Académique Documents
Professionnel Documents
Culture Documents
Swallowing and Dysphagia
Transféré par
Fernanda BecerraCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Swallowing and Dysphagia
Transféré par
Fernanda BecerraDroits d'auteur :
Formats disponibles
Swallowing and Dysphagia
Rehabilitation: Translating Principles
of Neural Plasticity Into Clinically
Oriented Evidence
SUPPLEMENT
JoAnne Robbins
University of Wisconsin and William S.
Middleton VA Hospital, Geriatric Research Purpose: This review presents the state of swallowing rehabilitation science as it relates
Education and Clinical Center, to evidence for neural plastic changes in the brain. The case is made for essential
Madison, WI collaboration between clinical and basic scientists to expand the positive influences
of dysphagia rehabilitation in synergy with growth in technology and knowledge. The
intent is to stimulate thought and propose potential research directions.
Susan G. Butler
Method: A working group of experts in swallowing and dysphagia reviews 10
Wake Forest University School of Medicine,
principles of neural plasticity and integrates these advancing neural plastic concepts
Winston-Salem, NC
with swallowing and clinical dysphagia literature for translation into treatment
paradigms. In this context, dysphagia refers to disordered swallowing associated with
Stephanie K. Daniels central and peripheral sensorimotor deficits associated with stroke, neurodegenerative
Michael E. DeBakey VA Medical Center, disease, tumors of the head and neck, infection, or trauma.
Houston, TX Results and Conclusions: The optimal treatment parameters emerging from increased
understanding of neural plastic principles and concepts will contribute to evidence-
Roxann Diez Gross based practice. Integrating these principles will improve dysphagia rehabilitation
University of Pittsburgh School of Medicine, directions, strategies, and outcomes. A strategic plan is discussed, including several
Pittsburgh, PA experimental paradigms for the translation of these principles and concepts of neural
plasticity into the clinical science of rehabilitation for oropharyngeal swallowing
Susan Langmore disorders, ultimately providing the evidence to substantiate their translation into
University of California, San Francisco, CA clinical practice.
KEY WORDS: rehabilitation, nervous system, swallowing treatment, dysphagia,
Cathy L. Lazarus evidence-based practice
New York University School of Medicine,
New York, NY
Bonnie Martin-Harris
T
Medical University of South Carolina, his review seeks to stimulate translational research in the field of
Charleston, SC swallowing and swallowing disorders. Important developments can
be made in our understanding of swallowing disorders and their re-
Daniel McCabe habilitation with the testing of neural plasticity principles in both human
Bath VA Medical Center, Bath, NY and animal research designs. This review presents the principles of neural
plasticity and applies them to current evidence of both behavioral and
Nan Musson neural plasticity in swallowing. A strategic plan is formulated to faci-
North Florida/South Georgia Veterans litate the conduct of research based on the principles of neural plasticity.
Healthcare System, Gainesville, FL This document resulted from a workshop on plasticity/neurorehabilita-
tion research that was held at the University of Florida in Gainesville,
John C. Rosenbek Florida (April 10–13, 2005) and sponsored by the Brain Rehabilita-
University of Florida, Gainesville, FL tion Research Center, a Veterans Administration ( VA) Rehabilitation
Research and Development Center of Excellence. This article aims to en-
courage swallowing clinicians and researchers to partner with neu-
roscientists and imaging specialists in using animal models and advanced
S276 Journal of Speech, Language, and Hearing Research • Vol. 51 • S276–S300 • February 2008 • D American Speech-Language-Hearing Association
1092-4388/08/5101-S276
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
imaging techniques to further the swallowing rehabili- control during the early stage of the swallow may offer
tation evidence base. access to the patterned response. Given the sensorimotor
neuromuscular mechanisms of dysphagia and the crea-
tivity of clinicians, it is becoming clear that a multitude of
Background avenues may facilitate improved swallowing behavior
and outcomes. Advances in imaging methods will now per-
Speech pathologists are called upon tens of thou- mit understanding of the potential of these intervention
sands of times every day to improve swallowing in the techniques (and those yet to be developed) to promote
estimated 18 million adults suffering from dysphagia in adaptive neural plasticity.
the United States and many millions more internation-
ally. With such life-threatening conditions as malnutrition,
dehydration, and airway disease, including pneumonia,
among the health-related consequences of swallowing
Definition of Neural Plasticity
impairment, the urgency to provide care has elicited an Loosely defined, neural plasticity describes the abil-
enormous response from many professions in the health ity of the brain to change (Cohen et al., 1998). Central ner-
care industry. Speech-language pathologists have been vous system plasticity refers to the ability of neuronal
at the forefront of the clinical movement. However, as is systems to alter function in response to changes in input,
often the case in health care, clinical practices have out- both physiological and pathophysiological (Buonomano &
paced the science and evidence to support them (Langmore, Merzenich, 1998)—that is, change and adaptation in a
1995; Rosenbek, 1995). neural substrate, leading to associated behavioral changes,
Until relatively recently, swallowing had been viewed occur in response to training, environmental cues, experi-
as a sequence of pharyngeal and esophageal events, and ence, aging, injury, or disease (Tinazzi et al., 1998; Urasaki,
neural control was considered reflexive (Patten, 1977; Genmoto, Wada, Yokota, & Akamatsu, 2002; Ziemann
Walton, 1985). With this traditional assumption of re- et al., 1998). Change in synaptic function within a par-
flexive neurological substrates, few researchers or cli- ticular central neural substrate—either through synapto-
nicians were approaching dysphagia from a behavioral genesis, long-term potentiation, long-term suppression, or
point of view. Alternate modes of nutritional intake such cell death—comprises neural plasticity. During the last
as tube feedings were the remediation of choice in the two decades, a number of studies have revealed the mech-
medical setting until the past decade. With the 1980s anisms responsible for plasticity and their relationship
came a turning point, as behavioral, medical, or surgical with injury (Cohen et al., 1998); however, understanding
interventions emerged to modify the oropharyngeal bio- of neural plasticity and behavioral modeling or reshap-
mechanics of swallowing. The past 20 years have wit- ing remains unclear.
nessed an explosion in the diagnosis and treatment of Although neural plasticity may result in a behavioral
oropharyngeal swallowing disorders (Logemann, 1983; change, not all behavioral change necessarily involves
ECRI Report, 1999) and, in particular, what is now being neural plasticity. Some behavioral changes result from
referred to as the swallow response (Kahrilas, Dodds, Dent, compensation, involving a substitution or use of different
Logemann, & Shaker, 1988; Robbins, 1996). The integra- neural substrate(s) for producing a behavior or learning a
tion of volitional and reflexive sensorimotor events are of new function. More commonly, neural plasticity is the
great relevance, and work defining the functional neuro- alteration in function of the original neural substrate
anatomy of voluntary swallowing is emerging (Zald & used to produce a behavior through changes in synaptic
Pardo, 1999) for application to our current understanding function. At present, although there is increasing
and practice. evidence that neural plasticity plays a substantial role
A large-scale distributed swallowing neural network in centrally remodeling human function after cerebral
beginning to be elucidated (Robbins, 1999; Zald et al., injury, an understanding of how it relates both to path-
1999) supports previous suspicions of complex underlying ophysiology and functional recovery remains limited,
neural substrates, reflected in the term patterned swallow and its role in recovery of swallowing behavior is even
response (Kahrilas et al., 1988; Robbins, 1996; Robbins, less understood.
1999). Certainly behavioral (Shanahan, Logemann,
Rademaker, Pauloski, & Kahrilas, 1993; Rasley et al.,
1993) and sensory (Lazarus et al., 1993; Rosenbek, Roecker,
Wood, & Robbins, 1996) interventions aimed at modifi-
Principles of Neural Plasticity
cation of a patterned response have more treatment Ten principles of neural plasticity are identified by
potential than if aimed at a reflex! Such revolutionary Kleim and Jones (2008; this issue) as having emerged
conceptualization encourages clinicians who have been from two or more decades of research in basic neurosci-
hypothesizing, as reflected in their practices, that willful ence. These principles are evidenced in basic research
Robbins et al.: Neural Plasticity, Swallowing, and Dysphagia Rehabilitation S277
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
and are beginning their appearance in rehabilitation, and poses a threat to functional recovery in the long
most notably in upper limb and locomotion research. term. The clinical solutions are not transparent. It might
However, they have yet to be examined systematically in be hypothesized, however, that patients with oropharyn-
relation to human swallowing, although progress is being geal dysphagia and life-threatening aspiration should be
made. The 10 principles are summarized in the following offered systematic swallowing drills but without using a
subsections, each principle accompanied by reference to bolus. The goal would be to improve their swallowing
the extant swallowing literature where relevant and with skill, albeit only on “dry” or saliva swallows. Intuitively,
direction for future research where data are nonexistent. such activity—if it emphasizes multiple repetitions of
more immediate, stronger swallows—will help preserve
cortical and subcortical representations and make the pa-
Use It or Lose It tient’s return to oral nutrition easier and faster.
Numerous examples of this principle in humans Methodologies supported by Phase I and II evidence
exist, indicating that if a neural substrate is not bio- of effect on the peripheral swallowing mechanism, iden-
logically active, its function can degrade. As reviewed by tified by the Swallowing Work Group and discussed at
Ludlow et al. in a companion article (2008; this issue), length later in this review, are listed in Tables 1–4. The
Merzenich and colleagues in the 1980s demonstrated cited works are not all inclusive but rather are meant to
that following the loss of peripheral input to the sensory provide a representative sample of peer-reviewed re-
cortex from the hand, cortical somatosensory represen- search for specific therapeutic techniques. The imple-
tation was reduced (Kaas, Merzenich, & Killackey, 1983; mentation of a selected subset of these methods, which
Merzenich et al., 1983). Conversely, basic research has may be used during swallowing and even during the early
demonstrated that by increasing environmental input, period of NPO status, is critical to testing the applicabil-
cortical representation could be altered or enhanced ity of the Use It or Lose It principle. In addition to en-
(Nudo, Jenkins, & Merzenich, 1990). Studies addressing hancing understanding of practical applicability to dys-
methods of preventing cortical loss following peripheral phagia, it will invite not only documentation of behavioral
deafness are an example of relevance to human commu- plasticity, operationally defined as apparent change in
nication (Wong-Riley, Walsh, Leake-Jones, & Merzenich, task performance without clear evidence of associated
1981). Following brain injury, however, further cortical neural systems alteration(s), but also documentation of
loss can occur without training, as the movements formerly their influence on neural plasticity. This last notion brings
represented in the lesioned zone do not reappear in us to the obverse or guiding principle of neural plasticity—
adjacent cortical regions (Friel, Heddings, & Nudo, 2000; Use It and Improve It.
Nudo & Milliken, 1996). Failure to drive specific brain
function through training can lead to further degrada- Use It and Improve It
tion of a function (Kleim et al., 2002).
This second principle is an extension of the first
Swallowing clinicians recognize this principle; how-
principle, indicating that with increased biological
ever, tests of the principle remain to be performed. Some
data, however, are relevant. The necessity of swallowing
“warm-up times” in patients with neurogenic dysphagia Table 1. Sensory methods of swallowing intervention (i.e., sensory
or loss of the volitional swallowing motor patterns (Robbins modifications or stimulation used in swallowing treatment). Demonstrated
& Levine, 1993) in stroke patients who aspirate has been evidence of behavioral or neural plasticity (+) or the lack thereof (–)
reported. These patients not only receive nutrition through is noted. E-stim = electrical stimulation; DPNS = deep pharyngeal
alternative routes (e.g., tube feeding) for extended periods neuromuscular stimulation; trach = tracheostomy.
of time, but they expectorate their own saliva rather than
swallow. For years, and in many places to this day, the Behavioral Neural
assumption in the clinical swallowing community has been Bolus effects
that tube feeding is justified because it prevents prandial Volume + –
aspiration and thereby reduces the chance of aspiration Viscosity + –
pneumonia. Increasingly, clinicians are uneasy with nil per Temperature + –
os (NPO) status for at least two reasons. First, it is now Taste enhancement + –
recognized that aspiration is not alleviated by tube feed- Stimulation
ing (Cataldi-Betcher, Seltzer, Slocum, & Jones, 1983; Thermal-tactile stimulation + +
Langmore et al., 1998) in many circumstances. Second, the E-stim + +
clinical challenge posed by such patients when finally their DPNS – –
rehabilitation is attempted is explicable in light of the Use Occluding trach + –
It or Lose It principle. More specifically, disuse of the swal- Visual feedback + –
lowing mechanism may diminish its cortical representation
S278 Journal of Speech, Language, and Hearing Research • Vol. 51 • S276–S300 • February 2008
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
Table 2. Compensatory methods of swallowing intervention. Table 4. “Motor without swallow” methods of intervention (i.e.,
Demonstrated evidence of behavioral or neural plasticity (+) or methods of swallowing intervention that are defined as motor and
the lack thereof (–) is noted. do not include the act of swallowing). Demonstrated evidence of
behavioral or neural plasticity (+) or the lack thereof (–) is noted.
Intervention method Behavioral Neural
Intervention method Behavioral Neural
Chin tuck + –
Head rotation + – ROM + –
Head tilt + – Strengthening–tonguea + –
Head back – – Strengthening–respiratorya + –
Side lying + – Tongue control + –
Breath hold + – Shakera + –
Bolus consistency + – LSVTa + –
Pharyngeal exercisesa – –
Gargling – –
activity, future functioning is enhanced, especially if that Vocal exercises – –
activity involves skill training or what could be called Velar elevation – –
target practice. This principle contains at least one sub- Airway closure/breath hold + –
tlety. The object is not merely to use a function but rather Note. ROM = range of motion; LVST = Lee Silverman Voice Treatment.
to use a function with increasing competence, whether a
Workshop prioritized as potential for plasticity.
that competence is measured as efficiency or accuracy.
The point is that simply swallowing will not necessarily
improve swallowing by a person with dysphagia. Rather,
section. What is important to the Use It and Improve It
goals for improvement must be specified and perfor-
principle is to discover which of these methods, in which
mance adequacy evaluated. During the past decade, an
patients, has maximum effects on both behavioral and
emerging literature has demonstrated that training in
neural plasticity. At issue is whether strengthening
other abilities can lead to an enhancement of function
exercises change both behavioral and neural plasticity.
and the underlying neural mechanisms involved in that
Consider the recently popular approaches to muscle
behavior (Cohen et al., 1998; Nudo, 2003; Rioult-Pedotti,
strengthening, including expiratory muscle strength
Friedman, & Donoghue, 2000; Rioult-Pedotti, Friedman,
training (Saleem, Sapienza, & Okun, 2005), lingual
Hess, & Donoghue, 1998). What remains to be discovered
strength training (Robbins, Gangnon, Theis, Kays, &
is what methods for improving swallowing will have
Hind, 2005; Lazarus, Logemann, Huang, & Rademaker,
similar effects on behavioral and neural plasticity.
2003; Robbins, Kays, Gangnon, Hewitt, & Hind, 2007) and
Certainly a variety of methods, most notably those the head-raise exercise (Shaker et al., 1997). Although it
for strengthening the swallowing musculature, are gain- has been posited that strengthening exercises change
ing attention for diseases that affect various levels of the vascularity but not cortical or subcortical maps, skill
neuromuscular system. As will be obvious in subsequent training—such as that involved in the Mendelsohn
sections of this article, a variety of swallowing rehabil- maneuver—may change both. On the other hand, it stands
itation methods have emerged, primarily from the clinic to reason that stronger muscles provide the behavioral
rather than from the laboratory in the last two or so de- framework for increased skill. In this case, strengthen-
cades. A classification of these is proposed in a subsequent ing may lead to improved swallowing (and thus no other
treatment may be required) or to the establishment of
Table 3. “Motor with swallow” methods of intervention (i.e., methods greater potential for skills further refined with specific
of swallowing intervention that are defined as motor and include the swallowing exercises. The immediate lesson for the swal-
act of swallowing). Demonstrated evidence of behavioral or neural
lowing clinician, however, is that training—even the
plasticity (+) or the lack thereof (–) is noted.
training of a patient who is aspirating and at high risk for
pulmonary or other health consequences—appears pref-
Intervention method Behavioral Neural
erable to merely observing and documenting.
