Académique Documents
Professionnel Documents
Culture Documents
Ankle Arthrodesis
Transféré par
ariearifinCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Ankle Arthrodesis
Transféré par
ariearifinDroits d'auteur :
Formats disponibles
Ankle Arthrodesis: Indications and Techniques
Nicholas A. Abidi, MD, Gary S. Gruen, MD, and Stephen F. Conti, MD
Abstract
Patients with ankle arthritis and deformity can experience severe pain and func- use of a walking cast has also been
tional disability. Those patients who do not respond to nonoperative treatment suggested as a trial device to evalu-
modalities are candidates for ankle arthrodesis, provided pathologic changes in ate patient acceptance and degree
the subtalar region can be ruled out. Several techniques are available for per- of pain relief prior to performing an
forming the procedure; the most successful combine an open approach with ankle arthrodesis.15
compression and internal fixation. The foot must be positioned with regard to Nonsteroidal anti-inflammatory
overall limb alignment and in the optimal position for function. A nonunion drugs can be helpful in relieving
rate as high as 40% has been reported. Osteonecrosis of the talus and smoking ankle pain. If long-term use is ex-
are known risk factors for nonunion. When good surgical technique is used in pected, patients should be screened
carefully selected patients, ankle arthrodesis can be a reliable procedure for the for contraindications, and appropri-
relief of functionally disabling ankle arthritis, deformity, and pain. ate blood and urine studies should
J Am Acad Orthop Surg 2000;8:200-209 be performed. Intra-articular injec-
tions of corticosteroid-anesthetic
combinations can be used to de-
crease joint pain and inflammation,
The ankle joint consists of a highly and functional disability. A variety but the injections should be at least
constrained articulation of the talus of techniques for ankle arthrodesis 3 months apart.
with the tibial plafond and the dis- have been described over the years Arthroscopic ankle-joint debride-
tal fibula. With weight bearing, as surgical measures to relieve the ment may temporarily relieve the
congruity between the sulcus of the pain and functional disability associ- symptoms of early arthritis. This
talus and the tibial plafond pro- ated with a damaged ankle joint.1-14 technique permits direct visualiza-
vides stability in the sagittal plane tion of intra-articular and intracap-
in a normal ankle joint. Torn or sular structures, thus allowing accu-
detached ligaments around the Treatment of the
ankle joint, however, allow abnor- Symptomatic Ankle Joint
mal coronal-plane instability with
weight bearing. Nonoperative treatment of a symp- Dr. Abidi is Assistant Professor of Orthopaedic
Surgery, Jefferson Medical College, Thomas
The deep deltoid ligament carries tomatic degenerative ankle joint in- Jefferson University, and Chief, Division of
the primary blood supply to the cludes the use of shoe inserts or Orthopaedic Foot and Ankle Surgery, Rothman
medial aspect of the body of the shoe modifications. A shoe with a Institute, Philadelphia. Dr. Gruen is Associate
talus from the posterior tibial artery. cushioned heel and a stiff, rocker- Professor and Chief, Division of Orthopaedic
Therefore, at least on a theoretical bottom sole usually helps patients Trauma Surgery, University of Pittsburgh
Medical Center, Pittsburgh. Dr. Conti is Asso-
basis, an effort should be made to with less severe ankle-joint dam- ciate Professor and Chief, Division of Foot and
preserve the deltoid ligament dur- age.15 If more support is needed, Ankle Surgery, University of Pittsburgh Medi-
ing surgical procedures on or about the use of a molded ankle-foot cal Center.
the ankle joint. orthosis or a double-upright type of
Damage to the ankle joint from brace attached to the patientÕs shoe Reprint requests: Dr. Gruen, Department of
trauma or disease can result in pro- can be used. Such a brace tends to Orthopaedic Surgery, University of Pittsburgh
Medical Center, Suite 911 Kaufmann Building,
gressive loss of the tibiotalar articu- decrease joint inflammation and 3471 Fifth Avenue, Pittsburgh, PA 15213.
lar cartilage surface, with resulting pain by restricting ankle-joint mo-
inflammation, synovitis, osteophyte tion. Some patients are helped by Copyright 2000 by the American Academy of
formation, progressive loss of ankle- supporting the arthritic ankle joint Orthopaedic Surgeons.
joint motion, weight-bearing pain, in a walking cast for 6 weeks. The
200 Journal of the American Academy of Orthopaedic Surgeons
Nicholas A. Abidi, MD, et al
rate diagnostic evaluation and the Factors that determine whether Clinical results support the con-
opportunity for immediate thera- ankle reconstruction is a viable cept that late reconstruction of a
peutic intervention. Removal of option include the condition of the malunited ankle provides pain
loose osteochondral fragments or articular cartilage at the time of revi- relief and improved patient func-
impinging osteophytes by arthrot- sion and the quality of fracture tion.19,21,23-25 Reconstruction most
omy or arthroscopy can provide reduction. Other variables, such as frequently involves fibular or tibial
effective relief of pain. 16 Several length of time from injury to the osteotomy, but may be combined
large series have documented a reconstructive procedure and the age with syndesmotic stabilization as
high incidence of impinging spurs of the patient at time of presentation, well.
in football players (up to 45%)17 and have not been shown to influence
in dancers (up to 59.3%).18 Because outcome. Anatomic reconstruction
this entity is frequently encountered of a malunited ankle joint will pre- Indications for
in athletes, it has been referred to as vent further progression of ankle Arthrodesis
ÒathleteÕs ankleÓ and ÒfootballerÕs arthritis, even in the presence of
ankle.Ó17 The suspected mechanism early disease.21 Furthermore, precise The principal indication for ankle
consists of extreme ankle dorsiflex- restoration of ankle-joint anatomic arthrodesis is persistent ankle-joint
ion with resultant anterior joint relationships is critical to a successful pain and stiffness that is functionally
impingement and posterior joint outcome. In one series,22 good to ex- disabling to the patient and is not
distraction. It is theorized that re- cellent results were achieved in 85% alleviated by nonoperative treat-
petitive anterior ankle impingement of patients after reconstruction of ment methods. This may be the
causes anterior subperiosteal hem- ankle malunions. Factors associated result of previous fracture, infec-
orrhages and subsequent sclerotic with favorable patient outcome in- tion, osteonecrosis, or arthritis.
bone growth. cluded position of the talus in the Radiographic changes in the
Periarticular osteotomy and syn- mortise, stability of the syndesmosis, ankle joint are best assessed on
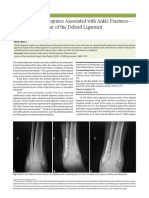
desmotic reconstruction for mal- correct length of the fibula, and qual- weight-bearing standing anteropos-
united ankle fractures is a treat- ity of the joint surface at the time of terior (Fig. 1, A), lateral (Fig. 1, B),
ment alternative for patients who reconstruction. and mortise views. Computed
do not demonstrate joint-space col-
lapse on weight-bearing radio-
graphs. Symmetry of the tibiotalar
joint space must be maintained,
and the seating of the fibula in the
incisura fibularis of the tibia must
be evaluated. The two findings
most often cited as indicators of
abnormal relationships are (1) di-
minished overlap of the distal fibu-
la and anterior aspect of the tibia
and (2) excessive widening of the
tibiofibular clear space. A signifi-
cant and frequent component of
ankle fracture malunion is rotation
and shortening of the fibula. 19
Ankle malalignment secondary to
malreduction or impingement re-
sults in shifting of the talus, persis-
tent instability, and valgus tilt. As
little as 1 mm of lateral talar dis-
placement has been demonstrated
to alter tibiotalar contact by as A B
much as 40%. 20 With the loss of
Figure 1 Weight-bearing anteroposterior (A) and lateral (B) radiographs of the ankle
joint congruity, damage to the car- show complete joint-space collapse, valgus malalignment, and an old medial malleolar
tilage surface occurs progressively fracture.
over time.
