Académique Documents
Professionnel Documents
Culture Documents
Dopler en Chiari
Transféré par
jdelta28Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Dopler en Chiari
Transféré par
jdelta28Droits d'auteur :
Formats disponibles
TECHNIQUE APPLICATION
TAILORED OPERATIVE TECHNIQUE FOR CHIARI TYPE I
MALFORMATION USING INTRAOPERATIVE COLOR
DOPPLER ULTRASONOGRAPHY
Thomas H. Milhorat, M.D. OBJECTIVE: We describe an operative technique for Chiari Type I malformation that
Department of Neurosurgery, The uses color Doppler ultrasonography as a guide for performing patient-specific posterior
Chiari Institute, North Shore
University Hospital, Long Island
fossa decompressions. The technique has been used since 1999 in more than 300
Jewish Health System, operations.
Manhasset, New York METHODS: On the basis of real-time anatomic and physiological measurements, the
following goals of surgery were monitored: 1) adequate decompression of the cervi-
Paolo A. Bolognese, M.D.
comedullary junction; 2) creation of a retrocerebellar space of 8 to 10 cm3 volume;
Department of Neurosurgery, The
Chiari Institute, North Shore
and 3) establishment of optimal cerebrospinal fluid flow between the cranial and
University Hospital, Long Island spinal compartments.
Jewish Health System,
Manhasset, New York
RESULTS: The size of the craniectomy was tailored to conform to the area of cerebellar
impaction as demarcated by compressed subarachnoid spaces. A laminectomy was
Reprint Requests: not performed unless the cerebellar tonsils were herniated below C1. Before opening
Thomas H. Milhorat, M.D., the dura, color Doppler ultrasonography imaging was invaluable in planning operative
Department of Neurosurgery, The
Chiari Institute, North Shore
strategies. A simple duraplasty without additional steps was found to be appropriate
University Hospital, Long Island treatment in occasional patients with minimal tonsillar herniation (5–8 mm). In all
Jewish Health System, 300 other cases, it was necessary to perform an internal decompression that included lysis
Community Drive, Manhasset, NY
11030.
of the arachnoid and shrinkage of the cerebellar tonsils to achieve the goals of surgery.
Email: Milhorat@nshs.edu Optimal cerebrospinal fluid flow through the foramen magnum in anesthetized, prone
patients was found to have the following characteristics: a peak velocity of 3 to 5 cm/s,
Received, December 18, 2002. bidirectional movement, and a waveform exhibiting vascular and respiratory varia-
Accepted, June 4, 2003.
tions. The attainment of surgical goals was confirmed in most patients by postoperative
neuroimaging.
CONCLUSION: Color Doppler ultrasonography imaging is an important technological
advance that permits the neurosurgeon to tailor the steps of Chiari surgery according
to patient-specific variables. The success of this technique depends on the mastery of
a new and sophisticated monitoring modality.
KEY WORDS: Cerebrospinal fluid flow, Chiari Type I malformation, Color Doppler imaging, Intraoperative
ultrasound imaging, Posterior fossa decompression
Neurosurgery 53:899-906, 2003 DOI: 10.1227/01.NEU.0000083591.22113.CB www.neurosurgery-online.com
T
he surgical treatment of Chiari Type I use a fixed operative technique, this approach
malformation (CMI) has not been stan- has limitations, given the great variability of
dardized. Of the available operative patient-specific findings.
techniques, the most widely performed is a Since 1999, we have used intraoperative
posterior fossa decompression consisting of color Doppler ultrasonography (CDU) as a
suboccipital craniectomy, C1 laminectomy, guide to posterior fossa decompression in pa-
and duraplasty (1, 4, 9, 15). Controversy exists tients with CMI. The technology can be
concerning the extent of the bony decompres- adapted to measure cerebrospinal fluid (CSF)
sion and the need for additional steps such as flow and provides real-time information re-
shrinkage or resection of the cerebellar tonsils. garding neural displacements, vascular anat-
Although experienced neurosurgeons tend to omy, and CSF circulation at the cervicomed-
NEUROSURGERY VOLUME 53 | NUMBER 4 | OCTOBER 2003 | 899
MILHORAT AND BOLOGNESE
ullary junction. Distinct advantages of CDU imaging include wave and color Doppler filters; time gain compensation; and
complication avoidance and the ability to tailor operative focusing of B-scan real time. Each of these commands must be
steps according to patient-specific variables. The methodology fine-tuned to achieve optimal images and Doppler informa-
of CDU and the details of the tailored operative technique are tion. Experience is required to recognize artifacts and the
presented. aliasing of color Doppler images. Acuson Corp. has reviewed
the measurements of CSF flow in this study and confirmed
METHODOLOGY OF CDU IMAGING their validity.
Historical Background CSF Volume Measurements
Modern techniques of intraoperative ultrasonography are The Acuson Sequoia 512 system has a preloaded software
based on B-scan real-time imaging. The basic methodology package for calculating the volume of an area of interest,
provides real-time bidimensional anatomic images and has which is obtained by measuring the area in three planes; two
been used in neurosurgery since the early 1980s for the intra- scan orientations perpendicular to each other are obtained.
operative localization of a wide variety of intracerebral and Cisterna magna volumes, for example, were calculated by
intramedullary lesions (3). First-generation ultrasound ma- measuring the superoinferior (length) and anteroposterior
chines were easy to use and required limited training for (depth) dimensions in the sagittal plane. The width of the
competence in data acquisition. With advances in machine space was measured in the axial plane. Volume calculations
design, including the introduction of electronic probes, it was were made by means of the following formula:
possible to complement anatomic imaging with pulse-wave
Volume ⫽ 共D1 ⫻ D2 ⫻ D3兲/6
Doppler and color Doppler coding. Specific advantages of
triplex CDU imaging include the high definition of vascular where D1, D2, and D3 are the three measurements of the
structures and the ability to measure arterial and venous cisterna magna.
blood flow patterns.
Beginning in 1983, one of us (PAB), working in conjunction Surgical Database
with Victor A. Fasano at the University of Turin, investigated
Between November 1999 and November 2002, CDU was
the uses of intraoperative ultrasonography in more than 1200
used in 315 operations for CMI. All operations were per-
neurosurgical procedures. Included in this experience was the
formed by the senior author (THM). There were 152 primary
in vivo testing of numerous probes, machines, and calibration
operations and 163 reoperations for failed Chiari surgery.
techniques. The results of these investigations led to the intro-
Before surgery, patients underwent whole-neuraxis magnetic
duction of CDU in aneurysm surgery (2). In recent years, we
resonance imaging (MRI), cine phase contrast MRI, and three-
have investigated the feasibility of using CDU for imaging
dimensional computed tomography of the head and neck.
CSF flow during Chiari surgery.
