Académique Documents
Professionnel Documents
Culture Documents
Ultrasound Basics
Transféré par
JCopyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Ultrasound Basics
Transféré par
JDroits d'auteur :
Formats disponibles
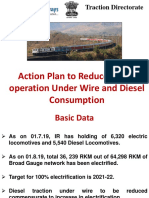
ULTRASOUND
BASICS Erika Wierman, DVM
www.eimedical.com • 1.866.365.6596 • info@eimedical.com
TABLE OF CONTENTS
Table Of Contents ii
How To Read An Ultrasound Image 1
How Does Ultrasound Work? 4
What Impact Does Frequency Have On Ultrasound Imaging? 5
Choosing the Correct Transducer 6
Frequency 6
Depth 6
Shape of array 6
Length of array 7
Shape of transducer 7
Understanding Gain 8
Imaging a Deep Structure 8
Poor Contact 8
Monitor Brightness Setting 9
Increasing Gain Settings to Overcome Shadowing 9
When to Adjust Gain 9
Want More? 10
© 2019 E.I. Medical Imaging
HOW TO READ AN ULTRASOUND IMAGE
Have you ever looked at an ultrasound image and wondered what you are looking at?
Ever wonder which end is up? When others are discussing bull or heifer, ovarian diag-
nosis, or metritis treatment, are you still looking to decide just what it is?
Well, if you feel left in the dark when it comes to ultrasound images, let’s start with
the basics.
Ultrasound is a non-invasive, immediate tool used to image tissue. It will not pene-
trate bone (like an X-Ray).
The first step to help you read the ultrasound image is to be familiar with the
anatomy that you are imaging. Various body tissues conduct sound differently. Some
tissues absorb sound waves while others reflect them. The density of the tissue
dictates the speed at which the echoes return.
If you remember that FLUID is always BLACK and TISSUE is always GRAY. The denser
the tissue, is the brighter white it will appear in ultrasound, with the brightest white
being bone.
Ultrasound Gray Scale
BONE TISSUE FLUID
E.I. Medical Imaging Ultrasound Basics...1
Now, let’s look at a few images...
Bovine Ultrasound: Early Pregnancy
Bovine Ultrasound: Heifer Calf
E.I. Medical Imaging Ultrasound Basics...2
Equine Ultrasound: 13-day Pregnancy
Sheep Ultrasound: 63-day Pregnancy
Remember, the more images you look at, the easier they will be to read!
E.I. Medical Imaging Ultrasound Basics...3
HOW DOES ULTRASOUND WORK?
If you’re new to ultrasound, an image may look like nothing more than a swirling
array of grey tones on the screen. Interpretation requires an understanding of
anatomy and physiology, but also of how ultrasound technology functions.
Consider the sonar produced by a bat in flight. The bat emits high frequency sounds,
which then bounce off of objects in its proximity and return to the bat. The animal
uses the strength, direction, and timing of the returning sound to determine where
those objects are and to avoid a collision.
The transducer (probe) of an ultrasound system emits
high frequency sound waves, which transmit into the
tissue beneath a body surface and reflect off struc-
tures along the way. Dense or rigid structures don’t
allow the sound waves to pass through, and therefore
reflect most back to the transducer. Such structures
will create a strong echo, which appears bright white
on the screen. By comparison, fluid transmits sound waves flawlessly; no returning
signal means fluid appears black on the screen.
Naturally, most tissues will fall somewhere in between, appearing some shade of
grey. Fluid with a high degree of cellular debris might look black with floating flecks
of grey or white (snowglobe effect). Hepatic or splenic parenchyma will be a medium
shade of grey, and the surface of fetal bone or bladder stones will be nearly white.
The time required for the signal to return tells the ultrasound how far that structure
is from the probe surface. For example, if there is a long delay from the signal trans-
mission to its return, the ultrasound interprets that as a structure that is situated well
below the surface, and therefore it
will appear lower on the screen in the
image that is produced.
In this image of a pregnancy, you’ll
see that the fluid within the uterus is
black, the fetal and uterine tissues are
varying shades of grey, and the fetal
skeleton is white.
The top of the image corresponds to
the surface of the transducer, while
the bottom is the deepest section of
tissue being imaged.
E.I. Medical Imaging Ultrasound Basics...4
WHAT IMPACT DOES FREQUENCY HAVE ON ULTRASOUND IMAGING?
