Académique Documents
Professionnel Documents
Culture Documents
Preceptb13 2
Transféré par
Serious LeoTitre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Preceptb13 2
Transféré par
Serious LeoDroits d'auteur :
Formats disponibles
West Visayas State University College of Medicine Class of 2021
B13M1L2: History and PE in Pediatric Respiratory
Medicine
Dr. Emiliana G. Carmona | February 27, 2019
Trans Group 12: Pino, Pueblo, Puey | Editor: Postrado | 0929-335-4878
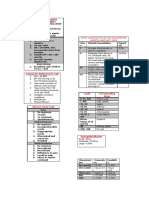
OUTLINE Characteristics
o Quality (e.g. Is cough productive or not productive?)
I. History 1 o Severity (Is it so severe that the child should miss his class
A. General Considerations 1 or just mild that does not affect ADL?)
B. Chief Complaint 1 Associated symptoms
C. History of Present Illness 1 Aggravating and precipitating factors
D. Medical History 2
E. Family History 2
Relieving factors
F. Personal and Social History 3 Current situations
II. Physical Examination 3 o improving or deteriorating
A. Inspection 3 o If medications were given, was there relief?
B. Palpation 4 Effects on activities of daily living
C. Percussion 4 Exercise is a common trigger factor for cough and wheezing
D. Auscultation 4 in many patients with hyperactive airways.
Diurnal variation of symptoms may be apparent, and
LEGEND attention should be paid to changes that occur at night.
Previous diagnosis of similar episodes (Are you having a
Important Lecturer Book Old Trans Trans problem which is recurrent in nature?)
Comm Previous treatment and efficacy
○ From the drugs alone, you will already have an idea on
what the patient is having.
HISTORY B. CHIEF COMPLAINT
The historian should identify the chief complaint and the COUGH
person most concerned about it. Ask for quality, severity, timing, duration, and precipitating
The illness at presentation should be documented in detail factors.
regarding onset and duration, the environment and If the cough happens after eating, think of aspiration.
circumstances under which it developed, its manifestations Was the patient exposed to fire, perfume, or toxins?
and their treatments, and its impact on the patient and Explain how it happened.
family. How did it progress, was it self-limiting or did you do
Symptoms should be defined by qualitative and quantitative something to stop the series of coughs?
characteristics as well as by their timing, location, Cough and vomiting
aggravating or alleviating factors, and associated If the cough has been there for more than 2 weeks, think of
manifestations. TB.
Common symptoms are fever, cough and sputum production, For severity: Does it awaken you at night?
wheezing or noisy breathing, dyspnea, and chest pain. If the timing is related to food intake, think of GERD.
Relevant past medical and laboratory data should be included If the cough occurs at night and early morning, think of
in the documentation of present illness allergic cough or bronchial asthma.
A. GENERAL CONSIDERATIONS DYSPNEA
ONSET A subjective feeling of difficulty in breathing
The first thing that you ask when you get the history. To know Grunting (At rest? Or after strenuous activity?)
if the problem is acute or chronic. An audible expiratory sound.
Gradual (e.g., with some interstitial disease) Posture can help differentiate if cardiac or respiratory in
Sudden (e.g., with foreign body obstruction) origin e.g. squatting in TOF
The historian should ask about initial manifestations and who
TACHYPNEA
noticed them first.
The age at first presentation is important because respiratory An objective finding of an increase in respiratory rate.
disease that manifest soon after birth are more likely to have May not only of respiratory in origin but can also be in cardiac.
been inherited or to be related to congenital malformations. CHEST PAIN
Location Ask for timing, severity, radiation
Radiation HEMOPTYSIS
Duration
May also be non-pulmonary
Frequency, chronology
Ask for amount of blood
CLASSIFICATION Significant to cause you anxiety?
Classification Based on Duration of Illness Frank blood or mixed with sputum?
Acute <3 weeks Associated with leg pain, chest pain, or shortness of breath?
Subacute 3 weeks to 3 months In pulmonary embolism, you may also have hemoptysis or
Chronic >3 months pulmonary congestion.
