Académique Documents
Professionnel Documents
Culture Documents
Journal - Obstructed Tracheostomy Tubes
Transféré par
Von_Adrian_Lor_4365Description originale:
Copyright
Formats disponibles
Partager ce document
Partager ou intégrer le document
Avez-vous trouvé ce document utile ?
Ce contenu est-il inapproprié ?
Signaler ce documentDroits d'auteur :
Formats disponibles
Journal - Obstructed Tracheostomy Tubes
Transféré par
Von_Adrian_Lor_4365Droits d'auteur :
Formats disponibles
Obstructed
tracheostomy
tubes By Joan Webber-Jones, EdM, RN-C, ONC
Clearing
the air
A TRACHEOSTOMY IS a percuta- your patient for signs and symp- try to remove any mucous plugs
neously or surgically created toms of respiratory distress such that may be present.3 If you feel
opening in the anterior wall of as shortness of breath, tachypnea, resistance and the patient’s signs
the trachea inferior to the cricoid labored breathing, diaphoresis, and symptoms don’t improve with
cartilage that provides tracheal agitation, accessory muscle use, suctioning, another problem is
access for airway management. reduced SpO2, hypoxemia, and causing the respiratory distress.
A temporary or permanent tra- hypercapnia. • an overinflated herniated tra-
cheostomy tube is inserted into cheostomy tube cuff. Overinflation
the opening to maintain airway All blocked up of the tracheostomy tube cuff can
patency. A common complication Common causes of tracheostomy obstruct the tube lumen by the in-
associated with tracheostomy tube obstruction include: creasing pressure, causing it to
tubes is obstruction. Obstruction • a dried mucous plug. This is the narrow. Overinflation can also
of the tracheostomy tube is a life- most common cause of obstruc- cause the cuff to distend distally
threatening emergency, so if you tion.1 Airway suctioning is the and partially or completely cover
suspect your patient has or is de- most important intervention for and obstruct the distal lumen.4
veloping a tracheostomy tube ob- maintaining a patent airway and Tracheostomy tube cuff herniation
struction, you’ll need to intervene preventing mucous plugs. Most may occur from a manufacturing
immediately. tracheostomy patients have a defect and cuff fabric fatigue. High
diminished cough reflex and re- compliance (low volume, high
Be prepared for trouble quire suctioning to remove air- pressure) cuffs have a history of
Whenever you care for a patient way secretions.2 Coarse crackles herniation if overinflated.4 Cuff
with a tracheostomy tube, you and rhonchi are indications for pressure should be between 20 to
need to be ready for any emer- suctioning. Inhaled, heated, or 25 mm Hg to achieve an air seal.
gency that can threaten airway room temperature humidification If suctioning doesn’t improve the
patency, leading to respiratory dis- is vital for maintaining tube pa- patient’s signs and symptoms, de-
tress and failure. (See Be prepared! tency.1 It’s also important to keep flate the tracheostomy tube cuff
for a list of equipment that should the patient properly hydrated, with the healthcare provider’s order
be readily accessible at the pa- such as with I.V. fluids. If the to ensure the cuff hasn’t herniated
tient’s bedside.) patient demonstrates signs and over the tip of the tube, obstruct-
To recognize an obstructed tra- symptoms of respiratory distress, ing it. Attempt to pass a suction
cheostomy tube, closely monitor suction the tracheostomy tube to catheter through the tube again; if
www.Nursing2010.com January | Nursing2010 | 49
you feel resistance, the tube is show if it’s kinked, and a new tube Resizing of the tracheostomy tube
still obstructed and cuff hernia- is inserted. is required for the tube to be
tion isn’t the problem.3 • a displaced tracheostomy tube. securely placed in the trachea
• tracheostomy tube bevel resting A tracheostomy tube may be dis- having bypassed the pocket, fis-
against the tracheal wall. If the dis- placed in subcutaneous tissue, a tula, or blind pouch.2
tal tube lumen rests against the tracheoesophageal fistula, or an
tracheal wall, the patient’s respira- abnormal anatomical tissue Prevention and aftercare
tory status will slowly deteriorate. pocket. If the upper airway is The best way to prevent an ob-
Bag-mask ventilation will become patent, the patient can breathe struction from occurring is to
increasingly difficult with in- and may show minimal signs and monitor the patient closely. Know
creased resistance to bag compres- symptoms of respiratory compro- the type of tracheostomy tube
sion. A chest X-ray is performed mise, such as mild tachypnea.6 If that’s in place and the possible
to identify tube placement. If the the upper airway isn’t patent, the risks associated with the tube.
