Académique Documents
Professionnel Documents
Culture Documents
The Diagnostic Dilemma of Thrombotic Thrombocytopenic Purpura/hemolytic Uremic Syndrome in The Obstetric Triage and Emergency Department: Lessons From 4 Tertiary Hospitals
Transféré par
Mahmoud DiaaDescription originale:
Titre original
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
The Diagnostic Dilemma of Thrombotic Thrombocytopenic Purpura/hemolytic Uremic Syndrome in The Obstetric Triage and Emergency Department: Lessons From 4 Tertiary Hospitals
Transféré par
Mahmoud DiaaDroits d'auteur :
Formats disponibles
Research www. AJOG.
org
OBSTETRICS
The diagnostic dilemma of thrombotic thrombocytopenic
purpura/hemolytic uremic syndrome in the obstetric triage
and emergency department: lessons from 4 tertiary hospitals
Caroline L. Stella, MD; John Dacus, MD; Edwin Guzman, MD; Pushpinder Dhillon, MD;
Kristin Coppage, MD; Helen How, MD; Baha Sibai, MD
OBJECTIVE: We report a series of occurrences of thrombotic thrombo- drome/preeclampsia, whereas patients who were seen in the ED had a
cytopenic purpura (TTP)/hemolytic uremic syndrome (HUS) in preg- diagnosis that is commonplace in the ED (panic attack, domestic vio-
nancy that emphasizes early diagnosis. lence, gastroenteritis). Latency from the onset of symptoms to diagno-
sis ranged from 1-7 days. Plasmapheresis treatments in early gestation
STUDY DESIGN: Fourteen pregnancies with TTP (n ⫽ 12) or HUS (n
resulted in favorable maternal-neonatal outcome. Maternal and perina-
⫽ 2) were studied. Analysis focused on clinical and laboratory find-
tal mortality rates were 25% each.
ings on examination, initial diagnosis, and treatment.
CONCLUSION: TTP/HUS is a challenging diagnosis in obstetric triage
RESULTS: There were 14 pregnancies in 12 patients; 2 cases of TTP
and ED areas. We propose a management scheme that suggests how to
were diagnosed as recurrent. Five women were admitted to the emer-
triage patients for early diagnosis in pregnancy.
gency department (ED), and 7 patients were admitted to an obstetrics
triage. Patients who were evaluated by an obstetrician were treated ini- Key words: hemolytic uremic syndrome, maternal and fetal mortality,
tially for hemolysis, elevated liver enzymes and low platelets syn- plasmapheresis, pregnancy, thrombotic thrombocytopenic purpura
Cite this article as: Stella CL, Dacus J, Guzman E, et al. The diagnostic dilemma of thrombotic thrombocytopenic purpura/hemolytic uremic syndrome in the
obstetric triage and emergency department: lessons from 4 tertiary hospitals. Am J Obstet Gynecol 2009;200:381.e1-381.e6.
T hrombotic thrombocytopenic pur-
pura (TTP)/ hemolytic uremic syn-
drome (HUS) are 2 microangiopathic
primary pathologic feature of TTP lies in
the formation of platelet aggregates, of
which the exact cause remains un-
and exaggerated renal abnormalities in
HUS.7 As such, TTP and HUS are consid-
ered to be a continuum of diseases with an
disorders that are both rare; they afflict 1 known.3 The most accepted postulate is unidentified common pathway.8-10
in 100,000 pregnancies to 1:1,000,000 endothelial damage from the abnormal The classic diagnosis of TTP includes
people in the general population1,2 The production and metabolism of the von the pentad of Coomb’s negative hemo-
Willebrand factor multimers that are lytic anemia, thrombocytopenia, neuro-
From the University of Cincinnati College of caused by severe deficiency of the von logic changes, renal symptoms, and fe-
Medicine, Department of Obstetrics & Willebrand factor-cleaving metallopro- ver.5,6 This pentad is only present 40% of
Gynecology (Drs Stella, How, and Sibai) and tease known as ADAMTS13 (a disinte- the time.1 In most cases, the signs and
TriHealth Hospital System, Department of grin-like and metalloprotease with symptoms are subtle, often indiscern-
Obstetrics & Gynecology (Dr Coppage), thrombospondin type 1 motif 13) pro- ible. The most common reported signs
Cincinnati, OH; Greenville Hospital System, duced by hepatocytes.2 These large von and symptoms are nonspecific and in-
Department of Obstetrics & Gynecology (Dr Willebrand factor multimers increase clude nausea, vomiting, abdominal pain,
Dacus), Greenville, SC; and St. Peter’s
platelet adhesiveness and impair fibrino- weakness, bleeding, easily bruisability,
Hospital, Department of Obstetrics &
Gynecology (Drs Guzman and Dhillon),
lytic activity subsequently.4 When the and flu-like symptoms.8-10
New Brunswick, NJ. multimers are cleaved to smaller and When TTP/HUS does occur during
Received June 30, 2008; revised Sept. 4,
less active forms in maternal circula- pregnancy, they often are confused ini-
2008; accepted Oct. 7, 2008 tion, microvascular platelet thrombi tially with obstetric diagnoses such as se-
Reprints not available from the authors. form.5 HUS usually is described in as- vere preeclampsia; hemolysis, elevated
Authorship and contribution to the manuscript sociation with infection by the Shiga liver enzymes and low platelets (HELLP)
is limited to the 7 authors indicated. There was toxin-producing enterohemorrhagic syndrome; acute fatty liver of pregnancy;
no outside funding or technical assistance with strains of Escherichia coli.6 Despite eclampsia, and antiphospholipid anti-
the production of this article.