Recurrent symptoms are clearly discontinuous It is also important to know where the blood came from e.g.
with documented intervals of well-being tonsils (sputum mixed with streaks of blood)
B13M1L2: History and PE in Pediatric Respiratory Medicine DVS – MED 2 1/5
CYANOSIS SPUTUM PRODUCTION
Primarily cardiac Productive Cough - When it brings up (produces) mucus or
Central versus peripheral some sort of fluid, including blood.
Associated wheezing? No need to measure the volume of expectorated fluid.
If pediatric patient + difficulty breathing + cyanosis = status Unproductive Cough - Is one that does not bring up any
asthmaticus mucus or other secretion. Also known as a dry cough, a non-
EXERCISE TOLERANCE productive cough often is caused by some sort of irritation in
Ask if the infant eats slowly, tires during feeding, cyanosis the throat. Many people with describe the irritation as a
with feeding "tickling" or "scratchy" sensation.
Children – inability to keep up with others if the same age Volume might not be that reliable in children as some children
The closest differential diagnoses that you will have which will just swallow the phlegm.
refer to your respiratory system are also problems which refer Color:
to your cardiovascular system. Viral (whitish)
WHEEZING bacterial (yellow)
allergic (whitish)
Ask for timing
lower resp. tract infection e.g. pneumonia with
FAINTING AND SYNCOPE consolidation (rusty)
Weakness, light headedness, loss of consciousness, relation to Chronic cough with yellow color does not always mean
posture infection it might be neutrophilic.
OTHER ASSOCIATED SIGNS AND SYMPTOMS Amount
Fever Consistency
Malaise Mucoid? Purulent? Watery?
Fatigue Time of the day when sputum production is worse
Anorexia D. MEDICAL HISTORY
Night sweats (e.g. in TB) Allergies, including seasonal and environmental
Palpitation ○ common respiratory problems in the pediatric age group
Weight loss are allergic cough, bronchial asthma, or allergic rhinitis
GI reflux Medications used, over-the-counter and prescription meds
Runny nose Herbal / traditional preparations
Sore throat
Growth rate – failure to thrive often exhibits slow weight gain
Stridor
relative to height
○ Pathology usually in the upper airway.
Immunization status
○ High pitched, inspiratory. A serious manifestation that is
○ (before HiB vaccine, Haemophilus influenza type B is
sometimes an emergency.
the most common etiologic agent of cough in children)
○ Differentials: Laryngotracheobronchitis, epiglottitis,
bacterial tracheitis Medical conditions, admissions, surgeries
○ If patient presents with recurrent stridor since birth or ○ Frequency of colds and respiratory infections, recent
chronic stridor, think of laryngomalacia viral illness, communicable diseases
○ Nasal polyps, chronic sinusitis, asthma, bronchitis,
C. HISTORY OF PRESENT ILLNESS pneumonia, Chronic obstructive pulmonary disease
ONSET (COPD), TB (disease or exposure, mantoux test, CXR),
Gradual or Sudden Onset. cancer, cystic fibrosis
○ How did it start, when did it start. ○ Diabetes mellitus, thyroid disorder, renal disease
SMOKING ○ Joint pain or swelling, cardiac murmurs, valvular heart
disease
Not only that of the patient but of exposure from family ○ Down’s syndrome
members or from community.
Exposure to substances while in utero
DIFFICULTY OF BREATHING Blood transfusion
“Ginalagas ang pagginhawa” Ask the patient what he exactly Birth and prenatal history if you are dealing with a neonate
means. because you might be dealing with neonatal pneumonia,
How will you ask children? sepsis or congenital malformations.
o You can ask them to draw. They might draw someone The historian should inquire about the course of pregnancy,
being strangulated indicating that he has difficulty of particularly whether the mother and fetus suffered from
breathing infections, metabolic disorder, or exposure to noxious
OCCUPATIONAL HISTORY agents.
Some parents nowadays bring their children to work. Duration of pregnancy, possible multiple births and
Whatever work exposure the parents has the children circumstances leading to the onset of labor should be noted.
experiences it too. Difficult labor and delivery may cause respiratory problems
COUGH WITH POST-TUSSIVE VOMMITING at birth and the physician should ask about birth weight and
Apgar scores.