Vol 8, No 3, May/June 2000 201
Ankle Arthrodesis
tomography, alone or in combina- the externally rotated gait that placed into the medial aspect of the
tion with arthrography, can be use- patients adopt to avoid Òrolling tibia, the calcaneus, and the neck of
ful for assessing joint-surface overÓ a plantar-flexed foot.26 the talus and are of larger diameter
defects, degenerative joint changes, than those used with the Calan-
and the location of osteophytes. External Fixation druccio device. Compression can
The bones of the subtalar complex Before CharnleyÕs report in 1951 be exerted across the arthrodesis
(the talocalcaneal, talonavicular, on the results obtained with a com- site by adding a compression de-
and calcaneocuboid joints) should pression arthrodesis technique vice to the external fixator appara-
be in normal alignment and without involving use of an external fixator, tus prior to placement on the pa-
arthritic changes. A bone scan or ankle arthrodesis was associated tient.
selective joint injections can help to with high rates of failure because of
determine whether joints other than nonunion.2 The Charnley method Arthroscopic Arthrodesis
the tibiotalar joint have degenera- combined open surgical debride- The intra-articular portion of an
tive changes. Following a success- ment of the ankle-joint cartilage ankle fusion can be done with an
ful ankle arthrodesis, it has been with the application of an external arthroscope, but this technique
shown that motion in the subtalar fixator by placing one pin through should be limited to patients with
complex increases by an average of the tibia and another through the arthritic ankles with minimal de-
11 degrees during the first year.6 neck of the talus, with connecting formity, because it is difficult to
bars running between the two pins. correct ankle deformity arthroscop-
Compression across the arthrodesis ically.8 For this technique, arthros-
Surgical Techniques site relies on an intact Achilles ten- copy is performed through two or,
don functioning as a tension band. occasionally, three portals. One
Selection of the surgical technique Patients are allowed to bear weight portal is medial to the tibialis ante-
should be based on the underlying on the treated ankle during the first rior tendon, and the other is lateral to
disorder. As a general rule, exter- 8 weeks after surgery. After re- the extensor digitorum longus ten-
nal fixators are preferred for pa- moval of the external fixator, pa- don. A third portal can be placed
tients undergoing arthrodesis for a tients are immobilized in a plaster lateral to the peroneus tertius tendon
preexisting septic joint and for walking cast for an additional 4 and can then be used to remove
those with severe osteopenia. Ar- weeks. debris generated during articular-
throscopic arthrodesis or the Òmini- The Calandruccio external fixa- surface denuding.
openÓ arthrodesis should be used tor makes use of a triangular con- The joint space is widened with
only for patients with minimal figuration to achieve stability and a noninvasive distractor or a unilat-
deformity. Open arthrodesis is ap- compression across the tibiotalar eral external fixator. A 4.5-mm bur
propriate for patients with signifi- joint,4 which provides added resis- and curettes are used to denude the
cant ankle deformity and foot and tance to torsional forces at the ankle articular surfaces. After prepara-
ankle malalignment. joint. After surgical removal of the tion, compression of the joint sur-
Regardless of the surgical tech- ankle-joint articular cartilage, fixa- faces can be obtained with either
nique chosen, the optimal postoper- tion pins are placed through the internal or external fixation. Pref-
ative position of the affected foot tibia, through the neck and body of erably, two cannulated screws are
and ankle joint is the same.26 The the talus, and, occasionally, into the placed across the tibia into the
foot should be externally rotated 20 calcaneus. The fusion site is then talus. The first screw runs from the
to 30 degrees relative to the tibia,27 buttressed with bimalleolar onlay lateral aspect of the tibia into the
with the ankle joint in neutral flex- bone grafts. This external fixator neck of the talus. The second screw
ion (0 degrees), 5 to 10 degrees of technique does not require an intact runs from the medial malleolus into
external rotation, and slight valgus Achilles tendon to serve as a ten- the lateral aspect of the talus.
(5 degrees). This position provides sion band. Patients are kept in non-weight-
the best extremity alignment and A simplified alternative method bearing status for 5 weeks postop-
accommodation of hip and knee of external fixation with the use of eratively and then are allowed to
motion. Fusion of the ankle in a unilateral frame was reported in bear weight progressively until
plantar-flexion results in genu 1994. 13 This method appears to joint fusion is demonstrated radio-
recurvatum when placing the foot provide adequate resistance to both graphically.
flat on the floor and subsequent lax- dorsiflexion and plantar-flexion In an attempt to achieve the
ity of the medial collateral ligament forces at the tibiotalar joint. The advantages of both the open and
of the knee, which develops from unilateral external fixator pins are arthroscopic techniques, a Òmini-
202 Journal of the American Academy of Orthopaedic Surgeons
Nicholas A. Abidi, MD, et al
openÓ technique was reported in third of the medial malleolus. Both arthrodesis site and assists in pre-
1996. 11 This technique decreases exposures are carried out carefully venting lateral drifting of the talus.
