Académique Documents
Professionnel Documents
Culture Documents
SG Nutrisi
Transféré par
Gung AyuTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
SG Nutrisi
Transféré par
Gung AyuDroits d'auteur :
Formats disponibles
Study Guide Clinical Nutrition & disorders
CORE CURRICULUM
Clinical Nutrition and Disorder
Aims
Capable to explain the concept of human nutrition and set the comprehensive action for nutritional
problems, in health and disease in the primary care settings.
Learning outcomes
1. Explain the roles of macronutrients and micronutrients in health and diseases, and its food
sources
2. Estimate the general nutritional and energy requirements in relation to age, sex, activity, stress,
pregnancy and nursing mother.
3. Explain the general principles of well-balanced diet
4. Assess the nutritional status in health and diseases, include determining nutritional deficiency
and excess
5. Determine the difference of concepts among vitamin deficiency, dependency and toxicity
6. Identify mineral deficiency and toxicity
7. Explain the nutrition concepts, specialties and burdens through the life cycle
8. Explain the nutrition concepts for obesity and weight management, dislipidaemia and
hyperurecemia
9. Explain the concept of medical nutrition therapy in primary care setting
10. Explain the concept of food supplement and functional food in primary care setting
11. Diagnose and manage common problems and diseases of micronutrient defieciencies in the
primary care settings.
12. Explain the basic concepts and principles of enteral and parenteral (IntraVenous) nutrition.
Curriculum content
1. Role and food sources of nutrients
2. Need of general nutritional and energy requirements in specific physiological conditions
3. Macro and micronutrients
4. The concept of well-balanced diet and it’s implementation
5. Assessment of general nutritional status that has been used in community as well as in
clinical setting
6. Management of common nutritional problems :
6.1 Malnutrition (Undernutrition)
6.2 Obesity
6.3 Weight management
6.4 Infant Feeding Practice
6.5 Dislipidaemia
6.6 Hyperurecemia
7. The principles of medical nutritional therapy (MNT)
8. The principles of enteral and parenteral nutrition
9. Food Supplement and Functional Food
Udayana University Faculty of Medicine, DME, 2018 1
Study Guide Clinical Nutrition & disorders
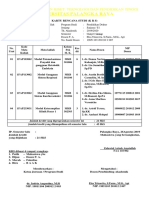
~ PLANNERS TEAM ~
No Name Departement Phone
Community &
1 Dr. dr. Gde Ngr Indraguna Pinatih, M.Sc, Sp.GK Preventive 08123816424
Medicines
Anesthetic &
2 Dr. dr. I Wayan Suranadi, Sp.An-KIC 08123847675
Reanimation
3 Dr. dr. I Gst Lanang Sidiarta, Sp.A(K) Pediatrics 08123966008
Community &
4 Dr. dr. I Wayan Weta, MS, Sp.GK Preventive 081337005360
Medicines
5 dr. I Wayan Gede Sutadarma, M.Gizi, Sp.GK Biochemistry 082144071268
~ LECTURERS ~
NO NAME DEPT PHONE
Community and
Dr. dr. Gde Ngr Indraguna Pinatih, M.Sc, Sp.GK
1 Preventive 08123816424
(GNIP)
Medicines
Community and
2 Dr. dr. I Wayan Weta, MS, Sp.GK (WT) Preventive 081337005360
Medicines
Anesthtic and
3 Dr. dr. I Wayan Suranadi, Sp.An-KIC (WSR) 08123847675
Reanimation
4 Dr.dr. I Gst Lanang Sidiarta, SpA.(K) (IGLS) Pediatrics 08123966008
dr. I Wayan Gede Sutadarma, M.Gizi, Sp.GK
5 Biochemistry 082144071268
(SUT)
Udayana University Faculty of Medicine, DME, 2018 2
Study Guide Clinical Nutrition & disorders
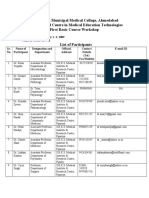
~ FACILITATORS ~
Regular Class (Class A)
Venue
No Name Group Departement Phone
(3rd floor)
3rd floor:
1 dr. Yukhi Kurniawan, Sp.And A1 Andrology 08123473593
R.3.09
3rd floor:
2 dr. Made Widhi Asih, Sp.Rad(K) A2 Radiology 081916442626 R.3.10
3rd floor:
3 dr. I Gde Haryo Ganesha S.Ked A3 DME 081805391039 R.3.11
dr. dr. luh Putu Ratna Sundari, 3rd floor:
4 A4 Physiology 081933070077 R.3.12
M.Biomed
3rd floor:
5 dr. I Made Dwi Ariawan, S.Ked A5 Public Health 081339798632 R.3.13
3rd floor:
6 dr. Ida Ayu Sri Indrayani, Sp.S A6 Neurology 081338645671 R.3.14
dr. I Made Putra Swi Antara, Sp.JP, 3rd floor:
7 A7 Cardiology 08123804782 R.3.15
FIHA
3rd floor:
8 dr. I Kadek Swastika, M.Kes A8 Parasitology 08124649002 R.3.16
Dr. dr. Komang Januartha Putra 3rd floor:
9 A9 Microbiology 08123831710
Pinatih, M.Kes R.3.17
dr. Ida Ayu Dewi Wiryanthini, 3rd floor:
10 A10 Biochemistry 081239990399
M.Biomed R.3.19
Regular English (Class B)
Venue
No Name Group Departement Phone
(3rd floor)
3rd floor:
1 dr. I Made Winarsa Ruma, S.Ked. PhD B1 Biochemistry 087785356853
R.3.09
dr. Ni Nengah Dwi Fatmawati, Sp.MK, 3rd floor:
2 B2 Microbiology 087862200814 R.3.10
Ph.D
dr. I Gde Ardika Nuaba, Sp.T.H.T.K.L 0811389489/ 3rd floor:
3 B3 ENT R.3.11
(K)., FICS 08123802689
dr. Ni Made Ayu Surasmiati, 3rd floor:
4 B4 Opthalmology 081338341860 R.3.12
M.Biomed, Sp.M
3rd floor:
5 dr. Yuliana, M.Biomed B5 Anatomy 085792652363 R.3.13
3rd floor:
6 dr. I Putu Adiartha Griadhi, M.Fis B6 Physiology 081999636899 R.3.14
3rd floor:
7 dr. Luh Nyoman Alit Aryani, Sp.KJ (K) B7 Psychiatry 085737717244 R.3.15
3rd floor:
8 dr. Kadek Budi Santosa, Sp.U B8 Surgery 081339977799 R.3.16
dr. I.B. Made Suryawisesa, Sp.B(K) 3rd floor:
9 B9 Surgery 087862245922
Onk R.3.17
3rd floor:
10 dr. Agung Nova Mahendra, M.Sc B10 Pharmacology 087861030195
R.3.19
Udayana University Faculty of Medicine, DME, 2018 3
Study Guide Clinical Nutrition & disorders
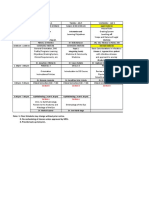
TIME TABLE
Time
Learning
Days/date English Regular Place PIC
Activity
Class Class
Introduction of
08.00-09.00 09.00-10.00 Class room
the Theme
1st day 09.00-10.30 10.00-11.30 Independent
Learning GNIP
Thursday
Discussion
21 June 10.30-12.00 12.00-13.30 SGD
room
2018 12.00-12.30 11.30-12.00 Break
12.30-13.30 13.30-14.30 Plenary
13.30-15.00 14.30-16.00 Student project
Nutrition and Class room
08.00-09.00 09.00-10.00
Life Cycle
2nd Day 09.00-10.30 10.00-11.30 Independen
Learning
Friday
Discussion GNIP
22 June 10.30-12.00 12.00-13.30 SGD
room
2018 12.00-12.30 11.30-12.00 Break
12.30-13.30 13.30-14.30 Plenary Class room
13.30-15.00 14.30-16.00 Student project
Well Balance Class room
08.00-09.00 09.00-10.00
Diet
3rd Day 09.00-10.30 10.00-11.30 Independen
Learning
Monday
Discussion GNIP
25 June 10.30-12.00 12.00-13.30 SGD
room
2018 12.00-12.30 11.30-12.00 Break
12.30-13.30 13.30-14.30 Plenary Class room
13.30-15.00 14.30-16.00 Student project
Infant and Class room
Children
08.00-09.00 09.00-10.00
Feeding
Practice
4th Day
09.00-10.30 10.00-11.30 Independent IGLS
Tuesday
Learning
26 June Discussion
2018 10.30-12.00 12.00-13.30 SGD
room
12.00-12.30 11.30-12.00 Break
12.30-13.30 13.30-14.30 Plenary Class room
13.30-15.00 14.30-16.00 Student project
Udayana University Faculty of Medicine, DME, 2018 4
Study Guide Clinical Nutrition & disorders
Obesity and Class room
08.00-09.00 09.00-10.00 Weight
Management
5th Day 09.00-10.30 10.00-11.30 Independent
Thursday Learning GNIP
28 June Discussion
10.30-12.00 12.00-13.30 SGD
2018 room
12.00-12.30 11.30-12.00 Break