Occurred by vomiting only, think of gastrointestinal disease
After vomiting ask the appetite of the patient. E. FAMILY HISTORY
o If it is post-tussive (relating to cough) the patient will still The historian should review at least two generations on
have good appetite. Unlike when it is gastrointestinal in either side. The parents should be asked if they are
origin there will be loss of appetite. related by blood, and information should be obtained
In children, majority of patients presenting with vomiting about any childhood deaths in the family
would turn out to have pneumonia.
B13M1L2: History and PE in Pediatric Respiratory Medicine DVS – MED 2 2/5
The health of patient’s siblings and of brothers and ○ Degree of comfort or distress
sisters of both parents should be documented. ○ Growth parameters concordant with age
Particular attention should be paid to histories of ○ Character of cry
asthma, allergies and hay fever, chronic bronchitis, ○ Nutritional, hydration, and mental status
emphysema, tuberculosis, cystic fibrosis, and sudden For newborns and infants, feeding is a substantial physical
unexpected infant death. exercise and may lead to distress in the presence of
Others at home with similar symptoms respiratory distress. Inquiring how long it takes the patient to
Allergies, atopy, asthma, TB, cystic fibrosis, bronchitis finish a meal would equate to asking for exercise tolerance.
Diabetes mellitus CHEST APPEARANCE
Sudden Infant Death (SIDS) Observe shape/form:
Heart disease ○ Skeletal deformities e.g. kyphosis, scoliosis
F. PERSONAL AND SOCIAL HISTORY ○ Barrel chest (associated with pulmonary emphysema)
Feeding history ○ Pectus excavatum/Funnel chest
○ should include the amount, type, and schedule of ○ Pectus carinatum/Pigeon chest/Chicken Breast
food intake. Historian should ask if the child was fed Prominent subcutaneous blood vessels of the chest
by breast or bottle ○ Due to mediastinal disease
○ history of cough or choking during feeding should ○ Due to obstruction of the SVC, i.e. vena cava syndrome,
alert the historian to the possibility of pulmonary or azygos vein by a tumor (formation of collateral
aspiration. circulation)
Smoking history (number of packages/day, number of Chest circumference
years) ○ Smaller than the head circumference in the first 9-12
Exposure to second hand cigarette smoke, wood months of life
smoke, pets, ○ Larger than the head at 1 year due to the growth of the
chest muscles
Crowded living conditions
If HC>CC at 1 year, either there is a problem in the
Poor personal or environmental cleanliness
head e.g. hydrocephalus or a problem in the growth
High stress levels of the chest muscle in malnutrition.
Institutional living In infancy, AP diameter = Transverse diameter
Substance use At 2 years, AP diameter < Transverse diameter (wider chest)
○ alcohol, caffeine, street drugs, including injection
and inhaled drugs /solvents RESPIRATION
Human immunodeficiency virus (HIV) Both chest and abdomen move during normal respiration.
Obesity In infants:
○ Abdominal movements are more visible than thoracic
Immigration or travel abroad
movements
○ The abdomen bulges during inspiration (by the downward
PHYSICAL EXAMINATION movement of the diaphragm)
Best accomplished with the patient standing or comfortably ○ The thoracic cage moves upward and outward (chest
seated in an erect position. expansion)
Disadvantages of PE in the lying position: ○ The abdomen flattens and the thoracic cage returns to
○ Chest may not expand symmetrically resting position upon expiration.
○ Auscultation and percussion sounds may be dampened Observe the abdomen when measuring respiratory rates
since the chest wall is compressed Respiratory rates differ among sleep states and become more
It is important to use the anatomical reference points of the variable during wakefulness.
chest and back. Points to remember:
○ Normal rate depends on the age of the patient
Midscapular Line ○ Describe the patient’s behavioral state
Suprascapular Area
○ Count over at least one minute
Interscapular Area
Normal Respiratory Rates. From Adeos Notes.
