Académique Documents
Professionnel Documents
Culture Documents
10 Yr Followup RTOG Protocol 92
Transféré par
Dr.Ketaki PatilCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
10 Yr Followup RTOG Protocol 92
Transféré par
Dr.Ketaki PatilDroits d'auteur :
Formats disponibles
VOLUME 26 䡠 NUMBER 15 䡠 MAY 20 2008
JOURNAL OF CLINICAL ONCOLOGY O R I G I N A L R E P O R T
Ten-Year Follow-Up of Radiation Therapy Oncology Group
Protocol 92-02: A Phase III Trial of the Duration of Elective
Androgen Deprivation in Locally Advanced Prostate Cancer
Eric M. Horwitz, Kyounghwa Bae, Gerald E. Hanks, Arthur Porter, David J. Grignon, Harmar D. Brereton,
Varagur Venkatesan, Colleen A. Lawton, Seth A. Rosenthal, Howard M. Sandler, and William U. Shipley
From the Department of Radiation
Oncology, Fox Chase Cancer Center; A B S T R A C T
Department of Biostatistics, Radiation
Therapy Oncology Group, Philadelphia; Purpose
Northeast Radiation Oncology Center, To determine whether adding 2 years of androgen-deprivation therapy (ADT) improved outcome
Scranton, PA; Department of Radiation for patients electively treated with ADT before and during radiation therapy (RT).
Oncology, McGill University, Montréal,
Québec; Department of Radiation
Patients and Methods
Oncology, University of Western
Prostate cancer patients with T2c-T4 prostate cancer with no extra pelvic lymph node involvement
Ontario, London, Ontario, Canada; and prostate-specific antigen (PSA) less than 150 ng/mL were included. All patients received 4
Department of Pathology, Indiana months of goserelin and flutamide before and during RT. They were randomized to no further ADT
University, Indianapolis, IN; Department (short-term ADT [STAD] ⫹ RT) or 24 months of goserelin (long-term ADT [LTAD] ⫹ RT). A total of
of Radiation Oncology, Medical College 1,554 patients were entered. RT was 45 Gy to the pelvic nodes and 65 to 70 Gy to the prostate.
of Wisconsin, Milwaukee, WI; Depart-
Median follow-up of all survival patients is 11.31 and 11.27 years for the two arms.
ment of Radiation Oncology, Radiologi-
cal Associates of Sacramento, Results
Sacramento, CA; Department of Radia- At 10 years, the LTAD ⫹ RT group showed significant improvement over the STAD ⫹ RT group
tion Oncology, University of Michigan, for all end points except overall survival: disease-free survival (13.2% v 22.5%; P ⬍ .0001),
Ann Arbor, MI; and the Department of
disease-specific survival (83.9% v 88.7%; P ⫽ .0042), local progression (22.2% v 12.3%;
Radiation Oncology, Massachusetts
General Hospital, Boston, MA.
P ⬍ .0001), distant metastasis (22.8% v 14.8%; P ⬍ .0001), biochemical failure (68.1% v 51.9%;
P ⱕ .0001), and overall survival (51.6% v 53.9%, P ⫽ .36). One subgroup analyzed consisted of all
Submitted October 19, 2007; accepted
February 4, 2008; published online
cancers with a Gleason score of 8 to 10 cancers. An overall survival difference was observed
ahead of print at www.jco.org on April (31.9% v 45.1%; P ⫽ .0061), as well as in all other end points herein.
14, 2008.
Conclusion
Supported by Grants No. RTOG U10 LTAD as delivered in this study for the treatment of locally advanced prostate cancer is superior
CA21661, CCOP U10 CA37422, and to STAD for all end points except survival. A survival advantage for LTAD ⫹ RT in the treatment
STAT U10 CA32115 from the National of locally advanced tumors with a Gleason score of 8 to 10 suggests that this should be the
Cancer Institute.
standard of treatment for these high-risk patients.
Presented at the 48th Annual Meeting
of the American Society for Therapeutic J Clin Oncol 26:2497-2504. © 2008 by American Society of Clinical Oncology
Radiology and Oncology, November
5-9, 2006, Philadelphia, PA.
The contents of this article are solely indefinitely versus RT alone. A statistically signifi-
INTRODUCTION
the responsibility of the authors and do cant improvement in 10-year biochemical no evi-
not necessarily represent the official
The role of androgen-deprivation therapy (ADT) dence of disease (bNED) control, distant metastasis
views of the National Cancer Institute.
used in conjunction with external-beam radiation survival (DMS), local control (LC), and overall sur-
Authors’ disclosures of potential con-
flicts of interest and author contribu- therapy (RT) to treat locally advanced prostate can- vival (OS) was observed for patients treated with
tions are found at the end of this cer has been investigated since the 1960s.1 Early long-term ADT (LTAD).2 The role of short-term
article. ADT (STAD) was examined in RTOG 86-10. Pa-
studies demonstrated a benefit in clinical outcome
Corresponding author: Eric M. Horwitz, when ADT was used, but many questions remained tients were randomly assigned between ADT before
MD, Fox Chase Cancer Center, Depart-
ment of Radiation Oncology, 333 Cott-
unanswered, including the duration and timing of and during RT or RT alone. Significant improve-
man Ave, Philadelphia, PA 19111-2497; treatment. Substantial toxicity was also identified ment in LC was seen for patients treated with STAD.3
e-mail: eric.horwitz@fccc.edu. when hormones were used. Beginning in the 1980s, The difference between the two significant
© 2008 by American Society of Clinical the Radiation Therapy Oncology Group (RTOG) study arms from RTOG 85-31 and 86-10 was de-
Oncology developed trials based on information from these finitively tested in the largest phase III random-
0732-183X/08/2615-2497/$20.00 early studies, which incorporated new hormonal ized prospective trial of prostate cancer patients in
DOI: 10.1200/JCO.2007.14.9021 agents with less cardiovascular toxicity. RTOG North America. The first analysis of RTOG 92-02,
85-31 randomly assigned patients with locally ad- demonstrated statistically significant improve-
vanced prostate cancer between RT and goserelin ments in outcome in the long-term hormone arm
© 2008 by American Society of Clinical Oncology 2497
Downloaded from ascopubs.org by ASTRAZENECA on December 16, 2017 from 202.126.172.042
Copyright © 2017 American Society of Clinical Oncology. All rights reserved.