reliance on regular arthroscopic to maintain full-thickness flaps and Sharp dissection is used through
techniques in favor of using to identify and protect tendons and the lateral incision to elevate the
enlarged arthroscopic portals for neurovascular structures. After the scarred ankle capsule from the joint
exposure and removal of articular distal 10 cm of the fibula has been both anteriorly and posteriorly,
cartilage. Curettes and osteotomes exposed, the superior peroneal reti- thus allowing the vital structures
are used to denude the joint sur- naculum is incised posteriorly, and on both sides of the ankle joint to be
faces. This technique reportedly de- the peroneal tendons are mobilized protected by retractors. Soft-tissue
creases the amount of soft-tissue while protecting the sural and su- protection is provided through the
stripping required in the more perficial peroneal nerves. medial incision by a retractor. A
standard open techniques and is A small acetabular reamer can be large oscillating saw is used to
reported to be associated with used to morselize the fibula for bone make a cut perpendicular to the tib-
quicker radiographic fusion rates. graft material prior to its removal. A ial shaft at the level of the apex of
micro-oscillating saw is used to the dome of the articular surface,
Open Arthrodesis make an oblique osteotomy 10 cm allowing removal of the tibial pla-
The open ankle arthrodesis is from the fibular tip (Fig. 2, A). The fond (Fig. 2, B). An attempt should
performed through a two-incision remaining fibular fragment can then be made to preserve the medial
transfibular exposure. This tech- be excised. Alternatively, the distal malleolus so as to provide an area
nique can be used for any patient fibular soft-tissue attachment can be of solid fixation for the lateral-to-
but is particularly useful for patients preserved if the fibula has not been medial screw and to preserve the
with severe ankle-joint deformity. morselized. The medial half of the medial blood supply to the talus
Its benefits are better visualization fibula is cut away, and the remaining through the deltoid ligament.28
of the joint and improved access for fibula is turned down and away After removal of the distal tibial
bone resection, correction of defor- from the arthrodesis site. The blood articular surface, the talus is posi-
mity, and screw placement. Its supply is maintained because of the tioned so that the forefoot is in 5 to
drawbacks are the large incisions remaining ligamentous attachments. 10 degrees of external rotation and
and the amount of soft-tissue strip- The outer half of the fibula is secured the hindfoot is in 5 degrees of val-
ping required. to the tibia and the talus with two gus, with neutral dorsiflexion and
The first incision is made directly 3.5-mm screws later during the pro- displacement so that the posterior
over the fibula, and the second in- cedure. This lateral buttress gives margins of the talus and tibia are
cision is made along the anterior additional lateral stability to the flush. The foot must be aligned
A B
Figure 2 A, Through the lateral incision, the fibula is osteotomized 10 cm proximal to the tip with a micro-oscillating saw. The arrow
marks the distal fibula. B, Through the lateral approach, the distal articular surface of the tibia is removed at a 90-degree angle to the tib-
ial shaft with an oscillating saw. The arrow marks the distal tibia.
Vol 8, No 3, May/June 2000 203
Ankle Arthrodesis
with regard to the entire limb. A
cut through the dome of the talus is
then made parallel to the distal
tibia, resecting approximately 5 mm
of the talus. Alternatively, the joint
surfaces can be prepared with cu-
rettes and osteotomes. The remain-
ing joint surfaces are inspected
carefully for residual cartilage and
sclerotic bone. All joint surfaces are
drilled or curetted until bleeding
bone is noted. The fibula may be
used as a strut graft or as crushed
cancellous autograft to fill deep de-
fects if it has been morselized.
The talus is apposed flush to the A B
distal tibia. After the surface congru-
ency and joint position have been
checked, the joint position is secured
with two guide pins for large (7.0- to
7.3-mm) cannulated screws. The first
pin is started at the posterolateral cor-
ner of the tibia and is placed across
the joint and into the neck of the talus.
The second guide pin is placed from
the medial malleolus into the lateral
aspect of the talus. Alternatively, the
second pin may be placed from the
lateral process of the talus into the
medial cortex of the tibia. Pin place-
ment and bone apposition are
checked under fluoroscopy (Fig. 3, A
and B). Care must be taken that the
pins do not violate the subtalar joint. C D
Once pin placement and bone ap-
position have been found to be satis- Figure 3 Anteroposterior (A) and lateral (B) images obtained during fluoroscopy of the
ankle joint with guide pins in place confirm surface apposition. Anteroposterior (C) and
factory, short threaded cannulated lateral (D) views obtained after screw placement demonstrate that there is no penetration
screws with washers are placed into of the subtalar joint space.
the bone (Fig. 3, C and D). The
wounds are closed with a two-layer
technique, taking care to protect the
adjacent nerves. The extremity is unions after previous arthrodesis almost all fusion techniques used in
placed in a bulky cast padding and a attempts, or with neuropathic ankle these difficult situations.
plaster splint dressing, which is joints. Patients with symptomatic A technique for tibiotalocalcaneal
maintained for 2 weeks. A non- nonunions, osteonecrosis of the arthrodesis with the use of an angled
weight-bearing short leg cast is then talus, or Charcot arthropathy fre- blade-plate inserted through a poste-
applied, and weight bearing is not quently require substantial debride- rior approach was reported in 1991.29
permitted until evidence of ar- ment of devitalized bone from the This technique was proposed for use
throdesis is observed on the follow- talus. Bone grafting can be used in in patients with persistent ankle-joint
up radiographs, which usually oc- these patients to regain some of the nonunion. With the patient in the
curs 8 to 12 weeks postoperatively. lost height, but often tibiotalocal- prone position, the Achilles tendon is
The arthrodesis technique must caneal arthrodesis is required to osteotomized at its insertion into the
be modified for patients with com- achieve a successful fusion. More calcaneus and displaced cephalad
promised soft tissues, with non- rigid internal fixation is a part of with its attached bone block (Fig. 4).
204 Journal of the American Academy of Orthopaedic Surgeons
Nicholas A. Abidi, MD, et al
patients with nonbraceable neuro- drawbacks of retrograde nail fixa-
Achilles pathic ankle joints were reported tion include the risk of neurologic
tendon in 1994.30 A cannulated humeral and vascular injury during nail
Blade- blade-plate was placed into the insertion (Fig. 6, A),33 difficulty in
plate tibia and calcaneus through a later- providing compression across the
al approach for rigid fixation, aug- arthrodesis site, placement of
mented by an external compres- screws in the osteoporotic talus and
sion device and large cancellous calcaneus (Fig. 6, B), and stress frac-
screws (Fig. 5). The seven patients ture of the tibia after operation.34
in this series progressed to solid
fusion in an average of 5.2 months.
All became ambulatory in a lined, Results
Calcaneus molded bivalve ankle-foot arthro-
sis without the use of an ancillary Ankle arthrodesis, which was origi-
Figure 4 The posterior approach (with the device. nally a surgical treatment for tuber-
patient in the prone position) for blade- Mechanical difficulties reported culosis of the ankle joint, continues
plate insertion directly through the bed of
the Achilles tendon for the patient with pre-
with blade-plate techniques include to find use in patients functionally
existing anterior or lateral soft-tissue com- difficulty in placing the foot and disabled by ankle-joint destruction
promise who requires arthrodesis. (Re- ankle in the optimal functional due to a variety of causes. Several
produced with permission from Gruen GS,
Mears DC: Arthrodesis of the ankle and
position and difficulty associated scoring systems now are available
subtalar joints. Clin Orthop 1991;268:15-20.) with accurate placement of the to provide standardized methods of
blade-plate into a small talus and evaluating and comparing func-
calcaneus. The use of a retrograde tional results both before and after
intramedullary nail has been de- operative treatment as well as be-
After ankle-joint exposure, articular scribed for patients with soft-tissue tween the various techniques avail-
cartilage is removed from the joint compromise, failed prior arthrode- able for ankle arthrodesis. The
surfaces. The nonunion site is curet- sis, or diabetic neuropathy.31,32 The American Orthopaedic Foot and
ted until viable bone is seen. Autolo-
gous cancellous bone graft, harvested
from the proximal tibial metaphysis
or iliac crest, is packed into the non-
union site and the denuded joint.
