Académique Documents
Professionnel Documents
Culture Documents
Non Anesthetic Action of Local Anesthetics
Transféré par
web3351Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Non Anesthetic Action of Local Anesthetics
Transféré par
web3351Droits d'auteur :
Formats disponibles
PERIODICUM BIOLOGORUM UDC 57:61
VOL. 115, No 2, 113–117, 2013 CODEN PDBIAD
ISSN 0031-5362
Leading article
Non anesthetic action of local anesthetics
Summary
ALAIN BORGEAT
Local anesthetics are not only used as drugs to block the sodium channel to
Department of Anesthesiology provide analgesia and anti-arrhythmic action. The purpose of this review is to
Balgrist University Hospital highlight the new indications and limitations of this class of drugs. Recent
Forchstrasse 340 research has focused on the use of i.v. local anesthetics to improve bowel
CH-8008 Zurich / Switzerland
E-mail: alain.borgeat@balgrist.ch function after surgery or trauma, to protect the central nervous system, to find
new clues of local anesthetic effects in chronic neuropathic pain and to
investigate the long-term effect of anesthesia / analgesia provided by local
anesthetics on cancer recurrence. Recent facts dealing with myo- and chon-
Key words: Local anesthetics;
neuroprotection; chronic pain; drotoxicity are presented. There is growing evidence that local anesthetics
intrathecal administration; antimicrobial have a broad spectrum of indications aside analgesia and anti-arrhythmic
properties; cancer recurrence; myotoxicity; effect. Most of them are still insufficiently known and investigated. These new
chondrotoxicity indications will no doubt be intensively studied in the coming years.
INTRODUCTION
T he use of local anesthetics has long been focused on the treatment
of pain and cardiac arrhythmias. During the last decades several
studies have demonstrated that local anesthetics are able to interfere
with other receptors (1). This has led to the administration of local
anesthetics in different settings including postoperative ileus, neuro-
protection, decompression sickness, cerebral air embolism, cancer re-
currence and various types of inflammation. On the other hand some
concerns including chondrotoxicity have been the focus of different
investigations. The aim of this review is to provide an overview of
recent progress in terms of new indications and limitations of local
anesthetic application.
Recovery of bowel function
Postsurgical ileus is a common occurrence after abdominal surgery,
and is one of the major reasons to delay patient’s discharge. Previous
studies have shown that continuous infusion of lidocaine has positive
effects in this setting (2, 3). These preliminary results have been confirmed
by Harvey et al (4). The authors examined in a prospective, randomized
and double-blinded study whether systemic infusion of lidocaine
(1 mg/min for 24h) compared to a placebo could reduce postoperative
pain, duration of postsurgical ileus and time to discharge. Patients
receiving lidocaine had less postoperative pain, the return of bowel
movement was fastened and they were discharged home one day earlier
than the others. Paralytic ileus is a major concern in the acute phase of
spinal cord injury. The effect of i.v. lidocaine infusion (2–3 mg/min)
Received May 15, 2013. was investigated in seven patients with severe traumatic spinal cord
injury resistant to the administration of i.v. neostigmine. In five patients
A. Borgeat Non anesthetic action of local anesthetics
bowel function recovered 10–20 h after lidocaine initia- before and after i.v. administration of lidocaine. The
tion5. Among the possible hypothesis to explain the salu- authors found in this animal model that lidocaine when
tary effects of i.v. lidocaine, a reduction of the inflam- administered intravenously, did not abolish or diminish
matory reaction secondary to peritoneal distension and / the brain’s response as measured by functional magnetic
or reduction of post-traumatic – post-surgical stress have resonance imaging using the blood-oxygen-level depen-
been suggested (6, 7). dent activation to innocuous or acute noxious electrical
Beaussier et al (8). investigated the effects of parietal stimulation of the forepaw in normal rats. Moreover, this
analgesia on postoperative diaphragm dysfunction after investigation showed that lidocaine enhanced the soma-
major open colorectal surgery. Patient received ropiva- tosensory cortical response to acute noxious stimulation.