Infrascapular Area
AGE GROUP RR (BREATHS/MINUTE)
0-6 months 30-60
> 6 months-1 year 30-50
Axillary Area > 1-3 years 24-40
Anterior Axillary Area > 3-5 years 22-34
Infraaxillary Area > 5-12 years 14-25
Midaxillary Line > 12 years 12-20
Posterior Axillary Line Breathing character:
○ Hyperpnea- deep respiration
Midclavicular Line ○ Hypopnea- shallow respiration
Infraclavicular Area ○ Kussmaul breathing- deep, sighing breathing; in
Mammary Area metabolic acidosis
Midsternal Line
Rate changes:
Inframammary Area
○ Tachypnea
Reference points on the trunk. Decreased lung compliance
Metabolic acidosis
A. INSPECTION
Fever (increase at 5-7 breaths per minute/degree
Observe for the following: above 37˚C)
○ Acutely or chronically ill
B13M1L2: History and PE in Pediatric Respiratory Medicine DVS – MED 2 3/5
○ Bradypnea Atelectasis
Alkalosis Infiltrating tumor mass between the lungs and the
CNS depression chest wall
Rhythm changes: C. PERCUSSION
○ Periodic breathing- in newborns and preterms
Striking the chest wall and perceiving vibrations that are
cycles of regular and rapid breathing, may then stop
heard by the ears and felt by the fingers.
but regular breathing afterwards
Causes air-filled thorax and its contents to vibrate.
not associated with bradycardia and cyanosis
Fluid and tissues that do not contain air do not vibrate by
Apnea if a/w bradycardia and cyanosis.
ordinary percussion strokes.
○ Cheyne-Stokes respiration- cycles of increasing and
Not performed in all pediatric patients
decreasing tidal volume separated by apnea
○ Biot breathing- irregular cycles of respiration at variable Character of percussion notes is altered by:
tidal volumes interrupted by apnea ○ Ability of the chest wall to vibrate
An ominous finding in patients with severe brain ○ Vibrating response of the lung
damage. ○ Damping effect of solid organs or lesions
Points to remember:
SIGNS OF INCREASED RESPIRATORY EFFORT o Lesions 5 cm away from the chest wall or < 2-3 cm in
Dyspnea in older children diameter will not alter percussion note.
Objective signs of distressed breathing: o Free fluid in the pleural cavity may not be detected
○ Chest wall retractions unless the volume exceeds 200-250 mL, although it can
○ Alar flaring be detected by PE before it can be seen on X-ray.
○ Orthopnea Methods:
○ Paradoxical breathing movements ○ Direct- percuss directly to the area
Paradoxical respiration when the abdomen is flat at ○ Mediate- use of plexor and pleximeter
inspiration and prominent at expiration Avoid surface contact by any other part of the hand because
○ Visible use of accessory muscles this dampens out vibrations.
Scalenes Percussion notes:
Sternocleidomastoids ○ Resonant- normal chest
Trapezii ○ Dull- solid structures and fluid-filled areas
Latissimi dorsi ○ Tympanitic-hollow, air-filled areas
Abdominal muscles In pneumothorax and emphysema
Head bobbing can also be seen in respiratory distress. Expected in young infants with thin chest walls
B. PALPATION Percussion Notes and Their Characteristics
Symmetry
○ Movement is seen and felt
○ Done with the examiner behind the patient
Test for chest expansion
o Place your thumbs at about the level of the 10th ribs,
with your fingers loosely grasping and parallel to the
lateral rib cage. As you position your hands, slide them
medially just enough to raise a loose fold of skin on each
side between your thumb and the spine.
○ Ask the patient to inhale deeply. Watch the distance D. AUSCULTATION
between your thumbs as they move apart during
Goals:
inspiration, and feel for the range and symmetry of the
○ Listen to characteristics of breath sounds in different
rib cage as it expands and contracts. This is sometimes
areas.
termed lung excursion.
○ Compare the sounds on both sides of the same area.
Asymmetry of respiration if one hand is not moving or has
Points to remember:
lesser movement compared to the other.
o Listen directly over the chest wall without intervening
Lagging if one hand is moving slower than the other;
clothes
present in presence of fluid, consolidation, and
o In young infants, one must catch whatever is available in
atelectasis.
whatever position they are.