Horwitz et al
for disease-free survival (DFS), cause-specific survival (CSS), bio- LP, DM, BF, and DS death9 in the presence of competing risks. The log-rank
chemical failure (BF), distant metastasis (DM), and local failure test was used to test the significance between two treatment arms for end point
(LF).4 This study updates the results of RTOG 92-02 and reports of survival curves (OS and DFS).10 Gray’s test was used to test the significance
between two treatment arms for the end point of failure curves (LP, DM and
the clinical and biochemical results as well as toxicity at 10 years.
BF, and DS death).11 The testing was performed at a significance level of .05
with two-sided tests.
PATIENTS AND METHODS
RESULTS
Patient Population
Patients eligible for inclusion on RTOG 92-02 included those men with
histologically confirmed adenocarcinoma of the prostate (T2c-T4N0-X). A Table 1 shows pretreatment characteristics for 1,521 eligible patients.
pretreatment PSA less than 150 ng/mL was mandatory. The 1992 American There was no statistically significant difference between treatment
Joint Committee on Cancer Staging Manual was used for clinical staging.5 arms with respect to the stratification factors and other characteristics.
There could be no documented, DM and the participants’ Karnofsky perfor-
As reported by the institutions, RT was completed as assigned in 96%
mance status had to be at least 70%. No prior ADT, RT, or chemotherapy was
allowed. Institutional review board approval was obtained at each participat- of the cases in the STAD ⫹ RT arm and 95% of the cases in the LTAD
ing center before patient enrollment and data was transferred to a single ⫹ RT arm. Four percent and 3% of the reviewed cases were judged
statistical center per Health Insurance Portability and Accountability Act unacceptable major variations in the STAD ⫹ RT and LTAD ⫹ RT
(HIPAA) guidelines. Informed consent was obtained from each participant
before enrollment, random assignment, and treatment. The details of pretreat-
ment patient evaluations have been summarized in the previous report.4 After
RT was completed, follow-up with prostate-specific antigen (PSA) was every 3
to 6 months during the first 5 years, and then yearly. Table 1. Pretreatment Characteristics for All Eligible Patients
RT STAD ⫹ RT LTAD ⫹ RT
(n ⫽ 763) (n ⫽ 758)
All patients received conventional RT to the pelvis using a four-field
technique with megavoltage x-rays (ⱖ 4 MV) to 44 to 46 Gy. This was followed Characteristic No. % No. % 2 Test P
by a conedown to the prostate for a total dose of 65 to 70 Gy for T2c tumors and Age, years
67.5 to 70 Gy for T3 to T4 tumors. The prescribed dose was recorded at the Median 70 70
center of the prostate target volume. Range 43-87 43-88
ADT PSA, ng/mL
ADT was begun 2 months before the start of RT and continued until the ⱕ 30 511 67 510 67
RT was completed. All patients in this study received flutamide (250 mg three ⬎ 30 252 33 248 33 .8977
times a day) with goserelin (3.6 mg subcutaneously monthly) until the RT was Karnofsky status, %
completed. Patients were randomly assigned to no further treatment (STAD ⫹ 70 11 2 2 ⬍1
RT) or 24 additional months of monthly goserelin (LTAD ⫹ RT). 80 54 7 48 6
90 376 49 358 47
Study Design and End Points 100 322 42 350 46 .0425
This study was designed to test for an absolute 10% improvement in Intercurrent disease
DFS, from 40% to 50%, at 5 years. Randomization was performed before any No 254 33 246 33
treatment was started using the treatment allocation scheme described by Yes 503 66 508 67
Zelen.6 Patients were stratified according to stage, pretreatment PSA, grade, Unknown 6 1 4 ⬍1 .8881
and nodal status although the study was not powered to assess the primary end Clinical stage
point on the basis of these strata. RTOG 92-02 opened for accrual on June 26, T2 348 45 344 45
1992, and the study closed on April 15, 1995, with 1,554 registered cases. T3 394 52 376 50
Study end points included DFS, OS, local progression (LP), DM, BF, and T4 21 3 38 5 .0697
disease-specific survival (DSS). LP was defined as clinical evidence of local Pathological nodal status
recurrence (by any method) or persistent disease. DM was defined as the NX 658 87 648 86
clinical evidence of distant disease (by any method). Patients without an event N0 70 9 81 11
for either LP or DM end point were censored at the date of last follow-up or N1 24 3 18 2
death. BF was defined as the earliest of the following: three consecutive rises N2 11 1 11 1 .6328
after a post-treatment PSA nadir (the 1997 American Society for Therapeutic Institutional Gleason score
Radiology and Oncology [ASTRO] definition7), receiving additional ADT or 2-5 143 19 137 18
PSA greater than 4 ng/mL. Patients were censored at the date of last PSA. DFS 6 149 19 154 20
was defined as the first occurrence of LP, DF, BF, or death. DSS was defined as 7 226 30 251 33
a death resulting from to prostate cancer, treatment toxicity or unknown 8-10 187 24 174 23
causes with DM. All event times were measured from the date of random Unknown 58 8 42 6 .3386
assignment. Acute RT toxicities were defined as those occurring within 90 days Central Gleason score
from the start of RT. Any toxicity continuing or developing after 90 days was ⱕ6 118 15 116 15
considered a late RT toxicity. Results from a hypothesis-generating postran- 7 271 36 295 39
domization subset analysis of patients with a Gleason score of 8 to 10 was 8-10 108 14 107 14
performed in the first report and, on the basis of results from similar random- Unknown 266 35 240 32 .5013
ized prospective studies, was included in this update.