tube is against the tracheal side- patient will demonstrate signs Check for thick, viscous, and dry
wall, it’s removed and another in- and symptoms of respiratory sputum, and keep the patient hy-
serted 2 to 3 cm above the carina compromise and requires imme- drated. If the patient has abnormal
and centered in the trachea.2 A diate attention. You may identify breath sounds or a weak cough,
patient with a long neck, tracheal a displaced tube when passing be prepared to prevent or manage
stenosis, or tracheomalacia (an the suction catheter into the tra- the potential obstruction.
abnormal collapse of the tracheal cheostomy tube. If you feel resis- After an obstruction has been
wall) is a candidate for a tra- tance at 7 to 8 cm and obtain resolved, monitor the patient close-
cheostomy tube with a longer dis- minimal sputum, suspect a dis- ly for excess respiratory secretions.
tal vertical extension to prevent placed tube. Also be suspicious if Assist with airway clearance and
recurrence.2 the patient can speak clearly with suction, and be sensitive to any tis-
• a kinked tracheostomy tube. This an unplugged tracheostomy tube; sue edema that may have devel-
may occur during postoperative re- a displaced tube may allow the oped. Monitor the patient’s oxygen
covery in patients with long tra- patient’s exhalations of air to pass saturation, maintaining a satura-
cheostomy tubes.5 When the tube by the vocal cords, producing tion level of 92% or above. As the
is inserted and locked in place at speech. If the tracheostomy tube patient recovers and is getting
the tracheal faceplate, it can be- is correctly placed in the trachea, ready for discharge, provide the
come kinked because it can’t move the patient can’t speak without patient and caregivers with infor-
in either direction. The patient will plugging the tracheostomy tube mation about proper tracheostomy
experience severe respiratory com- because exhaled air exits through care to prevent tracheostomy tube
promise, but a bronchodilator isn’t the tracheostomy tube and doesn’t obstruction at home. Teach the
effective and a chest X-ray appears reach the vocal cords.6 An X-ray patient the signs and symptoms of
normal. Removal of the tube will is performed to confirm placement. a dried mucous plug and how to
prevent one from occurring. ■
Be prepared!
REFERENCES
To be ready for an airway emergency, make sure the following equipment is
1. Kapadia FN. Factors associated with blocked
available at the patient’s bedside: tracheal tubes. Intensive Care Med. 2001;27(10):
• a duplicate tracheostomy tube (the same size and type as the one the patient 1679-1681.
has in place) and another tube made by the same manufacturer that’s one size 2. St. John JE, Malen JF. Contemporary issues
smaller in adult tracheostomy management. Crit Care
Nurs Clin North Am. 2004;16(3):413-430.
• a manual resuscitation bag and oxygen source
3. Regan EN, Dallachiesa L. How to care for a
• suction source and suction equipment, including suction catheters that are half patient with a tracheostomy. Nursing. 2009;
the size of the tracheostomy tube 39(8):34-39.
• large diameter or tonsil-tip suction catheter 4. Saini S, Taxak S, Singh MR. Tracheostomy
tube obstruction caused by an overinflated
• small diameter suction catheters that will fit into the tracheostomy tube
cuff. Otolaryngol Head Neck Surg. 2000;122(5):
• tracheostomy tube obturator 768-769.