Optional studies included flexion-extension x-ray assessment
of the cervical spine, flexion-extension MRI, three-dimensional
Adaptations for Measuring CSF Flow
computed tomographic angiography, and metrizamide my-
The imaging of CSF flow by means of color Doppler tech- elography. MRI scans of the cervical spine and cine phase
nology poses technical challenges. In contrast to blood, CSF contrast MRI were obtained 3 to 12 months after surgery.
has the following characteristics: 1) a very low content of cells
and proteins, which limits the reflection of ultrasound waves;
2) a low-velocity circulation with nonhomogeneous flow
TAILORED OPERATIVE TECHNIQUE
through a network of irregular spaces rather than vessels; and (see video at web site)
3) a significant component of to-and-fro movement. To ad-
dress these technical issues, it was necessary to use high- Surgical Indications
performance equipment that was capable of maximizing
Doppler sensitivity. Most of the results in the current study Radiographic Criteria
were obtained with the Acuson Sequoia 512 system (Acuson All of the patients in this series had demonstrable impaction
Corp., Mountain View, CA) equipped with standard high- of the foramen magnum with MRI evidence of tonsillar her-
definition probes. niation, obliteration of the cisterna magna, and reduced or
Because CDU machines are designed to measure blood absent CSF flow at the cervicomedullary junction (as assessed
flow, the steps of data acquisition must be adapted according by cine phase contrast MRI). The vast majority of patients had
to the unique features of CSF flow. This can be accomplished some osseous features of CMI (12), such as hypoplasia of the
by manually adjusting the controls for B-scan real-time pro- posterior fossa, reduced length of the supraocciput, increased
cessing, pulse-wave Doppler imaging, and color Doppler im- slope of the tentorium, and reduced length of the clivus. Other
aging. Adjustments of machine default values include recali- findings that were present in some patients included anterior
bration of the following commands: B-scan gain; pulse-wave displacement of the cerebellum, kinking of the medulla, ret-
and color Doppler scales; pulse-wave Doppler gain; pulse- roflexion of the odontoid, basilar invagination, scoliosis,
900 | VOLUME 53 | NUMBER 4 | OCTOBER 2003 www.neurosurgery-online.com
OPERATIVE TECHNIQUE FOR CHIARI TYPE I MALFORMATION
Klippel-Feil anomaly, and hydrocephalus. Syringomyelia or a Each of the operative steps of posterior fossa decompression
presyrinx state was present in 182 patients. In 163 patients was guided by CDU using real-time anatomic and physiolog-
undergoing reoperation for failed Chiari surgery, there was ical measurements. The goals of surgery were as follows: 1)
radiographic evidence of one or more of the following find- adequate decompression of the cervicomedullary junction; 2)
ings: underdecompression of the posterior fossa; overdecom- creation of a retrocerebellar space of 8 to 10 cm3 volume; and
pression of the posterior fossa with cerebellar ptosis; pseudo- 3) establishment of optimal CSF flow between the cranial and
meningocele formation; surgical meningocele; cranial settling; spinal compartments.
basilar invagination; and hydrocephalus.
External Decompression
Clinical Criteria
Posterior fossa decompressions were performed under so-
The definition of what constitutes a symptomatic CMI has matosensory evoked potential monitoring with the patient in
been addressed elsewhere (12). In the current series, the indi- the prone position and the head flexed in a Mayfield head-
cations for operation and were limited to one or more of the holder. The suboccipital area was exposed through a midline
following criteria: 1) evidence of progressive neurological de- incision that extended from the inion to the second cervical
terioration; 2) presence of intractable or disabling symptoms spine. When a pericranial graft was harvested for duraplasty,
with a Karnofsky Performance Scale score of 70 or less; and 3) the incision was extended two fingerbreadths above the inion.
MRI evidence of syrinx propagation. The mean Karnofsky The size of the bony decompression was guided by CDU.
Performance Scale score in this series was 60 (unable to per- After a small suboccipital opening was made, the atlantooc-
form normal activities; requires occasional assistance). The cipital membrane was excised to facilitate imaging. Thereafter,
indications for reoperation on patients with failed Chiari sur- the craniectomy was enlarged in a stepwise manner to expose
gery were the same as those for patients undergoing primary the dura overlying the area of cerebellar impaction, as demar-
operations. cated by compressed or obliterated subarachnoid spaces. The
superior limit of the craniectomy was never above the prepy-
Surgical Decision Making ramidal fissure. Laterally, the craniectomy was widened to
The presence of clinically significant anterior compression create a nearly circular bony opening. The final dimensions of
of the cervicomedullary junction by a retroflexed or invagi- the craniectomy were generally in the range of 3.5 ⫻ 3.5 cm.
nated odontoid was regarded as a contraindication for pri- After completion of the craniectomy, a decision was made
mary decompression of the posterior fossa. Anterior compres- regarding whether or not to perform a laminectomy. The
sions were divided into two groups by cervical traction. determining factors were the extent of tonsillar herniation and
Irreducible compressions were managed by transoral odon- the required length of the dural incision. CDU was used to
toidectomy, then a craniovertebral fusion at the time of pos- establish the true position of the tonsillar tips, which was
terior decompression. Reducible compressions were managed typically 3 to 6 mm lower than predicted by MRI. A laminec-
by a one-stage posterior decompression and fusion. tomy was not performed for herniations above C1. In patients
with intermediate hernia-
tions (12–15 mm), the supe-
rior aspect of the C1 arch was
sometimes underbitten (Fig.
1). Herniations of more than
15 mm generally required a
standard C1 laminectomy.
Similar guidelines were ap-
plied to herniations at lower
levels. The relationship of the
cerebellar tonsils to bony
landmarks was altered by
anomalies such as assimila-
tion of the atlas.
CDU Imaging before
Opening of the Dura
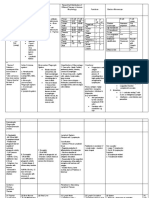
FIGURE 1. CDU images of cervicomedullary junction in a 42-year-old woman with CMI and syringomyelia. A,
sagittal image showing a 13-mm tonsillar herniation that extends to within 0.38 cm (distance between asterisks) of C1. Before opening of the dura,
Trapezoid outlines color Doppler sample volume. B, sagittal image after underbiting superior arch of C1, which CDU was used for anatomic
increases space between C1 and tonsillar tips to 0.97 cm (distance between asterisks). D, dura; P, posteroinferior orientation and to establish
cerebellar artery; T, cerebellar tonsil; SC, spinal cord; tbv, tonsillar blood vessel. Dashed line demarcates shadow baseline measurements of CSF
artifact of bone. flow (Fig. 2). Structures that
NEUROSURGERY VOLUME 53 | NUMBER 4 | OCTOBER 2003 | 901
MILHORAT AND BOLOGNESE
were routinely imaged included the cerebellar tonsils, the uvula, Cisterna magna volumes of less than 0.5 cm3 and CSF flow
the medulla, the upper cervical spinal cord, both vertebral arter- velocities in the range of 0 to 0.8 cm/s anterior and posterior to
ies, both posteroinferior cerebellar arteries, the marginal sinuses, the cervicomedullary junction were typical baseline findings.