Abbreviations: STAD ⫹ RT, short-term androgen deprivation with external-
Statistical Methods beam radiation therapy; LTAD ⫹ RT, long-term androgen deprivation with
The Kaplan-Meier method was used to estimate the survival rate for OS external-beam radiation therapy followed by goserelin.
and DFS.8 The cumulative incidence approach was used to estimate the rate for
2498 © 2008 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Downloaded from ascopubs.org by ASTRAZENECA on December 16, 2017 from 202.126.172.042
Copyright © 2017 American Society of Clinical Oncology. All rights reserved.
Long-Term Results of RTOG 92-02
arm, respectively. The median follow-up for all living patients in this the cases in the STAD ⫹ RT arm and 7% and 3% of the cases in the
study is 11.3 years for both arms. LTAD ⫹ RT arm, respectively. One patient died as a result of proctitis
and one as a result of sigmoid perforation in the STAD ⫹ RT arm, and
Toxicity one patient died as a result of colostomy obstruction in the LTAD ⫹
Toxicity from treatment was scored using the previously re- RT arm. Three patients experienced grade 3 cardiac toxicities, one in
ported RTOG criteria.12 Acute and late RT and hormone toxicities are the STAD ⫹ RT group (congestive heart failure [CHF]) and two in the
listed in Table 2. Nine percent and 1% of the cases have reported grade LTAD ⫹ RT arm (one with CHF and one with ischemia). There was
3 and grade 4 acute toxicity, respectively, caused by RT in the STAD ⫹ no statistically significant difference in cardiac toxicity between the
RT arm. Seven percent and 1% of the cases have reported grade 3 and two groups, and there were no grade 4 or 5 cardiac events, although
grade 4 acute toxicity, respectively, caused by RT in the LTAD ⫹ RT this may be an underestimation.
arm. Hormone grade 3 and grade 4 toxicities are 4% and less than 1%,
respectively, at any time in both arms. One patient in the LTAD ⫹ RT Treatment Outcomes
arm died as a result of chemical hepatitis during the hormone treat- Table 3 shows the 10-year treatment outcomes for the entire
ment. As seen in Table 2, LTAD increased late toxicity. Grade 3 and study population. The estimated DFS (the primary end point) at 10
grade 4 late toxicity caused by RT have been reported in 6% and 1% of years was 13.2% and 22.5% for the STAD ⫹ RT arm and LTAD ⫹ RT
Table 2. Acute and Chronic Toxicity for All Eligible Patients
STAD ⫹ RT (n ⫽ 763) LTAD ⫹ RT (n ⫽ 758)
Toxicity Grade 1 Grade 2 Grade 3 Grade 4 Grade 5 Grade 1 Grade 2 Grade 3 Grade 4 Grade 5
Acute radiotherapy toxicityⴱ
Skin 205 97 2 1 0 192 111 3 1 0
Bladder 284 188 36 3 0 289 177 22 1 0
Bowel 229 358 10 0 0 212 354 14 0 0
Other GU 45 19 4 0 0 41 22 1 1 0
Other GI 63 38 1 0 0 45 55 1 0 0
Other 82 54 20 6 0 68 62 16 7 0
Maximum toxicity per patient 198 418 65 10 0 213 406 50 10 0
% 26 55 9 1 0 28 54 7 1 0
Late radiotherapy toxicity†
Skin 47 19 0 0 0 55 17 0 0 0
Bladder 200 98 31 2 0 169 121 25 13 0
Bowel 228 112 5 2 1 216 107 15 2 2
Other GU 115 34 7 2 0 115 45 4 3 0
Other GI 76 24 2 0 0 93 31 4 2 0
Other 94 28 5 0 0 78 36 10 1 0
Maximum toxicity per patient 282 210 45 5 1 236 210 50 19 2
% 37 28 6 1 ⬍1 31 28 7 3 ⬍1
Hormone toxicity‡
Nausea 0 3 0 0 0 0 0 2 0 0
Vomiting 1 2 0 0 0 0 1 1 0 0
Diarrhea 12 32 7 1 0 0 21 7 1 0
Headache 0 0 1 0 0 0 0 0 0 0
Fluid retention 0 1 0 0 0 0 0 0 0 0
Gynecomastia 0 0 0 0 0 1 0 0 0 0
Skin Rash 1 1 0 0 0 1 1 1 0 0
Infection 1 1 0 0 0 0 1 0 0 0
Elevated AST 51 20 8 1 0 95 22 11 1 1
Thrombophi/emboli 1 0 0 0 0 0 0 0 0 0
Cardiac 0 0 1 0 0 0 0 2 0 0
Hot Flashes 0 0 0 0 0 1 0 0 0 0
Impotence 0 0 1 0 0 0 0 0 0 0
Other 40 16 15 1 0 64 14 13 3 1
Maximum toxicity per patient 72 56 29 2 0 119 45 34 5 1
% 9 7 4 ⬍1 0 16 6 4 1 ⬍1
NOTE. P values calculated from statistics ⱕ grade 2 versus ⱖ grade 3 between the two arms.
Abbreviations: STAD ⫹ RT, short-term androgen deprivation with external-beam radiation therapy; LTAD ⫹ RT, long-term androgen deprivation with external-beam
radiation therapy followed by goserelin; GU, genitourinary.
ⴱ 2
test P ⫽ .2104; n ⫽ 763 for STAD ⫹ RT and 758 for LTAD ⫹ RT.
†2 test P ⫽ .0269 (statistically significant at ␣ ⫽ .05); n ⫽ 762 for STAD ⫹ RT and 755 for LTAD ⫹ RT.
‡2 test P ⫽ .9789; n ⫽ 763 for STAD ⫹ RT and 758 for LTAD ⫹ RT.
www.jco.org © 2008 by American Society of Clinical Oncology 2499
Downloaded from ascopubs.org by ASTRAZENECA on December 16, 2017 from 202.126.172.042
Copyright © 2017 American Society of Clinical Oncology. All rights reserved.