You’ve probably noticed that the transducers, or
probes, on your ultrasound system are named
or marked with a number followed by MHz,
most likely in the 1-20 range. Often this is how a L7HD [5-9 MHz, 15cm depth]
company advertises their products—for example,
a 7MHz linear rectal transducer. Perhaps you’ve wondered what this number refers to
or the significance of having a higher or lower number on your probe.
This number (or range of numbers) refers to the frequency of the sound waves
produced by that particular transducer. As sound waves travel through tissue, some
of them are absorbed or attenuated, and some are reflected back to the transducer
to produce an image. Sound waves of a higher frequency are more affected by atten-
uation, but due to their shorter wavelength are also more accurate in discriminating
between two adjacent structures. In contrast, lower frequency sound waves are not
as easily absorbed but, due to the longer wavelength, may not discern smaller struc-
tures as well.
What does that mean for you? Transducers with
CL3E [2-6.4 MHz, 30cm depth]
higher frequencies produce a higher resolution
image but do not penetrate as well. They are
used for imaging small, superficial structures at
shallow depths and high resolution. Powerful
low-frequency probes are required for imaging
at greater depths, although the resulting image may not have the fine detail of one
produced at higher frequencies. When operating an ultrasound system, then, it is
prudent to select a transducer with the appropriate frequency for the chosen applica-
tion.
Fortunately, most modern transducers are broadband, which means that they can
operate at a range of frequencies. A good rule of thumb is to scan at the highest
frequency possible for the penetration that you need to achieve, so that you can opti-
mize the resolution of your image regardless of the depth. Increasing the frequency
is a good way to improve the resolution of your image, and decreasing the frequency
will help you if you’re struggling to reach deeper structures.
In veterinary medicine, for example, high frequency transducers in the 12-20MHz
(~2-6cm depth) range are used to image superficial nerves (regional anesthesia),
tendons, and eyes, among other things. Companion animal abdominal and cardiac
exams as well as large animal transrectal reproductive exams are typically performed
in the 5-12MHz (~6-15cm depth) range, and transabdominal and thoracic imaging
of horses, cattle, small ruminants, swine, and even large dogs may be done in the
1-5MHz (~15-30cm depth) range.
E.I. Medical Imaging Ultrasound Basics...5
CHOOSING THE CORRECT TRANSDUCER
There are an overwhelming number of transducer (probe)
options on the market these days, marketed for different
species and applications. What do you need to consider
when selecting one? Whether you are shopping for a new
L14X
system or transducer, or simply deciding which of your
current probes to use for a specific purpose, here are a few
tips to keep in mind.
Frequency
The frequency range can have a big effect on the image that you produce, so always
remember the bottom line—higher frequency equals greater resolution, lower
frequency equals better penetration.
Depth
Closely related to frequency is depth of penetration.
If you are imaging the abdomen of a horse, you will need
significantly greater depth than you would if you were CL3E
imaging superficial nerves and tendons in a dog, for example.
In order to achieve this, you’ll need a lower frequency transducer to maximize depth.
While some ultrasound models will automatically change the frequency as you adjust
the depth, others allow you to adjust the two independent of each other. Find the
depth that you need first, and then adjust the frequency to maximize the resolution
while maintaining the penetration.
Shape of array
The array is the part of the probe in contact with the C6E
patient—it is most often made up of a grayish rubber mate-
rial covering the crystal elements that produce the sound
waves to create an image. Arrays can be flat or curved
(convex), and the shape of the array will determine the shape of the image you see.
A flat array produces a square or rectangular image, and a curved array will produce a
wedge- or pie-shaped image.
You can interpret this as a wider field of view with a convex probe, but it also means
that you may see some distortion or loss of resolution in the far field, where sound
beams spread out as they get further from the probe. The tighter the radius (the more
profound the curvature of the array), the more you will see that effect. We tend to use
convex probes in body cavities like the abdomen and thorax and linear probes for
small, superficial structures like tendons, nerves, and vessels.
E.I. Medical Imaging Ultrasound Basics...6
Length of array
A longer array will fit more anatomy beneath it, making it L3ASE
more appropriate for larger or deeper structures. A short
array is appropriate for smaller structures so that they
appear larger on the screen relative to the probe. This is one
reason that a linear rectal probe, for example, is not the best choice for equine distal
limb exams; the transverse sections of the tendons will appear relatively small within
the longer array.
The animal science (carcass) probe is an example of a specialty probe with an excep-
tionally long array, designed to capture and measure an image of a large section of
muscling in beef cows.