Mendelsohna + – Although effects of rehabilitation in the form of
Super supraglottic + – strengthening the swallowing mechanism are gaining
Supraglottic + – attention and clarity at the lower motor neuron and
Effortfula + – muscle level, rehabilitation strategies to address the
Tongue holda + –
neurologic underpinnings are less clear when weakness
Swallow (frequency) + –
is due to loss or absence of sufficient excitation input to
a
Workshop prioritized as potential for plasticity. the motor neurons to produce sustained discharge in
high-threshold motor units. Loss of a significant portion
Robbins et al.: Neural Plasticity, Swallowing, and Dysphagia Rehabilitation S279
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
of the cortex that provides excitation to the tongue motor cerebral mechanisms contribute to communication and
neurons, or an interruption of central pathways to these volitional swallowing, this remains an experimental ques-
motor neurons, will result in loss of maximal strength of tion to be tested carefully and systematically in the future.
the tongue. To be normally strong (with great implication
for normal speed), it takes more than strong muscles; Repetition Matters
firing sufficient motor neurons to the muscle is critical
(Luschei, 1991). A testable hypothesis is when a “nor- Neural substrates may be modified by extensive and
malized” motor pattern accompanies a stronger oral prolonged practice. Further, behavioral change is evi-
phase; the volitional oral events are “recognized” more denced before lasting neural changes (Kleim et al.,
readily and therefore trigger the pharyngeal swallow 2004). The work of Nudo et al. (Nudo, Wise, SiFuentes, &
response more efficiently. Such events may be a function Milliken, 1996), Kilgard and Merzenich (1998), and others
of neural plastic adaptation. For the execution of safe (Pascual-Leone et al., 1993) has shown the importance of
and effective swallowing to be understood and, more- repetition in inducing brain changes and maintaining such
over, restored if damaged, increased knowledge of the changes. From a clinical perspective, findings sug-
relationship of change with strengthening at all levels of gest a source of evidence to support the need for con-
the neuraxis will serve us well and is now achievable sistent practice to acquire and maintain an improved
with carefully designed systematic paradigms. swallow. Some evidence for the viability of this principle
in swallowing is available. As is discussed in subsequent
sections, methods requiring systematic repetition, such
Plasticity Is Experience Specific as the Lee Silverman Voice Treatment ( LSVT), isometric
lingual exercise, and the head-raise exercise, have in-
This principle, suggesting that changes may occur
fluenced swallowing behavior. Their influence on neural
only in the neural substrates involved in the particular
plasticity is to be established. If one accepts that no
behavior being trained (Kleim et al., 2002), is of rele-
behavior change is possible without nervous system
vance to swallowing rehabilitation. Deafferentation in
change, then it can be posited that the repetition in-
one modality has been shown to cause marked changes
volved in such methodology is key. Simple repetition,
in cortical representations of different sensory modalities
however, may not be enough. The number and duration
(Rauschecker, 1995). For example, these cross-modal
of repetitions are probably critical.
changes have been postulated to be the substrate of the
improved sound localization or tactile abilities of the blind.
Studies using neuroimaging and electrophysiological Intensity Matters
techniques have indicated that the occipital cortex of A nonlinear relationship between the intensity of
participants who became blind early in life is activated exercise-induced stimulation and the markers of neural
in association with tactile discrimination tasks such as plasticity (cortical representation, synaptogenesis, and
Braille reading (Sadato et al., 1996), whereas sighted in- behavioral representation) has been demonstrated. On
dividuals do not typically use the occipital cortex for iden- the one hand, there appears to be a threshold of intensity
tification of embossed Roman letters. Finding the occipital required to elicit neural changes (Luke, Allred, & Jones,
cortex is a critical functioning component of the network 2004; Lisman & Spruston, 2005; Peinemann et al., 2004),
involved in Braille reading supports the idea that per- yet there is the possibility of excitotoxicity with too great a
ceptions are dynamically determined by the character- level of stimulation (DeBow, McKenna, Kolb, & Colbourne,
istics of the sensory inputs rather than only by the brain 2004; Humm, Kozlowski, Bland, James, & Schallert, 1999;
region receiving those inputs (Pons, 1996; Rauschecker, Humm, Kozlowski, James, Gotts, & Schallert, 1998;
1995). These results indicate that cross-modal plasticity, Kozlowski, James, & Schallert, 1996; Risedal, Zeng, &
as identified electrophysiologically or by neuroimaging Johansson, 1999). The translation of this principle to
techniques in humans, plays a functionally compensatory human response deserves prioritization to optimize posi-
role (Cohen et al., 1998). tive outcomes and minimize negative effects, particularly
Although it has been hypothesized that training in with regard to specific populations suffering from neu-
swallowing, for instance, after stroke, induces changes rogenic dysphagia. Our data on intensity are limited.
in the neural network involved in swallowing (Martin et al., Evidence is building that the intensity of swallowing
2004) but might not alter function in other cortical regions therapy is important for swallowing rehabilitation (Teasell
involved in voice production (Huang, Carr, & Cao, 2002), & Kalra, 2005). However, training long does not necessar-
preliminary evidence challenging such a perspective ily imply training hard. Rosenbek and colleagues (Rosenbek
recently emerged—that is, in addition to improving vocal et al., 1996, 1998; Rosenbek, Robbins, Fishback, & Levine,
intensity, a vocal exercise was found to affect swallow kine- 1991) compared an average of 150, 300, 450, and approx-
matics and bolus flow (Sharkawi et al., 2002). Although the imately 540 trials per week of tactile thermal stimula-
authors predict that common modifications in underlying tion on swallowing in stroke patients; however, none of
S280 Journal of Speech, Language, and Hearing Research • Vol. 51 • S276–S300 • February 2008
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
the dosages (even the approximate 540 trials per week generalization of animal results to humans must be ap-
condition) emerged as the most therapeutic. Although proached with caution, pairing appropriate environmental
the investigation lacked sufficient power to provide strong stimuli (e.g., taste, smell) with rehabilitation efforts may
evidence for this intensity question, the work shows the have a positive influence on recovery.
future need for greater clarity in the dosing of dysphagia
therapies. Age Matters
This principle is especially important in all of
Younger nervous systems are more responsive to
speech-language pathology, where the treatment norm
training and adaptive neural plasticity than older ones.
is for patients to be provided with one, two, or three ses-
Nonetheless, neural plasticity does occur over the life
sions per week for a length of time more determined by
span, although outcomes are demonstrated to decrease
the limits of third-party pay than by data-driven treat-
with age (Kramer, Bherer, Colcombe, Dong, & Greenough,
ment decisions that examine time of treatment and
2004; Sawaki, Yaseen, Kopylev, & Cohen, 2003). Although
“rigor” or effort expended during that time. The evidence
minimal evidence is available relative to age-related
as cited here suggests that low-intensity treatment is un-
swallowing-specific neural plasticity, cortical representa-
likely to support maximum behavioral or neural plastic-
tions of swallowing in older adults show greater activa-
ity. The solutions are to discover the optimum intensity
tion in right motor, premotor, and prefrontal regions
for each treatment and then to work out delivery models
compared to young adults in association with swallowing
that allow achievement of that intensity.
water compared to saliva swallows. It has been hypoth-
esized that this overactivation may represent a neural
Time Matters compensatory response to the demands of swallowing
Protracted (rather than short) periods of training water in the face of age-related diminution of oral sensory
and continuous (rather than intermittent) training may motor function (Martin et al., 2004).
maximize neural change (Fisher & Sullivan, 2001). How-
ever, the time of intervention initiation postinjury often Transference
dictates the intensity of rehabilitation. Although there is
little doubt that facilitating safe and effective swallowing Transference is defined as “the ability of plasticity
early in recovery—for instance, poststroke—is appeal- within one set of neural circuits to promote concurrent or
ing and has been promoted as cost effective (Odderson, subsequent plasticity” (Kleim & Jones, 2008, p. S232). Ex-
Keaton, & McKenna, 1995), comorbidities often preclude amples of the principle include evidence from skill learn-
early implementation of single interventions that are ing and transcranial magnetic stimulation ( TMS) of
hypothesized as most likely to access neural plastic adap- changes in cortical excitability and size of cortical rep-
tations. To maximize swallowing rehabilitation with this resentations of body structure in the cortex. Evidence of
specific principle in mind, pairing compensatory strategies transference in swallowing has been provided primarily
with those that access neural adaptation early in recovery by data on the influence of electrical stimulation of the
versus later may be a fruitful area of future investigation. pharynx on cortical swallowing center excitability and
map size and locus (Fraser et al., 2003; Hamdy et al., 1996,
1997b, 2003; Hamdy, Rothwell, Aziz, Singh, & Thompson,
Salience Matters
1998; Fraser et al., 2002). Detailed discussion of the
As Ludlow et al. (2008) point out in motor speech findings appears later.
(see article in this issue), it has been promoted that sim- In general, the reported experimentation does not
ple repetitive movements or strength training likely do pair peripheral sensory stimulation with skill training.
not enhance skilled movement and induce changes in It is conceivable that transference would be enhanced by
neural function. Rather, neural plasticity is best induced the pairing of peripheral stimulation and skill training
when the movement is purposeful and related to the be- as demonstrated for other primarily motor deficits in
havior being trained (Morgen et al., 2004; Plautz, animals (Plautz et al., 2003) or by cortical electrical stim-
Milliken, & Nudo, 2000; Remple, Bruneau, VandenBerg, ulation and skill training. A testable hypothesis is that
Goertzen, & Kleim, 2001). On the other hand, the prin- transference resulting from sensory stimulation alone
ciple that salience is important to swallowing may be is inadequate to cause maximum functional change in
distinct. Learning has been shown to be as related to the swallowing and that combined stimulation and skill
behavioral importance of the stimulus as it is to the learning is critical.
frequency of occurrence, so a stimulus that is relevant to
the organism ( location of food) may be learned in a single
trial. Marking the importance of a stimulus with input
Interference
from more basic neural structures is facilitative of func- Interference refers to “the ability of plasticity within
tional reorganization (Kilgard et al., 1998). Although a given neural circuitry to impede the induction of new, or
Robbins et al.: Neural Plasticity, Swallowing, and Dysphagia Rehabilitation S281
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
during transient sensory deprivation: A preliminary study. Ziemann, U., Hallett, M., & Cohen, L. G. (1998). Mecha-
Journal of Clinical Neurophysiology, 19, 219–231. nisms of deafferentation-induced plasticity in human motor
Walton, J. N. (1985). Brain’s disease of the nervous system. cortex. Journal of Neuroscience, 18, 7000–7007.
Oxford, England: Oxford University Press.
Welch, M., Logemann, J. A., Rademaker, A. W., Pauloski, Received February 10, 2006
B. R., & Kahrilas, P. J. (1993). Changes in pharyngeal
Accepted August 2, 2007
dimensions affected by chin tuck. Archives of Physical
Medicine and Rehabilitation, 74, 178–181. DOI: 10.1044/1092-4388(2008/021)
Wong-Riley, M. T., Walsh, S. M., Leake-Jones, P. A., & Contact author: JoAnne Robbins, VAMC GRECC 11G,
Merzenich, M. M. (1981). Maintenance of neuronal activity 2500 Overlook Terrace, Madison, WI 53705.
by electrical stimulation of unilaterally deafened cats E-mail: jrobbin2@wisc.edu.
demonstrable with cytochrome oxidase technique. Annals
Susan Langmore is now with the Department of Otolaryngology–
of Otology, Rhinology & Laryngology, 90, 30–32.
Head and Neck Surgery and the Department of Speech
Zald, D. H., & Pardo, J. V. (1999). The functional neuro- and Hearing Sciences, Boston University.
anatomy of voluntary swallowing. Annals of Neurology, 46,
281–286.
Robbins et al.: Neural Plasticity, Swallowing, and Dysphagia Rehabilitation S297
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
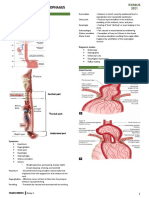
the volitional and automatic activities involved in swallow- interventions is derived primarily from Phase I and
ing. More specifically, the neural control of swallowing Phase II (Robey & Schultz, 1998) data reported in single
involves five major components: (a) afferent sensory fibers case designs and usually relatively small nonrandomized
contained in cranial nerves, ( b) cerebral and midbrain group designs. Unfortunately, these limitations reflect
fibers that synapse with the brain stem swallowing what meager information is available currently in this
centers, (c) paired swallowing centers in the brain stem, young field of dysphagia rehabilitation. Specifically,
(d) efferent motor fibers contained in cranial nerves and Phase I and II studies seek to determine the effect of
the ansa cervicalis, and (e) muscle end organs. For more an intervention. Phase I studies prove a response to the
detailed reviews of neural control processes, see work by treatment and establish the safety of the treatment.
Cot and McFarland (1996), Jean (2001), and Martin, Phase II studies extend the hypotheses of the Phase I
Goodyear, Gati, and Menon (2002). study and seek to determine dosing, protocol, and treat-
Much research attention has been given to identi- ment populations. It is not until a Phase III study that
fying and characterizing the brain stem pattern generat- treatment efficacy is studied through the use of ran-
ing circuitry responsible for the basic swallowing pattern domized controlled groups and/or cross-over designs with
(Jean, 2001; McFarland & Lund, 1995). For a detailed significant sample sizes (Ashford, McCabe, & Musson,
discussion of “reflexes” of the oral, pharyngeal, and laryn- 2005). Randomized clinical trials are small in number,
geal regions, see work by Arthur Miller (1999). Similar to with reports of larger studies only now emerging in the
breathing, chewing, and walking, interneurons have been literature (Brandt et al., 2006; Logemann et al., 2008;
identified in the brain stem that can generate a basic Robbins, Gensler, et al., 2007).
swallowing pattern in the absence of ascending (sensory)
or descending (cortical) inputs. These neural networks Sensory
are referred to as central pattern generators (CPGs). The
There is ample evidence to suggest that swallowing
swallowing CPG is sometimes erroneously interpreted
is not a static, unchanging event. All aspects of oropha-
as containing all of the neural circuitry necessary for the
ryngeal swallowing have been found to be modifiable
generation of the swallowing “reflex” or the currently
with varying sensory input. Bolus characteristics, in-
accepted term “swallow response” (i.e., the pharyngeal
cluding volume, viscosity, and taste, have been shown to
phase of swallowing). More recently, they are being
modify the timing, strength, and extent of the muscle
conceptualized as flexibly organized neural networks
activity for normal swallowing. Similarly, stimulation of
with multifunctional neurons that are biased to produce
structures with thermal, tactile, gustatory, and electri-
task-specific motor behaviors (Jean, 2001; Charbonneau,
cal stimulation have also been used with an intended
Lund, & McFarland, 2005). This flexible organization
goal of reducing thresholds of response. With these shifts
underlies not only the coordinated activity within the
in muscular and structural movement, bolus flow through
swallowing system but the cross-system coordination
the oropharynx has been found to shift, as well.
with respiratory and laryngeal systems, as well.
Understanding the underlying neural control param-
eters is crucial if we are to be able to properly diagnose
Bolus Effects
and treat swallowing disorders. The principles of neural Volume. Several aspects of oral and pharyngeal
plasticity provide a theoretical and practical framework swallowing are altered with bolus volume, including
to explore and determine optimal treatment parameters timing and extent of structural movement, duration of
for dysphagia rehabilitation. While elucidating linkages laryngeal vestibule closure, anterior and superior hyo-
between cerebral plasticity, brain stem plasticity, and laryngeal movement, upper esophageal sphincter ( UES)
behavioral plasticity, integration of the clinical and opening, base of tongue to posterior pharyngeal wall ap-
scientific literature in a translational context follows. proximation, and respiration cessation during swallow-
ing change with bolus volume (Dantas et al., 1990; Hiss,
Strauss, Treole, Stuart, & Boutilier, 2004; Logemann et al.,
The Interventions 1992). The extent of pharyngeal structural movement
has been found to increase with bolus volume, including
When standard practice and literature in the field increased extent of vertical and anterior hyoid and la-
of dysphagia were reviewed by the Swallowing Work ryngeal movement, superior upper esophageal sphincter
Group, it was decided that a pattern emerged as rep- movement, and width of UES opening (Jacob, Kahrilas,
resented in Tables 1–4, and behavioral swallow treat- Logemann, Shah, & Ha, 1989). Increases in lingual,
ments were identified and placed in categories including submental, and laryngeal muscle activity also have been
(a) Sensory; ( b) Compensatory; (c) Motor With Swal- found with increasing bolus volume (Cook et al., 1989;
low; and (d) Motor Without Swallow. Support of neural Jacob et al., 1989; Miller & Watkin, 1996; Perlman, Palmer,
plastic changes in response to a variety of swallowing McCulloch, & Vandaele, 1999; Shaker, Cook, Dodds, &
Robbins et al.: Neural Plasticity, Swallowing, and Dysphagia Rehabilitation S283
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
Hogan, 1988). Finally, bolus flow is altered with an the swallow with altered bolus-specific sensory input,
increase in intrabolus pressure, and bolus velocity is neural plasticity may play a role in these changes. Fol-
altered through the UES with increasing bolus volume lowing such studies, carefully controlled, thoughtful
(Jacob et al., 1989). investigations implementing validated measures and
Viscosity. Modifying bolus viscosity also alters as- methodologies are needed in this important area. In-
pects of both the oral and pharyngeal components of vestigations that examine the potential role of altered
swallowing, including systematic changes in lingual, sensory input provided by the bolus on neural plastic
submental, and hyo-laryngeal muscle activity (Dantas & changes at the cortical, subcortical, and /or brain stem
Dodds, 1990; Jacob et al., 1989; Miller & Watkin, 1996; levels, and whether those changes provide desired be-
Palmer, Rudin, Lara, & Crompton, 1992; Perlman et al., haviors, will be most informative.