caine 0.2% given at a rate of 10ml/h during 48 h through This is in contrast to what has been observed previously
a preperitoneal wound catheter. PCA-morphine was us- for opioid analgesics (15). These findings raised several
ed in the treatment and control group. Diaphragmatic challenging questions regarding the mode of action of
function was assessed by the sniff inspiratory pressure lidocaine in the setting of neuropathic pain. The efficacy
test. It was shown that patients receiving preperitoneal of lidocaine application to relieve neuropathic pain was
ropivacaine had a significant lower decrease in the sniff further confirmed by Kanai et al (16). They compared
inspiratory pressure compared to the control group at the metered-dose 8% lidocaine pump spray to saline
24h – 24% vs – 58% and at 48h – 11% vs – 44%, respec- placebo pump in patients having posttraumatic peri-
tively. It was hypothesized that the beneficial effect could pheral neuropathy. The pump sprays were applied di-
be attributed not only to analgesia, but also to the blockade rectly to painful skin areas. The results demonstrated
of peritoneal afferents involved in the reflex diaphragma- that the lidocaine pump spray, but not the placebo one,
tic dysfunction induced by intra-abdominal surgery (9). significantly decreased the intensity of the continuing pain
and tactile allodynia. Compared to patch this system has
Neuroprotection / chronic pain the advantages to have a more rapid onset of action and
the possibility to increase the dose when necessary.
Several studies have previously shown that lidocaine
at antiarrhythmic doses (10) or lower doses (11) demon- There is growing evidence that local anesthetics mo-
strates neuroprotective effects. These potential properties dulate a wide range of ion channels other than sodium
are of great importance since the severity of neurologic channels. How systemic application of lidocaine exerts
sequelae and the relatively limited therapeutic inter- its analgesic effect is not entirely clear. In order to better
ventions make this an important area of research. Post- document this effect Muth-Selbach et al (17) administer-
operative neurocognitive decline is detected in more than ed intrathecally on rats l-serine (an agonist at the gly-
50% of patients after cardiac surgery and is still present 6 cine-binding site at the NMDA receptor), its inactive
months later in 30%. Mathew et al (12) investigated in a isomer I-serine CGP 78608 (antagonist at the glycineB-
prospective, randomized double-blinded, placebo con- -site of the NMDA receptor) and strychnine (antagonist
trolled study whether a continuous infusion of lidocaine at inhibitory glycine receptor) after the animals received
(bolus 1mg/kg followed by 1mg/min for the next 48h) i.v. lidocaine and formalin s.c. in the paw. The results
would reduce postoperative cognitive dysfunction after indicated a modulatory effect of lidocaine on the NMDA
cardiac surgery using cardiopulmonary bypass. This work receptor and since lidocaine-induced antinociception was
demonstrated that lidocaine did not reduce the incidence antagonized by both glycineB-site modulators and strych-
of cognitive dysfunction, but in non-diabetic patients a nine, this would favour the hypothesis of a general gly-
secondary analysis did show a protective effect, which cine-like action on inhibitory strychnine-sensitive recep-
was still present 1 year after surgery. This study suggests tors and on strychnine-insensitive glycine receptors. This
that certain patients, but not all, may benefit from this is one new possible mechanism to explain lidocaine ef-
treatment. fect. However, chronic / neuropatic pain is such a com-
plex process that research is still needed to have a better
Neuropathic pain is a chronic condition characteriz- understanding.
ed by spontaneous pain, allodynia, hyperalgesia, and
sensory deficits in the painful area. Treatment is still MDMA (3.4 methylene-dioxy-methamphetamine) is
often inadequate. Gormen et al (13) were able to show commonly consumed by many teenagers and young adults.