After proper joint alignment has
been achieved, a 95-degree 50-mm
five-hole blade-plate is seated into an
appropriate slot prepared in the sur-
face of the posterior calcaneus. After
application of the tension device to
the free end of the plate, the screws
are inserted into the plate, and the
Achilles tendon is reattached to the
calcaneus with a 6.5-mm cancellous
screw and ligamentous washer. A
short windowed leg cast with a rock-
er bottom is applied on the third
postoperative day, and touch-down
gait is allowed for the next 6 to 8
weeks, progressing to weight bear-
ing as tolerated. The total cast-
immobilization time after this proce- A B
dure averages 12 to 16 weeks.
Figure 5 A, Intraoperative lateral view of a tibiotalocalcaneal arthrodesis with placement
The results with use of a com- of a 90-degree blade-plate guide and large cancellous-screw guide pins prior to blade-plate
pression arthrodesis technique for impaction. B, Lateral radiograph obtained after insertion of lateral blade-plate.
tibiocalcaneal arthrodesis in seven
Vol 8, No 3, May/June 2000 205
Ankle Arthrodesis
The same system was used by
Scranton12 in 1985 to evaluate inter-
nal compression in arthrodesis of
the ankle. Scranton used a T plate
medially for compression of the
ankle arthrodesis site. His patients
achieved functional improvement
from an average preoperative score
of 47 points to an average postop-
erative score of 82 points. A simi-
lar study reporting the use of an
anterior tension-band plate showed
an average postoperative score of
only 70 points, suggesting that this
technique may not be as successful
as others.7
Lateral
plantar In 1991, Malarkey and Binski 4
artery reported the results in 12 patients
and nerve who had undergone ankle arthro-
desis with use of the Calandruccio-
Plantar frame external fixator and bimalleo-
incision
lar onlay grafting. Eleven patients
achieved a solid osseous union.
A B Eight patients were available for
evaluation; the results in 6 were
Figure 6 A, Plantar retrograde nail insertion site at the junction of the calcaneal body and
the sustentaculum, adjacent to the lateral plantar neurovascular bundle. B, Retrograde
rated as good or excellent, and those
nail insertion, with placement of one screw into the talus and one screw into the calcaneus, in the other 2 were rated as poor (1
accompanied by insertion of bone graft at the tibiotalar arthrodesis site and impaction of patient with nonunion and 1 patient
the construct before screw placement into the tibia. (Reproduced with permission from
Paul Cooper, MD, and DePuy ACE Medical Company, El Segundo, Calif.)
not rated because of underlying dis-
ease that limited ambulation).
In 1991, Myerson and Quill 8
evaluated the results obtained with
Ankle Society has published a 100- to 9 years previously. The outcome arthroscopic ankle arthrodesis
point scoring system for the evalua- was graded as excellent in 61% of compared with conventional open
tion of ankle and hindfoot pain and the patients, good in 18%, fair in arthrodesis performed with use of
function (Table 1).35 The most re- 19%, and poor in 2%. Six patients 6.5- and 7.0-mm screws. Joint fu-
cent scoring system introduced for had a limp, and 2 had persistent sion was achieved an average of 8.7
assessing patients with osteoarthri- pain because of unrecognized sub- weeks after arthroscopic arthrode-
tis of the ankle is the ÒAnkle Osteo- talar arthritis. A high rate of com- sis, compared with an average of
arthritis Scale,Ó which is based on a plications related to pin-track infec- 14.5 weeks after arthrodesis with
visual analog scale completed by tions was noted in this series of conventional internal fixation.
the patient.36 Unfortunately, nei- patients. However, the patients who under-
ther has yet been used to assess the An early scoring system for as- went arthroscopic arthrodesis had
functional results in a large series of sessment of patient function and gait arthritic ankles with only minimal
patients with ankle arthrodesis. after ankle arthrodesis was pub- deformity, whereas those for whom
Prior to 1979, the results ob- lished by Mazur et al37 in 1979. This the open technique was chosen had
tained with ankle arthrodesis were system is based on a maximum pos- more severe deformities.
generally graded as good if ar- sible score of 90 points. The patients The results of arthrodesis in pa-
throdesis was achieved or poor if who were evaluated in that report tients who require revision are more
nonunion resulted. In 1959 Ratliff had an average preoperative score of difficult to evaluate because of the
reported retrospectively on 59 pa- 40 points and an average postopera- small number of patients in reported
tients who had undergone com- tive score of 80 points, reflecting an series. In one study,29 five patients
pression arthrodesis of the ankle improvement in patient function underwent revision arthrodesis for
with a Charnley external fixator 1 after ankle arthrodesis. nonunion in which an angled blade-
206 Journal of the American Academy of Orthopaedic Surgeons
Nicholas A. Abidi, MD, et al
plate was inserted through a poste-
Table 1 rior approach for tibiotalar, tibio-
American Foot and Ankle Society Clinical Ankle-Hindfoot Rating Scale*
talocalcaneal, or tibiocalcaneal
arthrodesis. All five progressed to
Total solid ankle fusion after 16 weeks.
Possible
On a modified Boston ChildrenÕs
Criterion Points Points
Hospital rating scale, the average
preoperative rating of the five
Pain 40
None 40 patients was 13 points (of a possible
Mild, occasional 30 50 points), and the average postoper-
Moderate, daily 20 ative rating was 44 points. Three pa-
Severe, almost always present 0 tients subjectively rated their result
as excellent, and two rated it good.
Function 50 The use of a combined open-
Activity limitations, support requirement
compression arthrodesis technique
No limitations, no support 10
No limitation of daily activities, limitation of
in a subsequent report dealing with
recreational activities, no support 7 nonbraceable neuropathic ankle
Limited daily and recreational activities, cane use 4 joints resulted in solid fusion in all
Severe limitations of daily and recreational seven patients at an average of 5.2
activities; use of walker, crutches, wheelchair, brace 0 months.31 All became ambulatory
Maximum walking distance, blocks in a lined, molded bivalve ankle-
Greater than 6 5 foot arthrosis without the use of an
4 to 6 4 ancillary device.
1 to 3 2
Less than 1 0
Walking surfaces
No difficulty on any surface 5
Risk Factors for Nonunion
Some difficulty on uneven terrain, stairs,
Ankle arthrodesis is a technically
inclines, ladders 3
Severe difficulty on uneven terrain, stairs, inclines, ladders 0 difficult surgical procedure that is
Gait abnormality frequently associated with complica-
None, slight 8 tions. Patients being considered for
Obvious 4 ankle arthrodesis should be screened
Marked 0 carefully for identifiable risk factors.