their different pathologic origins, TTP body syndrome.1,11 This might be re-
0002-9378/$36.00 and HUS manifest similar clinical and lated to the fact that the disease entity is
© 2009 Mosby, Inc. All rights reserved.
doi: 10.1016/j.ajog.2008.10.037 laboratory findings, with more pro- rare and often is unexpected. Neverthe-
found neurologic symptoms in TTP less, a delay in diagnosis of TTP/HUS
APRIL 2009 American Journal of Obstetrics & Gynecology 381.e1
Research Obstetrics www.AJOG.org
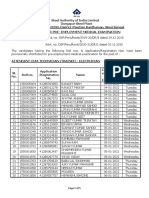
TABLE 1
Clinical data and evaluation
Highest
Site of blood Gestational
Initial initial pressure Proteinuria 24-Hr age at Latency Race/
Patient diagnosis visit Symptoms Fever (mm Hg) (dipstick) protein diagnosis (d) ethnicity
1a HELLP Obstetrics Slurred (⫺) 147/96 30 399 mg Postpartum 4 White
triage speech, period
headaches
................................................................................................................................................................................................................................................................................................................................................................................
2 Panic attack Emergency Anxiety (⫺) 137/60 (⫹) 75 mg 12 6 White
department
................................................................................................................................................................................................................................................................................................................................................................................
a
3 Idiopathic, Emergency Nausea, (⫺) 126/62 150 3379 mg 21 6 White
thrombocytopenic department vomiting
purpura
................................................................................................................................................................................................................................................................................................................................................................................
a
4 Sepsis Obstetrics Abdominal (⫹) 153/96 300 N/A Postpartum 2 Hispanic
triage pain period
................................................................................................................................................................................................................................................................................................................................................................................
a,b
5 Preeclampsia Obstetrics Lethargy (⫺) 145/94 100 4g 21 1 African
triage American
................................................................................................................................................................................................................................................................................................................................................................................
a,b
5 Preeclampsia Obstetrics Nausea, (⫺) 134/79 (⫺) N/A 38 5 African
triage vomiting American
................................................................................................................................................................................................................................................................................................................................................................................
6 Leukemia Emergency Loss of (⫺) 123/76 Trace 0.25 g 24 1 African
department consciousness American
................................................................................................................................................................................................................................................................................................................................................................................
b c
7 HUS Emergency Flu-like (⫹) 140/104 (⫺) N/A Postpartum N/A White
department symptoms period
................................................................................................................................................................................................................................................................................................................................................................................
8 HELLP Obstetrics Abdominal (⫺) 144/76 (⫺) 23.9 mg 8 2 African
triage pain, American
headaches
................................................................................................................................................................................................................................................................................................................................................................................
9 Preeclampsia/ Obstetrics Fatigue, dark (⫺) 167/84 (⫺) N/A Postpartum 5 White
HELLP triage urine period
................................................................................................................................................................................................................................................................................................................................................................................
a
10 Pyelonephritis Obstetrics Lethargy, (⫺) 166/94 (⫺) N/A 39 1 White
triage hematuria
................................................................................................................................................................................................................................................................................................................................................................................
a
11 Domestic Emergency Obtunded, (⫺) 155/86 300 N/A 30 4 African
violence department confused American
................................................................................................................................................................................................................................................................................................................................................................................
a,b
12 HELLP Obstetrics Nausea, (⫹) 160/80 N/A N/A 26 7 White
triage vomiting
................................................................................................................................................................................................................................................................................................................................................................................
b
12 TTP Obstetrics Cough, (⫺) 140/90 N/A 5357 mg 21 N/A White
triage hemoptysis
................................................................................................................................................................................................................................................................................................................................................................................
(⫺), absent; (⫹) present; HELLP, hemolysis, elevated liver enzymes and low platelets; HUS, hemolytic uremic syndrome; N/A, not available; TTP, thrombotic thrombocytopenic purpura.
a
Multiparous; b Recurrent; c HUS was misdiagnosed before index pregnancy.
................................................................................................................................................................................................................................................................................................................................................................................
Stella. The diagnostic dilemma of TTP/HUS in the obstetric triage and emergency department. Am J Obstet Gynecol 2009.
may result in life-threatening maternal M ATERIALS AND M ETHODS obtained from all medical centers that
and fetal consequences. A retrospective chart review of women were involved.