12.30-13.30 13.30-14.30 Plenary
13.30-15.00 14.30-16.00 Student project Class room
Primary Protein Class room
08.00-09.00 09.00-10.00 and Energy
Malnutrition
6th Day 09.00-10.30 10.00-11.30 Independent
Friday Learning WT
29 June SGD Discussion
10.30-12.00 12.00-13.30
2018 room
12.00-12.30 11.30-12.00 Break
12.30-13.30 13.30-14.30 Plenary Class room
13.30-15.00 14.30-16.00 Student project
Secondary Classroom
Protein and
08.00-09.00 09.00-10.00
Energy
Malnutrition
7th day 09.00-10.30 10.00-11.30 Independent
Monday Learning WT
2 July 2018 SGD Discussion
10.30-12.00 12.00-13.30
room
12.00-12.30 11.30-12.00 Break
12.30-13.30 13.30-14.30 Plenary Classroom
13.30-15.00 14.30-16.00 Student project
Minerals
08.00-09.00 09.00-10.00 Class room
Deficiency
09.00-10.30 10.00-11.30 Independent
8th day Learning
Tuesday SGD Discussion
10.30-12.00 12.00-13.30 SUT
3 July 2018 room
12.00-12.30 11.30-12.00 Break
12.30-13.30 13.30-14.30 Plenary Class room
13.30-15.00 14.30-16.00 Student project
Vitamins
08.00-09.00 09.00-10.00 Class room
Deficiency
9th day 09.00-10.30 10.00-11.30 Independent
Wednesday Learning SUT
4 July 2018 SGD Discussion
10.30-12.00 12.00-13.30
room
12.00-12.30 11.30-12.00 Break
Udayana University Faculty of Medicine, DME, 2018 5
Study Guide Clinical Nutrition & disorders
12.30-13.30 13.30-14.30 Plenary Class room
13.30-15.00 14.30-16.00 Student project
Food
Supplement
08.00-09.00 09.00-10.00 (Functional Class room
Food and
Antioxidant)
10th day 09.00-10.30 10.00-11.30 Independent
Thursday Learning SUT
5 July 2018 Discussion
10.30-12.00 12.00-13.30 SGD
room
12.00-12.30 11.30-12.00 Break
12.30-13.30 13.30-14.30 Plenary Class room
13.30-15.00 14.30-16.00 Student project
Medical
08.00-09.00 09.00-10.00 Nutritional Class room
Therapy
11th day Independent
09.00-10.30 10.00-11.30
Friday Learning
SUT
6 July 2018 Discussion
10.30-12.00 12.00-13.30 SGD
room
12.00-12.30 11.30-12.00 Break
12.30-13.30 13.30-14.30 Plenary Class room
13.30-15.00 14.30-16.00 Student project
Enteral and
08.00-09.00 09.00-10.00 Parenteral Classroom
Nutrition
Independent
12th day 09.00-10.30 10.00-11.30
Learning
Monday Discussion WSR
9 July 2018 10.30-12.00 12.00-13.30 SGD
room
12.00-12.30 11.30-12.00 Break
12.30-13.30 13.30-14.30 Plenary Classroom
13.30-15.00 14.30-16.00 Student project
Nutrition
Management for
08.00-09.00 09.00-10.00 Dyslipidemia Classroom
and
13th day Hyperuricemia
Tuesday WT
Independent
10 July 09.00-10.30 10.00-11.30
Learning
2018
Discussion
10.30-12.00 12.00-13.30 SGD
room
12.00-12.30 11.30-12.00 Break
12.30-13.30 13.30-14.30 Plenary Classroom
13.30-15.00 14.30-16.00 Student project
Udayana University Faculty of Medicine, DME, 2018 6
Study Guide Clinical Nutrition & disorders
Nutrition
Management for
08.00-09.00 09.00-10.00 Diabetes Classroom
Mellitus and
14th day Hypertension
Wednesday WT
Independent
11 July 09.00-10.30 10.00-11.30
Learning
2018
Discussion
10.30-12.00 12.00-13.30 SGD
room
12.00-12.30 11.30-12.00 Break
12.30-13.30 13.30-14.30 Plenary Classroom
13.30-15.00 14.30-16.00 Student project
15th day
Thursday Final
08.00-14.00 Class room TEAM
12 July Examinatiom
2018
Udayana University Faculty of Medicine, DME, 2018 7
Study Guide Clinical Nutrition & disorders
STUDENT PROJECT
The aim of the student project in this block is to provide the opportunity for the student to learn more
deeply on recent vitamin and mineral deficiency issues. In the mild situation these kind of problem
usually asymptomatic or the symptom appears in different aspect of organ disease, but then it can
give serious impact to the person who get it. For example folic acid deficiency in pregnant mother
causing neural defect to the offspring. This situation often called as hidden malnutrition accordingly.
Students shall disparted themself in group following the small discusiion group and then for the
topic below
A1 Vitamin A in Pregnancy B1 Potasium in Pregnancy
A2 Vitamin D in Pregnancy B2 Phosphor in Pregnancy
A3 Vitamin E in Pregnancy B3 Magnesium in Pregnancy
A4 Vitamin K in Pregnancy B4 Vitamin B12 in Pregnancy
A5 Folic Acid in Pregnancy B5 Vitamin B6 in Pregnancy
A6 Vitamin C in Pregnancy B6 Selenium in Pregnancy
A7 Iron in Pregnancy B7 Omega 3 in Pregnancy
A8 Zinc in Pregnancy B8 Biotin in Pregnancy
A9 Calcium in Pregnancy B9 Iodine in Pregnancy
A10 Sodium in Pregnancy B10 Vitamin B1 in Pregnancy
The report shall follow the scientific writing procedure produced by the university of Udayana. The
Reference used in the the project shall be the most recent one, may be not older than 2010, except
there isn’t any recent literature available to the particular topic.
Fascilitators are requested to fascilitate and examine these project.
REPORT FORMAT
1. Introduction
2. Review
a. Definition
b. Digestion and Absorption
c. Metabolism
d. RDA
e. Toxicity
3. Conclusion
4. Referrence
REPORT SHALL BE SUBMITED
TUESDAY, 10th July 2018
Udayana University Faculty of Medicine, DME, 2018 8
Study Guide Clinical Nutrition & disorders
LEARNING TASK
1st day
INTRODUCTION OF THE THEME
Case 1.
Looking at Indonesian household study on health from 2007-2013 Indonesia has faced two burdens
on nutrition over and undernourished which then called malnutrition. In one way we still facing
chronic malnutrition shown as stuntet which will create problems on non communicable diseases in
the future, in the other way the number of obesity and its related diseases are increasing .
Furthermore, concerning health including nutrition we have other burdens those are teens and
elderly, as the number of yiung adult as well as old people are also increasing. All these need more
effort and budget to handle the problems. Poverty and natural disaster lead to increase nutritional
problems especialy undernutrition. In other side, increasing wellness on small group of population
lead to increase the risk of overnutrition and degenerative diseases. To minimize the risk of
nutritional problem, optimal nutrition is needed to be applied in all population groups.
1. Explain, what does it mean by optimal nutrition, whilst human eating food?
2. Discuss how optimal nutrition can be apllied within individual as well as community
3. Explain, what causing people to get malnourished, under or overweight?
4. Mention stages of nutrition development and how to assess it?
5. What is the main nutritional problems in Indonesia and what is the arising nutrition problem
today and its health risk?
Case 2.
A 5 years old girl, taken by her mother to the clinic (Health Centre). Her mother tells the doctor that
she often got sick, it is nearly monthly. Her appetite also told as less. Looking at her growth
monitoring chart, her weight falling down since she was 1 year. She got breast milk only 3 month
because her mother has gone for a work and she is under her grandma cares when her parent is
absent for work. She looks shorter to her mostly friend, she is less active for her age and irrtable.