1999; Pouderoux & Kahrilas, 1995; Reimers-Neils,
Logemann, & Larson, 1994; Shaker et al., 1988; Takahashi
& Nakazawa, 1991). A systematic increase in extent of
Stimulation and Plasticity
vertical and anterior hyoid and laryngeal motion and In the late 1990s, Hamdy and colleagues (1996) con-
width of UES opening during swallowing has been found ducted a series of studies using TMS. They concluded
relative to viscosity independent of volume (Dantas et al., that dysphagia secondary to cortical lesion results when
1990). Temporal changes include increased duration of the hypothesized swallowing-dominant hemisphere is
laryngeal vestibule closure, increased duration of UES affected, and recovery occurs as an accompaniment to an
opening during swallowing, and a later initiation of the expansion of cortical swallowing areas in the nondamaged
swallow apneic period relative to propulsion of the bolus hemisphere. They subsequently confirmed the relation-
with increased bolus viscosity (Dantas & Dodds, 1990; ship of the dominant pharyngeal region to the presence or
Dantas et al., 1990; Hiss et al., 2004; Lazarus et al., 1993; absence of dysphagia following cortical stroke (Hamdy,
Robbins, Hamilton, Lof, & Kempster, 1992). Aziz, Rothwell, Crone, et al., 1997). Hamdy and Rothwell
Thermal, taste, tactile. The effects of taste on swal- (1998) observed that “swallowing might be an excellent
lowing have not been studied extensively in humans. system for studying cortical plasticity” ( p. 278). They
However, current data do support shifts in both the oral also echoed Diamant (1996) by observing that their
and pharyngeal components of swallowing with bolus findings “might prove useful in the development of new
tastes. Specifically, sour has been found to result in ear- therapies aimed at accelerating reorganization in the
lier onset of lingual activity to propel a bolus into the undamaged hemisphere after unilateral cerebral injury”
pharynx, faster triggering of the pharyngeal motor re- (Hamdy & Rothwell, 1998, p. 278).
sponse, and a shorter pharyngeal component of the swallow Support of transcutaneous electrical muscle stimu-
in patients subsequent to stroke or mixed neurologic lation as a method to promote increased neural connec-
etiologies (Logemann, Pauloski, Colangelo, Lazarus, & tions important to swallowing (Humbert et al., 2006;
Fujiu, 1995; Pelletier & Lawless, 2003). These authors Ludlow et al., 2007) is sparse. Nonetheless, Hamdy and
attributed the temporal shifts with the sour bolus to the his group (1998) demonstrated that a specific frequency
possible sensory alerting stimulus to the brain stem and of 5 Hz of electrical stimulation applied directly to
cortical swallowing centers. Although bolus temperature pharyngeal mucosa effectively altered the size of cortical
has not been found to result in changes in swallow phys- motor maps for the pharynx bilaterally but asymmetri-
iology alone (Bisch, Logemann, Rademaker, Kahrilas, & cally. Expansion was in an anterolateral direction and
Lazarus, 1994), work with carbonated boluses claims to appeared to come at the expense of esophageal represen-
improve the oropharyngeal swallow by shortening the tation, which decreased. A similar pattern was observed
pharyngeal component, reducing the amount of residue for cortical excitability, another measure of plasticity in
(i.e., improving clearance), and reducing aspiration (Bulow, response to treatment. In a follow-up study, Fraser and
Olsson, & Ekberg, 2003). However, careful review of the colleagues (2002) demonstrated that 10 min of 5 Hz
methodology behind these claims reveals flaws, and future direct pharyngeal mucosal stimulation at 75% of max-
carefully designed controlled studies are necessary in imum tolerated intensity positively influenced cortical
order to clarify the translational value of carbonation excitability, size of pharyngeal area, and swallowing
into practice. function, including penetration and aspiration events at
In summary, as evidenced with temporospatial anal- 1 hr poststimulation. Changes were greatest in the un-
yses obtained from videofluoroscopic recordings, there affected hemisphere in participants with acute-onset,
are systematic shifts in oropharyngeal kinematics and hemispheric stroke. Although these studies appear to
bolus flow that occur with specific sensory input from support a plastic response to specific sensory stimulation
the bolus in both normal and neurologically impaired of select muscle groups in the form of electrical stimula-
swallows. Although few studies have incorporated im- tion, replication of this work has been difficult, and until
aging technology to document cortical changes during confirmed, findings must be interpreted with caution.
S284 Journal of Speech, Language, and Hearing Research • Vol. 51 • S276–S300 • February 2008
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
The use of supplemental stimulation of the faucial & Kahrilas, 1994; Ohmae, Ogura, Kitahara, Karaho, &
arches with cold and pressure have shown shifts, includ- Inouye, 1998; Rasley et al., 1993; Shanahan et al., 1993;
ing faster initiation of lingual activity, improved trigger- Welch, Logemann, Rademaker, Pauloski, & Kahrilas,
ing of the pharyngeal motor response, and faster speed of 1993). It was determined that this category of treat-
swallowing (Hamdy et al., 2003; Lazzara, Lazarus, & ments would not be an ideal initial testing ground for
Logemann, 1986; Rosenbek et al., 1996). Further, me- neural plasticity. However, the utility of such treatments
chanical stimulation to the base of the faucial arch (i.e., as a component of a comprehensive swallowing program,
glossopharyngeal) region has been found to result in which includes securing safe swallowing status as a foun-
electrophysiologic changes within the cortex in humans, dation on which to superimpose sensory and motor inter-
indicative of polysynaptic connections and possible in- ventions, is of great interest. Their role in facilitating
volvement of suprabulbar structures (Fujiu, Toleikis, neural plastic adaptation in response to a comprehensive
Logemann, & Larson, 1994). swallowing program warrants examination.
Despite these data suggesting neural plastic changes
in response to stimulation, the matter is not so simple.
Some nervous system changes can be associated with
Motor With Swallow
degraded behavior, and some changes in brain represen- Motor exercises accomplished during swallows are
tation are unaccompanied by behavioral changes. The used to reduce the deficiencies within the swallow pat-
Manchester group (Power et al., 2004) has demonstrated tern itself. Their use is predicated on the assumption
all three conditions. They applied 10 min of electrical that changes in muscle strength, range of motion, and
stimulation to the faucial pillars at 0.2, 1, and 5 Hz. coordination will occur in response to specific exercises
Their prediction of central ( hemispheric) and peripheral that increase the effort, duration, and force of muscle
(improved swallowing) effects from 5 Hz stimulation was patterns. Although strength and range of motion changes
not confirmed. Indeed, 5 Hz stimulation inhibited the traditionally are considered peripheral via musculo-
cortical response and slowed the swallow. Reduced spinal pathways that innervate the limb musculature,
stimulation (i.e., 0.2 Hz) facilitated the cortical response bulbar innervated structures differ. Additionally, the
but had no influence on the swallow. They point out that increases seen in coordination may be fertile ground for
this study was with healthy participants, and different the investigation of neural plasticity.
results may have been found in patients with stroke. The “motor with swallow” category comprises swal-
Nonetheless, the lessons from this study are important. low maneuvers (see Table 3), including Mendelsohn,
A sensory treatment’s intensity may have indifferent, supraglottic swallow, super supraglottic swallow, effort-
therapeutic, or contratherapeutic effects, depending on ful swallow, tongue hold, and double swallow. To date,
site of application. In addition, all changes in the nervous all of these techniques have some evidence of behavioral
system may not be accompanied by a behavior change. plasticity but not neural plasticity. Volitional modula-
Although these are not revolutionary findings, they are tion of specific biomechanical components of swallowing
unique in swallowing rehabilitation. occurs during implementation of these techniques.
Specifically, the extent and duration of UES opening
Compensatory has been identified with the Mendelsohn maneuver (Ding,
Larson, & Rademaker, 2002; Kahrilas, Logemann, Krugler,
Compensatory interventions are used in the treat- & Flanagan, 1991). The supraglottic swallow and super
ment of dysphagia to compensate for structural and phys- supraglottic swallows are designed to facilitate the
iologic deficits. They include alterations in diet consistency timing and extent of laryngeal closure at specific levels
or positioning. These treatment techniques exploit re- of the larynx. The effortful swallow is designed to in-
tained abilities, and the majority of these techniques crease base-of-tongue retraction and results in increased
seek to alter the circumstances of the swallow instead of tongue propulsive force (Pouderoux & Kahrilas, 1995);
the swallow patterns themselves. In this sense, compen- increased oral pressure, duration, and extent of hyoid
satory interventions are behavioral with anticipated movement and laryngeal vestibule closure (Hind et al.,
temporary effect, and, when used alone, generally are 2001); and longer duration of pharyngeal pressure and
not believed to modify neural plastic underpinnings as a UES relaxation (Hiss & Huckabee, 2005). The tongue-
treatment outcome. hold maneuver increases anterior motion of the poste-
The postural techniques comprising the “compen- rior pharyngeal wall at the level of the tongue base
satory” category were identified by the Swallowing Work (Fujiu & Logemann, 1996). Different maneuvers may
Group as having evidence in support of behavioral plas- produce similar biomechanical effects as evidenced by
ticity but not neural plasticity (see Table 2). These tech- increased tongue base–pharyngeal wall pressures and
niques included chin tuck, head rotation, head tilt, head contact duration when performing the effortful swallow,
back, and side lying (Logemann, Rademaker, Pauloski, tongue-hold, Mendelsohn, and super supraglottic swallow
Robbins et al.: Neural Plasticity, Swallowing, and Dysphagia Rehabilitation S285
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
maneuvers (Lazarus, Logemann, Song, Rademaker, & Lingual Exercise
Kahrilas, 2002).
Behavioral plasticity of swallowing can occur as the
This “motor with swallow” category of techniques
result of lingual exercising. Lazarus and colleagues
centers on the principles of experience-dependent neural
reported that lingual strength increased as a result of
plasticity as presented by Kleim and Jones (2008; this
nonswallowing strengthening exercises (Lazarus et al.,
issue) and warrants investigative prioritization in elu-
2003). Robbins and her group not only demonstrated
cidating the translation of basic principles to the clinic.
that the lingual muscles have a propensity for increasing
Most notable among these are the principles of Use It or
strength and mass, but they also demonstrated that as
Lose It, Use It and Improve It, and Repetition Matters.
a result of nonswallowing exercising, improvement in
All of these techniques are used during the swallow with
swallowing pressures on liquid boluses occurred, Pene-
the goal of increasing the success of the swallow itself. As
tration Aspiration Scores were reduced (Robbins et al.,
previously noted, this may result in the preservation of
2005; Robbins, Kays, et al., 2007), and dysphagia-specific
synapses and the maintenance of allocated cortical rep-
quality of life improved ( McHorney et al., 2000). Thus,
resentation (Kleim, Barbay, & Nudo, 1998; Nudo et al.,
swallowing ability improved because of lingual resistance
1996; Perier, Buyse, Lechat, & Stenuit, 1986; Reale,
training in this cohort, a subgroup of whom demon-
Brugge, & Chan, 1987).
strated improvements in speech as well. Lingual strength-
ening regimens are currently underway with combined
Motor Without Swallow systematic data collection of cerebral hemodynamic re-
sponse to explore exercise-induced neural plasticity during
The “motor without swallow” category (see Table 4)
swallowing recovery (Kays et al., 2007).
includes exercises to improve range of motion and
strengthening (lingual, velar, pharyngeal, laryngeal [non-
speech and speech], and respiratory). Nonswallowing Head-Lifting Exercise
exercising of the oral, pharyngeal, laryngeal, and re- Behavioral plasticity of swallowing apparently
spiratory (i.e., swallowing) musculature holds a great occurs as the result of completing a head-lifting exercise.
deal of promise in treating individuals with severe dys- Shaker and colleagues observed adults, including a small
phagia. Nonswallowing exercising allows patients to number of patients dependent on tube feeding, who com-
progress through a training regimen safely without pleted a regimen of head-lifting exercises and experienced
limitations that may be imposed if the swallowing of increased laryngeal anterior excursion and cross-sectional
boluses is necessary for functional gain. However, at opening of the UES (Shaker et al., 1997). In addition,
least three questions exist relative to nonswallowing improved swallowing function was reported, with de-
exercising (i.e., strength training). First, does swallow- creased postswallow aspiration and an ability to return
ing musculature increase in muscle strength and tone to various levels of oral intake (Shaker et al., 2002).
as a function of resistance exercising? Second, does in- Replication of these studies will determine their trans-
creased muscle strength and tone translate into im- lational value and, if validated, may be paired with ex-
proved function? Third, what are the neural underpinnings perimental methods to explore accompanying neural
of change in function as a result of increased strength plastic modulation.
and tone?
One of the premises of neural plasticity is it oc- LSVT
curs with experience-specific conditions. Thus, the role
of isometric exercising appears equivocal—that is, an Recently, behavioral plasticity of swallowing has
experience-specific condition to improve swallowing neu- been shown to occur as the result of exaggerated respira-
rally would be swallowing. However, evidence exists tory, laryngeal, and articulatory exercising. In Parkinson’s
that some of the swallowing musculature has a propen- patients, Sharkawi et al. (2002) observed that oral transit
sity for increasing muscle strength / tone with nonswal- time, pharyngeal transit time, and vallecular residue
low exercising (e.g., resistance exercise), and increased decreased following completion of 1 month of LSVT
strength/tone translates into improved function (i.e., be- (Sharkawi et al., 2002). Another form of nonswallowing
havioral plasticity; Robbins et al., 2005, 2007). Although respiratory training has been found to improve swallow-
neural plasticity as a function of nonswallowing exer- ing in patients with normal swallow, with improved hyoid
cising has not been studied, it is highly plausible that motion and improved bolus clearance through the pharynx
neural plastic changes occur in the presence of behav- (Sapienza & Wheeler, 2006). LSVT and lingual strength-
ioral plasticity. Behavioral plasticity of swallowing has ening are examples of nonswallowing exercises that may
been demonstrated from three different nonswallowing provide evidence of neural plastic transference.
exercising techniques: lingual exercising, head lifting, In summary, motor exercises without swallow have
and LSVT. been shown to increase range of motion and strength in
S286 Journal of Speech, Language, and Hearing Research • Vol. 51 • S276–S300 • February 2008
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
those muscles used for swallowing, to improve the application to the numerous elders with dysphagia who
swallow itself, and to demonstrate associated behavioral are rapidly increasing in numbers in this country. The
plasticity. Indeed, transference is a principle of neural argument that clinical needs outpace evidence-based re-
plasticity that has been evidenced. Various combina- search is true. Nonetheless, an organized, carefully planned
tions of motor exercises with and without swallowing approach to patient care can integrate well-controlled
should be studied to ascertain the parts that each plays studies, attending to both the needs of the patients and
in swallow recovery as a result of neural plasticity. the clinician’s immediate need for answers—that is,
future studies addressing the principles outlined in the
companion paper by Kleim and Jones (2008; this issue)—
Evidence of Plasticity who to treat, at what intensity, how many repeti-
tions, when to initiate interventions in the course of the
Principles of neural plasticity have been presented disease—will improve the clinician’s ability to effect sig-
and discussed in relationship to dysphagia treatments nificant and long-lasting improvement.
(see Table 5). Establishing the evidence for these re-
lationships and how to optimize them for better patient
care warrants a major focus and hopefully will drive Neural
continuing evolution of this young field.