Our objective was to report on the with a discharge diagnosis of TTP and A diagnosis of TTP or HUS was made
symptoms, initial diagnosis, treatment, HUS that were associated during preg- based on the following criteria: evidence
and outcome of patients with TTP/HUS nancy or the postpartum period from of hemolysis detected on a peripheral
during pregnancy/postpartum period 1999-2007 at The University Hospital blood smear with elevated lactate dehy-
that have been encountered in 4 tertiary (TUH; Cincinnati, OH), St. Peter’s Uni- drogenase (LDH) levels, severe throm-
care centers in the United States. The versity Hospital (New Brunswick, NJ), bocytopenia, presence of renal or neuro-
emphasis is on pitfalls in the diagnosis of Greenville Health System (Greenville, logic symptoms and/or fever. Final
these syndromes. In addition, we will SC), and TriHealth Hospital System diagnosis was made by the consulting
propose a plan of evaluation for early de- (Cincinnati, OH) was performed. Insti- hematologist after excluding other etiol-
tection of these microangiopathies. tutional Review Board approvals were ogies. Twelve women (14 pregnancies)
381.e2 American Journal of Obstetrics & Gynecology APRIL 2009
www.AJOG.org Obstetrics Research
TABLE 2
Summary of laboratory results
Platelet Aspartate Alanine
count Hematocrit Peripheral LDH Creatinine aminotransferase transaminase
Patient (103/mm3) (%) smear (U/L) (mg/dL) (U/L) (U/L)
1 30 23.2 (⫹) 5918 1.6 73 80
................................................................................................................................................................................................................................................................................................................................................................................
2 4 24.2 (⫹) 2302 1.2 44 14
................................................................................................................................................................................................................................................................................................................................................................................
3 13 22.2 (⫹) 420 0.5 14 10
................................................................................................................................................................................................................................................................................................................................................................................
4 20 19.8 (⫹) 1445 7.09 279 63
................................................................................................................................................................................................................................................................................................................................................................................
a
5a 12 21.7 (⫹) 6005 1.5 243 144
................................................................................................................................................................................................................................................................................................................................................................................
5b 43 23.1 (⫹) 583 0.9 22 12
................................................................................................................................................................................................................................................................................................................................................................................
6 3 20.6 (⫹) 1218 0.8 33 37
................................................................................................................................................................................................................................................................................................................................................................................
7 67 15 (⫹) 4396 2.3 173 63
................................................................................................................................................................................................................................................................................................................................................................................
8 8 22 (⫹) 395 0.8 56 120
................................................................................................................................................................................................................................................................................................................................................................................
9 69 20 (⫹) 1512 1.7 384 152
................................................................................................................................................................................................................................................................................................................................................................................
10 8 27.9 (⫹) 1438 1.0 32 19
................................................................................................................................................................................................................................................................................................................................................................................
11 7 23.9 (⫹) 4710 2.3 1706 525
................................................................................................................................................................................................................................................................................................................................................................................
a
12a 12 20.9 (⫹) 933 0.7 N/A N/A
................................................................................................................................................................................................................................................................................................................................................................................
12b 13 20 (⫹) 800 1.0 18 26
................................................................................................................................................................................................................................................................................................................................................................................
LDH, lactate dehydrogenase; N/A, not available.
a
Recurrent.
................................................................................................................................................................................................................................................................................................................................................................................
Stella. The diagnostic dilemma of TTP/HUS in the obstetric triage and emergency department. Am J Obstet Gynecol 2009.
were identified, of which 12 pregnancies fresh-frozen plasma, as needed. Hemo- ⫽ 50,190), Greenville Health System (n ⫽
were complicated with TTP and 2 preg- dialysis was performed for renal failure. 42,493), and TriHealth Hospital System (n
nancies were complicated with HUS. Indicators of residual sequelae included ⫽ 81,733). Of the 14 pregnancies, 12 had
Thrombocytopenia was defined as plate- renal failure, neurologic impairment, or TTP, and 2 had HUS. There were a total of
let count ⬍ 100,000 L/mm3. Microangio- death either during hospitalization or on 16 fetuses (2 patients had twin gestation).
pathic hemolysis was defined as the pres- follow-up evaluation. All but 1 case were diagnosed for the first
ence of schistocytes, echinocytes, or red Data were collected regarding clinical time during pregnancy (1 case was diag-
blood cell fragments on the peripheral presentation to the obstetrics triage, nosed before index pregnancy and had
smear, elevated LDH levels that were ⬎ 2 physician’s office, or emergency depart- recurrence during pregnancy), and 2
times the upper limit of normal or anemia ment and included signs and symptoms cases had recurrences in subsequent
(hematocrit level, ⬍ 25%). Preeclampsia and relevant laboratory findings. Initial pregnancies.
was defined as the presence of hyperten- diagnosis and treatment, latency period Maternal age ranged from 20-40 years.
sion (systolic blood pressure ’ 140 mm Hg in days (defined as onset of symptoms to Nausea, vomiting, abdominal pain, and
or diastolic blood pressure ’ 90 mm Hg that plasmapheresis), initial therapeutic in- mental status changes were the most
occurred after 20 weeks of gestation) and terventions, laboratory findings, num- common symptoms. Twelve of the 14
proteinuria either from a random urine ber of plasmapheresis cycles, maternal pregnancies were diagnosed initially
dipstick or urinary excretion of 0.3 g of and neonatal outcomes, and long-term with other clinical conditions (medical
protein from a 24-hour urine specimen. sequelae were noted. or obstetric) during the initial evaluation
Treatment of these women included in the emergency department or the ob-
plasmapheresis, optimization of fluid stetrics triage area. The other 2 pregnan-
balance, hemodynamic status, and serial R ESULTS cies were known before pregnancy to
assessment of hematologic, renal and he- The study population consisted of 12 have either HUS or TTP.