Pain and tenderness
Lying, prone, or supine, but not lying on one side
Position of the trachea Sitting especially when held by a parent.
Tactile fremitus o Use the bell of the stethoscope in younger infants since
○ Employ palm or ulnar surface of the hand the diaphragm will pick up sounds from too large an area.
○ Sound vibrations that originate in the larynx pass down o Make sure the chest piece is not too cold.
the bronchi and causes the lungs and chest walls to o Make sure that the child is not shivering.
vibrate. o Child’s face must be in neutral position.
○ May be diminished or absent in females since the female o Examine the chest in a methodical fashion to include all
voice is of higher frequency than the lungs. parts of the chest.
○ High-pitched in children corresponding to small lungs. Clinical points about normal breath sounds:
○ Increased with lung consolidation as in pneumonia o Inspiratory phase duration is twice as long as expiration
○ Decreased or may disappear in: o There is no pause between inspiration and expiration
Effusion or fluid between the lungs and the chest o The end of expiratory phase is silent
wall
Thickening of the pleura
B13M1L2: History and PE in Pediatric Respiratory Medicine DVS – MED 2 4/5
Sounds heard at auscultation:
○ Normal vesicular sounds
REVIEW QUESTIONS
Common normal sounds heard all over the chest, 1. The following are sign of respiratory distress, EXCEPT
particularly over the axilla and infrascapular area a. Cheyne-Stokes respiration
Transmission of sounds is through the alveoli b. Alar flaring
Heard over the entire phase of inspiration c. Use of accessory muscles of respiration
Expiration immediately follows d. Chest retractions
○ Bronchial breath sounds 2. Which of the following is a cause of prominent veins in the
Heard over the trachea and over the midline chest?
Elsewhere, it is usually pathologic a. Portal hypertension
○ Bronchovesicular b. Vena cava syndrome
Heard more on infants with thin chest wall c. Respiratory distress
Characteristics of Breath Sounds d. Congestive heart failure
3. Which of the following is TRUE in respiratory rate changes?
a. Metabolic acidosis presents with tachypnea
b. Bradypnea is a sign of decreased lung compliance
c. Respiratory rate changes in newborns are always
pathologic
d. Fever has an unpredictable effect on RR
4. Which of the following is FALSE regarding chest dimensions?
a. An increased HC relative to CC would indicate
hydrocephalus
b. The head is always larger in the first months of life in
normal neonates.
c. A child with an equal HC and CC is a well-developed,
balanced child.
d. In infancy, AP diameter=Transverse diameter
5. Which of the following pertains to bronchial breath sounds?
a. These are added breath sounds
b. Inspiratory and expiratory sounds are equal in duration
c. These are soft sounds
d. Usually heard over the trachea
A, B, A, C, D
REFERENCES
1. Bickley, L.S. (2013). Chapter 8. Bates’ Guide to Physical
Examination and History Taking.
2. Carmona, E.G. (2019 February). History and PE of the Chest
in Pediatric Patients.
○ Adventitious sounds 3. WVSU-MED 2019 (2017, February). History and PE of the Chest
Crackles in Pediatric Patients.
Wheezes
Rhonchi
Adventitious or Added Breath Sounds
Diminished or absent breath sounds due to absence of air flow
from either total or partial obstruction.
o Due to constriction, consolidations, fluids, or collapse of
the lungs.