When they check her appetite, actually she eats heartlily
Learning Task
1. What the appropriate information and assessment you should collect to support diagnose of
the nutrition problem?
2. Looking at the sysmtoms above what illness might possible happenned to this girl and does
it a reversible disease?
3. Should you think that it is a reversible disease, what is your advise to reverse her problem?
4. Beside nutrition factors, what is the others contributing factors might influence these
conditions?
2nd day
NUTRITION AND THE LIFE CYCLE
Case
Young mother come to your private clinic with her 6 months old girl infant. She complains that her
infant’s weight gain was different with the neighbor’s one. She gives exclusive breastfeeding for her
baby and she ask you when she must start to give solid foods?
Learning Task
1. What is the meaning of exclusive breastfeeding and how long should it be given?
2. How to start solid foods, when to start solid foods and what kind of foods should be given to
start with the solid food in infant feeding practice?
Udayana University Faculty of Medicine, DME, 2018 9
Study Guide Clinical Nutrition & disorders
Self-Assessment
1. Describe some of the nutrient and immunological attributes of breast milk.
2. Describe criteria would you use in selecting an infant formula.
3. Describe when an infant is ready to start eating solid food.
4. List foods that are inappropriate for infants and discuss why they are inappropriate.
5. List strategies for introducing nutritious foods to children.
6. Describe changes in nutrient needs from childhood to adolescence.
3rd day
WELL BALANCE DIET
Case 1.
A young athlete 19 years old, height 178 cm, weight 70 kg. wants to maintain his ideal body weight
as well as performance. He practice as athelete everyday with vigorous activity in the afternoon.
After calculating his energy need, he is dicided to get 3000 kcal perday
Learning Task :
1. Calculate the macronutient (carbohydrate, protein and fat) need following to his energy need
and to get balanced diet.
2. Put your calculation into meal frequency include snack
3. Translate into food stuff that shall be given to meet his need
4. Discuss whether he needs special food before, during and after training.
5. Discuss whether he need an extra supplement to add his intake, and what supplement is best
to be given to him.
Case 2
A 26 years old woman, have just married, weight 54 kg, and height 160 cm, come to obstetric clinic
to ask for advice on maintaining healthy pregnancy. She is worry of falling into nutritional deficiency
when she get and during her pregnancy. Therefore, to prevent it she needs as many as information
and advises on how to keep the optimal fetal growth and optimal nutrition status of pregnant and
lactating mother.
Learning task.
1. Calculate energy requirement of pregnant woment within 1st, 2nd, and 3rd trimester of
pregnancy
2. Translate the total energy requirement of pregnant women in the all trimester into daily
foodstuff. Make sure that the composition is appropriate to the requirement of balanced diet
3. What kind of protein resources is better to be used to get an optimal nutrition in the
pregnancy? Explain why is it so
4. In menu planning, split all foodstuff into three main menu (breakfast, lunch and dinner) and
two snack?
5. To optimize the nutrient availability what kind of foodstuff should be included in the menu?
6. If any case you find nutrient deficiency in the daily food intake, what suggestion shall be
given to prevent and reverse it? Give the reason of your particular suggestion!
7. What shall you do to fill adequately all nutrient intake, both the quality and the quantity ?
8. For maintaining optimal infant growth and healthy mother, what kind of food are selected to
the mother?
9. List and explain the steps that have to be done before planning a meal
10. To facilitate you to plan an adequate diet, you need some tools such as RDA
(Recommended Daily Allowance), and Food Exchange List. Describe the adventage and
disadvantage of both these two tools
Udayana University Faculty of Medicine, DME, 2018 10
Study Guide Clinical Nutrition & disorders
4th day
INFANT AND CHILDREN FEEDING PRACTICE
Case
Young mother come to your private clinic with her 6 months old girl infant. She complains that her
infant’s weight gain was different with the neighbor’s one. She gives exclusive breastfeeding for her
baby and she ask you went she must start to give solid foods?
Learning Task
3. What is the meaning of exclusive breastfeeding and how long should be given?
4. How to start solid foods, when to start solid foods and what kind of foods were given at the
first time?
Self-Assessment
7. Describe some of the nutrient and immunological attributes of breast milk.
8. Describe criteria would you use in selecting an infant formula.
9. Describe when an infant is ready to start eating solid food.
10. List foods that are inappropriate for infants and discuss why they are inappropriate.
11. List strategies for introducing nutritious foods to children.
5th day
OBESITY AND WEIGHT MANAGEMENT
Case 1.
Suharni, 27 years old, has got her gained weight since 4 years ago when she delivered her baby.
Before pregnant her weight was 55 kg while her heigt was 160 cm. When she was pregnant, her
weight increase 16 kg, and now her weight is 80 kg. She wants to have baby and she has been
trying to do it unsuccesfully since one year ago. The obstetricus suggest her to reduce her weight,
before trying it again.
Learning task:
1. Count Suharni’s Body Mas Index before and after she gain weight and her nutrition status
base on her BMI.
2. Discuss what is happening on her untill she gain her weight that much
3. What measurement need to be added to diagnose such condition above
4. Discuss the laboratory tested need to be carried out to distinguish whether she got the
comorbidity or not
5. Theoritically what is the cause for obesity
6. Should She has to reduce her weight what she need to do.
6th day
PRIMARY PROTEIN and ENERGY MALNUTRITION
Case 1.
A 28 years old man, height 178 cm, and 24 years old woman, height 164 cm, want to maintain their
ideal body weight. Both of them are in moderate activity.
Learning task
1. For the two people, calculate the Ideal Body Weight, energy requirement, energy intake to
meet energy balanced
Udayana University Faculty of Medicine, DME, 2018 11
Study Guide Clinical Nutrition & disorders
Note:
Total energy output is the summary of your’s body three uses of energy:
a) Resting metabolic rate (RMR)
b) Thermic effect of food (TEF)
c) Physical activity
a) RMR (use general formula) :
Women : 0.9 kcalories/kg bb/hr
Men : 1.0 kcalories/kg bb/hr
b) TEF : 10% of total energy intake
c) Physical activity
Average activity level Energy cost (% or RMR)
Sedentary 20
Very light 30
Moderate 40
Heav 50
d) Calculate Total energy output :
Total energy output (kcal) = …..(RMR) + ….(TEF) + …..(Physical activity).
2. Calculate the Carbohydrate, Protein and fat composition to get a healthy diet.
Case 2.
In a party, there will be many kinds of food will be served. Mostly of those foods will comprise of
animal base food such as pork, beef and or fish and cooked in several kind of menu
Learning task.
1. If someone always eat a big portion of meet but less fish, what kind of fatty acid will be eaten
more? What is the type of fatty acid will be in the pork and the beef?
2. What is the impact of such fatty acid to the health if daily menu consist of mostly fatty meat?
3. What kind of fatty acid are composed in the fish?
4. If some one eats fish more frequent, what is the beneficial effect of fish fat to the health?
Explain your reason!
5. Compare saturated, monounsaturated, and polyunsaturated fatty acids in term of their : a)
chemical composistion, b) effect on health, c) usuall food sourches.
6. Describe the meaning of P:S ratio of fatty acid and the ideal composition
7. Name the essential fatty acids. Why they are called essential? What will happen if the
essential fatty acids are in a short supply? What suggestion should be given in this situation?
8. Differentiate the clinical benefit of essential fatty acid between omega-3 and 6
9. What are the potential problems associated with excess amount of eating fat in generall?
Case 3.
A 60 years old vegetarian man, his daily meal consist of sereal, soybean, spinach and some
supplement and never take milk, egg nad other animal base food
Learning task.
1. What your opinion about the quality of protein intake?
2. How does the healing process of the injured tissue in vegan people?
3. If pregnant women is a vegan food pattern what the the possibility risk might happen to the
pregnancy (mother and fetal)?
4. For optimal growth and development, the body need good quality of protein. Why?
5. Explain the kind of protein in the food refer to the amino acid contained?
6. What is the meaning of essential amino acid, conditional essential amino acid
7. Define the reference of protein?
Udayana University Faculty of Medicine, DME, 2018 12
Study Guide Clinical Nutrition & disorders
8. What does it mean by biological value of protein? Explain the biological value of different
food protein resources?
