Académique Documents
Professionnel Documents
Culture Documents
Mulluscum Contagiosum Cantharone Article PDF
Transféré par
masjokoDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Mulluscum Contagiosum Cantharone Article PDF
Transféré par
masjokoDroits d'auteur :
Formats disponibles
case challenges • case challenges: dermatology• case challenges
Treatment of Molluscum Contagiosum
with Cantharidin: A Practical Approach
Erin F.D. Mathes, MD; and Ilona J. Frieden, MD
ABSTRACT
M
olluscum contagiosum is very com- of the social stigma of visible lesions. No one
mon. In this article we discuss the treatment is uniformly effective.
use of cantharidin as a treatment Treatment options include destructive
option for molluscum contagiosum and give therapies (curettage, cryotherapy, canthari-
detailed information about distribution sources, din, and keratolytics, among others), immu-
how to apply it, and caveats regarding its use. nomodulators (imiquimod, cimetidine, and
Molluscum contagiosum is a common vi- Candida antigen), and antivirals (cidofovir).
ral disease of childhood caused by a poxvirus, In this article we discuss and describe our first-
which presents with small, firm, dome-shaped, line treatment approach for those molluscum
umbilicated papules. It is generally benign and needing treatment — cantharidin.
self-limited, with spontaneous resolution within
6 months to several years. Watchful waiting can Erin F. Mathes, MD, is Pediatric Dermatology
often be an appropriate management strategy; Fellow, Department of Dermatology University of
however, some patients either desire or require California, San Francisco. Ilona J. Frieden, MD, is
treatment. Reasons for actively treating mol- Professor of Dermatology and Pediatrics, Depart-
luscum contagiosum may include alleviation of ments of Dermatology and Pediatrics University of
discomfort and itching (particularly in patients California, San Francisco.
where an eczematous eruption — the so-called Address correspondence to: Erin F. Mathes, MD,
“molluscum eczema” — is seen in association) 1701 Divisadero St., Box 0316, San Francisco, CA
or in patients with ongoing atopic dermatitis 94143-0316; fax 415-353-7850; e-mail mathese@
where more lesions are likely to be present. derm.ucsf.edu.
Other reasons for treatment include limitation Dr. Mathes and Dr. Frieden have disclosed no rel-
of spread to other areas and people, prevention evant financial relationships.
of scarring and superinfection, and elimination doi: 10.3928/00904481-20100223-03
For treatment, see page 125.
Editor’s note: Each month, this department features a discussion of an unusual diagnosis in genetics, radiology,
or dermatology. A description and images are presented, with the diagnosis and an explanation of how the diagnosis
was determined following. As always, your comments are welcome. E-mail pedann@slackinc.com.
124 | www.PediatricSuperSite.com PEDIATRIC ANNALS 39:3 | MARCH 2010
3903CaseChallenges.indd 124 3/3/2010 3:20:07 PM
case challenges
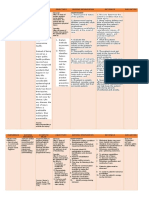
T R E A T M E N T SIDEBAR 1.
Cantharidin Application Instructions
(also see Figure 1 and Figure 2)
Treat only a few lesions (no more than four to five) at the first visit. In subsequent
A recent review of evidence sup- visits, treat no more than 12 to 15 lesions.
porting various treatment options Try to get the child’s cooperation, explaining that the medication will not hurt. If the
concluded that cantharidin may be the child is fearful and moving, assistance will be needed to apply without accidentally
getting the medication on normal, unaffected skin.
treatment of choice in young children
Use the wooden end of a cotton applicator to apply a small drop of cantharidin
because it is painless and effective.1
directly to each lesion, taking care not to apply to the surrounding skin. If medication
Cantharidin, a phosphodiesterase accidentally is applied to normal skin (as may happen in a moving infant), immedi-
inhibitor that causes vesiculation of ately wash off the medication.
the skin, was originally derived from Allow the cantharidin to dry for at least 5 to 10 minutes to minimize the risk of spread
the blister beetle, but now is synthe- to adjacent unaffected skin.