patic function. Hematology and/or renal women and involved 14 pregnancies. Dur-
service were consulted in all cases to con- ing the study time period, there were Site of presentation
firm diagnosis and for treatment. Sup- 192,848 deliveries at the study institutions Four of 12 cases were evaluated initially
portive measures included the use of in- that were subdivided in the following in the emergency department and diag-
travenous or oral corticosteroids and manner: The University Hospital (n ⫽ nosed with either a panic attack, idio-
transfusion of packed red blood cells or 18,432), St. Peter’s University Hospital (n pathic, thrombocytopenic purpura, do-
APRIL 2009 American Journal of Obstetrics & Gynecology 381.e3
Research Obstetrics www.AJOG.org
area or physician’s office. Physicians in
TABLE 3 the emergency department appeared
Maternal and perinatal outcome mainly to consider more common diag-
Maternal outcome Perinatal outcome noses such as panic attack, domestic vi-
Patient Death Renal injury Death Abortion Preterm olence or gastroenteritis, rather than the
1 No No No No
rare conditions such as TTP/HUS. Ob-
.............................................................................................................................................................................................................................................. stetricians, on the other hand, consis-
2 No No No No
.............................................................................................................................................................................................................................................. tently seemed to consider severe pre-
3 No No No No eclampsia or HELLP syndrome as a
..............................................................................................................................................................................................................................................
4 No Yes (HUS) No No Yes a
default diagnosis, even in patients with-
..............................................................................................................................................................................................................................................
5 No No No No No out hypertension and/or proteinuria at
..............................................................................................................................................................................................................................................
term or during the postpartum period
6 No No No No No
.............................................................................................................................................................................................................................................. and in those who were evaluated at ⬍ 24
a
7 Yes (cardiac No No No Yes weeks of gestation. Because of the high
tamponade)
.............................................................................................................................................................................................................................................. maternal and fetal mortality rates that
8 No No No Yes No are associated with TTP/HUS, it is of
..............................................................................................................................................................................................................................................
a,b
9 Yes (stroke) No No No Yes crucial importance that these 2 diag-
..............................................................................................................................................................................................................................................
10 Yes (organ No No No No noses remain in the differential diagnosis
failure) of the astute clinician caring for preg-
..............................................................................................................................................................................................................................................
11 No No Yes No Yes a nant/postpartum women.1,11 Pregnant
..............................................................................................................................................................................................................................................
b,c a women comprise 7%13 of TTP/HUS pa-
12 No No Yes — Yes
.............................................................................................................................................................................................................................................. tients for 2 reasons: pregnancy is an in-
HUS, hemolytic uremic syndrome.
a
citing factor, and the female-to-male ra-
Indicated delivery; b Twin gestation; c Subsequent pregnancy.
.............................................................................................................................................................................................................................................. tio is 3:2.14 Although all patients in our
Stella. The diagnostic dilemma of TTP/HUS in the obstetric triage and emergency department. Am J Obstet Gynecol case series had far-encompassing array
2009. of symptoms, their hematologic profile
revealed profoundly decreased or pro-
mestic violence, or gastroenteritis; 2 of come (term delivery, liveborn fetus). gressively decreasing platelet count and
these 4 were discharged home 2-3 times Four patients were diagnosed and re- severe anemia. When Coomb’s negative
before hospitalization. Eight of 12 cases ceived plasmapheresis at 25-39 weeks of hemolytic anemia and thrombocytope-
that were evaluated by an obstetrician gestation; 2 of these patients died despite nia are present, TTP/HUS should be sus-
were diagnosed initially with either plasmapheresis. Three of the 5 infants (1 pected in the absence of hypertension
HELLP syndrome/preeclampsia (n ⫽ 6), set of twins) of these women survived. A and/or proteinuria in patients who are
pyelonephritis (n ⫽ 1), or sepsis (n ⫽ 1). patient who had HUS had residual renal near term or after delivery and in those
The latency period ranged from 1-7 days. failure and Budd Chiari syndrome and patients with evidence of severe pre-
On diagnosis, all patients had severe who remained in remission for 5 years eclampsia/HELLP developing at ⬍ 24
thrombocytopenia, hemolysis, severe died of presumed cardiac tamponade. weeks of gestation (when HELLP syn-
anemia, and hematuria. Clinical data for No autopsy was available. Another pa- drome is rare).