that both AMPA/GluR5 antagonist (NS 1209) and lido- MDMA is more and more frequently consumed with a
caine reduced significantly brush – evoked allodynia and local anesthetic, cocaine. The influence of this "cocktail"
cold allodynia in a small group of patients with well- on motor activity, anxiety, memory and brain mono-
-defined neuropathic pain symptoms. These are key ele- amines in adolescent mice has been assessed18. This
ments of neuropathic pain suggesting that AMPA recep- investigation showed that both drugs, administered alone
tor ligands may be involved in pain modulation and also or concurrently, produced hyperactivity and decrease in
that lidocaine may interfere with this receptor. In order to social contacts. However, an anxiolytic effect assessed by
elucidate the question whether lidocaine analgesic ef- means of elevated plus maze and expressed as an increase
fects are mediated through central rather than peripheral in the time on the open arms, was observed only in those
nervous system action, Luo et al (14) performed fMRI in animals treated with both MDMA and cocaine. Mice
anesthetized rats to quantify brain activation patterns in treated with MDMA did not present significant changes
response to innocuous and noxious forepaw stimulation in brain monoamines, while those receiving both drugs
114 Period biol, Vol 115, No 2, 2013.
Non anesthetic action of local anesthetics A. Borgeat
showed a decrease in dopamine in the striatum, which TNS is still unknown. In order to have a better under-
was accompanied by an increase in the serotonin con- standing of the possible neurotoxicity of lidocaine, freely
centration in the striatum and cortex 30min after ad- moving rats received either saline, 400 or 1000ug of lido-
ministration. It is known that acute activation of neurons caine intrathecally (23). The impact of a pre-treatment
by cocaine induces long-term changes in behaviour by with an NMDA glutamate antagonist and a COX2 inhi-
activating transcriptional complexes and that young ado- bitor was also assessed. Cerebrospinal PGE2 levels in-
lescent male rats have greater locomotor responses than creased to 400% of baseline and remained elevated for
adults after acute low dose cocaine administration. 90–120min after intrathecal lidocaine at both doses. Pre-
treatment with both inhibitors attenuated this increase.
The purpose of Caster’s investigation (19) was to
A 40 min period of enhanced pain after von Frey filament
correlate cocaine-induced locomotor activity with neu-
stimulation – temporary state of spinal cord sensitization
ronal activation in different regions in the brain by acute
– was observed during and after sensory and motor block
cocaine in young adolescents and adult rats by mea-
recovery. This work showed that intrathecal lidocaine
suring the induction of the plasticity-associated imme-
provokes a transient period of hyperalgesia. Yet, the link
diate early genes c-fos and zif268. It was found that low
with the PGE2 increase and the occurrence of hyper-
dose cocaine induced more locomotor activity and stria-
algesia (TNS?) needs to be further investigated.
tal c-fos expression in adolescents than adults whereas
high dose cocaine induced more locomotor activity, striatal Despite adequate needle placement, application of
c-fos and striatal zif268 expression in adults. Locomotor the right local anesthetic at the adequate concentration,
activity correlated with the expression of both genes in 2–3 % of spinals still fail. Steiner et al (24) assessed
adults but correlated with striatal c-fos only in adoles- bupivacaine cerebrospinal fluid (CSF) concentration in
cents. There was also a significant correlation between all patients with inadequate block, after intrathecal ap-
the expression of c-fos and zif 268 in the adult striatum plication of bupivacaine 0,5%. In this investigation 2600
but not in adolescents. These interesting results suggest spinals were considered. The failure rate was 2.7%. A
that the coordinated expression of transcription factors CSF concentration of bupivacaine of 73ug ml–1 was con-
by cocaine continues to develop during adolescence. The sidered adequate for a successful spinal. In the failure
immature regulation of transcription factors by cocaine group the CSF concentration was between 3.36 and 1020
could explain why adolescents show unique sensitivity to ug.ml–1. A large number of failures had a concentration
specific long-term behavioural alterations following co- below 73ug.ml–1, but some of them were above, suggest-
caine treatment. ing maldistribution of local anesthetic to explain the
failure. This work highlights the fact that inadequate
Intrathecal administration CSF local anesthetic concentration may explain some
cases, but not all, of spinal failure in the absence of
Local anesthetics are frequently administered intra- technical problem. Other issue like drug maldistribution
thecally for various procedures or pathologies. Tian et al should be considered.