Horwitz et al
Table 3. 10-Year Treatment Outcomes for All Eligible Patients
STAD ⫹ RT (n ⫽ 763) LTAD ⫹ RT (n ⫽ 758)
Outcome No. of Failures Estimated Rate 95% CI No. of Failures Estimated Rate 95% CI Log-Rank 2 Test P
Disease-free survival 653 13.2 11 to 16 571 22.5 19 to 26 ⬍ .0001ⴱ
Overall survival 351 51.6 48 to 55 330 53.9 50 to 58 .3590
Disease-specific survival 116 83.9 81 to 87 80 88.7 86 to 91 .0042ⴱ
Local progression 166 22.2 19 to 25 90 12.3 10 to 15 ⬍ .0001ⴱ
Distant metastasis 167 22.8 20 to 26 107 14.8 12 to 17 ⬍ .0001ⴱ
Biochemical failure 513 68.1 65 to 71 384 51.9 48 to 55 ⬍ .0001ⴱ
Abbreviations: STAD ⫹ RT, short-term androgen deprivation with external-beam radiation therapy; LTAD ⫹ RT, long-term androgen deprivation with external-beam
radiation therapy followed by goserelin.
ⴱ
Statistically significant at .05.
arm, respectively (P ⬍ .0001). The 10-year OS rates are 51.6% and differences in DFS, DSS, LP, DM, and BF were observed within the
53.9% for the STAD ⫹ RT and LTAD ⫹ RT arms, respectively entire population, with patients randomly assigned to the LTAD ⫹ RT
(P ⫽ .359). The LTAD ⫹ RT arm statistically significantly improved arm demonstrating superior outcome. The primary end point testing
patients’ 10-year DFS (P ⬍ .0001) and DSS (P ⫽ .004), and reduced LP for an absolute 10% improvement in DFS, from 40% to 50%, was
(P ⬍ .0001), DM (P ⬍ .0001) and BF (P ⬍ .0001) compared with the positive at 5 and 10 years. This trial was not designed to detect a
STAD ⫹ RT arm. These differences remain when adjusted for PSA survival difference, yet a difference in cause-specific mortality was
and T stage (Table 4). The LTAD ⫹ RT arm significantly improved seen. The subset of patients with a Gleason score of 8 to 10 treated with
patients’ DFS (P ⬍ .0001), DSS (P ⫽ .002), LP (P ⬍ .0001), DM LTAD ⫹ RT had statistically significant improvements in OS, DFS,
(⬍ 0.0001), and BF (P ⬍ .0001) at 10 years compared with the STAD and DSS, and statistically significant reductions in LP, DM, and BF.
⫹ RT arm (Fig 1). Toxicity remained low, although patients who received LTAD had
increased rates of GI toxicity.
Treatment Outcomes of the Subgroup With a Gleason The RTOG began investigating the role of ADT combined with
Score of 8 to 10 RT in the treatment of locally advanced prostate cancer in the 1980s.
For patients with a Gleason score of 8 to 10, there are statistically The long-term results of RTOG 85-31, which randomly assigned 977
significant improvements in DFS (P ⬍ .0001), OS (P ⫽ 0061), and
patients to receive between 65 and 70 Gy external beam RT and
DSS (P ⫽ .0072), and reductions in LP (P ⫽ .0338), DM (P ⫽ .0019),
goserelin started during the last week of RT (arm 1) and continuing
and BF (P ⬍ .0001) for the patients in the LTAD ⫹ RT arm compared
indefinitely versus RT alone (arm 2) were reported by Pilepich et al2
with the STAD ⫹ RT arm (Table 5; Fig 2).
and demonstrated significant differences between the two treatment
arms at 10 years for bNED control, DMF, LF, and OS (P ⬍ .0001) after
DISCUSSION long follow-up.
RTOG 86-10 opened after RTOG 85-31 began accruing patients.
In this study, we report the long-term clinical, biochemical, and tox- Prostate cancer patients with T2b-4N0-1M0 and tumors larger than
icity results from RTOG 92-02. At 10 years, statistically significant 25 cm2 were randomly assigned between goserelin and flutamide 2
Table 4. 10-Year Multivariate Analysis for All Eligible Patients
Outcome Comparison HR 95% CI 2 Test P
Disease-free survival STAD⫹RT RL 0.582 to 0.726 ⬍ .0001ⴱ
LTAD⫹RT 0.65
Overall survival STAD⫹RT RL 0.804 to 1.057 .2447
LTAD⫹RT 0.922
Disease-specific survival STAD⫹RT RL 0.504 to 0.857 .0019ⴱ
LTAD⫹RT 0.657
Local progression STAD⫹RT RL 0.399 to 0.663 ⬍ .0001ⴱ
LTAD⫹RT 0.514
Distant metastasis STAD⫹RT RL 0.456 to 0.732 ⬍ .0001ⴱ
LTAD⫹RT 0.578
Biochemical failure STAD⫹RT RL 0.476 to 0.621 ⬍ .0001ⴱ
LTAD⫹RT 0.544
NOTE. Multivariate Cox proportional hazard models include the following covariates: prostate-specific antigen (ⱕ 30 关RL兴, ⬎ 30 ng/mL), T stage (T2 关RL兴, T3, T4)
and treatment (STAD ⫹ RT 关RL兴, LTAD⫹RT).
Abbreviations: STAD ⫹ RT, short-term androgen deprivation with external-beam radiation therapy; LTAD ⫹ RT, long-term androgen deprivation with external-beam
radiation therapy followed by goserelin; HR, hazard ratio; RL, reference level.
ⴱ
Statistically significant at .05.
2500 © 2008 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Downloaded from ascopubs.org by ASTRAZENECA on December 16, 2017 from 202.126.172.042
Copyright © 2017 American Society of Clinical Oncology. All rights reserved.