B13M1L2: History and PE in Pediatric Respiratory Medicine DVS – MED 2 5/5
Vous aimerez peut-être aussi
- Thyroid Gland Agenesis/dysgenesisDocument4 pagesThyroid Gland Agenesis/dysgenesisSerious LeoPas encore d'évaluation
- CBC DidacticsDocument22 pagesCBC DidacticsSerious LeoPas encore d'évaluation
- M - Mask Adjustment R - Reposition Airway S - Suction Mouth and Nose O - Open Mouth P - Pressure Increase A - Airway AlternativeDocument4 pagesM - Mask Adjustment R - Reposition Airway S - Suction Mouth and Nose O - Open Mouth P - Pressure Increase A - Airway AlternativeSerious LeoPas encore d'évaluation
- Level of Bilirubin To Cause Jaundice in Older Children and AdultsDocument2 pagesLevel of Bilirubin To Cause Jaundice in Older Children and AdultsSerious LeoPas encore d'évaluation
- Cardiopulmonary Disease?: Guaiac-Positive StoolsDocument3 pagesCardiopulmonary Disease?: Guaiac-Positive StoolsSerious LeoPas encore d'évaluation
- Tickler Final PDFDocument29 pagesTickler Final PDFSerious LeoPas encore d'évaluation
- IM NotesDocument13 pagesIM NotesRoendel BustilloPas encore d'évaluation
- Indications For Weaning: Kilips Classification of Ami With Expected Hospital Mortality RateDocument8 pagesIndications For Weaning: Kilips Classification of Ami With Expected Hospital Mortality RateSerious LeoPas encore d'évaluation
- West Notes-1 PDFDocument17 pagesWest Notes-1 PDFSerious LeoPas encore d'évaluation
- West Notes-1 PDFDocument17 pagesWest Notes-1 PDFSerious LeoPas encore d'évaluation
- IM NotesDocument13 pagesIM NotesRoendel BustilloPas encore d'évaluation
- CBG Coverage CBG Coverage: Actrapid Sliding ScaleDocument10 pagesCBG Coverage CBG Coverage: Actrapid Sliding ScaleSerious LeoPas encore d'évaluation
- Tickler Final PDFDocument29 pagesTickler Final PDFSerious LeoPas encore d'évaluation
- HPI HPI: Personal/Social: Educ'l Level: Occupation: Personal/Social: Educ'l Level: OccupationDocument2 pagesHPI HPI: Personal/Social: Educ'l Level: Occupation: Personal/Social: Educ'l Level: OccupationJohn Christopher LucesPas encore d'évaluation
- AlprazolamDocument2 pagesAlprazolamFATHICHAHPas encore d'évaluation
- (09-06-17) Second SGD - 2nd SessionDocument2 pages(09-06-17) Second SGD - 2nd SessionSerious LeoPas encore d'évaluation
- AD ManagementDocument2 pagesAD ManagementSerious LeoPas encore d'évaluation
- Neural Mechanisms of ItchDocument2 pagesNeural Mechanisms of ItchSerious LeoPas encore d'évaluation
- Coping With StressDocument1 pageCoping With StresslindaPas encore d'évaluation
- Dermatology Preceptorial: Med 2B Group 8Document2 pagesDermatology Preceptorial: Med 2B Group 8Serious LeoPas encore d'évaluation
- SGD 8 October 6, 2017: Inputs/Resources Activities Output EffectDocument1 pageSGD 8 October 6, 2017: Inputs/Resources Activities Output EffectSerious LeoPas encore d'évaluation
- First SGD - 3rd SessionDocument4 pagesFirst SGD - 3rd SessionSerious LeoPas encore d'évaluation
- PPH (Uterine Atony)Document4 pagesPPH (Uterine Atony)Serious LeoPas encore d'évaluation
- CPC Case PDFDocument5 pagesCPC Case PDFSerious LeoPas encore d'évaluation
- CPC Case PDFDocument5 pagesCPC Case PDFSerious LeoPas encore d'évaluation
- SGD - HPVDocument3 pagesSGD - HPVSerious LeoPas encore d'évaluation
- Adult Cardiopulmonary ResuscitationDocument3 pagesAdult Cardiopulmonary ResuscitationSerious LeoPas encore d'évaluation
- Repro SGDDocument3 pagesRepro SGDSerious LeoPas encore d'évaluation
- SGD - HPVDocument3 pagesSGD - HPVSerious LeoPas encore d'évaluation
- SGD - DigestiveDocument4 pagesSGD - DigestiveSerious LeoPas encore d'évaluation