9. Explain the term protein-sparing effect.
10. List and describe factors that affect the need on dietary protein!
11. What does it mean by nitrogen balance? How does it relate to protein turn over
7th day
SECONDARY PROTEIN and ENERGY MALNUTRITION
Case 1
A man age 35 year old has lost his weight since two month ago. His previous weight was 65 kg and
his height is 172 cm, but now his weight is 48 kg. He also suffer from chronic diarrhea and coughing
and just very recently his cough followed by blood split. He has had lost his appetite since he felt
sore in his mouth and throat 1 month ago.
He works as a tour guide but beside that he often sell his body to satisfy his client lust.
Learning task
1. Mention what is happening nutritionally to this man
2. Discuss What causing him loose his weight so quick
3. Decribe indicators used to pictures clearly his situation
4. Discuss can we proposed him to get his normal weight again
5. Explain the principal of food intevention that can be given to Him
Case 2
Beny aged 20 months was born in only 2000 grams of weight though he born under aterm
pregnanacy. Her mother was also very thin when carrying on him. He got breastfed but not
exclusive since is also working in the field to support the family life budget. Now his weight is 9 kg
(average weight for his age is 11,8 kg). He often get ill and in the daily life he is very irritable.
Learning task
1. Mention what is happening nutritionally to this infant
2. Discuss risk factors causing him fall into this situation
3. Discuss the progonsis of his particular problem short and long termly
4. Explain the principle of nutritional approach/therapy of this infant
8th day
MINERALS DEFICIENCY
Case
A 20 years old male suffering from delayed wound healing since one month ago. Food intake has
been declining due to lack of appetite. The wound was not healed so it still looks wet.
Learning task.
1. What kind of mineral might be deficient in this case
2. What other symptoms and signs shall be found out in such cases?
3. What kind of food should be consumed as well as avoided to reverse the condition?
4. Describe the basic concept of essentiality in mineral (trace element)
5. Describe the action (metabolism), function, clinical application, RDI and food resources
of major mineral
6. Describe factors that influence the bioavailability (promoter and inhibitor) and absorption
of particular mineral
Udayana University Faculty of Medicine, DME, 2018 13
Study Guide Clinical Nutrition & disorders
9th day
VITAMINS DEFICIENCY
Case
An old lady 65 years old can no longer walk properly since she suffer from bow leg. She has seen a
doctor and was told to have exposed with sun rays in the morning that she has rarely had it before
because of worryness to get dark skin, and also she was ask to drink milk and some fruit mostly
avocado.
Learning Task
1. Mention the vitamin is deficient in this old woman, and explain the risk factors that bring
people to geat it.
2. What this disease is called when it happened in older people as well as the young one
3. Explain symptom and sign of this particular vitamin deficiency either in older people and in
young children
4. What kind of food should be consumed to reverse the condition?
5. Describe the definition and the basic concept of vitamins
6. Describe the basic concept of the difference between water and fat soluble vitamins
7. Describe the action, function, RDI, clinical application, side effect and food resources of fat
soluble vitamins (A,D,E,K)
8. Describe the action, function, RDI, clinical application, side effect and food resources of
water soluble vitamins (B and C)
10th day
NUTRITION MANAGEMENT FOR DYSLIPIDEMIA AND HYPERURICEMIA
Case
Boby 35 year old visits a doctor because he feels he gets heavy chest, feels weak and pain mostly
in his ankle. He has suffer from it for about one week. He is 120 kg weight and 170 height. He likes
eating out and very lazy to do excercise. From his blood test, he finds out that his blood cholesterol
is 300 mg/l and the LDL cholesterol is 200 mg/l and the HDL is 30 mg/l. The triglyceride is 400 mg/l
and the uric acid is 9.
Learning task
1. Diagnose the situation of this patient
2. Calculate the atherogenic index of this patient
3. Discuss the nutritional approach for this patient
4. Discuss what suggestion shall be given to the patient to get better result
11th day
MEDICAL NUTRITION THERAPY
Case
45-year-old man admitted to hospital for diabetes mellitus with complications of kidney disorders.
She looked thin and weak. Food intake is inadequate because of nausea and vomiting. He can not
eat solid food and can only drink milk. His body weight was 60kg and he had lost 10kg weight in 6
Udayana University Faculty of Medicine, DME, 2018 14
Study Guide Clinical Nutrition & disorders
months. The body height is 170cm with a 15cm upper arm circumference. Based on laboratory
results, Hb level was 9 g/dL and albumin was 2.5 g/dL
Learning task
1. To confirm the patients diagnose, what kind assessment you have to do?
2. To meet nutrition need of the patients, what other information you need for appropriate
nutrition support?
3. What route of feeding and diet should be considered to promote healing?
4. What kind of supplement to be added to the daily menu of the patient? What is the
reason?
5. How do you arrange the frequency of daily food intake?
12th day
FOOD SUPPLEMENT
(FUNCTIONAL FOOD and ANTIOXIDANT)
Case 1
A 25 years old man is a very active athlete. He exercises regularly 5 times a week with heavy
intensity. He is always on to go often grabbing something quick to eat like fast food or skipping meal
altogether. Never the less, he feels confident his health will not suffer because he takes a daily
vitamins and minerals supplement.
Learning Task
1. Is a food supplement warranted in this case?
2. Why or why not?
3. What is your suggestion for the patients?
Case 2
A 50 year old man, come to consult a doctor. Currently he is suffering from hypertension stage 1
and hypercholesterolemia. On physical examination found that body weight 85 kg, height 165 cm,
and abdominal circumference of 100 cm. In addition to taking medication given by doctors, he also
wants to consume omega 3 fatty acids, garlic supplements and vitamin E after reading an article.
She says that garlic supplements claim to lower blood pressure, omega-3 fatty acids have anti-
inflammatory properties and Vitamin E is good for the heart among other benefits.
Learning Task
1. Are all supplements warranted in this case?
2. Why or why not?
3. What is the side effect of the supplements?
4. What is your suggestion for the patients?
13th day
ENTERAL AND PARENTERAL NUTRITION
Case
A 25 years old young man, admitted to the intensive care unit with multiple trauma due to motorbike
accident. On patient examination, it was found to have GCS 8 with respiratory depression. The
patient was normotensive 130/80 but tachycardic (118 beats per minute). Abdomen was not
distended and bowel sounds were present. A nasogastric tube was placed with a return of 200 mL
of clear gastric juice. A left femoral fracture and multiple superficial contusion were noted with no
evidence of external bleeding. The patient was placed on a ventilator and resucitated.
Udayana University Faculty of Medicine, DME, 2018 15
Study Guide Clinical Nutrition & disorders
Laboratory data
Abdominal series : Nasogastric tube in stomach, no bowel distension, no ileus.
Chest radiography : without abnormalities
Extremity rontgen : left femoral fracture
CT scan of head : cerebral edema without intracranial hematoma
Body composition
Height : 183 cm
Actual body weight : 85 kg
Learning Task
a. What is the preferred route of access for nutritional intervention, if the gut is intact and
functional?
b. How can you prevent tube feeding complications?
Self Assessment
1. Describe benefits of enteral feeding for gastrointestinal physiology and function!
2. Describe indication and contraindication for nasoenteric tube placement!
3. Figure out common sites of inserting Central Venous Access!
4. What is main indication for parenteral nutrition
Udayana University Faculty of Medicine, DME, 2018 16
Study Guide Clinical Nutrition & disorders
ABSTRACTS
INTRODUCTION of THE THEME
Abstract
Indonesia recently is in transition of epidemiologic periode. Its mean that Indonesia has both
nutrition problem, undernutrition as well as overnutrition. Decreasing in undernutrition problem
(protein energy malnutrition, nutrition anemia, vitamin A deficiency, iodine deficiency) and infectious
diseases, coincindence with increasing prevalence of overnutrition and degenerative disease (type
2 of diabetes, heart disease, hypertension, gout, osteoporosis, cancer, etc). Its has been known that
nutrition is closely related to disease entity mainly infectious and degenerative diseases.
Appropriate nutrition intervention is needed for successful treatment of the diseases. The medical
nutrition therapy should be individualized by providing optimal nutrition therapy to optimized the
nutrient availability, absorption, transportation, utilization and its effects. To meet the optimal
nutrition therapy, the student need a broad knowledge about :
1. The function of nutrient and its influence to health and diseases and the food sources
2. Principle of well balanced diet and menu planning
3. Simple nutritional assessment (Dietary, anthropometric, biochemical and clinical sign)
4. Pathophysiology of nutritional deficiencies and excess
5. Concept of medical nutrition therapy (MNT)
In hospital based, medical nutrition therapy is part of health care team, consist of physician incharge
and nutrition team. Nutritrition team are consist of medical/clinical nutrition specialist, dietitian,
nurse, and include patient and family.