Long-Term Results of RTOG 92-02
A 1.0 B 1.0
0.9 0.9
0.8 0.8
DSS Non Failure Rate
STAD + RT STAD + RT
LTAD + RT LTAD + RT
Non Failure Rate
0.7 P = .0042 0.7 P < .0001
0.6 0.6
0.5 0.5
0.4 0.4
0.3 0.3
0.2 0.2
0.1 763 722 631 552 441 322 0.1 763 690 578 506 393 279
758 714 640 552 453 336 758 698 611 518 418 314
0 1 2 3 4 5 6 7 8 9 10 0 1 2 3 4 5 6 7 8 9 10
Time Since Random Assignment (years) Time Since Random Assignment (years)
C 1.0 D 1.0
0.9 0.9
0.8 0.8
Non Failure Rate
0.7 0.7
Survival Rate
0.6 0.6
0.5 0.5
0.4 0.4
STAD + RT STAD + RT
0.3 LTAD + RT 0.3 LTAD + RT
P < .0001 P = .3590
0.2 0.2
0.1 763 398 243 182 138 98 0.1 763 722 631 552 441 322
758 607 366 282 207 152 758 714 640 552 453 336
0 1 2 3 4 5 6 7 8 9 10 0 1 2 3 4 5 6 7 8 9 10
Time Since Random Assignment (years) Time Since Random Assignment (years)
Fig 1. (A) Disease-specific survival, (B) distant metastasis failure, (C) biochemical failure, and (D) overall survival for all eligible patients. STAD, short-term
androgen-deprivation therapy; LTAD, long-term androgen-deprivation therapy; RT, radiotherapy.
months before and during RT (arm 1, 226 patients) and RT alone treated with conventional RT doses (65 to 70 Gy).3 Both of these
(arm 2, 232 patients). At 8 years, a significant difference in LC was seen studies showed statistically significant improvements in outcome for
between the two arms (P ⫽ .004) as well as an improvement in PFS for patients treated with RT and ADT compared with patients treated
arm I (P ⫽ .0019). With longer follow-up, a difference in the rate of with RT alone; however, the ideal duration and timing of hormones
DM was observed between the two groups (P ⫽ .04). All patients in remained unknown. One of the primary goals of RTOG 92-02 was to
RTOG 85-31 and 86-10, as well as those in the current study were determine the duration of the ADT. The initial report with 5-year data
Table 5. 10-Year Treatment Outcomes for Patients With a Gleason Score of 8 to 10 and N0/NX
STAD ⫹ RT (n ⫽ 171) LTAD ⫹ RT (n ⫽ 166)
No. of Failures 10-Year No. of Failures 10-Year
Outcome by 10 Years Estimate (%) 95% CI (%) by 10 Years Estimate (%) 95% CI (%) Log-Rank 2 Test P
Overall survival 111 31.91 24.62 to 39.203 85 45.05 37.07 to 53.03 .0061
Disease-free survival 154 9.35 4.90 to 13.80 127 20.81 14.30 to 27.32 ⬍ .0001
Disease-specific survival 53 66.91 59.60 to 74.21 30 79.81 73.38 to 86.24 .0072
Local progression 46 27.26 20.49 to 34.02 29 17.77 11.87 to 23.67 .0338
Distant metastasis 66 39.69 32.16 to 47.21 39 25.56 18.64 to 32.48 .0019
Biochemical failure 126 73.87 67.20 to 80.55 89 55.95 48.06 to 63.83 ⬍ .0001
Abbreviations: STAD ⫹ RT, short-term androgen deprivation with external-beam radiation therapy; LTAD ⫹ RT, long-term androgen deprivation with external-beam
radiation therapy followed by goserelin.
www.jco.org © 2008 by American Society of Clinical Oncology 2501
Downloaded from ascopubs.org by ASTRAZENECA on December 16, 2017 from 202.126.172.042
Copyright © 2017 American Society of Clinical Oncology. All rights reserved.
Horwitz et al
A 1.0 B 1.0
0.9 0.9
0.8 0.8
DSS Non Failure Rate
STAD + RT STAD + RT
LTAD + RT LTAD + RT
Non Failure Rate
0.7 P = .0061 0.7 P = .0019
0.6 0.6
0.5 0.5
0.4 0.4
0.3 0.3
0.2 0.2
0.1 171 160 133 106 75 45 0.1 171 160 133 106 75 45
166 161 142 119 98 58 166 161 142 119 98 58
0 1 2 3 4 5 6 7 8 9 10 0 1 2 3 4 5 6 7 8 9 10
Time Since Random Assignment (years) Time Since Random Assignment (years)
C 1.0 D 1.0
0.9 0.9
0.8 0.8
Non Failure Rate
0.7 0.7
Survival Rate
0.6 0.6
0.5 0.5
0.4 0.4
STAD + RT STAD + RT
0.3 LTAD + RT 0.3 LTAD + RT
P < .0001 P = .7159
0.2 0.2
0.1 171 77 45 30 22 15 0.1 499 475 418 377 308 227
166 140 76 58 45 28 522 484 439 385 316 250
0 1 2 3 4 5 6 7 8 9 10 0 1 2 3 4 5 6 7 8 9 10
Time Since Random Assignment (years) Time Since Random Assignment (years)
Fig 2. (A) Overall survival, (B) distant metastasis failure, and (C) biochemical failure) for the subgroup of patients with a Gleason score of 8 to 10 and N0/NX. (D) Overall
survival for the subgroup of patients with a Gleason score of 2 to 7 and N0/NX subgroup. STAD, short-term androgen-deprivation therapy; LTAD, long-term
androgen-deprivation therapy; RT, radiotherapy.
demonstrated the superiority of LTAD, and one of the strengths of the that the difference in CSS persisted with longer follow-up in this study.
present analysis is that these results remain valid at 10 years. The subset analysis performed on patients with a Gleason score of 8 to
RTOG 92-02 showed improved results with LTAD for all end 10 demonstrated statistically significant improvements in OS and
points with additional follow-up, except OS. Were these benefits ob- CSS. Bolla et al14 reported the early results from the successor trial to
served elsewhere? Bolla et al13 reported results from European Organi- EORTC 22863 in 2007. EORTC 22961 was designed to test whether
sation for Research and Treatment of Cancer (EORTC) 22863, where similar prostate cancer patients would benefit from STAD therapy
415 men were randomized between RT alone (70 Gy), and RT with instead of 3 years of LTAD therapy. An interim analysis demonstrated
goserelin starting the first day of treatment and continuing for 3 years. decreased PFS in the STAD therapy arm (68.9% v 81.8% at 5 years).