• water-soluble lubricant 5. Sharma A, Elliot S, Mallick A. Kinking of a
• tracheostomy insertion tray long tracheostomy tube can present as severe
acute asthma. Anaesthesia. 2002;57(12):1238-
• 10-mL syringe (for a cuffed tube) 1240.
• tracheostomy tube securement device 6. Seay SJ, Gay SL, Strauss M. Tracheostomy
• tracheostomy collar with heated or room temperature humidity emergencies. Am J Nurs. 2002;102(3):59, 61, 63.
• inner cannula cleaning materials.2 Joan Webber-Jones is a nurse educator at Fletcher
Allen Health Care in Burlington, Vt.
50 | Nursing2010 | January www.Nursing2010.com
Vous aimerez peut-être aussi
- Shoe Dog: A Memoir by the Creator of NikeD'EverandShoe Dog: A Memoir by the Creator of NikeÉvaluation : 4.5 sur 5 étoiles4.5/5 (537)
- Test ScienceDocument2 pagesTest Sciencejam syPas encore d'évaluation
- The Yellow House: A Memoir (2019 National Book Award Winner)D'EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Évaluation : 4 sur 5 étoiles4/5 (98)
- Review1 ScheduleDocument3 pagesReview1 Schedulejayasuryam.ae18Pas encore d'évaluation
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeD'EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeÉvaluation : 4 sur 5 étoiles4/5 (5794)
- Ito Na Talaga Yung FinalDocument22 pagesIto Na Talaga Yung FinalJonas Gian Miguel MadarangPas encore d'évaluation
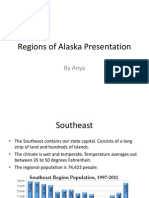
- Regions of Alaska PresentationDocument15 pagesRegions of Alaska Presentationapi-260890532Pas encore d'évaluation
- The Little Book of Hygge: Danish Secrets to Happy LivingD'EverandThe Little Book of Hygge: Danish Secrets to Happy LivingÉvaluation : 3.5 sur 5 étoiles3.5/5 (400)
- CEE Annual Report 2018Document100 pagesCEE Annual Report 2018BusinessTech100% (1)
- Grit: The Power of Passion and PerseveranceD'EverandGrit: The Power of Passion and PerseveranceÉvaluation : 4 sur 5 étoiles4/5 (588)
- Financial Accounting 2 SummaryDocument10 pagesFinancial Accounting 2 SummaryChoong Xin WeiPas encore d'évaluation
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureD'EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureÉvaluation : 4.5 sur 5 étoiles4.5/5 (474)
- Oracle Forms & Reports 12.2.1.2.0 - Create and Configure On The OEL 7Document50 pagesOracle Forms & Reports 12.2.1.2.0 - Create and Configure On The OEL 7Mario Vilchis Esquivel100% (1)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryD'EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryÉvaluation : 3.5 sur 5 étoiles3.5/5 (231)
- Borang Ambulans CallDocument2 pagesBorang Ambulans Callleo89azman100% (1)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceD'EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceÉvaluation : 4 sur 5 étoiles4/5 (895)
- Chemistry: Crash Course For JEE Main 2020Document18 pagesChemistry: Crash Course For JEE Main 2020Sanjeeb KumarPas encore d'évaluation
- Team of Rivals: The Political Genius of Abraham LincolnD'EverandTeam of Rivals: The Political Genius of Abraham LincolnÉvaluation : 4.5 sur 5 étoiles4.5/5 (234)
- Introduction-: Microprocessor 68000Document13 pagesIntroduction-: Microprocessor 68000margyaPas encore d'évaluation
- Never Split the Difference: Negotiating As If Your Life Depended On ItD'EverandNever Split the Difference: Negotiating As If Your Life Depended On ItÉvaluation : 4.5 sur 5 étoiles4.5/5 (838)
- Waterstop TechnologyDocument69 pagesWaterstop TechnologygertjaniPas encore d'évaluation