sized commercially.2 Careful appli- Attempting to wash off the medication is controversial. Some authors recommend
cation to the skin typically results in doing so after 2 to 6 hours, but the polymer created by the collodion makes this dif-
a small vesicle. Because molluscum ficult. Another option is leaving the medication on overnight, only attempting to wash
it off if visible blisters are noted a few hours later, although it is doubtful that this will
are very superficial skin lesions, ap-
actually halt the blistering effects.
plication causes skin vesiculation,
with extrusion of the molluscum
body, leading to the resolution of the SIDEBAR 2.
lesion.2 Although the evidence for Helpful Hints
the efficacy of cantharidin is mainly Gently shake the bottle, then stir with the applicator before applying to ensure an even
limited to retrospective case series, concentration of cantharidin.
many physicians use cantharidin as Do not treat intertriginous areas, or the face, initially. After determining typical response to
a treatment, and its use has a high medication, treatment in these areas can be considered:
rate of parental (60% to 90%) and For facial lesions, warn parents about the possibility of pigmentary alteration.
physician (92%) satisfaction.1,3-8 Do not treat lesions that are directly adjacent to the eye.
In 1997, President Clinton ap- For intertriginous areas, warn parents about the greater risk of excessive blistering, especial-
proved an amendment to the Food, ly in hot weather. If the weather is very hot, limit the number of lesions treated to just a few.
Drug and Cosmetic Act of 1962 that Do not treat inflamed molluscum, at least initially, as they may resolve spontaneously.
provides that certain drug products If there was little or no response after the first treatment, at the next visit, advise the patient
may be compounded by a physician to leave the cantharidin on for longer, or not to wash it off at all.
or pharmacist for individual patients. Over-the-counter oral analgesics, such as ibuprofen or acetaminophen, may help
with discomfort.
The Food and Drug Administration
Topical petrolatum may help soothe irritated skin. Before applying petrolatum, make sure
(FDA) has included cantharidin in
that the cantharidin has been thoroughly washed off. Liberal petrolatum application to
the proposed list of bulk substances areas with active cantharidin can cause spread of cantharidin and widespread blisters.10
that physicians and pharmacists are If surrounding dermatitis is present, treat it with 1% hydrocortisone ointment
permitted to compound for use in in- (over-the-counter).
dividual patients.5
APPLICATION ring, we (and others) believe the safety tage, is that application of cantharidin
Treating molluscum with canthari- profile is sufficiently favorable to con- is painless. Although pain (typically
din is not technically difficult. Although tinue using it for this purpose.1,3-5,7,8 very minor) may occur several hours
there is a small risk for adverse effects, A major advantage over certain treat- to a day later, children rarely associate
such as excessive blistering and scar- ments, such as cryotherapy and curet- this with their recent doctor visit, and
PEDIATRIC ANNALS 39:3 | MARCH 2010 www.PediatricSuperSite.com | 125
3903CaseChallenges.indd 125 3/3/2010 3:20:08 PM
case challenges
SIDEBAR 3.
Anticipatory Guidance11
Several hours after application, mild discomfort at the site of application occasionally
occurs. This can be treated by using cool compresses and by administering over-the-
counter analgesics, although, in our experience, this is rarely necessary.
One day after application, a small blister often forms, although, in some cases, only
redness or mild crusting is noted. If the blister is tense and uncomfortable, draining
with a sterilized needle may help diminish pain, although this is also rarely necessary.
Two to 4 days after application, the blister will crust or drain, leaving a superficial ero-
sion. Apply an antibiotic ointment or sterile petrolatum to the eroded area to encour-
age re-epithelialization.
Within 1 week, the area is typically healed, although postinflammatory erythema may
persist for a week or two. In darker skin types, postinflammatory hyper- or hypopig-
mentation may persist, at times for several months.
Scarring is rare. Occasionally, even untreated molluscum leave tiny pitted scars.