the parenchymal arteries and veins, and bridging vessels sus-
pended by the arachnoid. The identification of aberrant vascular Dural Opening
anatomy, asymmetrical herniations, and neural displacements The dura was opened with a Y-shaped incision across the mar-
helped reduce the risk of surgical error (Fig. 3A). In patients ginal sinuses unless CDU imaging suggested a better line of entry.
undergoing reoperation for failed Chiari surgery, information The arachnoid was left intact, and imaging was repeated in appro-
concerning the location and extent of meningocerebral scarring priate cases to analyze whether duraplasty alone might be sufficient
was invaluable in planning dissection strategies (Fig. 3B). treatment. Opening the dura invariably resulted in some reexpan-
CSF circulation at the cervicomedullary junction was assessed sion of the cisterna magna, but a significant improvement in CSF
immediately before opening the dura. The following measure- flow was rarely observed. A simple duraplasty without additional
ments were made and stored: 1) the size and volume of the steps was performed in occasional patients who met the following
cisterna magna; 2) the size and volume of the dorsal cervical criteria: cisterna magna volume of at least 4 cm3; CSF velocity/flow
theca between C1 and the tonsillar tips; 3) CSF velocity/flow in of at least 2 cm/s; and CSF tracings demonstrating bidirectional
the cisterna magna; 4) CSF velocity/flow in the dorsal cervical movement with vascular and respiratory variations.
theca; and 5) CSF velocity/flow in the premedullary cisterns.
Internal Decompression
The arachnoid was opened,
and CSF was allowed to drain
spontaneously. We used mag-
nification vision to visualize
the area. The arachnoid was
resected widely, and adhe-
sions to the cerebellar tonsils,
posteroinferior cerebellar ar-
teries, and spinal cord were
coagulated and divided. The
tonsils were mobilized, and
the posteroinferior cerebellar
arteries were protected with
moist cotton patties. On the
FIGURE 2. CDU images of cervicomedullary junction after external decompression and before opening the dura.
basis of direct inspection, a de-
A, sagittal image in a 9-year-old boy with CMI showing an 11-mm tonsillar herniation, intact C1, and regional
vascular anatomy. B, pulse-wave Doppler tracing (bottom) with sagittal target image (top) in a 38-year-old man
cision was made whether or
with CMI and syringomyelia showing no cisterna magna and minimal CSF flow caudal to cerebellar tonsils (cur- not to shrink the cerebellar
sor). D, dura; P, posteroinferior cerebellar artery; VA, vertebral artery; T, cerebellar tonsil; SC, spinal cord; av, tonsils. The tonsils were not
arachnoid vessel; aa, arachnoid adhesion. Dashed line demarcates shadow artifact of bone. shrunken if the obex area was
open and a pulsatile flow of
CSF could be observed to exit
from the fourth ventricle into
the dorsal cervical theca. In
most cases, the tonsils were re-
duced with low-voltage, bipo-
lar coagulation until the tonsil-
lar tips were positioned at or
slightly above the putative
level of the foramen magnum.
Expansile Duraplasty
The dura was closed with a
FIGURE 3. A, axial B-scan real-time image of cervicomedullary junction in a 47-year-old woman with CMI and
graft of autogenous pericra-
syringomyelia showing an 18-mm asymmetrical tonsillar herniation with spinal cord displacement. B, sagittal CDU nium or reconstituted cadav-
image of cervicomedullary junction in a 3-year-old girl undergoing reoperation for failed Chiari surgery showing eric dura. Cadaveric grafts,
meningocerebral cicatrix with dura adherent to posteroinferior cerebellar artery and tonsillar branches. D, dura; P, which most closely resemble
posterior inferior cerebellar artery; T, cerebellar tonsil; tbv, tonsillar blood vessel; SC, spinal cord. living dura, were discontin-
902 | VOLUME 53 | NUMBER 4 | OCTOBER 2003 www.neurosurgery-online.com
OPERATIVE TECHNIQUE FOR CHIARI TYPE I MALFORMATION
ued for general use in 2001 because of limited supply and con- following characteristics: a peak velocity of 3 to 5 cm/s; bidi-
cerns related to transmissible prions. A graft of approximately 5 rectional movement; and a waveform exhibiting arterial, ve-
cm in length and 2.5 cm in width was usually sufficient to nous, and respiratory variations (Fig. 4). Figures 5 and 6 show
produce a competent retrocerebellar space. The graft was an- typical findings before and after lysis of the arachnoid, shrink-
chored to the poles of the incision and sewn in place with age of the tonsils, and duraplasty. Postoperative neuroimag-
continuous locking sutures of 5-0 Gore-Tex (W.L. Gore & Asso- ing demonstrated a normal-sized cisterna magna and unre-
ciates, Inc., Flagstaff, AZ). Before the last suture was tied down, stricted CSF flow anteriorly and posteriorly through the
the retrocerebellar space was inflated with 30 to 40 ml of sterile foramen magnum in most patients. Overly generous duraplas-
saline to expand the graft and to eliminate intradural air bubbles, ties and iatrogenic meningoceles were associated with subop-
which can degrade CDU images. Valsalva maneuvers were per- timal CSF flow velocities (⬍1 cm/s) (Fig. 7A). The problem
formed to ensure a watertight closure. CSF leaks were corrected could usually be corrected by tightening the graft with rein-
by oversewing the suture line. forcing sutures or adding a restrictive graft (Fig. 7B). Excessive
CSF flow velocities (⬎8 cm/s) were most often encountered
during reoperations in which the dura was densely scarred
CDU Imaging after Closing the Dura and thickened. Such observations are consistent with princi-
After dural closure, CDU imaging was repeated to assess ples of fluid mechanics governing rates of flow through spaces
the goals of surgery. Optimal CSF flow was found to have the of varying compliance and cross sectional area.
Wound Closure
The suboccipital craniectomy
was covered with a titanium
mesh/acrylic cranioplasty to
protect the duraplasty and limit
FIGURE 4. Optimal CSF flow characteristics. Pulse-wave Doppler tracings in a 38-year-old woman with a 19-mm the extent of extradural scar-
tonsillar herniation after lysis of arachnoid, shrinkage of tonsils, and duraplasty show a peak CSF velocity of 4 ring. The paraspinal muscles
cm/s, bidirectional movement, arterial pulsations (A), and respiratory and venous variations (B). were sewn to the inferior border
of the plate. In patients at risk
for a CSF leak, a lumbar drain
was inserted after surgery.