all patients are summarized in Table 1, tient with HUS that was diagnosed after Although ADAMTS13 is reported
and laboratory data are described in Ta- delivery had immediate plasma ex- widely in literature as an adjunctive lab-
ble 2. All patients had plasmapheresis change for 14 days until she was dis- oratory test that is used in diagnosing
once the diagnosis of TTP/HUS was charged home with no residual renal TTP, this test was not obtained in our
made. damage. patient series. This may be attributed to
Maternal-perinatal outcome its limited availability because it is a
Maternal and perinatal outcomes are de- C OMMENT send-out test (available only in 2 states),
scribed in Table 3. Six patients were di- Our study reveals that, during pregnancy hence making it difficult to order and
agnosed at ⬍ 24 weeks of gestation. All 6 and the postpartum period, TTP/HUS obtain results immediately.12 However,
patients received plasmapheresis and continue to be a challenging diagnosis to a more plausible explanation may be that
survived. Of these 6 patients, 3 women the clinician.11,12 There was delay in di- providers in our series were not enter-
had term live births; 1 woman had a agnosis of TTP/HUS by both obstetri- taining TTP or HUS as primary diag-
missed abortion, and 2 women had in- cians and emergency medicine physi- noses to obtain such testing. Of note,
trauterine fetal death (1 set of twins). cians in most patients in this series. The pregnancy affects ADAMTS13 levels,
Three patients who had daily plasma ex- differential diagnosis, however, differed and ADAMTS13 levels are likewise de-
change at ⬍ 24 weeks of gestation until in the emergency department area as op- creased in HELLP syndrome.15 How-
delivery had favorable perinatal out- posed to the diagnosis in obstetrics triage ever, these levels remain always ⬎10%,
381.e4 American Journal of Obstetrics & Gynecology APRIL 2009
www.AJOG.org Obstetrics Research
whereas in TTP the levels are usually ⬍
5%.8,9 TABLE 4
In some of our patients who had the Frequency of signs, symptoms and laboratory
shortest latency from diagnosis to treat- findings of TTP/HUS vs HELLP syndrome1,22
ment, maternal-fetal outcomes proved Signs/symptoms/
to be most favorable. Hence, early con- laboratory findings TTP HUS HELLP
sideration of plasmapheresis in a patient Hypertension (%) 20-75 80-90 85
..............................................................................................................................................................................................................................................
with an otherwise stable condition may Proteinuria (%) with hematuria 80-90 90-95
..............................................................................................................................................................................................................................................
best allow for optimum outcome. In- Fever (%) 20-50 NR Absent
deed, we have observed in a subset of our ..............................................................................................................................................................................................................................................
patients that the earlier in the gestation Jaundice (%) Rare Rare 5-10
..............................................................................................................................................................................................................................................
plasmapheresis is performed, the higher Nausea and vomiting (%) Common Common 40
..............................................................................................................................................................................................................................................
the likelihood of a successful maternal- Abdominal pain (%) Common Common 60-80
..............................................................................................................................................................................................................................................
fetal outcome. Regarding plasmaphere- Central nervous system (%) 60-70 NR 40-60
sis, parturients and nonpregnant pa- ..............................................................................................................................................................................................................................................
tients both undergo the same procedure ADAMST13 activity ⬍ 5% 33-100 Rare Absent
..............................................................................................................................................................................................................................................
of plasma exchange with fresh frozen von Willebrand factor 80-90 90 Absent
plasma, cryosupernatant, or solvent/de- multimers (%)
..............................................................................................................................................................................................................................................
tergent-treated plasma.2 By virtue of the Platelet count (mm ) 3
ⱕ 20,000 ⬍ 20,000 ⬍ 20,000
..............................................................................................................................................................................................................................................
45% increase in blood volume in preg- Anemia (%) 100 100 ⬍ 50
nancy,16 larger volume of plasma ex- ..............................................................................................................................................................................................................................................
a a
Elevated transaminases (%) Usually absent Usually absent 100
changes usually are required in pregnancy. ..............................................................................................................................................................................................................................................
Making the diagnosis of TTP or HUS Elevated lactic 100 100 100
dehydrogenase (%)b
is akin to looking for the proverbial nee- ..............................................................................................................................................................................................................................................
dle in the haystack. Delay in diagnosis is HELLP, hemolysis, elevated liver enzymes and low platelets; HUS, hemolytic uremic syndrome; NR, not reported; TTP,
thrombotic thrombocytopenic purpura.
attributable to the rareness of TTP. An a
Present in case of liver involvement (values usually less than in HELLP); b Values usually much higher in TTP/HUS.
emergency department physician would ..............................................................................................................................................................................................................................................
encounter several patients with panic at- Stella. The diagnostic dilemma of TTP/HUS in the obstetric triage and emergency department. Am J Obstet Gynecol
2009.
tack or gastroenteritis on a daily basis.
However, these conditions will not be as-
sociated with thrombocytopenia. For the Based on our experience and the re-
TTP/HUS. Finally, a red flag should be
obstetrician, severe preeclampsia or
raised if delivery does not normalize lab- view of the literature, we recommend the
HELLP syndrome is certainly a more
oratory values (usually within 2-3 days) following treatment plan for the early de-
common diagnosis (0.5% of all pregnan-
or improve the neurologic, abdominal, tection of TTP/HUS. Pregnant women
cies) than TTP; however, both patho-
or renal symptoms in women with a pre- with vague neurologic, abdominal, gas-
logic conditions are characterized by
sumed diagnosis of HELLP syndrome or trointestinal, or renal symptoms who are
thrombocytopenia and hemolysis, which
eclampsia.1,12,17 evaluated in the obstetrics triage area or
are neurologic symptoms with or with-
out hypertension. Thus, TTP should be Women who experience TTP during the emergency department area should
suspected in women with the aforemen- pregnancy should be made aware of the receive complete blood count testing.