The differences in clinical outcome persist between the two arms is Biochemical PFS was also improved with LTAD (78.3% v 58.9%).
similar to the results observed in the present study. LC, PSA DFS, and Preliminary results of this trial support the conclusion observed in the
OS were 98%, 50%, and 70%, respectively for the combined modality 10-year results of RTOG 92-02, although the survival advantage in the
arm compared with 84%, 20%, and 40%, respectively for the RT alone EORTC study may be explained by the inclusion of patients with more
arm. These differences were all statistically significant (P ⬍ .0001). advanced disease (⫹N2).
Patients in the control arm in the EORTC 22863 study received no As the benefits of ADT have become known, so has the potential
adjuvant ADT, whereas the patients in the control arm of RTOG 92-02 toxicity of this treatment.15,16 Patients treated with LTAD had overall
received 4 months of neoadjuvant and adjuvant ADT. The difference increased late toxicity. This has been observed in the Fox Chase expe-
in the trial design may be one explanation for the failure of RTOG rience reported by Feigenberg et al. The authors reported the results
92-02 to demonstrate an OS benefit for the entire trial cohort. Another for 1,204 patients were treated for prostate cancer with three-
reason may include the age of the patients in this study and the issue of dimensional conformal RT (3DCRT). STAD therapy was adminis-
competing medical comorbidities. It is encouraging and significant tered to 140 patients, 119 patients received LTAD therapy and 945
2502 © 2008 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Downloaded from ascopubs.org by ASTRAZENECA on December 16, 2017 from 202.126.172.042
Copyright © 2017 American Society of Clinical Oncology. All rights reserved.
Long-Term Results of RTOG 92-02
patients received no ADT. Independent predictors of grade 2 or higher should be regarded as the standard treatment for patients with pros-
GI morbidity in the multivariable analysis were the use of AD (P ⫽ tate cancer patients with a Gleason score of 8 to 10. Subsequent RTOG
.0079), higher total radiation dose (P ⬍ .0001), the lack of a rectal trials have adopted this regimen of LTAD ⫹ RT as the control arm in
shield (P ⫽ .0003), and older age (P ⫽ .0009). The 5-year actuarial risk randomized clinical trials evaluating new therapies for patients with
of grade 2 or higher GI morbidity was 17% for no AD versus 18% for high-risk prostate cancer. Two successor trials introduced cytotoxic
STAD and 26% for LTAD (P ⫽ .017).17 Recent studies have docu- chemotherapy after the RT has been completed, with the strategy of
mented the potential long-term cardiovascular risks associated with intensifying systemic therapy. RTOG 99-02 utilized a three-drug reg-
ADT.16 In RTOG 92-02, only three grade 3 cardiovascular events were imen of paclitaxel, etoposide, and estramustine, in addition to LTAD
documented, one in the STAD ⫹ RT arm and two in the LTAD ⫹ ⫹ RT.20 RTOG 05-21 utilizes a similar schema, but with docetaxel-
RT arm. based chemotherapy. Updated RT techniques, such as intensity-
Although answering many questions, the results in this study modulated radiation therapy, and doses are utilized in contemporary
leave several questions unanswered. These long-term results from trials. The fact that the experimental arm of RTOG 92-02 is still being
RTOG 92-02 strongly support the recommendation that LTAD ther- utilized as the basis of the control arm in ongoing clinical trials for
apy used in conjunction with RT for locally advanced nonmetastatic high-risk, poorly differentiated prostate cancer provides additional
prostate cancer is superior to STAD ⫹ RT. However, an OS advantage testimony to the significance of the results of this trial.
was not observed for the entire study group. Is it possible the excess The long-term results of RTOG 92-02 demonstrate that 24
toxicity for the LTAD arm negated a positive effect on CSS? Was the months of ADT after total androgen suppression and RT is superior to
study underpowered to detect a survival difference? The arms were total androgen suppression and RT alone in all end points except
evenly balanced, and the accrual goals were exceeded. We do not survival for patients with locally advanced nonmetastatic prostate
believe that excess toxicity is a probable reason. One potential expla- cancer. In a hypothesis-generating postrandomization analysis, an
nation for the lack of an OS advantage is that the follow-up interval is overall survival benefit was observed in patients with tumors hav-
not yet long enough for the patients with lower Gleason scores. Pa- ing a Gleason score of 8 to 10. No change in significant results from
tients with a Gleason score of 7 and lower represented more than 70% 5-year to 10-year follow-up was observed, proving the durability of
of the patient population, and so despite the locally advanced nature of these results.
the patient sample, the number of patients with a Gleason score of 8 to
10 at highest risk for DS mortality is relatively small. RTOG 92-02 has
enough follow-up to observe a survival advantage in the high-grade AUTHORS’ DISCLOSURES OF POTENTIAL CONFLICTS
OF INTEREST
patients because their life expectancy would be less, but there may not
be enough follow-up time to see a difference in the low-grade patients.