Figure 1. Cantharadin bottle with applicators.
are usually willing to have the medica- lation, which combines a higher con- these adverse effects occur in ap-
tion applied on subsequent visits. centration of cantharidin (1%) mixed proximately 6% to 46% of patients,
We disagree with a recent review with podophyllin and salycilic acid, in our experience, the rate is at the
by Silverberg that suggested that can- and has a much greater risk for caus- low end of this range.3,4,8 Temporary
tharidin should not be applied by pedi- ing excessive blistering, scarring, and erythema can occur in up to 37% of
atricians in their offices.9 Pediatricians even chemical cellulitis. patients.4,5 Care should be taken to
and family physicians perform many Cantharidin can only be applied avoid spreading the cantharidin to
procedures that are more complicated in a physician’s office and should unaffected areas or to the eyes. There
than cantharidin application, such as never be dispensed to patients for may be temporary pigment alteration
splinting, venipuncture, lumbar punc- that should resolve without scarring.
ture, intramuscular injection, lacera- Several “helpful hints” to use the
tion repair, and incision and drainage. Cantharidin can only be medication effectively and minimize
In this article, we give detailed instruc- size effects are summarized in Sidebar
tions regarding the use of cantharidin,
applied in a physician’s 2 (see page 125). The first time can-
including sources for purchasing, office and should never be tharidin is used, it is prudent to treat
techniques for application, potential only three or four lesions to assess the
pitfalls and adverse effects, and billing dispense to patients for individual patient’s response. Warn
codes for in-office treatment with this self-application. parents that although the medication is
medication. We believe that with the applied sparingly, there is a 1% to 5%
following information and guidance, chance of a larger blister developing.
cantharidin can become a very useful self-application (see Sidebar 1, page There is controversy regarding wheth-
tool for treating molluscum in the pri- 125, and Figure 1, and Figure 2, er the medication should be washed
mary physician’s office. page 127, for application instruc- off a few hours after application. Some
Cantharidin is commercially avail- tions). Most patients improve after authors recommend this practice, but
able in a 0.7% concentration, in a one or two visits.3,4,8 Complications because cantharidin is dissolved in
collodion base (see Table, page 127, include excessive blistering, pain, collodion, it forms a film upon drying,
for sources). This 0.7% formulation pruritis, and burning (see Figure 3, which is probably not easily removed
is strongly preferred for molluscum page 128, and Figure 4, page 128). with soap and water.7 Follow-up visits
treatment over a more potent formu- Although some authors estimate that to assess efficacy and perform further
126 | www.PediatricSuperSite.com PEDIATRIC ANNALS 39:3 | MARCH 2010
3903CaseChallenges.indd 126 3/3/2010 3:20:08 PM
case challenges
TABLE.
Distribution Sources: How to Purchase for Medical Offices*
Product
Company Formulation Address/phone E-mail/Website
Name
0.7% canthari- 91 Kelfield, Suite 5, Rexdale, On-
Dormer
Cantharone din in a col- tario, Canada M9W 5A3; (416) www.dormer.ca
Laboratories
lodion base 242 6167; fax: 877 436 7637
0.7% cantharidin 997 Seguin, Hudson, Quebec,
Pharmscience/
Canthacur in a collodion Canada J0P 1H0; 450-458-0158; CustomerServicePaladin@pharmascience.com
Omniderm
base fax: 450-458-7499
Cantharidin
crystals and
608 13th Ave., Council Bluffs,
collodion base
Delasco Cantharidin IA 51501-6401; (800) 831-6273; questions@delasco.com
sold separately
fax: (800) 320-9612
for in-office
compounding
3505 Austin Bluffs Parkway,
College Compounded to
Cantharidin Suite 101, Colorado Springs, CO info@collegepharmacy.com**
Pharmacy order
80918
*Cantharidin’s use is limited to in-office treatment by a physician. Please contact the suppliers for ordering requirements.
**Shipping to selected states only
treatments are typically scheduled ev-
ery 2 to 4 weeks. If patients have not
had any adverse reactions, more le-
sions can be treated than at the initial
visit. Individual lesions of molluscum
typically resolve after one treatment
but occasionally require retreatment,
particularly if they are large. In many
cases, after two to three treatments, the
molluscum will diminish in number
and gradually resolve. Sidebar 3 (see
page 126) outlines recommendations
for anticipatory guidance.