Shape of transducer
The shape of the probe housing itself is often designed for
a specific purpose. Most common probes have a traditional
grip with the array on the far end of the housing, intended CLI3E
to be placed on top of a body surface and held in the palm
of the hand. Rectal probes are the most obvious exception in veterinary medicine,
where the array is oriented along the side of the probe and the cable exits at the rear.
E.I. Medical’s CLi transducers are an interesting hybrid design—they incorporate the
array of our large transabdominal probe into a rectal grip. This unique design allows
the probe to be used for both applications.
By understanding these transducer properties, you will be better equipped to choose
the correct tool for your next job!
E.I. Medical Imaging Ultrasound Basics...7
UNDERSTANDING GAIN
low gain high gain optimal gain
All ultrasounds have gain control. It’s often a knob, button, and/or a series of sliders
on the console, and it’s one of the most used and adjusted scanning parameters... but
do you know what it really does?
Most people think of gain as a brightness adjuster, and while it’s true that turning
your gain up will brighten the image, it’s helpful to understand how it actually works.
Gain is a uniform amplification of the ultrasonic signal that is returning to the trans-
ducer after it travels through the tissue. So rather than brightening the monitor, the
image on the screen is whitened by a uniform margin, as though the returning signal
is stronger than it is, to make it easier to see.
However, caution should be taken to not “over-gain.” Too much amplification can
result in a washed-out image with loss of detail or production of artifact. If you find
that you are constantly reaching for the gain control, consider why your image may
be darker than you prefer.
Imaging a Deep Structure
If the signal is being strongly attenuated because you’re trying to see anatomy that
is quite deep to the body surface, consider lowering the operating frequency of your
probe. As outlined in previous blog entries, lower frequency sound waves penetrate
more powerfully than higher frequencies do, so you can expect to get a stronger
returning signal.
Poor Contact
For ultrasound waves to travel efficiently, you need to make an effort to minimize
the interruptions between the transducer and the structures you’re examining.
Remember that air is the enemy of ultrasound, and even microscopic quantities of air
between the probe and body surface will impair transmission of the sound waves and
result in a dark image.
Consider clipping away hair, cleaning dirt and debris from the skin, prepping the
area with alcohol, and using a coupling gel to get the least possible disruption of
your ultrasound signal. For transrectal ultrasound, remove as much fecal material as
possible, and use liberal amounts of lubricant as a contact medium.
E.I. Medical Imaging Ultrasound Basics...8
Monitor Brightness Setting
Among your ultrasound machine’s settings you will likely find a way to change the
brightness of the actual LCD monitor. Like your mobile phone, you might determine
that you need to make adjustments based on the ambient light in your scanning
environment. You may be able to overcome the need for some gain by dialing up the
screen brightness.
Increasing Gain Settings to Overcome Shadowing
Dense structures such as bladder stones as well as gas within the tissue can cast
shadows in your image. Try changing patient or transducer positioning, performing a
re-check exam after gas has had a chance to move through, or fasting patients prior
to scheduled ultrasound exams.
Shadowing can also occur in the form of edge artifact, which occurs at the edges of
round structures. If you encounter this often, talk to your manufacturer’s customer
support team about changing settings such as harmonics and compounding to make
the ultrasound beam behave in such a way as to dampen these effects.
When to Adjust Gain
If you have considered all of these suggestions and your image is still dark, adjust
your gain as necessary to optimize the brightness of the image while preserving
detail.
E.I. Medical Imaging Ultrasound Basics...9
WANT MORE?
Enjoy more informative blog posts @ http://www.eimedical.com/blog.
Built for the toughest veterinary environments, our Ibex® ultrasound platforms are
the latest evolution of portable ultrasound technology. We deliver this with great
image quality and processing power, all in weather-sealed, lightweight units. All plat-
forms incorporate user-friendly patient management software. Transducer cables are
tested to 1.2 million flex cycles, ensuring seasons of uninterrupted use.
We are THE gold standard for veterinary ultrasound, used in top veterinary hospitals,
clinics and universities. For more information or for a demonstration, contact us at
1.866.365.6596 or visit us at www.eimedical.com to learn more.