Sagittal motion (flexion plus extension) Even in series combining an open
Normal or mild restriction (30¡ or more) 8 approach with internal fixation,
Moderate restriction (15¡ to 29¡) 4 compression, and bone grafting, the
Severe restriction (less than 15¡) 0 most frequently encountered compli-
Hindfoot motion (inversion plus eversion)
cation associated with ankle arthrod-
Normal or mild restriction (75% to 100% of normal) 6
esis was nonunion.
Moderate restriction (25% to 74% of normal) 3
Marked restriction (less than 25% of normal) 0 In one study, Frey et al 38 re-
Ankle-hindfoot stability (anteroposterior, varus-valgus) viewed 78 ankle arthrodeses to
Stable 8 identify factors that might predis-
Definitely unstable 0 pose patients to nonunion. Compli-
cations occurred in 44 (56%) of the
Alignment 10 78 patients at an average follow-up
Good, plantigrade foot, ankle-hindfoot well aligned 10
interval of 4 years. These included
Fair, plantigrade foot, some degree of ankle-hindfoot
malalignment observed, no symptoms 5
32 nonunions (41%), 7 infections
Poor, nonplantigrade foot, severe malalignment, symptoms 0 (9%), 2 nerve injuries (3%), 2 mal-
unions (3%), and 2 wound problems
100 (3%). Risk factors associated with
nonunion in this series included a
* Adapted with permission from Kitaoka HB, Alexander IJ, Adelaar RS, Nunley JA, severe fracture, an open injury, local
Myerson MS, Sanders M: Clinical rating systems for the ankle-hindfoot, midfoot, hal- infection, evidence of osteonecrosis
lux, and lesser toes. Foot Ankle Int 1994;15:349-353.
of the talus, and coexisting major
Vol 8, No 3, May/June 2000 207
Ankle Arthrodesis
medical problems. Factors not asso- effects from the patient has not externally rotating the ankle by 5 to
ciated with nonunion included been established, but 1 week has 10 degrees, and displacing the talus
patient age, past history of undergo- been empirically suggested.40 posteriorly. Appropriate position-
ing a subtalar or triple arthrodesis, A careful attempt should be ing of the foot during arthrodesis
and the surgical arthrodesis tech- made to try to learn the reason for helps to avoid altering the patientÕs
nique selected. A prior diagnosis of nonunion in patients in whom revi- gait significantly and also helps to
a combined plafond-talus fracture sion surgery is contemplated. This preserve hip and knee function.
led to the worst prognosis, followed should include a complete workup Several surgical techniques for
by Hawkins II or III talar fractures. to rule out local infection and to performing ankle arthrodesis are
Large-fragment screw fixation led to attempt to identify associated risk available. External fixators are rec-
higher fusion rates, possibly be- factors that might compromise a ommended for fixation in patients
cause less soft-tissue stripping was successful outcome. undergoing arthrodesis because of a
required for screw fixation com- preexisting septic joint or osteope-
pared with plating or possibly be- nia. Arthroscopic arthrodesis or the
cause these screws provide better Summary Òmini-openÓ arthrodesis can be con-
compression at the arthrodesis site. sidered for patients with minimal
Nonunion after ankle arthrode- A thorough history and physical deformity. Open arthrodesis is
sis has also been associated with examination will help to determine advisable for patients with signifi-
smoking. 39 In patients without which form of treatment will pro- cant ankle deformity and foot and
other risk factors, the risk of non- vide pain relief and improved func- ankle malalignment. Nonunion of
union in smokers has been estimat- tion in a patient with advanced ankle arthrodeses can occur in up to
ed to be 16 times the risk of non- ankle arthritis. If nonoperative 40% of patients. Smoking cessation,
union in nonsmokers. The effects treatment measures fail, operative awareness and control of known
of nicotine on the peripheral circu- intervention should be considered. risk factors such as metabolic dis-
lation and the effects of hydrogen Careful examination of all lower- eases and osteonecrosis, careful pre-
cyanide and carbon monoxide on extremity joints, limb alignment, operative planning, and meticulous
the oxygen-carrying capacity of and the relationship of the hindfoot operative technique all contribute to
hemoglobin have been cited as pos- to the forefoot, as well as gait ap- a successful outcome.
sible causes of the high rate of praisal, should be carried out pre-
nonunion in smokers. The period operatively. A plantigrade foot po- Acknowledgment: The authors would like
of smoking cessation prior to ankle sition can be obtained by placing to thank John J. Gartland, MD, for his assis-
surgery necessary to clear the toxic the heel in 5 to 7 degrees of valgus, tance in the preparation of this manuscript.
References
1. Barr JS, Record EE: Arthrodesis of the talar arthrodesis. J Bone Joint Surg Am 12. Scranton PE Jr: Use of internal com-
ankle joint: Indications, operative tech- 1985;67:546-550. pression in arthrodesis of the ankle. J
nic and clinical experience. N Engl J 7. Mears DC, Gordon RG, Kann SE, Bone Joint Surg Am 1985;67:550-555.
Med 1953;248:53-56. Kann JN: Ankle arthrodesis with an 13. Thordarson DB, Markolf KL, Crac-
2. Charnley J: Compression arthrodesis anterior tension plate. Clin Orthop chiolo A III: External fixation in
of the ankle and shoulder. J Bone Joint 1991;268:70-77. arthrodesis of the ankle: A biomechan-
Surg Br 1951;33:180-191. 8. Myerson MS, Quill G: Ankle arthro- ical study comparing a unilateral
3. Holt ES, Hansen ST, Mayo KA, San- desis: A comparison of an arthroscopic frame with a modified transfixion
georzan BJ: Ankle arthrodesis using and an open method of treatment. frame. J Bone Joint Surg Am 1994;76:
internal screw fixation. Clin Orthop Clin Orthop 1991;268:84-95. 1541-1544.
1991;268:21-28. 9. Ratliff AHC: Compression arthrodesis 14. Wang GJ, Shen WJ, McLaughlin RE,
4. Malarkey RF, Binski JC: Ankle ar- of the ankle. J Bone Joint Surg Br 1959; Stamp WG: Transfibular compression
throdesis with the Calandruccio frame 41:524-534. arthrodesis of the ankle joint. Clin
and bimalleolar onlay grafting. Clin 10. Newman A: Ankle fusion with the Orthop 1993;289:223-227.
Orthop 1991;268:44-48. Hoffmann external fixation device. 15. Scranton PE Jr: An overview of ankle
5. Mann RA, Van Manen JW, Wapner K, Foot Ankle 1980;1:102-109. arthrodesis. Clin Orthop 1991;268:96-101.
Martin J: Ankle fusion. Clin Orthop 11. Paremain GD, Miller SD, Myerson MS: 16. Scranton PE Jr, McDermott JE: An-
1991;268:49-55. Ankle arthrodesis: Results after the terior tibiotalar spurs: A comparison
6. Morgan CD, Henke JA, Bailey RW, miniarthrotomy technique. Foot Ankle of open versus arthroscopic debride-
Kaufer H: Long-term results of tibio- Int 1996;17:247-252. ment. Foot Ankle 1992;13:125-129.