- The Emperor of All Maladies: A Biography of CancerD'EverandThe Emperor of All Maladies: A Biography of CancerÉvaluation : 4.5 sur 5 étoiles4.5/5 (271)
- Chapter 1 To 5 For Printing.2Document86 pagesChapter 1 To 5 For Printing.2Senku ishigamiPas encore d'évaluation
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaD'EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaÉvaluation : 4.5 sur 5 étoiles4.5/5 (266)
- Iec TR 61010-3-020-1999Document76 pagesIec TR 61010-3-020-1999Vasko MandilPas encore d'évaluation
- On Fire: The (Burning) Case for a Green New DealD'EverandOn Fire: The (Burning) Case for a Green New DealÉvaluation : 4 sur 5 étoiles4/5 (74)
- Playful Homeschool Planner - FULLDocument13 pagesPlayful Homeschool Planner - FULLamandalecuyer88Pas encore d'évaluation
- Arens - Auditing and Assurance Services 15e-2Document17 pagesArens - Auditing and Assurance Services 15e-2Magdaline ChuaPas encore d'évaluation
- The Unwinding: An Inner History of the New AmericaD'EverandThe Unwinding: An Inner History of the New AmericaÉvaluation : 4 sur 5 étoiles4/5 (45)
- Methods of Recording Retruded Contact Position in Dentate PatientsDocument15 pagesMethods of Recording Retruded Contact Position in Dentate PatientsYossr MokhtarPas encore d'évaluation
- Chapter 1 ClassnotesDocument35 pagesChapter 1 ClassnotesAllison CasoPas encore d'évaluation
- Problem Set-02Document2 pagesProblem Set-02linn.pa.pa.khaing.2020.2021.fbPas encore d'évaluation
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersD'EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersÉvaluation : 4.5 sur 5 étoiles4.5/5 (345)
- ReadmeDocument3 pagesReadmedhgdhdjhsPas encore d'évaluation
- Theories of International InvestmentDocument2 pagesTheories of International InvestmentSamish DhakalPas encore d'évaluation
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyD'EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyÉvaluation : 3.5 sur 5 étoiles3.5/5 (2259)
- DPSD ProjectDocument30 pagesDPSD ProjectSri NidhiPas encore d'évaluation
- The Homework Song FunnyDocument5 pagesThe Homework Song Funnyers57e8s100% (1)
- LEIA Home Lifts Guide FNLDocument5 pagesLEIA Home Lifts Guide FNLTejinder SinghPas encore d'évaluation
- SimovertDocument41 pagesSimovertRamez YassaPas encore d'évaluation
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreD'EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreÉvaluation : 4 sur 5 étoiles4/5 (1090)
- Objective & Scope of ProjectDocument8 pagesObjective & Scope of ProjectPraveen SehgalPas encore d'évaluation
- 8.ZXSDR B8200 (L200) Principle and Hardware Structure Training Manual-45Document45 pages8.ZXSDR B8200 (L200) Principle and Hardware Structure Training Manual-45mehdi_mehdiPas encore d'évaluation
- Psychological Contract Rousseau PDFDocument9 pagesPsychological Contract Rousseau PDFSandy KhanPas encore d'évaluation
- Hole CapacityDocument2 pagesHole CapacityAbdul Hameed OmarPas encore d'évaluation
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)D'EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Évaluation : 4.5 sur 5 étoiles4.5/5 (121)
- Elements of ArtDocument1 pageElements of Artsamson8cindy8louPas encore d'évaluation
- History of The Sikhs by Major Henry Cour PDFDocument338 pagesHistory of The Sikhs by Major Henry Cour PDFDr. Kamalroop SinghPas encore d'évaluation
- Her Body and Other Parties: StoriesD'EverandHer Body and Other Parties: StoriesÉvaluation : 4 sur 5 étoiles4/5 (821)