OTHER CONSIDERATIONS
Another problem that often Figure 2. Application of cantharadin to molluscum.
arises is the presence of so-called
“molluscum eczema,” a dermatitis present. Although the individual treated with a low to mid-potency
virtually identical to atopic derma- molluscum can be treated with can- topical steroid to alleviate it and
titis, which preferentially occurs in tharidin, even in sites of dermati- prevent autoinnoculation with fur-
areas of skin where molluscum are tis, the dermatitis itself should be ther spread of the virus.
PEDIATRIC ANNALS 39:3 | MARCH 2010 www.PediatricSuperSite.com | 127
3903CaseChallenges.indd 127 3/3/2010 3:20:09 PM
case challenges
Although there are few, random-
ized, prospective trials on treatments
for molluscum, a recent large retro-
spective study on cantharidin by Sil-
verberg et al found that 90% of 300
patients cleared and an additional
8% improved in an average of 2.1
treatments. Parental satisfaction was
95%.4,6 In their retrospective study
of 110 patients, Cathcart et al found
a 96% efficacy after approximately
two treatments and a parental satis-
faction rate of 78%.8 In contrast, in Figure 3. Chemical irritation from cantharidin application; this response is very unusual.
their prospective randomized trial
of four treatment modalities, Hanna
et al found that 36.7% of patients in
the cantharidin group were cured af-
ter one visit, an additional 43% after
two visits, and the remaining 20%
after three or more visits. The paren-
tal satisfaction rate for cantharidin
was 60%. The parental satisfaction
for curettage (the preferred treat-
ment modality in Hanna’s study)
was almost 90%.3 The practice envi-
ronment in Hanna’s study is signifi-
cantly different than most U.S. prac-
tices because phamacologic sedation
is available as needed for curettage.
In our experience, curettage is an ef-
Figure 4. Blisters following cantharidin application; the amount of blistering is more than
fective and acceptable treatment for typically occurs.
older children, especially when it is
difficult for the family to return for
several more visits.
The Current Procedural Termi-
nology (CPT) codes for billing for
destruction of molluscum are well-
established: CPT: 17110 (destruction
of up to 14 lesions) and 17111 (de-
struction of 15 or more lesions).
CONCLUSIONS
With appropriate precautions and
information provided, we believe
that the use of this medication by
pediatricians and other primary care Figure 5. Verruca vulgaris ring wart from cantharadin application.
128 | www.PediatricSuperSite.com PEDIATRIC ANNALS 39:3 | MARCH 2010
3903CaseChallenges.indd 128 3/3/2010 3:20:11 PM
case challenges
providers is safe and well within 2. Wolverton SE. Comprehensive Derma- views 2006, Issue 2. Art. No.: CD004767.
tologic Drug Therapy. Philadelphia, PA: DOI:10.1002/14651858.CD004767.pub2.
the technical expertise of any well-
Saunders; 2001;532. 7. Coloe J, Morrell DS. Cantharadin use
trained practitioner. 3. Hanna D, Hatami A, Powell J, et al. A among pediatric dermatologists in the treat-
Finally, although cantharidin is an prospective randomized trial comparing ment of molluscum contagiosum. Pediatr
excellent treatment option for mollus- the efficacy and adverse effects of four Dermatol. 2009;26(4):405-408.
recognized treatments of molluscum con- 8. Cathcart S, Coloe J, Morrell DS. Parental
cum, we do not recommend its use for tagiosum in children. Pediatr Dermatol. satisfaction, efficacy, and adverse events
common warts. For unknown reasons, 2006;23(6):574-579. in 54 patients treated with cantharidin for
the noninflammatory blisters caused 4. Silverberg NB, Sidbury R, Mancini AJ. molluscum contagiosum infection. Clin
Childhood molluscum contagiosum: Pediatr (Phila). 2008;48(2):161-165.
by the medication can result in so- experience with cantharidin therapy 9. Silverberg NB. A practical approach to
called “ring warts” (see Figure 5, page in 300 patients. J Am Acad Dermatol. molluscum contagiosum. Part 2. Contem-
128), leading to wart spread, rather 2000;43(3):503-507. porary Pediatrics. 2007;24(9):63-72.
5. Moed L, Shwayder TA, Chang MW. 10. Shah A, Treat J, Yan AC. Spread of can-
than improvement.