DISCUSSION
The surgical treatment of
CMI requires familiarity with
a great number of technical
options, some of which are
controversial. Among the un-
settled questions are the fol-
lowing: the size of the crani-
FIGURE 5. CSF flow in a 39-year-old woman with a ectomy (8, 10, 16); the extent
10-mm tonsillar herniation before and after lysis of arach- of the laminectomy (10, 15);
noid, shrinkage of tonsils, and duraplasty. A, pulse-wave the need to preserve (13) or
Doppler tracing (bottom) with sagittal target image open (1) the arachnoid; the
(top) before opening the dura, showing no significant need for additional steps
CSF flow caudal to cerebellar tonsils (cursor). B, pulse- such as lysis of the arachnoid
wave Doppler tracing (bottom) with sagittal target im- (9, 15), shrinkage or resection
age (top) after internal decompression showing CSF ve- of the cerebellar tonsils (1, 7),
locity of 3 cm/s. Red signal on target image (cursor)
stenting of the fourth ventri-
represents CSF flow; multicolor blots represent aliasing
from vascular structures. C, sagittal CDU image after
cle (5), and plugging the obex
internal decompression showing CSF flow (red signal) (14); the need to close dura
through the cisterna magna and dorsal cervical theca. (15) or leave it open (19); the
Multicolor blots represent aliasing from vascular struc- size of the duraplasty (10, 16);
tures. D, dura; DP, duraplasty; P, posteroinferior cere- the optimal material for dura-
bellar artery; T, cerebellar tonsil; SC, spinal cord; CSF, plasty (1, 9, 10); and the need
cerebrospinal fluid. for a cranioplasty (17). There
NEUROSURGERY VOLUME 53 | NUMBER 4 | OCTOBER 2003 | 903
MILHORAT AND BOLOGNESE
The introduction of CDU as an intraoperative guide for
posterior fossa surgery is an important technological advance
that permits the neurosurgeon to tailor operative steps accord-
ing to patient-specific variables on the basis of real-time ana-
tomic and physiological measurements. Of its potential uses,
CDU is particularly well suited for Chiari surgery in which
technical decisions are based largely on preoperative neuro-
radiological findings. A potential disadvantage of CDU is its
sophisticated methodology. Special training is required for
competence in the acquisition and interpretation of data.
The development of strategies for tailoring the steps of
Chiari surgery by the use of CDU involved a number of
assumptions. The first of these was that the area of cerebellar
impaction conforms to the area of compressed or obliterated
subarachnoid spaces. Supporting this assumption is neurora-
diological evidence that effacement of the subarachnoid space
is one of the earliest signs of cerebral displacement and that
FIGURE 6. CSF flow in a 40-year-old man undergoing reoperation for extra-axial masses tend to produce a congruent area of cortical
failed Chiari surgery after lysis of arachnoid, shrinkage of tonsils, and sulcus compression (6). Another assumption was that the ideal
duraplasty. Sagittal CDU image shows jet stream flow of CSF (blue sig- volume of the reconstructed retrocerebellar space should be in
nal) out of the fourth ventricle (arrow) with a peak velocity of 4 cm/s as the range of 8 to 10 cm3. This was based on two pieces of
compared with no flow before internal decompression. Variations in color evidence: anatomic estimates of cisterna magna size (18), and
coding are a function of direction of flow. D, dura; T, cerebellar tonsil; SC, volumetric measurements of the posterior cranial fossa indi-
spinal cord. cating that total CSF volume (26.7 ⫾ 7.3 cm3) is reduced by a
mean of 10.8 ⫾ 7.1 cm3 in patients with CMI (12). No assump-
tions could be made concerning normal rates of CSF flow at
is no consensus on these matters and little in the way of the cervicomedullary junction. The measurements reported
scientifically controlled comparative data. here were obtained in anesthetized patients in the prone po-
Complicating the treatment of CMI is the wide range of sition before and after posterior fossa decompression. Under
patient-specific variables. These include the level of tonsillar the conditions of operation, an optimal rate of CSF flow was
descent, the degree of craniovertebral dysmorphism, the tight- assumed to have been achieved in patients with adequate
ness of the posterior fossa, the completeness of the CSF block, decompressions, visible evidence of an unrestricted and pul-
and the presence or absence of syringomyelia. It is doubtful satile flow of CSF from the fourth ventricle into the dorsal
that any operative technique with fixed steps and inalterable cervical theca, and a competent duraplasty. Mean peak veloc-
dimensions of decompression can deal effectively with all of ities after decompression ranged from 3 to 5 cm/s as com-
these variables. pared with 0 to 0.8 cm/s before decompression. Because nor-
mal CSF exhibits to-and-fro
movements with distinct vas-
cular and respiratory varia-
tions (11), the presence of
these findings on postdecom-
pression waveform tracings
suggests that the flow veloc-
ities achieved were in a phys-
iological range. Postopera-
tive cine phase contrast MRI
confirmed the presence of
unrestricted CSF flow anteri-
orly and posteriorly through
the foramen magnum in
most patients.
FIGURE 7. CDU images of cervicomedullary junction in a 49-year-old woman undergoing reoperation for failed
Chiari surgery and meningocele formation. A, pulse-wave Doppler tracing (bottom) with sagittal target image
The ability to adjust surgi-
(top) showing no CSF flow in the cisterna magna (cursor) before repair of the meningocele. Multicolor blots rep- cal strategies on the basis of
resent aliasing from vascular structures. B, pulse-wave Doppler tracing (bottom) with sagittal target image (top) real-time anatomic and phys-
showing CSF velocity of 3 cm/s in the cisterna magna (cursor) after repair of the meningocele with restrictive iological measurements is a
duraplasty. M, meningocele; T, cerebellar tonsil; DP, old duraplasty; RD, restrictive duraplasty. defining step in the evolution
904 | VOLUME 53 | NUMBER 4 | OCTOBER 2003 www.neurosurgery-online.com
OPERATIVE TECHNIQUE FOR CHIARI TYPE I MALFORMATION
of Chiari surgery. It remains to be analyzed which strategies Acknowledgment
are optimal. Ultimately, the value of the current technique will The authors received no financial support in conjunction with the conduct of
depend on the results of an ongoing longitudinal study that the study described in this article.
correlates CDU-guided operative steps with pre- and postop-
erative MRI scans, pre- and postoperative cine phase contrast
MRI scans, symptoms and signs, and long-term patient
outcome. COMMENTS
REFERENCES
T he authors present their extensive experience with the use
of intraoperative color Doppler ultrasonography (CDU) as
a guide in tailoring suboccipital decompressive surgery in
patients with Chiari Type I malformation (CMI). In their ex-
1. Batzdorf U: Treatment of syringomyelia associated with Chiari I malforma- perience, overdecompression as well as underdecompression
tion, in Tamaki N, Batzdorf U, Nagashima T (eds): Syringomyelia: Current
Concepts in Pathogenesis and Management. Tokyo, Springer-Verlag, 2001, pp
may result in less than optimal neurological outcomes. Mea-
121–135. surement of cerebrospinal fluid (CSF) pulsation velocities and
2. Bolognese PA, Fasano VA: Intraoperative ultrasonography in neurosurgery, calculation of the volume of the cisterna magna before and
in Paletto AE (ed): Trattato di Technica Chirugia. Turin, UTET, 1990, vol XIII, after reconstruction may aid in tailoring the operation for each
tome 1, pp 157–186.
patient. Use of the technique clearly requires dedication and
3. Dohrmann GJ, Rubin JM: Use of ultrasound in neurosurgical operations: A
preliminary report. Surg Neurol 16:362–366, 1981. experience. As the authors point out, its validation depends on
4. Ellenbogen RG, Zeidman SM: Craniovertebral decompression for Chiari longitudinal studies correlating CDU findings with measure-
malformation, in Kaye A, Black PMcL (eds): Operative Neurosurgery. ments on the basis of cine magnetic resonance imaging and
Edinburgh, Churchill Livingstone, 2000, pp 1725–1741. functional outcome.