Many of the neural plasticity principles provided and
reviewed by Kleim and Jones (2008) are of high clinical
Behavioral relevance to swallowing rehabilitation and are just be-
Evidence of behavioral plasticity is abundant in the ginning to be explored in focused areas (as evidenced by
available swallowing literature to date. Such a strong “+” in Table 1), including two modes of sensory stim-
focus most likely relates to the critical need for func- ulation: thermal tactile and electrical stimulation (Fujiu
tional outcomes assessment of patients being treated. et al., 1994; Power et al., 2004). The challenges that lie
Documentation of the kinematic relationship of the ahead are many: Do training paradigms that are shown
14 physiologic components and the bolus flow outcomes effective in limb striated musculature pertain to cranio-
(i.e., direction, duration, and clearance) now is often facial bulbar and respiratory mechanisms? Does oromo-
obtained due to commonly available instrumentation to tor strength training transfer beyond the level of the
do so (e.g., videofluoroscopy). Also, the critical and time- muscle to facilitate improved swallowing? Can geriatric
sensitive need to identify a safe and effective swallowing adults relearn the automatic swallowing pattern estab-
regimen to prevent or minimize life-threatening changes lished in childhood?
in health status warrants the “quick fix” that compensa- The concept of neural plasticity tempts a reasonable
tory interventions often provide. However, these immedi- speculation that stimulation of one sensorimotor system
ately executable interventions (e.g., postural adjustment) may not only result in positive neural plastic changes in
appear to have no long-lasting effects, must be imple- the brain but also may cause detrimental changes to re-
mented for each swallow, and may diminish the pleasure lated sensorimotor systems. There is sparse but emerging
associated with dining. Further, the contributions reported evidence pointing to corollary influences of one sensori-
in the literature comprise small cohorts, many of which motor system on another, and these corollary influences
are normal, young, or heterogeneous and have limited in a rehabilitative setting are thought to augment the
Table 5. Principles of neural plasticity that relate to swallowing treatments. (+) indicates that the principle applies (not necessarily in a positive
manner; e.g., transference); (–) indicates that the principle does not apply; (?) indicates unknown.
Sensory methods Sensory methods
Principle bolus effects stimulation Compensatory Motor with swallow Motor without swallow
Use it or lose it + + + + +
Use it and improve it + + + + +
Specificity + + + + +
Repetition matters + + + + +
Intensity matters + + + + +
Time matters ? ? + + +
Salience matters + + + + –
Age matters + + + + +
Transference + + + + +
Interference + + ? – +
Robbins et al.: Neural Plasticity, Swallowing, and Dysphagia Rehabilitation S287
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
therapeutic result. However, there exists a logical pos-
sibility that the opposite may be true in a system that is a Needs for Translational Research
functional agonist to the target system. Neurophysiologic in Swallowing and Dysphagia
studies of breathing and swallowing activity have dem-
Figure 2 emerged from the Swallowing Work Group
onstrated evidence for influential swallow behavior on
representing translational research as an interactive
the otherwise resilient respiratory central pattern gen-
process between basic translational studies and feasi-
erator (CPG). Airflow and kinematic data support the
bility studies.
hypothesis that swallowing activity results in respiratory
phase resetting by the respiratory CPG (Charbonneau
et al., 2005; Feroah, Forster, Fuentes, Lang, et al., 2002; Basic Research
Paydarfar, Gilbert, Poppel, & Nassab, 1995). Further,
Animal models. Translational research using ani-
patient instructions and peripheral modulations of swal-
mal models has not been fully developed in the research
lowing (bolus, volumes, method of intake) appear to dif-
of swallowing rehabilitation. Identifying animal models
ferentially impact respiratory activity (apnea duration,
for the purpose of studying effects of swallowing treat-
respiratory phase) surrounding the swallow (Martin-
ment would advance the field’s swallowing rehabilita-
Harris et al., 2005; Dozier, Brodsky, Michel, Walters Jr.,
tion research much more expeditiously than relying on
& Martin-Harris, 2006). Given the proximity of the
human research alone. The group agreed that the search
central respiratory, cardiac, and swallowing central neu-
for appropriate animal models and their validation should
rons in the medulla, and the common pathways that
be conducted simultaneously with human studies.
mediate these functions at the periphery (i.e., vagus
nerve), it is not surprising that tachycardia and arrhyth- A primary variable that limits statistically adequate
mias have also been recorded in patients attempting numbers in research is heterogeneity of the sample
swallowing rehabilitation maneuvers and exercises that studied. For example, it is difficult to assess the effects of
require alteration of the cardiopulmonary dynamics, a given swallowing treatment in individuals poststroke
such as the effortful breath hold or valsalva (Chaudhuri because the locations and sizes of the infarcts vary tre-
et al., 2002). Negative influences on swallowing behavior mendously and, subsequently, sample size suffers. In
also have resulted in tandem with positive treatment contrast, an animal model can be uniformly cortically
effects of botulinum toxin injections into the intrinsic “lesioned” to produce dysphagia, providing a relatively
laryngeal musculature (Ludlow et al., 2007). Although homogeneous sample.
the latter studies represent less compelling evidence for The field of physical therapy has already teamed
true central reorganization, the possibility of negative with neuroscientists to incorporate the use of animal
effects on a sensorimotor system related to the target models in investigating neural plasticity following cor-
must be considered, observed, and, ideally, controlled tical lesions impairing limb mobility. Researchers have
during rehabilitation efforts. For now, we reviewed each demonstrated that in the rat model, variables of repe-
principle and the current knowledge base that may trans- tition, intensity, and time postlesion do matter in the re-
late to swallowing rehabilitation. The remainder of this habilitation of limb movement following lesion. Through
article addresses strategic approaches to the translation sacrificing rats during various stages of rehabilitation,
of the principles of neural plasticity into feasibility stud- physical therapy has enabled researchers to learn that
ies on dysphagia rehabilitation. skilled movement training is superior to nonskilled
Figure 2. Translational research represented as an interactive process among basic, feasibility, and
translational studies. CVA = cerebral vascular accident.
S288 Journal of Speech, Language, and Hearing Research • Vol. 51 • S276–S300 • February 2008
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
exercise in yielding new, multiple synapses (Remple et al., anatomy and physiology have used varying animal mod-
2001). Functional and neural plasticity has been repeat- els, as no single model has been deemed optimal. Sheep,
edly demonstrated in other similar rat models for skilled goats, pigs, and cats have been used to investigate swallow-
versus nonskilled motor tasks, as evidenced by synapto- ing and respiration coordination (Connelly, Dobbins, &
genesis and increased corresponding cortical representa- Feldman, 1992; Feldman, Loewy, & Speck, 1985; Feroah,
tion (Kleim et al., 2002; Kleim, Lussnig, Schwarz, Comery, Forster, Fuentes, Wenninger, et al., 2002; German,
& Greenough, 1996). Crompton, & Thexton, 1998; Jiang & Shen, 1991; Miller
An obstacle in using an animal model for swallowing & Loizzi, 1974; Miller & Sherrington, 1916; Reix, Arsenault,
research is the difference demonstrated at the func- Langlois, Niyonsenga, & Praud, 2004). Dogs have been
tional and biochemical level between humans and vary- used extensively for laryngeal research (Broniatowski,
ing species of animals. One concern is that presumably, Dessoffy, Shields, & Strome, 1999; Koizumi, Kogo, &
animals project the bolus from the oral cavity to the esoph- Matsuya, 1996; Sant’Ambrogio, Sant’Ambrogio, & Matthew,
agus with “less complex” pharyngeal involvement than 1986) and surgical outcomes research (Sasaki, Koe, &
humans. However, similar functional and biochemical Albert, 2001). Rabbits, piglets, and cats have been used
obstacles exist for using animal models in limb research. for oral, masticatory functioning (German, Crompton,
Thus, although an animal may not be identified with Owerkowicz, & Thexton, 2004; Meng, Uchida, Sato,
Yamamura, & Yamada, 1999; Miyaoka, Inoue, Shimada, &
identical anatomy and functioning compared with the
Yamada, 1998; Hiiemae & Crompton, 1985) and pha-
human, the animal model, nonetheless, allows for strong
ryngeal research (Fukushima et al., 2003; Miyaoka,
research design and statistical answers to neural and
Kyuhachiro, & Yamada, 1997). Neurophysiologically, the
behavioral underpinnings of swallowing rehabilitation.
sheep, cat, and rat have been used extensively.
There are many issues in swallowing disorders that
A major element of human clinical recovery not ad-
may benefit from animal model research. For example,
dressed in most animal studies is rehabilitation. Although
little is understood about surface electrical stimulation
animal studies currently may not replicate important
of the skin overlying the submental musculature and
aspects of human rehabilitation and recovery, they do
throat in dysphagia (also known as neuromuscular
suggest directions for human study and offer opportu-
electrical stimulation). The appropriate site(s), stimula-
nities for fruitful collaboration. An alternative is to in-
tion frequency, amplitude, phase duration, optimal fre-
corporate even more simple animal models. For example,
quency, and length of an individual stimulation treatment
Aplysia—snails that are approximately 5 in. long—are
and potential effects are unknown.
capable of operant conditioning despite their lower order
The Use It or Lose It principle may be refined by and have been used to learn about neuronal function and
performing controlled studies on animals. Many acute or sensory motor integration (Lum, Zhurov, Cropper, Weiss,
chronically ill patients develop dysphagia in the absence & Brezina, 2005). Such organisms are experimentally ad-
of an identifiable neurologic, metabolic, or mechanical vantageous because the relationship between feeding be-
etiology. Researchers may be able to use animal models haviors and neuronal adaptation can be more direct (i.e.,
to study the neural substrates of animals receiving nutri- food or nonfood). More basic animal models may not only
tion nonorally (that is, simulating NPO for prolonged provide similar answers as higher order animal research
periods of time) to determine whether swallowing dete- (e.g., rats) but may also provide beginning substrates
riorates with nonoral use and what changes occur in sen- upon which computer models of swallowing can be fur-
sory representation in the oral and pharyngeal mucosa; ther developed.
more specifically, whether the response loses its normal Computational models. Swallowing biomechanics
timing and the importance of the pairing of stimuli over and bolus flow properties are subject to the laws of
different regions in improving the impaired pharyngeal physics and can be expressed by mathematical equations
swallow. In these circumstances, it is of interest to deter- (Chang, Rosendall, & Finlayson, 1998; Kahrilas, Lin, Chen,
mine whether cell death occurs along with axonal degen- & Logemann, 1995; Lin, Chen, Hertz, & Kahrilas, 1996;
eration, and, if so, whether a decrease in swallowing Nicosia & Robbins, 2001). Dysphagia researchers who
cortical representation also is observed. collaborate with computer experts will be able to con-
The nonhuman primate brain is highly similar to tinue the development of computation models that can
the human brain in structure and function. However, be- explain basic neurologic functions not yet understood.
cause of political pressure and the expense and care re- Such collaborations can also be applied to swallowing
quired, research on recovery from acquired CNS lesions central pattern generators to clarify how they use inter-
in nonhuman primates is possible but not commonly nal and external sensory input to modify the output.
conducted. Animal models for swallowing rehabilitation Ultimately, direct input of muscle activity and /or images
research may pose a greater challenge than for limb into specially designed computer programs (Kim, Chung,
mobility research. Research investigations of swallowing Kwang-Ho, & Robbins, 2000; Luccichenti et al., 2003;
Robbins et al.: Neural Plasticity, Swallowing, and Dysphagia Rehabilitation S289
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
Table 6. Outcome measures. A repertoire of swallowing-related outcomes.
Physiological Bolus flow kinematics Functional
Central markers—cortical representation Direction Swallowing-related QOL
Peripheral markers—evoked potentials Duration Diet
Oropharyngeal biomechanics–temporospatial–strength Clearance Health status
Note. QOL = quality of life.
Stier, Stein, Schwaiger, & Heidecke, 2004) can be used to the way to marked improvements in present strategies
determine normative and disorder values (Das, Reddy, & for therapy (Barker & Dunnett, 1999).
Narayanan, 2001; Neustadter, Drushel, Crago, Adams, & The comments of Barker and Dunnett (1999) re-
Chiel, 2002) that can be used to determine patient- garding motor function after neurotransplantation have
specific repetition and intensity parameters that will evoke great relevance to current issues and the current status
neurologic change. The interaction of systematically al- of swallowing rehabilitation, as pointed out by Turkstra
tered material properties (e.g., viscosity, yield stress) and et al. (Turkstra, Holland, & Bays, 2003). Available tech-
neurologic adaptation to them in the context of swallow- nology facilitates conduct of translational studies. We
ing biomechanics and bolus flow outcomes may be derived are poised to develop a body of work determining the de-
by computational models developed collaboratively among gree of neural plasticity that can be affected within the
food scientists, engineers, neuroscientists, and rehabilita- neuronal substrates of the swallowing mechanism in
tion experts. In addition, measurements that express sta- animals, healthy young and old humans, and following
bility or lack thereof within complex motor acts such as disease or injury. Translational studies may be designed
swallowing (Jing, Cropper, Hurwitz, & Weiss, 2004; Lum to determine the effects of and the degree to which neu-
et al., 2005) can be used to predict how long rehabilitation ral substrates involved in swallowing can be altered in
may take and assist with the decision as to whether or not normal and neurologically impaired individuals. For
a nasogastric or gastric feeding tube would be best for the example, how does damage to a “center” or pattern gen-
patient. Finally, the application of computer modeling to erator versus damage to white matter tracts respond to
new imaging tools (such as fMRI) will continue to advance various forms of manipulation be they sensory, compen-
our knowledge and will generate new hypotheses in swal- satory, motor with or without swallow?
lowing as it has in many other fields of neuroscience.
Translational studies. We need to consider not only
the anatomic connectivity needed to reconstruct the Conceptual Framework for Feasibility
damaged circuitry but also the relearning and retraining
of the normal adult’s rich repertoire of motor skills and
Studies in Swallowing
habits. This is the realm of the rehabilitation specialists, A number of experiments for the study of neural
who, to this point, have not been active participants in plasticity in swallowing disorders are proposed. Studies
existing transplantation programs. We might expect, will identify subject variables, including age and cog-
though, that they have much to offer, and the marriage of nitive status, disease process, and co-morbidities, and
rehabilitation and neurobiological disciplines may pave will examine the effects of interventions, including the
Table 7. A template for conceptual organization useful for study design.
Intervention Independent variable Plasticity measurement method Dependent variable
e-STIM Intensity TMS Direction of bolus flow
Thermal-tactile Repetition PET Duration
Mendelsohn Timing and age fMRI Clearance
Experience specific MEG ROM
Salience EEG Strength
Transference Electron microscopy SWAL-QOL
Interference Chemical assays
Note. TMS = transcranial magnetic stimulation; PET = positron emission tomography; fMRI = functional magnetic resonance imaging;
MEG = magnetoencephalography; EEG = electroencephalography; SWAL-QOL = swallowing-related quality of life.
S290 Journal of Speech, Language, and Hearing Research • Vol. 51 • S276–S300 • February 2008
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
swallow-related salient outcomes (see Table 6) and asso- clarifying limits to neural plasticity in other systems.
ciated changes in neurophysiological function. Although Such limitations must be elucidated in swallowing re-
suggested studies are designed to address a variety of spe- habilitation as well.
cific populations by species, age, disease, site, and extent
of injury, Table 7 is a study design template structured
Acknowledgments
for conceptual organization.
This work was done under the auspices of the Swallowing
Work Group, led by JoAnne Robbins. We would like to thank
Strategic Plan—Focused Raymond Kent, David McFarland, and Arthur Miller for their
and Integrated Research review of this article and their important contributions.
The Swallowing Work Group developed a strategic
plan for the translation of concepts seeded in the neural References
plasticity literature into the clinical science of swallow- Ashford, J., McCabe, D., & Musson, N. (2005, November).
ing rehabilitation. See the Appendix for a nonexclusive Systematic review of seven dysphagia therapies: A VA
list of suggested goals and methods to achieve them. taskforce report. Presented at the Annual Convention of
the American Speech-Language-Hearing Association,
San Diego, CA.