(20) investigated the best dosage of lidocaine administer-
ed intrathecally in a rat model of established thermal
hyperalgesia and tactile allodynia. The following dosages Antimicrobial properties
were compared: 2, 6.5, 15 and 35mg/kg. Behavioural tests Local anesthetics have long been known to inhibit the
indicated that 6.5, 15 and 35mg/kg showed different de- growth of different species in vitro (25). Infiltration of
grees of reversal of thermal hyperalgesia lasting 2–8 days, surgical wound with 2ml lidocaine 2% prior to inocu-
while 2mg/kg did not. The inhibition of tactile allodynia lation was associated with an average decrease in bacte-
was only observed in rats receiving 15 and 35mg/kg. rial count of >70%26. Epidural abscess is an uncommon
Considering the ratio benefits/side-effects, the dosage of yet serious complication of epidural catheterisation. Cogh-
15 mg/kg was the most suitable for this indication. How- lan et al (27) investigated the antibacterial activity of
ever, the mechanisms of action remain to be elucidated. various local anesthetics and additives used in epidural
infusions, against a range of micro-organisms associated
Ambulatory surgical procedures are more and more
with epidural abscess. Different concentrations of bupi-
commonly used worldwide. Spinal anesthesia is a good
vacaine, ropivacaine and levobupivacaine with or with-
and reliable technique in this setting. However, lido-
out fentanyl, adrenaline or clonidine were tested. Bupi-
caine, which has been frequently used in this indication,
vacaine was shown to have the most efficient activity
has been reported to be neurotoxic. In order to look for
against micro-organisms. It showed antibacterial activity
more suitable alternative Takenami et al (21) compared
against staphylococcus aureus, enterococcus faecalis and
the clinical course and toxicity of different local anesthetics
escherichia coli with minimum inhibitory concentra-
administered intrathecally in rats. Different concentra-
tions between 0.125% and 0.25%. However, bupivacaine
tions of prilocaine, mepivacaine, procaine or bupivacaine
did not inhibit the growth of pseudomonas aeruginosa.
were compared. Among the 4 local anesthetics tested,
Levobupivacaine and ropivacaine had no activity against
procaine has the mildest neurotoxicity and the fastest
any of the micro organisms tested. The presence of fent-
recovery time to ambulation.
anyl, adrenaline and clonidine had no additional effect
Lidocaine has been implicated in the occurrence of on the antimicrobial activity of any of the local anesthetic
TNS (22). However, the exact mechanism explaining tested. While the clinical implications of this in vitro
Period biol, Vol 115, No 2, 2013. 115
A. Borgeat Non anesthetic action of local anesthetics
study are not known, consideration should be given to control group. This study indicates that i.v. lidocaine
use higher concentration of LA (bupivacaine 0.25% has a reduces surgery-induced immune alterations. The long-
greater antimicrobial activity than 0.125%) in epidural -term clinical implications of these findings are unknown
infusion in order to take advantage of this property. and warrant future investigations.
The application of EMLA® cream is indicated for
topical anesthesia of the skin in connection with i.v. CONCLUSIONS
cannulation, as vascular access is often linked with noso- It is fascinating that more than decades after the intro-
comial infection. The impact of EMLA® cream (an eu- duction of local anesthetics for perioperative analgesia,
tectic mixture of lidocaine 2.5% and prilocaine 2.5%) on we may still discover new properties and anticipate new
the skin flora was investigated by Batai et al (28). They applications of this class of drugs. Various types of in-
compared the bacteriostatic / bactericidal effect of EMLA® flammation including neuroprotection, acute lung inju-
with Skinsept Pur® (alcohol based disinfectant) disinfec- ry, bowel function recovery and maybe cancer recurrence
tion. Samples were taken from 0 to 12h after treatment. may be positively influenced by the application of local
EMLA® cream was shown to have a similar bactericidal anesthetics. These issues are without any doubt the chal-
effect than Skinsept Pur® and a longer bacteriostatic lenges of the coming years.
effect. This difference was significant after 4h. Whether
this finding may have clinical relevance in terms of re-
ducing nosocomial infection need further studies.