E.I. Medical Imaging Ultrasound Basics...10
Vous aimerez peut-être aussi
- The Physics and Technology of Diagnostic Ultrasound: A Practitioner's Guide (Second Edition)D'EverandThe Physics and Technology of Diagnostic Ultrasound: A Practitioner's Guide (Second Edition)Pas encore d'évaluation
- Pass Ultrasound Physics Exam Study Guide ReviewD'EverandPass Ultrasound Physics Exam Study Guide ReviewÉvaluation : 4.5 sur 5 étoiles4.5/5 (2)
- Komoiboros Inggoris-KadazandusunDocument140 pagesKomoiboros Inggoris-KadazandusunJ Alex Gintang33% (6)
- ESSAYSDocument5 pagesESSAYSDGM RegistrarPas encore d'évaluation
- Ultrasound Physics GuideDocument9 pagesUltrasound Physics GuideawansurfPas encore d'évaluation
- The Physics and Technology of Diagnostic Ultrasound: Study Guide (Second Edition)D'EverandThe Physics and Technology of Diagnostic Ultrasound: Study Guide (Second Edition)Pas encore d'évaluation
- Ultrasound ImagingDocument103 pagesUltrasound Imagingsolomong100% (1)
- Physics of UltarasoundDocument195 pagesPhysics of Ultarasoundhossam62683% (6)
- Basic UltrasoundDocument73 pagesBasic UltrasoundSuhazeli Abdullah100% (6)
- Lower Extremity Venous Protocol 14Document3 pagesLower Extremity Venous Protocol 14api-276847924Pas encore d'évaluation
- Ultrasound and DopplerDocument22 pagesUltrasound and Dopplerpri_292100% (1)
- Textbook of Cardiovascular Medicine in Dogs and Cats (VetBooks - Ir)Document1 112 pagesTextbook of Cardiovascular Medicine in Dogs and Cats (VetBooks - Ir)Jonathan Mann100% (1)
- Chord ProgressionDocument6 pagesChord ProgressiongernPas encore d'évaluation
- UltrasoundDocument104 pagesUltrasoundlrp sPas encore d'évaluation
- Basic Principles of Ultrasound.: Dr/Abd Allah Nazeer. MDDocument50 pagesBasic Principles of Ultrasound.: Dr/Abd Allah Nazeer. MDAmeer MattaPas encore d'évaluation
- Ultrasound Made EasyDocument7 pagesUltrasound Made EasyAnonymous ZUaUz1wwPas encore d'évaluation
- Ultrasound Imaging Basics ExplainedDocument14 pagesUltrasound Imaging Basics Explainedpriyadharshini100% (1)
- Introduction To Basic UltrasoundDocument25 pagesIntroduction To Basic UltrasoundAriadna Mariniuc100% (3)
- Ultrasound Basics Webinar SlidesDocument105 pagesUltrasound Basics Webinar SlidesVioleta Naghiu100% (3)
- UZVDocument56 pagesUZVGoran MaliPas encore d'évaluation
- Textbook of Urgent Care Management: Chapter 35, Urgent Care Imaging and InterpretationD'EverandTextbook of Urgent Care Management: Chapter 35, Urgent Care Imaging and InterpretationPas encore d'évaluation
- UltrasoundDocument78 pagesUltrasoundAmeer MattaPas encore d'évaluation
- Women's Imaging: MRI with Multimodality CorrelationD'EverandWomen's Imaging: MRI with Multimodality CorrelationMichele A. BrownÉvaluation : 5 sur 5 étoiles5/5 (1)
- WHO Ultrasound Manual Vol2 PDFDocument529 pagesWHO Ultrasound Manual Vol2 PDFRobert ChristevenPas encore d'évaluation
- Doppler Ultrasound PhysicsDocument12 pagesDoppler Ultrasound PhysicsMuhammad Shayan Farooq100% (1)
- Ultrasound ImagingDocument20 pagesUltrasound ImagingSitanshu SatpathyPas encore d'évaluation
- Medical Biophysics Ultrasound LecturesDocument69 pagesMedical Biophysics Ultrasound LecturesworkshoppePas encore d'évaluation
- Ultrasound Basics Principles ExplainedDocument106 pagesUltrasound Basics Principles Explainedtasawwur zahoorPas encore d'évaluation
- Sonography PhysicsDocument42 pagesSonography PhysicsAhmad AliPas encore d'évaluation
- Accutron HPDocument6 pagesAccutron HPsensaadPas encore d'évaluation
- Ultrasound Guided ProceduresDocument71 pagesUltrasound Guided Proceduresg1381821Pas encore d'évaluation
- Preguntas de Gineco ObstetriciaDocument21 pagesPreguntas de Gineco ObstetriciawatitorocaPas encore d'évaluation