5. Griebel ML, Oakes J, Worley G: The Chiari malformation associated with
myelomeningoceles, in Rekate HL (ed): Comprehensive Management of Spina Robert G. Grossman
Bifida. Boca Raton, CRC Press, 1991, pp 83–89.
Houston, Texas
6. Grossman RI, Yosem DM: Neuroradiology: The Requisites. St. Louis, C.V.
Mosby, 1994, pp 149–169.
7. Guyotat J, Bret P, Jouanneau E, Ricca A, Lapras C: Syringomyelia associated
with type I Chiari malformation: A 21-year retrospective study on 75 cases
I n general, excellent outcomes are expected in the treatment
of patients with hindbrain herniation or CMI. It is definitely
true, however, that this group of patients encompasses a large
treated by foramen magnum decompression with a special emphasis on the
value of tonsils resection. Acta Neurochir (Wien) 140:745–754, 1998. number of different conditions and degrees of severity. It
8. Holly LT, Batzdorf U: Management of cerebellar ptosis following craniover- makes a great deal of sense to tailor the operation to the
tebral decompression for Chiari I malformation. J Neurosurg 94:21–26, 2001.
specific needs of the individual patient, and the use of CDU is
9. Klekamp J, Batzdorf U, Samii M, Bothe HW: The surgical treatment of Chiari
I malformation. Acta Neurochir (Wien) 138:788–801, 1996. a logical way of distinguishing which patients need what type
10. Lazareth JA, Galarza M, Gravori T, Spinks TJ: Tonsillectomy without crani- of operation. The goal of creating a 10-cm3 volume for the
ectomy for the management of infantile Chiari I malformation. J Neurosurg newly created cisterna magna likewise is logical and ensures
97:1018–1022, 2002. adequate transmission of CSF pulses from the cranial to the
11. Milhorat TH: Hydrocephalus and the Cerebrospinal Fluid. Baltimore, Williams
& Wilkins, 1972, pp 7–11.
cerebrospinal compartments and the mixing of CSF from ce-
12. Milhorat TH, Chou MW, Trinidad EM, Kula RW, Mandell M, Wolpert C, rebrospinal to cortical subarachnoid spaces.
Speer MC: Chiari I malformation redefined: Clinical and radiographic find- Logically, the authors decided the proper parameters of
ings for 364 symptomatic patients. Neurosurgery 44:1005–1017, 1999. treatment, and they performed CDU to verify that they
13. Oldfield EH: Editorial: Cerebellar tonsils and syringomyelia. J Neurosurg
achieved those objectives. This study does not analyze
97:1009–1010, 2002.
14. Peerless SJ, Durward QJ: Management of syringomyelia: A pathophysiolog- whether these parameters are superior to other proposed
ical approach. Clin Neurosurg 30:531–576, 1983. treatments for the condition, such as more extensive bone
15. Rekate HL: Management of Chiari malformations, in Dickman CA, Spetzler removal or scoring rather than patching of the dura (1, 2, 4).
RF, Sonntag VKH (eds): Surgery of the Craniovertebral Junction. New York, “Shrinking” of the cerebellar tonsils is commonly performed
Thieme, 1998, pp 507–521.
16. Sahuquillo J, Rubio E, Poca MA, Rovira A, Rodriguez-Baeza A, Cervera C:
to ensure that there is sufficient room for the creation of a new,
Posterior fossa reconstruction: A surgical technique for the treatment of more copious cisterna magna. My preference is to avoid this
Chiari I malformation and Chiari I/syringomyelia complex—Preliminary maneuver, because the cerebellum tends to adhere to the dural
results and magnetic resonance imaging quantitative assessment of hind- patch if the pial surface is violated. If more room is needed
brain migration. Neurosurgery 35:874–884, 1994.
than can be provided by the patch itself, I recommend reat-
17. Sakamoto H, Nishikawa M, Hakuba A, Yasui T, Kitano S, Nakanishi N,
Inoue Y: Expansive suboccipital cranioplasty for the treatment of syringo- taching the piece of cranium that has been removed from the
myelia associated with Chiari malformation. Acta Neurochir (Wien) 123: posterior fossa after it has been rotated to create an enlarged
949–961, 1999. posterior fossa. I then use a central dural tacking stitch to hold
18. Schaefer GB, Thompson JN, Bodensteiner JB, Gingold M, Wilson M, Wilson the patch against the bone to ensure that there is a new
D: Age-related changes in the relative growth of the posterior fossa. J Child
Neurol 6:15–19, 1991.
cisterna magna. Sakamoto et al. (3) used this technique suc-
19. Williams B: Surgery for hindbrain related syringomyelia. Adv Tech Stand cessfully. I think that performing CDU to document the cre-
Neurosurg 20:107–164, 1993. ation of an adequate cisterna magna, thereby allowing the
NEUROSURGERY VOLUME 53 | NUMBER 4 | OCTOBER 2003 | 905
MILHORAT AND BOLOGNESE
procedure to be tailored to the individual patient, holds leagues and I have performed routinely for a number of years.
promise. This can be accomplished by using bipolar current as de-
scribed (1), but occasionally when the tonsils are gliotic or
Harold L. Rekate
large, subpial resection should also be considered.
Phoenix, Arizona
Ulrich Batzdorf
Los Angeles, California
1. Gambardella G, Caruso G, Caffo M, Germano A, La Rosa G, Tomasello F:
Transverse microincisions of the outer layer of the dura mater combined with
foramen magnum decompression as treatment for syringomyelia with Chiari
I malformation. Acta Neurochir (Wien) 140:134–139, 1998. 1. Halamandaris G, Batzdorf U: Adult Chiari malformation. Contemp
2. James HE, Brant A: Treatment of the Chiari malformation with bone decom- Neurosurg 11(26), 1989.
pression without durotomy in children and young adults. Childs Nerv Syst 2. Sahuquillo J, Rubio E, Poca MA, Rovira A, Rodriguez-Baeza A, Cervera C:
18:202–206, 2002. Posterior fossa reconstruction: A surgical technique for the treatment of
3. Sakamoto H, Nishikawa M, Hakuba A, Yasui T, Kitano S, Nakanishi N, Inoue Chiari I malformation and Chiari I/syringomyelia complex—Preliminary
Y: Expansive suboccipital cranioplasty for the treatment of syringomyelia results and magnetic resonance imaging quantitative assessment of hindbrain
associated with Chiari malformation. Acta Neurochir (Wien) 141:949–961, migration. Neurosurgery 35:874–885, 1994.