208 Journal of the American Academy of Orthopaedic Surgeons
Nicholas A. Abidi, MD, et al
17. McMurray TP: FootballerÕs ankle. J 25. Yablon IG, Leach RE: Reconstruction of ographic and anatomic analysis. Foot
Bone Joint Surg Br 1950;32:68-69. malunited fractures of the lateral malle- Ankle Int 1997;18:233-235.
18. Stoller SM, Hekmat F, Kleiger B: A olus. J Bone Joint Surg Am 1989;71:521-527. 34. Lidor C, Ferris LR, Hall R, Alexander
comparative study of the frequency of 26. Buck P, Morrey BF, Chao EYS: The opti- IJ, Nunley JA: Stress fracture of the
anterior impingement exostoses of the mum position of arthrodesis of the ankle: tibia after arthrodesis of the ankle or
ankle in dancers and nondancers. Foot A gait study of the knee and ankle. J the hindfoot. J Bone Joint Surg Am
Ankle 1984;4:201-203. Bone Joint Surg Am 1987;69:1052-1062. 1997;79:558-564.
19. Weber BG: Lengthening osteotomy of 27. Mann RA: Biomechanical approach to 35. Kitaoka HB, Alexander IJ, Adelaar RS,
the fibula to correct a widened mortice the treatment of foot problems. Foot Nunley JA, Myerson MS, Sanders M:
of the ankle after fracture. Int Orthop Ankle 1982;2:205-212. Clinical rating systems for the ankle-
1981;4:289-293. 28. Mann RA, Rongstad KM: Arthrodesis hindfoot, midfoot, hallux, and lesser
20. Ramsey PL, Hamilton W: Changes in of the ankle: A critical analysis. Foot toes. Foot Ankle Int 1994;15:349-353.
tibiotalar area of contact caused by lat- Ankle Int 1998;19:3-9. 36. Domsic RT, Saltzman CL: Ankle Os-
eral talar shift. J Bone Joint Surg Am 29. Gruen GS, Mears DC: Arthrodesis of teoarthritis Scale. Foot Ankle Int 1998;
1976;58:356-357. the ankle and subtalar joints. Clin 19:466-471.
21. Marti RK, Raaymakers EL, Nolte PA: Orthop 1991;268:15-20. 37. Mazur JM, Schwartz E, Simon SR:
Malunited ankle fractures: The late 30. Alvarez RG, Barbour TM, Perkins TD: Ankle arthrodesis: Long-term follow-
results of reconstruction. J Bone Joint Tibiocalcaneal arthrodesis for non- up with gait analysis. J Bone Joint Surg
Surg Br 1990;72:709-713. braceable neuropathic ankle deformi- Am 1979;61:964-975.
22. Rosen H: Reconstructive procedures ty. Foot Ankle Int 1994;15:354-359. 38. Frey C, Halikus NM, Vu-Rose T, Ebram-
about the ankle joint, in Jahss MH (ed): 31. Pinzur MS, Kelikian A: Charcot ankle zadeh E: A review of ankle arthrodesis:
Disorders of the Foot and Ankle: Medical fusion with a retrograde locked Predisposing factors to nonunion. Foot
and Surgical Management, 2nd ed. intramedullary nail. Foot Ankle Int Ankle Int 1994;15:581-584.
Philadelphia: WB Saunders, 1991, vol 1997;18:699-704. 39. Cobb TK, Gabrielsen TA, Campbell DC
3, pp 2593-2613. 32. Kile TA, Donnelly RE, Gehrke JC, II, Wallrichs SL, Ilstrup DM: Cigarette
23. Offierski CM, Graham JD, Hall JH, Werner ME, Johnson KA: Tibiotalo- smoking and nonunion after ankle
Harris WR, Schatzker JL: Late revision calcaneal arthrodesis with an intramed- arthrodesis. Foot Ankle Int 1994;15:64-67.
of fibular malunion in ankle fractures. ullary device. Foot Ankle Int 1994;15: 40. Lind J, Kramhoft M, Bodtker S: The
Clin Orthop 1982;171:145-149. 669-673. influence of smoking on complications
24. Weber BG, Simpson LA: Corrective 33. Flock TJ, Ishikawa S, Hecht PJ, Wap- after primary amputations of the
lengthening osteotomy of the fibula. ner KL: Heel anatomy for retrograde lower extremity. Clin Orthop 1991;
Clin Orthop 1985;199:61-67. tibiotalocalcaneal roddings: A roentgen- 267:211-217.
Vol 8, No 3, May/June 2000 209
Vous aimerez peut-être aussi
- Os 13 1465Document9 pagesOs 13 1465Mar HernandezPas encore d'évaluation
- Closing Wedge Osteotomy of The Tibia and The FemurDocument12 pagesClosing Wedge Osteotomy of The Tibia and The Femuralyek92Pas encore d'évaluation
- Coste Et Al. - 1968 - Rheumatoid ForefootDocument2 pagesCoste Et Al. - 1968 - Rheumatoid ForefootYuki SATAKEPas encore d'évaluation
- Marcheggianimuccioli 2019Document12 pagesMarcheggianimuccioli 2019Ghusun MadaniPas encore d'évaluation
- Realignment Surgery For Malunited Ankle Fracture: Clinical ArticleDocument5 pagesRealignment Surgery For Malunited Ankle Fracture: Clinical ArticleGio VandaPas encore d'évaluation
- AAOS Foot Ankle 2018abDocument54 pagesAAOS Foot Ankle 2018abFasa Roshada100% (3)
- Acl Recon With BPT GraftDocument6 pagesAcl Recon With BPT Graftpaper coe medanPas encore d'évaluation
- Clinical Analysis of The Frosch Approach in The Treatment of Posterolateral Tibial Plateau Fractures Combined With Lateral Tibial Plateau FracturesDocument11 pagesClinical Analysis of The Frosch Approach in The Treatment of Posterolateral Tibial Plateau Fractures Combined With Lateral Tibial Plateau FracturesraynaldidjohariofcPas encore d'évaluation
- ArtosDocument22 pagesArtosRia Rahmadiyani IIPas encore d'évaluation
- Ortho ArticleDocument2 pagesOrtho ArticleSamantha Dela Paz100% (1)
- Surgical Treatment of Habitual Patella Dislocation With Genu ValgumDocument3 pagesSurgical Treatment of Habitual Patella Dislocation With Genu ValgumfitrianiPas encore d'évaluation
- Use of External Fixation in The Reconstruction of The Charcot Foot and AnkleDocument21 pagesUse of External Fixation in The Reconstruction of The Charcot Foot and AnkleAnonymous kdBDppigEPas encore d'évaluation
- Multiple Ligament InjuredDocument6 pagesMultiple Ligament InjuredMayra BeltranPas encore d'évaluation
- Tratamiento No Convencional de ArtrosisDocument11 pagesTratamiento No Convencional de ArtrosisHenny CasanovaPas encore d'évaluation