- AIUM Medical Ultrasound SafetyDocument60 pagesAIUM Medical Ultrasound Safetyscuby660Pas encore d'évaluation
- Ultrasound PhysicsDocument26 pagesUltrasound PhysicsAmi Desai50% (2)
- Ultrasound Scanning of Fetal AnomalyDocument19 pagesUltrasound Scanning of Fetal AnomalyFA Khan0% (1)
- Zlib - Pub Radiography Essentials For Limited PracticeDocument657 pagesZlib - Pub Radiography Essentials For Limited PracticeLucjan KrawczyszynPas encore d'évaluation
- Critical Care Ultrasound NotesDocument32 pagesCritical Care Ultrasound Notesnot here 2make friends sorryPas encore d'évaluation
- Chapter 1-Contrast MediaDocument18 pagesChapter 1-Contrast MediaFisiha FikiruPas encore d'évaluation
- Emergency sonography for trauma: FAST protocolDocument101 pagesEmergency sonography for trauma: FAST protocolChavo Delocho100% (9)
- Imaging Abdominal Trauma Focus On FAST Revisi DR - BahtiarDocument54 pagesImaging Abdominal Trauma Focus On FAST Revisi DR - BahtiarJackson HakimPas encore d'évaluation
- Ultrasound Guidance - PollardDocument72 pagesUltrasound Guidance - Pollardmasquebolso100% (3)
- (Philip T. English DCR, Christine Moore DCR (Auth.Document188 pages(Philip T. English DCR, Christine Moore DCR (Auth.Åri Budianto100% (1)
- Basic Abdominal Ultrasound - BestDocument36 pagesBasic Abdominal Ultrasound - Bestifeanyi100% (2)
- Radiology OSCE Review: Key Imaging Findings and DiagnosesDocument44 pagesRadiology OSCE Review: Key Imaging Findings and DiagnosesWedha Jati Tyas100% (1)
- Practical Physics of UltrasoundDocument31 pagesPractical Physics of UltrasoundJazib ShahidPas encore d'évaluation
- Ultrasound Equipment Quality Assurance - CHAPTER 14Document3 pagesUltrasound Equipment Quality Assurance - CHAPTER 14Pengcab PARI Kota BekasiPas encore d'évaluation
- 2004 Emergency UltrasoundDocument226 pages2004 Emergency Ultrasoundpgiaf5935100% (1)
- Lesson 10 - UltrasoundDocument62 pagesLesson 10 - UltrasoundDesignPas encore d'évaluation
- Basics of UltrasoundDocument55 pagesBasics of UltrasoundDrChauhan100% (2)
- Medical Imaging JournalDocument44 pagesMedical Imaging JournalKamrulhak AnsariPas encore d'évaluation
- The Manchester Handbook of Ultrasound TechniquesDocument22 pagesThe Manchester Handbook of Ultrasound TechniquesAzie Azizah AGPas encore d'évaluation
- Palmer Ultrasound ImagingDocument354 pagesPalmer Ultrasound ImagingRajeshPilot100% (13)
- Acr Mri BiradsDocument3 pagesAcr Mri BiradsFilipe BarraPas encore d'évaluation
- MRIDocument274 pagesMRIGuillermo Sasso Pacheco100% (2)
- Contrast Media Administration Guidelines by The ACR (American College of Radiology) Version 6 - 2008Document92 pagesContrast Media Administration Guidelines by The ACR (American College of Radiology) Version 6 - 2008radiology_resources100% (25)
- ISUOGMidTrimester Guidelines 2011 PresentationDocument22 pagesISUOGMidTrimester Guidelines 2011 Presentationmihaela8023Pas encore d'évaluation
- MRI Artifacts - Detecting Distortions: Devi KrishnaDocument11 pagesMRI Artifacts - Detecting Distortions: Devi KrishnaDiya Krishna100% (1)
- Basic Abdominal Sonographic Anatomy and ProtocolDocument41 pagesBasic Abdominal Sonographic Anatomy and ProtocolMj Briones100% (5)
- Clinical PET/MRID'EverandClinical PET/MRIOnofrio Antonio CatalanoPas encore d'évaluation
- Basic Legal CitationDocument502 pagesBasic Legal CitationJ100% (1)
- Road DoctorDocument2 pagesRoad DoctorOsannah IrishPas encore d'évaluation
- AAHA Diabetes Guidelines - FinalDocument21 pagesAAHA Diabetes Guidelines - FinalKátia SouzaPas encore d'évaluation
- Equine-03-Review of The UsesDocument5 pagesEquine-03-Review of The UsesJPas encore d'évaluation
- 10.track1 .4-ForelimbDocument4 pages10.track1 .4-ForelimbJPas encore d'évaluation