REFERENCES
1. CASSUTO J, SINCLAIR R, BONDEROVIC M 2006 Anti-inflam-
Cancer recurrence matory properties of local anesthetics and their present and potential
Surgery still remains a cornerstone in the manage- clinical implications. Acta Anaesheiol Scand 50: 265-82
2. GROUDINE S B, FISHER H A, KAUFMAN R P JR., PATEL M
ment of cancer patients. However, surgery inevitably K, WILKINS L J, MEHTA S A, LUMB P D 1998 Intravenous
induces a profound neuroendocrine, metabolic, and cy- lidocaine speeds the return of bowel function, decreases postopera-
tokine response. A retrospective analysis has suggested tive pain, and shortens hospital stay in patients undergoing radical
that paravertebral anesthesia and analgesia for breast retropubic prostatectomy. Anesth Analg 86: 235-9
3. KABA A, LAURENT S R, DETROZ B J, SESSLER D I, DURIEUX
cancer surgery reduced the risk of recurrence of meta- M E, LAMY M L, JORIS J L 2007 Intravenous lidocaine infusion
stasis during the initial years of follow-up (29). Biki et al facilitates acute rehabilitation after laparoscopic colectomy. Anesthe-
(30) performed a similar retrospective review of cancer siology 106: 11-8
patients after radical prostatectomy. They compared out- 4. HARVEY K P, ADAIR J D, ISHO M, ROBINSON R 2009 Can
intravenous lidocaine decrease postsurgical ileus and shorten hospi-
come between a group having general anesthesia with tal stay in elective bowel surgery? A pilot study and literature review.
either opioid analgesia or epidural analgesia. This analy- Am J Surg 198: 231-6
sis showed that open prostatectomy surgery with general 5. BAUMANN A, AUDIBERT G, KLEIN O, MERTES P M 2009
anesthesia, substituting epidural analgesia for postopera- Continuous intravenous lidocaine in the treatment of paralytic ileus
due to severe spinal cord injury. Acta Anaesthesiol Scand 53: 128-30
tive opioids, was associated with substantially less risk of 6. NELLGARD P, JONSSON A, BOJO L, TARNOW P, CASSUTO J
biochemical cancer recurrence. These exciting perspecti- 1996 Small-bowel obstruction and the effects of lidocaine, atropine
ves warrant prospective, randomized trials to evaluate and hexamethonium on inflammation and fluid losses. Acta Ana-
this association. General anesthesia, pain, sympathetic esthesiol Scand 40: 287-92
7. BAUER A J, BOECKXSTAENS G E 2004 Mechanisms of post-
blockade, all are involved in the modulation of the im- operative ileus. Neurogastroenterol Motil 16 (Suppl 2): 54-60
mune system. The natural killer cells (NK) are an im- 8. BEAUSSIER M, EL’AYOUBI H, ROLLIN M, PARC Y, ATCHA-
portant part of non-specific cellular-mediated and anti- BAHIAN A, CHANQUES G, CAPDEVILA X, LIENHART A,
tumoral immunity. Forget and De Kock (31) performed a JABER S 2009 Parietal analgesia decreases postoperative diaphragm
dysfunction induced by abdominal surgery: a physiologic study. Reg
systematic review to recapitulate data over NK activity Anesth Pain Med 34: 393-7
during the perioperative period and the influence of 9. MANIKIAN B, CANTINEAU J P, BERTRAND M, KIEFFER E,
anesthesia, analgesia and modulation of sympathetic sys- SARTENE R, VIARS P 1988 Improvement of diaphragmatic func-
tem. It came out from this review that local anesthetics, tion by a thoracic extradural block after upper abdominal surgery.
Anesthesiology 68: 379-86
contrary to opioids, stimulate the activity of NK cells 10. LEI B, POPP S, CAPUANO-WATERS C, COTTRELL J E, KASS
during the perioperative period. However, it is important I S 2004 Lidocaine attenuates apoptosis in the ischemic penumbra
to keep in mind that the long term consequences of each and reduces infarct size after transient focal cerebral ischemia in rats.