The Future Barker, R. A., & Dunnett, S. B. (1999). Neural repair, trans-
plantation, and rehabilitation. Hove, England: Psychology
The relevance of established principles of learning Press.
to the recovery of swallowing function appears clinically Bisch, E. M., Logemann, J. A., Rademaker, A. W., Kahrilas,
intuitive and evident in an emerging body of literature, P. J., & Lazarus, C. L. (1994). Pharyngeal effects of bolus
but the direct application of these principles in system- volume, viscosity, and temperature in patients with dys-
atic rehabilitation, including exercise of the upper aero- phagia resulting from neurologic impairment and in normal
subjects. Journal of Speech and Hearing Research, 37,
digestive tract musculature, is yet to be established and 1041–1049.
is under investigation in many basic and clinical lab-
Brandt, D. K., Hind, J. A., Robbins, J. A., Lindblad, A. S.,
oratories. Efforts to expedite such focused work must be Gensler, G., Gill, G., et al. (2006). Challenges in the design
systematic and multifactorial. and conduct of a randomized study of two interventions
The principles of neural plasticity address issues for liquid aspiration. Clinical Trials, 3, 457–468.
that are potentially critical (timely and important) to Broniatowski, M., Dessoffy, R., Shields, R. W., & Strome,
recovery and rehabilitation of dysphagia. During recent M. (1999). Vagal stimulation for reciprocal coupling between
glottic and upper esophageal sphincter activities in the
years, it has been shown that swallowing relies on a
canine. Dysphagia, 14, 196–203.
large-scale distributed neural network (Zald & Pardo,
Bulow, M., Olsson, R., & Ekberg, O. (2003). Videoradio-
1999) supporting complex underlying neural substrates
graphic analysis of how carbonated thin liquids and
reflected in the term patterned response, an alternative thickened liquids affect the physiology of swallowing in
to the long-held notion that swallowing is a traditional subjects with aspiration on thin liquids. Acta Radiologica,
reflex (Kahrilas et al., 1991). Such revolutionary concep- 44, 366–372.
tualization encourages clinicians who have been hypoth- Buonomano, D. V., & Merzenich, M. M. (1998). Cortical
esizing, as reflected in their practices, that willful control plasticity: From synapses to maps. Annual Review of
during the early and even middle stages of swallowing may Neuroscience, 21, 149–186.
offer access to the patterned response. Evaluating effect Cataldi-Betcher, E. L., Seltzer, M. H., Slocum, B. A., &
sizes of both peripheral and central changes in response Jones, K. W. (1983). Complications occurring during enteral
nutrition support: A prospective study. Journal of Parenteral
to treatment as well as their temporal order will inform
and Enteral Nutrition, 7, 546–552.
the next generation of clinical scientists about brain be-
Chang, M. W., Rosendall, B., & Finlayson, B. A. (1998).
havior interactions in ways that attention to either one
Mathematical modeling of normal pharyngeal bolus trans-
alone cannot. port: A preliminary study. Journal of Rehabilitation Research
The promise that creative application of imaging and Development, 35, 327–334.
techniques holds for advances in our basic understand- Charbonneau, I., Lund, J. P., & McFarland, D. H. (2005).
ing of neural networks as they relate to physiology and Persistence of respiratory-swallowing coordination after
behavior is enormous. In addition, the use of animal mod- laryngectomy. Journal of Speech and Hearing Research,
48, 34–44.
els offers an ability to target, more appropriately, prin-
ciples of neural plasticity such as time, repetition, and Chaudhuri, G., Hildner, C. D., Brady, S., Hutchins, B.,
Aliga, N., & Abadilla, E. (2002). Cardiovascular effects
intensity in an efficient, cost-effective manner before ap- of the supraglottic and super-supraglottic swallowing
plying those principles to human clinical studies. Both maneuvers in stroke patients with dysphagia. Dysphagia,
advanced imaging techniques and animal studies are 17, 19–23.
Robbins et al.: Neural Plasticity, Swallowing, and Dysphagia Rehabilitation S291
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
Cohen, L. G., Ziemann, U., Chen, R., Classen, J., Hallett, swallows on breathing in awake goats. Journal of Applied
M., Gerloff, C., et al. (1998). Studies of neuroplasticity with Physiology, 92, 1923–1935.
transcranial magnetic stimulation. Journal of Clinical Feroah, T. R., Forster, H. V., Fuentes, C. G., Wenninger,
Neurophysiology, 15, 305–324. J., Martino, P., Hodges, M., et al. (2002). Contributions
Connelly, C. A., Dobbins, E. G., & Feldman, J. L. (1992). from rostral medullary nuclei to coordination of swallowing
Pre-Botzinger complex in cats: Respiratory neuronal dis- and breathing in awake goats. Journal of Applied Phys-
charge patterns. Brain Research, 590, 337–340. iology, 93, 581–591.
Connor, N. P., Jackson, M., Mann, L., Russell, J., Lee, K., Fisher, B. E., & Sullivan, K. J. (2001). Activity-dependent
Kluender, K. R., et al. (2005). Increased tongue forces factors affecting poststroke functional outcomes. Topics
following progressive resistance exercise in aged rats. in Stroke Rehabilitation, 8, 31–44.
Washington, DC: Society for Neuroscience. (Program Fraser, C., Power, M., Hamdy, S., Rothwell, J. C., Hobday,
No. 397.20.2005). D., Hollander, I., et al. (2002). Driving plasticity in adult
Cook, I. J., Dodds, W. J., Dantas, R. O., Kern, M. K., human motor cortex is associated with improved motor
Massey, B. T., Shaker, R., et al. (1989). Timing of video- function after brain injury. Neuron, 34, 831–840.
fluoroscopic, manometric events, and bolus transit during Fraser, C., Rothwell, J., Power, M., Hobson, A., Thompson,
the oral and pharyngeal phases of swallowing. Dysphagia, D., & Hamdy, S. (2003). Differential changes in human
4, 8–15. pharyngoesophageal motor excitability induced by swal-
Cot, F., & McFarland, D. H. (1996). Anatomie-physiologie de lowing, pharyngeal stimulation, and anesthesia. American
la déglutition (Anatomy and physiology of swallowing). In Journal of Physiology, 285, G137–G144.
F. Cot (Ed.), La dysphagie oropharyngée chez l’adulte (Oropha- Friel, K. M., Heddings, A. A., & Nudo, R. J. (2000). Effects
ryngeal dysphagia in the adult; pp. 1–28). Paris: Edisem. of postlesion experience on behavioral recovery and neuro-
Dantas, R. O., & Dodds, W. J. (1990). Effect of bolus volume physiologic reorganization after cortical injury in primates.
and consistency on swallow-induced submental and infrahyoid Neurorehabilitation and Neural Repair, 14, 187–198.
electromyographic activity. Brazilian Journal of Medical Fujiu, M., & Logemann, J. A. (1996). Effect of a tongue-
and Biological Research, 23, 37–44. holding maneuver on posterior pharyngeal wall movement
during deglutition. American Journal of Speech-Language-
Dantas, R. O., Kern, M. K., Massey, B. T., Dodds, W. J.,
Pathology, 5, 23–30.
Kahrilas, P. J., Brasseur, J. G., et al. (1990). Effect of
swallowed bolus variables on oral and pharyngeal phase Fujiu, M., Toleikis, J. R., Logemann, J. A., & Larson, C. R.
of swallowing. American Journal of Physiology, 675–681. (1994). Glossopharyngeal evoked potentials in normal sub-
jects following mechanical stimulation of the anterior faucial
Das, A., Reddy, N. P., & Narayanan, J. (2001). Hybrid fuzzy
pillar. Electroencephalography and Clinical Neurology,
logic committee neuronal networks for recognition of swallow
92, 183–195.
acceleration signals. Computer Methods and Programs in
Biomedicine, 64, 87–99. Fukushima, S., Shingai, T., Kitagawa, J., Takahashi, Y.,
Taguchi, Y., Noda, T., et al. (2003). Role of the pharyngeal
DeBow, S. B., McKenna, J. E., Kolb, B., & Colbourne, F. branch of the vagus nerve in laryngeal elevation and UES
(2004). Immediate constraint-induced movement therapy pressure during swallowing in rabbits. Dysphagia, 18,
causes local hyperthermia that exacerbates cerebral corti- 58–63.
cal injury in rats. Canadian Journal of Physiology and
Pharmacology, 82, 231–237. German, R. Z., Crompton, A. W., Owerkowicz, T., &
Thexton, A. J. (2004). Volume and rate of milk delivery
Diamant, N. (1996). Firing up the swallowing mechanism. as determinants of swallowing in an infant model animal.
Nature Medicine, 2, 1190–1191. Dysphagia, 19, 147–154.
Ding, R., Larson, C. R., & Rademaker, A. W. (2002). Sur- German, R. Z., Crompton, A. W., & Thexton, A. J. (1998).
face electromyographic and electroglottographic studies in The coordination and interaction between respiration and
normal subjects under two swallow conditions: Normal deglutition in young pigs. Journal of Comparative Physiol-
and during the Mendelsohn maneuver. Dysphagia, 17, ogy [A, Sensory Neural and Behavioral Physiology], 182,
1–12. 539–547.
Dozier, T. S., Brodsky, M. B., Michel, Y., Walters, B. C., Jr., Hamdy, S., Aziz, Q., Rothwell, J. C., Crone, R., Hughes,
& Martin-Harris, B. (2006). Coordination of swallowing D. G., Tallis, R. C., et al. (1997). Explaining oropharyngeal
and respiration in normal sequential cup swallows. dysphagia after unilateral hemispheric stroke. Lancet, 350,
Laryngoscope, 116, 1489–1493. 686–692.
ECRI Report. (1999). Diagnosis and treatment of swallowing Hamdy, S., Aziz, Q., Rothwell, J. C., Hobson, A., Barlow,
disorders (dysphagia) in acute-care stroke patients: Evidence J., & Thompson, D. G. (1997). Cranial nerve modulation
Report/Technical Assessment No. 8 ( Publication No. 99- of human cortical swallowing motor pathways. American
E024). Rockville, MD: Agency for Health Care Policy and Journal of Physiology, 272, G802–G808.
Research.
Hamdy, S., Aziz, Q., Rothwell, J. C., Singh, K., Barlow, J.,
Feldman, J. L., Loewy, A. D., & Speck, D. F. (1985). Pro- Hughes, D., et al. (1996). The cortical topography of human
jections from the ventral respiratory group to phrenic swallowing musculature in health and disease. Nature
and inercostal motoneurons in cat: An autoradiographic Medicine, 2, 1217–1224.
study. Journal of Neuroscience, 8, 1993–2000.
Hamdy, S., Jilani, S., Price, V., Parker, C., Hall, N., &
Feroah, T. R., Forster, H. V., Fuentes, C. G., Lang, I. V., Power, M. (2003). Modulation of human swallowing be-
Beste, D., Martino, P., et al. (2002). Effects of spontaneous havior by thermal and chemical stimulation in health and
S292 Journal of Speech, Language, and Hearing Research • Vol. 51 • S276–S300 • February 2008
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
after brain injury. Neurogastroenterology and Motility, 15, peripheral nerve damage in adult and developing animals.
69–77. Annual Review of Neuroscience, 6, 325–356.
Hamdy, S., & Rothwell, J. C. (1998). Gut feelings about Kahrilas, P. J., Dodds, W. J., Dent, J., Logemann, J. A., &
recovery after stroke: The organization and reorganization Shaker, R. (1988). Upper esophageal sphincter function
of human swallowing motor cortex. Trends in Neurosciences, during deglutition. Gastroenterology, 95, 52–62.
21, 278–282. Kahrilas, P. J., Lin, S., Chen, J., & Logemann, J. A. (1995).
Hamdy, S., Rothwell, J. C., Aziz, Q., Singh, K., & Thompson, Three-dimensional modeling of the oropharynx during
D. G. (1998). Long-term reorganization of human motor swallowing. Radiology, 194, 575–579.
cortex driven by short-term sensory stimulation. Nature Kahrilas, P. J., Logemann, J. A., Krugler, C., & Flanagan,
Neuroscience, 1, 64–68. E. (1991). Volitional augmentaion of upper esophageal
Hiiemae, K. M., & Crompton, A. W. (1985). Mastication, sphincter during swallow. American Journal of Physiology,
food transport and swallowing. In M. Hildebrand, D. 260, G450–G456.
Bramble, K. Liem, & D. Wake ( Eds.), Functional vertebrate Kays, S., Humbert, I. A., Reeder, S., Brittain, J., Porcaro,
morphology ( pp. 262–290). Cambridge, MA: Harvard E., Hind, J., et al. (2007, March). Lingual tissue in healthy
University Press. younger and older adults: MRI fat-water separation using
Hind, J. A., Nicosia, M., Roecker, E., Carnes, M., Doyle, IDEAL method, part II. Paper presented at the 15th Annual
J., Dengal, G. A., et al. (2001). Comparison of effortful and Meeting of the Dysphagia Reseach Society, Vancouver,
noneffortful swallows in healthy middle aged and older British Columbia, Canada.
adults. Archives of Physical Medicine and Rehabilitation, Kilgard, M. P., & Merzenich, M. M. (1998, March 13).
82, 1661–1665. Cortical map reorganization enabled by nucleus basalis
Hiss, S. G., & Huckabee, M. L. (2005). Timing of pharyngeal activity. Science, 279, 1714–1718.
and upper esophageal sphincter pressures as a function of Kim, H., Chung, C. S., Kwang-Ho, L., & Robbins, J. (2000).
normal and effortful swallowing in young healthy adults. Aspiration subsequent to a pure medullary infarction:
Dysphagia, 20, 149–156. Lesion sites, clinical variables, and outcome. Archives of
Hiss, S. G., Strauss, M., Treole, K., Stuart, A., & Boutilier, Neurology, 57, 478–483.
S. (2004). Effects of age, gender bolus volume, bolus vis- Kleim, J. A., Barbay, S., Cooper, N. R., Hogg, T. M.,
cosity, and gustation on swallowing apnea onset relative Reidel, C. N., Remple, M. S., et al. (2002). Motor learning-
to lingual bolus propulsion onset in normal adults. Journal dependent synaptogenesis is localized to functionally
of Speech and Hearing Research, 47, 572–583. reorganized motor cortex. Neurobiology of Learning and
Huang, J., Carr, T. H., & Cao, Y. (2002). Comparing cortical Memory, 77, 63–77.
activations for silent and overt speech using event-related Kleim, J. A., Barbay, S., & Nudo, R. J. (1998). Functional
fMRI. Human Brain Mapping, 15, 39–53. reorganization of the rat motor cortex following motor
Humbert, I. A., Poletto, C. J., Saxon, K. G., Kearney, P. R., skill learning. Journal of Neurophysiology, 80, 3321–3325.
Crujido, L., Wright-Harp, W., et al. (2006). The effect of Kleim, J. A., Hogg, T. M., VandenBerg, P., Cooper, N. R.,
surface electrical stimulation on hyo-laryngeal movement in Bruneau, R., & Remple, M. S. (2004). Cortical synapto-
normal individuals at rest and during swallowing. Journal genesis and motor map reorganization occur during late, but
of Applied Physiology, 101, 1657–1663. not early, phase of motor skill learning. Journal of Neuro-
Humm, J. L., Kozlowski, D. A., Bland, S. T., James, D. C., science, 24, 628–633.
& Schallert, T. (1999). Use-dependent exaggeration of Kleim, J. A., & Jones, T. A. (2008). Principles of experience-
brain injury: Is glutamate involved? Experimental Neu- dependent neural plasticity: Implications for rehabilitation
rology, 157, 349–358. after brain damage. Journal of Speech, Language, and
Humm, J. L., Kozlowski, D. A., James, D. C., Gotts, J. E., Hearing Research, 51, S225–S239.
& Schallert, T. (1998). Use-dependent exacerbation of Kleim, J. A., Lussnig, E., Schwarz, E. R., Comery, T. A., &
brain damage occurs during an early post-lesion vulnerable Greenough, W. T. (1996). Synaptogenesis and fox expres-
period. Brain Research, 783, 286–292. sion in the motor cortex of the adult rat after complex motor
Jacob, P., Kahrilas, P., Logemann, J. A., Shah, V., & Ha, T. skill acquisition. Journal of Neuroscience, 16, 4529–4535.
(1989). Upper esophageal sphincter opening and modulation Koizumi, H., Kogo, M., & Matsuya, T. (1996). Coordina-
during swallowing. Gastroenterology, 97, 469–478. tion between palatal and laryngeal muscle activities in
Jean, A. (2001). Brain stem control of swallowing: Neuronal response to rebreathing and lung inflation. Cleft Palate-
network and cellular mechanisms. Physiological Reviews, Craniofacial Journal, 33, 459–462.
81, 929–969. Kozlowski, D. A., James, D. C., & Schallert, T. (1996). Use-
Jiang, C., & Shen, E. (1991). Respiratory neurons in the dependent exaggeration of neuronal injury after unilateral
medulla of the rabbit: Distribution, discharge patterns and sensorimotor cortex lesions. Journal of Neuroscience, 46,
spinal projections. Brain Research, 541, 284–292. 4776–4786.