Cantharidin revisited: a blistering defense tharidin after petrolatum use resulting
of an ancient medicine. Arch Dermatol. in a varicelliform vesicular dermatitis.
REFERENCES 2001;137(10):1357-1360. J Am Acad Dermatol. 2008;59(2 Suppl
1. Brown J, Janniger CK, Schwartz CZ, Sil- 6. Van der Wouden JC, et al. Interventions 1):S54-S55.
verberg NB. Childhood molluscum conta- for cutaneous molluscum contagiosum. 11. Cantharone brochure. www.dormer.ca.
giosum. Int J Dermatol. 2006;45(2):93-99. Cochrane Database of Systematic Re- Dormer Laboratories, Canada.
3903CaseChallenges.indd 130 3/3/2010 3:20:14 PM
Vous aimerez peut-être aussi
- Treatment of Molluscum Contagiosum With Cantharidin: A Practical ApproachDocument7 pagesTreatment of Molluscum Contagiosum With Cantharidin: A Practical Approach79lalalaPas encore d'évaluation
- Ax00cwavtu34vwcn - Practical Management of Common Skin Injuries Lacerations Wounds Trigger Fingers and BurnsDocument10 pagesAx00cwavtu34vwcn - Practical Management of Common Skin Injuries Lacerations Wounds Trigger Fingers and BurnsEvelyn AtuyaPas encore d'évaluation
- Dermatology Case Reports: Diagnosis, Treatment and Prevention of Scabies: A Short CommentaryDocument2 pagesDermatology Case Reports: Diagnosis, Treatment and Prevention of Scabies: A Short CommentaryNidhaSavitriPas encore d'évaluation
- PPE-Rx DermatitisDocument2 pagesPPE-Rx DermatitisSAJIN ALEXANDERPas encore d'évaluation
- Jurnal Kulit AcneDocument7 pagesJurnal Kulit AcnePsyhlaPas encore d'évaluation
- Update On The Treatment of Molluscum Contagiosum in ChildrenDocument9 pagesUpdate On The Treatment of Molluscum Contagiosum in Childrensamsara vrindaPas encore d'évaluation
- Canmedaj01659 0013Document2 pagesCanmedaj01659 0013Andrew SuryaPas encore d'évaluation
- Scabies Treatment Complication and Progn Ca29e321Document4 pagesScabies Treatment Complication and Progn Ca29e321Ari KurniawanPas encore d'évaluation
- Skin Therapy Letter PDFDocument8 pagesSkin Therapy Letter PDFSherlocknovPas encore d'évaluation
- Permethrin Beats Benzyl Benzoate for Scabies CureDocument7 pagesPermethrin Beats Benzyl Benzoate for Scabies CureNicoleta PlesaPas encore d'évaluation
- Current and Emerging Treatments For VitiligoDocument13 pagesCurrent and Emerging Treatments For VitiligoAnnisa Tria FadillaPas encore d'évaluation
- A - Pratic Guide Pediatric Wound CareDocument9 pagesA - Pratic Guide Pediatric Wound CareLicia GabriellePas encore d'évaluation
- Tinea Faciei - Relato de CasoDocument3 pagesTinea Faciei - Relato de CasoJosé Paulo Ribeiro JúniorPas encore d'évaluation
- Acne in Childhood Wendy Kim, Do and Anthony J. Mancini, MDDocument10 pagesAcne in Childhood Wendy Kim, Do and Anthony J. Mancini, MDPrajnamita Manindhya El FarahPas encore d'évaluation
- Luka ModernDocument1 pageLuka Modernahmad iffa maududyPas encore d'évaluation
- Pi Is 0190962217328724Document3 pagesPi Is 0190962217328724Muhammad Irfan AnwarPas encore d'évaluation
- Cantharidin therapy for molluscum contagiosumDocument1 pageCantharidin therapy for molluscum contagiosumAai LestariPas encore d'évaluation
- PIIS0190962223010174Document7 pagesPIIS01909622230101745jnpzgz4cqPas encore d'évaluation
- Tinea CorporisDocument7 pagesTinea CorporisAziza Ulfie WijayaniPas encore d'évaluation