The significance of RT dose in this setting is also unclear. Other The author(s) indicated no potential conflicts of interest.
randomized, prospective studies have demonstrated the importance
of dose, but this has not been formally tested with STAD or LTAD AUTHOR CONTRIBUTIONS
therapy in North America. The University of Texas M.D. Anderson
Cancer Center trial reported by Pollack et al18 is the most mature
Conception and design: Eric M. Horwitz, Gerald E. Hanks,
randomized prospective prostate cancer dose escalation trial. In this William U. Shipley
study, 301 men were randomly assigned to between 70 Gy and 78 Gy. Administrative support: Kyounghwa Bae, David J. Grignon,
With 60 months of median follow-up, patients with an initial pretreat- Howard M. Sandler
ment PSA greater than 10 ng/mL experienced the greatest benefit, Provision of study materials or patients: Gerald E. Hanks, Arthur
whereas the additional 8 Gy had no effect on the more favorable Porter, Varagur Venkatesan, Colleen A. Lawton, Seth A. Rosenthal,
patients (pretreatment PSA ⱕ 10 ng/mL). In the second randomized Howard M. Sandler, William U. Shipley
Collection and assembly of data: Eric M. Horwitz, Kyounghwa Bae,
prospective trial reported by Zietman et al,19 393 patients with stage
Gerald E. Hanks, David J. Grignon, Harmar D. Brereton, Varagur
T1b/T2b prostate cancer and PSA levels less than 15 ng/mL were Venkatesan, Seth A. Rosenthal, Howard M. Sandler, William U. Shipley
randomly assigned to a total dose of either 70.2 Gy (conventional Data analysis and interpretation: Eric M. Horwitz, Kyounghwa Bae,
dose) or 79.2 Gy (high dose) with a combination of conformal photon Gerald E. Hanks, Arthur Porter, David J. Grignon, Harmar D. Brereton,
and proton beams. The 5-year rates of biochemical control were Varagur Venkatesan, Colleen A. Lawton, Seth A. Rosenthal, Howard M.
61.4% for conventional-dose and 80.4% for high-dose therapy (P ⬍ Sandler, William U. Shipley
.001). The advantage to high-dose therapy was observed in both the Manuscript writing: Eric M. Horwitz, Kyounghwa Bae, Gerald E. Hanks,
Seth A. Rosenthal, Howard M. Sandler
low-risk and the higher-risk subgroups. Final approval of manuscript: Eric M. Horwitz, Kyounghwa Bae, Gerald
The long-term results for RTOG 92-02 presented in this report E. Hanks, Arthur Porter, David J. Grignon, Harmar D. Brereton, Varagur
demonstrated an OS benefit for prostate cancer patients with a Glea- Venkatesan, Colleen A. Lawton, Seth A. Rosenthal, Howard M. Sandler,
son score of 8 to 10 treated with prolonged LTAD ⫹ RT. LTAD ⫹ RT William U. Shipley
www.jco.org © 2008 by American Society of Clinical Oncology 2503
Downloaded from ascopubs.org by ASTRAZENECA on December 16, 2017 from 202.126.172.042
Copyright © 2017 American Society of Clinical Oncology. All rights reserved.
Horwitz et al
7. American Society for Therapeutic Radiology trial 22961. J Clin Oncol 25:238s, 2007 (suppl; abstr
REFERENCES and Oncology Consensus Panel: Consensus state- 5014)
ment: Guidelines for PSA following radiation ther- 15. Rosenthal SA, Linstadt DE, Leibenhaut MH,
1. Zagars GK, Johnson DE, von Eschenbach AC, apy. Red Journal 37:1035-1041, 1997 et al: Flutamide-associated liver toxicity during treat-
et al: Adjuvant estrogen following radiation therapy 8. Kaplan EL, Meier P: Nonparametric estima- ment with total androgen suppression and radiation
for stage C adenocarcinoma of the prostate: Long- tion from incomplete observations. J Am Stat Assoc therapy for prostate cancer. Radiology 199:451-455,
term results of a prospective randomized study. Red 53:457-481, 1958 1996
Journal 14:1085-1091, 1988 9. Kalbfleisch JD, Prentice RL: The Statistical 16. D’Amico AV, Denham JW, Crook J, et al:
2. Pilepich MV, Winter K, Lawton CA, et al: Analysis of Failure Time Data. New York, NY, John Influence of androgen suppression therapy for pros-
Androgen suppression adjuvant to definitive radio- Wiley & Sons, 1980 tate cancer on the frequency and timing of fatal
therapy in prostate carcinoma: Long-term results of 10. Mantel N, Haenszel W: Statistical aspects of myocardial infarctions. J Clin Oncol 25:2420-2425,
phase III RTOG 85-31. Int J Radiat Oncol Biol Phys the analysis of data from retrospective studies of 2007
61:1285-1290, 2005 17. Feigenberg SJ, Hanlon AL, Horwitz EM, et al:
disease. J Natl Cancer Inst 22:719-748, 1959
3. Pilepich MV, Winter K, John MJ, et al: Phase Long-term androgen deprivation increases grade 2
11. Gray RJ: A class of K-sample tests for com-
III radiation therapy oncology group (RTOG) trial and higher late morbidity in prostate cancer patients
paring the cumulative incidence of a competing risk.
86-10 of androgen deprivation adjuvant to definitive treated with three-dimensional conformal radiation
Ann Stat 16:1141-1154, 1988
radiotherapy in locally advanced carcinoma of the therapy. Int J Radiat Oncol Biol Phys 62:397-405,
12. Cox JD, Stetz J, Pajak TF: Toxicity criteria of
prostate. Int J Radiat Oncol Biol Phys 50:1243-1252, 2005
the Radiation Therapy Oncology Group (RTOG) and
2001 18. Pollack A, Zagars GK, Antolak JA, et al: Pros-
the European Organization for Research and Treat-
4. Hanks GE, Pajak TF, Porter A, et al: Phase III tate biopsy status and PSA nadir level as early
trial of long-term adjuvant androgen deprivation after ment of Cancer (EORTC). Int J Radiat Oncol Biol surrogates for treatment failure: Analysis of a pros-
neoadjuvant hormonal cytoreduction and radiother- Phys 31:1341-1346, 1995 tate cancer randomized radiation dose escalation
apy in locally advanced carcinoma of the prostate: 13. Bolla M, Collette L, Blank L, et al: Long-term trial. Int J Radiat Oncol Biol Phys 54:677-685, 2002
The Radiation Therapy Oncology Group protocol results with immediate androgen suppression and 19. Zietman AL, DeSilvio ML, Slater JD, et al:
92-02. J Clin Oncol 21:3972-3978, 2003 external irradiation in patients with locally advanced Comparison of conventional-dose vs high-dose con-
5. American Joint Committee on Cancer: Pros- prostate cancer (an EORTC study): A phase III formal radiation therapy in clinically localized adeno-
tate, in Beahrs OH, Henson DE, Hutter RVP, et al randomised trial. Lancet 360:103-106, 2002 carcinoma of the prostate: A randomized controlled
(eds): Manual for the Staging of Cancer (ed 4). 14. Bolla M, van Tienhoven G, De Reijke TM, et al: trial. JAMA 294:1233-1239, 2005
Philadelphia, PA, JB Lippincott, 1992, pp 181-186 Concomitant and adjuvant androgen deprivation 20. Sandler H, DeSilvio M, Pienta K, et al: Prelim-
6. Zelen M: The randomization and stratification (ADT) with external beam irradiation (RT) for locally inary analysis of RTOG 92-02: Increased toxicity
of patients to clinical trials. J Chronic Dis 27:365- advanced prostate cancer: 6 months versus 3 years observed with the use of adjuvant chemotherapy.