1999.
4. Sindou M, Chavez-Machuca J, Hashish H: Cranio-cervical decompression for
Chiari type I-malformation, adding extreme lateral foramen magnum open-
ing and expansile duroplasty with arachnoid preservation: Technique and
long-term functional results in 44 consecutive adult cases—Comparison with
M ilhorat and Bolognese report an excellent technique ap-
plication. Dr. Milhorat is a member of the scientific
community who possibly performs more CMI operations than
literature data. Acta Neurochir (Wien) 144:1005–1019, 2002.
any other surgeon in the United States. He shows that he
meticulously studies each patient and each approach so that
M ilhorat and Bolognese describe their observations in per-
forming intraoperative CDU. The use of this elegant
investigational technique has permitted them to gauge the
he may improve on what has been done previously. The
authors achieve the simple goal of convincing the reader that
amount of bone that they wish to remove in a given situation CDU is a safe, effective, and efficient adjuvant in surgery
and has provided them with a demonstration of anatomy. In performed for hindbrain malformations. Clearly, this modal-
addition, these studies have generated some interesting quan- ity requires the right equipment and skill to be used and
titative data regarding CSF flow and the size of the cisterna interpreted correctly. However, it is presented as yet another
magna before and after decompressive surgery. noninvasive technique (in addition to the cine phase contrast
From the practical point of view, approximate measure- magnetic resonance imaging) that does not contaminate the
ments for optimal bone removal in an individual patient can entity it is attempting to evaluate, specifically the CSF and its
be made on the basis of preoperative magnetic resonance flow patterns. This is an enormous advantage for those sur-
imaging scans. It is clear on the basis of this study that the geons who base their treatment on the correction of the ana-
large bony decompressions that were once widely used are tomic and thus the physiological conditions that exist in the
not necessary. The problem is really with the tonsils them- posterior fossa. The authors are enthusiastic about the possi-
selves, even though I think that the underlying anatomic bility that this technique may alter individual surgical ap-
abnormality is smaller than the usual posterior fossa volume. proaches to CMI on the basis of specific, real-time anatomic
It is not necessary, however, to enlarge the entire posterior and physiological factors. This may well be true. First, how-
fossa to achieve tonsillar decompression. ever, the authors must show how this technique and the
Because the authors noted a small cisterna magna before subsequent tailored surgical approach correlate with patient
performing tonsil reduction and duraplasty, and because the outcome in terms of symptoms and radiological criteria such
establishment of a larger cisterna magna seems to correlate as magnetic resonance imaging. In the next several years, I
with good outcome (2), it is difficult to understand their
have little doubt that Milhorat and Bolognese will do precisely
reluctance to perform a complete C1 laminectomy in every
that.
patient. If nothing else, performing this procedure permits one
to create a larger cisterna magna. I concur with the desirability Richard G. Ellenbogen
of reducing the mass of the cerebellar tonsils, which my col- Seattle, Washington
Vous aimerez peut-être aussi
- Anderson 2016Document2 pagesAnderson 2016Pallavi SutarPas encore d'évaluation
- Video-Atlas of Open Thoracoabdominal Aortic Aneurysm RepairDocument6 pagesVideo-Atlas of Open Thoracoabdominal Aortic Aneurysm Repairvan le hoangPas encore d'évaluation
- Video-Atlas of Open Thoracoabdominal Aortic Aneurysm RepairDocument6 pagesVideo-Atlas of Open Thoracoabdominal Aortic Aneurysm Repairvan le hoangPas encore d'évaluation
- Exemplu 5Document5 pagesExemplu 5Pavel SebastianPas encore d'évaluation
- Endoscopic Skull Base SurgeryDocument25 pagesEndoscopic Skull Base Surgerypramod454992Pas encore d'évaluation
- (10920684 - Neurosurgical Focus) Meningiomas - The Role of Preoperative Angiography and EmbolizationDocument4 pages(10920684 - Neurosurgical Focus) Meningiomas - The Role of Preoperative Angiography and EmbolizationBesseMarwah AgusHusainPas encore d'évaluation
- IphoneDocument8 pagesIphonegerrymikepalisocPas encore d'évaluation
- Step Ladder Expansive Cranioplasty CT StudyDocument7 pagesStep Ladder Expansive Cranioplasty CT StudyDebashree SenguptaPas encore d'évaluation
- 2012-Elhamady-Retrosigmoid ApproachDocument23 pages2012-Elhamady-Retrosigmoid ApproachHaris GiannadakisPas encore d'évaluation
- Arteriovenous Shunt Measurement During Endovascular Therapy For Cerebrospinal LesionsDocument11 pagesArteriovenous Shunt Measurement During Endovascular Therapy For Cerebrospinal LesionsFachrul TamrinPas encore d'évaluation
- (10920684 - Neurosurgical Focus) Surgical Management of Trigeminal Schwannomas - Defining The Role For Endoscopic Endonasal ApproachesDocument9 pages(10920684 - Neurosurgical Focus) Surgical Management of Trigeminal Schwannomas - Defining The Role For Endoscopic Endonasal ApproachesasiyazaidiaPas encore d'évaluation
- (Journal of Neurosurgery) Neuroendoscopic Approach To Intraventricular LesionsDocument10 pages(Journal of Neurosurgery) Neuroendoscopic Approach To Intraventricular LesionsAniaPas encore d'évaluation
- Embolizacion 3dDocument5 pagesEmbolizacion 3dMai GonzalezPas encore d'évaluation
- 586 2012 Article 2505Document6 pages586 2012 Article 2505sulthoni ikaPas encore d'évaluation
- Abstract No. 301 - Angiographic Catheters - A Comprehensive Review For The Interventionalist In-TrainingDocument2 pagesAbstract No. 301 - Angiographic Catheters - A Comprehensive Review For The Interventionalist In-TrainingPeter LiPas encore d'évaluation