- Nursing Interventions and Rationales - Impaired Skin IntegrityDocument11 pagesNursing Interventions and Rationales - Impaired Skin IntegrityJOSHUA DICHOSOPas encore d'évaluation
- VitiligoDocument13 pagesVitiligoFebyan AbotPas encore d'évaluation
- Case Studies From Dermatology WorkshopDocument35 pagesCase Studies From Dermatology Workshopstarn.serventisPas encore d'évaluation
- Acne in Adolescents: BackgroundDocument4 pagesAcne in Adolescents: BackgroundMuthu RaajendhiraPas encore d'évaluation
- Referat Kandidosis Kutis - Dhira Dan A. Fari-70700120034 Dan 038Document14 pagesReferat Kandidosis Kutis - Dhira Dan A. Fari-70700120034 Dan 038Ahmad Fari Arief LopaPas encore d'évaluation
- Impaired Skin IntegrityDocument2 pagesImpaired Skin IntegrityEli AyasePas encore d'évaluation
- Original Article: AbstractDocument3 pagesOriginal Article: Abstractyohanes22Pas encore d'évaluation
- Corneal Ulcer - The Fisrt ArticuleDocument3 pagesCorneal Ulcer - The Fisrt Articuleduvan LinaresPas encore d'évaluation
- Tinea CorporisDocument2 pagesTinea CorporisImas Puterii MunthePas encore d'évaluation
- Pengģunaan ABDocument8 pagesPengģunaan ABPrashetyaQusnaPas encore d'évaluation
- Ali 2019Document8 pagesAli 2019Ana Claudia Kordelos DinizPas encore d'évaluation
- PanaceaJMedSci 11 2 289 296Document8 pagesPanaceaJMedSci 11 2 289 296Jenerio PanggabeanPas encore d'évaluation
- Jurnal FixDocument29 pagesJurnal FixPanji Wage KosasihPas encore d'évaluation
- Jurnal Luka Bakar - MetcovazinDocument7 pagesJurnal Luka Bakar - MetcovazinJokosatya99 Jokosatya99Pas encore d'évaluation
- Psoriasis Case StudyDocument4 pagesPsoriasis Case StudyMIKAELLA BALUNANPas encore d'évaluation
- Antifungal AgentsDocument5 pagesAntifungal AgentsSanti AprilianaPas encore d'évaluation
- AAD Monkeypox Caring For SkinDocument2 pagesAAD Monkeypox Caring For SkinBHUVANESHWARAN KARTHIKEYAN (DHRUVA)Pas encore d'évaluation
- Controlling Scabies: Updated Diagnosis and Treatment StrategiesDocument16 pagesControlling Scabies: Updated Diagnosis and Treatment StrategiesToñi González RuizPas encore d'évaluation
- Critical Appraisal OM - Ni WayanDocument7 pagesCritical Appraisal OM - Ni WayanwayanPas encore d'évaluation
- Review in Peeling ComplicationsDocument8 pagesReview in Peeling ComplicationschipanzePas encore d'évaluation
- Jurnal FixDocument27 pagesJurnal FixPanji Wage KosasihPas encore d'évaluation
- IntroductionDocument21 pagesIntroductionfarmasi_hmPas encore d'évaluation
- Maryville NURS 623 ExamDocument14 pagesMaryville NURS 623 ExamWizzardPas encore d'évaluation
- Crisaborole RCTDocument6 pagesCrisaborole RCTNotfor TaoPas encore d'évaluation
- PPK Perdoski 2017 Skabies (English)Document3 pagesPPK Perdoski 2017 Skabies (English)yumizonePas encore d'évaluation
- New Drugs: Self-Test QuestionsDocument3 pagesNew Drugs: Self-Test QuestionscPas encore d'évaluation
- A Case Study On Bullous PemphigoidDocument2 pagesA Case Study On Bullous PemphigoidMedtext PublicationsPas encore d'évaluation
- Use of Co Mupimet Powder for Infected Lacerated WoundsDocument5 pagesUse of Co Mupimet Powder for Infected Lacerated WoundsAB MISHRAPas encore d'évaluation
- Medicina 58 00115Document12 pagesMedicina 58 00115satriaPas encore d'évaluation