375, 1974 ADT—Results of the randomized EORTC phase III Int J Radiat Oncol Biol Phys 63:123, 2005
■ ■ ■
Acknowledgment
We thank all of the patients, physicians, and support staff whose care and effort made the successful completion of this study possible.
2504 © 2008 by American Society of Clinical Oncology JOURNAL OF CLINICAL ONCOLOGY
Downloaded from ascopubs.org by ASTRAZENECA on December 16, 2017 from 202.126.172.042
Copyright © 2017 American Society of Clinical Oncology. All rights reserved.
Vous aimerez peut-être aussi
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Hiradc Om - Talian AtasDocument57 pagesHiradc Om - Talian AtasapnadiPas encore d'évaluation
- HgedgergtDocument84 pagesHgedgergtWRGWSRPas encore d'évaluation
- Assessment Environmental Toxicity ReportDocument43 pagesAssessment Environmental Toxicity ReportStan LeePas encore d'évaluation
- Cosmetic Surgery EssayDocument7 pagesCosmetic Surgery Essayalisharenee0550% (2)
- Star Health ProjectDocument52 pagesStar Health ProjectParvat Patil83% (6)
- Dwnload Full Wardlaws Contemporary Nutrition A Functional Approach 5th Edition Wardlaw Test Bank PDFDocument36 pagesDwnload Full Wardlaws Contemporary Nutrition A Functional Approach 5th Edition Wardlaw Test Bank PDFamoeboid.amvis.uiem100% (9)
- Lung Contusion & Traumatic AsphyxiaDocument17 pagesLung Contusion & Traumatic AsphyxiaLady KeshiaPas encore d'évaluation
- Summary of Non Sexist CityDocument2 pagesSummary of Non Sexist CityIMY KARDAS100% (3)
- Manual of Homeopathic Practice (1876)Document864 pagesManual of Homeopathic Practice (1876)Dr. JimPas encore d'évaluation
- ObamaDeception SupplementalBookletDocument34 pagesObamaDeception SupplementalBookletAccurateHistorian100% (4)
- Mirizzi Syndrome - UpToDateDocument15 pagesMirizzi Syndrome - UpToDateEdgar Miguel ContrerasPas encore d'évaluation
- PI - Standard - Seafood Processing - Issue 5.0 - 1-February-2019Document65 pagesPI - Standard - Seafood Processing - Issue 5.0 - 1-February-2019pebru yuwono0% (1)
- Roland Morris Disability QuestionnaireDocument2 pagesRoland Morris Disability QuestionnaireSaumya SumeshPas encore d'évaluation
- NammaKPSC - February 2020Document138 pagesNammaKPSC - February 2020anandawarPas encore d'évaluation
- Neet-Pg 2023-Notice Board PDFDocument1 046 pagesNeet-Pg 2023-Notice Board PDFHarish kammaraPas encore d'évaluation
- Magnetis Polus AmboDocument4 pagesMagnetis Polus Amboadi.mititean1585Pas encore d'évaluation
- Planet Assist Release FormDocument2 pagesPlanet Assist Release FormJonathan W. VillacísPas encore d'évaluation
- MINITACDocument2 pagesMINITACapi-19808945100% (1)
- DNAlysis MygeneRx Sample ReportDocument13 pagesDNAlysis MygeneRx Sample ReportTrustPas encore d'évaluation
- Your Wellness Profile: Laboratory ActivitiesDocument4 pagesYour Wellness Profile: Laboratory Activitiesdusty kawiPas encore d'évaluation
- Mental Health Resources - OrganizedDocument39 pagesMental Health Resources - OrganizedGabrielle Costello-GuerraPas encore d'évaluation
- PATHFIT 1 Prelim Lesson 2 and 3Document29 pagesPATHFIT 1 Prelim Lesson 2 and 3hiimleoPas encore d'évaluation
- PICS GMP Inspection PackagingDocument8 pagesPICS GMP Inspection PackagingArpita NaikPas encore d'évaluation
- Special Consideration in Neonatal Resuscitation - 2022 - Seminars in PerinatologDocument8 pagesSpecial Consideration in Neonatal Resuscitation - 2022 - Seminars in PerinatologEduardo Rios DuboisPas encore d'évaluation
- Disease AssignDocument11 pagesDisease AssignQaran PrintingPas encore d'évaluation
- Pet Registration FormDocument1 pagePet Registration FormBRGY MABUHAYPas encore d'évaluation
- CIC-My Vision of CounsellingDocument4 pagesCIC-My Vision of CounsellingChristeeba F MPas encore d'évaluation
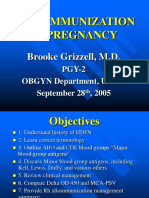
- Alloimmunization in Pregnancy: Brooke Grizzell, M.DDocument40 pagesAlloimmunization in Pregnancy: Brooke Grizzell, M.DhectorPas encore d'évaluation
- Penlon Absorbedor A200Document68 pagesPenlon Absorbedor A200Manuel FloresPas encore d'évaluation
- Essential DrugsDocument358 pagesEssential Drugsshahera rosdiPas encore d'évaluation