tioned findings who are normotensive or potential for relapse and the risk of re- The presence of thrombocytopenia war-
nonproteinuric during the third trimes- lapse in subsequent pregnancies.7,18-20 rants an immediate peripheral blood
ter or the postpartum period. In addi- Two patients in our series had recurrent smear after exclusion of other causes of
tion, it should be suspected in those TTP during pregnancy. Therefore, these thrombocytopenia, such as severe pre-
women with hypertension, proteinuria, women should be instructed about the eclampsia, idiopathic thrombocytopenic
and abnormal laboratory tests at ⬍ 24 symptoms of early relapse and about the purpura, connective tissue disease, and
weeks of gestation.11 Moreover, the ab- importance of reporting these symptoms human immunodeficiency virus infec-
normal laboratory values in TTP are of- immediately. There are few case reports tion. To reach a correct diagnosis, it is im-
ten extreme or profound, as opposed to that describe recurrent TTP-HUS in portant to consider TTP/HUS when the
gestational thrombocytopenia (platelet subsequent pregnancies;10,18-21 how- abnormal laboratory values are extreme or
count, ⬍ 100,000 L/mm3). Addition- ever, the risk of this recurrence remains profound and/or disproportionate to
ally, the liver enzymes are elevated signif- unknown because of limited data. Vesely laboratory values that are expected in
icantly and proportional to the degree of et al18 reported data from the Oklahoma HELLP syndrome1,12 (Table 4). For a
thrombocytopenia in HELLP syn- TTP-HUS registry that indicated that clinical picture that is utterly unexplain-
drome.1 In contrast, liver enzymes are 18% of patients have recurrence of TTP- able, the diagnosis of TTP/HUS should
usually normal or mildly elevated in HUS with subsequent pregnancy. be considered if there is severe thrombo-
APRIL 2009 American Journal of Obstetrics & Gynecology 381.e5
Research Obstetrics www.AJOG.org
cytopenia, severe anemia, and elevated 3. Moake JL. Thrombotic microangiopathies. 14. Török TJ, Holman RC, Chorba TL. Increas-
LDH levels with minimal elevation of as- N Engl J Med 2002;347:589. ing mortality from thrombotic thrombocytope-
4. Sadler JE, Moake JL, Miyata T, George JN. nic purpura in the United States: analysis of na-
partate aminotransferase, even in the ab- Recent advances in thrombotic thrombocy- tional mortality data, 1968-1991. Am J Hematol
sence of the classic pentad.11 A periph- topenic purpura. Hematology 2004;2004: 1995;50:84-90.
eral blood smear should be performed 407-23. 15. Lattuada A, Rossi E, Calzarossa C, Candolfi
immediately to confirm hemolysis. In 5. Galbusera M, Noris M, Remuzzi G. Throm- R, Mannucci PM. Mild to moderate reduction of
botic thrombocytopenic purpura: then and von Willebrand factor cleaving protease (AD-
general, the percentage of schistocytes
now. Semin Thromb Hemost 2006;32:81-9. AMTS-13) in pregnant women with HELLP mi-
on peripheral smear is much higher in 6. Karmali MA, Petric M, Lim C, Fleming PC, croangiopathic syndrome. Haematologica 2003;
TTP (2-5%) than in HELLP (usually ⬍ Arbus GS, Lior H. The association between id- 88:1029-34.
1%). In addition, ADAMTS13 should be iopathic hemolytic uremic syndrome and infec- 16. Cardiovascular disease. In: Cunningham
obtained, and plasmapheresis initiated tion by verotoxin-producing Escherichia coli. FG, Leveno KJ, Hauth JC, Gilstrap LC III, Wen-
J Infect Dis 1985;151:775-82. strom KD, editors. Williams obstetrics. 22nd ed.
as soon as possible.1,12 7. Dashe JS, Ramin SM, Cunningham FG. The New York: McGraw Hill; 2005:1017-41.
In summary, the spectrum of TTP/ long-term consequences of thrombotic mi- 17. Rosen M, Brauer KI, Alperin JB, Hankins
HUS is a diagnostic challenge that must croangiopathy (thrombotic thrombocytopenic GDV, Saade G. Postpartum hemorrhagic shock
be triaged methodically. When severe purpura and hemolytic uremic syndrome) in resulting in thrombotic thrombocytopenic pur-
pregnancy. Obstet Gynecol 1998;91:662-8. pura-hemolytic uremic syndrome. J Matern Fe-
thrombocytopenia and hemolysis are
8. George JN, Terrell DR, Swisher KK, Vesely tal Neonatal Med 2003;12:208-10.
present in the absence of hypertension in SK. Lessons learned from the Oklahoma 18. Vesely SK, George JN, Lämmle B, et al.
any trimester, the diagnosis of TTP Thrombotic Thrombocytopenic Purpura-He- ADAMTS13 activity in thrombotic thrombocyto-
needs to be strongly considered. If severe molytic Uremic Syndrome registry. J Clin penic purpura-hemolytic uremic syndrome: re-
renal dysfunction is also present, HUS Apheresis 2008;23:129-37. lation to presenting features and clinical out-
9. George JN. The association of pregnancy comes in a prospective cohort of 142 patients.
should be considered. Timely identifica- with thrombotic thrombocytopenic purpura-he- Blood 2003;102:60-8.
tion of patients with TTP/HUS may im- molytic uremic syndrome. Clin Opin Hematol 19. Ezra Y, Rose M, Elder A. Therapy and pre-
pact favorably the high maternal and fe- 2003;10:339-44. vention of thrombotic thrombocytopenic pur-
tal mortality rates that are seen with these 10. George JN. Thrombotic thrombocytopenic pura during pregnancy: a clinical study of 16
diagnoses during pregnancy or the post- purpura. N Engl J Med 2006;354:1927-35. pregnancies. Am J Hematol 1996;51:1-6.
