart failure. Br Heart J 63: 234-237.
Routine preoperative preparation consists of phenoxybenzamine; an 16. Bloemen OJ, De Koning M, Boot E, Booij J, van Amelsvoort T (2008)
α-adrenoceptor blocker started 7-14 days preoperatively [7]. The goal Challenge and therapeutic studies using alpha-methyl-para-tyrosine (AMPT)
is to suppress catecholamine excess in order to control blood pressure, in neuropsychiatric disorders: a review. Central Nervous System Agents in
Medicinal Chemistry (Formerly Current Medicinal Chemistry-Central Nervous
heart rate and volume status. β-Adrenergic receptor blockers are needed System Agents). 8: 249-256.
when catecholamine or α-blocker induced tachyarrhythmia occur.
Conclusion
The patient in this case presented with hypertensive emergency and
acute cardiogenic pulmonary edema, with no other previous symptoms
of pheochromocytoma. In patients presenting with heart failure
without an obvious cause, the diagnosis of pheochromocytoma should
be contemplated and worked up. Delay in diagnosis and treatment
could result in potential harm to the patient.
References
1. Kudva YC, Young Jr WF, Thompson GB, Grant CS, van Heerden JA (1999)
Adrenal incidentaloma: an important component of the clinical presentation
spectrum of benign sporadic adrenal pheochromocytoma. The endocrinologist
9: 77-80.
J Clin Case Rep Volume 5 • Issue 4 • 1000524
ISSN: 2165-7920 JCCR, an open access journal
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Uworld Step 3 Educational ObjectivesDocument4 pagesUworld Step 3 Educational Objectivesaap203Pas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Merck Microbiology Manual 12thDocument689 pagesMerck Microbiology Manual 12thChristian Denk95% (20)
- Pheochromocytoma PresentationDocument28 pagesPheochromocytoma PresentationMoriel PimentelPas encore d'évaluation
- Mnemonics For USMLE Step 1Document33 pagesMnemonics For USMLE Step 1Sara Sabra100% (9)
- AT1 Angiotensin Receptors - Vascular and RenalDocument5 pagesAT1 Angiotensin Receptors - Vascular and RenalLisandro KoyamaPas encore d'évaluation
- 1999 Storpirtis DeOliveira Rodrigues MaranhoDocument17 pages1999 Storpirtis DeOliveira Rodrigues MaranhoLisandro KoyamaPas encore d'évaluation
- 1 Congestive Heart Failure - An Uncommon Presentation of PheochromocytomaDocument3 pages1 Congestive Heart Failure - An Uncommon Presentation of PheochromocytomaLisandro KoyamaPas encore d'évaluation
- G2 - Clinical Pharmacology Relevant To Older Adults With Cardiovascular DiseaseDocument4 pagesG2 - Clinical Pharmacology Relevant To Older Adults With Cardiovascular DiseaseLisandro KoyamaPas encore d'évaluation
- Basic Laboratory Procedures in Clinical BacteriologyDocument175 pagesBasic Laboratory Procedures in Clinical BacteriologyAlyaa90% (10)
- Artigo: Medications As Asthma TriggersDocument22 pagesArtigo: Medications As Asthma TriggersLisandro KoyamaPas encore d'évaluation
- Adrenalectomy PDFDocument12 pagesAdrenalectomy PDFAnonymous uMjKQ0APMa100% (1)
- PHEOCHROMOCYTOMADocument28 pagesPHEOCHROMOCYTOMAQueenElsaPas encore d'évaluation
- Endocrine HTNDocument32 pagesEndocrine HTNatik mayasariPas encore d'évaluation
- FlushingDocument10 pagesFlushing林昌恩Pas encore d'évaluation
- Bexarotene Induced Central HypothyroidisDocument257 pagesBexarotene Induced Central HypothyroidisAnghel Ana-MariaPas encore d'évaluation
- Competency Appraisal 1 Disturbance in Metabolism EndocrineDocument46 pagesCompetency Appraisal 1 Disturbance in Metabolism EndocrineJohn Paul M. TagapanPas encore d'évaluation
- Rokh 2e ST4 PDFDocument141 pagesRokh 2e ST4 PDFMahmud DipuPas encore d'évaluation
- Chapterwise Question Bank-1Document188 pagesChapterwise Question Bank-1msreyaPas encore d'évaluation
- Pheochromocytoma and HyperaldosteronismDocument18 pagesPheochromocytoma and HyperaldosteronismMouhammad DawoudPas encore d'évaluation
- Pheochromocytoma Symptoms, Treatment, Diagnosis, TestDocument1 pagePheochromocytoma Symptoms, Treatment, Diagnosis, TestIulian GherasimPas encore d'évaluation
- Pheochromocytoma Poster FINALDocument1 pagePheochromocytoma Poster FINALJulie-Thuy Nguyen100% (1)
- IM - Facts From Case Files CRCDocument80 pagesIM - Facts From Case Files CRCridin007Pas encore d'évaluation
- Adrenal PathophysiologyDocument5 pagesAdrenal PathophysiologyditabokPas encore d'évaluation
- Pituitary Disorders - Adrenal Disorders - Thyroid DiseasesDocument207 pagesPituitary Disorders - Adrenal Disorders - Thyroid Diseasesnurliah armandPas encore d'évaluation
- 2016 Imitadores de PreeclmapsiaDocument9 pages2016 Imitadores de PreeclmapsiaMaria del Pilar Devis MoralesPas encore d'évaluation
- Questions Med SurgDocument6 pagesQuestions Med SurgMyung Dae ChoiPas encore d'évaluation
- SCE Practicaldiabetes - ElzohryDocument251 pagesSCE Practicaldiabetes - ElzohryAE100% (1)
- ADR PharmacologyDocument30 pagesADR PharmacologySumanth Kumar ReddyPas encore d'évaluation
- Adrenal and PheochromocytomaDocument86 pagesAdrenal and Pheochromocytomarajan kumar100% (1)
- Pheochromocytoma and Paraganglioma NEJMDocument14 pagesPheochromocytoma and Paraganglioma NEJMLeo AcPas encore d'évaluation
- Dr. Faiza Hashim SoomroDocument25 pagesDr. Faiza Hashim SoomroFaiza Hashim SoomroPas encore d'évaluation
- Hesi Exit Exam RN 2017 2018 Most Recent UpdatedDocument38 pagesHesi Exit Exam RN 2017 2018 Most Recent Updatedbhangglassilyihpok100% (12)
- Adrenal Tumor-Pheochromocytoma 10-10-19Document30 pagesAdrenal Tumor-Pheochromocytoma 10-10-19JessicaPas encore d'évaluation
- Disorders of The Adrenal Glands: Adrenal Cortical Adenoma and CarcinomaDocument9 pagesDisorders of The Adrenal Glands: Adrenal Cortical Adenoma and Carcinomahussain AltaherPas encore d'évaluation
- PheochromocytomaDocument97 pagesPheochromocytomajamestery100% (1)
- Hipertensioni Arterial Sekondar AutosavedDocument80 pagesHipertensioni Arterial Sekondar AutosavedFlo FlaPas encore d'évaluation
- PheochromocytomaDocument24 pagesPheochromocytomacamelle sisonPas encore d'évaluation