technique on patient’s outcome warrant further investi- Neuroscience 125: 691-701
11. CAO H, KASS I S, COTTRELL J E, BERGOLD P J 2005 Pre- or
gations. Yardeni et al (32) assessed pain intensity and postinsult administration of lidocaine or thiopental attenuates cell
immune reactivity in two groups of female patients sche- death in rat hippocampal slice cultures caused by oxygen-glucose
duled for transabdominal surgery assigned either to i.v. deprivation. Anesth Analg 101: 1163-9
lidocaine started 20min before surgery or a placebo. All 12. MATHEW J P, MACKENSEN G B, PHILLIPS-BUTE B, GRO-
COTT H P, GLOWER D D, LASKOWITZ D T, BLUMEN-
patients had patient-controlled epidural analgesia. In the THAL J A, NEWMAN M F 2009 Randomized, double-blinded,
lidocaine group postoperative pain at rest and during placebo controlled study of neuroprotection with lidocaine in cardiac
coughing was less in the first 8 postoperative hours. The surgery. Stroke 40: 880-7
in vivo production of IL-1ra and IL-6 was significantly 13. GORMSEN L, FINNERUP N B, ALMQVIST P M, JENSEN T S
2009 The efficacy of the AMPA receptor antagonist NS1209 and
reduced, whereas the lymphocyte proliferation response lidocaine in nerve injury pain: a randomized, double-blind, pla-
to phytohemmaglutinin-M was better maintained in the cebo-controlled, three-way crossover study. Anesth Analg 108: 1311-9
116 Period biol, Vol 115, No 2, 2013.
Non anesthetic action of local anesthetics A. Borgeat
14. LUO Z, YU M, SMITH S D, KRITZER M, DU C, MA Y, VOL- levels in cerebrospinal fluid: a microdialysis study in freely moving
KOW N D, GLASS P S, BENVENISTE H 2009 The effect of rats. Br J Anaesth 101: 716-22
intravenous lidocaine on brain activation during non-noxious and 24. StEINER L A, HAUENSTEIN L, RUPPEN W, HAMPL K F,
acute noxious stimulation of the forepaw: a functional magnetic SEEBERGER M D 2009 Bupivacaine concentrations in lumbar
resonance imaging study in the rat. Anesth Analg 108: 334-44 cerebrospinal fluid in patients with failed spinal anaesthesia. Br J
15. WISE R G, WILLIAMS P, TRACEY I 2004 Using fMRI to quantify Anaesth 102: 839-44
the time dependence of remifentanil analgesia in the human brain. 25. PARR A M, ZOUTMAN D E, DAVIDSON J S 1999 Antimicrobial
Neuropsychopharmacology 29: 626-35 activity of lidocaine against bacteria associated with nosocomial
16. KANAI A, SEGAWA Y, OKAMOTO T, KOTO M, OKAMOTO H wound infection. Ann Plast Surg 43: 239-45
2009 The analgesic effect of a metered-dose 8% lidocaine pump
26. STRATFORD A F, ZOUTMAN D E, DAVIDSON J S 2002 Effect
spray in posttraumatic peripheral neuropathy: a pilot study. Anesth
Analg 108: 987-91 of lidocaine and epinephrine on Staphylococcus aureus in a guinea
pig model of surgical wound infection. Plast Reconstr Surg 110:
17. MUTH-SELBACH U, HERMANNS H, STEGMANN JU, KOL- 1275-9
LOSCHE K, FREYNHAGEN R, BAUER I, LIPFERT P 2009
Antinociceptive effects of systemic lidocaine: involvement of the 27. COGHLAN M W, DAVIES M J, HOYT C, JOYCE L, KILNER R,
spinal glycinergic system. Eur J Pharmacol 613: 68-73 WATERS M J 2009 Antibacterial activity of epidural infusions.