Jing, J., Cropper, E. C., Hurwitz, I., & Weiss, K. R. (2004). Kramer, A. F., Bherer, L., Colcombe, S. J., Dong, W., &
The construction of movement with behavior-specific and Greenough, W. T. (2004). Environmental influences on cog-
behavior-independent modules. Journal of Neuroscience, 24, nitive and brain plasticity during aging. Journal of Gerontology:
6315–6325. Biological and Medical Sciences, 59, M940–M957.
Kaas, J. H., Merzenich, M. M., & Killackey, H. P. (1983). Langmore, S. E. (1995). Efficacy of behavioral treatment for
The reorganization of somatosensory cortex following oropharyngeal dysphagia. Dysphagia, 10, 259–262.
Robbins et al.: Neural Plasticity, Swallowing, and Dysphagia Rehabilitation S293
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
Langmore, S. E., Terpenning, M. S., Schork, A., Chen, Y., Lum, C. S., Zhurov, Y., Cropper, E. C., Weiss, K. R., &
Murray, J. T., Lopatin, D., et al. (1998). Predictors of aspi- Brezina, V. (2005). Variability of swallowing performance
ration pneumonia: How important is dysphagia? Dysphagia, in intact, freely feeding Aplysia. Journal of Neurophysiology,
13, 69–81. 94, 2427–2446.
Lazarus, C., Logemann, J., Huang, C., & Rademaker, A. Luschei, E. S. (1991). Development of objective standards of
(2003). Effects of two types of tongue strengthening exer- non-speech oral strength and performance: An advocate’s
cises in young normals. Folia Phoniatrica et Logopedica, views. In C. A. Moore, K. M. Yorkston, & D. R. Beukelman
55, 199–205. ( Eds.), Dysarthria and apraxia of speech: Perspectives on
management ( pp. 3–14). Baltimore: Paul H. Brookes.
Lazarus, C., Logemann, J. A., Song, C. W., Rademaker, A. W.,
& Kahrilas, P. J. (2002). Effects of voluntary maneuvers on Martin, R., MacIntosh, B., Barr, A., Smith, R., Stevens, T.,
tongue base function for swallowing. Folia Phoniatrica Taves, D., et al. (2004, October). Cerebral cortical pro-
et Logopedica, 54, 171–176. cessing of swallowing in older adults. Paper presented at the
13th Annual Meeting of the Dysphagia Research Society,
Lazarus, C. L., Logemann, J. A., Rademaker, A. W.,
Montreal, Quebec, Canada.
Kahrilas, P. J., Pajak, T., Lazar, R., et al. (1993). Effects
of bolus volume, viscosity and repeated swallows in non- Martin, R. E., Goodyear, B. G., Gati, J. S., & Menon, R. S.
stroke subjects and stroke patients. Archives of Physical (2002). Cerebral cortical representation of automatic and
Medicine and Rehabilitation, 74, 1066–1070. volitional swallowing in humans. Journal of Neurophys-
iology, 85, 938–950.
Lazzara, G., Lazarus, C., & Logemann, J. (1986). Impact
of thermal stimulation on the triggering of the swallowing Martin-Harris, B., Brodsky, M. B., Michel, Y., Ford, C. L.,
reflex. Dysphagia, 1, 73–77. Walters, B., & Heffner, J. (2005). Breathing and swal-
lowing dynamics across the adult lifespan. Archives of
Lin, S., Chen, J., Hertz, P., & Kahrilas, P. (1996). Dynamic Otolaryngology–Head and Neck Surgery, 131, 762–770.
reconstruction of the oropharyngeal swallow using computer
based animation. Computerized Medical Imaging and Martin-Harris, B., Michel, Y., & Castell, D. O. (2005).
Graphics, 20, 69–75. Physiologic model of oropharyngeal swallowing revisited.
Otolaryngology–Head and Neck Surgery, 133, 234–240.
Lisman, J., & Spruston, N. (2005). Postsynaptic depolariza-
tion requirements for LTP and LTD: A critique of spike timing- McFarland, D. H., & Lund, J. P. (1995). Modification of
dependent plasticity. Nature Neuroscience, 8, 839–841. mastication and respiration during swallowing in the adult
human. Journal of Neurophysiology, 74, 1509–1517.
Logemann, J. A. (1983). Evaluation and treatment of
McHorney, C., Bricker, D., Kramer, A., Rosenbek, J.,
swallowing disorders. San Diego, CA: College Hill Press.
Robbins, J., Chignell, K., et al. (2000). The SWAL-QOL
Logemann, J. A., Gensler, G., Robbins, J. A., Lindblad, outcomes tool for oropharyngeal dysphagia in adults: I.
A. S., Brandt, D. K., Hind, J. A., et al. (2008). A randomized Conceptual foundation and item development. Dysphagia,
study of three interventions for aspiration of thin liquids 15, 115–121.
in patients with dementia or Parkinson’s disease. Journal of
McHorney, C. A., Bricker, D. E., Robbins, J. A., Kramer,
Speech, Language, and Hearing Research, 51, 173–183.
A. E., Rosenbek, J. C., & Chignell, K. A. (2000). The
Logemann, J. A., Kahrilas, P. J., Cheng, J., Pauloski, SWAL-QOL outcomes tool for oropharyngeal dysphagia
B. R., Gibbons, P. J., Rademaker, A. W., et al. (1992). in adults: II. Item reduction and preliminary scaling.
Closure mechanisms of the laryngeal vestibule during Dysphagia, 15, 122–133.
swallow. American Journal of Physiology, 262, B338–B344. McHorney, C. A., Robbins, J. A., Lomax, K., Rosenbek,
Logemann, J. A., Pauloski, B. R., Colangelo, L., Lazarus, C., J. C., Chignell, K. A., Kramer, A. E., et al. (2002). The
& Fujiu, M. (1995). The effects of a sour bolus on oropha- SWAL-QOL outcomes tool for oropharyngeal dysphagia in
ryngeal swallowing measures in patients with neurogenic adults: III. Extensive evidence of reliability and validity.
dysphagia. Journal of Speech and Hearing Research, 38, Dysphagia, 17, 97–114.
556–563. Meng, Y., Uchida, K., Sato, T., Yamamura, K., & Yamada, Y.
Logemann, J. A., Rademaker, A. W., Pauloski, B. R., & (1999). Difference in the burst patterns of digastric and
Kahrilas, P. J. (1994). Effects of postural change on aspi- mylohyoid activities during feeding in the freely behaving
ration in head and neck surgical patients. Otolaryngology– rabbit. Dysphagia, 14, 78–84.
Head and Neck Surgery, 110, 222–227. Merzenich, M. M., Kaas, J. H., Wall, J. T., Sur, M., Nelson,
Luccichenti, G., Cademartiri, F., Fecci, L., Carbognani, R. J., & Felleman, D. J. (1983). Progression of change fol-
P., Rusca, M., & Pavone, P. (2003). Non-neoplastic trachel lowing median nerve section in the cortical representation
lesions: Comparison between virtual CT endoscopy and of the hand in areas 3b and 1 in adult owl and squirrel
fiberoptic bronchoscopy. La Radiologia Medica ( Torino), monkeys. Neuroscience, 10, 639–665.
106, 147–153. Miller, A. J. (1999). The neuroscientific principles of swallow-
Ludlow, C. L., Humbert, I., Saxon, K., Poletto, C., Sonies, ing and dysphagia. San Diego, CA: Singular Publishing
B., & Crujido, L. (2007). Effects of surface electrical Group.
stimulation both at rest and during swallowing in chronic Miller, A. J., & Loizzi, R. F. (1974). Anatomical and func-
pharyngeal dysphagia. Dysphagia, 22, 1–10. tional differentiation of superior laryngeal nerve fibers af-
Luke, L. M., Allred, R. P., & Jones, T. A. (2004). Unilateral fecting swallowing and respiration. Experimental Neurology,
ischemic sensorimotor cortical damage induces contralesional 42, 369–387.
synaptogenesis and enhances skilled reaching with the Miller, F. R., & Sherrington, C. S. (1916). Some observations
ipsilateral forelimb in adult male rats. Synapse, 54, 187–199. on the buccoo-pharyngeal stage of reflux deglutition in
S294 Journal of Speech, Language, and Hearing Research • Vol. 51 • S276–S300 • February 2008
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
the cat. Quarterly Journal of Experimental Physiology, 9, Paydarfar, D., Gilbert, R. J., Poppel, C. S., & Nassab, P. F.
147–186. (1995). Respiratory phase resetting and airflow changes
induced by swallowing in humans. The Journal of Phys-
Miller, J. L., & Watkin, K. L. (1996). The influence of bolus
iology ( London), 483, 273–288.
volume and viscosity on anterior lingual force during the
oral stage of swallowing. Dysphagia, 11, 117–124. Peinemann, A., Reimer, B., Loer, C., Quartarone, A.,
Munchau, A., Conrad, B., et al. (2004). Long-lasting
Miyaoka, Y., Inoue, M., Shimada, K., & Yamada, Y. (1998).
increase in corticospinal excitability after 1800 pulses of
Reflexogenic areas for velopharyngeal closure in rabbits.
subthreshold 5 Hz repetitive TMS to the primary motor
Dysphagia, 13, 159.
cortex. Clinical Neurophysiology, 115, 1519–1526.
Miyaoka, Y., Kyuhachiro, S., & Yamada, Y. (1997). Vagal
Pelletier, C. A., & Lawless, H. T. (2003). Effect of citric acid
control of pharyngeal constrictor activity in rabbits. Dys-
and citric acid-sucrose mixtures on swallowing in neurogenic
phagia, 12, 39–42.
oropharyngeal dysphagia. Dysphagia, 18, 231–241.
Morgen, K., Kadom, N., Sawaki, L., Tessitore, A., Perier, O. J., Buyse, M., Lechat, J., & Stenuit, A. (1986).
Ohayon, J., Frank, J., et al. (2004). Kinematic specificity Deprivation and morphological changes in the central
of cortical reorganization associated with motor training. nervous system. Acta Oto-laryngologica (Supplement),
NeuroImage, 21, 1182–1187. 429, 45–50.
Muellbacher, W., Boroojerdi, B., Ziemann, U., & Hallet, Perlman, A., Palmer, P., McCulloch, T., & Vandaele, D.
M. (2001). Analogous corticocortical inhibition and facilitation (1999). Electromyographic activity from human laryngeal,
in ipsilateral and contralateral human motor cortex repre- pharyngeal and submental muscles during swallowing.
sentations of the tongue. Journal of Clinical Neurophysiology, Journal of Applied Physiology, 86, 1663–1669.
18, 550–558.
Plautz, E. J., Barbay, S., Frost, S. B., Friel, K. M.,
Neustadter, D. M., Drushel, R. F., Crago, P. E., Adams, Dancause, N., Zoubina, E. V., et al. (2003). Post-infarct
B. W., & Chiel, H. J. (2002). A kinematic model of swallow- cortical plasticity and behavioral recovery using concurrent
ing in Aplysia californica based on radula/odontophore kine- cortical stimulation and rehabilitative training: A feasibility
matics and in vivo magnetic resonance images. Journal of study in primates. Neurological Research, 25, 801–810.
Experimental Biology, 205, 3177–3206.
Plautz, E. J., Milliken, G. W., & Nudo, R. J. (2000). Effects
Nicosia, M. S., & Robbins, J. A. (2001). The fluid mechanics of repetitive motor training on movement representations
of bolus ejection from the oral cavity. Journal of Biome- in adult squirrel monkeys: Role of use versus learning.
chanics, 34, 1537–1544. Neurobiology of Learning and Memory, 74, 27–55.
Nudo, R. J. (2003). Functional and structural plasticity in motor Pons, T. (1996, April 11). Novel sensations in the congenitally
cortex: Implications for stroke recovery. Physical Medicine blind. Nature, 380, 479–480.
and Rehabilitation Clinics of North America, 14, S57–S76.
Pouderoux, P., & Kahrilas, P. J. (1995). Deglutitive tongue
Nudo, R. J., Jenkins, W. M., & Merzenich, M. M. (1990). force modulation by volition, volume and viscosity in humans.
Repetitive microstimulation alters the cortical representa- Gastroenterology, 108, 1418–1426.
tion of movements in adult rats. Somatosensory and Motor
Research, 7, 463–483. Power, M., Fraser, C., Hobson, A., Rothwell, J. C., Mistry,
S., Nicholson, D. A., et al. (2004). Changes in pharyn-
Nudo, R. J., & Milliken, G. W. (1996). Reorganization of geal corticobulbar excitability and swallowing behavior
movement representations in primary motor cortex follow- after oral stimulation. American Journal of Physiology–
ing focal ischemic infarcts in adult squirrel monkeys. Gastrointestinal and Liver Physiology, 286, G45–G50.
Journal of Neurophysiology, 75, 2144–2149.
Rasley, A., Logemann, J. A., Kahrilas, P. J., Rademaker,
Nudo, R. J., Wise, B. M., SiFuentes, F., & Milliken, A. W., Pauloski, B. R., & Dodds, W. J. (1993). Prevention
G. W. (1996, June 21). Neural substrates for the effects of of barium aspiration during videofluoroscopic swallowing
rehabilitative training on motor recovery after ischemic studies: Value of change in posture. American Journal of
infarct. Science, 272, 1791–1794. Roentgenology, 160, 1005–1009.
Odderson, I. R., Keaton, J. C., & McKenna, B. S. (1995). Rauschecker, J. P. (1995). Compensatory plasticity and
Swallow management in patients on an acute stroke sensory substitution in the cerebral cortex. Trends in
pathway: Quality is cost effective. Archives of Physical Neurosciences, 18, 36–43.
Medicine and Rehabilitation, 76, 1130–1133.
Reale, R. A., Brugge, J. F., & Chan, J. C. (1987). Maps
Ohmae, Y., Ogura, M., Kitahara, S., Karaho, T., & Inouye, of auditory cortex in cats reared after unilateral cochlear
T. (1998). Effects of head rotation on pharyngeal function ablation in the neonatal period. Brain Research, 431,
during normal swallow. Annals of Otology, Rhinology & 281–290.
Laryngology, 107, 344–348.
Reimers-Neils, L., Logemann, J., & Larson, C. (1994).
Palmer, J. B., Rudin, J. H., Lara, G., & Crompton, A. W. Viscosity effects on EMG activity in normal swallow. Dys-
(1992). Coordination of mastication and swallowing. Dys- phagia, 9, 101–106.
phagia, 7, 187–200.
Reix, P., Arsenault, J., Langlois, C., Niyonsenga, T., &
Pascual-Leone, A., Cammarota, A., Wassermann, E. M., Praud, J. P. (2004). Nonnutritive swallowing and respira-
Brasil-Neto, J. P., Cohen, L. H., & Hallett, M. (1993). tion relationships in preterm lambs. Journal of Applied
Modulation of motor cortical outputs to the reading hand Physiology, 97, 1283–1290.
of braille readers. Annals of Neurology, 34, 33–37.
Remple, M. S., Bruneau, R. M., VandenBerg, P., Goertzen,
Patten, J. (1977). Neurological differential diagnosis. London: C., & Kleim, J. A. (2001). Sensitivity of cortical move-
Harold Stroke. ment representations to motor experience: Evidence that
Robbins et al.: Neural Plasticity, Swallowing, and Dysphagia Rehabilitation S295
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
skill learning but not strength training induces cortical Saleem, A. F., Sapienza, C., & Okun, M. (2005). Respiratory
reorganization. Behavioral and Brain Research, 123, muscle strength training: Treatment and response duration
133–141. in a patient with early idiopathic Parkinson’s disease.
Rioult-Pedotti, M. S., Friedman, D., & Donoghue, J. P. Neurorehabilitation, 20, 323–333.
(2000, October 20). Learning-induced LTP in neocortex. Sant’Ambrogio, G., Sant’Ambrogio, F. B., & Matthew, O. P.
Science, 290, 533–536. (1986). Effect of cold air on laryngeal mechanoreceptors in
Rioult-Pedotti, M. S., Friedman, D., Hess, G., & Donoghue, the dog. Respiration Physiology, 64, 45–56.
J. P. (1998). Strengthening of horizontal cortical connec- Sapienza, C. M., & Wheeler, K. (2006). Respiratory muscle
tions following skill learning. Nature Neuroscience, 1, strength training: Functional outcomes versus plasticity.
230–234. Seminars in Speech and Language, 27, 236–244.