- Comminuted Intraarticular Fractures of The Tibial Plateau Lead To Posttraumatic Osteoarthritis of The Knee: Current Treatment ReviewDocument7 pagesComminuted Intraarticular Fractures of The Tibial Plateau Lead To Posttraumatic Osteoarthritis of The Knee: Current Treatment ReviewGustavoBecerraPas encore d'évaluation
- Medial Femoral Condyle Fracture During An Oxford UDocument3 pagesMedial Femoral Condyle Fracture During An Oxford Uestefania1994Pas encore d'évaluation
- Arthrodesis of The Metacarpophalangeal and Interphalangeal Joints of The Hand:Current ConceptsDocument55 pagesArthrodesis of The Metacarpophalangeal and Interphalangeal Joints of The Hand:Current ConceptsM BaqirPas encore d'évaluation
- Outcome Assesment of Proximal Fibular Osteotomy in Medial Compartment Knee OsteoarthritisDocument3 pagesOutcome Assesment of Proximal Fibular Osteotomy in Medial Compartment Knee OsteoarthritisPrashant GuptaPas encore d'évaluation
- Osteoarthritis of HipDocument3 pagesOsteoarthritis of Hipjcachica21Pas encore d'évaluation
- Triple Artrodesis TobilloDocument17 pagesTriple Artrodesis TobilloIsrael CucsPas encore d'évaluation
- Traatment Gonatroza Prin ArthroplastieDocument5 pagesTraatment Gonatroza Prin Arthroplastieandre_moarcasPas encore d'évaluation
- Total Knee Arthroplasty in Osteopetrosis Using Patient-Specific InstrumentationDocument4 pagesTotal Knee Arthroplasty in Osteopetrosis Using Patient-Specific InstrumentationDavidBeatonComuladaPas encore d'évaluation
- Ankle FracturesDocument133 pagesAnkle FracturesAtiekPalludaPas encore d'évaluation
- Our Experience On Peroneus Longus As Graft For Arthroscopic ACL ReconstructionDocument9 pagesOur Experience On Peroneus Longus As Graft For Arthroscopic ACL ReconstructionInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- Knupp 2011Document7 pagesKnupp 2011orlandoPas encore d'évaluation
- 1348 6456 4 PBDocument7 pages1348 6456 4 PB林良駿Pas encore d'évaluation
- Pes Cavus ....Document34 pagesPes Cavus ....Rupika Sodhi100% (2)
- Knee - Total Knee ArthroplastyDocument17 pagesKnee - Total Knee Arthroplastyshaannivas50% (2)
- Lateral Uka Survivorship Short To MidtermDocument5 pagesLateral Uka Survivorship Short To Midtermapi-267962692Pas encore d'évaluation
- All-Epiphyseal, All-Inside Anterior Cruciate Ligament Reconstruction Technique For Skeletally Immature PatientsDocument9 pagesAll-Epiphyseal, All-Inside Anterior Cruciate Ligament Reconstruction Technique For Skeletally Immature Patientshieuminhduong7Pas encore d'évaluation
- Iowaorthj00001 0076Document10 pagesIowaorthj00001 0076alyek92Pas encore d'évaluation
- TKA Scope Arthrolysis Knee Surg Sports Traumatol Arthrosc 2010 Mar 18 (3) 346-351Document6 pagesTKA Scope Arthrolysis Knee Surg Sports Traumatol Arthrosc 2010 Mar 18 (3) 346-351Fayza RihastaraPas encore d'évaluation
- Kulkarni2012 PDFDocument7 pagesKulkarni2012 PDFAby SuryaPas encore d'évaluation
- Elbow Arthritis and Removal of Loose Bodies and SpursDocument11 pagesElbow Arthritis and Removal of Loose Bodies and SpurspuchioPas encore d'évaluation
- Presented By: DR Venkatesh V Moderator: DR Harish KDocument81 pagesPresented By: DR Venkatesh V Moderator: DR Harish KPankaj VatsaPas encore d'évaluation
- Jurnal Tendinitis 2Document7 pagesJurnal Tendinitis 2gismaputri santosoPas encore d'évaluation
- Surgicaltreatmentof Intra-Articularcalcaneal Fractures: John J. Stapleton,, Thomas ZgonisDocument8 pagesSurgicaltreatmentof Intra-Articularcalcaneal Fractures: John J. Stapleton,, Thomas Zgonisthzone1986Pas encore d'évaluation
- Foot Ankle Clin - 2021 Jun - 26 (2) - 391-405.Document15 pagesFoot Ankle Clin - 2021 Jun - 26 (2) - 391-405.Biblioteca Centro Médico De Mar del PlataPas encore d'évaluation
- Distal Tibia Paper 2Document6 pagesDistal Tibia Paper 2Rajib DebnathPas encore d'évaluation
- Arthrodesis Techniques in The Management of Stage II and III Acquired Adult Flatfoot Deformity.Document12 pagesArthrodesis Techniques in The Management of Stage II and III Acquired Adult Flatfoot Deformity.C Martin TraumatoPas encore d'évaluation
- Bagus PDFDocument4 pagesBagus PDFAditya KrisnaPas encore d'évaluation
- Anterolateral Ligament Reconstruction Technique An Anatomic BasedDocument5 pagesAnterolateral Ligament Reconstruction Technique An Anatomic BasedEmilio Eduardo ChoquePas encore d'évaluation
- 2014 Article 9237Document6 pages2014 Article 9237Mahmoud A KhatabPas encore d'évaluation
- Surgery Ortho - TaskDocument4 pagesSurgery Ortho - TasknicewanPas encore d'évaluation
- Arthritis: OsteoarthritisDocument8 pagesArthritis: OsteoarthritisAlex DaniPas encore d'évaluation
- Laprade 2012Document11 pagesLaprade 2012Aaron BPas encore d'évaluation
- Tka ValgusDocument11 pagesTka ValgusOvidiu RusuPas encore d'évaluation
- Management of Patellofemoral Chondral InjuriesDocument24 pagesManagement of Patellofemoral Chondral InjuriesBenalPas encore d'évaluation
- Fai 2011 0818Document4 pagesFai 2011 0818Mohamed GoudaPas encore d'évaluation
- Corso 1995Document6 pagesCorso 1995Matei RazvanPas encore d'évaluation
- Distal Amputations For The Diabetic Foot PDFDocument4 pagesDistal Amputations For The Diabetic Foot PDFGiuliana ReyesPas encore d'évaluation
- (Literally "Re-Forming of Joint") : ArthroplastyDocument93 pages(Literally "Re-Forming of Joint") : ArthroplastykotraePas encore d'évaluation
- Treatment of Gonarthrosis by Total Knee ArthroplasDocument6 pagesTreatment of Gonarthrosis by Total Knee ArthroplasAhmad MaulanaPas encore d'évaluation