At the end of this study, the student is expected to know the role of optimal nutrition in healing of
diseases and promoting health
PRIMARY PROTEIN and ENERGY MALNUTRITION
Abstract
Carbohydrate as sourches of energy for human bodies. Human bodies need adequate
amount of energy daily to promote and maintain optimal health. There are several type of
carbohydrate both refine and nonrefine that compose daily product widely spread include in
Indonesia. It has been known that refine carbohydrate is related to degenerative diseases which are
increasing in the last decade. So, increasing intake of non-refined or whole grain carbohydrate
sources give a protective effect to the degenerative diseses. Other type of carbohydrate has been
identified has protective effect for health namely low and high glycemic index of carbohydrate.
Fat as sourches of energy more efficiently than carbohydrate. Fat has benefit and bad effect
to health according to fatty acid containing in food (meat, fish, grain and others). So an adequate fat
intake and appropriate ratio of saturated and unsaturated fatty acid is play a role in promoting and
maintaining optimal health.
Protein as a body building is important to maintain optimal biologic function of cells (growth,
regeneration, reproduction, etc) to promote and maintain optimal health. To achieve optimal health,
good quality of protein intake of animal sources should be consumed in adequate amount daily.
Objectives
At the end of this session, student must be able to
1. Describe the type, function and sources of carbohydrate, as well as its effect to health.
2 . Describe the type, functionand sources of protein as well as the effect to human health.
Udayana University Faculty of Medicine, DME, 2018 17
Study Guide Clinical Nutrition & disorders
SECONDARY PROTEIN and ENERGY MALNUTRITION
Abstract
PEM is a condition due to lack or deficit intake of carbohydrates, lipids, and protein from diet. These
conditions signed by mobilized or oxidized all of energy source in the body. The impacts of
mobilized energy are reduce body weight (fat, and muscle mass), reduce metabolic rate.
Natural history of disorder innisiated by light, moderate and the last severe PAM. Light and
moderate PEM could usually handled significantly by nutrition support. Severe PEM always followed
by clinical complication with followed by some diseases, so the management of the condition should
be need hospitalized beside nutrition care.
PEM in child bearing period could disturb growth and development. In adult PEM decreased health
status, and risks to suffer from some both communicable and non-communicable diseases.
VITAMINS DEFICIENCY
Abstract
Nutrients in food are grouped into two major group i.e. macro and micro nutrients. Macronutrients
comprise of substances that give energy such as carbohydrate, protein and fat, while micronutrients
comprise of vitamins and minerals. The human requirement for micronutrient is not as big as
macronutrient even some minerals, the requirement is very small but though they are very essential
as the human body can not produce it except vitamin D, and shall be accordingly included in the
human food.
Vitamins, according to its solubility, are classified into two very distinctive groups: fat soluble
and water soluble. This separation is also made in consider to its effect on human body and
metabolism even though they are working together in carrying out body function. Human will not be
deficient in fat soluble vitamin i.e. vitamin A, D, E, and K, unless they are on fat free diet for a
longtime, because fat is the main resources for fat soluble vitamins. In addition most fat soluble
vitamins are stored in human body or organ, even vitamin D is produced by our body using the food
we eat and helped by the ultraviolet from the sun. Unlike the fat soluble, the water soluble vitamins
are not stored and always excreted out after being used through sweat, urine and stools, therefore
human needs to intake it daily from their food. Some foods content previtamin in which the body will
transform it into vitamin when it is ingested.
Vitamin works specifically in human function. Though they have multiple roles and action in
the human body, they are working independently but cooperatively with other nutrient to support
body/organ function and because they are very specific their presence can not be substitute by
others.
Objective
At the end of the study, the student is expected able to describe the type, funtions, effect to human
health and food sources of each vitamin
MINERALS DEFICIENCY
Abstract
Likewise vitamin, minerals also classified into two or even three group: major, trace element and
some trace which the essentialities are unclear. The classification is made base on the amount
needed by human body, while the major mineral requirement shall be equal or above 100 mg/day,
the trace elements are below 100 mg. Major mineral comprise of Calcium (Ca), Sodium (Na),
Udayana University Faculty of Medicine, DME, 2018 18
Study Guide Clinical Nutrition & disorders
Potassium (K), Phosphorus (P), Chloride (Cl), Sulfur (S). The trace element are Iron (Fe), Iodine (I),
Zinc (Zn), Copper (Cu), Manganese (Mn), Chromium (Cr), Cobalt (Co), Selenium (Se), Molybdenum
(Mo), and Fluoride (F); and the unclear trace elements include Silicon (Si), Vanadium (V), Tin (Sn),
Nickel (Ni), Cadmium (Cd), Arsenic (As), Aluminum (Al), Boron (B)
There are some similarities between mineral and vitamins. The essentiality, unique role,
interactions and its impact to chronic diseases are similar between mineral and vitamins but the
structure, absorption (mode of absorption), classification, roles in the body, the amount needed and
the stability are different.
Objective
At the end of the study, the student is expected able to :
1. Describe the funtions and effect to human health and food sources of each mineral
2. Explain the factors that influence the availability of mineral
WELL BALANCE DIET AND MENU PLANNING
Abstract
Balanced diet is important in promoting health. Balanced diet is planned to replace in and balance
to the daily energy expended. Balanced diet consist of all nutrient in adequate amount to fullfil
person need. Factor determine energy expenditure are : age, sex, physical activity, special
condition, temperature, illness, etc.
To plan balance diet, several steps should follows :
1. Decide total energy requirement (energy expenditure) of individual or patients
2. Decide the composition of macronutrient appropriate for balanced diet
3. Use food composition table, food exchange list or nutrisurvei to translate energy required
into daily food needed appropriate to balance diet.
4. Split daily foodstuff into 3 main menu (breakfast, lunch, and dinner) and 2 snack portion
Objective
At the end of the study, the sutend is expected :
1. Undertnad the concept of balanced diet and menu planning
2. Able to use food composition table or nutrsurvey package
3. Able to analyses nutrient content of diet by using food composition table or nutri-survei
Indonesia
4. Able to plan menu appropriate to balance diet
INFANT AND CHILDREN FEEDING PRACTICE
Abstract
Malnutrition is still high, especially in developing countries, such as Indonesia. Malnutrition has been
responsible for two-thirds of death annually among children under five. Well over two-third of these
deaths are associated with inappropriate feeding practices, mainly during the first year of life.
Inappropriate feeding practices including low prevalence of exclusive breastfeeding, too early or too
late beginning of complementary feeding, and nutritionally inadequate and unsafe of complementary
foods. Malnourished children who survive are more frequently sick and suffer the life-long
consequences of impaired development.
Udayana University Faculty of Medicine, DME, 2018 19
Study Guide Clinical Nutrition & disorders
Objective
At the end of the study, the student is expected to be able to describe the feeding practices
in infants and young children.
NUTRITION MANAGEMENT FOR DISLIPIDAEMIA AND HIPERURECEMIA
Abstract
Dyslipidemia is condition of abnormality of blood lipid profile concentration. Lipid profile such
as triglycerides, LDL-cholesterol usually higher, and HDL-cholesterol lower than normal condition.
This condition usually due to the imbalance of diet, especially excess of carbohydrate and saturated
fat.
Usually, the disorder occurs in person with obesity. Diet management such as decreased
carbohydrate and saturated fat diet. Diet contain omega 3-poly unsaturated fatty (n-3 PUFA), often
use to normalized blood lipid concentration.
Hyperuricemia, the condition increased blood uric acid concentration above the normal level.
Uric acid is metabolic product of nucleic acid (purine, pyrimidine), that construct DNA. Hyperucemia
could caused by lack metabolism of uric acid due to enzyme deficient, and or too much purine
intake from the diet.
OBESITY AND WEIGHT MANAGEMENT
Abstract
Recently obesity is counted as a disease which attack human body systematically. It is
predominantly caused by over eating and less out put. However there are plenty of risk factors can
influence or even support this situation.
As it is said as a systemic disease, if it is not treated well, it can underly several kind of diseases
especially non contagious disease. Even the qonsequence of having obesity, when the patient got a
disease, it can perform more severe compare to non obese patient.