Risedal, A., Zeng, J., & Johansson, B. B. (1999). Early Sasaki, C. T., Koe, J. K., & Albert, S. (2001). Efficacy of
training may exacerbate brain damage after focal brain adjunctive cricopharyngeus myotomy in supraglottic laryn-
ischemia in the rat. Journal of Cerebral Blood Flow and gectomy. Dysphagia, 16, 19–22.
Metabolism, 19, 997–1003. Sawaki, L., Yaseen, Z., Kopylev, L., & Cohen, L. G. (2003).
Robbins, J. (1996). Normal swallowing and aging. Seminars Age-dependent changes in the ability to encode a novel
in Neurology, 16, 309–317. elementary motor memory. Annals of Neurology, 53,
521–524.
Robbins, J. (1999). The evolution of swallowing neuroanat-
omy and physiology in humans: A practical perspective. Shaker, R., Cook, I. J. S., Dodds, W. J., & Hogan, W. J.
Annals of Neurology, 46, 279–280. (1988). Pressure flow dynamics of the oral phase of swallow-
ing. Dysphagia, 3, 79–84.
Robbins, J., Gangnon, R., Theis, S., Kays, S. A., & Hind,
J. (2005). The effects of lingual exercise on swallowing in Shaker, R., Easterling, C., Kern, M., Nitschke, T., Massey,
older adults. Journal of the American Geriatrics Society, 53, B. T., Daniels, S. K., et al. (2002). Rehabilitation of swal-
1483–1489. lowing by exercise in tube-fed patients with pharyngeal
dysphagia secondary to abnormal UES opening. Gastro-
Robbins, J. A., Gensler, G., Hind, J. A., Logemann, J. A., enterology, 122, 1314–1321.
Lindblad, A. S., Brandt, D. K., et al. (2007). Comparison
of two interventions for liquid aspiration on pneumonia Shaker, R., Kern, M., Bardan, E., Taylor, A., Stewart, E.,
incidence: A randomized, controlled trial. Manuscript sub- Hoffman, R. G., et al. (1997). Augmentation of degluti-
mitted for publication. tive upper esophageal sphincter opening in the elderly
by exercise. American Journal of Physiology, 272,
Robbins, J. A., Hamilton, J. W., Lof, G. L., & Kempster, G. G1518–G1522.
(1992). Oropharyngeal swallowing in normal adults of
different ages. Gastroenterology, 103, 823–829. Shanahan, T. K., Logemann, J. A., Rademaker, A. W.,
Pauloski, B. R., & Kahrilas, P. J. (1993). Chin-down
Robbins, J., Kays, S. A., Gangnon, R., Hewitt, A., & Hind, posture effect on aspiration in dysphagic patients.
J. (2007). The effects of lingual exercise in stroke patients Archives of Physical Medicine and Rehabilitation, 74,
with dysphagia. Archives of Physical Medicine and Reha- 736–739.
bilitation, 88, 150–158.
Sharkawi, A. E., Ramig, L., Logemann, J. A., Pauloski,
Robbins, J., & Levine, R. (1993). Swallowing after lateral B. R., Rademaker, A. W., Smith, C. H., et al. (2002). Swal-
medullary syndrome plus. Clinics in Communication lowing and voice effects of Lee Silverman Voice Treatment
Disorders, 3, 45–55. ( LSVT): A pilot study. Journal of Neurology, Neurosurgery
Robey, R. R., & Schultz, M. C. (1998). A model for conduct- and Psychiatry, 72, 31–36.
ing clinical outcome research: An adaptation of the stan- Stier, A. W., Stein, H. J., Schwaiger, M., & Heidecke, C. D.
dard protocol for use in aphasiology. Aphasiology, 12, (2004). Modeling of esophageal bolus flow by functional
787–810. data analysis of scintigrams. Diseases of the Esophagus, 17,
Rosenbek, J. (1995). Efficacy in dysphagia. Dysphagia, 10, 51–57.
263–267. Takahashi, J., & Nakazawa, F. (1991). Effects of viscosity of
Rosenbek, J., Roecker, E., Wood, J., & Robbins, J. (1996). liquid foods on palatal pressure. Journal of Texture Studies,
Thermal application reduces the duration of stage transition 22, 13–24.
in dysphagia after stroke. Dysphagia, 11, 225–233. Teasell, R. W., & Kalra, L. (2005). What’s new in stroke
Rosenbek, J. C., Robbins, J. A., Fishback, B., & Levine, rehabilitation: Back to basics. Stroke, 36, 215–217.
R. (1991). Effects of thermal application on dysphagia Tinazzi, M., Zanette, G., Volpato, D., Testoni, R., Bonato,
after stroke. Journal of Speech and Hearing Research, 34, C., Manganotti, P., et al. (1998). Neurophysiological evi-
1257–1268. dence of neuroplasticity at multiple levels of the somatosensory
Rosenbek, J. C., Williford, W., Schiltz, A., Robbins, J., system in patients with carpal tunnel syndrome. Brain, 121,
Sowell, T., Deutsch, S., et al. (1998). Comparing treatment 1785–1794.
intensities of tactile-thermal application. Dysphagia, 13, Turkstra, L. S., Holland, A. L., & Bays, G. A. (2003). The
1–9. neuroscience of recovery and rehabilitation: What have we
Sadato, N., Pascu al-Leone, A., Grafman, J., Ibanez, V., learned from animal research? Archives of Physical Medicine
Deiber, M. P., Dold, G., et al. (1996, April 11). Activation and Rehabilitation, 84, 604–612.
of the primary visual cortex by Braille reading in blind Urasaki, E., Genmoto, T., Wada, S., Yokota, A., & Akamatsu,
subjects. Nature, 380, 526–528. N. (2002). Dynamic changes in area 1 somatosensory cortex
S296 Journal of Speech, Language, and Hearing Research • Vol. 51 • S276–S300 • February 2008
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
during transient sensory deprivation: A preliminary study. Ziemann, U., Hallett, M., & Cohen, L. G. (1998). Mecha-
Journal of Clinical Neurophysiology, 19, 219–231. nisms of deafferentation-induced plasticity in human motor
Walton, J. N. (1985). Brain’s disease of the nervous system. cortex. Journal of Neuroscience, 18, 7000–7007.
Oxford, England: Oxford University Press.
Welch, M., Logemann, J. A., Rademaker, A. W., Pauloski, Received February 10, 2006
B. R., & Kahrilas, P. J. (1993). Changes in pharyngeal
Accepted August 2, 2007
dimensions affected by chin tuck. Archives of Physical
Medicine and Rehabilitation, 74, 178–181. DOI: 10.1044/1092-4388(2008/021)
Wong-Riley, M. T., Walsh, S. M., Leake-Jones, P. A., & Contact author: JoAnne Robbins, VAMC GRECC 11G,
Merzenich, M. M. (1981). Maintenance of neuronal activity 2500 Overlook Terrace, Madison, WI 53705.
by electrical stimulation of unilaterally deafened cats E-mail: jrobbin2@wisc.edu.
demonstrable with cytochrome oxidase technique. Annals
Susan Langmore is now with the Department of Otolaryngology–
of Otology, Rhinology & Laryngology, 90, 30–32.
Head and Neck Surgery and the Department of Speech
Zald, D. H., & Pardo, J. V. (1999). The functional neuro- and Hearing Sciences, Boston University.
anatomy of voluntary swallowing. Annals of Neurology, 46,
281–286.
Robbins et al.: Neural Plasticity, Swallowing, and Dysphagia Rehabilitation S297
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
Appendix (p. 1 of 3). Suggested goals and methods.
Goal: To promote the translation of principles of experience-dependent plasticity from animal models to humans for improved understanding of normal
swallowing and its rehabilitation.
A. Develop common definitions and goals to initiate translational research from animal models to humans of various ages and with neurogenic swallowing
disorders of known cause, including iatrogenically induced (e.g., chemoradiation treatment for head and neck cancer).
1. Facilitate discussions between neuroscientists and rehabilitation researchers to develop common definitions and goals to initiate translational research
from animal models to humans.
Prior Direction: Translational research from basic animal models to humans in the areas of normal and disordered swallowing has been limited. As a
result, there is/are not a common vocabulary, definitions, or research goals.
Suggested Actions:
· Invite neuroscientists to participate in meetings and conferences with speech-language pathology organizations and related professional
rehabilitation organizations.
· Request funding from professional organizations such as the American Speech-Language-Hearing Association (ASHA) and the Dysphagia
Research Society ( DRS) to co-sponsor meetings with neuroscientific organizations.
· Request funding from organizations such as the National Institutes of Health ( NIH), the National Institute on Deafness and Other Communication
Disorders ( NIDCD), the National Institute of Neurological Disorders and Stroke ( NINDS), and the National Institute on Aging ( NIA) to host
consensus conference with neuroscientists and multidisciplinary teams comprising rehabilitation specialists and/or gerontologists.
2. Identify optimal ways to measure (quantitatively) the neural plastic changes pre- and postswallowing treatment/rehabilitation.
Prior Direction: The outcome of swallowing rehabilitation has focused primarily on physiology of the oropharyngeal swallow with emphasis on
aspiration or penetration of material in the airway before, during, or after the swallow. Secondary outcomes such as health status, diet variations,
dysphagia-specific quality of life (McHorney, Bricker, Kramer, et al., 2000; McHorney, Bricker, Robbins, et al., 2000; McHorney et al., 2002), and
patient satisfaction have only begun to be explored. Currently, there are few outcome measures for neural plastic changes postrehabilitation.
Suggested Action: Collaborate with a variety of disciplines—including neuroscientists, radiologists, neurologists, gerontologists, and medical
physicists—to facilitate interdisciplinary research, to recommend and test optimal methods (or a combination of methods; see Table 7) to measure
neural plastic changes in human populations of different ages and with neurogenic dysphagia.
3. Identify potential animal models that may be used for future research to evaluate ways to measure neural plastic changes as well as treatment/
rehabilitation outcomes pre- and postbrain injury/damage. If there are no animal models available or deemed appropriate, then collaborate with
neuroscientists to study swallow function in “normal” ( healthy) human development, “normal human aging,” sudden neurological events such as stroke
and traumatic head injury, and degenerative diseases such as Parkinson’s disease or amyotrophic lateral sclerosis.
Prior Direction: Neuroscientists have studied rodents, cats, sheep, and primates to assess discrete portions of the swallow but have not found a model that
evaluates the swallow function as defined by speech pathology, including the oral preparatory, oral transition, pharyngeal, and upper esophageal
phases of the swallow. Perhaps we need to reformulate our models of swallowing when generalizing from animal to human models.
B. To promote translational research by designing a systematic progressive research plan based upon current evidence of human rehabilitation in swallowing,
animal models, and clinical practice.
1. Replicate (refine) existing behavioral treatments to further define neural plastic, in addition to the more traditional behavioral, physiological, health,
nutrition, and quality-of-life outcomes.
Prior Direction: Based on systematic literature reviews, there are primarily Phase I and Phase II studies published, with very few evaluating the neural
plastic changes in normal or brain damaged adults (see Tables 1–4). By replicating existing studies with the addition of current imaging methodologies,
neural plastic changes may be assessed and compared with other outcome measures to define those that would be most useful clinically.
Suggested Action:
· Form a collaborative task force with professional organizations such as ASHA, DRS, the Organization for Human Brain Mapping (OHMB), the
Department of Veterans Affairs ( VA), and NIH to develop prioritization and a systematic research plan to replicate existing treatments with the
expansion of design and methodology to assess for potential neural plastic changes.
· Establish a patient-oriented research consortium—academic medical centers with interested teams of SLPs, neuroscientists, imagers, gerontologists,
pediatricians, and rehabilitative specialists will collaborate in a coordinated manner to conduct investigations of specified age groups, patient
populations, research designs, and outcome measures to elucidate the interrelationship of swallowing, neural plasticity, and rehabilitation.
Example: Chin Tuck
The chin tuck strategy has been demonstrated to be active ( Phase I and II studies) but is traditionally thought of as a compensatory strategy with no long-
term changes in swallow physiology if the strategy is not incorporated during each swallow. However, there are no studies assessing potential neural
plastic changes using this technique. Nor has there been a systematic approach to measuring the technique across the potential principles set forth
by neuroscientists such and Kleim and Jones (2008). For example, chin tuck may be a strategy that would maintain swallow function until the individual
recovered from a stroke ( Use It or Lose It) or would promote improved swallow function temporarily ( Use It and Improve It). Such neural plastic
principles have not been evaluated, and these principles may hold true for additional compensatory strategies (see Table A-1). Table A-1 is a
suggested approach to outlining a systematic hypothesis and assessment of principles and rehabilitation options.
S298 Journal of Speech, Language, and Hearing Research • Vol. 51 • S276–S300 • February 2008
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
Appendix (p. 2 of 3). Suggested goals and methods.
Table A-1. Suggested approach to outlining a systematic hypothesis and assessment of both principles and
rehabilitation options (see B1 example).
Treatment Chin tuck Head rotation
Animals No No
Humans Yes Yes
Behavioral Tx Active +/– Yes (+) Yes (+)
Principles of Neural Plasticity
Use It or Lose Ita Hypothesis #1 Hypothesis #1
Use It and Improve Itb Hypothesis #2 Hypothesis #2
Specificityc — —
Repetition Mattersd — —
Intensity Matterse — —
Time Mattersf — —
Salience Mattersg — —
Age Mattersh — —
Transferencei — —
Interferencej — —
Note. Tx = treatment or therapy.
a
Failure to drive specific brain functions can lead to functional degradation. b Training that drives a specific brain function can
lead to an enhancement of that function. c The nature of the training experience dictates the nature of the plasticity. d Induction of
plasticity requires sufficient repetition. e Induction of plasticity requires sufficient training intensity. f Different forms of plasticity
occur at different times during training. g The training experience must be sufficiently salient to induce plasticity. h Training-
induced plasticity occurs more readily in younger brains. iPlasticity in response to one training experience can enhance the
acquisition of similar behaviors. jPlasticity in response to one experience can interfere with the acquisition of other behaviors.
Additional examples for systematic research: The Work Group identified three treatments with potential variables, measures, and mechanics in Table 7
as priorities for future research.
2. Identify rehabilitation techniques that have no Phase I or II studies and further define neural plastic, behavioral, physiological, health, nutrition, and
quality-of-life outcomes.
Prior Direction: Rehabilitation techniques are used in clinical practice but do not have the published evidence to support use of the technique ( No Phase I,
II, or III studies). By identifying those techniques, future research may be initiated to include assessment of potential neural plastic changes in adults
with normal brain function or with brain damage (see Tables 1–4) and may be designed to include the principles as set forth by neurorehabilitation
scientists. These existing treatments may be assessed and compared with other outcome measures to define those that would be most clinically useful.
Suggested Action: Form a collaborative task force with professional organizations such as ASHA, DRS, OHMB, NIH, and VA to develop a targeting
and systematic research plan to replicate existing treatments and assess for potential associated neural plastic changes.
3. Review treatments that may be paired during rehabilitation for future systematic research.
Prior Direction: Research has typically evaluated one treatment technique at a time, but in reality, clinicians apply a variety of techniques during
interventions. For example: Chin tuck, thermal-tactile stimulation, and bolus viscosity may all be used in a patient with delayed swallow initiation.
The evidence for combined treatment is nonexistent, and the potential associated neural plastic changes are also unknown.
Example: Lingual Strengthening/Tongue Exercise ( TE) With or Without Chin Tuck (CT)
“Motor without swallow” strengthening exercises, when performed repetitively and intensely, have been associated with improved strength in both
animals and humans, and changes in swallowing ( behavioral plasticity) in humans. However, the necessary repetition and intensity may take time to
be effective ( Repetition, Intensity, Time Matters). Compensatory strategies (e.g., chin tuck) often are implemented by patients with dysphagia early
poststroke or trauma or during the acute phases of chemoradiation therapy to permit oral nutritional intake ( Use It or Lose It, Use It and Improve It),
albeit limited to a modified diet and thickened fluids in many cases. A systematic approach to measuring outcomes related to rigorous tongue exercise
“motor without swallow” only and NPO compared to the same TE protocol performed by patients with swallowing facilitated, even if only allowing
limited intake, by a compensatory strategy would permit examination of the principles set forth by Kleim and Jones (2008), as indicated in Table A-2.
Such designs are essential for hypothesis testing and for clarifying the usefulness of applying principles of neural plasticity to determine the optimal
combination for rehabilitation strategic planning. The “motor without swallow” tasks raise provocative questions applicable to study in animal models
(Connor et al., 2005) as well as humans (Robbins et al., 2005; Robbins, Gensler, et al., 2007; Robbins, Kays, et al., 2007).