- Transtubular Image-Guided Surgery For Spinal Intradural Lesions: Techniques, Results, and Complications in A Consecutive Series of 60 PatientsDocument9 pagesTranstubular Image-Guided Surgery For Spinal Intradural Lesions: Techniques, Results, and Complications in A Consecutive Series of 60 PatientswilsonwqaPas encore d'évaluation
- 2013 9 1 045 ChuangDocument8 pages2013 9 1 045 ChuangRamaMahardikaPas encore d'évaluation
- Pericardial DiseaseDocument20 pagesPericardial DiseaseGeorgePas encore d'évaluation
- Klatt 2013Document4 pagesKlatt 2013Sung Soon ChangPas encore d'évaluation
- CT Angiography Versus Digital Subtraction Angiography For Intracranial Vascular Pathology in A Clinical SettingDocument9 pagesCT Angiography Versus Digital Subtraction Angiography For Intracranial Vascular Pathology in A Clinical SettingPari Pengda BaliPas encore d'évaluation
- Legnani 2013Document6 pagesLegnani 2013wedawisnawaPas encore d'évaluation
- 1 s2.0 S1878875023005466 MainDocument6 pages1 s2.0 S1878875023005466 MainJay ParkPas encore d'évaluation
- Reconstruction of Skull Base Defects After Minimally Invasive Endoscopic Resection of Anterior Skull Base NeoplasmsDocument7 pagesReconstruction of Skull Base Defects After Minimally Invasive Endoscopic Resection of Anterior Skull Base NeoplasmsFemale calmPas encore d'évaluation
- Thoracic Endoscopic Spine Surgery A ComprehensiveDocument11 pagesThoracic Endoscopic Spine Surgery A Comprehensivesanjay chhawraPas encore d'évaluation
- The Minipterional Craniotomy For Anterior.5Document8 pagesThe Minipterional Craniotomy For Anterior.5J Alan SantosPas encore d'évaluation
- Gibson Et Al-2012-Transforaminal Endoscopic Spinal SurgeryDocument7 pagesGibson Et Al-2012-Transforaminal Endoscopic Spinal SurgeryjuanguapoPas encore d'évaluation
- Contrast-Enhanced Interstitial Transpedal MR Lymphangiography For Thoracic Chylous Effusions.Document9 pagesContrast-Enhanced Interstitial Transpedal MR Lymphangiography For Thoracic Chylous Effusions.Carlos CostaPas encore d'évaluation
- 10 1 1 525 6842Document6 pages10 1 1 525 6842sandyPas encore d'évaluation
- The Role of Endoscopic Biopsy and Third Ventriculostomy in TheDocument8 pagesThe Role of Endoscopic Biopsy and Third Ventriculostomy in TheCarlos Daniel Giménez MéndezPas encore d'évaluation
- Radiologic Assessment of The Paranasal SinusesDocument8 pagesRadiologic Assessment of The Paranasal SinusesNicolás HenaoPas encore d'évaluation
- Contribution of Cardiac Imaging (CT and Mri) in Thediagnosis of Chronic Constrictive Pericarditis: A Series of 76 CasesDocument12 pagesContribution of Cardiac Imaging (CT and Mri) in Thediagnosis of Chronic Constrictive Pericarditis: A Series of 76 CasesIJAR JOURNALPas encore d'évaluation
- Annals of Medicine and Surgery: SciencedirectDocument7 pagesAnnals of Medicine and Surgery: SciencedirectBagoes AsPas encore d'évaluation
- Comparative Study of MR Sialography and Digital Subtraction Sialography For Benign Salivary Gland DisordersDocument8 pagesComparative Study of MR Sialography and Digital Subtraction Sialography For Benign Salivary Gland DisordersTanu_Harry_8699Pas encore d'évaluation
- 1 s2.0 S2666250720300985 MainDocument2 pages1 s2.0 S2666250720300985 MainFernando OrozcoPas encore d'évaluation
- Epidermoid Cysts TNEDocument10 pagesEpidermoid Cysts TNEbello_england_209552Pas encore d'évaluation
- Zaidi 2014Document7 pagesZaidi 2014Yusuf BrilliantPas encore d'évaluation
- 05.01 - Intraoperative MRI DevelopmentsDocument223 pages05.01 - Intraoperative MRI DevelopmentsBivolaru AlinPas encore d'évaluation
- Patients Selection For Awake Neurosurgery: Original ArticleDocument9 pagesPatients Selection For Awake Neurosurgery: Original Articleserena7205Pas encore d'évaluation
- Management of Parapharyngeal-Space TumorsDocument6 pagesManagement of Parapharyngeal-Space Tumorsstoia_sebiPas encore d'évaluation
- Remote Access Endoscopic Parathyroidectomy: A Study of 17 Cases From Central IndiaDocument6 pagesRemote Access Endoscopic Parathyroidectomy: A Study of 17 Cases From Central IndiaKriti KumariPas encore d'évaluation
- DownloadDocument12 pagesDownloadhasan nazzalPas encore d'évaluation
- Leong 2005Document6 pagesLeong 2005kwpang1Pas encore d'évaluation
- Automatic Tool Segmentation and Tracking During Robotic Intravascular Catheterization For Cardiac InterventionsDocument23 pagesAutomatic Tool Segmentation and Tracking During Robotic Intravascular Catheterization For Cardiac InterventionsNishant UzirPas encore d'évaluation
- Transcutaneous Transfacial Approaches To The Anterior Skull BaseDocument4 pagesTranscutaneous Transfacial Approaches To The Anterior Skull Basequesti0neverythin9Pas encore d'évaluation
- Andronik Ou 2013Document16 pagesAndronik Ou 2013MayPas encore d'évaluation
- Sci J Al Azhar Med Fac Girls 2020 4 1 34 41 EngDocument8 pagesSci J Al Azhar Med Fac Girls 2020 4 1 34 41 EngDr vishnu rathwaPas encore d'évaluation
- Preface: Recent Innovations in Vascular Imaging XV: Christopher J. FrançoisDocument4 pagesPreface: Recent Innovations in Vascular Imaging XV: Christopher J. FrançoisHector Hernandez-SoriaPas encore d'évaluation
- Three-Hand Endoscopic Endonasal Transsphenoidal Surgery: Experience With An Anatomy-Preserving Mononostril Approach TechniqueDocument8 pagesThree-Hand Endoscopic Endonasal Transsphenoidal Surgery: Experience With An Anatomy-Preserving Mononostril Approach TechniqueIvonne PerezPas encore d'évaluation
- Tongue Tumor Detection in Hyperspectral Images Using Deep Learning Semantic SegmentationDocument11 pagesTongue Tumor Detection in Hyperspectral Images Using Deep Learning Semantic Segmentationanchal18052001Pas encore d'évaluation
- Spine Minimally Invasive Spine Surgery Historical PerspectivesDocument10 pagesSpine Minimally Invasive Spine Surgery Historical PerspectivesNoura RosePas encore d'évaluation