Weight manajement shall be perform to obese patient with or without comorbid of any related
disease.
Objectives
At the end of this session, student is able to:
1. Define obesity by using several kind of measurement
2. Explain the risk factors of overweight and obesity
3. Describe other kind of diseases where obesity is the underlying factor
4. Describe methods that usually used to reduce or manage weight
NUTRITION AND LIFE CYCLE
Abstract
Nutrition is important to health and wellness throughout ones lifespan. Knowledge of changing
nutritional requirements is important to deliver quality health care. The student will develop a diet
plan for individuals in various life stages. All healthy people need the same nutrients during each life
Udayana University Faculty of Medicine, DME, 2018 20
Study Guide Clinical Nutrition & disorders
stage, just in different amounts. Infancy – Birth to one year; Childhood – one year to puberty;
Adolescence – puberty to adulthood; Adulthood – last from adolescence to old age; and specially
condition are Pregnancy and Lactation.
Objective
At the end of the study, the student is expected able to describe the characteristic of each life stage
and nutrients requirement.
MEDICAL NUTRITION THERAPY
Abstract
Medical nutrition therapy refers to specific nutrition procedure including assessment and intervention
in the treatment of an illness, injury and disease condition. Medical nutrition therapy procedures
define the level, content and frequency of nutrition service that are appropriate for optimal care and
nutrition outcome. There are many component to medical nutrition therapy. Screening may be
completed by a registered dietitian (RD), dietetic technician registered (DTR) or health care
professional. Nutritional care process include assessment,establishment of client’s selfmanagement
goals, development of a nutrtion plan, documentation, communication with the primary care
provider, evaluation and reassessment and outcome measurements.
Objectives
At the end of the study, the medical student is expected to
1. Comprehend the step of medical nutrition therapy
2. Comprehend the medical nutritional care team is work together to promote patient healing
and health.
FOOD SUPPLEMENT (FUNCTIONAL FOOD/ANTIOXIDANT)
Abstract
Most people nowadays are aware that deficiency diseases can be cured, and that adequate
intakes of essential nutrients can be assured either by taking purified nutrients as supplements or in
fortified foods. By analogy, perhaps some of the benefits of a modern recommended diet could be
obtained by taking supplements that contain the active ingredients of foods that may help to prevent
diseases such as cancer, heart disease and osteoporosis. This would allow us to eat our preferred
‘unhealthy’ fat- and sugar-rich diet but still enjoy at least some of the health benefits of eating a
more prudent diet.
Dietary supplements could include food preparations designed to meet all or part of the
nutritional and energy needs of invalids, sports drinks, slimming foods and hundreds of herbal
medicines that can be marketed as dietary supplements. The term functional foods could include
every fortified food and every food for which some sort of health claim has been made, such as
most breakfast cereals.
A few of the substances used as dietary supplements are also licensed medicines: some
generic vitamins (vitamins A and D, folic acid and cyanocobalamin, vitamin B12); a multi-vitamin
preparation designed to meet the needs of children; a fish oil preparation; and an iron and folic acid
supplement intended for pregnant women. It is permissible to make medicinal claims for these
products, for example that a fish oil preparation, lowers raised plasma triacylglycerols and so helps
to prevent heart attacks and pancreatitis. Other fish oil preparations marketed as dietary
supplements are not allowed to make such claims. Similarly, it is permissible to refer to an iron and
Udayana University Faculty of Medicine, DME, 2018 21
Study Guide Clinical Nutrition & disorders
folic acid supplement intended for pregnant women’s role in reducing the risk of babies being born
with a neural tube defect but such claims are not allowed for other dietary supplements that contain
folic acid.
To get a medicine licensed can take up to a decade and cost many millions of pounds; this is
why many manufacturers of nutrients, ‘natural substances’ and herbal preparations choose to
market them as dietary supplements instead. This means that they are subject to legal regulations
relating to food rather than to medicines. Anything which is taken orally and not classified as a
medicine is, by default, classified as food. This has major commercial advantages for the
manufacturer who not only bypasses the expensive and slow process of getting the product
licensed but is also subject to the much less stringent legal regulations relating to food. It is illegal to
sell food which is harmful to health and it is illegal to dishonestly describe or advertise a food. This
means that although it is illegal to make false health claims for a dietary supplement it is the
prosecution that must ‘prove’ a claim to be false, whereas a medicine must be shown to be safe and
effective before it is licensed.
People take supplements for a variety of reasons, such as to compensate for a perceived or
potential inadequacy in the diet, to compensate for some perceived increase in need or defective
handling of a nutrient, to treat or prevent non-deficiency diseases or to improve athletic
performance. In many cases it is difficult to give a definitive answer or even a fairly confident answer
to the question of whether supplements or functional foods are actually effective (or even safe).
When assessing the effectiveness of a dietary supplement or functional food one must decide what
measure or measures are to be used as indicators of success or failure. In some cases, one can
monitor the effect of a supplement on the signs and or symptoms of a disease. Thus when dietary
deficiency diseases were first being identified, one could confirm the beneficial effects of a vitamin
or mineral by testing the effect upon symptoms and disease progression of purified supplements or
foods rich in the nutrient.
ENTERAL and PARENTERAL FEEDING
Abstract
Increase case admitted to the intensive care unit in uncocius condition need proper medical nutrition
therapy to prevent undernutrition. For this condition the MNT route is enteral and/or parentral is
prefered. For appropriate dicission the indication, energy and nutrient needed, choosing formula,
route of nutrtional intervention shuld be considered.
At the end of the study, student is expected to know the indication, benefit or risk each feeding
formula and the complicatiom of eneteral and parentral feeding
Udayana University Faculty of Medicine, DME, 2018 22
Study Guide Clinical Nutrition & disorders
REFFERENCE
1. Halsted, C.H., 1992. Toward standardized training of physicians in clinical nutrition. Am J
Clin Nutr; 56: 1-3
2. WHO, 2003. Diet nutrition and the prevention of chronic diseases. WHO tecnicval series
Report. 916
3. William, S.W. and Schelenker, E. D., 2003. Nutrion and Health. Essential of Nutrition & Diet
Therapy. 8th ed , Mosby, St Louis, Missouri,p 4-21; 45-214; 373-388; 408-434
4. Dinarto M., 2002. Tim Nutrisi, Gizi Medik Indonesia, 1: 7-8
5. Torun B. and Chew F., 1981. Protein Energy Malnutrition. In R, E. Berhman and R.M
Kliegman., editors, Nelson Essential of Pediatrics.4th ed..Toronto; pp.983-988
6. Ross A.,C. 1981. Vitamin A and retginoids. In R, E. Berhman and R.M Kliegman., editors,
Nelson Essential of Pediatrics.4th ed..Toronto; pp 306-324
7. Pronsky Z.M., and Crowe J.P., 2008., AssessmentFood-Drug Interaction. In Krause’s Food
Nutrition Therapy. Ed. Mahan L.K., and Escott-Stump S., WB. Saunders., pp.432-452
8. Hathcock J.N., Rader J.L, 1999. Food Additives, contaminants, and Natural Toxins. In
Modern Nutrition in Health and Disease, 9th ed. Williams & Wilkins, Baltimore. pp1837-1856
9. DEPKES RI, 2002. Pedoman umum Gizi Seimbang (PUGS)
10. WHO-Unicef, 2003, Global Strategy for Infant and Child Feeding, WHO Geneva
Udayana University Faculty of Medicine, DME, 2018 23
Study Guide Clinical Nutrition & disorders
CURRICULUM MAP
Program or curriculum blocks
10 Senior Clerkship
9 Senior Clerkship
8 Senior Clerkship
Health System- Community-based Evidence-based Special topics : Elective Study IV Compre 18
7 based Practice practice Medical Health Ergonomy & (evaluation) Clinic
(3 weeks) Practice Health Environment Orientation
(4 weeks) (2 weeks) (Clerkship)
BCS (1 weeks) (2 weeks) (2 weeks) + medical
ethic
(4 weeks)
The Medical The Urinary The Reproductive Elective Study III 19
6 Cardiovascular Emergency System and System and Disorders
System and (3 weeks) Disorders (3 weeks) (3 weeks)
Disorders (3 weeks)
(3 weeks) BCS (1 weeks) BCS (1 weeks) BCS (1 weeks)
BCS (1 weeks)
Neuroscience and The Respiratory The skin & Special Topic : Forensic Medicine Elective 18
5 neurological System and hearing system - Palliative med and Medicolegal Study II
disorders Disorders & disorders - Complemnt & (2 weeks) (2 weeks)
(3 weeks) (3 weeks) (3 weeks) Alternative Med.