- Topical Formic Acid Puncture Technique For The Treatment of Common WartsDocument6 pagesTopical Formic Acid Puncture Technique For The Treatment of Common WartsAndrea CalderaPas encore d'évaluation
- Effectiveness of Oral Albendazole As A Treatment For Pediculosis CapitisDocument8 pagesEffectiveness of Oral Albendazole As A Treatment For Pediculosis CapitisFlorensia WodaPas encore d'évaluation
- Treatment of Scabies and Crusted VariantsDocument4 pagesTreatment of Scabies and Crusted Variantsduch2020Pas encore d'évaluation
- Current Issues in The Treatment of Acne VulgarisDocument8 pagesCurrent Issues in The Treatment of Acne VulgarisajiPas encore d'évaluation
- Konsep Pelayanan Kesehatan Primer DalamDocument7 pagesKonsep Pelayanan Kesehatan Primer DalamIqbal FahmiPas encore d'évaluation
- Effectiveness of Oral Albendazole As A Treatment For Pediculosis CapitisDocument6 pagesEffectiveness of Oral Albendazole As A Treatment For Pediculosis CapitisAlmuizzu NurjannahPas encore d'évaluation
- InJPharPract 13 4 355Document4 pagesInJPharPract 13 4 355Yeol LoeyPas encore d'évaluation
- Chemical Peels Deep, Medium, and LightDocument9 pagesChemical Peels Deep, Medium, and LightDeborah DobieszPas encore d'évaluation
- ICU Toxic Epidermal Necrolysis Guideline PDFDocument9 pagesICU Toxic Epidermal Necrolysis Guideline PDFaleexiipsszPas encore d'évaluation
- GENERAL SANTOS DOCTORS’ MEDICAL SCHOOL FOUNDATION NURSING CARE PLANDocument4 pagesGENERAL SANTOS DOCTORS’ MEDICAL SCHOOL FOUNDATION NURSING CARE PLANFran LanPas encore d'évaluation
- Nutrition 101 Presentation PDFDocument20 pagesNutrition 101 Presentation PDFViktória MolnárPas encore d'évaluation
- Molluscumcontagiosum RecentPatentsonInflammation May2017Document11 pagesMolluscumcontagiosum RecentPatentsonInflammation May2017masjokoPas encore d'évaluation
- Molluscumcontagiosum RecentPatentsonInflammation May2017Document11 pagesMolluscumcontagiosum RecentPatentsonInflammation May2017masjokoPas encore d'évaluation
- Narative Text Kancil Dan BuayaDocument2 pagesNarative Text Kancil Dan BuayamasjokoPas encore d'évaluation
- Mulluscum Contagiosum Cantharone Article PDFDocument6 pagesMulluscum Contagiosum Cantharone Article PDFmasjokoPas encore d'évaluation
- Daftar PustakaDocument3 pagesDaftar PustakamasjokoPas encore d'évaluation
- Daftar Pustaka 1.: DR Daniel J Bell A.Prof Frank GaillardDocument2 pagesDaftar Pustaka 1.: DR Daniel J Bell A.Prof Frank GaillardmasjokoPas encore d'évaluation
- Daftar Pustaka 1.: DR Daniel J Bell A.Prof Frank GaillardDocument2 pagesDaftar Pustaka 1.: DR Daniel J Bell A.Prof Frank GaillardmasjokoPas encore d'évaluation
- GcagdhsgdhjsagdhjsgdhsgdhsgdhDocument1 pageGcagdhsgdhjsagdhjsgdhsgdhsgdhmasjokoPas encore d'évaluation
- Abnormal Psychology Movie Character AnalysisDocument11 pagesAbnormal Psychology Movie Character AnalysisEsaïe Greña100% (1)
- Ra-031103 - Professional Teacher - Secondary (Tle) - Tacloban - 10-2022Document135 pagesRa-031103 - Professional Teacher - Secondary (Tle) - Tacloban - 10-2022AILENPas encore d'évaluation
- IV Complications Ward ClassDocument28 pagesIV Complications Ward ClassMel Belisario TubeoPas encore d'évaluation
- Practice Quiz For EpidemiologyDocument4 pagesPractice Quiz For EpidemiologyOsama Alhumisi100% (3)