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (399)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (73)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (120)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- July2005 Vitamin Research NewsDocument16 pagesJuly2005 Vitamin Research Newsullikeit100% (1)
- Comparision US UK Japan RegulationsDocument5 pagesComparision US UK Japan RegulationsProschool HyderabadPas encore d'évaluation
- Diabetesmeds AcceptablecombDocument2 pagesDiabetesmeds AcceptablecombCotton LogicPas encore d'évaluation
- Priyanka Sen Final Practice School Internship ReportDocument35 pagesPriyanka Sen Final Practice School Internship ReportThakur Aditya PratapPas encore d'évaluation
- Dosis Antibiotik: November 2015Document8 pagesDosis Antibiotik: November 2015subchaan waruPas encore d'évaluation
- Jimma University: Institute of Health Faculty of Health Science School of PharmacyDocument69 pagesJimma University: Institute of Health Faculty of Health Science School of PharmacyMaህPas encore d'évaluation
- 1-Diabetes Package - PO2693771771-269Document6 pages1-Diabetes Package - PO2693771771-269KishorePas encore d'évaluation
- Prescription PsychologyDocument7 pagesPrescription PsychologyJose LuisPas encore d'évaluation
- Perineal Urethrostomy PUDocument2 pagesPerineal Urethrostomy PUclara FPas encore d'évaluation
- N-Ophth Disorders in HIVDocument6 pagesN-Ophth Disorders in HIVdwongPas encore d'évaluation
- Konsensus IBDDocument15 pagesKonsensus IBDTaufikPas encore d'évaluation
- New Microsoft Word DocumentDocument3 pagesNew Microsoft Word DocumentHazim YusoffPas encore d'évaluation
- Vasopressors For ShockDocument21 pagesVasopressors For ShocknugrahaPas encore d'évaluation
- Dr. Adarsh Chandra Swami - Anaesthesia Doctor in Mohali - Fortis HealthcareDocument1 pageDr. Adarsh Chandra Swami - Anaesthesia Doctor in Mohali - Fortis Healthcarej01scottPas encore d'évaluation
- RabdoDocument7 pagesRabdoErik Ulises Teolotitla RoslaesPas encore d'évaluation
- Acute Cholecystitis: Jochen Schuld Matthias GlanemannDocument3 pagesAcute Cholecystitis: Jochen Schuld Matthias GlanemannNabilla DamarPas encore d'évaluation
- 83 Nutripuncture OverviewDocument12 pages83 Nutripuncture OverviewTimoteo Pereira TfmpPas encore d'évaluation
- Drug Study - LevetiracetamDocument3 pagesDrug Study - LevetiracetamCath Bril100% (4)
- Peat 1Document37 pagesPeat 1Denise Junio100% (4)
- Case Study.... Group-BDocument33 pagesCase Study.... Group-BNazmul HossainPas encore d'évaluation
- Lampi DragerDocument68 pagesLampi DragerAlin Mircea PatrascuPas encore d'évaluation
- Oxford GastroenterologyDocument673 pagesOxford Gastroenterologymymamym100% (1)
- LINKSERVE Training MaterialsDocument15 pagesLINKSERVE Training MaterialslisingynnamaePas encore d'évaluation
- Graves Disease in ChildrenDocument7 pagesGraves Disease in ChildrengarethPas encore d'évaluation
- Antenatal Care: Muhammad Wasil Khan and Ramsha MazharDocument55 pagesAntenatal Care: Muhammad Wasil Khan and Ramsha MazharmarviPas encore d'évaluation
- Allen Part Pedia CaseDocument3 pagesAllen Part Pedia CasePaul Michael Baguhin0% (1)
- Mrs. Manisha Chichani 29032023 064453 PMDocument1 pageMrs. Manisha Chichani 29032023 064453 PMManisha ChichaniPas encore d'évaluation
- Health Education For Patients With Urinary CathetersDocument2 pagesHealth Education For Patients With Urinary CathetersTriXie SorrillaPas encore d'évaluation
- Systemic Lupus Erythematosus Disease Activity Index 2000: Key Indexing TermsDocument4 pagesSystemic Lupus Erythematosus Disease Activity Index 2000: Key Indexing TermsRandom PersonPas encore d'évaluation
- Fixation of Mandibular Fractures With 2.0 MM MiniplatesDocument7 pagesFixation of Mandibular Fractures With 2.0 MM MiniplatesRajan KarmakarPas encore d'évaluation