BCS (1 weeks) BCS (1 weeks) BCS (1 weeks) (2 weeks)
Musculoskeletal Alimentary The Endocrine Clinical Nutrition The Visual 18
4 system & & hepatobiliary System, and Disorders system &
connective tissue systems & Metabolism and (2 weeks) disorders
disorders disorders Disorders (2 weeks)
(3 weeks) (3 Weeks) (3 weeks)
BCS (1 weeks) BCS (1 weeks) BCS (1 weeks) BCS (1 weeks) BCS (1weeks)
Behavior Change Basic Infection Immune system Hematologic Special Topic 19
3 and disorders & infectious & system & disorder & - Andro & aging
(3 weeks) diseases disorders clinical oncology - - Geriatri
(3 weeks) (2 weeks) (3 weeks) -Travel medicine
BCS (1 weeks) BCS (1 weeks) BCS (1 weeks) BCS (1 weeks) - (4 weeks)
BIOMEDIK III Growth Medical Medical Basic Elective 17
2 (4 weeks) & communication Professionalism Pharmaceutical Study I
development (2 weeks) (2 weeks) medicine & drug (2 weeks)
(2 weeks) etics
BCS: (1 weeks) BCS (1 weeks) BCS (1 weeks) (2 weeks)
Studium BIOMEDIK I The cell BIOMEDIK II 19
1 Generale and (8 weeks) as biochemical (6 weeks)
Humaniora machinery
(2 weeks) (2 weeks)
BCS(1 weeks)
Pendidikan Pancasila & Kewarganegaraan ( 3 weeks )
Udayana University Faculty of Medicine, DME, 2018 24
Vous aimerez peut-être aussi
- Study Guide Growth Tayang 13 Maret 2020 TerupdateDocument53 pagesStudy Guide Growth Tayang 13 Maret 2020 TerupdateJocelin NathanielaPas encore d'évaluation
- Study Guide Endocrine Semester 5 Tayang 28 Oktober 2016Document46 pagesStudy Guide Endocrine Semester 5 Tayang 28 Oktober 2016Desak PratiwiPas encore d'évaluation
- Study Guide Medical Professionalism Tayang 6 Mei 2020Document44 pagesStudy Guide Medical Professionalism Tayang 6 Mei 2020Jocelin NathanielaPas encore d'évaluation
- Study Guide Blok VisualDocument81 pagesStudy Guide Blok VisualPutra AdyatmaPas encore d'évaluation
- Musculoskeletal Tayang Semester IV Tayang 22 Pebruari FIXDocument67 pagesMusculoskeletal Tayang Semester IV Tayang 22 Pebruari FIXAnthony WijayaPas encore d'évaluation
- Study Guide Medical Professionalism Tayang 6 Mei 2020Document45 pagesStudy Guide Medical Professionalism Tayang 6 Mei 2020Jocelin NathanielaPas encore d'évaluation
- Tetanus SDocument88 pagesTetanus SSantosa OkaPas encore d'évaluation
- Preface: Study Guide The Endocrine System, Metabolism & DisordersDocument48 pagesPreface: Study Guide The Endocrine System, Metabolism & DisordersAlvin AlvelinoPas encore d'évaluation
- Study Guide BCS VI 2023 RevisiDocument146 pagesStudy Guide BCS VI 2023 RevisiSGD blima semlimanamPas encore d'évaluation
- Modul Basic Clinical Skill Vi PDFDocument147 pagesModul Basic Clinical Skill Vi PDFOvie Hoshie100% (1)
- Jadwal Block 2.9 Infectious Diseases 2018 Edit BaruDocument8 pagesJadwal Block 2.9 Infectious Diseases 2018 Edit BaruPuspa YaNiPas encore d'évaluation
- Usulan Pengmas Dept Radup27feb3Document64 pagesUsulan Pengmas Dept Radup27feb3Zachrona Kusuma Dewi0% (1)
- MedicineDocument2 pagesMedicinePrakash RajaPas encore d'évaluation
- DHS SOP Part 1Document318 pagesDHS SOP Part 1Arun MahalingamPas encore d'évaluation
- STP Book PDFDocument744 pagesSTP Book PDFNitinTulsyanPas encore d'évaluation
- Matrix Schedule - 1st Sem Sy 2022-2023 (Final)Document40 pagesMatrix Schedule - 1st Sem Sy 2022-2023 (Final)NMD LIFESAVERPas encore d'évaluation
- Indiragandhi Institute of Child HealthDocument2 pagesIndiragandhi Institute of Child HealthRamen ModakPas encore d'évaluation
- Study Guide Behavior Semester IV FK UNUDDocument67 pagesStudy Guide Behavior Semester IV FK UNUDPadma PermanaPas encore d'évaluation
- Poliklinik Executive Sakura RSUD Abdoel Wahab Sjahranie SamarindaDocument1 pagePoliklinik Executive Sakura RSUD Abdoel Wahab Sjahranie SamarindaTiara GussyofnitriaPas encore d'évaluation
- Telangana CHC Yatra2017Document1 pageTelangana CHC Yatra2017GiksmkPas encore d'évaluation
- FORMAT KRS Semester 3 NewDocument2 pagesFORMAT KRS Semester 3 NewRahasPas encore d'évaluation
- Letter Order To DR ANAND and SPM For DALY StudiesDocument1 pageLetter Order To DR ANAND and SPM For DALY StudiesBEYOND CIVILIZATIONPas encore d'évaluation
- Participant NHLMCAhmedabad PDFDocument199 pagesParticipant NHLMCAhmedabad PDFAbhilasha Pathak0% (1)
- Ahmedabad DR Email MobileDocument233 pagesAhmedabad DR Email MobileNaveenJain100% (1)
- Bangalore DR ListDocument12 pagesBangalore DR ListAmey KPas encore d'évaluation
- Further Clinical Study On Kastartava W.S.R To Primary Dysmenorrhea & Its Management by MatraBastiDocument3 pagesFurther Clinical Study On Kastartava W.S.R To Primary Dysmenorrhea & Its Management by MatraBastiInternational Journal of Innovative Science and Research TechnologyPas encore d'évaluation
- Anti Ragging CommitteDocument1 pageAnti Ragging Committealtafksk07Pas encore d'évaluation
- ACE Inhibitors and Statins in Adolescents With Type 1 DiabetesDocument1 pageACE Inhibitors and Statins in Adolescents With Type 1 DiabetesalaaedinPas encore d'évaluation
- Study On The Incidence of Urinary Tract Infections, Organisms Causing It and Antibiotic Susceptibility in Patients With DIABETES MELLITUS IN AJIMS, MLORE" For The Registration of Dissertation To RajivDocument26 pagesStudy On The Incidence of Urinary Tract Infections, Organisms Causing It and Antibiotic Susceptibility in Patients With DIABETES MELLITUS IN AJIMS, MLORE" For The Registration of Dissertation To RajivR Hari0% (1)
- Guideline For WorkshopDocument9 pagesGuideline For Workshopretno widyastutiPas encore d'évaluation
- Facility Unit Name Unit Incharge Male/Female/Both Patient Day of The WeekDocument2 pagesFacility Unit Name Unit Incharge Male/Female/Both Patient Day of The WeekAdarsh ClinicPas encore d'évaluation
- Check List KredentialDocument2 pagesCheck List KredentialMade GustiawanPas encore d'évaluation
- E-Journal Udayana Medica: Issn Nomor: 1 January 2013Document3 pagesE-Journal Udayana Medica: Issn Nomor: 1 January 2013Edwin SridanaPas encore d'évaluation
- VICHARCHIKADocument6 pagesVICHARCHIKAdr amitPas encore d'évaluation
- UntitledDocument18 pagesUntitledSpace HRPas encore d'évaluation
- Daftar Rekapitulasi Proposal Ganjil 2020-2021Document3 pagesDaftar Rekapitulasi Proposal Ganjil 2020-2021RIDHA AYU NINGRUMPas encore d'évaluation
- OUHSDocument7 pagesOUHSdayalshashi2Pas encore d'évaluation
- Medical 230706Document1 pageMedical 230706api-26869023Pas encore d'évaluation
- Form Rekap Waktu Pelayanan Rawat JalanDocument2 pagesForm Rekap Waktu Pelayanan Rawat JalannaeniPas encore d'évaluation
- PIIS2213858723001195Document15 pagesPIIS2213858723001195Aparajita PraharajPas encore d'évaluation