- Knee Injuries: DR - Sindhu Meena MEM Resident MMHRCDocument30 pagesKnee Injuries: DR - Sindhu Meena MEM Resident MMHRCP Vinod KumarPas encore d'évaluation
- Prostop ArthroereisisDocument15 pagesProstop Arthroereisislucas guerraPas encore d'évaluation
- FootDocument59 pagesFootAnmar Hamid Abd AlmageedPas encore d'évaluation
- Deltoid Ligament Injuries Associated With Ankle Fractures - Argument For Repair of The Deltoid LigamentDocument3 pagesDeltoid Ligament Injuries Associated With Ankle Fractures - Argument For Repair of The Deltoid LigamentSaifuddin HaswarePas encore d'évaluation
- Catastrophic Talar Bone Loss From High Velocity Trauma Treated With Structural Tricorticate Fibula Autograft Compression Frame and Midfoot Distraction ArthroplastyDocument9 pagesCatastrophic Talar Bone Loss From High Velocity Trauma Treated With Structural Tricorticate Fibula Autograft Compression Frame and Midfoot Distraction ArthroplastyAthenaeum Scientific PublishersPas encore d'évaluation
- McGlamery Triple ArthrodesisDocument26 pagesMcGlamery Triple ArthrodesisTrudy SalmonPas encore d'évaluation
- Unicompartmental Knee Arthroplasty: Indications, Surgical Techniques and ComplicationsD'EverandUnicompartmental Knee Arthroplasty: Indications, Surgical Techniques and ComplicationsTad L. GerlingerPas encore d'évaluation
- Acl Immature PatientDocument10 pagesAcl Immature PatientariearifinPas encore d'évaluation
- Animal Models of Osteoporosis - Necessity and LimitationsDocument16 pagesAnimal Models of Osteoporosis - Necessity and LimitationsariearifinPas encore d'évaluation
- Peripheral Nervous System (PNS)Document16 pagesPeripheral Nervous System (PNS)ariearifinPas encore d'évaluation
- The Surgical Treatment of Morton's NeuromaDocument15 pagesThe Surgical Treatment of Morton's NeuromaariearifinPas encore d'évaluation
- Cardiovascular Disease Certification Examination Electrocardiograms and Imaging Studies - AbimDocument33 pagesCardiovascular Disease Certification Examination Electrocardiograms and Imaging Studies - AbimabimorgPas encore d'évaluation
- Dental Anatomy QuestionsDocument310 pagesDental Anatomy Questionsrbs2002Pas encore d'évaluation
- Nursing Republic Acts - PhilippinesDocument2 pagesNursing Republic Acts - PhilippinesLj Ferolino100% (11)
- Reading and Writing Ophthalmology NotesDocument7 pagesReading and Writing Ophthalmology NotesErik Anderson MD100% (2)
- Femoral Hernia RepairDocument17 pagesFemoral Hernia RepairIhsan AndanPas encore d'évaluation
- Techno - Obstetric miniOSCEDocument153 pagesTechno - Obstetric miniOSCEIssa JbourPas encore d'évaluation
- Bangalore DR ListDocument11 pagesBangalore DR Listkrisveli76% (42)
- ETC1010 Paper 1Document9 pagesETC1010 Paper 1wjia26Pas encore d'évaluation
- PREOPERATIVE ASSESSMENT NajiehahDocument26 pagesPREOPERATIVE ASSESSMENT NajiehahRuban AvadiarPas encore d'évaluation
- Cramp Pages 1Document10 pagesCramp Pages 1masi10Pas encore d'évaluation
- Askep DislokasiDocument19 pagesAskep DislokasiHana Syifana RobbyaniPas encore d'évaluation
- Male Internal Genital OrganDocument10 pagesMale Internal Genital OrganfiansisPas encore d'évaluation
- In-Service Training Programs For Nurses, 1st and 2nd Quarter, Calendar Year 2023Document4 pagesIn-Service Training Programs For Nurses, 1st and 2nd Quarter, Calendar Year 2023iamxai rnmanemtPas encore d'évaluation
- SBAR ExampleDocument13 pagesSBAR Examplejugdeep15Pas encore d'évaluation
- Common Probe FailuresDocument18 pagesCommon Probe FailuresEuris Otilio Dominguez AmadisPas encore d'évaluation
- Scary StoryDocument4 pagesScary Storyapi-386698528Pas encore d'évaluation
- Pedia Prelim ExamDocument7 pagesPedia Prelim ExamJojo JustoPas encore d'évaluation
- Action Plan of Directorate of Central Health EstablishmentDocument1 pageAction Plan of Directorate of Central Health EstablishmentDirectorate of Central Health EstablishmentsPas encore d'évaluation
- Rectal Cancer Contouring Guide: Econtour TeamDocument29 pagesRectal Cancer Contouring Guide: Econtour TeamRonna Marie Vijar PamalandongPas encore d'évaluation
- Gross Anatomy Urinary SystemDocument43 pagesGross Anatomy Urinary SystemMay LacdaoPas encore d'évaluation
- InstrumentsDocument7 pagesInstrumentsOllet Athive NatacabPas encore d'évaluation
- Pengantar Emergency Health Care SystemDocument23 pagesPengantar Emergency Health Care SystemErwin MaiyoPas encore d'évaluation
- Esophageal Perforation: Diagnostic Work-Up and Clinical Decision-Making in The First 24 HoursDocument7 pagesEsophageal Perforation: Diagnostic Work-Up and Clinical Decision-Making in The First 24 HourssyaifularisPas encore d'évaluation
- Celecoxib Drug StudyDocument2 pagesCelecoxib Drug Studymilkv100% (2)
- Uterine AtonyDocument2 pagesUterine AtonyBryan Relado AmbitoPas encore d'évaluation
- Supersize Me EssayDocument5 pagesSupersize Me EssayBrooke Cohn0% (1)
- Prospectus MBBS SMCW 2020Document30 pagesProspectus MBBS SMCW 2020activedudePas encore d'évaluation
- BJOG - 2023 - Lee - Tranexamic Acid As An Adjunct To Oxytocin Prophylaxis in The Prevention of Postpartum Haemorrhage inDocument9 pagesBJOG - 2023 - Lee - Tranexamic Acid As An Adjunct To Oxytocin Prophylaxis in The Prevention of Postpartum Haemorrhage inHayfa LayebPas encore d'évaluation
- Reflexions PDF Members Only OnlineDocument36 pagesReflexions PDF Members Only OnlineMihai PaunPas encore d'évaluation
- Article - Self-Scheduling For Hospital NursesDocument6 pagesArticle - Self-Scheduling For Hospital NursesDavidPas encore d'évaluation