- Thoracoscopic Sympathetic Block To Predict CompensatoryDocument9 pagesThoracoscopic Sympathetic Block To Predict Compensatory이민우Pas encore d'évaluation
- Perioperative Point-of-Care Ultrasonography: The Past and The Future Are in Anesthesiologists' HandsDocument3 pagesPerioperative Point-of-Care Ultrasonography: The Past and The Future Are in Anesthesiologists' HandsSyahrul Mubarak Danar SumantriPas encore d'évaluation
- Department of Neurosugery SDM College of Medical Sciences and Hospital, DharwadDocument7 pagesDepartment of Neurosugery SDM College of Medical Sciences and Hospital, DharwadKanak SoniPas encore d'évaluation
- Chicken Wing For Endosocpic MicrosuregryDocument6 pagesChicken Wing For Endosocpic MicrosuregryDavid LiPas encore d'évaluation
- Endoscopic Tumour Surgery - Current Limits and Future PossibilitiesDocument4 pagesEndoscopic Tumour Surgery - Current Limits and Future PossibilitiesIliasa IliasPas encore d'évaluation
- World Journal of Radiology PDFDocument8 pagesWorld Journal of Radiology PDFniluhPas encore d'évaluation
- Dose Evaluation For Skin and Organ in HepatocellulDocument11 pagesDose Evaluation For Skin and Organ in HepatocellulAnne MbrkPas encore d'évaluation
- 120th Issue-Article 101 PDFDocument10 pages120th Issue-Article 101 PDFRajendra ChavanPas encore d'évaluation
- Pola Cco 2013Document3 pagesPola Cco 2013akivaPas encore d'évaluation
- Endoscopic Procedures on the SpineD'EverandEndoscopic Procedures on the SpineJin-Sung KimPas encore d'évaluation
- Gastrointestinal Diseases During Pregnancy What DoDocument11 pagesGastrointestinal Diseases During Pregnancy What Dotakechi takechiPas encore d'évaluation
- Ontogeny and Phylogeny of Immune SystemDocument3 pagesOntogeny and Phylogeny of Immune SystemPM Basiloy - AloPas encore d'évaluation
- Package Insert - Varivax (Refrigerator)Document14 pagesPackage Insert - Varivax (Refrigerator)Jose Eduardo Oliva MarinPas encore d'évaluation
- Prittie-2006-Journal of Veterinary Emergency and Critical CareDocument11 pagesPrittie-2006-Journal of Veterinary Emergency and Critical Carejose fdoPas encore d'évaluation
- Mnemonics and Acronyms For Nursing SchoolDocument20 pagesMnemonics and Acronyms For Nursing SchoolFaye G.100% (3)
- Acne Keloidalis NuchaeDocument16 pagesAcne Keloidalis NuchaejalalfaizPas encore d'évaluation
- Maternal Obesity and Diabetes Mellitus As Risk Factors For Congenital Heart Disease in The OffspringDocument9 pagesMaternal Obesity and Diabetes Mellitus As Risk Factors For Congenital Heart Disease in The OffspringBianca CaterinalisendraPas encore d'évaluation
- Frederick Griffith: Bacterial TransformationDocument4 pagesFrederick Griffith: Bacterial Transformationrasha nada100% (1)
- Reading Sub-Test - Question Paper: Part A: Instructions To CandidatesDocument8 pagesReading Sub-Test - Question Paper: Part A: Instructions To CandidatesAditi ParmarPas encore d'évaluation
- REAL in Nursing Journal (RNJ)Document8 pagesREAL in Nursing Journal (RNJ)Anonymous 8hlR5KvPas encore d'évaluation
- Urnal Vox Sanguinis - 2023 - Pons - Prevalence of Red Blood Cell Alloantibodies Among Blood Donors in The French Military BloodDocument5 pagesUrnal Vox Sanguinis - 2023 - Pons - Prevalence of Red Blood Cell Alloantibodies Among Blood Donors in The French Military BloodFauzan.APas encore d'évaluation
- Trauma in Early Childhood: A Neglected PopulationDocument20 pagesTrauma in Early Childhood: A Neglected PopulationFrancisca AldunatePas encore d'évaluation
- Case Analysis PediatricsDocument31 pagesCase Analysis PediatricsLYNDLY AGAGEOPas encore d'évaluation
- 8 Cns StimulantsDocument46 pages8 Cns StimulantslouradelPas encore d'évaluation
- 5 4 3 2 1 Grounding Techniqueqspae PDFDocument2 pages5 4 3 2 1 Grounding Techniqueqspae PDFsheetcherry57Pas encore d'évaluation
- Polysomnography (PSG) : Patient Information Patient InformationDocument12 pagesPolysomnography (PSG) : Patient Information Patient Informationhotland sitorusPas encore d'évaluation
- What? Who?: DR - Mabel Sihombing Sppd-Kgeh DR - Ilhamd SPPD Dpertemen Ilmu Penyakit Dalam Rs - Ham/Fk-Usu MedanDocument45 pagesWhat? Who?: DR - Mabel Sihombing Sppd-Kgeh DR - Ilhamd SPPD Dpertemen Ilmu Penyakit Dalam Rs - Ham/Fk-Usu MedanM Rizky Assilmy LubisPas encore d'évaluation
- Formularium 2017Document87 pagesFormularium 2017Venita AgustinaPas encore d'évaluation
- "The Effects of Interpersonal Crime On Victims": Reporter: Michel O. Espinosa Bs-Psychology Code: 3175Document6 pages"The Effects of Interpersonal Crime On Victims": Reporter: Michel O. Espinosa Bs-Psychology Code: 3175Ezri Mariveles Coda Jr.Pas encore d'évaluation
- ADR Notes KINJAL S. GAMITDocument13 pagesADR Notes KINJAL S. GAMITKinjal GamitPas encore d'évaluation
- Lesson Plan On Nursing Care of A Patient With Acute Renal FailureDocument17 pagesLesson Plan On Nursing Care of A Patient With Acute Renal FailurePriyanka NilewarPas encore d'évaluation
- Punjab Public Service CommissionDocument2 pagesPunjab Public Service CommissionShehnila ShoukatPas encore d'évaluation
- Malabsorption SyndromeDocument7 pagesMalabsorption SyndromeHassan.shehri100% (4)
- Fetal DistressDocument111 pagesFetal DistressSakariye SuleimanPas encore d'évaluation
- 1-Cardiac AnatomyDocument5 pages1-Cardiac AnatomyZintan HospitalPas encore d'évaluation
- JaundiceDocument4 pagesJaundiceTaleb AbjiPas encore d'évaluation
- Pregnancy ComplicationsDocument14 pagesPregnancy Complicationsvienny kayePas encore d'évaluation
- ThesisDocument95 pagesThesisDrGeorge Saad AbdallaPas encore d'évaluation
- Clear Sky Recovery's Ibogaine Treatment Program To Be Featured On National GeographicDocument3 pagesClear Sky Recovery's Ibogaine Treatment Program To Be Featured On National GeographicPR.comPas encore d'évaluation
- Intrapartum HandoutDocument29 pagesIntrapartum HandoutZahPas encore d'évaluation