11. Martin JN Jr, Bailey AP, Rehberg JF, Owens 20. Egerman RS, Witlin A, Friedman S, Sibai
partum period. It is therefore extremely MT, Keiser SD, May WL. Thrombotic thrombo- BM. Thrombotic thrombocytopenic purpura
important to differentiate severe pre- cytopenic purpura in 166 pregnancies:1955- and hemolytic uremic syndrome in pregnancy:
eclampsia and HELLP syndrome from 2006. Am J Obstet Gynecol 2008;199:98-104. review of 11 cases. Am J Obstet Gynecol
these thrombotic microangiopathies be- 12. Rehberg JF, Briery CM, Hudson WT, Bofill 1996;175:950-6.
JA, Martin JN. Thrombotic thrombocytopenic 21. Hebisch G, Bernasconi MT, Gmuer J, Huch
cause of the differing treatments these
purpura masquerading as hemolysis, elevated A, Stallmach T. Pregnancy-associated recur-
diagnoses entail. f liver enzymes, low platelets (HELLP) syndrome rent hemolytic uremic syndrome with fetal vas-
in late pregnancy. Obstet Gynecol 2006;108: culopathy in the placenta. Am J Obstet Gynecol
817-20. 2001;185:1265-6.
REFERENCES 13. Terrell DR, Williams LA, Vesely SK, Lämmle 22. Hulstein JJJ, van Runnard Heimel PJ, Franx
1. Sibai BM. Imitators of severe preeclampsia. B, Hovinga JAK, George JN. The incidence of A, et al. Acute activation of the endothelium re-
Obstet Gynecol 2007;109:956-66. thrombotic thrombocytopenic purpura-hemo- sults in increased levels of active von Willebrand
2. Rock G, Porta C, Bobbio-Pallavicini F. lytic uremic syndrome: all patients, idiopathic factor in hemolysis, elevated liver enzymes and
Thrombotic thrombocytopenic purpura in year patients and patients with severe ADAMTS-13 low platelets (HELLP) syndrome. J Thromb
2000. Haematologica 2008;5:410-9. deficiency. J Thromb Haemost 2005;3:1432-6. Haemost 2006;4:2569-75.
381.e6 American Journal of Obstetrics & Gynecology APRIL 2009
Vous aimerez peut-être aussi
- Prismaflex User ManualDocument287 pagesPrismaflex User ManualMahmoud Diaa78% (9)
- Acute Hypercapnic Respiratory Failure Associated With HemodialysisDocument3 pagesAcute Hypercapnic Respiratory Failure Associated With HemodialysisMahmoud DiaaPas encore d'évaluation
- Retained Catheter Fragment From A Fractured Tunneled Catheter-A Rare and Potentially Lethal ComplicationDocument4 pagesRetained Catheter Fragment From A Fractured Tunneled Catheter-A Rare and Potentially Lethal ComplicationMahmoud DiaaPas encore d'évaluation
- 3 1 - N U M B e R 2 - 2 0 1 1: Official Publication of The Spanish Society of NephrologyDocument117 pages3 1 - N U M B e R 2 - 2 0 1 1: Official Publication of The Spanish Society of NephrologyMahmoud DiaaPas encore d'évaluation
- Prevention and Treatment of Systemic Glucocorticoid Side EffectsDocument10 pagesPrevention and Treatment of Systemic Glucocorticoid Side EffectsMahmoud DiaaPas encore d'évaluation
- Flash Pulmonary Oedema and Bilateral Renal Artery Stenosis: The Pickering SyndromeDocument8 pagesFlash Pulmonary Oedema and Bilateral Renal Artery Stenosis: The Pickering SyndromeMahmoud DiaaPas encore d'évaluation
- The Value of Failure: The Discovery of TNF and Its Natural Inhibitor Erythropoietin, A. CeramiDocument8 pagesThe Value of Failure: The Discovery of TNF and Its Natural Inhibitor Erythropoietin, A. CeramiMahmoud DiaaPas encore d'évaluation
- Composition and Clinical Use of HemodialysatesDocument14 pagesComposition and Clinical Use of HemodialysatesMahmoud DiaaPas encore d'évaluation
- Belco Formula User ManualDocument386 pagesBelco Formula User ManualMahmoud Diaa100% (21)
- Avoiding Common Technical Errors in Subclavian Central Venous Catheter PlacementDocument6 pagesAvoiding Common Technical Errors in Subclavian Central Venous Catheter PlacementMahmoud DiaaPas encore d'évaluation
- Gambro AK 96® Dialysis Machine Operator's ManualDocument506 pagesGambro AK 96® Dialysis Machine Operator's ManualMahmoud Diaa90% (67)
- Locking Solutions For Hemodialysis Catheters Heparin and Citrate - A Position Paper by ASDIN.Document3 pagesLocking Solutions For Hemodialysis Catheters Heparin and Citrate - A Position Paper by ASDIN.Mahmoud DiaaPas encore d'évaluation
- Nephrology Underpinning For The Young DoctorsDocument7 pagesNephrology Underpinning For The Young DoctorsMahmoud DiaaPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5795)