- Ayurveda Vol. 8 Issue No. 2 April June 2013Document68 pagesAyurveda Vol. 8 Issue No. 2 April June 2013Anonymous A3vTUVPas encore d'évaluation
- PG (Medical) Admissions 2023-24 - Consolidated S3 Eligible Candidates ListDocument7 pagesPG (Medical) Admissions 2023-24 - Consolidated S3 Eligible Candidates ListsureshPas encore d'évaluation
- Health Is FreeDocument16 pagesHealth Is FreeProf. MadhavanPas encore d'évaluation
- Jurnal Kayu Manis New PDFDocument4 pagesJurnal Kayu Manis New PDFFiona AmeliaPas encore d'évaluation
- Planers Team No Name Department Phone: Study Guide Blok Pemeriksaan Dan Diagnosis Fisioterapi - 2018Document22 pagesPlaners Team No Name Department Phone: Study Guide Blok Pemeriksaan Dan Diagnosis Fisioterapi - 2018Nengah VindiPas encore d'évaluation
- Efficiency of Matra Basti With Bala Taila in Janu Sandhigata Vata With W.S.R. To OsteoarthritisDocument5 pagesEfficiency of Matra Basti With Bala Taila in Janu Sandhigata Vata With W.S.R. To OsteoarthritisVAP NepalPas encore d'évaluation
- The Application of Art Therapy To Reduce The Level of Depression in Patients With HemodialysisDocument7 pagesThe Application of Art Therapy To Reduce The Level of Depression in Patients With Hemodialysisbardah wasalamahPas encore d'évaluation
- Participant Jlnmcwardha MaharashtraDocument248 pagesParticipant Jlnmcwardha MaharashtraKriti KumariPas encore d'évaluation
- Komdis Ke 70Document8 pagesKomdis Ke 70faisal prasetioPas encore d'évaluation
- Doctors of DelhiDocument137 pagesDoctors of DelhiAkash Panwar83% (6)
- Final SVGA List of Doctors Online Consultations With Disclaimer HAPPY TO HELPDocument4 pagesFinal SVGA List of Doctors Online Consultations With Disclaimer HAPPY TO HELPTRH RECRUITMENTPas encore d'évaluation
- First Announcement Sunshine 2023Document9 pagesFirst Announcement Sunshine 2023Muhammad Naqvi Al FarisiPas encore d'évaluation
- DAFTAR PUSTAKA GabunganDocument9 pagesDAFTAR PUSTAKA GabunganIda Bagus MustikaPas encore d'évaluation
- Daftar PustakaDocument6 pagesDaftar Pustakahildaali020Pas encore d'évaluation
- Mastitis GranulomatosaDocument9 pagesMastitis GranulomatosaJhoanPas encore d'évaluation
- Daftar Pustaka Penggunaan Obat RasionalDocument3 pagesDaftar Pustaka Penggunaan Obat RasionalandroPas encore d'évaluation
- AnnouncementDocument42 pagesAnnouncementzaki hetamiPas encore d'évaluation
- Regular and English Class FacilitatorsDocument1 pageRegular and English Class FacilitatorsgilangPas encore d'évaluation
- Daftar Pustaka DispepsiaDocument16 pagesDaftar Pustaka DispepsiaAnnisa Hyunnie ElfPas encore d'évaluation
- Balancing Traditions: Harnessing The Power Of Eastern And Western Medicine For Optimal WellnessD'EverandBalancing Traditions: Harnessing The Power Of Eastern And Western Medicine For Optimal WellnessPas encore d'évaluation
- #19 SY Vs CA Case DigestDocument1 page#19 SY Vs CA Case DigestJunna Rose PascoPas encore d'évaluation
- Bacteria Without Cell WallsDocument13 pagesBacteria Without Cell WallsNuura jeylani KasimPas encore d'évaluation
- PediatricsDocument21 pagesPediatricsJo Anne75% (8)
- Nursing Health History: Princess Jamela Camu Celline Isabelle ReyesDocument11 pagesNursing Health History: Princess Jamela Camu Celline Isabelle ReyesCelline Isabelle ReyesPas encore d'évaluation
- Thoracentesis IntroductionDocument8 pagesThoracentesis Introductionjyoti singhPas encore d'évaluation
- FengShui Inspection IDocument52 pagesFengShui Inspection IDavid Hu100% (3)
- Medicine2 - Myeloproliferative, Lymphoproliferative WorkshopDocument118 pagesMedicine2 - Myeloproliferative, Lymphoproliferative Workshopapi-3762917100% (1)
- GalemedicaljournalphobiasDocument4 pagesGalemedicaljournalphobiasapi-3954809780% (1)
- Sample Synthesis Essay - DepressionDocument3 pagesSample Synthesis Essay - DepressionKaren ReasonPas encore d'évaluation
- Briefing Practical Literature Searching and Critical Appraisal (Diagnosis and Therapy) - Dr. Lukman Ade Chandra, M.med., M. Phil (2022)Document16 pagesBriefing Practical Literature Searching and Critical Appraisal (Diagnosis and Therapy) - Dr. Lukman Ade Chandra, M.med., M. Phil (2022)Sheila Tirta AyumurtiPas encore d'évaluation
- Immunizations MeningococcalDocument2 pagesImmunizations MeningococcalVarun ArvindPas encore d'évaluation
- 21 Masterclass NLE Gapuz 2 - HANDOUTSDocument16 pages21 Masterclass NLE Gapuz 2 - HANDOUTSLimuel dale CaldezPas encore d'évaluation
- Human Behavior & Victimology FactorsDocument25 pagesHuman Behavior & Victimology FactorsAyessa Maycie Manuel OlgueraPas encore d'évaluation
- Complications of DiabetesDocument3 pagesComplications of Diabetesa7wfPas encore d'évaluation
- Preventing Non-Communicable Diseases Through Lifestyle ChangesDocument12 pagesPreventing Non-Communicable Diseases Through Lifestyle ChangesMeycauayan NHS (Region III - Meycauayan City)Pas encore d'évaluation
- Artritis Gout in Aviation MedicineDocument22 pagesArtritis Gout in Aviation MedicineBuyungPas encore d'évaluation
- Pentagon Review Royal PentagonDocument33 pagesPentagon Review Royal PentagonRichard Ines Valino99% (70)
- Complement System: Zaahira Gani, Cambridge, UKDocument2 pagesComplement System: Zaahira Gani, Cambridge, UKHarman SinghPas encore d'évaluation
- Comparison of Inflammatory Markers in HTNDocument6 pagesComparison of Inflammatory Markers in HTNDan JohnstonPas encore d'évaluation
- 11 Nutritional Problems of Adolescents 2Document30 pages11 Nutritional Problems of Adolescents 2Danilo Sare IIIPas encore d'évaluation
- Criminal Charges Swine Flu Edits v2 1Document112 pagesCriminal Charges Swine Flu Edits v2 1Kathlyn Stone100% (1)
- Non Follicular PyodermaDocument1 pageNon Follicular PyodermaMagPas encore d'évaluation
- Floating Clinic PresentationDocument28 pagesFloating Clinic PresentationAnonymous 9Q6gYJVbPas encore d'évaluation
- PATHOLOGY Board Exam ANsWERSDocument22 pagesPATHOLOGY Board Exam ANsWERSchristinejoan100% (1)
- Mini Stepper: Owner's ManualDocument9 pagesMini Stepper: Owner's ManualsalehgigPas encore d'évaluation
- Chest 1-4-1-1Document7 pagesChest 1-4-1-1Kahkashan HameedPas encore d'évaluation
- GIT SurgitoonsDocument127 pagesGIT Surgitoonswertfghuji100% (8)
- The Zombie FilesDocument6 pagesThe Zombie FilesVincent TomasinoPas encore d'évaluation
- Obesity: Sharmila A/P Rajendran E20141008930 Diploma Sains Dan MatematikDocument18 pagesObesity: Sharmila A/P Rajendran E20141008930 Diploma Sains Dan MatematikSharmila RajPas encore d'évaluation
- Causes of Pain in The Right Side of The HeadDocument3 pagesCauses of Pain in The Right Side of The HeadUtpal KumarPas encore d'évaluation