- Tentative Seat Vacancy For CSAB Special Rounds-202Document92 pagesTentative Seat Vacancy For CSAB Special Rounds-202Praveen KumarPas encore d'évaluation
- Final DSL Under Wire - FinalDocument44 pagesFinal DSL Under Wire - Finalelect trsPas encore d'évaluation
- Https WWW - Gov.uk Government Uploads System Uploads Attachment Data File 274029 VAF4ADocument17 pagesHttps WWW - Gov.uk Government Uploads System Uploads Attachment Data File 274029 VAF4ATiffany Maxwell0% (1)
- Airforce Group Y: Previous Y Ear P AperDocument14 pagesAirforce Group Y: Previous Y Ear P Aperajay16duni8Pas encore d'évaluation
- 0807 Ifric 16Document3 pages0807 Ifric 16SohelPas encore d'évaluation
- Absenteeism: It'S Effect On The Academic Performance On The Selected Shs Students Literature ReviewDocument7 pagesAbsenteeism: It'S Effect On The Academic Performance On The Selected Shs Students Literature Reviewapi-349927558Pas encore d'évaluation
- God Love Value CoreDocument11 pagesGod Love Value CoreligayaPas encore d'évaluation
- The Forum Gazette Vol. 2 No. 23 December 5-19, 1987Document16 pagesThe Forum Gazette Vol. 2 No. 23 December 5-19, 1987SikhDigitalLibraryPas encore d'évaluation
- Lesson Plan Maam MyleenDocument7 pagesLesson Plan Maam MyleenRochelle RevadeneraPas encore d'évaluation
- Chapter 1Document11 pagesChapter 1Albert BugasPas encore d'évaluation
- Readers TheatreDocument7 pagesReaders TheatreLIDYAPas encore d'évaluation
- Financial Accounting and ReportingDocument31 pagesFinancial Accounting and ReportingBer SchoolPas encore d'évaluation
- The Secret Path Lesson 2Document22 pagesThe Secret Path Lesson 2Jacky SoPas encore d'évaluation
- Bhikkhuni Patimokkha Fourth Edition - Pali and English - UTBSI Ordination Bodhgaya Nov 2022 (E-Book Version)Document154 pagesBhikkhuni Patimokkha Fourth Edition - Pali and English - UTBSI Ordination Bodhgaya Nov 2022 (E-Book Version)Ven. Tathālokā TherīPas encore d'évaluation
- Dr. Xavier - MIDocument6 pagesDr. Xavier - MIKannamundayil BakesPas encore d'évaluation
- 2-Library - IJLSR - Information - SumanDocument10 pages2-Library - IJLSR - Information - SumanTJPRC PublicationsPas encore d'évaluation
- Forouzan MCQ in Error Detection and CorrectionDocument14 pagesForouzan MCQ in Error Detection and CorrectionFroyd WessPas encore d'évaluation
- Cookery-10 LAS-Q3 Week5Document7 pagesCookery-10 LAS-Q3 Week5Angeline Cortez100% (1)
- Grade 1 English For KidsDocument4 pagesGrade 1 English For Kidsvivian 119190156Pas encore d'évaluation
- Pembaruan Hukum Melalui Lembaga PraperadilanDocument20 pagesPembaruan Hukum Melalui Lembaga PraperadilanBebekliarPas encore d'évaluation
- Price and Volume Effects of Devaluation of CurrencyDocument3 pagesPrice and Volume Effects of Devaluation of Currencymutale besaPas encore d'évaluation
- Round Rock Independent School District: Human ResourcesDocument6 pagesRound Rock Independent School District: Human Resourcessho76er100% (1)
- INDEX OF 3D PRINTED CONCRETE RESEARCH DOCUMENTDocument15 pagesINDEX OF 3D PRINTED CONCRETE RESEARCH DOCUMENTAkhwari W. PamungkasjatiPas encore d'évaluation
- M2M RF - RHNDocument3 pagesM2M RF - RHNNur Nadia Syamira Bt SaaidiPas encore d'évaluation
- ToonHub - Articles of PartnershipDocument13 pagesToonHub - Articles of PartnershipKingPas encore d'évaluation
- Entrepreneurship and Small Business ManagementDocument29 pagesEntrepreneurship and Small Business Managementji min100% (1)
- Practical Research 1 - Quarter 1 - Module 1 - Nature and Inquiry of Research - Version 3Document53 pagesPractical Research 1 - Quarter 1 - Module 1 - Nature and Inquiry of Research - Version 3Iris Rivera-PerezPas encore d'évaluation