- Manajemen Pre-Operatif Pasien Dengan DMDocument12 pagesManajemen Pre-Operatif Pasien Dengan DMyanayas28Pas encore d'évaluation
- Bipolar 1 Disorder NCPDocument3 pagesBipolar 1 Disorder NCPJoy-Rena Sabinay OchondraPas encore d'évaluation
- Digital Healthcare Market Research 3Document33 pagesDigital Healthcare Market Research 3Nero AngeloPas encore d'évaluation
- Fansidar Drug StudyDocument2 pagesFansidar Drug StudyjangziePas encore d'évaluation
- Emergency Department Approach to Allergic Reactions and AnaphylaxisDocument25 pagesEmergency Department Approach to Allergic Reactions and AnaphylaxisEden FerrerPas encore d'évaluation
- Skenario C Blok 22Document40 pagesSkenario C Blok 22Ambhi GanaPas encore d'évaluation
- Advocacy LetterDocument5 pagesAdvocacy Letterapi-381362041Pas encore d'évaluation
- Medical Leave CertificatesDocument4 pagesMedical Leave CertificatesDhana LakshmiPas encore d'évaluation
- Mis NotesDocument12 pagesMis NotesVasundharaPas encore d'évaluation
- DSHS Letter To Bowie County Judge GA-32 50 Percent Occupancy For BusinessesDocument2 pagesDSHS Letter To Bowie County Judge GA-32 50 Percent Occupancy For BusinessesField WalshPas encore d'évaluation
- Long-Term Results of the Kumamoto Study on Optimal Diabetes Control in Type 2 Diabetic PatientsDocument19 pagesLong-Term Results of the Kumamoto Study on Optimal Diabetes Control in Type 2 Diabetic PatientsCarlosZamPas encore d'évaluation
- BLOOD POST TEST REVIEWDocument11 pagesBLOOD POST TEST REVIEWCherry Ann Garcia DurantePas encore d'évaluation
- NUTR4320FINAL11Document10 pagesNUTR4320FINAL11rijzPas encore d'évaluation
- MrdicDocument18 pagesMrdicpapa0011Pas encore d'évaluation
- Aspects-of-Homeopathy-Ian-Watson.07907 - 2therapeutic Index PDFDocument4 pagesAspects-of-Homeopathy-Ian-Watson.07907 - 2therapeutic Index PDFSohail LatifPas encore d'évaluation
- Extraoral Examination 1Document58 pagesExtraoral Examination 1SyaZuWaN JaMiLPas encore d'évaluation
- CPR SeminarDocument76 pagesCPR SeminarAmy Lalringhluani Chhakchhuak100% (3)
- Areeb Organics Tri-Fold BrochureDocument6 pagesAreeb Organics Tri-Fold Brochurerubana reazPas encore d'évaluation
- The Vision, Mission and Core Values of The Institution: - o o o - o oDocument23 pagesThe Vision, Mission and Core Values of The Institution: - o o o - o oYvonne de ChavezPas encore d'évaluation
- EphedraDocument9 pagesEphedraapi-367367047Pas encore d'évaluation
- RICE Therapy for Common Soft Tissue InjuriesDocument2 pagesRICE Therapy for Common Soft Tissue InjuriesmoizitouPas encore d'évaluation
- The Black Death: A Deadly PandemicDocument1 pageThe Black Death: A Deadly PandemicPaul Christian G. SegumpanPas encore d'évaluation
- HOSPITALFORMULARYDocument32 pagesHOSPITALFORMULARYRana EhtishamPas encore d'évaluation
- An Analysis of Ethical Issues in Pharmaceutical IndustryDocument19 pagesAn Analysis of Ethical Issues in Pharmaceutical IndustrySuresh KodithuwakkuPas encore d'évaluation
- G-Ranitidine: Commonly used medicines for acid reflux and ulcersDocument4 pagesG-Ranitidine: Commonly used medicines for acid reflux and ulcersHoney Grace L LemorenasPas encore d'évaluation
- October 2023 PRC PLE Schedule and Reminders 2Document4 pagesOctober 2023 PRC PLE Schedule and Reminders 2TrisPas encore d'évaluation