Robbins et al.: Neural Plasticity, Swallowing, and Dysphagia Rehabilitation S299
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
Appendix (p. 3 of 3). Suggested goals and methods.
Table A-2. Comparison of tongue exercise (TE) alone to tongue exercise with chin tuck (CT; see B3 example).
Treatment TE alone TE and CT
Animals Yes —
Humans Yes Yes
Behavioral Tx Active +/– Yes Yes
Principles of Neural Plasticity
Use It or Lose It — Hypothesis #1
Use It and Improve It — Hypothesis #2
Specificity — —
Repetition Matters Hypothesis #1 Hypothesis #3
Intensity Matters Hypothesis #2 Hypothesis #4
Time Matters — Hypothesis #5
Salience Matters — —
Age Matters — —
Transference — —
Interference — —
Note. For an explanation of the Principles of Neural Plasticity, see the note at the bottom of Table A-1.
4. Assess the principle of Learning Matters (cognitive issues) relative to swallow function.
Prior Direction: Anecdotal clinical experience has suggested that individuals with poor cognitive function do not benefit from rehabilitation strategies,
but the principle of Learning Matters has not been defined in the literature.
Suggested Action: Invite professional organizations such as the Society for Neuroscience, the Alzheimer’s Association, and the NIH/NIA or National
Institute of Mental Health ( NIMH) to join ASHA and the American Psychological Association (APA) in developing a systematic research plan to evaluate
the principle of Learning Matters as set forth by our neuroscience colleagues. Patients with Parkinson’s disease with or without associated dementia
could be one excellent population (two subpopulations) for study. Research should include control (no treatment), behavioral, and nonprofessional
models to assess.
5. Identify specific neurogenic diseases or disorders that may be most appropriate for assessment of neural plastic changes in swallow function, may be
duplicated in animal models, and may respond to specific principles for rehabilitation.
Prior Direction: Although Phase I and II studies may originally have been initiated for rehabilitation strategies in a specific population, the treatment
has since been transferred clinically to a variety of diseases and disorders. For example: Supraglottic and super supraglottic swallowing techniques
were initially developed for head and neck cancer populations but have migrated to use with neurogenic patient populations. As a result, there is limited
evidence to support the transfer of such treatments clinically. In addition, there are few neural plastic measures to assess the outcome of such treatments
in neurogenic populations.
Suggested Action: Form a collaborative task force with related professional organizations to set forth hypotheses for the best disorders/disease
populations to assess neural plastic changes and rehabilitation principles.
Example: Parkinson’s disease may be a population to assess both voice and swallowing problems when examining treatments focused on respiratory
techniques.
C. To share the results of the consensus meetings and task force reports with funding resources, researchers, and clinicians.
Suggested Action:
· Publish peer-reviewed articles and/or a newsletter across disciplines.
· Present collaborative panels during professional and research meetings and conferences.
· Present documents to professional organizations and agencies with funding resources.
· Encourage graduate training programs and new investigator conferences to include neuroscience collaboration as a portion of the experience.
S300 Journal of Speech, Language, and Hearing Research • Vol. 51 • S276–S300 • February 2008
Downloaded From: http://jslhr.pubs.asha.org/ by a Universidad De Chile User on 04/16/2014
Vous aimerez peut-être aussi
- How I Use The Evidence in Dysphagia Management (2) : A Question of TasteDocument3 pagesHow I Use The Evidence in Dysphagia Management (2) : A Question of TasteSpeech & Language Therapy in Practice100% (3)
- Penasp ScaleDocument4 pagesPenasp Scaleapi-114739487Pas encore d'évaluation
- PmvbedsideevaluationDocument2 pagesPmvbedsideevaluationapi-114739487Pas encore d'évaluation
- PR Earth Users Guide EMILY1Document2 pagesPR Earth Users Guide EMILY1Azim AbdoolPas encore d'évaluation
- SP Patienthandout AphasicpatientDocument1 pageSP Patienthandout Aphasicpatientapi-11473948750% (2)
- ClockdrawingDocument2 pagesClockdrawingapi-114739487Pas encore d'évaluation
- Giesecke, Kay - 3-D Apraxic Therapy For KidsDocument6 pagesGiesecke, Kay - 3-D Apraxic Therapy For KidsampiccaPas encore d'évaluation
- To Taste or Not To TasteDocument3 pagesTo Taste or Not To TasteSpeech & Language Therapy in PracticePas encore d'évaluation
- Oral and Written Language Scales Listening Comprehension and Oral Expression (OWLS)Document13 pagesOral and Written Language Scales Listening Comprehension and Oral Expression (OWLS)alessarpon7557Pas encore d'évaluation
- Fois ScaleDocument1 pageFois Scalemaria.castillo1047897Pas encore d'évaluation
- The Quality of Life in The Dysarthric Speaker (QoL-DyS)Document15 pagesThe Quality of Life in The Dysarthric Speaker (QoL-DyS)enfanat23Pas encore d'évaluation
- Rev Grandfather PassageDocument1 pageRev Grandfather PassageAragornn ElessarrPas encore d'évaluation
- SLP Case StudyDocument8 pagesSLP Case StudyMaria Fernanda Leiva ArguelloPas encore d'évaluation
- Chapter 24 - The Solar SystemDocument36 pagesChapter 24 - The Solar SystemHeather Blackwell100% (1)
- Cilt HandoutDocument4 pagesCilt Handoutapi-454269640Pas encore d'évaluation
- Prevention Program BrochureDocument2 pagesPrevention Program Brochureapi-232834696Pas encore d'évaluation
- Dysphagia in The Elderly (Marco Teoìrico)Document12 pagesDysphagia in The Elderly (Marco Teoìrico)Nutriologo Luis Garcia CampechanoPas encore d'évaluation
- Cog RehabDocument55 pagesCog RehabHarsha RamchurnPas encore d'évaluation
- Physical Therapy and Occupational Therapy in Parkinson S DiseaseDocument15 pagesPhysical Therapy and Occupational Therapy in Parkinson S DiseaseGerman BuyattiPas encore d'évaluation
- Admission:Discharge Criteria in Speech-Language Pathology - ASHADocument16 pagesAdmission:Discharge Criteria in Speech-Language Pathology - ASHANádia MarquesPas encore d'évaluation
- Diseases of Esophagus.Document3 pagesDiseases of Esophagus.Isabel Castillo100% (2)
- Cognition and Falls HandoutDocument1 pageCognition and Falls Handoutapi-232834696Pas encore d'évaluation
- Aphasia: Western Aphasia Battery (WAB)Document13 pagesAphasia: Western Aphasia Battery (WAB)amandaPas encore d'évaluation
- Post Stroke WritingDocument9 pagesPost Stroke WritingAdi ParamarthaPas encore d'évaluation
- Effective SLPDocument10 pagesEffective SLPRené Ignacio Guzmán SalgadoPas encore d'évaluation
- Brusie Boyce AtkinsonDocument26 pagesBrusie Boyce AtkinsonEduardoCórdovaPas encore d'évaluation
- Mbs De-IdentifiedDocument2 pagesMbs De-Identifiedapi-645942287Pas encore d'évaluation
- 2014mshahandouts StoeckelDocument37 pages2014mshahandouts StoeckelAna Vogeley100% (1)
- AatpainassessmentDocument1 pageAatpainassessmentapi-114739487Pas encore d'évaluation
- AAC GuideDocument23 pagesAAC Guidejames.benedik92Pas encore d'évaluation
- McCurtin - 2012 - Evidence Based Practice in Speech Language TherapyDocument16 pagesMcCurtin - 2012 - Evidence Based Practice in Speech Language TherapymaximilianogaetePas encore d'évaluation
- Word Meaning Map I PDFDocument0 pageWord Meaning Map I PDFBrian HaynesPas encore d'évaluation
- How - . - I Train Others in Dysphagia.Document5 pagesHow - . - I Train Others in Dysphagia.Speech & Language Therapy in PracticePas encore d'évaluation
- 1 - Imp - The-Speech-and-Language-EvaluationDocument5 pages1 - Imp - The-Speech-and-Language-EvaluationMuskaan KhannaPas encore d'évaluation
- Anna Basso (Auth.), Audrey L. Holland PH.D., Margaret M. Forbes Ph.D. (Eds.) - Aphasia Treatment - World Perspectives-Springer US (1993)Document384 pagesAnna Basso (Auth.), Audrey L. Holland PH.D., Margaret M. Forbes Ph.D. (Eds.) - Aphasia Treatment - World Perspectives-Springer US (1993)jhernandez8394Pas encore d'évaluation
- Adductor Spasmodic Dysphonia: A Case For Speech and Language TherapyDocument3 pagesAdductor Spasmodic Dysphonia: A Case For Speech and Language TherapySpeech & Language Therapy in PracticePas encore d'évaluation
- SC22 Ukrainetz Teresa ExpositoryDocument21 pagesSC22 Ukrainetz Teresa Expositorygerardo.banalesPas encore d'évaluation
- TxreportmulticulturalDocument4 pagesTxreportmulticulturalapi-294798019Pas encore d'évaluation
- F S D G S: Eeding and Wallowing Ysfunction IN Enetic YndromesDocument11 pagesF S D G S: Eeding and Wallowing Ysfunction IN Enetic YndromespaulaPas encore d'évaluation
- FTP Phase 3 Soap NoteDocument1 pageFTP Phase 3 Soap Noteapi-313722056Pas encore d'évaluation
- Fluency ShapingDocument83 pagesFluency ShapingAltaf HasenPas encore d'évaluation
- Articulation and Phonological Processess SummarisedDocument2 pagesArticulation and Phonological Processess SummarisedSuné GreeffPas encore d'évaluation
- EMSTDocument10 pagesEMSTPilar Aguilera LópezPas encore d'évaluation
- Just For Adults Word RelatDocument40 pagesJust For Adults Word RelatMTRC SLPPas encore d'évaluation
- Tongue Twisters For Children To ReciteDocument3 pagesTongue Twisters For Children To ReciteChris MohankumarPas encore d'évaluation
- Reading Comprehension StrategiesDocument47 pagesReading Comprehension StrategiesJade H JamesPas encore d'évaluation
- Rainbow PassageDocument1 pageRainbow PassagePrriya RaathorePas encore d'évaluation
- Noun Derivation in LutirikiDocument74 pagesNoun Derivation in LutirikiBryan Birama0% (1)
- Objetivos ICF-Speech-Sound-Disorder (ASHA)Document2 pagesObjetivos ICF-Speech-Sound-Disorder (ASHA)labavillaPas encore d'évaluation
- Duffy Apraxia of SpeechDocument6 pagesDuffy Apraxia of SpeechRicardo OrdóñezPas encore d'évaluation
- 460 VoicedvsVoicelessDocument2 pages460 VoicedvsVoicelessNOR-ALI SOUDPas encore d'évaluation
- Clinical Reasoning Cycle PosterDocument1 pageClinical Reasoning Cycle PosterSigrid BristowPas encore d'évaluation
- Understanding Childhood Apraxia: Super Duper Handy Handouts!Document3 pagesUnderstanding Childhood Apraxia: Super Duper Handy Handouts!Staci NeustadtPas encore d'évaluation
- Printable Course Bookn : I."Document289 pagesPrintable Course Bookn : I."Kristen DesPommier EgerPas encore d'évaluation
- Autism and LenguageDocument13 pagesAutism and LenguageSergio Andres Villegas VillaPas encore d'évaluation
- Abbreviated Profile of Hearing Aid BenefitDocument4 pagesAbbreviated Profile of Hearing Aid BenefitAnn VillablancaPas encore d'évaluation
- Sample Treatment PlanDocument3 pagesSample Treatment PlanLiza NaumannPas encore d'évaluation
- Effectiveness of Deep Pharyngeal Neuromuscular Stimulation Versus Thermal Gustatory Stimulation in Decreasing Length of Swallow Initiation and Improving Lingual Movements - Maria H WillisDocument54 pagesEffectiveness of Deep Pharyngeal Neuromuscular Stimulation Versus Thermal Gustatory Stimulation in Decreasing Length of Swallow Initiation and Improving Lingual Movements - Maria H WillisconstantineeliaPas encore d'évaluation
- Diagnosis Treatment Planning FormDocument13 pagesDiagnosis Treatment Planning FormSitiKhadijahPas encore d'évaluation
- Occupational Therapy and Life Course Development: A Work Book for Professional PracticeD'EverandOccupational Therapy and Life Course Development: A Work Book for Professional PracticePas encore d'évaluation
- How To Be A Better StudentDocument2 pagesHow To Be A Better Studentct fatima100% (1)
- AMO Exercise 1Document2 pagesAMO Exercise 1Jonell Chan Xin RuPas encore d'évaluation
- Switching Lab-05b Configuring InterVLAN RoutingDocument2 pagesSwitching Lab-05b Configuring InterVLAN RoutingHernan E. SalvatoriPas encore d'évaluation
- Contemp Person Act.1Document1 pageContemp Person Act.1Luisa Jane De LunaPas encore d'évaluation
- Compact 1.8" Height Standardized Installation 9 Months To Flight Powerful and LightweightDocument2 pagesCompact 1.8" Height Standardized Installation 9 Months To Flight Powerful and LightweightStanley Ochieng' OumaPas encore d'évaluation
- ANS145 - Beef Cattle ProductionDocument52 pagesANS145 - Beef Cattle ProductionEgie BulawinPas encore d'évaluation
- Assessment 4 PDFDocument10 pagesAssessment 4 PDFAboud Hawrechz MacalilayPas encore d'évaluation
- AAR Shell ProgrammingDocument13 pagesAAR Shell ProgrammingMarimuthu MuthaiyanPas encore d'évaluation
- The Beauty of Laplace's Equation, Mathematical Key To Everything - WIRED PDFDocument9 pagesThe Beauty of Laplace's Equation, Mathematical Key To Everything - WIRED PDFYan XiongPas encore d'évaluation
- Auditory Evoked Potentials - AEPs - Underlying PrinciplesDocument19 pagesAuditory Evoked Potentials - AEPs - Underlying PrinciplesMansi SinghPas encore d'évaluation
- SodiumBenzoate PDFDocument3 pagesSodiumBenzoate PDFyotta024Pas encore d'évaluation
- Needle BasicsDocument31 pagesNeedle BasicsARYAN RATHOREPas encore d'évaluation
- 02 Chapter 2 - Corporate Governance MechanismDocument19 pages02 Chapter 2 - Corporate Governance MechanismHanis ZahiraPas encore d'évaluation
- Attachment 1 Fiber Data SheetDocument2 pagesAttachment 1 Fiber Data SheetflavioovPas encore d'évaluation
- 2011-11-09 Diana and AtenaDocument8 pages2011-11-09 Diana and AtenareluPas encore d'évaluation
- Slides - SARSDocument191 pagesSlides - SARSCedric PoolPas encore d'évaluation
- Big Bang Theory EpisodesDocument24 pagesBig Bang Theory EpisodesBroly dbzPas encore d'évaluation
- Grasa LO 915Document2 pagesGrasa LO 915Angelo Carrillo VelozoPas encore d'évaluation
- Afzal ResumeDocument4 pagesAfzal ResumeASHIQ HUSSAINPas encore d'évaluation
- Cheerios Media KitDocument9 pagesCheerios Media Kitapi-300473748Pas encore d'évaluation
- Islamiyat ProjectDocument21 pagesIslamiyat ProjectSubhan Khan NiaziPas encore d'évaluation
- 03-F10 Planned Job ObservationDocument1 page03-F10 Planned Job ObservationSn Ahsan100% (1)
- FHHR 013 Red Tag Procedure PDFDocument5 pagesFHHR 013 Red Tag Procedure PDFN3N5YPas encore d'évaluation
- Rocker ScientificDocument10 pagesRocker ScientificRody JHPas encore d'évaluation
- SKF Shaft Alignment Tool TKSA 41Document2 pagesSKF Shaft Alignment Tool TKSA 41Dwiki RamadhaniPas encore d'évaluation
- Uts Cmo Module 5Document31 pagesUts Cmo Module 5Ceelinah EsparazPas encore d'évaluation
- 7 ElevenDocument80 pages7 ElevenakashPas encore d'évaluation
- Individual Daily Log and Accomplishment Report: Date and Actual Time Logs Actual AccomplishmentsDocument3 pagesIndividual Daily Log and Accomplishment Report: Date and Actual Time Logs Actual AccomplishmentsMarian SalazarPas encore d'évaluation