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)
- Problems Within The FamilyDocument6 pagesProblems Within The FamilyDwinka PuspaPas encore d'évaluation
- Policy DocDocument6 pagesPolicy Docce mgnregsPas encore d'évaluation
- Health DLP STAGES OF INFECTIONDocument9 pagesHealth DLP STAGES OF INFECTIONmarielabianaPas encore d'évaluation
- Adviser Action PlanDocument3 pagesAdviser Action PlanJezelle ManaloPas encore d'évaluation
- Task1 LeiCastilloDocument4 pagesTask1 LeiCastilloTonie VillamarinPas encore d'évaluation
- g12 2nd Folk, Ballet, BallroomDocument82 pagesg12 2nd Folk, Ballet, BallroomJennifer ArnaizPas encore d'évaluation
- Geometry Thesis TopicsDocument6 pagesGeometry Thesis TopicsLindsey Sais100% (2)
- MPT Research ReportDocument7 pagesMPT Research ReportVenice De los ReyesPas encore d'évaluation
- Different Types of StretchingDocument7 pagesDifferent Types of StretchingAnee Muskan0% (2)
- Notice For PEMEDocument5 pagesNotice For PEMESwarnava LahaPas encore d'évaluation
- Maternal and Child Health (MHCH)Document4 pagesMaternal and Child Health (MHCH)rifkatu s. ibrahimPas encore d'évaluation
- PE11 - MELC 4 Module 4 - Week7 For Teacher PDFDocument24 pagesPE11 - MELC 4 Module 4 - Week7 For Teacher PDFRommel Cando80% (5)
- Mod Oncho Dip FinalDocument71 pagesMod Oncho Dip FinalEbsa MohammedPas encore d'évaluation
- Arco - Unit 4Document23 pagesArco - Unit 4Jovel ConsularPas encore d'évaluation
- Accomplishment February 2019Document8 pagesAccomplishment February 2019saphire donsolPas encore d'évaluation
- Restaurant Report Card - November 25, 2021Document6 pagesRestaurant Report Card - November 25, 2021KBTXPas encore d'évaluation
- Administrative Data Sheet Student Information:: Testing Public SchoolsDocument24 pagesAdministrative Data Sheet Student Information:: Testing Public SchoolsSabrina AguilarPas encore d'évaluation
- Diagnostic Utility of Fecal Elastase-1 in Exocrine Pancreatic Insufficiency - A Systematic Review and Meta-AnalysisDocument1 pageDiagnostic Utility of Fecal Elastase-1 in Exocrine Pancreatic Insufficiency - A Systematic Review and Meta-AnalysisguschinPas encore d'évaluation
- Lesson Plan - Phase 1 Student: Class Date: Lesson Title: Literacy - Spot The Rhyming Words Experiences & Outcomes (Maximum of 3)Document7 pagesLesson Plan - Phase 1 Student: Class Date: Lesson Title: Literacy - Spot The Rhyming Words Experiences & Outcomes (Maximum of 3)FardosPas encore d'évaluation
- Assignment On Marital Rape As A Ground For Divorce: Submitted ToDocument18 pagesAssignment On Marital Rape As A Ground For Divorce: Submitted ToAishwarya MathewPas encore d'évaluation
- Barangay Devepment PlanDocument21 pagesBarangay Devepment Planjeoffryabonitalla311Pas encore d'évaluation
- What Are The Current Benefits of Having Foods Made From Genetically Modified Crops?Document1 pageWhat Are The Current Benefits of Having Foods Made From Genetically Modified Crops?Shee YingPas encore d'évaluation
- GRN777 Web PDFDocument125 pagesGRN777 Web PDFsuresh samineniPas encore d'évaluation
- Effective Team Work: Prepared & Presented By: Okanlomo Goke-OlatejuDocument21 pagesEffective Team Work: Prepared & Presented By: Okanlomo Goke-OlatejuOkanlomo Goke-OlatejuPas encore d'évaluation
- The Velvet Rage - Overcoming The Pain of Growing Up Gay in A Straight Man's World - PDF RoomDocument248 pagesThe Velvet Rage - Overcoming The Pain of Growing Up Gay in A Straight Man's World - PDF RoomJasson Cerrato100% (3)
- hsp3c UDocument19 pageshsp3c Uapi-390148276Pas encore d'évaluation
- Paediatrics Updated General Exam in PaediatricsDocument35 pagesPaediatrics Updated General Exam in PaediatricsOmar AlsalmanPas encore d'évaluation
- L-2 Pharmacy As A CareerDocument2 pagesL-2 Pharmacy As A CareerSCN StaffPas encore d'évaluation
- How To Read People Like A Book - Speed-Read, Analyze, and Understand Anyone's Body LanguagDocument141 pagesHow To Read People Like A Book - Speed-Read, Analyze, and Understand Anyone's Body Languagjose roman zepedaPas encore d'évaluation
- Main - Employee Performance Appraisal FormDocument3 pagesMain - Employee Performance Appraisal FormPalak SinghalPas encore d'évaluation