Anaesth Intensive Care 37: 66-9
18. DAZA-LOSADA M, RODRIGUEZ-ARIAS M, MALDONADO
C, AGUILAR M A, GUERRI C, MINARRO J 2009 Acute beha- 28. BATAI I, BOGAR L, JUHASZ V, BATAI R, KERENYI M A 2009
vioural and neurotoxic effects of MDMA plus cocaine in adolescent comparison of the antimicrobial property of lidocaine/prilocaine
mice. Neurotoxicol Teratol 31: 49-59 cream (EMLA) and an alcohol-based disinfectant on intact human
skin flora. Anesth Analg 108: 666-8
19. CASTER J M, KUHN C M 2009 Maturation of coordinated im-
mediate early gene expression by cocaine during adolescence. Neuro- 29. EXADAKTYLOS A K, BUGGY D J, MORIARTY D C, MASCHA
science 160: 13-31 E, SESSLER D I 2006 Can anesthetic technique for primary breast
20. TIAN J, GU Y, SU D, WU Y, WANG X 2009 Effects of intrathecal cancer surgery affect recurrence or metastasis? Anesthesiology 105:
lidocaine on hyperalgesia and allodynia following chronic constric- 660-4
tion injury in rats. Eur J Pain 13: 130-7 30. BIKI B, MASCHA E, MORIARTY D C, FITZPATRICK J M,
21. TAKENAMI T, YAGISHITA S, NARA Y, TSAI Y H, HIRUMA H, SESSLER D I, BUGGY D J 2008 Anesthetic technique for radical
KAWAKAMI T, HOKA S 2009 Spinal procaine is less neurotoxic prostatectomy surgery affects cancer recurrence: a retrospective analy-
than mepivacaine, prilocaine and bupivacaine in rats. Reg Anesth sis. Anesthesiology 109: 180-7
Pain Med 34: 189-95 31. FORGET P, DE KOCK M 2009 [Could anaesthesia, analgesia and
22. ZARIC D, CHRISTIANSEN C, PACE N L, PUNJASAWAD- sympathetic modulation affect neoplasic recurrence after surgery? A
WONG Y 2005 Transient neurologic symptoms after spinal ane- systematic review centred over the modulation of natural killer cells
sthesia with lidocaine versus other local anesthetics: a systematic activity]. Ann Fr Anesth Reanim 28: 751-68
review of randomized, controlled trials. Anesth Analg 100: 1811-6 32. YARDENI I Z, BEILIN B, MAYBURD E, LEVINSON Y, BES-
23. UMBRAIN V, SHI L, LAUWERS M H, SMOLDERS I, MICHOT- SLER H 2009 The effect of perioperative intravenous lidocaine on
TE Y, CAMU F 2008 Intrathecal lidocaine elevates prostaglandin E2 postoperative pain and immune function. Anesth Analg 109: 1464-9
Period biol, Vol 115, No 2, 2013. 117
Vous aimerez peut-être aussi
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- 15 Day Detox ChallengeDocument84 pages15 Day Detox ChallengeDanii Supergirl Bailey100% (4)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Autonomic and Adrenocortical Reactivity and Buccal Cell Telomere Length in Kindergarten ChildrenDocument18 pagesAutonomic and Adrenocortical Reactivity and Buccal Cell Telomere Length in Kindergarten Childrenweb3351Pas encore d'évaluation
- Review Article - The Aetiology, Diagnosis, Mechanisms Andclinical Evidence For Food IntoleranceDocument14 pagesReview Article - The Aetiology, Diagnosis, Mechanisms Andclinical Evidence For Food Intoleranceweb3351Pas encore d'évaluation
- Ozone As A Modulator of The Immune SystemDocument10 pagesOzone As A Modulator of The Immune Systemweb3351Pas encore d'évaluation
- Use of Adrenaline in AllergyDocument18 pagesUse of Adrenaline in Allergyweb3351Pas encore d'évaluation
- Chronic Pain and Management JournalDocument8 pagesChronic Pain and Management Journalweb3351100% (1)
- Oxygen-Ozone Therapy in The Treatment of Adipose TissueDocument9 pagesOxygen-Ozone Therapy in The Treatment of Adipose Tissueweb3351100% (1)
- TR-AUTOHEMOTHERAPY AUTOLOGOUS BLOOD TRANSFUSION OZONE THERAPY Â AN UPDATEDocument43 pagesTR-AUTOHEMOTHERAPY AUTOLOGOUS BLOOD TRANSFUSION OZONE THERAPY Â AN UPDATEweb3351100% (1)
- Chapter 2Document13 pagesChapter 2Kumkumo Kussia KossaPas encore d'évaluation
- Cloud Comp PPT 1Document12 pagesCloud Comp PPT 1Kanishk MehtaPas encore d'évaluation
- Clark SM 616 Service ManualDocument20 pagesClark SM 616 Service Manualenid100% (55)
- Health Post - Exploring The Intersection of Work and Well-Being - A Guide To Occupational Health PsychologyDocument3 pagesHealth Post - Exploring The Intersection of Work and Well-Being - A Guide To Occupational Health PsychologyihealthmailboxPas encore d'évaluation
- Chapter 13 (Automatic Transmission)Document26 pagesChapter 13 (Automatic Transmission)ZIBA KHADIBIPas encore d'évaluation
- DBMS Lab ManualDocument57 pagesDBMS Lab ManualNarendh SubramanianPas encore d'évaluation
- MCI Approved Medical College in Uzbekistan PDFDocument3 pagesMCI Approved Medical College in Uzbekistan PDFMBBS ABROADPas encore d'évaluation
- Week-3-Q1-Gen Chem-Sep-11-15-DllDocument12 pagesWeek-3-Q1-Gen Chem-Sep-11-15-DllJennette BelliotPas encore d'évaluation
- Desktop 9 QA Prep Guide PDFDocument15 pagesDesktop 9 QA Prep Guide PDFPikine LebelgePas encore d'évaluation
- Tool Charts PDFDocument3 pagesTool Charts PDFtebengz100% (2)
- Lesson 3 - ReviewerDocument6 pagesLesson 3 - ReviewerAdrian MarananPas encore d'évaluation
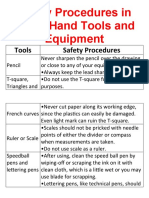
- Safety Procedures in Using Hand Tools and EquipmentDocument12 pagesSafety Procedures in Using Hand Tools and EquipmentJan IcejimenezPas encore d'évaluation
- Design of Combinational Circuit For Code ConversionDocument5 pagesDesign of Combinational Circuit For Code ConversionMani BharathiPas encore d'évaluation
- 50114a Isolemfi 50114a MonoDocument2 pages50114a Isolemfi 50114a MonoUsama AwadPas encore d'évaluation
- Injections Quiz 2Document6 pagesInjections Quiz 2Allysa MacalinoPas encore d'évaluation
- Applications SeawaterDocument23 pagesApplications SeawaterQatar home RentPas encore d'évaluation
- Catify To Satisfy - Simple Solutions For Creating A Cat-Friendly Home (PDFDrive)Document315 pagesCatify To Satisfy - Simple Solutions For Creating A Cat-Friendly Home (PDFDrive)Paz Libros100% (2)
- 1 - 2020-CAP Surveys CatalogDocument356 pages1 - 2020-CAP Surveys CatalogCristiane AokiPas encore d'évaluation
- LM2576/LM2576HV Series Simple Switcher 3A Step-Down Voltage RegulatorDocument21 pagesLM2576/LM2576HV Series Simple Switcher 3A Step-Down Voltage RegulatorcgmannerheimPas encore d'évaluation
- Where We Are in Place and Time "We Are Part of The Universe and Feel Compelled To Explore It."Document1 pageWhere We Are in Place and Time "We Are Part of The Universe and Feel Compelled To Explore It."Safia-umm Suhaim- FareedPas encore d'évaluation
- PDFDocument10 pagesPDFerbariumPas encore d'évaluation
- Z-Purlins: Technical DocumentationDocument11 pagesZ-Purlins: Technical Documentationardit bedhiaPas encore d'évaluation
- Subject Manual Tle 7-8Document11 pagesSubject Manual Tle 7-8Rhayan Dela Cruz DaquizPas encore d'évaluation
- EPAS 11 - Q1 - W1 - Mod1Document45 pagesEPAS 11 - Q1 - W1 - Mod1Alberto A. FugenPas encore d'évaluation
- Drug Addiction Final (Term Paper)Document15 pagesDrug Addiction Final (Term Paper)Dessa Patiga IIPas encore d'évaluation
- Progressive Muscle RelaxationDocument4 pagesProgressive Muscle RelaxationEstéphany Rodrigues ZanonatoPas encore d'évaluation
- Recitation Math 001 - Term 221 (26166)Document36 pagesRecitation Math 001 - Term 221 (26166)Ma NaPas encore d'évaluation
- Julia Dito ResumeDocument3 pagesJulia Dito Resumeapi-253713289Pas encore d'évaluation
- SSP 237 d1Document32 pagesSSP 237 d1leullPas encore d'évaluation